2011 Nursing Annual Report - Kaleida Health
2011 Nursing Annual Report - Kaleida Health
2011 Nursing Annual Report - Kaleida Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
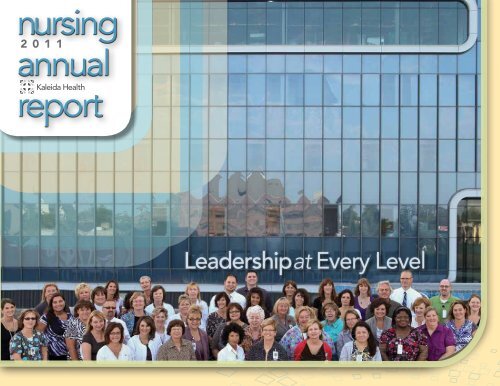
nursing<br />
<strong>2011</strong><br />
annual<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
report<br />
Leadershipat Every Level
ership advocacy caring<br />
ing leadership advocacy caring<br />
vocacy caring leadership advocacy<br />
advocacy caring leadership advocacy caring<br />
leadership<br />
advocacy<br />
caring
Celebrating Commitment –<br />
Expressing Gratitude<br />
Celebrating Our Nurses<br />
Jim Kaskie<br />
President and CEO<br />
Each May, the nation honors nursing<br />
professionals with National Nurses Week.<br />
Starting on Nurses Day and continuing<br />
through Florence Nightingale’s birthday, we<br />
pause to recognize our nursing staff for what<br />
they do each and every day.<br />
In this annual report, on behalf of all of those touched by your<br />
care, we salute all the nurses in the <strong>Kaleida</strong> <strong>Health</strong> family. Whether<br />
it is in an acute care, clinic, rehabilitation, long-term care or home<br />
health setting, our nurses truly impact our patients’ lives.<br />
The gratitude for your commitment and dedication is expressed<br />
in the countless letters and notes sent in by patients and their<br />
families. It is through their words that you can see the impact of<br />
your work. That is why it is always so heartwarming to receive<br />
notes complimenting the good things you do. Whether you see<br />
a patient for a minute, a day, a week or longer, you shape their<br />
perception of the care they received.<br />
Using the words caring, compassionate, attentive, professional and<br />
courteous, patients tell us why what you do is so important and<br />
how it aids their recovery.<br />
As we move forward and transform into a new health enterprise,<br />
the impact nurses have on our patients and in this organization is<br />
even more significant.<br />
To achieve these goals, nurses are leading initiatives that are<br />
evolving nursing care. Specifically, the Magnet Journey, Centralized<br />
Partnership Councils, Cohort and Residency programs,<br />
and Dedicated Education Units are all examples of how our<br />
exceptional nurses are providing extraordinary care and laying<br />
the foundation for future nursing generations. Moving forward,<br />
<strong>Kaleida</strong> <strong>Health</strong> will continue its commitment to the future of<br />
nursing and healthcare safety and quality.<br />
Personally, I can attest to the effect a nurse can have on a family’s<br />
experience.<br />
Thirteen years ago, I lost my father at age 79 to cancer, and a<br />
heart that just could not work any harder. He was an OB-GYN<br />
physician, and in “retirement” at age 60, became a full fledge<br />
Emergency Room doctor. Last August, my 92-year-old mother said<br />
she had “lived a great life” and let go.<br />
Why do I share this? I can only imagine that many of you think<br />
of me as just the “CEO,” the one focused only on numbers<br />
and “corporate stuff.” And you may wonder if I appreciate the<br />
unbelievable work our <strong>Kaleida</strong> <strong>Health</strong> nurses do, day in and day<br />
out, 24/7, 365 days a year.<br />
I began my career in health care as an emergency room tech in<br />
a trauma center in St. Louis. For six years, I worked side by side<br />
with nurses who amazed me daily. They amazed me with their<br />
skill, compassion, tireless efforts, and commitment to serve the<br />
patient seeking their care.<br />
2 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
Every day, for the 35 years that<br />
I have served in health care<br />
administration, I have worked with<br />
nurses and witnessed these same<br />
efforts every day. However, never<br />
Gates Legacy Celebration!<br />
did I truly appreciate the work of nurses<br />
more than when nurses were at my father’s bedside or attending to<br />
my mother, especially for the five years she was cared for in a longterm<br />
care facility.<br />
So on a professional, a “CEO” level, THANK YOU for your<br />
outstanding service. Thank you for the healing you bring to our<br />
patients and their families every day. I am so very proud of you.<br />
You are making the difference in so many peoples lives.<br />
Gates Legacy Celebration: A Tribute to Family,<br />
Friends and Excellence<br />
Two years ago, Gates Hospital President, Tammy Owen asked a<br />
group of employees to form a committee to look at celebrating<br />
Gates “legacy” prior to the collocation and closure of the facility<br />
in the spring of 2012. Tammy said when she came to Gates from<br />
DeGraff, she was very impressed by the community hospital<br />
feeling similar to that at DeGraff, but in a larger teaching-based<br />
hospital. Despite the excitement about the opportunities that the<br />
new GVI and collocation to the BNMC would have for staff, she<br />
knew the strong connections, personal and professional, needed<br />
to be celebrated before the move. Bev Tate, a 43-year employee,<br />
was asked to chair the committee with members, Annette Klosek -<br />
administration, Gina Sutor (the senior legacy committee member<br />
with 50 years as a Gates employee), Josephine Toldeo - gift<br />
shop manager, Phyllis Gentner - marketing, Adrienne Doepp<br />
- librarian, Barb Browning - marketing, Mary Bernosky-Rak -<br />
clinical education, Carol Rice - radiology, Pat Clabeaux - Human<br />
Resources, Claudia Pawlak - respiratory and Drs. Franklin and<br />
Campagna were also members of the interdisciplinary committee.<br />
The group’s focus was how to celebrate Gates Legacy. Bev says<br />
that the overriding theme of legacy was evocative of “family.” She<br />
says in a larger sense, Gates “families” extended beyond units and<br />
department; staff went to each others’ weddings and baby showers.<br />
Residents and house staff commented on the sense of teamwork<br />
they found throughout Gates and the supportive and nurturing<br />
environment it provided for house staff and students, which<br />
wasn’t uniformly felt in other hospitals. Gates nurses said they<br />
had a sense of “Pay it Forward” and everyone helped each other,<br />
again not defined or limited to units or departments. The legacy of<br />
nursing excellence was part of the School of <strong>Nursing</strong> impact and<br />
the implementation of the first nursing career ladder in the area<br />
in the 1980s. The career ladder had nurses receiving recognition<br />
for their educational accomplishments and was supported by one<br />
of the first tuition assistance programs in the area. Administration<br />
empowered the nursing staff to look at methods to alleviate the<br />
nursing shortage of the early 1980s. A committee of staff nurses<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
3
came up with 21<br />
initiatives to improve<br />
professional nursing<br />
and administration<br />
implemented 17 of them;<br />
the clinical ladder and tuition support were two of them.<br />
Penny Gast, director of perioperative services at Gates and a 22-<br />
year “alumns” of the facility, validates the standing of the hospital<br />
as progressive and innovative. After relocating to Buffalo from<br />
Alexandria, Virginia, the former laser safety officer was interviewed<br />
by <strong>Nursing</strong> OR Director Kitty Hart. Penny<br />
interviewed at several other facilities but chose<br />
Gates because it was an exciting innovative<br />
hospital with a community hospital feeling. Two<br />
decades ago<br />
Penny says<br />
traumas<br />
frequently<br />
went to<br />
Gates,<br />
especially<br />
those<br />
involving re-implants and<br />
they did over 1,000 hearts annually as well as supporting a, then,<br />
burgeoning nuero/stroke program.<br />
Penny says the surgical staff at Gates has a history of innovation<br />
and excellence; several of the surgeons had patents as well as Gates<br />
status as one of the first hospitals to do endovascular surgery. She<br />
remembers the first endovascular triple, which is a procedure<br />
for aortic aneurysms that dramatically increased survival and<br />
reduced complications from what was previously<br />
a sternum to belly incision and several days in<br />
the unit post-op. Today some patients go home<br />
the same day as endo surgery. Minimally invasive<br />
surgery was championed, along with some of the<br />
first cochlear implant surgeries. She feels the Gates surgical team<br />
including the post-op care was “extraordinary,” not only because<br />
they pioneered cutting edge surgery but were always focused<br />
on patients first. As a nurse Penny felt the teaching atmosphere<br />
helped all of the nursing staff grow as professionals. She says<br />
the nurses who comprise<br />
the nuero and heart teams<br />
as well as the surgical techs<br />
are equally committed to<br />
the patient. Marlene Traden,<br />
a Gates OR alumnus, was<br />
instrumental in bringing the<br />
RN First Assist program to the<br />
Millards. Another OR nurse<br />
alumnus and former Director<br />
of Surgical Services, Sharon<br />
McNamara, one of Penny’s<br />
mentors, served as national<br />
AORN president in 2005. Penny mentioned that Robin Frank was<br />
also a great mentor and role model: “Robin always encourages you<br />
to take on new challenges and coaches you to be successful.” She<br />
feels that the leadership team of Robin, Jodi Witherell and Tammy<br />
Owen has done a terrific job of assisting with the integration and<br />
reducing anxiety and promoting collaboration between colleagues<br />
at BGH and Gates.<br />
Rose Hansen is one of the Gates employees that had the ability to<br />
4 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
start working with her BGH colleagues late in <strong>2011</strong>. Rose, a 24-<br />
year alumnus, is a Gates diploma graduate who started working<br />
on her BSN when she knew the hospital would be integrating with<br />
BGH and the GVI. She completed her BSN in 2007 and her FNP<br />
in 2010; she did her thesis on stemis. As a new graduate in critical<br />
care, she worked in cardiac intervention before joining the team<br />
in the cath lab in 1997. Rose, like Penny, is proud of the history of<br />
family, teamwork and excellence she feels Gates is synonymous<br />
with. She gives Dr. Masud credit for the colleagueship among<br />
nurses,<br />
physicians<br />
and other<br />
support<br />
departments<br />
such as<br />
radiology, she<br />
notes he was<br />
instrumental<br />
in bringing<br />
angiography<br />
to the WNY area. Rose is very excited about the new TARV<br />
procedure and was a member of the team that went to New York<br />
City for training in November. Rose says she loves being part<br />
of this procedure that only a very few hospitals (7%) across the<br />
country have been authorized to perform. She sees this as similar<br />
to the feeling she gets with stemis. The ability to give hope and<br />
life to people who might otherwise die, is thrilling to Rose. She<br />
has been involved in two procedures but looks forward to the<br />
move to the GVI when the entire team, nuero, cardiac, vascular<br />
and radiology will be in the same area. She says they anticipate<br />
screening over 700 patients annually and performing around 100<br />
procedures in the<br />
first year. She feels<br />
lucky to be able to<br />
work in a world class<br />
cath lab focused<br />
on innovation,<br />
education and<br />
research, with people<br />
like Patti Arbogast, NP, and<br />
Dr. Iyer.<br />
Rose says she has scheduled herself to work the last day of<br />
the integration. She will miss Gates but knows that creating<br />
a sense of family, caring for patients and being excited and<br />
engaged in education and excellence are all commodities that are<br />
transportable to her new home. Her dream is to be able to be an<br />
advanced practice nurse in the cath lab and never stop learning or<br />
caring for her special patients.<br />
Rose Hansen, Gates<br />
Nurse Practitioner,<br />
excited about GVI<br />
Legacy celebration for Gates – June <strong>2011</strong><br />
– Connie Vari, COO with educators, Nurse<br />
Recruiter Lori Stoudmire and staff<br />
Robin Frank, Director of Surgical Services,<br />
and Jodi Witherell, Director of Nueroscience<br />
Services, came to Gates within a year and<br />
a half of each other and both commented<br />
on the warm welcome they received and<br />
what an accepting environment it was. They<br />
were impressed within their own specialties<br />
about the level of professional expertise and<br />
practice. They both feel the opportunity<br />
to have all the specialties under one roof<br />
will enhance patient outcomes and practice<br />
opportunities for their nursing staff.<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
5
The “Legacy Celebration” sold 730 tickets with participants<br />
coming from other states and many senior alumni. Several<br />
retired MDs, nurses and other staff members came from as far<br />
away as Michigan to celebrate and reminisce with their “family.”<br />
Participants said it was more like a family reunion than work<br />
celebration. Swanne Graves, a retired nursing supervisor who<br />
turns 85 this year, attended along with Marge Arnold, a former<br />
Gates DON, and Linda Scharf, a committee member and former<br />
Gates CEO.<br />
Committee members said the response to the event and<br />
accompanied sale of “momentoes,” cookbooks, jackets, Christmas<br />
ornaments and pins was overwhelming and exceeded the<br />
planning committee’s expectations. The timing of the event<br />
was to celebrate the 100 years of the original building erection,<br />
January 4, 1911. The theme, “A Century of Caring,” was printed<br />
on commemorative pins with the façade of the old hospital.<br />
Committee members were especially proud of the cookbook as it<br />
had personal memories of employees’ experiences at Gates along<br />
with recipes; a labor of “love.”<br />
Leadership and Empowerment<br />
at Every Level<br />
<strong>Kaleida</strong> Nurses attend <strong>2011</strong> Magnet Conference<br />
in Baltimore and Come Back Wowed<br />
A second contingent of <strong>Kaleida</strong> nurses attended the national<br />
magnet conference in Baltimore this past October. Five <strong>Kaleida</strong><br />
nurses representing each of our acute care sites attended with<br />
nursing leadership. It was the largest conference to date with<br />
7,500 participants, mostly staff<br />
nurses, celebrating excellence<br />
in nursing and patient care.<br />
Donna Gatti, BGH<br />
Donna is a 1982 BGH diploma<br />
graduate and has spent 23<br />
of her 24 years in behavioral<br />
health. Before she went to the<br />
magnet conference she didn’t<br />
really know a lot about it. As chair<br />
of her UPC and member of site<br />
and corporate UPCs, Donna is interested in making changes to<br />
improve nursing and patient satisfaction.<br />
Marygrace Piskorowski, Lisa Loffredo and<br />
Marybeth Farruggio at Magnet Conference<br />
Donna was blown away by the energy of the 7,500 nurses at the<br />
national magnet conference who, she says, clearly expressed<br />
their passion for the profession of nursing. She returned with the<br />
conviction that “magnet is simply being the best nurse you can,”<br />
October <strong>2011</strong><br />
National Magnet<br />
Conference Baltimore<br />
6
she feels it is how she has cared for<br />
her patients throughout her career.<br />
She wants magnet for <strong>Kaleida</strong> nurses<br />
because of what it means with respect<br />
to quality care, evidence based practice<br />
and nurses being highly respected.<br />
As a diploma graduate, she felt she<br />
got a great education but understands<br />
both the importance of the “BSN in<br />
Ten” and professional certification. Donna<br />
understands the need for all nurses to stay<br />
current and incorporate “best practice” into their practice. Donna<br />
hopes to be a member of the Cohort V for Executive Leadership<br />
and Change program with Daemen College. Magnet is about life<br />
long learning and this, Donna feels, is definitely professional<br />
nursing.<br />
Lisa Loffredo, MFSH<br />
Marybeth Farruggio and Lisa Loffredo<br />
at Magnet Conference<br />
Graduating in 1994, Lisa attended nursing school at Millard<br />
Fillmore Hospital School of <strong>Nursing</strong>. She later returned for her<br />
BSN at the University of Buffalo. Lisa has been an employee at<br />
MFG since her graduation in 1994. She started at MFG as a staff<br />
nurse on a medical step down unit. After 2 years, she transferred<br />
to MFSH as a critical care float RN. After another 2 years, she<br />
was offered the opportunity for a nursing supervisor position.<br />
Her career includes critical care, charge and a year long diabetes<br />
research position before returning to supervision at MFSH. Lisa<br />
sees nursing supervision as her true calling; “I love to have the<br />
ability to work with nurses and staff throughout the entire hospital<br />
every day, supporting, coaching and teaching the nurses.” Lisa<br />
loves the variety of the role of supervision. She sees every day as a<br />
different challenge. Lisa feels her main job is to keep staff positive<br />
and motivated; in turn she hopes that she makes a difference in the<br />
care they give.<br />
Lisa was thrilled with the opportunity to attend the magnet<br />
conference. “We were celebrating ourselves, our profession and<br />
our accomplishments in nursing, it was awesome,” Lisa shares.<br />
She said she loved watching the nurses who had obtained magnet<br />
for the first time, and noted how much pride they had in their<br />
accomplishment and in their hospital. Lisa said it was like being at<br />
a pep rally, watching the nurses with pompoms, banners, confetti<br />
and clappers, running through the aisles in celebration. Lisa feels<br />
she and all <strong>Kaleida</strong> nurses are the primary reason patients come to<br />
hospitals, saying “we spend more time with our patients than any<br />
other profession, we are the faces of <strong>Kaleida</strong>.” All <strong>Kaleida</strong> nurses<br />
need to promote <strong>Kaleida</strong> nursing. After attending the conference,<br />
Lisa, as chair of MFSH’s Central Partnership Council, CPC, felt her<br />
goal was to promote and build the shared governance model, help<br />
enhance professional pride, and as a nurse, take accountability for<br />
the quality of patient care. At her first CPC meeting after attending<br />
the conference, Lisa said she was able to extend a new excitement<br />
to the staff; five additional nurses have joined since she came back.<br />
Lisa said the conference break-out sessions gave her a lot of great<br />
ideas for working on CPC goals. She hopes to have a few of the<br />
initiatives in place by Nurses Week 2012.<br />
Peggy Meyer, DeGraff<br />
Peggy Meyer, a 13-year veteran of DeGraff and a 1998 graduate of<br />
ECC, said the conference helped her identify the need to focus on<br />
strengthening their CPC, providing more structure so nurses can<br />
really make a difference. Peggy shared, “It made me realize how<br />
much work we have to do, but how many opportunities to make<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
7
Chuck Baker, Sandy Nizinkiewicz<br />
and Peggy Meyer<br />
a difference we have if we do the<br />
work.” She feels that having more<br />
structure and setting attainable<br />
goals for each meeting could really<br />
drive progress.<br />
Peggy, a “second career nurse,”<br />
had five children when she started<br />
back to school while working as<br />
an aide at DeGraff. Her children<br />
ranged from 1 to 8 years old but<br />
Peggy was determined and she<br />
said she got a lot of support and<br />
flexibility from her manager regarding nursing school. Peggy<br />
transferred to the OR 4 years ago and loves it; “everyone really<br />
works as a team, no titles, the patients come first.”<br />
Peggy said she was involved in reigniting the spirit and<br />
corresponding CPC a few years ago. She feels CPCs and UPCs<br />
are a great way to get things done and quickly resolve little issues<br />
so they don’t turn into big ones. She is inspired by the ability to<br />
solve problems at the staff and unit level; she feels it enhances<br />
the respect and value for bedside nurses and feels it challenges<br />
nurses to grow and become leaders. Peggy feels the advocacy role<br />
establishes nurses as bedside leaders. Magnet, as Peggy views it, “is<br />
all about nurses doing all they can for their patients.” Peggy feels<br />
that DeGraff nurses are ready to embrace magnet and is excited to<br />
be part of it.<br />
Marygrace Piskorowski, WCHOB<br />
Marygrace Piskorowski, a L and D nurse at WCHOB and another<br />
“second career nurse,” completed a bachelors in social work<br />
before completing an AAS at Genesee Community College 2 years<br />
ago. Marygrace found the magnet conference was personally<br />
and professionally life altering. Recently she had enrolled in the<br />
NP program at Daemen but is now planning to change to the<br />
Executive Leadership and Change program. Marygrace said it<br />
was so exciting to see what other staff nurses were accomplishing<br />
throughout the country. She said she was interested in magnet<br />
when the position for a magnet champion was first posted at<br />
WCHOB and she was thrilled to be able to attend the conference.<br />
Marygrace said she now feels empowered after listening to other<br />
staff nurses at the conference and hear what they were able to<br />
accomplish without looking to their manager to do it for them.<br />
She feels now is the perfect time to take responsibility for patient<br />
care problems and move forward. Through the UPCs and CPCs,<br />
Marygrace feels “the voice we have together as staff nurses is<br />
powerful!” Magnet recognition is the reward for a job well done;<br />
Marygrace tells nurses, “forget about the title, magnet is about<br />
doing it better for yourself, your colleagues and your patients.”<br />
Sandy Nizinkiewicz, Gates<br />
Sandy Nizinkiewicz works in the GVI, in the cardiac cath lab<br />
previously at Gates. Although she was sad to see Gates close, she<br />
loves the GVI and the opportunities to practice there. Sandy said<br />
taking call at BGH helped with the transition and having familiar<br />
faces before the collocation. She felt rejuvenated by the magnet<br />
conference. Sandy said she was intrigued when she viewed a video<br />
of nurses obtaining magnet at a Rochester facility and wanted that<br />
for herself and her colleagues. The magnet experience in Baltimore<br />
“was phenomenal.” Sandy shares. She wishes every <strong>Kaleida</strong> nurse<br />
could have the opportunity to attend this. Sandy describes the<br />
culture of magnet as something she wishes she could bottle; “it’s<br />
8 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
just about being in the best hospital, with the best nurses and<br />
being the best you.” Sandy says the conference has changed her<br />
professionally as well. She feels the need to find a way to “get her<br />
BSN.” Sandy admits she never really thought about this before she<br />
attended the national magnet conference. She feels those nurses<br />
that don’t embrace magnet don’t understand what it is. She feels<br />
the answer is to talk about magnet and don’t stop; help nurses see<br />
the big picture that magnet is a major culture change that helps<br />
everyone. She feels managers can help by empowering nurses. She<br />
said one of her favorite seminars at the conference was one with a<br />
nurse manager relating her story of reversing a high turn-over, low<br />
staff and patient satisfaction unit. Sandy said the manager turned<br />
the unit around by involving the staff in every aspect of change.<br />
“It was the magnet, shared governance model, with the manager<br />
giving the nurses ownership for creating the type of unit they<br />
wanted to work in.”<br />
Future of <strong>Nursing</strong> at <strong>Kaleida</strong> <strong>Health</strong> -<br />
(<strong>Kaleida</strong> participates in Future of <strong>Nursing</strong> Conference<br />
at Roswell)<br />
<strong>Kaleida</strong> <strong>Nursing</strong> is making tremendous strides to pave the way for<br />
a future of health safety and quality in the metropolitan Buffalo<br />
area. The national Robert Wood Johnson Foundation Initiative<br />
on the Future of <strong>Nursing</strong>, at the Institute of Medicine (IOM),<br />
published a report in <strong>2011</strong> that serves as a road map for regional<br />
nurses to begin needed transformation in our healthcare systems.<br />
Nurses are encouraged to download this report or the report brief,<br />
free of charge at http://www.iom.edu/.<br />
<strong>Kaleida</strong> nurses were invited to attend a free event on November<br />
16, <strong>2011</strong> at Roswell Park Cancer Institute, to learn the details<br />
about the Future of <strong>Nursing</strong> report and ask questions about how<br />
it relates to their personal practice from the Vice Chair of this IOM<br />
Committee, Linda Burnes Bolton, DrPH, RN, FAAN. Amy Klopp,<br />
RN from Millard Fillmore Gates Circle, recounted the event was<br />
“energizing, to see what a difference nurses can and must make in<br />
hospitals and it was helpful how all of the research was presented<br />
in a way that a staff nurse could clearly understand.”<br />
<strong>Kaleida</strong> nursing collaborated closely with Roswell Park Cancer<br />
Institute’s <strong>Nursing</strong> Research Council to plan and prepare the event<br />
that over 200 regional nurses and nursing students attended.<br />
Through poster presentations, <strong>Kaleida</strong> nurses proudly showcased<br />
their work on preventing falls, enhancing safety during patient<br />
hand-off and shift report, leading support groups, building<br />
teamwork and teaching self-care to new graduate nurses.<br />
“The event was very affirming, to see how much of the nationally<br />
recommended work <strong>Kaleida</strong> nurses have already begun,” reports<br />
Michele Natwora from clinical education. The IOM report includes<br />
eight recommendations. The first three recommendations from<br />
the report and nurse-led <strong>Kaleida</strong> initiatives are as follows (with<br />
additional recommendations to be addressed in future articles):<br />
1. Remove scope of practice barriers. The values and philosophy<br />
embedded in nursing practice includes care that is centered on the<br />
unique needs of individual patients, known as person-centered<br />
Dr. Burnes Bolton (second from left) with WNY panel on Future of <strong>Nursing</strong><br />
<strong>Kaleida</strong> <strong>Health</strong><br />
9
care. National initiatives to change healthcare focus on access,<br />
quality and value-driven principles inherent to nursing education<br />
and practice. While the IOM report focuses on advanced scope of<br />
practice and reimbursement variations, the importance of hospital<br />
nurses practicing to their full knowledge-base was also addressed.<br />
Supporting bedside leadership via our AHEC Leadership program<br />
and Daemen/<strong>Kaleida</strong> partnership along with self governance<br />
via CPCs,UPCs and NAC are all strategies to increase the<br />
ability for nurses to drive quality and innovation at the bedside.<br />
The utilization of TeamSTEPPS tools throughout <strong>Kaleida</strong> as<br />
opportunities to enhance patient quality and safety encourages<br />
nurses to “fully practice.”<br />
2. Expand opportunities for nurses to lead and diffuse<br />
collaborative improvement efforts. Nurses are in a key position to<br />
lead and develop innovative models of care and solutions that will<br />
improve outcomes and infuse a patient-centered philosophy into<br />
existing care processes.<br />
Managers have focused on educating staff regarding quality<br />
indicators as barometers for practice and utilizing the information<br />
to craft performance improvement projects. Nurses at BGMC and<br />
MFSH have focused on reducing VAP rates and central line infection<br />
rates. Innovative skin care projects as well as falls prevention<br />
programs are being implemented throughout the five acute care<br />
sites. The “White Wreath” program and Schwartz Rounds at<br />
WCHOB and BGMC are activities that nursing has taken a lead in<br />
to enhance compassion for caregivers, patients and families.<br />
3. Implement nurse residency programs. The skills and knowledge<br />
needed to deliver safe, quality care need refinement and continued<br />
learning after graduation. Nurse residency programs support the<br />
transition from school to practice by offering tailored professional<br />
development for new graduate nurses. The Future of <strong>Nursing</strong><br />
report stresses that nurse residency programs need to reach<br />
community settings in addition to hospitals.<br />
Thanks to the generous support of the John R. Oishei Foundation<br />
and the collaboration of WNY area Chief <strong>Nursing</strong> Officers,<br />
the new graduate nurses hired in the summer months of 2010<br />
and <strong>2011</strong> at <strong>Kaleida</strong>, Roswell Park, ECMC and the VA, have<br />
participated in a collaborative nurse residency program. The<br />
first program of its kind in WNY, <strong>Kaleida</strong> <strong>Health</strong> provided the<br />
leadership for this program and the 12 modules that comprise<br />
the year-long program. Jessica Castner, faculty coordinator (on<br />
loan from D’Youville College), helped actualize the program along<br />
with a education team from all 4 partners. The program fosters<br />
opportunities to practice bedside leadership skills. In the spirit of<br />
the Future of <strong>Nursing</strong> report, the program is also supporting and<br />
assisting Hospice Buffalo and networking with the Catholic <strong>Health</strong><br />
System to implement nurse residency programs.<br />
Remaining recommendations from the Future of <strong>Nursing</strong> <strong>Report</strong><br />
to be addressed in future articles:<br />
4. Increase the proportion of nurses with a baccalaureate degree to<br />
80 percent by 2020<br />
5. Double the nurses with a doctorate by 2020<br />
6. Ensure nurses engage in lifelong learning<br />
7. Prepare and enable nurses to lead change to advance health<br />
8. Build an infrastructure for the collection and analysis of interprofessional<br />
health care workforce data.<br />
10 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
<strong>Kaleida</strong> nursing leadership is proud of the organizational efforts<br />
and structure set to prepare for the future of nursing. <strong>Nursing</strong><br />
leadership at <strong>Kaleida</strong> is committed to advancing our organization<br />
toward an ideal vision of the “Future of <strong>Nursing</strong>.”<br />
Acknowledgements: Sincere thanks and congratulations to the<br />
following nurses from <strong>Kaleida</strong> who presented or co-authored<br />
posters: Anthony Szarzanowicz, Donna Gatti, Kristen Kennedy,<br />
Kristina Marquez, Mary Krebs, Mary Kennedy, Diane Ceravolo,<br />
Kelly Foltz-Ramos, Michele Natwora and Renee Sylvies.<br />
Shared Governance<br />
All four CPCs have begun the work of creating magnet champions<br />
in their membership. Although it is early in our journey towards<br />
magnet, our rally cry, “Exceptional Nurses providing Extraordinary<br />
Care” is something all CPCs have embraced with pride.<br />
Additionally, the CPCs all plan to provide greater education to<br />
their colleagues through UPC regarding the “evidences of magnet”<br />
and linking them to current <strong>Kaleida</strong> nursing initiatives.<br />
BGH/Gates<br />
The two CPCs joined together several months ago to focus on<br />
integrating the two committees prior to the March collocation. The<br />
group has reached out to support services to work on solutions for<br />
identified problems. They have also used the group as a forum to<br />
promote patient safety by discussing near misses, actual events on<br />
patient units and to minimize chance of reoccurrence. The group<br />
also utilizes the monthly meeting to discuss EMR concerns and<br />
troubleshoot solutions. The committee will support issues central<br />
to the success of the merger and staff impacted during 2012.<br />
DeGraff is continuing to focus on growing its membership. Its<br />
main focus has been on decreasing the time for ED admits to<br />
get to the unit. Unit nurses were frustrated at what appeared<br />
to be multiple admits with staff perception of indifference to<br />
patient safety. ED nurses perception was that unit nurses were<br />
not sensitive to their and their patients’ need to get to a unit<br />
expeditiously. Both groups were aware of the negative impact<br />
on the patient. The group worked on a flow chart to assist in<br />
decreasing the time frame from ED to unit. Anyone interested in<br />
joining should contact Paul Peterangelo, chair.<br />
MFSH with chair, supervisor Lisa Loffredo, as with DeGraff and<br />
BGH/Gates CPC, sees facilitating and enhancing communication<br />
within the nursing and interdisciplinary staff a critical need for<br />
the group. Their group provided leadership and dissemination of<br />
education on a variety of initiatives such as MOLST Question and<br />
Answer Quick Reference sheet for units, process of Immunizations<br />
given on admission to improve compliance (previously some<br />
units gave on discharge), reducing hospital acquired infections via<br />
encouraging hand washing at unit level, support for EMR Go-<br />
Lives, facilitation of questions and answers and support for Hourly<br />
Rounding. The group has supported processes that improve<br />
quality indicators, including skin care, falls and patient satisfaction.<br />
Included in their goals for 2012 are focusing on nurses and patient<br />
satisfaction and hospital acquired infections.<br />
WCHOB Central Partnership Council, with co-chairs Lisa Gunn-<br />
Taylor and Michelle Szefler, have been supporting a number of<br />
system initiatives such as enhancing the communication throughout<br />
their site and the system through Unit Practice Councils, UPC,<br />
and the <strong>Nursing</strong> Advisory Council, NAC. The group provides<br />
support and communication for all interdisciplinary projects such<br />
as dietary reports, EMR, interdisciplinary Round Tables, Schwartz<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
11
Rounds, TeamSTEPPS tools and new project support such as<br />
nursing peer review. Future goals include identifying initiatives to<br />
enhance patient and nurse satisfaction.<br />
NAC, <strong>Nursing</strong> Advisory Council-<br />
Corporate Shared Governance<br />
NAC members also participate in their site central partnership<br />
and/or unit practice committees. Their focus for <strong>2011</strong> was the<br />
development of educational materials and posters to assist their<br />
colleagues in understanding the importance of a magnet journey.<br />
All members participated in visiting the site central partnership<br />
meetings with a “Magnet Traveling Road Show” to foster<br />
understanding and generate excitement for magnet. The posters<br />
and presentation highlighted the forces of magnetism and what<br />
opportunities exist to work toward this. They also brought this to<br />
the <strong>Nursing</strong> Executive meeting to ensure nursing leadership was<br />
on the same page regarding the importance of magnet. What the<br />
NAC members think is the most important take away from the<br />
presentation, “magnet is about what happens to you as a nurse<br />
and a department on the journey to magnet; it’s the right thing to<br />
do for nurses and patients.”<br />
White Wreath project Developed by Bedside<br />
Leaders from MICU UPC<br />
After attending an End of Life <strong>Nursing</strong> Education Consortium in<br />
August, Cathy Papia, Family Liaison Nurse in the MICU, wanted<br />
to do something more to make the process of dying in the ICU<br />
less traumatic, so she brought the issue to her UPC, Unit Practice<br />
Council. After a brainstorming session about how they<br />
could support patients and families of terminal<br />
weans, the idea of placing a wreath on the door<br />
White Wreathe Program-Buddhist<br />
to designate<br />
the patient’s<br />
terminal<br />
status was<br />
identified.<br />
Along with<br />
the wreath,<br />
the unit<br />
identified<br />
additional<br />
items and<br />
MICU staff with “white wreath” basket<br />
ideas that could<br />
make the environment more nurturing and supportive. The group<br />
felt it would be great to have a collection of music that might<br />
support the family as well as the patient, placing white flowers on<br />
the secretaries’ desk to make all members of the team aware of the<br />
imminent loss of a patient, having scented lotion families could<br />
use to rub the arms of their loved one, were all part of the project.<br />
MICU RNs, Rose St. Pierre, Cynthia Hamm, Kimberly Dale,<br />
and Loraine Hawthorn (who personally shopped for the “White<br />
Wreath” items) were part of the UPC brainstorming group that<br />
developed the idea. Start-up funds for the program were provided<br />
by Lucy Campbell, MD, MICU medical director and Pat Holtz,<br />
nurse manager for the MICU<br />
The “White Wreath” protocol helps create a cultural awareness<br />
and respect for an individual’s ethnicity, age, religion and<br />
spirituality; allows for the appropriate modification of the ICU<br />
environment for an actively dying patient, (minimizing noise,<br />
conversation and lights when possible) and provides support for<br />
the ICU nurse providing end-of-life care. When a terminal wean or<br />
dying patient is identified by the team, the “White Wreath” basket<br />
12
is brought out, containing in addition to the items mentioned<br />
previously, a Bible, Koran, prayer rug, room fragrance and a new<br />
fleece blanket and angel pin for the patient’s gown. The last two<br />
items are given to the family as a remembrance.<br />
Cathy said staff was skeptical when the program started this past<br />
October. Several staff members said, “oh great, one more thing<br />
to do.” In a very short time period the staff was won over by the<br />
family’s response to the protocol. Cathy said she had started the<br />
project by placing the wreath on the door after speaking to the<br />
family and filling out the MOLST form. She was concerned about<br />
engaging the night shift but in the second week of the project, she<br />
came in to find a night nurse had initiated the process by hanging<br />
the wreath on the door of a terminal wean patient. She was thrilled<br />
that most of the committee was comprised of her most seasoned<br />
nurses with the exception of Kim Dale. Cathy mentioned that after<br />
the program was highlighted in OneVoice on <strong>Kaleida</strong>Scope, she<br />
had non-clinical people stopping by to tell her how wonderful they<br />
thought the program was.<br />
Historically, Cathy said that most families, no matter how<br />
supportive the unit has been, do not follow up with a note; she<br />
feels it is very difficult to write about the experience. She has,<br />
however, had many families return to thank the staff or bring<br />
food. The families in the white wreath program have all taken the<br />
blanket and pins when the family member expired. Cathy said<br />
everyone has become engaged in this project; recently a family had<br />
requested AC/DC music for their loved one who was in his 60s.<br />
This wasn’t a part of the MICU music collection so their attending,<br />
Jim Hereth, brought his iPod in and downloaded the music for<br />
a very grateful family. More recently the MICU had a practicing<br />
Buddhist whose family was very spiritual; the family was extremely<br />
grateful for the white wreath protocol and donated some items to<br />
support a Buddhist patient in the future. They were touched with<br />
the staff’s interest in their religious customs and appreciated the<br />
CD player, although they brought their own music reflective of<br />
their brother’s personal taste. They were also touched by the fleece<br />
blanket which was theirs to keep. “Everyone is trying to find a way<br />
to meet the needs of the dying patient,” Cathy shares. One patient’s<br />
family member, an elderly retired nurse, shared how wonderful she<br />
felt this program is.<br />
Hi Cathy,<br />
I just read the article on the white wreath protocol that you initiated<br />
and I wanted to share something with you. My dad died of lung cancer<br />
with brain mets over 26 years ago and to this day I still remember one<br />
seemingly insignificant incident that happened in the ICU. Dad was<br />
having a very bad day, struggling just to take a breath and obviously<br />
it was a very stressful time for all of us. Watching someone you love<br />
not only dying but dying a slow, agonizing death is totally consuming<br />
to everyone involved. There is no world around you; there is only here<br />
and now, this moment, this place. You can’t even imagine that there<br />
is anything else, let alone care about anything else. My mother, sister<br />
and I stood by dad’s bed, hopelessly trying to comfort him, wishing we<br />
could breathe for him, holding back tears while looking at the panic<br />
in his eyes as he struggled to get air into his lungs that were rapidly<br />
failing him. Suddenly we were all made acutely aware of where we<br />
were. There was the very loud sound of laughter coming from the<br />
nurse’s station. A group of 3 or 4 ICU staff members were sharing<br />
a humorous moment and even though I had no right to be upset by<br />
someone’s happiness, I felt so hurt by this. I guess I resented the fact<br />
that we were going through the worst time of our lives, watching<br />
someone we all loved so much dying slowly, painfully. All I could think<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
13
was, “how can you laugh when we are in so much emotional pain?”<br />
It felt cruel and insensitive at the time, even though it was totally<br />
unintentional. So, I want to thank you for the people that you will<br />
provide comfort to in the future with the white wreath protocol.<br />
Donna Sauer, RN, BSN, Director VNA immunization program<br />
The loss of a loved one is one of the most difficult experiences a<br />
family can go through. The ability to create memories within an<br />
acute care setting that acknowledge the uniqueness of the patient<br />
and family and express a collective honor and respect for the loss<br />
can have a significant positive impact on the grief process for the<br />
family.<br />
The “White Wreath” protocol is also being expanded to include<br />
the ILCU. ILCU staff embraced the idea of offering support and<br />
comfort to the families of a patient with a terminal wean. They<br />
took cues from the MICU and put together bereavement trays, a<br />
coffee maker was donated along with a lamp and picture to place<br />
on the unit when this is occurring.<br />
This article/program has been published in the ELNEC, National<br />
Organization’s Winter Connections Newsletter, End of Life in<br />
<strong>Nursing</strong> Care.<br />
Anyone who would like to donate new fleece blankets or $5 Tim<br />
Horton’s cards (for families) please contact Cathy Papia.<br />
<strong>Kaleida</strong> uses AHEC Manager Training Grant Money<br />
as Opportunity to Develop Bedside Leaders<br />
RAHEC, Rural Area <strong>Health</strong> Education, a federal government<br />
funded, not for profit, whose mission is to provide education and<br />
training to healthcare workers and organizations, approached<br />
<strong>Kaleida</strong> <strong>Health</strong> <strong>Nursing</strong> Leadership in <strong>2011</strong> with the opportunity<br />
Bedside leaders attend<br />
National Emergency<br />
Nurses Convention (L to R)<br />
Roseann Mohney RN, CEN,<br />
CPEn (Lakeshore Hospital);<br />
Karen Taggart RN, CEN<br />
(BGH); Cheryl Marcel RN,<br />
CEN (BGH)<br />
to train nurse managers. AHEC had contracted with Daemen<br />
College to provide the leadership training. Since 2008 <strong>Kaleida</strong><br />
<strong>Nursing</strong> Leadership has had a contract with Daemen College,<br />
initially focused on developing our front line nurse managers but<br />
in its second year, focused equally on developing bedside leaders,<br />
staff nurses. We asked AHEC if we could model the curriculum<br />
after our <strong>Kaleida</strong> Daemen partnership which provides 6 graduate<br />
credits in Executive Leadership and Change. We also suggested,<br />
based on the Institute’s of Medicine’s, IOM, report, the need to<br />
have staff nurses fully practice required support for leadership<br />
skills. We then asked to select 25 managers and have them select<br />
25 informal staff nurse leaders to partner with and go through the<br />
two-day training together. The first training session took place on<br />
September 13th (it also provided the opportunity for our cover<br />
and theme: Leadership at Every Level) and the second, two and<br />
one half hour class on November 1st.<br />
Dr. Mary Lou Rusin, chair of the Department of <strong>Nursing</strong> at<br />
Daemen College, presented the first module entitled “Leadership,<br />
the Driver of quality and safe patient care.” She covered a variety<br />
of topics including, the Code of Ethics for Nurses (ANA 2001),<br />
which places the focus of care around the patient and gives<br />
the RN the responsibility to work to improve the healthcare<br />
environment. She spoke to the unique role RNs have to change<br />
14 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
culture, empower colleagues and ensure safe, quality care. She<br />
reinforced the power inherent in the team, rather then the team<br />
leader. Citing research, she emphasized that the “best CNO can’t<br />
change culture and practice, staff nurses can and must.” Sharing<br />
information regarding transformational leadership and Covey’s 7<br />
Habits of Highly Effective People, she emphasized the importance<br />
of strong convictions and a win/win attitude regarding conflict<br />
along with the encouragement to, “find your voice” and encourage<br />
others to find theirs. Robert Greenleaf’s Servant Leadership model<br />
was also discussed with the focus on staff identifying barriers to<br />
patient care and then solutions, so the manger can effectively work<br />
to empower staff to deliver the best possible care. In discussing<br />
nursing turn-over, Dr. Rusin cited multiple research studies that<br />
manager behavior and leadership styles do impact nurse turnover.<br />
She showed a You Tube video, “Leadership lessons from The<br />
Dancing Guy,” to emphasize the important relationship between<br />
leaders, followers and the equally significant impact of both on<br />
outcomes.<br />
On November 1, <strong>2011</strong>, the 25 managers and their staff nurse<br />
leaders attended the second part of the two-session series, a lecture<br />
on Emotional Intelligence. E.I. is the constructive ability for self<br />
awareness; empathy and the ability to self regulate our emotional<br />
environment. The speaker, Lisa Ball, RN, DNP and Daemen<br />
<strong>Nursing</strong> faculty and researcher, believes it is the hallmark of a<br />
great nurse. The speaker discussed the difficulties in caring for<br />
patients and remaining caring in today’s challenging environment.<br />
She shared current E.I. research that suggests that the greater<br />
the emotional intelligence of the nurse manager the greater the<br />
retention, productivity and commitment of employees and more<br />
positive work culture. She also spoke to the issue of ownership and<br />
accountability, nurses needing to hold each other and support staff<br />
Daemen<br />
Graduation-<br />
Cohort III<br />
accountable to the patient. Lisa said, by utilizing E.I. concepts, we<br />
can develop a positive culture and be in the position of finding<br />
respect and happiness in and at work. Evaluations of the twosession<br />
program were overwhelmingly positive with both leaders<br />
and staff members acknowledging the opportunity and desire to<br />
utilize the idea of emotional intelligence and accountability in their<br />
professional practice.<br />
Daemen Cohort III graduates<br />
Cohort IV began January 2012<br />
The third year of the <strong>Kaleida</strong> Daemen Leadership Partnership<br />
finished with a third graduation this past November. The<br />
11-member cohort presented their performance improvement<br />
projects during the graduation ceremony to recognize their<br />
completion of 6 graduate credits in Executive Leadership and<br />
Change. Cohort IV will have 11 staff nurses out of the 17<br />
participants. The program originally began in 2009 and focused on<br />
developing leadership skills in nurse managers. In its second year,<br />
Cohort II included staff nurses supporting the IOM’s report on,<br />
The Future of <strong>Nursing</strong> and the need to grow bedside leaders.<br />
Feedback from the third cohort mirrored sentiments of the first<br />
and second, the significant impact of the leadership courses on<br />
their practice. Jim Giallella, 13 North manager, said the passion<br />
as well as knowledge of the professors is something he takes<br />
back to work and helps to energize him. Chris Moden, ED<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
15
Leadership presentation on response to call lights-<br />
Deb Boss, Sofia Arutunian, Chris Moden and Jim<br />
Giallella<br />
manager at MFSH,<br />
feels that the<br />
professors provide<br />
an outsiders’<br />
perspective on<br />
issues that help<br />
him become more<br />
objective and gives<br />
him new tools to<br />
do his job. Lem<br />
Mogavero joined<br />
the program as<br />
a staff nurse and found he loved the opportunity management<br />
provided for a greater impact on<br />
patient care. When he graduated,<br />
he moved to the role of supervisor<br />
on the stroke unit at Gates. He feels<br />
the program has helped him grow<br />
professionally and personally and<br />
as a new leader provided essential<br />
leadership skills. Lem says he now<br />
sees problems as opportunities and<br />
feels more successful in dealing<br />
with them proactively. Staff nurse from<br />
MFSH, Michelle Monte, said that she has always felt she was a<br />
good nurse but now has a greater understanding of the need for<br />
effective communication. Michelle shared she now feels inspired to<br />
“go back to her floor and knock down negativity and build more<br />
trusting relationships.” She feels that bedside leaders can drive a<br />
positive culture change.<br />
Professor with (left to right) Mickey Monte, Lem Mogavero, Anne Hoar,<br />
Luanne Finiki and Andrea Daniel-Sanders<br />
Luanne Finiki, manager in the ICU and SCU at DeGraff, shared<br />
that she was struggling in her leadership role; finding it very hard<br />
to find work - life balance. She said the class helped her to focus<br />
on becoming a transformational leader, she says she feels she can<br />
both grow and let the “small stuff” go and focus on the “big stuff.”<br />
Debbie Boss found the classes empowering and said her biggest<br />
discovery was self insight, realizing the only thing she can control<br />
to any extent is herself.<br />
Performance improvement projects were presented by cohort<br />
III at the February <strong>Nursing</strong> Executive meeting which included<br />
representatives from NAC. The goal is to have the projects<br />
replicated throughout <strong>Kaleida</strong>, a summary of the two projects are<br />
as follows:<br />
Reducing Infection rates: Team - Lem<br />
Mogavero, RN supervisor Stroke, Michelle<br />
Monte, staff nurse MFSH, Luanne Finiki,<br />
manager ICU DeGraff, Anne Hoar, IST<br />
MFSH and Andrea Daniel- Sanders MICU<br />
RN BGH.<br />
Hospital acquired infections are no longer<br />
being reimbursed by the Center for<br />
Medicare/Medicaid Services. Our group<br />
picked a project targeted at reducing and/or<br />
preventing hospital acquired infections. We looked first at theory<br />
involved in change. We knew engagement and empowerment of<br />
staff nurses was critical; in order for a group to change they must<br />
feel empowered.<br />
Using education and empowerment as our tools and aptly named<br />
“Clean Freaks,” our team received the support of the Manager<br />
16 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
on 2 Southwest, Michele Hubert, a member of Daemen cohort II<br />
and a scholarship recipient currently completing her Master’s in<br />
Executive Leadership and Change, to pilot our project there. Our<br />
goal was to decrease the rate of hospital acquired C-diff infections.<br />
The project took a multidisciplinary approach utilizing a pre/post<br />
survey to assess level of knowledge, perceived barriers as well<br />
as staff’s view of their ability to address the problem. Following<br />
our pre-survey assessment, the cohort developed and instituted<br />
an educational/empowerment blitz of the unit. We followedup<br />
with coaching and educational reviews to staff at specific<br />
periods over the next several months. In our three-month time<br />
period we did not see a significant reduction in C-diff. Our post<br />
education survey however did reveal a significant increase in the<br />
knowledge regarding C-diff and a greater sense of empowerment<br />
on the part of the nursing staff. We felt that the time frame was<br />
not extensive enough to see the results of our education and<br />
coaching on infection rates but the increased knowledge did<br />
suggest that this could improve over the next quarter. Manager<br />
Michele Hubert says, “the staff are definitely engaged in finding a<br />
solution and since the project rollout of the Clean Freaks, we have<br />
identified some other ways that may have affected the transmission<br />
(cleaning practices) as well as educating families and staff about<br />
the importance of proper hand washing and empowering them to<br />
address improper practices.” Michele said this is discussed in the<br />
staff’s quality meetings with the focused on reducing the hospital<br />
acquired infections on their unit. Michele said that they have<br />
had numerous patients on the unit that have been transferred or<br />
admitted and appropriately identified by staff as having C-diff on<br />
admission or transfer. Michele feels the heightened education and<br />
empowerment on the part of her staff points to the success of<br />
the project.<br />
Hourly rounding to enhance response time to<br />
answering call lights: Team - Nurse Managers, Jim<br />
Giallella, Chris Moden, Debbie Boss and supervisor, Sofia<br />
Arutunian<br />
Our group wanted to make an impact on patient<br />
satisfaction at <strong>Kaleida</strong> <strong>Health</strong>. Understanding the patient<br />
experience and measuring patient satisfaction is becoming<br />
increasingly important as healthcare organizations strive<br />
to improve processes, become more patient focused/<br />
patient centered and improve profitability. The team did<br />
patient rounding on 13 North as an opportunity to gain<br />
information about the patient’s perceptions and then met<br />
with staff to introduce the project, brainstorm, identify<br />
barriers and engage the stakeholders. The question on<br />
the patient focused survey was: “After you pressed the<br />
call button, how often did you get help as soon as you<br />
wanted it?”<br />
Purposeful hourly rounding was implemented to improve<br />
the identified patients concern that this was not happening<br />
on a regular basis, from their perspective. The availability<br />
of a nurse and nursing presence at the bedside are known<br />
predictors of patient satisfaction. Routine purposeful<br />
rounding is when a nurse or member of the nursing<br />
team goes into a patient’s room every hour to assess and<br />
meet patient needs proactively. Because patients perceive<br />
their needs are being met in a timely manner, it fosters<br />
satisfaction with their care. In addition, the team provided<br />
customer service training (Achieving Service Excellence)<br />
which took approximately 45 minutes to one hour per<br />
session and included using the AIDET tool.<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
17
Throughout the training, the team was able to interact with the<br />
staff and reaffirm the need to be responsive in answering call<br />
lights and anticipating a patient’s needs. The team stressed to<br />
the staff that the implementation of hourly rounding, timely call<br />
light response and better teamwork/communication would serve<br />
two purposes. First, it would have an immediate impact on the<br />
Press Ganey scores as they relate to the promptness of call light<br />
response and second, it would actually decrease their workload.<br />
This new approach of asking patients if they needed anything else<br />
before they left the room, identifying when they would be back to<br />
see them again and the increased awareness of the team concept<br />
would increase job satisfaction and better teamwork would<br />
decrease individual work.<br />
Measurement of Success: the team continued to monitor the Press<br />
Ganey Survey results through the process. Baseline,<br />
year to date (YTD) survey results specific to this<br />
question was 76%. After the staff meeting and<br />
brainstorming session, just bringing the problem<br />
to light for the staff, the results improved to 84%.<br />
After implementing purposeful hourly rounding, the<br />
September results were 79%. October results were<br />
87.5%, the YTD results were 79.5% or an increase<br />
of 3.5%. Now, the challenge is to maintain the gains.<br />
Staff has asked for ongoing staff meetings to keep<br />
focused on patient satisfaction and achieving service<br />
excellence (customer service). They realize that the<br />
implementation of this plan was just the beginning<br />
of the process and have concerns about maintaining<br />
the momentum and how to deal with those staff<br />
members who remain resistant to change.<br />
Daemen Leadership Cohort I Scholarship recipients with<br />
Mary Beth Campo; front row: Linda Eschberger, Mary<br />
Beth and Sue Brooks - back row, Sandy Boneberg, Peggy<br />
Schlotterbeck and Michele Hubert<br />
Stroke Nurse Manager is one of first Scholarship<br />
Recipients and Graduate of the <strong>Kaleida</strong> Daemen<br />
Leadership Program<br />
Ask Sue Brooks what is different about her since starting as a<br />
part of the then pilot, Cohort I (we are now into Cohort IV), in<br />
the annual <strong>Kaleida</strong> Daemen Executive Leadership and Change<br />
program, and she might reply, “Everything. The program taught<br />
me how to think differently, to develop a perspective that includes<br />
that of my team, our patients and other departments. It opens up a<br />
myriad of possibilities on finding the best solution, not limited by<br />
one perspective. I have also understood the value and importance<br />
of a shared vision with concrete measurable goals for the team.<br />
You can’t improve if you don’t know where the bar is set. As with<br />
understanding the value of multiple perspectives, I am now acutely<br />
aware that there is not a singular path to<br />
goal achievement and everyone on the<br />
team has something to offer on the best<br />
way to get there.”<br />
Sue says she has come to believe that<br />
a lot of leadership is communicating,<br />
communicating, communicating and<br />
making sure the message you sent is<br />
what your team receives. She is also<br />
committed to be empowered, knowing<br />
this is critical in order to pass the<br />
empowerment on to her staff. She<br />
feels one of the perks of investing and<br />
developing her team is that they in turn<br />
develop and challenge her professional<br />
growth. Sue is thrilled that several of her<br />
staff members have returned to school<br />
18 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
and shared with Sue that it was her example that motivated them<br />
to do so. Sue had one of her long-term nurses, 20+ years, complete<br />
her BSN recently and she says, “I couldn’t be prouder of her.”<br />
Sue shares that her change in thinking and “doing” has impacted<br />
her personal life as well. As mom to three boys, Sue has role<br />
modeled the importance of being a continual learner. She also<br />
says her boys, whom she sees as natural leaders, have emphasized<br />
to her the importance of caring and compassion as a leader and<br />
agrees that by doing so, staff is likely to follow. To colleagues<br />
contemplating returning to school Sue shares, “find the time, there<br />
are plenty of reasons not to, but who you might become on the<br />
journey could be amazing.”<br />
Supporting the WNY and<br />
Global Community<br />
<strong>Kaleida</strong> Nurses Feed the WNY Community<br />
The idea for the Food Bank Holiday drive orchestrated by<br />
<strong>Kaleida</strong> nurses came from WCHOB <strong>Nursing</strong> Advisory Board,<br />
NAC, members Lisa Gunn Taylor<br />
and Michelle Szefler. Lisa and<br />
Michelle shared the information<br />
about WCHOB’s cereal drive with<br />
their NAC colleagues; the project<br />
supported by WCHOB’s Central<br />
Partnership Council benefited<br />
economically disadvantaged school<br />
age children who receive breakfast<br />
at school but do not receive this<br />
during the summer. The cereal<br />
NAC members with Polla Milligan-Food Bank of WNY<br />
drive is a national program originating with a consortium of<br />
children’s hospitals. WCHOB participated in this during this past<br />
summer (<strong>2011</strong>) via the Food Bank of WNY, which serves Erie and<br />
Niagara county residents. WCHOB readily embraced the idea of<br />
helping children and families with the most basic of needs, fighting<br />
childhood hunger. Over 100 boxes of cereal were collected in the<br />
week-long drive in June of <strong>2011</strong>.<br />
Polla Milligan from the Food Bank of WNY attended the<br />
September 6 NAC meeting and gave the group the background<br />
on hunger in WNY. Polla, who loves her job and thinks “it is<br />
the best job ever,” shared her respect and admiration for nurses<br />
who have the ability to make a significant difference in the lives<br />
of the community every day. Polla whose energy and passion is<br />
infectious, shared a bit of her background with the group.<br />
She started as a rock musician and lived and worked in<br />
L.A. for over 2 decades, making, according to Polla, “a<br />
lot of money” writing jingles. She had lived in Buffalo as<br />
a teenager when her father accepted a faculty position<br />
in the history department at UB. She graduated from<br />
Bennett High School and is most proud of her position<br />
as President of the Black Student Union; she says she has<br />
always been a great believer in causes. Polla left L.A. and<br />
returned to the WNY area to care for family. She can’t<br />
say enough about the Food Bank of WNY and through it<br />
NAC -WNY Food Bank<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
19
her ability to be part of ensuring that basic needs, such<br />
as food, are met for our community. A prolific grant<br />
writer, Polla is both creative and relentless in her passion<br />
for serving the food needs of our community; 93,000<br />
people receive food via the food bank monthly. The food<br />
bank serves Erie, Niagara, Cattaraugus and Chautauqua<br />
counties. It supports 385 agencies with food, including<br />
the “Meals on Wheels” program, after school programs,<br />
food banks, soup kitchens, City Mission, senior<br />
programs and group homes. Additionally they sponsor<br />
community gardens to help people grow their own<br />
fresh fruits and vegetables, a back pack program to send<br />
food home for the weekend to those children in the breakfast<br />
and lunch program. In the “back pack program,” the food bank<br />
provides food to fill a child’s back pack with nonperishable foods<br />
on Friday to ensure the child and the family have food to eat over<br />
the weekend; $385 supports one child and their family for a year.<br />
Polla goes into the school programs and educates children on<br />
nutrition and has cooking programs for adults in group homes on<br />
how to prepare nutritious meals on a budget. Anyone interested<br />
in more information on any of the programs can contact Polla<br />
at pmilligan@foodbankWNY.org. For every $1 donated the food<br />
bank is able to purchase 7 pounds of food. The drive ran from<br />
November 1, to the 14th with barrels at all five acute care sites.<br />
Thanks to the generosity of <strong>Kaleida</strong> employees, the holiday drive<br />
collected over 1290 pounds of food at the five sites with additional<br />
donations of cash and backpacks for the backpack program. NAC<br />
members placed this on screen savers, white boards and posted<br />
flyers thoughout their respective sites. Diana Kornacki had an<br />
immediate donation of 11 back packs for the back pack program<br />
and Rhonda Francis started a sign up list at MFSH for volunteers<br />
to work at the food bank.<br />
RN Nancy Reynolds in Rwanda<br />
<strong>Kaleida</strong> <strong>Health</strong> Helps Nurse with<br />
Mission to Train Nurses in Ruanda<br />
Nancy Reynolds grew up in Western New<br />
York and attended Holy Angels High School<br />
in North Buffalo prior to leaving for college in<br />
Canada. After completing her B.A. in Biology<br />
with a minor in Psychology, Nancy returned<br />
to Buffalo to complete a BSN at D’Youville in<br />
1981. Her first position was a staff nurse at<br />
BGH on a med-surg unit. Nancy says she knew<br />
during her years at D’Youville her decision to<br />
switch her original career goal from medicine to<br />
nursing was correct: “I was surrounded by nursing faculty at D’YC<br />
who had passion for what they taught and emphasized our ability<br />
as student nurses to make a difference. As a result, I was fully<br />
drawn into nursing.”<br />
Nancy’s first year at BGH was cut short when she married a<br />
man with a career in international banking. The family moved<br />
frequently, every 2-3 years for almost three decades spending<br />
time in, Toronto, Dublin, Trinidad, St. Marten, Grand Cayman<br />
and London, where the family currently resides. Nancy said she<br />
worked as a nurse at Toronto’s Sick Children’s Hospital off and on<br />
for eight years as well as in the Caribbean for a number of years. It<br />
was challenging to work in<br />
hospitals in the Caribbean,<br />
Nancy says, as even with<br />
basic resources,<br />
equipment and<br />
technology,<br />
nursing education<br />
Nancy<br />
Reynolds<br />
in Rwanda<br />
20 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
and practice was not at U.S. standards or even clearly defined.<br />
Critical care for adults and pediatric patients was limited; as a<br />
result patients requiring this level of care often had poor outcomes.<br />
It was the impact of the educational and<br />
economic disparities in the Caribbean,<br />
and facing them on a daily basis, that left<br />
Nancy feeling a need to “do something.”<br />
She initially became involved in teaching<br />
literacy skills in the hills of Trinidad.<br />
According to Nancy, these were the people<br />
who worked as gardeners and maids and<br />
lived in abject poverty. By teaching them<br />
to read and write a minimum amount of<br />
new words a month, within 6 months<br />
they could read and write enough to fill<br />
out government forms that could enhance their<br />
quality of living and dramatically change their lives and that of<br />
their families. Nancy said this was so humbling for her – that<br />
just the most basic of vocabulary could make such a profound<br />
difference; how could she not help?<br />
In 2009, Nancy and her husband had the opportunity to travel<br />
to Kenya for two weeks. Her intent and that of the business<br />
organization she traveled with, was to set up a clinic on Lake<br />
Victoria for an isolated population of 5,000 women and children<br />
with multiple health issues including rampant AIDS. It was a side<br />
trip to Rwanda that changed Nancy’s mind and her “mission.”<br />
Her group was able to meet with the President of Rwanda and<br />
his cabinet. She was impressed with his focused desire for<br />
development of his people and his country and his abhorrence of<br />
corruption. In a subsequent visit with the Director of <strong>Nursing</strong> in<br />
Gates 7 West Staff with Nancy Reynolds<br />
Rwanda, Nancy was told that, if she, and the group she is working<br />
with, really wanted to make a difference, not to set up a clinic to<br />
care for people, but to assist in the building of nursing capacity<br />
and capability, and help them take care of their own. This made<br />
so much sense to Nancy and was so<br />
different from the corruption and lack<br />
of progress in parts of Kenya, that<br />
she knew she wanted to work with<br />
the Director of <strong>Nursing</strong> in Rwanda:<br />
training nurse educators who could in<br />
turn train other nurses.<br />
In Rwanda, the 1994 genocide<br />
decimated the nursing population<br />
and education infrastructure; even<br />
today, there are only about 80 BSN<br />
prepared nurses for over 10 million people. In the courtyard of<br />
one nursing school she visited, a grave was in the center. When<br />
Nancy inquired why it was there, she was told it was the Director<br />
of <strong>Nursing</strong> killed during the genocide. The bulk of the country’s<br />
nursing workforce mainly consists of health care workers with<br />
2 to 3 years of high school education, with a total of one course<br />
with a nursing component, who are called nurses and who provide<br />
some form of health care. There is<br />
critical need for strengthening of<br />
nursing education. Many people<br />
in the rural populations are still<br />
dependent on traditional healers,<br />
often unsafe and with medically<br />
compromising results.<br />
Nancy Reynolds in a village in Rwanda<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
21
Nancy strongly felt she needed an advanced degree if she was<br />
going to teach nursing educators in Rwanda. She had been away<br />
from the bedside for almost two decades and enrolled in a RN<br />
refresher program with the University of Delaware as part of<br />
her first step toward obtaining her Master’s. She simultaneously<br />
applied to and was accepted into Georgetown University in their<br />
Master of Science in <strong>Nursing</strong> Education program. Her plan is to<br />
return to Rwanda and train nurse educators after completion of the<br />
program. It was while Nancy was looking for a clinical practice site<br />
as a requirement for her refresher program that she reached out to<br />
the system where she had first practiced and got a warm reception<br />
from the staff at Gates.<br />
Nancy readily shares how grateful she is to <strong>Kaleida</strong> and the staff on<br />
7W (now 14S-BGMC); “I was accepted right away and felt fully<br />
part of the staff.” Nancy says the quality of the experience on 7W<br />
offered “much better learning” then her traditional program, so<br />
she gives high marks to her time on 7W. Nancy says her preceptor,<br />
Theresa Morgan was terrific, a very gifted and competent teacher,<br />
and made her feel she could do this, safely and well. Her first few<br />
days were by Theresa’s side watching and learning. The first night<br />
shift she worked Nancy said she couldn’t even understand report<br />
but by day three this had changed for her. She said in precepting<br />
with the charge nurse she was able to see a broad picture and is<br />
emphatic about how positive it was: “If I was living in Buffalo, this<br />
is the staff I would want to work with,” Nancy shares.<br />
Nancy is excited about the opportunity for both her and her<br />
husband to help. Her husband is already working to help “develop<br />
entrepreneurs” and business acumen for the people of Rwanda as<br />
Nancy works to educate nurses. She says the President of Rwanda<br />
has reduced the percent of foreign aid to support his budget<br />
to 37% versus many other African countries where it is closer<br />
to 80% and higher. She loves his “can do” approach, built on<br />
education and expertise for his people. At <strong>Kaleida</strong> we are grateful<br />
to have been a part of Nancy’s vision and look for opportunities to<br />
continue to support this is the future. Nancy gave a talk with slide<br />
presentation to a group of <strong>Kaleida</strong> nurses on August 9th as her way<br />
of thanking us for the opportunity to complete her requirements<br />
for the clinical portion of her refresher course. The presentation<br />
included pictures of the Rwandan people Nancy hopes to help<br />
by supporting nursing training, standards and scope of practice.<br />
She has touched all of us and we welcome opportunities to make<br />
a difference in the nursing global community by supporting her<br />
mission.<br />
<strong>Nursing</strong> Education, Innovation,<br />
Quality and Research<br />
Education Update<br />
Jen Jennings, RN, FNP, DNP<br />
Manager of Clinical Education<br />
The changes occurring throughout our system, including<br />
the consolidation of campuses, has presented a number of<br />
opportunities for clinical educators to support the transition of<br />
staff into new roles, services and/or units. We have supported<br />
staff learning needs created by the integration of BGH and Gates.<br />
Through the creation of integration teams, the specialty educators<br />
are paired with specialty managers to focus on the “need to know”<br />
education, with particular attention paid to providing safe and<br />
competent care. Our projects have targeted bedside care, patient<br />
safety and best practice for caregivers. Interdisciplinary teamwork<br />
22 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
across the system has helped drive consistency in protocol and<br />
practice (based on national guidelines and best practice) for RNs<br />
and UAP. We have revised the glucometer recertification policy<br />
and engaged educators in working with managers and staff to<br />
devise a train the trainer program to ensure compliance with<br />
regulatory requirements across our acute care sites. This multisite,<br />
multidisciplinary task force<br />
is representative of laboratory<br />
leadership, clinical educators<br />
and union representatives from<br />
each <strong>Kaleida</strong> <strong>Health</strong> site. The<br />
old adage “The only constant is<br />
change” has been our mantra<br />
this past year and we have<br />
worked hard to embrace change<br />
together as a team, with a focus<br />
on working smarter not harder.<br />
Oishei Residency Planning Committee<br />
We continue to collaborate on chemotherapy education with<br />
our colleagues at Roswell. With the support of a nursing team of<br />
directors, managers and educators representing each site, we were<br />
able to forge a partnership, with RPCI nurses attending <strong>Kaleida</strong><br />
ACLS training and our KH nurses receiving chemo training, after<br />
successful completion of the Oncology Nurses Society (ONS)<br />
chemo program. A core group of educators have attended the<br />
training and follow-up practice in the Roswell out-patient chemo<br />
clinic, in order to trouble shoot and support staff who will be<br />
administering chemotherapy to <strong>Kaleida</strong> patients. They have<br />
designed some simulation education for our staff targeting chemo<br />
administration, potential complications and safe disposal of<br />
chemotherapeutic agents post infusion.<br />
Through best practice re-assessment, we have consistently<br />
reviewed the literature and collaborated with centers such as<br />
Johns’ Hopkins and Baylor to revise our Central Venous Line<br />
(CVL) removal practices for ICU RNs. This will ensure that we<br />
are cutting edge with evidence based practice and our patients are<br />
receiving the best and safest care. Orientation of our new nurses is<br />
being streamlined without reducing<br />
quality or effectiveness. Our <strong>Kaleida</strong><br />
<strong>Nursing</strong> Advisory committee,<br />
which includes chairs and Deans<br />
from WNY <strong>Nursing</strong> Programs, has<br />
been expanded to include nursing<br />
leadership from Roswell, CHS, VA<br />
and ECMC; our focus is creating<br />
educational assessments for senior<br />
nursing students that would<br />
enhance transition into practice<br />
anywhere in WNY. In response to an identified need, nursing<br />
education also designed a generic curriculum/template for onboarding<br />
new Nurse Practitioners.<br />
Mosby will become an enhanced database for our nurses and staff<br />
to access in 2012. A nursing focus group has worked diligently<br />
to link any unique <strong>Kaleida</strong> procedures to the corresponding<br />
Mosby policy for ease of use reducing duplication of resources<br />
in creating <strong>Kaleida</strong> policies that already exist in Mosby. Using a<br />
prospective approach, we will begin to analyze “Mosby updates”<br />
through specialty committee chairs for approval and the ability<br />
to “<strong>Kaleida</strong>size” the index located on the Mosby site. Once each<br />
committee examines the recommendations and analyzes the<br />
evidence, they will then approve, disapprove, or approve with KH<br />
updates or nurse alert. Staff will have to rely less on lengthy policy/<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
23
procedures and can access Mosby, best practice based and user<br />
friendly, to identify the KH approved procedures.<br />
Educators are also involved in nursing research that has the<br />
potential to reduce costs and improve care. We look forward to<br />
enhanced technological advancements, such as our bar code<br />
scanners, to scan employees ID badges and be uploaded directly<br />
to Talent Management, reducing human error and enhancing<br />
efficiency. In addition, we are using “I clickers” to enhance<br />
participation in classroom activities, soliciting real time feedback<br />
and adjusting the education accordingly. Early in 2012 <strong>Nursing</strong><br />
Education moved from Gates to its temporary home at 1028<br />
Main Street.<br />
WNY Residency Program Begins Third year<br />
Michele Natwora, nurse educator under the guidance of Jessica<br />
Castner, took over coordination of the WNY Residency program<br />
in its second year which began<br />
in September of <strong>2011</strong>. The<br />
community collaboration with<br />
partners Roswell Park, VA and<br />
ECMC incorporated “lessons<br />
learned” in year one to modify<br />
the program in its second<br />
year. The Western New York<br />
Nurse Residency Program is<br />
an investment that supports<br />
the transition for new graduate<br />
nurses, which involves a<br />
steep learning curve which can be<br />
negatively impacted by personal stressors. The residency program<br />
continues to offer simulation in rapid response and code response<br />
preparation, along<br />
with providing<br />
education on the<br />
importance of self<br />
care for healthcare<br />
workers.<br />
The <strong>2011</strong>-2012<br />
WNY NRP<br />
cohort has 45<br />
participants from<br />
<strong>Kaleida</strong> <strong>Health</strong>.<br />
Oishei Resident with manager<br />
Participants continue<br />
to meet every other month with our community partners, in<br />
addition to meeting monthly as an organization. Included in<br />
the facilitation process this year, are past nurse residents, who<br />
associate their successful transition with attending the first nurse<br />
residency program with <strong>Kaleida</strong> <strong>Health</strong><br />
in 2010. They, along with their nurse<br />
managers, recognize the importance of<br />
supporting this transition and they assist<br />
with small group facilitation for the <strong>2011</strong><br />
group of nurse residents monthly. Mentoring<br />
continues to be an essential component<br />
of the residency program; an experienced<br />
nurse offering emotional support to enhance<br />
the mentee’s confidence and success. These<br />
partnerships ideally can be a career long<br />
Residency Coordinators Jessica Castner and Michele Natwora, with<br />
Connie Vari, UB faculty Linda Steeg and Mimi Haskins<br />
relationship and unlike that of a preceptor,<br />
does not necessarily end with orientation. The<br />
largest group of mentor volunteers came from our 2010 resident<br />
graduates. Nurse Residency Programs are identified as future best<br />
24 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
Educators Mary Marohn and Kelly Foltz-Ramos during<br />
Residency self care day<br />
practice and are being considered a requirement by the National<br />
Council of State Boards of <strong>Nursing</strong> for first license renewal.<br />
Changes to year two include, starting the program after orientation<br />
completion and nursing state board exams, NCLEX, creating<br />
more opportunities for Residents to network and share stories and<br />
utilizing first year “graduates” as mentors and program facilitators.<br />
Residency Self-help posters<br />
Manager of the CVICU and SICU<br />
is a Champion for the Oishei Residency Program<br />
Peggy Schlotterbeck is the manager of the CVICU and a strong<br />
believer in the Oishei nurse residency program. She believes the<br />
program assists the new graduate to effectively assimilate into<br />
practice. Peggy feels when that assimilation is into a critical care<br />
unit the residency program can be an essential tool to ensure<br />
success. Peggy says she is a bit in awe of the new graduate who<br />
wants critical care; she says she was not ready for it when she<br />
graduated from D’Youville College 28 years ago.<br />
Peggy feels the cohort model and the collaboration with ECMC,<br />
VA and Roswell provides the resident with a unique perspective;<br />
“the ability to learn from new nurses from around the WNY area<br />
makes for a great experience and a stronger resident.” She likens<br />
the residency program to giving residents the skills to “build<br />
skyscrapers.” She said some of her new graduates thought it was<br />
redundant but she encourages them to take advantage of the<br />
opportunity and feels the support for self reflection is important to<br />
enable new nurses to build a solid foundation from which to grow<br />
professionally.<br />
Peggy spent her first five years as a new graduate at the University<br />
of Virginia, first in neurology, and eventually in critical care. She<br />
worked as a travel nurse for 5 years before returning to Buffalo and<br />
taking a position in critical care at BGH. She’s worked in critical<br />
care education but feels management is where she can really make<br />
a difference. A member of the first Daemen /<strong>Kaleida</strong> Leadership<br />
and change cohort, Peggy was also one of the first scholarship<br />
recipients and completes her Master’s this month. She encourages<br />
<strong>Kaleida</strong> nurses, staff and managers to consider the program in<br />
which she says she has learned as much about herself as a leader<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
25
as she has about leadership theory. She feels she is a more effective<br />
manager and is conscious of how she questions her staff, such<br />
as, “in what way might we do this, rather then why are we doing<br />
this.” She says she has also learned not to sweat the small stuff.<br />
Peggy feels her staff is empowered and comes up with great ideas.<br />
They have been “Huddling” consistently for about 18 months. She<br />
says it is definitely hard wired in the CVICU where they huddle,<br />
as an interdisciplinary team, three times a day. Peggy shares she is<br />
so proud of her staff saying, “they come up with great ideas, they<br />
see the big picture of critical care needs not just the CVICU,” She<br />
is amazed at what they are willing to do to help. Peggy is currently<br />
working to hardwire Huddles into SICU practice.<br />
2010 Residency Graduate is now Mentor and<br />
Facilitator for <strong>2011</strong> Residents<br />
When requests went out to managers and 2010 resident<br />
participants for facilitators for the <strong>2011</strong> Residency group, Kristina<br />
Marquez, RN in the CVICU, wanted to volunteer. Her manager<br />
Peggy Schlotterback arranged<br />
her schedule so the one day<br />
per month of the program<br />
would be one of her work<br />
days. Kristina says, “Peggy is a<br />
strong supporter of education<br />
and looks for opportunities<br />
for her nurses to grow<br />
professionally via certification<br />
and formal education.”<br />
Kristina, a 2010 graduate<br />
of the University of Buffalo<br />
Kristina Marquez, WNY Nurse Residency facilitator<br />
and a participant in the first WNY Residency class, was a second<br />
career nurse. She had a Bachelor’s in exercise physiology and was<br />
a personal trainer before joining the Air Force where she served in<br />
Iraq as a respiratory therapist. She completed a Master’s in Public<br />
<strong>Health</strong> and then her BSN.<br />
Kristina admits the facilitator role was scary at first; she didn’t<br />
have any experience speaking in front of a group of people. She<br />
says she was a bit intimidated that so many people had so much<br />
clinical and teaching experience. However Kristina shared that<br />
“everyone went out of their way to make me feel comfortable and<br />
I had a ‘buddy/co-facilitator’ for the first session.” The skill stations<br />
were more comfortable for Kristina who says she can’t believe how<br />
much she has learned and grown in 18 months; “chest pain or<br />
cardiac, I’m amazed at how much I know.” Kristina says she has<br />
learned a lot from the educators, “they have such phenomenal<br />
clinical experience and are able to develop limitless scenarios.”<br />
Kristina says watching the new graduates has brought her first year<br />
as a new nurse full circle; “Wow, I realized now even more acutely<br />
that the fears, anxiety and lack of confidence is a global experience<br />
for all new graduates from across all facilities.” Observing these<br />
new graduates, Kristina states, validated the universality of the new<br />
graduate experience. “I am amazed where I am in just 18 months,<br />
I don’t worry that I will forget everything if I’m off for 2 days.”<br />
Kristina says the residency program is a critical part of successful<br />
transition and also gives credit for her transition into confident<br />
nurse to her two extraordinary preceptors, Carol Varga and Judy<br />
Lawson. Kristina says they are phenomenal and still support her,<br />
teaching when she gets a very complex patient. Carol just got<br />
her CCRN and Kristina received hers early in 2012. “I really feel<br />
confident in caring for patients and in teaching the new graduates<br />
how much I do know; it’s really neat, I really am a nurse!”<br />
26 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
DEU model encourages <strong>Kaleida</strong><br />
Nurses to continue their<br />
Education<br />
The DEU, Dedicated Education Unit, an<br />
innovative student nurse teaching model,<br />
celebrates the completion of its fourth<br />
year at <strong>Kaleida</strong>, this month. The model,<br />
just a decade old, was brought to the U.S.<br />
from Australia by Dr. Susan Moscato, professor<br />
emeritus of Portland University. At a conference last July in<br />
Portland, Dr. Moscato complimented <strong>Kaleida</strong> on its passion for<br />
the model and its ability to see a broader picture, partnering with<br />
multiple nursing programs and engaging other systems in DEU<br />
research and dialogue. Although formal research on the model is<br />
still limited, preliminary research does suggest that utilizing our<br />
expert nurses as CIs, clinical instructors, results in a 25% increase<br />
in RNs returning for BSNs and MSs on DEU units. We have seen<br />
a number of nurses through-out <strong>Kaleida</strong> and on our DEU units<br />
return to school for further education. The following are a few of<br />
your colleagues and their stories about why they are investing in<br />
themselves and their careers.<br />
During DEU orientation this past fall a panel of <strong>Kaleida</strong> nurses,<br />
nurse manager and CI’s from 9S shared their passion for the DEU<br />
model and what it does<br />
for the unit, the student<br />
and the CI. Ann Strong a<br />
seasoned 9S nurse and CI<br />
shared that the opportunity<br />
to guide and teach students<br />
Theresa Morgan, RN, Nancy<br />
Reynolds and Manager Sue Brooks<br />
and imbue high standards for<br />
patient care was important to<br />
her as a nurse. She also shared<br />
that the opportunity to role<br />
model professional passion<br />
to the students was equally<br />
important to her. Ann admitted<br />
that as a seasoned nurse who<br />
13 North DEU-student “Thank-You” to CI Laura Overhoff, Jim Giallella, manager<br />
CI, Josh Schouldice and faculty Theresa Arida<br />
has precepted “about a million<br />
nurses,” she was starting to get<br />
a bit burned out; the students reignited her passion for precepting.<br />
She also said she loves seeing the students gain confidence and<br />
lose their fear and truly become part of the team on the unit. She<br />
also notices the difference between first and second semester<br />
students, especially those who have been exposed to a DEU.<br />
Yasmine, a staff nurse at Gates, who also had her DEU experience<br />
there, said it was amazing and a lot of her confidence as a new<br />
graduate nurse came from the DEU experience. Marlene Schiferle,<br />
the nurse manager on 9S, said it is truly a partnership between the<br />
faculty members, managers, CIs and students. Everyone has to<br />
be committed to making it work; having staff prepared to be a CI<br />
both through the <strong>Kaleida</strong> preceptor program, the academic partner<br />
orientation and non CI staff commitment to ensuring the CIs work<br />
the same days consistently during the semester. Faculty partners<br />
shared the “contagious” quality of DEU excitement; the ability for<br />
CIs to professionally develop new nurses is thrilling for faculty to<br />
observe. Another faculty member shared the ability of staff and<br />
faculty to better understands each other’s perspective, “we’re no<br />
longer guests, we’re part of the team.” Ashley a new nurse on 9S<br />
and a DEU student said the hardest thing after a DEU experience<br />
is not having another one. April, another 9S nurse from a DEU<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
27
experience, shared that her preceptor as a new graduate nurse,<br />
Marquita was also her CI when she was a student and it was,<br />
“wonderful.”<br />
Theresa Morgan has been a nurse for a short time but is passionate<br />
about nursing and the importance of continuing education. She<br />
serves as a CI, for the DEU on her unit 14S and loves her students.<br />
A 2008 graduate of Trocaire College with an AAS in <strong>Nursing</strong>,<br />
Theresa completed her BSN in May <strong>2011</strong>. Theresa started out at<br />
<strong>Kaleida</strong> as a CNA in 2006, became a LPN a year later, graduating<br />
from the LPN program at Trocaire. Theresa said her decision to<br />
return to school was about professional pride. She definitely feels<br />
the BSN program at D’YC has helped make her feel more prepared<br />
to deal with complex patients and nursing care in general. Theresa<br />
plans to continue her nursing education and perhaps teach<br />
nursing. Theresa says she has gotten “so much” out of each level<br />
of her nursing education and practice. She loves Bridge and the<br />
EMR and feels the impact they have on patient safety is critical<br />
and worth the challenges each presented initially. Theresa was<br />
the preceptor for Nancy Reynolds featured in, “<strong>Kaleida</strong> in the<br />
Community.” Theresa said she was so inspired by Nancy and<br />
her stories regarding nursing in Rwanda; the most basic safety<br />
equipment that we take for granted here is unavailable in third<br />
world countries like Rwanda. As a result there is a high incidence<br />
of nurses with needle stick injuries. The seriousness of this is<br />
further defined by the high number of AIDS and HIV patients in<br />
the general population. Theresa says the experience of precepting<br />
Nancy and hearing her stories, has made her value the resources<br />
we have for nursing practice, including Mosby’s. Theresa loves her<br />
unit, nursing and education and isn’t planning to stop anytime<br />
soon.<br />
Nurses returning for BSN Sue Brooks and<br />
Debbie Jankowiak<br />
Debbie Jankowiak is<br />
not new to nursing.<br />
She celebrates her 27th<br />
year as a professional<br />
nurse this month,<br />
graduating from ECC<br />
in 1984. Debbie’s first<br />
RN position was as a<br />
substitute school nurse<br />
and she also worked<br />
in LTC prior to joining<br />
<strong>Kaleida</strong> in 2005 at<br />
BGH. Debbie said she was attracted to the 12-hour shifts offered<br />
at Gates and transferred to 7W in 2006 to work them. Debbie left<br />
briefly to work on a telemetry/cardiac floor at MFSH but said she<br />
missed the patients and her colleagues “too much” and returned<br />
to 7W, now 14S. She “loves her stroke patients.” She feels there is<br />
so much to learn and she enjoys this. Debbie has been a CI on her<br />
unit since its inception and said it was one of the motivators for<br />
her to return to school for her BSN. Debbie says she had previously<br />
made a few attempts to return to school, but the time wasn’t right.<br />
She says working in the role of CI made her feel she needed the<br />
same educational preparation as her BSN students. Debbie says<br />
she encourages her colleagues to consider returning for their BSN<br />
and loves the program at Daemen College where she feels she has<br />
learned the importance of nursing research, particularly at the<br />
bedside. Graduating this past December, Debbie is thrilled about<br />
her accomplishment and shares her gratitude for the support her<br />
manager, Sue Brooks has supplied. The fact that her manager was<br />
also a student was inspirational; role modeling the importance of<br />
education at every level.<br />
28 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
DEU Experience<br />
for 13 North Nurse<br />
Comes Full Circle<br />
Laurie Overhoff, a 2010<br />
D’Youville College graduate,<br />
became a DEU CI this<br />
past September of <strong>2011</strong>.<br />
“In just a short time I’m<br />
helping students learn, it’s<br />
unbelievable,” Laurie shares.<br />
She was hired on 13 North in<br />
September of 2010; it was the DEU unit where Laurie had her<br />
senior experience and where she wanted to work. Josh, Laurie’s<br />
preceptor as an orientee on 13 N, was a clinical instructor, CI,<br />
when Laurie had her DEU experience there. Laurie says when the<br />
DEU faculty, Theresa Arida (her former professor), asked her to<br />
consider becoming a CI, she was honored. Laurie said the idea that<br />
she had something to offer new nurses and could help them learn<br />
was very satisfying. “Having the students ask me questions and<br />
look up to me makes me realize how far I have come in a short<br />
period of time,” Laurie explained. Laurie said she also thinks the<br />
students find it reassuring that she was so recently a student from<br />
the same program.<br />
About future goals Laurie is uncertain, she says she<br />
loves her floor and can’t imagine moving away from the<br />
bedside. Laurie says she works at being a team player<br />
and keeping good working relationships with all of her<br />
colleagues. She admits it can be challenging but believes<br />
in honesty and respecting her colleagues by sharing her<br />
concerns directly with them. Laurie says her manager<br />
Jim Giallella, 13 N Clinical Instructors and students with Laurie<br />
Overhoff (front center)<br />
Jim Giallella is great, “he speaks a lot to us about the<br />
importance of teamwork and dealing with conflict.”<br />
Laurie is considering joining her UPC in the future; she<br />
is currently the rep for the skin care team on her floor.<br />
When asked what she would say to someone<br />
considering becoming a CI, Laurie replies “it’s the<br />
opportunity to help someone be a better nurse. You can<br />
give a student a lot of confidence and an experience so<br />
much better then the traditional model where students<br />
spend a lot of their time waiting for the instructor.” In<br />
the DEU model, Laurie explains, “you really get to see what a<br />
nurse does and feel like part of the team.” To her students Laurie<br />
says she tells them, “I’ve been here over 18 months and I still ask<br />
questions; as a nurse you’re always learning.”<br />
Will I be Good Enough?<br />
Jessica Castner, RN, MS, CEN<br />
I was privileged to attend a recent Gates-BGH Central Partnership<br />
Council where frontline staff met to discuss some of their<br />
concerns about the upcoming integration of the two hospitals in<br />
an exercise led by educator Michele Natwora. A recurring theme<br />
in the discussion was nagging feelings of inadequacy as nursing<br />
staff imagine new work<br />
teams, patient populations,<br />
group norms and tasks<br />
that lay ahead. With<br />
compelling honesty, expert<br />
and experienced nursing<br />
Jessica Castner, Judy Laurenzi, Kelly<br />
Foltz-Ramos, Denise Sullivan and<br />
Bonnie Burmaster<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
29
staff who I admire implicitly revealed their doubts: Will I be good<br />
enough?<br />
The questions got me thinking about an inspiring nursing journey.<br />
Picture Mary Jo Satusky, a nurses’ nurse who needs to stand on a<br />
box to reach podium microphones. She had 20 years of nursing<br />
experience and had been prepared with a hospital diploma in<br />
nursing. Her husband’s job moved them around quite a bit; and<br />
she was faced with the challenge of starting in a new specialty with<br />
a patient population she’d had almost no experience: Orthopedics.<br />
Mary Jo took on the challenge and nagging doubts of inadequacy<br />
by studying for her certification in orthopedics, which she<br />
achieved two years after her new job in the specialty.<br />
Mary Jo didn’t stop at certification, like a gateway drug to learning;<br />
her journey for certification lit a fire for her to return to school<br />
for a bachelor’s degree in nursing and to take active roles in<br />
her nursing organization. Today, Mary Jo is the president of the<br />
National Association of Orthopedic Nurses. Keep in mind she<br />
started the journey because of a new job in a new specialty—an<br />
experience many <strong>Kaleida</strong> nurses are about to face. As I looked<br />
around the Gates-BGH Central Partnership Council, I got the<br />
chills imagining such an amazing journey may lie ahead for each<br />
and every member of the<br />
<strong>Kaleida</strong> nursing staff should<br />
they choose to take it—you are certainly good enough! You can<br />
learn more about Mary Jo’s story at www.nursingnoteslive.com<br />
We don’t have to look to the national stage for inspiring stories<br />
about certification and lifelong learning. Cheryl Marcel is a<br />
certified emergency nurse in the BGH emergency department.<br />
While she and fellow nurses did take a certification review course,<br />
Cheryl found that bedside nurses teaching bedside nurses was one<br />
of the most gratifying parts of the certification journey. A group<br />
of nurses got certification review books (thanks to a generous<br />
donation from a physicians group)–when one got stuck on a<br />
question or rationale, they would ask the other bedside nurses<br />
for input and encouragement. “We found it really empowered<br />
us to find our voice. We knew the rationale for what we were<br />
doing because of those questions and we could speak up for<br />
patients to teach patients, inform other nurses, or collaborate<br />
with physicians.” Peggy Schlotterbeck, manager of BGH CVICU,<br />
reports that a core group of certified critical care nurses in her unit<br />
are encouraging and mentoring a second cohort to study for their<br />
certification as well…Imagine how nurses could raise empowered<br />
voices and improve practice all over <strong>Kaleida</strong> if each unit had a core<br />
group of nurses just reviewing practice certification questions<br />
and rationales!<br />
Research on adult learning shows the number one motivator<br />
for new learning is a major change at work. The integration,<br />
and all the doubts that accompany the changes, can become a<br />
constructive experience for nurses who begin the certification<br />
journey. But many of us get hung up on a hate for exams and a<br />
fear of failure. Personally, I bought a certification review book to<br />
informally review the questions and rationales without intending<br />
to sit for the exam—the review was an excellent way to update my<br />
30 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
nursing practice.<br />
Like Mary Jo,<br />
my family had<br />
been relocated<br />
and I was having<br />
doubts that I was<br />
good enough or<br />
knowledgeable<br />
enough about the new patient population. I did eventually take<br />
the exam, six years later, and my CEN is my proudest credential to<br />
date.<br />
As a nurse, you can get board certified in medical/surgical,<br />
oncology, pediatrics, critical care, emergency, ambulatory care,<br />
and a myriad of other types of specialties. Many certifications are<br />
obtained through the ANCC (http://www.nursecredentialing.org) or<br />
through your specialty professional organization. Most bookstores<br />
offer nursing certification review books that offer an excellent way<br />
to start the journey at your own pace.<br />
The journey to certification can help answer the question with<br />
confidence, “Will I be good enough?” The answer is,<br />
certifiably, yes!<br />
<strong>Kaleida</strong> <strong>Health</strong> Coordinates BSN dialogue<br />
with WNY <strong>Health</strong> Care Systems<br />
On September 21st, Dr. Barb Zittell, formerly with the NY State<br />
Office of the Professions and for several decades, the authority on<br />
professional practice in NYS, visited Buffalo. She is the immediate<br />
past Executive Secretary to the NYS Board of <strong>Nursing</strong>. Zittell was<br />
responsible for licensure, scope of practice and discipline for over<br />
340,000 nurses. The trip was the first in NYS, with Buffalo as a<br />
pilot, for dialogue with health care leaders, Nurse Managers and<br />
staff nurses regarding the importance of the currently proposed<br />
legislation (BSN in Ten) to nurses, patient and families. Dr. Zittell<br />
shared her own entry into practice via an AAS program and her<br />
doctorate obtained after age 40. Dr. Zittell recently retired from<br />
the NYS Department of Education to promote the legislation. Jodi<br />
Witherell Director of Stoke services at <strong>Kaleida</strong> <strong>Health</strong> and current<br />
president of the local chapter of Nurse Executives and Diane<br />
Ceravolo, Director of <strong>Nursing</strong> Practice coordinated the event for<br />
the WNY area. Dr. Zittell was impressed with the collaboration<br />
among the WNY area nurse leaders and their support of nursing<br />
education. The<br />
Catholic <strong>Health</strong><br />
System, Erie County<br />
Medical Center and<br />
Roswell Park along<br />
with <strong>Kaleida</strong> <strong>Health</strong>,<br />
hosted Dr. Zittel in her<br />
day long lecture series.<br />
She began her day at<br />
Gates and shared data<br />
dating back to 2003<br />
with the Linda Aiken<br />
study which first identified<br />
reduced mortality rate in<br />
BSN in 10 event-back left to right: Cecilia<br />
Ahenkan, Theresa Morgan, Jodi Witherell,<br />
Mary Beth Campo, front left to right: Connie<br />
Vari, Claire Murray and Diane Ceravolo<br />
patients based on the percent of BSN graduates in an institution.<br />
The study was replicated in 2005 by Estabrooks, by Tourangeau in<br />
2007 and most recently by Blegen and Goode in 2009. Blegen and<br />
Goode’s 2009 study involved 21 US hospitals and results validated<br />
that hospitals with a higher portion of BS nurses had, lower rates<br />
of CHF mortality, fewer hospital acquired pressure ulcers and<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
31
lower rates of failure to rescue and shorter hospitalizations.<br />
Dr. Zittel also discussed the changes in nursing and medical<br />
technology, decreased lengths of stay, increase in multi cultural<br />
patients, required increased educational preparation in order<br />
to competently practice safe and quality care. She pointed to<br />
pharmacists and physical therapists who increased their education<br />
from a bachelor to doctorate level as a result of the increase<br />
in information and skill required to be competent; the drug<br />
formulary increased from 6,000 to 12,000 medications. She also<br />
shared the trend internationally to move nursing to a four-year<br />
degree. England and the European Union, Australia, Canada<br />
and the Philippines all require a BSN as entry into practice.<br />
Dr. Zittel recognized the importance of allowing perspective<br />
students to access nursing through both AAS and BSN programs.<br />
She emphasized the positive impact all nurses, diploma, AAS,<br />
BSN and advanced degree nurses have on patient care and the<br />
profession. We are fortunate in WNY to have a number of RN<br />
to BSN programs for nurses to select from, many programs offer<br />
a one day option plus on-line courses to accommodate adult<br />
learners and minimize impact on personal responsibilities. AAS<br />
and BSN program faculty participated in the event and highlighted<br />
their desire to support current nurses who want to continue their<br />
education. They asked the audience of staff nurses how they can<br />
make it easier for them to return to school. One of the staff nurses<br />
currently enrolled in a BSN program said, “Treat us like colleagues,<br />
help us with acquiring high school transcripts and filling out a<br />
FASFA and make class scheduling reflect personal responsibilities<br />
of adult and working students.”<br />
The BSN in Ten legislation (giving nurses 10 years from date<br />
of implementation to complete a BSN), which is before the NY<br />
State Senate and Assembly, would grandfather in all current<br />
nurses without a BSN, including any perspective students and<br />
those on nursing school waiting lists. It would not eliminate<br />
AAS programs but encourage them to partner with colleges and<br />
Universities as many in WNY already have, to allow AAS prepared<br />
nurses to easily transition post graduation and licensure into a<br />
BSN completion program. Theresa Morgan, a FT nurse on 14S<br />
(previously 7W at Gates) and an AAS and BSN completion student<br />
shared her story. Theresa, a recent AAS graduate completed her<br />
BSN in two years, combining FT work and school and caring for<br />
her two young children and husband. Theresa shared that she<br />
is a better nurse and a more confident bedside leader as a result<br />
of her BSN education. Although FT school, work and family<br />
were challenging, Theresa said that her investment in her career<br />
and education was a positive role model for her young children.<br />
Several BSN completion nurses shared that they hadn’t expected<br />
the ‘”degree” to change their practice and were surprised when<br />
it did. One of the Roswell Park nurses shared that she started<br />
out as a lab tech but wanted to be more involved with patients.<br />
After graduating from an AAS program and working on the Bone<br />
Marrow Transplant Unit, BMT, she said she knew she needed more<br />
education. She feels that not only did the BSN completion help<br />
her with leadership skills as both a charge nurse and a preceptor,<br />
but as a result of understanding the importance of, Evidence<br />
Based Practice and nursing research she is a “stronger, more<br />
compassionate and holistic nurse.” A nurse at ECMC shared that<br />
with the movement to interdisciplinary rounds everyone on the<br />
team had a minimum of a Bachelor’s education and she felt as a<br />
nurse and the only one with 24/7 oversight for the patient, she<br />
should have this as well. Debbie Heigel an ECMC nurse shared<br />
that her BSN education helped her become a “more articulate”<br />
32 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
voice to advocate for herself and her patients. Tina, a CHS nurse<br />
said the BSN made her feel empowered; she recently completed<br />
her BSN via the Roberts Wesleyan on-campus program. She<br />
shared that reading professional journals and now being able to<br />
understand them was a skill from her completion program. As<br />
a result, she said she feels as if she can do anything and is herself<br />
a champion for nursing education. Anyone interested in<br />
additional information on RN to BSN programs, e-mail<br />
dceravolo@kaleidahealth.org.<br />
Schwartz Rounds Keeping Compassion in<br />
<strong>Health</strong>care<br />
Schwartz Rounds ended<br />
the <strong>2011</strong> year in November<br />
with the topic of “Medical<br />
Error.” The panel<br />
comprised of a nursing<br />
supervisor, pharmacist and<br />
clinical nurse specialist<br />
presented a patient case in<br />
which the patient ultimately<br />
died due to an error in<br />
medication administration.<br />
The topic was a difficult one and several members of the audience,<br />
including house staff shared experiences where an error resulted<br />
in death. One attending discussed what she believed families need<br />
to hear after the loss of a loved one due to error. She said it is what<br />
she or any of us would need to find closure, the truth and as much<br />
transparency as we can provide and allow the family to “be.”<br />
Schwartz Rounds which began at WCHOB almost 2 years ago had<br />
its first “presentation,” at BGH in Swift Auditorium in July of <strong>2011</strong><br />
with 134 participants.<br />
The topic, “When patient<br />
outcomes are not what<br />
you or the patient hoped<br />
for,” was presented by<br />
a interdisciplinary team<br />
comprised of a nurse,<br />
chief resident, patient<br />
care liaison and PT.<br />
The panel discussed the<br />
challenges, frustrations and<br />
discouragement these incidents can create in caregivers. The<br />
second Rounds in September, “What do you do when you patient<br />
is afraid of dying?” captured 84 interdisciplinary staff members<br />
with a panel comprised of a nurse, housekeeper and family nurse<br />
liaison.<br />
The Rounds are supported by an endowment from the Schwartz<br />
Center in Boston, Massachusetts and supports healthcare facilities<br />
in providing “Rounds” through the subsidy of a lunch, to attract<br />
participants. Unlike clinically focused rounds, Schwartz Rounds<br />
provide a safe place for care providers to discuss the inherent<br />
challenges, frustrations and anxiety that caring for patients<br />
involves. The focus of the Rounds<br />
is not clinical, although a patient<br />
is presented, the focus is not about<br />
changing the outcome or doing a<br />
root cause analysis, but rather a<br />
Schwartz Center Rounds - Lem<br />
Mogavero-supervisor neuro, Cathy<br />
Papia-family liaison, Dr. Lucy Campbell-<br />
MICU, Father Richard Augustyn Back<br />
Row: Dr. Naughton, Dr. Brewer<br />
Schwartz Center Rounds-front left to right:<br />
Elaine David, Fannie White, Norm McCarter,<br />
back Dr. Brewer<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
33
discussion of how it made those<br />
involved feel. The audience is<br />
encouraged to share similar<br />
experience and feelings. Dr.<br />
John Brewer does a great job of<br />
facilitator and Dr. Robert Milch<br />
Schwartz Center Rounds is the moderator for the program.<br />
An interdisciplinary planning committee coordinates the Rounds.<br />
It is through this experience of providing a safe place to share<br />
feelings that the ability for staff to continue to be able to deliver<br />
compassionate care is supported. Rounds continued in 2012 with<br />
the first Rounds in January entitled, “When your patient is morally<br />
offensive to you.” Rounds are open to all staff, students and<br />
volunteers; CME credits are provided.<br />
Collaboration Results in Reduction of VAP rates<br />
at BGH and MFSH<br />
Deb Grande, ICU manager at MFSH,<br />
is thrilled with her team’s success with<br />
VAP rates. She ended <strong>2011</strong> with a less<br />
then 1% VAP (Ventilator Acquired<br />
Pneumonia) rate, a reduction from<br />
the 2010 rate of 2.48%. Deb shares<br />
her success with BGH MICU manager<br />
Pat Holtz who had, via Critical Care<br />
standards and with support from BGH<br />
pharmacist Kim Zimmit, developed<br />
a sedation protocol. The change in<br />
Debbie’s unit’s sedation protocol along<br />
with a “VAP Bundle” resulted in a significant reduction in MFSH’s<br />
ICU VAP rates.<br />
ICU Manager Deb Grande with MFSH ICU staff<br />
Pat Holtz shared that the Critical Care Standards Committee<br />
first started exploring the issue of sedation in 2010. Kim Zamet<br />
had found Vanderbilt Medical Center’s web site on delirium in<br />
reference to ICU ventilator patients, www.ICUdelirium.edu. Best<br />
practice suggested that drips such as Antivan and Versed, used to<br />
sedate ICU ventilator patients, increased the difficulty in weaning<br />
them from the ventilator and consequently increased vent days,<br />
LOS and increased the patient’s risk for VAP. Additionally, the<br />
web site research suggested that heavy sedation via IV drips could<br />
create episodic delirium up to 6 months after the sedation was<br />
discontinued. The new protocol decreased ventilator days and ICU<br />
delirium. Pat’s nurses, similar to Debbie’s, were not immediately<br />
comfortable with the new sedation protocol. “It was a change in<br />
culture,” Pat states, “ICU nurses want their ventilator patients<br />
to be comfortable for effective ventilation and they associate this<br />
with sedation.” Utilizing the same drugs except in bolus form in<br />
the first 12 hours after intubation, the nurses<br />
have been able to minimize the use of drips and<br />
consequently have realized a reduction in VAP<br />
by 75% as well as LOS and vent days. In the first<br />
quarter of <strong>2011</strong>, Pat saw an increase in VAPS;<br />
the committee reviewed their VAP bundle and<br />
added Chlorhexidine mouthwash to their oral<br />
care in addition to elevating the HOB higher than<br />
30 degrees, oral pharyngeal suctioning every 4<br />
hours, turning and positioning every 2 hours and<br />
early extubation. As a result of these changes,<br />
their rate went from 3.3 to 1.8 %. Pat’s VAP<br />
Bundle is slightly different then Debbie’s but she says the<br />
most effective items on the protocol are the simplest, keeping the<br />
HOB elevated and giving good oral care with suctioning.<br />
34 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
Like Pat’s Bundle, Debbie’s protocol includes<br />
minimizing the use of drips such as Versed<br />
and instead prescribing them as prn. She has<br />
also realized a reduction in total vent days.<br />
Debbie had sent several of her nurses to the<br />
MICU in the spring of 2010 to observe the new<br />
sedation protocol and VAP Bundle. Debbie’s<br />
nurses rounded with the physicians and MICU<br />
nurses and were able to see and verbalize the<br />
impact of the change in the sedation protocol<br />
on the vent patients. Debbie said her experience<br />
in rolling it out in her unit met with some of the<br />
same resistance, for the same reasons, as Pat’s did; nurses were<br />
concerned that the patients wouldn’t be managed as comfortably,<br />
might even be attempting to climb out of bed and pull at tubes<br />
and that families would be upset if patients were perceived to<br />
be less comfortable. Debbie thanks her clinical education team,<br />
Diana, Judy and Janeen for their help in educating staff on the<br />
new protocol. She said within a short period of time “everyone<br />
was a believer,” as patients were able to be extubated sooner and<br />
ICU length of stay started to drop as well. They saw no significant<br />
difference in the comfort level of patients with the change from<br />
drips to prn orders. Vent days dropped from 2,815 in 2010 to<br />
2,000 at the end of <strong>2011</strong>.<br />
Debbie charged her UPC with the job of assisting with the<br />
reduction of VAP rates. Unlike BGH, the suctioning sets at MFSH<br />
didn’t have a Y-connector so the staff used oral kits that had a<br />
compatible Y-connector. As a result it wasn’t a closed system;<br />
the team identified the opportunity to reduce infection rates by<br />
utilizing the same type of suction kits as BGH with a Y connector<br />
that was compatible and a covered Yankauer. Simultaneously, they<br />
Interdisciplinary focus changes MICU patient<br />
outcomes; Kim Zammit, Pharmacist; Dr. Lucy Campbell;<br />
Nurse Manager Pat Holtz and team<br />
introduced gloves for anyone entering the vent<br />
patient’s room, including MDs, x-ray techs and<br />
visitors; a sign on the patient’s door underscored<br />
these instructions. One of her team members,<br />
Jackie finished her DNP last semester and<br />
utilized the VAP Bundle as part of her thesis; she<br />
laminated the protocol and has it posted throughout<br />
the unit. Although Debbie and her team’s goal<br />
for VAP rates was “0” for the end of <strong>2011</strong>, she was<br />
thrilled to get it to less than 1%. MFSH presented<br />
these at Grand Rounds and the VAP bundle is<br />
available on talent management for the education<br />
of new critical care staff.<br />
Cardiovascular Open Heart Program going for<br />
Three Star Rating<br />
Our cardiovascular surgery program is .2% away from being<br />
a three star cardiac hospital, a national cardiothoracic surgery<br />
program designation awarded by the Society of thoracic surgeons<br />
for the quality of the open heart by-pass surgery program.<br />
Only 14% of all cardiothoracic surgery programs receive this<br />
designation. The turn around in the cardiothoracic program has<br />
been an intensive three year team<br />
approach connecting, pre-surgical<br />
and post-op aspects of care to<br />
minimize infection and reduce<br />
mortality rates.<br />
Cardiovascular Open Heart Program; left<br />
to right back: Judy Lawson, CCRN, Rachel<br />
Ludwig, NP, Caryla Clement, CCRN,<br />
Kristen Kennedy, RN, front Karen Camillo,<br />
Peggy Schlotterbeck<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
35
Peggy Schlotterbeck, CVICU nurse manager and her nursing<br />
team in the CVICU are thrilled. The team worked with their OR<br />
colleagues and under the leadership of NP Patti Arbogast, they<br />
discovered that deep sternal infections occurred in the OR, inside<br />
out, not post-op. Patti also worked on standardizing care for these<br />
patients with respect to dressing change, post-op care and added<br />
nasal swabbing to the pre-op checklist. They could identify MRSA<br />
pre-op and take precautions to avoid post-op wound<br />
infection by this organism. Having NP coverage 24/7<br />
in the unit has also enhanced the post-op care and<br />
follow-up for these patients. The ASCOM phones<br />
have enabled nursing staff to remain with the patient,<br />
providing care while they access the NP or physician<br />
for orders. SVO2 monitoring has taken cardiac<br />
output monitoring to the next level by providing<br />
trending read-outs that allow for more effective<br />
intervention and care. With the support of nursing<br />
leadership, Peggy was able to provide 1:1 nursing<br />
ratios for the first 4-6 hours after open heart surgery.<br />
Peggy said the nursing and medical staff also looked at the ability<br />
to limit overflow patients to those without infection or elevated<br />
WBC’s, use disposable EKG leads from OR to unit to floor. They<br />
also have changed the post-op placement of these patients to 13N<br />
versus on a general surgical floor such as 10S. Peggy is extremely<br />
proud of what the CVICU team has accomplished together. She<br />
points to the number of nurses who have received their CCRN,<br />
bringing the percent of CCRN certified nurse in the unit up to 30%<br />
including RNs, Caryla Clement, Judy Lawson, Carol Varga, Leithe<br />
Trapper, Kris Marquez, Laura Szczesniak, Karen Ryan and Lisa<br />
Berlinghoff.<br />
Left to right (standing): Deanna Galkiewicz,<br />
Glori Brucato, Gabrielle Sullivan, sitting: Ann<br />
Mallare and Sharon Logue<br />
MFSH Mother/Baby Unit Pilot Program<br />
becomes National Model<br />
The Mother Baby Unit at MFSH participated in a Department of<br />
<strong>Health</strong> initiative along with 10 other hospitals in NYS who had<br />
high breast feeding rates. The initiatives’ goal was to do even better<br />
with breastfeeding; to create exclusive units where breastfeeding<br />
was the norm. The impact of increasing breastfeeding has both a<br />
health and financial impact; if 90% of US families<br />
complied with medical recommendations to<br />
breastfeed for 6 months, the US could save $13<br />
billion per year and prevent almost 1000 deaths<br />
(NICH, NYSDOH). Breast fed infants have<br />
fewer infections including respiratory, GI, ear<br />
and more serious infections such as meningitis<br />
and septicemia. It can also provide protection<br />
against the development of diseases such as type I<br />
Diabetes, obesity, cardiovascular disease and certain<br />
childhood cancers such as leukemia, Hodgkin’s,<br />
nueroblastoma and Ulcerative colitis. Moms also<br />
realize personal health benefits with breastfeeding their infant.<br />
Breastfeeding decreases the risk for pre and post menopausal breast<br />
cancer and some forms of ovarian cancer.<br />
The unit employed a number of strategies to enhance breastfeeding<br />
rates, including, initiating breastfeeding within 1 hour post<br />
delivery, within 2 hours post delivery and breastfeeding exclusively<br />
throughout the stay, no formula supplements. Having the baby<br />
“room-in” with the Mom at least 9 hours out of a 12-hour shift<br />
was another strategy to enhance breastfeeding rates. Recently, the<br />
CDC began national roll out of this DOH initiative, called the NYS<br />
model.<br />
36 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
Recognition and Awards<br />
Mary Beth Campo was<br />
the recipient of the New<br />
York State Association of<br />
Nurse Executive’s Western<br />
Region leadership award.<br />
The award is given to<br />
nursing leaders who<br />
exemplify creative and<br />
contemporary leadership<br />
in nursing practice. Mary Beth<br />
was recognized for outstanding<br />
CNO’s recognize Mary Beth Campo at retreat<br />
left to right: Jodi Witherell, LuAnne Brown, Mary Beth<br />
Campo and Mary Beth Ferruggio<br />
leadership in the community and within <strong>Kaleida</strong>. Her leadership<br />
for innovative programs was noted, including the WNY Nurse<br />
Residency program, DEU teaching model, TeamSTEPPS initiatives<br />
throughout <strong>Kaleida</strong> as well as our mentorship and preceptorship<br />
programs. Mary Beth is past president of the WNY region of<br />
NYONE. <strong>Kaleida</strong> was also recognized for the third year in a row<br />
with the NYONE “Best Practice Award” for its Daemen leadership<br />
program targeted at growing bedside leaders. It won last year<br />
for the Communication initiatives and the previous year for the<br />
implementation of the DEU education model at all five sites.<br />
The <strong>Annual</strong> Education and Leadership Awards were given<br />
out at the 4th annual Leadership retreat this past December.<br />
Peggy Schlotterbeck received the Heart of <strong>Kaleida</strong> award for her<br />
compassionate leadership and commitment to excellence and<br />
to her staff in the CVICU. Peggy is currently the manager in the<br />
SICU and CVICU. Peggy has been a professional nurse for 28<br />
years and a <strong>Kaleida</strong> nurse for 20 of those years. She has 15 years<br />
of management experience, six years in her current role. Peggy is<br />
a true “nurse’s nurse who is respected by supervisors, physicians,<br />
and house staff and by all the nurses she manages, nurtures,<br />
support and coaches. She is passionate about nurses and nursing<br />
care. Peggy is a role model for professionalism, high standards<br />
and the importance of education. Peggy graduates from Daemen<br />
College with her Master’s in Executive Leadership and Change<br />
this month. She was in the first Daemen cohort and one of the<br />
first scholarship recipients. Peggy supported the implementation<br />
of the TeamSTEPPS Huddle in her unit and has been a consistent<br />
supporter of engaging her nurses in shared governance through<br />
ensuring they have time to attend UPC, CPCs, NAC, and the<br />
<strong>Nursing</strong> Executive Committee meetings. She is also a strong<br />
advocate for the Nurse Residency program. She is a highly visible<br />
leader who is willing to do whatever is needed to support her<br />
patients and staff.<br />
Michele Natwora received the Educator of the Year Award for her<br />
leadership during the past year, with EMR support, collocation<br />
activities, and oversight for the nurse Residency and orientation<br />
program. Michele has been a nurse educator for two years but<br />
is a seasoned <strong>Kaleida</strong> nurse with 21 years at BGH. In a short<br />
time, Michele has become one of the “go to” educators with her<br />
proactive approach to challenges and her “thank you for the<br />
opportunity,” response to requests for assistance. She has been an<br />
original and engaged member of NAC and a magnet champion.<br />
She has been supportive of nursing research, the mentorship<br />
program and feels personally responsible for the success of the<br />
new nurses under her care. She was a trainer for TeamSTEPPS and<br />
communication and exemplifies professional nursing passion and<br />
clinical competence.<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
37
The Level Five Leadership Award went to Terri Haist, manager<br />
of the MFSH OR. Terri has been a RN for 15 years. She started in<br />
a trauma/ortho unit at Temple in Philadelphia and then jumped<br />
at the chance for an OR internship at Baylor University in Dallas.<br />
Terri said her dream was always to become an OR nurse. She<br />
has been in the OR at MFSH since 1980, serving as manager for<br />
the past five years. Terri led her team through the OR renovation<br />
projects a few years ago when 10, state of the art rooms were<br />
added. The volume of cases in the OR at Suburban has increased<br />
by 31% over the last year, due in a large part to Terri’s leadership.<br />
She was a strong supporter of the DaVinci Robot project which has<br />
increased satisfaction at all levels. Terri manages a staff of 125 and<br />
is-on-top and current with evaluations. She is famous for her hand<br />
written notes to thank employees and recognize accomplishments.<br />
Terri also serves on the board of Directors for her local professional<br />
organization, AORN.<br />
Steve Handzel, behavioral health at BGH, was awarded Best New<br />
Manager. Steve is described as, “hitting the ground running,”<br />
in the short time he joined the management team in behavioral<br />
health. Steve started as a critical care nurse at <strong>Kaleida</strong> five years<br />
ago, went into nursing supervision at Gates and a year ago<br />
accepted his current position. Steve was new to behavioral health<br />
when he joined the team over 18 months ago but immersed<br />
himself in learning mental health laws and patient care needs.<br />
His willingness to go above and beyond extends to staff, patients<br />
and management. His innovation on the unit has led to improved<br />
patient care work flow. He worked around the clock on the EMR<br />
implementation and was instrumental in the successful DNV survey<br />
in <strong>2011</strong> for behavioral health. Steve’s colleagues say he exemplifies,<br />
“attitude is everything,” he is noted for his willingness to tackle any<br />
staff or patient need and always with a positive outlook and a smile.<br />
VNA Telehealth team: back row: Stephanie Haberl, RN, Lynn Larson, RN and Ed<br />
Green, LPN, front row: Shelee Basile, RN and Pam Hayman, RN<br />
Visiting Nurses Association<br />
of WNY<br />
<strong>2011</strong> VNA <strong>Nursing</strong> year in<br />
Review<br />
Lisa Greisler, RN<br />
VP, Clinical Services Home Care<br />
The VNA experienced another great year<br />
in <strong>2011</strong>, from financial performance<br />
and growth to satisfaction and patient<br />
outcomes. A few highlights are<br />
noted below.<br />
From a quality and satisfaction perspective, there were many<br />
successes. Like other healthcare organizations, CMS reports on the<br />
performance of home care agencies in relation to patient outcomes.<br />
These outcomes include specific performance measures such as<br />
improvement in ambulation and transferring as well as reduction<br />
38 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
in hospitalizations. Process measures look at<br />
processes of care such as assessment for falls<br />
risk and pressure ulcer risk assessments on all<br />
patients. Of the 22 patient outcomes and process<br />
measures, the VNA finished the year at or above<br />
the benchmark in 18 out of 22 with marked<br />
improvement overall. The results we have seen<br />
in our outcomes are a direct result of the care<br />
provided by our nurses and therapists through their<br />
focus on improving patient function, preventing complications,<br />
and keeping our patients safely in the community.<br />
Key quality measures for wounds were all at, or above, national<br />
benchmarks. These include measures related to pressure ulcers as<br />
well as surgical wounds. At the same time that patient outcomes<br />
in wounds improved, our wound specialists were able to decrease<br />
wound supply costs by $120,000 through utilization controls and<br />
best practices.<br />
On the satisfaction front, patient satisfaction results from Press<br />
Ganey showed that the VNA was at the benchmark of 86% for<br />
patients who would rate<br />
us a 9 or 10 and at 84%<br />
(above the benchmark<br />
of 82%) for patients<br />
who would definitely<br />
recommend the VNA<br />
to others. Our staff- led<br />
patient satisfaction<br />
committee was very<br />
creative again in <strong>2011</strong> in<br />
implementing measures<br />
VNA RN Teresa Skowronski with her patient.<br />
VNA Wound Team: Kelly Toporek, RN, Judy LeFevre, RN<br />
and Corrine Cintron, RN<br />
to improve patient satisfaction. As you can<br />
see from the results they were successful!<br />
Physician satisfaction for <strong>2011</strong> was at 98%<br />
while discharge planners indicated a 100%<br />
satisfaction rate. While a great deal of our<br />
quality focus for <strong>2011</strong> was on improving<br />
outcome and satisfaction scores, VNA staff<br />
also were in a preparatory mode for our<br />
accreditation survey. VNA made a decision<br />
to move to CHAP (Community <strong>Health</strong> Accreditation Program) as<br />
our accrediting body. This organization solely accredits home care<br />
organizations making this accreditation more aligned with our<br />
needs. Accreditation is only required for one small portion of the<br />
VNA business–we choose to be accredited in order to benchmark<br />
ourselves against national standards.<br />
From a growth perspective, the VNA saw tremendous growth<br />
across the organization in nearly all areas. Some branches, like<br />
Allegany and Niagara, experienced double digit growth in visits<br />
during <strong>2011</strong>! The Care Transitions program grew 270% and<br />
Telehealth grew to over 500 monitors<br />
(from around 400 the previous year). Care<br />
Transitions and Telehealth are two programs<br />
specifically designed to impact hospital<br />
readmissions, and both have been very<br />
successful in doing so.<br />
A very generous donation from the Ralph<br />
Wilson Foundation helped in providing a<br />
number of services including Telehealth,<br />
Adult Day Care, Lifeline, Medication<br />
Planners and Falls Prevention kits to a<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
39
number of needy patients. All of these tools are used to reduce<br />
patient risk, improve patient safety and avoid hospitalizations.<br />
The success of the VNA in <strong>2011</strong> is a result of the hard work of all<br />
of our staff from the drivers and warehouse staff; the clerical, office<br />
and administrative support<br />
staff; the Pharmacy, Lifeline<br />
and Home Care Services<br />
departments along with all of<br />
our nurses, therapists, home<br />
health aides and other clinical<br />
staff. The VNA team is excited<br />
about the opportunities that<br />
lie ahead for home care and<br />
are looking forward to a<br />
great 2012.<br />
VNA Expands into<br />
Steuben County<br />
The Visiting <strong>Nursing</strong><br />
Association of Western New<br />
York (VNA) was selected as<br />
the provider of choice to purchase<br />
the Steuben County Public <strong>Health</strong> & <strong>Nursing</strong> Certified Home<br />
<strong>Health</strong> Agency (CHHA) and Long-Term Home <strong>Health</strong> Care<br />
Program (LTHHCP). Steuben County is a large rural county<br />
located directly east of Allegany County on the Pennsylvania<br />
border. It includes the cities of Corning and Hornell and the<br />
Village of Bath. In 2010, the Steuben County Public <strong>Health</strong> &<br />
<strong>Nursing</strong> program performed over 22,000 home visits. The notfor-profit<br />
VNA will immediately start providing care in Steuben<br />
VNA RN Stephanie with her patient.<br />
County, beginning with a services and management agreement.<br />
The agreement will allow the VNA to employ nurses and therapists<br />
and supply them to Steuben County soon after January 1, 2012.<br />
“We are very excited to expand the VNA’s reach into Steuben<br />
County,” said Judy Baumgartner, VNA president. “It is heartening<br />
to know that another municipality has<br />
entrusted our organization to serve<br />
their community’s home health needs.<br />
On behalf of our dedicated nurses and<br />
staff, we are honored to be able to care<br />
for the residents of Steuben County.”<br />
VNA RN Amy Chandler with her patient.<br />
40 <strong>2011</strong> <strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
Long-Term Care<br />
<strong>2011</strong> was an exciting year for the <strong>Kaleida</strong> Long-Term Care<br />
sites. DeGraff Memorial’s Skilled <strong>Nursing</strong> Facility received<br />
the AdvisorMed “<strong>2011</strong> Great American <strong>Nursing</strong> Home<br />
Award” which places them among an elite group of nursing<br />
homes nationwide who consistently exceed their residents’<br />
expectations. The Deaconess<br />
Center was recognized in<br />
the US News & World <strong>Report</strong><br />
listing of “Best <strong>Nursing</strong><br />
Homes in <strong>2011</strong>.”<br />
The year ended with the<br />
opening of HighPointe on<br />
Michigan. On December<br />
3 and 4, Deaconess and<br />
Millard Fillmore Gates<br />
Skilled <strong>Nursing</strong> Facility closed their doors as residents<br />
and staff from both locations moved into their “new<br />
home” at 1031 Michigan Ave. HighPointe is a newly<br />
built 300-bed facility with 9 resident care areas<br />
including: sub-acute/rehab, adult ventilator, LTC pediatrics,<br />
adult medically complex LTC as well as dementia,<br />
memory and behavioral care units.<br />
Thank you to all of the long-term care RNs<br />
and LPNs for your continued dedication and<br />
commitment to our residents and the entire<br />
healthcare team.<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
41
Linda Browning•Mary Gebhard-Vandeusen•Blanche Junn•Tina Ford•Jeanine Funnell•Karleen<br />
Bordonaro•Nancy Martone •Jennifer Carroll•Diane Frankiewic<br />
•Diane Henninger•Jacqueline Sayeta•Michael Foley •Darlene<br />
Dolan•Jaclin Phillips•Wendy Green •Danielle Brodfuehrer<br />
•Elizabeth Nation•Jacqueline Tompkins•Shalondra Evans<br />
•Maureen Stroka•Amy Carlin•Sandra Leverenz•Karen Toye<br />
•Julie Chasey•Carol Heverin•Carrie<br />
LTC<br />
Peplowski•Mary Nowocien•Marie<br />
nurses...<br />
Thermidor•Dana Durkee•Cheryl Milijour•Teresa<br />
Zephro•Stacy Sperduti•Leslie Sweeney•Linda Lambe•Maureen Caruana•Susan Illig-Certo•Joan Hawco•Sandra Sopko•Eva<br />
Skompinski•Lorraine McLaughlin•Ralph Guastaferro•Maryalice Cislarski•Cynthia Pett•Heather Martindale•Gloria<br />
Porter•Deborah Buccilli•Mica Shegog•Patricia Nwokolo•Gertrude<br />
make<br />
Siaby•Donna Brown•Maria<br />
a<br />
Miles•Dorothy Leonard-<br />
Brucz•Janet Simmons•Michael Sayeta•Cheryl Brooks•Eve Evans•Shateeka Stevens•Dianna Harmon•Daria Harris•Ramona<br />
Richardson•Racheal Colom•Theresa Smart•Jamie Cunningham•Briana Campbell•Patrice Hennings•Kathleen<br />
Grzebinski•Roxane Amborski•Veronica Williamson•Willa Gibbs<br />
difference<br />
•Libby Vullo•Jessica Surles•Renee Taschetta•Nekeisha Thompson<br />
•Mieasha Walker•Kristin Matthews•Gabrielle Schwab•Tamara<br />
Besstak•Liza Baisa•Colleen McNatty•Patricia Heppner•Anita White<br />
•Darnelle Eady•Jennifer<br />
everyday!<br />
Barczykowski••Yvette Gilmore •Tamika Petty<br />
•Brandy Triplette•Julie Kuster•Dorena Wagner•Amanda Swain•Lacyana<br />
Boatwright•Bonnie Saraceni•Colleen Czerwiec•Tina Ojeda•Jody Mazurek<br />
•Roselyn Rust•Joanne Weber•Denise Hamilton•Renee Lane•Lisa Giglio•Lisa<br />
Drake•Jennifer Louie•Marlene Sims•Kathleen Semrau•Cynthia Kozlowski•Beula<br />
George•Rochelle McNeair•Lynette Williams•Sharon<br />
Watson•Natalie Galbo•Rosetta Heard•Heidi Bowens<br />
•Michael Howell•Kathleen Zwolak•Beatrice Lash•James Schichtel•Marilyn Jackson•Janet Plummer•Sandora<br />
Gray•Keira McGlothin•Shar’ron Young•Celia Borak•Amanda Catalano•Beverly Lynch •Sandra Bails<br />
•Annette Ford•Valerie Martin•Deborah Colkey-Johnson•Lynn Keith•Susan Farry•Bonnie Pirowski •Yalew<br />
Yohalashut•Maura Kelleher•Kevin Naffky•Jeanine Rhodes•Cierra Morrow•Lisa Stevens •Marisa Longacre<br />
•Hayley Guzowski•Teresa Thomson•Darlene Lozada •Linda Kelley•Donna Woroniecki•Danielle<br />
Conorozzo•Aida Babista•Shannon Nixon•Kristen Martin•Jennifer Arcovio•Rachel<br />
Collins•Taylor Chamberlain•Christina Wolf•Cheryl Serdin•Katherine Long•Seth<br />
Berchie•Martha Taylor•Lacheri Gordon•Lynn Flens•Elizabeth Mehltretter•<br />
42
thank you..<br />
Our sincere thanks to Connie Vari, RN, COO,<br />
retiring after 35 years of dedicated service<br />
to <strong>Kaleida</strong> <strong>Health</strong>. A true champion for<br />
nurses and nursing education.<br />
She will be missed by all.<br />
<strong>Kaleida</strong> <strong>Health</strong><br />
Editorial Staff:<br />
Nurse Recruiters<br />
Diane Ceravolo, RN, MS - Contributing Editor Buffalo General Medical Center/Gates Vascular Institute........Sandra Boneberg, RN ~ 716-859-4647<br />
Cherie Hepp, RNC, BSN - Editor<br />
DeGraff Memorial Hospital & SNF........................................ Maryellen Demmy, RN ~ 716-690-2136<br />
Mary Beth Campo, VP/CNO - Editor Ex-Officio HighPointe on Michigan...................................................................Cherie Hepp, RN ~ 716-878-7952<br />
Kerry Zilka - Graphic Designer<br />
Millard Fillmore Suburban Hospital....................................... Maryellen Demmy, RN ~ 716-568-3515<br />
Women & Children’s Hospital of Buffalo.........................................Cherie Hepp, RN ~ 716-878-7952<br />
Photos courtesy of <strong>Kaleida</strong> <strong>Health</strong> -<br />
VNA of WNY..........................................................................Candyce Thayer-Roselli ~ 716-630-8601<br />
Medical Photography and Diane Ceravolo<br />
and Lori Stoudmire, RN~ 716-630-8644<br />
For career opportunities visit our website at www.kaleidanursing.org<br />
43