Efficacy of nebulized epinephrine versus salbutamol in ... - sepeap
Efficacy of nebulized epinephrine versus salbutamol in ... - sepeap
Efficacy of nebulized epinephrine versus salbutamol in ... - sepeap
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Pediatric Pulmonology 31:284±288 (2001)<br />
Ef®cacy <strong>of</strong> Nebulized Ep<strong>in</strong>ephr<strong>in</strong>e Versus Salbutamol<br />
<strong>in</strong> Hospitalized Infants With Bronchiolitis<br />
Pablo Bertrand, MD, Hector AranõÂbar, MD, Edelmira Castro, NU, and Ignacio SaÂnchez, MD*<br />
Summary. We enrolled 30 <strong>in</strong>fants (median age 3 months, range 1±12 months), hospitalized for<br />
bronchiolitis <strong>in</strong> a randomized double-bl<strong>in</strong>d trial, to exam<strong>in</strong>e the ef®cacy and safety <strong>of</strong> <strong>nebulized</strong><br />
<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> compared to <strong>salbutamol</strong>. Once admitted, patients were treated with either <strong>nebulized</strong><br />
0.5 mg <strong>of</strong> an 0.1% <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> solution (0.5 mL <strong>in</strong> 3.5 mL normal sal<strong>in</strong>e (NS)) or 2.5 mg <strong>nebulized</strong><br />
<strong>salbutamol</strong> (0.5 mL <strong>in</strong> 3.5 mL NS). They were evaluated daily before and after nebulization until<br />
discharge. The outcome measures used were: basel<strong>in</strong>e cl<strong>in</strong>ical score (based on respiratory rate,<br />
subcostal retraction, presence <strong>of</strong> wheez<strong>in</strong>g, and O 2 requirement), change <strong>in</strong> cl<strong>in</strong>ical O 2 score after<br />
nebulization, duration <strong>of</strong> O 2 therapy, and duration <strong>of</strong> hospitalization.<br />
A signi®cant improvement <strong>in</strong> the cl<strong>in</strong>ical score was noted on the ®rst day <strong>of</strong> hospitalization <strong>in</strong><br />
subjects receiv<strong>in</strong>g <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> (P ˆ 0:025); that change was not seen <strong>in</strong> those on <strong>salbutamol</strong><br />
(P ˆ 0:6). Nebulized <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> decreased the basel<strong>in</strong>e cl<strong>in</strong>ical score faster than <strong>salbutamol</strong><br />
(P ˆ 0:02), though on the fourth study day there was no signi®cant difference between the two<br />
scores. On the fourth and ®fth days <strong>of</strong> study there were more patients hospitalized <strong>in</strong> the<br />
<strong>salbutamol</strong> group than <strong>in</strong> the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group (P ˆ 0:03 vs. P ˆ 0:025). No adverse effects<br />
were associated with <strong>nebulized</strong> therapy.<br />
We conclude that <strong>nebulized</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> is a more effective agent than <strong>salbutamol</strong> <strong>in</strong> the <strong>in</strong>itial<br />
treatment <strong>of</strong> bronchiolitis and is equally safe. Pediatr Pulmonol. 2001; 31:284±288.<br />
ß 2001 Wiley-Liss, Inc.<br />
Key words: bronchiolitis; wheez<strong>in</strong>g; bronchodilators; <strong>in</strong>fants; <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>; airway<br />
hyperresponsiveness; healthcare costs; respiratory syncytial virus.<br />
INTRODUCTION<br />
Bronchiolitis is the ma<strong>in</strong> cause <strong>of</strong> acute respiratory<br />
illness <strong>in</strong> <strong>in</strong>fants under 12 months <strong>of</strong> age, 1,2 and is one <strong>of</strong><br />
the lead<strong>in</strong>g causes <strong>of</strong> hospital admissions <strong>in</strong> this age group<br />
dur<strong>in</strong>g the w<strong>in</strong>ter season <strong>in</strong> the United States. 3 Therapy<br />
for bronchiolitis <strong>in</strong>cludes supportive measures such as<br />
adequate hydration, management <strong>of</strong> secretions, and supplementary<br />
oxygen. The use <strong>of</strong> bronchodilator therapy <strong>in</strong><br />
this disease rema<strong>in</strong>s controversial. Some studies have<br />
demonstrated modest cl<strong>in</strong>ical improvement 4±7 or an<br />
improvement <strong>in</strong> pulmonary function 8,9 with beta agonist<br />
therapy. Other studies have concluded that <strong>salbutamol</strong><br />
does not bene®t <strong>in</strong>fants. 10,11 Importantly, some studies<br />
implicate <strong>salbutamol</strong> as caus<strong>in</strong>g arterial oxygen desaturation<br />
<strong>in</strong> <strong>in</strong>fants with acute bronchiolitis. 12,13 Despite this,<br />
<strong>salbutamol</strong> is <strong>of</strong>ten the ®rst drug <strong>of</strong> choice for treatment<br />
<strong>of</strong> bronchiolitis <strong>in</strong> cl<strong>in</strong>ical practice and <strong>in</strong> emergency<br />
rooms.<br />
Wohl and Chernick 14 postulated that mucosal edema <strong>in</strong><br />
the bronchioles may be an important cause <strong>of</strong> airway<br />
obstruction <strong>in</strong> bronchiolitis, and therefore, an alpha/beta<br />
agonist might be useful <strong>in</strong> the treatment <strong>of</strong> this disease.<br />
There are published data <strong>in</strong>dicat<strong>in</strong>g that <strong>nebulized</strong> racemic<br />
<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> is bene®cial <strong>in</strong> patients with bronchiolitis<br />
ß 2001 Wiley-Liss, Inc.<br />
without caus<strong>in</strong>g adverse effects, and is more effective<br />
than placebo 15 or albuterol. 16,17 In our previous study, 16<br />
we compared only a s<strong>in</strong>gle dose <strong>of</strong> drug.<br />
The purpose <strong>of</strong> the present study was to compare the<br />
cl<strong>in</strong>ical ef®cacy <strong>of</strong> multiple doses <strong>of</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> vs.<br />
<strong>salbutamol</strong> <strong>in</strong> <strong>in</strong>fants hospitalized with acute bronchiolitis.<br />
METHODS<br />
From May 1, 1994 to September 30, 1994 (w<strong>in</strong>ter <strong>in</strong><br />
the Southern Hemisphere), 30 patients admitted to our<br />
hospital were enrolled <strong>in</strong> a prospective randomized<br />
double-bl<strong>in</strong>d study. The <strong>in</strong>clusion criteria for the diagnosis<br />
<strong>of</strong> bronchiolitis were <strong>in</strong>fants under 1 year <strong>of</strong> age,<br />
®rst wheez<strong>in</strong>g episode, acute onset <strong>of</strong> respiratory distress,<br />
and an x-ray study <strong>of</strong> the chest compatible with<br />
Department <strong>of</strong> Pediatrics, School <strong>of</strong> Medic<strong>in</strong>e, Catholic University <strong>of</strong><br />
Chile, Santiago, Chile.<br />
*Correspondence to: Ignacio SaÂnchez, M.D., Section <strong>of</strong> Pediatric<br />
Pulmonology, Department <strong>of</strong> Pediatrics, Catholic University <strong>of</strong> Chile, Lira<br />
40, Casilla 114-D, Santiago, Chile. E-mail: igsan@med.puc.cl<br />
Received 21 June 1999; Accepted 20 October 2000.
Ep<strong>in</strong>ephr<strong>in</strong>e vs. Salbutamol <strong>in</strong> Bronchiolitis 285<br />
TABLE 1ÐCl<strong>in</strong>ical Scor<strong>in</strong>g System, Adapted From Bierman and Pierson 13 as Modi®ed by<br />
Tal et al. 14 Respiratory rate (breaths/m<strong>in</strong>)<br />
Score 6 months Wheez<strong>in</strong>g Retractions O 2 supply (%)<br />
0 60 Audible <strong>in</strong>spiratory and ‡‡‡ >35<br />
expiratory<br />
bronchiolitis. Exclusion criteria were: prematurity, chronic<br />
lung or cardiac disease, lower respiratory tract <strong>in</strong>fection<br />
with<strong>in</strong> the previous 3 months, and bronchodilator or<br />
steroid therapy with<strong>in</strong> the previous month. The Catholic<br />
University Hospital Research Ethics Committee approved<br />
the study. Each parent gave <strong>in</strong>formed consent<br />
and signed authorization forms for the study.<br />
The patients were randomized <strong>in</strong> a double-bl<strong>in</strong>d protocol<br />
to receive either <strong>salbutamol</strong> (Aerol<strong>in</strong> 0.5%, Glaxo)<br />
0.5 mL (2.5 mg) plus sal<strong>in</strong>e solution (0.9%) 3.5 mL to<br />
make a total volume <strong>of</strong> 4 mL, or <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> (Adrenal<strong>in</strong>e<br />
1:1,000, Astra) 0.5 mL (0.5 mg) plus 3.5 mL <strong>of</strong> sal<strong>in</strong>e<br />
solution. Both solutions were prepared by the same nurse<br />
every day. Children received nebulization every 2±4 hr<br />
by face mask, us<strong>in</strong>g a Hudson updraft nebulizer driven at<br />
6±8 L/m<strong>in</strong> by cont<strong>in</strong>uous oxygen ¯ow. They received the<br />
study drug dur<strong>in</strong>g the entire hospital admission under<br />
the supervision <strong>of</strong> their own physician, who rema<strong>in</strong>ed<br />
bl<strong>in</strong>ded. Basel<strong>in</strong>e assessment was performed on the ®rst<br />
day <strong>of</strong> admission.<br />
The patients had a complete physical exam<strong>in</strong>ation performed<br />
daily by one <strong>of</strong> the two <strong>in</strong>vestigators (P.B., H.A.),<br />
who followed each patient dur<strong>in</strong>g the entire study period.<br />
Prior to the study, bl<strong>in</strong>ded pilot scor<strong>in</strong>g done by the same<br />
physicians showed excellent agreement <strong>in</strong> 10 <strong>in</strong>fants<br />
with acute bronchiolitis, with no difference greater than 1<br />
po<strong>in</strong>t. We found differences ma<strong>in</strong>ly <strong>in</strong> scor<strong>in</strong>g <strong>of</strong><br />
wheez<strong>in</strong>g and chest retractions. The score <strong>of</strong> Bierman and<br />
Pierson 18 as modi®ed by Tal et al. 19 was used (Table 1).<br />
This cl<strong>in</strong>ical scor<strong>in</strong>g system <strong>in</strong>cludes respiratory rate<br />
(modi®ed for age), wheez<strong>in</strong>g, use <strong>of</strong> accessory muscles,<br />
and presence <strong>of</strong> cyanosis (modi®ed by measur<strong>in</strong>g oxygen<br />
concentration needed to keep SaO 2 at 94±97%). The<br />
ABBREVIATIONS<br />
NS Normal sal<strong>in</strong>e<br />
O 2 Oxygen<br />
PICU Pediatric <strong>in</strong>tensive care unit<br />
RE Racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
RSV Respiratory syncytial virus<br />
SaO 2 Oxygen saturation<br />
WBC White blood cell<br />
score was done immediately before and with<strong>in</strong> 20 m<strong>in</strong><br />
after nebulizer treatment, with the subject be<strong>in</strong>g either<br />
quietly awake or asleep. Daily scor<strong>in</strong>g cont<strong>in</strong>ued until<br />
discharge from hospital. All <strong>in</strong>fants were tested for<br />
respiratory syncytial virus (RSV). The <strong>in</strong>fants' pediatricians<br />
followed their patients throughout the study period<br />
and could withdraw them from the study if they noticed<br />
any adverse reaction, poor response to treatment as de-<br />
®ned by an <strong>in</strong>crease <strong>in</strong> nebulization <strong>of</strong> greater than every<br />
2 hr, or admission to the pediatric <strong>in</strong>tensive care unit, or<br />
by parental request. The study was considered over when<br />
the <strong>in</strong>fants were weaned <strong>of</strong>f supplemental oxygen or had<br />
a cl<strong>in</strong>ical score below 4, whichever came ®rst. At this<br />
po<strong>in</strong>t, the patients were ready to be discharged, with<br />
<strong>salbutamol</strong> on a p.r.n. basis.<br />
The outcome measures used were: daily basel<strong>in</strong>e cl<strong>in</strong>ical<br />
score, oxygen saturation (SaO 2 ), change <strong>in</strong> score<br />
after nebulization, respiratory rate change, and duration<br />
<strong>of</strong> O 2 therapy and <strong>of</strong> hospitalization. Concomitant treatment<br />
<strong>in</strong> both groups <strong>in</strong>cluded oxygen supplementation,<br />
¯uids, and general care. Adverse effects were looked for<br />
<strong>in</strong> regards to tachycardia, tremor, and <strong>in</strong>crease <strong>in</strong> systolic<br />
or diastolic blood pressure after nebulization <strong>of</strong> each<br />
medication.<br />
Statistical analysis was performed us<strong>in</strong>g t-tests (twotailed)<br />
for quantitative variables, chi-square test for<br />
nom<strong>in</strong>al data, and log-rank test for actuarial analysis.<br />
Statistical signi®cance was de®ned as P < 0:05.<br />
RESULTS<br />
Patient Population<br />
Thirty-three <strong>in</strong>fants were eligible dur<strong>in</strong>g the study<br />
period. Three <strong>of</strong> them were excluded: two were on steroids,<br />
and the other withdrew because <strong>of</strong> parental request.<br />
Fourteen patients were randomized to the <strong>salbutamol</strong><br />
group, and 16 to the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group. There were 16<br />
male patients (53%). The mean age was 3.7 0.6 months<br />
<strong>in</strong> the <strong>salbutamol</strong> group and 3.9 0.4 months ( SEM)<br />
<strong>in</strong> the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group (P ˆ 0:64). There was no difference<br />
between groups <strong>in</strong> general basel<strong>in</strong>e characteristics<br />
(Table 2).
286 Bertrand et al.<br />
TABLE 2ÐCharacteristics <strong>of</strong> Patients on Admission<br />
Salbutamol Ep<strong>in</strong>ephr<strong>in</strong>e<br />
Variable (n ˆ 14) (n ˆ 16) P-value<br />
Males 7 (50%) 9 (56%) 0.73<br />
Age (months SEM) 3.7 0.6 3.9 0.4 0.64<br />
Age
Ep<strong>in</strong>ephr<strong>in</strong>e vs. Salbutamol <strong>in</strong> Bronchiolitis 287<br />
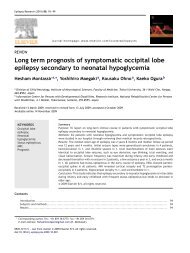
Fig. 1. Evolution <strong>of</strong> cl<strong>in</strong>ical score <strong>in</strong> both groups. Note that<br />
<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> produced a decrease <strong>in</strong> basal cl<strong>in</strong>ical score to less<br />
than 5 more rapidly than did <strong>salbutamol</strong> (log-rank test, P < 0:02).<br />
4.5 1.2; P ˆ 0.07). None <strong>of</strong> the patients had readmission<br />
<strong>in</strong> a 2-week period after discharge. In the<br />
<strong>salbutamol</strong> group, 3 patients had atelectasis, vs. none <strong>in</strong><br />
the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group.<br />
Adverse Effects<br />
Although use <strong>of</strong> <strong>salbutamol</strong> was associated with an<br />
<strong>in</strong>crease <strong>in</strong> heart rate on the second day which was<br />
statistically signi®cant (146 4 bpm vs. 153 2.9 bpm;<br />
P ˆ 0.02), this was not cl<strong>in</strong>ically relevant. Ep<strong>in</strong>ephr<strong>in</strong>e<br />
therapy was not associated with any adverse effects<br />
dur<strong>in</strong>g the study period.<br />
DISCUSSION<br />
Our data <strong>in</strong>dicate that <strong>nebulized</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> (as opposed<br />
to <strong>salbutamol</strong>) therapy improved cl<strong>in</strong>ical symptoms<br />
<strong>in</strong> <strong>in</strong>fants with bronchiolitis <strong>in</strong> several ways. First, <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
decreased the cl<strong>in</strong>ical score after nebulization<br />
dur<strong>in</strong>g the ®rst day follow<strong>in</strong>g admission. Secondly, <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
was associated with a more rapid improvement <strong>in</strong><br />
basel<strong>in</strong>e cl<strong>in</strong>ical score compared to <strong>salbutamol</strong>. This<br />
improvement was re¯ected <strong>in</strong> reduced hospitalization<br />
time <strong>in</strong> the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group.<br />
Reijonen et al. 17 studied patients <strong>in</strong> an early phase <strong>of</strong><br />
bronchiolitis and showed a signi®cant improvement <strong>in</strong><br />
heart rate and oxygen saturation but not <strong>in</strong> cl<strong>in</strong>ical score<br />
when racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> was used. In the emergency<br />
room, Menton et al. 23 us<strong>in</strong>g regular <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> showed<br />
greater improvement <strong>in</strong> heart rate and oxygen saturation<br />
compared to <strong>salbutamol</strong>, but they also did not ®nd any<br />
difference <strong>in</strong> cl<strong>in</strong>ical score. However, they observed a<br />
signi®cant decrease <strong>in</strong> the hospitalization rate <strong>in</strong> <strong>in</strong>fants<br />
treated with <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>. These two studies showed a<br />
bene®cial effect <strong>of</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> <strong>in</strong> the early stages <strong>of</strong><br />
bronchiolitis.<br />
Several studies have evaluated whether there is a<br />
bene®cial effect <strong>of</strong> bronchodilators <strong>in</strong> bronchiolitis. Two<br />
recent meta-analyses that addressed the ef®cacy <strong>of</strong> beta-2<br />
agonist <strong>in</strong> bronchiolitis showed a modest impact <strong>in</strong> the<br />
evolution <strong>of</strong> the disease. Flores and Horwitz 20 attributed<br />
the absence <strong>of</strong> evidence to the lack <strong>of</strong> well-designed<br />
<strong>in</strong>patient trials and to the fact that beta-2 agonists had a<br />
statistically signi®cant but cl<strong>in</strong>ically <strong>in</strong>signi®cant impact<br />
on SaO 2 and heart rate <strong>in</strong> outpatient trials. Similarly,<br />
Kellner et al. 21 showed a modest short-term improvement<br />
<strong>in</strong> cl<strong>in</strong>ical features, but not <strong>in</strong> length <strong>of</strong> hospitalization.<br />
There is recent evidence <strong>of</strong> a bene®cial effect <strong>of</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
compared to albuterol <strong>in</strong> the acute phase <strong>of</strong><br />
bronchiolitis. Recent cl<strong>in</strong>ical trials have shown <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
to be superior to placebo 15,22 and to <strong>salbutamol</strong>. 16,23<br />
SaÂnchez et al. 16 showed a signi®cant cl<strong>in</strong>ical change 30<br />
m<strong>in</strong> after nebulization and also a decrease <strong>in</strong> pulmonary<br />
resistance us<strong>in</strong>g racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>, but not with <strong>salbutamol</strong>.<br />
In the present study we obta<strong>in</strong>ed the same cl<strong>in</strong>ical<br />
change as assessed by a modi®ed Bierman and Pierson<br />
score <strong>in</strong> a similar age group <strong>of</strong> patients (< 12 months)<br />
and a similar cl<strong>in</strong>ical score (5.6 1), but we used regular<br />
<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> rather than racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>.<br />
We used <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> <strong>in</strong> our study because it is more<br />
readily available than racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> (RE) and less<br />
costly. RE conta<strong>in</strong>s an equal amount <strong>of</strong> d- and l-isomers<br />
<strong>of</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>, but the ma<strong>in</strong> pharmacologic activity is by<br />
the l-isomer (15 times more potent than the d-isomer,<br />
which has m<strong>in</strong>imal activity). 24 There is good evidence<br />
that <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> has similar ef®cacy to RE <strong>in</strong> the treatment<br />
<strong>of</strong> <strong>in</strong>fants with croup. 24 Our study would suggest<br />
that <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> is also ef®cacious <strong>in</strong> the treatment <strong>of</strong><br />
<strong>in</strong>fants with bronchiolitis. Mucosal edema <strong>in</strong> croup and<br />
bronchiolitis may be dim<strong>in</strong>ished by alpha receptor stimulation<br />
caus<strong>in</strong>g constriction <strong>of</strong> precapillary arterioles,<br />
thereby reduc<strong>in</strong>g microvascular leakage. 25<br />
After admission, 3 patients developed atelectasis <strong>in</strong> the<br />
<strong>salbutamol</strong> group, and none <strong>in</strong> the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group. We<br />
do not have a clear explanation for this phenomenon, but<br />
it could be related to the presence <strong>of</strong> more edema <strong>in</strong> the<br />
small airways <strong>in</strong> the <strong>salbutamol</strong> group.<br />
The statement that <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> would produce more<br />
undesirable cardiovascular effects than RE has not been<br />
proven. In one study 26 <strong>in</strong> patients with laryngotracheitis<br />
compar<strong>in</strong>g RE and <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>, there was no difference<br />
between groups <strong>in</strong> cardiovascular adverse reactions. This<br />
result is consistent with our ®nd<strong>in</strong>g and the reports <strong>of</strong><br />
other authors who looked for adverse effects us<strong>in</strong>g<br />
l-<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>. Based on previous studies with RE,<br />
Menton et al. 23 used the maximum equivalent dose <strong>of</strong><br />
l-<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> (3 mg), and reported no adverse effects.<br />
The presence <strong>of</strong> pallor <strong>in</strong> that study was not assessed. We<br />
did not ®nd any adverse effect us<strong>in</strong>g one-sixth <strong>of</strong> their<br />
dose <strong>of</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong>. We still do not know the ideal dose,<br />
but we believe that the dose <strong>of</strong> <strong>nebulized</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> has<br />
to be similar for each patient regardless <strong>of</strong> weight. (Note<br />
that the amount <strong>of</strong> drug that reaches the lungs is related to
288 Bertrand et al.<br />
tidal volume, and is thus corrected for weight.) Our<br />
prediction <strong>of</strong> the ideal dose is approximately 1 mg per<br />
nebulization, tak<strong>in</strong>g <strong>in</strong>to consideration previous reports <strong>in</strong><br />
patients with croup. 26,27<br />
This is the ®rst study which has shown a signi®cant<br />
decrease <strong>in</strong> cl<strong>in</strong>ical score severity dur<strong>in</strong>g <strong>in</strong>-hospital<br />
treatment <strong>in</strong> bronchiolitis patients treated with <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
vs. <strong>salbutamol</strong>. In our study, recovery from the disease<br />
(measured <strong>in</strong> comparison to basel<strong>in</strong>e cl<strong>in</strong>ical score) was<br />
more rapid <strong>in</strong> the <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> group compared to the<br />
<strong>salbutamol</strong> group. The importance <strong>of</strong> this is the potential<br />
bene®t <strong>of</strong> reduc<strong>in</strong>g healthcare costs by reduc<strong>in</strong>g hospitalization<br />
time, based on a better cl<strong>in</strong>ical basel<strong>in</strong>e score.<br />
The difference <strong>in</strong> hospitalized days between both groups<br />
was approximately one day (3.9 0.4 vs. 5.2 0.6).<br />
Although we did not ®nd a signi®cant difference <strong>in</strong> the<br />
average length <strong>of</strong> hospitalization compar<strong>in</strong>g both groups,<br />
we did ®nd a real difference on the fourth and ®fth days <strong>of</strong><br />
study <strong>in</strong> the number <strong>of</strong> patients still hospitalized. In the<br />
USA, One day <strong>of</strong> hospitalization costs around $500 per<br />
patient, and s<strong>in</strong>ce bronchiolitis results <strong>in</strong> over 54,000<br />
hospitalizations a year, this difference could mean a<br />
sav<strong>in</strong>g <strong>of</strong> $27 million a year.<br />
In summary, this study showed the greater ef®cacy <strong>of</strong><br />
l-<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> over <strong>salbutamol</strong> <strong>in</strong> treat<strong>in</strong>g bronchiolitis by<br />
improv<strong>in</strong>g cl<strong>in</strong>ical status after nebulization and by more<br />
rapidly decreas<strong>in</strong>g the basel<strong>in</strong>e cl<strong>in</strong>ical score on followup.<br />
S<strong>in</strong>ce we only recruited 30 patients, we could not<br />
demonstrate a difference <strong>in</strong> length <strong>of</strong> hospitalization and<br />
oxygen dependence time. Nebulized <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> was not<br />
associated with any adverse effects, and it should be<br />
considered as the drug <strong>of</strong> choice <strong>in</strong> the treatment <strong>of</strong> acute<br />
bronchiolitis because <strong>of</strong> its low cost and general<br />
availability. Considerable sav<strong>in</strong>gs <strong>in</strong> healthcare dollars<br />
may be an additional bene®t related to the use <strong>of</strong><br />
<strong>nebulized</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> for the treatment <strong>of</strong> bronchiolitis.<br />
ACKNOWLEDGMENTS<br />
The authors thank Dr. Victor Chernick for his critical<br />
review <strong>of</strong> the manuscript.<br />
REFERENCES<br />
1. Denny FW, Clyde WA Jr. Acute lower respiratory tract <strong>in</strong>fections<br />
<strong>in</strong> nonhospitalized children. J Pediatr 1986;108:635±646.<br />
2. Phelan PD, Ol<strong>in</strong>sky A, Robertson CF. Respiratory illness <strong>in</strong> children.<br />
Oxford, UK: Blackwell Scienti®c Publications; 1994. p 71±77.<br />
3. Institute <strong>of</strong> Medic<strong>in</strong>e. Appendix N: prospects for immuniz<strong>in</strong>g<br />
aga<strong>in</strong>st respiratory syncytial virus. In: New vacc<strong>in</strong>e development:<br />
establish<strong>in</strong>g priorities. Diseases <strong>of</strong> importance <strong>in</strong> United States.<br />
Wash<strong>in</strong>gton, DC: National Academy Press; 1985. p 397±409.<br />
4. Klassen TP, Rowe PC, Sutcliffe T, Ropp LJ, McDowell IW, Li<br />
MM. Randomized trial <strong>of</strong> <strong>salbutamol</strong> <strong>in</strong> acute bronchiolitis<br />
J Pediatr 1991;118: 807±811.<br />
5. Schuh S, Canny G, Reisman JJ, Kerem E, Bentur L, Petric M,<br />
Levison H. Nebulized albuterol <strong>in</strong> acute bronchiolitis J Pediatr<br />
1990;117:633±637.<br />
6. Schweich PJ, Hurt TL, Walkley EI, Mullen N, Archibald LF. The<br />
use <strong>of</strong> <strong>nebulized</strong> albuterol <strong>in</strong> wheez<strong>in</strong>g <strong>in</strong>fants. Pediatr Emerg<br />
Care 1992;8:184±188.<br />
7. Alario AJ, Lewander WJ, Dennehy P, Seifer R, Mansell AL. The<br />
ef®cacy <strong>of</strong> <strong>nebulized</strong> metaproterenol <strong>in</strong> wheez<strong>in</strong>g <strong>in</strong>fants and<br />
young children. Am J Dis Child 1992;146:412±418.<br />
8. Sly PD, Lanteri CJ, Raven JM. Do wheezy <strong>in</strong>fants recover<strong>in</strong>g<br />
from bronchiolitis respond to <strong>in</strong>haled <strong>salbutamol</strong>? Pediatr Pulmonol<br />
1991;10:36±39.<br />
9. Tepper R, Rosenberg D, Eigen H, Reister T. Bronchodilator<br />
responsiveness <strong>in</strong> <strong>in</strong>fants with bronchiolitis. Pediatr Pulmonol<br />
1994;17:81±85.<br />
10. Gadomski AM, Lichenste<strong>in</strong> R, Horton L, K<strong>in</strong>g J, Keane V,<br />
Permutt T. Ef®cacy <strong>of</strong> albuterol <strong>in</strong> the management <strong>of</strong><br />
bronchiolitis. Pediatrics 1994;93:907±912.<br />
11. Wang EEL, Milner R, Allen U, Maj H. Bronchodilators for<br />
treatment <strong>of</strong> mild bronchiolitis: a factorial randomized trial. Arch<br />
Dis Child 1992;67:289±293.<br />
12. O'Callaghan C, Milner AD, Swabrick A. Paradoxical deterioration<br />
<strong>in</strong> lung function after <strong>nebulized</strong> <strong>salbutamol</strong> <strong>in</strong> wheezy <strong>in</strong>fants<br />
Lancet 1986;8521:1424±1425.<br />
13. Ho L, Collis G, Landau LI, Le Souef PN. Effect <strong>of</strong> <strong>salbutamol</strong> on<br />
oxygen saturation <strong>in</strong> bronchiolitis. Arch Dis Child 1991;66:<br />
1061±1064.<br />
14. Wohl MEB, Chernick V. State <strong>of</strong> the art: Bronchiolitis. Am Rev<br />
Respir Dis 1978;53:707±709.<br />
15. KristjaÂnsson S, Lodrup Carlsen KC, Wennergren G, Strannegard<br />
IL, Carlsen KH. Nebulized racemic adrenal<strong>in</strong>e <strong>in</strong> the treatment <strong>of</strong><br />
acute bronchiolitis <strong>in</strong> <strong>in</strong>fants and toddlers. Arch Dis Child 1993;<br />
69:650±654.<br />
16. SaÂnchez I, De Koster J, Powell RE, Wolste<strong>in</strong> R, Chernick V.<br />
Effect <strong>of</strong> racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> and <strong>salbutamol</strong> on cl<strong>in</strong>ical score<br />
and pulmonary mechanics <strong>in</strong> <strong>in</strong>fants with bronchiolitis. J Pediatr<br />
1993;122:145±151.<br />
17. Reijonen T, Korppi M, Pitkakangas S, Tenhola S, Remes K. The<br />
cl<strong>in</strong>ical ef®cacy <strong>of</strong> <strong>nebulized</strong> racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> and albuterol <strong>in</strong><br />
acute bronchiolitis. Arch Pediatr Adolesc Med 1995;149:686±692.<br />
18. Bierman CW, Pierson WE. The pharmacologic management <strong>of</strong><br />
status asthmaticus <strong>in</strong> children. Pediatrics 1974;54:245±247.<br />
19. Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses<br />
SW. Dexamethasone and <strong>salbutamol</strong> <strong>in</strong> the treatment <strong>of</strong> acute<br />
wheez<strong>in</strong>g <strong>in</strong> <strong>in</strong>fants. Pediatrics 1983;71:13±18.<br />
20. Flores G, Horwitz R. Ef®cacy <strong>of</strong> beta 2 agonist <strong>in</strong> bronchiolitis: a<br />
reappraisal and meta-analysis. Pediatrics 1997;100:233±239.<br />
21. Kellner JD, Ohlsson A, Gadomski A, Wang EEL. Ef®cacy <strong>of</strong><br />
bronchodilator therapy <strong>in</strong> bronchiolitis. A meta-analysis. Arch<br />
Pediatr Adolesc Med 1996;150:1166±1172.<br />
22. Weenergren G, KristjaÂnsson S, Sten G, Bjure J, Engstrom Y.<br />
Nebulized racemic adrenal<strong>in</strong>e for wheezy bronchitis. Acta<br />
Paediatr Scand 1991;80:375±377.<br />
23. Menton K, Sutcliffe T, Klassen TP. A randomized trial compar<strong>in</strong>g<br />
the ef®cacy <strong>of</strong> <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> with <strong>salbutamol</strong> <strong>in</strong> the treatment <strong>of</strong><br />
acute bronchiolitis. J Pediatr 1995;126:1004±1007.<br />
24. Fraser BD. Nebulized levo-<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> as a alternative to racemic<br />
<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> <strong>in</strong> croup. Can J Hosp Pharmacy 1995;48:303±305.<br />
25. Coupe MU, Guly U, Brown E, Barnes PJ. Nebulized adrenal<strong>in</strong>e <strong>in</strong><br />
acute severe asthma: comparison with <strong>salbutamol</strong>. Eur J Respir<br />
Dis 1987;71:227±232.<br />
26. Waisman Y, Kle<strong>in</strong> BL, Boenn<strong>in</strong>g DA, Young GM, Chamberla<strong>in</strong><br />
JM, O'Donnell R, Ochsenschlagger DW. Prospective randomized,<br />
double-bl<strong>in</strong>d study compar<strong>in</strong>g l-<strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong> and racemic <strong>ep<strong>in</strong>ephr<strong>in</strong>e</strong><br />
aerosols <strong>in</strong> the treatment <strong>of</strong> laryngotracheitis (croup).<br />
Pediatrics 1992;89:302±306.<br />
27. Ellis JF, Taylor JC, Lefkowitz MD. Racemic adrenal<strong>in</strong>e <strong>in</strong> croup.<br />
Pediatrics 1974;53:291±292.