Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Bipolar Disorder: how effective is our<br />
screening in primary care<br />
April 2010 By Helena Du Toit, Raja Mukherjee, Rebecca Farrell <strong>and</strong> Sudhir Rastogi<br />
Introduction<br />
Bipolar Affective Disorder (BPD) is a<br />
serious, recurrent psychiatric illness<br />
characterised by periods of mania or<br />
hypomania, <strong>and</strong> depression (ICD-10,<br />
1992). BPD has a global prevalence of<br />
approximately 1-2%, which is stable over<br />
all population groups, however, when all<br />
forms of Bipolar Spectrum Disorder are<br />
included; the global lifetime prevalence<br />
rises to approximately 5% (Kessler RC et<br />
al, 1994; Angst J, 1998).<br />
It is a leading worldwide cause of disability<br />
(Hunter R et al, 2004), is associated with a<br />
high suicide risk (Sachs GS, 2003; Kasper,<br />
2003) <strong>and</strong> costs the UK economy about<br />
£2 billion per annum through active costs<br />
of managing the disorder as well as<br />
through loss of productivity (Das Gupta R<br />
& Guest JF, 2002).<br />
The condition usually presents in<br />
adolescence or early adulthood <strong>and</strong> has a<br />
recurring, often lifelong course, <strong>and</strong><br />
greatly affects the individual’s functioning<br />
in several areas <strong>and</strong> has wide reaching<br />
implications for close family, friends <strong>and</strong><br />
colleagues (Kasper S, 2003; Weissman<br />
MM et al, 1988; Stang P et al, 2007).<br />
In spite of this, it is often several years<br />
from the first presentation of the illness<br />
until the diagnosis is finally established,<br />
sometimes being delayed by as long as<br />
10 years. The under-recognition of BPD is<br />
due to several factors. Firstly, the illness<br />
often first presents with a depressive<br />
episode, <strong>and</strong> there may be several<br />
depressive episodes before the sufferer<br />
experiences a manic/hypomanic episode.<br />
These depressive episodes are often very<br />
difficult to distinguish from unipolar<br />
depression. Equally, the marked shifts in<br />
affect characteristic of emotionally<br />
unstable personality disorder <strong>and</strong><br />
cyclothymia can be mistaken for BPD<br />
(Corona et al, 2007). Additionally,<br />
patients often do not present to medical<br />
services during hypomanic <strong>and</strong><br />
sometimes even manic phases, as they<br />
find their increased energy levels <strong>and</strong><br />
creativity during these periods quite<br />
enjoyable <strong>and</strong> often do not recognize<br />
them as pathological. Furthermore,<br />
clinicians often fail to screen for a past<br />
history of manic/hypomanic symptoms in<br />
patients presenting with a depressive<br />
episode (Brickman et al, 2002). Delayed<br />
diagnosis often leads to inadequate<br />
management of the illness, with<br />
associated recurrent illness, diminished<br />
social <strong>and</strong> occupational functioning <strong>and</strong><br />
significant distress for both the sufferer<br />
<strong>and</strong> his/her family. To make matters<br />
worse, treating bipolar depression with<br />
antidepressant monotherapy is not only<br />
associated with a high rate of treatment<br />
failure, but also with a switch to rapid<br />
cycling BPD, increased mood instability<br />
<strong>and</strong> greater treatment resistance (Wehr<br />
TA & Goodwin FK, 1987).<br />
Conversely, there is good evidence that if<br />
the condition is diagnosed early <strong>and</strong><br />
managed appropriately, it is associated<br />
with a significantly improved outcome<br />
<strong>and</strong> preserved social <strong>and</strong> occupational<br />
functioning (Bauer MS et al, 2006; Perry<br />
A et al, 1999), as well as a significant<br />
decrease in the suicide risk.<br />
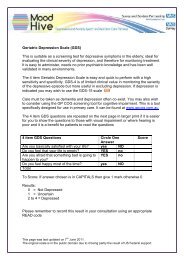
The Mood Disorders Questionnaire<br />
(MDQ) is a short, self administered<br />
questionnaire that has been validated in<br />
several countries (including the UK) as<br />
being an appropriate screening tool for<br />
use in the community or a primary care<br />
setting (Hirschfeld RM 2002; de Dois et<br />
al, 2008). It has both acceptable<br />
sensitivity <strong>and</strong> specificity to be used as a<br />
screening tool, <strong>and</strong> although some<br />
studies have suggested that the false<br />
positive rate is unacceptably high, the<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 9