Thermoregulation in the ICU MS.pdf - SASSiT
Thermoregulation in the ICU MS.pdf - SASSiT
Thermoregulation in the ICU MS.pdf - SASSiT
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
MGL Spruyt<br />
Dept of Critical Care<br />
University of <strong>the</strong> Free State<br />
<strong>Thermoregulation</strong> <strong>in</strong> <strong>the</strong> <strong>ICU</strong><br />
Physiology of <strong>the</strong>rmoregulation<br />
Heat ga<strong>in</strong>:<br />
cont<strong>in</strong>uous metabolic activity<br />
$ Physical activity<br />
$ Shiver<strong>in</strong>g<br />
$ Environment<br />
Heat loss:<br />
$ Conduction<br />
$ Convection<br />
$ Radiation<br />
$ Evaporation<br />
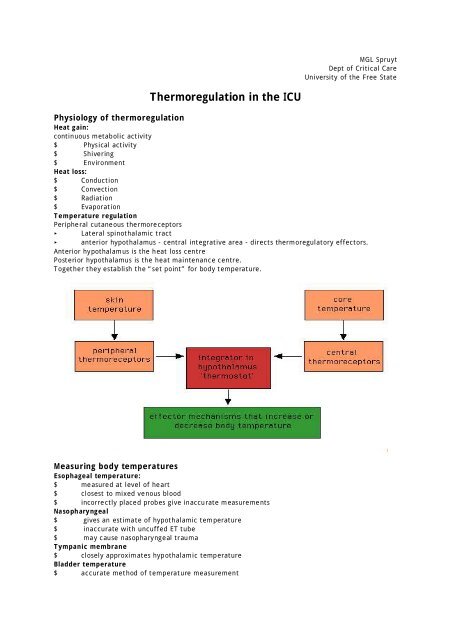
Temperature regulation<br />
Peripheral cutaneous <strong>the</strong>rmoreceptors<br />
Lateral sp<strong>in</strong>othalamic tract<br />
anterior hypothalamus - central <strong>in</strong>tegrative area - directs <strong>the</strong>rmoregulatory effectors.<br />
Anterior hypothalamus is <strong>the</strong> heat loss centre<br />
Posterior hypothalamus is <strong>the</strong> heat ma<strong>in</strong>tenance centre.<br />
Toge<strong>the</strong>r <strong>the</strong>y establish <strong>the</strong> “set po<strong>in</strong>t” for body temperature.<br />
Measur<strong>in</strong>g body temperatures<br />
Esophageal temperature:<br />
$ measured at level of heart<br />
$ closest to mixed venous blood<br />
$ <strong>in</strong>correctly placed probes give <strong>in</strong>accurate measurements<br />
Nasopharyngeal<br />
$ gives an estimate of hypothalamic temperature<br />
$ <strong>in</strong>accurate with uncuffed ET tube<br />
$ may cause nasopharyngeal trauma<br />
Tympanic membrane<br />
$ closely approximates hypothalamic temperature<br />
Bladder temperature<br />
$ accurate method of temperature measurement
$ <strong>in</strong>accuracies dur<strong>in</strong>g abdom<strong>in</strong>al surgery<br />
Rectal temperature<br />
$ affected by cool blood return<strong>in</strong>g from lower extremities, <strong>in</strong>sulation by faeces and heat<br />
produc<strong>in</strong>g bowel organisms.<br />
Oral temperature<br />
$ poorly reflects core temperature<br />
$ 0,3 - 0,6C below rectal temperature<br />
Axilla<br />
$ convenient<br />
$ very <strong>in</strong>accurate<br />
Sk<strong>in</strong> temperature<br />
$ <strong>in</strong>accurate<br />
Fever vs Hyper<strong>the</strong>rmia<br />
Fever<br />
Def<strong>in</strong>ition: State of <strong>in</strong>creased core temperature. The Society of Critical Care Medic<strong>in</strong>e def<strong>in</strong>es<br />
fever <strong>in</strong> <strong>ICU</strong> as temperature >38,3 C<br />
Febrile response (of which fever is a component):<br />
complex physiological response to disease consist<strong>in</strong>g of<br />
$ cytok<strong>in</strong>e-mediated <strong>in</strong>crease of core temperature set po<strong>in</strong>t.<br />
$ generation of acute phase reactions<br />
$ activation of physiological, endocr<strong>in</strong>ological and immunological systems.<br />
Hyper<strong>the</strong>rmia<br />
Unregulated <strong>in</strong>crease <strong>in</strong> temperature - pyroxenic cytok<strong>in</strong>es are not <strong>in</strong>volved <strong>in</strong> this process.<br />
$ standard antipyretics are <strong>in</strong>effective<br />
$ failure of <strong>the</strong>rmoregulatory homeostasis<br />
$ uncontrolled heat production<br />
$ <strong>in</strong>adequate heat loss<br />
defective hypothalamic <strong>the</strong>rmoregulation<br />
Hasday and Garrison CID 2000;31 (Suppl 5)
Significance of fever<br />
Benefits:<br />
Fever is an adaptive response to help rid <strong>the</strong> host of <strong>in</strong>vad<strong>in</strong>g pathogens.<br />
Increased temperature enhances <strong>the</strong> parameters of immune function:<br />
• Antibody production<br />
• T-cell activity<br />
• Production of cytok<strong>in</strong>es<br />
• macrophage function<br />
• Some pathogens (eg S pneumoniae) are <strong>in</strong>hibited by febrile temperatures<br />
Increased body temperature is associated with improved outcome from <strong>in</strong>fectious disease.<br />
• a positive correlation has been found between <strong>the</strong> maximum temperature on <strong>the</strong> day of<br />
bacteraemia and survival (Bryant)<br />
• fever associated with improved survival <strong>in</strong> patients with spontaneous bacterial peritonitis,<br />
polymicrobial sepsis, E coli bacteraemia and P aerug<strong>in</strong>osa sepsis.<br />
• conversely, retrospective studies have shown that human survival from serious <strong>in</strong>fections is<br />
reduced <strong>in</strong> <strong>the</strong> face of hypo<strong>the</strong>rmia (Tc41°C are usually<br />
due to non<strong>in</strong>fectious causes. Hypo<strong>the</strong>rmia, if associated with bacteraemia, signifies a poor<br />
prognosis.<br />
! Frequency<br />
Most patients have remittent or <strong>in</strong>termittent fever that, when due to <strong>in</strong>fections usually follow a<br />
diurnal<br />
variation.<br />
! Intermittent (septic, quotidian) fever with wide fluctuations may be due to localised<br />
pyogenic <strong>in</strong>fections and bacterial endocarditis, present<strong>in</strong>g with chills and<br />
leukocytosis.<br />
! Quotidian (daily spike), tertian(every third day) or quartan (every fourth day)<br />
commonly with leukopaenia, may suggest malaria.<br />
! A double quotidian pattern may be helpful <strong>in</strong> <strong>the</strong> diagnosis of salmonellosis, miliary<br />
tuberculosis, double malaria <strong>in</strong>fections, and Neisseria endocarditis.<br />
! <strong>in</strong>termittent hectic (Charcot’s) fever (sporadic episodes) is frequently seen <strong>in</strong><br />
cholangitis, usually associated with cholelithiasis, jaundice, leukocytosis and toxic<br />
signs.<br />
! Susta<strong>in</strong>ed (cont<strong>in</strong>uous) fever may be seen <strong>in</strong> patients with gram-negative pneumonia<br />
or CNS damage.<br />
! The time po<strong>in</strong>ts <strong>in</strong> <strong>the</strong> course of illness may provide diagnostic clues.<br />
! Pulse/temperature relationship<br />
Relative tachycardia (pulse <strong>in</strong>creased out of proportion to temperature) may po<strong>in</strong>t to a tox<strong>in</strong>mediated<br />
fever (eg gas gangrene) or non-<strong>in</strong>fectious causes.<br />
Relative bradycardia is an <strong>in</strong>dication of legionnaires disease or (<strong>in</strong> <strong>the</strong> presence of normal chest X-<br />
rays) drug fever.
! Fever defervescence<br />
Viral <strong>in</strong>fections tend to cause a slow defervescence of fever, while bacterial <strong>in</strong>fections show a<br />
prompt response to appropriate treatment. However, different <strong>in</strong>fections may respond differently<br />
to treament<br />
Post-operative temperature<br />
72% of fevers with<strong>in</strong> 48hrs after surgery are non-<strong>in</strong>fectious. (Garibaldi RA, Infect Contr 6:273,1985)<br />
Pulmonary atelectasis has classically been described as <strong>the</strong> cause of early potoperative fever, but<br />
more recent evidence has failed to demonstrate an association between atelectasis and body<br />
temperature <strong>in</strong> <strong>the</strong> absence of pulmonary <strong>in</strong>fection. (Engoren M. Chest 1995;107:81 - 4) A<br />
regulated elevation <strong>in</strong> <strong>the</strong> core temperature setpo<strong>in</strong>t occurs normally after surgery. The elevation<br />
is associated with <strong>the</strong> extent and duration of surgery, and with a cytok<strong>in</strong>e response, suggest<strong>in</strong>g that<br />
early postoperative fever is a manifestation of perioperative stress and tissue <strong>in</strong>jury.<br />
Frank et al found that approximately 25% of patient post-operatively had a core temperature<br />
38,5°C, suggest<strong>in</strong>g that <strong>the</strong> traditional def<strong>in</strong>ition of post-operative fever of 38,5°C is too<br />
str<strong>in</strong>gent.<br />
Drug fever<br />
Drug fever should be considered <strong>in</strong> patients with an o<strong>the</strong>rwise unexpla<strong>in</strong>ed fever, especially if <strong>the</strong>y<br />
are receiv<strong>in</strong>g -lactam antibiotics. Typically, drug fever presents with high spik<strong>in</strong>g temperature and<br />
shak<strong>in</strong>g chills, and may be associated with leukocytosis and eos<strong>in</strong>ophilia.<br />
Fever <strong>in</strong> neurosurgical patients<br />
The <strong>in</strong>cidence of pyrexia is <strong>in</strong>creased <strong>in</strong> patients with a Glasgow Coma scale of 2X). Fever <strong>in</strong> <strong>the</strong> bra<strong>in</strong> <strong>in</strong>jured<br />
patient exacerbates ischaemic neuronal damage and physiological dysfunction. Pyrexia affects <strong>the</strong><br />
acutely <strong>in</strong>jured bra<strong>in</strong> through several mechanisms:<br />
! <strong>in</strong>creased glutamate release, Oxygen free radical production<br />
! Augments permeability of <strong>the</strong> blood bra<strong>in</strong> barrier, <strong>in</strong>creas<strong>in</strong>g edme<br />
! <strong>in</strong>creases cyto-skeletal prote<strong>in</strong> degradation<br />
Fever <strong>in</strong> HIV <strong>in</strong>fected patients<br />
Fever is common <strong>in</strong> HIV <strong>in</strong>fected patients. The <strong>in</strong>itial acute <strong>in</strong>fection is characterised by a<br />
mononucleosis-like syndrome with fever. An acute febrile illness of 2 -3 weeks duration occurs 2-4<br />
weeks after seroconversion <strong>in</strong> 50 - 70% of HIV-<strong>in</strong>fected patients. The diagnosis may be established<br />
by demonstrat<strong>in</strong>g a high viral load comb<strong>in</strong>ed with negative or <strong>in</strong>determ<strong>in</strong>ate HIV serology followed<br />
by seroconversion. Approximately 20% of AIDS patients receiv<strong>in</strong>g trimethoprim-sulfamethoxazole<br />
develop fever, usually accompanied by a typical rash or pruritus. Fever <strong>in</strong> <strong>the</strong> subsequent course of<br />
HIV <strong>in</strong>fection usually represents superimposed complications of late-stage disease.<br />
Management of fever<br />
To treat or not: benefit vs risk<br />
Fever is a host defence mechanism. Temperature <strong>in</strong> <strong>the</strong> range of usual fever renders host defences<br />
more active and many pathogens more susceptible to defences. Temperature is also an important<br />
physical sign <strong>in</strong> <strong>the</strong> monitor<strong>in</strong>g of <strong>the</strong> response to treatment. Therefore <strong>in</strong> is recommended that<br />
febrile episodes should not be rout<strong>in</strong>ely treated with anti-pyretic <strong>the</strong>rapy; relative benefits and<br />
risks of treatment should be evaluated <strong>in</strong> every case.<br />
Fever should be treated <strong>in</strong> patients with acute bra<strong>in</strong> <strong>in</strong>sults, with limited cardiorespiratory reserve,<br />
and <strong>in</strong> patients <strong>in</strong> whom <strong>the</strong> temperature <strong>in</strong>creases above 40°C.<br />
Physical cool<strong>in</strong>g<br />
Hypo<strong>the</strong>rmia blankets, etc have been found to be no more effective than antipyretics. They may be
associated with large temperature fluctuations and rebound hyper<strong>the</strong>rmia. Due to <strong>the</strong> higher<br />
setpo<strong>in</strong>t, <strong>the</strong> patient already responds as if to a cold environment. External cool<strong>in</strong>g may lead to<br />
<strong>in</strong>creased hypermetabolism and persistent fever (Marik PE; Chest 117:3; March 2000), and <strong>in</strong>creased<br />
oxygen consumption. It is also associated with a significant <strong>in</strong>crease <strong>in</strong> adrenal<strong>in</strong>e and noradrenal<strong>in</strong>e<br />
levels. Lenhardt et al suggest that a more rational strategy for treat<strong>in</strong>g fevers unresponsive to<br />
antipyretic drugs is to promote heat loss by warm<strong>in</strong>g selected sk<strong>in</strong> surfaces, <strong>the</strong>reby reduc<strong>in</strong>g <strong>the</strong><br />
vasoconstriction and shiver<strong>in</strong>g thresholds associated with <strong>the</strong> elevated hypothalamic <strong>the</strong>rmal set<br />
po<strong>in</strong>t. (Lenhardt R et al Acta Anaes<strong>the</strong>siol Scan Suppl 1996;109)<br />
Antipyretics<br />
Antipyretics<br />
• do not lower temperature unless fever is present (ie elevated set po<strong>in</strong>t)<br />
• do not affect circadian rhythm of temperature.<br />
Most antipyretic drugs work by <strong>in</strong>hibit<strong>in</strong>g <strong>the</strong> enzyme cyclooxygenase and reduc<strong>in</strong>g <strong>the</strong> levels of PGE 2<br />
with<strong>in</strong> <strong>the</strong> hypothalamus. O<strong>the</strong>r mechanisms of action have been suggested, <strong>in</strong>clud<strong>in</strong>g <strong>the</strong> drugs’<br />
ability to reduce pro<strong>in</strong>flammatory mediators, enhance anti-<strong>in</strong>flammatory signals at sites of <strong>in</strong>jury, or<br />
boost antipyretic messages with<strong>in</strong> <strong>the</strong> bra<strong>in</strong>. Antipyretics <strong>in</strong> common use today <strong>in</strong>clude paracetamol,<br />
aspir<strong>in</strong> and o<strong>the</strong>r nonsteroidal anti-<strong>in</strong>flammatory drugs (NSAIDs).<br />
Cyclooxygenase<br />
The major mechanism of action of aspir<strong>in</strong> and o<strong>the</strong>r antipyretics <strong>in</strong>volves lower<strong>in</strong>g PGE 2<br />
by direct<br />
<strong>in</strong>hibition of COX enzyme activity. Sodium salicylate, aspir<strong>in</strong>’s major metabolite, exhibits similar<br />
antipyretic and anti-<strong>in</strong>flammatory properties as aspir<strong>in</strong> but only weak <strong>in</strong>hibition of COX-1 and COX-2<br />
<strong>in</strong> vitro.<br />
NSAIDs are also capable of reduc<strong>in</strong>g PGE 2<br />
production by down-regulat<strong>in</strong>g <strong>the</strong> expression of COX<br />
enzymes. Salicylates and some o<strong>the</strong>r NSAIDs like ibuprofen also work by prevent<strong>in</strong>g NF-B<br />
translocation <strong>in</strong> endo<strong>the</strong>lial cells and leukocytes. Indomethac<strong>in</strong> and <strong>the</strong>rapeutic doses of<br />
paracetamol, however, do not appear to affect NF-B.<br />
Noncyclooxygenase targets for antipyretics<br />
Some of <strong>the</strong> cl<strong>in</strong>ically useful actions of antipyretics may be COX <strong>in</strong>dependent, and with anti<strong>in</strong>flammatory<br />
effects seen only with doses much higher than required to suppress COX activity. For<br />
example, <strong>the</strong> also suppress tissue <strong>in</strong>flammation through dim<strong>in</strong>ished leukocyte-endo<strong>the</strong>lial cell<br />
<strong>in</strong>teractions, reduced pyrogenic cytok<strong>in</strong>e production or enhanced expression of anti-<strong>in</strong>flammatory<br />
molecules.<br />
Mechanisms such as boost<strong>in</strong>g <strong>the</strong> activity of endogenous antipyretic messengers have been described.<br />
Associated with <strong>the</strong> febrile response is <strong>the</strong> activation of multiple endogenous antipyretic systems<br />
that serve to suppress <strong>the</strong> magnitude or duration of fever. These <strong>in</strong>clude neuroactive substances of<br />
neural and humoral orig<strong>in</strong>, eg glucocorticoids, vasopress<strong>in</strong> and melanocort<strong>in</strong>s. It is thought that<br />
endogenous antipyretic systems protect <strong>the</strong> host aga<strong>in</strong>st <strong>the</strong> destructive effects of unchecked fever.<br />
The endogenous antipyretic substances participate <strong>in</strong> <strong>the</strong> antipyretic mechanism of salicylates and<br />
related NSAIDs, but not paracetamol.<br />
NSAIDs, particularly those with substantial COX -1 <strong>in</strong>hibition, are potentially damag<strong>in</strong>g to <strong>the</strong> kidneys<br />
and gastro-<strong>in</strong>test<strong>in</strong>al tract.<br />
Under conditions of decreased renal perfusion, <strong>the</strong> production of renal PGs serves as an important<br />
compensatory mechanism.<br />
Renal effects of NSAIDs are based on <strong>the</strong>ir pharmacologic mechanism of action. These effects are<br />
relatively mild and rare <strong>in</strong> healthy <strong>in</strong>dividuals but can be serious <strong>in</strong> patients whose renal function is<br />
prostagland<strong>in</strong>-dependent. Patients with contracted effective <strong>in</strong>travascular fluid volume are more<br />
likely to experience NSAID-related changes <strong>in</strong> renal function.
Acute renal failure with NSAID <strong>the</strong>rapy is mediated haemodynamically as a result of decreased renal<br />
perfusion after <strong>in</strong>hibition of prostacycl<strong>in</strong> syn<strong>the</strong>sis. Renal effects of specific COX-2 <strong>in</strong>hibitors seem to<br />
be similar to those seen with traditional NSAIDs.<br />
Very rare adverse renal effects of NSAID <strong>the</strong>rapy <strong>in</strong>clude nephritic syndrome and papillary necrosis.<br />
Acute <strong>in</strong>terstitial nephritis can develop at any time dur<strong>in</strong>g <strong>the</strong>rapy and is usually comb<strong>in</strong>ed with<br />
m<strong>in</strong>imal-change glomerulonephritis. The adverse renal effects of NSAIDs have been observed to occur<br />
more frequently under physiologic conditions that have been previously correlated with <strong>in</strong>creased<br />
dependence of renal function on Pgs.<br />
Certa<strong>in</strong> antipyretic drugs may cause coronary vasoconstriction <strong>in</strong> patients with coronary artery<br />
disease. Indomethac<strong>in</strong> has been shown to cause significant <strong>in</strong>creases <strong>in</strong> mean arterial pressure,<br />
coronary vascular resistance and myocardial arteriovenous oxygen difference. Therefore, myocardial<br />
oxygen demand <strong>in</strong>creases <strong>in</strong> <strong>the</strong> face of a decrease <strong>in</strong> coronary blood flow after adm<strong>in</strong>istration of<br />
<strong>in</strong>domethac<strong>in</strong>. (Friedman et al; NEJM 1981;305)<br />
Hyper<strong>the</strong>rmia<br />
Heat syndromes:<br />
! Heat cramps to heat stroke.<br />
Heat stroke is def<strong>in</strong>ed cl<strong>in</strong>ically as a core body temperature that rises above 40°C and is<br />
accompanied by hot, dry sk<strong>in</strong> and central nervous system abnormalities such as delirium, convulsions<br />
or coma. Heat stroke develops as a result of exposure to high environmental temperature or from<br />
strenuous exercise. Bouchama et al (NEJM 346:25; 2002) suggest an alternative def<strong>in</strong>ition: heat<br />
stroke is a form of hyper<strong>the</strong>rmia associated with a systemic <strong>in</strong>flammatory response lead<strong>in</strong>g to a<br />
syndrome of multiorgan dysfunction <strong>in</strong> which encephalopathy predom<strong>in</strong>ates.
Endo<strong>the</strong>lial-cell <strong>in</strong>jury and diffuse microvascular thrombosis are prom<strong>in</strong>ent features of heat stroke.<br />
The most serious complications <strong>in</strong>clude encephalopathy, rhabdomyolysis, acute renal failure, ARDS,<br />
myocardial <strong>in</strong>jury, hepatocellular <strong>in</strong>jury, <strong>in</strong>test<strong>in</strong>al ischaemia or <strong>in</strong>farction, pancreatic <strong>in</strong>jury and<br />
haemorrhagic complication, especially dissem<strong>in</strong>ated <strong>in</strong>travascular coagulation with pronounced<br />
thrombocytopenia.
Treatment of heatstroke<br />
The two ma<strong>in</strong> <strong>the</strong>rapeutic objectives <strong>in</strong> heat stroke are immediate cool<strong>in</strong>g and support of organsystem<br />
function. Therapeutic cool<strong>in</strong>g techniques are aimed at accelerat<strong>in</strong>g <strong>the</strong> transfer of heat from<br />
<strong>the</strong> sk<strong>in</strong> to <strong>the</strong> environment without compromis<strong>in</strong>g sk<strong>in</strong> perfusion. To overcome <strong>the</strong> cutaneous<br />
vasoconstriction and shiver<strong>in</strong>g result<strong>in</strong>g form rapid cool<strong>in</strong>g of <strong>the</strong> sk<strong>in</strong>, <strong>the</strong> patient may be vigorously<br />
massaged, sprayed with tepid water (40°C) or exposed to hot mov<strong>in</strong>g air. Antipyretic agents and<br />
drugs that accelerate cool<strong>in</strong>g are not useful <strong>in</strong> <strong>the</strong> treatment of heatstroke.<br />
Cool<strong>in</strong>g techniques<br />
Conductive cool<strong>in</strong>g<br />
External<br />
Coldwater immersion<br />
cold packs or ice slush<br />
Use of cool<strong>in</strong>g blankets.<br />
Internal<br />
Iced gastric lavage<br />
Iced peritoneal lavage<br />
Evaporative or convective cool<strong>in</strong>g<br />
Fann<strong>in</strong>g <strong>the</strong> undressed patient at room<br />
temperature (20°C - 22°C)<br />
Wett<strong>in</strong>g <strong>the</strong> body surface dur<strong>in</strong>g<br />
cont<strong>in</strong>uous fann<strong>in</strong>g<br />
! Neuroleptic Malignant syndrome<br />
N<strong>MS</strong> is a drug-<strong>in</strong>duced disorder present<strong>in</strong>g with rigidity, dysk<strong>in</strong>esia, rhabdomyolysis, hyper<strong>the</strong>rmia,<br />
changes <strong>in</strong> mental status, and autonomic nervous system <strong>in</strong>stability. It is uncommon but lifethreaten<strong>in</strong>g.<br />
The disorder is associated particularly with <strong>the</strong> use of antipsychotic, neuroleptic drugs.<br />
Treatment consists of immediate discont<strong>in</strong>uation of <strong>the</strong> suspected medication. Supportive care<br />
<strong>in</strong>cludes iv hydration, and monitor<strong>in</strong>g of cardiac rhythm, respiratory status and renal perfusion.<br />
Pharmacologic <strong>the</strong>rapy is aimed at <strong>in</strong>creas<strong>in</strong>g dopam<strong>in</strong>ergic activity with bromocript<strong>in</strong>e and<br />
dantrolene sodium.<br />
! Malignant hyper<strong>the</strong>rmia.<br />
MH is a life-threaten<strong>in</strong>g disorder occurr<strong>in</strong>g <strong>in</strong> susceptible patients after receiv<strong>in</strong>g <strong>in</strong>halation<br />
anaes<strong>the</strong>tics (eg halothane) and succ<strong>in</strong>ylchol<strong>in</strong>e. It presents with fever 40°C, muscle rigidity,<br />
tachycardia and tachypnoea. It affects multiple systems <strong>in</strong> <strong>the</strong> body and can lead to dissem<strong>in</strong>ated<br />
<strong>in</strong>travascular coagulation and precipitate seizures if not diagnosed and treated.<br />
Treatment<br />
Anaes<strong>the</strong>sia is discont<strong>in</strong>ued and <strong>the</strong> patient hyperventilated with 100% oxygen. Dantrolene sodium is<br />
given <strong>in</strong>travenously. Signs and symptoms can be manifested up to 12 hours after anaes<strong>the</strong>sia with<br />
causative agents.
Medications for treatment of<br />
hyper<strong>the</strong>rmia<br />
Convulsions<br />
Diazepam 5 - 20 mg iv<br />
Mannitol 1mg/kg to reduce cerebral edema<br />
Phenobarbital 130 - 260mg <strong>in</strong>itially iv<br />
Hypocalcaemia<br />
no treatment unless cardiac symptoms<br />
present<br />
Hypokalaemia<br />
Replace deficits carefully<br />
Myoglob<strong>in</strong>uria<br />
Mannitol 12,5g <strong>in</strong>itially iv, <strong>the</strong>n 12,5g/litre<br />
crystalloid.<br />
Ma<strong>in</strong>ta<strong>in</strong> ur<strong>in</strong>e output at 50ml/h<br />
Alkal<strong>in</strong>ise ur<strong>in</strong>e with bicarbonate<br />
Dialysis if <strong>in</strong>dicated
Hypo<strong>the</strong>rmia<br />
Medical illness<br />
Secondary hypo<strong>the</strong>rmia results when a disease state <strong>in</strong>terferes with <strong>the</strong>rmoregulation. Hypo<strong>the</strong>rmia<br />
may be associated with medical conditions such as sepsis, chronic heart failure, diabetes mellitus<br />
and hypothyroidism.<br />
Accidental<br />
! peri-operative<br />
! Exposure<br />
! Trauma<br />
Therapeutic.<br />
Hypo<strong>the</strong>rmia improves survival from many <strong>in</strong>sults. Studies have suggested benefit of <strong>in</strong>duced<br />
hypo<strong>the</strong>rmia applied <strong>in</strong> <strong>the</strong> <strong>ICU</strong> <strong>in</strong> traumatic bra<strong>in</strong> <strong>in</strong>jury and ARDS, and possibly anoxic bra<strong>in</strong> <strong>in</strong>jury.<br />
Potential applications <strong>in</strong> <strong>the</strong> <strong>ICU</strong> <strong>in</strong>clude:<br />
Neurosurgery<br />
! traumatic bra<strong>in</strong> <strong>in</strong>jury<br />
! Cerebral aneurysm<br />
Neurology<br />
! Anoxic bra<strong>in</strong> <strong>in</strong>jury<br />
! cerebral haemorrhage<br />
! Carbon Monoxide poison<strong>in</strong>g<br />
! status epilepticus<br />
! Air Embolism Syndrome<br />
General Surgery<br />
! burns<br />
Respiratory system<br />
! Acute respiratory distress syndrome<br />
! Asthma<br />
Cardiology<br />
! refractory tachyarrhythmias<br />
O<strong>the</strong>r<br />
! eclampsia<br />
! Sepsis syndrome<br />
The method of achiev<strong>in</strong>g reduction <strong>in</strong> body temperature, whe<strong>the</strong>r forced or regulated, may have a<br />
profound effect on <strong>the</strong> <strong>the</strong>rapeutic efficacy of hypo<strong>the</strong>rmia. Regulated hypo<strong>the</strong>rmia seems to be<br />
<strong>the</strong> best means of achiev<strong>in</strong>g <strong>the</strong>rapeutic benefit. Forc<strong>in</strong>g body temperature below <strong>the</strong> set po<strong>in</strong>t<br />
temperature results <strong>in</strong> an immediate response to <strong>in</strong>crease heat production and reduce heat loss. If<br />
body temperature were reduced by a regulated mechanism, <strong>the</strong> onset of <strong>the</strong> regulated hypo<strong>the</strong>rmic<br />
response would be characterised by peripheral vasodilatation, sweat<strong>in</strong>g and suppression of heat ga<strong>in</strong><br />
<strong>the</strong>rmoeffectors. Activation of physiological systems such as tachycardia, tachypnoea,<br />
corticosteroid and adrenal<strong>in</strong>e release would be expected to be m<strong>in</strong>imal dur<strong>in</strong>g regulated<br />
hypo<strong>the</strong>rmia<br />
Classification:<br />
! mild 32C - 35C<br />
! moderate 28C - 32C<br />
! severe < 28C<br />
Committee on Trauma of <strong>the</strong> American College of Surgeons<br />
!
Consequences of hypo<strong>the</strong>rmia<br />
Mild hypo<strong>the</strong>rmia<br />
• tachypnoea<br />
• vasoconstriction<br />
• tachycardia<br />
• ataxia<br />
• dysarthria<br />
• loss of f<strong>in</strong>e motor coord<strong>in</strong>ation<br />
• lethargy<br />
• confusion<br />
• shiver<strong>in</strong>g<br />
Moderate hypo<strong>the</strong>rmia<br />
• shiver<strong>in</strong>g stops<br />
• delirium<br />
• reflexes slowed<br />
• level of consciousness dim<strong>in</strong>ishes<br />
• bradycardia<br />
• J wavers on ECG<br />
• Cold diuresis<br />
Severe hypo<strong>the</strong>rmia<br />
• unresponsiveness or coma<br />
• hypotension very cold sk<strong>in</strong> pulmonary edema<br />
• acidaemia<br />
• may appear dead<br />
• ventricular fibrillation<br />
• loss of reflexes<br />
Hypo<strong>the</strong>rmia-<strong>in</strong>duced complications<br />
Myocardial Ischaemia<br />
High risk patients with only 1,3°C core hypo<strong>the</strong>rmia are three times as likely to experience adverse<br />
myocardial outcomes. Hypo<strong>the</strong>rmia causes hypertension <strong>in</strong> elderly patients and those at high risk<br />
for cardiac complications, and is associated with a threefold <strong>in</strong>crease <strong>in</strong> plasma noradrenal<strong>in</strong>e<br />
concentration which may <strong>in</strong>crease cardiac irritability and <strong>the</strong> development of ventricular<br />
arrythmias. (Frank et al JAMA 1997/Cl<strong>in</strong>Sci 1996; Anes<strong>the</strong>siology 1995)<br />
Coagulopathy<br />
Mild hypo<strong>the</strong>rmia <strong>in</strong>creases blood loss. (Schmied et al Lancet1996) Just 1,6°C core temperature loss<br />
may <strong>in</strong>crease blood loss by 500ml (30%). Hemostatic benefits are achieved by ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g<br />
<strong>in</strong>traoperative normo<strong>the</strong>rmia.<br />
Three mechanisms contribute to temperature-related coagulation disorders: platelet function,<br />
clott<strong>in</strong>g factor enzyme function, and fibr<strong>in</strong>olytic activity. In hypo<strong>the</strong>rmic coagulopathy standard<br />
coagulation tests, <strong>in</strong>clud<strong>in</strong>g <strong>the</strong> prothromb<strong>in</strong> time and <strong>the</strong> partial thromboplast<strong>in</strong> times, rema<strong>in</strong><br />
normal because <strong>the</strong> tests are performed at 37°C regardless of what <strong>the</strong> patient’s temperature is.
Fibr<strong>in</strong>olysis appears to rema<strong>in</strong> normal dur<strong>in</strong>g mild hypo<strong>the</strong>rmia but is significantly <strong>in</strong>creased dur<strong>in</strong>g<br />
hyper<strong>the</strong>rmia. Thromboelastography suggests that hypo<strong>the</strong>rmia impairs clot formation ra<strong>the</strong>r than<br />
facilitat<strong>in</strong>g clot degeneration.<br />
Wound <strong>in</strong>fection and Heal<strong>in</strong>g.<br />
Hypo<strong>the</strong>rmia impairs neutrophil function directly, or <strong>in</strong>directly by trigger<strong>in</strong>g subcutaneous<br />
vasoconstriction and subsequent tissue hypoxia. 1,9°C core hypo<strong>the</strong>rmia triples <strong>the</strong> <strong>in</strong>cidence of<br />
surgical wound <strong>in</strong>fection after colon resection. Hypo<strong>the</strong>rmia also <strong>in</strong>creases <strong>the</strong> duration hospital<br />
stay by 20% and aggravates postoperative prote<strong>in</strong> wast<strong>in</strong>g.<br />
Pharmacok<strong>in</strong>etics and pharmacodynamics.<br />
• The duration of action of muscle relaxants are generally prolonged <strong>in</strong> <strong>the</strong> presence of<br />
hypo<strong>the</strong>rmia.<br />
• The tissue solubility of volatile anaes<strong>the</strong>tics <strong>in</strong>creases with hypo<strong>the</strong>rmia, so that body<br />
anaes<strong>the</strong>tic content is <strong>in</strong>creased at subnormal temperatures. This does not alter<br />
anaes<strong>the</strong>tic potency but may slow recovery from anaes<strong>the</strong>sia because larger amounts of<br />
anaes<strong>the</strong>tic eventually need to be exhaled.<br />
Recovery duration and <strong>the</strong>rmal discomfort.<br />
• Mild hypo<strong>the</strong>rmia produces marked postoperative <strong>the</strong>rmal discomfort and may delay<br />
discharge of adult patient from <strong>the</strong> postanaes<strong>the</strong>sia care unit.<br />
M<strong>in</strong>or consequences<br />
• mild hypokalaemia<br />
• <strong>in</strong>creased cardiotoxicity of bupivaca<strong>in</strong>e.<br />
• Sufficient vasoconstriction result<strong>in</strong>g partly from hypo<strong>the</strong>rmia can obliterate <strong>the</strong> pulse<br />
oximeter signal.<br />
Treatment of hypo<strong>the</strong>rmia<br />
Accidental hypo<strong>the</strong>rmia<br />
Prognosis<br />
Patients found <strong>in</strong> a hypo<strong>the</strong>rmic situation should not be pronounced dead until reassessment after<br />
rewarm<strong>in</strong>g to at least 33°C.<br />
Mortality among hypo<strong>the</strong>rmic patients is variable (12 - 80%), and depends on <strong>the</strong> cause of<br />
hypo<strong>the</strong>rmia, <strong>the</strong> patient’s age and background, <strong>the</strong> delay before treatment, and probably<br />
sometimes <strong>the</strong> rewarm<strong>in</strong>g modality.<br />
Severity factors <strong>in</strong>clude old age, low blood pressure, low blood bicarbonate level, high SAPS II score,<br />
need for mechanical ventilation or vasoactive drugs, discovery of <strong>the</strong> patient at home, hypo<strong>the</strong>rmia<br />
not due to acute <strong>in</strong>toxication, and long delay before rewarm<strong>in</strong>g.<br />
The basel<strong>in</strong>e temperature is not a factor of poor prognosis accord<strong>in</strong>g to most studies. In trauma<br />
cases, however, retrospective studies have found an association between higher mortality and<br />
degree of hypo<strong>the</strong>rmia. Jurkovich et al (J Trauma 1987) found that no trauma patient whose core<br />
temperature fell below 32°C survived. The rewarm<strong>in</strong>g rate and <strong>the</strong> delay after <strong>the</strong> accident appear<br />
to be most important prognostic factors. In-hospital rewarm<strong>in</strong>g requir<strong>in</strong>g >12h is a grave prognostic<br />
sign. Major hyperkalaemia (>10mmol/l) is a factor of poor prognosis only <strong>in</strong> asphyxiated avalanche<br />
victims.<br />
Treatment<br />
Cardiopulmonary resuscitation should be <strong>in</strong>stituted if no pulse is present.<br />
• many arrhythmias convert spontaneously upon rewarm<strong>in</strong>g, and aggressive <strong>the</strong>rapy of m<strong>in</strong>or<br />
arrhythmias is not warranted. Transient ventricular arrhythmias, bradycardia or atrial<br />
arrhythmias should be ignored.<br />
• Defibrillate at 2 J/kg if <strong>the</strong> patient is <strong>in</strong> ventricular fibrillation or ventricular tachycardia,<br />
and promptly adm<strong>in</strong>ister amiodarone. Success rates of defibrillation are low if <strong>the</strong> core
temperature is less than 32°C.<br />
• If defibrillation fails, attempts should be repeated after every 1°C rise <strong>in</strong> body temperature.<br />
• Rapid fluid resuscitation usually is necessary because cardiovascular efficiency improves<br />
with crystalloid adm<strong>in</strong>istration.<br />
• Hypotension is treated by volume replacement and rewarm<strong>in</strong>g. Vasopressors should be<br />
avoided because <strong>the</strong>y have little effect on vasoconstriction secondary to hypo<strong>the</strong>rmia and<br />
can precipitate ventricular fibrillation.<br />
The cornerstone of treatment is rewarm<strong>in</strong>g <strong>the</strong> patient.<br />
Passive rewarm<strong>in</strong>g<br />
• Insulat<strong>in</strong>g or reflective blanket<br />
• Raise ambient temperature<br />
• keep patient dry<br />
Active external rewarm<strong>in</strong>g: External heat applied to <strong>the</strong> patient’s sk<strong>in</strong> <strong>in</strong> a non<strong>in</strong>vasive manner.<br />
• Immersion <strong>in</strong> water bath at 40°C (makes monitor<strong>in</strong>g and resuscitation difficult.<br />
• Radiant heat sources; heated blankets and heat<strong>in</strong>g pads.<br />
• Forced -air rewarm<strong>in</strong>g can rewarm as fast as 2,4°C/h (eg convective warm<strong>in</strong>g covers)<br />
Active core rewarm<strong>in</strong>g<br />
• humidify <strong>in</strong>spired air<br />
• warm <strong>in</strong>travenous fluids and blood products. These methods are used as an adjunct to o<strong>the</strong>r<br />
methods.<br />
• Heated gastric and colonic lavage.<br />
• pleural lavage<br />
• peritoneal lavage<br />
• mediast<strong>in</strong>al or closed thoracic lavage: These methods may <strong>in</strong>duce ventricular fibrillation and<br />
should only be used if cardiopulmonary bypass is immediately available.<br />
Extracorporal blood rewarm<strong>in</strong>g<br />
• Haemodialysis<br />
• Cont<strong>in</strong>uous arteriovenous rewarm<strong>in</strong>g (CAVR)<br />
• Venovenous rewarm<strong>in</strong>g<br />
• Cardiopulmonary bypass. Standard cardiopulmonary bypass requires not only specialised<br />
equipment and staff, but also mandated systemic anticoagulation and is not suitable for use<br />
<strong>in</strong> manag<strong>in</strong>g hypo<strong>the</strong>rmia <strong>in</strong> trauma victims.<br />
Conclusion:<br />
Both fever and hypo<strong>the</strong>rmia have benefits and detrimental effects. These should be weighed <strong>in</strong> <strong>the</strong><br />
decision to treat; <strong>the</strong> etiology and pathophysiology should lead decisions on how to treat. Both<br />
hyper- and hypo<strong>the</strong>rmia may also have <strong>the</strong>rapeutic uses.<br />
13