Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
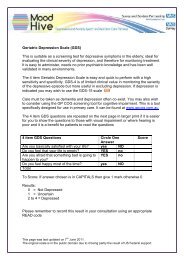
Research <strong>and</strong> Audit<br />
rate of false negatives is consistently low<br />
(Twiss J et al, 2008). It is therefore<br />
recommended that all patients screening<br />
positive for BPD on the MDQ (using a<br />
cut off of 9 positive responses as a<br />
positive test) should be referred for<br />
diagnostic assessment by a professional<br />
mental health worker. Additionally a<br />
large study in a USA health centre with 1<br />
million adult members identified that by<br />
administering one off screening for BPD<br />
to patients presenting with depressive<br />
symptoms, <strong>and</strong> following up positive<br />
screening results with a referral to a<br />
psychiatrist, reduced 5 year health care<br />
costs for that health centre by an<br />
estimated $1.94 million. This reduction<br />
was mostly due the difference in<br />
treatment costs between recognized<br />
versus unrecognized BPD sufferers<br />
(Menzin J et al, 2009).<br />
The importance of screening for<br />
hypomania/mania is that BPD sufferers<br />
are often misdiagnosed as suffering from<br />
unipolar depression, frequently leading<br />
to incorrect treatment. A single episode<br />
of mania constitutes a diagnosis of BPD,<br />
whilst an episode of hypomania should<br />
increase vigilance in looking out for<br />
future episodes of depression.<br />
Aims <strong>and</strong> Objectives of the<br />
Audit<br />
The purpose of the audit was to assess<br />
whether patients presenting to primary<br />
care practices within our catchment area<br />
were being screened for BPD.<br />
Additionally we wanted to establish how<br />
effective our service was at correctly<br />
identifying both true BPD sufferers, <strong>and</strong><br />
those suffering from other mental health<br />
conditions. We intend to examine this<br />
data <strong>and</strong> consider whether further<br />
awareness <strong>and</strong> screening is required.<br />
To summarize, our study aimed to<br />
answer 3 questions: Within the context<br />
of our service-<br />
1. Do primary care physicians <strong>and</strong><br />
Mental Health Nurse Practitioners<br />
(MHNPs), specialist psychiatric nurses<br />
working in both primary <strong>and</strong><br />
secondary care, screen for BPD?<br />
2. Does screening for BPD increase the<br />
likelihood of identifying this<br />
condition?<br />
3. Is there a good correlation between<br />
the diagnosis proposed by GPs <strong>and</strong><br />
MHNPs <strong>and</strong> the final diagnosis made<br />
by the psychiatrist?<br />
St<strong>and</strong>ard<br />
Currently no gold st<strong>and</strong>ard or NICE<br />
guidelines exist regarding screening for<br />
BPD in primary care; therefore we did<br />
not stipulate the use of a specific<br />
screening tool for our study. There are<br />
also no globally agreed cut-off points for<br />
what constitutes an acceptable<br />
screening test, although most<br />
researchers would agree that any good<br />
screening measure should have both a<br />
low false positive rate <strong>and</strong> a low false<br />
negative rate. The actual values that a<br />
researcher may deem acceptable are<br />
related to several variables, such as<br />
prevalence of condition, cost of<br />
screening <strong>and</strong> burden associated with<br />
missing the condition vs. burden<br />
associated with over diagnosing the<br />
condition (Simon S, 2007). For the<br />
purposes of our study, we set 80%<br />
sensitivity <strong>and</strong> 80% specificity as the<br />
st<strong>and</strong>ard, based upon levels set in other<br />
published research (Twiss J et al, 2008).<br />
Although these are arbitrary cut-off<br />
values, they are in line with generally<br />
accepted st<strong>and</strong>ards for psychiatric<br />
screening tests.<br />
Although we did not require the use of a<br />
specific screening tool for this study, we<br />
previously mentioned that a brief <strong>and</strong><br />
acceptable screening tool is available,<br />
<strong>and</strong> we may consider using this tool<br />
routinely in the future.<br />
10 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal