DISCHARGE SUMMARY
DISCHARGE SUMMARY
DISCHARGE SUMMARY
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
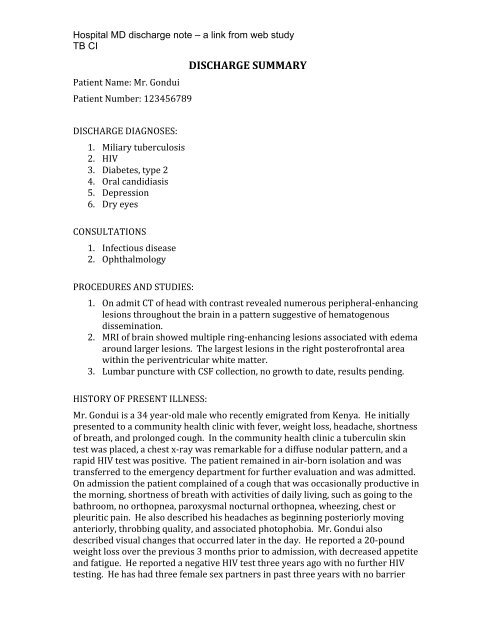
Hospital MD discharge note – a link from web study<br />
TB CI <br />
Patient Name: Mr. Gondui <br />
Patient Number: 123456789 <br />
<strong>DISCHARGE</strong> <strong>SUMMARY</strong> <br />
<strong>DISCHARGE</strong> DIAGNOSES: <br />
1. Miliary tuberculosis <br />
2. HIV <br />
3. Diabetes, type 2 <br />
4. Oral candidiasis <br />
5. Depression <br />
6. Dry eyes <br />
CONSULTATIONS <br />
1. Infectious disease <br />
2. Ophthalmology <br />
PROCEDURES AND STUDIES: <br />
1. On admit CT of head with contrast revealed numerous peripheral-‐enhancing <br />
lesions throughout the brain in a pattern suggestive of hematogenous <br />
dissemination. <br />
2. MRI of brain showed multiple ring-‐enhancing lesions associated with edema <br />
around larger lesions. The largest lesions in the right posterofrontal area <br />
within the periventricular white matter. <br />
3. Lumbar puncture with CSF collection, no growth to date, results pending. <br />
HISTORY OF PRESENT ILLNESS: <br />
Mr. Gondui is a 34 year-‐old male who recently emigrated from Kenya. He initially <br />
presented to a community health clinic with fever, weight loss, headache, shortness <br />
of breath, and prolonged cough. In the community health clinic a tuberculin skin <br />
test was placed, a chest x-‐ray was remarkable for a diffuse nodular pattern, and a <br />
rapid HIV test was positive. The patient remained in air-‐born isolation and was <br />
transferred to the emergency department for further evaluation and was admitted. <br />
On admission the patient complained of a cough that was occasionally productive in <br />
the morning, shortness of breath with activities of daily living, such as going to the <br />
bathroom, no orthopnea, paroxysmal nocturnal orthopnea, wheezing, chest or <br />
pleuritic pain. He also described his headaches as beginning posteriorly moving <br />
anteriorly, throbbing quality, and associated photophobia. Mr. Gondui also <br />
described visual changes that occurred later in the day. He reported a 20-‐pound <br />
weight loss over the previous 3 months prior to admission, with decreased appetite <br />
and fatigue. He reported a negative HIV test three years ago with no further HIV <br />
testing. He has had three female sex partners in past three years with no barrier
Hospital MD discharge note – a link from web study<br />
TB CI <br />
methods used as protection from sexually transmitted infections. Denies any IVDU <br />
ever. He has had no known tuberculosis contacts. <br />
PAST MEDICAL HISTORY: <br />
1. Diabetes, type 2, diet controlled per patient. <br />
2. Erectile dysfunction. <br />
ALLERGIES: <br />
No known drug allergies <br />
SOCIAL HISTORY: <br />
Mr. Gondui came to the United States from Kenya about 10 months prior to <br />
admission. His family remains in Kenya. He currently lives with two married <br />
friends, without children, in an apartment. <br />
HABITS: <br />
TOBACCO: Smokes 1 ½ to 2 packs per day for 10 years, quit 7 years ago. <br />
ALCOHOL: No alcohol use since arriving in the United States. <br />
FAMILY HISTORY: <br />
No known diabetes, tuberculosis, or HIV. <br />
PHYSICAL EXAMINATION: <br />
GENERAL: A very thin male who is in mild respiratory distress, able to engage in <br />
conversation <br />
VITAL SIGNS: Temperature: 38.4 c; blood pressure 120/80; pulse 134; respiration <br />
16, O2 saturation 98% on room air. <br />
HEENT: Oropharynx with significant white plaques on buccal mucosa, palate, and <br />
posterior tongue. <br />
CARDIOVASCULAR: tachycardic regular rhythm without murmurs. <br />
LUNGS: Clear to auscultation bilaterally <br />
ABDOMEN: Bowel sounds present. Soft, non-‐tender, non distended. <br />
EXTREMITIES: Warm and well perfused. On left forearm where tuberculin skin test <br />
was placed is an area of induration of approximately 10 mm. <br />
NEUROLOGIC: Mr. Gondui is alert and oriented X3. Cranial nerves II – XII intact <br />
except for right facial droop. Strength 5/5 in upper and lower extremities
Hospital MD discharge note – a link from web study<br />
TB CI <br />
bilaterally. Deep tendon reflexes were 1+ in upper and lower extremities bilaterally. <br />
Toes were down-‐going bilaterally. Finger-‐nose-‐finger was intact and gait was <br />
normal. <br />
LABORATORY DATA: <br />
The metabolic panel was unremarkable except for slightly low sodium of 125 mg/dL <br />
and an elevated glucose of 320. White blood cell (WBC) 6.09, hematocrit 33%, <br />
platelets 304. Arterial blood gas was 7.4/27/84. Liver function tests (LFT) were <br />
normal except for a low albumin of 2.2. Chest x-‐ray showed diffuse nodular <br />
opacities bilaterally. Electrocardiogram showed sinus rhythm with a rate of 120 <br />
beats per minute. <br />
HOSPITAL COURSE BY PROBLEM: <br />
1. Miliary tuberculosis. Mr. Gondui was admitted to the hospital unit without a <br />
clear diagnosis. Other considerations included Pneumocystis pneumonia (PCP) or <br />
miliary malignancy. Given his positive tuberculin skin test (TST) and chest x-‐ray <br />
findings he was admitted to a negative pressure air-‐born isolation room. He was <br />
started on IV Bactrim for possible PCP. By hospital day #2, his sputum showed a <br />
positive stain for acid fast bacilli (AFB). In addition, the patient had a head CT which <br />
showed multiple ring-‐enhancing lesions. A lumbar puncture (LP) was performed <br />
which was negative for TB polymerase chain reaction (PCR), and thus far the culture <br />
taken from the cerebrospinal fluid (CSF) is still negative for AFB. Infectious Disease <br />
was consulted and Mr. Gondui began a 4-‐drug therapy for TB. He did well with no <br />
increase in his neurologic symptoms during the hospital course. Mr. Gondui was <br />
started on phenytoin (Dilantin) for prophylaxis. On the day of discharge his sputum <br />
was still positive for AFB and he was discharged with isolation precautions for his <br />
home. He will be followed by the TB Clinic for directly observed therapy. <br />
2. HIV. Mr. Gondui was admitted with positive rapid HIV test in community health <br />
clinic, but previously unknown to have HIV. A CD4 count was drawn at the hospital <br />
and was returned at 117 cells/mL. Mr. Gondui was not started on antiretroviral <br />
medications at this time due to the concern for immune reconstitution syndrome <br />
with his concurrent miliary TB and CNS lesions. He will be followed by the HIV <br />
clinic for appropriate management and care. He was started on <br />
sulfamethoxazole/trimethoprim (Bactrim) prophylaxis during this hospitalization. <br />
3. Diabetes. Mr. Gondui reported a history of elevated blood glucose levels. States <br />
he has been controlling elevated blood glucose levels with diet. On admission his <br />
blood glucose level was elevated at 320 mg/dL and his hemoglobin A1C was <br />
elevated at 8.9. He was started in glyburide 5 mg PO daily, and in turn this was <br />
titrated up to 10 mg PO daily. With the increased dose, his fasting blood glucose <br />
levels remained mostly within normal range. His treatment for diabetes can further <br />
be managed as an outpatient.
Hospital MD discharge note – a link from web study<br />
TB CI <br />
4. Depression. Mr. Gondui was quite affected by both his new diagnoses of miliary <br />
TB and HIV. He expressed depressive symptoms as well as anxiety on multiple <br />
occasions. He said he felt TB and HIV to be two of the worst diseases to have. He <br />
was started on Paxil 20 mg PO daily, and although this will not affect him during the <br />
hospitalization, he was feeling more hopeful by the time of discharge. <br />
5. Dry eyes. Mr. Gondui reported a scratchy feeling on admission to the hospital. <br />
Ophthalmology was consulted and recommended a lubricant and eye drops, which <br />
were prescribed upon discharge. <br />
6. Oral candida. Mr. Gondui has obvious white plaques on his buccal mucosa and <br />
palate on admission to the hospital. He was started on fluconazole and will continue <br />
for a 21-‐day course of treatment. <br />
CONDITION UPON <strong>DISCHARGE</strong>: <br />
Stable. <br />
MEDICATIONS: <br />
1. Fluconazole 200 mg PO daily X 14 days <br />
2. Zolpidem (Ambien) 5 mg PO Q HS <br />
3. Ophthalmic lubricant ½ inch, OU Q HS <br />
4. Carboxymethylcellulose 1%, 1 drop OU, four times daily <br />
5. Glipizide 10 mg PO Q morning <br />
6. Dilantin 400 mg PO Q HS <br />
7. Bactrim DS 1 tab PO daily <br />
8. Paxil 20 mg PO daily <br />
9. Prenatal vitamin 1 PO daily <br />
10. Isonaizid, rifampin, ethambutol, pyrazinamide, and pyridoxine to be prescribed <br />
by the TB Clinic. <br />
FOLLOW UP: <br />
Mr. Gondui was discharged in the care of the TB Clinic, who will follow the patient <br />
closely. Mr. Gondui will also follow up with the HIV clinic. <br />
________________________________________________________________________________________________