Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
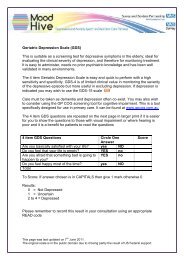
Research <strong>and</strong> Audit<br />
Table 5 shows how the GPs <strong>and</strong> MHNPs<br />
combined diagnoses (BPD or another<br />
condition) performed against the<br />
psychiatrists final diagnosis, which is used<br />
as the gold st<strong>and</strong>ard in this study.<br />
Thirty-three patients were seen by both<br />
the psychiatrist <strong>and</strong> their GP. Of the 7<br />
patients diagnosed with BPD by the<br />
psychiatrist 5 were correctly identified by<br />
their GP whilst 2 received another<br />
diagnosis. However in 4 patients where<br />
the psychiatrist diagnosed another<br />
condition the GP suggested a diagnosis<br />
of BPD. The corresponding sensitivity <strong>and</strong><br />
specificity of the GPs diagnoses were<br />
71.4% <strong>and</strong> 84.6%. The PPV for the GPs<br />
diagnoses was 55.6% while the NPV was<br />
91.7%. However the LR+ <strong>and</strong> LR- were<br />
4.75 <strong>and</strong> 0.34 respectively which are<br />
outside of the limits of a good diagnostic<br />
test. (Please refer to Fields A, 2009 for a<br />
detailed explanation of these terms.)<br />
Twenty patients were seen by a MHNP<br />
before seeing the psychiatrist. The MHNP<br />
correctly picked up BPD in 2 of the 4<br />
cases diagnosed with BPD by the<br />
psychiatrist. However in 6 out of 16 cases<br />
the MHNP diagnosed BPD whilst the<br />
psychiatrist diagnosed another condition.<br />
The sensitivity, specificity, PPV <strong>and</strong> NPV<br />
for the MHNPs diagnoses were 50%,<br />
62.5%, 25% <strong>and</strong> 80% respectively.<br />
Again the LR+ <strong>and</strong> LR- which are 1.35<br />
<strong>and</strong> 0.8 respectively fall outside of the<br />
limits of an acceptable diagnostic test.<br />
Discussion<br />
There is a growing body of evidence<br />
showing the importance of correctly<br />
identifying <strong>and</strong> treating sufferers of BPD<br />
to improve their quality of life, preserve<br />
their social <strong>and</strong> occupational functioning<br />
<strong>and</strong> to lessen the financial burden of<br />
healthcare costs related to the<br />
mismanagement of this important<br />
condition. Equally, the fact that there is<br />
often a delay of several years before this<br />
condition is correctly identified, highlights<br />
the importance of vigilantly screening for<br />
BPD, especially in the primary care setting.<br />
Our first aim was to establish the<br />
frequency with which our primary care<br />
practitioners screened for BPD. In this<br />
sample of patients presenting with<br />
affective symptoms, only 21.1% of those<br />
referred by their GP showed any evidence<br />
that they had been screened for BPD.<br />
Although this figure rose to 38.9% for<br />
MHNPs, this still represents a rather low<br />
proportion of screening for patients who<br />
are within the at risk category. This is<br />
especially important as tools such as the<br />
MDQ are available, short, <strong>and</strong> easy to<br />
use, <strong>and</strong> could easily be administered in<br />
the context of a primary care assessment.<br />
A potential downfall of this study design<br />
is that it relied on evidence from the<br />
referral letter that the clinician had<br />
screened for BPD <strong>and</strong> therefore it is<br />
possible that where a patient screened<br />
negative, it was not mentioned in the<br />
referral letter. However, a good referral<br />
should mention both positive <strong>and</strong> salient<br />
negative findings <strong>and</strong> routine use of the<br />
MDQ could circumnavigate this issue.<br />
Secondly, we aimed to establish whether<br />
screening for BPD increases the likelihood<br />
of correctly identifying the signs <strong>and</strong><br />
symptoms of this disorder. In our study<br />
both GPs <strong>and</strong> MHNPs almost exclusively<br />
(with the exception of one patient in<br />
each case) only proposed a diagnosis of<br />
BPD when there was evidence that they<br />
had screened for hypomania. These<br />
highly significant results show that it was<br />
highly unlikely that clinicians would<br />
propose a diagnosis of BPD when they<br />
had not screened for the condition. These<br />
results emphasize the great importance<br />
of consistent screening.<br />
Our third question looks at the accuracy<br />
with which GPs <strong>and</strong> MHNPs were able to<br />
rule in or rule out BPD in their patients.<br />
As previously mentioned, a good<br />
screening tool should have both good<br />
sensitivity (low false negatives) <strong>and</strong> good<br />
specificity (low false positives). We also<br />
looked at PPV <strong>and</strong> NPV as well as LR+<br />
<strong>and</strong> LR- as these give additional<br />
information about the quality of a<br />
screening test.<br />
14 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal