Secondary Chondrosarcoma
Secondary Chondrosarcoma
Secondary Chondrosarcoma
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
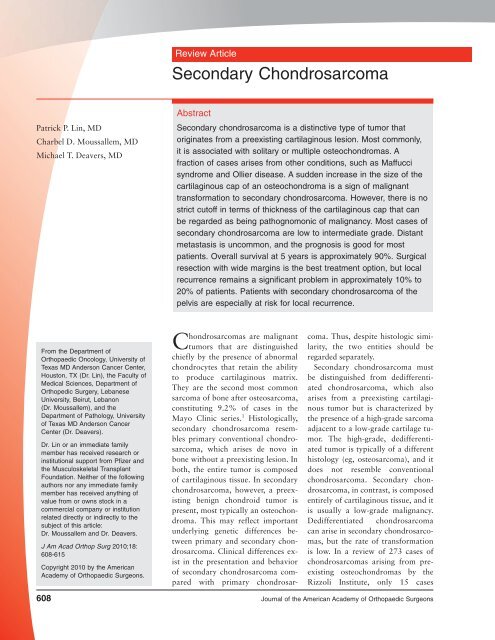
Review Article<br />
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Patrick P. Lin, MD<br />
Charbel D. Moussallem, MD<br />
Michael T. Deavers, MD<br />
Abstract<br />
<strong>Secondary</strong> chondrosarcoma is a distinctive type of tumor that<br />
originates from a preexisting cartilaginous lesion. Most commonly,<br />
it is associated with solitary or multiple osteochondromas. A<br />
fraction of cases arises from other conditions, such as Maffucci<br />
syndrome and Ollier disease. A sudden increase in the size of the<br />
cartilaginous cap of an osteochondroma is a sign of malignant<br />
transformation to secondary chondrosarcoma. However, there is no<br />
strict cutoff in terms of thickness of the cartilaginous cap that can<br />
be regarded as being pathognomonic of malignancy. Most cases of<br />
secondary chondrosarcoma are low to intermediate grade. Distant<br />
metastasis is uncommon, and the prognosis is good for most<br />
patients. Overall survival at 5 years is approximately 90%. Surgical<br />
resection with wide margins is the best treatment option, but local<br />
recurrence remains a significant problem in approximately 10% to<br />
20% of patients. Patients with secondary chondrosarcoma of the<br />
pelvis are especially at risk for local recurrence.<br />
From the Department of<br />
Orthopaedic Oncology, University of<br />
Texas MD Anderson Cancer Center,<br />
Houston, TX (Dr. Lin), the Faculty of<br />
Medical Sciences, Department of<br />
Orthopedic Surgery, Lebanese<br />
University, Beirut, Lebanon<br />
(Dr. Moussallem), and the<br />
Department of Pathology, University<br />
of Texas MD Anderson Cancer<br />
Center (Dr. Deavers).<br />
Dr. Lin or an immediate family<br />
member has received research or<br />
institutional support from Pfizer and<br />
the Musculoskeletal Transplant<br />
Foundation. Neither of the following<br />
authors nor any immediate family<br />
member has received anything of<br />
value from or owns stock in a<br />
commercial company or institution<br />
related directly or indirectly to the<br />
subject of this article:<br />
Dr. Moussallem and Dr. Deavers.<br />
J Am Acad Orthop Surg 2010;18:<br />
608-615<br />
Copyright 2010 by the American<br />
Academy of Orthopaedic Surgeons.<br />
<strong>Chondrosarcoma</strong>s are malignant<br />
tumors that are distinguished<br />
chiefly by the presence of abnormal<br />
chondrocytes that retain the ability<br />
to produce cartilaginous matrix.<br />
They are the second most common<br />
sarcoma of bone after osteosarcoma,<br />
constituting 9.2% of cases in the<br />
Mayo Clinic series. 1 Histologically,<br />
secondary chondrosarcoma resembles<br />
primary conventional chondrosarcoma,<br />
which arises de novo in<br />
bone without a preexisting lesion. In<br />
both, the entire tumor is composed<br />
of cartilaginous tissue. In secondary<br />
chondrosarcoma, however, a preexisting<br />
benign chondroid tumor is<br />
present, most typically an osteochondroma.<br />
This may reflect important<br />
underlying genetic differences between<br />
primary and secondary chondrosarcoma.<br />
Clinical differences exist<br />
in the presentation and behavior<br />
of secondary chondrosarcoma compared<br />
with primary chondrosarcoma.<br />
Thus, despite histologic similarity,<br />
the two entities should be<br />
regarded separately.<br />
<strong>Secondary</strong> chondrosarcoma must<br />
be distinguished from dedifferentiated<br />
chondrosarcoma, which also<br />
arises from a preexisting cartilaginous<br />
tumor but is characterized by<br />
the presence of a high-grade sarcoma<br />
adjacent to a low-grade cartilage tumor.<br />
The high-grade, dedifferentiated<br />
tumor is typically of a different<br />
histology (eg, osteosarcoma), and it<br />
does not resemble conventional<br />
chondrosarcoma. <strong>Secondary</strong> chondrosarcoma,<br />
in contrast, is composed<br />
entirely of cartilaginous tissue, and it<br />
is usually a low-grade malignancy.<br />
Dedifferentiated chondrosarcoma<br />
can arise in secondary chondrosarcomas,<br />
but the rate of transformation<br />
is low. In a review of 273 cases of<br />
chondrosarcomas arising from preexisting<br />
osteochondromas by the<br />
Rizzoli Institute, only 15 cases<br />
608 Journal of the American Academy of Orthopaedic Surgeons
Patrick P. Lin, MD, et al<br />
Table 1<br />
Major Series on <strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Study<br />
No. of<br />
Cases<br />
Preexisting<br />
Lesion (No.)<br />
Grade 14<br />
(No. of Cases)<br />
52 Solitary OC (21), HME (4),<br />
Coley and<br />
N/A<br />
Higinbotham 6 enchondroma (23), Ollier<br />
disease (4)<br />
Garrison et al 7 75 Solitary OC (40), HME (35) 1 (64), 2 (10), 3 (1)<br />
Hudson et al 8 15 Solitary OC (12), HME (3) 1 (11), 2 (3), 3 (1)<br />
Sun et al 12 5 Maffucci syndrome (all) 1 (1), 2 (3), N/A (1)<br />
Liuetal 9 12 Ollier disease (all) 1 (10), 2 (2)<br />
Merchan et al 10 4 HME (all) 1 (4)<br />
Wuisman<br />
45 Solitary OC (16), HME (29) 1 (30), 2 (13), 3 (2)<br />
et al 13<br />
Schaison<br />
29 Solitary OC (17), Ollier<br />
1(9),2(18),N/A(2)<br />
et al 11 disease (12)<br />
Ahmed et al 4 107 Solitary OC (61), HME (46) 1 (97), 2 (10)<br />
Altayetal 5 32 Solitary OC (14), HME (10), enchondroma<br />
(6), Ollier disease<br />
(1), Maffucci syndrome (1)<br />
1(28),2(4)<br />
HME = hereditary multiple exostosis, N/A = not available, OC = osteochondroma<br />
Table 2<br />
Risk Factors for <strong>Secondary</strong><br />
<strong>Chondrosarcoma</strong><br />
Clinical<br />
Pain<br />
Increasing size of a palpable lesion<br />
Male predominance (2:1)<br />
Location in the pelvis or hip<br />
Peak age in mid 30s<br />
Radiographic<br />
Surface irregularity<br />
Blurriness of the border<br />
Osteochondroma >5 cm<br />
Increase in size of osteochondroma<br />
Cartilage cap >2 cm<br />
Inhomogeneous mineralization of large<br />
cartilage cap<br />
Genetic<br />
Hereditary multiple exostosis (EXT1,<br />
EXT2, EXT3 mutations)<br />
Ollier disease<br />
Maffucci syndrome<br />
(5.5%) underwent dedifferentiation. 2<br />
Most cases of dedifferentiated chondrosarcomas<br />
appear to originate<br />
from central primary chondrosarcoma;<br />
it is estimated that the fraction<br />
of primary chondrosarcomas undergoing<br />
dedifferentiation may be as<br />
high as 15.4%. 3 In most cases, the<br />
prognosis of patients with dedifferentiated<br />
chondrosarcoma is dismal,<br />
which is quite unlike the prognosis<br />
of patients with secondary chondrosarcoma.<br />
<strong>Secondary</strong> chondrosarcoma is a<br />
well-recognized clinical diagnosis.<br />
However, relatively little has been<br />
published on the subject, perhaps as<br />
a result of the rarity of the condition.<br />
In a review of the literature, we<br />
found only 10 studies pertaining directly<br />
to the subject that were not<br />
case reports (Table 1).<br />
Clinical Presentation<br />
The most frequent presenting complaints<br />
with secondary chondrosarcoma<br />
are a palpable mass and pain.<br />
In many cases, the signs and symptoms<br />
are subtle, and the complaints<br />
are not severe. Large masses in the<br />
pelvis and thigh are easily hidden<br />
from patient and clinician alike. New<br />
onset of pain in a preexisting osteochondroma<br />
should alert the physician<br />
to the possibility of enlargement<br />
of the cartilaginous cap. Rarely,<br />
some tumors in the pelvis may cause<br />
urinary and bowel irregularities.<br />
A male predilection for secondary<br />
chondrosarcoma seems to be evident.<br />
Based on combined data from the<br />
published series, 63% of patients<br />
with the disease are male and 37%<br />
are female, resulting in a male:female<br />
ratio of approximately 2:1. 4-13 The<br />
mean age of persons with secondary<br />
chondrosarcoma is 34 years, which<br />
is notably younger than the average<br />
age of persons with primary conventional<br />
chondrosarcoma. 4-13 The most<br />
common site of involvement is the<br />
pelvis, followed by the proximal femur.<br />
The scapula and proximal humerus<br />
are also relatively common<br />
sites. Clinical, radiographic, and genetic<br />
features associated with secondary<br />
chondrosarcomas are summarized<br />
in Table 2.<br />
Our review of the major published<br />
series indicates that the great majority<br />
of cases arise in osteochondromas<br />
(88%), with solitary osteochondroma<br />
being slightly more common<br />
than multiple osteochondromas (ie,<br />
hereditary multiple exostosis). 4-7,11,13<br />
<strong>Secondary</strong> chondrosarcoma can also<br />
occur in persons with Ollier disease<br />
(ie, multiple enchondromas) and<br />
Maffucci syndrome (ie, multiple enchondromas<br />
associated with softtissue<br />
hemangiomas). Other benign<br />
cartilaginous lesions that have been<br />
reported, although rarely to result in<br />
secondary chondrosarcoma include<br />
solitary enchondroma, synovial<br />
chondromatosis, and chondromyxoid<br />
fibroma. 6,15-20 These lesions have<br />
been noted mostly in case reports,<br />
and there may be some question<br />
whether some cases were malignant<br />
at the outset. 6,15-20<br />
October 2010, Vol 18, No 10 609
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Figure 1<br />
<strong>Secondary</strong> chondrosarcoma arising from a pelvic osteochondroma. A, Preoperative AP pelvic radiograph<br />
demonstrating a large calcified tumor arising from the iliac wing. The surfaces of the calcified areas are indistinct and<br />
not well-delineated. B, Postoperative AP pelvic radiograph following wide excision of the tumor. C, Photograph of the<br />
cut specimen after resection demonstrating a thick layer of white, glistening hyaline cartilage. The central area shows a<br />
small area of ossified bone (arrow), which represents the stalk of the preexisting osteochondroma. D, T1-weighted<br />
axial magnetic resonance image demonstrating fatty marrow in the central portion of the sessile stalk emanating from<br />
the iliac crest, indicating the presence of an ossified central portion of the original osteochondroma. E, T2-weighted<br />
axial magnetic resonance image demonstrating the thick layer of cartilaginous tumor surrounding the central ossified<br />
stalk, which appears dark. F, Gadolinium-enhanced fat-saturated T1-weighted magnetic resonance image showing a<br />
subtle speckled pattern of enhancement within the tumor.<br />
Radiologic Features<br />
Conventional radiography may offer<br />
important clues regarding the diagnosis<br />
of secondary chondrosarcoma.<br />
Osteochondromas have well-defined<br />
bony edges, including the subchondral<br />
bone of the cartilaginous cap. In<br />
contrast, secondary chondrosarcomas<br />
demonstrate irregularity or blurriness<br />
of the surface of the osteochondroma<br />
(Figure 1). A soft-tissue<br />
mass outside the osseous portion of<br />
the osteochondroma may be subtly<br />
appreciable, and this mass may exhibit<br />
scattered foci of calcification. 4,5<br />
CT and MRI are important in<br />
demonstrating the malignant features<br />
of the tumor. Most critically,<br />
they reveal an abnormally large cartilaginous<br />
cap on the osteochondroma<br />
(Figure 1, D through F). The<br />
portion of the osteochondroma that<br />
becomes malignant is the cartilaginous<br />
tissue that forms the cap of the<br />
lesion. The osseous tissue that makes<br />
up the base or stalk is not thought to<br />
610 Journal of the American Academy of Orthopaedic Surgeons
Patrick P. Lin, MD, et al<br />
undergo malignant transformation.<br />
Plain radiography may not demonstrate<br />
the cartilage cap as well as either<br />
CT or MRI do, which may lead<br />
the unwary clinician to underestimate<br />
the true size of the cap.<br />
Osteochondromas may have the<br />
appearance of an enlarged cartilage<br />
cap on T2-weighted magnetic resonance<br />
images when there is a large<br />
bursa around the cap. The fluid<br />
within the bursa appears similar to<br />
that of cartilage tissue because both<br />
entities have high water content.<br />
Gadolinium contrast is used to distinguish<br />
bursal structures from true<br />
cartilage tissue. The bursas have only<br />
rim enhancement of the bursal tissue<br />
without contrast enhancement of the<br />
fluid inside the bursa.<br />
Many clinicians believe that a cartilage<br />
cap with a thickness of 2 cm seems to be<br />
strong evidence for the presence of<br />
secondary chondrosarcoma.<br />
Some authors have stressed the importance<br />
of the character of the cartilage<br />
cap in addition to its absolute<br />
size. Ahmed et al 4 stated that “a<br />
qualitative assessment of the cartilaginous<br />
cap was more helpful than a<br />
precise measurement of cap thickness.”<br />
Irregularity of the surface of<br />
the cartilage cap correlated with the<br />
fuzzy appearance of the lesions on<br />
radiographs; this irregularity may reflect<br />
an increased invasive nature of<br />
the lesion.<br />
Pathology<br />
The diagnosis of secondary chondrosarcoma<br />
is confirmed by histologic<br />
examination of biopsy samples. Like<br />
conventional chondrosarcoma, secondary<br />
chondrosarcoma is not always<br />
easy to diagnose, and the histologic<br />
features alone may not be<br />
sufficient to determine that a lesion<br />
has become malignant. Most secondary<br />
chondrosarcomas are low grade.<br />
The overlap in appearance between<br />
benign lesions and low-grade cartilage<br />
tumors has led to a high rate of<br />
inter- and intraobserver variability in<br />
diagnosis. 24 Critical information<br />
from the clinical history and imaging<br />
studies must be correlated with the<br />
pathologic data to render the correct<br />
diagnosis.<br />
On the pathology slides, sarcomatous<br />
transformation is usually identified<br />
by the presence of malignant<br />
chondroid tissue. Hallmarks include<br />
hypercellularity, binucleate cells,<br />
multiple cells in lacunae, atypical nuclei,<br />
and myxoid changes in the hyaline<br />
cartilage matrix (Figure 2).<br />
Thickening of the cartilage cap can<br />
be observed grossly. 23<br />
A few abnormal features may<br />
make it difficult to distinguish the<br />
cartilage of osteochondromas from<br />
low-grade chondrosarcomas on the<br />
basis of histologic findings alone,<br />
even for experienced pathologists. 25,26<br />
There may be mild nuclear atypia,<br />
slight hypercellularity, and occasional<br />
binucleate cells. In these cases,<br />
the radiographic and clinical findings<br />
are important. 27 A lesion with a thin<br />
cartilage cap that has not grown or<br />
changed for years is unlikely to have<br />
transformed into a malignant tumor.<br />
Conversely, sudden growth in a cap<br />
with marked enlargement of the cap<br />
strongly suggests the presence of<br />
chondrosarcoma, even when the histologic<br />
findings show minimal abnormalities<br />
that would be compatible<br />
only with a diagnosis of grade 1<br />
chondrosarcoma (low grade).<br />
An important feature consistent<br />
with malignancy is permeative infiltration<br />
of soft tissues and the presence<br />
of discrete nodules of cartilage<br />
in the soft tissues separated from the<br />
main tumor mass. In one study, 57%<br />
of all cases of secondary chondrosarcoma<br />
showed histologic evidence of<br />
such permeative changes on the pathology<br />
slides. 4 Medullary extension<br />
of cartilaginous tumor into bone also<br />
demonstrates invasive and malignant<br />
behavior. This may be found in up to<br />
one third of cases, and it tends to be<br />
more common in broad-based osteochondromas.<br />
13<br />
The grading of secondary chondrosarcomas<br />
is similar to that of primary<br />
chondrosarcomas and includes<br />
grade 1, low; grade 2, intermediate;<br />
and grade 3, high. 14,28 In general, increasing<br />
grade is associated with<br />
greater cellularity, number of binucleate<br />
cells, and mitoses.<br />
Most secondary chondrosarcomas<br />
are grade 1 or 2 lesions. In the pub-<br />
October 2010, Vol 18, No 10 611
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
lished data of the large series that we<br />
reviewed, more than three fourths of<br />
the cases were grade 1 tumors, and<br />
nearly all of the remaining lesions<br />
were grade 2. 4,5,7,11,13 Only 1% of<br />
cases were reported to be grade 3.<br />
Figure 2<br />
Genetics and Mutations<br />
Histologic comparison of osteochondroma and secondary chondrosarcoma.<br />
A, Cartilaginous tissue of an osteochondroma demonstrating features that<br />
recapitulate the hyaline cartilage of articular surfaces. Note the gradual<br />
enlargement of cells as they near the subchondral bone and become<br />
hypertrophic. Most cells reside in solitary lacunae, with occasional lacunae<br />
having two cells (arrowhead). The cells are relatively sparse in the abundant<br />
extracellular matrix (hematoxylin-eosin, original magnification ×40). B, Grade<br />
2 secondary chondrosarcoma demonstrating greater cellularity and less<br />
discernible organization of the chondrocytes. Lacunae with multiple cells are<br />
more common. Because cells retract from the walls of the lacunae during the<br />
fixation process, pleomorphism of cells is not easy to identify (hematoxylineosin,<br />
original magnification ×20). C, Osteochondroma under high-power<br />
magnification demonstrating cells that are fairly well-spaced in their lacunae.<br />
Slight atypia may be visible, making the distinction between benign lesions<br />
and low-grade chondrosarcoma difficult on the basis of histology alone.<br />
Certain lacunae contain two cells (hematoxylin-eosin, original magnification<br />
×400). D, Grade 1 secondary chondrosarcoma under high-power<br />
magnification demonstrating atypical features, such as the binucleate cell in<br />
the center of the field. No significant nuclear pleomorphism is present<br />
(hematoxylin-eosin, original magnification ×400).<br />
Hereditary multiple exostosis<br />
(HME), also referred to as multiple<br />
hereditary exostosis and hereditary<br />
multiple osteochondromatosis, is a<br />
rare familial disease characterized by<br />
multiple osteochondromas throughout<br />
the skeleton. The disease is inherited<br />
as an autosomal dominant condition<br />
with high penetrance. Three<br />
related genes have been implicated in<br />
the disorder, EXT1, EXT2, and<br />
EXT3, which are located on 8q24,<br />
11p13, and 19p, respectively. 29-31<br />
EXT1 and EXT2 mutations are<br />
more common and make up most<br />
cases. 32 Patients with EXT1 mutation<br />
tend to have more severe phenotypes<br />
than do patients with EXT2<br />
mutation. 32 It is not clear how the<br />
EXT genes are related to the pathophysiology<br />
of osteochondromas.<br />
Mutation of the genes usually results<br />
in truncated forms of the proteins,<br />
which are needed for the synthesis of<br />
heparan sulfate. This may secondarily<br />
impair diffusion of cellsignaling<br />
molecules. 33<br />
A genetic model for cartilaginous<br />
tumorigenesis in the setting of HME<br />
has been proposed. 34 First, inactivation<br />
of both copies of the EXT1 gene<br />
in cartilage cells is essential for the<br />
formation of osteochondroma. This<br />
typically occurs via loss of heterozygosity<br />
in sporadic cells. Cells that<br />
maintain one normal copy of the<br />
gene are apparently normal. Of note,<br />
it appears that solitary osteochondromas<br />
also develop as a result of<br />
mutation of both copies of an EXT<br />
gene, the difference being that this<br />
occurs in isolated cells and no germline<br />
mutation is inherited. Without<br />
further mutations in other genes, the<br />
lesion remains benign; most osteochondromas<br />
remain in this state and<br />
do not progress further. One or more<br />
additional mutations in other genes<br />
612 Journal of the American Academy of Orthopaedic Surgeons
is required for secondary chondrosarcomas<br />
to arise within the benign<br />
cartilaginous origin. This process is<br />
sometimes accompanied by chromosomal<br />
instability and aneuploidy, the<br />
severity of which may depend on the<br />
particular genes that are mutated.<br />
These have not been well characterized.<br />
Most secondary chondrosarcomas<br />
arise in osteochondromas; thus, it<br />
seems as though the model of tumorigenesis<br />
starting with mutation of<br />
EXT genes would apply to most of<br />
the tumors. However, this may not<br />
account for all secondary chondrosarcomas,<br />
and the genetic pathway<br />
may well be distinct in chondrosarcomas<br />
that arise in enchondromas.<br />
Ollier disease and Maffucci syndrome<br />
are characterized by multiple<br />
enchondromas dispersed through the<br />
skeleton. Maffucci syndrome is distinguished<br />
from Ollier disease by the<br />
presence of multiple soft-tissue hemangiomas,<br />
and it is less common<br />
than Ollier disease. Both diseases are<br />
known to give rise to secondary<br />
chondrosarcoma, but because of the<br />
rarity of the conditions, the rate at<br />
which malignant transformation occurs<br />
is not well-documented. Estimates<br />
range from 10% to 40% in<br />
patients with Ollier disease at longterm<br />
follow-up. 9,11,35 Some authors<br />
believe that patients with Maffucci<br />
syndrome may be at greater risk of<br />
developing malignancy; in one series,<br />
4 of 7 patients with Maffucci syndrome<br />
developed chondrosarcoma. 35<br />
However, reviews of published case<br />
reports have indicated estimates approximately<br />
15% to 20%. 12,36<br />
The genetics of Ollier disease and<br />
Maffucci syndrome differ from those<br />
of HME. Both diseases seem to arise<br />
sporadically without an obvious genetic<br />
inheritance pattern. It is believed<br />
that a combination of multiple<br />
genes may be involved, but those<br />
have not been identified. One report<br />
identified two cases of a mutation<br />
(one somatic, one germline) in the<br />
gene encoding the PTH/PTHrP type I<br />
receptor. 37 It was hypothesized that<br />
the mutation could delay the differentiation<br />
of proliferating chondrocytes<br />
by constitutively activating<br />
hedgehog signaling. However, this<br />
mutation was not found consistently<br />
in other tumors upon further study. 38<br />
Prevention, Treatment,<br />
and Outcome<br />
The risk of malignant transformation<br />
of benign cartilage tumors has not been<br />
well established, and estimates vary<br />
widely. For solitary osteochondromas,<br />
the risk is most likely 5-year<br />
follow-up. 5,7,13 Patients with solitary<br />
osteochondromas tend to have a better<br />
overall prognosis, with a 5-year<br />
mortality rate of 6.5%, compared<br />
with 19.6% for patients with HME. 7<br />
Metastasis may be more apt to occur<br />
in the rare high-grade secondary<br />
chondrosarcoma. 7<br />
October 2010, Vol 18, No 10 613
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Local recurrence is a significant<br />
problem for patients with secondary<br />
chondrosarcoma, and this may affect<br />
10% to 20% of patients. 4,5,13 Local<br />
control of disease is particularly important<br />
for patients with pelvic and<br />
centrally located disease. In one series,<br />
more deaths occurred from local<br />
recurrence than from distant metastasis.<br />
4 The ramifications of local recurrence<br />
on the patient’s chances for<br />
survival should not be underestimated.<br />
Local recurrence of conventional,<br />
primary low-grade chondrosarcoma<br />
has been associated with<br />
decreased survival, increased metastasis,<br />
and increased grade of tumor.<br />
44,45 Thus, an oncologically<br />
sound operation for the primary tumor<br />
with wide surgical margins is of<br />
critical importance to maximize the<br />
chances for long-term patient survival.<br />
Summary<br />
<strong>Secondary</strong> chondrosarcoma is an uncommon<br />
tumor that arises from a<br />
benign cartilaginous lesion. The tumor<br />
frequently develops in the context<br />
of a syndrome that produces<br />
multiple cartilaginous tumors, including<br />
HME, Ollier disease, and<br />
Maffucci syndrome. It appears most<br />
commonly in the pelvis and proximal<br />
femur. Several signs may alert the clinician<br />
to the possibility of malignant<br />
transformation, such as new onset of<br />
pain, sudden growth of a lesion, and<br />
radiographic changes.<br />
The size of the cartilage cap of an<br />
osteochondroma is important. MRI<br />
with gadolinium contrast may help<br />
define the thickness of the cap. Although<br />
no demarcation in size of the<br />
cap can be considered diagnostic of<br />
malignant transformation, a cap<br />
thickness of >1 cm is worrisome,<br />
particularly when there is documented<br />
growth of the cap.<br />
The overall prognosis for patients<br />
is good. Most tumors are low grade,<br />
and distant metastasis is uncommon.<br />
<strong>Secondary</strong> chondrosarcomas must be<br />
distinguished from dedifferentiated<br />
chondrosarcomas, which are very<br />
aggressive, high-grade tumors with a<br />
poor prognosis. The management of<br />
secondary chondrosarcoma relies<br />
chiefly on wide surgical excision. Inadequate<br />
surgical resection can lead<br />
to uncontrollable local recurrence,<br />
which is perhaps as likely a cause of<br />
demise as distant metastasis.<br />
References<br />
Evidence-based Medicine: Levels of<br />
evidence are described in the table of<br />
contents. In this article, references<br />
23, 30, 31, 33, 34, 37, and 38 are<br />
level III studies. References 2-18, 27-<br />
29, 32, 35, 39-42, 44, and 45 are<br />
level IV studies. References 1, 19-21,<br />
24-26, 36, and 43 are level V expert<br />
opinion.<br />
Citation numbers printed in bold<br />
type indicate references published<br />
within the past 5 years.<br />
1. Unni KK: <strong>Chondrosarcoma</strong> (primary,<br />
secondary, dedifferentiated, and clear<br />
cell), in Dahlin’s Bone Tumors: General<br />
Aspects and Data on 11,087 Cases, ed5.<br />
Philadelphia, PA, Lippincott-Raven,<br />
1996, pp 71-108.<br />
2. Staals EL, Bacchini P, Mercuri M,<br />
Bertoni F: Dedifferentiated<br />
chondrosarcomas arising in preexisting<br />
osteochondromas. J Bone Joint Surg Am<br />
2007;89(5):987-993.<br />
3. Staals EL, Bacchini P, Bertoni F:<br />
Dedifferentiated central<br />
chondrosarcoma. Cancer 2006;106(12):<br />
2682-2691.<br />
4. Ahmed AR, Tan TS, Unni KK, Collins<br />
MS, Wenger DE, Sim FH: <strong>Secondary</strong><br />
chondrosarcoma in osteochondroma:<br />
Report of 107 patients. Clin Orthop<br />
Relat Res 2003;411:193-206.<br />
5. Altay M, Bayrakci K, Yildiz Y, Erekul S,<br />
Saglik Y: <strong>Secondary</strong> chondrosarcoma in<br />
cartilage bone tumors: Report of 32<br />
patients. J Orthop Sci 2007;12(5):415-<br />
423.<br />
6. Coley BL, Higinbotham NL: <strong>Secondary</strong><br />
chondrosarcoma. Ann Surg 1954;139(5):<br />
547-559.<br />
7. Garrison RC, Unni KK, McLeod RA,<br />
Pritchard DJ, Dahlin DC: <strong>Chondrosarcoma</strong><br />
arising in osteochondroma.<br />
Cancer 1982;49(9):1890-1897.<br />
8. Hudson TM, Springfield DS, Spanier SS,<br />
Enneking WF, Hamlin DJ: Benign<br />
exostoses and exostotic chondrosarcomas:<br />
Evaluation of cartilage<br />
thickness by CT. Radiology 1984;152(3):<br />
595-599.<br />
9. Liu J, Hudkins PG, Swee RG, Unni KK:<br />
Bone sarcomas associated with Ollier’s<br />
disease. Cancer 1987;59(7):1376-1385.<br />
10. Merchan EC, Sanchez-Herrera S,<br />
Gonzalez JM: <strong>Secondary</strong> chondrosarcoma:<br />
Four cases and review of the<br />
literature. Acta Orthop Belg 1993;59(1):<br />
76-80.<br />
11. Schaison F, Anract P, Coste F, De<br />
Pinieux G, Forest M, Tomeno B:<br />
<strong>Chondrosarcoma</strong> secondary to multiple<br />
cartilage diseases: Study of 29 clinical<br />
cases and review of the literature<br />
[French]. Rev Chir Orthop Reparatrice<br />
Appar Mot 1999;85(8):834-845.<br />
12. Sun TC, Swee RG, Shives TC, Unni KK:<br />
<strong>Chondrosarcoma</strong> in Maffucci’s<br />
syndrome. J Bone Joint Surg Am 1985;<br />
67(8):1214-1219.<br />
13. Wuisman PI, Jutte PC, Ozaki T:<br />
<strong>Secondary</strong> chondrosarcoma in<br />
osteochondromas: Medullary extension<br />
in 15 of 45 cases. Acta Orthop Scand<br />
1997;68(4):396-400.<br />
14. Evans HL, Ayala AG, Romsdahl MM:<br />
Prognostic factors in chondrosarcoma of<br />
bone: A clinicopathologic analysis with<br />
emphasis on histologic grading. Cancer<br />
1977;40(2):818-831.<br />
15. Atalar H, Başarir K, Uraş I, Yildiz Y,<br />
Erekul S, Sağlik Y: Chondromyxoid<br />
fibroma: An evaluation of 11 patients<br />
[Turkish]. Acta Orthop Traumatol Turc<br />
2007;41(1):31-35.<br />
16. Müller PE, Dürr HR, Nerlich A,<br />
Pellengahr C, Maier M, Jansson V:<br />
Malignant transformation of a benign<br />
enchondroma of the hand to secondary<br />
chondrosarcoma with isolated<br />
pulmonary metastasis. Acta Chir Belg<br />
2004;104(3):341-344.<br />
17. Peiper M, Zornig C: <strong>Chondrosarcoma</strong> of<br />
the thumb arising from a solitary<br />
enchondroma. Arch Orthop Trauma<br />
Surg 1997;116(4):246-248.<br />
18. Springfield DS, Gebhardt MC, McGuire<br />
MH: <strong>Chondrosarcoma</strong>: A review. Instr<br />
Course Lect 1996;45:417-424.<br />
19. Sah AP, Geller DS, Mankin HJ, et al:<br />
Malignant transformation of synovial<br />
chondromatosis of the shoulder to<br />
chondrosarcoma: A case report. J Bone<br />
Joint Surg Am 2007;89(6):1321-1328.<br />
20. Bertoni F, Bacchini P, Hogendoorn PC:<br />
614 Journal of the American Academy of Orthopaedic Surgeons
Patrick P. Lin, MD, et al<br />
<strong>Chondrosarcoma</strong>, in Fletcher CDM,<br />
Unni KK, Mertens F, eds: World Health<br />
Organization Classification of Tumours:<br />
Pathology & Genetics: Tumours of Soft<br />
Tissue and Bone. Lyon, France, IARC<br />
Press, 2002, pp 247-251.<br />
21. Huvos AG: Solitary and multiple<br />
osteochondromas and enchondromas,<br />
juxtacortical chondroma, Mafucci’s<br />
disease, in Huvos AG, ed: Bone Tumors:<br />
Diagnosis, Treatment and Prognosis.<br />
Philadelphia, PA, WB Saunders<br />
Company, 1991, pp 253-294.<br />
22. Spjut HJ, Dorfman HD, Fechner RE,<br />
Ackerman LV: Tumors of cartilaginous<br />
origin, in Firminger HI, ed: Atlas of<br />
Tumor Pathology, Second Series, Fascicle<br />
5: Tumors of Bone and Cartilage.<br />
Washington, DC, Armed Forces Institute<br />
of Pathology, 1971, pp 33-116.<br />
23. Forest M: Osteochondroma, in Forest<br />
M, Tomeno B, Vanel D, eds: Orthopedic<br />
Surgical Pathology: Diagnosis of Tumors<br />
and Pseudotumoral Lesions of Bone and<br />
Joints. Edinburgh, Scotland, Churchill<br />
Livingstone, 1998, pp 117-190.<br />
24. Eefting D, Schrage YM, Geirnaerdt MJ,<br />
et al: Assessment of interobserver<br />
variability and histologic parameters to<br />
improve reliability in classification and<br />
grading of central cartilaginous tumors.<br />
Am J Surg Pathol 2009;33(1):50-57.<br />
25. Flemming DJ, Murphey MD:<br />
Enchondroma and chondrosarcoma.<br />
Semin Musculoskelet Radiol 2000;4(1):<br />
59-71.<br />
26. Campanacci M: Multiple chondromas<br />
(chondromatosis, Ollier’s disease,<br />
Maffucci’s syndrome), in Campanacci<br />
M: Bone and Soft Tissue Tumors, ed2.<br />
New York, NY, Springer, 1999, pp 235-<br />
245.<br />
27. Mirra JM: The osteochondroma, solitary<br />
and multiple, in Mirra JM, ed: Bone<br />
Tumors: Diagnosis and Treatment.<br />
Philadelphia, PA, JB Lippincott, 1980,<br />
pp 520-532.<br />
28. O’Neal LW, Ackerman LV: <strong>Chondrosarcoma</strong><br />
of bone. Cancer 1952;5(3):551-<br />
577.<br />
29. Cook A, Raskind W, Blanton SH, et al:<br />
Genetic heterogeneity in families with<br />
hereditary multiple exostoses. Am J Hum<br />
Genet 1993;53(1):71-79.<br />
30. Wu YQ, Heutink P, de Vries BB, et al:<br />
Assignment of a second locus for<br />
multiple exostoses to the pericentromeric<br />
region of chromosome 11. Hum Mol<br />
Genet 1994;3(1):167-171.<br />
31. Le Merrer M, Legeai-Mallet L, Jeannin<br />
PM, et al: A gene for hereditary multiple<br />
exostoses maps to chromosome 19p.<br />
Hum Mol Genet 1994;3(5):717-722.<br />
32. Porter DE, Lonie L, Fraser M, et al:<br />
Severity of disease and risk of malignant<br />
change in hereditary multiple exostoses:<br />
A genotype-phenotype study. J Bone<br />
Joint Surg Br 2004;86(7):1041-1046.<br />
33. Wuyts W, Van Hul W, De Boulle K,<br />
et al: Mutations in the EXT1 and EXT2<br />
genes in hereditary multiple exostoses.<br />
Am J Hum Genet 1998;62(2):346-354.<br />
34. Bovée JV, Cleton-Jansen AM, Wuyts W,<br />
et al: EXT-mutation analysis and loss of<br />
heterozygosity in sporadic and hereditary<br />
osteochondromas and secondary<br />
chondrosarcomas. Am J Hum Genet<br />
1999;65(3):689-698.<br />
35. Schwartz HS, Zimmerman NB, Simon<br />
MA, Wroble RR, Millar EA, Bonfiglio<br />
M: The malignant potential of<br />
enchondromatosis. J Bone Joint Surg Am<br />
1987;69(2):269-274.<br />
36. Lewis RJ, Ketcham AS: Maffucci’s<br />
syndrome: Functional and neoplastic<br />
significance. Case report and review of<br />
the literature. J Bone Joint Surg Am<br />
1973;55(7):1465-1479.<br />
37. Hopyan S, Gokgoz N, Poon R, et al: A<br />
mutant PTH/PTHrP type I receptor in<br />
enchondromatosis. Nat Genet 2002;<br />
30(3):306-310.<br />
38. Rozeman LB, Sangiorgi L, Briaire-de<br />
Bruijn IH, et al: Enchondromatosis<br />
(Ollier disease, Maffucci syndrome) is<br />
not caused by the PTHR1 mutation<br />
p.R150C. Hum Mutat 2004;24(6):466-<br />
473.<br />
39. Florez B, Mönckeberg J, Castillo G,<br />
Beguiristain J: Solitary osteochondroma<br />
long-term follow-up. J Pediatr Orthop B<br />
2008;17(2):91-94.<br />
40. Schmale GA, Conrad EU III, Raskind<br />
WH: The natural history of hereditary<br />
multiple exostoses. J Bone Joint Surg Am<br />
1994;76(7):986-992.<br />
41. Wicklund CL, Pauli RM, Johnston D,<br />
Hecht JT: Natural history study of<br />
hereditary multiple exostoses. Am J Med<br />
Genet 1995;55(1):43-46.<br />
42. Murphey MD, Choi JJ, Kransdorf MJ,<br />
Flemming DJ, Gannon FH: Imaging of<br />
osteochondroma: Variants and<br />
complications with radiologic-pathologic<br />
correlation. Radiographics 2000;20(5):<br />
1407-1434.<br />
43. Pierz KA, Womer RB, Dormans JP:<br />
Pediatric bone tumors: Osteosarcoma<br />
ewing’s sarcoma, and chondrosarcoma<br />
associated with multiple hereditary<br />
osteochondromatosis. J Pediatr Orthop<br />
2001;21(3):412-418.<br />
44. Schwab JH, Wenger D, Unni K, Sim FH:<br />
Does local recurrence impact survival in<br />
low-grade chondrosarcoma of the long<br />
bones? Clin Orthop Relat Res 2007;462:<br />
175-180.<br />
45. Weber KL, Pring ME, Sim FH:<br />
Treatment and outcome of recurrent<br />
pelvic chondrosarcoma. Clin Orthop<br />
Relat Res 2002;397:19-28.<br />
October 2010, Vol 18, No 10 615