Annual Report 2007 / 2008 - South West London and St George's ...
Annual Report 2007 / 2008 - South West London and St George's ...
Annual Report 2007 / 2008 - South West London and St George's ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Our year<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts <strong>2007</strong>/08<br />
Helping people take back<br />
control over their lives<br />
<strong>Annual</strong> Review 07 / 08 1
contents<br />
Chairman’s welcome 3<br />
Chief Executive’s introduction 4<br />
About us 5<br />
Our vision 6<br />
Our services 7<br />
Our objectives <strong>and</strong> our performance 21<br />
Financial review 34<br />
Remuneration 41<br />
Our Board 43<br />
Did you know?<br />
21,766<br />
3,830<br />
2,700<br />
720<br />
£170m<br />
21,766 people are<br />
currently receiving<br />
treatment <strong>and</strong> care<br />
from the Trust in<br />
the community<br />
We had<br />
3,830 inpatient<br />
admissions<br />
in <strong>2007</strong>/08<br />
We employ<br />
about<br />
2,700 staff<br />
We have<br />
720<br />
inpatient beds<br />
Our annual<br />
budget is<br />
£170 million<br />
2 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Meeting major challenges<br />
Welcome from the Trust’s Chairman<br />
This is a very exciting time for<br />
the Trust. As is obvious with<br />
the major building work going<br />
on at Springfield University<br />
Hospital we are forging ahead<br />
with the construction of the<br />
W<strong>and</strong>sworth Acute Unit.<br />
This is the first phase of<br />
implementing the overall<br />
vision for the 80-acre site.<br />
Looking forward, in 2009 we hope<br />
to become an NHS foundation trust<br />
providing health <strong>and</strong> social care. This<br />
means giving an opportunity for local<br />
people to join us as members <strong>and</strong><br />
become involved in our decision making.<br />
Through the members the Trust will be<br />
more accountable to the local people<br />
we serve <strong>and</strong> to our partners, including<br />
the borough councils.<br />
We continue to face major challenges<br />
<strong>and</strong> to help meet these we have<br />
appointed two new non-executive<br />
directors (NEDs) with strong professional<br />
backgrounds. Iain McCusker, a<br />
chartered accountant, <strong>and</strong> Susan<br />
Dark, the managing director of<br />
Nikko Healthcare, will be using their<br />
independence, skills <strong>and</strong> experience to<br />
help plan <strong>and</strong> oversee Trust services.<br />
As well as our two new NEDs we have<br />
welcomed two new executive members<br />
of the Board – Kim Goddard, Director<br />
of Nursing <strong>and</strong> Governance, <strong>and</strong> Dr Ben<br />
Nereli, our new Medical Director, further<br />
strengthening the executive <strong>and</strong> clinical<br />
leadership of the Trust.<br />
I would like to thank all members of the<br />
Board for their contribution in the last year.<br />
I believe we have a very strong <strong>and</strong> talented<br />
executive team led by Peter Houghton.<br />
Most of all I want to thank the staff of<br />
the Trust, both those who have direct<br />
contact with the people we serve<br />
<strong>and</strong> also those who work tirelessly<br />
in the background. On behalf of the<br />
Board <strong>and</strong> everyone who uses our<br />
services, thank you.<br />
John Rafferty<br />
Chairman<br />
3
Improving clinical care<br />
Introduction by the Chief Executive<br />
The past year has seen the<br />
Trust make real progress,<br />
with notable achievements<br />
in important areas.<br />
These include: the work we have<br />
undertaken to improve the quality<br />
of the environment for service users<br />
<strong>and</strong> staff; our increasing profile in the<br />
local community <strong>and</strong> the media as we<br />
attempt to engage with people from<br />
diverse communities <strong>and</strong> to tackle the<br />
stigma associated with serious mental<br />
illness; <strong>and</strong> our sound management of<br />
the Trust finances, now recognised in<br />
an improved rating by NHS <strong>London</strong>.<br />
In my introduction to last year’s report<br />
I said that delivering safe <strong>and</strong> effective<br />
clinical care was a top priority. This<br />
remains so <strong>and</strong> is the key theme of this<br />
year’s report. I am delighted that we<br />
have achieved real improvements over<br />
the past year as we said we would.<br />
These would not have happened unless<br />
we had involved service users, carers<br />
<strong>and</strong> other stakeholders in our work<br />
<strong>and</strong> been determined to learn from our<br />
experiences <strong>and</strong> from others.<br />
I will single out three examples:<br />
Service users told us in surveys that they could not always get the help they<br />
needed in a crisis. Thanks to the efforts throughout the year of staff <strong>and</strong><br />
managers in each borough, we now have crisis <strong>and</strong> home treatment teams<br />
<strong>and</strong> early intervention teams in place from April <strong>2008</strong>.<br />
The improvement programme that has been implemented in our forensic unit,<br />
the Shaftesbury Clinic, has ensured a safer, more effective <strong>and</strong> responsive service<br />
for service users. <strong>St</strong>aff have spent much time reflecting on the problems of<br />
the past, learning from experience elsewhere, <strong>and</strong> introducing new working<br />
practices.<br />
The first phase of the redevelopment of Springfield began in autumn <strong>2007</strong><br />
with the start of the building work for the new W<strong>and</strong>sworth Acute Unit.<br />
This will provide a new Psychiatric Intensive Care Unit <strong>and</strong> an admission ward<br />
for adults who are acutely ill. Clinical teams <strong>and</strong> service users are working with<br />
the builders <strong>and</strong> designers to ensure that the very best practice is incorporated<br />
from elsewhere, both in the UK <strong>and</strong> abroad.<br />
Looking to the year ahead, the Board<br />
has four overriding priorities:<br />
First is the need to continue raising<br />
st<strong>and</strong>ards <strong>and</strong> delivering health <strong>and</strong><br />
social care performance targets.<br />
This will improve the quality <strong>and</strong><br />
effectiveness of the care <strong>and</strong> support<br />
we provide for service users <strong>and</strong> carers.<br />
Second is to continue to manage<br />
our finances well, ensuring that we<br />
deliver value for money <strong>and</strong> meet our<br />
obligations as stewards of<br />
public resources.<br />
Last, <strong>and</strong> by no means least,<br />
is the work we need to do to become<br />
a foundation trust.<br />
Finally, I would like to thank three<br />
groups of people without whom<br />
the achievements of the past year<br />
would not have been possible: service<br />
users <strong>and</strong> carers for their ideas <strong>and</strong><br />
honest feedback; our staff for their<br />
commitment <strong>and</strong> creativity; <strong>and</strong> our<br />
commissioners <strong>and</strong> partners for their<br />
active engagement in the transformation<br />
of services we want to achieve.<br />
Third is to deliver the Springfield<br />
Regeneration Programme successfully<br />
so that we can significantly improve<br />
the environment in which we provide<br />
treatment <strong>and</strong> care at Springfield<br />
University Hospital <strong>and</strong> elsewhere in<br />
the Trust.<br />
Peter Houghton<br />
Chief Executive<br />
4
About us<br />
<strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s<br />
Mental Health NHS Trust was formed in<br />
1994 but our history goes back much<br />
further. Our services began on the site of<br />
Springfield University Hospital in Tooting<br />
(the Trust’s headquarters) 170 years ago.<br />
Today we provide mental health <strong>and</strong><br />
social care services to a population of<br />
about one million people across the five<br />
<strong>London</strong> boroughs of Kingston, Merton,<br />
Richmond, Sutton <strong>and</strong> W<strong>and</strong>sworth <strong>and</strong><br />
specialist services for people throughout<br />
the United Kingdom.<br />
We provide a full range of services<br />
for children, young people, adults<br />
<strong>and</strong> older people including:<br />
• mental health services for adults <strong>and</strong><br />
older people<br />
• mental health services for people who<br />
have had contact with the criminal<br />
justice system<br />
• specialist children’s services<br />
• learning disability services<br />
• substance misuse services<br />
• community <strong>and</strong> inpatient services<br />
for people with drug <strong>and</strong> alcohol<br />
problems<br />
• other specialist mental health services,<br />
such as eating disorders.<br />
We work with a range of partners<br />
including local authorities, primary care<br />
trusts, GPs <strong>and</strong> other statutory <strong>and</strong><br />
voluntary services to deliver care <strong>and</strong><br />
support to people in their homes <strong>and</strong><br />
from hospital <strong>and</strong> community bases. The<br />
Trust also provides training, education<br />
<strong>and</strong> research with four academic<br />
institutions. We deliver statutory social<br />
care to people with mental health needs<br />
in south west <strong>London</strong> on behalf of the<br />
five boroughs we serve.<br />
Our main inpatient sites are Springfield<br />
University Hospital, Tooting; Tolworth<br />
Hospital; Queen Mary’s Hospital,<br />
Roehampton; <strong>and</strong> Sutton Hospital.<br />
Becoming a foundation trust<br />
We remain committed to becoming<br />
a foundation trust <strong>and</strong> our plan is to<br />
achieve this by spring 2009.<br />
Becoming a foundation trust will give<br />
us more control over our future. We<br />
will have greater financial freedoms to<br />
develop new services that focus on the<br />
needs of local people <strong>and</strong> improve the<br />
treatment <strong>and</strong> care we provide.<br />
As members, local people, <strong>and</strong> those<br />
who use our services <strong>and</strong> the people<br />
who care for them will have a greater<br />
say in how we develop our services.<br />
They will have greater opportunities<br />
to be consulted on existing services<br />
<strong>and</strong> future plans. We will be able to<br />
use members’ feedback to improve<br />
our services by using the care <strong>and</strong><br />
treatments that work best.<br />
Above:<br />
The Trust’s headquarters<br />
Springfield University Hospital<br />
Right:<br />
Joining the Trust<br />
Journalist <strong>and</strong> broadcaster Sir Trevor<br />
McDonald signs up to become a member<br />
5
Our vision<br />
Our vision is a future in which people with mental health problems<br />
have the same opportunity as other citizens to participate in <strong>and</strong><br />
contribute to our communities.<br />
Our values<br />
The most important people in our<br />
services are those who use them<br />
<strong>and</strong> their relatives, friends <strong>and</strong> carers.<br />
The most important resources that we<br />
have are the staff that provide their<br />
care <strong>and</strong> support.<br />
In all our actions, we will recognise<br />
<strong>and</strong> value the diversity that exists in<br />
our services <strong>and</strong> our local community<br />
<strong>and</strong> strive to ensure equality of access,<br />
experience <strong>and</strong> outcome irrespective<br />
of race or ethnicity, disability, age,<br />
gender, sexuality or religious belief,<br />
or place of residence.<br />
We will treat everyone with dignity <strong>and</strong><br />
respect, involve them in decisions that<br />
affect them <strong>and</strong> provide them with<br />
whatever information they feel will<br />
help them.<br />
In all that we do we strive for excellence,<br />
equity <strong>and</strong> the efficient use of resources.<br />
Our purpose<br />
The Trust recognises that everyone<br />
with mental health problems faces the<br />
challenge of retaining or recovering a<br />
life that is as meaningful, satisfying <strong>and</strong><br />
valued as possible.<br />
The purpose of the Trust is to help<br />
people with mental health problems to<br />
do the things they want to do, live the<br />
lives they want to live <strong>and</strong> access those<br />
opportunities that all citizens should take<br />
for granted.<br />
To achieve this purpose we will work<br />
in partnership with those who use our<br />
services, their relatives, carers <strong>and</strong> friends<br />
<strong>and</strong> other stakeholders to:<br />
• foster hope in those whom we<br />
serve <strong>and</strong> do our best to ensure that<br />
everyone’s experience of using our<br />
services is a positive one<br />
• provide effective treatment <strong>and</strong> help<br />
people to take back control over their<br />
problems <strong>and</strong> their lives <strong>and</strong> the help<br />
they receive<br />
• improve people’s life chances by<br />
promoting their health, safety <strong>and</strong><br />
wellbeing <strong>and</strong> assisting them to access<br />
the opportunities that they value:<br />
homes, jobs, friends, relationships,<br />
education, social pursuits, leisure<br />
activities <strong>and</strong> spiritual possibilities<br />
• undertake teaching <strong>and</strong> research, to<br />
enable us to continue to do this work<br />
for those who will use our services in<br />
the future<br />
• cultivate a workforce that is<br />
committed to pursuing our vision<br />
<strong>and</strong> purpose <strong>and</strong> ensure they have<br />
the support <strong>and</strong> development<br />
opportunities they need to do so.<br />
Above:<br />
Mobile technology<br />
Delivering improvements in<br />
community services<br />
6 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Our services<br />
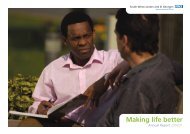
Left:<br />
Reaching black <strong>and</strong> minority<br />
ethnic patients <strong>and</strong> their families<br />
Admiral Nurse Vincent Goodorally led our<br />
award-winning project on dementia which<br />
won a national Care Services Improvement<br />
Partnership (CSIP) award<br />
Some of our proudest moments in <strong>2007</strong>/08:<br />
• The Government’s Social Exclusion<br />
Task Force chose us as one of 12<br />
national pilot sites to provide a<br />
new service for chronically<br />
excluded adults<br />
• Two wards at Springfield University<br />
Hospital were accepted on the <strong>St</strong>ar<br />
Wards programme for mental health<br />
trusts, a national programme which<br />
aims to improve acute inpatients’<br />
daily experiences <strong>and</strong> outcomes.<br />
To win a place on the programme,<br />
wards need to demonstrate a<br />
sufficiently high level of nursing<br />
practice, user <strong>and</strong> carer focus <strong>and</strong><br />
access to therapies <strong>and</strong> activities on<br />
the ward<br />
Left:<br />
<strong>St</strong>aying healthy<br />
At <strong>South</strong>bank House residents grow<br />
their own vegetables<br />
• Our vocational services (see page<br />
12) were cited as an example of good<br />
practice by the Sainsbury Centre for<br />
Mental Health, the Royal College<br />
of Psychiatrists <strong>and</strong> (in a Health<br />
Service Journal article) by the NHS<br />
Confederation, which also mentioned<br />
our involvement of service users<br />
• Our Early Intervention Service (see<br />
page 11) won a BUPA Foundation’s<br />
national Clinical Excellence award<br />
for its success in getting more than<br />
80 per cent of the young people it<br />
sees back into work or education<br />
after a first experience of a psychotic<br />
illness<br />
• We were chosen as one of only<br />
eight sites nationwide to pioneer<br />
a new £4.95 million project<br />
sponsored by the Health Foundation.<br />
Co-creating Health aims to transform<br />
the traditional doctor/patient<br />
relationship. The Trust is one of<br />
only two pilot sites focusing on<br />
mental health<br />
• The Trust became one of only ten<br />
pilot projects in Engl<strong>and</strong> to introduce<br />
a new form of treatment known<br />
as Multisystemic Therapy (MST).<br />
MST is based on a family therapy<br />
approach which has been used for<br />
many years in the USA, <strong>and</strong> has been<br />
particularly successful in working with<br />
adolescents with serious anti-social<br />
behaviour <strong>and</strong> their families<br />
• A project, based in Kingston, to<br />
reach black <strong>and</strong> minority ethnic<br />
(BME) patients <strong>and</strong> their families in<br />
Kingston, was the winning entry,<br />
nationwide, in the Recognising<br />
Diversity category at the Care<br />
Services Improvement Partnership<br />
(CSIP) Positive Practice Awards<br />
• Our pioneering annual Happy Soul<br />
Festival (see page 19) engaged black<br />
<strong>and</strong> minority ethnic communities<br />
using arts, events <strong>and</strong> films with<br />
mental health themes<br />
• One of our staff won the Nursing<br />
<strong>St</strong><strong>and</strong>ard Mental Health Nurse of<br />
the Year award (see page 17).<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 7
Child <strong>and</strong> adolescent mental health services<br />
a consultant psychiatrist’s story<br />
Like many psychiatrists<br />
working in multidisciplinary<br />
child <strong>and</strong> adolescent mental<br />
health services (CAMHS), Dr<br />
Ann York, Consultant Child<br />
<strong>and</strong> Adolescent Psychiatrist<br />
at Richmond Royal Hospital,<br />
has to cope with relentless<br />
dem<strong>and</strong>s on her team’s<br />
services, the pressure of<br />
targets <strong>and</strong> lack of time.<br />
Under her leadership, her team has<br />
developed an innovative service<br />
model which is cited as a model of<br />
good practice in the National Service<br />
Framework for Children update report.<br />
Together with a consultant psychiatrist<br />
at Hertfordshire Partnership Foundation<br />
Trust, she has continued to develop<br />
<strong>and</strong> describe this model for managing<br />
dem<strong>and</strong> <strong>and</strong> capacity to deliver high<br />
quality services to children <strong>and</strong> families.<br />
Ann put what she had learned <strong>and</strong><br />
developed into a book – The 7 HELPFUL<br />
Habits of Effective CAMHS <strong>and</strong> the<br />
Choice <strong>and</strong> Partnership Approach –<br />
with a supporting website at www.<br />
camhsnetwork.co.uk. She has also<br />
worked with hundreds of clinicians,<br />
managers <strong>and</strong> commissioners in the<br />
UK, <strong>and</strong> overseas, on how they can<br />
apply the model to their services.<br />
Ann says: “The model uses dem<strong>and</strong><br />
<strong>and</strong> capacity theory as applied to<br />
CAMHS, <strong>and</strong> incorporates the NHS<br />
Institute’s 10 High Impact Changes for<br />
Services Improvement <strong>and</strong> Delivery,<br />
the Department of Health’s New Ways<br />
of Working in Mental Health <strong>and</strong> Our<br />
Choices in Mental Health alongside user<br />
choice <strong>and</strong> care planning frameworks.<br />
In our own <strong>and</strong> other services the result<br />
has been enhanced clinical effectiveness<br />
<strong>and</strong> team working, with improved user<br />
engagement <strong>and</strong> choice.<br />
“We started running service improvement<br />
workshops four years ago at the request<br />
of colleagues <strong>and</strong> increasingly were asked<br />
to talk about what we were doing in our<br />
own clinical teams. I find it enormously<br />
exciting that this service model started<br />
here in Richmond in 2000 <strong>and</strong> we have<br />
helped other services become more<br />
efficient <strong>and</strong> effective for the benefit of<br />
users <strong>and</strong> staff.<br />
8
Responding to children<br />
<strong>and</strong> young people<br />
“To help others adapt the model to<br />
their own services we’ve named it CAPA<br />
– the Choice <strong>and</strong> Partnership Approach<br />
(see below). CAPA – which is cited in the<br />
Healthcare Commission’s forthcoming<br />
Value for Money study – puts into practice<br />
many of the 7 HELPFUL Habits <strong>and</strong> sits<br />
well with the evidence of factors that<br />
improve outcomes for children with<br />
mental health problems. We encourage<br />
teams to adapt this flexible approach<br />
to their own circumstances so that they<br />
can help users to have choices <strong>and</strong> to be<br />
directly involved in care planning.<br />
“Other clinical teams are finding that CAPA<br />
also works for them. This clinical system<br />
that evolved from what the Trust has been<br />
doing in Richmond CAMHS is now being<br />
widely implemented across the UK <strong>and</strong> as<br />
far away as New Zeal<strong>and</strong> <strong>and</strong> Australia.”<br />
Below left:<br />
Managing dem<strong>and</strong> <strong>and</strong> capacity<br />
Ann York with members of her team in Richmond<br />
our<br />
approach<br />
The Choice <strong>and</strong> Partnership<br />
Approach (CAPA) is a clinical<br />
system that helps CAMHS to<br />
do the right things (working<br />
towards goals the family <strong>and</strong><br />
young person wants)<br />
• with the right people (with<br />
clinicians with the right skills)<br />
• at the right time (in a timely<br />
manner without waiting lists)<br />
<strong>and</strong> to provide a service that<br />
is user-focused, accessible <strong>and</strong><br />
evidence-based.<br />
Each of the five boroughs<br />
served by the Trust has<br />
a child <strong>and</strong> adolescent<br />
mental health team<br />
working to deliver<br />
responsive, effective<br />
<strong>and</strong> appropriate care to<br />
children <strong>and</strong> young people<br />
<strong>and</strong> their families <strong>and</strong><br />
carers. As well as the CAMHS clinics, our staff<br />
work in a wide range of settings to ensure that<br />
our services are targeted at those most in need.<br />
The Trust has a number of specialist services<br />
for children <strong>and</strong> young people. These include:<br />
an inpatient adolescent service <strong>and</strong> adolescent<br />
assertive outreach team; a specialist learning<br />
disability outpatient service; a child <strong>and</strong><br />
adolescent inpatient <strong>and</strong> targeted outpatient<br />
eating disorder service; <strong>and</strong> a national deaf<br />
service for children.<br />
The Trust’s CAMHS work to provide clinically<br />
effective, high quality services which are<br />
delivered by highly skilled, committed <strong>and</strong><br />
qualified child <strong>and</strong> adolescent mental<br />
health professionals.<br />
Our services work to NICE (National Institute for<br />
Health <strong>and</strong> Clinical Excellence) guidance where<br />
it is available <strong>and</strong> use routine outcome measures<br />
such as Health of the Nation Outcome Scales for<br />
Children <strong>and</strong> Adolescents to measure outcomes<br />
for our service users. This ensures that the<br />
treatment we offer is effective <strong>and</strong> appropriate.<br />
Our services for children <strong>and</strong> young people are<br />
supported by the Trust’s clinical lead for CAMHS as<br />
well as by a governance manager. <strong>St</strong>ructures are<br />
in place which allow us to review best practice.<br />
Services are always planned in partnership with<br />
the relevant local primary care trust <strong>and</strong> local<br />
authority <strong>and</strong> delivered through the multiagency<br />
children <strong>and</strong> young people’s plans.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>Annual</strong> <strong>and</strong> Review Accounts 07 // 08 9
Early intervention<br />
a service user’s story<br />
Naomi, 21, is one of 160<br />
young people being helped<br />
by our Early Intervention<br />
Service after a first episode<br />
of psychosis.<br />
Naomi says: “After I was<br />
first sectioned five years ago<br />
I was transferred to Early<br />
Intervention. For most of that<br />
time Rachel has been my care<br />
coordinator. She’s really good<br />
<strong>and</strong> always asks questions to<br />
work out what I’m doing. We<br />
meet regularly to talk about<br />
what’s stressing me out <strong>and</strong><br />
what my plans are.<br />
“Rachel helped me write an advance<br />
directive of what I want to happen if I<br />
get unwell but she also helps prevent<br />
me getting ill. She asks my friends <strong>and</strong><br />
family how I’m doing. My family meet<br />
her regularly to look at my ‘relapse<br />
plan’ – how to stop me getting unwell.<br />
She also goes over it with staff in the<br />
supported housing Early Intervention<br />
found for me.<br />
“Rachel made it easier for me to talk<br />
about how not taking my medication<br />
led to my being readmitted. My illness<br />
was caused by smoking weed, <strong>and</strong> not<br />
eating or sleeping properly. I’ve now<br />
given up drugs – <strong>and</strong> cigarettes – <strong>and</strong><br />
feel much more lively <strong>and</strong> awake. I’m on<br />
a mood stabiliser, helping me keep on<br />
one level rather than being ecstatically<br />
happy. I used to be angry <strong>and</strong> have a<br />
bad temper. I’ve calmed down a lot.<br />
To stay well I go to bed by midnight <strong>and</strong><br />
don’t study through the night.<br />
“The Early Intervention team found my<br />
degree course <strong>and</strong> get me any extra<br />
help I need. I take education seriously<br />
– before, I couldn’t wait to leave school<br />
<strong>and</strong> get a job. I used to work as well as<br />
study but when I’m hectic I get stressed.<br />
I didn’t realise I could have Disability<br />
Living Allowance <strong>and</strong> a Freedom Pass<br />
– Rachel sorted it out.<br />
“My relationship with my family is<br />
improving – Rachel’s helped strengthen<br />
the bond between me <strong>and</strong> my mum.<br />
“I’m now in control. No one<br />
will tell me off if I don’t take<br />
the tablets but I know what<br />
the consequences will be.<br />
And I can negotiate with<br />
Rachel about how much<br />
medication I should be on.<br />
“The Early Intervention team never<br />
put me down or say what I do is weird<br />
– anyone can become unwell. I can<br />
contact them with issues or problems<br />
<strong>and</strong> have a crisis line to call if I need to.<br />
Without them I’d have been a stubborn<br />
brat.<br />
“I don’t plan to get admitted again.<br />
I’d miss out on so much – particularly<br />
my freedom. The Early Intervention team<br />
have helped to tackle my illness early.<br />
I know people who are still in the<br />
hospital ward when I return <strong>and</strong> I<br />
wouldn’t want to be in their situation.”<br />
.<br />
Above:<br />
Now in control<br />
Naomi with her care<br />
coordinator Rachel Langley<br />
10 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Our award-winning<br />
Early Intervention Service<br />
The Trust’s Early Intervention Service focuses on<br />
people aged 17 to 30 who have been experiencing<br />
the symptoms of psychosis for the first time. The<br />
most well known type of psychosis, schizophrenia<br />
can affect young people at a crucial stage in their<br />
development.<br />
<strong>St</strong>udies have shown that with sustained treatment,<br />
over 80 per cent of individuals achieve symptomatic<br />
remission from a first episode of psychosis within six<br />
months. However, intervening early in the first few<br />
years of illness is critical in maximising the potential<br />
for recovery <strong>and</strong> in preventing relapse.<br />
80%<br />
<strong>St</strong>udies have shown<br />
that with sustained<br />
treatment, over 80 per<br />
cent of individuals achieve<br />
symptomatic remission<br />
from a first episode<br />
of psychosis within<br />
six months. However,<br />
intervening early in the<br />
first few years of illness is<br />
critical in maximising the<br />
potential for recovery <strong>and</strong><br />
in preventing relapse.<br />
The Trust adopted early intervention in 2001, when<br />
there were only nine other services nationally.<br />
Initially encompassing a small service across Merton,<br />
Sutton <strong>and</strong> W<strong>and</strong>sworth, it grew incrementally<br />
over the next six years with a particular focus<br />
on employment <strong>and</strong> education. This combines<br />
vocational rehabilitation with medical care to<br />
encourage people to take up work or study<br />
opportunities as soon as possible after they have<br />
recovered from their initial treatment. As a result,<br />
81 per cent of those seen by the service, working<br />
alongside an employment specialist from the Trust,<br />
were back at work or in mainstream education<br />
within 18 months as part of their recovery.<br />
For its achievement in bucking a national trend,<br />
the Service received a<br />
Clinical Excellence award<br />
in November <strong>2007</strong> from a<br />
medical research charity,<br />
the BUPA Foundation.<br />
The original service was<br />
increased substantially as<br />
a result of the Trust’s Adult<br />
Service Reviews in <strong>2007</strong>/08, <strong>and</strong> has now been<br />
disaggregated into a Sutton <strong>and</strong> Merton team <strong>and</strong><br />
a separate W<strong>and</strong>sworth team to enable a greater<br />
borough focus. To meet local need, a team was<br />
also established in Richmond during <strong>2007</strong>/08,<br />
with support from the primary care trust <strong>and</strong> the<br />
borough council. By the end of the year the team<br />
had its full caseload target of 71 patients.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 11
Individual placement <strong>and</strong> support<br />
a vocational service manager’s story<br />
Adults with mental health<br />
problems often see the ability<br />
to return to work or education<br />
as a yardstick of their recovery.<br />
The Trust has been recognised for many<br />
years now as a pioneer in developing<br />
effective services that support them<br />
to do this. Most recently the Trust<br />
was cited as a model of good practice<br />
by the Royal College of Psychiatrists<br />
in their report on Mental Health<br />
<strong>and</strong> Employment as part of the<br />
Government’s review of the health of<br />
Britain’s working age population.<br />
The Trust has implemented in Kingston,<br />
Merton <strong>and</strong> W<strong>and</strong>sworth the Individual<br />
Placement <strong>and</strong> Support (IPS) approach<br />
to vocational rehabilitation. The IPS<br />
approach is the most widely studied <strong>and</strong><br />
effective method of helping people with<br />
severe mental health problems to gain<br />
<strong>and</strong> retain paid employment. The overall<br />
goals of this evidence-based practice<br />
are to assist service users in finding<br />
jobs consistent with their preferences<br />
<strong>and</strong> skills, <strong>and</strong> to support their efforts<br />
in working. Research suggests this<br />
improves their chances of recovery.<br />
Miles Rinaldi, the Trust’s Head of<br />
Recovery <strong>and</strong> Social Inclusion, says:<br />
“A key principle of the IPS approach is<br />
the integration of employment support<br />
<strong>and</strong> clinical services. This means that an<br />
employment specialist works as part of<br />
a community mental health team <strong>and</strong><br />
service users have access to this specialist<br />
as well as to psychiatrists, psychologists,<br />
nurses, social workers, occupational<br />
therapists <strong>and</strong> other care providers.<br />
“All staff within the team collaborate<br />
together to provide support to address<br />
the service user’s health <strong>and</strong> social care<br />
needs, including retaining or gaining<br />
employment, mainstream education<br />
or voluntary work. Research that the<br />
Trust was involved in shows that people<br />
with mental health problems in paid<br />
employment experience positive changes<br />
in self identity, increased quality of life<br />
<strong>and</strong> reduced hospital admissions.”<br />
One of the success stories that Miles cites<br />
is that of Marsha, 31, who had always<br />
wanted to work in a hairdressing salon.<br />
Miles says: “When diagnosed<br />
with schizophrenia Marsha<br />
thought she would never<br />
be able to work, but her<br />
care coordinator recognised<br />
that with support from the<br />
employment specialist <strong>and</strong><br />
himself, she could achieve<br />
her goal.<br />
12 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Investing for the future<br />
at Springfield<br />
integrated<br />
services<br />
“The employment specialist met with<br />
Marsha <strong>and</strong> after a brief vocational<br />
assessment a vocational plan was<br />
developed. Within a short time she began<br />
working in a salon, with day release to<br />
attend college to train as a stylist.<br />
“Marsha met regularly for support with<br />
the employment specialist, who also<br />
liaised with Marsha’s care coordinator<br />
<strong>and</strong> psychologist. The employment<br />
specialist <strong>and</strong> care coordinator provided<br />
ongoing support to enable Marsha to<br />
overcome a number of problems that<br />
arose as she adjusted to working life.<br />
Marsha qualified <strong>and</strong> continues to<br />
work as a stylist.”<br />
Above left:<br />
Service users have<br />
access to an employment<br />
specialist on the<br />
community mental<br />
health team as well<br />
as to psychiatrists,<br />
psychologists, nurses,<br />
social workers,<br />
occupational therapists<br />
<strong>and</strong> other care providers.<br />
Integrating employment<br />
support <strong>and</strong> clinical services<br />
Miles Rinaldi<br />
In the coming year a<br />
decision will be made on<br />
whether our 170-year-old<br />
site at Springfield University<br />
Hospital will receive the long<br />
awaited investment it needs<br />
for the future.<br />
The Springfield<br />
Regeneration Programme will provide stateof-the-art<br />
new mental health facilities while<br />
simultaneously upgrading other areas of the site<br />
with new amenities for the community, new homes<br />
<strong>and</strong> a new public park.<br />
This will be a complex <strong>and</strong> lengthy task but its<br />
primary aim is quite simple: to strengthen the Trust<br />
as a centre of excellence in mental health care by<br />
providing the best possible treatment environment<br />
for Springfield University Hospital <strong>and</strong> its service<br />
users. There will be challenges but the opportunity<br />
it presents to the Trust, its partners <strong>and</strong> the<br />
surrounding community is unprecedented.<br />
The consultation on how this centre of excellence<br />
will be created is ongoing. The project is currently<br />
at the ‘outline planning’ stage <strong>and</strong> separate, more<br />
detailed planning applications for the new facilities<br />
will be made later as the consultation progresses. As<br />
with the new W<strong>and</strong>sworth Acute Unit (scheduled<br />
for completion in Spring 2009 in the first phase of<br />
the Springfield Regeneration Programme), staff,<br />
service users <strong>and</strong> carers will all play a part in shaping<br />
how the facilities can best meet everyone’s needs.<br />
The upgrading of the Trust’s facilities will not just<br />
be limited to Springfield. Significant improvements<br />
are also being planned for Tolworth Hospital in<br />
Kingston <strong>and</strong> further refurbishment works are also<br />
in the pipeline for other parts of the Trust’s estate.<br />
The Trust recognises the real benefits that a<br />
therapeutic environment can bring to the healing<br />
process <strong>and</strong> in the design of these new <strong>and</strong><br />
upgraded facilities it will endeavour to create the<br />
most appropriate surroundings possible.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 13
Wellbeing service<br />
a nurse adviser’s story<br />
Improving physical health<br />
can be an important factor<br />
in helping people recover<br />
from mental illness as they<br />
tend to have worse physical<br />
health than the general<br />
population <strong>and</strong> poorer access<br />
to appropriate healthcare<br />
services. The Trust’s mental<br />
health workers have a key<br />
role to play in this.<br />
Gardner Gwashavanhu, a wellbeing<br />
nurse adviser in Richmond, works<br />
collaboratively with the local GP practice,<br />
the multi-disciplinary team <strong>and</strong> service<br />
users to provide <strong>and</strong> promote physical<br />
assessments <strong>and</strong> health screenings.<br />
He also gives presentations on wellbeing<br />
<strong>and</strong> physical health across Richmond<br />
to teams such as senior nurses’ forums<br />
<strong>and</strong> helps organise wellbeing days for<br />
inpatient teams.<br />
Gardner says: “I provide a weekly inhouse<br />
clinic on a one-to-one basis. Every<br />
month we offer all clients check-ups for<br />
blood pressure <strong>and</strong> blood sugar levels,<br />
advice on managing side-effects <strong>and</strong><br />
monitoring of their body mass index<br />
(BMI). We also offer practical advice<br />
to individual clients on managing<br />
weight loss.<br />
“Our Healthy Lifestyle group meets<br />
weekly <strong>and</strong> provides help with healthy<br />
eating options, weight management <strong>and</strong><br />
cutting back smoking. The proportion<br />
of clients in the group who smoke has<br />
dropped from 90 per cent to 70 per cent<br />
<strong>and</strong> 71 per cent say they are now more<br />
confident about their physical health<br />
<strong>and</strong> wellbeing. A recent evaluation of<br />
our client group highlighted that 86 per<br />
cent of those who attend the weekly<br />
group session have changed their<br />
eating habits.<br />
“Our daily one-to-one walks <strong>and</strong> the<br />
peer-led sessions have also been a<br />
success. The average BMI of clients<br />
attending these sessions has fallen from<br />
27.6 to 24 over a three-month period<br />
<strong>and</strong> they have all regained fitness.<br />
By working collaboratively with our<br />
client group, we have managed to get<br />
half of the female clients into local gyms,<br />
where they have kept up attendance<br />
for 10 months.<br />
Below :<br />
Promoting<br />
a healthy<br />
lifestyle<br />
Gardner<br />
Gwashavanhu (left)<br />
with Anthony<br />
14 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Our new acute unit<br />
for W<strong>and</strong>sworth<br />
“My role has also given me<br />
the opportunity to share my<br />
knowledge of engaging with<br />
people with mental illness<br />
with other nursing staff in<br />
Richmond’s inpatient units.<br />
“I have also managed to maintain<br />
a co-working partnership <strong>and</strong> share<br />
knowledge with other professionals<br />
such as community dietitians,<br />
community diabetic nurses <strong>and</strong> GP<br />
nurse practitioners as well as mental<br />
health nurses in the Trust.<br />
“Promoting physical health need not be<br />
a complex task. The aim is to encourage<br />
service users to take up more exercise by<br />
creating activity <strong>and</strong> leisure groups that<br />
enable them to do so.”<br />
86%<br />
of those who attended<br />
our weekly Healthy<br />
Lifestyle group session<br />
have changed their<br />
eating habits, according<br />
to a recent evaluation.<br />
The Trust celebrated the<br />
‘topping out’ of its new<br />
W<strong>and</strong>sworth Acute Unit<br />
at Springfield University<br />
Hospital in March <strong>2008</strong>.<br />
The special ceremony, led<br />
by Ruth Carnall, Chief<br />
Executive of NHS <strong>London</strong>,<br />
was witnessed by around<br />
70 staff <strong>and</strong> user/carer representatives <strong>and</strong> a<br />
number of distinguished guests including the<br />
Mayor of W<strong>and</strong>sworth.<br />
The event was a milestone in the construction<br />
of this state-of-the-art facility which, when<br />
complete, will replace John Meyer <strong>and</strong> Bluebell<br />
wards with a 10-bed psychiatric intensive care<br />
unit <strong>and</strong> an 18-bed adult acute admission ward.<br />
The new wards will have private bedrooms with<br />
en-suite facilities, comfortable dining, recreation,<br />
reception <strong>and</strong> visitors’ areas, <strong>and</strong> direct access to<br />
open space. There will also be new facilities for<br />
outpatient services <strong>and</strong> clinical teams.<br />
The £22.9m project will be completed by<br />
February 2009, with patients moving into the<br />
new building in March. It is being managed by<br />
a multi-disciplinary project team with the full<br />
involvement of clinicians, service users <strong>and</strong> carers.<br />
To take full advantage of the new facility, new<br />
models of care are being designed that will be<br />
fully implemented by the time the new wards<br />
open. These will include a greater focus on<br />
recreational <strong>and</strong> therapeutic activities as part<br />
of an individual client’s care plan <strong>and</strong> a more<br />
structured daily routine, making use of flexible<br />
communal spaces as well as more secluded areas.<br />
Service users will also have 24-hour access to<br />
drinks <strong>and</strong> snacks <strong>and</strong> will be able to receive<br />
visitors in private.<br />
The new facilities will provide an environment<br />
of a high st<strong>and</strong>ard, offering service users a<br />
balance between security <strong>and</strong> inclusion. It will be<br />
designed to maximise service users’ therapeutic<br />
experience <strong>and</strong> to promote privacy <strong>and</strong> dignity,<br />
<strong>and</strong> will potentially improve recovery times.<br />
15
Zoning<br />
a carer’s story<br />
When Rebecca’s boyfriend was<br />
discharged from hospital she<br />
suddenly found herself in the<br />
role of carer <strong>and</strong> wondered<br />
how she would cope. “I felt<br />
that if we were going to have<br />
a future together I needed<br />
strategies to help keep him<br />
well,” she said.<br />
“We attended a Springfield Hospital<br />
open day where consultant nurse<br />
Catherine Gamble told us how the Trust<br />
now has a ‘traffic-light system’ called<br />
zoning. This uses green, amber <strong>and</strong><br />
red colours to share information about<br />
the state of clients’ safety <strong>and</strong> level<br />
of risk. The aim is to increase clinical<br />
effectiveness.<br />
“Green indicates patients who<br />
are stable; amber signifies<br />
people who are unwell <strong>and</strong><br />
need some additional support;<br />
<strong>and</strong> red shows clients who are<br />
high-risk or in crisis.<br />
“Catherine explained how making<br />
information available in this way helps<br />
prevent clients from relapsing <strong>and</strong><br />
improves services for them <strong>and</strong><br />
their families.<br />
“I felt this could be useful, so we asked<br />
the consultant psychiatrist to refer us.<br />
We had several visits from Catherine<br />
<strong>and</strong> a social worker, Sinead Dervin, first<br />
to take a history of what happened <strong>and</strong><br />
then to look back at the months leading<br />
up to the last hospital admission. My<br />
boyfriend <strong>and</strong> I each had homework<br />
to do independently – setting out his<br />
thoughts, behaviours <strong>and</strong> feelings up<br />
to his becoming unwell. We came<br />
back together to compare notes<br />
– <strong>and</strong> this was very helpful.<br />
“A year <strong>and</strong> a half after his stay in<br />
hospital, my boyfriend had been well<br />
for six months <strong>and</strong>, as planned, was<br />
discharged from the community mental<br />
health team.<br />
“He now came under his GP’s care but<br />
he needed someone to keep an eye<br />
on him. Zoning helped find a toolkit<br />
that wasn’t just dependent on me.<br />
What came through was that his manic<br />
behaviour was masking depression, low<br />
self esteem. Through our discussions<br />
I began to underst<strong>and</strong> that vulnerability,<br />
<strong>and</strong> to talk about my own feelings too.<br />
“The emphasis is on prevention, looking<br />
at what people can do for themselves<br />
<strong>and</strong> how families can help them.<br />
If you support people in green <strong>and</strong> their<br />
families you will have fewer hospital<br />
admissions <strong>and</strong> carers are more likely to<br />
stay on board in their caring role. I now<br />
find it easier, on a day-to-day basis,<br />
to identify what’s normal <strong>and</strong> what’s a<br />
sign of becoming unwell <strong>and</strong> to help<br />
my boyfriend get from mild amber<br />
back into green. And we feel sufficiently<br />
confident about the future that we’ve<br />
been able to start a family together.”<br />
Above right:<br />
More confident<br />
about the future<br />
Rebecca with her boyfriend<br />
<strong>and</strong> their baby son<br />
16 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Zoning in the Trust<br />
The Trust is aiming to become the first mental<br />
health trust to introduce the zoning traffic-light<br />
system to all its service areas. During the year<br />
there was a 23 per cent growth in the numbers<br />
of teams which had adopted zoning. Every team<br />
across the Trust is now using the zoning approach<br />
in some way <strong>and</strong> more than half of them have<br />
now fully implemented it.<br />
Zoning supports better team working <strong>and</strong> risk<br />
management, using regular reviews of individual<br />
service users’ needs <strong>and</strong> providing continuity<br />
throughout their care. It helps staff prioritise<br />
high-risk cases <strong>and</strong> gives teams a common<br />
language for them to engage users <strong>and</strong> carers<br />
– helping prevent clients from relapsing while<br />
improving services for them <strong>and</strong> their families.<br />
This fits in with the Trust’s recovery approach to<br />
mental illness.<br />
Our success on zoning was<br />
recognised in March <strong>2008</strong> when<br />
Catherine Gamble, Consultant<br />
Nurse at the Trust, won the<br />
Nursing <strong>St</strong><strong>and</strong>ard Mental Health<br />
Nurse of the Year award for<br />
her work in implementing the<br />
approach.<br />
Right:<br />
Mental<br />
Health Nurse<br />
of the Year<br />
Catherine Gamble<br />
innovative<br />
system<br />
The Trust now has a<br />
‘traffic-light system’<br />
called zoning.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 17
Talking therapies<br />
a graduate mental health worker’s story<br />
Waiting lists for psychotherapy<br />
are coming down <strong>and</strong> the Trust<br />
can give service users more<br />
personalised services based<br />
around their individual needs.<br />
Psychological Therapies in Primary<br />
Care (PTiPC), the Trust’s response to<br />
the government’s Improving Access to<br />
Psychological Therapies (IAPT) initiative,<br />
is making a big difference to the service<br />
we offer to new service users with<br />
depression or anxiety.<br />
The Trust has a PTiPC team in<br />
most boroughs, working alongside<br />
mainstream primary care services.<br />
Clare Watts is a graduate mental<br />
health worker – the equivalent of an<br />
assistant psychologist – in W<strong>and</strong>sworth.<br />
She previously worked on the Mood<br />
Manager DVD which was developed<br />
by W<strong>and</strong>sworth Teaching Primary Care<br />
Trust in collaboration with the Trust.<br />
Clare says: “Our role is to be the first<br />
point of contact for anyone with mild or<br />
moderate mental health problems who<br />
their GP has referred for psychotherapy.<br />
If their problems are more complex the<br />
GP will refer them to the community<br />
mental health team.<br />
“We start by talking to the person<br />
on the telephone to get a picture<br />
of their problems. Using measures<br />
recommended by NICE (the National<br />
Institute for Health <strong>and</strong> Clinical<br />
Excellence) we gauge what the main<br />
difficulties are <strong>and</strong> assess the level of<br />
risk <strong>and</strong> the need for social support.<br />
We take this information to our weekly<br />
case management meeting with clinical<br />
psychologists where possible treatment<br />
outcomes are discussed.<br />
“For mild to moderate symptoms<br />
we can offer computerised cognitive<br />
behavioural therapy (cCBT), which<br />
can be particularly effective. We use<br />
two packages recommended by NICE<br />
– FearFighter for treatment of anxiety<br />
<strong>and</strong> Beating the Blues for depression.<br />
These can be accessed at libraries <strong>and</strong><br />
community centres. We also facilitate<br />
groups on anxiety, depression, selfconfidence,<br />
<strong>and</strong> anger management.<br />
“The philosophy behind PTiPC is to<br />
screen people early on <strong>and</strong> to refer up<br />
to clinical or counselling psychologists<br />
only those whose symptoms are more<br />
complex. The aim is to reduce waiting<br />
lists <strong>and</strong> give people more options about<br />
what sort of treatment they can have.<br />
“Psychological therapy is now seen as<br />
less about having to see an expert to<br />
sort your problems out for you <strong>and</strong> more<br />
about guided self-help: what skills do I<br />
need to be able to cope with my mental<br />
health problem if it occurs again?<br />
“People are now being seen<br />
a lot quicker. Within days we<br />
can touch base <strong>and</strong> assess the<br />
risk. And making that phone<br />
call is a much more human<br />
approach than generating an<br />
appointment letter.”<br />
Above:<br />
A first point<br />
of contact<br />
Clare Watts<br />
18 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Happy Soul Festival<br />
Working with many local partners across south<br />
west <strong>London</strong>, the Trust ran two film <strong>and</strong> arts<br />
festivals in July <strong>2007</strong> <strong>and</strong> in March <strong>2008</strong> in local<br />
cinemas <strong>and</strong> community venues.<br />
These week-long Happy Soul Festivals, with new<br />
movies, live music <strong>and</strong> arts, focused on raising<br />
awareness of mental health among the black<br />
<strong>and</strong> Asian communities of Kingston, Merton,<br />
Richmond, Sutton <strong>and</strong> W<strong>and</strong>sworth, who<br />
had proved hard to reach via st<strong>and</strong>ard health<br />
promotion methods.<br />
Happy Soul attracted large numbers of people<br />
from the African-Caribbean, Asian <strong>and</strong> Korean<br />
communities, exploring the difficult subject of<br />
mental health <strong>and</strong> what it means to them.<br />
More than 200 of those attending the second<br />
Happy Soul Festival were surveyed. They<br />
responded very positively, with 53 per cent<br />
saying that their attitudes to mental health had<br />
changed as a result of attending a festival event.<br />
Described by the Department of Health’s<br />
Delivering Race Equality programme as an<br />
example of national good practice, our Happy<br />
Soul Festivals helped the Trust to forge new<br />
relationships with community partners across five<br />
<strong>London</strong> boroughs, <strong>and</strong> to find new <strong>and</strong> effective<br />
ways of communicating with BME communities.<br />
Our success was<br />
recognised by the<br />
Department of<br />
Health <strong>and</strong> the<br />
NHS Institute for<br />
Innovation <strong>and</strong><br />
Improvement’s<br />
Health <strong>and</strong> Social<br />
Care Awards, with<br />
the presentation,<br />
in April <strong>2008</strong>, of a Mental Health <strong>and</strong><br />
Wellbeing Award to the Trust’s Equality<br />
<strong>and</strong> Diversity Team.<br />
Right:<br />
Our Happy Soul Festivals reached<br />
out to local African-Caribbean, Asian<br />
<strong>and</strong> Korean communities<br />
19
Social care in partnership<br />
a social worker’s story<br />
As an Approved Social Worker,<br />
Mark <strong>St</strong><strong>and</strong>ing has the legal<br />
authority to assess people<br />
under the Mental Health<br />
Act. This responsibility – to<br />
determine whether detention<br />
in hospital or a less restrictive<br />
option will best meet a<br />
person’s needs – is something<br />
he doesn’t take lightly.<br />
Mark says: “Social work has a strong<br />
client focus <strong>and</strong> we always start by<br />
looking, beyond the initial clinical<br />
diagnosis, at the particular social<br />
circumstances that the client is in <strong>and</strong><br />
what support networks they have.”<br />
Although employed by W<strong>and</strong>sworth<br />
Council, Mark works in the Trust as a<br />
Principal Social Worker, based at Queen<br />
Mary’s Hospital. He provides professional<br />
supervision of the other social workers in<br />
Trust roles in Putney <strong>and</strong> Roehampton.<br />
“I work in the community mental<br />
health team which includes professionals<br />
from many different disciplines.<br />
They often ask social workers for<br />
advice” he says. “We’ve had training<br />
in mental health law <strong>and</strong> the other<br />
legislation associated with it <strong>and</strong><br />
we’ve also developed knowledge<br />
about housing <strong>and</strong> benefits.”<br />
One of the Trust’s key responsibilities<br />
is to safeguard vulnerable adults from<br />
harm. Mark says: “Vulnerable adults<br />
sometimes behave in a way that is a risk<br />
to themselves or others, or can be open<br />
to abuse or persuasion to part with their<br />
money. I take a lead in this area of work.<br />
“Many people using mental<br />
health services are entitled<br />
to social care funding, <strong>and</strong><br />
increasingly have choices over<br />
how this is spent. They can<br />
receive or control the money<br />
themselves through a direct<br />
payment or individual<br />
budget. I have a key role<br />
in promoting this.”<br />
Mark’s work frequently brings him<br />
into contact with other agencies in the<br />
borough. This might include a case<br />
conference organised by the borough’s<br />
children <strong>and</strong> families team to discuss<br />
the children being cared for by one<br />
of his clients, or a housing forum<br />
meeting where the housing officers are<br />
concerned about the behaviour of one<br />
of the tenants.<br />
“We also work very closely with<br />
W<strong>and</strong>sworth’s carers’ centre” Mark<br />
says. “As well as looking at the needs of<br />
mental health clients we do what we can<br />
to support those caring for them. They<br />
have needs <strong>and</strong> rights too – perhaps for<br />
more information, for specific services<br />
or just a listening ear. And we can apply<br />
to the local authority on their behalf<br />
for funding to provide respite care –<br />
enabling them to take a short break<br />
from their caring responsibilities. The<br />
Trust needs to work in partnership with<br />
carers <strong>and</strong> families to support them <strong>and</strong><br />
the people they care for.<br />
“I enjoy this job because I feel I can<br />
make a real difference to the lives of<br />
mental health service users <strong>and</strong> help<br />
them in their recovery.”<br />
Right:<br />
Making a real<br />
difference<br />
Mark <strong>St</strong><strong>and</strong>ing<br />
20 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Our performance in <strong>2007</strong>/08<br />
1<br />
At the beginning of <strong>2007</strong>/08, the Trust identified six key strategic objectives for the year:<br />
Providing clinical services that are demonstrably<br />
effective <strong>and</strong> safe<br />
The Chief Operating Officer led a successful review of adult services.<br />
Our implementation of the review’s findings has meant the largest change<br />
in Trust services for 20 years. This has affected most adult community<br />
services, with the jobs of hundreds of staff altered. Since March <strong>2008</strong>,<br />
the Trust has provided, for the first time, full Early Intervention <strong>and</strong> Crisis<br />
Resolution services to the local population. The Trust can now provide the<br />
critical best practice elements that were outlined in the National Service<br />
Framework for Mental Health.<br />
2<br />
3<br />
Alongside these structural changes we trained staff to use Health of the<br />
Nation Outcome Scales (HoNOS). This will allow a universal scale to outline<br />
the changes in the wellbeing of people using our services. HoNOS can now<br />
be recorded on our clinical information system, RiO, <strong>and</strong> their use will be<br />
exp<strong>and</strong>ed in the years to come.<br />
Providing a recovery approach across the organisation<br />
‘Recovery’ is about building a sense of self, meaning <strong>and</strong> purpose in life<br />
– growing beyond what has happened to you to make the most of your<br />
life. It is about people’s whole lives – not just their problems.<br />
The Trust believes a ‘recovery’ approach will provide the best outcomes<br />
for people using our services. During the year we provided introductory<br />
training to over 1,300 staff <strong>and</strong> in-depth, three-day training to over 85 staff<br />
to enable them to become recovery experts.<br />
We have also set up a robust programme management structure to sustain<br />
a culture change in the organisation that will promote recovery. The<br />
programme board, chaired by Maresa Ness, the Chief Operating Officer,<br />
<strong>and</strong> led by Miles Rinaldi who has been appointed Head of Recovery <strong>and</strong><br />
Social Inclusion, is now called Recovery <strong>and</strong> Self Directed Support to reflect<br />
the Trust’s commitment to deliver on local authorities’ personalised care<br />
agenda. We will enable people to use social care monies in more diverse<br />
<strong>and</strong> creative ways of their choice, supporting that recovery. Each of the five<br />
boroughs we serve now has a lead person <strong>and</strong> implementation group as<br />
well as committees relating to specific types of client, such as older people<br />
<strong>and</strong> children/adolescents.<br />
Ensuring the sustainability of services<br />
The Trust was disappointed by its Healthcare Commission rating of ‘Fair’ for<br />
quality of services <strong>and</strong> ‘Fair’ for use of resources <strong>and</strong> is prioritising measures<br />
to help improve this. <strong>St</strong>rategies for every service area were completed<br />
during summer <strong>2007</strong> <strong>and</strong> were summarised in the Service Development<br />
<strong>St</strong>rategy (published on our website), which will form a cornerstone of our<br />
application for foundation trust status.<br />
As a result of the Adult Service Review the Trust will for the first time meet<br />
all the critical targets, which should help to improve our rating.<br />
We also competed for six major tenders <strong>and</strong> Trust managers <strong>and</strong> clinicians have<br />
been trained in tendering <strong>and</strong> marketing in preparation for future competition.<br />
“We have also set up<br />
a robust programme<br />
management structure to<br />
sustain a culture change<br />
in the organisation that<br />
will promote recovery.“<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 21
Our performance in <strong>2007</strong>/08<br />
4<br />
5<br />
6<br />
Maximising the value of the estate<br />
High capital charges <strong>and</strong> backlog maintenance costs make our large <strong>and</strong><br />
old estate a financial burden. During the next three to five years the Trust<br />
intends to dispose of unnecessary buildings, lease others <strong>and</strong> redevelop<br />
the Springfield site to create modern <strong>and</strong> flexible mental health facilities,<br />
as outlined in an Estates <strong>St</strong>rategy during the year. The W<strong>and</strong>sworth Acute<br />
Unit, currently being built, will open in 2009.<br />
Creating a workforce that is fit for purpose<br />
To provide modern services the Trust needs to modernise the workforce,<br />
<strong>and</strong> to ensure that there is strong leadership at all levels <strong>and</strong> that staff are<br />
adequately trained <strong>and</strong> supported to perform their duties. During the year<br />
we introduced ‘development centres’ to help current staff underst<strong>and</strong> their<br />
own professional development needs. We also introduced assessment<br />
centres to ensure a rigorous <strong>and</strong> effective assessment of new clinical staff<br />
wishing to work for the Trust.<br />
The Electronic <strong>St</strong>aff Record we have introduced will provide comprehensive<br />
staffing information to aid effective management <strong>and</strong> streamline human<br />
resource processes.<br />
Maintaining financial balance<br />
We have built on our good record of delivering financial balance by<br />
achieving the required surplus to support our foundation trust application<br />
<strong>and</strong> the Healthcare Commission’s reviews of our performance. The Trust<br />
has developed a more business-oriented approach <strong>and</strong> is planning for new<br />
business opportunities, especially those afforded by the vacant space in the<br />
estate.<br />
The summary annual accounts are set out on pages 37 to 39.<br />
“During the next<br />
three to five years<br />
the Trust intends to<br />
create modern<br />
<strong>and</strong> flexible mental<br />
health facilities.”<br />
Below:<br />
Making performance<br />
information more<br />
accessible<br />
Demonstrating The Pulse,<br />
our new data warehouse<br />
As well as progress against its strategic<br />
objectives, the Trust has sought to<br />
make performance information more<br />
accessible to managers <strong>and</strong> clinicians.<br />
During the year, we introduced<br />
‘The Pulse’. This provides real-time<br />
activity information to staff on a range<br />
of performance measures, allowing<br />
them to see information relating to their<br />
own work, their team’s practice <strong>and</strong><br />
the Trust’s performance. In this way, we<br />
hope to make performance reporting<br />
relevant <strong>and</strong> helpful to the people who<br />
are delivering the services as well as<br />
those monitoring the services.<br />
The Trust is proud to be one of the<br />
few mental health organisations to<br />
continually monitor service users’<br />
experience of our services. The<br />
Director of Quality Assurance <strong>and</strong><br />
User/Carer Experience, Dr Rachel Perkins,<br />
has repeated the survey for a further<br />
year, allowing us to monitor<br />
changes in how services are received <strong>and</strong><br />
highlight areas that need improvement.<br />
Poorly performing teams from the<br />
first survey have shown substantial<br />
improvements in key areas of the service<br />
user experience <strong>and</strong> the survey has now<br />
proved a critical tool in assuring the<br />
quality of these services.<br />
We also exp<strong>and</strong>ed the range of<br />
performance measures to include key<br />
support services. For example, the<br />
Estates <strong>and</strong> Facilities department can<br />
now demonstrate their performance,<br />
which shows that they complete 92 per<br />
cent of maintenance tasks within the<br />
expected timescale.<br />
22 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
<strong>Annual</strong> health check<br />
Two years ago, the Healthcare Commission introduced its system for assessing <strong>and</strong><br />
rating the performance of all NHS healthcare organisations in Engl<strong>and</strong>. Aimed at<br />
driving improvements in healthcare for service users, it provides an annual health<br />
check <strong>and</strong> is designed to give service users a comprehensive view of how the Trust<br />
is performing in a wide range of areas including safety, cleanliness, planning for<br />
emergencies <strong>and</strong> managing finances.<br />
All NHS organisations receive a two-part scoring – the first part looks at the quality of<br />
its services <strong>and</strong> the second part looks at how well an organisation uses its resources.<br />
For 2006/07, the Trust received a ‘fair’ rating for both its quality of<br />
services <strong>and</strong> its use of resources. A number of Trust-wide initiatives<br />
have been introduced to strengthen the Trust’s compliance <strong>and</strong> to<br />
help us improve our rating for <strong>2007</strong>/08, including:<br />
• completion of a review of the Trust’s adult services. This aims to provide our service<br />
users with prompt, safe, accessible <strong>and</strong> effective treatment <strong>and</strong> support based on the<br />
best evidence available, consistent with individual preferences <strong>and</strong> priorities<br />
• implementation of a quality improvement programme. This builds on examples of<br />
excellent practice taking place across the Trust <strong>and</strong> focuses on ‘dignity <strong>and</strong> respect’,<br />
‘informing <strong>and</strong> communicating’ <strong>and</strong> ‘involving <strong>and</strong> valuing’<br />
“prompt, safe,<br />
accessible <strong>and</strong> effective<br />
treatment <strong>and</strong> support”<br />
• participation in a national programme, led by the Royal College of Psychiatrists,<br />
which should improve prescribing practice across the Trust<br />
• completion of an extensive review of the Trust’s forensic services<br />
• promotion of recovery <strong>and</strong> facilitating social inclusion, recognising that everyone<br />
with mental health problems faces the challenge of retaining or recovering a life<br />
that is meaningful, satisfying <strong>and</strong> valued<br />
• development of a management development training programme available to<br />
all Trust staff<br />
“promote recovery<br />
<strong>and</strong> facilitate social<br />
inclusion”<br />
• achieving a 100 per cent score for a Level 1 assessment against a series of risk<br />
management st<strong>and</strong>ards led by the NHS Litigation Authority, demonstrating that the Trust<br />
is doing its reasonable best to manage risk in line with its Risk Management <strong>St</strong>rategy.<br />
In April <strong>2008</strong>, the Trust submitted its final declaration against the 24 national core<br />
st<strong>and</strong>ards for the period <strong>2007</strong>/08 to the Healthcare Commission. Progress has been made<br />
against a number of the core st<strong>and</strong>ards since the previous year, including improvements<br />
to the provision <strong>and</strong> quality of service user <strong>and</strong> carer information.<br />
There is still more that needs to be done before we are compliant with all the core<br />
st<strong>and</strong>ards. The Trust has made significant progress towards ensuring all our buildings<br />
meet the Healthcare Commission’s criteria. The Trust has opened two new single-sex<br />
wards <strong>and</strong> improved inpatient services for older people in W<strong>and</strong>sworth <strong>and</strong> Merton,<br />
opening a refurbished ward segregated by gender. However, the Trust awaits the<br />
completion of the W<strong>and</strong>sworth Acute Unit (see page 15) to enable us to declare<br />
compliance against all the core st<strong>and</strong>ards.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 23
Our objectives for the next three years<br />
Over the past year the Trust has made good progress in reconfiguring community<br />
teams to deliver targets <strong>and</strong> has improved the quality <strong>and</strong> effectiveness of its<br />
forensic services.<br />
In the next three years the Trust plans to make significant changes in seven<br />
key priority areas. The first three priority areas will transform the quality <strong>and</strong><br />
effectiveness of our services <strong>and</strong> the next four constitute enabling strategies to<br />
underpin this transformation.<br />
1<br />
2<br />
3<br />
4<br />
Embedding recovery <strong>and</strong> self-directed care<br />
The Trust provides exemplary vocational services that are the basis for the<br />
introduction of the recovery approach to care. The Trust’s approach has been<br />
refined during <strong>2007</strong>/08 <strong>and</strong> we will continue to train staff <strong>and</strong> manage the<br />
outcomes of the approach. We expect this model to be extended into housing<br />
<strong>and</strong> social care domains in the medium term.<br />
We will embed the recovery approach into all aspects of our service<br />
development <strong>and</strong> delivery. This will include ensuring that all staff have at<br />
least received the introductory training. The impact of this way of working will<br />
become increasingly apparent in all service plans <strong>and</strong> will have a growing<br />
impact on service user outcomes.<br />
Providing clinical services that are demonstrably effective<br />
<strong>and</strong> safe<br />
The Trust has successfully created the full range of teams required under<br />
the National Service Framework to meet best practice guidance. To support<br />
developments in clinical practice, the Trust has focused on improving the<br />
recording of diagnosis <strong>and</strong> has introduced RiO (the new clinical electronic<br />
information system whereby care professionals can plan, schedule <strong>and</strong> record<br />
treatment <strong>and</strong> can access up-to-date information easily). We are currently<br />
implementing the Health of the Nation Outcome Scale (HoNOS), which is a<br />
tool for measuring improved outcomes resulting from health <strong>and</strong> social care<br />
interventions for people experiencing mental health problems.<br />
These developments will prepare us for robust outcome reporting in the future<br />
<strong>and</strong> enable us to plan our services better.<br />
Ensuring that we attain targets<br />
Changes in clinical delivery have enabled us to meet the National Service<br />
Framework team targets from April <strong>2008</strong>. We now fully meet the key targets<br />
for mental health. Over the coming year we will meet caseload <strong>and</strong> activity<br />
targets <strong>and</strong> aim to improve our annual health check <strong>and</strong> Auditors’ Local<br />
Evaluation rating.<br />
Becoming a foundation trust<br />
Preparatory work undertaken in <strong>2007</strong>/08 has provided a robust infrastructure<br />
for our foundation trust application. We believe that the changes we have<br />
already made will equip us to become a successful <strong>and</strong> effective foundation<br />
trust in a year’s time. Work to engage service users, staff <strong>and</strong> external<br />
stakeholders is well underway <strong>and</strong> we have embedded the strategic direction of<br />
working towards this goal within all our planning for the year.<br />
“We believe that the<br />
changes we have<br />
already made will<br />
equip us to become<br />
a successful <strong>and</strong><br />
effective foundation<br />
trust in a year’s time.”<br />
24 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
5<br />
6<br />
Developing our estate<br />
As we shift our resources more towards daycare <strong>and</strong> care in the<br />
community, the need for inpatient admission has continued to decrease.<br />
Although the rate of decrease is slowing down, the Trust has reduced<br />
its adult bed numbers by 27 per cent over the past five years, which has<br />
affected the clinical <strong>and</strong> financial viability of smaller inpatient sites. The<br />
Trust is working with local commissioners collectively to identify a way<br />
forward which achieves an effective balance between local access for<br />
service users <strong>and</strong> carers <strong>and</strong> clinical safety <strong>and</strong> cost effectiveness.<br />
These objectives are encapsulated within our Estates <strong>St</strong>rategy, a key<br />
element of which is the regeneration <strong>and</strong> redevelopment of the Springfield<br />
Hospital site. The overall programme may take up to 20 years to realise but<br />
concrete steps will be taken in <strong>2008</strong>/09 to ensure momentum is achieved<br />
to take this ambitious <strong>and</strong> exciting programme forward.<br />
Creating a workforce that is fit for purpose<br />
To provide modern services the Trust needs to remodel the workforce,<br />
<strong>and</strong> to ensure that there is strong leadership at all levels <strong>and</strong> that staff are<br />
adequately trained <strong>and</strong> supported to perform their duties.<br />
The Trust has implemented a programme of assessment <strong>and</strong> development<br />
centres during the year to ensure that staff have the skills <strong>and</strong> support<br />
needed to perform their duties. The rollout of the Knowledge <strong>and</strong> Skills<br />
Framework (KSF) has been completed during the year under review <strong>and</strong><br />
the Electronic <strong>St</strong>aff Record is currently being introduced across the Trust.<br />
“We are committed<br />
to implementing<br />
New Ways of Working<br />
for all staff.”<br />
Over the next five years, service users will increasingly be supported on a<br />
daily basis by workers trained in the recovery approach.<br />
7<br />
This is reflected in our commitment to implementing New Ways of<br />
Working for all staff. Consequently, the new Medical Director <strong>and</strong><br />
the Director of Nursing <strong>and</strong> Governance, along with the Heads of<br />
Occupational Therapy, Psychology & Psychotherapies <strong>and</strong> Social Work,<br />
will be remodelling the multi-professional team in close collaboration<br />
with the Director of Human Resources <strong>and</strong> the borough service directors.<br />
Maintaining financial balance<br />
The Trust has a good record of delivering financial balance. We are<br />
developing a more business-oriented approach. By underst<strong>and</strong>ing our costbase,<br />
<strong>and</strong> by ensuring income through signing service level agreements<br />
early in the year, we are underpinning the delivery of effective <strong>and</strong><br />
sustainable services in the years to come.<br />
These priorities are monitored <strong>and</strong> assured by a compliance framework<br />
overseen by the Board <strong>and</strong> the requirement to fulfil our statutory duties.<br />
We have also put in place new structures to ensure compliance with<br />
equalities legislation <strong>and</strong> to ensure that the experience of service users<br />
<strong>and</strong> carers is integral to planning at all levels within the organisation. The<br />
Clinical Services Development Programme assures service user input into<br />
service development <strong>and</strong> Service User Experience Audits provide robust,<br />
continuous information on service users’ views.<br />
Above:<br />
Adil Akram<br />
Adil, who works at the Trust,<br />
is Walport Academic Clinical<br />
Fellow <strong>and</strong> Specialist Registrar in<br />
Psychiatry <strong>and</strong> also a documentary<br />
film-maker. Adil’s film, Over my<br />
Left Shoulder, tells the story of<br />
a mother of two young sons,<br />
who was treated at Springfield’s<br />
Mother <strong>and</strong> Baby Unit for<br />
post-natal depression<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 25
Overview<br />
Forensic service<br />
Our forensic service partly re-opened<br />
in June <strong>2007</strong> <strong>and</strong> fully reopened in<br />
August, following the conclusion of<br />
the Making Connections review led<br />
by Professor Tony Maden. The review<br />
examined the performance of the service<br />
<strong>and</strong> its relationship with psychiatric<br />
intensive care units <strong>and</strong> challenging<br />
behaviour rehabilitation services within<br />
the Trust. The review team’s report<br />
<strong>and</strong> recommendations demonstrated<br />
the considerable service improvement<br />
achieved over the past year in procedural,<br />
relational <strong>and</strong> environmental security.<br />
Professor Maden commented that<br />
the management of the service had<br />
been transformed <strong>and</strong> that systems<br />
<strong>and</strong> attitudes had changed completely,<br />
indicating that the forensic service is not<br />
only more effective but a happier place<br />
in which to work. Eighteen of the review<br />
team’s recommendations have been<br />
completed successfully. Significant progress<br />
has been made on two of the remaining<br />
three objectives – to create a rotation<br />
scheme for B<strong>and</strong> 5 nursing staff in forensic<br />
wards <strong>and</strong> to establish a single challenging<br />
behaviour service across the Trust. We will<br />
seek to achieve these in the coming year.<br />
The sole outst<strong>and</strong>ing recommendation is<br />
that the forensic service should establish<br />
a multi-disciplinary group of advanced<br />
practitioners to lead a specialised<br />
substance misuse treatment programme.<br />
After investigation it was agreed that<br />
current resources would not permit such<br />
a development but it remains a priority<br />
for the future.<br />
Promoting equality<br />
The Trust is implementing its<br />
Disability Equality Scheme action<br />
plan, directed at promoting disability<br />
equality in employment <strong>and</strong> in the<br />
services we provide. We have made<br />
progress towards making the physical<br />
environment more accessible <strong>and</strong> each<br />
borough is addressing ways in which it<br />
can further meet the needs of people<br />
with mobility <strong>and</strong> sensory impairments<br />
<strong>and</strong> long-term health conditions.<br />
The Trust also has a Gender Equality<br />
Scheme <strong>and</strong> has been addressing<br />
the requirements of the new age<br />
discrimination legislation <strong>and</strong> also the<br />
need to promote equality for lesbian,<br />
gay <strong>and</strong> bisexual staff <strong>and</strong> service users.<br />
The Trust is an equal opportunities<br />
employer <strong>and</strong> welcomes job applications<br />
from people who have experienced<br />
mental health problems. Our User<br />
Employment programme facilitates<br />
access to employment within the<br />
organisation for people who have<br />
themselves experienced mental health<br />
problems. It has supported more than<br />
150 employees with mental health<br />
problems in 180 job roles in the Trust.<br />
Since 1999 at least 17 per cent of newly<br />
recruited employees have had personal<br />
experience of mental health problems. In<br />
<strong>2007</strong>/08 the figure for new recruits had<br />
risen to 24 per cent. People with mental<br />
health problems have been employed at<br />
all levels of the organisation <strong>and</strong> within<br />
all the mental health professions.<br />
Delivering race equality<br />
in mental health<br />
In Delivering Race Equality, the<br />
Department of Health said that by<br />
2010 mental health services should<br />
be characterised by:<br />
• less fear of mental health services<br />
among black <strong>and</strong> minority ethnic<br />
(BME) communities<br />
• increased satisfaction with services<br />
• a reduction in the rate of<br />
admission of people from BME<br />
communities to psychiatric<br />
inpatient units<br />
• fewer violent incidents<br />
• a reduction in the use of seclusion<br />
• the prevention of deaths in mental<br />
health services following physical<br />
intervention<br />
• increased BME access to<br />
counselling <strong>and</strong> psychological<br />
therapies<br />
• more active outreach <strong>and</strong> working<br />
with BME communities to promote<br />
access <strong>and</strong> the delivery of culturally<br />
sensitive services.<br />
We also have race equality responsibilities<br />
as an employer to promote equality<br />
of opportunity among our workforce<br />
irrespective of race (<strong>and</strong> also gender or<br />
disability). Our workforce, our professions,<br />
<strong>and</strong> the ethnic profile of junior <strong>and</strong> senior<br />
positions should largely reflect the ethnic<br />
profile of our local community.<br />
The delivery of race equality represents<br />
huge challenges for the Trust as a service<br />
provider <strong>and</strong> as an employer.<br />
Talking to BME populations about their<br />
perspectives <strong>and</strong> needs is the most<br />
important thing in delivering ethnically<br />
sensitive services. But mental illness<br />
can be a taboo subject in some of<br />
our cultures – <strong>and</strong> so the incidence<br />
of mental illness gets hidden within<br />
communities. Individuals who need help<br />
at an early intervention stage, but are<br />
26 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
not able to access treatment, may then<br />
develop severe mental illness. Mental<br />
health services, including our own,<br />
consistently show a higher proportion of<br />
BME patients detained under the Mental<br />
Health Act than would be expected from<br />
the population profile.<br />
As a Trust, we have organised the Happy<br />
Soul Festival (see page 19) to engage<br />
<strong>and</strong> raise the mental health awareness of<br />
our local BME populations. This involved<br />
running film <strong>and</strong> arts events with mental<br />
health themes, <strong>and</strong> discussions with<br />
BME role models <strong>and</strong> celebrities. Our<br />
most recent Happy Soul events attracted<br />
1,200 members of the public.<br />
We employ community development<br />
workers to engage with <strong>and</strong> provide a<br />
link between BME populations <strong>and</strong> the<br />
Trust. Their work with communities is<br />
tireless <strong>and</strong> is an important contributor<br />
to our responsibility to delivering race<br />
equality. For instance, we are now<br />
able to provide information in many<br />
languages about mental illnesses <strong>and</strong><br />
the services we provide.<br />
The Trust’s Race Equality <strong>St</strong>eering Group<br />
develops action plans <strong>and</strong> monitors<br />
their progress against a number of key<br />
race equality indicators. We are seeing<br />
positive trends in the use of seclusion;<br />
the experience of BME patients on our<br />
wards; <strong>and</strong> the use of restraint. However,<br />
there is still much work to do in areas<br />
such as use of the Mental Health Act.<br />
We will continue to challenge our<br />
processes as an employer. For instance,<br />
some of our professions (such as<br />
nursing) are currently over-represented<br />
by people from BME groups while<br />
others (such as psychology) are underrepresented.<br />
Some of this disparity is a<br />
reflection of our wider society but we<br />
must continually question ourselves if<br />
we are going to accept the challenge of<br />
delivering race equality.<br />
Left:<br />
We value our staff<br />
Community Psychiatric Nurse<br />
Joyce Mutabeni (left) with Christine<br />
in the art room<br />
Valuing our staff<br />
The fifth annual NHS staff survey took place in autumn <strong>2007</strong>. Survey<br />
questionnaires focusing on 26 key areas were sent to a r<strong>and</strong>om sample<br />
of our staff. The survey’s results are important to us in providing feedback on<br />
how our staff feel about the organisation they work for. In this most recent<br />
survey staff told us that things had improved in nine important areas.<br />
In particular, staff indicated that they felt more valued because the quality<br />
of work-life balance had improved, they received more support from their<br />
immediate manager <strong>and</strong> their job satisfaction had increased. The improved<br />
results also include a reduction in the number of staff working extra hours <strong>and</strong> a<br />
reduction in the percentage of staff reporting work pressure.<br />
We are also pleased that 81 per cent of our staff received relevant training,<br />
learning <strong>and</strong> development during the year under review. This is a great<br />
improvement on the previous year <strong>and</strong> puts us in the highest 20 per cent of<br />
mental health <strong>and</strong> learning disability trusts. Giving staff the opportunity for the<br />
right development <strong>and</strong> learning is a vital part of our workforce strategy <strong>and</strong> we<br />
will continue to strengthen <strong>and</strong> build on this.<br />
Early last year we ran a number of focus groups to find out how we could<br />
enhance our welcome to staff joining the Trust. Our new-look two-day induction<br />
programme has proved very successful <strong>and</strong> gives those joining us more time to<br />
get to know the organisation.<br />
Our annual good practice marketplace event, which is also open to the public,<br />
provides a unique opportunity for networking <strong>and</strong> self-directed learning by staff.<br />
This year’s event, attended by over 340 people, was our largest ever, with over<br />
60 display stalls showcasing good practice <strong>and</strong> inspirational innovations in mental<br />
health services. It was followed by our <strong>2007</strong> Quality Awards ceremony where<br />
over 200 invited guests honoured outst<strong>and</strong>ing service, dedication <strong>and</strong> innovation<br />
by Trust staff. There were 16 awards, with 46 teams or individuals making the<br />
shortlist. In total, 87 people nominated their colleagues for special recognition<br />
– a 53 per cent increase on the previous year.<br />
During the year we completed the implementation of the Electronic <strong>St</strong>aff<br />
Record (ESR) project <strong>and</strong> many staff in the Finance, Human Resource <strong>and</strong> IM&T<br />
departments worked together to ensure this could happen. The next phase of<br />
work is now underway <strong>and</strong> as a result our ability to forecast useful trends, for<br />
example track vacancy rates <strong>and</strong> training undertaken, will improve.<br />
During the year we have reviewed a number of new HR policies including<br />
managing sickness absence <strong>and</strong> our bullying <strong>and</strong> harassment (dignity at work)<br />
policies. We have put processes in place to support staff in raising any concerns<br />
they may have through the proper channels.<br />
Throughout the year we have continued to work as closely as we can with staff<br />
representatives to achieve improvements <strong>and</strong> changes to the services we provide.<br />
We have received positive feedback that we are involving staff more fully.<br />
However, we know that we have more to do in this area <strong>and</strong> we will be working<br />
on a revised partnership agreement with union <strong>and</strong> staff representatives in the<br />
next couple of months. We will also continue to develop our ways of informing<br />
<strong>and</strong> involving staff at all levels of the organisation on issues that affect their<br />
employment <strong>and</strong> the strategy <strong>and</strong> business of the Trust.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 27
Overview<br />
Communicating<br />
with staff<br />
During the year we continued<br />
to update our staff on key<br />
developments at the Trust through<br />
our weekly briefing by email to<br />
all staff, our quarterly newsletter<br />
Trustwide, a monthly team briefing,<br />
<strong>and</strong> monthly site briefings.<br />
Our intranet, Quick, has proved to be a<br />
vital communication tool in conveying<br />
messages quickly to our staff who<br />
are based at more than 90 different<br />
sites. In response to staff feedback we<br />
relaunched Quick in March <strong>2008</strong>. The<br />
redesigned intranet has a more newsoriented<br />
home page with links, which<br />
are easier to use, to the most popular<br />
pages <strong>and</strong> sections.<br />
Working with<br />
our partners<br />
The Trust has a long history of<br />
involving those who use our services<br />
<strong>and</strong> their relatives, friends <strong>and</strong><br />
carers. We aim to include our service<br />
users in all aspects of our operation<br />
<strong>and</strong> future development.<br />
We also believe we can provide better<br />
care through working in partnership<br />
with a range of other organisations from<br />
the public <strong>and</strong> independent sectors.<br />
During the year, our most successful<br />
new service programmes have been the<br />
result of effective partnership working.<br />
Examples include:<br />
• with Secure Healthcare, the<br />
tender to provide mental health<br />
<strong>and</strong> substance misuse services to<br />
W<strong>and</strong>sworth Prison<br />
• our Adults who are Chronically<br />
Excluded (ACE) programme with<br />
a range of agencies including<br />
probation, primary care <strong>and</strong> social<br />
services <strong>and</strong> funded by the Social<br />
Exclusion Task Force<br />
• our Co-Creating Health<br />
programme with W<strong>and</strong>sworth<br />
Teaching Primary Care Trust <strong>and</strong><br />
the Health Foundation.<br />
We have a major partnership with social<br />
services in Kingston, Merton, Richmond,<br />
Sutton <strong>and</strong> W<strong>and</strong>sworth <strong>and</strong> we strive<br />
to ensure that health <strong>and</strong> social care is<br />
provided through integrated, coherent<br />
teams. These teams help to minimise<br />
the difficulties for those experiencing<br />
mental health problems by ensuring<br />
that statutory sector resources can be<br />
accessed together in one place. This<br />
has been enhanced in services for<br />
older people during the year with full<br />
integration of community teams in all<br />
areas. These partnership arrangements<br />
are governed by formal agreements.<br />
The four primary care trusts (PCTs)<br />
covering the five boroughs we serve<br />
provide the majority of mental health<br />
care, especially for common mental<br />
health problems, through GP surgeries.<br />
They also commission secondary services<br />
for their populations from the Trust. This<br />
dual relationship means the Trust has<br />
close links with the PCTs. The Trust has<br />
service level agreements with all local<br />
PCTs to cover the provision of generic<br />
services <strong>and</strong> agreements with PCTs<br />
throughout <strong>London</strong> <strong>and</strong> nationally to<br />
provide specialist mental health services.<br />
In providing support for people<br />
experiencing mental health problems,<br />
particularly around vocational <strong>and</strong><br />
advocacy services, the Trust has active<br />
partnerships with several agencies in<br />
the independent <strong>and</strong> voluntary sectors,<br />
including Rethink, Sound Minds<br />
<strong>and</strong> MIND.<br />
We also work closely with the police <strong>and</strong><br />
acute hospitals, as well as local academic<br />
organisations, which help meet the<br />
education <strong>and</strong> training requirements of<br />
our staff as well as providing support for<br />
research <strong>and</strong> development.<br />
Above:<br />
Working in partnership<br />
Linda Lutchmayah, Ward<br />
Manager in the Phoenix Unit at<br />
Springfield University Hospital<br />
28 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Listening to our<br />
service users<br />
To improve our services, we have<br />
to underst<strong>and</strong> people’s experience<br />
of using them. Every year we ask<br />
people who have used our services<br />
to complete, anonymously, a<br />
questionnaire. This information is then<br />
fed back to teams within the Trust to<br />
develop action plans for improving the<br />
service they offer.<br />
We are very grateful to the 1650<br />
people who returned questionnaires<br />
in <strong>2007</strong>/08:<br />
• 91 per cent said that the service<br />
they received was ‘good’, ‘very<br />
good’ or ‘excellent’<br />
• at least 80 per cent said that<br />
their doctor, nurse <strong>and</strong> other<br />
professionals they saw listened to<br />
them carefully <strong>and</strong> treated them<br />
with dignity <strong>and</strong> respect.<br />
In comparison with the surveys<br />
conducted in 2006/07, there were<br />
improvements in a number of important<br />
areas including:<br />
• the extent to which people felt<br />
they had a say in decisions about<br />
their treatment <strong>and</strong> care <strong>and</strong> had<br />
their diagnosis fully explained<br />
to them<br />
• the proportion of people who<br />
knew the name of their care<br />
coordinator<br />
• the proportion of people who<br />
had an out-of-hours telephone<br />
number they could call in an<br />
emergency <strong>and</strong> the proportion<br />
who got through immediately<br />
when they called.<br />
In addition to our local surveys, the<br />
Healthcare Commission organises its<br />
own national survey, using a r<strong>and</strong>om<br />
sample, of people using mental health<br />
trust services – <strong>and</strong> the improvements<br />
observed in local surveys are reflected in<br />
the Commission’s published results.<br />
To help organisations compare their<br />
performance with that of other trusts,<br />
the Healthcare Commission produces<br />
‘benchmark indicators’ in four key areas:<br />
patient dignity, involvement in care<br />
planning, care coordination <strong>and</strong> out-ofhours<br />
help.<br />
On these indicators, <strong>South</strong> <strong>West</strong> <strong>London</strong><br />
<strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust<br />
performed better than all other <strong>London</strong><br />
mental health trusts. In comparison with<br />
other <strong>London</strong> trusts, a higher proportion<br />
of those using our services said that:<br />
• staff treated them with dignity<br />
<strong>and</strong> respect<br />
• they were involved in decisions<br />
about their care plan<br />
• they could get help out of hours<br />
when they needed it.<br />
In only one other <strong>London</strong> trust did a<br />
higher proportion of people know the<br />
name of their care coordinator.<br />
Despite this success we know that there<br />
is more that we can do to improve<br />
people’s experiences of our services.<br />
Over the coming year we will strive to<br />
further improve the information that we<br />
provide to people, <strong>and</strong> do our best to<br />
ensure that everyone feels fully involved<br />
in decisions about all aspects of their<br />
treatment <strong>and</strong> support <strong>and</strong> gets the help<br />
they need when they are in crisis.<br />
Improving the<br />
hospital environment<br />
Having a safe, clean <strong>and</strong> modern<br />
environment for our inpatient<br />
facilities is important to service<br />
users’ recovery. As well as the<br />
major development work for the new<br />
W<strong>and</strong>sworth Acute Unit, developments<br />
over the last year include:<br />
• enhancements to a number of<br />
wards, including the opening of<br />
the newly refurbished Crocus ward<br />
at Springfield University Hospital<br />
• upgrading <strong>and</strong> refurbishment of<br />
more than 20 patient bathrooms<br />
<strong>and</strong> toilets as part of our Quality<br />
Improvement Programme<br />
• the continuation of our<br />
programme of refurbishment <strong>and</strong><br />
redecoration in the Trust’s main<br />
buildings.<br />
We have continued to implement<br />
the Estates <strong>St</strong>rategy to help achieve<br />
our aim that all our buildings should<br />
be to a recognised acceptable st<strong>and</strong>ard<br />
by 2017.<br />
Going green<br />
The Trust has continued to<br />
implement a number of measures<br />
to address the green agenda. These<br />
have included:<br />
• setting up an Energy Action Group<br />
to ensure that energy is conserved<br />
<strong>and</strong> utilised in the best possible<br />
way. We have continued to<br />
promote energy awareness among<br />
staff <strong>and</strong> are investing in a number<br />
of capital schemes that will reduce<br />
energy consumption<br />
• implementing a Green Travel Plan<br />
that has included a Cycling to<br />
work event <strong>and</strong> promoting cycling<br />
generally across the Trust. The<br />
Trust has now joined the <strong>London</strong><br />
Cycling Scheme which works with<br />
the Trust to promote the benefits<br />
of cycling. As part of the Plan<br />
we will install additional cycling<br />
facilities such as showers <strong>and</strong><br />
secure cycle shelters<br />
• introducing a recycling scheme at<br />
Springfield in April <strong>2008</strong>. We will<br />
roll it out across the Trust during<br />
<strong>2008</strong>/09.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 29
Overview<br />
Going Lean<br />
In striving for excellence, equity <strong>and</strong><br />
the efficient use of resources the<br />
Trust is increasingly applying Lean<br />
thinking <strong>and</strong> Lean techniques in<br />
both clinical <strong>and</strong> non-clinical services.<br />
Simply put, this means using less to do<br />
more. Lean techniques help us focus on<br />
activities that provide value as perceived<br />
by our ‘customers’ <strong>and</strong> eliminate parts of<br />
our work that are wasteful.<br />
For clinical services, value is any activity<br />
which improves the patient’s health,<br />
wellbeing <strong>and</strong> experience. Waste on the<br />
other h<strong>and</strong> is the time that the patient<br />
spends waiting unnecessarily, or receiving<br />
less effective care or unnecessary tests.<br />
One of many local examples is the<br />
‘Releasing Time to Care’ initiative<br />
currently running on seven wards. The<br />
Trust successfully bid for funding to train<br />
10 frontline staff in this approach. Our<br />
partners in this programme, the NHS<br />
Institute for Innovation <strong>and</strong> Improvement,<br />
found that across the country nurses<br />
spend less than 40 per cent of their time<br />
on direct patient care.<br />
Giving frontline staff the tools <strong>and</strong> skills to<br />
look at their own processes <strong>and</strong> systems<br />
from a Lean perspective aims to turn this<br />
situation around. It makes quality <strong>and</strong><br />
waste the concern of every employee,<br />
<strong>and</strong> gives them the means <strong>and</strong> authority<br />
to change things. This in turn energises<br />
staff <strong>and</strong> contrasts with a traditional<br />
approach of quality inspection <strong>and</strong> driving<br />
efficiencies through cuts.<br />
Information<br />
Management <strong>and</strong><br />
Technology (IM&T)<br />
<strong>2007</strong>/08 was a very productive<br />
year for IM&T. The main<br />
achievements were:<br />
• the development of a new IM&T<br />
<strong>St</strong>rategy for the Trust<br />
• the completion of the rollout of<br />
RiO (the new electronic patient<br />
record system)<br />
• the further development <strong>and</strong><br />
rollout of the ‘data warehouse’<br />
<strong>and</strong> its associated reporting<br />
tool. The data warehouse brings<br />
together clinical, financial <strong>and</strong><br />
workforce datasets <strong>and</strong> enables<br />
managers <strong>and</strong> senior clinicians<br />
to view up-to-date performance<br />
reports<br />
• the provision of computers in ward<br />
areas for service users to use. This<br />
provides a facility to support service<br />
users in their recovery <strong>and</strong> to gain<br />
IT skills<br />
• the implementation of ITIL (IT<br />
Infrastructure Library) – an industry<br />
best practice st<strong>and</strong>ard for IT<br />
services. This has enabled the IT<br />
department to improve the quality<br />
of its service<br />
• support for the implementation of<br />
the Electronic <strong>St</strong>aff Record<br />
• the piloting of mobile technology<br />
in clinical teams<br />
• the approval of a business case to<br />
invest in mobile technology.<br />
The IT Service Desk received national<br />
accreditation (making us the first mental<br />
health trust, <strong>and</strong> the second <strong>London</strong><br />
trust to achieve this) <strong>and</strong> our IM&T<br />
services were the runners-up in the<br />
national Health Informatics Accolade<br />
Scheme, for the implementation of RiO.<br />
Some other projects which began in<br />
<strong>2007</strong>/08 will be completed in the coming<br />
year. These include:<br />
• the introduction of smartcards<br />
for staff to use when accessing<br />
computers <strong>and</strong> national systems<br />
such as RiO<br />
• the upgrading of RiO to version 5<br />
• the rollout of mobile technology to<br />
community-based clinicians<br />
• electronic ordering (e-procurement).<br />
Mobile working<br />
A business case for implementing<br />
mobile technology in community<br />
services was approved by the Trust<br />
Board in December <strong>2007</strong>, following a<br />
successful pilot in September.<br />
The Mobile Technology Project is set to<br />
change the way clinicians work. Clinicians<br />
who spend 50 per cent or more of their<br />
working week away from their team base<br />
or Trust site working with clients will use<br />
portable tablet PCs (a laptop-like device),<br />
providing secure wireless access to<br />
electronic patient records (RiO), email <strong>and</strong><br />
access to information ‘on-the-go’.<br />
The benefits expected from the Project are:<br />
• reduced travel costs<br />
• more informed clinical decisionmaking<br />
30 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
• increased clinical productivity<br />
• a reduction in clinical risk<br />
• saving of office space<br />
• improvements in work-life balance<br />
• enhancement of the Trust’s image<br />
<strong>and</strong> reputation<br />
• improvements in service user<br />
confidence.<br />
The deployment of devices <strong>and</strong> staff<br />
training will begin in May <strong>2008</strong> with the<br />
project scheduled to be completed by<br />
January 2010. Over this period, 1000<br />
tablet PCs will be issued.<br />
Research <strong>and</strong><br />
development<br />
The Department of Health (DH)’s<br />
strategy document Best Research for<br />
Best Health was published in 2005.<br />
Since its publication the Trust has worked<br />
conscientiously towards streamlining key<br />
administrative processes in its research<br />
<strong>and</strong> development work, in line with<br />
emerging DH policy <strong>and</strong> guidance, <strong>and</strong><br />
strengthening existing partnerships with<br />
Royal Holloway, University of <strong>London</strong><br />
<strong>and</strong> Kingston University. It has also<br />
successfully gained a foothold in the<br />
national research arena via local hub<br />
membership of both the DH-funded<br />
research networks in Mental Health<br />
(MHRN) <strong>and</strong> Comprehensive Local<br />
Research (CLRN). This will validate the<br />
quality <strong>and</strong> impact of the Trust’s current<br />
research activity <strong>and</strong> facilitate future<br />
collaborative work, ensuring that they<br />
reflect the true multidisciplinary nature of<br />
service delivery within clinical settings.<br />
The Trust’s commitment to fundamental<br />
policy drivers such as research governance,<br />
quality assurance, cost- <strong>and</strong> clinical<br />
effectiveness has led to the development<br />
of innovations in diagnostic techniques,<br />
novel treatments <strong>and</strong> service models, with<br />
material benefits to service users <strong>and</strong> carers.<br />
In our research <strong>and</strong> development work we<br />
will continue to enable the development<br />
of good local <strong>and</strong> national service delivery<br />
models <strong>and</strong> organisation, along with the<br />
promotion of clinical effectiveness.<br />
Left:<br />
Changing the way clinicians work<br />
Jawad Chaudhry from our Information<br />
Management <strong>and</strong> Technology department<br />
demonstrates a portable tablet PC<br />
Above:<br />
Providing information,<br />
advice <strong>and</strong> support<br />
Louise Dymoke, PALS Manager<br />
Our PALS<br />
The Trust’s Patient Advice <strong>and</strong> Liaison Service (PALS) seeks to resolve<br />
concerns before they escalate into major problems by providing<br />
information, advice <strong>and</strong> support for service users, their families <strong>and</strong><br />
carers. Here are just three examples. (We have changed details to<br />
preserve anonymity <strong>and</strong> confidentiality.)<br />
• A mother of a 28-year-old inpatient was angry that the cognitive<br />
behavioural therapy in her daughter’s care plan did not seem to have<br />
been carried out. The daughter, however, did not want her to be<br />
involved. PALS played an important role in containing the mother’s<br />
anxieties through listening, supporting <strong>and</strong> advising her <strong>and</strong> liaising<br />
with the staff involved. Eventually the mother gained different<br />
insights <strong>and</strong> her confidence in the service was restored.<br />
• A community patient who was dependent on alcohol was unable to<br />
stop drinking <strong>and</strong> felt very ill <strong>and</strong> frightened. After listening to her<br />
concerns PALS offered to tell the community mental health team<br />
about her distress <strong>and</strong> ask the duty worker or community practice<br />
nurse to contact her.<br />
• A community patient had attended an assessment consultation after<br />
being referred to our services by his GP. However he did not feel<br />
comfortable with the consultant for reasons to do with his illness.<br />
He didn’t want to offend the consultant by telling her his thoughts<br />
but wondered whether he could have a second assessment with a<br />
different consultant. As he had also moved house since the initial<br />
assessment, the resolution of this enquiry involved a considerable<br />
amount of liaison between PALS, the GP <strong>and</strong> the consultant.<br />
Eventually he was referred to another trust by his GP.<br />
Between April <strong>2007</strong> <strong>and</strong> March <strong>2008</strong>, PALS dealt with 504 enquiries.<br />
You can contact PALS on 020 8682 5915 or at pals@swlstg-tr.nhs.uk<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 31
Overview<br />
Complaints<br />
The Trust welcomes all comments from<br />
patients <strong>and</strong> sees complaints as an<br />
important source of information about<br />
how we can do things better.<br />
Many improvements have been made as<br />
a result of complaints, including:<br />
• the introduction of customer<br />
service training to tackle concerns<br />
over the attitude of some staff<br />
• the appointment of a patient<br />
information officer as a result of<br />
concerns over a lack of information<br />
given to patient/carers upon first<br />
admission to mental health services.<br />
In <strong>2007</strong>/08 we received 167 complaints<br />
<strong>and</strong> answered 58 per cent within the<br />
national target of 25 working days.<br />
We continue to filter complaints that<br />
can be responded to sooner than the 25<br />
working day guideline by sending them<br />
to the relevant service for direct action.<br />
Our complaints procedures meet the<br />
spirit of the Parliamentary <strong>and</strong> Health<br />
Service Ombudsman’s Principles of<br />
Remedy but do not formally incorporate<br />
these principles. We shall review the<br />
procedures in the coming year to<br />
achieve this.<br />
Risk training<br />
In response to a number of learning<br />
points from Serious Untoward<br />
Incidents the Trust reviewed its<br />
clinical risk assessment training for<br />
all multidisciplinary staff in <strong>2007</strong>.<br />
We developed a new training <strong>and</strong><br />
education programme, designed for<br />
all the Trust’s healthcare professionals,<br />
which was launched in April <strong>2008</strong>.<br />
The training package involves the<br />
use of specially commissioned films,<br />
produced by the Trust, demonstrating<br />
mental health skills in a variety of risk<br />
assessments <strong>and</strong> clinical management<br />
scenarios.<br />
It has been designed <strong>and</strong> is facilitated<br />
by a multi-professional team of senior<br />
clinicians from within the Trust <strong>and</strong><br />
operates at a variety of levels:<br />
• Level One: a half-day’s training<br />
on patient safety <strong>and</strong> clinical risk<br />
introduces the principles of risk<br />
assessment <strong>and</strong> the responsibilities<br />
related to individual roles within<br />
the team<br />
• Level Two: a one-day, evidencebased<br />
training <strong>and</strong> education<br />
programme, tailored to the needs<br />
of specific clinical teams<br />
• Level Three: a five-day academic<br />
module, in association with the<br />
Faculty of Health Care Sciences<br />
at Kingston University, providing<br />
greater depth <strong>and</strong> applied<br />
theory to risk assessment <strong>and</strong> risk<br />
management <strong>and</strong> using the same<br />
techniques <strong>and</strong> resources to focus<br />
on the development of practical<br />
skills in this vital area.<br />
The course evaluation feedback so far<br />
from participants has been very positive.<br />
Risk management<br />
Risk is the threat that an event<br />
or action will adversely affect<br />
the Trust’s ability to achieve its<br />
objectives <strong>and</strong> to successfully<br />
execute its strategies.<br />
Risk management is the process of<br />
systematically identifying risks, analysing<br />
the likelihood <strong>and</strong> impact of their<br />
occurrence, <strong>and</strong> then deciding what<br />
action to take to prevent, minimise,<br />
accept or transfer these risks in a way<br />
that will enable the Trust to minimise<br />
losses <strong>and</strong> maximise opportunities.<br />
All NHS trusts are required to:<br />
• regularly assess the risks to which<br />
they are exposed<br />
• report that they are taking all<br />
reasonable steps to manage risks<br />
of all kinds<br />
• provide an assurance to key<br />
stakeholders that an effective<br />
system of risk management is<br />
in place.<br />
The Trust’s Risk <strong>St</strong>rategy (available on<br />
our website at http://www.swlstg-tr.nhs.<br />
uk/uploads/documents/tb07126_-_risk_<br />
management_strategy_<strong>2007</strong>.doc)<br />
is revised annually <strong>and</strong> sets out how<br />
we aim to:<br />
• minimise risks to the quality <strong>and</strong><br />
delivery of patient care through<br />
creating awareness throughout the<br />
organisation about the importance<br />
of recognising <strong>and</strong> taking positive<br />
action to manage risks of all<br />
kinds <strong>and</strong> providing staff with a<br />
clear framework <strong>and</strong> associated<br />
processes for managing risks<br />
• continue to innovate <strong>and</strong> pioneer<br />
service developments within a<br />
framework of risk management<br />
• protect the services, reputation,<br />
<strong>and</strong> finances of the organisation<br />
through a process of risk<br />
identification, assessment,<br />
prevention, reduction, elimination<br />
<strong>and</strong> transfer.<br />
The management of risks of all kinds is<br />
an essential element in improving clinical<br />
<strong>and</strong> non-clinical services. It directly<br />
benefits the st<strong>and</strong>ard of patient care <strong>and</strong><br />
staff satisfaction, <strong>and</strong> reduces costs.<br />
The importance to the NHS of learning<br />
from previous mistakes <strong>and</strong> actively<br />
seeking to prevent re-occurrence is<br />
described in An organisation with a<br />
memory (Department of Health Expert<br />
Group, 2000). Out of this the National<br />
Patient Safety Agency developed what it<br />
calls Seven <strong>St</strong>eps to Patient Safety. The<br />
Trust has worked towards embedding<br />
these principles into its services.<br />
Developing a safety culture <strong>and</strong><br />
promoting reporting<br />
There is evidence that when open<br />
reporting <strong>and</strong> even-h<strong>and</strong>ed analysis of<br />
what went wrong are encouraged, in<br />
principle <strong>and</strong> by example, this can have<br />
a positive <strong>and</strong> quantifiable impact on the<br />
performance of an organisation.<br />
32 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
The Trust has reviewed its policies<br />
<strong>and</strong> procedures in reflecting <strong>and</strong><br />
encouraging a more open reporting<br />
culture. The Trust has encouraged active<br />
reporting of incidents. In the last two<br />
years the Trust has increased its incident<br />
reporting by 23 per cent <strong>and</strong> as a result<br />
of sharing, learning <strong>and</strong> addressing<br />
these issues there has been a 41 per<br />
cent reduction in more serious incidents.<br />
Involving <strong>and</strong> communicating<br />
with patients <strong>and</strong> general public<br />
when an incident has gone<br />
wrong<br />
Despite our best efforts mistakes are<br />
sometimes made or our service users<br />
have cause to complain. During 2006 to<br />
<strong>2008</strong> we have concentrated on training<br />
staff to be open when things go wrong.<br />
More than 250 staff were trained to<br />
the National Patient Safety Agency gold<br />
st<strong>and</strong>ard.<br />
Our ‘Being Open’ policy supports<br />
staff to:<br />
• acknowledge, apologise <strong>and</strong><br />
explain when things go wrong<br />
• conduct a thorough investigation<br />
into the incident <strong>and</strong> reassure<br />
patients <strong>and</strong>/or their carers that<br />
lessons learned will help prevent<br />
the incident recurring<br />
• provide support to cope with<br />
the physical <strong>and</strong> psychological<br />
consequences of what happened.<br />
Taking this approach is not always easy<br />
but we believe it is fundamental to the<br />
partnership between patients <strong>and</strong> those<br />
who provide their care.<br />
Learning <strong>and</strong> sharing<br />
safety lessons<br />
In order to learn, underst<strong>and</strong> <strong>and</strong><br />
develop patient safety solutions,<br />
all serious untoward incidents are<br />
investigated using a root cause analysis<br />
approach. Root cause analysis is a<br />
technique for undertaking a systematic<br />
investigation that looks beyond the<br />
individuals concerned <strong>and</strong> seeks to<br />
underst<strong>and</strong> the underlying causes <strong>and</strong><br />
environmental context in which the<br />
incident happened. The benefits include<br />
a structured <strong>and</strong> consistent approach<br />
to incident investigation. It shifts the<br />
focus away from individuals <strong>and</strong> on to<br />
the system to help build an open <strong>and</strong><br />
fair culture. It increases awareness of<br />
patient safety issues <strong>and</strong> helps engage<br />
patients in the investigation. Changes<br />
<strong>and</strong> recommendations are effected as a<br />
result of identifying the root cause.<br />
Since 2005 over 190 Trust managers<br />
<strong>and</strong> clinicians received formal training in<br />
using root cause analysis principles.<br />
Personal data-related incidents<br />
There was one personal data-related<br />
incident during the year. A fault was<br />
reported to the Trust’s IT Service<br />
Desk involving a member of staff’s<br />
caseload. In dealing with the fault <strong>and</strong><br />
responding to a request from BT to<br />
supply screenshots of error messages<br />
we omitted to remove some patient<br />
identifiable data from the information<br />
we sent them. The error was identified<br />
two hours later <strong>and</strong> we then sent<br />
amended data to BT with all patient<br />
identifiable information removed.<br />
Emergency planning<br />
Our Emergency Planning committee<br />
meets quarterly, with Board<br />
representation, to address Emergency<br />
<strong>and</strong> Business continuity planning<br />
throughout the Trust. The committee<br />
also reviews its major incident plans<br />
annually. This meets all national<br />
guidance <strong>and</strong> is fully compliant with<br />
the NHS Emergency Planning Guidance<br />
2005 <strong>and</strong> the Department of Health’s<br />
document Mass casualty incidents:<br />
A framework for planning.<br />
We continue to liaise closely with other<br />
trusts, primary care trusts (PCTs) <strong>and</strong><br />
local authorities within south west<br />
<strong>London</strong> through our membership of<br />
Emergency Planning committees. This<br />
multi-agency working is key to effective<br />
planning.<br />
In June <strong>2007</strong> we conducted, without<br />
notice, an internal out-of-hours<br />
communications exercise. We tested<br />
all email, telephone <strong>and</strong> pager<br />
systems including external agency<br />
emergency contact numbers. This<br />
was in response to the Department of<br />
Health’s Emergency planning guidance<br />
requiring all organisations to undertake<br />
a communications exercise once every<br />
six months.<br />
A Sutton borough business continuity<br />
exercise was conducted in September<br />
<strong>2007</strong> at Sutton Hospital’s Chiltern wing.<br />
The exercise, which involved a simulated<br />
fire <strong>and</strong> utilities failure, involved all the<br />
Sutton borough management team,<br />
Sutton Council, Sutton <strong>and</strong> Merton PCT<br />
<strong>and</strong> Epsom <strong>and</strong> <strong>St</strong> Helier’s acute trust. A<br />
number of key learning points came out<br />
which have contributed to local business<br />
continuity plans.<br />
The Trust took part in two external<br />
exercises in November <strong>2007</strong>. These<br />
were: Exercise Gerhard, a comm<strong>and</strong> <strong>and</strong><br />
control exercise involving all other health<br />
organisations in south west <strong>London</strong>,<br />
which enabled us to test our plans <strong>and</strong><br />
communication systems; <strong>and</strong> a <strong>London</strong>wide<br />
desktop exercise, Exercise Phoenix,<br />
which focused on the recovery phase of<br />
a flu p<strong>and</strong>emic.<br />
We held a series of surgeries for oncall<br />
directors. Twelve directors from<br />
the on-call rota were inducted to the<br />
out-of-hours emergency control room<br />
in Yew ward, outlining their roles <strong>and</strong><br />
responsibilities.<br />
The Health Protection Agency runs<br />
Loggist training for team members to<br />
gain experience of recording events as<br />
they unfold in a major incident. More<br />
than 12 managers <strong>and</strong> administrators<br />
attended a series of these courses<br />
during the year.<br />
Five managers attended a series of<br />
business continuity training courses run<br />
by the Cabinet Office.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 33
Resources – financial review<br />
Surplus for the year<br />
The Trust was required by NHS <strong>London</strong> to achieve a £1.7m surplus for the year<br />
ended 31 March <strong>2008</strong>. Despite facing some financial pressures during the year, the<br />
Trust managed to deliver the surplus. The Trust has a good financial record as it has<br />
achieved a surplus each year since being formed.<br />
Financial results – 3 year summary<br />
<strong>2007</strong>/08<br />
£000<br />
2006/07<br />
£000<br />
2005/06<br />
£000<br />
Operating income 177,222* 168,595 153,480<br />
Retained surplus for year 1,738 2,670 1,532<br />
Financial outlook<br />
The Trust has recently submitted a plan to NHS <strong>London</strong> showing modest income<br />
growth <strong>and</strong> surpluses for the next three years <strong>and</strong> for <strong>2008</strong>/09 the budget has been<br />
set on this basis. The Trust faces challenges as it is required to save approximately<br />
3 per cent of its budget every year because clinical income from PCTs is reduced<br />
(after inflation uplifts) in order to achieve the efficiency target set by Department of<br />
Health. The following table shows the next three years’ income <strong>and</strong> surplus targets:<br />
* Includes £4.4m non-recurrent income<br />
Financial results – 3 year financial plan<br />
<strong>2008</strong>/09<br />
£000<br />
2009/10<br />
£000<br />
2010/11<br />
£000<br />
Operating income 170,000 171,000 175,000<br />
Retained surplus for year 1,700 1,710 1,750<br />
Operating income<br />
for <strong>2007</strong>/08<br />
The majority of the Trust’s income comes<br />
from agreements with primary care trusts<br />
to provide healthcare for people living<br />
within their catchment area, including<br />
£130.2m from the Trust’s four local PCTs,<br />
as set out in the chart to the right.<br />
£22.8m<br />
Other income from activities<br />
£8.8m<br />
Education, training <strong>and</strong> research<br />
£4.7m<br />
Other non-patient related income<br />
The level of income reported in the<br />
Accounts has increased by £8.6m after<br />
the loss of some clinical income.<br />
The main changes reflect:<br />
• inflation on 2006/07 agreements; <strong>and</strong><br />
• repayment of surpluses created in<br />
2005/06 <strong>and</strong> 2006/07 of £4.4m.<br />
This has been used to meet the loss<br />
of clinical income <strong>and</strong> also to cover<br />
expenditure on training <strong>and</strong> estates<br />
development costs.<br />
£10.7m<br />
Local authorities<br />
£21.2m<br />
Kingston Primary<br />
Care Trust<br />
£47.4m<br />
W<strong>and</strong>sworth Primary Care Trust<br />
£38.4m<br />
Sutton & Merton Primary Care Trust<br />
£23.2m<br />
Richmond & Twickenham Primary Care Trust<br />
Total £177.2m<br />
34 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Operating expenditure<br />
for <strong>2007</strong>/08<br />
From a total operating expenditure<br />
of £176.0m, 68 per cent of our<br />
expenditure is on staff costs. Our staff<br />
costs were £119.1m (£113.4m in<br />
2006/07), of which £96.9m or 81 per<br />
cent related to staff directly involved<br />
in patient care. The proportion of staff<br />
expenditure relating to staff directly<br />
involved in patient care has remained<br />
between 81 per cent <strong>and</strong> 82 per cent<br />
since 2001/02. The average number<br />
of staff employed during the year was<br />
2,771 (2,676 in 2006/07).<br />
£15.7m<br />
Depreciation, dividends<br />
<strong>and</strong> amortisation<br />
£96.9m<br />
Clinical services staffing<br />
£41.2m was spent on services <strong>and</strong><br />
consumables supporting patient care.<br />
£15.7m was spent on charges for<br />
capital. The chart on the right shows<br />
how the Trust spent its money in<br />
the year.<br />
£41.2m<br />
Non-pay<br />
£22.2m<br />
Non-clinical staffing<br />
Total<br />
£176.0m<br />
Liquidity/External Financing Limit<br />
The Trust is required to remain within the prescribed external financing limit (EFL).<br />
The Trust managed cash balances throughout the year <strong>and</strong> maintained a positive<br />
bank balance. At year end the cash balance was £0.5m.<br />
The Department of Health set the Trust an External Financing Limit of £3.4m.<br />
The Trust underspent against this limit by £4.1m due to the slippage on capital<br />
projects. This underspend was agreed with the Department of Health.<br />
Capital resources (Capital Cost Absorption Rate)<br />
This refers to the rate of return achieved on capital investment. As one of its<br />
performance measures the Trust must demonstrate it has achieved an investment<br />
yield (i.e. income generated from its capital investments) of between 3 <strong>and</strong> 4 per<br />
cent. This measure is calculated by comparing the Trust Debt Remuneration paid with<br />
Average Net Relevant Assets. The Trust achieved a rate of 3.58 per cent for the year.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 35
Resources – Financial review<br />
Capital expenditure<br />
The Trust is allocated specific funding<br />
for capital expenditure, <strong>and</strong> is required<br />
to remain within this prescribed Capital<br />
Resource Limit (CRL).<br />
The Trust was set a CRL of £16.9m for<br />
<strong>2007</strong>/08. The Trust incurred capital<br />
expenditure of £12.5m, an allowed<br />
underspend of £4.4m. This was mainly<br />
due to the slippage on the psychiatric<br />
intensive care unit <strong>and</strong> the new<br />
W<strong>and</strong>sworth Acute Unit projects.<br />
The capital plan for the coming year<br />
is £17.5m, £13.3m of which is for the<br />
W<strong>and</strong>sworth Acute Unit due to be<br />
completed in March 2009. The major<br />
capital projects are shown in the table<br />
on the right.<br />
2006/07<br />
£m<br />
<strong>2007</strong>/08<br />
£m<br />
<strong>2008</strong>/09<br />
£m<br />
New W<strong>and</strong>sworth Acute Unit 2.5 6.7 13.3<br />
Shaftesbury Unit security 0.8<br />
Information Technology equipment 0.8 1.0 0.5<br />
Jasper Ward (refurbishment) 0.8 0.3<br />
Crocus Ward (refurbishment) 0.7 0.3<br />
Other schemes 4.9 3.4 5.0<br />
Gross capital expenditure 9.7 12.5 18.8<br />
Less: book value of disposals -1.1 -1.3<br />
Net capital expenditure 8.6 12.5 17.5<br />
Public Sector Payment Policy – measure of compliance<br />
In addition to the four key financial duties, the NHS Executive requires that Trusts pay their<br />
non-NHS trade creditors in accordance with the CBI prompt payment code <strong>and</strong> Government<br />
Accounting rules. The target is to pay 95 per cent of non-NHS trade creditors within 30 days<br />
of receipt of goods or a valid invoice (whichever is the later) unless other payment terms have<br />
been agreed with the supplier. The Trust successfully achieved this target for <strong>2007</strong>/08.<br />
number<br />
<strong>2007</strong>/08<br />
£m<br />
2006/07<br />
£m<br />
Total bills paid 54,282 48.9 37.1<br />
Total bills paid within target 51,702 46.9 34.5<br />
Percentage of bills paid within target 95.2% 95.8% 93.9%<br />
Management costs<br />
Management costs 9.4 8.3<br />
Relevant income 177.2 168.8<br />
Percentage of relevant income 5.28% 4.90%<br />
Salary <strong>and</strong> pension entitlements of senior managers<br />
Full details of senior managers’ remuneration are provided in the Remuneration report<br />
on pages 41 to 42.<br />
Audit arrangements<br />
The Trust’s external auditors for <strong>2007</strong>/08 were the Audit Commission, who first<br />
undertook the audit of the final accounts in 2002/03.<br />
The audit fee for the statutory audit <strong>and</strong> services carried out in relation to the statutory<br />
audit for <strong>2007</strong>/08 was £168,000.<br />
As part of the final accounts exercise, each director of the Trust has made a declaration<br />
that, as far as s/he is aware, there is no relevant audit information of which the NHS body’s<br />
auditors are unaware, <strong>and</strong> s/he has taken all the steps that s/he ought to have taken as a<br />
director in order to make him/herself aware of any relevant audit information.<br />
36 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
The accounts<br />
Summary financial statements<br />
The following statements represent a summary of financial information about the<br />
Trust. The full accounts are available on request from:<br />
Director of Finance <strong>and</strong> IT<br />
<strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong>. George’s Mental Health NHS Trust<br />
Springfield University Hospital<br />
61 Glenburnie Road<br />
<strong>London</strong> SW17 7DJ<br />
Telephone 020 8682 6000<br />
Signed on behalf of the Board<br />
Peter Houghton<br />
Chief Executive<br />
Peter Cardell<br />
Director of Finance<br />
A summary of the Trust accounts is shown on pages 37 to 39.<br />
Income <strong>and</strong> expenditure account<br />
For the year ended 31 March<br />
Figures in £000s<br />
<strong>2007</strong>/08 <strong>2008</strong>/09<br />
Income from activities: Continuing operations 163,699 155,449<br />
Other operating income 13,523 13,146<br />
Operating expenses: Continuing operations (166,308) (157,989)<br />
Operating surplus: Continuing operations 10,914 10,606<br />
Profit (loss) on disposal of fixed assets 0 132<br />
Surplus (deficit) before interest 10,914 10,738<br />
Interest receivable 491 464<br />
Interest payable 0 0<br />
Surplus (deficit) for the financial year 11,405 11,202<br />
Public Dividend Capital dividends payable (9,667) (8,532)<br />
Retained surplus (deficit) for the year* 1,738 2,670<br />
Financial target performance 3.6% 3.4%<br />
* No financial support is included in the retained surplus for the year.<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 37
The accounts<br />
Balance sheet<br />
As at 31 March<br />
Figures in £000s<br />
<strong>2007</strong>/08 2006/07<br />
Fixed assets<br />
Intangible assets 13 112<br />
Tangible assets 288,761 263,954<br />
288,774 264,066<br />
Current assets<br />
<strong>St</strong>ocks <strong>and</strong> work in progress 135 176<br />
Debtors: amounts falling due:<br />
after one year 0 0<br />
within one year 8,732 11,787<br />
Investments 0 0<br />
Cash at bank <strong>and</strong> in h<strong>and</strong> 498 484<br />
9,365 12,447<br />
Creditors: amounts falling due within one year (14,106) (11,704)<br />
Net current assets (liabilities) (4,741) 743<br />
Total assets less current liabilities 284,033 264,809<br />
Creditors: amounts falling due after more than one year<br />
Provisions for liabilities <strong>and</strong> charges (89) (116)<br />
Total assets employed 283,944 264,693<br />
Financed by: capital <strong>and</strong> reserves<br />
Public Dividend Capital 111,276 111,987<br />
Revaluation reserve 162,060 144,033<br />
Donated asset reserve 3,278 3,081<br />
Other reserves 750 750<br />
Income <strong>and</strong> expenditure reserve 6,580 4,842<br />
Total capital <strong>and</strong> reserves 283,944 264,693<br />
<strong>St</strong>atement of total recognised gains <strong>and</strong> losses<br />
For the year ended 31 March<br />
Figures in £000s<br />
<strong>2007</strong>/08 2006/07<br />
Surplus for the financial year before dividend payments 11,405 11,202<br />
Fixed asset impairment losses 0 0<br />
Unrealised surplus on fixed asset revaluations/indexation 18,280 16,874<br />
Increases in the donated asset & government grant reserve due to receipt of<br />
donated & government grant financed assets<br />
14 0<br />
Additions/(reductions) in ‘other reserves’ 0 0<br />
Total recognised gains <strong>and</strong> losses for the financial year 29,699 28,076<br />
Prior period adjustment 0 0<br />
Total gains <strong>and</strong> losses recognised in the financial year 29,699 28,076<br />
38 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Cash flow statement<br />
For the year ended 31 March<br />
Figures in £000s<br />
<strong>2007</strong>/08 2006/07<br />
Operating activities<br />
Net cash inflow from operating activities 21,023 11,900<br />
Returns on investments <strong>and</strong> servicing of finance<br />
Interest received 491<br />
Interest paid 0 0<br />
Interest element of finance leases 0 0<br />
Net cash inflow/(outflow) from returns on investments<br />
<strong>and</strong> servicing of finance 491 464<br />
Capital expenditure<br />
Payments to acquire tangible fixed assets (11,122) (8,708)<br />
Receipts from sale of tangible fixed assets 0 1,197<br />
(Payments to acquire)/ receipts from sale of intangible assets 0 (98)<br />
Net cash inflow (outflow) from capital expenditure (11,122) (7,609)<br />
Dividends paid (9,667) (8,532)<br />
Net cash inflow/(outflow) before management<br />
of liquid resources <strong>and</strong> financing 725 (3,777)<br />
Management of liquid resources<br />
Purchase of investments 0 0<br />
Sale of investments 0 0<br />
Net cash inflow/(outflow) from management<br />
of liquid resources<br />
0 0<br />
Net cash inflow/(outflow) before financing 725 (3,777)<br />
Financing<br />
Public dividend capital received 3,459 3,803<br />
Public dividend capital repaid (not previously accrued) (4,170) 0<br />
Public dividend capital repaid (accrued in prior period) 0 0<br />
Loans received 0 0<br />
Loans repaid 0 0<br />
Other capital receipts 0 0<br />
Cash transferred from/to other NHS bodies 0 0<br />
Capital element of finance lease rental payments 0 0<br />
Net cash inflow/(outflow) from financing (711) 3,803<br />
Increase/(decrease) in cash 14 26<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 39
The accounts<br />
Independent auditor’s report to the Directors<br />
of the Board of <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong><br />
<strong>St</strong> George’s Mental Health NHS Trust<br />
on the Summary Financial <strong>St</strong>atements<br />
I have examined the summary financial statements set out on pages 37 to 39.<br />
This report is made solely to the Board of <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s<br />
Mental Health NHS Trust in accordance with Part II of the Audit Commission Act<br />
1998 <strong>and</strong> for no other purpose, as set out in paragraph 36 of the <strong>St</strong>atement<br />
of Responsibilities of Auditors <strong>and</strong> of Audited Bodies, prepared by the Audit<br />
Commission.<br />
Respective responsibilities of directors <strong>and</strong> auditors<br />
The directors are responsible for preparing the <strong>Annual</strong> <strong>Report</strong>. My responsibility is to<br />
report to you my opinion on the consistency of the summary financial statements<br />
with the statutory financial statements. I also read the other information contained<br />
in the <strong>Annual</strong> <strong>Report</strong> <strong>and</strong> consider the implications for my report if I become<br />
aware of any misstatements or material inconsistencies with the summary financial<br />
statements.<br />
Basis of opinion<br />
I conducted my work in accordance with Bulletin 1999/6 ‘The auditor’s statement on<br />
the summary financial statements’ issued by the Auditing Practices Board. My report<br />
on the statutory financial statements describes the basis of our audit opinion on<br />
these financial statements.<br />
Opinion<br />
In my opinion the summary financial statements are consistent with the statutory<br />
financial statements of the Trust for the year ended 31 March <strong>2008</strong> on which I have<br />
issued an unqualified opinion.<br />
Jon Hayes<br />
Audit Commission<br />
1st Floor Millbank Tower<br />
Millbank<br />
<strong>London</strong> SW1P 4QH<br />
20 June <strong>2008</strong><br />
40 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
Remuneration report<br />
Remuneration <strong>and</strong> Terms of Service Committee<br />
The Committee is chaired by the Trust’s Chairman, <strong>and</strong> the membership comprises<br />
all the non-executive directors. The committee is considered quorate if it has a<br />
minimum of three non-executive directors present.<br />
The Chief Executive attends all meetings of the Committee but is not present for<br />
discussions about his/her own remuneration. The Director of Human Resources acts<br />
as Secretary to the Committee but is not present for discussions about his/her own<br />
remuneration.<br />
The Committee:<br />
• determines the remuneration <strong>and</strong><br />
terms of service of the Chief Executive<br />
<strong>and</strong> those directors that report directly<br />
to the Chief Executive (all other senior<br />
managers are covered by Agenda for<br />
Change)<br />
• reviews the performance of those<br />
directors who report directly to the<br />
Chief Executive, through reports<br />
submitted by the Chief Executive,<br />
Salaries <strong>and</strong> allowances<br />
no later than May each year. The<br />
Chair will similarly report on the<br />
performance of the Chief Executive<br />
• periodically reviews pay data from<br />
similar organisations in order to ensure<br />
that appropriate arrangements have<br />
been made for the salaries of these<br />
directors<br />
• oversees appropriate contractual<br />
arrangements for such staff, including<br />
the proper calculation <strong>and</strong> scrutiny<br />
of termination payments, for these<br />
<strong>and</strong> other senior staff, taking account<br />
of such national guidance as is<br />
appropriate<br />
• meets annually as a minimum, but<br />
may meet on other occasions as may<br />
be required from time to time.<br />
<strong>2007</strong>/08 2006/07<br />
Name<br />
Title<br />
Salary<br />
(b<strong>and</strong>s of<br />
£5,000)<br />
Other<br />
renumeration<br />
(b<strong>and</strong>s of £5,000)<br />
Salary<br />
(b<strong>and</strong>s of<br />
£5,000)<br />
Other<br />
renumeration<br />
(b<strong>and</strong>s of £5,000)<br />
Mr John Rafferty Chairman 20-25 0 20-25 0<br />
Mr Raficq Abdulla Non-Executive Director (to 31/12/07) 5-10 0 5-10 0<br />
Ms Judith Chegwidden Non-Executive Director 5-10 0 5-10 0<br />
Mr Arthur de Frisching Non-Executive Director (to 31/03/08) 5-10 0 5-10 0<br />
Mr Emir Feisal Non-Executive Director (to 31/12/07) 5-10 0 5-10 0<br />
Prof Roger Horton Non-Executive Director 5-10 0 5-10 0<br />
Ms Elizabeth Owen Non-Executive Director 5-10 0 5-10 0<br />
Dr Diana Rose Associate Non-Executive Director (to 31/10/07) 5-10 0 0-5 0<br />
Dr B E Nereli Medical Director (from 1/11/07) 45-50 15-20 0 0<br />
Dr Debbie <strong>St</strong>inson Joint Interim Medical Director (1/05/07 - 1/11/07) 10-15 0 0 0<br />
Dr James Bolton Joint Interim Medical Director (1/05/07 - 1/11/07) 10-15 0 0 0<br />
Dr Deji Oyebode Medical Director (to 30/04/07) 10-15 0 85-90 115-120<br />
Mr Peter Houghton Chief Executive 150-155 0 105-110 * 0<br />
Mr Peter Cardell Director of Finance <strong>and</strong> IT 105-110 0 95-100 0<br />
Ms Maresa Ness Chief Operating Officer 95-100 0 90-95 0<br />
Ms S<strong>and</strong>y Gillett Director of Human Resources 85-90 0 75-80 0<br />
Ms Kim Goddard Director of Corporate Affairs (to 30/06/07) 5-10 0 35-40 0<br />
Ms Kim Goddard Director of Nursing (from 1/07/07) 60-65 0 0 0<br />
Mr Andrew Simpson Director of Planning (to 30/06/07) 15-20 0 0 0<br />
*part-year salary<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 41
Performance arrangements<br />
The performance of executive directors is assessed by the Chief Executive on an<br />
annual basis. The performance of non-executive directors <strong>and</strong> the Chief Executive is<br />
appraised by the Chair.<br />
Most senior managers have a basic salary which is based on national Agenda for<br />
Change pay <strong>and</strong> remuneration guidelines. Executive directors remain on local Trust<br />
conditions of service, <strong>and</strong> their salaries are reviewed annually by the Remuneration<br />
Committee. Executive directors received cost of living increases in line with the Very<br />
Senior Managers’ Pay Framework, <strong>and</strong> the Remuneration Committee awarded<br />
differential pay increases, based on achievements against objectives (as assessed by<br />
the Chief Executive) <strong>and</strong> market rates.<br />
Senior managers’ contracts which fall within this remit are all substantive <strong>and</strong><br />
permanent. Notice periods are in line with employment law.<br />
Payments to past senior managers<br />
No compensation payments were made to senior managers in the financial year<br />
under review.<br />
Pension benefits<br />
Real<br />
increase<br />
in pension<br />
at age 60<br />
(b<strong>and</strong>s of<br />
£2,500)<br />
Lump sum<br />
at age 60<br />
related to<br />
increase<br />
in pension<br />
(b<strong>and</strong>s of<br />
£2,500)<br />
Total<br />
accrued<br />
pension at<br />
age 60 at<br />
31 March<br />
<strong>2008</strong><br />
(b<strong>and</strong>s of<br />
£5,000)<br />
Lump sum<br />
at age 60<br />
related to<br />
accrued<br />
pension at<br />
31 March<br />
<strong>2008</strong><br />
(b<strong>and</strong>s of<br />
£5,000)<br />
Cash<br />
equivalent<br />
transfer<br />
value at<br />
31 March<br />
<strong>2008</strong><br />
Cash<br />
equivalent<br />
transfer<br />
value at<br />
31 March<br />
<strong>2007</strong><br />
Real<br />
increase<br />
in cash<br />
equivalent<br />
transfer<br />
value<br />
Employer’s<br />
contribution<br />
to<br />
stakeholder<br />
pension<br />
Name<br />
£’000<br />
£’000<br />
£’000<br />
£’000<br />
£’000<br />
£’000<br />
£’000<br />
£’000<br />
Mr Peter Houghton 0-2.5 5.0-7.5 45-50 145-150 712 650 31 0<br />
Mr Peter Cardell 2.5-5.0 7.5-10.0 10-15 40-45 N/A N/A N/A 0<br />
Ms Maresa Ness 2.5-5.0 10.0-12.5 35-40 105-110 613 529 49 0<br />
Dr Deji Oyebode 0-2.5 0-2.5 30-35 100-105 569 503 3 0<br />
Ms S<strong>and</strong>y Gillett 2.5-5.0 7.5-10.0 25-30 75-80 483 415 40 0<br />
Ms Kim Goddard 5.0-7.5 17.5-20.0 25-30 75-80 371 261 72 0<br />
Mr Andrew Simpson 0-2.5 0-2.5 10-15 35-40 158 134 4 0<br />
Dr B E Nereli 0-2.5 2.5-5.0 20-25 65-70 311 251 22 0<br />
Dr Debbie <strong>St</strong>inson 0-2.5 0-2.5 30-35 95-100 505 459 12 0<br />
Dr James Bolton 2.5-5.0 10.0-12.5 25-30 75-80 420 225 66 0<br />
42 <strong>South</strong> <strong>West</strong> <strong>London</strong> <strong>and</strong> <strong>St</strong> George’s Mental Health NHS Trust
The Board<br />
Non-executive directors<br />
Executive directors<br />
John Rafferty<br />
Chairman<br />
Appointed December 2004<br />
Peter Houghton<br />
Chief Executive<br />
Appointed July 2006<br />
Judith Chegwidden Vice Chairman<br />
Appointed June 1998; reappointed January 2006<br />
Chair of Audit Committee<br />
• Director of Roskill Information Services Ltd<br />
<strong>and</strong> of Roskill Consulting Group Ltd<br />
Susan Dark Non-Executive Director<br />
Appointed April <strong>2008</strong><br />
• Managing Director of Nikko Healthcare<br />
Emir Feisal JP Non-Executive Director<br />
Appointed January 2006, left December <strong>2007</strong><br />
Member of Audit Committee<br />
• Associate Managing Editor, The Sunday Times<br />
• Member, Ministerial Advisory Board, The Royal<br />
Parks Agency<br />
• Magistrate, <strong>West</strong>minster Bench<br />
• Trustee, Vitalise<br />
Arthur de Frisching Non-Executive Director<br />
Appointed June 2002; reappointed June 2006,<br />
left March <strong>2008</strong><br />
Member of Audit Committee<br />
Professor Roger Horton<br />
Non-Executive Director<br />
Appointed December 2003<br />
Member of Audit Committee<br />
• Vice-Principal of <strong>St</strong> George’s, University of<br />
<strong>London</strong> until 30 September <strong>2007</strong><br />
Iain McCusker<br />
Non-Executive Director<br />
Appointed April <strong>2008</strong><br />
Maresa Ness<br />
Chief Operating Officer<br />
<strong>and</strong> Deputy Chief Executive<br />
Appointed November 2004<br />
• Trustee, Mosaic Clubhouse (charity)<br />
Peter Cardell<br />
Director of Finance <strong>and</strong> IT<br />
Appointed May 1998<br />
• External member of the University Audit<br />
Committee, Kingston University<br />
• Director, Mosaic Clubhouse (charity)<br />
Professor Mary Chambers<br />
Chief Nurse <strong>and</strong> Professor<br />
of Mental Health Nursing<br />
Appointed February 2004, left April <strong>2007</strong><br />
Kim Goddard<br />
Director of Nursing <strong>and</strong> Governance<br />
Appointed 6 June <strong>2007</strong><br />
Appointed Interim Director of Nursing <strong>and</strong><br />
Governance on 1 April <strong>2007</strong><br />
Dr Ben Nereli<br />
Medical Director<br />
Appointed 1 November <strong>2007</strong><br />
Dr Deji Oyebode<br />
Medical Director<br />
Appointed July 2002, left 1 May <strong>2007</strong><br />
Elizabeth Owen<br />
Non-Executive Director<br />
Appointed May 2006<br />
Member of Estates Committee<br />
• Legal Adviser – construction industry<br />
Dr James Bolton<br />
Joint Interim Medical Director<br />
Appointed 1 May <strong>2007</strong>, left 31 October <strong>2007</strong><br />
Raficq Abdulla<br />
Associate Non-Executive Director<br />
(non-voting)<br />
Appointed September 2006, left December <strong>2007</strong><br />
• Trustee, World without TB<br />
• Trustee, Poetry Society, Planet Poetry, English PEN<br />
Dr Diana Rose<br />
Associate Non-Executive Director<br />
(non-voting)<br />
Appointed October 2006, left December <strong>2007</strong><br />
Dr Debbie <strong>St</strong>inson<br />
Joint Interim Medical Director<br />
Appointed 1 May <strong>2007</strong>, left 31 October <strong>2007</strong><br />
S<strong>and</strong>y Gillett<br />
Director of Human Resources<br />
(non-voting)<br />
Appointed August 2005<br />
• Trustee, Radio Lollipop<br />
<strong>Annual</strong> <strong>Report</strong> <strong>and</strong> Accounts 07 / 08 43
Main Trust locations<br />
M4<br />
M3<br />
TEDDINGTON<br />
HAMPTON<br />
TWICKENHAM<br />
31<br />
BUSHY PARK<br />
HAMPTON COURT<br />
PARK<br />
KEW<br />
GARDENS<br />
2<br />
3<br />
1 4 5<br />
7<br />
6 WANDSWORTH<br />
30<br />
26<br />
KEW<br />
RICHMOND<br />
RICHMOND<br />
29<br />
25<br />
RICHMOND<br />
PARK<br />
KINGSTON<br />
UPON-THAMES<br />
SURBITON<br />
24<br />
HOOK<br />
CHESSINGTON<br />
28<br />
27<br />
NEW MALDEN<br />
KINGSTON<br />
WORCESTER<br />
PARK<br />
BARNES<br />
BARNES<br />
COMMON<br />
ROEHAMPTON<br />
WIMBLEDON<br />
COMMON<br />
PUTNEY<br />
WIMBLEDON<br />
SOUTHFIELDS<br />
23<br />
MORDEN<br />
PARK<br />
WIMBLEDON<br />
PARK<br />
MERTON<br />
RAYNES<br />
PARK<br />
MORDEN<br />
CHEAM<br />
22<br />
21<br />
9<br />
10 8<br />
EARLSFIELD<br />
COLLIERS<br />
WOOD<br />
16<br />
MERTON<br />
18<br />
19<br />
SUTTON<br />
BATTERSEA<br />
PARK<br />
CLAPHAM<br />
COMMON<br />
WANDSWORTH<br />
COMMON<br />
12 13 14<br />
15<br />
SUTTON<br />
BATTERSEA<br />
CLAPHAM<br />
JUNCTION<br />
BALHAM<br />
TOOTING<br />
17<br />
CARSHALTON<br />
TOOTING BEC<br />
COMMON<br />
MITCHAM<br />
MITCHAM<br />
COMMON<br />
BEDDINGTON<br />
PARK<br />
20<br />
11<br />
WALLINGTON<br />
Acre Road<br />
Barnes Hospital<br />
Cheam Resource Centre<br />
Guildhall<br />
Haydon House<br />
Henderson Hospital<br />
Henderson Outreach<br />
Maddison Clinic<br />
Mapleton Centre<br />
Nelson Hospital<br />
Norfolk Lodge<br />
Old Church<br />
Queen Mary’s Hospital<br />
Richmond Royal Hospital<br />
Rose Lodge<br />
Rosel<strong>and</strong>s<br />
<strong>South</strong> Bank House<br />
<strong>South</strong> Place Day Centre<br />
Springfield University Hospital<br />
<strong>St</strong> George’s Hospital<br />
<strong>St</strong> Helier Hospital<br />
<strong>St</strong> John’s Hospital <strong>and</strong> Amy<strong>and</strong> House<br />
<strong>St</strong> John’s Therapy Centre<br />
Sutton Hospital<br />
Thrale Road<br />
Tolworth Hospital<br />
Wallington Resource Centre<br />
<strong>West</strong>moor House<br />
William Harvey Clinic<br />
Wilson Hospital<br />
York Road<br />
29<br />
3<br />
23<br />
30<br />
8<br />
22<br />
11<br />
31<br />
7<br />
18<br />
15<br />
14<br />
4<br />
2<br />
28<br />
27<br />
26<br />
25<br />
12<br />
16<br />
19<br />
1<br />
10<br />
21<br />
13<br />
24<br />
20<br />
6<br />
5<br />
17<br />
9<br />
Useful contact details<br />
Barnes Hospital 020 8878 4981<br />
Henderson Hospital, Sutton 020 7622 9337<br />
Nelson Hospital, Raynes Park 020 8296 3795<br />
Queen Mary’s Hospital, Roehampton 020 8487 6000<br />
Richmond Royal Hospital 020 8940 3331<br />
Springfield University Hospital, Tooting 020 8682 6000 (Trust headquarters)<br />
Sutton Hospital 020 8296 2000<br />
Tolworth Hospital 020 8390 0102<br />
www.swlstg-tr.nhs.uk<br />
Extra copies of this annual report are available<br />
from the Communications Department on 020 8772 5532.<br />
This report is available in other formats <strong>and</strong> languages by request.<br />
Please contact the Communications Department on 020 8772 5532.<br />
Let us know what you think of this annual report.<br />
Email us at communications@swlstg-tr.nhs.uk<br />
Produced by Raffertys