Anaesthesia, Intensive Care and Pain Medicine - St Vincent's ...
Anaesthesia, Intensive Care and Pain Medicine - St Vincent's ...
Anaesthesia, Intensive Care and Pain Medicine - St Vincent's ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Department of <strong>Anaesthesia</strong>, <strong>Intensive</strong> <strong>Care</strong> <strong>and</strong> <strong>Pain</strong> <strong>Medicine</strong><br />
<strong>St</strong>.Vincent’s Healthcare Group<br />
157 staff trained as ACLS Providers.<br />
538 staff trained as Basic Life Support Providers.<br />
An Intern orientation programme presented for the first time<br />
proved very popular.<br />
Other courses include Basic Rhythm Recognition Workshop,<br />
Cardiac Arrest Management Workshop. Numerous lectures <strong>and</strong><br />
in-services were presented on a variety of topics associated<br />
with resuscitation.Ward-based training proved most popular <strong>and</strong><br />
it is hoped to increase the number of sessions provided in 2004.<br />
At the end of 2003 an election was held to select a new<br />
Chairman of SEDDA. Dr.Alan McShane was elected to the<br />
post of Chairman of SEDDA for a term.<br />
I wish to express my thanks to the secretary of SEDDA, Ms<br />
Louise McNicholas <strong>and</strong> to the secretary of the Department of<br />
<strong>Anaesthesia</strong>,<strong>St</strong>.Vincent’s University Hospital,Ms Róisin Crowe,<br />
for all their help throughout my term as Chairman of SEDDA.<br />
Dr. Edward Gallagher<br />
Outgoing Co-ordinator<br />
South East Dublin Department of <strong>Anaesthesia</strong><br />
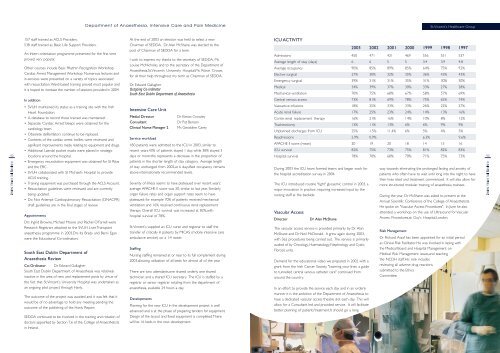
ICU ACTIVITY<br />
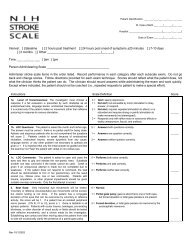
2003 2002 2001 2000 1999 1998 1997<br />
Admissions 450 471 421 469 556 551 537<br />
Average length of stay (days) 6 6 5 5 3.4 3.9 4.8<br />
Average occupancy 90% 85% 89% 85% 64% 75% 92%<br />
Elective surgical 27% 30% 32% 35% 36% 43% 43%<br />
Emergency surgical 39% 31% 31% 35% 31% 30% 30%<br />
Medical 34% 39% 37% 30% 33% 27% 28%<br />
Mechanical ventilation 70% 75% 68% 67% 58% 57% 69%<br />
In addition<br />
Central venous access 73% 81% 69% 78% 75% 65% 74%<br />
92<br />
• SVUH maintained its status as a training site with the Irish<br />
Heart Foundation.<br />
• A database to record those trained was maintained.<br />
• Separate ‘Cardiac Arrest’ bleeps were obtained for the<br />
cardiology team.<br />
• Obsolete defibrillators continue to be replaced.<br />
• Contents of the cardiac arrest trollies were reviewed <strong>and</strong><br />
s i g n i ficant improvements made relating to equipment <strong>and</strong> dru g s .<br />
• Additional Laerdal pocket masks were placed in strategic<br />
locations around the hospital.<br />
• Emergency resuscitation equipment was obtained for <strong>St</strong> Ritas<br />
<strong>and</strong> the ERC.<br />
• SVUH collaborated with <strong>St</strong> Michael’s Hospital to provide<br />
ACLS training.<br />
• Training equipment was purchased through the ACLS A c c o u n t .<br />
• Resuscitation guidelines were reviewed <strong>and</strong> are currently<br />
being updated.<br />
• Do Not Attempt Cardiopulmonary Resuscitation (DNACPR)<br />
draft guidelines are in the final stages of review.<br />
Appointments<br />
Drs Ingrid Browne, Michael Moore <strong>and</strong> Rachel O’Farrell were<br />
Research Registrars attached to the SVUH Liver Transplant<br />
anaesthesia programme in 2003.Drs Ita Brady <strong>and</strong> Berni Egan<br />
were the Educational Co-ordinators.<br />
South East Dublin Department of<br />
<strong>Anaesthesia</strong> Review<br />
Co-Ordinator Dr. Edward Gallagher<br />
South East Dublin Department of <strong>Anaesthesia</strong> was relatively<br />
inactive in the area of new <strong>and</strong> replacement posts by virtue of<br />
the fact that <strong>St</strong>.Vincent’s University Hospital was undertaken as<br />
an ongoing pilot project through Hanly.<br />
The outcome of the project was awaited <strong>and</strong> it was felt that it<br />
would be of no advantage to hold any meeting pending the<br />
outcome of the publishing of the Hanly Report.<br />
SEDDA continued to be involved in the training <strong>and</strong> rotation of<br />
d o c t o rs appointed by Section 7.6 of the College of Anaesthetists<br />
in Irel<strong>and</strong>.<br />
<strong>Intensive</strong> <strong>Care</strong> Unit<br />
Medial Director<br />
Consultant<br />
Clinical Nurse Manager 2<br />
Service workload<br />
Dr Kieran Crowley<br />
Dr Pat Benson<br />
Ms Geraldine <strong>Care</strong>y<br />
450 patients were admitted to the ICU in 2003, similar to<br />
recent years.43% of patients stayed 1 day, while 38% stayed 3<br />
days or more:this represents a decrease in the proportion of<br />
patients in the shorter length of stay category. Average length<br />
of stay unchanged from 2002,at 6 days.Bed occupancy remains<br />
above internationally recommended levels.<br />
Severity of illness seems to have plateaued over recent years:<br />
average APACHE II score was 20, similar to last year. Similarly<br />
organ failure rates <strong>and</strong> organ support rates seem to have<br />
plateaued: for example 70% of patients received mechanical<br />
ventilation <strong>and</strong> 16% received continuous renal replacement<br />
therapy. Overall ICU survival was increased at 82%,with<br />
hospital survival of 78%.<br />
<strong>St</strong>.Vincent’s supplied an ICU nurse <strong>and</strong> registrar to staff the<br />
transfer of critically ill patients by MICAS (mobile intensive care<br />
ambulance service) on a 1:4 roster.<br />
<strong>St</strong>affing<br />
N u rsing staffing remained at or near to its full complement duri n g<br />
2003,allowing utilization of all beds for almost all of the year.<br />
There are two attendants,one shared orderly, one shared<br />
technician <strong>and</strong> a shared ICU secretary. The ICU is staffed by a<br />
registrar or senior registrar rotating from the department of<br />
anaesthesia, available 24 hours a day.<br />
Developments<br />
Planning for the new ICU in the development project is well<br />
advanced <strong>and</strong> is at the phase of preparing tenders for equipment.<br />
Design of the layout <strong>and</strong> fixed equipment is completed.There<br />
will be 16 beds in the new development.<br />
Vasoactive infusions 18% 25% 33% 33% 26% 22% 27%<br />
Acute renal failure 17% 25% 23% 24% 14% 13% 16%<br />
Contin.renal replacement therapy 16% 21% 16% 14% 10% 8% 12%<br />
Tracheostomy 13% 11% 13% 6% 6% 9% 9%<br />
Unplanned discharges from ICU 25% 1.5% 11.4% 6% 5% 4% 5%<br />
Readmissions 2.9% 0.9% 6.3% 9.6%<br />
APACHE II score (mean) 20 19 20 18 14 15 16<br />
ICU survival 82% 75% 73% 75% 81% 82% 83%<br />
Hospital survival 78% 70% 68% 70% 71% 75% 73%<br />
During 2003 the ICU team formed teams <strong>and</strong> began work for<br />
the hospital accreditation survey in 2004.<br />
The ICU introduced routine "tight" glycaemic control in 2003, a<br />
major innovation in practice, requiring increased input by the<br />
nursing staff at the bedside.<br />
Vascular Access<br />
Director<br />
Dr Alan McShane<br />
The vascular access service is provided primarily by Dr Alan<br />
McShane <strong>and</strong> Dr Neil McDonald. It grew again during 2003,<br />
with 362 procedures being carried out. The service is primarily<br />
availed of by Oncology, Haematology, Nephrology <strong>and</strong> Cystic<br />
Fibrosis units.<br />
Dem<strong>and</strong> for the educational video we prepared in 2002 with a<br />
grant from the Irish Cancer Society, "Learning your lines: a guide<br />
to tunnelled central venous catheter care" continued from<br />
around the country.<br />
In an effort to provide the service each day <strong>and</strong> in an orderly<br />
manner it is the ambition of the Department of <strong>Anaesthesia</strong> to<br />
have a dedicated vascular access theatre slot each day. This will<br />
allow for a Consultant led <strong>and</strong> provided service. It will facilitate<br />
better planning of patients’treatment.It should go a long<br />
way towards eliminating the prolonged fasting <strong>and</strong> anxiety of<br />
patients who often have to wait until long into the night to have<br />
their lines sited <strong>and</strong> treatment commenced. It will also allow for<br />
more structured modular training of anaesthesia trainees.<br />
During the year, Dr McShane was asked to present at the<br />
Annual Scientific Conference of the College of Anaesthetists.<br />
He spoke on "Vascular Access Procedures". In June he also<br />
attended a workshop on the use of Ultrasound for Vascular<br />
Access Procedures,at Guy’s Hospital,London.<br />
Risk Management<br />
Dr Richard Assaf has been appointed for an initial period<br />
as Clinical Risk Facilitator. He was invo l ved in liasing with<br />
the Medical Board <strong>and</strong> Hospital Management on<br />
Medical Risk Management issues,<strong>and</strong> teaching<br />
the NCDH staff.His role includes<br />
reviewing all adverse drug reactions<br />
submitted to the Ethics<br />
Committee.<br />
93