Organization (PPO) Dental - United Concordia
Organization (PPO) Dental - United Concordia
Organization (PPO) Dental - United Concordia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume<br />
UNITED CONCORDIA COMPANIES, INC.<br />
America’s Premier <strong>Dental</strong> Insurer<br />
Preferred Provider<br />
<strong>Organization</strong> (<strong>PPO</strong>)<br />
<strong>Dental</strong> Reference Guide
UNITED CONCORDIA COMPANIES, INC.<br />
<strong>PPO</strong> <strong>Dental</strong> Reference Guide<br />
Corporate Headquarters<br />
4401 Deer Path Road, Harrisburg, PA 17110<br />
Phone 800.332.0366 • www.unitedconcordia.com
UNITED CONCORDIA COMPANIES, INC<br />
<strong>PPO</strong> DENTAL REFERENCE GUIDE<br />
TABLE OF CONTENTS<br />
SECTION 1 – SU<strong>PPO</strong>RT SERVICES<br />
<strong>Dental</strong> Professional Relations Representatives.............................................................. 1.1<br />
Communication Sources.................................................................................................... 1.1<br />
<strong>Dental</strong> Customer Service Representatives ...................................................................... 1.1<br />
Interactive Voice Response (IVR) System...................................................................... 1.2<br />
My Patients’ Benefits.......................................................................................................... 1.2<br />
Provider Reference Guide................................................................................................. 1.2<br />
Dentist Advisors ................................................................................................................. 1.3<br />
Provider Newsletter............................................................................................................ 1.3<br />
Special Mailings ................................................................................................................... 1.3<br />
Internet ................................................................................................................................. 1.3<br />
Mailing Addresses for Claim Submission ....................................................................... 1.4<br />
Mailing Addresses for Inquiries........................................................................................ 1.4<br />
Telephone Numbers........................................................................................................... 1.5<br />
Special Account Support ................................................................................................... 1.5<br />
SECTION 2 – AUTOMATED SERVICES<br />
My Patients’ Benefits.......................................................................................................... 2.1<br />
Interactive Voice Response (IVR) System...................................................................... 2.2<br />
SECTION 3 – OUR PRODUCT PORTFOLIO<br />
<strong>Concordia</strong> Flex .................................................................................................................... 3.1<br />
<strong>Concordia</strong> Choice/<strong>Concordia</strong> Select............................................................................... 3.1<br />
<strong>Concordia</strong> Access................................................................................................................ 3.2<br />
<strong>Concordia</strong> Preferred........................................................................................................... 3.2<br />
<strong>Concordia</strong> EPO................................................................................................................... 3.2<br />
<strong>Concordia</strong> Plus .................................................................................................................... 3.2<br />
SECTION 4 – UNITED CONCORDIA NETWORKS<br />
<strong>Concordia</strong> Advantage......................................................................................................... 4.1<br />
National Fee-for-Service.................................................................................................... 4.1<br />
<strong>Concordia</strong> Advantage Plus................................................................................................. 4.2<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
<strong>Concordia</strong> Access................................................................................................................ 4.2<br />
SECTION 5 – PARTICIPATING WITH UNITED CONCORDIA<br />
Advantages of Participation .............................................................................................. 5.1<br />
How to Become a Participating Dentist.......................................................................... 5.2<br />
How Individual Provider Identification Numbers are Established............................ 5.3<br />
Group Practice .................................................................................................................... 5.3<br />
How to Form a Group Practice ....................................................................................... 5.3<br />
Changes In Group Practice Membership ....................................................................... 5.4<br />
Maintaining Provider Data ................................................................................................ 5.4<br />
Where to Send Notification of Change(s) ...................................................................... 5.5<br />
How to Resign from Participation................................................................................... 5.5<br />
Non-Participating Dentists................................................................................................ 5.5<br />
Example: Request for <strong>Dental</strong> Group Account (form 5565)<br />
Example: Request for Addition and/or Deletion of a Participating Provider(s)<br />
Identification Number to an Existing Group Account (form 5704)<br />
SECTION 6 – POLICIES, LIMITATIONS AND EXCLUSIONS<br />
General Policies................................................................................................................... 6.2<br />
Policies and Limitations<br />
Diagnostic Procedures ........................................................................................ 6.3<br />
Preventive Procedures......................................................................................... 6.4<br />
Restorative Procedures........................................................................................ 6.5<br />
Crowns, Inlays and Onlays................................................................................. 6.7<br />
Endodontic Procedures ...................................................................................... 6.9<br />
Periodontal Procedures ....................................................................................6.10<br />
Removable Prosthetic Procedures .................................................................6.12<br />
Fixed Prosthetic Procedures ............................................................................6.13<br />
Oral Surgery Procedures ..................................................................................6.14<br />
Palliative Emergency Treatment......................................................................6.15<br />
Anesthesia ...........................................................................................................6.16<br />
Position Statements ..........................................................................................................6.16<br />
Placement of Restorations................................................................................6.16<br />
Overhead Expenses...........................................................................................6.17<br />
Amalgam..............................................................................................................6.17<br />
Procedure Code Reporting Chart....................................................................6.18<br />
Diagnostic Material Requirements Chart.......................................................6.28<br />
SECTION 7 – CLAIM SUBMISSION GUIDELINES<br />
Completing the Claim Form ............................................................................................. 7.1<br />
Claim Filing Deadline......................................................................................................... 7.4<br />
Contract ID Number ......................................................................................................... 7.4<br />
Signature Requirements ..................................................................................................... 7.5<br />
Treatment Plan /Release of Information........................................................................ 7.5<br />
Assignment of Benefits...................................................................................................... 7.5<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Dentist’s Signature.............................................................................................................. 7.5<br />
Supporting Documentation............................................................................................... 7.6<br />
Other Supporting Documentation................................................................................... 7.6<br />
Third Party Liability (TPL)................................................................................................ 7.7<br />
Requesting Predeterminations .......................................................................................... 7.7<br />
Predetermination and Coordination of Benefits............................................................ 7.8<br />
Orthodontic Services.......................................................................................................... 7.8<br />
Policies and Limitations for Orthodontic Procedures.................................................. 7.9<br />
Payment for Orthodontic Services................................................................................... 7.9<br />
Orthodontic Lifetime Maximum....................................................................................7.10<br />
Orthodontic Treatment “In-Progress” .........................................................................7.10<br />
Billing Orthodontic Services ...........................................................................................7.12<br />
Billing for New Orthodontic Patients ...........................................................................7.12<br />
How to Complete a <strong>Dental</strong> Claim Form for New Orthodontic Patients................7.12<br />
Billing for a Patient Whose Orthodontic Treatment “In-Progress” Has Not<br />
Been Previously Paid by Another Insurance Carrier...................................................7.13<br />
Orthodontic Inquiries ......................................................................................................7.14<br />
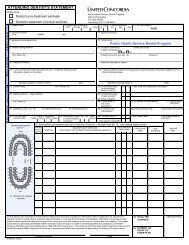
Example: Standard Claim Form<br />
SECTION 8 – ELECTRONIC CLAIM SUBMISSION<br />
Xpress Claim ......................................................................................................................... 8.1<br />
Electronic Data Interchange (EDI)................................................................................. 8.1<br />
Benefits of Submitting Claims Electronically................................................................. 8.2<br />
How to Submit Claims Requiring Attachments ............................................................ 8.2<br />
Reports.................................................................................................................................. 8.3<br />
997 Functional Acknowledgement Report...................................................... 8.3<br />
277 CA Claims Acknowledgement Report...................................................... 8.3<br />
835 Healthcare Claim Payment/Advice Report ............................................. 8.4<br />
SECTION 9 – COORDINATION OF BENEFITS<br />
Determining the Primary Plan.......................................................................................... 9.1<br />
Payment When UCCI Is Primary..................................................................................... 9.2<br />
Payment When UCCI Is Secondary .............................................................................. 9.2<br />
SECTION 10 – CLAIM REVIEW PROCESS<br />
Initial Review .....................................................................................................................10.1<br />
Professional Review by Dentist Advisors.....................................................................10.1<br />
Second Review ..................................................................................................................10.2<br />
SECTION 11 – PAYMENTS AND REQUESTS FOR INFORMATION<br />
<strong>Dental</strong> Explanation of Benefits (DEOB) .....................................................................11.1<br />
How to Read the DEOB.................................................................................................11.1<br />
Request for Additional Information..............................................................................11.3<br />
Changing or Combining Reported Procedure Codes .................................................11.3<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Example: Summary Payment Voucher – <strong>Dental</strong> Explanation of Benefits (DEOB)<br />
SECTION 12 – APPEALS<br />
Initial Processing...............................................................................................................12.1<br />
Second Review/Appeal....................................................................................................12.1<br />
What May Not Be Reviewed/Appealed........................................................................12.2<br />
How to Request a Second Review/Appeal ..................................................................12.2<br />
SECTION 13 – BENEFIT SAFEGUARDS<br />
Utilization Review (UR)...................................................................................................13.1<br />
Data Collection and Statistical Analysis ........................................................................13.1<br />
The UR Process ................................................................................................................13.1<br />
Professional Consultant Reviews ...................................................................................13.2<br />
Follow-up Actions ............................................................................................................13.2<br />
Utilization Letters .............................................................................................................13.2<br />
The Special Investigation Unit (SIU).............................................................................13.2<br />
Regulatory Compliance....................................................................................................13.3<br />
Coding and Billing ............................................................................................................13.3<br />
Documentation .................................................................................................................13.3<br />
SECTION 14 – GLOSSARY OF TERMS<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Section<br />
SU<strong>PPO</strong>RT SERVICES<br />
<strong>Dental</strong> Professional Relations Representatives<br />
nited <strong>Concordia</strong> maintains a field staff of <strong>Dental</strong> Professional Relations Representatives who<br />
U<br />
are dedicated exclusively to assisting dentists and their staff in understanding the dental<br />
programs and products offered by <strong>United</strong> <strong>Concordia</strong>. <strong>Dental</strong> Professional Relations Representatives<br />
are available to answer policy questions, provide professional support, furnish information regarding<br />
the dental programs and products, and assist with problems that require more than a telephone call<br />
or letter to our Customer Service Department. Although these representatives can usually resolve a<br />
question or concern by telephone, they also visit dental offices to provide in-person support.<br />
Communication Sources<br />
nited <strong>Concordia</strong> is committed to providing accurate and timely information about our dental<br />
U<br />
programs, products, and policies to subscribers and treating dentists. To do this, we use a<br />
number of communication channels:<br />
ü <strong>Dental</strong> Customer Service Representatives<br />
ü Interactive Voice Response (IVR) System<br />
ü My Patients’ Benefits (formerly <strong>Dental</strong> Inquiry)<br />
ü <strong>Dental</strong> Reference Guide<br />
ü Dentist Advisors<br />
ü Provider Newsletter - Connection<br />
ü Special Mailings<br />
ü Internet web site: www.unitedconcordia.com<br />
<strong>Dental</strong> Customer Service Representatives<br />
nited <strong>Concordia</strong>’s <strong>Dental</strong> Customer Service Department consists of approximately 160<br />
U<br />
Customer Service personnel trained to assist in responding to inquiries about our dental<br />
programs and products.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
1.1
To contact Customer Service by email, complete the form accessible by clicking on Contact Us at the<br />
bottom of the Dentist page of our website. Or you may write to the <strong>Dental</strong> Customer Service<br />
Department at:<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
<strong>Dental</strong> Customer Service<br />
PO Box 69420<br />
Harrisburg, PA 17106-9420<br />
When contacting <strong>United</strong> <strong>Concordia</strong>, whether by email, telephone or letter, the following information<br />
is needed:<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Subscriber’s Name<br />
Subscriber’s Identification Number<br />
Patient’s Name<br />
Patient’s Date of Birth<br />
Claim or Inquiry Number, if applicable<br />
Dentist’s Identification Number (UCCI Provider Number)<br />
Interactive Voice Response (IVR) System<br />
VR is an automated Interactive Voice Response system available to provide patient eligibility and<br />
I<br />
benefits, claim status, orthodontic information, procedure history, maximum/deductible<br />
accumulations, co-payment listings, fee schedules and procedure allowances. You may also finalize<br />
predeterminations using the IVR system. A touch-tone telephone is required and an immediate<br />
response can be provided by telephone, fax and/or mail. The IVR system is available to respond to<br />
your inquiries 24 hours a day, 7 days a week, except when our databases are undergoing scheduled<br />
maintenance. IVR is available by dialing 1-800-332-0366. Refer to Automated Services section for<br />
more information.<br />
My Patients’ Benefits<br />
atient information such as eligibility, benefits, claim status, maximums/deductibles, procedure<br />
P<br />
history, procedure code information and allowances can be obtained through My Patients’<br />
Benefits, an electronic inquiry product offered by <strong>United</strong> <strong>Concordia</strong>. My Patients’ Benefits may be<br />
accessed through the Internet with a web browser of 5.0 or greater. This service is available 24 hours<br />
a day, 7 days a week, except when our databases are undergoing scheduled maintenance. Refer to<br />
Automated Services section for more information.<br />
<strong>Dental</strong> Reference Guide<br />
he <strong>Dental</strong> Reference Guide is developed by <strong>United</strong> <strong>Concordia</strong> to provide dental offices with<br />
T<br />
important information concerning <strong>United</strong> <strong>Concordia</strong>’s Fee for Service programs. This guide<br />
reviews the relevant policies; provides information concerning participation with <strong>United</strong> <strong>Concordia</strong><br />
and establishes the procedures to follow when submitting claims or seeking a review. This<br />
valuable reference tool is available to all dentists.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
1.2
Dentist Advisors<br />
hould you have questions concerning claims previously reviewed by a Dentist Advisor, please<br />
S<br />
contact us at 1-800-772-1133 between the hours of 8:00 a.m. and 4:15 p.m. Eastern Time. You<br />
may call us at this toll free number to:<br />
q<br />
q<br />
q<br />
Receive instructions for requesting an appeal.<br />
Obtain information pertaining to an Advisor determination.<br />
Make arrangements to discuss a claim with an Advisor.<br />
When writing to <strong>United</strong> <strong>Concordia</strong> to request or provide additional information on claims involving<br />
a Dentist Advisor review, send your request to:<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Dentist Advisor Review<br />
PO Box 69420<br />
Harrisburg, PA 17106-9420<br />
Provider Newsletter<br />
ne of the most important ways we communicate with dentists and their office staff is through<br />
O<br />
our newsletter, the Connection.<br />
This newsletter is designed to:<br />
q<br />
q<br />
q<br />
q<br />
Advise dental offices of new dental policies and procedures or changes to existing policies<br />
Present guidelines for accurate and timely claims submission<br />
Inform dentists and their staff of new benefits and guidelines, and<br />
Provide corporate updates<br />
The Connection is distributed to all participating dentists, and is considered official notification for<br />
policies and procedure changes.<br />
Special Mailings<br />
n addition to the Connection, <strong>United</strong> <strong>Concordia</strong> uses special mailings to inform dental offices of<br />
I<br />
significant changes in coverage, claim payment policies or procedures. Special mailings are used<br />
when we want to send information quickly or when the information is too complicated or lengthy to<br />
include in the Connection.<br />
Internet<br />
nited <strong>Concordia</strong>'s Internet Website, www.unitedconcordia.com, provides detailed information<br />
Uon<br />
certain Commercial Programs, Government Programs, Electronic Claims, Corporate<br />
Information, Automated Services, Press Releases and much more.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
1.3
Mailing Addresses for Claim Submission<br />
<strong>United</strong> <strong>Concordia</strong> and<br />
Highmark Blue Shield Claims ..............................................<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Claims Processing<br />
PO Box 69421<br />
Harrisburg, PA 17106-9421<br />
DentaBenefits (Mutual of Omaha) Claims........................DentaBenefits Claims Processing<br />
PO Box 69416<br />
Harrisburg, PA 17106-9416<br />
Mailing Addresses for Inquiries<br />
Routine Inquiries and Advisor<br />
Review Inquiries.......................................................................<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
<strong>Dental</strong> Customer Service<br />
PO Box 69420<br />
Harrisburg, PA 17106-9420<br />
<strong>Dental</strong> Electronic Services .....................................................<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
<strong>Dental</strong> Electronic Services<br />
PO Box 69408<br />
Harrisburg, PA 17106-9408<br />
Change in Provider Information...........................................<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Provider Data Management<br />
PO Box 69415<br />
Harrisburg, PA 17106-9415<br />
Refunds .......................................................................................<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Cashier<br />
PO Box 69402<br />
Harrisburg, PA 17106-9402<br />
Special Investigation Unit......................................................<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Special Investigations Unit<br />
4401 Deer Path Road, DP4F<br />
Harrisburg, PA 17110<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
1.4
Telephone Numbers<br />
<strong>Dental</strong> Customer Service .............................................1-800-332-0366<br />
<strong>Dental</strong> Customer Service Fax......................................1-717-260-7029<br />
<strong>Dental</strong> Customer Service (TDD)................................1-800-345-3837<br />
Dentist Advisor Unit ....................................................1-800-772-1133<br />
Changing Provider Information Fax ..........................1-717-260-6834<br />
Special Investigation Unit Fraud Hotline...................1-877-968-7455<br />
<strong>Dental</strong> Electronic Services...........................................1-800-633-5430<br />
Special Account Support<br />
AR Health Advantage/USAble/Blue Advantage .....1-800-746-5684<br />
Carnegie Mellon University (Faculty & Staff) ...........1-800-423-7461<br />
Catholic Health East*...................................................1-866-886-7981<br />
Chevron Texaco (FFS).................................................1-877-424-3876<br />
Chevron Texaco (DHMO) ..........................................1-877-889-6149<br />
City of San Diego..........................................................1-866-215-2358<br />
Exelon/PECO* ............................................................1-877-454-3833<br />
FEP (FFS only until 4:15pm) ......................................1-800-746-5687<br />
Hershey Foods ..............................................................1-800-682-2395<br />
Highmark Employees...................................................1-800-485-2889<br />
House of Representatives (Pennsylvania) ..................1-877-408-9690<br />
IBAC/Interagency Task Force (ITF) .........................1-888-898-0370<br />
LAUSD ..........................................................................1-866-291-2304<br />
Metro Goldwyn Mayer .................................................1-866-291-2304<br />
Mine Safety Appliance (MSA)* ...................................1-800-263-1222<br />
Penn State University (PSU)........................................1-800-423-8217<br />
QVC ...............................................................................1-800-746-5681<br />
Rentway .........................................................................1-877-527-4782<br />
Sound (The) Partnership..............................................1-866-850-8791<br />
State of Maryland* ........................................................1-888-638-3384<br />
University of Pittsburgh*.............................................1-877-215-3616<br />
YMCA (Metro Los Angeles)........................................1-866-291-2304<br />
* These groups consist of Fee-for-Service and DHMO contracts. Please verify contract type prior to<br />
contacting customer service.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
1.5
Section<br />
AUTOMATED SERVICES<br />
My Patients’ Benefits<br />
U<br />
q<br />
nited <strong>Concordia</strong> provides direct, up-to-the-minute access to member information on our<br />
website. With My Patients’ Benefits, you have on-line access to the following information:<br />
Eligibility: Provides membership information including effective dates, types of plans and<br />
cancellation dates.<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Benefits: Gives detailed information on a patient's benefits and limitations.<br />
Claim Status: Determines if a claim is still in process or has finalized. If the claim has finalized,<br />
the check number, amount, date, and payee will be displayed. You can determine what<br />
maximums, deductibles or coinsurances have been applied. If a claim is rejected, a rejection<br />
description is provided.<br />
Maximum/Deductible: Gives maximum and deductible calculations and thresholds applicable<br />
to the patient.<br />
Procedure History: Lets you determine specific services that are on record at <strong>United</strong><br />
<strong>Concordia</strong> for a particular patient and the dates they were last provided.<br />
Allowance Information: Provides access to the Maximum Allowable Charge (MAC) Schedules.<br />
Procedure Code Information: Gives instant access to procedure code descriptions, valid place<br />
of service, tooth related information, radiograph requirements and appropriate benefit categories<br />
for coverage.<br />
Access our website to register for My Patients’ Benefits. On-line access to My Patients’ Benefits<br />
using your computer is available 24 hours a day, 7 days a week.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
2.1
Interactive Voice Response (IVR) System<br />
U<br />
nited <strong>Concordia</strong>'s <strong>Dental</strong> Customer Service IVR System offers dentists and most subscribers<br />
access to information stored in <strong>United</strong> <strong>Concordia</strong>'s records via the telephone and the capability<br />
of finalizing predeterminations for payment. You can choose to listen to the information or in most<br />
instances, request the information by fax or mail.<br />
The IVR System connects you directly to our databases and gives you access to:<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Patient eligibility and benefits<br />
Claim/predetermination status information<br />
Orthodontic information<br />
Procedure history<br />
Maximum/deductible accumulations<br />
Co-payment listings<br />
Fee schedules<br />
Procedure allowances<br />
The IVR System is accessible through <strong>United</strong> <strong>Concordia</strong>’s toll-free Customer Service number at 1-<br />
800-332-0366. The IVR system is available 24 hours a day, 7 days a week, except when our databases<br />
are undergoing scheduled maintenance.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
2.2
Section<br />
OUR PRODUCT PORTFOLIO<br />
U<br />
nited <strong>Concordia</strong> offers a diverse selection of fee-for-service plan designs for our members.<br />
Product Type Available<br />
Networks<br />
Key Features and Benefits<br />
<strong>Concordia</strong><br />
Flex<br />
Indemnity<br />
• Not Applicable<br />
(no network)<br />
• Maximum freedom of provider choice.<br />
• Claims reimbursed at 80th or 90th percentile of<br />
<strong>United</strong> <strong>Concordia</strong> (UC) charge data regardless of<br />
the dentist selected; dentists can balance bill.<br />
<strong>Concordia</strong><br />
Flex<br />
Passive<br />
<strong>PPO</strong><br />
• National Fee<br />
for Service<br />
• <strong>Concordia</strong><br />
Advantage<br />
• <strong>Concordia</strong><br />
Advantage Plus<br />
• Paid-in-full benefits (minus applicable coinsurance<br />
and deductibles) when a participating<br />
dentist provides services.<br />
• Freedom to choose any dentist to provide care;<br />
however, member savings are maximized when<br />
selecting a participating dentist.<br />
• Full range of insured dental benefits with standard<br />
benefit options.<br />
• Typical co-insurance coverage: 100% preventive,<br />
80% basic, 50% major<br />
<strong>Concordia</strong><br />
Choice<br />
or<br />
<strong>Concordia</strong><br />
Select<br />
Passive<br />
<strong>PPO</strong><br />
• <strong>Concordia</strong><br />
Advantage<br />
• <strong>Concordia</strong><br />
Advantage Plus<br />
• Affordable voluntary dental plan (no employer<br />
contribution to premium required).<br />
• Waiting periods for basic and major services.<br />
• Optional orthodontic coverage.<br />
• Discount vision plan from Davis Vision included<br />
with all plans.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
3.1
Product Type Available<br />
Networks<br />
Key Features and Benefits<br />
<strong>Concordia</strong><br />
Access<br />
Hybrid:<br />
Passive<br />
<strong>PPO</strong> and<br />
Discounts<br />
• <strong>Concordia</strong><br />
Access<br />
• Paid-in-full preventive care from participating<br />
dentists.<br />
• Discounted basic and/or major services from<br />
participating dentists.<br />
• No claims filings required for discounted services.<br />
• Member pays discounted services directly to<br />
dentist.<br />
<strong>Concordia</strong><br />
Preferred<br />
Active <strong>PPO</strong><br />
• <strong>Concordia</strong><br />
Advantage<br />
• <strong>Concordia</strong><br />
Advantage Plus<br />
• Out-of-network benefits less than in-network.<br />
• Member savings are maximized when selecting a<br />
participating dentist.<br />
• Full range of in-network dental benefits with<br />
standard benefit options.<br />
<strong>Concordia</strong><br />
EPO<br />
Active <strong>PPO</strong><br />
• <strong>Concordia</strong><br />
Advantage<br />
• Copayment schedule limits members’ out of<br />
pocket expenses.<br />
(regional network)<br />
• Larger network of dentists than a DHMO.<br />
• No referrals or coordination of care.<br />
• No out-of-network benefits.<br />
<strong>Concordia</strong><br />
Plus<br />
DHMO<br />
• <strong>Concordia</strong> Plus<br />
(regional<br />
network)<br />
• Emphasis on preventive treatment and high<br />
quality care.<br />
• Copayment schedule limits patient’s out of pocket<br />
expenses.<br />
• Uses a capitated general dentist and specialty<br />
network.<br />
• No out-of-network benefits.<br />
This publication is not a solicitation of coverage. Not all products are currently available on an insured<br />
basis for employers/groups in all states. Refer to our website and view the Regulatory Information to<br />
learn more.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
3.2
Section<br />
UNITED CONCORDIA NETWORKS<br />
T<br />
he success of <strong>United</strong> <strong>Concordia</strong> is based primarily on our ability to provide access to care<br />
through our network of participating dentists. Our network strategy provides two Preferred<br />
Provider <strong>Organization</strong> programs for participation. The National Fee-for-Service (NFFS) Network is<br />
our original and longstanding traditional network. <strong>Concordia</strong> Advantage, introduced in 2001, is an<br />
integration of our NFFS and ParNet Networks. <strong>Concordia</strong> Advantage Plus, introduced in 2003, is a<br />
blending of our <strong>Concordia</strong> Advantage and NFFS Networks to provide optimal access for our<br />
members.<br />
To confirm your participation status, you may access the <strong>United</strong> <strong>Concordia</strong> Provider Directory on<br />
our website or by calling 1-800-332-0366.<br />
The following information is not to be considered a solicitation for participation.<br />
<strong>Concordia</strong> Advantage<br />
oncordia Advantage is available for most <strong>United</strong> <strong>Concordia</strong> fee-for-service or <strong>PPO</strong> products.<br />
C<br />
Members using this network may choose from more than 45,000 dentists at over 60,000<br />
locations across the nation. The <strong>Concordia</strong> Advantage Network consists of ParNet providers in<br />
major metropolitan areas and NFFS providers in other locations.<br />
ParNet dentists are automatically considered part of the <strong>Concordia</strong> Advantage Network. No<br />
additional paperwork is necessary. If you participate in the NFFS Network, depending on your<br />
primary office location, you may also be considered part of the <strong>Concordia</strong> Advantage Network.<br />
National Fee-for-Service<br />
nited <strong>Concordia</strong>’s NFFS Network is one of the nation’s largest, with more than 56,000 dentists<br />
U<br />
at over 74,000 locations within the continental <strong>United</strong> States, Puerto Rico, Guam and the<br />
Virgin Islands. This network is also used to administer the world’s largest dental contract, the<br />
TRICARE <strong>Dental</strong> Program (TDP), plus many local and national commercial accounts.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
4.1
<strong>Concordia</strong> Advantage Plus<br />
nited <strong>Concordia</strong>’s Advantage Plus is a blend of our networks that support our fee-for-service or<br />
U<br />
<strong>PPO</strong> products. Advantage Plus provides our members with access to more than 63,000 dentists<br />
at over 82,000 locations within the continental <strong>United</strong> States, Puerto Rico, Guam and the Virgin<br />
Islands.<br />
<strong>Concordia</strong> Access<br />
nited <strong>Concordia</strong>’s <strong>Concordia</strong> Access Network supports the <strong>Concordia</strong> Access hybrid product<br />
U<br />
introduced in 2003, and combines the best of insured and discount-only dental plans to provide<br />
affordable benefits and access to groups who are in need of a lower-cost option.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
4.2
Section<br />
PARTICIPATING WITH UNITED<br />
CONCORDIA<br />
E<br />
nrollees may receive dental care from any licensed dentist of their choice. However, members<br />
are encouraged to visit the offices of participating dentists with the understanding that it will<br />
save them time, paperwork and money.<br />
A licensed dentist who is not currently excluded, sanctioned or suspended by your licensing<br />
authority, is eligible to become a <strong>United</strong> <strong>Concordia</strong> participating dentist. Participating dentists agree<br />
to accept <strong>United</strong> <strong>Concordia</strong>’s allowance as payment in full for covered services, collect patient cost<br />
shares and submit claims to <strong>United</strong> <strong>Concordia</strong> on behalf of <strong>United</strong> <strong>Concordia</strong> members.<br />
Advantages of Participation<br />
articipating dentists are an important part of the <strong>United</strong> <strong>Concordia</strong> network. There are<br />
P<br />
participating dentists in every clinical specialty, and in all 50 <strong>United</strong> States, the District of<br />
Columbia, Guam, Puerto Rico, and the U.S. Virgin Islands. <strong>United</strong> <strong>Concordia</strong> is dedicated to<br />
fostering a mutually beneficial relationship with participating dentists by offering the following<br />
business incentives:<br />
1. All payments for services are mailed directly to participating dentists.<br />
2. Names, addresses, and phone numbers of participating dentists are regularly made<br />
available to all members on our website.<br />
3. Participating dentists servicing our members receive <strong>United</strong> <strong>Concordia</strong>'s quarterly<br />
newsletter.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
5.1
4. Participating dentists servicing our members will receive the Reference Guide and any<br />
subsequent updates.<br />
5. Participating dentists may be eligible to participate in the HONORS program. This<br />
program recognizes participating dentists who consistently provide cost-effective care to<br />
our customers by relaxing the requirement for radiograph submissions and other clinical<br />
documentation.<br />
How to Become a Participating Dentist<br />
T<br />
o be eligible to participate in <strong>United</strong> <strong>Concordia</strong>’s <strong>PPO</strong> networks a dentist must:<br />
1. Demonstrate a Utilization Review Pattern acceptable to <strong>United</strong> <strong>Concordia</strong>;<br />
2. Complete a <strong>United</strong> <strong>Concordia</strong> Credentialing Application (the law requires dentists in<br />
certain states to submit a state specific application);<br />
3. Complete a signed Participating Dentist Agreement with <strong>United</strong> <strong>Concordia</strong> Companies,<br />
Inc. (the law requires dentists in certain states to submit a state specific agreement);<br />
4. Hold an active, valid license to practice dentistry in the state(s) in which he/she<br />
practices;<br />
5. Hold current professional liability insurance;<br />
6. Have no current sanction, termination or other peer review action by a professional<br />
review body; state dental board or Health and Human Service (HHS);<br />
7. Hold an active unrestricted federal Drug Enforcement Agency (DEA) certificate, if<br />
applicable.<br />
Any negative report on the attestation will be investigated. Additional information may be necessary<br />
in certain states due to state specific requirements.<br />
All paperwork and supporting documentation should be forwarded to:<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Provider Data Management<br />
P.O. Box 69415<br />
Harrisburg, PA 17106-9415<br />
Fax (717) 260-6834<br />
You will be notified in writing of your assigned provider number and effective date of participation.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
5.2
How Individual Provider Identification Numbers<br />
Are Established<br />
o payment can be made to you or your patient for eligible services until you have secured an<br />
N<br />
individual provider identification number. All dentists are assigned an individual provider<br />
identification number with <strong>United</strong> <strong>Concordia</strong> when the first claim is submitted and a copy of your<br />
valid dental license is received.<br />
If you would like to obtain a provider number and become a participating dentist, please refer to<br />
"How to Become a Participating Dentist" (page 5-2) for details. Upon approval, you will be<br />
notified of your status and provider number.<br />
Non-participating dentists may obtain a provider identification number by submitting a claim. The<br />
system will automatically generate a development letter with your assigned number, requesting a copy<br />
of your current dental license, tax document and verification of other pertinent provider information<br />
(i.e., address, telephone number). This letter and all the information requested should be returned to<br />
our office for processing and for final adjudication of the claim(s) within the designated timeframe.<br />
Group Practice<br />
he purpose of establishing a group practice is to permit two or more dentists to submit claims<br />
T<br />
and receive payment using one provider number. All payments will then be payable to the group<br />
practice and under the group practice tax identification number. The application for both the<br />
individual dentist and group account should be submitted concurrently.<br />
How to Form a Group Practice<br />
o form a group practice, these conditions must be met:<br />
T<br />
1. The billing entity must be arranged in the following manner:<br />
q<br />
Group Practice - Two or more dentists practicing as a group may establish a group<br />
practice to have the group recognized as a single entity for purposes of billing and<br />
payment. Examples of typical group practice arrangements are:<br />
A. Two or more dentists practicing as a partnership.<br />
B. A group of dentists forms a professional corporation and the corporation<br />
becomes the employer of the dentists.<br />
C. A dentist employs one or more other dentists as associates in his or her practice.<br />
2. All members of a group practice must be either participating or all members of the<br />
group practice must be non-participating with <strong>United</strong> <strong>Concordia</strong> in order to establish<br />
the group practice.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
5.3
3. To form a participating group, all required paperwork must be completed and submitted<br />
for each individual member concurrent with forming the group practice.<br />
To establish a group practice, please complete the Request for <strong>Dental</strong> Group Account Form<br />
(5565). Refer to a sample of Form 5565 at the end of this section. Completed forms should be<br />
returned to:<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Provider Data Management<br />
PO Box 69415<br />
Harrisburg, PA 17106-9415<br />
Or fax to (717) 260-6834<br />
Changes in Group Practice Membership<br />
ou must notify <strong>United</strong> <strong>Concordia</strong> in writing of any changes in the group’s personnel by<br />
Y<br />
completing the Group Account Change Form (5704). Refer to a sample of Form 5704 at the<br />
end of this section.<br />
When a new provider joins a participating group practice, the provider should complete an<br />
application and agreement, as well as Form 5704.<br />
When a provider leaves the group, please notify <strong>United</strong> <strong>Concordia</strong> of the dentist’s new address and<br />
current tax identification number (either an Employer Identification Number or Social Security<br />
Number, as appropriate) if known. Notifying <strong>United</strong> <strong>Concordia</strong> of a member no longer associated<br />
with the group will minimize inappropriate claims payment under the group’s Tax Identification<br />
Number.<br />
Maintaining Provider Data<br />
nited <strong>Concordia</strong> maintains a Provider Database, which contains pertinent information on all<br />
U<br />
individual dentists and group accounts who have submitted claims, or whose patients have<br />
submitted claims to <strong>United</strong> <strong>Concordia</strong>. Your record remains active on the provider database as long<br />
as you or your patients submit claims to <strong>United</strong> <strong>Concordia</strong> or until we receive notification of<br />
retirement, death, license suspension/revocation or HHS debarment.<br />
It is important that our provider database contains accurate information regarding your practice and<br />
group practice. <strong>United</strong> <strong>Concordia</strong> urges you to keep your provider information current by reporting<br />
any changes in writing. For security reasons, we strongly recommend these changes be verified by<br />
the dentist's signature appearing on the letter. Please report changes to any of the items listed below:<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Practice Name<br />
Address (physical location) of Practice<br />
Mailing Address (if different from above)<br />
Specialty<br />
Tax Identification Number<br />
Telephone Number<br />
Change in Group Practice<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
5.4
Keeping <strong>United</strong> <strong>Concordia</strong> informed of these changes will ensure timely delivery of checks and<br />
mailings.<br />
Where to Send Notification of Change(s)<br />
end written notification of any changes in your group practice or individual provider information<br />
S<br />
to:<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Provider Data Management<br />
P.O. Box 69415<br />
Harrisburg, PA 17106-9415<br />
Fax to (717) 260-6834<br />
How to Resign from Participation<br />
o resign from participation with <strong>United</strong> <strong>Concordia</strong>, you must send a signed, written statement to<br />
T<br />
the Provider Data Management Department at the previously specified address. You may<br />
submit a resignation at any time. Resignations are normally effective 60 days following the date<br />
<strong>United</strong> <strong>Concordia</strong> receives your letter, but may vary due to state specific mandates or regulations. A<br />
letter indicating the effective date of your resignation will be sent to you. When resigning an entire<br />
group, please include a resignation letter or signed document with each group members signature.<br />
Non-Participating Dentists<br />
on-participating dentists do not sign an agreement with <strong>United</strong> <strong>Concordia</strong> and, therefore, have<br />
N<br />
no contractual obligation to accept <strong>United</strong> <strong>Concordia</strong>’s fees as payment-in-full. However, nonparticipating<br />
dentists are required to accurately report services performed and fees charged. <strong>United</strong><br />
<strong>Concordia</strong> sends payment for covered services performed by non-participating dentists directly to<br />
the member, unless the member assigns payment to the non-participating dentist. Assignment of<br />
benefits is available on a state-by-state and contract basis.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
5.5
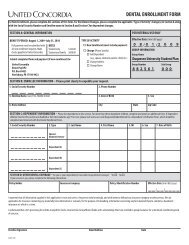
(AACOMB)<br />
REQUEST FOR DENTAL GROUP ACCOUNT<br />
Complete a separate form for each Practice Location.<br />
Name of Account<br />
Practice Address<br />
(P.O. Box Numbers<br />
will NOT be accepted)<br />
Mailing Address<br />
(If Applicable)<br />
Phone #<br />
FAX #<br />
THIS SECTION MUST BE COMPLETED<br />
IRS #<br />
Copy of notification or coupon from the IRS must be attached.<br />
Type of Corporation (check one): Professional Business Partnership<br />
NAME(S) OF DENTAL GROUP ACCOUNT MEMBERS<br />
DENTIST NAME (typed/printed)<br />
UCCI<br />
PROVIDER NO.<br />
(if known)<br />
SOCIAL SECURITY<br />
NUMBER<br />
SPECIALTY<br />
INDIVIDUAL DENTIST<br />
SIGNATURE (*)<br />
Please indicate the <strong>Dental</strong> Network(s) in which you wish to enroll*:<br />
UCCI-Parnet <strong>Concordia</strong> Preferred PaBS Penndental<br />
National Fee for Service/TDP<br />
(*) By my signature, I agree to abide by the <strong>Dental</strong> Group Account Agreement listed on the reverse side of this form.<br />
5565 E 12/02
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
<strong>Dental</strong> Group Account Agreement<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
7.<br />
8.<br />
We hereby agree that<br />
(Account Name)<br />
those services performed by the individual members of the Account.<br />
(the "Account") will bill only for<br />
We certify that the IRS Number given for the Account is the one assigned to the group. If<br />
this is not the case, we will identify the entity whose IRS Number is being used.<br />
We certify that each member of the Account agrees to assign his/her fee to the Account.<br />
We agree that every claim submitted for <strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
subscribers/beneficiaries will identify the individual provider who performed the service.<br />
We agree that the Account and each individual member will be jointly and severally liable<br />
for any overpayment that the Account may receive.<br />
We agree to notify <strong>United</strong> <strong>Concordia</strong> Companies, Inc. in writing of any subsequent changes<br />
in the membership of the Account prior to the effective date of each change.<br />
We agree to timely completion and return of the <strong>United</strong> <strong>Concordia</strong> Companies, Inc. <strong>Dental</strong><br />
Group Account Information Update form. This form will be mailed to the Account each<br />
year for verification of current Account membership, location of practice, specialties of<br />
member providers, and other pertinent information. We understand that failure to respond<br />
may result in the termination of the <strong>Dental</strong> Group Account.<br />
We have carefully reviewed the Request for <strong>Dental</strong> Group Account and <strong>Dental</strong> Group<br />
Account Agreement, and each member has verified the accuracy and completeness of all<br />
information provided.<br />
On behalf of the group, I verify that all members have reviewed this document and have<br />
authorized me to sign this Agreement on behalf of the Group.<br />
Signature of Authorized Representative of Group<br />
(Must be a Professional Member of this Account.)<br />
Date<br />
Title<br />
Area Code/Phone Number
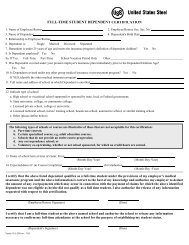
GROUP ACCOUNT CHANGE FORM<br />
(AAADDE)<br />
Request for Addition and/or Deletion of a Provider(s)<br />
Identification Number to an Existing Group Account<br />
Name of Account<br />
Account Number<br />
Practice Address<br />
Mailing Address<br />
IRS # Telephone # ( ) Specialty<br />
FAX # ( )<br />
DENTIST NAME<br />
(TYPED/PRINTED)<br />
UCCI<br />
PROVIDER<br />
NUMBER<br />
SOCIAL SECURITY<br />
NUMBER<br />
INDIVIDUAL DENTIST SIGNATURE<br />
(REQUIRED FOR ADDITIONS)<br />
ADDITION<br />
1<br />
DELETION<br />
2<br />
1<br />
2<br />
By my signature, I, as a member of this account, fully agree to abide by the Group Account requirements listed on the reserve side of this form.<br />
Deletions - Please provide the following information for providers being deleted from the Group Account.<br />
DENTIST NAME<br />
(TYPED/PRINTED)<br />
UCCI<br />
PROVIDER<br />
NUMBER<br />
NEW ADDRESS<br />
NEW<br />
TELEPHONE NUMBER<br />
5704 G 3/04<br />
(see reverse side)
<strong>United</strong> <strong>Concordia</strong> Companies<br />
<strong>Dental</strong> Group Account Agreement<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
7.<br />
8.<br />
We hereby agree that, (the "Account") will bill only for those services<br />
(Account Name)<br />
performed by the individual members of the Account.<br />
We certify that the IRS Number given for the Account is the one assigned to the group. If this is not the case, we will identify the entity<br />
whose IRS Number is being used.<br />
We certify that each member of the Account agrees to assign his/her fee to the Account.<br />
We agree that every claim submitted for <strong>United</strong> <strong>Concordia</strong> Companies subscribers/beneficiaries will identify the the individual provider<br />
who performed the service.<br />
We agree that the Account and each individual member will be jointly and severally liable for any overpayment that the Account may<br />
receive.<br />
We agree to notify <strong>United</strong> <strong>Concordia</strong> Companies in writing of any subsequent changes in the membership of the Account prior to the<br />
effective date of each change.<br />
We agree to timely completion and return of the <strong>United</strong> <strong>Concordia</strong> Companies <strong>Dental</strong> Group Account Information Update form. This<br />
form will be mailed to the Account each year for verification of current Account membership, location of practice, specialities of<br />
member providers, and other pertinent information. We understand that failure to respond may result in the termination of <strong>Dental</strong><br />
Group Account.<br />
We have carefully reviewed the Request for <strong>Dental</strong> Group Account and <strong>Dental</strong> Group Account Agreement, and each member has<br />
verified the accuracy and completeness of all information provided.<br />
On behalf of the group, I verify that all members have reviewed this document and have authorized me to sign this Agreement on behalf<br />
of the Group.<br />
Please mail completed forms to:<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Provider Data Management<br />
P.O. Box 69415<br />
Harrisburg, PA 17110<br />
Or<br />
Fax to Provider Data Management at (717) 260-6834
Section<br />
POLICIES, LIMITATIONS AND<br />
EXCLUSIONS<br />
U<br />
nited <strong>Concordia</strong>'s contracts with customers place limitations and exclusions on benefits. These<br />
exclusions and limitations may vary by state due to regulatory requirements and by group<br />
customer based on coverage purchased. A few of the common exclusions include charges for<br />
hospitalization costs, cosmetic services, treatment of TMD, treatment of malignancies or neoplasms,<br />
and house calls. Common limitations include one full mouth series of radiographs every five years<br />
and one prophylaxis every six months. These examples are not all-inclusive. If you would like to<br />
know the exclusions and limitations for particular group contracts under which your members are<br />
covered, you may use My Patients’ Benefits to obtain information specific to that contract.<br />
The policies and limitations listed within this section are used in administering dental benefits for<br />
standard fee for service dental programs. They reflect current and acceptable practices within the<br />
dental community while ensuring cost-effective measures are applied according to the dental<br />
contract. These policies do not apply to dental managed care programs or the TRICARE <strong>Dental</strong><br />
Program.<br />
Procedures should be reported using the American <strong>Dental</strong> Association’s current dental procedure<br />
codes and terminology. If a procedure code is not available to report a specific service, a complete<br />
description of the procedure provided, including applicable tooth numbers should be reported.<br />
Procedures that are an inherent part of another procedure are considered to be integral and not<br />
eligible for separate payment. Integral procedures are not billable to the member by a participating<br />
<strong>United</strong> <strong>Concordia</strong> dentist.<br />
<strong>Dental</strong> coverage varies by contract. To verify if a procedure is covered under a specific contract,<br />
please contact <strong>Dental</strong> Customer Service at the phone number listed on the member’s identification<br />
card.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.1
General Policies<br />
All covered procedures are subject to the following general policies:<br />
• Procedures must be necessary and meet accepted standards of dental practice. Procedures<br />
determined to be unnecessary or that do not meet accepted standards of practice are not billable<br />
to the member by a participating dentist, unless the dentist notifies the member of his/her<br />
liability prior to treatment and the member chooses to receive the treatment. Participating<br />
dentists should document such notification in their records.<br />
• Claims submitted for payment more than 12 months after the month in which a procedure is<br />
provided are not eligible for payment. A participating dentist may not bill the member for<br />
procedures that are denied for this reason.<br />
• Procedures, including evaluations, which are routinely provided in conjunction with, or as part of<br />
another procedure, are considered integral. Participating dentists may not bill members for<br />
procedures denied as integral to another procedure.<br />
• Participating dentists may not bill <strong>United</strong> <strong>Concordia</strong> or the member for the completion of claim<br />
forms and submission of required information for determination of benefits.<br />
• Infection control procedures and fees associated with Occupational Safety and Health<br />
Administration (OSHA) and/or other Governmental agency compliance are considered part of<br />
the dental procedures provided and may not be billed separately by a participating dentist.<br />
• Local anesthesia is considered integral to the procedure(s) for which it is provided.<br />
• For reporting and benefit purposes, the completion date for crowns, inlays, onlays, buildups,<br />
post and cores or fixed prostheses is the cementation date.<br />
• For reporting and benefit purposes, the completion date for removable prostheses is the<br />
insertion date.<br />
• For reporting and benefit purposes, the completion date for root canal therapy is the date the<br />
tooth is sealed.<br />
• For procedures specifically annotated in the procedure code nomenclature or descriptor as child<br />
or adult, a child will be considered any person 12 years of age or younger, and an adult will be<br />
considered any person 13 years of age or older.<br />
• An Alternate Benefit Provision (ABP) will be applied if a dental condition can be treated by<br />
means of a professionally acceptable procedure, which is less costly than the treatment<br />
recommended by the dentist. The ABP does not commit the member to the less costly<br />
treatment. However, if the member and dentist choose the more expensive treatment, the<br />
member is responsible for the additional charges beyond those allowed for the ABP. For<br />
example, an amalgam or resin restoration may be allowed in lieu of a crown, or a removable<br />
partial denture may be allowed in lieu of fixed partial dentures.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.2
• Implantology and all related procedures, including restoration of implants are not covered unless<br />
benefits are provided for under an implant rider.<br />
• The treatment of temporomandibular joint disorders (TMD/TMJ) is not covered unless benefits<br />
are provided for under a TMD rider.<br />
• Time limitations are applied based upon consecutive days, months or years.<br />
Policies and Limitations for Diagnostic<br />
Procedures<br />
• Periodic oral evaluations (D0120) are limited to one per six-month period.<br />
[This limitation may vary among states and group contracts.]<br />
• Comprehensive oral evaluations (D0150) are only covered if the member has not received<br />
another oral evaluation (D0120, D0150, D0160, D0180) within the previous 36 months from the<br />
same office.<br />
• Limited oral evaluations - problem focused (D0140) are limited to one per member, per dentist<br />
in a 12-month period. They are considered integral when provided on the same day, by the same<br />
dentist as another oral evaluation.<br />
• Detailed and extensive oral evaluations - problem focused (D0160) are only payable by report<br />
upon review by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor. They are limited to one per member, per<br />
dentist, per eligible diagnosis. They are not eligible if related to noncovered procedures such as<br />
TMD.<br />
• Detailed and extensive oral evaluations - problem focused are considered integral when provided<br />
on the same day, by the same dentist as definitive treatment or another oral evaluation.<br />
• Comprehensive periodontal evaluations (D0180) are limited to one per member, per dentist in a<br />
36-month period. They are considered integral when provided on the same day, by the same<br />
dentist as another oral evaluation.<br />
• Radiographs that are not of diagnostic quality are not covered and may not be charged to the<br />
member when provided by a participating dentist.<br />
• One full mouth radiograph (D0210 - complete series of radiographs or D0330 - panoramic<br />
radiograph) is covered in a five-year period.<br />
[This limitation may vary among states and group contracts.]<br />
• Panoramic and full mouth series radiographs are not routinely covered for members age four and<br />
younger unless member specific rationale (specific signs or symptoms) is submitted and<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.3
approved by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor. A fee cannot be charged to the member by a<br />
participating dentist.<br />
• Periapical or bitewing radiographs taken on the same day, by the same dentist as a full mouth<br />
series of radiographs are considered integral.<br />
• Periapical radiographs taken on the same day, by the same dentist as a panoramic radiograph are<br />
considered integral.<br />
• One set of bitewing radiographs, consisting of up to four bitewing radiographs per visit, is<br />
covered during a 12-month period for members age 14 and older. Two sets are allowed during a<br />
12-month period for members age 13 and younger.<br />
[This limitation may vary among states and group contracts.]<br />
• Vertical bitewings – 7 to 8 films (D0277) are paid at the same allowance as four bitewings and<br />
are subject to the same benefit limitations as four bitewing radiographs.<br />
• Cephalometric films (D0340) are limited to one per member, per lifetime.<br />
• Radiographs are not a covered benefit when taken by a radiograph laboratory, unless billed by a<br />
licensed dentist.<br />
• If the total allowance for individually reported periapicals, bitewings and/or occlusal radiographs<br />
equals or exceeds the allowance for a complete series, the individually reported radiographs are<br />
paid as a complete series and are subject to the same benefit limitations as a complete series. A<br />
participating dentist cannot charge the member the difference between the dentist’s charge for<br />
the individual radiographs and the amount paid by <strong>United</strong> <strong>Concordia</strong> for the complete series.<br />
• The radiograph taken to diagnose the need for root canal therapy is eligible for payment in<br />
addition to the root canal therapy. All other radiographs taken within 30 days of, and in<br />
conjunction with root canal therapy, including post-treatment radiographs are considered integral<br />
and should not be billed separately.<br />
• Study models (D0470) are considered integral to all procedures.<br />
• Pulp vitality tests (D0460) are considered integral to all procedures.<br />
Policies and Limitations for Preventive<br />
Procedures<br />
• One routine prophylaxis is covered in a six-month period.<br />
[This limitation may vary among states and group contracts.]<br />
• Routine prophylaxes are considered integral when provided on the same day, by the same dentist<br />
as scaling and root planing, periodontal surgery or periodontal maintenance.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.4
• A routine prophylaxis is considered integral when provided in conjunction with or as a finishing<br />
procedure to periodontal scaling and root planing, periodontal maintenance or periodontal<br />
surgical procedures.<br />
• A routine prophylaxis includes associated scaling and polishing procedures. There are no<br />
provisions for any additional allowance based on degree of difficulty.<br />
• Periodontal scaling in the presence of gingival inflammation is considered to be a routine<br />
prophylaxis and is paid as such. Participating dentists may not bill the member for any difference<br />
in fees.<br />
• One topical fluoride application is covered in a six-month period for members through age 18.<br />
[This limitation may vary among states and group contracts.]<br />
• The fluoride codes should only be reported when a prescription strength fluoride product<br />
designed solely for use in the dental office is used and delivered to the teeth under the direct<br />
supervision of a dental professional. The use of a prophylaxis paste containing fluoride qualifies<br />
for payment only as a component of a prophylaxis.<br />
• Space maintainers are covered for members through age 18 when replacing primary molars and<br />
permanent first molars.<br />
[This limitation may vary among states and group contracts.]<br />
• One space maintainer per tooth area is covered in a three-year period.<br />
• Repair of a damaged space maintainer is not a covered benefit.<br />
• Recementation of a space maintainer is covered once per six months. It is integral when<br />
provided within six months of insertion by the same dentist.<br />
• Sealants are covered on permanent first and second molars through age 15. The teeth must be<br />
caries free with no previous restoration on the mesial, distal or occlusal surfaces. One sealant per<br />
tooth is covered in a three-year period.<br />
[This limitation may vary among states and group contracts.]<br />
• Sealants provided on the same day and the same tooth as a restoration of the occlusal surface are<br />
considered integral procedures.<br />
• Restorations placed for preventive purposes, which do not extend into the dentin, are considered<br />
sealants for purposes of determining benefits.<br />
Policies and Limitations for Restorative<br />
Procedures<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.5
• Restorative procedures are covered only when necessary due to decay or tooth fracture.<br />
• The payment for restorations includes all related procedures including, but not limited to,<br />
etching, bases, liners, dentinal adhesives, local anesthesia, polishing, caries removal, preparation<br />
of gingival tissue, occlusal/contact adjustments, and detection agents.<br />
• Restorations placed for preventive purposes, which do not extend into the dentin, are considered<br />
sealants for purposes of determining benefits.<br />
• Repair or replacement of restorations by the same dentist, involving the same tooth surfaces,<br />
provided within 12 months of the previous restoration is considered integral. A separate fee is<br />
not chargeable to the member by a participating dentist. However, payment may be allowed if<br />
the repair or replacement is due to a fracture of the tooth, or if the restoration involves the<br />
occlusal surface of a posterior tooth or the lingual surface of an anterior tooth and is placed<br />
following root canal therapy.<br />
• Restorations are not covered when provided after the placement of any type of crown or onlay,<br />
on the same tooth, by the same dentist unless approved by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor.<br />
• For purposes of determining benefits, a restoration involving two or more surfaces will be<br />
processed using the appropriate multiple surface restoration code.<br />
• Multiple restorations provided on the same day, by the same dentist, on the same surface of a<br />
posterior tooth without involvement of a second surface will be processed as a single surface<br />
restoration.<br />
• If multiple posterior restorations involving multiple surfaces with at least one common surface<br />
are reported, an allowance will be made for a single restoration reflecting the number of different<br />
surfaces involved.<br />
• Multiple restorations involving contiguous (touching) surfaces provided on the same date of<br />
service by the same dentist will be processed as one restoration reflective of the number of<br />
different surfaces reported.<br />
• An amalgam or resin restoration reported with a pin (D2951), in addition to a crown is<br />
considered a pin build up (D2950 or D6973).<br />
• An amalgam or resin restoration reported with a crown buildup or post and core is considered<br />
an integral procedure.<br />
• Resin (composite) restorations provided on posterior teeth are processed under the Alternate<br />
Benefit Provision as a comparable amalgam restoration. The member is responsible for the<br />
difference between the dentist’s charge for the resin restoration and the amount paid by <strong>United</strong><br />
<strong>Concordia</strong> for the amalgam restoration.<br />
• Replacement of amalgam restorations due to mercury sensitivity is not covered.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.6
• Pin retention is covered only when reported in conjunction with an eligible restoration. The<br />
allowance for pins is paid per restoration, regardless of the number of pins used.<br />
• Sedative restorations (D2940) are not a covered benefit.<br />
• Prefabricated stainless steel crowns (D2930, D2931) are covered once per tooth, per lifetime for<br />
member’s age 13 and younger. They are not covered for member’s age 14 and older.<br />
• Prefabricated stainless steel crowns with resin window (D2933) and prefabricated resin crowns<br />
(D2932) are processed under the Alternate Benefit Provision as a prefabricated stainless steel<br />
crown (D2930, D2931). The member is responsible for the difference between the dentist’s<br />
charge for the prefabricated stainless steel crown with resin window/prefabricated resin crown<br />
and the amount paid by <strong>United</strong> <strong>Concordia</strong> for the prefabricated stainless steel crown.<br />
• Resin-based composite crowns placed on anterior teeth (D2390) are limited to one per tooth per<br />
12-month period. Repair or replacement within 12-months of placement by the same dentist is<br />
considered integral. Placement within 12 months of a previous restoration is not covered. A<br />
separate fee is not chargeable to the member by a participating dentist.<br />
• Prefabricated esthetic coated stainless steel crowns placed on primary teeth (D2934) are<br />
processed under the Alternate Benefit Provision as a regular stainless steel crown (D2930). The<br />
member is responsible for the difference between the dentist’s charge for the prefabricated<br />
esthetic coated crown and the amount paid by <strong>United</strong> <strong>Concordia</strong> for the regular stainless steel<br />
crown.<br />
• Temporary crowns placed in preparation for permanent crowns are considered integral.<br />
Policies and Limitations for Crowns, Inlays and<br />
Onlays<br />
• The charge for a crown, inlay or onlay should include all charges for work related to its<br />
placement including, but not limited to, preparation of gingival tissue, tooth preparation,<br />
temporary crown, diagnostic casts (study models), impressions, try-in visits, and cementation of<br />
both permanent and temporary crowns.<br />
• For reporting and benefit purposes, the completion date for crowns, inlays, onlays and buildups<br />
is the cementation date.<br />
• Single inlays are processed under the Alternate Benefit Provision as amalgam restorations based<br />
upon the number of different surfaces reported. The member is responsible for the difference<br />
between the dentist’s charge for the inlay and the amount paid by <strong>United</strong> <strong>Concordia</strong> for the<br />
amalgam restoration. Inlays can be reviewed for coverage by a <strong>United</strong> <strong>Concordia</strong> Dentist<br />
Advisor only when radiographs and member specific documentation are submitted, which<br />
support that an inlay is the only method of restoring the tooth.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.7
• Replacement of crowns, inlays, onlays, build-ups and post and cores is covered only if the<br />
existing restoration was inserted at least five years prior to the replacement and satisfactory<br />
evidence is presented that the existing restoration is not, and cannot be made serviceable.<br />
• Onlay and crown restorations for members age 13 years or younger are excluded from coverage<br />
unless specific rationale is provided indicating the reason for such treatment (e.g., tooth fracture,<br />
etc.) and is approved by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor.<br />
• Onlays, crowns and post and cores are payable only when necessary due to decay or tooth<br />
fracture. However, if the tooth can be adequately restored with another material such as<br />
amalgam, payment will be made for that procedure. This payment can be applied towards the<br />
cost of the onlay, crown or post and core. This provision only applies where the restorative<br />
procedure provided is due to decay or tooth fracture. If the procedure is provided for some<br />
other purpose, e.g., esthetics, an alternative procedure such as an amalgam or composite<br />
restoration is not eligible for payment.<br />
• Recementation of permanent single crowns and onlays is eligible once per 12-month period. It is<br />
considered integral when placed within 12 months of insertion of a crown or onlay by the same<br />
dentist.<br />
• Recementation of a post and core (D2915) is considered integral to recementation of a crown<br />
when provided on the same day by the same dentist.<br />
• Glass ionomer restorations are processed as amalgam restorations for posterior teeth and resin<br />
restorations for anterior teeth.<br />
• Canal preparation and fitting of a preformed dowel or post (D3950) is not a covered benefit.<br />
• Core buildups and post and cores are not eligible on primary teeth. A fee cannot be charged to<br />
the member by a participating dentist.<br />
• Core buildups (D2950) can be considered for benefits only when the tooth requires a crown and<br />
there is insufficient retention for the crown. A buildup should not be reported when the<br />
procedure only involves a filler used to eliminate undercuts, box forms or concave irregularities<br />
in the preparation.<br />
• Cast post and cores (D2952) are processed as an alternate benefit of a prefabricated post and<br />
core (D2954). The member is responsible for the difference between the dentist’s charge for the<br />
cast post and core and the amount paid by <strong>United</strong> <strong>Concordia</strong> for the prefabricated post and core.<br />
• Additional posts (D2953, D2957) are considered integral to all procedures.<br />
• Additional procedures required to construct a crown under an existing partial denture framework<br />
(D2971) is eligible once per tooth per five-year period<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.8
Policies and Limitations for Endodontic<br />
Procedures<br />
• For reporting and benefit purposes, the completion date for root canal therapy is the date the<br />
tooth is sealed.<br />
• No allowance is made for the treatment of additional canals.<br />
• The final restoration following root canal therapy is covered as a separate procedure.<br />
• Incomplete endodontic therapy (D3332) is not a covered benefit.<br />
• The retreatment of a root canal (D3346-D3348) is covered once per tooth, per lifetime.<br />
• Apicoectomy (D3410-D3426) is not generally covered when provided within 30 days following<br />
root canal therapy.<br />
• Treatment of a root canal obstruction (D3331) is considered an integral procedure.<br />
• Internal repair of a perforation defect (D3333) can only be considered for coverage when it is the<br />
result of resorption or decay. It is not a covered benefit when the perforation is caused by the<br />
dentist providing the treatment. A pre-treatment radiograph and a report detailing the procedure<br />
provided are required for review.<br />
• Pulp capping (D3110, D3120) is considered an integral procedure.<br />
• Pulpotomy (D3220) is covered when provided as a final endodontic procedure and is payable on<br />
primary teeth only. A pulpotomy provided on a permanent tooth is considered initiation of root<br />
canal therapy and is not separately reimbursable. A pulpotomy placed in an emergency to relieve<br />
acute pain can be considered for benefits as palliative emergency treatment.<br />
• Pulpotomy is considered integral when provided by the same dentist within a 180-day period<br />
prior to the completion of root canal therapy.<br />
• Pulpal debridement (D3221) is eligible when provided to relieve acute pain. It is considered<br />
integral to root canal therapy or palliative emergency treatment when provided on the same day,<br />
by the same dentist.<br />
• Pulpal therapy (D3230, D3240) is a benefit once per tooth, per lifetime. Payment for pulpal<br />
therapy will be offset by the allowance for a pulpotomy provided within 180 days preceding<br />
pulpal therapy on the same tooth, by the same dentist.<br />
• Pulpal therapy is a benefit for members through age five on primary incisor teeth and through<br />
age eleven on primary molars and cuspids.<br />
• Apical curettage is considered an integral procedure.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.9
• Canal preparation and fitting of a preformed dowel or post (D3950) is not a covered benefit.<br />
• The apexification final visit code (D3353) includes the last phase of complete root canal therapy.<br />
Root canal therapy reported in addition to the apexification treatment is not a separately<br />
reimbursable procedure.<br />
• An open and drain performed on an abscessed tooth to relieve pain in an emergency is<br />
considered palliative emergency treatment.<br />
Policies and Limitations for Periodontal<br />
Procedures<br />
• Gingivectomy/gingivoplasty (D4210, D4211) is not covered within two years following<br />
gingivectomy or periodontal surgical procedures in the same mouth area.<br />
• Gingivectomy/gingivoplasty provided in conjunction with the placement of crowns, inlays,<br />
onlays, buildups, post and cores, fixed bridges or basic restorations is considered integral.<br />
• Gingivectomy/gingivoplasty is considered integral to gingival flap procedure when provided on<br />
the same day, by the same dentist in the same mouth area.<br />
• Gingivectomy/gingivoplasty provided in a limited area (D4211, one to three contiguous teeth or<br />
bounded teeth spaces per quadrant) will be paid at 40 percent of the full quadrant allowance.<br />
• Gingival flap procedure (D4240, D4241) is not covered within two years following gingival flap<br />
procedure, periodontal surgical procedures or scaling and root planing in the same mouth area.<br />
• Gingival flap procedure is considered integral when provided on the same day, by the same<br />
dentist in the same mouth area as periodontal surgical procedures, endodontic procedures and<br />
oral surgery procedures.<br />
• Gingival flap procedure provided in a limited area (D4241, one to three contiguous teeth or<br />
bounded teeth spaces per quadrant) will be paid at 40 percent of the full quadrant allowance.<br />
• Apically repositioned flap (D4245) is considered integral to other periodontal procedures.<br />
• Osseous surgery (D4260, D4261) is not covered within two years following osseous surgery or<br />
periodontal surgical procedures in the same mouth area.<br />
• Osseous surgery provided in a limited area (D4261, one to three contiguous teeth or bounded<br />
teeth spaces per quadrant) will be paid at 40 percent of the full quadrant allowance.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.10
• Osseous surgery is considered an integral procedure when provided in a limited area in<br />
conjunction with crown lengthening on the same day, by the same dentist in the same mouth<br />
area.<br />
• Soft tissue grafts (D4270, D4271, D4273, D4275, D4276) are processed according to the<br />
number of separate sites involved. Multiple separate sites reported on the same day will be<br />
reviewed by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor. Complete periodontal charting and a diagnosis<br />
are required for review.<br />
• Soft tissue grafts are considered integral when provided on the same day, in the same mouth area<br />
as osseous surgery.<br />
• Subepithelial connective tissue grafts (D4273) and combined connective tissue and double<br />
pedicle grafts (D4276) are payable at the same allowance as free soft tissue grafts. The member is<br />
responsible for the difference between the dentist’s charge for the subepithelial connective tissue<br />
graft or combined graft and the amount paid by <strong>United</strong> <strong>Concordia</strong>.<br />
• Distal wedge procedure (D4274) is considered integral to other periodontal surgical procedures<br />
provided on the same day, by the same dentist, in the same mouth area.<br />
• Bone replacement grafts (D4263, D4264) are only eligible when provided to treat teeth with<br />
periodontal defects.<br />
• Bone grafts provided for ridge preservation (D7953) (socket grafts) are not covered. This<br />
includes bone grafts provided for reasons, such as filling in an extraction site or a defect resulting<br />
from an apicoectomy or cyst removal.<br />
• A single site for reporting bone replacement grafts consists of one contiguous area, regardless of<br />
the number of teeth involved. Another site on the same tooth is considered part of the first site<br />
reported. Non-contiguous areas involving different teeth may be reported as additional sites.<br />
• Multiple bone replacement grafts reported on the same day, by the same dentist require review<br />
by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor. A diagnosis, complete periodontal charting, and<br />
radiographs are required for review.<br />
• Guided tissue regeneration (D4266, D4267) is only eligible to treat specific types of periodontal<br />
defects, i.e., class II furcation involvements or craters. It is eligible once per site, per lifetime. A<br />
diagnosis, complete periodontal charting and radiographs are required for review.<br />
• Surgical revision procedure (D4268) is considered integral to other periodontal procedures.<br />
• Periodontal scaling and root planing (D4341, D4342) is indicated to treat periodontal disease,<br />
which generally does not occur with frequency in younger members. Periodontal scaling and root<br />
planing submitted for members under the age of 19 will require a specific diagnosis, complete<br />
periodontal charting, and radiographs to substantiate the presence of periodontal disease.<br />
• Periodontal scaling and root planing provided within 24 months following periodontal scaling<br />
and root planing or periodontal surgical procedures in the same mouth area is not covered.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.11
• Periodontal scaling and root planing is considered integral when provided on the same day, by<br />
the same dentist as periodontal surgical procedures.<br />
• Periodontal scaling and root planing provided in a limited area (D4342, one to three teeth per<br />
quadrant) will be paid at 25 percent of the full quadrant allowance.<br />
• Periodontal scaling and root planning provided in a limited area within 30 days following a<br />
prophylaxis is considered integral.<br />
• Periodontal maintenance (D4910) is generally covered when it follows active periodontal<br />
treatment.<br />
• An evaluation provided in addition to periodontal maintenance is processed as a separate<br />
procedure, subject to the policy and limitations applicable to oral evaluations.<br />
• Periodontal maintenance is limited to two times within a 12-month period.<br />
[This limitation may vary among states and group contracts.]<br />
• Periodontal maintenance is considered integral when provided on the same day as periodontal<br />
scaling and root planing or periodontal surgical procedures.<br />
• Full mouth debridement to enable comprehensive evaluation and diagnosis (D4355) is not a<br />
covered benefit. It is considered integral when provided on the same day as scaling and root<br />
planing, routine prophylaxis, or periodontal maintenance.<br />
• Payment for multiple periodontal surgical procedures provided in the same mouth area during<br />
the same course of treatment is based on the greater surgical procedure. The lesser procedure(s)<br />
is considered integral.<br />
Policies and Limitations for Removable<br />
Prosthetic Procedures<br />
• Removable cast base and flexible base partial dentures for members under age 14 are excluded<br />
from coverage, unless specific rationale is provided indicating the necessity for that treatment<br />
and is approved by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor.<br />
• Removable flexible base partial dentures (D5225, D5226) will be processed as an alternate<br />
benefit of a cast metal partial denture (D5213, D5214). The member is responsible for the<br />
difference between the dentist’s charge for the flexible base partial denture and the amount paid<br />
by <strong>United</strong> <strong>Concordia</strong> for the cast metal partial denture.<br />
• For reporting and benefit purposes, the completion date for removable prosthetics is the<br />
insertion date.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.12
• The relining or rebasing of a denture is considered integral when provided within six months<br />
following the insertion of that denture. A reline/rebase is covered once in any 36 months.<br />
• Adjustments provided within six months of the insertion of an initial or replacement denture<br />
are integral to the denture.<br />
• Payment for a denture or an overdenture made with precious metals is based on the fee for a<br />
conventional denture. Any additional cost is the member’s responsibility.<br />
• Precision attachments, personalization, precious metal bases and other specialized techniques are<br />
not covered.<br />
• A fixed partial denture and removable partial denture are not covered benefits in the same<br />
arch. Payment will be made for a removable partial denture to replace all missing teeth in the<br />
arch.<br />
• Replacement of removable and fixed prostheses is covered only if the existing prostheses were<br />
inserted at least five years prior to the replacement and satisfactory evidence is presented that the<br />
existing prostheses are not and cannot be made serviceable.<br />
• [This limitation may vary among states and group contracts.]<br />
• Replacement of all teeth and acrylic on a cast metal framework (D5670, D5671) is covered once<br />
per arch per five-year period. Previous payment for this procedure or another denture within five<br />
years precludes payment for D5670 or D5671.<br />
• Interim (temporary) dentures are not a covered benefit.<br />
Policies and Limitations for Fixed Prosthetic<br />
Procedures<br />
• Fixed partial dentures, build-ups, and posts and cores for members under age 14 are not<br />
covered unless specific rationale is provided indicating the necessity for such treatment and it<br />
is approved by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor.<br />
• Cast post and cores (D6970) are processed as an alternate benefit of a prefabricated post and<br />
core (D6972). The member is responsible for the difference between the dentist’s charge for the<br />
cast post and core and the amount paid by <strong>United</strong> <strong>Concordia</strong> for the prefabricated post and core.<br />
• Additional posts (D6976, D6977) are considered integral to all procedures.<br />
• For reporting and benefit purposes, the completion date for fixed prosthetics is the<br />
cementation date.<br />
• Temporary fixed partial dentures are not a covered benefit. They are considered integral<br />
procedures when provided in conjunction with fixed partial dentures.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.13
• Recementation is eligible once per 12 months. It is integral when provided within 12 months<br />
of insertion by the same dentist. If it is necessary following root canal treatment or as a result<br />
of an accidental injury, it is eligible regardless of the time limitation. Recementation using<br />
temporary cement for a trial period is not eligible.<br />
• Precision attachments, personalization, precious metal bases, and other specialized techniques<br />
are not covered.<br />
• A fixed partial denture and removable partial denture are not covered benefits in the same<br />
arch. Payment will be made for a removable partial denture to replace all missing teeth in the<br />
arch.<br />
• Replacement of removable and fixed prostheses is covered only if the existing prostheses were<br />
inserted at least five years prior to the replacement and satisfactory evidence is presented that the<br />
existing prostheses are not and cannot be made serviceable.<br />
[This limitation may vary among states and group contracts.]<br />
• In cases where alternative methods of treatment exist, payment will be made for the least<br />
costly, professionally accepted treatment. For example, payment may be made for a removable<br />
partial denture towards the cost of a proposed fixed partial denture. This determination is not<br />
a recommendation of which treatment should be provided; should the dentist and member<br />
decide to proceed with the fixed partial denture, the member will be financially responsible for<br />
the difference between the dentist’s charge for the fixed partial denture and the amount paid<br />
for the removable partial denture.<br />
Policies and Limitations for Oral Surgery<br />
Procedures<br />
• Fiberotomies (D7291) are covered only on permanent first bicuspids and permanent anterior<br />
teeth. They are paid on a per tooth basis and are limited to once per tooth, per lifetime.<br />
• The incision and drainage of an intraoral soft tissue abscess (D7510, D7511) is only covered<br />
when provided as the definitive treatment of an abscess. Routine follow up care is considered<br />
integral to the procedure.<br />
• The complicated incision and drainage of an intraoral soft tissue abscess (D7511) requires a<br />
report detailing the member’s condition.<br />
• The incision and drainage of an intraoral soft tissue abscess is considered integral when<br />
provided in conjunction with definitive treatment, such as root canal therapy.<br />
• The removal of a complete bony impaction with unusual surgical complications (D7241) is<br />
reviewed by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor. Pretreatment radiographs and a description of<br />
the complicating factors are required for review.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.14
• Removal of impacted third molars in members’ age 14 and younger and age 31 and older is not<br />
covered unless specific documentation is provided that substantiates the need for removal and<br />
is approved by a <strong>United</strong> <strong>Concordia</strong> Dentist Advisor. A fee cannot be charged to the member<br />
by a participating dentist.<br />
• Routine postoperative care, such as suture removal is considered integral to the fee for the<br />
surgery.<br />
• Removal of small cysts (D7450) is considered integral to extractions and surgical procedures<br />
provided in the same mouth area, by the same dentist.<br />
• Frenulectomy (D7960) is considered integral when provided on the same day, in the same mouth<br />
area as soft tissue grafts.<br />
• Frenuloplasty (D7963) is considered integral when provided on the same day, in the same mouth<br />
area as periodontal surgery or frenulectomy.<br />
• Alveoloplasty/alveolectomy involving three or fewer teeth is considered integral to the extraction<br />
of teeth.<br />
• Synthetic bone grafts for augmentation (D7995) are eligible when provided in preparation of the<br />
mouth for dentures. They are not eligible when provided for reasons such as filling in a defect<br />
following extractions, cyst removal or apicoectomy.<br />
• Bone grafts provided for ridge preservation (socket grafts) (D7953) are not covered unless<br />
benefits are provided for under an implant rider.<br />
• Crown lengthening - hard tissue (D4249) is eligible only when bone is removed. It is limited to<br />
once per tooth, per lifetime. Osseous surgery is considered an integral procedure when provided<br />
on the same day, by the same dentist, in the same mouth area.<br />
• For the purpose of determining benefits, the surgical exposure of an impacted third molar is<br />
considered excision of pericoronal gingiva (D7971) (operculectomy).<br />
• Root removal (D3450, D7250) is considered integral to a hemisection (D3920).<br />
Policies and Limitations for Palliative Emergency<br />
Treatment<br />
• Palliative emergency treatment (D9110) is eligible when an oral condition occurs suddenly and<br />
unexpectedly and requires immediate care. It is considered integral if provided on the same day<br />
as definitive treatment.<br />
• In order for palliative emergency treatment to be covered, the dentist must provide treatment to<br />
alleviate the member’s problem. If the only service provided is to evaluate the member and refer<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.15
to another dentist and/or prescribe medication, it will be considered a limited oral evaluation –<br />
problem focused (D0140).<br />
• Palliative emergency treatment is payable once per member, per dentist, per date of service.<br />
Policies and Limitations for Anesthesia<br />
• When deep sedation/general anesthesia (D9220, D9221) or intravenous conscious sedation<br />
(D9241, D9242) are covered benefits, they are eligible by report when provided in conjunction<br />
with specific covered procedures, and determined to be medically or dentally necessary for<br />
documented handicapped or uncontrollable members or justifiable medical or dental conditions.<br />
• For reporting purposes, anesthesia time begins when the provider rendering the anesthesia is<br />
first in attendance with the member for the purpose of creating the anesthetic state, and ends<br />
when he/she is no longer in personal attendance (that is, when the member may be safely placed<br />
under the customary post-operative supervision.)<br />
• Local anesthesia is considered integral to the procedure(s) for which it is provided.<br />
POSITION STATEMENTS<br />
he following statements reflect the position of <strong>United</strong> <strong>Concordia</strong> in regards to specific subjects.<br />
T<br />
These statements are used in administering dental benefits.<br />
Placement of Restorations<br />
T<br />
he standard dental contract provides coverage for restorations determined to be necessary to<br />
treat diseased or accidentally broken teeth. The determination of necessity is based on policy,<br />
which reflects a thorough review of current, scientific literature and the professional opinion of<br />
Dentist Advisors, who are engaged in active clinical practice.<br />
It is our position that the placement of restorations due to decay should be limited to those cases<br />
where the decay has progressed into the dentin. In cases where this has not occurred, other more<br />
conservative approaches, such as the use of fluoride and sealants should be considered to avoid<br />
destroying tooth structure. Under the terms of the dental contract, sealants are considered a<br />
preventive service, not a restorative service.<br />
This position is supported by the teachings of dental schools and respected literary sources, such as<br />
the International Symposium on the Criteria for the Placement and Replacement of <strong>Dental</strong><br />
Restorations. To date, we are not aware of any scientific studies that contradict or discredit this<br />
position.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.16
Overhead Expenses<br />
C<br />
harges itemized and distinguished from the professional service provided are considered<br />
overhead expenses. These include, but are not limited to charges such as facility and room fees,<br />
heat, light, rent, equipment, and office staff. Overhead expenses should not be billed separately to<br />
<strong>United</strong> <strong>Concordia</strong>. Additionally, the Participating Dentist Agreement prohibits a Participating Dentist<br />
from billing or collecting such charges from the member.<br />
Amalgam<br />
D<br />
iscussions about the content of dental amalgam have gone on for many years. While dental<br />
amalgam contains mercury, it is chemically bound to the other metals in the filling, creating an<br />
alloy of metals. Many scientific studies have been conducted to assess the safety of dental amalgam.<br />
No study has ever demonstrated that the mercury contained in dental amalgam has caused any health<br />
problems or specific chronic diseases in any person studied, with the rare exception of the member<br />
who is truly allergic to any of the metals contained in amalgam alloy.<br />
There are some dentists and lay people who oppose the use of dental amalgam, and cite alleged or<br />
unproven adverse effects of the amalgam alloy, and promote the use of alternative materials as more<br />
safe or effective. Some of these alternative materials to dental amalgam, in fact, contain components<br />
that have been proven to be potentially hazardous to humans. The choice of filling material best<br />
indicated for a specific member, and presents the best health potential, is the subject of professional<br />
judgment by the dentist, with input from the member.<br />
<strong>United</strong> <strong>Concordia</strong> provides insurance benefits for amalgam fillings and continues to support their<br />
use. This support is consistent with the endorsement for dental amalgam given by the American<br />
<strong>Dental</strong> Association, the scientific community, as well as the US Surgeon General. <strong>Dental</strong> amalgam<br />
continues to be a successful and safe dental filling material, with many clinical applications. <strong>United</strong><br />
<strong>Concordia</strong> will continue to support its' participating dentists, as they inform members of the<br />
appropriate filling material, and alternative materials, and fully supports the right of the individual<br />
member to give informed consent prior to any treatment.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.17
PROCEDURE CODE REPORTING<br />
CHART<br />
The Procedure Code Reporting Chart provides a listing of those procedure codes that require<br />
specific information when they are reported. (To verify if a member has coverage for a specific<br />
procedure, contact <strong>Dental</strong> Customer Service at the phone number listed on the member’s<br />
identification card.)<br />
The columns and symbols used in the chart are described as follows:<br />
Column 1<br />
Column 2<br />
Column 3<br />
Procedure Code<br />
Lists the applicable ADA procedure code.<br />
Nomenclature (description of service)<br />
Provides the current ADA description of service for that procedure code.<br />
Tooth/Arch/Quadrant<br />
Indicates whether a tooth number, arch or, quadrant indicator is required for that<br />
procedure.<br />
T = the specific tooth number is required when submitting claims for that<br />
procedure. Use numbers 1-32 for permanent teeth or letters A-T for primary teeth.<br />
A = the arch (maxillary or mandibular) is required when submitting claims for that<br />
procedure.<br />
Q = the quadrant is required when submitting claims for that procedure.<br />
The following designations may be used to identify quadrants<br />
UL = Maxillary Left<br />
UR = Maxillary Right<br />
LL = Mandibular Left<br />
LR = Mandibular Right<br />
T/A = either the tooth or arch is required when submitting claims for that<br />
procedure.<br />
T/Q = either the tooth/teeth or quadrant is required when submitting claims for<br />
that procedure.<br />
T/A/Q = either the tooth, arch, or quadrant is required when submitting claims for<br />
that procedure.<br />
Column 4<br />
Surface<br />
Indicates if the surface of the tooth is required for that procedure.<br />
Yes = tooth surface(s) is required when submitting claims for that procedure.<br />
Blank = tooth surface(s) is not required when submitting claims for that procedure.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.18
Procedure<br />
Code<br />
PROCEDURE CODE REPORTING CHART<br />
Nomenclature (description of service)<br />
Tooth/<br />
Arch/<br />
Quad<br />
Surface<br />
D1351 Sealant - per tooth T<br />
D1510 Space maintainer - fixed - unilateral T<br />
D1515 Space maintainer - fixed - bilateral T<br />
D1520 Space maintainer - removable - unilateral T<br />
D1525 Space maintainer - removable - bilateral T<br />
D1550 Recementation of space maintainer T<br />
D2140 Amalgam - one surface, primary or permanent T Yes<br />
D2150 Amalgam - two surfaces, primary or permanent T Yes<br />
D2160 Amalgam - three surfaces, primary or permanent T Yes<br />
D2161 Amalgam - four or more surfaces, primary or permanent T Yes<br />
D2330 Resin-based composite - one surface, anterior T Yes<br />
D2331 Resin-based composite - two surfaces, anterior T Yes<br />
D2332 Resin-based composite - three surfaces, anterior T Yes<br />
D2335 Resin-based composite - four or more surfaces or involving incisal T Yes<br />
angle (anterior)<br />
D2390 Resin-based composite crown, anterior T<br />
D2391 Resin-based composite – one surface, posterior T Yes<br />
D2392 Resin-based composite – two surfaces, posterior T Yes<br />
D2393 Resin-based composite – three surfaces, posterior T Yes<br />
D2394 Resin-based composite – four or more surfaces, posterior T Yes<br />
D2410 Gold foil - one surface T Yes<br />
D2420 Gold foil - two surfaces T Yes<br />
D2430 Gold foil - three surfaces T Yes<br />
D2510 Inlay - metallic - one surface T Yes<br />
D2520 Inlay - metallic - two surfaces T Yes<br />
D2530 Inlay - metallic - three or more surfaces T Yes<br />
D2542 Onlay – metallic - two surfaces T Yes<br />
D2543 Onlay - metallic - three surfaces T Yes<br />
D2544 Onlay - metallic - four or more surfaces T Yes<br />
D2610 Inlay - porcelain/ceramic - one surface T Yes<br />
D2620 Inlay - porcelain/ceramic - two surfaces T Yes<br />
D2630 Inlay - porcelain/ceramic - three or more surfaces T Yes<br />
D2642 Onlay - porcelain/ceramic - two surfaces T Yes<br />
D2643 Onlay - porcelain/ceramic - three surfaces T Yes<br />
D2644 Onlay - porcelain/ceramic - four or more surfaces T Yes<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.19
Procedure<br />
Code<br />
Nomenclature (description of service)<br />
Tooth/<br />
Arch/<br />
Quad<br />
Surface<br />
D2650 Inlay - resin-based composite - one surface T Yes<br />
D2651 Inlay - resin-based composite - two surfaces T Yes<br />
D2652 Inlay - resin-based composite - three or more surfaces T Yes<br />
D2662 Onlay - resin-based composite - two surfaces T Yes<br />
D2663 Onlay - resin-based composite - three surfaces T Yes<br />
D2664 Onlay - resin-based composite - four or more surfaces T Yes<br />
D2710 Crown – resin-based composite (indirect) T<br />
D2712 Crown – 3/4 resin-based composite (indirect) T<br />
D2720 Crown - resin with high noble metal T<br />
D2721 Crown - resin with predominantly base metal T<br />
D2722 Crown - resin with noble metal T<br />
D2740 Crown - porcelain/ceramic substrate T<br />
D2750 Crown – porcelain fused to high noble metal T<br />
D2751 Crown – porcelain fused to predominantly base metal T<br />
D2752 Crown – porcelain fused to noble metal T<br />
D2780 Crown - 3/4 cast high noble metal T<br />
D2781 Crown - 3/4 cast predominantly base metal T<br />
D2782 Crown - 3/4 cast noble metal T<br />
D2783 Crown - 3/4 porcelain/ceramic T<br />
D2790 Crown - full cast high noble metal T<br />
D2791 Crown - full cast predominantly base metal T<br />
D2792 Crown - full cast noble metal T<br />
D2794 Crown – titanium T<br />
D2799 Provisional crown T<br />
D2910 Recement inlay, onlay, or partial coverage restoration T<br />
D2915 Recement cast or prefabricated post and core T<br />
D2920 Recement crown T<br />
D2930 Prefabricated stainless steel crown - primary tooth T<br />
D2931 Prefabricated stainless steel crown - permanent tooth T<br />
D2932 Prefabricated resin crown T<br />
D2933 Prefabricated stainless steel crown with resin window T<br />
D2934 Prefabricated esthetic coated stainless steel crown – primary tooth T<br />
D2940 Sedative filling T<br />
D2950 Core buildup, including any pins T<br />
D2951 Pin retention - per tooth, in addition to restoration T<br />
D2952 Cast post and core in addition to crown T<br />
D2953 Each additional cast post - same tooth T<br />
D2954 Prefabricated post and core in addition to crown T<br />
D2955 Post removal (not in conjunction with endodontic therapy) T<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.20
Procedure<br />
Code<br />
Nomenclature (description of service)<br />
Tooth/<br />
Arch/<br />
Quad<br />
D2957 Each additional prefabricated post - same tooth T<br />
D2960 Labial veneer (resin laminate) - chairside T<br />
D2961 Labial veneer (resin laminate) - laboratory T<br />
D2962 Labial veneer (porcelain laminate) - laboratory T<br />
D2971 Additional procedures to construct new crown under existing partial T<br />
denture framework<br />
D2975 Coping T<br />
D2980 Crown repair, by report T<br />
D2999 Unspecified restorative procedure, by report T<br />
D3110 Pulp cap – direct (excluding final restoration) T<br />
D3120 Pulp cap – indirect (excluding final restoration) T<br />
D3220 Therapeutic pulpotomy (excluding final restoration) – removal of pulp T<br />
coronal to the dentinocemental junction and application of medicament<br />
D3221 Pulpal debridement, primary and permanent teeth T<br />
D3230 Pulpal therapy (resorbable filling) – anterior, primary tooth (excluding T<br />
final restoration)<br />
D3240 Pulpal therapy (resorbable filling) – posterior, primary tooth (excluding T<br />
final restoration)<br />
D3310 Anterior root canal (excluding final restoration) T<br />
D3320 Bicuspid root canal (excluding final restoration) T<br />
D3330 Molar root canal (excluding final restoration) T<br />
D3331 Treatment of root canal obstruction; non-surgical access T<br />
D3332 Incomplete endodontic therapy; inoperable, unrestorable or fractured T<br />
tooth<br />
D3333 Internal root repair of perforation defects T<br />
D3346 Retreatment of previous root canal therapy – anterior T<br />
D3347 Retreatment of previous root canal therapy – bicuspid T<br />
D3348 Retreatment of previous root canal therapy – molar T<br />
D3351 Apexification/recalcification – initial visit (apical closure/calcific repair T<br />
of perforations, root resorption, etc.)<br />
D3352 Apexification/recalcification – interim medication replacement (apical T<br />
closure/calcific repair of perforations, root resorption, etc.)<br />
D3353 Apexification/recalcification – final visit (includes completed root canal T<br />
therapy – apical closure/calcific repair of perforations, root resorption,<br />
etc.)<br />
D3410 Apicoectomy/Periradicular surgery- anterior T<br />
D3421 Apicoectomy/Periradicular surgery- bicuspid (first root) T<br />
D3425 Apicoectomy/Periradicular surgery- molar (first root) T<br />
D3426 Apicoectomy/Periradicular surgery (each additional root) T<br />
D3430 Retrograde filling – per root T<br />
D3450 Root amputation – per root T<br />
Surface<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.21
Procedure<br />
Code<br />
Nomenclature (description of service)<br />
Tooth/<br />
Arch/<br />
Quad<br />
D3460 Endodontic endosseous implant T<br />
D3470 Intentional reimplantation (including necessary splinting) T<br />
D3920 Hemisection (including any root removal), not including root canal T<br />
therapy<br />
D3950 Canal preparation and fitting of preformed dowel or post T<br />
D3999 Unspecified endodontic procedure, by report T<br />
D4210 Gingivectomy or gingivoplasty – four or more contiguous teeth or Q<br />
bounded teeth spaces per quadrant<br />
D4211 Gingivectomy or gingivoplasty – one to three teeth contiguous teeth or T<br />
bounded teeth spaces per quadrant<br />
D4240 Gingival flap procedure, including root planing - four or more<br />
Q<br />
contiguous teeth or bounded teeth spaces per quadrant<br />
D4241 Gingival flap procedure, including root planing – one to three teeth T<br />
contiguous teeth or bounded teeth spaces per quadrant<br />
D4245 Apically positioned flap Q<br />
D4249 Clinical crown lengthening - hard tissue T<br />
D4260 Osseous surgery (including flap entry and closure) - four or more Q<br />
contiguous teeth or bounded teeth spaces per quadrant<br />
D4261 Osseous surgery (including flap entry and closure) one to three<br />
T<br />
contiguous teeth or bounded teeth spaces per quadrant<br />
D4263 Bone replacement graft - first site in quadrant T<br />
D4264 Bone replacement graft - each additional site in quadrant T<br />
D4265 Biologic materials to aid in soft and osseous tissue regeneration T<br />
D4266 Guided tissue regeneration - resorbable barrier, per site T<br />
D4267 Guided tissue regeneration - nonresorbable barrier, per site (includes T<br />
membrane removal)<br />
D4268 Surgical revision procedure, per tooth T<br />
D4270 Pedicle soft tissue graft procedure T<br />
D4271 Free soft tissue graft procedure (including donor site surgery) T<br />
D4273 Subepithelial connective tissue graft procedure, per tooth T<br />
D4274 Distal or proximal wedge procedure (when not performed in<br />
T/Q<br />
conjunction with surgical procedures in the same anatomical area)<br />
D4275 Soft tissue allograft T<br />
D4276 Combined connective tissue and double pedicle graft, per tooth T<br />
D4341 Periodontal scaling and root planing - four or more teeth per quadrant Q<br />
D4342 Periodontal scaling and root planing – one to three teeth per quadrant T<br />
D4381 Localized delivery of antimicrobial agents via a controlled release T<br />
vehicle into diseased crevicular tissue, per tooth, by report<br />
D4999 Unspecified periodontal procedure, by report T/Q<br />
D5211 Maxillary partial denture - resin base (including any conventional clasps,<br />
rests and teeth)<br />
T<br />
Surface<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.22
Procedure<br />
Code<br />
D5212<br />
D5213<br />
Nomenclature (description of service)<br />
Mandibular partial denture - resin base (including any conventional<br />
clasps, rests and teeth)<br />
Maxillary partial denture - cast metal framework with resin denture<br />
bases (including any conventional clasps, rests and teeth)<br />
Tooth/<br />
Arch/<br />
Quad<br />
T<br />
D5214 Mandibular partial denture - cast metal framework with resin denture T<br />
bases (including any conventional clasps, rests and teeth)<br />
D5225 Maxillary partial denture – flexible base (including any clasps, rests and T<br />
teeth)<br />
D5226 Mandibular partial denture – flexible base (including any clasps, rests T<br />
and teeth)<br />
D5281 Removable unilateral partial denture - one piece cast metal (including T<br />
clasps and teeth)<br />
D5520 Replace missing or broken teeth - complete denture (each tooth) T<br />
D5640 Replace broken teeth - per tooth T<br />
D5650 Add tooth to existing partial denture T<br />
D5860 Overdenture – complete, by report A<br />
D5861 Overdenture – partial, by report A<br />
D5899 Unspecified removable prosthodontic procedure, by report T/A<br />
D5999 Unspecified maxillofacial prosthesis, by report T<br />
D6010 Surgical placement of implant body: endosteal implant T<br />
D6040 Surgical placement: eposteal implant T<br />
D6050 Surgical placement: transosteal implant T<br />
D6053 Implant/abutment supported removable denture for completely<br />
T<br />
edentulous arch<br />
D6054 Implant/abutment supported removable denture for partially<br />
T<br />
edentulous arch<br />
D6056 Prefabricated abutment – includes placement T<br />
D6057 Custom abutment – includes placement T<br />
D6058 Abutment supported porcelain/ceramic crown T<br />
D6059 Abutment supported porcelain fused to metal crown (high noble metal) T<br />
D6060 Abutment supported porcelain fused to metal crown (predominantly T<br />
base metal)<br />
D6061 Abutment supported porcelain fused to metal crown (noble metal) T<br />
D6062 Abutment supported cast metal crown (high noble metal) T<br />
D6063 Abutment supported cast metal crown (predominantly base metal) T<br />
D6064 Abutment supported cast metal crown (noble metal) T<br />
D6065 Implant supported porcelain/ceramic crown T<br />
D6066 Implant supported porcelain fused to metal crown (titanium, titanium T<br />
alloy, high noble metal)<br />
D6067 Implant supported metal crown (titanium, titanium alloy, high noble<br />
metal)<br />
T<br />
T<br />
Surface<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.23
Procedure<br />
Code<br />
Nomenclature (description of service)<br />
Tooth/<br />
Arch/<br />
Quad<br />
Surface<br />
D6068 Abutment supported retainer for porcelain/ceramic FPD T<br />
D6069 Abutment supported retainer for porcelain fused to metal FPD (high T<br />
noble metal)<br />
D6070 Abutment supported retainer for porcelain fused to metal FPD<br />
T<br />
(predominantly base metal)<br />
D6071 Abutment supported retainer for porcelain fused to metal FPD (noble T<br />
metal)<br />
D6072 Abutment supported retainer for cast metal FPD (high noble metal) T<br />
D6073 Abutment supported retainer for case metal FPD (predominantly base T<br />
metal)<br />
D6074 Abutment supported retainer for case metal FPD (noble metal) T<br />
D6075 Implant supported retainer for ceramic FPD T<br />
D6076 Implant supported retainer for porcelain fused to metal FPD (titanium, T<br />
titanium alloy, high noble metal)<br />
D6077 Implant supported retainer for cast metal FPD (titanium, titanium alloy, T<br />
high noble metal)<br />
D6078 Implant/abutment supported fixed denture for completely edentulous A<br />
arch<br />
D6079 Implant/abutment supported fixed denture for partially edentulous arch T<br />
D6090 Repair implant supported prosthesis, by report T<br />
D6094 Abutment supported crown – (titanium) T<br />
D6095 Repair implant abutment, by report T<br />
D6100 Implant removal, by report T<br />
D6194 Abutment supported retainer crown for FPD – (titanium) T<br />
D6199 Unspecified implant procedure, by report T<br />
D6205 Pontic – indirect resin based composite T<br />
D6210 Pontic – cast high noble metal T<br />
D6211 Pontic – cast predominantly base metal T<br />
D6212 Pontic – cast noble metal T<br />
D6214 Pontic – titanium T<br />
D6240 Pontic – porcelain fused to high noble metal T<br />
D6241 Pontic – porcelain fused to predominantly base metal T<br />
D6242 Pontic – porcelain fused to noble metal T<br />
D6245 Pontic – porcelain/ceramic T<br />
D6250 Pontic – resin with high noble metal T<br />
D6251 Pontic – resin with predominantly base metal T<br />
D6252 Pontic – resin with noble metal T<br />
D6253 Provisional pontic T<br />
D6545 Retainer – cast metal for resin bonded fixed prosthesis T<br />
D6548 Retainer – porcelain/ceramic for resin bonded fixed prosthesis T<br />
D6600 Inlay – porcelain/ceramic, two surfaces T Yes<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.24
Procedure<br />
Code<br />
Nomenclature (description of service)<br />
Tooth/<br />
Arch/<br />
Quad<br />
Surface<br />
D6601 Inlay – porcelain/ceramic, three or more surfaces T Yes<br />
D6602 Inlay – cast high noble metal, two surfaces T Yes<br />
D6603 Inlay – cast high noble metal, three or more surfaces T Yes<br />
D6604 Inlay – cast predominantly base metal, two surfaces T Yes<br />
D6605 Inlay – cast predominantly base metal, three or more surfaces T Yes<br />
D6606 Inlay – cast noble metal, two surfaces T Yes<br />
D6607 Inlay – cast noble metal, three or more surfaces T Yes<br />
D6608 Onlay – porcelain/ceramic, two surfaces T Yes<br />
D6609 Onlay – porcelain/ceramic, three or more surfaces T Yes<br />
D6610 Onlay – cast high noble metal, two surfaces T Yes<br />
D6611 Onlay – cast high noble metal, three or more surfaces T Yes<br />
D6612 Onlay – cast predominantly base metal, two surfaces T Yes<br />
D6613 Onlay – cast predominantly base metal, three or more surfaces T Yes<br />
D6614 Onlay – cast noble metal, two surfaces T Yes<br />
D6615 Onlay – cast noble metal, three or more surfaces T Yes<br />
D6624 Inlay – titanium T<br />
D6634 Onlay – titanium T<br />
D6710 Crown – indirect resin based composite T<br />
D6720 Crown – resin with high noble metal T<br />
D6721 Crown – resin with predominantly base metal T<br />
D6722 Crown – resin with noble metal T<br />
D6740 Crown – porcelain/ceramic T<br />
D6750 Crown – porcelain fused to high noble metal T<br />
D6751 Crown – porcelain fused to predominantly base metal T<br />
D6752 Crown – porcelain fused to noble metal T<br />
D6780 Crown – 3/4 cast high noble metal T<br />
D6781 Crown – 3/4 cast predominantly base metal T<br />
D6782 Crown – 3/4 cast noble metal T<br />
D6783 Crown – 3/4 porcelain/ceramic T<br />
D6790 Crown – full cast high noble metal T<br />
D6791 Crown – full cast predominantly base metal T<br />
D6792 Crown – full cast noble metal T<br />
D6793 Provisional retainer crown T<br />
D6794 Crown –<br />
T<br />
titanium<br />
D6930 Recement fixed partial denture T<br />
D6970 Cast post and core in addition to fixed partial denture retainer T<br />
D6971 Cast post as part of fixed partial denture retainer T<br />
D6972 Prefabricated post and core in addition to fixed partial denture retainer T<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.25
D6973 Core build up for retainer, including any pins T<br />
Procedure<br />
Nomenclature (description of service)<br />
Tooth/<br />
Code<br />
Arch/<br />
Quad<br />
D6975 Coping - metal T<br />
D6976 Each additional cast post - same tooth T<br />
D6977 Each additional prefabricated post - same tooth T<br />
D6980 Fixed partial denture repair, by report T<br />
D6985 Pediatric partial denture, fixed T<br />
D6999 Unspecified fixed prosthodontic procedure, by report T<br />
D7111 Extraction, coronal remnants – deciduous tooth T<br />
D7140 Extraction, erupted tooth or exposed root (elevation and/or forceps T<br />
removal)<br />
D7210 Surgical removal of erupted tooth requiring elevation of mucoperiosteal T<br />
flap and removal of bone and/or section of tooth<br />
D7220 Removal of impacted tooth - soft tissue T<br />
D7230 Removal of impacted tooth - partially bony T<br />
D7240 Removal of impacted tooth - completely bony T<br />
D7241 Removal of impacted tooth - completely bony with unusual surgical T<br />
complications<br />
D7250 Surgical removal of residual tooth roots (cutting procedure) T<br />
D7270 Tooth reimplantation and/or stabilization of accidentally evulsed or T<br />
displaced tooth<br />
D7272 Tooth transplantation (includes reimplantation from one site to another T<br />
and splinting and/or stabilization)<br />
D7280 Surgical access of an unerupted tooth T<br />
D7282 Mobilization of erupted or malpositioned tooth to aid eruption T<br />
D7283 Placement of device to facilitate eruption of impacted tooth T<br />
D7290 Surgical repositioning of teeth T<br />
D7291 Transseptal fiberotomy/supra crestal fiberotomy, by report T<br />
D7310 Alveoloplasty in conjunction with extractions - per quadrant T/Q<br />
D7311 Alveoloplasty in conjunction with extractions – one to three teeth or T<br />
tooth spaces, per quadrant<br />
D7320 Alveoloplasty not in conjunction with extractions - per quadrant T/Q<br />
D7321 Alveoloplasty not in conjunction with extractions – one to three teeth T<br />
or tooth spaces, per quadrant<br />
D7510 Incision and drainage of abscess - intraoral soft tissue T/A<br />
D7953 Bone replacement graft for ridge preservation – per site T<br />
D7971 Excision of pericoronal gingiva T<br />
D7995 Synthetic graft - mandible or facial bones, by report T/Q<br />
D8999 Unspecified orthodontic procedure, by report A<br />
D9110 Palliative (emergency) treatment of dental pain - minor procedure T/A/Q<br />
D9910 Application of desensitizing medicament T<br />
Surface<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.26
D9911 Application of desensitizing resin for cervical and/or root surface, per T<br />
tooth<br />
D9970 Enamel microabrasion T<br />
D9971 Odontoplasty 1-2 teeth; includes removal of enamel projections T<br />
D9972 External bleaching - per arch A<br />
D9973 External bleaching - per tooth T<br />
D9974 Internal bleaching - per tooth T<br />
D9999 Unspecified adjunctive procedure, by report T/Q/A<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
6.27
W<br />
DIAGNOSTIC MATERIAL REQUIREMENTS<br />
hen covered, the following procedures require diagnostic materials for review. (To verify if a member has coverage for a specific procedure,<br />
contact <strong>Dental</strong> Customer Service at the phone number listed on the member’s identification card.) For those procedures requiring radiographs,<br />
dentists are requested to submit all radiographs used for diagnosis and treatment planning. The radiographs should be of diagnostic quality, mounted<br />
and identified with the dentist’s name, address and provider number, as well as the member’s name and Identification Number. Also include the date<br />
the radiographs were taken. If a copy of the radiographs is submitted, left or right should be marked on the copy. If for some reason, radiographs are<br />
not available, a brief explanation should be included on the claim form.<br />
Diagnostic materials are required for the following procedures:<br />
Pre-<br />
Treatment<br />
*Post<br />
Rct<br />
Full<br />
Arch<br />
Full<br />
Mouth<br />
Perio<br />
Charting<br />
Diagnosis<br />
Report/<br />
Op Notes Other<br />
X 1<br />
Code<br />
Description<br />
D0160 Detailed and extensive oral evaluation, problem<br />
focused, by report<br />
D2510 Inlay - metallic - one surface X * 6<br />
D2520 Inlay - metallic - two surfaces X * 6<br />
D2530 Inlay - metallic - three or more surfaces X * 6<br />
D2542 Onlay – metallic – two surfaces X *<br />
D2543 Onlay - metallic - three surfaces X *<br />
D2544 Onlay - metallic - four or more surfaces X *<br />
D2610 Inlay - porcelain/ceramic - one surface X * 6<br />
D2620 Inlay - porcelain/ceramic - two surfaces X * 6<br />
D2630 Inlay - porcelain/ceramic - three or more surfaces X * 6<br />
D2642 Onlay - porcelain/ceramic - two surfaces X *<br />
D2643 Onlay - porcelain/ceramic - three surfaces X *<br />
D2644 Onlay - porcelain/ceramic - four or more surfaces X *<br />
D2650 Inlay – resin-based composite - one surface X * 6<br />
D2651 Inlay – resin-based composite - two surfaces X * 6<br />
D2652 Inlay – resin-based composite - three or more<br />
X * 6<br />
surfaces<br />
D2662 Onlay – resin-based composite - two surfaces X *<br />
May 2005 6.28<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Code<br />
Description<br />
Pre-<br />
Treatment<br />
*Post<br />
RCT<br />
Full<br />
Arch<br />
Full<br />
Mouth<br />
Perio<br />
Charting<br />
Diagnosis<br />
Report/<br />
Op Notes Other<br />
D2663 Onlay – resin-based composite - three surfaces X *<br />
D2664 Onlay – resin-based composite - four or more<br />
X *<br />
surfaces<br />
D2710 Crown - resin-based composite (indirect) X *<br />
D2712 Crown – 3/4 resin-based composite (indirect) X *<br />
D2720 Crown - resin with high noble metal X *<br />
D2721 Crown - resin with predominantly base metal X *<br />
D2722 Crown - resin with noble metal X *<br />
D2740 Crown - porcelain/ceramic substrate X *<br />
D2750 Crown - porcelain fused to high noble metal X *<br />
D2751 Crown - porcelain fused to base predominantly base X *<br />
metal<br />
D2752 Crown - porcelain fused to noble metal X *<br />
D2780 Crown – ¾ cast high noble metal X *<br />
D2781 Crown – ¾ cast predominately base metal X *<br />
D2782 Crown – ¾ cast noble metal X *<br />
D2783 Crown – ¾ porcelain /ceramic X *<br />
D2790 Crown - full cast high noble metal X *<br />
D2791 Crown - full cast predominantly base metal X *<br />
D2792 Crown - full cast noble metal X *<br />
D2794 Crown - titanium X *<br />
D2950 Core buildup, including any pins X *<br />
D2952 Cast post and core in addition to crown X * 7<br />
D2954 Prefabricated post and core in addition to crown X *<br />
D2980 Crown repair, by report X 4<br />
D2999 Unspecified restorative procedure, by report X 5<br />
D3333 Internal root repair of perforation defects X X<br />
D3999 Unspecified endodontic procedure, by report X 5<br />
D4210 Gingivectomy or gingivoplasty – four or more<br />
contiguous teeth or bounded teeth spaces per<br />
quadrant<br />
X X X<br />
May 2005 6.29<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Code<br />
Description<br />
D4211 Gingivectomy or gingivoplasty – one to three<br />
contiguous teeth or bounded teeth spaces per<br />
quadrant<br />
D4240 Gingival flap procedure, including root planning –<br />
four or more contiguous teeth or bounded teeth<br />
spaces per quadrant<br />
D4241 Gingival flap procedure, including root planning –<br />
one to three contiguous teeth or bounded teeth<br />
spaces per quadrant<br />
D4260 Osseous surgery (including flap entry and closure) –<br />
four or more contiguous teeth or bounded teeth<br />
spaces per quadrant<br />
D4261 Osseous surgery (including flap entry and closure) –<br />
one to three contiguous teeth or bounded teeth<br />
spaces per quadrant<br />
Pre-<br />
Treatment<br />
*Post<br />
RCT<br />
Full<br />
Arch<br />
Full Perio Diagnosis<br />
Mouth Charting<br />
X X X<br />
Report/<br />
Op Notes<br />
Other<br />
X X X 1<br />
X X X 1<br />
X X X<br />
X X X<br />
D4263 Bone replacement graft - first site in quadrant X X X<br />
D4264 Bone replacement graft – each additional site in<br />
X X X<br />
quadrant<br />
D4266 Guided tissue regeneration - resorbable barrier, per<br />
X X X<br />
site<br />
D4267 Guided tissue regeneration - nonresorbable barrier,<br />
X X X<br />
per site (includes membrane removal)<br />
D4270 Pedicle soft tissue graft procedure X X<br />
D4271 Free soft tissue graft procedure (including donor<br />
X X<br />
site surgery)<br />
D4273 Subepithelial connective tissue graft procedures, per<br />
X X<br />
tooth<br />
D4275 Soft tissue allograft X X<br />
D4276 Combined connective tissue and double pedicle<br />
graft, per tooth<br />
X X<br />
May 2005 6.30<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Code<br />
Description<br />
Pre-<br />
Treatment<br />
*Post<br />
RCT<br />
Full<br />
Arch<br />
Full<br />
Mouth<br />
Perio<br />
Charting<br />
Diagnosis<br />
Report/<br />
Op Notes Other<br />
D4341 Scaling and root planing – four or more teeth per<br />
X X X 2<br />
quadrant<br />
D4342 Scaling and root planing - one to three teeth per<br />
X X X 2<br />
quadrant<br />
D4999 Unspecified periodontal procedure, by report X 5<br />
D5899 Unspecified removable prosthodontic procedure, by<br />
X 5<br />
report<br />
D5999 Unspecified maxillofacial prosthesis, by report X 5<br />
D6205 Pontic – indirect resin based composite X<br />
D6210 Pontic – cast high noble metal X<br />
D6211 Pontic – cast predominantly base metal X<br />
D6212 Pontic – cast noble metal X<br />
D6214 Pontic – titanium X<br />
D6240 Pontic – porcelain fused to high noble metal X<br />
D6241 Pontic – porcelain fused to predominantly base<br />
X<br />
metal<br />
D6242 Pontic – porcelain fused to noble metal X<br />
D6245 Pontic – porcelain/ceramic X<br />
D6250 Pontic – resin with high noble metal X<br />
D6251 Pontic – resin with predominantly base metal X<br />
D6252 Pontic – resin with noble metal X<br />
D6545 Retainer – cast metal for resin bonded fixed<br />
* X<br />
prosthesis<br />
D6548 Retainer – porcelain/ceramic for resin bonded fixed<br />
* X<br />
prosthesis<br />
D6600 Inlay – porcelain/ceramic, two surfaces * X<br />
D6601 Inlay – porcelain/ceramic, three or more surfaces * X<br />
D6602 Inlay – cast high noble metal, two surfaces * X<br />
D6603 Inlay – cast high noble metal, three or more<br />
* X<br />
surfaces<br />
D6604 Inlay – cast predominantly base metal, two surfaces * X<br />
May 2005 6.31<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Pre-<br />
Treatment<br />
*Post Full<br />
RCT Arch<br />
* X<br />
Code<br />
Description<br />
D6605 Inlay – cast predominantly base metal, three or<br />
more surfaces<br />
D6606 Inlay – cast noble metal, two surfaces * X<br />
D6607 Inlay – cast noble metal, three or more surfaces * X<br />
D6608 Onlay – porcelain/ceramic, two surfaces * X<br />
D6609 Onlay – porcelain/ceramic, three or more surfaces * X<br />
D6610 Onlay – cast high noble metal, two surfaces * X<br />
D6611 Onlay – cast high noble metal, three or more<br />
* X<br />
surfaces<br />
D6612 Onlay – cast predominantly base metal, two<br />
* X<br />
surfaces<br />
D6613 Onlay – cast predominantly base metal, three or<br />
* X<br />
more surfaces<br />
D6614 Onlay – cast noble metal, two surfaces * X<br />
D6615 Onlay – cast noble metal, three or more surfaces * X<br />
D6624 Inlay – titanium * X<br />
D6634 Onlay – titanium * X<br />
D6710 Crown – indirect resin based composite * X<br />
D6720 Crown - resin with high noble metal * X<br />
D6721 Crown - resin with predominantly base metal * X<br />
D6722 Crown - resin with noble metal * X<br />
D6740 Crown – porcelain/ceramic * X<br />
D6750 Crown - porcelain fused to high noble metal * X<br />
D6751 Crown - porcelain fused to predominantly base<br />
* X<br />
metal<br />
D6752 Crown - porcelain fused to noble metal * X<br />
D6780 Crown – ¾ cast high noble metal * X<br />
D6781 Crown – ¾ cast predominately base metal * X<br />
D6782 Crown – ¾ cast noble metal * X<br />
D6783 Crown – ¾ porcelain/ceramic * X<br />
D6790 Crown - full cast high noble metal * X<br />
Full<br />
Mouth<br />
Perio<br />
Charting<br />
Diagnosis<br />
Report/<br />
Op Notes<br />
Other<br />
May 2005 6.32<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Code<br />
Description<br />
Pre-<br />
Treatment<br />
*Post<br />
RCT<br />
Full<br />
Arch<br />
Full<br />
Mouth<br />
Perio<br />
Charting<br />
Diagnosis<br />
Report/<br />
Op Notes Other<br />
D6791 Crown - full cast predominantly base metal * X<br />
D6792 Crown - full cast noble metal * X<br />
D6794 Crown – titanium * X<br />
D6970 Cast post and core in addition to fixed partial<br />
* X 7<br />
denture retainer<br />
D6972 Prefabricated post and core in addition to fixed<br />
* X<br />
partial denture retainer<br />
D6973 Core buildup for retainer, including any pins * X<br />
D6980 Fixed partial denture repair, by report X 4<br />
D6999 Unspecified fixed prosthodontic procedure, by<br />
X 5<br />
report<br />
D7230 Removal of impacted tooth – partially bony X 8<br />
D7240 Removal of impacted tooth – completely bony X 8<br />
D7241 Removal of impacted tooth - complete bony, with X<br />
X<br />
unusual surgical complications<br />
D7350 Vestibuloplasty – ridge extension (including soft<br />
X<br />
tissue grafts, muscle reattachment, revision of soft<br />
tissue attachment and management of<br />
hypertrophied and hyperplastic tissue)<br />
D7511 Incision and drainage of abscess – intraoral soft<br />
X<br />
tissue – complicated (includes drainage of multiple<br />
fascial spaces)<br />
D7912 Complicated suture – greater than 5 cm X<br />
D7995 Repair of maxillofacial soft and/or hard tissue<br />
X<br />
defect<br />
D7999 Unspecified oral surgery procedure, by report X 5<br />
D8999 Unspecified orthodontic procedure, by report X<br />
D9930 Treatment of complications (post-surgical) -unusual<br />
X<br />
circumstances, by report<br />
D9999 Unspecified adjunctive procedure, by report X 5<br />
May 2005 6.33<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
(*) If root canal treatment has been provided, a postoperative endodontic x-radiograph showing all apices is also required.<br />
(1) A report is required detailing the member’s condition.<br />
(2) Radiographs, charting and diagnosis are required for members under age 19.<br />
(4) A copy of the laboratory bill should also be submitted if available.<br />
(5) Radiographs may be required depending upon the treatment described.<br />
(6) Single inlays are routinely processed as an alternate benefit of a basic restoration. For groups not applying the alternate benefit, diagnostic materials<br />
are required for review.<br />
(7) Cast post and cores are routinely processed as an alternate benefit of a prefabricated post and core.<br />
(8) Pretreatment x-rays and specific rationale supporting the need for removal are required for members age 14 and younger and 31 and older.<br />
May 2005 6.34<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association
Section<br />
CLAIM SUBMISSION GUIDELINES<br />
U<br />
nited <strong>Concordia</strong> strongly suggests you submit claims electronically. Electronically submitted<br />
claims are processed faster than paper claims and that means faster reimbursement to you.<br />
Refer to Electronic Claim Submission section for more information. If you choose to submit<br />
paper claims, you should use an ADA standard format claim form. Submitting your claim on an<br />
ADA standard format claim form to the appropriate address will help ensure that your claim will<br />
be received in the appropriate area for processing. A claim form can be downloaded from our<br />
website.<br />
Always print or type the necessary information on the claim form. Clear, concise reporting will<br />
help avoid misunderstanding or misinterpretation of this information. Please check to be sure you<br />
have filled out the claim form completely. Claims submitted with missing information will cause a<br />
delay in processing.<br />
Completing the Claim Form<br />
o complete a <strong>United</strong> <strong>Concordia</strong> dental claim form, refer to the instructions below.<br />
T<br />
Fields 1-15 may be filled out by the dentist or by the family member who is receiving dental care.<br />
1. Patient’s Name: Enter last name, first name, and middle initial of the person being<br />
treated.<br />
2. Relationship to Subscriber: Enter the patient’s relationship to the subscriber, e.g., child<br />
or spouse.<br />
3. Sex: Check the appropriate box.<br />
4. Date of Birth: Enter the month, day, and year of the patient’s birth. Be sure the birth<br />
date is correct.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.1
5. If Student: Please indicate whether the patient is a student, the name of the school, and<br />
the city in which the school is located.<br />
6. Subscriber’s Name: Enter the first name, middle initial, and last name of the subscriber.<br />
8. Subscriber’s Mailing Address: Please enter the home address of the subscriber. Indicate<br />
city, state, and zip code.<br />
9. Contract ID: Enter the subscriber’s contract ID number.<br />
10. Employer: Enter Employer (company) name and address.<br />
11. Group Number: Enter Employer’s group number.<br />
12. Location: The location of the home office of the group may be entered here.<br />
13. Are Other Family Members Employed?: It is only necessary to complete this section if<br />
another family member also has coverage. Please include their Employer’s name along<br />
with the other family member’s contract ID number.<br />
14. Name & Address of Employer in Item #13: Again, it is only necessary to complete this<br />
section if you completed item 13.<br />
15. Is the Patient Covered by Another <strong>Dental</strong> Plan?: Check “No” if the patient has no<br />
other dental insurance. If the patient has additional dental insurance, please check “Yes”<br />
and include the plan name, the social security number of the contract holder, the group<br />
number, and the address of the other carrier.<br />
Note: The area below field 14 is to be signed if the family member, parent, or guardian assigns payment of<br />
benefits to the dentist. Because participating dentists receive payment directly from UCCI, they do not need to<br />
obtain the patient’s signature in this area. However, the patient must always sign the area under field 15. If<br />
the family member is under 18 years old, the parent or guardian must sign the form.<br />
Dentists should complete all fields from 16 through the end of the form.<br />
16. Dentist Name: Enter your name here. If you bill through a group practice account that<br />
has been approved by UCCI, the group practice name should be entered in this field. To<br />
the right of your name, please list your <strong>United</strong> <strong>Concordia</strong> provider number.<br />
17. Mailing Address: Enter the dentist’s office mailing address.<br />
18. Dentist SS# or T.I.N.: Enter the dentist’s social security number or Tax<br />
Identification Number.<br />
19. Dentist License Number: Please include the number shown on the treating dentist’s<br />
license.<br />
20. Dentist Phone Number: Enter the dentist’s office phone number, complete with the<br />
three-digit area code.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.2
21. First Visit Date: Enter the initial treatment date if the services reported on the claim are<br />
part of a larger treatment plan.<br />
22. Place of Treatment: Enter where the patient was treated, i.e., in the office, in the<br />
hospital, in an emergency care facility, or in another location.<br />
23. Radiographs and/or Documentation Enclosed?: Please check Yes or No to indicate<br />
whether x-rays or any documentation is enclosed. If x-rays are enclosed, please indicate<br />
how many.<br />
24. Is Treatment the Result of Occupational Illness or Injury?: Mark Yes if the treatment<br />
was a result of work-related injury and include a brief description of injury and the date it<br />
occurred. Check No if the treatment was not required due to occupational illness or<br />
injury.<br />
25. Is Treatment the Result of Auto Accident?: Mark Yes or No to indicate whether the<br />
treatment is a result of an auto accident. If Yes, please include the date of the accident<br />
along with the state that the accident occurred in.<br />
26. Other Accident?: If treatment is due to some other type of accident, please check Yes<br />
and indicate the date and nature of this accident.<br />
27. Are Any Services Covered by Another Plan?: If the services are covered by another<br />
plan, e.g., Auto, Homeowners, etc., please mark Yes and list the name and policy number<br />
of the other plan.<br />
28. If Prosthesis, is this the Initial Placement?: Mark Yes or No. If No, please include a<br />
reason for the replacement and a date (field 29) of the previous placement.<br />
30. Is Treatment for Orthodontics?: If the family member is seeking treatment related to<br />
orthodontics, please mark Yes. Please include appliance insertion date and estimated total<br />
length of active treatment from the date of banding or appliance placement to case<br />
completion.<br />
31-32. Treatment Specifics Should be Entered in this Section: Please use a separate line for<br />
each service provided and billed. Do not combine services and/or fees. When describing<br />
treatment, enter the universal tooth number for permanent teeth (1-32) or tooth letter for<br />
primary teeth (A-T), surface of the tooth, description of services, and the month, day, and<br />
year the services were completed. Enter the current five-digit alphanumeric CDT<br />
procedure code and fee for each procedure. For predeterminations, enter all information<br />
except date of service. NOTE: If there is no date listed and there is no indication<br />
that services are for predetermination, we will consider the date the claim was<br />
signed as the date of service.<br />
Dentist’s Signature: The treating dentist or authorized representative must sign here.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.3
Claim Filing Deadline<br />
e recommend that you send the claim form to <strong>United</strong> <strong>Concordia</strong> as soon as possible after<br />
W<br />
the service is completed, typically within 60 days of the date of service. (Timely filing<br />
deadlines may vary by contract.) Claims submitted more than 12 months after the month in which<br />
the service was provided will be denied.<br />
Contract ID Number<br />
ue to Federal and State Laws, <strong>United</strong> <strong>Concordia</strong> has taken steps to protect our member's<br />
D<br />
privacy and reduce potential for identity theft. One of the steps we have taken is redacting<br />
our member's social security numbers when the social security number is our member's contract<br />
identification number. In most states we are redacting the social security numbers by replacing all<br />
numbers except for the last four numbers of the social security number with X's (XXX-XX-1234).<br />
However, some states require the entire number to be replaced with X's (XXX-XX-XXXX) and<br />
other states require removing the number completely on all communications including the<br />
member's <strong>Dental</strong> Insurance Identification card. And to make things even more confusing, some of<br />
our customers require the use of unique identification numbers that are not the members' social<br />
security number.<br />
While insurers have to protect their member's social security numbers to be compliant with state<br />
and federal laws, it is becoming more difficult for a provider to know what identification number<br />
to report when submitting a claim. However, it is just as important that you report the correct<br />
identification number when submitting claims to ensure the privacy of your patient's records.<br />
Reporting an incorrect identification number could cause your patient's protected health<br />
information to be sent to another <strong>United</strong> <strong>Concordia</strong> member as the number reported could be a<br />
valid contract identification number for another of our members.<br />
In order to protect your patient's information, it is important to submit the correct identification<br />
number and here's how:<br />
• Ask for your patient's current <strong>Dental</strong> Insurance Identification card and verify with them<br />
that the information is correct and valid.<br />
• If the identification number is reported on the card as XXX-XX-XXXX report the<br />
insured's Social Security Number.<br />
• If the identification number is reported on the card as XXX-XX-last 4 numbers of<br />
Insured's Social Security Number, report all 9 numbers of the insured's Social Security<br />
Number (do not report any X's).<br />
• If no number is reported on the identification card, report all 9 numbers of the insured's<br />
Social Security Number.<br />
• If a number is reported on the identification card report the entire number including any<br />
letters as the insured's identification number. (Unique member identification numbers<br />
often have one or more letters within the number).<br />
If you have any doubts about having the correct identification number on file, you can verify your<br />
patient's eligibility through "My Patients’ Benefits" which is available on our website. Simply click<br />
on the Dentist button at the top of our home page and select "My Patients’ Benefits".<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.4
Signature Requirements<br />
entists and patients should sign all claim forms submitted to <strong>United</strong> <strong>Concordia</strong> for services<br />
D<br />
rendered to <strong>United</strong> <strong>Concordia</strong> subscribers. Failure to supply the necessary signature may<br />
result in delayed payment or denial of the claim. Therefore, it is important for you to review the<br />
following information to assure that claims submitted to <strong>United</strong> <strong>Concordia</strong> are in compliance with<br />
these requirements. There are three important signature fields on claims submitted to <strong>United</strong><br />
<strong>Concordia</strong>:<br />
q<br />
q<br />
q<br />
Treatment Plan / Release of Information<br />
Assignment of Benefits<br />
Dentist’s Signature<br />
Treatment Plan / Release Of Information<br />
here are two acceptable methods for completing this field:<br />
T<br />
Option 1 Patient or Guardian Signature: If the patient has reviewed the treatment plan<br />
and authorizes the release of information related<br />
to their claim, please have the patient or guardian<br />
sign his or her full name.<br />
Option 2 Signature On File:<br />
<strong>United</strong> <strong>Concordia</strong> will also accept the phrase<br />
“signature on file” entered in this field. Please<br />
remember if you wish to use this method, you<br />
must obtain a release from the patient using the<br />
text as found in the signature block and retain<br />
the release in the patient’s file.<br />
Assignment of Benefits<br />
f you are a participating dentist, it is not necessary to have the patient’s signature or “signature<br />
I<br />
on file” entered in this block. Claim payments will automatically be mailed to the participating<br />
dentist.<br />
If you are a non-participating dentist, you can receive direct payment in certain states on an<br />
individual contract basis. You must obtain the patient’s signature or use “signature on file” to<br />
receive direct payment. Payment will be issued to the patient if the "Assignment of Benefits"<br />
block is not completed. When using “signature on file” in this field, you must obtain a release<br />
from the patient directing payment to you. This statement is in addition to the statement necessary<br />
for release of information. (See Treatment Plan / Release of Information for more details.)<br />
Dentist’s Signature<br />
he treating dentist or his/her authorized representative should sign the claim form. We can<br />
T<br />
also accept a computer-scanned signature or stamped facsimile.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.5
Supporting Documentation<br />
entists are requested to submit duplicate radiographs used for diagnosis and treatment<br />
D<br />
planning when submitting claims for certain services. The radiographs should be of<br />
diagnostic quality, mounted and identified with the dentist’s name and address, as well as the<br />
patient’s name. Also include the date the radiographs were taken. If a copy of the radiographs is<br />
submitted, left or right should be marked on the copy. Duplicate radiographs will be returned only<br />
when a request to return is included with the claim.<br />
The following is a list of procedures that require radiographs for review (refer to the Diagnostic<br />
Materials Requirements Chart in the Policies, Limitations and Exclusions Section for a detailed<br />
listing):<br />
q<br />
q<br />
q<br />
Single crowns, inlays, onlays, cast post and cores, prefabricated posts and cores, bridges, crown<br />
build-ups - pretreatment radiographs. If single or abutment crowns, post and cores, or crown<br />
build-ups are to be placed on teeth which have been treated endodontically, a post-treatment<br />
radiograph of the completed root canal therapy is also required.<br />
Incomplete Root Canal - pretreatment and working radiographs along with a narrative.<br />
Gingivectomies, mucogingival procedures, osseous surgery, bone replacement grafts, guided<br />
tissue regeneration - pretreatment radiographs of the entire mouth, perio-charting and<br />
diagnosis.<br />
Note: It is <strong>United</strong> <strong>Concordia</strong>’s intent to request only those radiographs that are generally taken as<br />
part of diagnosis and treatment planning. If, for some reason, the radiographs listed were not<br />
taken or are not available, a brief explanation should be included with the claim.<br />
If <strong>United</strong> <strong>Concordia</strong> requires more information than originally provided with the claim form, we<br />
will contact you by telephone or by letter. Responding promptly to information requests will<br />
ensure processing of the claim is not delayed.<br />
Other Supporting Documentation<br />
ccasionally, additional supporting documentation is necessary. Below is a list of additional<br />
O<br />
q<br />
information that must be documented on the claim form:<br />
Orthodontic claims - indicate the total fee and estimated length of treatment.<br />
q<br />
q<br />
Coordination of Benefits claims - indicate the amount paid by the primary insurance company<br />
and provide a copy of the primary <strong>Dental</strong> Explanation of Benefits (DEOB).<br />
“By report” procedure - include a brief narrative statement explaining why the service was<br />
necessary and/or any unusual circumstances.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.6
Third Party Liability (TPL)<br />
hen a dental procedure is necessary due to an accident, e.g. job related, automotive, etc., the<br />
W<br />
claim must be reviewed for possible Third Party Liability. When submitting TPL claims,<br />
please document as much information as possible about the accident. Please be aware that there<br />
may be an additional delay while <strong>United</strong> <strong>Concordia</strong> contacts the patient for additional information<br />
for TPL.<br />
Requesting Predeterminations<br />
nited <strong>Concordia</strong> encourages the use of predeterminations to determine the extent of coverage<br />
U<br />
for a proposed course of treatment.<br />
This allows both you and the member to know if the proposed service(s) will be covered and the<br />
anticipated amount of payment by <strong>United</strong> <strong>Concordia</strong> before treatment. The results will be<br />
communicated to both the member and the dentist through a DEOB. <strong>United</strong> <strong>Concordia</strong> suggests<br />
predetermination of benefits for the following non-emergency types of treatments, including<br />
onlays, single crowns, prosthetics, periodontics, orthodontics, and oral surgery services.<br />
To request predetermination, the dentist or the member must submit a dental claim form and<br />
indicate on the form, by checking the appropriate box, that predetermination is being requested. A<br />
claim form may contain both requests for payment lines and predetermination lines. No dates of<br />
service should be reported on those line items for which predetermination is being requested. The<br />
predetermination claim will be processed in accordance with <strong>United</strong> <strong>Concordia</strong> benefits,<br />
exclusions, and limitations.<br />
Once the predetermination is finalized, <strong>United</strong> <strong>Concordia</strong> will notify both the member and dentist.<br />
A predetermination is not a guarantee of payment but indicates how much would be<br />
payable given the information available to <strong>United</strong> <strong>Concordia</strong> at the time the determination<br />
is processed. When the predetermined services have been provided, use one of the following<br />
methods to request payment.<br />
q<br />
q<br />
q<br />
Electronic Claims – Simply include the claim number printed on the Predetermination<br />
Notification and Request for Payment Form in the remarks field of your electronic claim<br />
request for payment.<br />
Telephone Access via the Interactive Voice Response (IVR) System - Begin by calling<br />
the toll-free IVR system at 1-800-332-0366. The automated system will ask for the date of<br />
service (MM/DD/CCYY), along with the following information, which may be found on the<br />
Predetermination Notification and Request for Payment Form: <strong>United</strong> <strong>Concordia</strong> Provider<br />
Number, Subscriber’s Contract ID Number, Patient’s Birth Month and Year (MM/CCYY) and<br />
Claim Number. The entry process generally takes only 20 seconds.<br />
Return via Mail - Mail the form titled <strong>Dental</strong> Predetermination Notification and Request for<br />
Payment to <strong>United</strong> <strong>Concordia</strong> with the completed date(s) of service(s) entered in the ‘Service<br />
Date(s)’ column. Dates should only be entered if the service has been completed. Do not<br />
attach additional claim forms to the <strong>Dental</strong> Predetermination Notification and Request for<br />
Payment Form if submitting a request for payment via mail. Submitting a new claim form may<br />
delay payment or possibly result in unnecessary requests for supporting documentation.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.7
A <strong>United</strong> <strong>Concordia</strong> predetermination will remain valid for 12 months from the date of<br />
finalization. The <strong>Dental</strong> Predetermination Notification and Request for Payment form contains<br />
the date that the predetermination is approved through. Services performed after the approval<br />
has expired will be subject to another review and should be submitted with the appropriate<br />
radiographs and supporting documentation for payment consideration.<br />
Predetermination and Coordination of Benefits<br />
nited <strong>Concordia</strong> is unable to make a COB determination on claims submitted for<br />
U<br />
predetermination. If predetermination is requested, a benefit determination will be made as<br />
though no other insurance existed. Secondary liability will be determined only when the services<br />
are completed and the claim is submitted for payment.<br />
Orthodontic Services<br />
rthodontic treatment is covered under the orthodontic portion of the <strong>Dental</strong> Benefits Program<br />
O<br />
when all the following conditions exist:<br />
1) The patient has orthodontic coverage.<br />
2) The orthodontic treatment is for the correction of a handicapping malocclusion.<br />
3) The orthodontic treatment involves appliance therapy.<br />
It is important that you review the Orthodontic Benefits prior to billing <strong>United</strong> <strong>Concordia</strong> for<br />
orthodontic services. Understanding this information will help ensure timely and accurate payment<br />
for your orthodontic services.<br />
Treatment plans are based upon the type of dentition involved – transitional, adolescent, or adult.<br />
Limited Orthodontic Treatment<br />
D8010 Limited orthodontic treatment of the primary dentition<br />
D8020 Limited orthodontic treatment of the transitional dentition<br />
D8030 Limited orthodontic treatment of the adolescent dentition<br />
D8040 Limited orthodontic treatment of the adult dentition<br />
Interceptive Orthodontic Treatment – Phase I<br />
D8050 Interceptive orthodontic treatment of the primary dentition<br />
D8060 Interceptive orthodontic treatment of the transitional dentition<br />
Comprehensive Orthodontic Treatment – Phase II<br />
D8070 Comprehensive orthodontic treatment of the transitional dentition<br />
D8080 Comprehensive orthodontic treatment of the adolescent dentition<br />
D8090 Comprehensive orthodontic treatment of the adult dentition<br />
Minor Treatment to Control Harmful Habits<br />
D8210 Removable appliance therapy<br />
D8220 Fixed appliance therapy<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.8
Policies and Limitations for Orthodontic<br />
Procedures<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Initial payment for orthodontic services will not be made until a banding date has been<br />
submitted to <strong>United</strong> <strong>Concordia</strong>.<br />
Payment for diagnostic services performed in conjunction with orthodontics is applied to the<br />
patient’s annual/lifetime orthodontic maximum.<br />
All retention and case finishing procedures are integral to the total case fee.<br />
Observations and adjustments are integral to the payment for retention appliances.<br />
Repair of damaged orthodontic appliances is not covered.<br />
The replacement of a lost or missing appliance is not a covered benefit.<br />
Periodic orthodontic treatment visits are considered an integral part of a complete orthodontic<br />
treatment plan and are not reimbursable as a separate service.<br />
Recementation of an orthodontic appliance is not covered.<br />
Payment for Orthodontic Services<br />
Payment Mechanism<br />
Orthodontic payments are generally based on the anticipated length of treatment. If the length<br />
of treatment is six months or less, <strong>United</strong> <strong>Concordia</strong>’s allowance will be made in one payment.<br />
Under certain circumstances, lump sum payments may be made on treatment plans over 6<br />
months in length if <strong>United</strong> <strong>Concordia</strong>’s total liability is $1000 or less. In most cases,<br />
orthodontic treatment will involve an initial payment, followed by monthly/quarterly<br />
payments. The monthly/quarterly payments are processed automatically, no further claims are<br />
required. Contractual and/or group specific exceptions may apply.<br />
Payments for Orthodontic Services are generally issued as follows:<br />
q<br />
q<br />
Twenty-five percent of the total amount payable by <strong>United</strong> <strong>Concordia</strong> will be paid upon<br />
placement of the bands or appliance as the initial payment.<br />
The remaining 75 percent is paid by <strong>United</strong> <strong>Concordia</strong> in equal monthly/quarterly payments,<br />
and one final payment based on the estimated length of the treatment and the patient’s<br />
benefits.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.9
q<br />
q<br />
The subscriber/patient must be enrolled with <strong>United</strong> <strong>Concordia</strong> during each month/quarter<br />
that payment is made.<br />
Monthly/quarterly payments are automatically processed. It is not necessary to submit<br />
claims for monthly/quarterly payments.<br />
Orthodontic Lifetime Maximum<br />
ll orthodontic payments are typically subject to the patient’s annual/lifetime orthodontic<br />
A<br />
maximum. If the patient’s orthodontic maximum has been met prior to the completion of<br />
the payment schedule, further payments are discontinued. (This may occur if more than one<br />
dentist submitted orthodontic claims for the same patient.)<br />
Orthodontic Treatment “In Progress”<br />
New Enrollee<br />
The subscriber/patient must be enrolled on the date of banding or appliance placement to receive<br />
payment for these services. If the patient is enrolled after appliance placement, they may be eligible<br />
to receive monthly/quarterly payments for treatment “in progress.”<br />
As soon as the patient becomes eligible for <strong>United</strong> <strong>Concordia</strong> orthodontic benefits, you should<br />
submit a claim for the orthodontic treatment “in progress.” Be sure to include the diagnosis,<br />
treatment plan, total fee, banding or appliance date and estimated total duration of<br />
treatment on the claim (see example attached). UCCI then calculates the amount the plan will<br />
cover for the remaining treatment in monthly/quarterly payments. The <strong>Dental</strong> Explanation of<br />
Benefits (DEOB) indicates the amount the plan will cover for the remainder of the “in progress”<br />
treatment.<br />
Transferring from Another Dentist<br />
If the patient transfers to a different dentist, the new dentist must submit a claim to <strong>United</strong><br />
<strong>Concordia</strong> indicating the total remaining months of treatment, total fee, and the banding date if the<br />
patient was rebanded. Payment for services provided by the new dentist will be calculated based on<br />
the remaining orthodontic benefits and remaining length of treatment.<br />
Please remember:<br />
q<br />
q<br />
q<br />
It is the dentist’s and the patient’s responsibility to notify <strong>United</strong> <strong>Concordia</strong> <strong>Dental</strong> Customer<br />
Service at 1-800-332-0366 if orthodontic treatment is discontinued, completed sooner than<br />
anticipated, or if the patient transfers to another dentist.<br />
If you are rebanding the transfer patient, please indicate that the patient was rebanded and the<br />
rebanding date.<br />
If the patient was not rebanded, please indicate the date the new dentist assumed responsibility<br />
for the treatment plan.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.10
The following is an example of how to report an orthodontic treatment plan for a transfer patient<br />
that is rebanded:<br />
TRANSFER PATIENT THAT<br />
IS REBANDED<br />
Comprehensive Orthodontic<br />
Treatment<br />
2,000 00<br />
Patient Rebanded<br />
2 10 04<br />
8 months remaining<br />
The following is an example of how to report an orthodontic treatment plan for a transfer patient<br />
that is not rebanded:<br />
TRANSFER PATIENT NOT<br />
REBANDED<br />
Comprehensive Orthodontic<br />
Treatment<br />
1,500 00<br />
Patient Not Rebanded Take Over<br />
2 10 04<br />
10 months remaining<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.11
Billing Orthodontic Services<br />
he following instructions and sample forms will help you in preparing orthodontic claims and<br />
T<br />
understanding <strong>United</strong> <strong>Concordia</strong>’s payment for orthodontic services.<br />
Billing For New Orthodontic Patients<br />
lease submit a complete treatment plan for all <strong>United</strong> <strong>Concordia</strong> patients beginning<br />
P<br />
orthodontic treatment. It is best to file electronically. You may also use an ADA standard<br />
format claim form. Always print or type the necessary information when using a paper claim form.<br />
Clear, concise reporting on the claim will help avoid any misinterpretation of the information.<br />
Incorrect information may result in incorrect payment or claim denials. Since missing information<br />
may delay the processing of your claim be certain no information is omitted.<br />
Claims should be submitted to:<br />
<strong>United</strong> <strong>Concordia</strong> and Highmark Blue Shield Claims<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
Claims Processing<br />
PO Box 69421<br />
Harrisburg, PA 17106-9421<br />
Or<br />
DentaBenefits (Mutual of Omaha)<br />
DentaBenefits Claims Processing<br />
PO Box 69416<br />
Harrisburg, PA 17106-9416<br />
How to Complete a <strong>Dental</strong> Claim Form for New<br />
Orthodontic Patients<br />
lease adhere to the following guideline when completing a <strong>Dental</strong> Claim form:<br />
P<br />
q<br />
Use a separate line for each service being provided and billed.<br />
q<br />
q<br />
q<br />
Enter the five-digit alpha-numeric procedure code for each service.<br />
For predeterminations, enter all information, except the date of service.<br />
List diagnostic services using a separate line for each procedure. Enter the description of the<br />
service, date of service (if not predetermining), procedure code number, and fee charged. Use<br />
the amounts paid column, only if the subscriber has paid the dentist directly, and indicate the<br />
amount paid.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.12
q<br />
q<br />
List the total treatment plan as indicated by the appropriate procedure code. Report the total<br />
case fee, excluding diagnostic services. This fee should include retention and case finishing<br />
procedures that should not be reported or billed separately.<br />
Report the anticipated length of active treatment in months as well as the initial banding date if<br />
applicable. For reporting purposes, the length of estimated treatment should include the<br />
month the patient was banded.<br />
The following is an example of how to report an orthodontic treatment plan for new orthodontic<br />
patients:<br />
Orthodontic Evaluation<br />
Panoramic Film<br />
Cephalometric Film<br />
Diagnostic Casts<br />
2 10 04<br />
2 10 04<br />
2 10 04<br />
2 10 04<br />
D0150<br />
D0330<br />
D0340<br />
D0470<br />
25 00<br />
46 00<br />
50 00<br />
25 00<br />
Comprehensive Orthodontic<br />
Treatment<br />
D8080 3,500 00<br />
Estimated Length of Treatment –<br />
24 Months<br />
Banding Date<br />
Billing for A Patient Whose Orthodontic<br />
Treatment “In-Progress” Has Not Been<br />
Previously Paid By Another Insurance Carrier<br />
he following instructions are applicable to patients who have not had previous dental<br />
T<br />
coverage, and who had orthodontic treatment initiated prior to becoming eligible for<br />
orthodontics. Please prepare a complete treatment plan following the same guidelines specified for<br />
new patients, except for the following:<br />
q<br />
q<br />
Do not list any services rendered before the patient became eligible. This will usually<br />
include diagnostics. A banding date will be required to determine the number of<br />
months prior to coverage.<br />
On the <strong>Dental</strong> Claim form, list the following information:<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.13
1. Starting date of treatment (banding date).<br />
2. The total treatment plan as indicated by the appropriate procedure code. On this<br />
line also include total case fee, excluding diagnostics. This fee includes retention<br />
and case finishing procedures that should not be listed or billed separately.<br />
3. Total length of treatment in months.<br />
The following is an example of how to report a treatment plan for orthodontic patients with<br />
treatment in progress:<br />
Initial Banding Date<br />
2 10 05<br />
Comprehensive Orthodontic<br />
Treatment<br />
D8080 3,500 00<br />
Total Length of Treatment –<br />
24 Months<br />
Orthodontic Inquiries<br />
hould you have any questions regarding <strong>United</strong> <strong>Concordia</strong>’s determination of payment to you,<br />
Scontact <strong>Dental</strong> Customer Service at 1-800-332-0366.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
7.14
Check One<br />
<br />
<br />
Dentist's pre-treatment estimate<br />
Please submit claim to: <strong>Dental</strong> Claims<br />
Dentist's statement of actual services<br />
P.O. Box 69421<br />
Harrisburg, PA 17106-9421<br />
1. Patient name 2. Relationship to employee<br />
self spouse child other<br />
3. Sex<br />
m f<br />
4. Patient birthdate<br />
mo day year<br />
5. If full time student<br />
school<br />
city<br />
P<br />
A<br />
T<br />
I<br />
E<br />
N<br />
T<br />
6. Employee/subscriber name<br />
First middle last<br />
8. Employee/subscriber mailing address<br />
City, State, Zip<br />
9. Contract ID #<br />
10. Employer (company) name and address<br />
S<br />
E<br />
C<br />
T<br />
I<br />
O<br />
N<br />
D<br />
E<br />
N<br />
T<br />
I<br />
S<br />
T<br />
S<br />
E<br />
C<br />
T<br />
I<br />
O<br />
N<br />
11. Group Number 12. Location (Local) 13. Are other family members employed?<br />
Employee name Contract ID #<br />
15. Is patient covered by<br />
another dental plan?<br />
I have reviewed the following treatment plan. I authorize release of any information relating to<br />
this claim. I understand that I am responsible for all costs of dental treatment.<br />
17. Mailing address<br />
City, state, zip<br />
18. Dentist soc. sec. or T.I.N.<br />
21. First visit date<br />
current series<br />
TOOTH<br />
NO. OR<br />
LETTER<br />
<strong>Dental</strong> plan name<br />
SURFACE<br />
DESCRIPTION OF SERVICES<br />
(INCLUDING X-RAYS, PROPHYLAXIS, MATERIALS USED,ETC.)<br />
LINE NO.<br />
I hereby authorize payment directly to the below name dentist of the group insurance benefits<br />
otherwise payable to me.<br />
Signature (patient or parent if minor)<br />
Date<br />
Signature (insured person)<br />
Date<br />
The signer agrees that any personally identifiable health information about the signer or signer's enrolled dependents is protected by the Health Insurance Portability and Accountability Act of 1996 and other privacy laws. In<br />
accordance with those laws, <strong>United</strong> <strong>Concordia</strong> may use and disclose Protected Health Information for treatment, payment and health care operations as described in its Notice of Privacy Practices.<br />
16. Dentist name<br />
24. Is treatment result No Yes If yes, enter brief description and dates<br />
of occupational<br />
illness or injury?<br />
Identify missing teeth<br />
with "X"<br />
19. Dentist license no. 20. Dentist phone no.<br />
22. Place of treatment<br />
Office Hosp. ECF Other<br />
Union local<br />
Group no.<br />
23. Radiographs or No Yes How<br />
models enclosed? Many?<br />
Name and address of carrier<br />
25. Is treatment result<br />
of auto accident?<br />
26. Other accident?<br />
27. Are any services<br />
covered by<br />
another plan?<br />
28. If prosthesis, is<br />
this initial<br />
placement?<br />
30. Is treatment for<br />
orthodontics?<br />
14. Name and address of employer in item 13<br />
DATE SERVICE<br />
PERFORMED<br />
MO. DAY YR.<br />
(If no, reason for replacement)<br />
If services<br />
already<br />
commenced<br />
enter<br />
31. Examination and treatment plan-list in order from Tooth No. 1 through Tooth No. 32 - Use charting system shown.<br />
PROCEDURE<br />
CODE<br />
Date appliances placed<br />
Use charting<br />
system shown<br />
FEE<br />
29. Date of prior<br />
placement<br />
Mos. treatment<br />
remaining<br />
FOR<br />
ADMINISTRATIVE<br />
USE ONLY<br />
I hereby certify that the procedures as indicated by date have been completed and that the fees submitted are the actual fees I have charged<br />
and intend to collect for those procedures.<br />
Signature (Dentist)<br />
Date<br />
TOTAL<br />
FEE<br />
CHARGED<br />
Any person who knowingly and with intent to defraud any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals for the purpose of misleading,<br />
information concerning any fact material thereto, commits a fraudulent insurance act which is a crime and subjects such person to criminal and civil penalties.<br />
Arizona: For your protection Arizona law requires the following statement to appear on this form. Any person who knowingly presents a false or fraudulent claim for payment of a loss is subject to criminal and civil penalties.<br />
California: For your protection California law requires that the following appear on the form: Any person who knowingly presents a false claim for the payment of a loss is guilty of a crime and may be subject to fines and confinement<br />
in state prison.<br />
Florida: Any person who knowingly, and with intent to injure, defraud, or deceive any insurer files a statement of claim or an application containing any false, incomplete or misleading information is guilty of a felony in the third<br />
degree.<br />
New Jersey: Any person who knowingly files a statement of claim containing any false or misleading information is subject to criminal and civil penalties.<br />
New York: Any person who knowingly and with intent to defraud any insurance company or other person files an application for insurance or statement of claim containing any materially false information, or conceals for the purpose<br />
of misleading, information concerning any fact material thereto, commits a fraudulent insurance act, which is a crime, and shall also be subject to a civil penalty not to exceed five thousand dollars and the stated value of<br />
the claim for each such violation.<br />
Louisiana: Any person who knowingly presents a false or fraudulent claim for payment of a loss or benefit or knowingly presents false information in an application for insurance is guilty of a crime and may be subject to fines and<br />
confinement in prison.<br />
Virginia: Any person who within the intent to defraud or knowing that he is facilitating a fraud against an insurer, submits an application or files a claim containing a false or deceptive statement may have violated the state law.<br />
Tennessee: It is a crime to knowingly provide false, incomplete or misleading information to an insurance company for the purpose of defrauding the company. Penalties include imprisonment, fines and denial of insurance benefits.<br />
5574 G 8/04
Section<br />
ELECTRONIC CLAIMS SUBMISSION<br />
U<br />
nited <strong>Concordia</strong> provides dentists with state-of-the-art systems for claims submission and<br />
administration.<br />
Dentists can submit claims/encounters electronically to <strong>United</strong> <strong>Concordia</strong> by using either of the<br />
following methods:<br />
q<br />
q<br />
Xpress Claim – Participating and non-participating dentists can submit FREE<br />
claims/encounters electronically to <strong>United</strong> <strong>Concordia</strong> using Xpress Claim. If you have<br />
Internet access and version 5.0 or greater web browser, you can use Xpress Claim to submit<br />
claims directly to <strong>United</strong> <strong>Concordia</strong> for FREE paperless processing! This real-time<br />
processing feature provides you with immediate processing results. You can also run daily<br />
reports summarizing your practice’s activities including the number of claims and<br />
encounters submitted, finalized and/or pending. You can obtain immediate access to<br />
Xpress Claim by registering on our website.<br />
Electronic Data Interchange (EDI) – In addition to Xpress Claim, electronic<br />
claims/encounters can be submitted to <strong>United</strong> <strong>Concordia</strong> through a clearinghouse or<br />
billing service that collects the claims from your office and forwards them to <strong>United</strong><br />
<strong>Concordia</strong>. Also, electronic claims can be submitted directly to us if your practice<br />
management software allows for a direct connection to <strong>United</strong> <strong>Concordia</strong>. For more<br />
information on direct electronic claims/encounters submission or to receive a listing of<br />
the software vendors, billing services, and clearinghouses that are currently in production<br />
with <strong>United</strong> <strong>Concordia</strong>, please call <strong>Dental</strong> Electronic Services at 1-800-633-5430.<br />
<strong>Dental</strong> Electronic Services has established agreements with the following clearinghouses<br />
or vendors to provide free or reduced fees for electronic claims submission.<br />
- PracticeWorks, Inc. – A subsidiary of Eastman Kodak Company (1-800-262-8593)<br />
- WebMD <strong>Dental</strong> Services (1-888-416-0673)<br />
- EDI – Health Group, LLC (1-800-576-6412)<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
8.1
- Quality Systems, Inc. (1-949-255-2600)<br />
- BRS Computing LLC (1-914-747-0201)<br />
- Tesia – PCI Corporation (1-800-724-7240)<br />
- Affililiated Network Services (ANS) (1-312-236-6616)<br />
To find out more about how these clearinghouses/vendors can assist your office in making the<br />
electronic link to <strong>United</strong> <strong>Concordia</strong>, contact them directly at the telephone numbers listed.<br />
* Vendors and offers are valid as of the publication date and are subject to change.<br />
Benefits of Submitting Claims Electronically<br />
here are a number of significant benefits to submitting claims/encounters electronically:<br />
T<br />
q<br />
Elimination of paperwork and postage costs: By submitting claims electronically, you can<br />
eliminate the staff time and postage costs required to prepare and mail paper claims.<br />
q Accessibility: Except during routine system maintenance, you can submit claims<br />
electronically 24 hours a day and 7 days a week.<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Improve cash flow: Paper claims usually require a week or more for mailing and<br />
administrative handling before processing begins. Electronic claims frequently process to<br />
completion on the same day they are received. Faster receipt and processing of your claim<br />
means faster payment to you.<br />
Accuracy: Because electronic claims are entered directly into <strong>United</strong> <strong>Concordia</strong>’s automated<br />
claims processing system, your claims process more quickly and the chance of processing<br />
errors is significantly reduced.<br />
Flexibility: You control the frequency and volume of submission.<br />
Dedicated support personnel: <strong>United</strong> <strong>Concordia</strong> has a department dedicated to supporting<br />
electronic claim billers known as <strong>Dental</strong> Electronic Services (DES). The members of this<br />
department provide information about electronic services available with <strong>United</strong> <strong>Concordia</strong>,<br />
assist throughout the testing process, and supply ongoing support during the production<br />
phase.<br />
Security: Your computer files remain secure and confidential. The only data we can read are<br />
the claims that you send to us. You initiate the request to send us files; we can never call your<br />
computer or read the data in it.<br />
Electronic Reports: Detailed explanations of <strong>United</strong> <strong>Concordia</strong>’s reports are provided in this<br />
section.<br />
How Do I Submit Claims Requiring Attachments<br />
nited <strong>Concordia</strong> developed a hassle free process for submitting electronic claims and<br />
U<br />
attachments. This process saves dental offices time and money by accelerating processing<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
8.2
and eliminating the need for duplicating and mailing x-rays.<br />
<strong>United</strong> <strong>Concordia</strong> is working with National Electronic Attachment, Inc. (NEA) to receive dental<br />
attachments electronically, via FastAttach. This system enables approved electronic dental<br />
offices to transmit attachments (x-rays, perio charts, intra-oral pictures, narratives and EOB’s)<br />
using the Internet to NEA’s repository.<br />
<strong>United</strong> <strong>Concordia</strong> is able to access the repository and view the attachments required to adjudicate<br />
the electronically submitted claims. Please visit www.nea-fast.com for additional information or<br />
call National Electronic Attachment, Inc. at 1-800-782-5150.<br />
<strong>United</strong> <strong>Concordia</strong> is also working with Dentrix, a software vendor to receive electronic<br />
attachments. Dentrix has included the electronic attachment feature as part of their Practice<br />
Management system. This update allows dental offices to send electronic attachments (perio<br />
charts, x-rays or any other images) with electronic claims. Please visit www.nationalinfo.com for<br />
additional information or call National Information Services (NIS), the Dentrix eClaims service<br />
partner at 1-800-734-5561.<br />
Any questions concerning electronic claims submission may be directed to the <strong>Dental</strong> Electronic<br />
Services (DES) department at 1-800-633-5430, Monday through Friday from 8:30AM to 5:00PM<br />
ET.<br />
Reports<br />
With Xpress Claim, you will receive a daily report that summarizes your submissions.<br />
I<br />
f you send your electronic claims directly to <strong>United</strong> <strong>Concordia</strong>, you will receive a 997 Functional<br />
Acknowledgement Report and a 277CA Report. If you utilize a clearinghouse or billing service,<br />
these reports are sent to the clearinghouse that is then responsible for passing the report<br />
information back to your office. Listed below are the reports and a brief explanation of their<br />
purpose.<br />
997 Functional Acknowledgement Report<br />
f you bill directly to us, after you transmit a file of claims/encounters, you will receive a 997<br />
I<br />
Functional Acknowledgement Report which will tell you if we received your claims/encounters.<br />
If you use a clearinghouse or billing service, they receive the 997 Functional Acknowledgement<br />
Report from us.<br />
277 CA Claims Acknowledgement Report<br />
ithin 24 hours after your claims/encounters are submitted and accepted through the 997<br />
W<br />
Functional Acknowledgement Report process, they are subject to a set of edits in our<br />
computer system to make sure that all the information is reported correctly. The results of this edit<br />
check are outlined on the 277 Claims Acknowledgement Report, which indicates whether all, none<br />
or some of the claims were accepted. If the entire file or some of the claims are rejected, you must<br />
correct the errors identified and resubmit the file or corrected claims for processing.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
8.3
If you bill directly to us, it is necessary that you retrieve this report. If you use a clearinghouse or<br />
billing service, it is their responsibility to retrieve this report and pass it on to you.<br />
835 Healthcare Claim Payment/Advice Report<br />
nited <strong>Concordia</strong> provides a weekly 835 Healthcare Claim Payment/Advice Report to assist in<br />
U<br />
your accounts receivable process. Please contact <strong>Dental</strong> Electronic Services for more<br />
information on receiving this report.<br />
Some of the information contained in this report includes:<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
Provider number of the dentist or group receiving payment<br />
Patient’s name, patient control number, service rendered, date of service and billed<br />
charge<br />
Allowed amount for the service<br />
Actual payment made for the service<br />
Amount applied to the patient’s deductible, if applicable<br />
Check number and issue date<br />
Reason for rejection of denied service<br />
Remember to visit our website at www.unitedconcordia.com for more information<br />
regarding <strong>United</strong> <strong>Concordia</strong>’s electronic products and services.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
8.4
Section<br />
COORDINATION OF BENEFITS<br />
C<br />
oordination of Benefits (COB) applies when a member is covered by two or more group<br />
insurance policies. The purpose of COB is to allow members to receive the highest level of<br />
benefits they are entitled to, up to 100 percent of the cost of covered services. COB also ensures<br />
that no one collects more than the actual cost of his/her dental expenses.<br />
The program that takes precedence in the order of making payment is called the “primary plan."<br />
The program that is responsible for paying after the primary program is called the “secondary<br />
plan."<br />
Determining the Primary Plan<br />
nited <strong>Concordia</strong> follows these general guidelines for determining the primary plan.<br />
U<br />
q<br />
If a spouse has his/her own dental plan, the spouse’s plan would be considered primary and<br />
<strong>United</strong> <strong>Concordia</strong> would be secondary for services rendered to the spouse.<br />
q<br />
Dependent Child and the Birthday Rule – When children’s dental expenses are involved,<br />
<strong>United</strong> <strong>Concordia</strong> follows the “birthday rule.” The plan of the parent whose birthday falls<br />
earlier in the calendar year is the primary plan. If both parents have the same birthday, the<br />
plan that has covered either of the parents the longest is the primary plan. However, if the<br />
other plan follows the “gender rule” with male coverage always primary, <strong>United</strong> <strong>Concordia</strong> will<br />
follow the rules of that plan.<br />
In situations where the parents are divorced or separated and there are two dental plans,<br />
<strong>United</strong> <strong>Concordia</strong> considers the plan of the parent with custody to be the primary plan. If the<br />
parent with custody has remarried, the step-parent’s plan will be secondary and will pay before<br />
the parent without custody. If the parents have joint custody, the “birthday rule” will then<br />
apply. An exception to the custody rule occurs where there is a court decree specifying which<br />
parent is responsible for insurance coverage.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
9.1
However, if the court decree specifies both parents are responsible for the coverage, the<br />
“custody rule” will be applied. In situations where the parents are unmarried and living<br />
together, the “birthday rule” will apply. If the parents are unmarried and not living together,<br />
the “custody rule” will be applied.<br />
If you are uncertain which dental plan is the primary plan for the patient, contact the <strong>Dental</strong> Customer Service<br />
Department at 1-800-332-0366.<br />
Payment When UCCI is Primary<br />
hen <strong>United</strong> <strong>Concordia</strong> is the primary plan, payment is made for covered services without<br />
W<br />
regard to what the other plan might pay. The secondary plan then, depending upon its<br />
particular provisions and limitations may pay the amounts not covered by <strong>United</strong> <strong>Concordia</strong>.<br />
Because participating dentists have agreed to accept <strong>United</strong> <strong>Concordia</strong>’s allowance as payment in full<br />
for covered services, they should bill the secondary carrier for the patient’s coinsurance, any amounts<br />
exceeding the annual or lifetime maximums and/or any amounts applied towards the patient’s<br />
deductible or non-covered services.<br />
Payment When UCCI is Secondary<br />
hen <strong>United</strong> <strong>Concordia</strong> is secondary, payment is based on the amount that remains for each<br />
W<br />
covered service after the primary plan’s payment has been made. <strong>United</strong> <strong>Concordia</strong> will take<br />
into consideration the provider’s participation status with the primary plan. <strong>United</strong> <strong>Concordia</strong> will<br />
pay the lower of the amount for which the patient is still responsible after the primary carrier’s<br />
payment, or the amount that would have been paid if there were no other carrier involved.<br />
Example 1:<br />
Total bill for a periodontal procedure is $100.00. <strong>United</strong> <strong>Concordia</strong> allowance is $100.00. The<br />
dentist is non-participating with primary plan and submits a claim to <strong>United</strong> <strong>Concordia</strong> for $100.00<br />
with a <strong>Dental</strong> Explanation of Benefits (DEOB) from the primary plan.<br />
Step 1<br />
Step 2<br />
Step 3<br />
$100.00 <strong>United</strong> <strong>Concordia</strong> Allowance<br />
X 60% <strong>United</strong> <strong>Concordia</strong> Contracted Percentage<br />
---------<br />
$60.00 Amount Payable By <strong>United</strong> <strong>Concordia</strong> In Absence<br />
of Other Coverage<br />
$100.00 Billed Charge<br />
- $55.00 Paid by Primary Plan<br />
---------<br />
$45.00 Unpaid Balance<br />
<strong>United</strong> <strong>Concordia</strong> pays $45.00 since it is the lower of the two<br />
computations<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
9.2
Example 2:<br />
Total bill for a periodontal procedure is $100.00. <strong>United</strong> <strong>Concordia</strong> allowance is $100.00 and the<br />
primary plan paid $30.00. The dentist is non-participating with primary plan and submits a claim<br />
to <strong>United</strong> <strong>Concordia</strong> for $100.00 with a DEOB from the primary plan.<br />
Step 1<br />
Step 2<br />
Step 3<br />
$100.00 <strong>United</strong> <strong>Concordia</strong> Allowance<br />
X 60% <strong>United</strong> <strong>Concordia</strong> Contracted Percentage<br />
---------<br />
$60.00 Amount Payable By <strong>United</strong> <strong>Concordia</strong> In Absence<br />
of Other Coverage<br />
$100.00 Billed Charge<br />
- $30.00 Paid by Primary Plan<br />
---------<br />
$70.00 Unpaid Balance<br />
<strong>United</strong> <strong>Concordia</strong> pays $60.00 since it is the lower of the two<br />
computations. (<strong>United</strong> <strong>Concordia</strong> cannot pay more than it<br />
would have paid in absence of other insurance.)<br />
Example 3:<br />
Total bill for a periodontal procedure is $100.00. <strong>United</strong> <strong>Concordia</strong> allowance is $100.00 and the<br />
primary plan paid $30.00. The dentist submits a claim to <strong>United</strong> <strong>Concordia</strong> for $100.00 with a<br />
DEOB from the primary plan. The dentist is participating with the primary plan and has entered<br />
into an agreement to accept $70.00 as payment in full.<br />
Step 1<br />
Step 2<br />
$100.00 <strong>United</strong> <strong>Concordia</strong> Allowance<br />
X 60% <strong>United</strong> <strong>Concordia</strong> Contracted Percentage<br />
---------<br />
$60.00 Amount Payable By <strong>United</strong> <strong>Concordia</strong> In Absence<br />
of Other Coverage<br />
$100.00 Billed Charge<br />
$70.00 Contract Amount<br />
- $30.00 Paid by Primary Plan<br />
---------<br />
$40.00 Unpaid Balance<br />
Step 3<br />
<strong>United</strong> <strong>Concordia</strong> pays $40.00 since this is the unpaid portion of<br />
the contracted amount.<br />
When <strong>United</strong> <strong>Concordia</strong> is secondary, the claim should be sent to the primary plan first.<br />
Following the primary plan’s payment, a copy of the primary carrier’s DEOB should be sent with<br />
the claim to <strong>United</strong> <strong>Concordia</strong>.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
9.3
Section<br />
CLAIM REVIEW PROCESS<br />
U<br />
nited <strong>Concordia</strong> is responsible for ensuring that payment for services the members receive is<br />
appropriate and necessary. <strong>United</strong> <strong>Concordia</strong>’s dental review program helps fulfill this<br />
responsibility. This program consists of pre-payment and post-payment review. The pre-payment<br />
program is briefly described in the remainder of this section.<br />
Initial Review<br />
ll claims are initially reviewed by Claims Reviewers. Claims Reviewers may only approve<br />
A<br />
services for predetermination or payment. <strong>Dental</strong> services that cannot be approved based upon<br />
the initial review are forwarded to a Dentist Advisor Assistant who has the ability to approve cases<br />
that are more questionable. <strong>Dental</strong> services that cannot be approved based upon the review of the<br />
Dentist Advisor Assistant are referred to a Dentist Advisor. Final determination is based on the<br />
Dentist Advisor’s professional opinion.<br />
Professional Review by Dentist Advisors<br />
he Dentist Advisors provide professional opinions on patterns of practice and supply<br />
T<br />
professional input into the development of new claims processing procedures and policies.<br />
<strong>United</strong> <strong>Concordia</strong>’s Dentist Advisors are licensed dentists who represent the dental community at<br />
large. In addition to assisting <strong>United</strong> <strong>Concordia</strong> on a part time basis, all of the Dentist Advisors are<br />
engaged in active clinical practice. Among the Dentist Advisors are several general dentists, oral<br />
surgeons and periodontists.<br />
The Dentist Advisors render opinions by reviewing claims, reports, correspondence and diagnostic<br />
information such as radiographs. Following their review, the claim is processed based on the Dentist<br />
Advisor’s recommendation and the member’s dental benefits.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
10.1
Second Review<br />
f a participating provider or a member disagrees with the Dentist Advisor’s initial determination of<br />
I<br />
a claim, they may request a second review. (Refer to Appeals Section for more information).<br />
After receiving your request, we will present the case to a second Dentist Advisor for an independent<br />
evaluation and recommendation. You can arrange to have the Dentist Advisor contact you during<br />
the reconsideration. Following the reconsideration, we will inform you of our determination.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
10.2
Section<br />
PAYMENTS AND REQUESTS FOR<br />
INFORMATION<br />
<strong>Dental</strong> Explanation of Benefits<br />
he <strong>Dental</strong> Explanation of Benefits (DEOB) is a computer-generated statement that explains<br />
T<br />
how the claim was processed. The DEOB explains payment amounts, non-covered services,<br />
subscriber payment responsibility and co-insurance. If there is a co-insurance, you will need to bill<br />
that amount to your patient, as well as any costs for non-covered services.<br />
When <strong>United</strong> <strong>Concordia</strong> processes a claim for a member, a DEOB will be sent to the member.<br />
The member’s DEOB differs from the dentist’s in format. All participating dentists and nonparticipating<br />
dentists receive the DEOB. Please refer to an example of a DEOB at the end of this<br />
section.<br />
How to Read the DEOB<br />
Dentist Information<br />
At the top of the page, the following dentist information is indicated:<br />
1. Provider: The name of dentist who billed the service.<br />
2. TIN Number: Tax Identification Number as it appears on Federal 1099.<br />
3. Provider Number: <strong>United</strong> <strong>Concordia</strong>’s dentist identification number.<br />
4. Date: The date <strong>United</strong> <strong>Concordia</strong> generated the DEOB.<br />
5. Page: The number of pages in the Summary Payment Voucher.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
11.1
Patient Information<br />
6. Patient: The name of the member who received the listed services.<br />
7. Contract ID: Subscriber Identification Number.<br />
8. APPL/SUB Name: The name of the subscriber.<br />
Claim Information<br />
9. First date of service.<br />
10. Last date of service.<br />
11. Number of services reported for that procedure code.<br />
12. Place of service: The example provided lists “O”, the code for office. Other places of<br />
service include hospitals or emergency center facilities.<br />
13. Procedure code: Current ADA codes used to identify services performed by the dentist.<br />
14. Tooth numbers and surfaces: Identifies the teeth and surfaces that were treated.<br />
15. Provider charge: The amount the dentist charged for the procedure.<br />
16. Allowance: The amount <strong>United</strong> <strong>Concordia</strong> allows for the service reported.<br />
17. Non-chargeable amount: If services are performed by a participating dentist, the amount<br />
listed here will show the difference between the dentist’s charge and <strong>United</strong> <strong>Concordia</strong>’s<br />
allowance, as well as the amount for any non-billable services.<br />
18. Non-chargeable code: Indicates the reason for the non-chargeable amount and is explained<br />
in the message(s) section of the voucher.<br />
19. Subscriber liability amount: The amount the subscriber is responsible for such as<br />
deductible, coinsurance or the amount exceeding the maximum.<br />
20. Subscriber Liability Code: Identifies the nature of any dollar amounts for which the<br />
subscriber is liable. For example, C1 = Coinsurance.<br />
21. Other insurance amount: Amount paid by primary insurance when the subscriber or spouse<br />
has other dental insurance.<br />
22. Amount paid to provider: The amount <strong>United</strong> <strong>Concordia</strong> paid for the services to the dentist.<br />
23. Amount paid to the subscriber: The amount <strong>United</strong> <strong>Concordia</strong> paid to the subscriber.<br />
24. Message code: The code in this field matches the code in the explanation field at the bottom<br />
of the claim.<br />
25. Claim number: The identification number assigned to the claim by <strong>United</strong> <strong>Concordia</strong> for<br />
internal processing purposes.<br />
26. Totals and Narrative Information: Following the second table, a summary of DEOB totals,<br />
total subscriber payments, total provider payments and payment number will be listed.<br />
Narrative information provides explanations of any message codes, non-chargeable amount<br />
codes and subscriber liability codes listed in the fields above.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
11.2
Requests for Additional Information<br />
nited <strong>Concordia</strong> may request additional information to expedite the review and processing of a<br />
U<br />
claim and determine the appropriate level of benefits by letter or a phone call. The letter will<br />
reference the claim in question and will include the procedures listed on the original claim. The letter<br />
should be returned to the address provided, as soon as possible, with the requested information<br />
noted on the appropriate line(s) or with additional information attached. Failure to do so may result<br />
in the claim being denied.<br />
q<br />
In some instances, claims missing essential data elements may be denied as an incomplete claim.<br />
If this occurs, the denied services should be resubmitted to <strong>United</strong> <strong>Concordia</strong> with all essential<br />
information included.<br />
Changing or Combining Reported Procedure<br />
Codes<br />
n the process of administering <strong>United</strong> <strong>Concordia</strong> dental policies, there are occasions when the<br />
I<br />
reported procedure code may be changed or unbundled procedures may be recoded as a single<br />
complete procedure.<br />
Listed below are some of the situations when the information reported on the claim may be<br />
altered.<br />
q<br />
q<br />
q<br />
The procedure code does not match the reported description of service. It is <strong>United</strong><br />
<strong>Concordia</strong>’s policy to process claims based upon the description of service when the<br />
procedure code and description reported do not agree.<br />
Charges for services that are considered integral to another dental procedure, or that are<br />
unbundled, may be combined with the charge for the complete procedure. For example, the<br />
charge for the preparation of gingival tissue, performed in conjunction with a crown, will be<br />
combined with the charge for the crown.<br />
The alternate treatment provision of some <strong>United</strong> <strong>Concordia</strong>’s dental contracts allows the<br />
<strong>Dental</strong> Advisors to make a professional decision to limit <strong>United</strong> <strong>Concordia</strong>’s payment to the<br />
allowance for an adequate but less costly method of treatment. In these situations, the<br />
reported procedure code(s) will be changed to the code for the alternate treatment. For<br />
example, a <strong>Dental</strong> Advisor may recommend that <strong>United</strong> <strong>Concordia</strong>’s payment be limited to the<br />
allowance for a removable partial denture, as opposed to a fixed bridge, to replace missing<br />
teeth. The reported charges for all units of the fixed bridge will be combined and the reported<br />
procedure codes will be changed to a removable partial denture. Payment will be based on the<br />
fee for a removable partial denture. In such cases, <strong>United</strong> <strong>Concordia</strong> is not recommending<br />
which treatment should be provided. Should the dentist and member elect to have the more<br />
costly treatment, the member will be financially responsible for the difference between the<br />
dentist’s actual fee and <strong>United</strong> <strong>Concordia</strong>’s payment for the adequate, but less costly<br />
procedure.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
11.3
Section<br />
APPEALS<br />
I<br />
f a provider (dentist) or member disagrees with <strong>United</strong> <strong>Concordia</strong>’s benefit decision, the decision<br />
may be appealed. <strong>United</strong> <strong>Concordia</strong> provides full opportunity for eligible parties to appeal benefit<br />
decisions. A dentist can also request an appeal on behalf of the member if the member designates<br />
the dentist in writing as his or her representative or acts in accordance with state legislation.<br />
To appeal a claim, there must be an amount in dispute, unless otherwise regulated by specific<br />
state legislation. This means that there must be a charge or portion of a charge that <strong>United</strong><br />
<strong>Concordia</strong> has decided is not payable. The amount in dispute is calculated as the amount of money<br />
<strong>United</strong> <strong>Concordia</strong> would pay if the services involved had been determined to be payable. An<br />
exception is an adverse decision on a predetermination request that may also be appealed.<br />
Initial Processing<br />
U<br />
nited <strong>Concordia</strong>’s <strong>Dental</strong> Advisor Assistants will review the claim. They will review all<br />
documentation, including documentation submitted with the claims (e.g. narrative<br />
explanations, radiographs, clinical notes, photographs, etc.), and conduct a thorough<br />
investigation. They may contact the provider for additional information, and in some cases, refer the<br />
claim to a Dentist Advisor.<br />
The initial review may result in whole or partial approval of the claim. Once the claim has completed<br />
processing, notification will be sent to the member, dentist or requestor in the form of a <strong>Dental</strong><br />
Explanation of Benefits (DEOB). The DEOB will contain a customer service phone number to<br />
contact to request an appeal.<br />
Second Review/Appeal<br />
f a provider or member disagrees with the review decision, a second review may be requested.<br />
I<br />
A second independent Dentist Advisor will conduct this review. All documentation submitted with<br />
the request (clinical notes, radiographs, photographs, etc.) will be thoroughly examined and<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
12.1
investigated. Moreover, the provider may be contacted for additional information or to discuss the<br />
second review appeal. If you would like to speak with a Dentist Advisor during the second review,<br />
this should be indicated on your documentation. Include a telephone number where you can be<br />
reached and the times you will be available.<br />
The second review may result in whole or partial approval of the disputed costs, or confirmation of<br />
the initial decision and first review. Written notification is issued to the provider of the second<br />
review decision and what action, if any, will be taken. With upheld second review decisions, only the<br />
provider receives letter notification of the results, unless it is a predetermination, in which case the<br />
member will also receive a copy.<br />
What May Not be Reviewed/Appealed<br />
he following issues may not be reviewed/appealed:<br />
T<br />
q<br />
q<br />
q<br />
The amount <strong>United</strong> <strong>Concordia</strong> determines to be the allowable charge.<br />
Member eligibility.<br />
Denial of service(s) as exceeding the patient’s contract year maximum or orthodontic<br />
lifetime maximum.<br />
How to Request a Second Review/Appeal<br />
A dentist may request a second review/appeal at the following address:<br />
Dentist Advisor Unit<br />
<strong>United</strong> <strong>Concordia</strong> Companies, Inc.<br />
PO Box 69420<br />
Harrisburg, PA 17106-6420<br />
Fax – 717-260-7029<br />
* Please Note: Appeals/Reviews must be submitted separately from dental claims. If submitted together in the same<br />
envelope, the appeal/review may be processed as a claim and denied as a duplicate.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
12.2
Section<br />
BENEFIT SAFEGUARDS<br />
Utilization Review<br />
nited <strong>Concordia</strong>’s Utilization Review (UR) program is designed to help ensure that procedures<br />
U<br />
reported on behalf of our members are necessary, appropriate and rendered consistent with the<br />
provisions of their benefit programs. Because this program can affect any dentist who treats a<br />
patient covered by a <strong>United</strong> <strong>Concordia</strong> plan, it is important to understand its purpose and how it<br />
works.<br />
Data Collection & Statistical Analysis<br />
he UR begins with the submission of claims to <strong>United</strong> <strong>Concordia</strong>. As these claims move<br />
T<br />
through our claims processing system, the information reported is captured and stored in various<br />
databases. Periodically, this information is used to develop utilization profiles and frequency ratios<br />
for each dentist who reports services. These frequency ratios are based on the average number of<br />
times each service is reported per 100 patients. Each dentist’s utilization profile and frequency ratios<br />
are compared to the dentist’s peer group. The peer group is comprised of other dentists of the same<br />
specialty who practice in the same demographic location. For example, the profile of a general<br />
dentist would be compared to those of other general dentists who practice in the same state. It is<br />
also possible to compare a dentist’s profile to that of other dentists at a national level.<br />
The UR Process<br />
ost-payment utilization reviews generally begin with the identification of a potential problem<br />
P<br />
area. This can occur as the result of an inquiry or complaint from a patient or another dentist. It<br />
may also occur as a result of discrepancies noted during normal claims processing. More frequently,<br />
it is initiated based on statistical analyses and peer comparisons.<br />
As part of the review, a complete analysis of information available internally at <strong>United</strong> <strong>Concordia</strong>, as<br />
well as other relevant information, will generally be conducted. This may include a review of prior<br />
claim submissions, pending inquires, or complaints and statistical information. Records for a random<br />
sample of patients may be requested from the treating dentist.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
13.1
If warranted, an on-site review will be scheduled in the dentist’s office. Occasionally, a representative<br />
may need to contact patients directly. Patient contacts are conducted with extreme tact and care to<br />
avoid any improper reflection on the dentist.<br />
Professional Consultant Reviews<br />
hroughout the UR process, <strong>Dental</strong> Directors and/or Advisors who are licensed, practicing<br />
T<br />
dentists, are available to provide professional advice or answer questions requiring clinical<br />
knowledge. Usually, Advisors are asked to review any clinical records and diagnostic materials that<br />
may have been obtained and to render an opinion as to whether the records adequately document<br />
the services reported, the dental necessity and the level of care reported.<br />
Follow-up Actions<br />
pon completion of the review, a UR Representative or a <strong>United</strong> <strong>Concordia</strong> <strong>Dental</strong> Director<br />
U<br />
may contact the dentist to discuss his/her treatment patterns and the review findings. If<br />
problems were identified during the review that resulted in overpayments, an appropriate refund is<br />
calculated. Where problems of a general or repetitive nature are identified, the refund calculation<br />
may include an extrapolation against all like services paid to the dentist.<br />
If a refund is involved, the dentist will be informed of the amount, the reason(s) for the requested<br />
refund, the options for repayment and as appropriate his/her right to appeal.<br />
Utilization Letters<br />
nother important function of the UR program is to educate dentists who may unknowingly<br />
A<br />
have potential utilization problems. As a result of our statistical analysis capabilities, the UR<br />
staff is able to identify dentists whose pattern of practice differs significantly from that of other<br />
dentists. In some instances, this may involve a single procedure, while, in others, it may involve<br />
several procedures. In many of these instances, a letter, a copy of the statistical report and an<br />
explanation will be sent to the dentist. Other times, a letter specific to the procedure in question<br />
will be sent. Any time an UR letter is sent, a contact person and phone number is provided.<br />
The Special Investigations Unit (SIU)<br />
he SIU handles <strong>United</strong> <strong>Concordia</strong>’s Government and Commercial Line-of Business anti-fraud<br />
T<br />
efforts. SIU investigates all fraud allegations received by customers, members, dentists and<br />
internal employees. SIU also provides investigative assistance and resources to Federal or State<br />
law enforcement agencies, which have criminal or civil prosecutorial authority. The SIU is a<br />
dedicated unit not associated with other claim adjudication functions.<br />
SIU Mailing Address:<br />
Special Investigations Unit<br />
4401 Deer Path Road, DP-4E<br />
Harrisburg, PA 17110<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
13.2
SIU Toll-Free Fraud Hotline:<br />
1-877-968-7455<br />
SIU Fraud Complaint Form On-line:<br />
www.unitedconcordia.com<br />
Regulatory Compliance<br />
entists have a responsibility to ensure the claims they submit are truthful, accurate and comply<br />
D<br />
with all federal and state contractual regulations.<br />
<strong>United</strong> <strong>Concordia</strong> realizes ethical dentists and their staffs may make billing mistakes and errors<br />
through inadvertence or omission. When <strong>United</strong> <strong>Concordia</strong> determines that a billing error, honest<br />
mistake or omission has resulted in an inappropriate payment, <strong>United</strong> <strong>Concordia</strong> will request that the<br />
practice return the payment. However, the dental practice will not be subject to civil or criminal<br />
penalties.<br />
If a dentist knowingly submits a fraudulent claim, <strong>United</strong> <strong>Concordia</strong> will rely on federal and state<br />
criminal and civil health care fraud laws. These laws cover offenses that are committed with actual<br />
knowledge of the falsity of the claim, reckless disregard or deliberate ignorance of the falsity of the claim.<br />
Coding and Billing<br />
he following risk areas associated with billing have been among the most frequent subjects of<br />
T<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
q<br />
investigations and audits conducted by <strong>United</strong> <strong>Concordia</strong>’s SIU:<br />
Billing for items or services not rendered<br />
Submitting claims for services that are not reasonable or necessary<br />
Duplicate billings<br />
Billing for non-covered services as if covered<br />
Billing for unbundled services<br />
Upcoding the level of service provided<br />
Identity theft, and<br />
Routine waiver of co-payments or cost share<br />
Documentation<br />
imely, accurate and complete documentation is critical to nearly every aspect of a dental practice.<br />
TDocumentation<br />
is necessary to determine the appropriate dental treatment for the patient and is<br />
the basis for coding and billing determinations. Most importantly, failure to document properly has<br />
the potential to compromise good patient care.<br />
In addition to facilitating high quality patient care, a properly documented dental record accurately<br />
denotes what services were provided and why. The dental record may be used to validate:<br />
q<br />
q<br />
The site of service<br />
The appropriateness of the services provided, and<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
13.3
q<br />
The accuracy of the billing<br />
Accurate dental record documentation should comply with, at the minimum, the following<br />
principles:<br />
q<br />
q<br />
The dental record should be complete and legible, and<br />
The documentation of each patient encounter should include the reason for the encounter, any<br />
relevant history, physical examination findings, assessment, clinical impression, diagnosis,<br />
treatment plan, date and treatment performers, if applicable<br />
The current version CDT codes reported on the insurance claims form should be supported by<br />
documentation in the dental record and chart.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
13.4
Section<br />
GLOSSARY OF TERMS<br />
A<br />
Adjudication – Claim processing procedures to determine benefits.<br />
Allowance – The benefit amount that <strong>United</strong> <strong>Concordia</strong> calculates for each covered service. It<br />
includes the amount <strong>United</strong> <strong>Concordia</strong> can pay, as well as the member's coinsurance, if any.<br />
Allowed Fee – See “Allowance”.<br />
American National Standards Institute (ANSI) – The principal-standards development<br />
organization in the U.S. The US’s member body to the ISO, ANSI is a nonprofit, independent<br />
body that’s supported by trade organizations, professional societies and industry.<br />
Appeals/Reviews – Procedures provided for enrolled members and participating dentists who<br />
disagree with <strong>United</strong> <strong>Concordia</strong>’s claim decisions.<br />
Assignment of Benefits – Method by which payment for covered services is made to a nonparticipating<br />
dentist. If no assignment of benefits is made by the patient, payment will be made to<br />
the member for services provided by non-participating dentists. This benefit varies by state and by<br />
contract.<br />
Authorized Provider – A licensed dentist (DDS or DMD), dental hygienist, CRNA or<br />
anesthesiologist who provides services within the scope of his/her license or registration, and who<br />
has not been excluded or suspended from providing service by their state licensing authority.<br />
B<br />
Benefits – <strong>Dental</strong> services received by enrolled members for which all or part of the cost is<br />
authorized and paid for by <strong>United</strong> <strong>Concordia</strong>.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
14.1
Billing Service – An administrative service that a dentist may utilize to handle claim submissions,<br />
whether paper or electronic.<br />
By-Report Procedures – Procedures that require written justification/documentation from the<br />
treating dentist to be considered for coverage.<br />
C<br />
Certificate Holder – Individual that is enrolled under <strong>United</strong> <strong>Concordia</strong> through a contact holder.<br />
Certificate of Insurance – A description of coverage provided to the member.<br />
Claim – Request for payment for services rendered.<br />
Claim Form – Document that may be used either as a claim for payment or as a request for<br />
predetermination. If the date of service is left blank, the claim form will be considered a<br />
predetermination request.<br />
Clearinghouse – In insurance, it’s an intermediary that receives claims from dentists or other<br />
claimants and translates the data from a given format to one that is acceptable for the intended<br />
payer and then forwards the processed claim to the appropriate payer.<br />
Coinsurance – The portion of the dentist’s fee that the member is responsible for paying. This<br />
amount is indicated on the DEOB.<br />
Confirmation Report – An on-line report that is available for retrieval from UCCI via a modem.<br />
The report gives confirmation that UCCI has or has not received the file of claims that were<br />
electronically transmitted.<br />
Contract Holder – Employer or entity that holds contract with <strong>United</strong> <strong>Concordia</strong>.<br />
Contract Year – The 12-month period of time that the annual enrollee maximum applies.<br />
Coordination of Benefits – Rules that determine payment of claims when the member has other<br />
dental coverage in addition to <strong>United</strong> <strong>Concordia</strong>.<br />
D<br />
Date of Service – For purpose of determining coverage, the date a service is completed (e.g.,<br />
cementation date for a crown or bridge; insertion date of dentures; date root canal is sealed).<br />
Definitive Service – A definitive service is any dental service other than a diagnostic service.<br />
Dentist Advisors – Dentists who work with <strong>United</strong> <strong>Concordia</strong> staff to review claims,<br />
predetermination requests and appeals.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
14.2
<strong>Dental</strong> Inquiry – <strong>United</strong> <strong>Concordia</strong>'s on-line access to member information for dental providers.<br />
It is available through Internet access or through the use of <strong>United</strong> <strong>Concordia</strong>'s free software<br />
product.<br />
Dentist – Doctor of <strong>Dental</strong> Surgery or Doctor of <strong>Dental</strong> Medicine who is licensed to practice<br />
dentistry. Used in same states to also refer to certain Certified <strong>Dental</strong> Hygienists and Denturists<br />
authorized by law to provide specified dental services.<br />
DEOB – <strong>Dental</strong> Explanation of Benefits. Computer-generated notice mailed to members and<br />
dentists explaining benefit determinations, i.e., type of service received, the allowable charge, the<br />
amount billed, cost share amount, etc. If a service is not paid, the DEOB also explains why<br />
payment was not allowed and how to appeal that decision.<br />
E<br />
Electronic Claims Submission (ECS) – The process of transmitting insurance claims<br />
electronically from an office, billing service or clearinghouse to an insurance company.<br />
Electronic Data Interchange (EDI) – The electronic transmission of strategically important<br />
business data in a standard syntax by means of computer-to-computer exchange via a standard online<br />
transmission method.<br />
Eligibility – The rules set forth by the contract holder to determine which members may be<br />
enrolled in the dental program.<br />
Endodontic Services – Services relating to the treatment of diseases of the dental pulp, pulp<br />
chamber and root canals.<br />
Enrollment Date – The first day of the month following enrollment and payment of a dental<br />
premium. This date signifies when a member’s coverage begins.<br />
F<br />
Facsimile (Fax) – A device for transmitting copies of documents by wire or radio; also, a<br />
document transmitted by fax.<br />
H<br />
HIPAA – (Health Insurance Portability and Accountability Act) Federal Legislation that defines<br />
standard formats for health insurance transactions.<br />
I<br />
In-Progress Orthodontic Treatment – Orthodontic treatment that has already begun prior to<br />
the member’s enrollment in with <strong>United</strong> <strong>Concordia</strong>. Orthodontic treatment begins on the date<br />
appliances are inserted or bands are placed.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
14.3
Integral Services – Services that are performed in conjunction with another service that dentists<br />
would not normally itemize with a separate charge.<br />
Interactive Voice Response (IVR) system – An automated system used to provide enrollment,<br />
procedure history, annual maximum, claim status, and benefit information. The dental office uses<br />
a touch-tone telephone to enter the request and the response can be provided via telephone, fax<br />
machine and/or mailed.<br />
Internet – Any large network made up of several smaller networks. Capitalized, the international<br />
network of the networks that connects educational, scientific and commercial institutions.<br />
M<br />
Maximums – Total dollar amount (per member) payable by <strong>United</strong> <strong>Concordia</strong>. Maximum may be<br />
for the dental program orthodontics, TMJ or implants if insured under the contract.<br />
Members – Individuals who are enrolled in and eligible to receive benefits from <strong>United</strong><br />
<strong>Concordia</strong>.<br />
Modem (MOdulator-DEModulator) – A device to connect a user’s computer to communicate<br />
across standard telephone lines with other computers at different locations.<br />
N<br />
Non-participating Dentist – A dentist who has not signed a participating agreement with <strong>United</strong><br />
<strong>Concordia</strong>.<br />
O<br />
Oral Surgery – Services relating to the treatment of diseases, injuries, deformities, defects and<br />
esthetic aspects of the oral and maxillofacial region.<br />
Orthodontic Services – Services relating to the treatment of teeth in relation to the functions of<br />
occlusion and speech.<br />
Other <strong>Dental</strong> Insurance – Additional coverage through another employer, association, or private<br />
insurer. See “Coordination of Benefits”.<br />
P<br />
Participating Dentist – An authorized dentist who has signed a participating agreement with<br />
<strong>United</strong> <strong>Concordia</strong> and agrees to accept the <strong>United</strong> <strong>Concordia</strong> determined allowable charge as<br />
payment in full for covered services.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
14.4
Password – A word or group of characters a user has to enter to gain access to a computer or to<br />
files.<br />
Payer ID – Unique identifier assigned by a clearinghouse to indicate a specific insurance carrier.<br />
Periodontal Services – Services relating to the treatment of diseases of the supporting and<br />
surrounding tissues of the teeth.<br />
Predetermination – Written estimate provided by <strong>United</strong> <strong>Concordia</strong> in response to a request by a<br />
dentist or member for an estimate of coverage for future dental services.<br />
Procedure Codes - Codes used to identify and define specific dental services.<br />
Prosthodontic Services – Professional placement or maintenance of artificial teeth, either fixed<br />
or removable.<br />
R<br />
Review – First level of the Appeals process. It enables members and dentists to seek a separate<br />
review from the initial payment determination to assess whether the initial payment decision was<br />
correct.<br />
S<br />
Single Procedure – Each dental procedure with a separate assigned procedure code.<br />
Software – A computer program or set of programs held in some storage medium and loaded into<br />
read/write memory (RAM) for execution.<br />
Software Vendor – A business that programs electronic claims submission software and then sells<br />
the software to dentists.<br />
Student – Family member under age 23 who is enrolled at an accredited college or university and<br />
dependent on the service member for over 50 percent of his/her support.<br />
Summary Payment Voucher – The title given to the <strong>Dental</strong> Explanation of Benefits (DEOB)<br />
sent to the dentist. See “DEOB”.<br />
T<br />
Transmission – The dispatching of a signal, message, or other form of intelligence by wire, radio,<br />
telegraphy, telephone, facsimile or other means; a series of characters, messages or blocks,<br />
including control information and user data; the signaling of data over communications channels.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
14.5
U<br />
<strong>United</strong> <strong>Concordia</strong> – <strong>United</strong> <strong>Concordia</strong> Companies, Inc., a subsidiary of Highmark, Inc.,<br />
headquartered in Harrisburg, PA with support offices in Birmingham, AL; Phoenix, AZ;<br />
Woodland Hills, CA; Fresno, CA; Tampa, FL; Jacksonville, FL; Alpharetta, GA; Chicago, IL;<br />
Towson, MD; Troy, MI; Chesterfield, MO; Omaha, NE; Albuquerque, NM; New York, NY;<br />
Plainview, NY; King of Prussia/Philadelphia, PA; Pittsburgh, PA; Williamsport, PA; Dallas, TX;<br />
Houston, TX; San Antonio, TX; Glen Allen, VA; and Seattle, WA.<br />
W<br />
Windows® - A software operating system developed by Microsoft.<br />
May 2005<br />
www.unitedconcordia.com<br />
Current <strong>Dental</strong> Terminology © American <strong>Dental</strong> Association<br />
14.6