Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
Here - Surrey and Borders Partnership NHS Foundation Trust
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Issue 1<br />
Summer 2010<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> <strong>Partnership</strong><br />
<strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
Journal<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online<br />
www.sabp.nhs.uk/journal<br />
in this issue<br />
• Do you ever wonder why you agree to do things?<br />
• New Ways of Working – a three year study of the<br />
practice of a community mental health team<br />
• How can we improve recruitment into psychiatry?<br />
• An interview with Fiona Edwards
Contents<br />
Editorial<br />
Do you ever wonder why you agree to do things? ...........................................PAGE 3<br />
Raja Mukherjee<br />
Let’s do some research.....................................................................................PAGE 4<br />
Raj Persaud<br />
Research <strong>and</strong> Audit<br />
Bipolar Disorder: how effective is our screening in primary care........................PAGE 9<br />
Helena Du Toit et el<br />
Audit of risk assessment documentation in adult inpatients ...........................PAGE 17<br />
Abigail Crutchlow<br />
An evolving service – results of a 3 year follow up study of ...........................PAGE 21<br />
the practice of a community mental health team incorporating<br />
the principles of “New Ways of Working”<br />
Jeremy Mudunkotuwe et al<br />
Commentary <strong>and</strong> Debate<br />
How can we look at improving recruitment into psychiatry? ..........................PAGE 24<br />
Josie Jenkinson<br />
Book Reviews<br />
Psychiatry P.R.N. Principles, Reality, Next steps ...............................................PAGE 28<br />
Josie Jenkinson<br />
Interviews<br />
Interview with Fiona Edwards, ......................................................................PAGE 29<br />
Chief Executive SABP <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
Abigail Crutchlow<br />
Editorial Board<br />
Raja Mukherjee: Editor<br />
Laurence Church<br />
Philip Hall<br />
Jeremy Mudunkotuwe<br />
Abigail Crutchlow:<br />
Trainee representative<br />
Peer Review Panel<br />
All consultant<br />
psychiatrists unless<br />
otherwise stated<br />
Ruth Alloway<br />
Glen Cornish<br />
Ch<strong>and</strong>u De Alwis<br />
Antonio Fiahlo<br />
Ilenia Pampaloni<br />
Brian Parsons<br />
Raj Persaud<br />
Farida Yousaf<br />
Next edition December 2010: This will be<br />
open to the whole <strong>Trust</strong> <strong>and</strong> all specialities so<br />
please submit any articles you may have.<br />
Editorial guidance <strong>and</strong> st<strong>and</strong>ards as well as<br />
terms of reference can be obtained from the<br />
editor via email:<br />
raja.mukherjee@sabp.nhs.uk.<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal is<br />
published by <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> <strong>Partnership</strong><br />
<strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
18 Mole Business Park, Leatherhead,<br />
<strong>Surrey</strong> KT22 7AD Tel: 01883 383838<br />
Fax: 01372 203360 www.sabp.nhs.uk<br />
email: communications@sabp.nhs.uk<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> <strong>Partnership</strong> <strong>NHS</strong><br />
<strong>Foundation</strong> <strong>Trust</strong> © 2010<br />
Reproduction in whole or part without written<br />
permission from the publisher is strictly<br />
prohibited. The views expressed in articles in<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal are those of<br />
the authors, unless otherwise stated.<br />
2 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Do you ever wonder why you agree<br />
to do things?<br />
June 2010 By Raja Mukherjee, Editor<br />
Do you ever wonder why you agree<br />
to do things? The phrase “just say no”<br />
comes to mind, but for those of us of a<br />
certain generation, not in the context it<br />
was widely used back then! When<br />
Malcolm Hawthorne, then in his role as<br />
Medical Director, suggested setting up<br />
this journal, little did I realise I would be<br />
the one running with it. OK, naive I hear<br />
you cry. Maybe even stronger comments<br />
from some, but unfortunately I tend to<br />
agree with them. That phrase comes<br />
back to haunt you from time to time.<br />
The remit of the journal, to begin with at<br />
least, is to allow a space for doctors in<br />
the trust to develop skills at writing to a<br />
peer reviewed level. When I say that, I<br />
mean that it will not simply accept badly<br />
written or poorly thought out pieces. I<br />
will however, with my editorial board,<br />
look to develop the talent <strong>and</strong> skill of<br />
those in the trust who are interested in<br />
publishing. They may as yet not have the<br />
type of data that would interest national<br />
or international journals, but the piece<br />
may still be of interest to us locally.<br />
Primarily, this would initially aim at<br />
medical trainees but that should not<br />
exclusively mean it will be restricted to<br />
this group.<br />
My own experience of publishing is<br />
similar to that reported by Dr Persaud in<br />
his later editorial. It can be brutal out<br />
there. Like him, I think it is important to<br />
not give up <strong>and</strong> keep trying. Not only<br />
does it make you feel great when your<br />
name is in print, but even small new<br />
additions to what is known can be<br />
important. Perseverance can be<br />
important as it is not uncommon to get<br />
initially rejected. There are times I have<br />
wanted to throttle reviewers who have<br />
simply not understood what you were<br />
getting at. Did they actually read what<br />
you said or was it that you simply did not<br />
explain it well enough? Limitations on<br />
what you can present, in terms of word<br />
counts <strong>and</strong> restrictions on references<br />
makes it challenging. In the end though,<br />
establishing something new is never easy.<br />
That is unfortunately the reality of how<br />
things are. As such, better to learn in a<br />
non threatening environment with peers<br />
who you might actually know <strong>and</strong> will<br />
take your piece seriously.<br />
With this journal we have several aims.<br />
Firstly we wanted to allow the<br />
opportunity for people to present <strong>and</strong><br />
share work they are doing but that would<br />
not normally be of interest to those<br />
outside of the trust. Secondly it was an<br />
opportunity to hone skills. We are using<br />
the same set of internationally accepting<br />
st<strong>and</strong>ards for publishing that are adopted<br />
by many journals including the BMJ <strong>and</strong><br />
Lancet. Whilst I suspect we won’t publish<br />
anything of their calibre, we do hope it<br />
will be of a good st<strong>and</strong>ard. The articles<br />
will be placed onto the trust internet site<br />
<strong>and</strong> thus can be accessed by anyone with<br />
web access. This means you can be<br />
quoted in work by others <strong>and</strong> the<br />
information you produce will be<br />
accessible to the wider world. It will also<br />
count as a peer reviewed publication.<br />
In this first edition we present some<br />
audits undertaken by medical teams in<br />
the trust. There is a book review as well<br />
as an interview with our Chief Executive<br />
Fiona Edwards. Ok so it is not expansive<br />
but you have to start somewhere. We<br />
hope this will grow <strong>and</strong> that we can open<br />
it up to the whole trust <strong>and</strong> all specialties.<br />
Eventually we want it to grow into<br />
something we can all be proud of. We<br />
hope you enjoy this first edition. It is a<br />
start <strong>and</strong> will only succeed with your<br />
involvement. Thank you for taking the<br />
time to read <strong>and</strong> hopefully to contribute<br />
in the future.<br />
Editorial<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 3
Editorial<br />
Let’s do some research<br />
June 2010 By Raj Persaud<br />
I was asked to write this by Dr Raja<br />
Mukherjee for our <strong>Trust</strong>’s new<br />
journal. <strong>Here</strong> it is…<br />
If we asked you to predict now whether<br />
you were going to perform some<br />
research <strong>and</strong> publish it, say in the next<br />
year, what would your answer be?<br />
Perhaps, from past experience you might<br />
admit that this is not likely. On the other<br />
h<strong>and</strong>, even if wasn’t particularly likely,<br />
you may also feel that gathering data is<br />
something that you ought to be doing,<br />
<strong>and</strong> given the social pressure <strong>and</strong><br />
management dem<strong>and</strong>s (me asking you<br />
publicly what your research plans are) you<br />
might impulsively declare, that yes<br />
research is something you are planning<br />
<strong>and</strong> intending.<br />
Now, here is the interesting research<br />
question – in merely asking you to<br />
predict the future – do we change it?<br />
Let’s say we ran an experiment where we<br />
divided a sample of the electorate into<br />
two groups, <strong>and</strong> for one, we asked them<br />
to predict whether they were going to<br />
vote or not, while we did nothing<br />
pertinent to the second group; they acted<br />
as a control. Now, if we followed these<br />
two samples up into the future, to<br />
examine what they eventually did in the<br />
privacy of the polling booth; the<br />
astonishing result is that being asked to<br />
predict the future...does change it.<br />
Those who are asked to forecast whether<br />
they are going to vote, tend to confirm<br />
they will, <strong>and</strong> to do so much more than<br />
would be expected from their past<br />
behaviour. They are responding to<br />
external expectation (<strong>and</strong> internal drivers<br />
of a similar nature) so they manage the<br />
impression they want to create of being<br />
responsible citizens, by predicting a<br />
behaviour they were in fact much less<br />
likely to perform in reality. Having<br />
foretold that they will take part in a<br />
ballot, they tend to go ahead <strong>and</strong> actually<br />
vote. Yet if they weren’t asked to predict<br />
the future, they were not particularly<br />
likely to do any casting at all.<br />
We can demonstrate this experimentally<br />
by comparing the group asked to predict<br />
the future with the control group, who<br />
were not asked to make predictions. This<br />
second group vote at the lower baseline<br />
rate of the general population, which is,<br />
not that much.<br />
Why does being asked to predict that<br />
you are going to vote, make it much<br />
more likely that you will?<br />
The short answer is that this particular<br />
psychological phenomenon, like most<br />
others, inspires many theories that<br />
attempt to account for it, but no one is<br />
exactly sure which is the truth. A seminal<br />
paper on this effect in the Journal of<br />
Consumer Psychology by Business<br />
Psychologists Eric Spangenberg of<br />
Washington State University <strong>and</strong> Anthony<br />
Greenwald of the University of<br />
Washington, pointed out that the trend<br />
could be used powerfully to manipulate<br />
large populations into behaviours they<br />
had previously little intention of<br />
performing.<br />
Spangenberg <strong>and</strong> Greenwald are<br />
probably the two world authorities on<br />
this intriguing ‘self-prophecy effect’ <strong>and</strong><br />
their paper entitled ‘Social Influence by<br />
Requesting Self-Prophecy’ showed how<br />
asking people to predict their own<br />
behaviour in the future was associated,<br />
on follow up, with spectacularly less<br />
cheating in tests, significantly more<br />
attendance at health clubs, <strong>and</strong> more<br />
voting.<br />
One theory is that we like to see<br />
ourselves as consistent creatures, <strong>and</strong><br />
having made a prediction of our<br />
behaviour in the future, not to confirm<br />
the prediction by performing the<br />
behaviour, would force us to confront a<br />
rather unpalatable truth; we are<br />
unreliable, inconsistent people who don’t<br />
know our own minds.<br />
4 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
We are not so aware of the hidden forces<br />
at work generated by the social<br />
expectations of being asked about our<br />
plans in front of another, which push us<br />
into making a prediction at variance with<br />
what we would really do in the privacy of<br />
our own un-observed lives.<br />
Having made the prediction, we then<br />
work to fall into line with it.<br />
Another, related, theory is that this is an<br />
example of the power of expectation.<br />
Psychologists have demonstrated for<br />
almost half a century now, that if<br />
teachers are manipulated into expecting<br />
their pupils to be intelligent or stupid,<br />
they then work to render these<br />
expectations self-fulfilling prophecies.<br />
Judges give directions to juries at the<br />
beginnings of trials that appear to bias<br />
the outcome in line with the bench’s<br />
expectation of the future. We also<br />
directly seem to suffer for this effect – if<br />
our expectation of ourselves is<br />
manipulated experimentally, we then<br />
provide later behavioural confirmation of<br />
our expectations of ourselves.<br />
More on Expectations<br />
One of the most famous experiments in<br />
Social Psychology which demonstrated<br />
the power of expectation is a 1977 study<br />
by a team lead by Mark Snyder, now at<br />
the University of Minnesota, in which men<br />
were shown photographs of a woman to<br />
whom they would be talking by phone.<br />
The woman in the pictures was<br />
r<strong>and</strong>omised to being either extremely<br />
physically attractive or unattractive (as<br />
rated by other independent observers).<br />
What the men taking part in the<br />
experiment didn’t know, was that those<br />
sneaky psychologists had told a porky pie,<br />
<strong>and</strong> the photographs were not only<br />
r<strong>and</strong>omly assigned to the men, but they<br />
also did not correspond in any way to the<br />
actual woman with whom they had the<br />
phone conversation.<br />
While it would come as no surprise that<br />
the men behaved differently to the<br />
women during the phone conversation<br />
depending on their (manipulated) beliefs<br />
on her physical appearance, the really<br />
surprising finding was that independent<br />
ratings of the women's segments of the<br />
conversations revealed that females<br />
whose conversational partners believed<br />
them to be less appealing, actually<br />
behaved <strong>and</strong> sounded less attractively (eg<br />
they were rated as sounding less warm<br />
<strong>and</strong> interesting).<br />
The women, just as the men, had also<br />
been kept completely in the dark by the<br />
psychologists about the photograph<br />
manipulation. They were not aware it had<br />
taken place. This effect, therefore, had to<br />
have been mediated in some way through<br />
the men's behavior. One possibility, is that<br />
the men who were talking to someone<br />
they believed to be unattractive, were<br />
themselves less affable than men who<br />
believed they were talking to an attractive<br />
woman. This in turn had an impact on the<br />
way the women responded, <strong>and</strong> then<br />
they way they came over to an<br />
independent observer.<br />
The ‘Pygmalion Effect’ is a special instance<br />
of the self-fulfilling prophecy; where<br />
having an expectation of another, itself<br />
causes that target to modify their<br />
performance so it falls into line with the<br />
expectation of the first party.<br />
Just in case you are starting to think that<br />
Self-Fulfilling Prophecies only inhabit the<br />
obscure world of experimental<br />
Psychology, remember we are living<br />
through a banking crisis <strong>and</strong> suffering its<br />
long term impact, <strong>and</strong> banking crises are<br />
a form of self-fulfilling prophecy.<br />
Because a rumour starts that a bank may<br />
fail, this precipitates a run on that bank,<br />
which in itself inevitably leads to its<br />
collapse. This is why Chancellors of the<br />
Exchequer hot foot it to the nearest TV<br />
studio to ‘steady the markets’ at the<br />
slightest hint of such runs on major<br />
financial institutions. Governments, <strong>and</strong><br />
the whole financial system, live in terror<br />
of the power of the self-fulfilling<br />
prophecy.<br />
It’s so powerful <strong>and</strong> reliable that you can<br />
literally ‘bank’ on it.<br />
Editorial<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 5
Editorial<br />
Expectations <strong>and</strong> You<br />
Consider the continuing controversy<br />
over the benefits or costs of psychiatric<br />
diagnosis. Is it possible that the<br />
expectation set up in the patient <strong>and</strong><br />
their social circle, once a diagnosis of<br />
schizophrenia or depression is made, in<br />
itself serves to make the implicit<br />
prophecy entailed in such a diagnosis<br />
come true? Because of the powerful<br />
self-fulfilling prophecy effect of a<br />
psychiatric diagnosis – is it possible that<br />
users of mental health services would<br />
benefit more from ab<strong>and</strong>oning the use<br />
of such labels?<br />
At the heart of the education system,<br />
psychologists contend, are ever-present<br />
self-fulfilling prophecies. We constantly<br />
stream children <strong>and</strong> students into better<br />
classes or universities, then wonder why<br />
they do better, when the power of<br />
expectation <strong>and</strong> self-fulfilling prophecy<br />
might be the answer, rather than any<br />
inherent benefit of an elite education.<br />
Our <strong>Trust</strong><br />
Is it possible, coming back to research in<br />
our <strong>Trust</strong>, that the expectation of whether<br />
or not you are going to do research<br />
massively influences the outcome? Might<br />
it be of benefit to the <strong>Trust</strong> <strong>and</strong> the<br />
doctors working within it to transform<br />
the expectation so that we ‘become<br />
expected’, by managers, peers <strong>and</strong><br />
ourselves, to generate <strong>and</strong> publish much<br />
more research than we currently do?<br />
And doctors? Why should doctors<br />
bother to do research? Surely doctors’<br />
primary function is to heal the sick, <strong>and</strong><br />
other activities become a distraction?<br />
Can research by used by some as a<br />
‘noble’ from the heaving clinic? How do<br />
eminence <strong>and</strong> academic honour<br />
correlate with clinical acumen? Do<br />
publication lists still appear as a magic<br />
key in unlocking merit awards?<br />
There are some serious obstacles that<br />
will confront any doctor attempting<br />
research. Firstly, finding the time,<br />
support, advice <strong>and</strong> resources to<br />
conduct the study. On top of a<br />
burdensome caseload, anyone in an <strong>NHS</strong><br />
contract who is successful in producing<br />
papers is frequently met with the<br />
suspicion that they cannot be pulling<br />
their weight clinically.<br />
Half way through the study someone<br />
will usually helpfully point out some<br />
methodological consideration that<br />
renders all your meticulous data<br />
collection redundant, so you are faced<br />
with the prospect of starting all over<br />
again.<br />
Most papers hide the key story of the<br />
research project, which is in fact how the<br />
investigators overcame, through adept<br />
improvisation, often on the hoof, various<br />
unexpected impediments tripping them<br />
as they attempted to recruit subjects, or<br />
measure some variable.<br />
Once one nightmare study was over <strong>and</strong><br />
the data was presented at various<br />
conferences, a researcher was asked how<br />
he would do the study differently if he<br />
could start all over again. His response<br />
was that he would not do it at all.<br />
Once you assemble the data, statistics<br />
need to be applied. You visit statisticians<br />
with trepidation, remembering to pack<br />
your calculator. They take one cursory<br />
look at the reams of numbers you had<br />
painstakingly calculated <strong>and</strong> she bursts<br />
out laughing because (a) you measured<br />
the right thing but in the wrong way or<br />
(b) you measured the right way, but<br />
chose the wrong thing to measure or (c)<br />
you didn’t recruit enough subjects or (d)<br />
the measuring instrument you used isn’t<br />
compatible with the statistical test you<br />
hoped to apply…. And so it goes on.<br />
Some people find that, once you have to<br />
start using fancy statistics to illuminate<br />
your hypothesis, the finding isn’t worth<br />
the c<strong>and</strong>le. This should reassure the<br />
statistically naïve that genuine<br />
discoveries are still possible for the<br />
innumerate. Indeed in the world of<br />
research, suspicions mount as the<br />
statistical tests multiply.<br />
Another wonderful revelation was the<br />
(geeky nerdy) joy in just inspecting the<br />
raw data, like graphing it, without<br />
6 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
esorting too soon to complex statistical<br />
tests. This is a real issue in research in<br />
psychiatry – how to measure the elusive<br />
concepts we deal with daily. In the rest of<br />
medicine measuring blood sugar or bone<br />
density levels is much more<br />
straightforward, which is why these<br />
branches lend themselves so much more<br />
easily to research.<br />
So one early tip to the young researcher<br />
is to think very carefully before you start<br />
your study about precisely what you are<br />
evaluating <strong>and</strong> how you are measuring it.<br />
Lean heavily towards using an<br />
instrument, like a questionnaire, that is<br />
widely accepted in the field. Of course,<br />
some of the most gloriously innovative<br />
research in psychiatry involves pioneering<br />
a new measurement device, because the<br />
research community has neglected the<br />
concept you are investigating.<br />
But the problems don’t end there. Let’s say<br />
you dodged the statisticians’ scrutiny <strong>and</strong><br />
colleagues’ criticism. Then you may go on<br />
to long friendships being threatened by<br />
disputes over how to write it up. And,<br />
finally who is going to be first author?<br />
After that jockeying for position come the<br />
editors’ letters of rejection. This happens<br />
even to the most published of us. The<br />
record among people I have known is 10<br />
rejecting letters from editors for one<br />
paper <strong>and</strong> 30 rejections for a book.<br />
So given all these problems – why do<br />
research at all?<br />
I still firmly believe it’s worth it. Much of<br />
what we do as doctors arises because<br />
some researcher somewhere bravely<br />
chose to ask the question – what is the<br />
evidence for this piece of practice? There<br />
is nothing more exciting than pushing<br />
back the frontiers of knowledge <strong>and</strong><br />
discovering something new <strong>and</strong> – the<br />
icing on the ‘cake’ - is that it may alter<br />
clinical practice or improve the outcome<br />
for patients.<br />
Having a research interest keeps us<br />
stimulated <strong>and</strong> interested in our<br />
professional lives. It assists in engaging<br />
with those of similar interests all around<br />
the world <strong>and</strong> at a time when doctors<br />
frequently feel neglected or downtrodden<br />
by the <strong>NHS</strong>; it is great for the self-esteem<br />
<strong>and</strong> earns the respect of colleagues.<br />
I have been impressed at the clinical<br />
acumen <strong>and</strong> lively minds we are<br />
privileged to work alongside. I believe<br />
there would be many benefits, including<br />
raising clinical morale, for the <strong>Trust</strong> to<br />
engage more with a research ethos.<br />
Another advantage for the future is that<br />
rapidly climbing the <strong>NHS</strong> agenda now<br />
comes the issue of providing, proving <strong>and</strong><br />
improving the quality of care we provide<br />
our patients. It would be great for us to<br />
engage in research investigating what the<br />
determinants of high quality care are, in<br />
the eyes of patients as well as clinicians<br />
<strong>and</strong> scrutinize how to improve this. There<br />
may well be some surprising answers. It’s<br />
entirely possible that what doctors<br />
believe is crucial to treatment outcome is<br />
much more peripheral.<br />
Also while we are encouraged to<br />
constantly keep abreast of the latest<br />
research, its only by having done some<br />
yourself, that you are in the best position<br />
to properly evaluate an academic paper.<br />
This is because you will now be aware of<br />
many crucial issues the authors skate<br />
over, but which you know from hard<br />
experience, might be influencing the data<br />
they present.<br />
Its vital not to get pigeonholed – yes I<br />
have done brain scanning research, but I<br />
also got interested in qualitative research<br />
methods – <strong>and</strong> used them to sit <strong>and</strong><br />
observe what goes on in waiting rooms.<br />
These are spaces where our patients<br />
sometimes spend more time than they do<br />
actually seeing us!<br />
Commercial institutions like Banks had<br />
clearly put a lot of thought into<br />
considering <strong>and</strong> influencing the mental<br />
state of its customers, while they wait to<br />
see a member of staff. The <strong>NHS</strong> in<br />
contrast appeared to view the waiting<br />
room as some kind of detainment<br />
compound for undesirables. It was often<br />
at best an afterthought in planning.<br />
Yet by the time any doctor sees a patient<br />
Editorial<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 7
Editorial<br />
– the outcome of that crucial encounter<br />
may have already been partly <strong>and</strong><br />
significantly determined by what the<br />
patient experienced in the waiting room.<br />
Something the doctor may not just be<br />
unaware of, but may be usually beyond<br />
their control.<br />
Qualitative research has a long <strong>and</strong><br />
respectable history in Anthropology <strong>and</strong><br />
Sociology, though it may be sniffed at by<br />
medical colleagues; it’s just an example<br />
that other methodologies are available<br />
to us as research tools. You don’t need a<br />
high tech brain scanner to accomplish<br />
something meaningful. It should not be<br />
forgotten.<br />
<strong>Here</strong> are some possible research<br />
questions that I would be interested in<br />
assisting any staff member with<br />
conducting some kind of project, or<br />
which I believe others in the <strong>Trust</strong> may<br />
want to pick up.<br />
Why do patients complain <strong>and</strong> what is<br />
their experience of the complaints<br />
process? What leads to higher patient<br />
satisfaction after a complaint? What is<br />
the experience of the staff members<br />
who have been the subject of a<br />
complaint? What is the impact on them<br />
psychologically or in terms of the way<br />
they practice medicine afterwards?<br />
What is found most helpful by GPs in<br />
letters from Secondary Care clinics.<br />
What do they dislike the most in our<br />
letters to them? What impact do our<br />
letters have on care? What about a trial<br />
of different kinds of letters?<br />
When a patient first hears that a GP is<br />
thinking of referring them to a<br />
psychiatric services – what is their initial<br />
reaction? How does the encounter with<br />
services alter that?<br />
When trainees start psychiatry what are<br />
their expectations? How does doing a<br />
psychiatry placement alter this?<br />
Part of the new <strong>Trust</strong> journal could be<br />
devoted to throwing out research ideas<br />
<strong>and</strong> seeing who wants to collaborate<br />
over conducting. Part of the week could<br />
be set aside for doctors in the <strong>Trust</strong> to<br />
meet in order to discuss <strong>and</strong> assist with<br />
research projects.<br />
Remember as well that publishing<br />
doesn’t have to be restricted to<br />
publishing research – letters to journals<br />
can often be surprisingly influential. A<br />
good place to start in your research<br />
career is by submitting some letters. For<br />
that you must be aware of the literature<br />
<strong>and</strong> eventually dialogues <strong>and</strong><br />
collaborations may develop. before you<br />
critique it <strong>and</strong> then eventually dialogues<br />
<strong>and</strong> collaborations often develop out of<br />
such initial correspondence.<br />
Colleagues could get together <strong>and</strong><br />
submit more letters to journals - drawing<br />
attention to the implications of various<br />
research findings on clinical practice<br />
where we work?<br />
These are just questions – I don’t<br />
pretend to have the answers.<br />
But all great research at least starts with<br />
a good question.<br />
This is not as good a paper as I had<br />
hoped. It was done rather quickly <strong>and</strong><br />
under difficult circumstances. But it<br />
might stimulate you to think of doing<br />
research.<br />
Remember, if you predict you’ll do, you<br />
are more likely to do it.<br />
8 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Bipolar Disorder: how effective is our<br />
screening in primary care<br />
April 2010 By Helena Du Toit, Raja Mukherjee, Rebecca Farrell <strong>and</strong> Sudhir Rastogi<br />
Introduction<br />
Bipolar Affective Disorder (BPD) is a<br />
serious, recurrent psychiatric illness<br />
characterised by periods of mania or<br />
hypomania, <strong>and</strong> depression (ICD-10,<br />
1992). BPD has a global prevalence of<br />
approximately 1-2%, which is stable over<br />
all population groups, however, when all<br />
forms of Bipolar Spectrum Disorder are<br />
included; the global lifetime prevalence<br />
rises to approximately 5% (Kessler RC et<br />
al, 1994; Angst J, 1998).<br />
It is a leading worldwide cause of disability<br />
(Hunter R et al, 2004), is associated with a<br />
high suicide risk (Sachs GS, 2003; Kasper,<br />
2003) <strong>and</strong> costs the UK economy about<br />
£2 billion per annum through active costs<br />
of managing the disorder as well as<br />
through loss of productivity (Das Gupta R<br />
& Guest JF, 2002).<br />
The condition usually presents in<br />
adolescence or early adulthood <strong>and</strong> has a<br />
recurring, often lifelong course, <strong>and</strong><br />
greatly affects the individual’s functioning<br />
in several areas <strong>and</strong> has wide reaching<br />
implications for close family, friends <strong>and</strong><br />
colleagues (Kasper S, 2003; Weissman<br />
MM et al, 1988; Stang P et al, 2007).<br />
In spite of this, it is often several years<br />
from the first presentation of the illness<br />
until the diagnosis is finally established,<br />
sometimes being delayed by as long as<br />
10 years. The under-recognition of BPD is<br />
due to several factors. Firstly, the illness<br />
often first presents with a depressive<br />
episode, <strong>and</strong> there may be several<br />
depressive episodes before the sufferer<br />
experiences a manic/hypomanic episode.<br />
These depressive episodes are often very<br />
difficult to distinguish from unipolar<br />
depression. Equally, the marked shifts in<br />
affect characteristic of emotionally<br />
unstable personality disorder <strong>and</strong><br />
cyclothymia can be mistaken for BPD<br />
(Corona et al, 2007). Additionally,<br />
patients often do not present to medical<br />
services during hypomanic <strong>and</strong><br />
sometimes even manic phases, as they<br />
find their increased energy levels <strong>and</strong><br />
creativity during these periods quite<br />
enjoyable <strong>and</strong> often do not recognize<br />
them as pathological. Furthermore,<br />
clinicians often fail to screen for a past<br />
history of manic/hypomanic symptoms in<br />
patients presenting with a depressive<br />
episode (Brickman et al, 2002). Delayed<br />
diagnosis often leads to inadequate<br />
management of the illness, with<br />
associated recurrent illness, diminished<br />
social <strong>and</strong> occupational functioning <strong>and</strong><br />
significant distress for both the sufferer<br />
<strong>and</strong> his/her family. To make matters<br />
worse, treating bipolar depression with<br />
antidepressant monotherapy is not only<br />
associated with a high rate of treatment<br />
failure, but also with a switch to rapid<br />
cycling BPD, increased mood instability<br />
<strong>and</strong> greater treatment resistance (Wehr<br />
TA & Goodwin FK, 1987).<br />
Conversely, there is good evidence that if<br />
the condition is diagnosed early <strong>and</strong><br />
managed appropriately, it is associated<br />
with a significantly improved outcome<br />
<strong>and</strong> preserved social <strong>and</strong> occupational<br />
functioning (Bauer MS et al, 2006; Perry<br />
A et al, 1999), as well as a significant<br />
decrease in the suicide risk.<br />
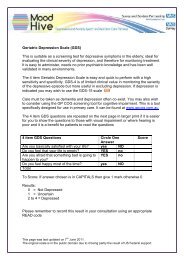
The Mood Disorders Questionnaire<br />
(MDQ) is a short, self administered<br />
questionnaire that has been validated in<br />
several countries (including the UK) as<br />
being an appropriate screening tool for<br />
use in the community or a primary care<br />
setting (Hirschfeld RM 2002; de Dois et<br />
al, 2008). It has both acceptable<br />
sensitivity <strong>and</strong> specificity to be used as a<br />
screening tool, <strong>and</strong> although some<br />
studies have suggested that the false<br />
positive rate is unacceptably high, the<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 9
Research <strong>and</strong> Audit<br />
rate of false negatives is consistently low<br />
(Twiss J et al, 2008). It is therefore<br />
recommended that all patients screening<br />
positive for BPD on the MDQ (using a<br />
cut off of 9 positive responses as a<br />
positive test) should be referred for<br />
diagnostic assessment by a professional<br />
mental health worker. Additionally a<br />
large study in a USA health centre with 1<br />
million adult members identified that by<br />
administering one off screening for BPD<br />
to patients presenting with depressive<br />
symptoms, <strong>and</strong> following up positive<br />
screening results with a referral to a<br />
psychiatrist, reduced 5 year health care<br />
costs for that health centre by an<br />
estimated $1.94 million. This reduction<br />
was mostly due the difference in<br />
treatment costs between recognized<br />
versus unrecognized BPD sufferers<br />
(Menzin J et al, 2009).<br />
The importance of screening for<br />
hypomania/mania is that BPD sufferers<br />
are often misdiagnosed as suffering from<br />
unipolar depression, frequently leading<br />
to incorrect treatment. A single episode<br />
of mania constitutes a diagnosis of BPD,<br />
whilst an episode of hypomania should<br />
increase vigilance in looking out for<br />
future episodes of depression.<br />
Aims <strong>and</strong> Objectives of the<br />
Audit<br />
The purpose of the audit was to assess<br />
whether patients presenting to primary<br />
care practices within our catchment area<br />
were being screened for BPD.<br />
Additionally we wanted to establish how<br />
effective our service was at correctly<br />
identifying both true BPD sufferers, <strong>and</strong><br />
those suffering from other mental health<br />
conditions. We intend to examine this<br />
data <strong>and</strong> consider whether further<br />
awareness <strong>and</strong> screening is required.<br />
To summarize, our study aimed to<br />
answer 3 questions: Within the context<br />
of our service-<br />
1. Do primary care physicians <strong>and</strong><br />
Mental Health Nurse Practitioners<br />
(MHNPs), specialist psychiatric nurses<br />
working in both primary <strong>and</strong><br />
secondary care, screen for BPD?<br />
2. Does screening for BPD increase the<br />
likelihood of identifying this<br />
condition?<br />
3. Is there a good correlation between<br />
the diagnosis proposed by GPs <strong>and</strong><br />
MHNPs <strong>and</strong> the final diagnosis made<br />
by the psychiatrist?<br />
St<strong>and</strong>ard<br />
Currently no gold st<strong>and</strong>ard or NICE<br />
guidelines exist regarding screening for<br />
BPD in primary care; therefore we did<br />
not stipulate the use of a specific<br />
screening tool for our study. There are<br />
also no globally agreed cut-off points for<br />
what constitutes an acceptable<br />
screening test, although most<br />
researchers would agree that any good<br />
screening measure should have both a<br />
low false positive rate <strong>and</strong> a low false<br />
negative rate. The actual values that a<br />
researcher may deem acceptable are<br />
related to several variables, such as<br />
prevalence of condition, cost of<br />
screening <strong>and</strong> burden associated with<br />
missing the condition vs. burden<br />
associated with over diagnosing the<br />
condition (Simon S, 2007). For the<br />
purposes of our study, we set 80%<br />
sensitivity <strong>and</strong> 80% specificity as the<br />
st<strong>and</strong>ard, based upon levels set in other<br />
published research (Twiss J et al, 2008).<br />
Although these are arbitrary cut-off<br />
values, they are in line with generally<br />
accepted st<strong>and</strong>ards for psychiatric<br />
screening tests.<br />
Although we did not require the use of a<br />
specific screening tool for this study, we<br />
previously mentioned that a brief <strong>and</strong><br />
acceptable screening tool is available,<br />
<strong>and</strong> we may consider using this tool<br />
routinely in the future.<br />
10 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Research Method<br />
The study was conducted in our local<br />
Primary Mental Health Care Team<br />
(PCMHT) which is a community<br />
psychiatric service that operates both in<br />
GP surgeries <strong>and</strong> secondary care. A<br />
retrospective survey was carried out of all<br />
the patients with affective symptoms that<br />
were referred to the T<strong>and</strong>ridge PCMHT<br />
over a 6 month period between January<br />
<strong>and</strong> June 2008. It was felt that this would<br />
be a sufficiently large sample to accurately<br />
<strong>and</strong> validly assess the efficacy of screening<br />
for BPD in our catchment area.<br />
Table 1: Proforma used to analyse case records<br />
These referrals came from local GP<br />
surgeries, through the Crisis Advisory<br />
service, the Home Treatment Team <strong>and</strong><br />
following discharge from the inpatient<br />
psychiatric unit at Epsom General<br />
Hospital. Some of these referrals also had<br />
a further triage assessment by a Mental<br />
Health Nurse Practitioner (MHNP) before<br />
being referred to the psychiatrist for<br />
confirmation of their diagnosis.<br />
We examined all patients’ records using<br />
an audit proforma that looked at the<br />
following parameters:<br />
GP assessment MHNP assessment Psychiatrist<br />
assessment<br />
Did the<br />
patient have<br />
2/more<br />
episodes of<br />
mental<br />
illness?<br />
Did the GP<br />
screen for<br />
hypomania?<br />
What<br />
diagnosis<br />
did the GP<br />
propose?<br />
Did the<br />
MHNP<br />
screen for<br />
hypomania?<br />
What<br />
diagnosis<br />
did the<br />
MHNP<br />
propose?<br />
Final<br />
Diagnosis<br />
Research <strong>and</strong> Audit<br />
On completion of the proforma’s the data was analysed using the SPSS statistical<br />
package.<br />
The Psychiatrist’s diagnosis was used as the gold st<strong>and</strong>ard next to which the other<br />
proposed diagnoses were measured for accuracy.<br />
Results<br />
Between 01/01/2008 – 30/06/2008 there were 58 patients referred to the T<strong>and</strong>ridge<br />
PCMHT that presented with affective symptoms. Seven records could not be retrieved,<br />
subsequently 51 patients were included in the audit.<br />
The demographics of our study population were as follows:<br />
Table 2: Demographics of study population<br />
Gender<br />
Age<br />
Male, N = 19<br />
Range, 19 – 62 years<br />
Female, N = 32<br />
Mean = 37.6<br />
(normal distribution)<br />
Out of the 38 patients referred by their GPs, 21 (55.3%) had had two or more<br />
episodes of mental illness whilst for 17 patients (44.7%) it was their first episode of<br />
mental illness. 13 patients were referred from other sources. In these cases the initial<br />
referral letter was analyzed in the same way as a GP referral <strong>and</strong> if they were also seen<br />
by a MHNP, this data was also included.<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 11
Research <strong>and</strong> Audit<br />
Table 3: Frequency with which GPs <strong>and</strong> MHNPs screened<br />
for hypomania<br />
%<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
% Yes<br />
% No<br />
GP<br />
MHNP<br />
Screened for hypomania (n) Frequency (n) Percent (%)<br />
GP Yes 8 21.1<br />
No 30 78.9<br />
Total 38 100<br />
MHNP Yes 14 38.9<br />
No 22 61.1<br />
Total 36 100<br />
Table 3 shows the total number (n) of patients that were screened for hypomania by<br />
the GP <strong>and</strong> the MHNP respectively as well as their representative frequencies. As<br />
indicated, only 21.1% of all patients were screened by their GP for symptoms of<br />
hypomania whilst 38.9% of patients who saw a MHNP were screened for hypomania.<br />
Table 4: Diagnoses made by GPs <strong>and</strong> MHNPs vs. screening for<br />
hypomania<br />
Combined GP Diagnosis<br />
Combined MHNP Diagnosis<br />
100<br />
100<br />
80<br />
80<br />
60<br />
Screened<br />
60<br />
Screened<br />
40<br />
Not Screened<br />
40<br />
Not Screened<br />
20<br />
20<br />
0<br />
BPD<br />
Total<br />
0<br />
BPD<br />
Total<br />
12 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Screened for Hypomania<br />
Yes No Total<br />
Combined GP Dx BPD 8 1 9<br />
Other 0 29 29<br />
Total 8 30 38<br />
Combined BPD 9 0 9<br />
MHNP Dx Other 1 13 14<br />
Total 10 13 23<br />
Chi-Square Tests<br />
Value df P value<br />
Pearson χ² 32.65 1 .000<br />
Cont.Corr. 27.52 1 .000<br />
Fisher’s Exact Test .000<br />
Pearson χ² 19.22 1 .000<br />
Cont.Corr. 15.63 1 .000<br />
Fisher’s Exact Test .000<br />
Key: (df) degrees of freedom, (χ²) Pearson’s chi-square value, (cont.corr.) continuity<br />
correction – done for 2x2 tables, Fisher’s Exact Test – performed as one or more cells<br />
<strong>and</strong> an expected count of
Research <strong>and</strong> Audit<br />
Table 5 shows how the GPs <strong>and</strong> MHNPs<br />
combined diagnoses (BPD or another<br />
condition) performed against the<br />
psychiatrists final diagnosis, which is used<br />
as the gold st<strong>and</strong>ard in this study.<br />
Thirty-three patients were seen by both<br />
the psychiatrist <strong>and</strong> their GP. Of the 7<br />
patients diagnosed with BPD by the<br />
psychiatrist 5 were correctly identified by<br />
their GP whilst 2 received another<br />
diagnosis. However in 4 patients where<br />
the psychiatrist diagnosed another<br />
condition the GP suggested a diagnosis<br />
of BPD. The corresponding sensitivity <strong>and</strong><br />
specificity of the GPs diagnoses were<br />
71.4% <strong>and</strong> 84.6%. The PPV for the GPs<br />
diagnoses was 55.6% while the NPV was<br />
91.7%. However the LR+ <strong>and</strong> LR- were<br />
4.75 <strong>and</strong> 0.34 respectively which are<br />
outside of the limits of a good diagnostic<br />
test. (Please refer to Fields A, 2009 for a<br />
detailed explanation of these terms.)<br />
Twenty patients were seen by a MHNP<br />
before seeing the psychiatrist. The MHNP<br />
correctly picked up BPD in 2 of the 4<br />
cases diagnosed with BPD by the<br />
psychiatrist. However in 6 out of 16 cases<br />
the MHNP diagnosed BPD whilst the<br />
psychiatrist diagnosed another condition.<br />
The sensitivity, specificity, PPV <strong>and</strong> NPV<br />
for the MHNPs diagnoses were 50%,<br />
62.5%, 25% <strong>and</strong> 80% respectively.<br />
Again the LR+ <strong>and</strong> LR- which are 1.35<br />
<strong>and</strong> 0.8 respectively fall outside of the<br />
limits of an acceptable diagnostic test.<br />
Discussion<br />
There is a growing body of evidence<br />
showing the importance of correctly<br />
identifying <strong>and</strong> treating sufferers of BPD<br />
to improve their quality of life, preserve<br />
their social <strong>and</strong> occupational functioning<br />
<strong>and</strong> to lessen the financial burden of<br />
healthcare costs related to the<br />
mismanagement of this important<br />
condition. Equally, the fact that there is<br />
often a delay of several years before this<br />
condition is correctly identified, highlights<br />
the importance of vigilantly screening for<br />
BPD, especially in the primary care setting.<br />
Our first aim was to establish the<br />
frequency with which our primary care<br />
practitioners screened for BPD. In this<br />
sample of patients presenting with<br />
affective symptoms, only 21.1% of those<br />
referred by their GP showed any evidence<br />
that they had been screened for BPD.<br />
Although this figure rose to 38.9% for<br />
MHNPs, this still represents a rather low<br />
proportion of screening for patients who<br />
are within the at risk category. This is<br />
especially important as tools such as the<br />
MDQ are available, short, <strong>and</strong> easy to<br />
use, <strong>and</strong> could easily be administered in<br />
the context of a primary care assessment.<br />
A potential downfall of this study design<br />
is that it relied on evidence from the<br />
referral letter that the clinician had<br />
screened for BPD <strong>and</strong> therefore it is<br />
possible that where a patient screened<br />
negative, it was not mentioned in the<br />
referral letter. However, a good referral<br />
should mention both positive <strong>and</strong> salient<br />
negative findings <strong>and</strong> routine use of the<br />
MDQ could circumnavigate this issue.<br />
Secondly, we aimed to establish whether<br />
screening for BPD increases the likelihood<br />
of correctly identifying the signs <strong>and</strong><br />
symptoms of this disorder. In our study<br />
both GPs <strong>and</strong> MHNPs almost exclusively<br />
(with the exception of one patient in<br />
each case) only proposed a diagnosis of<br />
BPD when there was evidence that they<br />
had screened for hypomania. These<br />
highly significant results show that it was<br />
highly unlikely that clinicians would<br />
propose a diagnosis of BPD when they<br />
had not screened for the condition. These<br />
results emphasize the great importance<br />
of consistent screening.<br />
Our third question looks at the accuracy<br />
with which GPs <strong>and</strong> MHNPs were able to<br />
rule in or rule out BPD in their patients.<br />
As previously mentioned, a good<br />
screening tool should have both good<br />
sensitivity (low false negatives) <strong>and</strong> good<br />
specificity (low false positives). We also<br />
looked at PPV <strong>and</strong> NPV as well as LR+<br />
<strong>and</strong> LR- as these give additional<br />
information about the quality of a<br />
screening test.<br />
14 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
In our sample the GPs screening method<br />
was very effective at ruling out BPD, but<br />
was less accurate when it came to ruling<br />
the condition in.<br />
The MHNPs’ method was also ineffective<br />
at ruling in BPD <strong>and</strong> although it was<br />
slightly better at ruling out this condition,<br />
only the NPV was above the cut off value.<br />
However for both groups of practitioners<br />
the LR+ <strong>and</strong> LR- of their methods, which<br />
reflects the value of a positive or negative<br />
test result, was well below the accepted<br />
cut off range. This suggests that the<br />
methods used by the primary care<br />
practitioners in our study had little value<br />
in correctly identifying the presence or<br />
absence of BPD.<br />
There are, however, some limitations to<br />
our study. We should note that this study<br />
encompassed relatively small numbers<br />
<strong>and</strong> this makes it difficult to make<br />
predictions about how these methods<br />
would perform in a larger population. In<br />
this study neither the GPs nor the MHNPs<br />
used a st<strong>and</strong>ardized screening tool;<br />
instead we were examining the validity of<br />
the methods they are already using.<br />
Although our results suggest that the GPs<br />
methods were slightly more effective<br />
than the MHNPs’ methods, it is also<br />
possible that the cases seen by the<br />
MHNPs were more complex <strong>and</strong><br />
displayed a less clear cut presentation.<br />
Another limitation of the study is that the<br />
psychiatrist’s diagnosis may not represent<br />
an accurate gold st<strong>and</strong>ard, particularly in<br />
patients suffering a first episode of<br />
affective illness.<br />
In summary, the results of our study show<br />
that within the primary care setting in our<br />
catchment area screening for BPD is<br />
currently unacceptably low. Also it clearly<br />
shows that screening for BPD greatly<br />
enhances the chances of recognising this<br />
condition <strong>and</strong> that current screening<br />
methods used by primary care<br />
practitioners could be improved.<br />
Recommendations<br />
1. Increase awareness of BPD <strong>and</strong> the<br />
importance of screening within our<br />
primary care setting. This could be<br />
achieved by doing a presentation for<br />
GPs <strong>and</strong> MHNPs regarding the findings<br />
of our study.<br />
2. Role out the use of the MDQ as a<br />
st<strong>and</strong>ard screening tool to be<br />
administered to all patients in primary<br />
care presenting with an affective<br />
episode.<br />
3. Improve communication between<br />
primary <strong>and</strong> secondary care<br />
practitioners. This could be through<br />
informal discussions or telephone<br />
advice.<br />
4. Re-audit in 12 months to see the<br />
change in practice.<br />
References<br />
• Angst J. The emerging epidemiology<br />
of hypomania <strong>and</strong> bipolar II disorder.<br />
Journal of Affective Disorders, 1998; 50:<br />
143-51.<br />
• Bauer MS, McBride L, Williford WO et<br />
al. Collaborative Care for Bipolar<br />
Disorder: Part II. Impact on Clinical<br />
Outcome, Function, <strong>and</strong> Costs.<br />
Psychiatric Services, July 2006; 57:937-<br />
945.<br />
• Brickman, Andrew L, LoPiccolo et al.<br />
Screening for bipolar disorder. Psychiatric<br />
Services, March 2002; 53/3(349): 1075-<br />
2730.<br />
• Corona, Rodrigo, Berlanga et al.<br />
Detection of bipolar disorder with a<br />
clinical screening questionnaire: The<br />
Spanish version of the Mood Disorder<br />
Questionnaire. Salud Mental, March<br />
2007; 30(2): 50-57.<br />
• Das Gupta R, Guest JF. Annual cost of<br />
bipolar disorder to UK society. British<br />
Journal of Psychiatry, 2002; 180: 227-33.<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 15
Research <strong>and</strong> Audit<br />
• de Dois, Consuelo, Ezquiaga et al.<br />
Usefulness of the Spanish version of the<br />
Mood Disorder Questionnaire for<br />
screening for bipolar disorder in routine<br />
clinical practice in outpatients with major<br />
depression. Clinical Practice <strong>and</strong><br />
Epidemiology in Mental Health, May<br />
2008; 4:1745-0179.<br />
• Field A. Discovering Statistics using<br />
SPSS, Sage Publications Limited, 2009.<br />
• Hirschfeld RM. The Mood Disorder<br />
Questionnaire: A simple, patient-rated<br />
screening instrument for bipolar<br />
disorder. Primary care companion to the<br />
Journal of Clinical Psychiatry, February<br />
2002; 4(1):9-11.<br />
• Hunter R, Fraser K, Martin M, Hudson<br />
S. Bipolar disorder – aetiology <strong>and</strong><br />
pathophysiology. Hospital Pharmacist,<br />
2004; 11: 129-32.<br />
• Kasper S. Issues in the treatment of<br />
bipolar disorder. European<br />
Neuropsychopharmacology, 2003;<br />
13(Suppl 2): S37-42.<br />
• Kessler RC, McGonagle KA, Zhao S et<br />
al. Lifetime <strong>and</strong> 12-month prevalence of<br />
DSM-III-R psychiatric disorders in the<br />
United States. Results from the National<br />
Comorbidity Survey. Archives of General<br />
Psychiatry, 1994; 51: 8-19.<br />
• Menzin J, Sussman M, Tafesse E et al. A<br />
model of the economic impact of a bipolar<br />
disorder screening program in primary<br />
care. Journal of Clinical Psychiatry,<br />
September 2009; 70(9):1230-6.<br />
• Perry A, Tarrier N, Morriss R et al.<br />
R<strong>and</strong>omized controlled trial of efficacy of<br />
teaching patients with bipolar disorder to<br />
recognized early symptoms of relapse <strong>and</strong><br />
obtain treatment. BMJ, 16 January<br />
1999;318:149-153.<br />
• Sachs GS. Unmet clinical needs in<br />
bipolar disorder. Journal of Clinical<br />
Psychopharmacology, 2003; 23: S2-8.<br />
• Simon S. An introduction to diagnostic<br />
tests. The Children’s Mercy Hospital<br />
2007.<br />
• Stang P, Frank C, Ulcickas Yood M, et<br />
al. Impact of bipolar disorder: Results<br />
from a screening study. Primary care<br />
companion to the Journal of clinical<br />
psychiatry, 2007; vol/is 9/1(142-47),<br />
1523-5998.<br />
• Twiss J, Jones S, Anderson I. Validation<br />
of the Mood Disorder Questionnaire for<br />
screening for bipolar disorder in a UK<br />
sample. Journal of affective disorders,<br />
September 2008; 110(1-2):180-4.<br />
• Wehr TA, Goodwin FK. Can<br />
antidepressants cause mania <strong>and</strong> worse<br />
the course of affective illness? American<br />
Journal of Psychiatry, 1987; 144: 1403-11.<br />
• Weissman MM, Leaf PJ, Tischler GL et<br />
al. Affective disorders in five United<br />
States communities. Psychol Med 1988;<br />
18: 147-53.<br />
• World Health Organization. The ICD-<br />
10 Classification of Mental <strong>and</strong><br />
Behavioural Disorders. Clinical<br />
Descriptions <strong>and</strong> Diagnostic Guidelines.<br />
Geneva: WHO, 1992.<br />
16 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Audit of risk assessment<br />
documentation in adult in-patients -<br />
adherence to <strong>Trust</strong> guidelines <strong>and</strong> how<br />
to improve performance in this area<br />
By Abigail Crutchlow<br />
Acknowledgements: Many thanks to Dr L Church for his help in finalising this document<br />
Background<br />
Current local policy for SABP <strong>NHS</strong><br />
<strong>Foundation</strong> <strong>Trust</strong> states that all adult<br />
patients admitted to an in-patient unit<br />
within the <strong>Trust</strong> should have a<br />
st<strong>and</strong>ardised risk assessment form<br />
completed on admission <strong>and</strong> this should<br />
be updated regularly at every ward round<br />
or if a significant change in risk occurs.<br />
The aim of this audit is to provide an<br />
overview of performance <strong>and</strong> whether<br />
these guidelines are being met <strong>and</strong>, if<br />
not, to implement methods to improve<br />
performance. Through re-audit, the<br />
benefit <strong>and</strong> impact of such interventions<br />
<strong>and</strong> their role in the future will also be<br />
assessed. Formal ethical approval was not<br />
required for this audit as all data were<br />
anonymous <strong>and</strong> patients were not<br />
directly approached or involved in the<br />
audit. The audit was registered <strong>and</strong><br />
approved by the <strong>Trust</strong> audit department.<br />
Method<br />
Initial audit<br />
The initial audit included all current adult<br />
in-patients on general adult wards at the<br />
Abraham Cowley Unit, Chertsey. The<br />
PICU unit was not included due to<br />
altered level of risk for these patients.<br />
Their notes were identified <strong>and</strong> their risk<br />
assessment on admission <strong>and</strong> its<br />
subsequent updates examined.<br />
The following questions were asked:<br />
1. Was a complete risk assessment<br />
recorded on admission?<br />
• This included a completed<br />
comprehensive risk assessment<br />
within 24h of admission<br />
2. Has the risk assessment been updated<br />
regularly /at each ward round?<br />
• Occasional or irregular updates<br />
were not considered satisfactory<br />
• If the patient had been an in-patient<br />
for a very short time <strong>and</strong> not yet<br />
been seen on a ward round<br />
(meaning regular updates may not<br />
yet have commenced) then this was<br />
noted <strong>and</strong> they were excluded from<br />
question 2<br />
3. Is the risk assessment accessible to<br />
staff?<br />
• Information needed to be clearly<br />
visible in the appropriate section of<br />
the notes<br />
It was recorded whether all, some or<br />
none of these three criteria were met for<br />
each set of notes reviewed. The length of<br />
stay, regularity with which the patient<br />
was seen on a consultant ward round<br />
<strong>and</strong> the team they were under were also<br />
recorded, as these were identified as<br />
possible factors that could influence the<br />
results.<br />
In order to meet the st<strong>and</strong>ard guidelines,<br />
all three criteria needed to be met. The<br />
data was then analysed <strong>and</strong> results<br />
identified as below.<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 17
Research <strong>and</strong> Audit<br />
Based on the results of the initial audit,<br />
strategies to improve performance were<br />
implemented. An e-mail was circulated to<br />
all consultants <strong>and</strong> junior doctors<br />
involved in risk assessment for adult inpatients<br />
highlighting the outcomes <strong>and</strong><br />
raising awareness of the need for<br />
adequate risk assessment. The three<br />
questions <strong>and</strong> the need to fulfill these<br />
were documented in the e-mail along<br />
with the intent to re-audit in 2 months’<br />
time. As the changeover for junior<br />
doctors occurred shortly after the audit,<br />
this e-mail was circulated to both those<br />
doctors completing their post <strong>and</strong> those<br />
taking over from them.<br />
Re-audit<br />
A re-audit was undertaken in May 2009.<br />
23 sets of notes were r<strong>and</strong>omly selected<br />
from all the in-patients currently on ACU<br />
(split equally across Blake <strong>and</strong> Clare<br />
wards). The 23 notes selected were then<br />
examined using the method <strong>and</strong> analysis<br />
outlined in the initial audit. Results were<br />
obtained for an overall view of the<br />
different criteria being assessed. There<br />
was no breakdown of results by<br />
consultant or regularity of ward round as<br />
this showed no impact in the initial audit.<br />
Results were analysed depending on<br />
length of stay, as this was identified as<br />
having an impact. These results were then<br />
compared with those of the initial audit to<br />
see if the heightened awareness had<br />
altered the recording of risk assessment<br />
Based on the results of the first re-audit<br />
<strong>and</strong> the possible areas of bias, further<br />
strategies to improve performance were<br />
implemented <strong>and</strong> second re-audit<br />
conducted in November 2009, which was<br />
towards the end of the post for the<br />
cohort of doctors included. The second<br />
re-audit followed the same method <strong>and</strong><br />
structure as the earlier re-audit in May<br />
2009. This ensured that there had been<br />
consistency in the doctors completing the<br />
documentation over the last four months<br />
<strong>and</strong> also a long enough time period to<br />
ensure no notes had been included in the<br />
previous audit cycle. Formal teaching on<br />
risk assessment was delivered to the new<br />
cohort doctors at the beginning of their<br />
post in psychiatry at the ACU, Chertsey.<br />
This included an explanation of the risk<br />
assessment form <strong>and</strong> its importance, <strong>and</strong><br />
was conducted by one of the in-patient<br />
consultants.<br />
Results<br />
Fig.1 Initial audit – distribution overall<br />
100<br />
90<br />
80<br />
70<br />
60<br />
% 50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Criteria<br />
Initial RA<br />
Initial complete RA<br />
Regular updates<br />
RA accessible to staff<br />
Meets st<strong>and</strong>ard guidelines<br />
18 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Fig. 2 Re-audit May 2009 – distribution overall<br />
100<br />
90<br />
80<br />
70<br />
Initial RA<br />
60<br />
% 50<br />
40<br />
30<br />
20<br />
Initial complete RA<br />
Regular updates<br />
RA accessible to staff<br />
Meets st<strong>and</strong>ard guidelines<br />
10<br />
0<br />
Criteria<br />
Fig. 3 Re-audit November 2009 – distribution overall<br />
100<br />
90<br />
80<br />
70<br />
Initial RA<br />
60<br />
% 50<br />
40<br />
30<br />
20<br />
Initial complete RA<br />
Regular updates<br />
RA accessible to staff<br />
Meets st<strong>and</strong>ard guidelines<br />
10<br />
0<br />
Criteria<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 19
Research <strong>and</strong> Audit<br />
Discussion<br />
When considering the results of the initial<br />
audit, the numbers in several categories<br />
are too small to be of value when<br />
analysing the data by the different factors<br />
felt to be possible influences on the<br />
results. Results should be interpreted with<br />
this in mind. There was no clear variation<br />
of results by consultant or regularity of<br />
ward round. There does however appear<br />
to be a link between increasing length of<br />
stay <strong>and</strong> decreasing fulfillment of criteria.<br />
This may be due to becoming less aware<br />
of a patient’s risk the longer they stay <strong>and</strong><br />
an assumption that the risk is stable <strong>and</strong><br />
therefore the update is not completed as<br />
frequently <strong>and</strong> is more likely to be<br />
forgotten. The achievement of the<br />
recommended targets actually<br />
deteriorated when re-audited. This was<br />
mainly due to a reduction in completed<br />
risk assessments on admission <strong>and</strong> also a<br />
smaller percentage of risk assessments<br />
were updated regularly. There was also<br />
less evidence on re-auditing that length<br />
of stay impacted on achievement of<br />
recommended targets.<br />
Heightened awareness by e mail appears<br />
to have been ineffective therefore in<br />
improving st<strong>and</strong>ards. However, various<br />
factors could have impacted upon this.<br />
As a large number of junior doctors<br />
changed between the two data collection<br />
points, this could have affected the<br />
results as new doctors were less likely to<br />
have experience <strong>and</strong> remember to<br />
complete risk assessment forms than<br />
those who had been doing the job a few<br />
months. Also some notes would have<br />
been included in the data collection on<br />
both occasions, <strong>and</strong> this may have also<br />
altered results. Notes which had not met<br />
st<strong>and</strong>ards initially were unlikely to meet<br />
st<strong>and</strong>ards in the re-audit, which would<br />
have led to a disproportionately larger<br />
amount of notes not meeting st<strong>and</strong>ards<br />
in the re-audit compared to the initial<br />
audit. It was therefore beneficial to<br />
repeat the audit at a later stage towards<br />
the end of one group of junior doctors’<br />
employment (i.e. November/December<br />
2009). This allowed a long enough time<br />
period to ensure that no notes audited in<br />
earlier cycles are audited for a second<br />
time, which was a source of bias in the<br />
initial re-audit. This also allowed for<br />
consistency in documentation completion<br />
<strong>and</strong> had the advantage of identifying if<br />
time spent working in psychiatry helped<br />
increase awareness <strong>and</strong> completion of<br />
risk assessments <strong>and</strong> gave a more<br />
accurate picture of the benefit of any<br />
interventions that were implemented.<br />
Formal teaching on risk assessment was<br />
recommended during induction or in an<br />
early teaching session for this cohort of<br />
doctors as this has not been included in<br />
previous years. An improvement in<br />
meeting the recommened guidelines was<br />
evident from the re-audit in all areas, <strong>and</strong><br />
length of stay appeared to have less<br />
impact than in the previous cycles.<br />
It appears from the second re-audit that<br />
structured interventions <strong>and</strong> formal<br />
teaching that heighten awareness of the<br />
importance of risk assessment <strong>and</strong> how<br />
to complete the relevant paperwork have<br />
led to improvements in meeting the<br />
recommended guidelines. With the<br />
introduction to the ACU of the new<br />
computer system, RIO, such interventions<br />
will become all the more important in<br />
order to ensure risk continues to be<br />
documented to the highest st<strong>and</strong>ard. The<br />
overall outcome of this audit suggests<br />
that formal face to face teaching along<br />
with time spent working in psychiatry<br />
<strong>and</strong> heightened awareness on the ward<br />
of risk documentation are all necessary to<br />
optimise meeting the guidelines <strong>and</strong> such<br />
interventions should be regularly<br />
employed by the <strong>Trust</strong> for doctors, both<br />
at induction <strong>and</strong> throughout their<br />
rotation.<br />
20 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
An evolving service – results of a 3<br />
year follow up study of the practice of<br />
a community mental health team<br />
incorporating the principles of “New<br />
Ways of Working”<br />
June 2010 By Jeremy Mudunkotuwe, Farida Yousaf<br />
Acknowledgements: Helena DuToit, Dipesh Naik<br />
Introduction<br />
In 2005 the National Steering Group<br />
published “New Ways of Working for<br />
Psychiatrists”1. This document outlined<br />
the way in which teams could change in<br />
order to facilitate the time spent by the<br />
psychiatrist with the team considering<br />
their training <strong>and</strong> skill set. The<br />
requirements for this change necessitated<br />
a major change in service at the<br />
community psychiatry level. The changes<br />
were principally to enhance patients care,<br />
but were also planning for a perceived<br />
lack of psychiatrists in the future, due to<br />
increased retirement <strong>and</strong> inadequate<br />
numbers of doctors in training. Services<br />
around the country made changes in-line<br />
with the National Service Framework, <strong>and</strong><br />
the authors sort a way to monitor the<br />
changes within our team with regards to<br />
psychiatrists’ practice.<br />
Aim<br />
To assess over time the nature of<br />
psychiatrists’ appointments in the Mole<br />
Valley Primary Care Mental Health Team<br />
with regard to the changes as outlined in<br />
the “New Ways of Working” document<br />
published in 2005.<br />
Method<br />
An audit tool listing 15 reasons for<br />
psychiatric doctor appointments has been<br />
adapted from an audit tool described in<br />
the NWW report of 2005 “The Bromley<br />
<strong>and</strong> Greenwich Medical Staff Outpatient<br />
Clinic Audit Tool”1(see table 1). Each year<br />
from 2005 to 2008, for a 2 month period<br />
the psychiatrists within the team were<br />
asked to complete the audit tool for each<br />
patient they saw, either in their<br />
outpatients’ clinic, home visit or any<br />
other planned or emergency<br />
appointment. After each 2 month data<br />
collection period the results were collated<br />
<strong>and</strong> in 2009 the results for the 3 periods<br />
of assessment were compared.<br />
Table 1: The audit tool<br />
Reasons for assessment<br />
• DNA<br />
• New Assessment<br />
• Carer / family education / support<br />
• Court report preparation<br />
• CPA, or planning for CPA<br />
• Crisis planning / resolution<br />
• Discharge appointment<br />
• Medication review / prescribing<br />
• Mental state exam / diagnostic<br />
assessment<br />
• Physical health care check<br />
• Reassurance & support<br />
• Risk assessment / monitoring<br />
• Reports / benefits<br />
• Session of therapy as part of on-going<br />
course of therapy<br />
• Support than only a consultant can<br />
give due to complexity<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 21
Research <strong>and</strong> Audit<br />
Results<br />
The results were entered into a database<br />
<strong>and</strong> simple comparisons were made<br />
between the results for each category<br />
over the 3 periods of data collection. The<br />
Chart 1 Comparison of results from 2005-2008<br />
50<br />
45<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
DNA<br />
New<br />
Assessment<br />
Discharge<br />
appointment<br />
psychiatrists were allowed to select,<br />
none, one, or more than one of the<br />
fifteen categories for each case that they<br />
saw. Eight of the categories registered<br />
any results over the assessment periods.<br />
The results are shown in Chart 1 below.<br />
Medication<br />
review/prescribing<br />
Mental state<br />
examination/diagnosic<br />
assessment<br />
Reassurance<br />
<strong>and</strong> support<br />
Assessments 2005/2006<br />
Assessments 2007<br />
Assessments 2008<br />
Risk assessment/<br />
risk montoring<br />
Some notable trends were seen in the data collected over the 3 years.<br />
Crisis planning/<br />
crisis resolution<br />
The percentage of medication review <strong>and</strong> prescribing increased year on year, from<br />
27% in 2005/06, to 34% in 2007, <strong>and</strong> then to 46% in 2008.<br />
There was a marked increase in mental state examination <strong>and</strong> diagnostic<br />
appointments in the 2008 period (43%) compared to the years before, 18% in 2007<br />
<strong>and</strong> 20% in 2005/06.<br />
The percentage of appointments for reassurance <strong>and</strong> support remained at a similar<br />
level in each of the assessment periods.<br />
Risk assessment/monitoring appointments initially decreased in 2007 (1%) from<br />
the previous period but then markedly increased in the 2008 (14%) period.<br />
Discussion<br />
The authors felt that some really<br />
encouraging results were collected over<br />
the past 3 years indicating one aspect of<br />
the NWW movement that had greatly<br />
altered practice.<br />
We believe that the increase in the<br />
proportion of medication review <strong>and</strong><br />
prescribing is a result of the appointments<br />
with the psychiatrists utilising their skills<br />
appropriately. Team members have seemly<br />
felt more able to arrange for the patients<br />
they care coordinate to attend for this<br />
specific advice.<br />
Mental state examination <strong>and</strong> diagnostic<br />
should a substantial increase in the last<br />
period <strong>and</strong> again the authors believe that<br />
this is an appropriate use of time for the<br />
psychiatrist in the team <strong>and</strong> would<br />
benefit patient care. Also with increased<br />
need for coding <strong>and</strong> monitoring of<br />
service this allowed accurate accounting<br />
of illnesses treated within the team.<br />
Risk assessments have increased markedly<br />
increased in the past year <strong>and</strong> is perhaps<br />
a marker of the increased concern in the<br />
present climate about serious incidents<br />
related to mental health. This could be<br />
seen as a retrograde step towards doctors<br />
22 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
having clinical responsibility for all of the<br />
patients within the team, instead of this<br />
being devolved to the respective care<br />
coordinator. Further research could<br />
establish what happens with the<br />
information gathered at this time to<br />
establish whether risk information adds<br />
to the care coordinators management<br />
plan in an appropriate manner.<br />
Appointments offering reassurance <strong>and</strong><br />
support have remained at a low level<br />
throughout the assessment period this<br />
shows that despite changes to the service<br />
there is an appropriate level of this that<br />
should be offered by the psychiatrists.<br />
The authors believe that were this to be<br />
eliminated from their role then this would<br />
be to the detriment of patient care <strong>and</strong><br />
job satisfaction.<br />
A reduction in the DNA rate over the 3<br />
periods of assessment could be seen to<br />
be a sign that patients appreciate the<br />
change in the nature of appointments<br />
that has occurred over time. The authors<br />
recognise that this surrogate marker for<br />
patient satisfaction may not be a true<br />
reflection of patients’ views. Future audits<br />
of this nature within the team will include<br />
more direct measures of patient<br />
satisfaction.<br />
Changes within the team that have<br />
facilitated this evolution are sometimes<br />
hard to pinpoint. As the population<br />
covered by the team have not changed<br />
<strong>and</strong> neither has the demographics of the<br />
people living in the area so the change<br />
has been within the team. The authors<br />
believe that increased <strong>and</strong> more effective<br />
supervision of the MDT has been a major<br />
factor <strong>and</strong> resulted in requests for fewer<br />
outpatient appointments.<br />
Conclusion<br />
Debate in the psychiatric literature<br />
continues about how the NWW<br />
movement impacts upon the<br />
psychiatrists’ role, job satisfaction <strong>and</strong><br />
even recruitment 2,3,4,5 This literature has<br />
undoubtedly uncovered strong feelings<br />
that the majority feel that this process<br />
acts to the detriment of the psychiatrists’<br />
practice. The authors believe that the<br />
audit shows that an evolutionary change<br />
in the service need not be a tremendous<br />
upheaval if managed well, <strong>and</strong> could<br />
improve psychiatrists’ working practices.<br />
The authors recognise that the process of<br />
change can only be attempted if others in<br />
the team are willing to take on new<br />
responsibilities. We believe that more<br />
effective <strong>and</strong> regular supervision from<br />
medical staff to non medical staff in the<br />
team has facilitated this change within<br />
our team. We are aware that our audit<br />
does not take into respect their view<br />
points <strong>and</strong> further work will address this<br />
as well as more direct measures of<br />
patient satisfaction.<br />
References<br />
1. Department of Health; Final report<br />
from the National Steering Group. New<br />
ways of working for psychiatrists:<br />
Enhancing effective, person-centred<br />
services through new ways of working in<br />
multidisciplinary <strong>and</strong> multiagency<br />
contexts. Department of Health;<br />
31 October 2005 67.<br />
2. Craddock N, Antebi D, Attenburrow<br />
M-J, et al. Wake-up call for British<br />
psychiatry. The British Journal of<br />
Psychiatry 2008 July 1, 2008;193(1):6-9.<br />
3. Dale J, Milner G. New Ways not<br />
working? Psychiatrists' attitudes.<br />
Psychiatr Bull 2009 June 1,<br />
2009;33(6):204-7.<br />
4. St John-Smith P, McQueen D, Michael<br />
A, et al. The trouble with <strong>NHS</strong> psychiatry<br />
in Engl<strong>and</strong>. Psychiatr Bull 2009 June 1,<br />
2009;33(6):219-25.<br />
5. Vize C, Humphries S, Br<strong>and</strong>ling J, et al.<br />
New Ways of Working: time to get off<br />
the fence. Psychiatr Bull 2008 February 1,<br />
2008;32(2):44-5.<br />
Research <strong>and</strong> Audit<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 23
Commentary <strong>and</strong> Debate<br />
How can we look at improving<br />
recruitment into psychiatry?<br />
January 2009<br />
By Josie Jenkinson<br />
If recent figures are to be believed, fewer<br />
UK graduates are entering higher<br />
specialist training in psychiatry than ever<br />
before. Just 6% of c<strong>and</strong>idates sitting<br />
Paper 1 of the MRCPsych in diet one of<br />
2008 were UK graduates (Oxtoby, 2008),<br />
<strong>and</strong> this is likely to be a national indicator<br />
of recruitment trends (Brown et al, 2009).<br />
This has lead to widespread attention<br />
being focused on potential ways of<br />
improving recruitment into psychiatry,<br />
<strong>and</strong> the Royal College of Psychiatrists<br />
having taken specific steps to address the<br />
issue (Royal College of Psychiatrists,<br />
2009).<br />
The current recruitment crisis is by no<br />
means a new problem. In fact, concerns<br />
regarding poor recruitment into<br />
psychiatry have been discussed since the<br />
1970’s <strong>and</strong> there have been similar issues<br />
in other countries, most notably in the<br />
USA (Brockington, 2002). As a result,<br />
there has been a substantial amount<br />
written on the subject of recruitment into<br />
psychiatry. Much of the literature has<br />
been concerned with identifying the<br />
factors influencing the choice of<br />
psychiatry as a career as well as<br />
suggesting strategies that might be<br />
adopted to improve recruitment based on<br />
these factors. However, in the light of<br />
ongoing change within the <strong>NHS</strong> <strong>and</strong><br />
medical education, as well as a current<br />
climate of doubt <strong>and</strong> uncertainty as to<br />
the future role of the psychiatrist this is a<br />
very real <strong>and</strong> current issue facing the<br />
profession. Increasing reliance on<br />
international medical graduates to<br />
support <strong>and</strong> maintain delivery of<br />
psychiatric care increases the pressure to<br />
improve the current situation even<br />
further, given the possible impact of<br />
Home Office immigration policy changes<br />
(Brown et al, 2009).<br />
Any strategy aimed at improving<br />
recruitment into psychiatry would need<br />
to take into account the possible reasons<br />
why people choose psychiatry as a career,<br />
as well as what might deter them. This<br />
may be difficult as processes which<br />
influence doctors in their choice of career<br />
have been described as “subtle <strong>and</strong><br />
complex” (Eagles 2007), however I shall<br />
outline some of the possibilities below.<br />
Prior to entering medical school, many<br />
specialties including psychiatry are rated<br />
as a very attractive option (Maidment et<br />
al, 2003). However, this attitude is not<br />
maintained throughout the years of<br />
undergraduate training, with medical<br />
students tending to develop more<br />
negative attitudes about the specialty<br />
(Brockington, 2002). This may in part be<br />
due to the negative attitudes towards the<br />
profession from non-psychiatrists <strong>and</strong><br />
even psychiatrists themselves, for<br />
example describing psychiatrists as ‘not<br />
proper doctors’ (Craddock, 2008 p70).<br />
This is confounded by the sadly ever<br />
present stigma surrounding those with<br />
mental health problems <strong>and</strong> those who<br />
treat them, which medical students are<br />
exposed to both inside <strong>and</strong> outside of<br />
their training (Brockington, 2002). Four<br />
broad categories of negative opinions<br />
surrounding psychiatry as a specialty have<br />
been identified amongst medical<br />
students. These are related to the<br />
assumption that psychiatry lacks<br />
objectivity <strong>and</strong> is unscientific, that<br />
treatments are ineffective, that<br />
psychiatrists are ‘emotionally unstable’<br />
<strong>and</strong> ‘second rate’ doctors, <strong>and</strong> a dislike of<br />
the patient population treated by<br />
psychiatrists (Scott, 1986 p99).<br />
However, undergraduate exposure to<br />
psychiatry seems to be particularly<br />
important as a potentially positive<br />
influence, with consultants in psychiatry<br />
citing a lasting influence of medical<br />
24 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
school exposure to psychiatry as an<br />
influence on their ultimate choice of<br />
specialty, even if their career choice was<br />
made after leaving medical school (Dein<br />
et al, 2007). Several studies have found<br />
that intentions of students to pursue<br />
psychiatry as a career were increased<br />
following exposure to a psychiatric<br />
attachment during their years at medical<br />
school. Specific factors are likely to be<br />
associated with a greater intention to<br />
pursue psychiatry as a career following a<br />
psychiatric attachment; namely receiving<br />
encouragement from consultants, seeing<br />
patients respond to treatment <strong>and</strong> having<br />
direct involvement in patient care<br />
(McParl<strong>and</strong>, 2003).<br />
Positive elements of career in psychiatry<br />
which have been identified as appealing<br />
to prospective trainees are empathy for<br />
patients with a mental disorder, better<br />
working conditions, <strong>and</strong> the interface of<br />
psychiatry with neuroscience <strong>and</strong> the<br />
social sciences (Dein et al, 2007). Other<br />
factors identified as being important<br />
when choosing psychiatry as a specialty<br />
are enthusiasm <strong>and</strong> commitment for the<br />
specialty, <strong>and</strong> self appraisal of one’s own<br />
skills <strong>and</strong> aptitudes (Goldacre, 2005).<br />
In the light of the above, it would seem<br />
that focusing on the undergraduate<br />
experience of psychiatry as a target for<br />
increasing recruitment is paramount.<br />
Historically, this has been the reaction to<br />
the recruitment problem, <strong>and</strong> as a result<br />
pre-clinical teaching in psychology, social<br />
science <strong>and</strong> behavioural science now has<br />
a much greater emphasis. Inclusion of a<br />
psychiatry placement is now universal,<br />
however unfortunately it would seem<br />
that in recent years with the ever<br />
exp<strong>and</strong>ing dem<strong>and</strong>s placed on the<br />
curriculum, placements have decreased in<br />
length (Brown et al 2009). As such it is<br />
increasingly important that the best use is<br />
made of these placements, with students<br />
being actively involved in clinical care,<br />
being taught enthusiastically with an<br />
emphasis on evidence based medicine<br />
<strong>and</strong> patient recovery. Psychiatric trainees<br />
may be ideally placed to provide<br />
additional teaching <strong>and</strong> support to<br />
medical students, <strong>and</strong> should be<br />
encouraged to do so by their supervising<br />
consultants. Liaison psychiatry<br />
placements have been identified as being<br />
of particular appeal to medical students<br />
<strong>and</strong> may have special value in aiding<br />
recruitment in the future (Brockington,<br />
2002). Medical students who show an<br />
interest in pursuing psychiatry as a career<br />
should be encouraged <strong>and</strong> given ongoing<br />
support <strong>and</strong> careers advice (Eagles et al,<br />
2007).<br />
Another potential target for recruitment<br />
are those who have not yet entered<br />
medical school. It has been found that<br />
the type of person likely to pursue<br />
psychiatry as a career tends to have an<br />
interest in more psychological,<br />
sociological <strong>and</strong> artistic subjects, with<br />
many tending to have one A-level in a<br />
non-science subject (Brockington, 2002).<br />
They are also more likely to be from a<br />
lower social class, come from cities <strong>and</strong><br />
be politically liberal (Eagle <strong>and</strong> Marcos,<br />
1980). It may be that development of<br />
widening participation schemes <strong>and</strong><br />
graduate entry programmes may result in<br />
a greater number of students with these<br />
interests <strong>and</strong> attributes entering medical<br />
school <strong>and</strong> hence moving into psychiatry,<br />
although the effect of these<br />
developments has yet to be evaluated.<br />
Greater public awareness of mental<br />
health issues <strong>and</strong> the ongoing challenge<br />
of tackling stigma, possibly by<br />
improvement in public education <strong>and</strong><br />
covering of mental health issues as part<br />
of the primary <strong>and</strong> secondary school<br />
curriculum may in time raise the profile of<br />
psychiatry <strong>and</strong> lead to greater<br />
underst<strong>and</strong>ing <strong>and</strong> appeal of the<br />
specialty, however this is unlikely to yield<br />
results in the short term.<br />
Several surveys have identified that the<br />
majority of people choose psychiatry as a<br />
career after graduation rather than<br />
during the undergraduate years<br />
(Brockington, 2002). With this in mind,<br />
increasing positive exposure to psychiatry<br />
during the foundation years may well<br />
have a positive effect on recruitment. By<br />
the end of their first year of work post<br />
Commentary <strong>and</strong> Debate<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 25
Commentary <strong>and</strong> Debate<br />
qualification, doctors surveyed reported<br />
work experience as being a more<br />
important determinant of career choice<br />
when choosing psychiatry than with<br />
other specialties (Goldacre 2005). This<br />
would indicate that foundation posts in<br />
psychiatry may have a positive effect on<br />
recruitment, <strong>and</strong> this has been borne out<br />
to some extent (Boyle et al, 2009). Even<br />
where a doctor is unable to work in a<br />
foundation post, tasters in psychiatry can<br />
be organized as part of the foundation<br />
programme in order to give the<br />
foundation some additional experience<br />
of psychiatry.<br />
Unfortunately, doctors’ experiences of<br />
psychiatry if they are not doing a<br />
foundation post may be limited to<br />
occasional acute presentations, which if<br />
they do not have access to a psychiatric<br />
liaison service may be very difficult <strong>and</strong><br />
frustrating to manage. Liaison psychiatry<br />
services, where they exist, may present<br />
valuable opportunities for psychiatrists to<br />
demonstrate the relevance of the specialty<br />
across all branches of medicine, to portray<br />
a positive image of psychiatry to our nonpsychiatric<br />
colleagues as well as to<br />
educate <strong>and</strong> motivate those doctors who<br />
are as yet undecided in their career choice<br />
towards considering psychiatry as a career.<br />
In summary, the major possible targets for<br />
recruitment into psychiatry would appear<br />
to be improving undergraduate experience<br />
in a variety of ways, maximising positive<br />
exposure to psychiatry during the<br />
foundation years, <strong>and</strong> supporting those<br />
who show an interest in psychiatry early<br />
on. Ideally any strategy should be coupled<br />
with an overarching aim to increase the<br />
profile <strong>and</strong> awareness of the importance<br />
<strong>and</strong> validity of psychiatry as a profession<br />
amongst the lay population as well as the<br />
medical community.<br />
So what has been done to address the<br />
problem? The Royal College of<br />
Psychiatrists has taken urgent steps by<br />
means of a Scoping Group on<br />
Undergraduate Education in Psychiatry,<br />
which has helped to develop a core<br />
curriculum for undergraduate psychiatry.<br />
Work is also being done with the<br />
Academic Faculty <strong>and</strong> the Association of<br />
University Teachers of Psychiatry to address<br />
issues within the undergraduate<br />
experience that adversely affect the image<br />
of psychiatry (Brown et al, 2009).<br />
The Royal College has also prioritised a<br />
process of engaging more closely with<br />
medical students. A student associate<br />
grade has been introduced, whereby<br />
interested students can sign up to the<br />
Royal College for free <strong>and</strong> gain access to<br />
various resources, such as electronic<br />
versions of the Royal College’s<br />
publications, a dedicated section of the<br />
Royal College website, reduced prices for<br />
college events <strong>and</strong> a variety of other<br />
benefits. An annual summer school has<br />
been organised in collaboration with the<br />
Institute of Psychiatry <strong>and</strong> South London<br />
<strong>and</strong> the Maudsley <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong>.<br />
A lot of this work has been done with the<br />
help of the Psychiatric Trainees<br />
Committee, who have also embarked on a<br />
project of developing student psychiatry<br />
societies in each medical school across the<br />
UK. These societies, with the support of<br />
local consultants, academic departments<br />
<strong>and</strong> trainees, aim to foster interest <strong>and</strong><br />
raise the profile of psychiatry within<br />
medical schools by means of talks, careers<br />
events <strong>and</strong> educational meetings (Royal<br />
College of Psychiatrists, 2008).<br />
There is an additional aim to exp<strong>and</strong> the<br />
numbers of foundation posts available<br />
within psychiatry, however this will require<br />
extensive negotiation <strong>and</strong> planning with<br />
the <strong>Foundation</strong> Schools <strong>and</strong> is an ongoing<br />
project. The Psychiatric Trainees<br />
Committee is also developing an e-<br />
learning project to enable foundation<br />
doctors to develop psychiatry<br />
competencies, which will be mapped to<br />
the new foundation curriculum, <strong>and</strong> with<br />
an emphasis on the overlap of psychiatric<br />
problems <strong>and</strong> physical health problems.<br />
This project endeavours to increase the<br />
resources available for foundation doctors<br />
to further their underst<strong>and</strong>ing of the<br />
relevance of psychiatry to the medical<br />
profession as a whole.<br />
26 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
The measures outlined above will<br />
hopefully go some way to addressing the<br />
current issues surrounding recruitment<br />
into psychiatry, however it seems clear<br />
these measures will require the support<br />
of the profession as a whole. Portraying a<br />
positive image of psychiatry, by means of<br />
emphasis on academia, use of evidence<br />
based treatments, enthusiastic <strong>and</strong> active<br />
involvement in teaching of medical<br />
students <strong>and</strong> foundation doctors requires<br />
the help of all psychiatrists (of any grade)<br />
who may encounter them. Medical<br />
students <strong>and</strong> foundation doctors are our<br />
potential colleagues of the future, <strong>and</strong><br />
we owe it to our patients to try to recruit<br />
the very best.<br />
References<br />
Boyle A.M. et al (2009) ‘Recruitment<br />
from <strong>Foundation</strong> year 2 posts into<br />
specialty training: a potential success<br />
story?’ Psychiatric Bulletin 33: 306-308<br />
Brockington I., Mumford D. (2002)<br />
‘Recruitment into Psychiatry’ Br J<br />
Psychiatry 180: 307-12<br />
Brown N., Vassilas C. A., Oakley, C.<br />
(2009) ‘Recruiting Psychiatrists – A<br />
Sisyphean task?’ Psychiatric Bulletin 33:<br />
390 - 392<br />
Craddock N. et al (2008) ‘Wake-up call<br />
for British Psychiatry’ Br J Psychiatry 193:<br />
6-9<br />
Eagles J. M., Wilson S., Murdoch J. M.,<br />
Brown T. (2007) ‘What impact do<br />
undergraduate experiences have upon<br />
recruitment into psychiatry?’ Psychiatric<br />
Bulletin 31: 70-2<br />
Maidment R., Livingston G., Katona M.,<br />
et al (2004) ‘Changes in attitudes to<br />
psychiatry <strong>and</strong> intention to pursue<br />
psychiatry as a career in newly qualified<br />
doctors: a follow up of two cohorts of<br />
medical students’ Medical Teacher 26:<br />
565 - 569<br />
McParl<strong>and</strong> M., Noble L. M., Livingston G.,<br />
&McManus, C. (2003) ‘The effect of a<br />
psychiatric attachment on students’<br />
attitudes to <strong>and</strong> intention to pursue<br />
psychiatry as a career’ Medical Education<br />
37 (5): 447-454<br />
Oxtoby K. (2008) ‘Psychiatry in Crisis’<br />
British Medical Journal classified<br />
supplement 27/8<br />
Royal College of Psychiatrists (2008)<br />
Tackling psychiatry’s recruitment crisis<br />
head on RCPSych News 2010 Jan<br />
(http//www.rcpsych.ac.uk/member/rcpsyc<br />
hnews/november2008)<br />
Royal College of Psychiatrists (2009)<br />
Dean’s newsletter Royal College of<br />
Psychiatrists website 2010 Jan<br />
(http://www.rcpsych.ac.uk/specialtytrainin<br />
g.aspx)<br />
Scott, J. (1986) ‘What puts medical<br />
students off psychiatry?’ Bulletin of the<br />
Royal College of Psychiatrists 10<br />
Commentary <strong>and</strong> Debate<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 27
Book Reviews<br />
Psychiatry P.R.N.<br />
Principles, Reality, Next steps<br />
June 2010<br />
By Jose Jenkinson<br />
Edited by Sarah Stringer, Laurence<br />
Church, Susan Davison, Maurice<br />
Lipsedge<br />
Publisher Oxford University Press<br />
ISBN 978-0-19-956198-8<br />
Price £24.99<br />
Psychiatry PRN is a new textbook<br />
primarily aimed at medical students,<br />
which introduces the specialty in a very<br />
practical <strong>and</strong> unique way. It offers a<br />
different approach to the majority of<br />
psychiatry texts by means of focussing on<br />
the key aspects of psychiatry from a<br />
clinical point of view rather than a purely<br />
academic one, whilst covering most of<br />
the subject matter needed by<br />
undergraduates to get the most out of<br />
their placements <strong>and</strong> to equip them for<br />
the OSCEs.<br />
Part one of the book gives an overview of<br />
psychiatry, including classification,<br />
interviewing skills, safety, mental health<br />
law <strong>and</strong> the basics of assessment. Part<br />
two consists of 20 chapters which cover<br />
the major areas of psychiatry including<br />
mood disorders, schizophrenia,<br />
personality disorder, addictions <strong>and</strong> old<br />
age psychiatry. Topics are covered in 3<br />
stages, as per the title. Each chapter<br />
starts with outlining the ‘principles’ of the<br />
subject in question, followed by taking<br />
the reader through the ‘reality’ of how<br />
such patients present, by means of case<br />
histories, <strong>and</strong> practice OSCE stations.<br />
‘Next steps’ then focuses on<br />
management <strong>and</strong> specific issues relevant<br />
to the subject, eg capacity issues in<br />
relation to dementia. This pattern is<br />
followed throughout the chapters <strong>and</strong><br />
the format makes it a very easy book to<br />
dip in <strong>and</strong> out of as the need arises.<br />
The book is beautifully illustrated, with<br />
many of the pictures serving as an aide<br />
memoire for major conditions. Use of film<br />
<strong>and</strong> book quotes to illustrate topics <strong>and</strong><br />
lists of books <strong>and</strong> films alongside books<br />
<strong>and</strong> papers for further reading bring the<br />
subject alive <strong>and</strong> further increase the<br />
accessibility <strong>and</strong> subjective relevance of<br />
psychiatry in the eyes of the reader.<br />
Additional online resources are also<br />
included, with video clips of assessments,<br />
downloadable OSCE mark sheets, an<br />
MMSE outline as well as all the artwork<br />
in the book which can be downloaded<br />
for use in teaching sessions.<br />
Overall: This book is very much focussed<br />
on practical ins <strong>and</strong> outs of assessing<br />
psychiatric patients, <strong>and</strong> the importance<br />
of communication <strong>and</strong> empathy, rather<br />
than purely focussing on diagnostic<br />
categorisation, psychotropics <strong>and</strong> exam<br />
questions. As a result this is an extremely<br />
useful aide for students, <strong>and</strong> very<br />
different from other undergraduate<br />
textbooks available. Read in conjunction<br />
with one of the other weightier texts this<br />
should provide students with sound<br />
knowledge <strong>and</strong> practical ability, as well as<br />
being useful for any doctor starting their<br />
first psychiatry post or wanting to refresh<br />
their basic knowledge of the subject. It<br />
will also be highly relevant for anyone<br />
who teaches medical students as a basis<br />
for structuring teaching sessions, running<br />
practice osces <strong>and</strong> providing useful<br />
h<strong>and</strong>outs. It is fairly lightweight (<strong>and</strong> very<br />
portable) <strong>and</strong> offers good value for<br />
money given the amount of materials<br />
included in the price.<br />
Highly recommended<br />
28 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Interview with Fiona Edwards, Chief<br />
Executive SABP <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
June 2010 By Abigail Crutchlow (supervised by Raja Mukherjee)<br />
Fiona Edwards is the Chief Executive of<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> <strong>Partnership</strong> <strong>NHS</strong><br />
<strong>Foundation</strong> <strong>Trust</strong> <strong>and</strong> I met with her<br />
recently to interview her about some of<br />
the current issues <strong>and</strong> her views <strong>and</strong><br />
opinions on her role <strong>and</strong> how the <strong>Trust</strong><br />
can progress:<br />
Q. Many people working in the <strong>Trust</strong><br />
may not know that much about you.<br />
Can you tell me a bit about your<br />
background <strong>and</strong> interests?<br />
“My background is human resources<br />
professional, originally in industry, before<br />
working for the <strong>NHS</strong>. I achieved seniority<br />
fairly early on in my career, <strong>and</strong> initially I<br />
was very focussed on that, <strong>and</strong> then<br />
thought “what’s next? What does my<br />
career look like?” I was interested in<br />
exposure to an industry that I thought<br />
would be more people based. I became<br />
HR director in a Community Mental<br />
Health <strong>and</strong> Learning Disability <strong>Trust</strong> in<br />
Berkshire <strong>and</strong> after about six years<br />
became very focused in wanting to move<br />
into general management <strong>and</strong> a Chief<br />
Executive role, largely because I felt my<br />
professional background <strong>and</strong> the nature<br />
of the services <strong>and</strong> the work would match<br />
well in terms of what I consider needed to<br />
be sorted in the Health Service, which is<br />
people management. In my spare time I<br />
do a lot of running; physical exercise is<br />
important to me, it is my personal <strong>and</strong><br />
switching off time. I am competing in the<br />
London ASICS 10k race”.<br />
Q. We have now been a <strong>Foundation</strong><br />
<strong>Trust</strong> for about two years. What do<br />
you feel has gone well so far?<br />
“I am pleased to have achieved<br />
foundation trust status in a struggling<br />
health <strong>and</strong> social care economy. <strong>Surrey</strong><br />
has never had a good reputation from a<br />
financial management point of view, <strong>and</strong><br />
given that one of the main issues for a<br />
foundation trust is competence in<br />
running the organisation <strong>and</strong> being<br />
focussed, that has been a big<br />
achievement. Key factors in this include a<br />
strong executive <strong>and</strong> board team working<br />
ethos. We have invested a lot of time at a<br />
senior level concentrating on how we<br />
work as a multidisciplinary team. The<br />
other bit is optimism - rather than<br />
spending all our time focussing on what<br />
is going wrong <strong>and</strong> what is worrying us.<br />
One example would be when we were<br />
thrown by a negative visit by the Health<br />
Commission where it did expose some<br />
genuine criticisms. You could then go<br />
into immediate disaster scenario,<br />
thinking: “Is this what all our Services are<br />
like?” which is what we did. But what we<br />
then did, to get ourselves into a positive<br />
frame of mind, was to then systematically<br />
look at all the issues, but also why we, as<br />
a board <strong>and</strong> executive team, were not on<br />
the alert to this. It meant we had a much<br />
more comprehensive view of things,<br />
which some people might think is quite<br />
bureaucratic <strong>and</strong> audit based, but has<br />
helped me <strong>and</strong> the board to really focus<br />
on the importance of local team<br />
leadership”.<br />
Q. What are your visions for the<br />
future <strong>and</strong> can you outline any<br />
particular challenges faced,<br />
particularly running a geographically<br />
large <strong>Trust</strong>?<br />
“Over the last year we have put a huge<br />
amount of effort into our Staff Survey,<br />
getting a high level of response, <strong>and</strong><br />
involving all of our staff. This is to<br />
demonstrate to staff that we really want<br />
to underst<strong>and</strong> where they are at, <strong>and</strong><br />
through managing that process via local<br />
managers <strong>and</strong> leaders it will help me to<br />
underst<strong>and</strong> <strong>and</strong> manage individuals<br />
better as well as the organisation. With<br />
Interview<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 29
Interview<br />
regard to challenges I don’t see the<br />
geography as such a problem as the<br />
clinicians on the ground, because I have<br />
worked in a multinational organisation<br />
with places in different countries <strong>and</strong><br />
actually this <strong>Trust</strong> is not that big in the<br />
terms of geographical spread, although<br />
admittedly it is not like a hospital in that<br />
we are not all on one site. For the<br />
clinicians on the ground I think it is about<br />
really working at our IT infrastructure<br />
better <strong>and</strong> realising that we do not all<br />
have to be in one place. If you can get<br />
the IT infrastructure connected then the<br />
organisation will feel more connected in<br />
a different way, rather than in the<br />
traditional way of all being in one<br />
hospital. The IT strategy includes a<br />
Blackberry pilot which is now beginning<br />
to take off <strong>and</strong> one very basic, simple<br />
thing that M<strong>and</strong>y Stevens, Director of<br />
Quality Performance, has (she comes<br />
from the Priory, which has sites across the<br />
country) is doing telephone<br />
conferencing”.<br />
Q. I suppose the other issue is having<br />
sufficient funding <strong>and</strong> resources there<br />
for rolling out the Blackberries, <strong>and</strong><br />
other more financially draining<br />
aspects of communications?<br />
“They are actually reasonably easy to<br />
deliver; we just need to make sure we are<br />
managing it at a decent pace, because<br />
we do have a lot of people (not least<br />
myself) who are not over confident with<br />
technology!”<br />
Q. That leads on to discussing money<br />
<strong>and</strong> other opportunities. If money<br />
was no object, as a hypothetical<br />
question, what other services would<br />
you like to bring in?<br />
“Well I would object to that question<br />
because that is not the real world. I think<br />
as an organisation we have to help<br />
people underst<strong>and</strong> that limited resources<br />
<strong>and</strong> service development go h<strong>and</strong> in<br />
h<strong>and</strong>. My particular interest is around<br />
having a much greater focus on<br />
wellbeing. I am very interested in the<br />
nature of the <strong>Surrey</strong> population <strong>and</strong> why<br />
<strong>Surrey</strong> has such a high usage of general<br />
hospitals acute care, when it is technically<br />
supposed to be one of the healthiest,<br />
wealthiest counties in the nation. I think<br />
we have some fantastic opportunities as<br />
a Mental Health <strong>and</strong> Learning Disability<br />
<strong>Trust</strong> to move away from looking at<br />
individual specialties <strong>and</strong> to try to use the<br />
expertise we have in our clinicians to start<br />
answering those questions for a bigger<br />
population. I think that getting people to<br />
underst<strong>and</strong> <strong>and</strong> think of the connection<br />
between mental <strong>and</strong> physical health, in<br />
the way Services are commissioned, is a<br />
real challenge”.<br />
Q. There have been some difficult<br />
decisions recently that have had to be<br />
made across the <strong>Trust</strong> regarding bed<br />
closures <strong>and</strong> reconfiguration. Do you<br />
think there are any particular lessons<br />
that came out of that?<br />
“I think one of the lessons is that there<br />
has been no reduction in the number of<br />
people that are being seen <strong>and</strong> the<br />
reason we have been able to close beds is<br />
because the system in the community is<br />
up <strong>and</strong> running well. Admittedly there<br />
has been some discontent around it, but<br />
not as much as there may have been<br />
elsewhere. The readiness of people to<br />
work with it <strong>and</strong> try it out is a<br />
phenomenal testimony to the sound<br />
clinical practice <strong>and</strong> teamwork in those<br />
systems. The best way to manage such<br />
issues is to have a strong multidisciplinary<br />
team locally, with strong confident<br />
clinicians, who are able to work<br />
collaboratively. My job is to make sure we<br />
have the right people in the senior<br />
leadership positions <strong>and</strong> the competence,<br />
confidence <strong>and</strong> climate so that people<br />
have the challenge <strong>and</strong> discussion before,<br />
rather than after, the event”.<br />
30 <strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal
Q. Very topical to that is the<br />
appointment of a new Medical<br />
Director of the <strong>Trust</strong>. How do you<br />
view the role of medical director? I<br />
underst<strong>and</strong> that there has been some<br />
discussion of the role changing in<br />
some respects. How do you envisage<br />
that role <strong>and</strong> how will you ensure you<br />
seek out <strong>and</strong> engage the right<br />
person?<br />
“I view the Medical Director as being the<br />
clinical leader of the organisation. What I<br />
really want to see is someone who brings<br />
a vision for the clinical tasks of the <strong>Trust</strong><br />
overall <strong>and</strong> pulling the whole thing<br />
together. This is someone who can talk to<br />
all clinicians, not just doctors, who can<br />
underst<strong>and</strong> where everyone is at <strong>and</strong><br />
someone who is excited by the thought<br />
of taking the leadership, rather than<br />
doing it out of evil necessity”.<br />
Q. How do view the role of medics<br />
<strong>and</strong> clinicians within the <strong>Trust</strong>? How<br />
do you feel they should be working<br />
with management to get a<br />
collaborative approach?<br />
“I think they should be part of the<br />
management team, not see themselves<br />
as separate from it. They should be<br />
confident leaders. I would like to see a<br />
little bit more pressure from the clinicians<br />
in the organisation, a bit more testing<br />
<strong>and</strong> more questioning <strong>and</strong> confidence in<br />
admitting what they don’t know, <strong>and</strong><br />
what they need in help in underst<strong>and</strong>ing<br />
about how a foundation trust <strong>and</strong> the<br />
finances work. I do see some really good<br />
examples where clinicians are very clear<br />
on their ambition for theirs services, for<br />
example a liaison service in one part of<br />
the <strong>Trust</strong> got up <strong>and</strong> running from the<br />
vision of the medical lead”.<br />
Q. Do you have any final comments<br />
that you would like to make?<br />
“The other area that I am really interested<br />
in for this organisation, going back to<br />
your question about what I get excited<br />
about, is research <strong>and</strong> education. I think<br />
we have more opportunities emerging in<br />
the sense of research for patient benefit.<br />
It is something we could build our<br />
reputation around in partnership with the<br />
service user community <strong>and</strong> also with the<br />
universities”.<br />
Q. That was one of the areas that the<br />
Care Quality Commission mentioned<br />
as lacking on their recent visit to the<br />
<strong>Trust</strong> so it is an important area. So<br />
again that is something quite<br />
important.<br />
“I wasn’t aware of that specific issue so<br />
much, but it doesn’t surprise me. What<br />
we are doing with the role of the Medical<br />
Director <strong>and</strong> the fact that we want to<br />
elevate the research <strong>and</strong> development<br />
directorate function, to have it more<br />
closely overseen by the Board, dovetails<br />
with seeking to address that concern. I<br />
am very clear as Chief Executive that we<br />
need to get it right, for the kind of<br />
organisation we are, but also pay much<br />
more strategic attention to it”.<br />
Interview<br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> Online Journal www.sabp.nhs.uk/journal 31
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> <strong>Partnership</strong><br />
<strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
<strong>Surrey</strong> <strong>and</strong> <strong>Borders</strong> <strong>Partnership</strong> <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
<strong>Trust</strong> Headquarters, 18 Mole Business Park<br />
Leatherhead, <strong>Surrey</strong> KT22 7AD<br />
Tel: 01883 383838 www.sabp.nhs.uk