CareFirst Blue Choice Option 11 – HMO
CareFirst Blue Choice Option 11 – HMO
CareFirst Blue Choice Option 11 – HMO
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
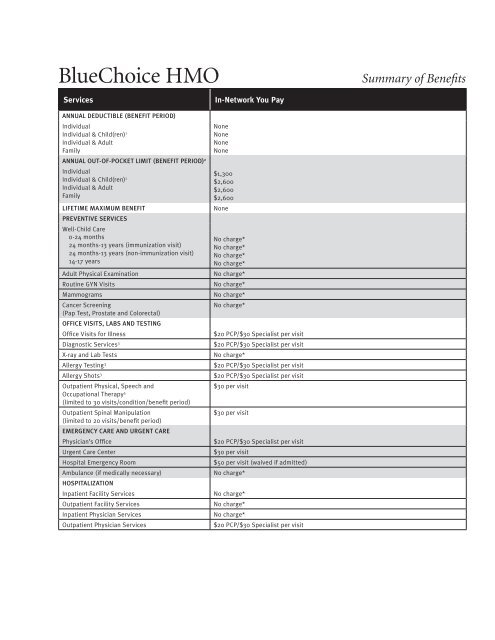
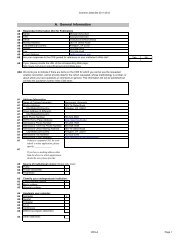
<strong>Blue</strong><strong>Choice</strong> <strong>HMO</strong><br />
Summary of Benefits<br />
Services<br />
ANNUAL DEDUCTIBLE (BENEFIT PERIOD)<br />
Individual<br />
Individual & Child(ren) 1<br />
Individual & Adult<br />
Family<br />
ANNUAL OUT-OF-POCKET LIMIT (BENEFIT PERIOD) 2<br />
Individual<br />
Individual & Child(ren) 1<br />
Individual & Adult<br />
Family<br />
LIFETIME MAXIMUM BENEFIT<br />
PREVENTIVE SERVICES<br />
Well-Child Care<br />
0-24 months<br />
24 months-13 years (immunization visit)<br />
24 months-13 years (non-immunization visit)<br />
14-17 years<br />
Adult Physical Examination<br />
Routine GYN Visits<br />
Mammograms<br />
Cancer Screening<br />
(Pap Test, Prostate and Colorectal)<br />
OFFICE VISITS, LABS AND TESTING<br />
Office Visits for Illness<br />
Diagnostic Services 3<br />
X-ray and Lab Tests<br />
Allergy Testing 3<br />
Allergy Shots 3<br />
Outpatient Physical, Speech and<br />
Occupational Therapy 5<br />
(limited to 30 visits/condition/benefit period)<br />
Outpatient Spinal Manipulation<br />
(limited to 20 visits/benefit period)<br />
EMERGENCY CARE AND URGENT CARE<br />
Physician’s Office<br />
Urgent Care Center<br />
Hospital Emergency Room<br />
Ambulance (if medically necessary)<br />
HOSPITALIZATION<br />
Inpatient Facility Services<br />
Outpatient Facility Services<br />
Inpatient Physician Services<br />
Outpatient Physician Services<br />
In-Network You Pay<br />
None<br />
None<br />
None<br />
None<br />
$1,300<br />
$2,600<br />
$2,600<br />
$2,600<br />
None<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
$20 PCP/$30 Specialist per visit<br />
$20 PCP/$30 Specialist per visit<br />
No charge*<br />
$20 PCP/$30 Specialist per visit<br />
$20 PCP/$30 Specialist per visit<br />
$30 per visit<br />
$30 per visit<br />
$20 PCP/$30 Specialist per visit<br />
$30 per visit<br />
$50 per visit (waived if admitted)<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
$20 PCP/$30 Specialist per visit
Services<br />
HOSPITAL ALTERNATIVES<br />
Home Health Care<br />
Hospice<br />
Skilled Nursing Facility<br />
MATERNITY<br />
Prenatal and Postnatal Office Visits<br />
Delivery and Facility Services<br />
Nursery Care of Newborn<br />
Initial Office Consulation(s) for Infertility<br />
Services/Procedures<br />
Artificial Insemination 4<br />
In Vitro Fertilization Procedures 4<br />
MENTAL HEALTH AND SUBSTANCE ABUSE<br />
Inpatient Facility Services<br />
Inpatient Physician Services<br />
Outpatient Facility Services<br />
Outpatient Physician Services<br />
Office Visits<br />
Partial Hospitalization Facility Services<br />
Partial Hospitalization Physician Services<br />
Medication Management<br />
MISCELLANEOUS<br />
Durable Medical Equipment<br />
Acupuncture<br />
Transplants<br />
Hearing Aids<br />
VISION<br />
Routine Exam (limited to 1 visit/benefit period)<br />
Eyeglasses and Contact Lenses<br />
In-Network You Pay<br />
No charge*<br />
No charge*<br />
No charge*<br />
$20 PCP/$30 Specialist per visit (not to exceed 10 times the copay per pregnancy)<br />
No charge*<br />
No charge*<br />
$20 PCP/$30 Specialist per visit<br />
$30 per visit<br />
Not covered<br />
No charge*<br />
No charge*<br />
No charge*<br />
No charge*<br />
$10 per visit<br />
No charge*<br />
No charge*<br />
$20 per visit<br />
25% of Allowed Benefit<br />
Not covered (except when approved by <strong>CareFirst</strong> when used for anesthesia)<br />
Covered as stated in Evidence of Coverage<br />
Not covered<br />
$10 per visit<br />
Discounts from participating Vision Centers<br />
* No copayments or coinsurance.<br />
1<br />
Please refer to your Evidence of Coverage to determine your coverage level.<br />
2<br />
If you have Individual and Adult, Individual and Child(ren) or Family coverage, each Member can satisfy his/her own Individual Out-of-Pocket Maximum by meeting the<br />
Individual Out-of-Pocket Maximum. In addition, eligible expenses of all covered family members can be combined to satisfy the Out-of-Pocket Maximum for the type of<br />
coverage in which the Subscriber is enrolled. However, an individual family member cannot contribute more than the Individual Out-of-Pocket Maximum toward meeting<br />
the Out-of-Pocket Maximum for the type of coverage in which the Subscriber is enrolled.<br />
3<br />
If office copayment has been paid, additional office copayment not required for this service.<br />
4<br />
Members who are unable to conceive have coverage for the evaluation of infertility services performed to confirm an infertility diagnosis, and some treatment option for<br />
infertility. However, assisted reproduction (AI & IVF) services performed as treatment option for infertility are only available under the terms of the members contract.<br />
Preauthorization required.<br />
5<br />
Visit Limitation does not apply to children ages 2-6 when Physical, Speech and Occupational Therapy is for treatment of Autism Spectrum Disorder.<br />
Note: Upon enrollment in <strong>CareFirst</strong> <strong>Blue</strong><strong>Choice</strong>, you will need to select a Primary Care Provider (PCP). To select a PCP, go to www.carefirst.com for the most current listing<br />
of PCPs from our online provider directory. You may also call the Member Services toll free phone number on the front of your <strong>CareFirst</strong> <strong>Blue</strong><strong>Choice</strong> ID card for assistance<br />
in selecting a PCP or obtaining a printed copy of the <strong>CareFirst</strong> <strong>Blue</strong><strong>Choice</strong> provider directory.<br />
Not all services and procedures are covered by your benefits contract. This plan summary is for comparison purposes only and does not create rights not given through the<br />
benefit plan.<br />
Policy form numbers: VA/CFBC/GC (R. 10/<strong>11</strong>) • VA/CFBC/EOC (R. 1/09) • VA/CFBC/DOL APPEAL (R. 7/<strong>11</strong>) • VA/CFBC/DOCS (R. 1/09) • VA/BC-OOP/SOB (R. 1/09) •<br />
VA/CFBC/ATTC (R. 1/10) • VA/BC-OOP/VISION (R. 6/04) • VA/CFBC/RX3 (R. 7/<strong>11</strong>) and any amendments.<br />
SUM1423-1P (2/12) ■ VA ■ 200+ <strong>Option</strong> <strong>11</strong><br />
www.carefirst.com<br />
<strong>CareFirst</strong> <strong>Blue</strong><strong>Choice</strong>, Inc. is an independent licensee of the <strong>Blue</strong> Cross and <strong>Blue</strong> Shield Association.<br />
® Registered trademark of the <strong>Blue</strong> Cross and <strong>Blue</strong> Shield Association. ®’ Registered trademark of <strong>CareFirst</strong> of Maryland, Inc.
Exclusions and Limitations<br />
10.1 Coverage Is Not Provided For:<br />
A. Any service, supply or item that is not Medically Necessary. Although a service may be listed as covered,<br />
benefits will be provided only if the service is Medically Necessary as determined by the Plan.<br />
B. Services that are Experimental or Investigational as determined by the Plan.<br />
C. The cost of services that:<br />
1. Are furnished without charge • or<br />
2. Are normally furnished without charge to persons without health insurance coverage;<br />
3. Would have been furnished without charge if you were not covered under this Certificate or under any health insurance.<br />
D. Services that are not described as covered in this Certificate or that do not meet all other conditions<br />
and criteria for coverage, as determined by the Plan. Referral by a Primary Care Physician and/<br />
or the provision of services by a Plan Provider does not, by itself, entitle a Member to benefits if the<br />
services are non-covered or do not otherwise meet the conditions and criteria for coverage.<br />
E. Routine foot care including any service related to hygiene including the trimming of corns or calluses,<br />
flat feet, fallen arches, chronic foot strain, or partial removal of a nail without the removal of the matrix<br />
except when we determine that Medically Necessary treatment was required because of an underlying<br />
health condition such as diabetes, and that all other conditions for coverage have been met.<br />
F. Dental care including extractions • treatment of cavities • care of the gums or bones supporting the teeth • treatment of<br />
periodontal abscess • removal of impacted teeth • orthodontia • false teeth • or any other dental services or supplies. These<br />
services may be covered under a separate rider or endorsement purchased by your Group and attached to this Certificate.<br />
G. Cosmetic surgery (except benefits for Breast Reconstructive Surgery) or other services primarily intended<br />
to correct, change or improve appearances. Cosmetic means a service or supply which is provided with the<br />
primary intent of improving appearances and not for the purpose of restoring bodily function or correcting<br />
deformity resulting from disease, trauma, or previous therapeutic intervention as determined by the Plan.<br />
H. Treatment rendered by a health care provider who is a member of the Member’s<br />
family (parents, spouse, brothers, sisters, children).<br />
I. Any prescription drugs obtained and self-administered by the Member for outpatient use unless the prescription drug is<br />
specifically covered under the Certificate or a rider or endorsement purchased by your Group and attached to this Certificate.<br />
J. Any procedure or treatment designed to alter an individual’s physical characteristics to those of the opposite sex.<br />
K. Services to reverse voluntary surgically induced infertility such as a reversal of sterilization.<br />
L. All assisted reproductive technologies (except artificial insemination) including in vitro fertilization, gamete<br />
intra-fallopian tube transfer, zygote intra-fallopian transfer cryogenic preservation or storage of eggs and embryo<br />
and related evaluative procedures, drugs, diagnostic services and medical preparations related to the same<br />
unless covered under a rider or endorsement purchased by your Group and attached to this Certificate.<br />
M. Fees or charges relating to fitness programs, weight loss or weight control programs • physical conditioning • pulmonary<br />
rehabilitation programs • exercise programs • physical conditioning • use of passive or patient-activated exercise equipment.<br />
N. Treatment for obesity except for the surgical treatment of Morbid Obesity.<br />
O. Medical or surgical treatment of myopia or hyperopia. Coverage is not provided for radial<br />
keratotomy and any other forms of refractive keratoplasty, or any complications.<br />
P. Services furnished as a result of a referral prohibited by law.<br />
Q. Services solely required or sought on the basis of a court order or as a condition of<br />
parole or probation unless authorized or approved by the Plan.<br />
R. Health education classes and self-help programs, other than birthing classes or for the treatment of diabetes.<br />
S. Acupuncture services except when approved or authorized by the Plan when used for anesthesia.<br />
T. Any service related to recreational activities. This includes, but is not limited to: sports • games •<br />
equestrian • and athletic training. These services are not covered unless authorized or approved by the<br />
Plan even though they may have therapeutic value or be provided by a health care provider.<br />
U. Cardiac rehabilitation programs.<br />
V. Any service received at no charge to the Member in any federal hospital or facility, or through any federal, state, or local<br />
governmental agency or department, not including Medicaid. This exclusion does not apply to care received in a Veteran’s<br />
Hospital or facility unless that care is rendered for a condition that is a result of the Member’s military service.<br />
W. Benefits will not be provided for Habilitative Services. Benefits for physical therapy, occupational<br />
therapy and speech therapy do not include benefits for Habilitative Services.<br />
10.2 Organ and Tissue Transplants. Benefits will not be provided for the following:<br />
A. Non-human organs and their implantation.<br />
B. Any hospital or professional charges related to any accidental injury or medical<br />
condition for the donor of the transplant material.<br />
C. Any charges related to transportation, lodging, and meals unless authorized or approved by the Plan.<br />
D. Services for a Member who is an organ donor when the recipient is not a Member.<br />
E. Any service, supply or device related to a transplant that is not listed as a benefit in this Certificate.
10.3 Inpatient Hospital Services. Benefits will not be provided for the following:<br />
A. Private room, unless Medically Necessary and authorized or approved by the Plan. If a private room is not authorized or<br />
approved, the difference between the charge for the private room and the charge for a semiprivate room will not be covered.<br />
B. Non-medical items and convenience items, such as television and phone rentals.<br />
C. A Hospital admission or any portion of a Hospital admission that had not been authorized or approved by the<br />
Plan, whether or not services are Medically Necessary and/or meet all other conditions for coverage.<br />
D. Private duty nursing unless authorized or approved by the Plan.<br />
10.4 Hospice Benefits. The following are not covered:<br />
A. Services, visits, medical equipment or supplies that are not included in the Plan-approved plan of treatment.<br />
B. Services in the Member’s home if it is outside the Service Area.<br />
C. Financial and legal counseling.<br />
D. Any service for which a Qualified Hospice Care Program does not customarily charge the patient or his or her family.<br />
E. Chemotherapy or radiation therapy, unless used for symptom control.<br />
F. Reimbursement for volunteer services.<br />
G. Domestic or housekeeping services.<br />
H. Meal on Wheels or similar food service arrangements.<br />
I. Rental or purchase of renal dialysis equipment and supplies.<br />
10.5 Outpatient Mental Health and Substance Abuse. Benefits will not be provided for:<br />
A. Psychological testing, unless Medically Necessary, as determined by the Plan,<br />
and appropriate within the scope of covered services.<br />
B. Services solely on court order or as a condition of parole or probation unless<br />
approved or authorized by the Plan’s Medical Director.<br />
C. Mental retardation, after diagnosis.<br />
D. Psychoanalysis.<br />
10.6 Inpatient Mental Health and Substance. The following services are excluded:<br />
A. Admissions as a result of a court order or as a condition of parole or probation<br />
unless approved or authorized by the Plan’s Medical Director.<br />
B. Custodial Care.<br />
C. Observation or isolation.<br />
10.7 Emergency Services and Urgent Care. Benefits will not be provided for:<br />
A. Emergency care if the Member could have foreseen the need for the care before it became<br />
urgent (for example, periodic chemotherapy or dialysis treatment).<br />
B. Medical services rendered outside of the Service Area which could have been<br />
foreseen by the Member prior to departing the Service Area.<br />
C. Charges for Emergency and Urgent Care services received from a non-Plan Provider after the<br />
Member could reasonably be expected to travel to the nearest Plan Provider.<br />
D. Charges for services when the claim filing and notice procedures stated in Section<br />
7 of this Certificate have not been followed by the Member.<br />
E. Charges for follow-up care received in the Emergency or Urgent Care facility outside of the Service Area unless the<br />
Plan determines that the member could not reasonably be expected to return to the Service Area for such care.<br />
F. Except for covered ambulance services, travel, whether or not recommended by a Plan Provider.<br />
8.8 Limitations and Exclusions for Medical Devices. Benefits will not be<br />
provided for the purchase, rental or repair of the following:<br />
A. Convenience item. Any item that increases physical comfort or convenience without serving a<br />
Medically Necessary purpose (e.g., elevators, hoyer/stair lifts, shower/bath bench).<br />
B. Furniture items. Movable articles or accessories which serve as a place upon which to rest<br />
(people or things) or in which things are placed or stored (e.g., chair or dresser).<br />
C. Exercise Equipment. Any device or object that serves as a means for energetic physical action or exertion in order to<br />
train, strengthen or condition all or part of the human body (e.g., exercycle or other physical fitness equipment).<br />
D. Institutional equipment. Any device or appliance that is appropriate for use in a medical<br />
facility and is not appropriate for use in the home (e.g., parallel bars).<br />
E. Environmental control equipment. Any device such as air conditioners, humidifiers, or electric air cleaners. These<br />
items are not covered even though they may be prescribed, in the individual’s case, for a medical reason.<br />
F. Eyeglasses, contact lenses, hearing aids, dental prostheses or appliances.<br />
G. Corrective shoes, unless they are an integral part of the lower body brace, shoe lifts or special shoe accessories.