Magnetic Resonance Angiography Techniques
Magnetic Resonance Angiography Techniques
Magnetic Resonance Angiography Techniques
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Magnetic</strong> <strong>Resonance</strong> <strong>Angiography</strong> <strong>Techniques</strong><br />
G. Laub 1 , J. Gaa 2 , M. Drobnitzky 1<br />
1<br />
Siemens AG, Medical Engineering Group, Erlangen, Germany<br />
2<br />
Institute for Clinical Radiology, University Hospital of Mannheim, Germany<br />
Introduction<br />
MR Imaging (MRI) depends on relaxation times T 1<br />
and T 2 and spin density . Furthermore, MRI is very<br />
sensitive to motion resulting in a variety of flow effects.<br />
On one hand, flow effects are responsible for a number<br />
of artifacts which can drastically impair the diagnostic<br />
value of the images; on the other hand, flow effects<br />
can be used advantageously to develop non-invasive<br />
techniques for imaging of the vascular anatomy. These<br />
techniques are referred to as <strong>Magnetic</strong> <strong>Resonance</strong><br />
<strong>Angiography</strong> (MRA). The techniques most commonly<br />
used for MRA can be classified into two major categories:<br />
Time-of-flight and phase contrast MR angiography.<br />
Both techniques rely on separate physical effects,<br />
and will result in images with different information<br />
about the vasculature. More recently, the use of contrast<br />
agents in combination with ultra-fast T 1-weighted<br />
imaging sequences has shown significant improvements<br />
in the delineation of the vessel lumen. It is important to<br />
note that a proper use of MRA techniques and correct<br />
interpretation of MR angiographic images requires<br />
a knowledge of the underlying physical mechanisms of<br />
flow sensitivity in MRI [1, 2].<br />
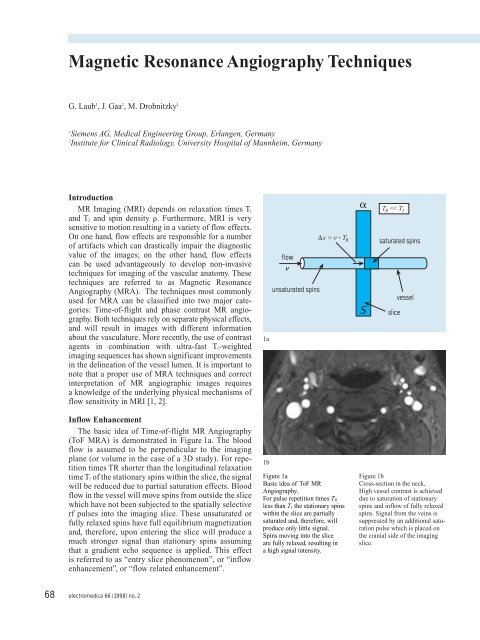
1a<br />
T R
A typical application of this effect is demonstrated<br />
in Figure 1b which shows a thin section acquired in<br />
the neck. Due to the relatively large flip angle of 40°<br />
in combination with a short pulse repetition rate of<br />
30 msec, the signal from stationary tissue is almost<br />
saturated. In general, blood flow signal from the veins<br />
can be sufficiently removed by the application of additional<br />
saturation pulses which are applied on the cranial<br />
side of the slice. A repetition of the same sequence at<br />
different slice positions results in a series of images<br />
which show the vascular tree as a sum of individual slices.<br />
The amount of inflow enhancement depends on<br />
several factors, including tissue specific parameters like<br />
T 1, sequence specific parameters (flip angle , and T R),<br />
and geometrical parameters like slice thickness and<br />
orientation, or blood flow velocity.<br />
Postprocessing of MR <strong>Angiography</strong> Data<br />
In principle, with this technique any vessel segment<br />
can be imaged by cutting through the vessel perpendicularly<br />
with regard to the flow direction. With repetitive<br />
increments of the slice position a three-dimensional data<br />
set of the complete vascular structure can be measured<br />
[3, 4]. For the observer, this form of representation<br />
requires experience in order to obtain the correct threedimensional<br />
spatial impression. Obviously, postprocessing<br />
methods should be used to extract two-dimensional<br />
projections of the vasculature from the three-dimensional<br />
volume data [5]. With these methods threedimensional<br />
perception can be obtained in two ways – by<br />
showing a sequence of projective images with different<br />
projection angles or by coding of the depth information<br />
onto the surface of the displayed objects.<br />
Since the surfaces of most vessels are relatively small,<br />
the first method – multiple projections with different<br />
angles – has proven more useful in practice. The starting<br />
point for this method must be a three-dimensional data<br />
set in which the structures to be extracted are associated<br />
with a characteristic range of signal intensity levels. In<br />
this case a projective image can be calculated by penetrating<br />
the data volume with a set of parallel projection<br />
rays and selecting along each of these rays only the data<br />
point that represents the maximum intensity as demonstrated<br />
in Figure 2. The inflow enhancement and proper<br />
pulse-sequence parameters (flip angle, pulse repetition<br />
time, and flow-compensation) assure that the maximum<br />
intensity is always associated with a blood vessel, as long<br />
as the projection ray intersects at least one [6, 7]. All of<br />
the other projection rays will just pick up a background<br />
pixel intensity of the three-dimensional data set. As a<br />
result, Figure 3 demonstrates a complete projection<br />
image at different viewing angle calculated from one<br />
single 3D data set.<br />
By varying the projection angle multiple projective<br />
images can be obtained retrospectively which allow the<br />
observer to obtain the correct spatial perception of the<br />
A<br />
B<br />
C<br />
D<br />
I<br />
I max<br />
Figure 2<br />
Principle of Maximum Intensity<br />
Projection (MIP). Along each ray<br />
only the pixel with the highest<br />
signal intensity I max is projected<br />
onto the imaging plane.<br />
Figure 3<br />
Application of MIP post-processing<br />
to a 3D data set in the neck.<br />
Different views can be calculated<br />
retrospectively to create a 3D<br />
perception of the carotid arteries.<br />
three-dimensional data set. By displaying a number of<br />
projections with projection increments of only a few<br />
degrees in a rapid fashion, the perception of a continuously<br />
rotated object will be generated which allows a<br />
correct three-dimensional visualization of such complex<br />
structures as a vessel tree.<br />
In some instances, particularly for the best assessment<br />
of a vessel narrowing, it is recommended to also evaluate<br />
the source images in addition to the MIP results. In complex<br />
anatomical situations as in the case of the depiction<br />
E<br />
electromedica 66 (1998) no. 2 69<br />
A<br />
B<br />
C<br />
D<br />
E
of the renal arteries it is clearly favorable to restrict the<br />
MIP algorithm to those parts of the whole data volume<br />
which covers the vasculature of interest thereby avoiding<br />
projection-related misinterpretations [9].<br />
ToF MR <strong>Angiography</strong> <strong>Techniques</strong><br />
ToF MR <strong>Angiography</strong> can be classified into three<br />
major categories as demonstrated in Figure 4. On the left<br />
side (Figure 4a), a sequential two-dimensional technique<br />
is shown which provides multiple thin sections of the<br />
vessels. Alternatively, a three-dimensional technique<br />
can be applied. As demonstrated in Figure 4b, the whole<br />
volume is excited simultaneously, and will then be<br />
subdivided into thin partitions, or slices by using an<br />
additional phase encoding scheme in the slice select<br />
direction. Unlike in 2D imaging, where the slice resolution<br />
is defined by the excitation profile of the radiofrequency<br />
pulse, the slice resolution is defined by spatially<br />
encoding magnetic field gradients and can be less than<br />
1 mm. Both techniques – 2D and 3D – are currently used<br />
in clinical applications. There are specific advantages,<br />
and disadvantages related to each of the techniques.<br />
While 2D techniques offer a high vessel/background<br />
contrast which is pretty much constant over the coverage<br />
of the vasculare structure, the vessel/background contrast<br />
in 3D techniques is typically lower, and is progressively<br />
getting smaller when spins penetrate through the<br />
imaging volume. The slab thickness, or vessel coverage<br />
in 3D techniques is therefore limited to a distance at<br />
which blood signal approaches a steady state signal.<br />
Typically, 3D techniques are applicable in combination<br />
with fast flow situations, while 2D techniques may be<br />
applied for the visualization of slower flow as well.<br />
Another aspect in selecting two- or three-dimensional<br />
techniques is related to the spatial resolution. In 2D techniques<br />
the spatial resolution is defined by the in-plane<br />
resolution (FOV divided by the matrix size, or number<br />
of lines, respectively), and the slice thickness of the<br />
sequence. Typically, in-plane resolution may be isotropic,<br />
like 0.8 mm x 0.8 mm, but slice thickness is more<br />
than that, like 2-3 mm, resulting in an anisotropic volume<br />
data set. Isotropic resolution, i.e. the voxel size has equal<br />
length in all directions, can be obtained with 3D techniques,<br />
which also offer a better signal-to-noise ratio due<br />
to the averaging effect of the phase encoding in the slab<br />
direction. Small vessels, as they typically occur in the<br />
intracranial vasculature are generally better visualized<br />
with a 3D technique, while larger vessel with a predominantly<br />
uni-directional flow, e. g. the common carotid<br />
artery, may be visualized very well with 2D techniques.<br />
slice #<br />
1<br />
2<br />
3<br />
single slab<br />
(3DFT)<br />
slab 4<br />
slab 3<br />
slab 2<br />
Figure 4<br />
<strong>Techniques</strong> for<br />
ToF MR <strong>Angiography</strong>:<br />
sequential 2D (a),<br />
volume imaging (b),<br />
multi-slab (c)<br />
N<br />
slab 1<br />
flow flow flow<br />
a b c<br />
flow<br />
<br />
small<br />
<br />
large<br />
MT pulse<br />
water<br />
Magnetization reduction<br />
as a result of<br />
magnetization transfer<br />
macromolecules<br />
frequency<br />
Figure 5<br />
<strong>Techniques</strong> to improve vessel<br />
contrast in ToF MR <strong>Angiography</strong>.<br />
5a: Ramped rf pulses are used to<br />
partially compensate for the progressive<br />
saturation of spins in 3D<br />
ToF MRA.<br />
5b: Magnetization transfer<br />
effects are used to improve the<br />
vessel-background contrast.<br />
imaging<br />
volume<br />
5a<br />
dipolar interaction<br />
between water<br />
and macromolecules<br />
5b<br />
70<br />
electromedica 66 (1998) no. 2
One of the major limitation in three-dimensional<br />
ToF MRA is the loss of vessel contrast as spins are<br />
penetrating into the imaging volume. This effect is due<br />
to progressive saturation when spins are experiencing<br />
the rf excitation pulses in the imaging volume.<br />
A technique which is used to address the spin saturation<br />
in 3D ToF MRA techniques is referred to as multislab<br />
MRA, or MOTSA (see Figure 4c) [8]. Several slabs<br />
are used to create sufficient coverage over the vasculature.<br />
Each of the slabs is thin enough to avoid significant<br />
spin saturation within this slab. All of the slabs are<br />
acquired in a sequential mode, i.e. one slab is acquired<br />
after the other. The advantage of this technique is that<br />
it combines the isotropic resolution capability of the<br />
3D technique with a relatively small amount of spin<br />
saturation similar to the 2D techniques. The disdvantage<br />
of the multi-slab technique is related to the imperfections<br />
of the slice profile. Therefore, all of the slabs need<br />
to overlap by about 20-30% to avoid venetian blind<br />
effects in areas in between the slabs.<br />
A more effective use of the magnetization is possible<br />
when using variable flip angles across the slab as shown<br />
in Figure 5a. At the entrance plane when spins enter with<br />
equilibrium magnetization a relatively small flip angle<br />
is used which still provides sufficient signal, with only<br />
little effects on the longitudinal magnetization. The flip<br />
angle is increased deeper in the imaging volume to<br />
compensate for the reduction of the longitudinal<br />
magnetization of the spins on their way through the<br />
volume, and so forth. In principle, it is possible to shape<br />
the flip angle distribution over the entire imaging volume<br />
according to the specific flow velocity and vessel<br />
coverage.<br />
Another improvement is possible by the application of<br />
magnetization transfer pulses (MTC) as demonstrated in<br />
Figure 5b. The idea is to use off-resonance rf pulses<br />
which do not directly affect the mobile protons which are<br />
used to create the signal in MRI. Protons with restricted<br />
mobility, however, do get saturated, and because of cross<br />
correlation or chemical exchange processes the magnetization<br />
will be transfered to some biological tissue such<br />
as grey, or white matter resulting in a partial saturation.<br />
Blood will not be affected by the MTC pulses, and as a<br />
result, there will be more contrast between blood and<br />
background.<br />
Flow-Induced Phase Shift<br />
The second class of MR <strong>Angiography</strong> techniques is<br />
based on the changes in the phase of the transverse<br />
magnetization. These phase shifts occur when the spins<br />
move along the magnetic field gradients which are used<br />
for position encoding in 2D and 3D Fourier imaging.<br />
For a gradient pulse pair as shown in Figure 6 the flowinduced<br />
phase shift V is given as<br />
= • • A • v<br />
V<br />
+ A<br />
<br />
-A<br />
V<br />
= • A • • v<br />
time<br />
Figure 6<br />
Motion along a bipolar gradient<br />
pulse pair results in a flow-induced<br />
phase shift of the transverse<br />
magnetization. Stationary spins<br />
will not be affected by the bipolar<br />
gradient pulse pair. The amount<br />
of phase shifts depends on the<br />
area of each gradient pulse, and<br />
distance between the pulses.<br />
which shows a linear relationship between the phase shift<br />
of a moving spin and its velocity. The flow-induced<br />
phase shift can be used for flow imaging and flow<br />
quantification techniques.<br />
Phase Contrast MR <strong>Angiography</strong><br />
The basic idea of phase-contrast MRA is to acquire<br />
two data sets with a different amount of flow sensitivity<br />
as shown in Figure 7 [10]. The first data set S 1 is<br />
acquired with a flow compensated sequence, i.e. without<br />
flow sensitivity. The second data set S 2 is acquired<br />
with a flow sensitive sequence. The amount of flow<br />
sensitivity is controlled by the strength of the gradient<br />
pulse pair which is incorporated into the sequence.<br />
After completion of the measurement, both signals are<br />
subtracted to create a complex difference ÆS. The length<br />
of the difference ÆS depends on the phase shift V<br />
within each pixel. An image which shows the signal<br />
intensity ÆS represents the velocity of spins at each point<br />
within the field of view. Both 2D and 3D acquisition<br />
techniques can be applied with phase contrast MRA<br />
[11-15]. Alternatively, the phase shift V can be evaluated<br />
from the measurement of S 1 and S 2. As shown<br />
above, the phase shift V is proportional to the spin’s<br />
velocity, and therefore the measurement of V allows<br />
the quantitative assessment of flow velocities.<br />
The difference signal ÆS has a maximum value for<br />
opposite directions of S 1 and S 2, i.e. for V = 180°. This<br />
velocity is typically referred to as venc, and depends on<br />
the sequence design, i.e. pulse amplitude and distance<br />
between the gradient pulse pair which is used for flow<br />
encoding. For velocities larger than venc the difference<br />
signal is decreased constantly until it gets zero for<br />
V = 360°. Therefore, in phase contrast (PC) MRA it is<br />
important to correctly set the venc of the sequence to the<br />
maximum flow velocity which is expected during the<br />
measurement.<br />
M y<br />
flow<br />
V<br />
stationary<br />
M x<br />
electromedica 66 (1998) no. 2 71
72<br />
M x<br />
flow compensated flow sensitive subtraction<br />
A bipolar gradient pulse pair produces a phase shift<br />
which depends on the velocity component along this<br />
gradient. For a complete measurement of the flow velocity<br />
more measurements are necessary with orthogonal<br />
flow sensitization, e.g.<br />
image 1: flow compensated<br />
relaxation times T 1<br />
repetition time T R of 10 msec.<br />
image 2: flow sensitization along x (e.g. read gradient)<br />
image 3: flow sensitization along y (e.g. phase encode<br />
gradient)<br />
image 4: flow sensitization along z (e.g. slice select This is due to shortening of the T 1<br />
gradient)<br />
postprocessing is done in the following way:<br />
v read = image 1 – image 2<br />
v phase = image 1 – image 3<br />
v slice = image 1 – image 4<br />
V = (v 2 read + v 2 phase + v 2 slice)<br />
G slice<br />
G phase<br />
electromedica 66 (1998) no. 2<br />
V<br />
Figure 8<br />
Typical sequence diagram for<br />
phase contrast MR <strong>Angiography</strong>.<br />
A bipolar flow encoding pulse<br />
pair is applied in subsequent<br />
measurements in slice, phase,<br />
and read direction, respectively.<br />
S 2<br />
V<br />
S 1<br />
Æ S<br />
Figure 7<br />
Basic idea of phase contrast<br />
<strong>Angiography</strong>. The complex<br />
subtraction ÆS of two data sets<br />
which are acquired with a<br />
different amount of flow sensitivity<br />
(e.g. flow compensated<br />
S 1 and flow sensitized S 2)<br />
produces an image with signal<br />
intensities depending on local<br />
flow velocities.<br />
Contrast-Enhanced MR <strong>Angiography</strong><br />
The signal response of a Flash-type sequence as a<br />
function of the flip angle is shown in the following<br />
diagram (Fig. 8) for tissues of various longitudinal<br />
assuming a sequence with a pulse<br />
In contrast-enhanced MR <strong>Angiography</strong> (CE-MRA),<br />
the use of a paramagnetic extracellular contrast agent<br />
(such as Gd-DTPA) increases the blood signal [16, 17].<br />
relaxation time of<br />
blood after contrast injection. The amount of signal<br />
enhancement with T 1 shortening is as shown in Figure 9.<br />
Depending on the actual concentration of Gd-DTPA<br />
the arterial blood T 1 can be as short as 50 ... 100 msec,<br />
substantially shorter than the T 1 of fat. Therefore, blood<br />
produces the largest signal, and thus the vessel lumen<br />
will be picked up with the maximum intensity program<br />
(MIP) to create an MR angiogram [18-20].<br />
Following the intravenous (IV) injection of the contrast<br />
agent, it is delivered to the vasculature of interest.<br />
Local blood signal is substantially enhanced. This<br />
result is optimal when data collection (in particular the<br />
center of k-space) occurs right when the contrast agent<br />
arrives at the vessels being imaged as shown in Figure<br />
10. Therefore, timing of the scan with respect to the<br />
intravenous injection of contrast agent is very important<br />
in CE-MRA. In a clinical setting the contrast arrival<br />
time is best determined by administering a small testbolus<br />
and continuously monitoring for vascular signal<br />
enhancement in the region of interest using a very fast<br />
gradient-echo technique with fluoroscopic image update.<br />
Furthermore, there will be venous enhancement<br />
visible when the acquisition window is long enough to<br />
catch the venous phase as well. Therefore, the acquisition<br />
window is limited to about 10 to 15 seconds in the<br />
carotid artery to avoid excessive signal enhancement in<br />
the jugular vein [22]. Similar constraints exist for the<br />
first-pass bolus width for imaging of the abdominal<br />
vasculature [21, 23].<br />
One major technical prerequisites for CE-MRA is the<br />
availability of a high-performance gradient system to
each the very short echo and repetition times needed<br />
to cover a resonable 3D-volume in the time given by<br />
the arterio-venous transit time. At the same time it is<br />
mandatory to use CP-phased array coils for complete<br />
volume coverage, fitted to the anatomy, to optimize<br />
signal-to-noise.<br />
The clinical significance of CE-MRA is expected to<br />
grow due to a number of reasons: T 1-shortening as the<br />
source of signal increase is virtually immune against<br />
signal loss due to flow-related dephasing especially for<br />
in-plane flow as encountered in ToF- and PC-MR<br />
angiography. This is clearly advantageous in situations<br />
of tortuous vessels and stenotic regions. Due to the fact<br />
that Gd-DTPA has no nephrotoxic potential its use in<br />
kidney studies is widely accepted. Furthermore it is<br />
reported in the literature that the depiction of large aneu-<br />
risms is markedly simplified with CE-MRA compared<br />
to DSA because filling and subsequent washout of<br />
contrast material is not immediate but can be traced<br />
over a longer period of time. The main advantage<br />
of CE-MRA compared to ToF- and PC-MRA is its intrinsic<br />
advantage in acquisition speed, if sufficient<br />
strong gradients are available. This results from the fact<br />
that the slice orientation can now be chosen independent<br />
of the primary vessel direction and must not longer be<br />
perpendicular to the vessel. Instead, the image plane can<br />
now be chosen to be along any major vessel axis.<br />
We consider CE-MRA as an emerging new vascular<br />
application of MR. Its specific advantages with respect<br />
to conventional DSA is currently been studied at major<br />
research centers. Outcome analysis and its potential<br />
to reduce costs are currently considered by a growing<br />
number of research groups.<br />
signal intensity<br />
T R = 10 ms<br />
T 1 = 50 ms<br />
Figure 9<br />
Relative signal intensity versus<br />
flip angle for a spoiled gradientecho<br />
sequence (FLASH) for<br />
tissues of various T 1, and a T R of<br />
10 msec. The flip angle is<br />
selected to produce the largest<br />
signal for the short T 1 tissues<br />
T 1 = 100 ms<br />
T 1 = 260 ms (fat)<br />
T 1 = 1200 ms (blood)<br />
contrast<br />
injection<br />
arterial phase<br />
venous phase<br />
Figure 10<br />
Timing of contrast-enhanced<br />
MR <strong>Angiography</strong>. In this study a<br />
series of ultrafast 3D measurements<br />
with only 4 sec scan time<br />
was acquired right after bolus<br />
injection of a single-dose<br />
Gd-DTPA. Note rapid filling<br />
of the aorta and subsequent<br />
filling of the renal vein, as an<br />
example.<br />
8 sec 12 sec 16 sec 20 sec 24 sec 28 sec 32 sec<br />
electromedica 66 (1998) no. 2 73
Figure 11<br />
Dual-phase contrast-enhanced<br />
MRA study. The first measurement<br />
(left) is done during the<br />
arterial phase. Twenty seconds<br />
later a second measurement<br />
is performed to get an image<br />
during the venous phase. Each<br />
measurement is done during<br />
a breath-hold of 24 seconds.<br />
Figure 12<br />
Carotid MR <strong>Angiography</strong>.<br />
Left: 2D-ToF technique.<br />
The stripe artifact is due to<br />
swallowing right during the<br />
acquisition of this particular<br />
slice.<br />
Right: Contrast-enhanced 3D<br />
MRA technique. A 3D volume is<br />
acquired with a scan time of<br />
only 10 seconds. Due to the short<br />
acquisition time the venous<br />
enhancement is relatively small.<br />
A stenosis is demonstrated in<br />
the left internal carotid artery.<br />
Figure 13<br />
Thoracic MR <strong>Angiography</strong>. Two<br />
maximum intensity projections<br />
are shown from the same 3D<br />
data set. A 1.5 mm isotropic<br />
resolution is acquired in a single<br />
breath-hold of 23 seconds<br />
after injection of a double-dose<br />
Gd-DTPA.<br />
Figure 14<br />
Application of contrastenhanced<br />
MR <strong>Angiography</strong> in<br />
the abdominal vasculature.<br />
Left: Demonstration of<br />
aneurysms in the abdominal<br />
aorta.<br />
Right: Demonstration of multivessel<br />
disease in the aorta and<br />
femoral artery.<br />
74<br />
electromedica 66 (1998) no. 2
Literature:<br />
General<br />
[1] Anderson, C. M., Edelman, R. R., Turski, P.A.: Clinical <strong>Magnetic</strong><br />
<strong>Resonance</strong> <strong>Angiography</strong>: New York, NY; Raven Press, 1993.<br />
[2] Potchen, J. E., Haacke, E. M., Siebert J. E., Gottschalk, A.:<br />
<strong>Magnetic</strong> <strong>Resonance</strong> <strong>Angiography</strong>: Concepts and Applications.<br />
St. Louis, MO; Mosby, 1993.<br />
Time-of-flight MRA<br />
[3] Masaryk, T. J., Modic, M. T., Ruggieri, P. M., et al: Three-dimensional<br />
(volume) gradient-echo imaging of the carotid bifurcation:<br />
preliminary clinical experience. Radiology 171: 801-806, 1989.<br />
[4] Masaryk, T. J., Modic, M. T., Ross, J. S., et al: Intracranial<br />
circulation: preliminary clinical experience with three-dimensional<br />
(volume) MR angiography . Radiology 171: 793-799, 1989.<br />
[5] Keller, P. J., Drayer, B. P., Fram, E. K., et al: MR angiography with<br />
two-dimensional acquisition and three-dimensional display, Radiology<br />
173: 527-532, 1989.<br />
[18] Marchal, G., Michiels, J., Bosmans, H., Van Hecke, P.: Contrastenhanced<br />
MRA of the brain. J Comput Assist Tomogr 16: 25-29, 1992.<br />
[19] Runge, V. M., Kirsch, J. E., Lee, C: Contrast-enhanced MR angiography,<br />
J Magn Reson Imaging 3: 233-239, 1993.<br />
[20] Lin, W., Haacke, E. M. , Smith, As., Clampitt, M. E.: Gadoliniumenhanced<br />
high-resolution MR angiography with adaptive vessel tracking:<br />
preliminary results in the intracranial circulation. J Magn Reson<br />
Imaging 2: 277-284, 1992.<br />
[21] Prince, M. R.: Body MR angiography with gadolinium contrast<br />
agents. Magn Reson Imaging Clin N Am 4: 11-24, 1996.<br />
[22] Levy, R., Prince, M.R.: Arterial-phase three-dimensional contrastenhanced<br />
MR angiography of the carotid arteries. Am J Roentgenol<br />
167: 211-215, 1996.<br />
[23] Gaa, J., Laub, G., Edelman, R. R., Georgi, M.: First clinical results<br />
of ultrafast, gadolinium-enhanced dual-phase 3D MR-angiography in<br />
the abdomen. Fortschr Röntgenstr 169,2: 135-139, 1998.<br />
[6] Marchal, G., Bosmans, H., VanFraeyenhoven, L., et al.: Intracranial<br />
vascular lesions: optimization and clinical evaluation of threedimensional<br />
time-of-flight MR angiography, Radiology 175: 443-448,<br />
1990.<br />
[7] Ruggieri, P. M., Laub, G. A., Masaryk, T. M., Modic, M. T.: Intracranial<br />
circulation: pulse-sequence considerations in three-dimensional<br />
(volume) MR angiography, Radiology 171: 785-791, 1989.<br />
[8] Parker, G. L., Yuan, C., Blatter, D. D.: MR angiography by multiple<br />
thin-slab 3D acquisition, Magn Reson Med 17: 434-451, 1991.<br />
[9] Litt, A. W., Eidelman, E. M., Pinto, R. S., et al: Diagnosis of<br />
carotid artery stenosis: comparison of 2DFT time-of-flight MR<br />
angiography with contrast angiography in 50 patients, AJNR 12: 149-<br />
154, 1991.<br />
Phase-contrast MRA<br />
[10] Axel, L., Morton, D.: MR flow imaging by velocity-compensated/<br />
uncompensated difference images, J Comput Assist Tomogr 11: 31-34,<br />
1987.<br />
[11] Dumoulin, C. L., Souza, S. P., Walker, M. F., Wagle, W.: Threedimensional<br />
phase contrast angiography, Magn Res Med 9: 139-149,<br />
1989.<br />
[12] Pernicone, J. R., Siebert, J. E., Potchen, E. J., et al: Three-dimensional<br />
phase contrast MR angiography in the head and neck: preliminary<br />
report, AJNR 11: 457-466, 1990.<br />
[13] Pelc, N. J., Bernstein, M. A., Shimakawa, A.: Encoding strategies<br />
for three-dimensional phase contrast MR imaging of flow, J Magn<br />
Reson Imag 1: 405-413, 1991.<br />
[14] Hausmann, R., Lewin, J. S., Laub, G.: Phase-contrast MR angiography<br />
with reduced acquisition time: new concepts in sequence design,<br />
J Magn Reson Imaging 1: 415-422, 1991.<br />
[15] Dumoulin, C. L.: Phase contrast magnetic resonance angiography,<br />
Neuroimaging Clinics of North America 2: 21-41, 1992.<br />
Contrast-enhanced MRA<br />
[16] Creasy, J. L., Price, R. R., Prsbrey, T., et al: Gadolinium-enhanced<br />
MR angiography, Radiology 175: 280-283, 1990.<br />
[17] Chakeres, D. W., Schmalbrock, P., Brogan, M., et al: Normal<br />
venous anatomy: demonstrated with gadopentetate dimeglumine in<br />
enhanced 3D MR angiography, AJNR 11: 1107-1118, 1990<br />
Author’s address:<br />
Dr. Gerhard Laub<br />
Siemens AG, Medical Engineering Group<br />
Henkestrasse 127<br />
D-91052 Erlangen, Germany<br />
electromedica 66 (1998) no. 2 75