RxAmerica Prior Authorization Criteria:
RxAmerica Prior Authorization Criteria:
RxAmerica Prior Authorization Criteria:
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
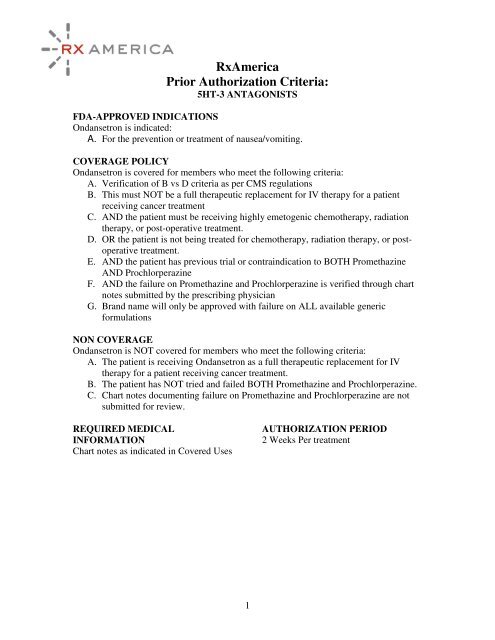
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
5HT-3 ANTAGONISTS<br />
FDA-APPROVED INDICATIONS<br />
Ondansetron is indicated:<br />
A. For the prevention or treatment of nausea/vomiting.<br />
COVERAGE POLICY<br />
Ondansetron is covered for members who meet the following criteria:<br />
A. Verification of B vs D criteria as per CMS regulations<br />
B. This must NOT be a full therapeutic replacement for IV therapy for a patient<br />
receiving cancer treatment<br />
C. AND the patient must be receiving highly emetogenic chemotherapy, radiation<br />
therapy, or post-operative treatment.<br />
D. OR the patient is not being treated for chemotherapy, radiation therapy, or postoperative<br />
treatment.<br />
E. AND the patient has previous trial or contraindication to BOTH Promethazine<br />
AND Prochlorperazine<br />
F. AND the failure on Promethazine and Prochlorperazine is verified through chart<br />
notes submitted by the prescribing physician<br />
G. Brand name will only be approved with failure on ALL available generic<br />
formulations<br />
NON COVERAGE<br />
Ondansetron is NOT covered for members who meet the following criteria:<br />
A. The patient is receiving Ondansetron as a full therapeutic replacement for IV<br />
therapy for a patient receiving cancer treatment.<br />
B. The patient has NOT tried and failed BOTH Promethazine and Prochlorperazine.<br />
C. Chart notes documenting failure on Promethazine and Prochlorperazine are not<br />
submitted for review.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
2 Weeks Per treatment<br />
1
FDA-APPROVED INDICATIONS<br />
Actimmune® is indicated:<br />
A. Chronic Granulomatous Disease<br />
B. Severe Malignant Osteopetrosis<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ACTIMMUNE<br />
COVERAGE POLICY<br />
Actimmune® is covered for members who meet the following criteria:<br />
A. Documented Chronic Granulomatous Disease or Severe Malignant Osteopetrosis<br />
B. AND have had CBC, differential, and platelet counts to illustrate Hepatic levels<br />
WNL. Tests need to be administered in three month intervals to avoid hepatic<br />
toxicity<br />
C. AND no history of myelosuppression.<br />
NON COVERAGE<br />
Actimmune® is NOT covered for members with the following criteria:<br />
A. Hypersensitivity to E.Coli derived products and/or interferon gamma.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
3 months<br />
2
FDA APPROVED INDICATIONS<br />
A. Osteoporosis<br />
B. Osteoporosis Prophylaxis<br />
C. Paget’s Disease:<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ACTONEL<br />
COVERAGE POLICY<br />
A. Patient has failure to generic alendronate or contraindication<br />
B. AND has diagnosis of Osteoporosis indicated by a T-Score of 2.5 or more<br />
standard deviations below the young-adult mean BMD or X-ray illustrating<br />
fracture in the spine and/or hip.<br />
C. For Paget’s Disease the member must have documented failure to alendronate<br />
therapy for 6 months or contraindication to alendronate<br />
NON COVERAGE<br />
Actonel is not covered for members who meet the following criteria:<br />
A. No documentation to failure to alendronate therapy,<br />
B. Or T-Score value that does not indicate osteoporosis<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart Notes. T-score or X-ray<br />
illustrating fracture<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
3
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ADAGEN<br />
FDA-APPROVED INDICATIONS<br />
Adagen® is indicated:<br />
A. Adenosine Deaminase (ADA) deficiency<br />
COVERAGE POLICY<br />
Adagen® is covered for members who meet the following criteria:<br />
A. Documented diagnosis of Adenosine Deaminase (ADA) deficiency<br />
B. AND patient has failed bone marrow transplantation or is not a suitable<br />
candidate for bone marrow transplantation<br />
C. AND is being used for direct replacement for deficient enzyme (no benefit<br />
achieved in patients with immunodeficiency due to other causes)<br />
NON COVERAGE<br />
Adagen® is NOT covered for members with the following criteria:<br />
A. Immunodeficencies that do not have an association with adenosine deaminase<br />
B. Patient has diagnosis of severe thrombocytopenia<br />
C. Use for preparatory or support therapy for bone marrow transplantation<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
4
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AFINITOR<br />
FDA-APPROVED INDICATIONS<br />
A. All FDA approved indications not otherwise excluded from Part D.<br />
COVERAGE POLICY<br />
Afinitor is covered for patient that meet the following criteria:<br />
A. Patient must have previous trial and failure with one of the following:<br />
a. Sutent<br />
b. Nexavar<br />
REQUIRED MEDICAL INFORMATION<br />
The following copies of chart notes/laboratory reports are required:<br />
A. Documentation of previous trial/failure of Sutent or Nexavar<br />
AGE RESTRICTIONS<br />
Patient must be 18 years of age or older<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
5
FDA-APPROVED INDICATIONS<br />
Agrylin® is indicated:<br />
A. Chronic Myelogenous Leukemia<br />
B. Polycythemia Vera<br />
C. Thrombocytosis<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AGRYLIN<br />
COVERAGE POLICY<br />
Agrylin® is covered for members who meet the following criteria:<br />
A. Agrylin® is not covered unless contraindication to the all commercially<br />
available generic anagrelide products. Therefore only generic anagrelide will<br />
be covered.<br />
B. AND is being used for Chronic Myelogenous Leukemia, Polycythemia Vera,<br />
Thrombocytosis<br />
a. Chronic Myelogenous Leukemia diagnosis:<br />
i. Persistent granulocyte count Greater than or equal to<br />
50,000/mcL w/o infection<br />
ii. Absoulte basophil count Greater than or equal to 100/mcL<br />
iii. Evidence for hyperplasia of the granulocytic line in the bone<br />
marrow<br />
iv. Philadelphia chromosome is present<br />
v. Luekocyte alkaline phosphatase Less than or equal to lower<br />
limit of the lab range<br />
b. Polycythemia Vera diagnosis:<br />
i. Increased red cell mass<br />
ii. Normal arterial oxygen saturation<br />
iii. Splenomegaly<br />
iv. Platelet Count Greater than or equal to 400,000/mcL w/o iron<br />
deficiency or bleeding<br />
v. Leukocytosis Greater than or equal to 12,000/mcL w/o<br />
infection<br />
vi. Elevated leukocyte alkaline phosphatase<br />
vii. Elevated serum B12<br />
c. Thrombosytosis diagnosis:<br />
i. Platelet Count Greater than or equal to900,000/mcL<br />
ii. Profound megakaryocytic hyperplasia in bone marrow<br />
iii. Absence of Philadelphia chromosome<br />
iv. Normal red cell mass<br />
v. Normal serum iron and ferritin and normal marrow iron stores<br />
C. AND patient does not have severe hepatic impairment<br />
D. AND patient does not have known or suspected heart disease a pre-treatment<br />
cardiovascular examination is required to ensure safety.<br />
6
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AGRYLIN<br />
(Continued)<br />
NON COVERAGE<br />
Agrylin® is NOT covered for members with the following criteria:<br />
A. Severe hepatic impairment<br />
B. Women who are or may become pregnant<br />
C. Known heart disease<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist or Hematologist<br />
AUTHORIZATION PERIOD<br />
2 months<br />
7
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ALDURAZYME<br />
FDA-APPROVED INDICATIONS<br />
Aldurazyme® is indicated:<br />
A. For patients with Hurler and Hurler-Scheie forms of Mucopolysaccharidosis I<br />
(MPS) and for patients with the Scheie form who have moderate-to-severe<br />
symptoms.<br />
COVERAGE POLICY<br />
Aldurazyme® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as Hurler syndrome (MPS 1H) or Hurler-Scheie<br />
syndrome (MPS IS).<br />
B. OR the diagnosis is documented as Scheie syndrome (MPS IS).<br />
C. AND the patient has at least two of the listed moderate-to-severe symptoms.<br />
Impaired vision Recurrent otitis media Recurrent<br />
sinopulmonary<br />
infections<br />
Impaired hearing Upper airway obstruction Malaise and reduced<br />
endurance<br />
Corneal clouding Macrocephaly Reduced joint range<br />
of motion<br />
Progressively<br />
coarse facial<br />
features<br />
Carpal tunnel<br />
syndrome<br />
Cardiac<br />
abnormalities and<br />
valvular disease<br />
Coarse facial features<br />
Delayed or regressed<br />
mental development<br />
Communicating<br />
hydrocephalus<br />
Umbilical and<br />
inguinal hermias<br />
Hepatosplenomegaly<br />
Spinal cord<br />
compression<br />
Sleep apnea Short stature Reduced pulmonary<br />
function<br />
Bone deformities<br />
D. AND diagnosis has been confirmed by diagnostic method (measurement of alphaiduronidase<br />
activity) or antenatal diagnosis (enzymatic assay).<br />
E. AND if the patient has previously received at least 26 weeks of Aldurazyme®<br />
therapy, they must show an improvement in lung function (forced vital capacity<br />
[FVC] from when therapy was started.<br />
8
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ALDURAZYME<br />
(Continued)<br />
NON COVERAGE<br />
Aldurazyme® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as Hurler syndrome, Hurler-Scheie syndrome<br />
or Scheie syndrome.<br />
B. If the diagnosis is Scheie syndrome and they do not have at least two mild-tomoderate<br />
severe symptoms.<br />
C. If the diagnosis has NOT been confirmed by diagnostic method or antenatal<br />
diagnosis.<br />
D. If the patient has previously received at least 26 weeks of Aldurazyme® therapy<br />
and they have not shown an Improvement in lung function [FVC].<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
9
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ALFERON N<br />
FDA-APPROVED INDICATIONS<br />
Alferon N® is indicated:<br />
A. For intralesional treatment of refractory or recurring external condylomata<br />
acuminate in patients 18 years or age or older.<br />
COVERAGE POLICY<br />
Alferon N® is covered for members who meet the following criteria:<br />
A. Patient has NO allergy to egg protein, immunoglobulin (IgG) or neomycin.<br />
B. AND the patient must have a diagnosis for Condylomata Acuminata.<br />
C. AND the patient is 18 years of age or older.<br />
D. AND the prescribing physician is a board certified dermatologist or obtained a<br />
consult from the listed specialty.<br />
E. AND the patient has tried, failed or intolerant to a 16 week course of Aldara®<br />
treatment.<br />
F. AND approval can be allowed for up to 8 weeks.<br />
G. AND if the patient has received previous therapy, the patient must not initiate<br />
therapy until 3 months after the initial course of therapy unless the warts enlarge<br />
or new warts appear.<br />
H. AND the initial therapy must have shown a clinical benefit that shows resolution<br />
or decrease in wart size. And approval can be allowed for up to 8 weeks.<br />
NON COVERAGE<br />
Alferon N® is NOT covered for members with the following criteria:<br />
A. Patient has an allergy to egg protein, immunoglobulin or neomycin.<br />
B. The diagnosis is NOT Condylomata Acuminata.<br />
C. If the diagnosis is for Condylomata Acuminata and the patient meets one or more<br />
of the following criteria:<br />
D. AND the patient is under the age of 18 years old<br />
E. AND/OR the prescribing physician is NOT a dermatologist or has NOT obtained<br />
a consult.<br />
F. AND/OR the patient has NOT tried, failed or is intolerant to a 16 week course of<br />
Aldara®.<br />
G. AND/OR the patient has received previous therapy and the request is NOT<br />
beyond 3 months from the initial request AND/OR NO new warts have appeared<br />
or enlarged<br />
H. AND/OR the initial therapy has NOT shown a clinical benefit.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
8 weeks<br />
10
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AMITIZA<br />
FDA-APPROVED INDICATIONS<br />
Amitiza® is indicated:<br />
A. For the treatment of chronic idiopathic constipation in adults.<br />
B. For the treatment of irritable bowel syndrome-constipation predominant<br />
C. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Amitiza® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as chronic idiopathic constipation OR irritable bowel<br />
syndrome-constipation predominant.<br />
B. AND patient is 18 years of age or older.<br />
C. AND the patient has NO history of mechanical gastrointestional obstruction.<br />
D. AND the patient is not pregnant if female.<br />
E. AND the patient meets 2 (two) or more of the following ROME criteria for the<br />
diagnosis of chronic constipation for at least 12 weeks in the preceding 12<br />
months:<br />
a. Straining during Greater than 25% of bowel movement.<br />
b. Lumpy or hard stools for Greater than 25% of bowel movement.<br />
c. Less than 3 (three) stools per week.<br />
d. Sensation of incomplete evacuation for Greater than 25% of bowel<br />
movement.<br />
e. Sensation of anorectal blockage for Greater than 25% of bowel movement.<br />
f. Loose stools not present.<br />
g. Manual maneuvers are needed to facilitate Greater than 25% of bowel<br />
movement.<br />
F. AND the patient has tried and failed a drug regimen of lactulose for greater than 3<br />
(three) months. (Please verify that the patient has received polyethylene glycol<br />
therapy for three months by reviewing the patient’s drug history or the patient’s<br />
chart notes).<br />
G. AND if the patient has received previous Amitiza® therapy, the physician must<br />
show a documented Improvement in the patient’s stool frequency, stool<br />
consistency and/or abdominal distention from the beginning of Amitiza®<br />
treatment.<br />
H. AND evidence of ROME criteria, failure to drug regimens and improvement in<br />
symptoms are documented in patient’s chart notes provided by prescribing<br />
provider.<br />
NON COVERAGE<br />
Amitiza® is NOT covered for members with the following criteria:<br />
A. Diagnosis is NOT documented as chronic constipation OR irritable bowel<br />
syndrome-constipation predominant.<br />
B. Patient is 17 years of age or younger.<br />
11
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AMITIZA<br />
(Cotninued)<br />
C. Patient does NOT meet 2 of the ROME criteria for chronic constipation.<br />
D. Patient has NOT failed a 3 month trial of polyethylene glycol.<br />
E. Patient has NOT failed a 3 month trial of lactulose.<br />
F. If the patient has had previous Amitiza® and has NOT shown an improvement in<br />
symptoms.<br />
G. Provider has NOT provided the patient’s chart notes for documentation.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
12
FDA-APPROVED INDICATIONS<br />
Agrylin® is indicated:<br />
A. Chronic Myelogenous Leukemia<br />
B. Polycythemia Vera<br />
C. Thrombocytosis<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ANAGRELIDE<br />
COVERAGE POLICY<br />
Agrylin® is covered for members who meet the following criteria:<br />
A. Agrylin® is not covered unless contraindication to the all commercially available<br />
generic anagrelide products. Therefore only generic anagrelide will be covered.<br />
B. AND is being used for Chronic Myelogenous Leukemia, Polycythemia Vera,<br />
Thrombocytosis<br />
a. Chronic Myelogenous Leukemia diagnosis:<br />
i. Persistent granulocyte count Greater than or equal to 50,000/mcL w/o<br />
infection<br />
ii. Absoulte basophil count Greater than or equal to 100/mcL<br />
iii. Evidence for hyperplasia of the granulocytic line in the bone marrow<br />
iv. Philadelphia chromosome is present<br />
v. Luekocyte alkaline phosphatase Less than or equal to lower limit of<br />
the lab range<br />
b. Polycythemia Vera diagnosis:<br />
i. Increased red cell mass<br />
ii. Normal arterial oxygen saturation<br />
iii. Splenomegaly<br />
iv. Platelet Count Greater than or equal to 400,000/mcL w/o iron<br />
deficiency or bleeding<br />
v. Leukocytosis Greater than or equal to 12,000/mcL w/o infection<br />
vi. Elevated leukocyte alkaline phosphatase<br />
vii. Elevated serum B12<br />
c. Thrombosytosis diagnosis:<br />
i. Platelet Count Greater than or equal to900,000/mcL<br />
ii. Profound megakaryocytic hyperplasia in bone marrow<br />
iii. Absence of Philadelphia chromosome<br />
iv. Normal red cell mass<br />
v. Normal serum iron and ferritin and normal marrow iron stores<br />
vi. AND patient does not have severe hepatic impairment<br />
vii. AND patient does not have known or suspected heart disease a pretreatment<br />
cardiovascular examination is required to ensure safety.<br />
13
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ANAGRELIDE<br />
(Continued)<br />
NON COVERAGE<br />
Agrylin® is NOT covered for members with the following criteria:<br />
A. Severe hepatic impairment<br />
B. Women who are or may become pregnant<br />
C. Known heart disease<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist or Hematologist<br />
AUTHORIZATION PERIOD<br />
2 months<br />
14
FDA-APPROVED INDICATIONS<br />
Antizol® is indicated:<br />
A. Ethylene Glycol Poisoning<br />
B. Methanol Poisoning<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ANTIZOL<br />
COVERAGE POLICY<br />
Antizol® is covered for members who meet the following criteria:<br />
A. Patient is suffering from acute methanol or ethylene glycol poisoning<br />
B. AND verification of all B vs. D criteria indicate coverage by Part D<br />
NON COVERAGE<br />
Antizol® is NOT covered for members with the following criteria:<br />
A. Known hypersensitivity to fomepizole or other pyrazoles<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
3 days<br />
15
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ATGAM<br />
FDA-APPROVED INDICATIONS<br />
Atgam® is indicated:<br />
A. Aplastic Anemia<br />
B. Kidney Transplant Rejection or prophylaxis<br />
COVERAGE POLICY<br />
Atgam® is covered for members who meet the following criteria:<br />
A. Patient is receiving concomitant immunosuppressive therapy<br />
B. AND verification of all B vs. D criteria indicate coverage by Part D<br />
NON COVERAGE<br />
Atgam® is NOT covered for members with the following criteria:<br />
A. Patients not receiving concomitant immunosuppressive therapy<br />
B. Medication should be administered through Medicare Part B<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Initial authorization: 14 days<br />
16
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AVONEX<br />
FDA-APPROVED INDICATIONS<br />
Avonex® is indicated:<br />
A. For the treatment of patients with relapsing forms of multiple sclerosis to slow the<br />
accumulation of physicial disability and decrease the frequency of clinical<br />
exacerbations. Safety and efficacy in patients with chronic progressive multiple<br />
sclerosis have not been established.<br />
COVERAGE POLICY<br />
Avonex® is covered for members who meet the following criteria:<br />
A. The prescribing provider is a neurologist or has obtained a consult from the listed<br />
specialty.<br />
B. AND the diagnosis is documented as Relapsing-Remitting Multiple Sclerosis.<br />
(Avonex® does not have the indication for primary progressive, secondary<br />
progressive or progressive relapsing multiple sclerosis).<br />
C. AND the patient has a history of at least two focal neurological deficits (e.g., loss<br />
of vision, double vision, localized numbness, localized weakness, walking gait<br />
abnormalities, slurred speech, tingling) in which the second deficit followed after<br />
the resolution of the first deficit.<br />
D. AND an MRI has been performed and is suggestive of multiple sclerosis<br />
(evidence of lesion).<br />
E. AND the patient will NOT be receiving Avonex® therapy in combination with<br />
interferon-beta therapy (e.g., Rebif®, or Betaseron®), Copaxone® or<br />
mitoxantrone. (Please verify that the patient is not on duplicate therapy by<br />
reviewing the patient’s drug history or chart).<br />
F. AND if the patient has received previous Avonex® therapy, the provider can<br />
document a decrease in the frequency of clinical relapses OR slowing in the<br />
progression of the disease OR the patient has remained stable OR lesions on MRI<br />
have diminished after initiation of therapy.<br />
NON COVERAGE<br />
Avonex® is NOT covered for members with the following criteria:<br />
A. The prescribing provider is NOT a neurologist or the prescribing provider has<br />
NOT obtained a consult from the listed specialty.<br />
B. The diagnosis is NOT documented as Relapsing-Remitting Multiple Sclerosis.<br />
C. The diagnosis is documented as primary progressive, secondary progressive or<br />
progressive relapsing multiple sclerosis.<br />
D. The patient has NO history of at least two focal neurological deficits.<br />
E. The patient has a history of at least two focal neurological deficits but the initial<br />
deficit did not resolve before the start of the second deficit.<br />
F. An MRI has NOT been performed.<br />
G. An MRI has been performed but is NOT suggestive of multiple sclerosis (no<br />
evidence of lesion).<br />
17
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AVONEX<br />
(Continued)<br />
H. The patient will be receiving Avonex® therapy in combination with interferonbeta<br />
therapy (e.g., Rebif® or Betaseron®), Copaxone® or mitoxantrone.<br />
I. If the patient has received previous Avonex® therapy and he/she cannot show a<br />
decrease in the frequency of clinical relapses or slowing in the progression of the<br />
disease or a decrease in the lesions on MRI or stability of the disease.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Neurologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
18
FDA-APPROVED INDICATIONS<br />
Azathioprine is indicated:<br />
A. Kidney rejection prophylaxis<br />
B. Rheumatoid arthritis<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
AZATHIOPRINE<br />
COVERAGE POLICY<br />
Azathioprine is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with Rheumatoid Arthritis<br />
a. Failure to 3 months therapy of NSAIDs<br />
B. Kidney Transplant Prophylaxis<br />
a. Coverage of Kidney transplant is not covered or was not covered by<br />
Medicare Part B<br />
NON COVERAGE<br />
Azathioprine is NOT covered for members with the following criteria:<br />
A. Kidney transplantation or other form of transplant surgery was covered by<br />
Medicare Part B.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
19
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
BANZEL<br />
FDA-APPROVED INDICATIONS<br />
Banzel® is indicated:<br />
A. For treatment of Lennox-Gastaut syndrome<br />
COVERAGE POLICY<br />
Banzel® is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with Lennox-Gastaut Syndrome<br />
B. Patient must be 4 years old or greater.<br />
NON COVERAGE<br />
Banzel® is NOT covered for members with the following criteria:<br />
A. Diagnosis is NOT Lennox-Gastaut Syndrome<br />
B. Patient is less than 4 years old<br />
C. Patient is diagnosed with Familial Short QT Syndrome<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
20
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
BETASERON<br />
FDA-APPROVED INDICATIONS<br />
Betaseron® is indicated:<br />
A. For the treatment of relapsing forms of multiple sclerosis to reduce the frequency<br />
of clinical exacerbations. Patients with multiple sclerosis in whom efficacy has<br />
been demonstrated include patients who have experienced a first clinical episode<br />
and have MRI features consistent with multiple sclerosis.<br />
COVERAGE POLICY<br />
Betaseron® is covered for members who meet the following criteria:<br />
A. The prescribing provider is a neurologist or has obtained a consult from the listed<br />
specialty.<br />
B. AND the diagnosis is documented as Relapsing-Remitting Multiple Sclerosis.<br />
(Betaseron® does not have the indication for primary progressive, secondary<br />
progressive or progressive relapsing multiple sclerosis).<br />
C. AND the patient has a history of at least two focal neurological deficits (e.g., loss<br />
of vision, double vision, localized numbness, localized weakness, walking gait<br />
abnormalities, slurred speech, tingling) in which the second deficit followed after<br />
the resolution of the first deficit. AND an MRI has been performed and is<br />
suggestive of multiple sclerosis (evidence of lesion).<br />
D. AND the patient will NOT be receiving Betaseron® therapy in combination with<br />
interferon-beta therapy (e.g., Rebif®, or Avonex®), Copaxone® or mitoxantrone.<br />
(Please verify that the patient is not on duplicate therapy by reviewing the<br />
patient’s drug history or chart).<br />
E. AND if the patient has received previous Betaseron® therapy, the provider can<br />
document a decrease in the frequency of clinical relapses OR slowing in the<br />
progression of the disease OR the patient has remained stable OR lesions on MRI<br />
have diminished after initiation of therapy.<br />
NON COVERAGE<br />
Betaseron® is NOT covered for members with the following criteria:<br />
A. A.The prescribing provider is NOT a neurologist or the prescribing provider has<br />
NOT obtained a consult from the listed specialty.<br />
B. B.The diagnosis is NOT documented as Relapsing-Remitting Multiple Sclerosis.<br />
C. The diagnosis is documented as primary progressive, secondary progressive or<br />
progressive relapsing multiple sclerosis.<br />
D. The patient has NO history of at least two focal neurological deficits.<br />
E. The patient has a history of at least two focal neurological deficits but the initial<br />
deficit did not resolve before the start of the second deficit.<br />
F. An MRI has NOT been performed.<br />
G. An MRI has been performed but is NOT suggestive of multiple sclerosis (no<br />
evidence of lesion).<br />
21
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
BETASERON<br />
(Continued)<br />
H. The patient will be receiving Betaseron® therapy in combination with interferonbeta<br />
therapy (e.g., Rebif® or Avonex®), Copaxone® or mitoxantrone.<br />
I. If the patient has received previous Betaseron® therapy and he/she cannot show a<br />
decrease in the frequency of clinical relapses or slowing in the progression of the<br />
disease or a decrease in the lesions on MRI or stability of the disease.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Neurologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
22
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
BUPHENYL<br />
FDA-APPROVED INDICATIONS<br />
Buphenyl® is indicated:<br />
A. Argininosuccinic acid synthease deficiency<br />
B. Carbamoyl Phosphate synthetase deficiency<br />
C. Ornithine Transcarbamoylase deficiency<br />
COVERAGE POLICY<br />
Buphenyl® is covered for members who meet the following criteria:<br />
A. Buphenyl® is used to treat urea cycle disorders diagnosed by FDA approved<br />
indications as stated above<br />
NON COVERAGE<br />
Buphenyl® is NOT covered for members with the following criteria:<br />
A. To treat hyperammonemia<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
23
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
BYETTA<br />
FDA-APPROVED INDICATIONS<br />
Byetta® is indicated:<br />
A. For adjunctive therapy to improve glycemic control in patients with type-2<br />
diabetes mellitus who are taking metformin, a sulfonylurea, a thiazolidinedione, a<br />
combination of metformin and a sulfonylurea, or a combination of metformin and<br />
a thiazolidinedione, but have not achieved adequate glycemic control.<br />
COVERAGE POLICY<br />
Byetta® is covered for members who meet the following criteria:<br />
A. The patient is diagnosed as having type-2 diabetes.<br />
B. AND the patient has an HbA1c level greater than 7.<br />
C. AND the patient’s current drug therapy includes metformin (eg. Metformin,<br />
Avandiamet®, or ActoPlus Met®) and therapy has been escalated to the highest<br />
tolerated dose, (Please verify that the patient has received metformin therapy by<br />
reviewing the patient’s drug history). OR if the patient is unable to take<br />
metformin due to clinical contraindications they can substitute the metformin<br />
requirement with a maximum tolerated dose of a sulfonylurea (chorpropramide,<br />
tolazamide, glipizide, glimepiride, or glyburide).<br />
D. AND the patient’s current drug therapy includes a thiazolidnedione (eg.<br />
Avandia®, Avandiamet®, Actos® or ActoPlus Met®) and therapy has been<br />
escalated to the highest tolerated dose. (Please verify that the patient has received<br />
thiazolidnedione therapy by reviewing the patient’s drug history).<br />
E. AND the patient has a creatinine clearance of greater than 30 ml/minute or normal<br />
kidney function.<br />
F. AND the patient does NOT have severe GI disease.<br />
G. AND the patient does NOT have gastroparesis.<br />
H. AND evidence of diagnosis and HbA1c is documented in the patient’s chart notes<br />
provided by the prescribing provider.<br />
I. AND if the patient has received previous Byetta® therapy, the physician must<br />
show a documented reduction in the patient’s HbA1c since initiating Byetta®<br />
therapy.<br />
24
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
BYETTA<br />
(Continued)<br />
NON COVERAGE<br />
Byetta® is NOT covered for members who meet the following criteria:<br />
A. The patient has NOT been diagnosed as having type-2 diabetes.<br />
B. The patient has an HbA1c level less than 7.<br />
C. The patient’s current drug therapy does NOT include metformin (eg. Metformin,<br />
Avandiamet®, or ActoPlus Met®) and therapy has NOT been escalated to the<br />
highest tolerated dose, (Please verify that the patient has received metformin<br />
therapy by reviewing the patient’s drug history). OR if the patient is unable to<br />
take metformin due to clinical contraindications they have NOT substituted the<br />
metformin requirement with a maximum tolerated dose of a sulfonylurea<br />
(chorpropramide, tolazamide, glipizide, glimepiride, or glyburide).<br />
D. The patient’s current drug therapy does NOT include a thiazolidnedione (eg.<br />
Avandia®, Avandiamet®, Actos® or ActoPlus Met®) and therapy has NOT been<br />
escalated to the highest tolerated dose. (Please verify that the patient has<br />
received thiazolidnedione therapy by reviewing the patient’s drug history).<br />
E. The patient has a creatinine clearance of less than 30 ml/minute.<br />
F. The patient has severe GI disease.<br />
G. The patient has gastroparesis.<br />
H. No evidence of diagnosis or HbA1c is documented in the patient’s chart notes<br />
provided by the prescribing provider.<br />
I. If the patient has received previous Byetta® therapy, and the physician has NOT<br />
shown a documented reduction in the patient’s HbA1c since initiating Byetta®<br />
therapy.<br />
J. Diagnosis is documented as weight loss.<br />
K. Diagnosis is documented as type-1 diabetes.<br />
L. Diagnosis is documented as ketoacidosis.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
25
FDA-APPROVED INDICATIONS<br />
Campath® is indicated:<br />
A. Chronic Lymphocytic Leukemia<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CAMPATH<br />
COVERAGE POLICY<br />
Campath® is covered for members who meet the following criteria:<br />
A. Campath® is approved for the diagnosis of Chronic Lymphocytic Leukemia<br />
B. AND if the medication meets B vs. D determination that the medication should be<br />
covered by Medicare Part D<br />
NON COVERAGE<br />
Campath® is NOT covered for members with the following criteria:<br />
A. To treat non-FDA indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
26
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CAMPRAL DELAYED-RELEASE TABLETS<br />
FDA-APPROVED INDICATIONS<br />
Campral® delayed-release tablets are indicated for maintenance of abstinence from<br />
alcohol in patients with alcohol dependence that are abstinent at treatment initiation.<br />
COVERAGE POLICY<br />
Campral® delayed-release tablets are covered for members who meet the following<br />
criteria:<br />
A. Clinical diagnosis for alcohol dependence<br />
B. AND clinical evidence indicated that the consumer will be abstinent at least 5<br />
days prior treatment initiation.<br />
C. AND a trial of naltrexone (oral/injectable) has been attempted, at clinically<br />
significant dosage and duration. Or therapy is documented to be clinically<br />
inappropriate (hepatic insufficiency, chronic pain medication use).<br />
D. AND medication administration should be part of a comprehensive psychosocial<br />
treatment program.<br />
NON COVERAGE<br />
Campral® delayed-release tablets are NOT covered for members with the following<br />
criteria:<br />
A. For patients who cannot reach abstinence prior to therapy initiation<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
6 months<br />
27
FDA-APPROVED INDICATIONS<br />
Camptosar® is indicated:<br />
A. Colorectal Cancer<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CAMPTOSAR<br />
COVERAGE POLICY<br />
Camptosar® is covered for members who meet the following criteria:<br />
A. Camptosar® is approved for the diagnosis of Colorectal Cancer<br />
B. AND if the medication meets B vs. D determination that the medication should be<br />
covered by Medicare Part D<br />
NON COVERAGE<br />
Camptosar® is NOT covered for members with the following criteria:<br />
A. To treat non-FDA indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
28
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CARIMUNE<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
a. Treatment of hypergammaglobulinemia<br />
B. AND the patient is diagnosed with primary immunodeficiency<br />
C. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
D. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency, OR<br />
Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
6 months<br />
29
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CELLCEPT<br />
FDA-APPROVED INDICATIONS<br />
Cellcept® is indicated:<br />
A. Heart Transplant Rejection Prophylaxis<br />
B. Kidney Transplant Rejection Prophylaxis<br />
C. Liver Transplant Rejection Prophylaxis<br />
COVERAGE POLICY<br />
Cellcept® is covered for members who meet the following criteria:<br />
A. If the patient is female and of childbearing years, she is NOT pregnant, has NO<br />
plans for pregnancy and has been educated on the potential dangers of Cellcept®<br />
therapy.<br />
B. AND diagnosis is documented as the prophylaxis of organ rejection in a patient<br />
receiving or received an organ transplant.<br />
C. AND the transplant was NOT covered by Medicare Part A/B. (Please verify the<br />
payer of the transplant. If Medicare paid for the transplant, Cellcept® is covered<br />
by Medicare Part A/B).<br />
D. AND approval can be allowed for up to one year.<br />
NON COVERAGE<br />
Cellcept® is NOT covered for members with the following criteria:<br />
A. Hypersensitivity to Mycophenolate<br />
B. The patient is female and of childbearing years and is pregnant or has plans for<br />
pregnancy.<br />
C. The diagnosis is NOT documented as prophylaxis of organ rejection after<br />
receiving an organ transplant or a compendia listed indication.<br />
D. The transplant was paid for by Medicare Part A/B<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
30
FDA-APPROVED INDICATIONS<br />
Ceredase® is indicated:<br />
A. Gaucher’s disease<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CEREDASE<br />
COVERAGE POLICY<br />
Ceredase® is covered for members who meet the following criteria:<br />
A. Patient has documented diagnosis of Gaucher’s disease<br />
B. AND can not tolerate Imiglucerase therapy<br />
C. AND B vs. D criteria is determined that this medication should be paid for by<br />
Medicare Part D<br />
NON COVERAGE<br />
Ceredase® is NOT covered for members with the following criteria:<br />
A. Patients who can tolerate Imiglucerase therapy<br />
B. When therapy is covered by Medicare Part B<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
31
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CEREZYME<br />
FDA-APPROVED INDICATIONS<br />
Cerezyme® is indicated:<br />
A. For long-term enzyme replacement therapy for pediatric and adult patients with a<br />
confirmed diagnosis of type-1 Gaucher disease that results in one or more of the<br />
following conditions: Anemia, thrombocytopenia, bone disease, hepatomegaly or<br />
splenomegaly.<br />
COVERAGE POLICY<br />
Cerezyme® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as mild-to-moderate type-1 Gaucher disease.<br />
B. AND diagnosis has been confirmed by bone marrow histology, DNA testing or<br />
measurement of b-glucocerebrosidase enzyme activity less than 30%.<br />
C. AND the patient has at least one of the following conditions: Anemia,<br />
thrombocytopenia, bone disease, hepatomegaly or splenomegaly.<br />
D. AND if the patient has previously received 24 months of Cerezyme® therapy,<br />
they must show a decrease in liver and spleen volume and/or increases in platelet<br />
count and/or increases in hemoglobin concentration since starting therapy.<br />
NON COVERAGE<br />
Cerezyme® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as mild-to moderate type-1 Gaucher disease.<br />
B. Diagnosis has NOT been confirmed by bone marrow histology, DNA testing or<br />
measurement of enzyme activity.<br />
C. The patient does not have at least one of the following conditions: Anemia,<br />
thrombocytopenia, bone disease, hepatomegaly or splenomegaly.<br />
D. If the patient has previously received 24 months of Cerezyme® therapy and they<br />
have NOT shown a decrease in liver and spleen volume and/or increases in<br />
platelet count and/or increases in hemoglobin concentration since starting therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
32
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CIMZIA<br />
FDA-APPROVED INDICATIONS<br />
Cimzia® is indicated:<br />
A. For treatment of moderately to severely active Crohn’s disease to reduce signs<br />
and symptoms and to maintain clinical response in patient who have an<br />
inadequate response to conventional therapy.<br />
COVERAGE POLICY<br />
Cimzia® is covered for members who meet the following criteria:<br />
A. Verification of B vs D criteria per CMS guidelines<br />
B. Patient has NO history of auto immune disease, recurring infections, heart failure,<br />
immuno suppression or malignancies.<br />
C. AND the diagnosis is documented as Crohn’s Disease<br />
D. AND the patient has tried, failed and/or had an inadequate response to a 60-day<br />
trial of at least two Crohn’s disease conventional therapies that may include the<br />
following: Sulfazalazine, Azulfidine®, balsalazide, Colazal®, mesalamine,<br />
Asacol®, Canasa®, Lialda®, Pentasa®, Rowasa®, azathioprine, Imuran®,<br />
cyclosporine, Neoral®, Sandimmune®, Gengraf®, methotrexate, mercaptopurine,<br />
or Purinethol®.<br />
E. OR if the patient has received previous Cimzia® therapy, the patient must see an<br />
improvement in clinical symptoms that can include reduced abdominal pain,<br />
diarrhea, cramps, and/or fistulas.<br />
F. AND the patient will NOT receive combination therapy with other biologic<br />
and/or retinoid therapy. (Eg. Enbrel®, Humira®, Remicade®, Kineret®,<br />
Orencia®, Soriatane® Tysabri®, Raptiva® and Rituxan®. (Please verify that the<br />
patient is not on duplicate therapy by reviewing the patient’s drug history or<br />
chart).<br />
G. AND evidence of diagnosis, previous failed therapy, or clinical improvement is<br />
documented in patient’s chart notes provided by prescribing provider.<br />
NON COVERAGE<br />
Cimzia® is NOT covered for members with the following criteria:<br />
A. Medication is paid for by Part B<br />
B. Patient has a history of auto immune disease, recurring infections, heart failure,<br />
immuno suppression or malignancies.<br />
C. The prescribing provider is NOT a gastroenterologist or obtained a consult from<br />
the listed specialty.<br />
D. The diagnosis is NOT documented as severe Crohn’s disease<br />
E. The diagnosis is listed as ulcerative colitis.<br />
F. The patient has NOT failed at least two 60-day conventional drug regimens.<br />
G. If the patient is receiving combination therapy that includes any one of the<br />
following medications: Enbrel®, Humira®, Remicade®, Tysabri®, Kineret®,<br />
Orencia®, Soriatane® or Rituxan®.<br />
33
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CIMZIA<br />
(Continued)<br />
H. If the patient has received previous Cimzia® therapy and the provider has NOT<br />
shown an improvement in clinical symptoms.<br />
I. Evidence of diagnosis, previous failed therapy and symptoms are NOT<br />
documented in patient’s chart notes provided by the prescribing provider.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes documenting previous trial failure of at least TWO of the following:<br />
Sulfazalazine, Azulfidine®, balsalazide, Colazal®, mesalamine, Asacol®, Canasa®,<br />
Lialda®, Pentasa®, Rowasa®, azathioprine, Imuran®, cyclosporine, Neoral®,<br />
Sandimmune®, Gengraf®, methotrexate, mercaptopurine, or Purinethol®.<br />
AGE RESTRICTIONS<br />
Patient must be 18 years of age or greater<br />
PRESCRIBER RESTRICTIONS<br />
Gastroenterologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
34
FDA-APPROVED INDICATIONS<br />
Cladribine is indicated:<br />
A. Hairy Cell Leukemia<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CLADRIBINE<br />
COVERAGE POLICY<br />
Cladribine is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with Hairy Cell Leukemia<br />
B. AND is being diagnosed by an Oncologist<br />
C. AND the medication meets B vs. D determination criteria that authorized<br />
coverage to Medicare Part D<br />
NON COVERAGE<br />
Cladribine is NOT covered for members with the following criteria:<br />
A. Non FDA approved indications<br />
REQUIREDMEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
7 days<br />
35
FDA-APPROVED INDICATIONS<br />
Amnesteem® is indicated:<br />
A. Acne Vulgaris<br />
B. Cystic Acne<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CLARAVIS<br />
COVERAGE POLICY<br />
Amnesteem® is covered for members who meet the following criteria:<br />
A. For the treatment of Acne Vulgaris and Cystic Acne<br />
B. AND Prescribed by a dermatologist<br />
C. AND documentation of failure oral antibiotics for 3 months<br />
D. AND documentation of failure of topical acne preparations for 3 months (benzoyl<br />
peroxide, topical tretinoin cream, topical antibiotics)<br />
E. AND in female patients a negative pregnancy test, mother is not breast feeding, or<br />
intentions of pregnancy<br />
F. AND No history of depression<br />
NON COVERAGE<br />
Amnestem® is NOT covered for members with the following criteria:<br />
A. Severe hepatic impairment<br />
B. Women who are or may become pregnant, or breast feeding<br />
C. History of depression<br />
D. Hypersensitivity to retenoids<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Dermatologist<br />
AUTHORIZATION PERIOD<br />
20 months<br />
36
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
COLONY STIMULATING FACTOR<br />
FDA-APPROVED INDICATIONS<br />
Colony Stimulating Factor is indicated:<br />
A. Chemotherapy Induced Neutropenia<br />
B. Febrile Neutropenia<br />
C. Neutropenia<br />
D. Peripheral Blood Stem Cell Mobilization<br />
COVERAGE POLICY<br />
Colony Stimulating Factor is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with approved indication as stated above<br />
B. AND lab values indicate necessity for therapy (Chart Notes required to<br />
substantiate need)<br />
C. AND B vs. D criteria indicates that coverage should be through Medicare Part D<br />
NON COVERAGE<br />
Colony Stimulating Factor is NOT covered for members with the following criteria:<br />
A. Inadequate chart notes to substantiate need for Colony Stimulating Factor<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
3 months<br />
37
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
COPAXONE<br />
FDA-APPROVED INDICATIONS<br />
Copaxone® is indicated:<br />
A. For reduction of the frequency of relapses in patients with Relapsing-Remitting<br />
Multiple Sclerosis.<br />
B. All other FDA approved indications not otherwise excluded from Part D.<br />
COVERAGE POLICY<br />
Copaxone® is covered for members who meet the following criteria:<br />
A. The prescribing provider is a neurologist or has obtained a consult from the listed<br />
specialty.<br />
B. AND the diagnosis is documented as Relapsing-Remitting Multiple Sclerosis.<br />
(Copaxone® does not have the indication for primary progressive, secondary<br />
progressive or progressive relapsing multiple sclerosis).<br />
C. AND the patient has a history of at least two focal neurological deficits (e.g., loss<br />
of vision, double vision, localized numbness, localized weakness, walking gait<br />
abnormalities, slurred speech, tingling) in which the second deficit followed after<br />
the resolution of the first deficit.<br />
D. AND the patient will NOT be receiving Copaxone® therapy in combination with<br />
interferon-beta therapy (e.g., Rebif®, Avonex®, or Betaseron®) or mitoxantrone.<br />
(Please verify that the patient is not on duplicate therapy by reviewing the<br />
patient’s drug history or chart).<br />
E. AND if the patient has received previous Copaxone® therapy, the provider can<br />
document a decrease in the frequency of clinical relapses OR slowing in the<br />
progression of the disease OR the patient has remained stable OR lesions on MRI<br />
have diminished after initiating therapy.<br />
NON COVERAGE<br />
Copaxone® is NOT covered for members with the following criteria:<br />
A. The prescribing provider is NOT a neurologist or the prescribing provider has<br />
NOT obtained a consult from the listed specialty.<br />
B. The diagnosis is NOT documented as Relapsing-Remitting Multiple Sclerosis.<br />
C. The diagnosis is documented as primary progressive, secondary progressive or<br />
progressive relapsing multiple sclerosis.<br />
D. The patient has NO history of at least two focal neurological deficits.<br />
E. The patient has a history of at least two focal neurological deficits but the initial<br />
deficit did not resolve before the start of the second deficit.<br />
F. An MRI has NOT been performed.<br />
G. An MRI has been performed but is NOT suggestive of multiple sclerosis (no<br />
evidence of lesion).<br />
H. The patient will be receiving Copaxone® therapy in combination with interferonbeta<br />
therapy (e.g., Rebif®, Avonex®, or Betaseron®) or mitoxantrone.<br />
38
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
COPAXONE<br />
(Continued)<br />
I. If the patient has received previous Copaxone® therapy and he/she cannot show a<br />
decrease in the frequency of clinical relapses or slowing in the progression of the<br />
disease or a decrease in the lesions on MRI or stability of the disease.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart Notes<br />
PRESCRIBER RESTRICTIONS<br />
Neurologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
39
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CYCLOPHOSPHAMIDE<br />
FDA-APPROVED INDICATIONS<br />
Cyclophosphamide is indicated:<br />
A. Acute Lymphocytic Leukemia<br />
B. Acute Myelogenous Leukemia<br />
C. Breast Cancer<br />
D. Burkitt’s Lymphoma<br />
E. Chronic Lymphocytic Leukemia<br />
F. Chronic Myelogenous Leukemia<br />
G. Cutaneous T-Cell Lymphoma<br />
H. Hodgkin’s Disease<br />
I. Multiple Myeloma<br />
J. Mycosis Fungoides<br />
K. Nephrotic Syndrome<br />
L. Neuroblastoma<br />
M. Non-Hodkin’s Lymphoma<br />
N. Ovarian Cancer<br />
O. Retinoblastoma<br />
P. Malignant histiocytosis<br />
Q. All other FDA approved<br />
indications not otherwise<br />
excluded from Part D<br />
COVERAGE POLICY<br />
Cyclophosphamide is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with FDA indicated diagnosis as described above<br />
B. AND the medication meets B vs. D determination criteria that authorized<br />
coverage to Medicare Part D<br />
NON COVERAGE<br />
Cyclophosphamide is NOT covered for members with the following criteria:<br />
A. Non FDA approved indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Initial authorization: 1 month<br />
40
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CYCLOSPORINE<br />
FDA-APPROVED INDICATIONS<br />
Cyclosporine is indicated:<br />
A. Heart Transplant Prophylaxis<br />
B. Kidney Transplant Prophylaxis<br />
C. Liver Transplant Prophylaxis<br />
D. Psoriasis<br />
E. Rheumatoid Arthiritis<br />
F. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Cyclosporine is covered for members who meet the following criteria:<br />
A. Approved for all prophylaxis diagnoses as described above (Heart, Kidney, Liver)<br />
B. AND prescribed by Transplant Surgeon<br />
C. AND B vs. D determination has been established that medication should be<br />
covered by Medicare Part D<br />
D. If diagnosis of Psoriasis must be diagnosed by a Dermatologist<br />
E. AND documented failure to at least two different topical steroids<br />
NON COVERAGE<br />
Cyclosporine is NOT covered for members with the following criteria:<br />
A. Non FDA approved indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
41
FDA-APPROVED INDICATIONS<br />
Cyklokapron® is indicated:<br />
A. Bleeding Prophylaxis<br />
B. Dysfunctional Uterine Bleeding<br />
C. Hemophilia A/B<br />
D. Hemorrhage<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CYKLOKAPRON<br />
COVERAGE POLICY<br />
Cyklokapron® is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with FDA approved indications as stated above<br />
B. AND the patient meets B vs. D determination that requires Medicare Part D<br />
payment<br />
NON COVERAGE<br />
Cyklokapron® is NOT covered for members with the following criteria:<br />
B. Non-FDA approved indications<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
1 month<br />
42
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
CYTARABINE<br />
FDA-APPROVED INDICATIONS<br />
Cytarabine is indicated:<br />
A. Acute Lymphocytic Leukemia<br />
B. Acute Myelogenous Leukemia<br />
C. Carcinomatous meningitis<br />
D. Chronic Myelogernous Leukemia<br />
E. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Cytarabine is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with FDA approved indications as stated above<br />
B. AND medication is being prescribed by an Oncologist<br />
C. AND patient does not have an active infection<br />
D. AND the patient meets B vs. D determination that requires Medicare Part D<br />
payment<br />
NON COVERAGE<br />
Cytarabine® is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
43
FDA-APPROVED INDICATIONS<br />
Dacogen® is indicated for:<br />
A. Myelodysplastic Syndrome<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
DACOGEN<br />
COVERAGE POLICY<br />
Dacogen® is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with Myelodysplastic Syndrome<br />
B. AND medication is prescribed by an Oncologist<br />
C. AND B vs. D criteria is met to ensure coverage should be through Medicare Part<br />
D.<br />
NON COVERAGE<br />
Dacogen® is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
B. Patient is pregnant<br />
C. Children<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
24 weeks<br />
44
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
DUREZOL<br />
FDA-APPROVED INDICATIONS<br />
Durezol® is indicated:<br />
A. For treatment of postoperative ocular pain<br />
B. For treatment of postoperative ocular inflammation<br />
COVERAGE POLICY<br />
Durezol® is covered for members who meet the following criteria:<br />
A. Prescribed by Ophthalmologist<br />
B. Must be used for postoperative ocular pain OR postoperative ocular inflammation<br />
NON COVERAGE<br />
Durezol® is NOT covered for members with the following criteria:<br />
A. Prescribed by non-ophthalmologist<br />
B. Used for non-postoperative treatment<br />
PRESCRIBER RESTRICTIONS<br />
Opthalmologist<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes per Covered Uses<br />
AUTHORIZATION PERIOD<br />
4 weeks<br />
45
FDA-APPROVED INDICATIONS<br />
Elaprase® is indicated:<br />
A. Hunter Syndrome<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ELAPRASE<br />
COVERAGE POLICY<br />
Elaprase is covered for members who meet the following criteria:<br />
A. Approve only for patients diagnosed with mucopolysaccharidosis II (Hunter<br />
Syndrome)<br />
NON COVERAGE<br />
Elaprase® is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
46
FDA-APPROVED INDICATIONS<br />
Elidel® is indicated:<br />
A. Atopic dermatitis (eczema)<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ELIDEL<br />
COVERAGE POLICY<br />
Elidel® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as atopic dermatitis or eczema<br />
B. The prescribing physician is a dermatologist<br />
C. The patient is age 2 or older<br />
D. Patients greater than 12 years of age have completed a documented trial and<br />
failure of first-line agents including high potency topical steroids or have<br />
documented intolerance or unresponsiveness to high potency topical steroids.<br />
E. The patient is not immunocompromised<br />
NON COVERAGE<br />
Elidel® is NOT covered for members who meet the following criteria:<br />
A. The documented diagnosis is NOT atopic dermatitis or eczema<br />
B. The prescribing physician is NOT a dermatologist<br />
C. The patient is less than 2 years old<br />
D. Patients greater than 12 years of age who have NOT completed a documented<br />
trial and failure of first-line agents including high potency steroids<br />
E. The patient is immunocompromised<br />
F. The patient has used Elidel® for 6 weeks or more without improvement<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Dermatologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
47
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ELIGARD<br />
FDA APPROVED FOR<br />
Eligard® is indicated:<br />
A. For the palliative treatment of advanced prostate cancer, particularly when<br />
orchiectomy or estrogen therapy are not indicated or are unacceptable<br />
B. For the management of endometriosis including pain relief and reduction of<br />
endometriotic lesions<br />
C. For the treatment of central precocious puberty (idiopathic or neurogenic) in<br />
children less than 8 or 9 years old<br />
D. For the preoperative treatment of anemia due to uterine leiomyomata (fibroids) in<br />
combination with iron supplementation when iron therapy alone fails to correct<br />
the anemia<br />
COVERAGE POLICY<br />
Eligard® is covered for members who meet the following criteria:<br />
A. The documented diagnosis is one of the FDA approved indications listed above.<br />
B. If the diagnosis is advanced prostate cancer, orchiectomy or estrogen therapy are<br />
documented as unacceptable.<br />
C. If the diagnosis is endometriosis the patient has completed documented trial and<br />
failures of oral contraceptives, medroxyprogesterone, and Danazol<br />
D. If the diagnosis is precocious puberty, patient must be less than 9 years old<br />
E. AND verification of all B vs. D criteria indicate coverage by Part D<br />
NON COVERAGE<br />
Eligard® is NOT covered for members with the following criteria:<br />
A. If there is not a documented diagnosis as listed under the FDA-approved<br />
indications above.<br />
B. If the diagnosis is advanced prostate cancer, orchiectomy or estrogen therapy are<br />
not indicated for are unacceptable.<br />
C. If the diagnosis is endometriosis, the patient has completed a documented trial<br />
and failure of oral contraceptives, medroxyprogesterone, and Danazol.<br />
D. If the diagnosis is precocious puberty, the patient must be less than 9 years old at<br />
beginning of treatment. Treatment should be discontinued before age 11 for<br />
females and age 12 for males.<br />
E. If the patient is female and she is pregnant, has plans for pregnancy or has NOT<br />
been educated on the potential dangers of Lupron® therapy in pregnancy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
48
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ELITEK<br />
FDA-APPROVED INDICATIONS<br />
Elitek® is indicated:<br />
A. For the prevention of hyperuricemia in patients with leukemia, lymphoma, or<br />
solid tumor malignancies who are receiving anti-cancer therapy expected to result<br />
in tumor lysis<br />
COVERAGE POLICY<br />
Elitek® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified oncologist.<br />
B. AND the use is documented as prevention of hyperuricemia<br />
C. AND the patient has leukemia, lymphoma or a solid tumor malignancy<br />
D. AND the patient is receiving chemotherapy expected to result in tumor lysis<br />
E. AND verification of all B vs. D criteria indicate coverage by Part D<br />
NON COVERAGE<br />
Elitek® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a board certified oncologist<br />
B. The use is NOT documented as prevention of hyperuricemia<br />
C. The patient does NOT have leukemia, lymphoma or a solid tumor malignancy<br />
D. The patient is NOT receiving chemotherapy expected to result in tumor lysis<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
49
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ELOXATIN<br />
FDA-APPROVED INDICATIONS<br />
Eloxatin® is indicated:<br />
A. For the treatment of stage III colon cancer patients who have undergone complete<br />
resection of the primary tumor<br />
B. For the treatment of advanced colorectal cancer<br />
COVERAGE POLICY<br />
Eloxatin® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified oncologist.<br />
B. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy and has been educated on the potential dangers of<br />
Eloxatin® therapy in pregnancy.<br />
C. AND the diagnosis is documented as treatment for stage III colon cancer and the<br />
patient has undergone complete resection of the primary tumor, or advanced<br />
colorectal cancer.<br />
D. AND Eloxatin® is to be administered with infusional 5-fluorouracil and<br />
leucovorin.<br />
NON COVERAGE<br />
Eloxatin® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a board certified oncologist or nephrologist.<br />
B. If the patient is female and she is pregnant, has plans for pregnancy or has NOT<br />
been educated on the potential dangers of Eloxatin ® therapy in pregnancy.<br />
C. The diagnosis is NOT documented as treatment for stage III colon cancer and the<br />
patient has undergone complete resection of the primary tumor, or advanced<br />
colorectal cancer.<br />
D. Eloxatin® is NOT administered with infusional 5-fluorouracil and leucovorin.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
50
FDA-APPROVED INDICATIONS<br />
Emend® is indicated:<br />
A. Nausea/Vomitting<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
EMEND<br />
COVERAGE POLICY<br />
Emend® is covered for members who meet the following criteria:<br />
A. Documented trial and failure to Ondansetron<br />
B. Part B will be billed if the medication is being used for cancer treatment and as a<br />
“full replacement” of intravenous administration within 48 hours of cancer<br />
treatment and<br />
C. The physical prescription written by the prescriber states: “As a full therapeutic<br />
replacement for an intravenous anti-emetic drug as part of a cancer<br />
chemotherapeutic regiment.”<br />
D. If the requirements in Step A and B are verified then 48 hours of therapy will be<br />
billed to Part B.<br />
E. If the requirements in Step 1 and 2 are not met, 48 hours past the administration<br />
of chemotherapy, or the initial 48 hours supply has been dispensed then the<br />
medication will be billed to Part D.<br />
Emend must also meet the above criteria and the following to be covered under Part B:<br />
A. Administered in combination with a 5HT 3 Antagonist (Zofran, Kytril, Anzemet)<br />
and dexamethasone.<br />
B. Beneficiary has received one or more of the following chemotherapeutic agents:<br />
a. Carmustine (BiCNU)<br />
b. Cisplatin (Platinol)<br />
c. Cyclophosphamide<br />
(Cytoxan)<br />
d. Dacarbazine (DTIC-<br />
Dome)<br />
NON COVERAGE<br />
Emend® is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
B. Nausea from non-oncologic related conditions or medications<br />
C. Has not had trial and failure to Ondansetron<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
e. Mechlorethamine<br />
(Mustargen)<br />
f. Streptozocin (Zanosar)<br />
g. Doxorubicin<br />
(Adriamycin)<br />
h. Epirubicin (Ellence)<br />
i. Lomustine (CeeNu)<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
51
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
EMSAM<br />
FDA-APPROVED INDICATIONS<br />
EMSAM® is indicated for:<br />
A. The treatment of major depressive disorder.<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
EMSAM® is covered for members who meet the following criteria:<br />
A. Clinical diagnosis of major depressive disorder not responsive other<br />
antidepressants<br />
B. At least 2 documented trials (clinically sufficient dose and duration) of the<br />
following: Selective Serotonin Reuptake Inhibitors (SSRI),<br />
Serotonin/Norepinephrine Reuptake Inhibitors (SNRI), bupropion, mirtazapine, or<br />
tricyclic/tetracyclic antidepressants<br />
C. Clinical diagnosis of major depressive disorder for those patients who cannot take<br />
any oral preparations (including commercially available liquid antidepressants).<br />
D. For requests over 6mg/24 hours, patient must agree to adhere to a tyramine<br />
restrictive diet.<br />
NON COVERAGE<br />
EMSAM® is NOT covered for members with the following criteria:<br />
A. Recent pharmacy claims of the following, unless provider can document an<br />
appropriate medication discontinuation date.<br />
a. At least 4-5 half-lives (approximately 1 week) for the following<br />
medication and their active metabolites: SSRIs, SNRIs, TCAs, MAOIs,<br />
meperidine, other analgesics (tramadol, methadone, and propoxyphene),<br />
dextromethorphan, St.John’s wort, mirtazapine, bupropion, or buspirone.<br />
b. Claims within 5 weeks for fluoxetine.<br />
B. Concurrent selegiline treatment.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Psychiatrist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
52
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ENBREL<br />
FDA-APPROVED INDICATIONS<br />
Enbrel® is indicated:<br />
A. For reducing signs and symptoms in patients with active ankylosing spondylitis.<br />
B. For the treatment of adult patients (18 years or older) with chronic moderate to<br />
severe plaque psoriasis who are candidates for systemic therapy or phototherapy.<br />
C. For reducing signs and symptoms of moderately to severely active polyarticularcourse<br />
juvenile rheumatoid arthritis (JRA) in patients who have had an inadequate<br />
response to 1 (one) or more disease-modifying antirheumatic drugs (DMARD).<br />
D. For reducing signs and symptoms, inducing major clinical response, inhibiting the<br />
progression of structural damage, and improving physical function in patients<br />
with moderately to severely active rheumatoid arthritis. Enbrel® can be initiated<br />
in combination with methotrexate (MTX) or used alone.<br />
E. For reducing signs and symptoms, inhibiting the progression of structural damage<br />
of active arthritis, and improving physical function in patients with psoriatic<br />
arthritis. Enbrel® can be used in combination with methotrexate in patients who<br />
do not respond adequately to methotrexate alone.<br />
COVERAGE POLICY<br />
Enbrel® is covered for members who meet the following criteria:<br />
A. Patient has NO history of auto immune disease, recurring infections, heart failure,<br />
immuno suppression or malignancies.<br />
B. AND the prescribing provider is a rheumatologist, dermatologist, orthopedist or<br />
has obtained a consult from the listed specialties.<br />
C. AND diagnosis is documented as moderate to severe active rheumatoid arthritis.<br />
a. AND the patient has at least four (4) of the following symptoms:<br />
i. Morning stiffness.<br />
ii. Arthritis of three (3) or more joint areas.<br />
iii. Arthritis of hand joints.<br />
iv. Symmetric arthritis.<br />
v. Rheumatoid nodules.<br />
vi. Serum rheumatoid factor.<br />
vii. Radiographic changes.<br />
b. AND the patient has had at least an 8-week maximum tolerated dose trial<br />
and failure to at least two 2 of the following DMARDS listed:<br />
Methotrexate, cyclosporine, Neoral®, Samdimmune®, Gengraf®,<br />
azathioprine, Imuran®, penicillamine, Cuprimine®, Depen®,<br />
sulfasalazine, Azulfidine®, leflunomide, Arava®, gold sodium thiomalate,<br />
Aurolate®, aurothioglucose, Solganal®, auranofin, Ridaura®,<br />
hydroxychoroquine, Plaquenil®. (Verification can be made by reviewing<br />
the patient’s drug history or patient’s chart).<br />
53
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ENBREL<br />
(Continued)<br />
c. AND if the patient has received previous Enbrel® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or delay<br />
in progression of disease.<br />
D. OR the diagnosis is juvenile rheumatoid arthritis.<br />
a. AND the age of the patient is 17 years old or less.<br />
b. AND the patient has had at least a 6-week duration of persistent arthritis in<br />
one or more joints.<br />
c. AND the patient has had at least an 8-week maximum tolerated dose trial<br />
and failure to at least two(2) of the following DMARDS listed:<br />
Methotrexate, cyclosporine, Neoral®, Samdimmune®, Gengraf®,<br />
azathioprine, Imuran®, penicillamine, Cuprimine®, Depen®,<br />
sulfasalazine, Azulfidine®, leflunomide, Arava®, gold sodium thiomalate,<br />
Aurolate®, aurothioglucose, Solganal®, auranofin, Ridaura®,<br />
hydroxychoroquine, Plaquenil®. (Verification can be made by reviewing<br />
the patient’s drug history or patient’s chart).<br />
d. AND if the patient has received previous Enbrel® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or delay<br />
in progression of disease.<br />
E. OR the diagnosis is documented as psoriatic arthritis.<br />
a. AND the patient has at least one of the following symptoms:<br />
i. Three (3) or more swollen joints.<br />
ii. Three (3) or more tender joints.<br />
b. AND the patient has had at least an 8-week maximum tolerated dose trial<br />
and failure to at least two (2) of the following DMARDS listed:<br />
(methorexate, cyclosporine, Neoral®, Sandimmune®, Gengraf®,<br />
azathioprine, Imuran®, penicillamine, Cuprimine®, Depen®,<br />
sulfasalazine, Azulfidine®, leflunomide, Arava®, gold sodium thiomalate,<br />
Aurolate®, aurothioglucose, Solganal®, auranofin, Ridaura®,<br />
hydroxychoroquine, Plaquenil®) if methotrexate is contraindicated.<br />
(Verification can be made by reviewing the patient’s drug history or<br />
patient’s chart).<br />
c. AND if the patient has received previous Enbrel® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or delay<br />
in progression of disease.<br />
54
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ENBREL<br />
(Continued)<br />
F. OR the diagnosis is documented as active ankylosing spondylitis.<br />
a. AND the patient has tried and failed at least a 60-day trial of at least two<br />
non-steroidal anti-inflammatory (NSAID) drugs that can include any two<br />
of the following medications: Diclofenac, etodolac, fenoprofen,<br />
flurbiprofen, ibuprofen, indomethacin, celecoxib, Celebrex®, ketoprofen,<br />
meclofenamate, nabumetone, naproxen, oxaprozin, piroxicam, sulinidac,<br />
or tolmetin. (Please verify that the patient has received NSAID therapy by<br />
reviewing the patient’s drug history).<br />
b. AND if the patient has received previous Enbrel® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or delay<br />
in progression of disease.<br />
G. OR the diagnosis is documented as chronic moderate to severe plaque psoriasis.<br />
a. AND the patient has had the disease for 1 year or greater.<br />
b. AND the patient’s age is 18 years old or older.<br />
c. AND the involvement of plaque psoriasis is 10% or greater of the patient’s<br />
total body surface area (BSA) OR if the BSA is less than 10%, the plaque<br />
psoriasis must involve areas that will prevent the patient from performing<br />
crucial daily functions such as walking (eg. feet).<br />
d. AND the patient has tried and failed at least a 60-day trial of three (3)<br />
conventional therapies that may include any of the following:<br />
i. High potency topical steroid treatment.<br />
ii. Calcipotriene (Dovenex®)<br />
iii. Phototherapy.<br />
iv. Retinoids (Soriatane®)<br />
v. Methotrexate.<br />
vi. Cyclosporine.<br />
e. AND If this is the initial plaque psoriasis request for Enbrel®, 50 mg<br />
twice a week therapy is ONLY approved for 3 months. OR if the patient<br />
has received Enbrel® therapy for greater than three(3) months, the patient<br />
must see a significant reduction in plaque thickness, erythemia,<br />
desquamation and affected body surface area. AND therapy is only<br />
allowed 50 mg once a week. (Please verify patient’s chart notes to verify<br />
clinical improvement).<br />
f. AND the patient will NOT receive combination therapy with other<br />
biologic and retinoid therapy. (Eg. Humira®, Remicade®, Kineret®,<br />
Orencia®, Soriatane®, Raptiva® and Rituxan®. (Please verify that the<br />
patient is not on duplicate therapy by reviewing the patient’s drug history<br />
or chart).<br />
g. AND evidence of diagnosis, previous failed therapy or clinical<br />
improvement is documented in patient’s chart notes provided by<br />
prescribing provider.<br />
55
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ENBREL<br />
(Continued)<br />
NON COVERAGE<br />
Enbrel® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as severe active rheumatoid arthritis, juvenile<br />
rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis or chronic<br />
moderate to severe plaque psoriasis.<br />
B. The diagnosis is listed as Crohn’s Disease or ulcerative colitis.<br />
C. If the diagnosis is listed as severe active rheumatoid arthritis, the patient does<br />
NOT have four of the listed symptoms.<br />
D. If the diagnosis is listed as severe active rheumatoid arthritis, the patient has NOT<br />
failed two 8-week maximum tolerated DMARD trials.<br />
E. If the diagnosis is juvenile rheumatoid arthritis and the patient is over the age of<br />
17 years old.<br />
F. If the diagnosis is juvenile rheumatoid arthritis and the patient has NOT had at<br />
least a 6-week duration of persistent arthritis on one or more joints.<br />
G. If the diagnosis is juvenile rheumatoid arthritis and the patient has NOT failed a<br />
two 8-week maximum tolerated DMARD trials.<br />
H. If the diagnosis is psoriatic arthritis and the patient does NOT have three swollen<br />
joints or three tender joints.<br />
I. If the diagnosis is psoriatic arthritis and the patient has NOT failed two 8-week<br />
maximum tolerated DMARD trials.<br />
J. If the diagnosis is ankylosing spondylitis and the patient has NOT failed two 60-<br />
day NSAID drug regimens.<br />
K. If the diagnosis is chronic moderate to severe plaque psoriasis and the patient has<br />
NOT had the disease for 1 year or greater.<br />
L. If the diagnosis is chronic moderate to severe plaque psoriasis and the<br />
involvement is less than 10% of body surface area or does NOT involve an area<br />
that will affect a critical daily function.<br />
M. If the diagnosis is chronic moderate to severe plaque psoriasis and the patient has<br />
NOT failed a 60-day trial to two conventional therapies.<br />
N. If the diagnosis is chronic moderate to severe plaque psoriases and the patient has<br />
received Enbrel® therapy greater than 3 months and the provider is requesting 50<br />
mg twice a week.<br />
O. If the diagnosis is chronic moderate to severe plaque psoriases and the patient has<br />
received Enbrel® therapy greater than 3 months and the patient has NOT shown a<br />
significant reduction in plaque thickness, erythemia, desquamation and affected<br />
BSA.<br />
P. If the patient is receiving combination therapy that includes any one of the<br />
following medications: Humira®,<br />
Q. Remicade®, Kineret®, Orencia®, Soriatane®or Rituxan®.<br />
56
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ENBREL<br />
(Continued)<br />
R. If the patient has received previous Enbrel® therapy and the provide has NOT<br />
shown an improvement in clinical symptoms.<br />
S. Evidence of diagnosis, previous failed therapy and symptoms are NOT<br />
documented in patient’s chart notes provided by the prescribing provider.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Rheumatologist and Dermatologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
57
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ERAXIS<br />
FDA-APPROVED INDICATIONS<br />
Eraxis® is indicated:<br />
A. For the treatment of candidemia and other Candida infections.<br />
COVERAGE POLICY<br />
Eraxis® is covered for members who meet the following criteria:<br />
A. The prescribing physician is an infectious disease specialist.<br />
B. AND the patient is 2 years of age or older.<br />
C. AND the diagnosis is documented as candidemia or another Candida infection<br />
D. AND the patient has completed a documented trial and failure of Fluconazole<br />
E. AND verification of all B vs. D criteria indicate coverage by Part D<br />
NON COVERAGE<br />
Eraxis® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT an infectious disease specialist<br />
B. The patient is under the age of 2 years old.<br />
C. The diagnosis is NOT documented as candidemia or another Candid infection<br />
D. The patient has NOT completed a documented trial and failure of Fluconazole<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Infectious Disease<br />
AUTHORIZATION PERIOD<br />
6 Months<br />
58
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ERYTHROPOIESIS STIMULATING AGENTS<br />
FDA-APPROVED INDICATIONS<br />
erythropoietin is indicated:<br />
A. For the treatment of anemia associated with chronic renal failure (CRF), including<br />
patients on dialysis and patients not on dialysis. Erythropoietin is indicated to<br />
elevate or maintain the red blood cell level (as manifested by the hematocrit or<br />
hemoglobin determinations) and to decrease the need for transfusions in these<br />
patients.<br />
B. Non-dialysis patients with symptomatic anemia considered for therapy should<br />
have a hemoglobin less than 10 g/dL.<br />
C. For the treatment of anemia related to therapy with zidovudine in HIV-infected<br />
patients.<br />
D. For the treatment of anemia in patients with non-myeloid malignancies where<br />
anemia is due to the effect of concomitantly administered chemotherapy.<br />
E. For the treatment of anemic patients (hemoglobin Greater than 10 to Less than or<br />
equal to 13 g/dL) who are at high risk for perioperative blood loss from elective,<br />
noncardiac, nonvascular surgery to reduce the need for allogenic blood<br />
transfusions.<br />
COVERAGE POLICY<br />
Erythropoietin is covered for members who meet the following criteria:<br />
A. Lab values have been completed within 30 days of the request.<br />
B. AND the diagnosis is documented as treatment for a surgery patient who is at<br />
high risk for perioperative blood loss.<br />
a. AND the patient’s hemoglobin is Greater than 10 to Less than or equal to<br />
12 g/dL OR hematocrit Less than or equal to 33%.<br />
b. AND the patient is receiving iron supplementation. (Please verify in the<br />
patient’s drug history or chart that the patient is receiving iron therapy).<br />
c. AND surgery is within 30 days of request.<br />
d. AND therapy is NOT being used to prevent a patient from receiving a<br />
transfusion for religious reasons.<br />
e. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
f. AND authorization can be allowed for up to one month. (Treatment can<br />
include 4 weekly doses).<br />
C. OR the diagnosis is documented as the treatment of anemia associated with<br />
chronic renal failure.<br />
a. AND the patient is NOT on dialysis. (Please verify if the patient is on<br />
dialysis. Medicare Part B pays for erythropoietin when the patient is<br />
receiving dialysis).<br />
ERYTHROPOIESIS STIMULATING AGENTS<br />
59
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
(Continued)<br />
b. AND it is the initial request for erythropoietin (Patient has not received<br />
erythropoietin therapy for at least 12 weeks):<br />
c. AND the patient’s transferrin saturation is at least 20%. (Please verify the<br />
lab value in the patient’s chart).<br />
d. AND the patient’s ferritin level is at least 100 ng/mL. (Please verify the<br />
lab value in the patient’s chart.)<br />
e. AND the patient’s hemoglobin is Less than or equal to 11 g/dL OR<br />
hematocrit Less than or equal to 33%.<br />
f. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
g. AND authorization can be allowed for up to 12 weeks.<br />
h. AND/OR the patient has received previous erythropoietin therapy within<br />
the last 12 weeks.<br />
i. AND the patient’s hemoglobin is Less than 12 g/dL OR hematocrit Less<br />
than 36%.<br />
j. AND the patient’s transferrin saturation is at least 20%.<br />
k. AND the patient’s ferritin level is at least 100 ng/mL.<br />
l. AND the patient has experienced an increase in hemoglobin or hematocrit<br />
since the initial erythropoietin treatment and therapy is needed to maintain<br />
the patient’s current hemoglobin or hematocrit level.<br />
m. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
n. AND authorization can be allowed for up to 24 weeks.<br />
D. OR the diagnosis is documented as treatment of anemia in an HIV-infected<br />
patient.<br />
a. AND it is the initial request for erythropoietin (Patient has not received<br />
erythropoietin therapy for at least 12 weeks):<br />
b. AND the patient is on anti-retroviral therapy. (e.g. Epivir, lamivudine,<br />
Zerit, stavudine, Hivid, Retrovir, zidovudine, Ziagen, Entriva, Combivir,<br />
Trizivir, Truvada, Epzicom, Viramune, Rescriptor, Sustiva, Atripla,<br />
Fuzeon). (Please verify the use of anti-retroviral by reviewing the<br />
patient’s chart or drug history).<br />
c. AND the patient’s transferrin saturation is at least 20%. (Please verify in<br />
the patient’s chart)<br />
d. AND the patient’s hemoglobin is Less than or equal to 11 g/dL OR<br />
hematocrit Less than or equal to 33%. (Please verify in the patient’s chart.)<br />
ERYTHROPOIESIS STIMULATING AGENTS<br />
60
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
(Continued)<br />
e. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
f. AND authorization can be allowed for up to 12 weeks.<br />
g. AND/OR the patient has received previous erythropoietin therapy within<br />
the last 12 weeks.<br />
h. AND the patient is on anti-retroviral therapy. (e.g. Epivir, lamivudine,<br />
Zerit, stavudine, Hivid, Retrovir, zidovudine, Ziagen, Entriva, Combivir,<br />
Trizivir, Truvada, Epzicom, Viramune, Rescriptor, Sustiva, Atripla,<br />
Fuzeon). (Please verify the use of anti-retroviral by reviewing the<br />
patient’s chart or drug history).<br />
i. AND the patient’s serum erythropoietin level was Less than or equal to<br />
500 mUnits/mL at the time therapy was initiated. (Please verify in the<br />
patient’s chart).<br />
j. AND the patient’s transferrin saturation is at least 20%. (Please verify in<br />
the patient’s chart)<br />
k. AND the patient’s hemoglobin is Less than or equal to 12 g/dL OR<br />
hematocrit Less than or equal to 36%. (Please verify in the patient’s<br />
chart.)<br />
l. AND the patient has experienced an increase in hemoglobin or hematocrit<br />
since the initial erythropoietin treatment and therapy is needed to maintain<br />
the patient’s current hemoglobin or hematocrit level.<br />
m. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
n. AND authorization can be allowed for up to 24 weeks.<br />
E. OR the diagnosis is documented as treatment of anemia in cancer patients on<br />
chemotherapy.<br />
a. AND it is the initial request for erythropoietin (Patient has not received<br />
erythropoietin therapy for at least 12 weeks):<br />
b. AND the patient has a non-myeloid malignancy.<br />
c. AND the patient is receiving a chemotherapy regimen to treat the nonmyeloid<br />
malignancy.<br />
d. AND the patient’s transferrin saturation is at least 20%. (Please verify in<br />
the patient’s chart)<br />
e. AND the patient’s serum erythropoietin level is Less than or equal to 200<br />
mUnits/mL. (Please verify in the patient’s chart. Levels above<br />
200mUnits/mL is not recommended).<br />
f. AND the patient’s hemoglobin is Less than or equal to 11 g/dL OR<br />
hematocrit Less than or equal to 33%. (Please verify in the patient’s<br />
Chart).<br />
ERYTHROPOIESIS STIMULATING AGENTS<br />
61
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
(Continued)<br />
g. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
h. AND authorization can be allowed for up to 12 weeks.<br />
i. AND/OR the patient has received previous erythropoietin therapy within<br />
the last 12 weeks.<br />
j. AND the patient has a non-myeloid malignancy.<br />
k. AND the patient is receiving a chemotherapy regimen to treat the nonmyeloid<br />
malignancy.<br />
l. AND the patient’s transferrin saturation is at least 20%.<br />
m. AND the patient’s serum erythropoietin level was Less than or equal to<br />
200 mUnits/mL at the time therapy was initiated. (Please verify in the<br />
patient’s chart. Levels above 200mUnits/mL is not recommended).<br />
n. AND the patient’s hemoglobin is Less than or equal to 12 g/dL OR<br />
hematocrit Less than or equal to 36%. (Please verify in the patient’s chart.)<br />
o. AND the patient has experienced an increase in hemoglobin or hematocrit<br />
since the initial erythropoietin treatment and therapy is needed to maintain<br />
the patient’s current hemoglobin or hematocrit level.<br />
p. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
q. AND authorization can be allowed for up to 24 weeks.<br />
F. OR the diagnosis is documented as anemia secondary to myelodysplasia.<br />
a. AND it is the initial request for erythropoietin (Patient has not received<br />
erythropoietin therapy for at least 12 weeks):<br />
b. AND the patient’s serum erythropoietin level is Less than or equal to 500<br />
mUnits/mL. (Please verify in the patient’s chart).<br />
c. AND the patient’s transferrin saturation is at least 20%. (Please verify in<br />
the patient’s chart)<br />
d. AND the patient’s hemoglobin is Less than or equal to 11 g/dL OR<br />
hematocrit Less than or equal to 33%. (Please verify in the patient’s chart.)<br />
e. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
f. AND authorization can be allowed for up to 12 weeks.<br />
g. AND/OR the patient has received previous erythropoietin therapy within<br />
the last 12 weeks.<br />
h. AND the patient’s serum erythropoietin level was less than or equal to 500<br />
mUnits/mL at the time therapy was initiated. (Please verify in the patient’s<br />
chart).<br />
ERYTHROPOIESIS STIMULATING AGENTS<br />
62
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
(Continued)<br />
i. AND the patient’s transferrin saturation is at least 20%. (Please verify in<br />
the patient’s chart)<br />
j. AND the patient’s hemoglobin is Less than or equal to 12 g/dL OR<br />
hematocrit Less than or equal to 36%. (Please verify in the patient’s chart.)<br />
k. AND the patient has experienced an increase in hemoglobin or hematocrit<br />
since the initial erythropoietin treatment and therapy is needed to maintain<br />
the patient’s current hemoglobin or hematocrit level.<br />
l. AND the patient is presenting to a retail pharmacy with a prescription for<br />
erythropoietin (Medicare Part B only pays for erythropoietin when a<br />
physician or facility dispenses the medication from their own supply).<br />
m. AND authorization can be allowed for up to 24 weeks.<br />
NON COVERAGE<br />
Erythropoietin is NOT covered for members who meet the following criteria:<br />
A. The patient’s transferrin saturation is NOT at least 20%. (Please verify the lab<br />
value in the patients chart).<br />
B. OR the patient’s ferritin level is NOT at least 100 ng/mL. (Please verify the lab<br />
value in the patients chart.)<br />
C. OR the patient’s hemoglobin is greater than 10 g/dL OR hematocrit greater than<br />
33%.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
12 weeks<br />
63
FDA-APPROVED INDICATIONS<br />
Amifostine is indicated:<br />
A. Nephrotoxicity Prophylaxis<br />
B. Xerostomia Prophylaxis<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ETHYOL<br />
COVERAGE POLICY<br />
Amifostine is covered for members who meet the following criteria:<br />
A. Patient is being treated for FDA indications as stated above<br />
B. AND being prescribed by an Oncologist<br />
C. AND B vs. D criteria indicates coverage should be through Medicare Part D<br />
NON COVERAGE<br />
Amifostine is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
B. Known hypotension with dehydration<br />
C. Hypersensitivity to aminothiol or mannitol<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
6 months<br />
64
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
EXELON<br />
FDA APPROVED INDICATIONS<br />
A. Alzheimers<br />
B. Parkinson’s Dementia<br />
C. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Exelon is covered for members who meet the following criteria:<br />
A. For treatment of Alzheimer’s Disease:<br />
a. Failure to at least a three month trial with Aricept<br />
B. For treatment of Parkinson’s Disease:<br />
a. Trial with at least TWO of the following:<br />
i. Amantadine<br />
ii. Bromocriptine<br />
iii. Carbidopa/Levodopa<br />
iv. Comtan<br />
v. Mirapex<br />
vi. Ropinirole<br />
vii. Selegiline<br />
NON COVERAGE<br />
Exelon is not covered for members who meet the following criteria:<br />
A. No documented trial and failure to Aricept and Namenda therapy<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart Notes<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
65
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
EXJADE<br />
FDA-APPROVED INDICATIONS<br />
Exjade® is indicated:<br />
A. For the treatment of chronic iron toxicity secondary to transfusional iron<br />
overload (e.g. due to transfusional hemosiderosis in patients with chronic<br />
anemias such as thalassemia and sickle cell anemia)<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Exjade® is covered for members who meet the following criteria:<br />
A. Patient has a diagnosis of transfusion-dependent anemia (β-thalassemia, sickle<br />
cell disease, Diamond-Blackfan anemia, or myelodysplastic syndrome) and<br />
chronic iron overload due to blood transfusions, evidenced by serum ferritin<br />
1,000-8,000ng/mL.<br />
B. Patient failed Desferal therapy due to compliance or is unable to use it<br />
(documentation of noncompliance, adverse effects, and/or contraindications).<br />
C. Exjade is being prescribed by a hematologist or other specialist.<br />
Recommended monitoring includes monthly serum ferritin, baseline and monthly serum<br />
creatinine, monthly urine protein, monthly LFTs, baseline and yearly auditory and<br />
ophthalmic testing, including slit-lamp examination and dilated funduscopy.<br />
NON COVERAGE<br />
Exjade® is NOT covered for members with the following criteria<br />
A. The diagnosis is not documented as chronic iron toxicity secondary to<br />
transfusional iron overload.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Hematologist<br />
AUTHORIZATION PERIOD<br />
3 months<br />
66
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
FABRAZYME<br />
FDA-APPROVED INDICATIONS<br />
Fabrazyme® is indicated:<br />
A. For use in patients with Fabry disease.<br />
COVERAGE POLICY<br />
Fabrazyme® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as a patient with Fabry disease.<br />
B. AND the diagnosis has been confirmed with an enzyme assay measuring a<br />
deficient activity of alpha-galactosidase enzyme.<br />
NON COVERAGE<br />
Fabrazyme® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as Fabry disease.<br />
B. The diagnosis has not been confirmed with an enzyme assay measuring the<br />
deficient activity of alpha-glactosidase enzyme.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
67
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
FLEBOGAMMA<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
B. Treatment of hypergammaglobulinemia<br />
C. AND the patient is diagnosed with primary immunodeficiency<br />
D. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
E. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
C. Medication is covered by Part B per CMS guidelines<br />
D. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency, OR<br />
Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
68
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
FORTEO<br />
FDA-APPROVED INDICATIONS<br />
Forteo® is indicated:<br />
A. For the treatment of postmenopausal women with osteoporosis who are at high<br />
risk for fracture. These include women with a history of osteoporotic fracture, or<br />
who have multiple risk factors for fracture, or who have failed or are intolerant of<br />
previous osteoporosis therapy.<br />
B. For the treatment to increase bone mass in men with primary or hypogonadal<br />
osteoporosis who are at high risk for fracture.<br />
COVERAGE POLICY<br />
Forteo® is covered for members who meet the following criteria:<br />
A. Patient has NOT been diagnosed with Paget’s disease nor has high levels of<br />
alkaline phosphatase.<br />
B. AND the patient does NOT have pre-existing hypercalcemia, skeletal<br />
malignancies, or prior radiation therapy involving the skeleton.<br />
C. AND if the patient is female, is she age 50 years old or older (postmenopausal).<br />
D. AND diagnosis is documented as postmenopausal women with osteoporosis or a<br />
man with primary or hypgonadal osteoporosis.<br />
E. AND the patient has at least two of the following fracture risk fractures:<br />
a. T score Less than or equal to - 2.5.<br />
b. <strong>Prior</strong> fragility fracture (Counts as two risk fractures).<br />
c. Age Greater than or equal to 70 years old.<br />
d. Family history (1 st degree relative).<br />
F. AND the patient has failed to have an adequate response to treatment with a<br />
bisphosphonate therapy (Fosamax®, alendronate, Actonel®, risedronate,<br />
Boniva® and/or Reclast®) for at least 1 year. (Please verify that the patient has<br />
received bisphosphonate therapy by reviewing the patient’s drug history or<br />
patient’s chart).<br />
G. AND patient has NOT had accumulative Forteo® therapy for more than 24<br />
months (Lifetime therapy).<br />
H. AND evidence of diagnosis, risk fractures, and tried bisphosphonate therapy is<br />
documented in patient’s chart notes provided by prescribing provider.<br />
NON COVERAGE<br />
Forteo® is NOT covered for members with the following criteria:<br />
A. Patient has been diagnosed with Paget’s disease and/or has high levels of alkaline<br />
phosphatase and/or has hypercalcemia and/or skeletal malignancies and/or prior<br />
radiation therapy involving the skeleton.<br />
B. If the patient is female and is under the age of 50 and has not experienced<br />
menopause.<br />
C. Diagnosis is NOT documented as osteoporosis.<br />
D. The patient does NOT have at least TWO risk factors.<br />
69
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
FORTEO<br />
(Continued)<br />
E. The patient has NOT had an adequate response to bisphosphonate treatment.<br />
F. The patient has had more than 24 months of Forteo® therapy.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
70
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
GAMASTAN<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
D. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
a. Treatment of hypogammaglobulinemia<br />
B. OR the patient is diagnosed as per FDA-Approved indications above<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
71
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
GAMMAGARD<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
B. Treatment of hypergammaglobulinemia<br />
C. AND the patient is diagnosed with primary immunodeficiency<br />
D. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
E. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency, OR<br />
Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
72
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
GAMUNEX<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
B. Treatment of hypergammaglobulinemia<br />
C. AND the patient is diagnosed with primary immunodeficiency<br />
D. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
E. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
6 months<br />
73
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
GLEEVEC<br />
FDA-APPROVED INDICATIONS<br />
Gleevec® is indicated:<br />
A. For newly diagnosed adult patients with Philadelphia chromosome positive<br />
chronic myeloid leukemia (Ph+CML) in chronic phase.<br />
B. For patients with Ph+CML in blast crisis, accelerated phase, or in chronic phase<br />
after failure of interferon-alpha therapy.<br />
C. For pediatric patients with Ph+CML in chronic phase who are newly diagnosed or<br />
whose disease has recurred after stem cell transplant or who are resistant to<br />
interferon-alpha therapy.<br />
D. For adult patients with relapsed or refractory Philadelphia chromosome positive<br />
acute lymphoblastic leukemia (Ph+ ALL).<br />
E. For adult patients with myelodysplastic/myeloproliferative diseases (MDS/MPD)<br />
associated with PDGFR (platelet-derived growth factor receptor) gene rearrangements.<br />
F. For adult patients with aggressive systemic mastocytosis (ASM) without the<br />
D816V c-Kit Mutation or with C-Kit mutation status unknown.<br />
G. For adult patients with hypereosinophilic syndrome (HES) and/or chronic<br />
eosinophilic Leukemia (CEL) who have the FIP1L1-PDGFR alpha fusion kinase,<br />
FIP1l1-PDGFR alpha fusion kinase negative or unkown.<br />
H. For adult patients with unresectable, recurrent and/or metastatic<br />
dermatofibrosarcoma protuberans (DFSP).<br />
I. For patients with Kit (CD117) positive unresectable and/or metastatic malignant<br />
gastrointestinal stromal tumors (GIST).<br />
COVERAGE POLICY<br />
Gleevec® is covered for members who meet the following criteria:<br />
A. The prescribing physician is board certified as an oncologist, hemaatologist or has<br />
obtained a consult from any of the listed specialties.<br />
B. AND if the patient is female, she is NOT pregnant AND has no plans to conceive.<br />
C. AND diagnosis is documented as KIT (CD117) positive unresectable and/or<br />
metastatic malignant gastrointestinal stromal tumors (GIST).<br />
D. OR diagnosis is documented as an adult patient with Philadelphia chromosome<br />
positive chronic myeloid leukemia (Ph+CML) in chronic phase, in blast crisis or<br />
in accelerated phase.<br />
E. OR an adult patient with relapsed or refractory Philadelphia chromosome positive<br />
acute lymphoblastic leukemia (Ph+ ALL).<br />
F. OR a pediatric patient with Ph+CML.<br />
a. And the pediatric patient is in a chronic phase.<br />
G. OR an adult patient with myelodysplastic/ myeloproliferative disease<br />
(MDS/MPD).<br />
a. AND the MDS/MPD is associated with PDGFR (platelet-derived growth<br />
factor receptor) gene re-arrangements.<br />
74
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
GLEEVEC<br />
(Continued)<br />
H. OR an adult patient with aggressive systemic mastocytosis (ASM).<br />
a. And the patient does not have a D816V C-Kit mutation or the c-Kit<br />
mutation status is unknown.<br />
I. OR an adult patient with hypereosinophilic syndrome (HES) and/or chronic<br />
eosinophilic leukemia (CEL).<br />
J. OR an adult patient with unresectable, recurrent and/or metastatic<br />
dermatofibrosarcoma protuberans (DFSP).<br />
K. AND if the patient has received previous Gleevec® therapy, the provider must<br />
show a documented hematologic or cytogenic response to imatinib.<br />
L. Patient is on duplicate therapy that can include interferon alpha therapy (eg.<br />
Intron-A®, Roferon A®, Pegasys®, and or Infergen®). (Please verify that the<br />
patient has received interferon alpha therapy by reviewing the patient’s drug<br />
history).<br />
M. AND evidence of diagnosis and hematologic or cytogenic response (for retreatment)<br />
documented in patient’s chart notes provided by the prescribing<br />
provider.<br />
NON COVERAGE<br />
Gleevec® is NOT covered for members with the following criteria:<br />
A. Patient is female is pregnant or plans to conceive.<br />
B. Patient’s diagnosis is NOT documented in the patient’s chart notes as KIT<br />
(CD117) positive unresectable and/or metastatic malignant GIST, or an adult with<br />
Ph+CML in chronic phase, blast crisis or in accelerated phase, or an adult patient<br />
with relapsed or refractory PH+ALL, or an adult patient with MDS/MPD that is<br />
NOT associated with PDGFR gene re-arrangements, or an adult diagnosed patient<br />
with HES and/or CEL or an adult patient diagnosed with unresectable, recurrent<br />
and/or metastatic DFSP.<br />
C. OR the diagnosis is a pediatric patient with Ph+CML not the in chronic phase.<br />
D. OR the diagnosis is an adult patient with MDS/MPD and is NOT associated with<br />
PDGFR gene re-arrangements.<br />
E. OR the patient has received previous Gleevec® therapy and has not shown a<br />
hematologic or cytogenic response.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
75
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HUMAN CHORIONIC GONADOTROPIN, HCG<br />
FDA-APPROVED INDICATIONS<br />
Gonadotropin is indicated for:<br />
A. Cryptorchidism<br />
B. Hypogonadotropic hypogonadism, In male patients<br />
COVERAGE POLICY<br />
Gonadotropin is covered for members who meet either of the following criteria:<br />
A. In a Male patient<br />
a. If the patient has a diagnosis of prepubertal cryptochidism not due to<br />
anatomic obstruction or hypogonadism secondary to a pituitary deficiency.<br />
b. AND If the patient does not have any signs of the following diagnoses:<br />
i. Precocious puberty, or<br />
ii. Prostatic carcinoma or other androgen dependent neoplasm<br />
c. And is not being used in the treatment of obesity.<br />
B. Not covered for female patients<br />
NON COVERAGE<br />
Gonadotropin is NOT covered for members of the following criteria:<br />
A. In a Male patient:<br />
a. If the patient does NOT have a diagnosis of prepubertal cryptochidism not<br />
due to anatomic obstruction or hypogonadism secondary to a pituitary<br />
deficiency.<br />
b. If the patient does have any signs of the following diagnoses:<br />
i. Precocious puberty, or<br />
ii. Prostatic carcinoma or other androgen dependent neoplasm<br />
c. If it is being used in the treatment of obesity.<br />
B. If patient is female<br />
REQUIRED MEDCIAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
76
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HEPATITIS C<br />
Indications / Required <strong>Criteria</strong>:<br />
Treatment will be approved when any of the following indication(s) exists:<br />
A. Chronic Hepatitis C Virus (HCV), Genotype 1 or 4<br />
a. Recent lab reports documenting elevated HCV RNA are required, along<br />
with genotype.<br />
b. Request is initiated by a GI or infectious disease specialist.<br />
c. Initial authorization will be given for 12 weeks. At 12 weeks, an early<br />
viral response (EVR) must be documented via repeat HCV RNA assay.<br />
(EVR during the first 12 weeks is predictive of the patients viral<br />
response3).<br />
d. For patients with a greater than2log reduction in viral load, therapy may<br />
be continued up to a total of 48 weeks treatment.<br />
e. For patients who fail to achieve a 2log reduction, treatment should be<br />
discontinued. These patients have a less then 2% chance of achieving an<br />
SVR with continued therapy3,4.<br />
B. Chronic Hepatitis C Virus (HCV), Genotype 2, 3, 5, or 6<br />
a. Recent lab reports documenting elevated HCV RNA are required, along<br />
with genotype.<br />
b. Request is initiated by a GI or infectious disease specialist. 12. Initial<br />
authorization will be given for 12 weeks. At 12 weeks, an early viral<br />
response (EVR) must be documented via repeat HCV RNA assay. (EVR<br />
during the first 12 weeks is predictive of the patient’s viral response3).<br />
c. For patients with a greater than2log reduction in viral load, therapy may<br />
be continued up to a total of 24 weeks treatment.<br />
d. For patients who fail to achieve a 2log reduction, treatment should be<br />
discontinued. These patients have a less then 2% chance of achieving an<br />
SVR with continued therapy3,4.<br />
C. Retreatment (not approvable)<br />
a. Re-treatment of non-responders to standard interferon-ribavirin<br />
combinations is not generally indicated, and therefore will not be<br />
approved. Only 15-20% of nonresponders achieve an SVR upon retreatment.<br />
Response rates are even poorer for those with Genotype 1.<br />
b. For patients who have relapsed after combination treatment, re-treatment<br />
is generally not indicated and is currently being studied. Upon retreatment,<br />
most of these patients relapse as well<br />
D. OR the indication is documented as chronic hepatitis B<br />
a. AND the patient has evidence of a positive HBsAg (+ or -) serological<br />
marker for greater than 6 months OR evidence by a liver biopsy showing<br />
chronic hepatitis<br />
b. AND the patient has a Hepatitis B viral load greater than 100,000 copies<br />
per ml<br />
77
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HEPSERA<br />
FDA-APPROVED INDICATIONS<br />
Hepsera® is indicated:<br />
A. For the treatment of chronic hepatitis B in patients Greater than or equal to 12<br />
years of age.<br />
COVERAGE POLICY<br />
Hepsera® is covered for members who meet the following criteria:<br />
A. Patient is age 12 years or older.<br />
B. AND the patient has been diagnosed with chronic hepatitis B.<br />
C. AND the patient has evidence of a positive HBsAg (+ or -) serological marker for<br />
greater than 6 months OR evidence by a liver biopsy showing chronic hepatitis.<br />
(Please verify that the patient has a HBsAg serological marker for greater than 6<br />
months or a positive liver biopsy by reviewing the patient’s drug history or chart).<br />
D. AND the patient has a Hepatitis B viral load greater than 100,000 copies per ml.<br />
E. AND the patient has elevations in liver aminotransferases (ALT or AST) that are<br />
two (2) times greater than normal.<br />
F. AND the patient has been tested for HIV. (Hepsera® therapy can cause HIV<br />
resistance in untreated HIV infection). AND if the patient has received previous<br />
Hepsera® treatment, there is documented clinical improvement shown by a drop<br />
in viral load or reduction in the patient’s liver aminotransferases. (Please verify<br />
patient’s chart notes to verify drop in viral load or reduction in liver<br />
aminotransferases from their starting level).<br />
G. AND the patient is not receiving duplicate therapy that includes Baraclude®,<br />
Tyzeka®, Epivir®, Intron A® and/or Infergen®. (Please verify that the patient<br />
does not have duplicate therapy by reviewing the patient’s drug history or chart).<br />
H. AND evidence of diagnosis, serological markers, liver biopsy, viral load, and<br />
liver aminotransferases is documented in patient’s chart.<br />
NON COVERAGE<br />
Hepsera® is NOT covered for members with the following criteria:<br />
A. Patient is under the age of 12 years old.<br />
B. Patient has NOT been diagnosed with chronic hepatitis B.<br />
C. Patient has NO evidence of a Hepatitis B serological marker for greater than 6<br />
months OR evidence by a positive liver biopsy.<br />
D. Patient does NOT have a Hepatitis B viral load greater than 100,000 copies per<br />
ml.<br />
E. Patient does NOT have liver aminotransferases (ALT or AST) that are two (2)<br />
times greater than normal.<br />
F. Patient has NOT been tested for HIV.<br />
G. Patient is on duplicate therapy that can include one of the following: Baraclude®,<br />
Tyzeka®, Epivir®, Intron-A®, and or Infergen®.<br />
79
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HEPSERA<br />
(Continued)<br />
H. Prescriber has provided no evidence of diagnosis, serological markers, viral load,<br />
duplicate therapy or liver Aminotransferases.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
80
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HUMIRA<br />
FDA-APPROVED INDICATIONS<br />
Humira® is indicated:<br />
B. For reducing signs and symptoms in patients with active ankylosing spondylitis.<br />
C. For the treatment of adult patients (18 years or older) with moderate to severe<br />
chronic plaque psoriasis who are candidates for systemic therapy or phototherapy.<br />
D. For reducing signs and symptoms, inducing major clinical response, inhibiting the<br />
progression of structural damage, and improving physical function in patients<br />
with moderately to severely active rheumatoid arthritis. Humira® can be used<br />
alone or in combination with methotrexate or other disease-modifying antirheumatic<br />
drugs (DMARDS).<br />
E. For reducing signs and symptoms, inhibiting the progression of structural damage,<br />
and improving physical function in patients with psoriatic arthritis. Humira® can<br />
be used in alone or in combination with DMARDS.<br />
F. For reducing signs and symptoms and inducing and maintaining clinical remission<br />
in adult patients with moderately to severely active Crohn’s disease who have had<br />
an inadequate response to conventional therapy. Humira® is indicated for<br />
reducing signs and symptoms and inducing clinical remission in patients who<br />
have lost response to or are intolerant to infliximab.<br />
G. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Humira® is covered for members who meet the following criteria:<br />
H. Patient has NO history of auto immune disease, recurring infections, heart failure,<br />
immuno suppression or malignancies.<br />
I. AND the prescribing provider is a gastroenterologist, rheumatologist,<br />
dermatologist, orthopedist or has obtained a consult from the listed specialties.<br />
J. AND diagnosis is documented as moderate to severe active rheumatoid arthritis.<br />
a. AND the patient has at least four (4) of the following symptoms:<br />
i. Morning stiffness.<br />
ii. Arthritis of three (3) or more joint areas.<br />
iii. Arthritis of hand joints.<br />
iv. Symmetric arthritis.<br />
v. Rheumatoid nodules.<br />
vi. Serum rheumatoid factor.<br />
vii. Radiographic changes.<br />
81
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HUMIRA<br />
(Continued)<br />
b. AND the patient has had at least an 8-week maximum tolerated dose trial<br />
and failure to at least two (2) of the following DMARDS listed:<br />
Methotrexate, cyclosporine, Neoral®, Sandimmune®, Gengraf®,<br />
azathioprine, Imuran®, penicillamine, Cuprimine®, Depen®,<br />
sulfasalazine, Azulfidine®, leflunomide, Arava®, gold sodium thiomalate,<br />
Aurolate®, aurothioglucose, Solganal®, auranofin, Ridaura®,<br />
hydroxychoroquine, Plaquenil®. (Verification can be made by reviewing<br />
the patient’s drug history or patient’s chart).<br />
c. AND if the patient has received previous Humira® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or<br />
progression of disease.<br />
K. OR the diagnosis is documented as psoriatic arthritis.<br />
a. AND the patient has at least one of the following symptoms:<br />
i. Three (3) or more swollen joints.<br />
ii. Three (3) or more tender joints.<br />
b. AND the patient has had at least an 8-week maximum tolerated dose trial<br />
and failure to at least two (2) of the following DMARDS listed:<br />
(cyclosporine, Neoral®, Sandimmune®, Gengraf®, azathioprine,<br />
Imuran®, penicillamine, Cuprimine®, Depen®, sulfasalazine,<br />
Azulfidine®, leflunomide, Arava®, gold sodium thiomalate, Aurolate®,<br />
aurothioglucose, Solganal®, auranofin, Ridaura®, hydroxychoroquine,<br />
Plaquenil®) if methotrexate is contraindicated. (Verification can be made<br />
by reviewing the patient’s drug history or patient’s chart).<br />
c. AND if the patient has received previous Humira® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or delay<br />
in progression of disease.<br />
L. OR the diagnosis is documented as active ankylosing spondylitis.<br />
a. AND the patient has tried and failed at least a 60-day trial of at least two<br />
non-steroidal anti-inflammatory (NSAID) drugs that can include any two<br />
of the following medications: Diclofenac, etodolac, fenoprofen,<br />
flurbiprofen, ibuprofen, indomethacin, celecoxib, Celebrex®, ketoprofen,<br />
meclofenamate, nabumetone, naproxen, oxaprozin, piroxicam, sulinidac,<br />
or tolmetin. (Please verify that the patient has received NSAID therapy by<br />
reviewing the patient’s drug history).<br />
b. AND if the patient has received previous Humira® therapy, the provider<br />
must show an improvement in clinical symptoms that may include<br />
improvement in tender and swollen joint count, mobility, stiffness or delay<br />
in the progression of disease.<br />
M. OR the diagnosis is documented as chronic moderate to severe plaque psoriasis.<br />
82
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HUMIRA<br />
(Continued)<br />
a. AND the patient has had the disease for 1 year or greater.<br />
b. AND the patient’s age is 18 years old or older.<br />
c. AND the involvement of plaque psoriasis is 10% or greater of the patient’s<br />
total body surface area (BSA) OR if the BSA is less than 10%, the plaque<br />
psoriasis must involve areas that will prevent the patient from performing<br />
crucial daily functions such as walking (eg. feet).<br />
d. AND the patient has tried and failed at least a 60-day trial of two (2)<br />
conventional therapies that may include any of the following:<br />
i. High potency topical steroid treatment.<br />
ii. Calcipotriene (Dovonex®)<br />
iii. Phototherapy.<br />
iv. Retinoids (Soriatane®)<br />
v. Methotrexate.<br />
vi. Cyclosporine.<br />
e. If the patient has received Humira® therapy for greater than three (3)<br />
months, the patient must see a significant reduction in plaque thickness,<br />
erythemia, desquamation and affected body surface area.(Please verify<br />
patient’s chart notes to verify clinical improvement).<br />
N. OR the diagnosis is documented as Crohn’s Disease:<br />
a. AND the patient has tried, failed and/or had an inadequate response to a<br />
60-day trial of at least two Crohn’s disease conventional therapies that<br />
may include the following: Sulfazalazine, Azulfidine®, balsalazide,<br />
Colazal®, mesalamine, Asacol®, Canasa®, Lialda®, Pentasa®,<br />
Rowasa®, azathioprine, Imuran®, cyclosporine, Neoral®, Sandimmune®,<br />
Gengraf®, methotrexate, mercaptopurine, or Purinethol®.<br />
b. AND if the patient has received previous Humira® therapy, the patient<br />
must see an improvement in clinical symptoms that can include reduced<br />
abdominal pain, diarrhea, cramps, and/or fistulas.<br />
c. AND the patient will NOT receive combination therapy with other<br />
biologic and/or retinoid therapy. (Eg. Enbrel®, Remicade®, Kineret®,<br />
Orencia®, Soriatane® Tysabri®, Raptiva® and Rituxan®. (Please verify<br />
that the patient is not on duplicate therapy by reviewing the patient’s drug<br />
history or chart).<br />
d. AND evidence of diagnosis, previous failed therapy, or clinical<br />
improvement is documented in patient’s chart notes provided by<br />
prescribing provider.<br />
NON COVERAGE<br />
Humira® is NOT covered for members with the following criteria:<br />
J. Patient has a history of auto immune disease, recurring infections, heart failure,<br />
immuno suppression or malignancies.<br />
83
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
HUMIRA<br />
(Continued)<br />
K. The prescribing provider is NOT a rheumatologist, gastroenterologist,<br />
dermatologist, orthopedist or obtained a consult from the listed specialties.<br />
L. The diagnosis is NOT documented as severe active rheumatoid arthritis, Crohn’s<br />
disease, psoriatic arthritis, ankylosing spondylitis or chronic moderate to severe<br />
plaque psoriasis.<br />
M. The diagnosis is listed as ulcerative colitis.<br />
N. If the diagnosis is listed as severe active rheumatoid arthritis, the patient does<br />
NOT have four of the listed symptoms.<br />
O. If the diagnosis is listed as severe active rheumatoid arthritis, the patient has NOT<br />
failed a 8-week maximum tolerated trial to at least two DMARDs.<br />
P. If the diagnosis is psoriatic arthritis and the patient does NOT have three swollen<br />
joints or three tender joints.<br />
Q. If the diagnosis is psoriatic arthritis and the patient has NOT failed a 8-week<br />
maximum tolerated trial to at least two DMARDs.<br />
R. If the diagnosis is ankylosing spondylitis and the patient has NOT failed two 60-<br />
day NSAID drug regimens.<br />
S. If the diagnosis is chronic moderate to severe plaque psoriasis and the patient has<br />
not had the disease for 1 year or greater.<br />
T. If the diagnosis is chronic moderate to severe plaque psoriasis and the<br />
involvement is less than 10% of body surface area or does NOT involve an area<br />
that will affect a critical daily function.<br />
U. If the diagnosis is chronic moderate to severe plaque psoriasis and the patient has<br />
NOT failed a 60-day trial to two conventional therapies.<br />
V. If the diagnosis is documented as Crohn’s disease and the patient has NOT failed<br />
at least two 60-day conventional drug regimens.<br />
W. If the patient is receiving combination therapy that includes any one of the<br />
following medications: Enbrel®, Remicade®, Tysabri®, Kineret®, Orencia®,<br />
Soriatane® or Rituxan®.<br />
X. If the patient has received previous Humira® therapy and the provider has NOT<br />
shown an improvement in clinical symptoms.<br />
Y. Evidence of diagnosis, previous failed therapy and symptoms are NOT<br />
documented in patient’s chart notes provided by the prescribing provider.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Rheumatologist, Dermatologist and<br />
Gastroenterology<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
84
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
IMITREX<br />
FDA-APPROVED INDICATIONS<br />
Imitrex® is indicated:<br />
A. For the treatment of migraine headache attacks with or without aura and cluster<br />
headache<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Imitrex® is covered for members who meet the following criteria:<br />
A. The patient is 18 years of age or older.<br />
B. AND the diagnosis is documented as migraine headache or cluster headache<br />
C. AND the the patient has completed a documented trial and failure of an abortive<br />
medication such as Fioricet, Fiorinal, Tylenol and NSAIDs<br />
NON COVERAGE<br />
Imitrex® is NOT covered for members who meet the following criteria:<br />
A. A. The patient is under the age of 18 years old. .<br />
B. The diagnosis is NOT migraine headache or cluster headache<br />
C. The patient has not completed a documented trial and failure of an abortive<br />
medication such as Fioricet, Fiorinal, Tylenol and NSAIDS<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart Notes<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
85
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INCRELEX<br />
FDA-APPROVED INDICATIONS<br />
Increlex® is indicated:<br />
A. For the long-term treatment of growth failure in children with severe primary<br />
IGF-1 deficiency (Primary IGFD) or with growth hormone (GH) gene deletion<br />
who have developed neutralizing antibodies to growth Hormone.<br />
COVERAGE POLICY<br />
Increlex® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified endocrinologist.<br />
B. AND the patient is between the age of 2 years old and 20 years old.<br />
C. AND the patient has no evidence of a closed epiphyses.<br />
D. AND the patient does NOT have any evidence of active malignancy.<br />
E. AND the patient is not being treated with chronic anti-inflammatory steroids.<br />
F. AND the diagnosis is documented as the treatment of growth failure in a child<br />
with severe primary IGF-1 deficiency or with growth hormone gene deletion who<br />
have developed neutralizing antibodies to growth hormone.<br />
G. AND the patient has a basal IGF-1 standard deviation score Less than or equal to<br />
-3 based on lab reference for age and sex. (Please verify the IGF-1 level in the<br />
patient’s chart notes and ensure the test was performed within 3 months of the<br />
initial request).<br />
H. AND the patient has a normal or elevated growth hormone level that has been<br />
confirmed with at least one growth hormone stimulation test. (Please verify the<br />
stimulation test result in the patient’s chart notes).<br />
I. AND the patient has severe growth retardation with a height standard deviation<br />
(SDS) score more than 3 SDS below the mean for chronological age and sex and<br />
their target height based on mid-parental height calculation. (Please verify the<br />
SDS score in the patient’s chart notes).<br />
J. AND all indications of secondary IGF-1 have been ruled out such as growth<br />
hormone deficiency, hypothyroidism and malnutrition.<br />
K. AND the patient is not taking or has no plans to receive growth hormone therapy<br />
in combination with Increlex® therapy. (Please review the patient’s drug history<br />
or drug chart to verify that the patient will not be receiving growth hormone<br />
therapy (e.g. Humatrope®, Genotropin®, Norditropin®, Serostim®, Nutropin®,<br />
Saizen®, Tev-Tropin®, Zorbtive®).<br />
L. AND if the patient has received previous mescasermin therapy, the patient must<br />
meet all of the following criteria:<br />
M. There has been an increase in height velocity Greater than 2.5 cm total growth in<br />
one year of therapy.<br />
N. There is no evidence of epiphyseal closure.<br />
O. The patient has NOT met their expected final adult height or targeted height based<br />
on mid-parental height calculation or their current absolute height is Less than or<br />
equal to 25 th percentile (defined as 68 inches in males and 63 inches in females.<br />
86
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INCRELEX<br />
(Continued)<br />
NON COVERAGE<br />
Increlex® is NOT covered for members with the following criteria:<br />
A. The prescribing physician is NOT a board certified endocrinologist.<br />
B. The patient is NOT between the age of 2 years old and 20 years old.<br />
C. The patient has evidence of a closed epiphyses.<br />
D. The patient has evidence of active malignancy.<br />
E. The patient is being treated with chronic anti-inflammatory steroids.<br />
F. The diagnosis is NOT documented as the treatment of growth failure in a<br />
child with severe primary IGF-1 deficiency or with growth hormone gene<br />
deletion who have developed neutralizing antibodies to growth hormone.<br />
G. If the diagnosis is documented as the treatment of growth failure in a child<br />
with severe primary IGF-1 deficiency or with growth hormone gene deletion<br />
who have developed neutralizing antibodies to growth hormone and the<br />
patient meets any of the following criteria:<br />
H. The patient has a basal IGF-1 standard deviation score Greater than -2.9 based<br />
on lab reference for age and sex.<br />
I. AND the patient has a low growth hormone level ([Max peak Less thanLess<br />
than 5ng/mL by RIA or Less than 2.5 ng/mL by IRMA]) that has been<br />
confirmed with at least one growth hormone stimulation test.<br />
J. The patient’s normal growth hormone level has not been confirmed by at least<br />
one growth hormone stimulation test.<br />
K. The patient does NOT have severe growth retardation.<br />
L. Indications of secondary IGF-1 have NOT been ruled out such as growth<br />
hormone deficiency, hypothyroidism and malnutrition.<br />
M. The patient is taking or has plans to receive growth hormone therapy in<br />
combination with Increlex® therapy.<br />
N. If the patient has received previous mescasermin therapy and the patient meets<br />
any of the following criteria:<br />
1. There has been an increase in height velocity Less than 2.5 cm total<br />
growth in one year of therapy.<br />
2. There is evidence of epiphyseal closure.<br />
3. The patient has met their expected final adult height or targeted height<br />
based on mid-parental<br />
height calculation or their current absolute height is Less than 25 th<br />
percentile (defined as 68 inches in males and 63 inches in females).<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
87
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INSPRA<br />
FDA-APPROVED INDICATIONS<br />
Inspra® is indicated:<br />
A. Improving survival of stable patients with left ventricular systolic dysfunction<br />
(LVEF Less than 40%) and CHF after an acute myocardial infarction.<br />
B. Hypertension, alone or combined with other agents.<br />
COVERAGE POLICY<br />
Inspra® is covered for members who meet the following criteria:<br />
A. The patient has had a serum potassium level taken within 10 days of initiation of<br />
therapy and the level is Less than 5.5 mEq/L.<br />
B. AND the patient is NOT receiving any potent CYP3A inhibitors that will affect<br />
the metabolism of Inspra®. (e.g. diltiazem, Cardizem®, Cartia XT®, Diltia<br />
XT®, Tiazac®, ketoconazole, verapamil, Calan®, Covera®, Verelan®, Isoptin®,<br />
vinblastine, doxorubicin, isoniazid, ritonavir, Norvir®, Kaletra®, cyclosporine,<br />
Viracept®, Crixivan®, Fortovase®, Invirase®, ciprofloxacin, Cipro®,<br />
itraconazole, Sporonax®, norfloxacin, voriconazole, Vfend®, rifampin, rifabutin).<br />
(Please verify that the patient is not receiving any of these medications by<br />
reviewing the patient’s drug history or chart).<br />
C. AND the diagnosis is documented as hypertension.<br />
D. AND the patient has tried and failed maximum tolerated doses of a 60-day trial or<br />
had unacceptable toxicity to spironolactone (Aldactone®, Spirono®). (Please<br />
review the patient’s drug history or chart to verify a trial to spironolactone).<br />
E. AND the patient does NOT have type-2 diabetes with microalbuminuria.<br />
F. AND the patient does NOT have a serum creatinine Greater than 2 mg/dL in<br />
males or Greater than 1.8 mg/dL in females.<br />
G. AND the patient does NOT have a creatinine clearance Less than or equal to 50<br />
mL/min.<br />
H. AND the patient is NOT or will be taking Inspra® in combination with potassium<br />
supplements or potassium sparing diuretics (e.g. amiloride, spironolactone or<br />
triamterene). (Please review the patient’s drug history or chart to verify no<br />
concomitant use with potassium supplements or potassium sparing diuretics).<br />
I. AND if the patient has had previous Inspra® therapy, he/she must show a<br />
decrease in systolic and diastolic blood pressure since initiating Inspra® therapy.<br />
J. AND/OR the diagnosis is documented as a patient with left ventricular systolic<br />
dysfunction and/or congestive heart failure after an acute myocardial infarction.<br />
K. AND the patient has tried and failed maximum tolerated doses of a 60-day trial or<br />
had unacceptable toxicity to spironolactone (e.g. Aldactone®, Spirono®). (Please<br />
review the patient’s drug history or chart to verify a trial to spironolactone).<br />
L. AND the patient does NOT have a creatinine clearance Less than or equal to 30<br />
mL/ min.<br />
M. AND if the patient has had previous Inspra® therapy, he/she must show an<br />
improvement in left ventricular systolic dysfunction and/or congestive heart<br />
failure symptoms (e.g. fatigue, edema, shortness of breath) since initiating<br />
Inspra® therapy.<br />
88
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INSPRA<br />
(Continued)<br />
NON COVERAGE<br />
Inspra® is NOT covered for members who meet the following criteria:<br />
A. The patient has NOT had a serum potassium level taken within 10 days of<br />
initiation of therapy.<br />
B. The patient has had a serum potassium level taken within 10 days of initiation of<br />
therapy and the level is Greater than 5.5 mEq/L.<br />
C. The patient is receiving a potent CYP3A inhibitors that will affect the metabolism<br />
of Inspra®.<br />
D. The diagnosis is NOT documented as hypertension, heart failure or left<br />
ventricular systolic dysfunction.<br />
E. The diagnosis is documented as hypertension and the patient meets any of the<br />
following criteria:<br />
F. The patient has NOT tried and failed maximum tolerated doses of at least a 60-<br />
day trial or had unacceptable toxicity to spironolactone (Aldactone®, Spirono®).<br />
G. The patient has type-2 diabetes with microalbuminuria.<br />
H. The patient has a serum creatinine Greater than 2 mg/dL in males or Greater than<br />
1.8 mg/dL in females.<br />
I. The patient has a creatinine clearance Less than or equal to 50 mL/min.<br />
J. The patient is or will be taking Inspra® in combination with potassium<br />
supplements or potassium sparing diuretics.<br />
K. If the patient has had previous Inspra® therapy and he/she has NOT shown a<br />
decrease in systolic and diastolic blood pressure since initiating Inspra® therapy.<br />
L. The diagnosis is documented as a patient with left ventricular systolic dysfunction<br />
and/or congestive heart failure after an acute myocardial infarction and the patient<br />
meets any of the following criteria:<br />
M. The patient has NOT tried and failed maximum tolerated doses of at least a 60-<br />
day trial or had unacceptable toxicity to spironolactone (e.g. Aldactone®,<br />
Spirono®).<br />
N. The patient has a creatinine clearance Less than or equal to 30 mL/ min.<br />
O. If the patient has had previous Inspra® therapy and he/she has NOT shown an<br />
improvement in left ventricular systolic dysfunction and/or congestive heart<br />
failure symptoms (e.g. fatigue, edema, shortness of breath) since initiating<br />
Inspra® therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Cardiologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
89
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INTRON A<br />
FDA-APPROVED INDICATIONS<br />
Intron® A is indicated:<br />
A. For the treatment of patients 18 years of age or older with hairy cell leukemia.<br />
B. For an adjuvant to surgical treatment in patients 18 years of age or older with<br />
malignant melanoma who are free of disease but at high risk for system<br />
recurrence, within 56 days of surgery.<br />
C. For the initial treatment of clinically aggressive follicular Non-Hodgkin’s<br />
Lymphoma in conjunction with anthracycline-containing combination<br />
chemotherapy in patients 18 years of age or older. (Efficacy in patients with lowgrade,<br />
low-tumor burden follicular Non-Hodgkin’s Lymphoma has not been<br />
demonstrated.)<br />
D. For intralesional treatment of selected patients 18 years of age or older with<br />
condylomata acuminate involving external surfaces of the genital and perianal<br />
areas.<br />
E. For the treatment of selected patients 18 years of age or older with AIDS-Related<br />
Kaposi’s Sarcoma.<br />
F. For the treatment of chronic hepatitis C in patients 18 years of age or older with<br />
compensated liver disease who have a history of blood or blood-product exposure<br />
and/or are HCV antibody positive.<br />
G. For the treatment of chronic hepatitis B in patients 1 years of age or older with<br />
compensated liver disease.<br />
COVERAGE POLICY<br />
Intron® A is covered for members who meet the following criteria:<br />
A. Patient has NO history of decompensated liver disease, autoimmune hepatitis or is<br />
an immunosuppressed transplant recipient.<br />
B. AND the patient does NOT have a history of a serious psychiatric condition or<br />
clinical depression.<br />
C. AND the patient has received an eye exam to screen and has NO evidence of an<br />
ophthalmologic disorder.<br />
D. AND the patient has a normal thyroid status or is maintained in the normal lab<br />
value range by medication.<br />
E. AND the patient has NO history of an autoimmune disease such as vasculitis,<br />
Raynaud’s phenomenon, rheumatoid arthritis, lupus erythematosus or<br />
rhabdomyolsis.<br />
F. AND the patient could NOT have undergone a liver transplant and therapy is<br />
being uses as a prophylaxis or treatment of established heptatis C to reduce<br />
allograft failure.<br />
G. AND the indication is documented as Hairy Cell Leukemia.<br />
a. AND the patient is 18 years of age or older.<br />
b. AND the prescribing physician is a board certified oncologist.<br />
c. AND approval can be allowed for up to 6 months.<br />
90
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INTRON A<br />
(Continued)<br />
d. AND if the patient has received previous therapy, the patient must meet<br />
previous criteria and experience a positive response to therapy that<br />
includes a delayed or no progression of disease.<br />
H. OR the indication is documented as Malignant Melonoma.<br />
a. AND the patient is 18 years of age or older.<br />
b. AND the prescribing physician is a board certified oncologist.<br />
c. AND the patient has received surgical treatment within 56 weeks of<br />
request.<br />
d. AND the patient is free of disease but at high risk for recurrence.<br />
e. AND approval can be allowed for up to 52 weeks.<br />
f. AND if the patient has received previous therapy, the patient must have<br />
had a recurrence of disease and surgical treatment within 56 weeks of<br />
request.<br />
I. OR the indication is documented as Follicular Non-Hodgkin’s Lymphoma.<br />
a. AND the patient is 18 years of age or older.<br />
b. AND the prescribing physician is a board certified oncologist.<br />
c. AND Intron® A therapy will be used in combination with an<br />
anthracycline-containing combination chemotherapy agent (eg.<br />
daunorubicin, doxorubicin, epirubicin, idarubicin, Cerubidine®,<br />
DaunoXome®, Adriamycin®, Rubex®, Doxil®, Evacet®, Ellence®,<br />
Idamycin®). (Please verify that the patient will be receiving<br />
anthracycline® therapy by reviewing the patient’s drug history or chart).<br />
d. AND the patient does not does not have low-grade, low-tumor burden<br />
disease (Efficacy has not been demonstrated).<br />
e. AND approval can be allowed for up to 1 year.<br />
f. AND if the patient has received previous therapy, the patient must have<br />
had treatment with an anthracycline-containing agent and meet the above<br />
criteria. Approval can be allowed for up to 1 year.<br />
J. OR the indication is documented as Condylomata Acuminata.<br />
a. AND the patient is 18 years of age or older.<br />
b. AND the prescribing physician is a board certified dermatologist or<br />
obtained a consult from the listed specialty.<br />
c. AND the area of involvement includes external surfaces of the genital<br />
and/or perianal area.<br />
d. AND the patient has tried, failed or intolerant to a 16 week course of<br />
Aldara® treatment.<br />
e. AND approval can be allowed for up to 3 weeks.<br />
f. AND if the patient has received previous therapy, the patient must initiate<br />
therapy on week 12 through 16 for an additional course of 3 weeks. The<br />
patient must also meet the same initial requirements and shown a positive<br />
benefit with the initial therapy defined as resolution or decrease in wart<br />
size.<br />
91
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INTRON A<br />
(Continued)<br />
K. OR the indication is documented as AIDS-Related Kaposi’s Sarcoma.<br />
a. AND the patient is 18 years of age or older.<br />
b. AND the prescribing physician is an infectious disease specialist or has<br />
obtained a consult from the listed specialty.<br />
c. AND approval can be allowed for up to one year.<br />
d. AND if the patient has received previous therapy, the patient must meet<br />
previous criteria and experience a positive response to therapy that<br />
includes a delay or NO disease progression. Approval can be allowed for<br />
up to one year.<br />
L. OR the indication is documented as Chronic Hepatitis C.<br />
a. AND the prescribing physician is a gastroenterologist or trained in<br />
infectious disease or has obtained a consult from the listed specialties.<br />
b. AND the diagnosis has been confirmed by a positive enzyme immunoassay<br />
(eg. EIA, ELISA).<br />
c. AND a HCV RNA quantitative assay has been performed to confirm<br />
active HCV replication.<br />
d. AND a biopsy has been performed showing that the patient has a fibrosis<br />
level of 1 through 4.<br />
e. AND the patient has had at least a 3 month trial and failure to Pegasys® or<br />
Peg-Intron®.<br />
f. AND the patient has had at least a 3 month trial and failure to ribavirin.<br />
g. AND therapy will be given in conjunction with ribivarin therapy.<br />
h. AND approval can be allowed for up to 16 weeks.<br />
i. AND if the patient has received previous 16 week therapy, the patient<br />
must meet previous criteria AND show a two-log drop in their HCV RNA<br />
level and a drop in AST and ALT lab values. If patient meets criteria,<br />
approval can be allowed up to a year with a lifetime maximum treatment<br />
of 24 months.<br />
M. OR the indication is documented as Chronic Hepatitis B.<br />
a. AND the prescribing physician is a gastroenterologist or trained in<br />
infectious disease or has obtained a consult from the listed specialties.<br />
b. AND the patient has evidence of a positive HBsAg (+ or -) serological<br />
marker for greater than 6 months OR evidence by a liver biopsy showing<br />
chronic hepatitis. (Please verify that the patient has an HBsAg serological<br />
marker for greater than 6 months or a positive liver biopsy by reviewing<br />
the patient’s drug history or chart).<br />
c. AND the patient has a Hepatitis B viral load greater than 100,000 copies<br />
per ml.<br />
d. AND the patient has elevations in liver aminotransferases (ALT or AST)<br />
that are two (2) times greater than normal.<br />
92
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INTRON A<br />
(Continued)<br />
e. AND if the patient is 12 years of age or older, they must have tried or<br />
failed at least a 6 month trial of Hepsera®, Baraclude® or Tyzeka®.<br />
Patients age 11 years or younger do not require a trial and failure.<br />
(Therapy can be verified by reviewing the patient’s chart as well as<br />
reviewing to see that there was no drop in viral load or reduction in liver<br />
aminotransferases.<br />
f. AND the patient is not receiving duplicate therapy that includes<br />
Baraclude®, Tyzeka®, Epivir®, Intron A® and/or Infergen®. (Please<br />
verify that the patient does not have duplicate therapy by reviewing the<br />
patient’s drug history or chart).<br />
g. AND approval can be allowed for up to one year.<br />
h. AND if the patient has received previous Intron® A treatment, there must<br />
be documented clinical improvement shown by a drop in viral load or<br />
reduction in the patient’s liver aminotransferases AND still the presence of<br />
a viral load for continued therapy. (Please verify patient’s chart notes to<br />
verify drop in viral load or reduction in liver aminotransferases from their<br />
starting level).<br />
N. OR the indication is documented as an indication listed in compendia.<br />
a. The prior authorization request should be reviewed by a prior<br />
authorization pharmacist. Pharmacist should review the drug study for:<br />
b. A study can be found.<br />
c. The study shows clinical improvement with treatment.<br />
d. If there are first line treatments, the patient has tried and failed.<br />
e. The patient meets the criteria of the study.<br />
f. The study has clinical validity (eg. blinded, substantial population).<br />
g. The study’s population meets the patient’s demographics.<br />
h. The patient’s disease status is not terminal and therapy will provide<br />
benefit.<br />
i. The patient will not receive duplicate therapy.<br />
j. <strong>Authorization</strong> period or re-treatment is within timeframe of study.<br />
NON COVERAGE<br />
Intron® A is NOT covered for members with the following criteria:<br />
A. Patient has a history of decompensated liver disease, autoimmune hepatitis or is<br />
an immunosuppressed transplant recipient.<br />
B. Patient has a history of a serious psychiatric condition or clinical depression.<br />
C. The patient has NOT received an eye exam and/or has evidence of an<br />
ophthalmologic disorder.<br />
D. The patient has an abnormal thyroid status that cannot be maintained by<br />
medication.<br />
E. The patient has a history of an autoimmune disease.<br />
93
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INTRON A<br />
(Continued)<br />
F. The patient has undergone a liver transplant and is using therapy as a prophylaxis<br />
or treatment to reduce allograft failure.<br />
G. The indication is Hairy Cell Leukemia and the patient is under the age of 18<br />
and/or<br />
a. The physician is NOT a board certified oncologist.<br />
b. If the patient has received a previous therapy and he/she shows<br />
progression of disease while on previous therapy.<br />
H. The indication is Malignant Melonoma and the patient is under the age of 18<br />
and/or:<br />
a. The physician is NOT a board certified oncologist.<br />
b. The patient has NOT received surgical treatment within 56 weeks of the<br />
request.<br />
c. The patient has evidence of disease.<br />
d. If the patient has received previous therapy and he/she shows NO positive<br />
response with previous treatment or has had NO surgical treatment within<br />
56 weeks of the request.<br />
I. The indication is Follicular Non-Hodgkin’s Lymphoma and the patient is under<br />
the age of 18 and/or: The physician is NOT a board certified oncologist.<br />
a. Therapy will NOT be used in combination with an anthracycline<br />
containing medication.<br />
b. The patient has low-grade, low-tumor burden.<br />
J. The indication is Condylomata Acuminata and the patient is under the age 18<br />
and/or:<br />
a. The physician is NOT a board certified dermatologist or obtained a<br />
consult.<br />
b. The area of involvement does NOT involve external surfaces of the genital<br />
and/or perianal area.<br />
c. The patient has NOT failed a 16 week course of Aldara® treatment.<br />
d. If the patient has received previous therapy and the request is not on week<br />
12 through 16 of treatment and/or has NOT shown a positive benefit.<br />
K. The indication is AIDS-Related Kaposi’s Sarcoma and the patient is under the age<br />
of 18 and/or:<br />
a. The physician is not an infectious disease specialist or obtained a consult.<br />
b. If the patient has had previous therapy and he/she does NOT show a delay<br />
in disease progression.<br />
L. The indication is Chronic Hepatitis C and the prescribing physician is NOT a<br />
gastroenterologist or trained in infectious disease or obtained a consult and/or:<br />
a. The diagnosis has NOT been confirmed by a positive enzyme immunoassay.<br />
b. No assay has been done to confirm active HCV replication.<br />
c. A biopsy has NOT been performed or does NOT show fibrosis.<br />
d. The patient has NOT had a trial and failure to Pegasys® or Peg-Intron®.<br />
94
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INTRON A<br />
(Continued)<br />
e. The patient has NOT had a trial and failure to ribivarin.<br />
f. If the patient has had previous therapy and he/she has NOT shown a twolog<br />
drop in their HCV RNA level and a drop in their AST and ALT lab<br />
values.<br />
g. The patient has had a lifetime therapy of 24 months.<br />
M. The indication is Chronic Hepatitis B and the prescribing physician is NOT a<br />
gastroenterologist or a trained Infectious disease specialist or obtained a consult<br />
and/or:<br />
a. The patient has NO evidence of an HBsAg serological marker for greater<br />
than 6 months or evidence of chronic hepatitis by liver biopsy.<br />
b. The patient does NOT have a viral load greater than 100,000 copies per<br />
ml.<br />
c. The patient does NOT have two times greater than normal liver<br />
aminotransferases.<br />
d. The patient is 12 years of age or older and has NOT had a 6 month trial<br />
and failure of Hepsera®, Baraclude® or Tyzeka®.<br />
e. The patient is receiving duplicate therapy with Hepsera®, Baraclude®,<br />
Epivir®, Infergen® or Tyzeka®.<br />
f. If the patient has had previous therapy and he/she has NOT shown a drop<br />
in viral load or reduction in their liver aminotransferases or NO presence<br />
of a viral load.<br />
N. The indication is listed as acute chronic hepatitis C. (Many individuals will clear<br />
their viral load with their own immune system).<br />
O. The indication is listed as a Compendia indication and no studies are found to<br />
validate efficacy and/or:<br />
a. The study shows NO clinical improvement with treatment.<br />
b. Patient has NOT tried first line therapy.<br />
c. The patient does NOT meet the criteria of the study.<br />
d. The study has NO clinical validity (eg. un-blinded, one patient).<br />
e. The study’s population does NOT meet the patient’s demographics.<br />
f. The patient’s disease status is terminal and therapy will provide no benefit.<br />
g. The patient is receiving duplicate therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Dermatologist, Oncologist, Infectious<br />
Disease<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
95
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INVEGA<br />
FDA-APPROVED INDICATIONS<br />
Invega® is indicated:<br />
A. For the acute and maintenance treatment of schizophrenia.<br />
COVERAGE POLICY<br />
Invega® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a psychiatrist or has obtained a consult from the<br />
listed specialty.<br />
B. AND the patient is 18 years of age or older.<br />
C. AND the diagnosis is NOT documented as dementia-related psychosis.<br />
D. AND the patient does NOT have congenital long QT syndrome or NO history of<br />
cardiac arrhythmias.<br />
E. AND the diagnosis is documented as schizophrenia.<br />
F. AND the patient has tried and failed (schizophrenia is unmanaged) a 30-day trial<br />
or had unacceptable toxicity to risperidone (Risperdal®) AND at least ONE of the<br />
following medications: Seroquel®, Zyprexa®, Geodon®, or Abilify®. (Please<br />
review the patient’s drug history or chart to verify a trial to risperidone and one<br />
other antipsychotic medication).<br />
G. AND Invega® therapy will NOT be used in combination with risperidone<br />
therapy. (Please review the patient’s drug history or chart to verify no<br />
combination use with risperidone (Risperdal®).<br />
H. AND if the patient has received previous Invega® therapy, the provider has seen<br />
clinical evidence demonstrating improvement in schizophrenia symptoms.<br />
NON COVERAGE<br />
Invega® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a psychiatrist or the prescriber has NOT<br />
obtained a consult from the listed specialty.<br />
B. The patient is under the age of 18 years old.<br />
C. The diagnosis is documented as dementia-related psychosis.<br />
D. The patient does have congenital long QT syndrome or has a history of cardiac<br />
arrhythmias.<br />
E. The diagnosis is NOT documented as schizophrenia.<br />
F. The patient has NOT tried and failed a 30-day trial or had unacceptable toxicity to<br />
risperidone (Risperdal®).<br />
G. The patient has NOT tried and failed a 30-day trial or had an unacceptable<br />
toxicity to at least ONE of the following medications: Seroquel®, Zyprexa®,<br />
Geodon®, or Abilify®.<br />
H. Invega® therapy will be used in combination with risperidone therapy.<br />
I. If the patient has received previous Invega® therapy and the provider has NOT<br />
seen any clinical evidence demonstrating improvement in schizophrenia<br />
symptoms.<br />
96
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INVEGA<br />
(Continued)<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Psychiatrist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
97
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ITRACONAZOLE<br />
FDA-APPROVED INDICATIONS<br />
Itraconazole is indicated:<br />
A. For Aspergillosis, histoplasmosis, blastomycosis, candidiasis, onychomycosis.<br />
COVERAGE POLICY<br />
Itraconazole is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as one of the above diagnoses.<br />
B. AND if diagnosis is aspergilosis the patient is intolerant of or refractory to<br />
amphotericin B therapy<br />
C. AND if the diagnosis is oropharyngeal candidiasis the patient is unresponsive or<br />
refractory to fluconazole therapy.<br />
D. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy, is on a form of contraception or has NO ability to<br />
conceive and has been educated on the potential dangers of Itraconazole therapy.<br />
NON COVERAGE<br />
Itraconazole is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as Aspergillosis, histoplasmosis,<br />
blastomycosis, candidiasis, onychomycosis.<br />
B. If the diagnosis is aspergillosis and the patient has NOT failed or is refractory to<br />
Amphotercin B therapy.<br />
C. If the diagnosis is onychomycosis due to dermatophytes (tinea unguium) and the<br />
patient IS NOT immunocompromised<br />
D. If the diagnosis is oropharyngeal and/or oral candidiasis and any formulation<br />
other than Itraconazole oral solution is requested.<br />
E. If the diagnosis is oropharyngeal candidiasis and the patient had NOT failed or is<br />
not refractory to fluconazole therapy.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
12 weeks<br />
98
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
IVEEGAM<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
B. Treatment of hypergammaglobulinemia<br />
C. AND the patient is diagnosed with primary immunodeficiency<br />
D. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
E. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency, OR<br />
Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
99
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
IXEMPRA<br />
FDA-APPROVED INDICATIONS<br />
Ixempra® is indicated:<br />
A. For the treatment of breast cancer in patients with metastatic or locally advanced<br />
breast cancer that is resistant or refractory to anthracyclines, taxanes, and<br />
capecitabine OR refractory to anthracyclines and taxanes when capecitabine is<br />
being used in combination.<br />
COVERAGE POLICY<br />
Ixempra® is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
B. Incident to a physician’s service<br />
C. AND the patient is diagnosed with metastatic or locally advanced breast cancer<br />
D. AND the patient has previous trial and failure on a taxane<br />
E. AND chart notes documenting previous failure to a taxane are received<br />
F. AND the patient has previous failure to anthracyclines or further therapy is<br />
contraindicated<br />
G. AND chart notes documenting failure or contraindication to anthracycline therapy<br />
are received<br />
H. AND treatment with Ixempra® follows 1 (ONE) of the following:<br />
I. Patient has previous trial and failure using capecitabine with chart notes<br />
documenting this failure are provided<br />
J. Patient will be using capecitabine in combination with Ixempra® and written<br />
medical summary is provided that shows dosing strategy<br />
NON COVERAGE<br />
Ixempra® is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT metastatic or locally advanced breast cancer<br />
C. The patient has NO previous treatment with anthracycline AND taxane<br />
D. Patient will NOT be receiving capecitabine in combination with Ixempra®<br />
treatment OR has not had previous failure on treatment with capecitabine<br />
E. Chart notes documenting previous failure or contraindication to anthracycline<br />
treatment, taxane trial and failure, and capecitabine failure or dosing strategy<br />
along with Ixempra® treatment are not received or do not address the needed<br />
information<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
100
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
KEPPRA XR<br />
FDA-APPROVED INDICATIONS<br />
Keppra XR® is indicated:<br />
A. For treatment of myoclonic seizures<br />
B. For treatment of partial seizures<br />
C. For treatment of tonic-clonic seizures<br />
COVERAGE POLICY<br />
Keppra XR® is covered for members who meet the following criteria:<br />
A. Patient must have previous trial/failure of generic Levetiracetam<br />
NON COVERAGE<br />
Keppra XR® is NOT covered for members with the following criteria:<br />
A. Diagnosis is NOT myoclonic, partial, or tonic-clonic seizures<br />
B. Patient has no previous trial/failure of generic Levetiracetam.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes per Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
101
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
KETEK<br />
FDA-APPROVED INDICATIONS<br />
Ketek® is indicated:<br />
A. For the treatment of community-acquired pneumonia*Ketek is no longer<br />
indicated for the treatment of sinusitis or bronchitis per FDA warning letter issued<br />
2/12/2007<br />
COVERAGE POLICY<br />
Ketek® is covered for members who meet the following criteria:<br />
A. The patient is diagnosed with community-acquired pneumonia<br />
B. AND the patient has had previous failed therapy on BOTH of the following:<br />
C. Azithromycin<br />
D. A fluoroquinolone<br />
E. AND chart notes are submitted that document failure on BOTH azithromycin<br />
AND a fluoroquinolone (including length of therapy of both agents)<br />
NON COVERAGE<br />
Ketek® is NOT covered for members who meet the following criteria:<br />
A. The diagnosis is NOT community-acquired pneumonia<br />
B. The patient has NO previous treatment with azithromycin AND a fluoroquinolone<br />
C. Chart notes documenting previous failure or contraindication to azithromycin<br />
AND a fluoroquinolone are not received or do not address the needed information<br />
D. The patient has previously shown macrolide hypersensitivity<br />
E. The patient has pre-existing QT prolongation or torsades de pointes<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
10 days<br />
102
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
KINERET<br />
FDA-APPROVED INDICATIONS<br />
Kineret® is indicated:<br />
A. For reducing the signs and symptoms and slowing the progression of structural<br />
damage of moderately to severely active rheumatoid arthritis in patients who have<br />
failed other therapies.<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Kineret® is covered for members who meet the following criteria:<br />
A. Verification of B vs. D coverage per CMS guidelines<br />
a. Incident to a physician’s service<br />
B. AND the patient must have a minimum of 4 of the following symptoms in<br />
accordance with American College of Rheumatology:<br />
a. Morning stiffness<br />
b. Arthritis of 3 or more joint areas<br />
c. Arthritis of hand joints<br />
d. Symmetric arthritis<br />
e. Rheumatoid nodules<br />
f. Serum rheumatoid factor<br />
g. Radiographic changes<br />
C. AND the patient must have previous trial and failure or contraindication on ALL<br />
of the following:<br />
a. 1 DMARD (Sulfasalazine, Hydroxychloroquine, Cyclosporine,<br />
oral/injectable Gold, Penicillamine, Azathioprine, Leflunomide,<br />
Methotrexate)<br />
b. Humira®<br />
D. AND chart notes documenting previous trial/failure of 1 DMARD AND Humira®<br />
NON COVERAGE<br />
Kineret® is NOT covered for members who meet the following criteria:<br />
A. Medication is paid for by Part B per CMS guidelines<br />
B. The diagnosis is NOT rheumatoid arthritis<br />
C. The patient has NO previous treatment with The patient has no previous<br />
trial/failure of at least 1 DMARD AND Humira®<br />
D. Chart notes documenting patient’s previous trials and failures are not provided or<br />
do not address the needed information.<br />
i. Route of administration is IM or IV<br />
ii. Patient is currently immunosuppressed or has current infection<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as per Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Rheumatologist and Neurologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
103
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LAMISIL AT TOPICAL SPRAY 1%<br />
FDA-APPROVED INDICATIONS<br />
Lamisil AT Topical Spray 1%® is indicated:<br />
A. For the treatment of tinea infections due to susceptible organisms Interdigital<br />
tinea pedis (athlete’s foot), tinea cruris (jock itch), or tinea corporis (ringworm).<br />
COVERAGE POLICY<br />
Lamisil AT Topical Spray 1%® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as interdigital tinea pedis (athlete’s foot), tinea cruris<br />
(jock itch), or tinea corporis (ringworm).<br />
B. Patient has completed a documented 4 week trail and failure of generic terbinafine<br />
cream.<br />
NON COVERAGE<br />
Lamisil AT Topical Spray 1%® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as interdigital tinea pedis (athlete’s<br />
foot), tinea cruris (jock itch), or tinea corporis (ringworm).<br />
B. The patient has not completed a documented 4 week trial and error of<br />
generic terbinafine cream.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
104
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LETAIRIS<br />
FDA-APPROVED INDICATIONS<br />
Letairis® is indicated:<br />
A. For the treatment of pulmonary hypertension in patients with WHO Class II or III<br />
symptoms, to improve exercise capacity and to delay clinical worsening.<br />
COVERAGE POLICY<br />
Letairis® is covered for members who meet the following criteria:<br />
A. The providing prescriber is a board certified pulmonologist or cardiologist.<br />
B. Diagnosis is documented as pulmonary hypertension in patients with WHO Class<br />
II or III symptoms.<br />
C. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy, is on a form of contraception or has NO ability to<br />
conceive and has been educated on the potential dangers of Letairis® therapy.<br />
D. PAH is not associated with portal hypertension, sickle cell disease, or<br />
thromboembolic disease.<br />
E. Baseline liver aminotranferases are less than 3X ULN.<br />
F. Mean PAP is greater than or equal to 25mm Hg at rest.<br />
G. Documented trial and failure of treatment with a calcium channel blocker.<br />
NON COVERAGE<br />
Letairis® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as pulmonary hypertension in patients with<br />
WHO Class II or III symptoms<br />
B. Diagnosis has NOT been confirmed by a board certified pulmonologist or<br />
cardiologist.<br />
C. The patient is female and of childbearing years, she is pregnant, has plans for<br />
pregnancy, is not on a form of contraception or has the ability to conceive.<br />
D. The patient has PAH associated with portal hypertension, sickle cell disease, or<br />
thromboembolic disease.<br />
E. Baseline liver aminotranferases are greater than 3X ULN.<br />
F. Mean PAP is less than 25mm Hg at rest.<br />
G. No documented trial and failure of treatment with a calcium channel blocker.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Pulmonologist and Cardiologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
105
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LEUCOVORIN<br />
FDA-APPROVED INDICATIONS<br />
Leucovorin is indicated:<br />
A. For the treatment of florouracil therapy, macrocytic anemia, megaloblastic<br />
anemia, MTX toxicity prophylaxis, pyrimethamine toxicity/prophylaxis,<br />
trimethoprim toxicity/prophylaxis, trimetrexate toxicity/prophylaxis<br />
COVERAGE POLICY<br />
Leucovorin is covered for members who meet the following criteria:<br />
A. Patient is prescribed Leucovorin for an indicated diagnosis as illustrated above<br />
B. AND patient does not suffer from pernicious anemia<br />
C. AND B vs. D criteria determines that the medications should be covered by<br />
Medicare Part D<br />
NON COVERAGE<br />
Leucovorin is NOT covered for members who meet the following criteria:<br />
A. Non approved indications<br />
B. Patients that have pernicious anemia<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
106
FDA-APPROVED INDICATIONS<br />
Cladribine is indicated:<br />
A. Hairy Cell Leukemia<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LEUSTATIN<br />
COVERAGE POLICY<br />
Cladribine is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with Hairy Cell Leukemia<br />
B. AND is being diagnosed by an Oncologist<br />
C. AND the medication meets B vs. D determination criteria that authorized<br />
coverage to Medicare Part D<br />
NON COVERAGE<br />
Cladribine is NOT covered for members with the following criteria:<br />
A. Non FDA approved indications<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
107
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LIDODERM<br />
FDA-APPROVED INDICATIONS<br />
Lidoderm® is indicated:<br />
A. For treatment of postherpetic neuralgia<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Lidoderm® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as postherpetic neuralgia<br />
B. Patient has completed a documented 1 month trial and failure of two of the<br />
following:<br />
a. Opiate analgesics<br />
b. Gabapentin<br />
c. Tricyclic antidepressants (amitriptyline, nortriptyline or desipramine)<br />
d. Topical capsaicin<br />
NON COVERAGE<br />
Lidoderm® is NOT covered for members who meet the following criteria:<br />
A. Diagnosis is NOT documented as postherpetic neuralgia<br />
B. Patient has NOT completed a documented 1 month trial and failure of two of the<br />
following:<br />
a. Opiate analgesics<br />
b. Gabapentin<br />
c. Tricyclic antidepressants (amitriptyline, nortriptyline or desipramine)<br />
d. Topical capsaicin.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
3 months<br />
108
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LOVAZA<br />
FDA-APPROVED INDICATIONS<br />
Lovaza® is indicated:<br />
A. As an adjunct to diet to reduce triglyceride levels in adult patients with very<br />
high (Greater than or equal to 500 mg/dL) triglyceride levels.<br />
COVERAGE POLICY<br />
Lovaza® is covered for members who meet the following criteria:<br />
A. The patient is 18 years of age or older.<br />
B. AND the patient has a triglyceride level of 500 mg/dL or greater. (Please review<br />
the patient’s chart to verify their triglyceride level).<br />
C. AND the patient has tried and failed or is intolerant to at least a 60-day drug<br />
regimen to two of the following drug classes (Please review the patient’s drug<br />
history or chart to verify the use of each drug class):<br />
a. Niacin (e.g. Niaspan®, Niacor®, niacin).<br />
b. Fenofibrate (e.g. Tricor®, Triglide®, Lofibra®, Antara®, fenofibrate).<br />
c. Gemfibrozil (e.g. gemfibrozil, Lopid®). does NOT have gastroparesis.<br />
D. AND if the patient has had previous Lovaza® therapy, he/she must show a<br />
reduction in their triglyceride level since initiating Lovaza® therapy.<br />
NON COVERAGE<br />
Lovaza® is NOT covered for members who meet the following criteria:<br />
A. The patient is under the age of 18 years old.<br />
B. The patient has a triglyceride level less than 500 mg/dL.<br />
C. The patient has NOT tried and failed or is intolerable to at least a 60-day drug<br />
regimen to two of the following drug classes:<br />
a. Niacin (e.g. Niaspan®, Niacor®, niacin).<br />
b. Fenofibrate (e.g. Tricor®, Triglide®, Lofibra®, Antara®, fenofibrate).<br />
c. Gemfibrozil (e.g. gemfibrozil, Lopid).<br />
D. If the patient has had previous Lovaza® therapy and he/she has not shown a<br />
reduction in their triglyceride level since initiating Lovaza® therapy.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
109
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
LUPRON DEPOT<br />
FDA-APPROVED INDICATIONS<br />
Lupron® is indicated:<br />
A. For the palliative treatment of advanced prostate cancer, particularly when<br />
orchiectomy or estrogen therapy are not indicated or are unacceptable<br />
B. For the management of endometriosis including pain relief and reduction of<br />
endometriotic lesions<br />
C. For the treatment of central precocious puberty (idiopathic or neurogenic) in<br />
children less than 8 or 9 years old<br />
D. For the preoperative treatment of anemia due to uterine leiomyomata (fibroids) in<br />
combination with iron supplementation when iron therapy alone fails to correct<br />
the anemia<br />
COVERAGE POLICY<br />
Lupron® is covered for members who meet the following criteria:<br />
A. The documented diagnosis is one of the FDA approved indications listed above.<br />
B. If the diagnosis is advanced prostate cancer, orchiectomy or estrogen therapy are<br />
documented as unacceptable.<br />
C. If the diagnosis is endometriosis the patient has completed documented trial and<br />
failures of at least two of the following: oral contraceptives,<br />
medroxyprogesterone, and Danazol<br />
D. If the diagnosis is precocious puberty, patient must be less than 9 years old<br />
E. AND verification of all B vs. D criteria indicate coverage by Part D<br />
NON COVERAGE<br />
Lupron® is NOT covered for members with the following criteria:<br />
A. If there is not a documented diagnosis as listed under the FDA-approved<br />
indications above.<br />
B. If the diagnosis is advanced prostate cancer, orchiectomy or estrogen therapy are<br />
not indicated for are unacceptable.<br />
C. If the diagnosis is endometriosis, the patient has NOT completed a documented<br />
trial and failure of at least two of the following: oral contraceptives,<br />
medroxyprogesterone, and Danazol.<br />
D. If the diagnosis is precocious puberty, the patient is NOT less than 9 years old at<br />
beginning of treatment. Treatment should be discontinued before age 11 for<br />
females and age 12 for males.<br />
E. If the patient is female and she is pregnant, has plans for pregnancy or has NOT<br />
been educated on the potential dangers of Lupron® therapy in pregnancy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
OBGYN and Oncologist and<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
3 months<br />
110
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MARINOL<br />
FDA-APPROVED INDICATIONS<br />
Marinol® is indicated:<br />
A. For the treatment of anorexia associated with weight loss in patients with AIDS.<br />
B. For the treatment of nausea and vomiting associated with cancer chemotherapy in<br />
patients who have failed to respond adequately to conventional antiemetic<br />
treatments.<br />
C. All other FDA approved indications not otherwise excluded from Part D.<br />
COVERAGE POLICY<br />
Marinol® is covered for members who meet the following criteria:<br />
A. The diagnosis is documented as anorexia associated with weight loss in a patient<br />
with AIDS.<br />
a. AND the patient has had an involuntary weight loss of Greater than 10%<br />
of pre-illness baseline body weight or body mass index (BMI) Less than<br />
20 kg/m 2 in the absence of a concurrent illness or medical condition other<br />
than HIV infection that may cause weight loss.<br />
b. AND the patient has failed to respond to a 30-day drug regimen of<br />
megestrol (Megace®) AND an anabolic steroid (e.g. Testim®,<br />
Androgel®, testosterone enanthate, testosterone cypionate, Testoderm®,<br />
Androderm®, methyltestosterone, or fluoxymesterone). (Please verify the<br />
use of megestrol and an anabolic steroid by reviewing the patient’s drug<br />
history or chart).<br />
c. AND if the patient has received previous Marinol® therapy, he/she must<br />
show a positive response to treatment by maintaining or increasing their<br />
initial weight and/or muscle mass before initiating Marinol® therapy.<br />
B. The diagnosis is documented as nausea and vomiting associated with cancer<br />
chemotherapy in a cancer patient.<br />
a. AND the patient is receiving a chemotherapy or radiation regimen.<br />
(Please verify in the patient’s chart notes).<br />
b. AND if Marinol® therapy is NOT being used as a full therapeutic<br />
replacement for an intravenous anti-emetic drug (e.g., Aloxi®, Zofran®).<br />
If Marinol® is used as a full replacement of IV antiemetic administration<br />
and the treatment is or will be within 48 hours of cancer treatment,<br />
Medicare Part B will pay for the therapy. Please verify with the provider).<br />
c. AND if Marinol® therapy is being used as a full therapeutic replacement<br />
for an intravenous anti-emetic drug (e.g., Aloxi®, Zofran® BUT<br />
Marinol® treatment will NOT be within 48 hours of cancer treatment. (If<br />
Marinol® is used as a full replacement of IV antiemetic administration<br />
and the treatment is or will be within 48 hours of cancer treatment,<br />
Medicare Part B will pay for the therapy. (Please verify with the provider).<br />
111
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MARINOL<br />
(Continued)<br />
d. AND the patient has had a full trial and failure through at least one cycle<br />
of chemotherapy with IV Zofran® AND at least two of the following oral<br />
anti-emetic agents:<br />
i. metoclopramide.<br />
ii. promethazine.<br />
iii. prochlorperazine.<br />
iv. dimenhydrinate.<br />
v. meclizine.<br />
vi. trimethobenzamide.<br />
vii. Oral 5-HT3 receptor Antagonist (e.g., Anzemet®, Zofran®,<br />
Kytril®, Zomig®).<br />
e. AND if the patient has received previous Marinol® therapy, he/she must<br />
show a positive response by showing a reduced incidence of emesis and/or<br />
nausea.<br />
NON COVERAGE<br />
Marinol® is NOT covered for members with the following criteria:<br />
A. The diagnosis is not documented as anorexia associated with weight loss in a<br />
patient with AIDS or nausea and vomiting associated with cancer chemotherapy<br />
in a cancer patient.<br />
B. The diagnosis is documented as anorexia associated with weight loss in a patient<br />
with AIDS and the patient meets any of the following criteria.<br />
a. The patient has NOT had an involuntary weight loss of Greater than 10%<br />
of pre-illness baseline body weight or body mass index (BMI) Less than<br />
20 kg/m 2 in the absence of a concurrent illness or medical condition other<br />
than HIV infection that may cause weight loss.<br />
b. The patient has NOT failed to respond to a 30-day drug regimen of<br />
megestrol (Megace®) AND an anabolic steroid (e.g. Testim®,<br />
Androgel®, testosterone enanthate, testosterone cypionate, Testoderm®,<br />
Androderm®, methyltestosterone, or fluoxymesterone).<br />
c. If the patient has received previous Marinol® therapy and he/she has NOT<br />
shown a positive response to treatment by maintaining or increasing their<br />
initial weight and/or muscle mass before initiating Marinol® therapy.<br />
C. The diagnosis is documented as nausea and vomiting associated with cancer<br />
chemotherapy in a cancer patient.<br />
a. The patient is NOT receiving a chemotherapy or radiation regimen.<br />
b. Marinol® therapy is being used as a full therapeutic replacement for an<br />
intravenous anti-emetic drug (e.g., Aloxi®, Zofran®) and treatment is or<br />
will be within 48 hours of cancer treatment.<br />
112
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MARINOL<br />
(Continued)<br />
c. The patient has NOT had a full trial and failure through at least one cycle<br />
of chemotherapy with IV Zofran® AND at least two of the following oral<br />
anti-emetic agents:<br />
i. metoclopramide.<br />
ii. promethazine.<br />
iii. prochlorperazine.<br />
iv. dimenhydrinate.<br />
v. meclizine.<br />
vi. trimethobenzamide.<br />
vii. Oral 5-HT3 receptor Antagonist (e.g., Anzemet®, Zofran®,<br />
Kytril®, Zomig®).<br />
d. If the patient has received previous Marinol® therapy and he/she has not<br />
shown a positive response by showing a reduced incidence of emesis<br />
and/or nausea.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
6 months<br />
113
FDA-APPROVED INDICATIONS<br />
Mesnex® is indicated:<br />
A. Hemorrhagic Cystitis<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MESNEX<br />
COVERAGE POLICY<br />
Mesnex® is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with approved indication as stated above<br />
B. AND patient is being administered with ifosfamide or cyclophosphamide<br />
C. AND B vs. D criteria indicates that coverage should be through Medicare Part D<br />
NON COVERAGE<br />
Mesnex® is NOT covered for members with the following criteria:<br />
A. Receiving medications other than ifosfamide or cyclophosphamide.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
3 months<br />
114
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MIACALCIN This PA criteria is for the injection only<br />
FDA-APPROVED INDICATIONS<br />
Miacalcin® is indicated:<br />
A. Hypercalcemia<br />
B. Osteoporosis<br />
C. Paget’s Disease<br />
COVERAGE POLICY<br />
Miacalcin® is covered for members who meet the following criteria:<br />
A. Injection for Hypercalcemia and Paget’s Disease:<br />
a. Patient is diagnosed with approved indication as stated above<br />
b. AND B vs. D criteria indicates that coverage should be through Medicare<br />
Part D<br />
B. Injection for Osteoporosis:<br />
a. Patient can not use Nasal Miacalcin<br />
b. AND has diagnosis of Osteoporosis indicated by a T-Score of 2.5 or more<br />
standard deviations below the young-adult mean BMD.<br />
NON COVERAGE<br />
Miacalcin® is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
115
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MYFORTIC<br />
FDA-APPROVED INDICATIONS<br />
Myfortic® is indicated:<br />
A. For the prophylaxis of organ rejection in patients receiving allogeneic renal<br />
transplants, administered in combination with cyclosporine and corticosteroids.<br />
COVERAGE POLICY<br />
Myfortic® is covered for members who meet the following criteria:<br />
A. If the patient is female and of childbearing years, she is NOT pregnant, has NO<br />
plans for pregnancy and has been educated on the potential dangers of Myfortic®<br />
therapy.<br />
B. AND diagnosis is documented as the prophylaxis of organ rejection in a patient<br />
receiving or received an organ transplant.<br />
C. AND the transplant was NOT covered by Medicare Part A. (Please verify the<br />
payer of the transplant. If Medicare paid for the transplant, Myfortic® is covered<br />
by Medicare Part B).<br />
D. AND approval can be allowed for up to one year.<br />
NON COVERAGE<br />
Myfortic® is NOT covered for members with the following criteria:<br />
A. The patient is female and of childbearing years and is pregnant or has plans for<br />
pregnancy.<br />
B. The diagnosis is NOT documented as prophylaxis of organ rejection after<br />
receiving an organ transplant or a compendia listed indication.<br />
C. The transplant was paid for by Medicare Part A.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
116
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
MYOZYME<br />
FDA-APPROVED INDICATIONS<br />
Myozyme® is indicated:<br />
A. For use in patients with Pompe disease (alpha glucosidase deficiency).<br />
Myozyme® has been shown to improve ventilator-free survival in patients with<br />
infantile-onset Pompe disease. Use of Myozyme® in patients with other forms of<br />
Pompe disease has not been adequately studied to assure safety and efficacy.<br />
COVERAGE POLICY<br />
Myozyme® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as infantile-onset Pompe disease (glycogen storage<br />
disease type II, GSD II, glycogenosis type II, acid maltase deficiency disease).<br />
B. AND diagnosis has been confirmed by an enzymatic assay showing a deficiency<br />
in acid alpha glucosidase.<br />
C. AND the patient is NOT receiving treatment at home. (Myozyme® therapy<br />
would be paid by Medicare Part B).<br />
D. AND/OR if the patient is in a hospital or long term care facility (LTC) or skilled<br />
nursing facility (SNF) and the payer of the stay is NOT Medicare Part A.<br />
(Medicare Part A can pay for the first 110 days and Myozyme® therapy would be<br />
paid by Medicare Part B. (Please verify payer).<br />
E. AND the medication is NOT being administered using an IMPLANTABLE<br />
F. PUMP. (Please verify the delivery method of the medication. Administration<br />
through an implantable pump is covered under Medicare Part B.)<br />
G. AND approval can be allowed for up to one year.<br />
NON COVERAGE<br />
Myozyme® is NOT covered for members who meet the following criteria:<br />
A. Diagnosis is NOT documented as infantile-onset Pompe disease (glycogen<br />
storage disease type II, GSD II, glycogenosis type II, acid maltase deficiency<br />
disease).<br />
B. Diagnosis is documented as late-onset Pompe disease.<br />
C. Diagnosis has NOT been confirmed by an enzymatic assay showing a deficiency<br />
in acid alpha glucosidase.<br />
D. The patient is receiving treatment at home. (Myozyme® therapy would be paid<br />
by Medicare Part B).<br />
E. The patient is in a hospital or long term care facility (LTC) or skilled nursing<br />
facility (SNF) and the payer of the stay is Medicare Part A. (Medicare Part B<br />
would pay for Myozyme® therapy).<br />
F. The patient is in a hospital or LTC or SNF and the medication is being<br />
administered using an IMPLANTABLE PUMP. (Administration through an<br />
implantable pump is covered under Medicare Part B.)<br />
REQUIRED MEDCIAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinology<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
117
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NAGALZYME<br />
FDA-APPROVED INDICATIONS<br />
Naglazyme® is indicated:<br />
A. For patients with Mucopolysaccharidosis VI (MPS VI).<br />
COVERAGE POLICY<br />
Naglazyme® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as mucopolysaccharidosis VI (MPS VI).<br />
B. AND diagnosis has been confirmed by an enzymatic assay showing a deficiency<br />
in N-acetylgalactosamine activity.<br />
C. AND the patient has at least one of the listed MPS VI symptoms.<br />
Impaired vision Recurrent otitis media. Recurrent<br />
sinopulmonary<br />
infections<br />
Impaired hearing Upper airway obstruction Malaise and reduced<br />
endurance<br />
Corneal clouding Macrocephaly Reduced joint range<br />
of motion<br />
Progressively<br />
coarse facial<br />
features<br />
Carpal tunnel<br />
syndrome<br />
Cardiac<br />
abnormalities and<br />
valvular disease<br />
Reduced<br />
pulmonary<br />
function<br />
Short stature<br />
Communicating<br />
hydrocephalus<br />
Spinal cord compression<br />
Hepatospenomegaly<br />
Umbilical and<br />
inguinal hernias<br />
Hepatosplenomegaly<br />
Sleep apnea<br />
Dysostosis mutiplex<br />
D. AND if the patient has previously received Naglazyme® therapy, they must show<br />
an improvement in walking and/or stair-climbing capacity since initiating therapy.<br />
NON COVERAGE<br />
E. Naglazyme® is NOT covered for members with the following criteria:<br />
F. The diagnosis is NOT documented as mucopolysaccharidosis VI (MPS VI).<br />
G. Diagnosis has NOT been confirmed by enzymatic assay that shows a deficiency<br />
in N-acetylgalactosamine activity.<br />
H. The patient does NOT have at least one of the listed symptoms of MPS VI.<br />
I. If the patient has previously received Naglazyme® therapy and they have not<br />
shown an improvement in walking or stair-climbing capacity.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
118
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NEURONTIN SOLUTION<br />
FDA-APPROVED INDICATIONS<br />
Neurontin® is indicated:<br />
A. For the symptomatic treatment of neuropathic pain associated with post-herpetic<br />
neuralgia and diabetic peripheral neuropathy<br />
B. For the adjunctive treatment of partial seizures with or without secondary<br />
generalized tonic-clonic seizures<br />
DOSE<br />
The recommended dose of Neurontin® is:<br />
A. Initially 300 mg PO three times per day. Can increase up to 3600 mg/day.<br />
COVERAGE POLICY<br />
Neurontin® is covered for members who meet the following criteria:<br />
A. The patient is diagnosed with either neuropathic pain OR partial seizures<br />
B. AND the patient has previous trial/failure with maximum doses of oral gabapentin<br />
capsules/tablets<br />
C. AND chart notes are received documenting trial of gabapentin capsules/tablets<br />
NON COVERAGE<br />
Neurontin® is NOT covered for members who meet the following criteria:<br />
A. The diagnosis is NOT neuropathic pain OR partial seizures<br />
B. The patient has NO previous treatment with maximum doses of gabapentin<br />
capsules/tablets<br />
C. Chart notes documenting previous failure or contraindication to gabapentin<br />
capsules/tablets are not received or do not address the needed information<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
119
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NEUTREXIN<br />
FDA-APPROVED INDICATIONS<br />
Neutrexin® is indicated:<br />
A. For the treatment of moderate-to-severe pneumocystis pneumonia (PCP) in<br />
immunocompromised patients<br />
COVERAGE POLICY<br />
Neutrexin® is covered for members who meet the following criteria:<br />
A. Verification of B vs. D criteria per CMS guidelines<br />
B. Incident to a physician’s service<br />
C. AND the patient is diagnosed with moderate to severe pneumocystis pneumonia<br />
(PCP)<br />
D. AND the patient is immunocompromised (including HIV and oncology patients)<br />
E. AND the patient has previous trial/failure or contraindication to<br />
sulfamethoxazole/trimethoprim AND pentamidine<br />
F. AND the patient is concurrently taking leucovorin with treatment<br />
G. AND chart notes are received that document patient’s immune status as well as<br />
previous trial and failure or contraindication to sulfamethoxazole/trimethoprim<br />
AND pentamidine<br />
NON COVERAGE<br />
Neutrexin® is NOT covered for members who meet the following criteria:<br />
A. Medication is paid for by Part B<br />
B. The diagnosis is NOT pneumocystis pneumonia<br />
C. The patient is NOT immunocompromised<br />
D. The patient has NO previous trials with sulfamethoxazole/trimethoprim AND<br />
pentamidine<br />
E. The patient is NOT taking leucovorin with treatment<br />
F. Chart notes documenting previous failure or contraindication to<br />
sulfamethoxazole/trimethoprim AND pentamidine are not received or do not<br />
address the needed information<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Infectious Disease<br />
AUTHORIZATION PERIOD<br />
21 days<br />
120
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NEXAVAR<br />
FDA-APPROVED INDICATIONS<br />
Nexavar® is indicated:<br />
A. For the treatment of unresectable hepatocellular carcinoma.<br />
B. For the treatment of advanced renal cell carcinoma.<br />
COVERAGE POLICY<br />
Nexavar® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified oncologist or nephrologist.<br />
B. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy and has been educated on the potential dangers of<br />
Nexavar® therapy in pregnancy.<br />
C. AND the patient will NOT be treated with interferon alfa (Roferon-A®,<br />
Pegasys®, Intron-A®, Peg-Intron®) or interleukin-2 (Proleukin®) therapy in<br />
combination with Nexavar® treatment. (Please verify the patient’s drug history or<br />
patient chart to verify that the patient is not on interferon alfa or interleukin-2<br />
therapy).<br />
D. AND the diagnosis is documented as treatment for hepatocellular carcinoma.<br />
a. AND the carcinoma is surgically unresectable.<br />
b. AND if the patient has received previous Nexavar® therapy, he/she has<br />
evidence of clinical improvement from the pretreatment report and or the<br />
patient has stable disease (tumor size within 25% of baseline).<br />
E. AND/OR the diagnosis is documented as metastatic (advanced) renal cell<br />
carcinoma.<br />
a. AND the carcinoma is surgically unresectable.<br />
b. AND if the patient has had previous Nexavar® therapy, he/she has<br />
evidence of clinical improvement from the pretreatment report and or the<br />
patient has stable disease (tumor size within 25% of baseline).<br />
NON COVERAGE<br />
Nexavar® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a board certified oncologist or nephrologist.<br />
B. If the patient is female and she is pregnant, has plans for pregnancy or has NOT<br />
been educated on the potential dangers of Nexavar® therapy in pregnancy.<br />
C. The patient will be receiving interferon alfa or Proleukin® therapy in combination<br />
with Nexavar® treatment.<br />
D. The diagnosis is NOT documented as treatment for hepatocellular or renal cell<br />
carcinoma.<br />
E. The diagnosis is documented as treatment for hepatocellular carcinoma and they<br />
meet any of the following criteria.<br />
a. The carcinoma is resectable.<br />
b. If the patient has received previous Nexavar® therapy and he/she has<br />
evidence of tumor growth greater than 25% of the baseline tumor size.<br />
121
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NEXAVAR<br />
(Continued)<br />
F. The diagnosis is documented as renal cell carcinoma and they meet any of the<br />
following criteria:<br />
a. The carcinoma is not metastatic.<br />
b. The carcinoma can be surgically resectable.<br />
c. If the patient has had previous Nexavar® therapy and he/she has evidence<br />
of tumor growth greater than 25% of the baseline tumor size.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
122
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NICOTROL<br />
FDA-APPROVED INDICATIONS<br />
Nicotrol® is indicated:<br />
A. For use as an aid in the treatment of nicotine withdrawal following cessation of<br />
smoking<br />
DOSE<br />
The recommended dose of Nicotrol® is:<br />
A. Nasal spray: 1 spray into each nostril 1-2 times each hour as needed whenever the<br />
patient feels the need to smoke. Recommended duration is three months.<br />
B. Inhaler: 24 to 64 mg (6 to 16 cartridges) per day for up to 12 weeks.<br />
COVERAGE POLICY<br />
Nicotrol® is covered for members who meet the following criteria:<br />
A. The patient is diagnosed with nicotine addiction or withdrawal following<br />
cessation of smoking<br />
B. AND the patient has stopped smoking previous to receiving medication<br />
C. AND the patient is enrolled in a smoking cessation program<br />
D. AND documentation verifying enrollment in a smoking cessation program is<br />
provided<br />
E. AND the request is for 3 months or less<br />
NON COVERAGE<br />
Nicotrol® is NOT covered for members who meet the following criteria:<br />
A. The diagnosis is NOT withdrawal due to smoking cessation<br />
B. The patient has NOT stopped smoking<br />
C. The patient is NOT enrolled in a smoking cessation program<br />
D. The request is for more than 3 months<br />
E. Documentation of enrollment in a smoking cessation program is received or does<br />
not address the needed information<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
3 months<br />
123
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NOVANTRONE<br />
\FDA-APPROVED INDICATIONS<br />
Mitoxantrone is indicated:<br />
A. For the treatment of acute myelogenous leukemia (AML)<br />
B. For the treatment of secondary (chronic) progressive, progressive relapsing, or<br />
worsening relapsing-remitting multiple sclerosis to reduce neurologic disability<br />
and/or frequency of clinical relapses<br />
C. For the palliative treatment of severe pain related to advanced hormone-refractory<br />
prostate cancer in combination with corticosteroids<br />
COVERAGE POLICY<br />
Mitoxantrone® is covered for members who meet the following criteria:<br />
A. For Acute myelogenous leukemia:<br />
a. The documented diagnosis is acute myelogenous leukemia<br />
B. For Multiple Sclerosis:<br />
a. The diagnosis is documented as secondary (chronic) progressive,<br />
progressive relapsing, or worsening relapsing-remitting multiple sclerosis<br />
C. For Prostate Cancer:<br />
a. Tthe diagnosis is documented as prostate cancer<br />
NON COVERAGE<br />
Mitoxantrone is NOT covered for members who meet the following criteria:<br />
A. The diagnosis is NOT acute myelogenous leukemia, prostate cancer or secondary<br />
(chronic) progressive, progressive relapsing, or worsening relapsing-remitting<br />
multiple sclerosis<br />
B. The diagnosis is documented as primary progressive multiple sclerosis<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
124
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
NOVAREL| OVIDREL | PREGNYL<br />
HUMAN CHORIONIC GONADOTROPIN, HCG<br />
FDA-APPROVED INDICATIONS<br />
Novarel is indicated for:<br />
A. Cryptorchidism<br />
B. Hypogonadotropic hypogonadism, In male patients<br />
C. Ovulation induction<br />
COVERAGE POLICY<br />
Novarel is covered for members who meet either of the following criteria:<br />
A. In a Male patient<br />
a. If the patient has a diagnosis of prepubertal cryptochidism not due to<br />
anatomic obstruction or hypogonadism secondary to a pituitary deficiency.<br />
b. AND If the patient does not have any signs of the following diagnoses:<br />
i. Precocious puberty, or<br />
ii. Prostatic carcinoma or other androgen dependent neoplasm<br />
c. And is not being used in the treatment of obesity.<br />
NON COVERAGE<br />
Novarel is NOT covered for members of the following criteria:<br />
A. In a Male patient:<br />
a. If the patient does NOT have a diagnosis of prepubertal cryptochidism not<br />
due to anatomic obstruction or hypogonadism secondary to a pituitary<br />
deficiency.<br />
b. If the patient does have any signs of the following diagnoses:<br />
i. Precocious puberty, or<br />
ii. Prostatic carcinoma or other androgen dependent neoplasm<br />
c. If it is being used in the treatment of obesity.<br />
B. If patient is female<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
125
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
OCTAGAM<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
a. Treatment of hypergammaglobulinemia<br />
B. AND the patient is diagnosed with primary immunodeficiency<br />
C. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
D. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency, OR<br />
Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
126
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
OCTREOTIDE | SANDOSTATIN LAR® | SANDOSTATIN<br />
FDA-APPROVED INDICATIONS<br />
Octreotide is indicated for:<br />
A. Acromegaly, Inadequate response to or ineligible for surgery, radiation, or<br />
bromocriptine mesylate<br />
B. Carcinoid syndrome, Metastatic; symptomatic treatment<br />
C. Vasoactive intestinal peptide-secreting tumor, Associated diarrhea<br />
Safety and efficacy in children not established<br />
COVERAGE POLICY<br />
Octreotide is covered for members who meet either of the following criteria:<br />
A. AND If the patient has ONE of the following diagnoses<br />
a. Acromegaly<br />
b. Vasoactive intestinal peptide-secreting tumor<br />
c. Carcinoid syndrome<br />
B. AND If the prescriber has documentation of the diagnosis with corresponding<br />
chemical markers of the above.<br />
NON COVERAGE<br />
Octreotide is NOT covered for members who meet either of the following criteria:<br />
A. If the patient does NOT have ONE of the following diagnoses?<br />
a. Acromegaly<br />
b. Vasoactive intestinal peptide-secreting tumor, or<br />
c. Carcinoid syndrome, or<br />
B. If the prescriber does NOT have documentation of the diagnosis with<br />
corresponding chemical markers of the above.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist, Gastroenterologist and<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
127
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ORENCIA<br />
FDA-APPROVED INDICATIONS<br />
Orencia® is indicated:<br />
A. For the treatment of moderate to severe rheumatoid arthritis AND juvenile<br />
idiopathic arthritis to reduce signs and symptoms of the disease, to induce major<br />
clinical response, to slow the progression of structural damage, and to improve<br />
physical function in patients with an inadequate response to one or more disease<br />
modifying anti-rheumatic drugs (DMARDs) such as methotrexate or TNF<br />
antagonists.<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Orencia® is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with rheumatoid arthritis OR juvenile idiopathic<br />
arthritis<br />
B. AND the patient must have a minimum of 4 of the following symptoms in<br />
accordance with American College of Rheumatology:<br />
a. Morning stiffness<br />
b. Arthritis of 3 or more joint areas<br />
c. Arthritis of hand joints<br />
d. Symmetric arthritis<br />
e. Rheumatoid nodules<br />
f. Serum rheumatoid factor<br />
g. Radiographic changes<br />
C. AND the patient must have previous trial and failure or contraindication on ALL<br />
of the following:<br />
a. 1 DMARD (Sulfasalazine, Hydroxychloroquine, Cyclosporine,<br />
oral/injectable Gold, Penicillamine, Azathioprine, Leflunomide,<br />
Methotrexate)<br />
b. Humira®<br />
D. AND chart notes documenting previous trial/failure of 1 DMARD AND Humira®<br />
NON COVERAGE<br />
Orencia® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with rheumatoid arthritis OR juvenile idiopathic<br />
arthritis<br />
B. The patient has Less than 4 of symptoms in accordance with American College of<br />
Rheumatology<br />
C. The patient has no previous trial/failure of at least 1 DMARDs AND Humira®<br />
D. Chart notes documenting patient’s previous trials and failures are not provided or<br />
do not address the needed information.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
128
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ORFADIN<br />
FDA-APPROVED INDICATIONS<br />
Orfadin® is indicated:<br />
A. For the treatment of heredity tyrosinemia type I.<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Orfadin® is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with hereditary tyrosinemia type I.<br />
B. AND the patient must have documented treatment protocol of protein-restricted<br />
diet that is low in phenylalanine.<br />
C. AND the patient’s baseline liver function tests (LFTs) must be within normal<br />
limits.<br />
D. AND the patient’s baseline LFTs must be submitted via the prescribing physician<br />
for evaluation.<br />
NON COVERAGE<br />
Orfadin® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with hereditary tyrosinemia type I<br />
B. The patient does NOT have documented treatment protocol of protein-restricted<br />
diet<br />
C. The patient’s baseline LFTs are not within normal limits<br />
D. Chart notes documenting patient’s baseline LFTs are not provided or do not<br />
address the needed information.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
129
FDA-APPROVED INDICATIONS<br />
Orthoclone® is indicated:<br />
A. Heart Transplant Rejection<br />
B. Kidney Transplant Rejection<br />
C. Liver Transplant Rejection<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ORTHOCLONE<br />
COVERAGE POLICY<br />
Orthoclone® is covered for members who meet the following criteria:<br />
A. Patients being treated for Heart, Lung, or Kidney transplant<br />
B. AND has been unresponsive to high dose steroids<br />
C. AND is suffering Acute rejection<br />
D. AND patient is free of hypervolemia<br />
E. AND B vs. D criteria is determined that coverage should be through Medicare<br />
Part D<br />
NON COVERAGE<br />
Orthoclone® is NOT covered for members who meet the following criteria:<br />
A. Not being used for Acute rejection<br />
B. Patient suffers hypervolemia<br />
C. If Medication should be covered by Medicare B<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
130
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
OXANDROLONE<br />
COVERAGE POLICY<br />
All FDA-approved indications not otherwise excluded from Part D<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
131
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
OXSORALEN<br />
FDA-APPROVED INDICATIONS<br />
Oxsoralen® is indicated:<br />
A. For the treatment of cutaneous T-cell lymphoma<br />
B. For the treatment of psoriasis<br />
C. For the treatment of vitiligo<br />
D. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Oxsoralen® is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with T-cell lymphoma OR psoriasis OR vitiligo.<br />
B. AND the patient must have previous trial/failure or contraindication to ALL of the<br />
following:<br />
a. At least 1 topical steroid<br />
b. Dovonex®.<br />
C. AND chart notes must be submitted documenting previous trials on topical steroid<br />
and Dovonex®.<br />
NON COVERAGE<br />
Orxsoralen® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with T-Cell lymphoma, psoriasis, or vitiligo<br />
B. The patient has NO previous trial on at least 1 topical steroid and Dovonex®<br />
C. Chart notes documenting patient’s previous trials on topical steroids and<br />
Dovonex® are not submitted or do not address the needed information.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Dermatologist and Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
132
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PAMIDRONATE<br />
FDA-APPROVED INDICATIONS<br />
pamidronate is indicated:<br />
A. For the treatment of hypercalcemia<br />
B. For the treatment of osteolytic metastases<br />
C. For the treatment of Paget’s disease<br />
D. Osteoporosis<br />
COVERAGE POLICY<br />
pamidronate is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with hypercalcemia<br />
B. AND the patient’s hypercalcemia must be associated with malignancy<br />
C. AND lab reports showing patient’s high calcium are submitted<br />
D. OR patient is diagnosed with osteolytic metastases<br />
E. AND the patient is also diagnosed with multiple myeloma<br />
F. AND the patient is currently receiving antineoplastic therapy<br />
G. OR the patient is diagnosed with Paget’s disease<br />
H. AND disease is moderate to severe<br />
I. AND patient has documented high alkaline phosphatasse and normal calcium<br />
levels<br />
J. AND osteomalacia has been ruled out<br />
K. OR diagnosis of osteoporosis<br />
L. AND the patient has previously failed at least 2 (TWO) of the following: Actonel,<br />
Fosamax, Boniva, Miacalcin<br />
M. AND Chart notes documenting failure on two of the above agents are received<br />
NON COVERAGE<br />
pamidronate is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with hypercalcemia, osteolytic metastases, Paget’s<br />
disease, or osteoporosis<br />
B. The patient does NOT have the appropriate comorbidities (i.e. cancer) if<br />
diagnosed with hypercalcemia or<br />
osteolytic metastases.<br />
C. The patient has no previous trial/failure of Actonel, Fosamax, Boniva, or<br />
Miacalcin if diagnosed with<br />
Osteoporosis<br />
D. Chart notes documenting patient’s previous trials and failures are not provided or<br />
do not address the needed information.<br />
E. Osteomalacia has not been ruled out if patient has diagnosis of Paget’s disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
133
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PANGLOBULIN<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
a. Treatment of hypergammaglobulinemia<br />
B. AND the patient is diagnosed with primary immunodeficiency<br />
C. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
D. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency, OR<br />
Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
134
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
POLYGAM<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
B. Treatment of hypergammaglobulinemia<br />
C. AND the patient is diagnosed with primary immunodeficiency<br />
D. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
E. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
135
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PREGNYL<br />
HUMAN CHORIONIC GONADOTROPIN, HCG<br />
FDA-APPROVED INDICATIONS<br />
Pregnyl is indicated for:<br />
A. Cryptorchidism<br />
B. Hypogonadotropic hypogonadism, In male patients<br />
COVERAGE POLICY<br />
Pregnyl is covered for members who meet either of the following criteria:<br />
A. In a Male patient<br />
a. If the patient has a diagnosis of prepubertal cryptochidism not due to<br />
anatomic obstruction or hypogonadism secondary to a pituitary deficiency.<br />
b. AND If the patient does not have any signs of the following diagnoses:<br />
i. Precocious puberty, or<br />
ii. Prostatic carcinoma or other androgen dependent neoplasm<br />
c. And is not being used in the treatment of obesity.<br />
NON COVERAGE<br />
Pregnyl is NOT covered for members of the following criteria:<br />
C. In a Male patient:<br />
d. If the patient does NOT have a diagnosis of prepubertal cryptochidism not<br />
due to anatomic obstruction or hypogonadism secondary to a pituitary<br />
deficiency.<br />
e. If the patient does have any signs of the following diagnoses:<br />
i. Precocious puberty, or<br />
ii. Prostatic carcinoma or other androgen dependent neoplasm<br />
f. If it is being used in the treatment of obesity.<br />
D. If patient is female<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
136
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PROGRAF<br />
FDA-APPROVED INDICATIONS<br />
Prograf® is indicated:<br />
A. For the prophylaxis of organ rejection in patients receiving allogeneic liver,<br />
kidney or heart transplants.<br />
COVERAGE POLICY<br />
Prograf® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as the prophylaxis of organ rejection in a patient<br />
receiving or received an organ transplant.<br />
B. AND the transplant was NOT covered by Medicare Part A. (Please verify the<br />
payer of the transplant. If Medicare paid for the transplant, Prograf® is covered<br />
by Medicare Part B).<br />
C. AND the transplant was paid by Medicaid or other sources<br />
D. OR is an approved compendia indication.<br />
E. AND the Prograf® formulation is the oral tablet.<br />
F. AND approval can be allowed for up to one year.<br />
G. OR the Prograf® formulation is the IV vial.<br />
H. AND the patient is in a hospital or long term care facility (LTC) or skilled nursing<br />
facility (SNF) and the payer of the stay is NOT Medicare Part A. (Medicare Part<br />
A can pay for the first 110 days and Prograf® therapy would be paid by Medicare<br />
Part B. Please verify payer).<br />
I. AND the medication is NOT being administered using an IMPLANTABLE<br />
PUMP. (Please verify the delivery method of the medication. Administration<br />
through an implantable pump is covered under Medicare Part B.)<br />
J. AND approval can be allowed for up to one year.<br />
K. AND/OR the patient is receiving treatment at home.<br />
L. AND the medication is NOT being administered using an IMPLANTABLE or<br />
EXTERNAL PUMP.<br />
M. AND approval can be allowed for up to one year.<br />
NON COVERAGE<br />
Prograf® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as prophylaxis of organ rejection after<br />
receiving an organ transplant or a compendia listed indication.<br />
B. The transplant was paid for by Medicare Part A.<br />
C. The request is for Prograf® IV formulation in a patient in a hospital or LTC or<br />
SNF that has Medicare Part A coverage.<br />
D. The request is for Prograf® IV formulation and the medication is being<br />
administered using an implantable pump.<br />
E. The request is for Prograf® IV formulation in a patient at home and the<br />
medication is being administered using an implantable or external pump.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
137
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PROMACTA<br />
FDA-APPROVED INDICATIONS<br />
Promacta® is indicated:<br />
A. For the treatment of idiopathic thrombocytic purpura<br />
B. For the treatment of thrombocytopenia<br />
COVERAGE POLICY<br />
Promacta® is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with idiopathic thrombocytic purpura OR<br />
thrombocytopenia<br />
B. AND Patient must have previous trial/failure to a corticosteroid<br />
C. OR Patient must have previous trial/failure to immune globulin<br />
D. OR Patient must have had splenectomy<br />
NON COVERAGE<br />
Promacta® is NOT covered for members with the following criteria:<br />
A. Patient is NOT diagnosed with idiopathic thrombocytic purpura OR<br />
thrombocytopenia<br />
B. Patient has not had previous trial/failure with corticosteroid OR immune globulin<br />
OR splenectomy<br />
C. Patient must not have pre-existing chronic hepatic disease<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes documenting previous trial/failure of corticosteroid OR immune globulin OR<br />
chart notes documenting splenectomy.<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
138
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PROVIGIL<br />
FDA-APPROVED INDICATIONS<br />
Provigil® is indicated:<br />
A. For improved wakefulness in adult patients with excessive sleepiness associated<br />
with narcolepsy, obstructive sleep apnea/hypopnea syndrome (OSAHS) and shift<br />
work sleep disorder (SWSD).<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Provigil® is covered for members who meet the following criteria:<br />
A. The prescribing physician is board certified as a sleep specialist, ear, nose and<br />
throat specialist, neurologist or pulmonologist or has obtained a consult from any<br />
of the listed specialties.<br />
B. Diagnosis is documented as excessive daytime sleepiness associated with<br />
narcolepsy.<br />
C. OR diagnosis is documented as shift work sleep disorder when the patient meets<br />
the following criteria<br />
D. OR diagnosis is documented as treatment of excessive daytime sleepiness<br />
associated with OSAHS when the patient meets the following criteria:<br />
a. The patient is receiving nasal continuous positive airway pressure (CPAP)<br />
or bi-level positive airway pressure (BIPAP) for at least 1 month,<br />
b. AND CPAP or BIPAP therapy must be continued on a routine basis in<br />
combination with Provigil® therapy,<br />
c. AND the daytime fatigue is significantly impacting, impairing, or<br />
compromising the patient’s ability to function normally,<br />
d. AND the patient is compliant with CPAP or BIPAP therapy.<br />
E. OR diagnosis is documented as fatigue associated with Multiple Sclerosis when<br />
the patient meets the following criteria:<br />
a. Patient has had an adequate trial of amantadine and fatigue is still<br />
unmanageable.<br />
b. AND Provigil® therapy will NOT be prescribed in combination with any<br />
of the following long acting medications used for insomnia: flurazepam,<br />
Dalmane®, eszopiclone, Lunesta®) estazolam, Prosom® temazepam,<br />
Restoril®.<br />
c. AND documentation that the patient is not on Xyrem® therapy.<br />
d. AND evidence of diagnosis documented in patient’s chart notes provided<br />
by prescribing provider.<br />
139
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PROVIGIL<br />
(Continued)<br />
NON COVERAGE<br />
Provigil® is NOT covered for members with the following criteria:<br />
A. The prescribing physician is NOT board certified as a sleep specialist, ear, nose<br />
and throat specialist, neurologist or pulmonologist or has NOT obtained a consult<br />
from any of the listed specialties.<br />
B. If the diagnosis is OSAHS and NO NPSG diagnostic has been performed.<br />
C. If the diagnosis is OSAHS and the patient has not received CPAP or BIPAP<br />
therapy for at least 1 month.<br />
D. If the diagnosis is OSAHS and the daytime fatigue is NOT significantly<br />
impacting, impairing, or compromising the patient’s ability to function normally.<br />
E. If the diagnosis is OSAHS and CPAP or BIPAP therapy is NOT being continued<br />
with Provigil® therapy.<br />
F. If the diagnosis is fatigue associated with Multiple Sclerosis and the patient has<br />
NOT had an adequate trial of amantadine.<br />
G. Patient is receiving a long acting medication for insomnia.<br />
H. Patient is currently receiving Xyrem® therapy.<br />
I. Provider does not provide patient chart notes for documentation.<br />
J. If the diagnosis is listed as depression, Parkinsons’ disease, or fatigue not<br />
associated with narcolepsy, OSAHS or shift work.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
140
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
PULMOZYME<br />
FDA-APPROVED INDICATIONS<br />
Pulmozyme® solution is indicated:<br />
A. For the management of cystic fibrosis patients to improve pulmonary function.<br />
COVERAGE POLICY<br />
Pulmozyme® is covered for members who meet the following criteria:<br />
A. The patient is a cystic fibrosis patient and medication is being used to improve<br />
pulmonary function and/or reduce the frequency of respiratory infections.<br />
B. AND the patient will be using one of the following nebulizers: Hudston T UPdraft<br />
II®, Marquest Acorn II®, PARI LC Jet+, Pari BABY®, Durable<br />
Sidestream®. (Safety and efficacy have only been shown with these nebulizers).<br />
C. AND the patient will be using one of the following compressors: Pulmo-Aide®,<br />
PARI PRONEB®, Mobilaire®, Porta-Neb®. (Safety and efficacy have only been<br />
shown with these compressors).<br />
D. AND the patient is being treated in a hospital or long-term care facility (LTC) or a<br />
skilled-nursing facility (SNF).<br />
E. AND the payer of the stay is NOT Medicare Part A. ((Medicare Part A can pay<br />
for the first 110 days and Pulmozyme® would be paid by Medicare Part B.<br />
Please verify payer).<br />
F. AND approval can be allowed for up to one year.<br />
G. AND/OR the patient is being treated at home.<br />
H. THEN Pulmozyme® is NOT covered. (Patients using a medication with a<br />
nebulizer are covered under Medicare Part B).<br />
I. AND if the patient has previously received Pulmozyme®, he/she must show an<br />
improvement in pulmonary function and/or reduction in the frequency of<br />
respiratory infections since initiating therapy.<br />
NON COVERAGE<br />
Pulmozyme® is NOT covered for members with the following criteria:<br />
A. Patient is NOT a cystic fibrosis patient.<br />
B. The medication is NOT being used to improve pulmonary function and/or reduce<br />
the frequency of respiratory infections.<br />
C. If the patient is being treated in a hospital or long-term facility (LTC) or a skillednursing<br />
facility (SNF) and the payer of the stay is Medicare Part A.<br />
D. The patient is being treated at home. (Patients using medication with a nebulizer<br />
are covered under Medicare Part B).<br />
E. If the patient has previously received Pulmozyme® and he/she has NOT shown<br />
an improvement in pulmonary function and/or reduction in the frequency of<br />
respiratory infections since initiating therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Pulmonologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
141
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
RANEXA<br />
FDA-APPROVED INDICATIONS<br />
Ranexa® is indicated:<br />
B. For the treatment of chronic angina. Because Ranexa® prolongs the QT interval,<br />
it should be reserved for patients who have not achieved an adequate response<br />
with other antianginal drugs. Ranexa® should be used in combination with<br />
amlodipine, beta-blockers or nitrates.<br />
COVERAGE POLICY<br />
Ranexa® is covered for members who meet the following criteria:<br />
A. The diagnosis documented as chronic angina with symptoms limiting daily<br />
activities.<br />
B. AND the prescribing physician is a board certified cardiologist or has obtained a<br />
consult from the listed specialty.<br />
C. AND the patient has NO pre-existing QT prolongation (eg. ventricular<br />
tachycardia, congenital long QT syndrome, uncorrected hypokalemia).<br />
D. AND the patient has NO hepatic impairment (Child-Pugh Classes A [mild], B<br />
[moderate], or C [severe].<br />
E. AND the patient is NOT receiving a medication that prolongs the QT interval (eg.<br />
amiodarone, Cordarone®, Pacerone®, droperidol, chlorpromazine, erythromycin,<br />
Biaxin®, clarithromycin, sotalol, Betapace®, thioridazine, Mellaril®, flecainide,<br />
Tambocor®, haloperidol, Haldol®, quinine, procainamide, quinidine, Geodon®,<br />
Effexor XR®, Propulsid®, Risperdal®, Serevent®, Imitrex®, tamoxifen,<br />
tizanidine, Zanaflex®, Zomig®, Seroquel®, Tikosyn®, Anzemet®,<br />
dysopyramide, Norpace®, Orap®, fluoxetine, Prozac®, Foscavir®, Dynacirc®,<br />
isradipine, Avelox®, Amerge®, Cardene®, Sandostatin®, paroxetine, Paxil®,<br />
mesoridazine, or Serentil®). (Please verify that the patient is not receiving any<br />
of these medications by reviewing the patient’s drug history or chart).<br />
F. AND the patient is NOT receiving any potent CYP3A inhibitors that will affect<br />
the metabolism of Ranexa®. (eg. diltiazem, Cardizem®, Cartia XT®, Diltia<br />
XT®, Tiazac®, ketoconazole, verapamil, Calan®, Covera®, Verelan®, Isoptin®,<br />
vinblastine, doxorubicin, isoniazid, ritonavir, Norvir®, Kaletra®, cyclosporine,<br />
Viracept®, Crixivan®, Fortovase®, Invirase®, ciprofloxacin, Cipro®,<br />
itraconazole, Sporonax®, norfloxacin, voriconazole, Vfend®, rifampin, rifabutin).<br />
(Please verify that the patient is not receiving any of these medications by<br />
reviewing the patient’s drug history or chart).<br />
G. AND the patient has tried, failed and/or been intolerant (continues to have angina<br />
that limits daily activities) to a 30-day trial of at least one agent two of the<br />
following three classes: (Please verify that the patient has tried, failed or is<br />
intolerant to at least one agent in each class for at least 30 days by reviewing the<br />
patient’s drug history or chart).<br />
a. Betablockers: (eg. Toprol XL®, atenolol, Coreg®, propranolol, bisprolol,<br />
metoprolol, timolol, acebutolol, nadolol, propranolol).<br />
142
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
RANEXA<br />
(Continued)<br />
b. Calcium Channel Blocker: (eg. amlodipine, nifedipine, nosoldipine,<br />
isradipine, diltiazem, nicardipine, felodipine, verapamil, Norvasc®,<br />
Exforge®, Caduet®, Lotrel®, Azor®).<br />
c. Nitrate: (eg. isosorbide, Isordil®, Dilatrate SR®, Monoket®, Ismo®,<br />
Imdur®, nitroglycerin, Nitro-Time®).<br />
H. AND therapy will be given in combination with amlodipine, a beta blocker and/or<br />
a nitrate. (eg. amlodipine, Norvasc®, Exforge®, Caduet®, Lotrel®, Azor®,<br />
Toprol XL®, metoprolol, atenolol, bisprolol, timolol, acebutolol, nadolol,<br />
propranolol, Coreg®, isosorbide, Isordil®, Dilatrate SR®, Monoket®, Ismo®,<br />
Imdur®, nitroglycerin, Nitro-Time®) (Please verify that the patient is or will be<br />
receiving one of these medications to be taken in combination with Ranexa® by<br />
reviewing the patient’s drug history or chart).<br />
I. AND if the patient has received prior treatment with Ranexa®.<br />
J. The patient must experience a decrease in angina frequency since initiating<br />
treatment.<br />
K. AND approval can be allowed for up to 3 months for the initial request (To ensure<br />
efficacy of the medication) and up to one year for extended authorization.<br />
NON COVERAGE<br />
Ranexa® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as chronic angina.<br />
B. The prescribing physician is NOT a board certified cardiologist or has NOT<br />
obtained a consult from the listed specialty.<br />
C. The patient has a pre-existing QT prolongation (eg. ventricular tachycardia,<br />
congenital long QT syndrome, uncorrected hypokalemia).<br />
D. The patient has hepatic impairment (Child-Pugh Classes A [mild], B [moderate],<br />
or C [severe].<br />
E. The patient is receiving a medication that prolongs the QT interval.<br />
F. The patient is receiving a potent CYP3A inhibitors that will affect the metabolism<br />
of Ranexa®.<br />
G. The patient has NOT tried, failed and/or been intolerant (continues to have<br />
angina) to a 30-day trial of at least one agent in two ot the three medication<br />
classes of beta blockers, calcium channel blockers and nitrates.<br />
H. Therapy will NOT be given in combination with amlodipine, a beta blocker<br />
and/or a nitrate.<br />
I. If the patient has received prior treatment with Ranexa® and has NOT<br />
experienced a decrease in angina frequency since initiating treatment.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Cardiologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
143
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
RAPAMUNE<br />
FDA-APPROVED INDICATIONS<br />
Rapamune® is indicated:<br />
A. For the prophylaxis of organ rejection in patients aged 13 years or older receiving<br />
renal transplants.<br />
COVERAGE POLICY<br />
Rapamune® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as the prophylaxis of organ rejection in a patient<br />
receiving or received an organ transplant.<br />
B. AND the transplant was NOT covered by Medicare Part A. (Please verify the<br />
payer of the transplant. If Medicare paid for the transplant, Rapamune® is<br />
covered by Medicare Part B).<br />
C. AND approval can be allowed for up to one year.<br />
D. OR the indication is documented as an indication listed in compendia.<br />
E. The prior authorization request should be reviewed by a prior authorization<br />
pharmacist. Pharmacist should review the drug study for:<br />
F. A study can be found.<br />
G. The study shows clinical improvement with treatment.<br />
H. If there are first line treatments, the patient must have tried and failed. (e.g.<br />
Psoriasis patients should have tried and failed methotrexate).<br />
I. The patient meets the criteria of the study.<br />
J. The study has clinical validity (e.g. blinded, substantial population).<br />
K. The study’s population meets the patient’s demographics.<br />
L. The patient’s disease status is not terminal and therapy will provide benefit.<br />
M. The patient will not receive duplicate therapy.<br />
N. <strong>Authorization</strong> period or re-treatment is within timeframe of study.<br />
NON COVERAGE<br />
Rapamune® is NOT covered for members with the following criteria:<br />
F. The diagnosis is NOT documented as prophylaxis of organ rejection after<br />
receiving an organ transplant or a compendia listed indication.<br />
G. The transplant was paid for by Medicare Part A.<br />
H. The indication is listed in compendia and the patient has not tried and failed first<br />
line therapy.<br />
I. The indication is listed in compendia and there is no study or the study has no<br />
clinical validity.<br />
J. The patient is receiving duplicate therapy.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
144
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
REGRANEX<br />
FDA-APPROVED INDICATIONS<br />
Regranex® is indicated:<br />
A. For the treatment of diabetic foot ulcer<br />
B. For the treatment of wound management<br />
COVERAGE POLICY<br />
Regranex® is covered for members who meet the following criteria:<br />
A. Must be used for treatment of lower-extremity diabetic ulcers<br />
B. AND the ulcer must extend into subcutaneous tissue<br />
C. AND the tissue must have an adequate blood supply<br />
D. AND the patient must have concurrent good ulcer treatment practices including<br />
ALL of the following:<br />
a. Debridgement<br />
b. Pressure relief<br />
c. Infection relief<br />
E. AND the above good ulcer treatment practices must be documented through chart<br />
notes<br />
F. AND the ulcer must be less than 10 cm 2 in size<br />
G. AND the patient must have somewhat controlled diabetes (A1c less than 10.0%)<br />
H. AND the patient’s A1c is verified though lab report submitted<br />
I. Initial authorization for 10 weeks. If additional authorization is needed chart<br />
notes showing at least a 30% reduction in ulcer size are required for additional<br />
approval of another 10 weeks. Total of 20 weeks of treatment.<br />
NON COVERAGE<br />
Regranex® is NOT covered for members who meet the following criteria:<br />
A. The patient is not diagnosed with diabetes<br />
B. The ulcer is greater than 10 cm 2 in size<br />
C. Good ulcer treatment practices are NOT being utilized<br />
D. Patient’s A1c is greater than 10.0%<br />
E. Chart notes documenting patient’s A1c are not received or do not address the<br />
needed information.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
10 weeks<br />
145
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
RELISTOR<br />
FDA-APPROVED INDICATIONS<br />
Reslistor® is indicated:<br />
A. For treatment of opiate-induced constipation in patients with advanced illness<br />
who are receiving palliative care when response to laxative therapy has been<br />
insufficient.<br />
COVERAGE POLICY<br />
Relistor® is covered for members who meet the following criteria:<br />
A. B vs D determination per CMS guidelines<br />
B. Patient must have previous trial/failure on BOTH of the following:<br />
a. Polyethylene Glycol<br />
b. Amitiza<br />
NON COVERAGE<br />
Relistor® is NOT covered for members with the following criteria:<br />
A. Diagnosis is NOT opiate-induced constipation<br />
B. Patient has no previous trial/failure of BOTH Polyethylene Glycol AND Amitiza<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes per Covered Uses<br />
AUTHORIZATION PERIOD<br />
4 Months<br />
146
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
REVATIO<br />
FDA-APPROVED INDICATIONS<br />
Revatio® is indicated:<br />
A. For the treatment of pulmonary arterial hypertension (WHO Group 1) to improve<br />
exercise ability.<br />
COVERAGE POLICY<br />
Revatio® is covered for members who meet the following criteria:<br />
A. Patient is age 18 years or older.<br />
B. AND the prescribing provider is a pulmonologist, and/or cardiologist or has<br />
obtained a consult from the listed specialties.<br />
C. AND the diagnosis is documented as pulmonary arterial hypertension.<br />
D. AND the patient is NOT on any nitrate therapy (eg. isosorbide, Isordil®, Diltrate-<br />
SR®, Ismo®, Monoket®, Imdur®, nitroglycerin, NitroQuick®, Nitrostat®,<br />
Nitrotab®, Nitro-Time®, Nitro-Bid®, Minitran®, Nitro-Dur®, Nitrek®).<br />
(Verification can be made by reviewing the patient’s drug history or patient’s<br />
chart).<br />
E. AND the patient does NOT have pulmonary veno-occlusive disease (PVOD),<br />
(contraindicated).<br />
F. AND the patient has NOT suffered a myocardial infarction (MI), stroke or lifethreatening<br />
arrhythmia with the last 6 months. (Contraindicated).<br />
G. AND the patient does NOT have coronary artery disease causing unstable angina.<br />
(Contraindicated).<br />
H. AND the patient does NOT have blood pressure Greater than 170/110.<br />
(Contraindicated).<br />
I. AND the patient does NOT have retinitis pigmentosa. (contraindicated).<br />
J. AND the patient has had an adequate trial and failure (4 weeks or more) or is not<br />
a candidate for calcium channel blocker therapy. (eg. nifedipine, Adalat CC®,<br />
Nifedical XL®, Procardia®, Procardia XL®, amlodipine, Norvasc®, diltiazem,<br />
Cardizem®, Cartia XT®, Dilacor XR®, Diltia XT®, Tiazac®, Cardizem CD®).<br />
(Verification can be made by reviewing the patient’s drug history or patient’s<br />
chart).<br />
K. AND the patient will NOT receive combination therapy with a prostacyclin<br />
(Flolan®, Ventavis®, Remodulin®) or an endothelin antagonist (Tracleer®) or a<br />
phosphodiesterase type-5 inhibitor (Viagra®) agent. Combination therapy has not<br />
been approved by the FDA. (Please verify that the patient is not on duplicate<br />
therapy by reviewing the patient’s drug history or chart).<br />
L. AND the diagnosis is documented as pulmonary arterial hypertension class 1<br />
defined by the World Health Organization (WHO).<br />
M. AND the diagnosis is NOT documented as pulmonary arterial hypertension class<br />
2, 3, or 4 defined by the WHO.<br />
N. AND therapy is being prescribed to improve exercise ability.<br />
O. AND the dose does not exceed 20 mg three times a day.<br />
147
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
REVATIO<br />
(Continued)<br />
P. AND if the patient has received previous Revatio® therapy, the patient must see<br />
an improvement in their exercise ability (walking distance), dyspnea fatigue<br />
and/or an improvement in functional status (New York Heart Association (NYHA<br />
functional class).<br />
NON COVERAGE<br />
Revatio® is NOT covered for members with the following criteria:<br />
A. Patient is under the age of 18 years old.<br />
B. The prescribing provider is NOT a pulmonologist, and/or cardiologist or obtained<br />
a consult from the listed specialties.<br />
C. The diagnosis is NOT listed as pulmonary hypertension.<br />
D. The diagnosis is listed as impotence.<br />
E. The patient is receiving nitrate therapy.<br />
F. The patient has pulmonary veno-occlusive disease (PVOD).<br />
G. The patient has suffered a MI, stroke or life-threatening arrhythmia within the last<br />
6 months.<br />
H. The patient has coronary artery disease causing unstable angina.<br />
I. The patient has a blood pressure Greater than 170/110.<br />
J. The patient has retinitis pigmentosa.<br />
K. The patient has NOT had an adequate 4-week trial and failure to a calcium<br />
channel blocker therapy.<br />
L. The patient will receive Tracleer®, Flolan®, Ventavis®, Viagra®, or<br />
Remodulin® therapy while receiving a Revatio® drug regimen. (Please verify<br />
that the patient does not have duplicate therapy by reviewing the patient’s drug<br />
history or chart).<br />
M. The patient’s pulmonary arterial hypertension has NOT been classified as class 1<br />
defined by the WHO.<br />
N. The patient’s pulmonary arterial hypertension has been classified as class 2, 3, or<br />
4 by the WHO.<br />
O. Revatio® is NOT being prescribed to improve exercise ability.<br />
P. The dose exceeds 20 mg three times a day.<br />
Q. If the patient has received previous Revatio® therapy and they have NOT seen an<br />
improvement in their exercise ability (walking distance) and/or an improvement<br />
in their NYHA functional classification.<br />
R. Evidence of diagnosis, WHO classification, and exercise ability and/or dyspnea<br />
fatigue is NOT documented in the patient’s chart notes provided by prescribing<br />
provider.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Pulmonologist and Cardiologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
148
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
REVLIMID<br />
FDA-APPROVED INDICATIONS<br />
Revlimid® is indicated:<br />
A. For the treatment of multiple myeloma when used in combination with<br />
dexamethasone in patients who have received at least one prior therapy.<br />
B. For the treatment of patients with transfusion-dependent anemia due to low or<br />
intermediate-1 risk myelodysplastic syndromes [MDS] associated with a deletion<br />
5q cytogenetic abnormality with or without additional cytogenetic abnormalities.<br />
C. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Revlimid® is covered for members who meet the following criteria:<br />
A. If the patient is female and is of childbearing age, she is NOT pregnant, does<br />
NOT have plans for pregnancy, is using a reliable method of contraception and is<br />
participating in the RxAssist program.<br />
B. AND if the patient is male, he has received both oral and written warnings of the<br />
potential risks of taking lenalidomide and exposing a fetus to the drug.<br />
C. AND diagnosis is documented as multiple myeloma.<br />
D. AND the patient has tried and failed to respond to at least one therapy listed<br />
below: (Please verify that the patient has failed previous therapy by reviewing the<br />
patient’s chart).<br />
a. Melphalan.<br />
b. Carmustine.<br />
c. Cyclophosphamide.<br />
d. Doxorubicin<br />
e. Doxorubicin liposomal.<br />
f. Bortezomib.<br />
g. Zoledronic Acid.<br />
E. AND the patient has tried and failed to respond to a thalidomide regimen. (Please<br />
verify that the patient has failed previous thalidomide therapy by reviewing the<br />
patient’s drug history and/or chart).<br />
F. AND lenalidomide therapy will and/or currently is being used in combination<br />
with dexamethasone. (Please verify by reviewing the patients drug history or<br />
chart).<br />
G. AND if the patient has received previous Revlimid® therapy, he/she has shown a<br />
delay or experienced no disease progression.<br />
H. AND/OR diagnosis is documented as transfusion-dependent anemia in a low or<br />
intermediate-1 risk myelodysplastic syndrome associated with a deletion 5q<br />
cytogenetic abnormality.<br />
I. AND the patient has received 2 or more units of red blood cells [RBC] within 8<br />
weeks of the reported anemia.<br />
J. AND if the patient has received previous Revlimid® therapy, he/she can show<br />
stabilization of anemia by having experienced one of the following:<br />
a. 50% reduction in blood transfusions.<br />
b. An increase in hemoglobin of at least 1g/dL over baseline.<br />
149
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
REVLIMID<br />
(Continued)<br />
c. The absence of the pretreatment cytogenetic abnormality or a reduction in<br />
the number of abnormal cells of at least 50%.<br />
NON COVERAGE<br />
Revlimid® is NOT covered for members with the following criteria:<br />
A. The patient is a female patient of child bearing age that is pregnant or has plans<br />
for pregnancy, is NOT using a reliable form of contraception or is NOT<br />
participating in the RxAssist program.<br />
B. The patient is a male and has NOT received both oral and written warnings on the<br />
potential risk of taking lenalidomide and exposing a fetus to the drug.<br />
C. The diagnosis is NOT documented as multiple myeloma or transfusion-dependent<br />
anemia in a low or intermediate-1 risk myelodysplastic syndrome associated with<br />
a deletion 5q cytogenetic abnormality.<br />
D. The diagnosis is documented as multiple myeloma and the patient has NOT tried<br />
and failed at least one of the following listed therapies: Melphalan, carmustine,<br />
cyclophosphamide, doxorubicin, bortezomib, or zoledronic acid.<br />
E. The diagnosis is documented as multiple myeloma and the patient has NOT tried<br />
and failed thalidomide therapy.<br />
F. The diagnosis is documented as multiple myeloma and the patient is NOT taking<br />
lenalidomide therapy in combination with dexamethasone.<br />
G. The diagnosis is documented as multiple myeloma in a patient previously<br />
receiving Revlimid® therapy and he/she has shown disease progression.<br />
H. The diagnosis is transfusion-dependent anemia in a low or intermediate-1 risk<br />
myelodysplastic syndrome associated with a deletion 5q cytogenetic abnormality<br />
and the patient has NOT received 2 or more units of red blood cells within 8<br />
weeks of the reported anemia.<br />
I. If the diagnosis is transfusion-dependent anemia in a low or intermediate-1 risk<br />
myelodysplastic syndrome associated with a deletion 5q cytogenetic abnormality<br />
in a patient that has received previous Revlimid® therapy and he/she has not<br />
shown stabilization of the anemia.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Hematologist and Oncologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
150
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
RISPERDAL<br />
FDA-APPROVED INDICATIONS<br />
Risperdal® is indicated:<br />
A. For the acute and maintenance treatment of schizophrenia<br />
B. For the short-term treatment of acute mania or mixed episodes associated with<br />
bipolar disorder (bipolar I disorder)<br />
C. Irritability related to autism<br />
COVERAGE POLICY<br />
Risperdal® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a psychiatrist or has obtained a consult from the<br />
listed specialty.<br />
B. AND the patient is 5 years of age or older.<br />
C. AND the diagnosis is NOT documented as dementia-related psychosis.<br />
D. AND the patient does NOT have congenital long QT syndrome or NO history of<br />
cardiac arrhythmias.<br />
E. AND the diagnosis is documented as schizophrenia, acute mania or autism<br />
F. AND Risperdal® will NOT be used in combination with another atypical<br />
antipsychotic drug. (Please reviewthe patient’s drug history or chart to verify no<br />
combination use with another atypical antipsychotic drug)<br />
G. AND if the patient has received previous Risperdal® therapy, the provider has<br />
seen clinical evidence demonstrating improvement in schizophrenia symptoms.<br />
NON COVERAGE<br />
Risperdal® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a psychiatrist or the prescriber has NOT<br />
obtained a consult from the listed specialty.<br />
B. The patient is under the age of 5 years old.<br />
C. The diagnosis is documented as dementia-related psychosis.<br />
D. The patient does have congenital long QT syndrome or has a history of cardiac<br />
arrhythmias.<br />
E. Risperdal® therapy will be used in combination with another atypical<br />
antipsychotic drug<br />
F. If the patient has received previous Risperdal® therapy and the provider has NOT<br />
seen any clinical evidence demonstrating improvement in schizophrenia<br />
symptoms.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart Notes<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
151
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ROTATEQ<br />
FDA-APPROVED INDICATIONS<br />
RotaTeq®® is indicated:<br />
A. For the prophylaxis of gastroenteritis caused by rotavirus infection<br />
COVERAGE POLICY<br />
RotaTeq® is covered for members who meet the following criteria:<br />
A. Must be used for prophylaxis against rotavirus infection<br />
B. AND the patient must be between 6-12 weeks old upon first dose<br />
C. AND the patient will receive all three doses before 32 weeks of age<br />
D. AND request is for 3 doses (or less if patient has already received 1-2 doses)<br />
NON COVERAGE<br />
RotaTeq® is NOT covered for members who meet the following criteria:<br />
A. RotaTeq® is not being used for ANY other diagnosis than prophylaxis against<br />
rotavirus infection<br />
B. The patient is less than 6 weeks old or greater than 12 weeks old<br />
C. Patient will not receive all three doses before 32 weeks of age<br />
D. Request is for more than 3 doses<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
152
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SAIZEN<br />
FDA-APPROVED INDICATIONS<br />
A. Somatropin is indicated (Not all branded medications have each indication listed<br />
below. Please refer to reference symbol for actual indication):<br />
A. For the long-term treatment of pediatric patients who have growth failure due to<br />
an inadequate secretion of endogenous growth hormone.<br />
B. For the long-term treatment of pediatric patients who have growth failure due to<br />
Prader-Willi syndrome.*<br />
C. For long-term replacement therapy in adults with growth hormone deficiency of<br />
either childhood or adult-onset etiology.*<br />
D. For the treatment of short stature associated with Turner syndrome in patients<br />
whose epiphyses are not closed.<br />
E. For the long-term treatment of idiopathic short stature, also called non-growth<br />
hormone deficient short stature, defined by height SDS less than or equal to -2.25<br />
and associated with growth rates unlikely to permit attainment of adult height in<br />
the normal range, in pediatric patients whose epiphyses are not closed and for<br />
whom diagnostic evaluation excludes other causes associated with short stature<br />
that should be observed or treated by other means.<br />
F. For replacement of endogenous growth hormone in adults with growth hormone<br />
deficiency who meet both of the following 2 criteria:<br />
a. Adult onset: Patients who have growth hormone deficiency either alone,<br />
or with multiple disease, hypothalamic disease, surgery, radiation therapy,<br />
or trauma.<br />
b. Child onset: Patients who were growth-hormone-deficient during<br />
childhood who have growth hormone deficiency confirmed as an adult.<br />
G. For the long-term treatment of children with growth failure due to inadequate<br />
secretion of endogenous growth hormone.<br />
H. For the treatment of growth failure associated with chronic renal insufficiency up<br />
to the time of renal transplantation.<br />
I. For the long-term treatment of growth failure associated with Turner syndrome.<br />
J. For the replacement of endogenous growth hormone in patients with adult growth<br />
hormone deficiency who<br />
K. meet both of the following 2 criteria:<br />
a. Adult onset: Patients who have adult growth hormone deficiency either<br />
alone or with multiple hormone deficiencies (hypopituitarism) as a result<br />
of pituitary disease, hypothalamic disease, surgery, radiation therapy, or<br />
trauma.<br />
b. Child onset: Patients who were growth hormone deficient during<br />
childhood, confirmed as an adult.<br />
L. For the treatment of HIV patients with wasting or cachexia to increase lean body<br />
mass and body weight, and improve physical endurance. Concomitant<br />
antiretroviral therapy is necessary.<br />
153
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SAIZEN<br />
(Continued)<br />
M. For the treatment of short bowel syndrome in patients receiving specialized<br />
nutritional support. =<br />
N. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Somatropin® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified endocrinologist or infectious disease<br />
specialist.<br />
B. The request for somatropin is the formulary covered agent. (Please review drug<br />
formulary to ensure prior authorization is for the formulary covered medication).<br />
C. The patient is 20 years of age or older.<br />
D. AND the patient does NOT have any evidence of active malignancy.<br />
E. AND the diagnosis is documented as growth hormone deficiency in an adult<br />
needing replacement with endogenous growth hormone.<br />
a. AND the patient has a biochemical diagnosis of growth hormone<br />
deficiency, means of a negative response to 2) standard growth hormone<br />
stimulation tests [Max peak less than 5ng/mL by RIA or Less than 2.5<br />
ng/mL by IRMA] OR an IGF-1 level that is two standard deviations below<br />
normal for the patient’s age group. (Please verify the growth hormone or<br />
IGF-1 level in the patient’s chart notes and ensure the tests were<br />
preformed within 3 months of the initial request).<br />
b. AND the growth hormone deficiency is due to at least one of the<br />
following etiologies:<br />
i. Pituitary or hypothalamus surgery<br />
ii. Pituitary or hypothalamus disease.<br />
iii. Pituitary or hypothalamus injury.<br />
iv. Radiation therapy.<br />
v. Growth-hormone deficiency during childhood. (Requires an<br />
additional stimulation test during adulthood).<br />
c. AND the patient has symptoms of growth hormone deficiency that<br />
includes one of the following:<br />
i. Reduced bone density of more than (1) standard deviation below<br />
the age and gender-specific mean.<br />
ii. Evidence of cardiac decompensation defined as reduced ejection<br />
fracture of Less than 50%.<br />
d. AND if the patient has received previous somatropin therapy, he/she has<br />
shown an improvement in quality of life and/or symptoms (bone mass,<br />
muscle mass, strength, body fat and/or cholesterol).<br />
F. AND/OR the diagnosis is documented as AIDS wasting or AIDS cachexia.<br />
154
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SAIZEN<br />
(Continued)<br />
a. AND the patient has had an involuntary weight loss of Greater than 10%<br />
of pre-illness baseline body weight or body mass index (BMI) Less than<br />
20 kg/m 2 in the absence of a concurrent illness or medical condition other<br />
than HIV infection that may cause weight loss.<br />
b. AND the patient has failed to respond to a 30-day drug regimen of<br />
megestrol (Megace®) AND an anabolic steroid (e.g. Testim®,<br />
Androgel®, testosterone enanthate, testosterone cypionate, Testoderm®,<br />
Androderm®, methyltestosterone, or fluoxymesterone). (Please verify the<br />
use of megestrol and an anabolic steroid by reviewing the patient’s drug<br />
history or chart).<br />
c. AND if the patient has received previous somatropin therapy, he/she must<br />
show a positive response to treatment by maintaining or increasing their<br />
initial weight and/or muscle mass before initiating somatropin therapy.<br />
G. AND/OR the diagnosis is documented as a patient with short bowel syndrome.<br />
a. AND the patient is receiving specialized nutritional therapy and parental<br />
nutrition stable.<br />
b. AND the small intenstine is Less than 200 cm in length and at least 2<br />
months post resection.<br />
c. AND the patient has 30% or greater functioning colon with at least 15 cm<br />
of intact jejunum or at least 90 cm of intact jejunum and/or ileum.<br />
d. AND the patient has an intach stomach and duodenum.<br />
e. AND the patient has stable hepatic and renal status (billirubin Less than 3<br />
X ULN and Creatinine Less than 3mL/dL).<br />
f. AND if the patient has received previous somatropin therapy, he/she must<br />
show a positive response by showing a reduction on their dependence on<br />
total parenteral nutrition.<br />
NON COVERAGE<br />
Somatropin® is NOT covered for members with the following criteria:<br />
A. The prescribing physician is NOT a board certified endocrinologist or infectious<br />
disease specialist.<br />
B. The request for somatropin is NOT the formulary covered agent.<br />
C. The patient has evidence of active malignancy.<br />
D. The patient is NOT 20 years of age or older.<br />
E. The diagnosis is NOT documented as growth hormone deficiency in an adult<br />
needing replacement with endogenous growth hormone, AIDS wasting or AIDS<br />
cachexia or short bowel syndrome.<br />
F. If the diagnosis is documented as growth hormone deficiency in adult and they<br />
meet any of the following criteria:<br />
155
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SAIZEN<br />
(Continued)<br />
a. The patient does NOT have a biochemical diagnosis of growth hormone<br />
deficiency to 2 standard growth hormone stimulation tests or an IGF-1<br />
level that is NOT two standard deviations below normal for the patient’s<br />
age group.<br />
b. The growth hormone deficiency is NOT due to at least one of the<br />
following etiologies:<br />
i. Pituitary or hypothalamus surgery<br />
ii. Pituitary or hypothalamus disease.<br />
iii. Pituitary or hypothalamus injury.<br />
iv. Radiation therapy.<br />
v. Growth-hormone deficiency during childhood.<br />
c. The patient does NOT have symptoms of growth hormone deficiency that<br />
includes one of the following:<br />
i. Reduced bone density of more than (1) standard deviation below<br />
the age and gender-specific mean.<br />
ii. Evidence of cardiac decompensation defined as reduced ejection<br />
fracture of Less than 50%.<br />
d. If the patient has received previous somatropin therapy and he/she does<br />
not show an improvement In quality of life and/or symptoms (bone mass,<br />
muscle mass, strength, body fat and/or cholesterol).<br />
G. If the diagnosis is documented as AIDS wasting or AIDS cachexia and they meet<br />
any of the following criteria:<br />
a.<br />
The patient has NOT had an involuntary weight loss of Greater than 10%<br />
of pre-illness baseline body weight or body mass index (BMI) Less than<br />
20 kg/m 2 .<br />
b. The patient has had an involuntary weight loss of Greater than 10% of preillness<br />
baseline body weight or body mass index (BMI) Less than 20<br />
kg/m2 but the weight loss happened with a concurrent illness or medical<br />
condition other than HIV infection.<br />
c. The patient has NOT failed a 30 day drug regimen of megestrol<br />
(Megace®) AND an anabolic steroid.<br />
d. If the patient has received previous somatropin therapy and he/she has<br />
NOT shown a positive response to treatment by maintaining or increasing<br />
their initial weight before initiating somatropin therapy.<br />
H. If the diagnosis is documented as a patient with short bowel syndrome and they<br />
meet any of the following criteria:<br />
a. The patient is NOT receiving specialized nutritional therapy or NOT<br />
parental nutrition stable.<br />
b. The small intenstine is Greater than 200 cm in length and NOT at least 2<br />
months post resection.<br />
c. The patient has Less than 30% or functioning colon with Less than 15 cm<br />
of intact jejunum or Less than 90 cm of intact jejunum and/or ileum.<br />
156
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SAIZEN<br />
(Continued)<br />
d. The patient does not have an intact stomach and duodenum.<br />
e. The patient does NOT have stable hepatic and renal status (billirubin<br />
Greater than 3 X ULN and Creatinine Greater than 3mL/dL).<br />
f. If the patient has received previous somatropin therapyand he/she has<br />
NOT shown a positive response by showing a reduction on their<br />
dependence on total parenteral nutrition.<br />
I. The diagnosis is for cystic fibrosis, Down syndrome, fibromyalgia, infertility,<br />
obesity, delayed growth and development, familial or idiopathatic short stature in<br />
an adult, dwarfism, skeletal dysplasia, osteogenesis imperfecta, Bloom syndrome,<br />
respiratory failure, inflammatory bowel disease, burn injuries, muscular<br />
dystrophy, Noonan syndrome, Spina Bifida, juvenile rheumatoid arthritis,<br />
osteoporosis, post-traumatic stress disorder, depression, hypertension,<br />
hypophosphatemic rickets or adult short stature.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
157
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SANCUSO<br />
FDA-APPROVED INDICATIONS<br />
Sancuso® is indicated:<br />
A. For prophylaxis of chemotherapy-induced nausea/vomiting in patients receiving<br />
moderately and/or highly emetogenic chemotherapy for up to 5 consecutive days<br />
COVERAGE POLICY<br />
Sancuso® is covered for members who meet the following criteria:<br />
A. Patient must have previous trial/failure on oral Ondansetron OR Granisetron.<br />
NON COVERAGE<br />
Sancuso® is NOT covered for members with the following criteria:<br />
A. Used for non-chemotherapy-induced nausea/vomiting<br />
B. Patient has no previous trial/failure of oral Ondansetron OR Granisetron.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
158
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SIMULECT<br />
FDA-APPROVED INDICATIONS<br />
Simulect® is indicated:<br />
A. Kidney Transplant Rejection Prophylaxis<br />
COVERAGE POLICY<br />
Simulect® is covered for members who meet the following criteria:<br />
A. Patient is undergoing Kidney Transplant<br />
B. AND the surgery is not paid for be Medicare Part B<br />
C. AND B vs. D criteria determines that the medication should be covered through<br />
Medicare Part D<br />
NON COVERAGE<br />
Simulect® is NOT covered for members who meet the following criteria:<br />
A. Transplant other than kidney<br />
B. Service is covered by Medicare Part A/B<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
159
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SOMAVERT<br />
FDA-APPROVED INDICATIONS<br />
Somavert® is indicated:<br />
A. For the treatment of acromegaly in patients who have an inadequate response to<br />
surgery and/or radiation therapy and/or other medical therapies, or for whom<br />
these therapies are not appropriate.<br />
COVERAGE POLICY<br />
Somavert® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as acromegaly.<br />
B. AND the diagnosis has been verified with an elevated IGF-1 level or growth<br />
hormone levels with a glucose tolerance test. (Please review the patient’s chart<br />
notes for documentation).<br />
C. AND the patient has received and failed surgery or radiation therapy. (Please<br />
review the patient’s chart notes for documentation of attempt to remove tumor by<br />
surgery or radiation).<br />
D. AND the patient has tried and failed at least a 3 month trial of Sandostatin® or<br />
octreotide or Somatuline® (lanveotide).<br />
E. AND liver tests (ALT, AST) have been performed and the upper limit of normal<br />
(ULN) is within a range of normal to 3 times ULN.<br />
F. AND the patient will not receive combination therapy that can include<br />
Sandostatin®, octreotide or Somatuline®.<br />
G. AND if the patient has previously received Somavert® therapy, they must have a<br />
reduction in their serum IGF-1 concentration level since starting therapy.<br />
NON COVERAGE<br />
Somavert® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as acromegaly.<br />
B. The patient chart notes do not show an elevated IGF-1 level or growth hormone<br />
levels with a glucose tolerance test.<br />
C. The patient has NOT failed surgery or radiation therapy.<br />
D. The patient has NOT tried and failed a 3 month trial of Sandostatin® or octreotide<br />
or Somatuline®.<br />
E. The patient has liver tests higher than three times the ULN.<br />
F. The patient is receiving Sandostatin®, octreotide or Somatuline® therapy.<br />
G. If the patient has received previous Somavert® therapy and he/she has NOT<br />
shown a reduction in their initial IGF-1 concentration since starting therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
160
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SPORANOX<br />
FDA-APPROVED INDICATIONS<br />
Sporanox® is indicated:<br />
A. For the treatment of infection with aspergillosis, blastomycosis, candidiasis,<br />
histoplasmosis, and onychomychosis<br />
COVERAGE POLICY<br />
Sporanox® is covered for members who meet the following criteria:<br />
A. Must be used for treatment of aspergillosis infection<br />
a. AND the patient must have previous trial/failure of amphotericin B<br />
b. AND chart notes documenting positive culture of aspergillosis as well as<br />
previous failure on amphotericin B must be received<br />
B. OR the patient must be diagnosed with blastomycosis (pulmonary or<br />
extrapulmonary)<br />
a. AND Dose is no more than 400 mg once daily PO.<br />
C. OR the patient must be diagnosed with candidiasis<br />
a. AND the patient has previous tried and failed or had contraindication to<br />
fluconazole<br />
b. AND the trial of fluconazole is documented in chart notes and submitted<br />
D. OR the patient is diagnosed with histoplasmosis<br />
a. AND the dose is no more than 400 mg/day*Note: if diagnosis is<br />
disseminated histoplasmosis treatment should be for 6-12 months<br />
E. OR the patient must be diagnosed with onychomycosis<br />
a. AND the patient must have previous trial and failure or contraindication to<br />
terbinafine<br />
b. AND chart notes are submitted that document trial and failure on<br />
terbinafine<br />
F. Brand name for 100 mg capsule will only be approved with failure on ALL<br />
available generic formulations<br />
NON COVERAGE<br />
Sporanox® is NOT covered for members who meet the following criteria:<br />
A. The patient is not diagnosed with an FDA-approved use (aspergillosis,<br />
blastomycosis, candidiasis, histoplasmosis, onychomycosis)<br />
B. The dosage is greater than 400 mg/day<br />
C. The patient is not properly tried on preceding first-line therapies for aspergillosis,<br />
candidiasis, and onychomycosis as outlined in Sanford Guide<br />
D. Chart notes documenting patient’s previous medication trials as indicated above<br />
are not received or do not address the needed information.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
12 Weeks<br />
161
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SUCRAID<br />
FDA-APPROVED INDICATIONS<br />
Sucraid® is indicated:<br />
A. For oral replacement therapy of the genetically determined sucrase deficiency,<br />
which is part of congenital sucrase-isomaltase deficiency (CSID)<br />
COVERAGE POLICY<br />
Sucraid® is covered for members who meet the following criteria:<br />
A. The patient must be diagnosed with congenital sucrase-isomaltase deficiency<br />
B. AND the diagnosis must be verified with chart notes showing specific genetic<br />
testing showing sucrase deficiency<br />
NON COVERAGE<br />
Sucraid® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with congenital sucrase-isomaltase deficiency<br />
B. The dosage is greater than 2 mL/day<br />
C. Patient has either yeast or glycerin hypersensitivity<br />
D. No genetic testing to specifically show sucrase deficiency has been performed<br />
E. Chart notes documenting genetic testing are not received or do not address the<br />
needed information.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
162
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SUTENT<br />
FDA-APPROVED INDICATIONS<br />
Sutent® is indicated:<br />
A. For the treatment of gastrointestinal stromal tumor after disease progression on or<br />
intolerance to imatinib mesylate.<br />
B. For the treatment of advanced renal cell carcinoma.<br />
COVERAGE POLICY<br />
Sutent® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified oncologist, gastroenterologist or<br />
nephrologist.<br />
B. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy and has been educated on the potential dangers of<br />
Sutent® therapy in pregnancy.<br />
C. AND the patient will NOT be treated with interferon alfa (Roferon-A®,<br />
Pegasys®, Intron-A®, Peg-Intron®) or interleukin-2 (Proleukin®) therapy in<br />
combination with Sutent® treatment. (Please verify the patient’s drug history or<br />
patient chart to verify that the patient is not on interferon alfa or interleukin-2<br />
therapy).<br />
D. AND the diagnosis is documented as treatment for gastrointestinal stromal tumor<br />
(GIST).<br />
a. AND GIST is unresectable and/or metastatic malignant.<br />
b. AND the patient has experienced disease progression while trying or<br />
intolerant to at least a 30-day Gleevec® drug regimen. (Please verify the<br />
patient’s drug history or chart to verify a trial of Gleevec®).<br />
c. AND if the patient has received previous Sutent® therapy, he/she has no<br />
evidence of disease progression (tumor growth) since initiating Sutent®<br />
therapy.<br />
E. AND/OR the diagnosis is documented as metastatic (advanced) renal cell<br />
carcinoma.<br />
a. AND the carcinoma is surgically unresectable.<br />
b. AND if the patient has had previous Sutent® therapy, he/she has no<br />
evidence of disease progression since initiating Sutent® therapy.<br />
NON COVERAGE<br />
Sutent® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a board certified oncologist, gastroenterologist<br />
or nephrologist.<br />
B. If the patient is female and she is pregnant, has plans for pregnancy or has NOT<br />
been educated on the potential dangers of Sutent® therapy in pregnancy.<br />
C. The patient will be receiving interferon alfa or Proleukin® therapy in combination<br />
with Sutent® treatment.<br />
163
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SUTENT<br />
(Continued)<br />
D. The diagnosis is NOT documented as treatment for gastrointestinal stromal tumor<br />
(GIST) or renal cell carcinoma.<br />
E. The diagnosis is documented as treatment for gastrointestinal stromal tumor<br />
(GIST) and they meet any of the following criteria.<br />
a. GIST is resectable.<br />
b. The patient has NOT had a 30-day Gleevec® drug trial.<br />
c. The patient has tried Gleevec® therapy and is NOT intolerant and has<br />
NOT experienced disease progression while receiving a 90-day Gleevec®<br />
drug regimen.<br />
d. If the patient has received previous Sutent® therapy and he/she has<br />
evidence of disease progression (tumor growth) since initiating Sutent®<br />
therapy.<br />
F. The diagnosis is documented as renal cell carcinoma and they meet any of the<br />
following criteria:<br />
a. The carcinoma is not metastatic.<br />
b. The carcinoma can be surgically resectable.<br />
c. If the patient has had previous Sutent® therapy and he/she has evidence of<br />
disease progression since initiating Sutent® therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
164
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SYMLIN<br />
FDA-APPROVED INDICATIONS<br />
Symlin® is indicated:<br />
A. For type-1 diabetes: As an adjunct treatment in patients who use mealtime insulin<br />
therapy and who have failed to achieve desired glucose control despite optimal<br />
insulin therapy.<br />
B. For type-2 diabetes: As an adjunct treatment in patients who use mealtime insulin<br />
therapy and who have failed to achieve desired glucose control despite optimal<br />
insulin therapy, with or without a concurrent sulfonylurea agent and/or<br />
metformin.<br />
COVERAGE POLICY<br />
Symlin® is covered for members who meet the following criteria:<br />
A. The patient does NOT have gastroparesis.<br />
B. AND the patient’s HbA1c is greater than 7% but lower than 9%. (Please verify<br />
the patient’s HbA1c by reviewing the patient’s chart notes).<br />
C. AND the patient has NOT had recurrent severe hypoglycemia during the past 6<br />
months.<br />
D. AND the patient will NOT be taken Symlin® in combination with any of the<br />
following medications that may alter gastrointestinal motility: metoclopramide,<br />
Reglan®, dexpanthenol, Zelnorm®, erythromycin, cisapride, Propulsid®,<br />
clarithromycin, Biaxin®, ranitidine, Zantac®, nizatidine, Axid®, neostigmine,<br />
lidocaine or Amitiza®. (Please verify the use of medications that can increase GI<br />
motility by reviewing the patient’s drug history or chart).<br />
E. AND the patient is over the age of 2 years old.<br />
F. AND the patient is NOT currently receiving a Byetta® drug regimen. (Please<br />
verify if the patient is receiving Byetta® by reviewing their drug history or chart).<br />
G. AND the diagnosis is documented as diabetes type-1.<br />
H. AND the patient has tried and failed at least a three-month optimization of insulin<br />
therapy that includes a trial and failure to short acting insulin. (e.g. Humulin® R,<br />
Novolin® R, Humulin® 70/30, Humulin® 50/50, Humalog®, Novolog®,<br />
Apidra® and Exubra®). (Please verify the use of short-acting insulin by<br />
reviewing the patient’s drug history or chart).<br />
I. AND the patient will continue the use of short-acting insulin during treatment<br />
with Symlin®.<br />
J. AND if the patient has had previous Symlin® therapy, he/she must show a<br />
reduction in their HbA1c since initiating Symlin® therapy.<br />
K. AND/OR the diagnosis is documented as diabetes type-2.<br />
L. AND the patient has tried and failed at least a three-month optimization of insulin<br />
therapy that includes a trial and failure to BOTH short and long-acting insulin.<br />
M. Short acting insulin: (e.g. Humulin® R, Novolin® R, Humulin® 70/30,<br />
Humulin® 50/50, Humalog®, Novolog®, Apidra® and Exubra®). (Please verify<br />
the use of a short-acting insulin by reviewing the patient’s drug history or chart).<br />
165
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SYMLIN<br />
(Continued)<br />
N. Long acting insulin: (e.g. NPH, Humulin® N, Novolin® N, Humulin® 70/30,<br />
Humulin® 50/50, Lente, Humulin® L, Humulin® U, Humalog® 75/30, Lantus®,<br />
Levenir®). (Please verify the use of a long-acting insulin by reviewing the<br />
patient’s drug history or chart).<br />
O. AND the patient will continue the use of short-acting insulin during treatment<br />
with Symlin®.<br />
P. AND if the patient has had previous Symlin® therapy, he/she must show a<br />
reduction in their HbA1c since initiating Symlin® therapy. (Please verify the<br />
HbA1c in the patient’s chart).<br />
NON COVERAGE<br />
Symlin® is NOT covered for members who meet the following criteria:<br />
A. The patient has gastroparesis.<br />
B. The patient’s HbA1c is less than 7% or greater than 9%.<br />
C. The patient has had recurrent severe hypoglycemia during the past 6 months.<br />
D. The patient will be taken Symlin® in combination with any of the following<br />
medications that may alter gastrointestinal motility: metoclopramide, Reglan®,<br />
dexpanthenol, Zelnorm®, erythromycin, cisapride, Propulsid®, clarithromycin,<br />
Biaxin®, ranitidine, Zantac®, nizatidine, Axid®, neostigmine, lidocaine or<br />
Amitiza®.<br />
E. The patient is under the age of 2 years old.<br />
F. The patient is currently receiving a Byetta® drug regimen.<br />
G. The diagnosis is NOT documented as diabetes type-1 or type-2.<br />
H. The patient has NOT tried and failed at least a three-month optimization of insulin<br />
therapy that includes a trial and failure to short acting insulin. (e.g. Humulin® R,<br />
Novolin® R, Humulin® 70/30, Humulin® 50/50, Humalog®, Novolog®,<br />
Apidra® and Exubra®).<br />
I. The patient will NOT continue to use short-acting insulin during treatment with<br />
Symlin®.<br />
J. The diagnosis is documented as diabetes type-2 and they have not tried and failed<br />
a three-month optimization of insulin therapy that includes a trial and failure to<br />
long-acting insulin.<br />
K. If the patient has had previous Symlin® therapy, he/she must show a reduction in<br />
their HbA1c since initiating Symlin® therapy.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
166
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
SYNAREL<br />
FDA-APPROVED INDICATIONS<br />
Synarel® is indicated:<br />
A. For treatment of endometriosis<br />
B. For treatment of precocious puberty<br />
C. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Synarel® is covered for members who meet the following criteria:<br />
A. The patient must be diagnosed with endometriosis<br />
a. AND the patient has previous trial and failure on ALL of the following:<br />
i. 1 form of oral contraceptive pills<br />
ii. Leuprolide<br />
b. AND treatment duration is no longer than 6 months<br />
B. OR the patient must be diagnosed with precocious puberty<br />
a. AND the patient is determined to have significant advancement of bone<br />
age due to significant early maturation<br />
b. AND the patient must be younger than 10 years old<br />
NON COVERAGE<br />
Synarel® is NOT covered for members who meet the following criteria:<br />
F. The patient is NOT diagnosed with endometriosis or precocious puberty<br />
G. The dosage is greater than 800 mcg/day is diagnosed with endometriosis OR 1800<br />
mcg/day if diagnosed with precocious puberty<br />
H. The patient is pregnant (category X)<br />
I. If diagnosed with endometriosis, no previous trial and failure on 1 form of oral<br />
contraceptive pills AND leuprolide<br />
J. Chart notes documenting trials on oral contraceptives pills and leuprolide are not<br />
received or do not address the needed information<br />
K. If diagnosed with precocious puberty, patient is 10 years old or older<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
OBGYN and Endocrinologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
167
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TAMIFLU<br />
FDA-APPROVED INDICATIONS<br />
Tamiflu® is indicated:<br />
A. For prophylaxis for infections due to influenza A or B following close contact<br />
with an infected individual or during a community outbreak<br />
B. For treatment of uncomplicated influenza type A or type B infection in patients<br />
who have been symptomatic for no more than 2 days<br />
C. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Tamiflu® is covered for members who meet the following criteria:<br />
A. The patient must be diagnosed with influenza A or B infection<br />
B. AND the patient must have been symptomatic for no more than 2 days<br />
C. AND treatment is for no more than 5 days<br />
D. OR The patient is receiving prophylaxis<br />
E. AND treatment is for no more than 6 weeks<br />
F. AND if treatment is greater than 10 days a written medical summary documenting<br />
need for more than 10 days must be submitted with request<br />
NON COVERAGE<br />
Tamiflu® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with influenza A or B infection or prophylaxis for<br />
influenza A or B infection after contact with infected individual<br />
B. The request is for more than 10 capsules (for prophylaxis, patient may fill up to 6<br />
weeks if initial 10 days is not effective)<br />
C. more than 10 days of therapy, a written medical summary illustrating need for<br />
additional treatment due to inefficacy of initial therapy is not received<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Up to 6 weeks<br />
168
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TARCEVA<br />
FDA-APPROVED INDICATIONS<br />
Tarceva® is indicated:<br />
A. For the monotherapy treatment of patients with locally advanced or metastatic<br />
non-small cell lung cancer after failure of at least one prior chemotherapy<br />
regimen.<br />
B. For the first-line treatment of patients with locally advanced, unresectable or<br />
metastatic pancreatic cancer when used in combination with gemcitabine.<br />
COVERAGE POLICY<br />
Tarceva® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified oncologist or nephrologist.<br />
B. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy and has been educated on the potential dangers of<br />
Tarceva® therapy in pregnancy.<br />
C. AND the diagnosis is documented as treatment for non-small cell lung cancer.<br />
a. AND the cancer is locally advanced or metastatic (Stage 3 or Stage 4).<br />
b. AND the patient’s disease has progressed after completing or had<br />
unacceptable toxicity to at least one of the following chemotherapy<br />
regimens:<br />
i. Platinum-based regimen: (e.g. carboplatin, Paroplatin®, cisplatin,<br />
Platinol®, oxaliplatin, or Eloxatin®)<br />
ii. axoid-based regimen: (e.g. paclitaxel, Taxol®, Onxol®,<br />
Abraxane®, docetaxel, or Taxotere®).<br />
c. AND Tarceva® therapy will NOT be used in combination with any other<br />
chemotherapy agent. (Please verify that the patient is not receiving<br />
additional chemotherapy by reviewing the patient’s drug history or chart.)<br />
d. AND if the patient has received previous Tarceva® therapy, the provider<br />
has evidence of clinical improvement from the pretreatment report by<br />
showing no increase in tumor size and/or progression of disease.<br />
D. AND/OR the diagnosis is documented as pancreatic cancer.<br />
a. AND the cancer is surgically unresectable.<br />
b. AND the cancer is locally advanced or metastatic (Stage 3 or Stage 4).<br />
c. AND the patient will and/or has received Tarceva® therapy in<br />
combination with gemcitabine (Gemzar®) on a 4 and/or 8 week cycle.<br />
d. AND if the patient has had previous Tarceva® therapy, the provider has<br />
evidence of clinical improvement from the pretreatment report by showing<br />
no increase in tumor size and/or progression of disease.<br />
169
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TARCEVA<br />
(Continued)<br />
NON COVERAGE<br />
Tarceva® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a board certified oncologist or nephrologist.<br />
B. If the patient is female and of childbearing years and she is pregnant, has plans for<br />
pregnancy or has NOT been educated on the potential dangers of Tarceva®<br />
therapy in pregnancy.<br />
C. The diagnosis is NOT documented as non-small cell lung cancer or pancreatic<br />
cancer.<br />
D. AND the diagnosis is documented as treatment for non-small cell lung cancer and<br />
the patient meets any of the following criteria:<br />
a. The cancer is NOT locally advanced or metastatic (Stage 3 or Stage 4).<br />
b. The patient’s disease has NOT progressed after completing a platinumbased<br />
or taxoid-based chemotherapy regimen.<br />
c. The patient did NOT complete or had NO unacceptable toxicity to a<br />
platinum-based or taxoid based chemotherapy regimen.<br />
i. Tarveca® therapy will or has been used in combination with<br />
another chemotherapy agent.<br />
ii. If the patient has received previous Tarceva® therapy and the<br />
provider has NO evidence of clinical improvement from the<br />
pretreatment report or shows an increase in tumor size and/or<br />
progression of disease.<br />
E. AND/OR the diagnosis is documented as pancreatic cancer and the patient meets<br />
any of the following criteria:<br />
a. The cancer is surgically resectable.<br />
b. The cancer is NOT locally advanced or metastatic (Stage 3 or Stage 4).<br />
c. The patient will NOT or has NOT received Tarceva® therapy in<br />
combination with gemcitabine (Gemzar®) on a 4 and/or 8 week cycle.<br />
d. If the patient has had previous Tarceva® therapy and the provider has NO<br />
evidence of clinical improvement from the pretreatment report or shows<br />
an increase in tumor size and/or progression of disease.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
170
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TARGRETIN<br />
FDA-APPROVED INDICATIONS<br />
Targretin® is indicated:<br />
A. Oral: For the treatment of cutaneous manifestations of cutaneous T-cell<br />
lymphoma (CTCL)<br />
B. Topical: For treatment of stage 1A or 1B cutaneous T-cell lymphoma who have<br />
refractory or persistent disease after other therapies or who have not tolerated<br />
other therapies<br />
COVERAGE POLICY<br />
Targretin® is covered for members who meet the following criteria:<br />
A. The patient must be diagnosed with cutaneous manifestations of cutaneous T-cell<br />
lymphoma (CTCL)<br />
B. AND the patient must have advanced disease (if oral is used)<br />
C. OR the patient must be diagnosed with stage 1A or 1B cutaneous T-cell<br />
lymphoma with cutaneous manifestations<br />
D. AND the patient has previously failed treatment with at least 1 (ONE) topical<br />
steroid OR phototherapy<br />
NON COVERAGE<br />
Targretin® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with cutaneous manifestations of cutaneous T-cell<br />
lymphoma<br />
B. If requesting oral, the patient does NOT have advanced disease<br />
C. If requesting topical, the patient does NOT have stage 1A or 1B<br />
D. If requesting topical, the patient has NOT previously attempted treatment with at<br />
least 1 (ONE) topical steroid OR phototherapy<br />
E. Chart notes documenting previous trial on topical steroid(s) or phototherapy are<br />
not received or do not address the needed information<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Dermatologist and Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
171
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TASIGNA<br />
FDA-APPROVED INDICATIONS<br />
Tasigna® is indicated:<br />
A. For the treatment of chronic phase and accelerated phase Philadelphia<br />
chromosome positive (Ph+) chronic myelogenous leukemia (CML) in patients<br />
resistant to or intolerant to prior therapy that included imatinib.<br />
COVERAGE POLICY<br />
Tasigna® is covered for members who meet the following criteria:<br />
A. The patient must be diagnosed with Philadelphia chromosome positive chronic<br />
myelogenous leukemia<br />
B. AND the dosing must be 400 mg twice daily<br />
C. AND the patient must have previous trial and failure or intolerance to prior<br />
therapy that included imatinib<br />
D. AND chart notes documenting previous trial/failure or intolerance to imatinib<br />
therapy must be received<br />
NON COVERAGE<br />
Tasigna® is NOT covered for members who meet the following criteria:<br />
A. The patient is NOT diagnosed with Philadelphia chromosome positive chronic<br />
myelogenous leukemia<br />
B. The request is for more than 400 mg twice daily<br />
C. The patient has NOT previously attempted treatment with imatinib<br />
D. Chart notes documenting previous trial on imitinib are not received or do not<br />
address the needed information<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
172
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TEV-TROPIN<br />
FDA-APPROVED INDICATIONS<br />
Somatropin is indicated (Not all branded medications have each indication listed below.<br />
Please refer to reference symbol for actual indication):<br />
A. For the long-term treatment of pediatric patients who have growth failure due to<br />
an inadequate secretion of endogenous growth hormone.<br />
B. For the long-term treatment of pediatric patients who have growth failure due to<br />
Prader-Willi syndrome.*<br />
C. For long-term replacement therapy in adults with growth hormone deficiency of<br />
either childhood or adult-onset etiology.*<br />
D. For the treatment of short stature associated with Turner syndrome in patients<br />
whose epiphyses are not closed.<br />
E. For the long-term treatment of idiopathic short stature, also called non-growth<br />
hormone deficient short stature, defined by height SDS less than or equal to -2.25<br />
and associated with growth rates unlikely to permit attainment of adult height in<br />
the normal range, in pediatric patients whose epiphyses are not closed and for<br />
whom diagnostic evaluation excludes other causes associated with short stature<br />
that should be observed or treated by other means.<br />
F. For replacement of endogenous growth hormone in adults with growth hormone<br />
deficiency who meet both of the following 2 criteria:<br />
a. Adult onset: Patients who have growth hormone deficiency either alone,<br />
or with multiple disease, hypothalamic disease, surgery, radiation therapy,<br />
or trauma.<br />
b. Child onset: Patients who were growth-hormone-deficient during<br />
childhood who have growth hormone deficiency confirmed as an adult.<br />
G. For the long-term treatment of children with growth failure due to inadequate<br />
secretion of endogenous growth hormone.<br />
H. For the treatment of growth failure associated with chronic renal insufficiency up<br />
to the time of renal transplantation.<br />
I. For the long-term treatment of growth failure associated with Turner syndrome.<br />
J. For the replacement of endogenous growth hormone in patients with adult growth<br />
hormone deficiency who meet both of the following 2 criteria:<br />
a. Adult onset: Patients who have adult growth hormone deficiency either<br />
alone or with multiple hormone deficiencies (hypopituitarism) as a result<br />
of pituitary disease, hypothalamic disease, surgery, radiation therapy, or<br />
trauma.<br />
b. Child onset: Patients who were growth hormone deficient during<br />
childhood, confirmed as an adult.<br />
K. For the treatment of HIV patients with wasting or cachexia to increase lean body<br />
mass and body weight, and improve physical endurance. Concomitant<br />
antiretroviral therapy is necessary.<br />
L. For the treatment of short bowel syndrome in patients receiving specialized<br />
nutritional support.<br />
173
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TEV-TROPIN<br />
(Continued)<br />
COVERAGE POLICY<br />
Somatropin® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified endocrinologist or infectious disease<br />
specialist.<br />
B. The request for somatropin is the formulary covered agent. (Please review drug<br />
formulary to ensure prior authorization is for the formulary covered medication).<br />
C. The patient is 20 years of age or older.<br />
D. AND the patient does NOT have any evidence of active malignancy.<br />
E. AND the diagnosis is documented as growth hormone deficiency in an adult<br />
needing replacement with endogenous growth hormone.<br />
a. AND the patient has a biochemical diagnosis of growth hormone<br />
deficiency, means of a negative response to 2) standard growth hormone<br />
stimulation tests [Max peak less than 5ng/mL by RIA or Less than 2.5<br />
ng/mL by IRMA] OR an IGF-1 level that is two standard deviations below<br />
normal for the patient’s age group. (Please verify the growth hormone or<br />
IGF-1 level in the patient’s chart notes and ensure the tests were<br />
preformed within 3 months of the initial request).<br />
b. AND the growth hormone deficiency is due to at least one of the<br />
following etiologies:<br />
i. Pituitary or hypothalamus surgery<br />
ii. Pituitary or hypothalamus disease.<br />
iii. Pituitary or hypothalamus injury.<br />
iv. Radiation therapy.<br />
v. Growth-hormone deficiency during childhood. (Requires an<br />
additional stimulation test during adulthood).<br />
c. AND the patient has symptoms of growth hormone deficiency that<br />
includes one of the following:<br />
i. Reduced bone density of more than (1) standard deviation below<br />
the age and gender-specific mean.<br />
ii. Evidence of cardiac decompensation defined as reduced ejection<br />
fracture of Less than 50%.<br />
d. AND if the patient has received previous somatropin therapy, he/she has<br />
shown an improvement in quality of life and/or symptoms (bone mass,<br />
muscle mass, strength, body fat and/or cholesterol).<br />
F. AND/OR the diagnosis is documented as AIDS wasting or AIDS cachexia.<br />
a. AND the patient has had an involuntary weight loss of Greater than 10%<br />
of pre-illness baseline body weight or body mass index (BMI) Less than<br />
20 kg/m 2 in the absence of a concurrent illness or medical condition other<br />
than HIV infection that may cause weight loss.<br />
174
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TEV-TROPIN<br />
(Continued)<br />
b. AND the patient has failed to respond to a 30-day drug regimen of<br />
megestrol (Megace®) AND an anabolic steroid (e.g. Testim®,<br />
Androgel®, testosterone enanthate, testosterone cypionate, Testoderm®,<br />
Androderm®, methyltestosterone, or fluoxymesterone). (Please verify the<br />
use of megestrol and an anabolic steroid by reviewing the patient’s drug<br />
history or chart).<br />
c. AND if the patient has received previous somatropin therapy, he/she must<br />
show a positive response to treatment by maintaining or increasing their<br />
initial weight and/or muscle mass before initiating somatropin therapy.<br />
G. AND/OR the diagnosis is documented as a patient with short bowel syndrome.<br />
a. AND the patient is receiving specialized nutritional therapy and parental<br />
nutrition stable.<br />
b. AND the small intenstine is Less than 200 cm in length and at least 2<br />
months post resection.<br />
c. AND the patient has 30% or greater functioning colon with at least 15 cm<br />
of intact jejunum or at least 90 cm of intact jejunum and/or ileum.<br />
d. AND the patient has an intach stomach and duodenum.<br />
e. AND the patient has stable hepatic and renal status (billirubin Less than 3<br />
X ULN and Creatinine Less than 3mL/dL).<br />
f. AND if the patient has received previous somatropin therapy, he/she must<br />
show a positive response by showing a reduction on their dependence on<br />
total parenteral nutrition.<br />
NON COVERAGE<br />
Somatropin® is NOT covered for members with the following criteria:<br />
A. The prescribing physician is NOT a board certified endocrinologist or infectious<br />
disease specialist.<br />
B. The request for somatropin is NOT the formulary covered agent.<br />
C. The patient has evidence of active malignancy.<br />
D. The patient is NOT 20 years of age or older.<br />
E. The diagnosis is NOT documented as growth hormone deficiency in an adult<br />
needing replacement with endogenous growth hormone, AIDS wasting or AIDS<br />
cachexia or short bowel syndrome.<br />
F. If the diagnosis is documented as growth hormone deficiency in adult and they<br />
meet any of the following criteria:<br />
a. The patient does NOT have a biochemical diagnosis of growth hormone<br />
deficiency to 2 standard growth hormone stimulation tests or an IGF-1<br />
level that is NOT two standard deviations below normal for the patient’s<br />
age group.<br />
b. The growth hormone deficiency is NOT due to at least one of the<br />
following etiologies:<br />
i. Pituitary or hypothalamus surgery<br />
175
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TEV-TROPIN<br />
(Continued)<br />
ii. Pituitary or hypothalamus disease.<br />
iii. Pituitary or hypothalamus injury.<br />
iv. Radiation therapy.<br />
v. Growth-hormone deficiency during childhood.<br />
c. The patient does NOT have symptoms of growth hormone deficiency that<br />
includes one of the following:<br />
i. Reduced bone density of more than (1) standard deviation below<br />
the age and gender-specific mean.<br />
ii. Evidence of cardiac decompensation defined as reduced ejection<br />
fracture of Less than 50%.<br />
d. If the patient has received previous somatropin therapy and he/she does<br />
not show an improvement In quality of life and/or symptoms (bone mass,<br />
muscle mass, strength, body fat and/or cholesterol).<br />
G. If the diagnosis is documented as AIDS wasting or AIDS cachexia and they meet<br />
any of the following criteria:<br />
a. The patient has NOT had an involuntary weight loss of Greater than 10%<br />
of pre-illness baseline body weight or body mass index (BMI) Less than<br />
20 kg/m 2 .<br />
b. The patient has had an involuntary weight loss of Greater than 10% of preillness<br />
baseline body weight or body mass index (BMI) Less than 20<br />
kg/m2 but the weight loss happened with a concurrent illness or medical<br />
condition other than HIV infection.<br />
c. The patient has NOT failed a 30 day drug regimen of megestrol<br />
(Megace®) AND an anabolic steroid.<br />
d. If the patient has received previous somatropin therapy and he/she has<br />
NOT shown a positive response to treatment by maintaining or increasing<br />
their initial weight before initiating somatropin therapy.<br />
H. If the diagnosis is documented as a patient with short bowel syndrome and they<br />
meet any of the following criteria:<br />
a. The patient is NOT receiving specialized nutritional therapy or NOT<br />
parental nutrition stable.<br />
b. The small intenstine is Greater than 200 cm in length and NOT at least 2<br />
months post resection.<br />
c. The patient has Less than 30% or functioning colon with Less than 15 cm<br />
of intact jejunum or Less than 90 cm of intact jejunum and/or ileum.<br />
d. The patient does not have an intact stomach and duodenum.<br />
e. The patient does NOT have stable hepatic and renal status (billirubin<br />
Greater than 3 X ULN and Creatinine Greater than 3mL/dL).<br />
f. If the patient has received previous somatropin therapyand he/she has<br />
NOT shown a positive response by showing a reduction on their<br />
dependence on total parenteral nutrition.<br />
176
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TEV-TROPIN<br />
(Continued)<br />
I. The diagnosis is for cystic fibrosis, Down syndrome, fibromyalgia, infertility,<br />
obesity, delayed growth and development, familial or idiopathatic short stature in<br />
an adult, dwarfism, skeletal dysplasia, osteogenesis imperfecta, Bloom syndrome,<br />
respiratory failure, inflammatory bowel disease, burn injuries, muscular<br />
dystrophy, Noonan syndrome, Spina Bifida, juvenile rheumatoid arthritis,<br />
osteoporosis, post-traumatic stress disorder, depression, hypertension,<br />
hypophosphatemic rickets or adult short stature.<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
177
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TORISEL<br />
FDA-APPROVED INDICATIONS<br />
Torisel® is indicated:<br />
A. For the treatment of advanced renal cell carcinoma<br />
COVERAGE POLICY<br />
Torisel® is covered for members who meet the following criteria:<br />
A. Verification of B vs. D criteria as per CMS regulations<br />
a. Incident to a physician’s service<br />
B. AND the patient must be diagnosed with renal cell carcinoma<br />
C. AND the patient must have advanced disease as indicated by 1 (ONE) of the<br />
following<br />
a. Patients with metastatic disease<br />
b. Patients with locally advanced disease not curable with resection<br />
D. AND must be prescribed by oncologist or nephrologist<br />
NON COVERAGE<br />
Torisel® is NOT covered for members who meet the following criteria:<br />
A. The medication is a Part B medication per CMS guidelines<br />
B. The diagnosis is NOT renal cell carcinoma<br />
C. The patient does NOT have advanced disease<br />
D. Prescribing physician is NOT an oncologist or nephrologist<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
178
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TRACLEER<br />
FDA-APPROVED INDICATIONS<br />
Tracleer® is indicated:<br />
A. For the treatment of pulmonary arterial hypertension in patients with World<br />
Health Organization Class III or IV symptoms, to improve exercise ability and<br />
decrease the rate of clinical worsening.<br />
COVERAGE POLICY<br />
Tracleer® is covered for members who meet the following criteria:<br />
A. If the patient is female and is of childbearing age, she is NOT pregnant, does<br />
NOT have plans for pregnancy and is using a reliable method of contraception.<br />
(contraindicated).<br />
B. AND the patient is not on a drug regimen for cyclosporine (eg. Gengraf®,<br />
Neoral®, Sandimmune®) and/or glyburide (eg. Diabeta®, Micronase®,<br />
Glynase®). (contraindicated). (Verification can be made by reviewing the<br />
patient’s drug history or patient’s chart).<br />
C. AND the patient does not have elevated aminotransferases (eg. AST, ALT)<br />
greater than three (3) times the upper limit of normal and/or bilirubin greater than<br />
two (2) times the upper limit of normal. (Verification can be made by reviewing<br />
the patient’s drug history or patient’s chart).<br />
D. AND the prescribing provider is a pulmonologist, and/or cardiologist or has<br />
obtained a consult from the listed specialties.<br />
E. AND the diagnosis is documented as pulmonary arterial hypertension.<br />
F. AND the patient does NOT have pulmonary veno-occlusive disease (PVOD),<br />
(contraindicated).<br />
G. AND the patient has had an adequate trial and failure (4 weeks or more) or is not<br />
a candidate for calcium channel blocker therapy. (eg. amlodipine, Norvasc®,<br />
nifedipine, Adalat CC®, Nifedical XL®, Procardia®, Procardia XL®, diltiazem,<br />
Cardizem®, Cartia XT®, Dilacor XR®, Diltia XT®, Tiazac®, Norvasc®,<br />
amlodipine, or Cardizem CD®). (Verification can be made by reviewing the<br />
patient’s drug history or patient’s chart).<br />
H. AND the patient will NOT receive combination therapy with a prostacyclin<br />
(Flolan®, Ventavis®, Remodulin®) or a phosphodiesterase type-5 inhibitor<br />
(Viagra®, Revatio®) agent. Combination therapy has not been approved by the<br />
FDA. (Please verify that the patient is not on duplicate therapy by reviewing the<br />
patient’s drug history or chart).<br />
I. AND the diagnosis is documented as pulmonary arterial hypertension class III or<br />
IV defined by the World Health Organization (WHO).<br />
J. AND the diagnosis is NOT documented as pulmonary arterial hypertension class I<br />
or II defined by the WHO.<br />
K. AND therapy is being prescribed to improve exercise ability.<br />
179
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TRACLEER<br />
(Continued)<br />
L. AND if the patient has received previous Tracleer® therapy, the patient must see<br />
an improvement in their exercise ability (walking distance), dyspnea fatigue, an<br />
improvement in functional status (New York Heart Association (NYHA<br />
functional class) and/or NO clinical worsening of pulmonary hypertension.<br />
NON COVERAGE<br />
Tracleer® is NOT covered for members with the following criteria:<br />
A. A female patient of child bearing age that is pregnant or has plans for pregnancy<br />
or is NOT using a reliable form of contraception.<br />
B. The patient will be taking cyclosporine and/or glyburide therapy concurrently<br />
with Tracleer® therapy.<br />
C. The patient has elevated aminotransferase levels greater than three (3) times the<br />
upper limit of normal and/or bilirubin greater than two (2) times the upper limit of<br />
normal.<br />
D. The prescribing provider is NOT a pulmonologist, and/or cardiologist or obtained<br />
a consult from the listed specialties.<br />
E. The diagnosis is NOT listed as pulmonary hypertension.<br />
F. The patient has pulmonary veno-occlusive disease (PVOD).<br />
G. The patient is a candidate for calcium channel blocker therapy (CCB) and has<br />
NOT had an adequate 4-week trial and failure to a CCB drug regimen.<br />
H. The patient will receive Revatio®, Flolan®, Ventavis®, or Remodulin® therapy<br />
while receiving a Tracleer® drug regimen. (Please verify that the patient does not<br />
have duplicate therapy by reviewing the patient’s drug history or chart).<br />
I. The patient’s pulmonary arterial hypertension has NOT been classified as class III<br />
or IV defined by the WHO.<br />
J. The patient’s pulmonary arterial hypertension has been classified as class I or II<br />
by the WHO.<br />
K. Tracleer® is NOT being prescribed to improve exercise ability.<br />
L. If the patient has received previous Tracleer® therapy and they have NOT seen an<br />
improvement in their exercise ability (walking distance), dyspnea fatigue and/or<br />
an improvement in their NYHA functional classification.<br />
M. Evidence of diagnosis, WHO classification, lab values and exercise ability is<br />
NOT documented in the patient’s chart notes provided by prescribing provider.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Pulmonologist<br />
AUTHORIZATION PERIOD<br />
6 months<br />
180
FDA-APPROVED INDICATIONS<br />
Tretinoin is indicated:<br />
A. Acne Vulgaris<br />
B. Cystic Acne<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TRETINOIN PRODUCTS<br />
COVERAGE POLICY<br />
Avita® is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with Acne Vulgaris or Cystic Acne<br />
B. AND failure to topical benzoyl peroxide products and topical antibiotics<br />
NON COVERAGE<br />
Tretinoin is NOT covered for members with the following criteria:<br />
A. Using for facial wrinkles or other cosmetic indications<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
3 months<br />
181
FDA APPROVED INDICATIONS<br />
A. Hyperlipopoteinemia<br />
B. Hypertriglyceridemia<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TRICOR<br />
COVERAGE POLICY<br />
Tricor is covered for members who meet the following criteria:<br />
A. Failure or contraindications to generic Fenofibrate<br />
NON COVERAGE<br />
Tricor is not covered for members who meet the following criteria:<br />
A. No failure or contraindications to Fenofibrate<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart Notes<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
182
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TYKERB<br />
FDA-APPROVED INDICATIONS<br />
Tykerb® is indicated:<br />
A. In combination with capecitabine, for the treatment of patients with advanced or<br />
metastatic breast cancer whose tumors over express HER2 and who have received<br />
prior therapy including an anthracycline, a taxane, and trastuzumab.<br />
COVERAGE POLICY<br />
Tykerb® is covered for members who meet the following criteria:<br />
A. The prescribing physician is a board certified oncologist.<br />
B. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy and has been educated on the potential dangers of<br />
Tarceva® therapy in pregnancy.<br />
C. AND the diagnosis is documented as treatment for breast cancer.<br />
D. AND the cancer is advanced or metastatic (Stage 3 or Stage 4).<br />
E. AND a fluorescence in situ hybridization (FISH) or immunohistochemistry (IHC)<br />
test has been preformed to confirm HER2 protein over expression with a score of<br />
+2 or better.<br />
F. AND patient’s disease has progressed after completing or had unacceptable<br />
toxicity to all three of the following chemotherapy regimens:<br />
a. Anthracycline regimen: (e.g. daunorubicin, DaunoXome®, doxorubicin,<br />
Adriamycin®, Doxil®, epirubicin, Ellence®, idarubicin, Idamycin®).<br />
b. Taxane regimen: (e.g. paclitaxel, Taxol®, Onxol®, Abraxane®,<br />
docetaxel, or Taxotere®).<br />
c. trastuzumab (Herceptin®).<br />
G. AND Tykerb® therapy will be or is being used in combination with capecitabine<br />
(Xeloda®). (Please verify that the patient is receiving Xeloda® therapy by<br />
reviewing the patient’s drug history or chart.)<br />
H. AND Tykerb® therapy will NOT be used in combination with an anthracycline<br />
regimen, Herceptin® or a Taxane regimen.<br />
I. AND if the patient has received previous Tykerb® therapy, the provider has<br />
evidence of clinical improvement from the pretreatment report by showing no<br />
increase in tumor size and/or progression of disease.<br />
NON COVERAGE<br />
Tykerb® is NOT covered for members who meet the following criteria:<br />
A. The prescribing physician is NOT a board certified oncologist.<br />
B. If the patient is female and of childbearing years and is pregnant, has plans for<br />
pregnancy or has NOT been educated on the potential dangers of Tarceva®<br />
therapy in pregnancy.<br />
C. The diagnosis is NOT documented as treatment for breast cancer.<br />
D. The diagnosis is documented as treatment for breast cancer and the patient meets<br />
any of the following criteria:<br />
183
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TYKERB<br />
(Continued)<br />
E. The cancer is NOT advanced or NOT metastatic (Stage 3 or Stage 4).<br />
F. A fluorescence in situ hybridization (FISH) or immunohistochemistry (IHC) test<br />
has NOT been preformed to confirm HER2 protein over expression.<br />
G. A FISH or IHC test has been performed but the score was less than +2.<br />
H. The patient has NOT completed and NOT failed an anthracycline, taxane and<br />
Herceptin® drug regimen.The patient’s disease has NOT progressed after<br />
completing an anthracycline, taxane and Herceptin® drug regimen.<br />
I. Tykerb® therapy will NOT be or is NOT being used in combination with<br />
capecitabine (Xeloda®).<br />
J. Tykerb® therapy will be used in combination with an anthracycline regimen,<br />
Herceptin® or a Taxane regimen.<br />
K. If the patient has received previous Tykerb® therapy and the provider has NO<br />
evidence of clinical improvement from the pretreatment report or shows an<br />
increase in tumor size and/or progression of disease.<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
184
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TYZEKA<br />
FDA-APPROVED INDICATIONS<br />
Tyzeka® is indicated:<br />
A. For the treatment of chronic hepatitis B in adults with evidence of active viral<br />
replication and either evidence of persistent elevations in serum aminotransferases<br />
(ALT or AST) or histologically active disease.<br />
COVERAGE POLICY<br />
Tyzeka® is covered for members who meet the following criteria:<br />
A. Patient is age 16 years or older.<br />
B. AND the prescribing provider is a gastroenterologist or trained in infectious<br />
disease or has obtained a consult from the listed specialties.<br />
C. AND the patient has been diagnosed with chronic hepatitis B.<br />
D. AND the patient has evidence of a positive HBsAg (+ or -) serological marker for<br />
greater than 6 months OR evidence by a liver biopsy showing chronic hepatitis.<br />
(Please verify that the patient has a HBsAg serological marker for greater than 6<br />
months or a positive liver biopsy by reviewing the patient’s drug history or chart).<br />
E. AND the patient has a Hepatitis B viral load greater than 100,000 copies per ml.<br />
F. AND the patient has elevations in liver aminotransferases (ALT or AST) that are<br />
two (2) times greater than normal.<br />
G. AND the patient has been tested for HIV. (Tyzeka® therapy can cause HIV<br />
resistance in untreated HIV infection).<br />
H. AND if the patient has received previous Tyzeka® treatment, there is documented<br />
clinical improvement shown by a drop in viral load or reduction in the patient’s<br />
liver aminotransferases. (Please verify patient’s chart notes to verify drop in viral<br />
load or reduction in liver aminotransferases from their starting level).<br />
I. AND the patient is not receiving duplicate therapy that includes Hepsera®,<br />
Baraclude®, Epivir®, Intron A® and/or Infergen®. (Please verify that the patient<br />
does not have duplicate therapy by reviewing the patient’s drug history or chart).<br />
J. AND evidence of diagnosis, serological markers, liver biopsy, viral load, and<br />
liver aminotransferases is documented in patient’s chart.<br />
NON COVERAGE<br />
Tyzeka® is NOT covered for members with the following criteria:<br />
A. Patient is under the age of 16 years old.<br />
B. The provider is NOT a gastroenterologist, trained in infectious disease or obtained<br />
a consult from the listed specialties.<br />
C. Patient has NOT been diagnosed with chronic hepatitis B.<br />
D. Patient has NO evidence of a Hepatitis B serological marker for greater than 6<br />
months OR evidence by a positive liver biopsy.<br />
E. Patient does NOT have a Hepatitis B viral load greater than 100,000 copies per<br />
ml.<br />
185
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
TYZEKA<br />
(Continued)<br />
F. Patient does NOT have liver aminotransferases (ALT or AST) that are two (2)<br />
times greater than normal.<br />
G. Patient has NOT been tested for HIV.<br />
H. Patient is on duplicate therapy that can include one of the following: Hepsera®,<br />
Baraclude®, Epivir®, Intron-A®, and or Infergen®.<br />
I. Prescriber has provided no evidence of diagnosis, serological markers, viral load,<br />
duplicate therapy or liver aminotransferases.<br />
REQUIRED MEDICAL INFORMATIONS<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Infectious Disease<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
186
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
VESANOID<br />
FDA-APPROVED INDICATIONS<br />
Vesanoid® is indicated:<br />
A. For the treatment of remission induction in acute promyelocytic leukemia<br />
COVERAGE POLICY<br />
Vesanoid® is covered for members who meet the following criteria:<br />
A. The patient is diagnosed with acute promyelocytic leukemia<br />
B. AND the medication is being used for induction of remission<br />
C. AND the patient has no previous history of trial on Vesanoid®<br />
D. AND the request is for no more than 90 days<br />
E. AND the request comes from an oncologist<br />
NON COVERAGE<br />
Vesanoid® is NOT covered for members who meet the following criteria:<br />
A. The diagnosis is NOT acute promyelocytic leukemia<br />
B. The medication is being used for maintenance therapy<br />
C. The patient has previous history of trial of Vesanoid®<br />
D. The request is for more than 90 days<br />
E. The request does not come from an oncologist<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
90 days<br />
187
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
VFEND<br />
FDA-APPROVED INDICATIONS<br />
Vfend® is indicated:<br />
A. For the treatment of infection with invasive aspergillosis, candidiasis, furariosis,<br />
Scedosporium apiospermum<br />
COVERAGE POLICY<br />
Vfend® is covered for members who meet the following criteria:<br />
A. The patient is diagnosed with invasive aspergillosis<br />
a. AND the patient has had previous trial and failure or contraindication to<br />
itraconazole*If aspergillosis infection is extrapulmonary no previous trial<br />
is required<br />
b. AND chart notes documenting trial and failure or contraindication to<br />
itraconazole are received<br />
B. OR the patient is diagnosed with candidiasis<br />
a. AND the patient has previous trial and failure or contraindication to<br />
BOTH fluconazole and itraconazole<br />
b. AND chart notes documenting trial and failure or contraindication to<br />
itraconazole are received<br />
C. OR the patient is diagnosed with furariosis or Scedosporium sp.<br />
a. AND Vfend® is being used as salvage therapy due to failure of other<br />
therapies<br />
b. AND chart notes documenting previous treatment failures is received<br />
NON COVERAGE<br />
Vfend® is NOT covered for members who meet the following criteria:<br />
A. The diagnosis is NOT invasive aspergillosis, candidiasis, furariosis, or<br />
Scedosporium sp. infection<br />
B. If being used for aspergillosis or candidiasis, previous medication regimens as<br />
noted have not been utilized<br />
C. If being used for furariosis or Scedosporium sp., NOT being used for salvage<br />
therapy<br />
D. Chart notes documenting previous regimens is not received or do not address<br />
needed information<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Infectious Disease<br />
AUTHORIZATION PERIOD<br />
1 month<br />
188
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
VIDAZA<br />
FDA-APPROVED INDICATIONS<br />
Vidaza® is indicated:<br />
A. For the treatment of myelodysplastic syndrome.<br />
COVERAGE POLICY<br />
Vidaza® is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
a. Incident to a physician’s service<br />
B. AND the patient is diagnosed with myelodysplastic syndrome<br />
C. AND the patient has low probability to respond to immunosuppressive therapy<br />
(IST)<br />
D. AND chart notes documenting low serum epopoietin as well as documentation<br />
showing reasoning for patient’s low probability to respond to IST<br />
E. AND for extended authorization, patient is showing benefit from treatment<br />
NON COVERAGE<br />
Vidaza® is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT myelodysplastic syndrome<br />
C. Patient has HIGH probability to respond to IST<br />
D. Chart notes documenting epopoietin levels and low probability for benefit from<br />
IST are not received or do not address the needed information<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Oncologist<br />
AUTHORIZATION PERIOD<br />
4 months<br />
189
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
VIMPAT<br />
FDA-APPROVED INDICATIONS<br />
All FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Vimpat® is covered for members who meet the following criteria:<br />
A. A.Patient will receive Vimpat as an adjunctive anticonvulsant.<br />
B. Patient has a documented trial/failure/contraindication to two or more of the<br />
following:<br />
a. Carbamazepine<br />
b. Divalproex<br />
c. Gabapentin<br />
d. Lamotrigine<br />
e. Levetiracetam<br />
f. Oxcarbazepine<br />
g. Phenytoin<br />
h. Pregabalin<br />
i. Tiagabine<br />
j. Topiramate<br />
k. Valproic acid<br />
l. Zonisamide<br />
REQUIRED MEDICAL INFORMATION<br />
The following copies of chart notes/laboratory reports are required:<br />
A. Documentation showing that Vimpat will be given as an adjunctive<br />
anticonvulsant<br />
B. Documentation showing that the patient has had a previous<br />
trial/failure/contraindication to two or more of the following:<br />
a. Carbamazepine<br />
b. Divalproex<br />
c. Gabapentin<br />
d. Lamotrigine<br />
e. Levetiracetam<br />
f. Oxcarbazepine<br />
g. Phenytoin<br />
h. Pregabalin<br />
i. Tiagabine<br />
j. Topiramate<br />
k. Valproic acid<br />
l. Zonisamide<br />
AGE RESTRICTIONS<br />
Covered for 17 years and older<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
190
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
VISTIDE<br />
FDA-APPROVED INDICATIONS<br />
Vistide® is indicated:<br />
A. Cytomegalovirus<br />
B. Cytomegalovirus retinitis<br />
C. Cytomegalovirus retinitis prophylaxis<br />
D. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Vistide® is covered for members who meet the following criteria:<br />
A. Patient is diagnosed with approved indication as stated above<br />
B. AND patient has AIDS<br />
C. AND patient is NOT taking one of the following medications:<br />
a. Aminoglycosides<br />
b. Amphotericin B<br />
c. Foscarnet<br />
d. NSAIDs<br />
e. Pentamidine<br />
f. Tacrolimus<br />
g. Vancomycin<br />
D. AND (in prophylaxis patients) CD4+ count is Less than 100-150 cells/ mm 3<br />
E. AND B vs. D criteria indicates that coverage should be through Medicare Part D<br />
NON COVERAGE<br />
Vistide® is NOT covered for members with the following criteria:<br />
A. Non-FDA approved indications<br />
B. Patients without AIDS<br />
C. If patient is taking<br />
a. Aminoglycosides<br />
b. Amphotericin B<br />
c. Foscarnet<br />
d. NSAIDs<br />
e. Pentamidine<br />
f. Tacrolimus<br />
g. Vancomycin<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Infectious Disease<br />
AUTHORIZATION PERIOD<br />
3 months<br />
191
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
VIVAGLOBIN<br />
FDA-APPROVED INDICATIONS<br />
Immune Globulin is indicated:<br />
A. For the treatment of primary immunodeficiency<br />
B. For the treatment of idiopathic thrombocytopenic purpura<br />
C. For the treatment of Kawasaki disease<br />
COVERAGE POLICY<br />
Immune Globulin is covered for members who meet the following criteria:<br />
A. Verify B vs. D criteria per CMS guidelines<br />
a. Treatment of hypergammaglobulinemia<br />
B. AND the patient is diagnosed with primary immunodeficiency<br />
C. OR the patient is diagnosed with idiopathic thrombocytopenic purpura<br />
D. OR the patient is diagnosed with Kawasaki disease<br />
NON COVERAGE<br />
Immune globulin is NOT covered for members who meet the following criteria:<br />
A. Medication is covered by Part B per CMS guidelines<br />
B. The diagnosis is NOT hypergammaglobulinemia, primary immunodeficiency,<br />
Idiopathic Thrombocytopenia Purpura OR Kawasaki disease<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
192
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
XENAZINE<br />
FDA-APPROVED INDICATIONS<br />
Xenazine® is indicated:<br />
A. For treatment of chorea associated with Huntington’s Disease<br />
COVERAGE POLICY<br />
Xenazine® is covered for members who meet the following criteria:<br />
A. Patient must be diagnosed with Huntington’s chorea<br />
B. Patient must have previous trial/failure of Haloperidol<br />
NON COVERAGE<br />
Xenazine® is NOT covered for members with the following criteria:<br />
A. Diagnosis is NOT Huntington’s chorea<br />
B. Patient has no previous trial/failure on Haolperidol<br />
C. Patient has significant hepatic disease<br />
D. Patient is taking concurrent MAOI therapy<br />
E. Patients diagnosed with torsade de pointes<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
193
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
XOLAIR<br />
FDA-APPROVED INDICATIONS<br />
Xolair® is indicated:<br />
A. For adults and adolescents (12 years of age and above) with moderate to severe<br />
persistent asthma who have a positive skin test to a perennial aeroallergen and<br />
whose symptoms are inadequately controlled with inhaled corticosteroids. Safety<br />
and efficacy have not been established in other allergic conditions.<br />
B. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Xolair® is covered for members who meet the following criteria:<br />
A. The patient must be 12 years of age or older.<br />
B. AND the prescribing provider is a board certified pulmonologist, allergist or<br />
immunologist.<br />
C. AND the patient is NOT a current smoker.<br />
D. AND the diagnosis is documented as moderate-to-severe persistent asthma and<br />
there is evidence of reversible disease (20% or greater improvement in peak<br />
expiratory flow [PEF] with a short acting bronchodilator challenge). (Please<br />
verify the patient’s chart notes for diagnosis).<br />
E. AND the patient has tested positive to a perennial aeroallergen skin test. (Please<br />
verify the patient’s chart notes for a positive aeroallergen skin test).<br />
F. AND the patient’s baseline IgE is between 30 and 700 IU/ mL. (Please verify IgE<br />
level in the patient’s chart notes).<br />
G. AND the patient has been compliant and maintained on standard inhaled<br />
corticosteroid therapy for at least 6-months and still remains inadequately<br />
controlled. (Please verify the patient’s chart notes or drug history to verify their<br />
use of an inhaled corticosteroid [e.g. QVAR®, Pulmicort®, AeroBid®, Flovent®,<br />
Azmacort®, Asmanex®).<br />
H. AND the patient has had a 3-month trial and failure or intolerant to a long acting<br />
beta agonist agent that can Include Symbicort®, Foradil®, Serevent®, or<br />
Advair®.<br />
I. AND if the patient has received prior treatment with Xolair®,<br />
J. The patient must experience a reduction in symptoms and improvement in their<br />
FEV1 or PEF before initiation of re-treatment.<br />
NON COVERAGE<br />
Xolair® is NOT covered for members with the following criteria:<br />
A. The patient is under the age of 12 year old.<br />
B. The prescribing provider is NOT a board certified pulmonologist, allergist or<br />
immunologist.<br />
C. The patient is a current smoker.<br />
D. The diagnosis is NOT documented as moderate-to-severe persistent asthma OR<br />
there is NO evidence of reversible disease.<br />
194
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
XOLAIR<br />
(Continued)<br />
E. The diagnosis is documented as a food (e.g. peanut) or latex allergy.<br />
F. The diagnosis is documented as allergic rhinitis.<br />
G. The patient has NOT tested positive to a perennial aeroallergen skin test.<br />
H. The patient’s baseline IgE is NOT between 30 and 700 IU/ mL.<br />
I. The patient has NOT been compliant and maintained on standard inhaled<br />
corticosteroid therapy for at least 6-months.<br />
J. The patient has NOT had a 3-month trial and failure or intolerant to a long acting<br />
beta agonist agent.<br />
K. If the patient has received prior treatment with Xolair® and NOT experienced a<br />
reduction in symptoms and improvement in their FEV1 or PEF.<br />
REQUIRED MEDICAL INFORMAITON<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Pulmonologist, allergist, or<br />
immunologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
195
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
XYREM<br />
FDA-APPROVED INDICATIONS<br />
Xyrem® is indicated:<br />
A. For the treatment of excessive daytime sleepiness and cataplexy in patients with<br />
narcolepsy.<br />
Xyrem® is only available through the Xyrem® Success Program. Physicians may contact<br />
the centralized pharmacy at 1-866-977-3688. The Xyrem® success program ensures that<br />
the patient reads and understands the risks associated with Xyrem® use.<br />
COVERAGE POLICY<br />
Xyrem® is covered for members who meet the following criteria:<br />
A. The prescribing provider is a board certified sleep specialist, pulmonologist,<br />
neurologist or psychiatrist.<br />
B. AND the diagnosis is documented as excessive daytime sleepiness with<br />
symptoms that limits their ability to perform normal daily activities.<br />
C. OR the diagnosis is documented as cataplexy (a condition characterized by weak<br />
or paralyzed muscles) in patients with narcolepsy. (Please verify cataplexy<br />
diagnosis in patient’s chart notes).<br />
D. AND the patient has tried and failed (continues to have symptoms) to at least a 4-<br />
week therapy of the highest tolerated dose of Provigil®. (Please verify the use of<br />
Provigil® by reviewing the patient’s drug history or chart notes).<br />
E. AND the patient is NOT being treated with a sedative hypnotic agent (e.g.<br />
flurazepam, Dalmane®, zolpidem, Ambien®, eszopiclone, Lunesta® estazolam,<br />
Prosom®, temazepam, Restoril®, chloral hydrate).(Please verify the use of a<br />
sedative hypnotic® by reviewing the patient’s drug history or chart notes).<br />
F. AND the patient will NOT be receiving combination therapy with Provigil®.<br />
(Please verify the potential Of combination use by reviewing the patient’s drug<br />
history or chart notes).<br />
G. AND if the patient has received prior treatment with Xyrem®.<br />
H. The patient must experience a decrease in daytime sleepiness and/or cataplexy in<br />
a narcoleptic patient.<br />
I. AND approval can be allowed for 3 months for the initial authorization or up to 1<br />
year for an additional request.<br />
NON COVERAGE<br />
Xyrem® is NOT covered for members with the following criteria:<br />
A. The prescribing provider is NOT a board certified sleep specialist,<br />
pulmonologist, neurologist or psychiatrist.<br />
B. The patient has NOT tried and failed at least a 4-week therapy of the highest<br />
tolerated dose of Provigil®.<br />
C. The patient is being treated with a sedative hypnotic agent.<br />
D. The patient is receiving combination Xyrem® therapy with Provigil®.<br />
196
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
XYREM<br />
(Continued)<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
3 months<br />
197
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZAVESCA<br />
FDA-APPROVED INDICATIONS<br />
Zavesca® is indicated:<br />
A. For the treatment of adult patients with mild-to-moderate type-1 Gaucher disease<br />
for whom enzyme replacement therapy is not a therapeutic option.<br />
COVERAGE POLICY<br />
Zavesca® is covered for members who meet the following criteria:<br />
A. Diagnosis is documented as mild-to-moderate type-1 Gaucher disease.<br />
B. AND the patient is 18 years of age or older.<br />
C. AND diagnosis has been confirmed by bone marrow histology, DNA testing or<br />
measurement of b-glucocerebrosidase enzyme activity less than 30%.<br />
D. AND the patient has a hemoglobin concentration above 9 g/dL or a platelet count<br />
above 50 x10 9 /L or active bone disease. (Zavesca® has not been evaluated in<br />
patients with severe disease).<br />
E. AND the patient has tried and failed enzyme replacement therapy (e.g.<br />
Ceredase®, Cerezyme®) or is not a therapeutic option (e.g. allergy,<br />
hypersensitivity). (Please verify trial in the patient’s drug history or chart).<br />
F. AND if the patient is female and of childbearing years, she is NOT pregnant, has<br />
NO plans for pregnancy, is on a form of contraception or has NO ability to<br />
conceive and has been educated on the potential dangers of Zavesca® therapy.<br />
G. AND if the patient has previously received 24 months of Zavesca® therapy, they<br />
must show a decrease in liver and spleen volume and/or increases in platelet count<br />
and/or increases in hemoglobin concentration.<br />
NON COVERAGE<br />
Zavesca® is NOT covered for members with the following criteria:<br />
A. The diagnosis is NOT documented as mild-to moderate type-1 Gaucher disease.<br />
B. The patient is under the age of 18 years old.<br />
C. Diagnosis has NOT been confirmed by bone marrow histology, DNA testing or<br />
measurement of enzyme activity.<br />
D. The patient has a hemoglobin concentration below 9 g/dL or a platelet count<br />
below 50 x10 9 /L or active bone disease.<br />
E. The patient has not tried, failed or intolerant to enzyme replacement therapy.<br />
F. If the patient is female and of childbearing years, she cannot be pregnant, have<br />
plans for pregnancy, and not educated on the potential risk of pregnancy with<br />
Zavesca® therapy.<br />
G. If the patient has previously received 24 months of Zavesca® therapy and has<br />
NOT shown a decrease in liver and spleen volume and/or increases in platelet<br />
count and/or increases in hemoglobin concentration since starting Zavesca®<br />
therapy.<br />
198
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZAVESCA<br />
(Continued)<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
199
FDA-APPROVED INDICATIONS<br />
Zemplar® is indicated:<br />
A. Secondary Hyperparathyroidism<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZEMPLAR<br />
COVERAGE POLICY<br />
Zemplar® is covered for members who meet the following criteria:<br />
A. Zemplar is being prescribed for Secondary Hyperparathyroidism<br />
B. AND Intact Parathyroid Hormone (iPTH) Greater than240 pg/mL (or Greater<br />
than4 times theupper limit of normal)<br />
C. AND Corrected serum calcium Less than 10.5 mg/dL<br />
D. AND Corrected Ca XP Less than 70<br />
E. OR Failure (or contraindication) of Rocaltrol/Calcijex/Hectorol oral or injection<br />
therapy by demonstrating iPTH level Greater than180 pg/mL (or Greater than 3<br />
times the upper limit of normal) despite adequate therapy<br />
F. OR Development of hypercalcemia (serum calcium Greater than 11.5 mg/dL)<br />
despite adequate therapy and discontinuance of calcium based phosphate binders<br />
For Renewal <strong>Authorization</strong>:<br />
A. iPTH Greater than 120 pg/mL (or 2 times the upper limit of normal)<br />
B. AND Corrected serum calcium Less than 11.5 mg/dL<br />
C. AND Corrected Ca XP Less than 75<br />
NON COVERAGE<br />
Zemplar® is NOT covered for members with the following criteria:<br />
D. Hypercalcemia<br />
E. Vitamin D toxicity<br />
F. Concurrent use with Vitamin D analogs<br />
REQUIRED MEDICAL INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
PRESCRIBER RESTRICTIONS<br />
Endocrinologist<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
200
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZENAPAX<br />
FDA-APPROVED INDICATIONS<br />
Zenapax® is indicated:<br />
A. Kidney Transplant Rejection Prophylaxis<br />
COVERAGE POLICY<br />
Zenapax® is covered for members who meet the following criteria:<br />
A. Zenapax is being prescribed for Kidney transplantation prophylaxis<br />
B. AND the patient is greater than 11 months old<br />
C. AND B vs. D criteria is determined that coverage should be through Medicare<br />
Part D.<br />
NON COVERAGE<br />
Zenapax® is NOT covered for members with the following criteria:<br />
A. Zenapax is NOT being prescribed for Kidney transplantation prophylaxis<br />
B. The patient is less than 11 months old<br />
C. B vs. D criteria is determined that coverage should be through Medicare Part B<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
10 weeks<br />
201
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZYPREXA ZYDIS<br />
FDA APPROVED INDICATIONS<br />
A. Acute Psychosis<br />
B. Agitation<br />
C. Bipolar Disorder<br />
D. Mania<br />
E. Schizophrenia.<br />
F. All other FDA approved indications not otherwise excluded from Part D<br />
COVERAGE POLICY<br />
Zyprexa-Zydis is covered for members who meet the following criteria:<br />
A. Patients that have an FDA approved indication that are NPO (Nothing By Mouth).<br />
B. Chart notes required indicating that patient can not take tablets or capsules.<br />
NON COVERAGE<br />
Zypresxa-Zydis is not covered for members who meet the following criteria:<br />
A. Patient has other tablets or capsules in their medication profile indicating that they can<br />
take Zyprexa tablets<br />
REQUIRED MEDICAL<br />
INFORMATION<br />
Chart Notes<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
202
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZYVOX<br />
FDA-APPROVED INDICATIONS<br />
Zyvox® is indicated For the following aerobic and facultative Gram-positive<br />
microorganisms.<br />
A. Vancomycin-Resistant Enterococcus faecium, including cases with concurrent<br />
bacteremia.<br />
B. Nosocomial pneumonia caused by Staphylococcus aureus (methicillin-susceptible<br />
and methicillin-resistant strains), or Streptococcus pneumoniae (including multidrug<br />
resistant strains [MDRSP]).<br />
C. Complicated skin and skin structure infections, including diabetic foot infections,<br />
without concomitant osteomyelitis, caused by Staphylococcus aureus (methicillinsusceptible<br />
and methicillin-resistant strains), Streptococcus pyogenes, or<br />
Streptococcus agalactiae. (Zyvox® has not been studied in the treatment of<br />
decubitus ulcers).<br />
D. Uncomplicated skin and skin structure infections caused by Staphylococcus<br />
aureus (methicillin-susceptible only) or Streptococcus pyogenes.<br />
E. Community-acquired pneumonia caused by Streptococcus pneumoniae (including<br />
multi-drug resistant strains [MDRS]), including cases with concurrent bacteremia<br />
or Staphylococcus aureus (methicillin-susceptible strains only).<br />
COVERAGE POLICY<br />
Zyvox® is covered for members who meet the following criteria:<br />
A. Therapy is NOT being used for prophylaxis therapy.<br />
B. The infection is NOT a decubitus ulcer. (Zyvox® has not been studied in the<br />
treatment of decubitus ulcers).<br />
C. The prescriber has provided chart notes, lab values and susceptibility results that<br />
document that the pathogen is susceptible to Zyvox®, other medications that the<br />
organism is susceptible to have been tried, the infection is a covered indication<br />
listed below, and the organism is a covered pathogen also listed below:<br />
D. A first time Zyvox® request to treat an infection caused by Vancomycin-<br />
Resistant Enterococcus faecium.<br />
a. AND approval can be allowed for 14 to 28 days.<br />
b. OR a request to extend Zyvox® treatment beyond the initial 14 to 28 day<br />
approved treatment for an infection caused by Vancomycin-Resistant<br />
Enterococcus faecium.<br />
c. AND an in-vitro susceptibility test (within 5-days of the request) that<br />
shows a continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
d. AND approval can be allowed for an additional 14 to 28 days.<br />
E. OR a first time Zyvox® request to treat a nosocomial pneumonia infection caused<br />
by Staphylococcus aureus (methicillin-susceptible and methicillin-resistant<br />
strains) or Streptococcus pneumoniae (including multi-drug resistant strains<br />
[MDRSP]).<br />
203
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZYVOX<br />
(Continued)<br />
a. AND the susceptibility report shows that the pathogen is not susceptible to<br />
any other antibiotic OR the provider can show a documented trial and<br />
failure or intolerance to the listed susceptible antibiotic.<br />
b. AND approval can be allowed for up to 14 days.<br />
c. OR a request to extend Zyvox® treatment beyond the initial 10-14 day<br />
approved treatment for a nosocomial pneumonia infection caused by<br />
Staphylococcus aureus or Streptococcus pneumoniae.<br />
d. AND an in-vitro susceptibility test (within 5-days of the request) that<br />
shows a continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
e. AND approval can be allowed for up to 14 days.<br />
F. OR a first time Zyvox® request to treat complicated skin and skin structure<br />
infections, including diabetic foot infections, without concomitant osteomyelitis,<br />
caused by Staphylococcus aureus (methicillin-susceptible and methicillin-resistant<br />
strains) OR Streptococcus pyogenes OR Streptococcus agalactiae.<br />
a. AND the susceptibility report shows that the pathogen is not susceptible to<br />
any other antibiotic OR the provider can show a documented trial and<br />
failure or intolerance to the listed susceptible antibiotic.<br />
b. AND the patient does NOT have osteomyelitis.<br />
c. AND approval can be allowed for up to 14 days.<br />
G. OR a request to extend Zyvox® treatment beyond the initial 10-14 day approved<br />
treatment for a complicated skin and skin structure infections, including diabetic<br />
foot infections, without concomitant osteomyelitis, caused by Staphylococcus<br />
aureus (methicillin-susceptible and methicillin-resistant strains) OR Streptococcus<br />
pyogenes OR Streptococcus agalactiae..<br />
a. AND in-vitro susceptibility test (within 5-days of the request) that shows a<br />
continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
b. AND the patient does NOT have osteomyelitis.<br />
c. AND approval can be allowed for up to 14 days.<br />
H. OR a first time Zyvox® request to treat uncomplicated skin and skin structure<br />
infections caused by methicillin-susceptible only -Staphylococcus aureus.<br />
a. AND the pathogen is methicillin-susceptible only.<br />
b. AND the susceptibility report shows that the pathogen is not susceptible to<br />
any other antibiotic OR the provider can show a documented trial and<br />
failure or intolerance to the listed susceptible antibiotic.<br />
c. AND approval can be allowed for up to 14 days.<br />
d. OR a request to extend Zyvox® treatment beyond the initial 10-14 day<br />
approved treatment for an uncomplicated skin and skin structure infections<br />
caused by methicillin-susceptible only -Staphylococcus aureus.<br />
e. AND the pathogen is methicillin-susceptible only.<br />
204
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZYVOX<br />
(Continued)<br />
f. AND in-vitro susceptibility test (within 5-days of the request) that shows a<br />
continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
g. AND approval can be allowed for up to 14 days.<br />
I. OR a first time Zyvox® request to treat uncomplicated skin and skin structure<br />
infections caused by Streptococcus pyogenes.<br />
a. AND the susceptibility report shows that the pathogen is not susceptible to<br />
any other antibiotic OR the provider can show a documented trial and<br />
failure or intolerance to the listed susceptible antibiotic.<br />
b. AND approval can be allowed for up to 14 days.<br />
c. OR a request to extend Zyvox® treatment beyond the initial 10-14 day<br />
approved treatment for an uncomplicated skin and skin structure infections<br />
caused by Streptococcus pyogenes.<br />
d. AND in-vitro susceptibility test (within 5-days of the request) that shows a<br />
continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
e. AND approval can be allowed for up to 14 days.<br />
J. OR a first time Zyvox® request to treat community-acquired pneumonia caused<br />
by Streptococcus pneumoniae (including multi-drug resistant strains [MDRS]),<br />
including cases with concurrent bacteremia.<br />
a. AND the susceptibility report shows that the pathogen is not susceptible to<br />
any other antibiotic OR the provider can show a documented trial and<br />
failure or intolerance to the listed susceptible antibiotic.<br />
b. AND approval can be allowed for up to 14 days.<br />
c. OR a request to extend Zyvox® treatment beyond the initial 10-14 day<br />
approved treatment for a community-acquired pneumonia caused by<br />
Streptococcus pneumoniae.<br />
d. AND in-vitro susceptibility test (within 5-days of the request) that shows a<br />
continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
e. AND approval can be allowed for up to 14 days.<br />
K. OR a first time Zyvox® request to treat community-acquired pneumonia caused<br />
by Staphylococcus aureus (methicillin-susceptible strains only).<br />
a. AND the pathogen is methicillin-susceptible.<br />
b. AND the susceptibility report shows that the pathogen is NOT susceptible<br />
to any other antibiotic OR the provider can show a documented trial and<br />
failure or intolerance to the listed susceptible antibiotic.<br />
c. AND approval can be allowed for up to 14 days.<br />
d. OR a request to extend Zyvox® treatment beyond the initial 10-14 day<br />
approved treatment for a community-acquired pneumonia caused by<br />
Staphylococcus aureus (methicillin-susceptible strains only).<br />
e. AND the pathogen is methicillin-susceptible.<br />
205
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ZYVOX<br />
(Continued)<br />
f. AND in-vitro susceptibility test (within 5-days of the request) that shows a<br />
continued presence of the pathogen and the organism’s continued<br />
susceptibility to Zyvox®.<br />
g. AND approval can be allowed for up to 14 days.<br />
NON COVERAGE<br />
A. Therapy is being used for prophylaxis.<br />
B. The infection is a decubitus ulcer.<br />
C. The diagnosis is neutropenia.<br />
D. The prescriber has not provided chart notes to document diagnosis, organism,<br />
susceptibility results and failure to other medications.<br />
E. The infection is caused by Enterococcus faecium but is NOT Vancomycin-<br />
Resistant.<br />
F. Susceptibility test shows the pathogen susceptible to another antibiotic and no<br />
drug regimen and been tried and failed.<br />
G. The patient has received previous Zyvox® therapy and an in-vitro susceptibility<br />
test has NOT been provided OR is NOT within 5 days of the request OR the<br />
pathogen is no longer susceptible to Zyvox®.<br />
H. The diagnosis is nosocomial pneumonia but the infection is NOT caused by<br />
Staphylococcus aureus or Streptococcus pneumoniae.<br />
I. The diagnosis is complicated skin and skin structure infections and the patient has<br />
osteomyelitis.<br />
J. The diagnosis is complicated skin and skin structure infections and NOT caused<br />
by Staphylococcus aureus or Streptococcus pyogenes or Streptococcus agalactiae.<br />
K. The diagnosis is uncomplicated skin and skin structure infections and the<br />
infection is caused by methicillin resistant Staphylococcus aureus.<br />
L. The diagnosis is uncomplicated skin and skin structure infections and the<br />
infection is NOT caused by methicillin susceptible Staphylococcus aureus or<br />
Streptococcus pyogenes.<br />
M. The diagnosis is community-acquired pneumonia and the infection is NOT caused<br />
by Streptococcus pneumoniae OR methicillin-susceptible Staphylococcus aureus.<br />
N. The diagnosis is community-acquired pneumonia and the infection is caused by<br />
methicillin-resistant Staphylcoccus aureus.<br />
REQUIRED MEDICAL<br />
INFORMAITON<br />
Chart notes as indicated in Covered Uses<br />
AUTHORIZATION PERIOD<br />
Plan Year<br />
206
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
INDEX<br />
5<br />
5HT-3 ANTAGONISTS ....................................1<br />
A<br />
ACTIMMUNE ...................................................2<br />
ACTONEL .........................................................3<br />
ADAGEN ...........................................................4<br />
AFINITOR .........................................................5<br />
AGRYLIN..........................................................6<br />
ALDURAZYME ................................................8<br />
ALFERON N....................................................10<br />
AMITIZA .........................................................11<br />
ANAGRELIDE ................................................13<br />
ANTIZOL.........................................................15<br />
ATGAM ...........................................................16<br />
AVONEX .........................................................17<br />
AZATHIOPRINE.............................................19<br />
B<br />
BANZEL ..........................................................20<br />
BETASERON ..................................................21<br />
BUPHENYL.....................................................23<br />
BYETTA ..........................................................24<br />
C<br />
CAMPATH ......................................................26<br />
CAMPRAL DELAYED-RELEASE TABLETS<br />
.....................................................................27<br />
CAMPTOSAR..................................................28<br />
CARIMUNE.....................................................29<br />
CELLCEPT ......................................................30<br />
CEREDASE .....................................................31<br />
CEREZYME ....................................................32<br />
CHORIONIC GONADOTROPIN ...................76<br />
CIMZIA............................................................33<br />
CLADRIBINE..................................................35<br />
CLARAVIS......................................................36<br />
COLONY STIMULATING FACTOR.............37<br />
COPAXONE ....................................................38<br />
CYCLOPHOSPHAMIDE ................................40<br />
CYCLOSPORINE............................................41<br />
CYKLOKAPRON............................................42<br />
CYTARABINE ................................................43<br />
D<br />
DACOGEN ......................................................44<br />
DUREZOL .......................................................45<br />
E<br />
ELAPRASE......................................................46<br />
ELIDEL ........................................................... 47<br />
ELIGARD........................................................ 48<br />
ELITEK ........................................................... 49<br />
ELOXATIN..................................................... 50<br />
EMEND........................................................... 51<br />
EMSAM .......................................................... 52<br />
ENBREL.......................................................... 53<br />
ERAXIS........................................................... 58<br />
ERYTHROPOIESIS STIMULATING AGENTS<br />
.................................................................... 59<br />
ETHYOL ......................................................... 64<br />
EXELON ......................................................... 65<br />
EXJADE .......................................................... 66<br />
F<br />
FABRAZYME ................................................ 67<br />
FLEBOGAMMA............................................. 68<br />
FORTEO.......................................................... 69<br />
G<br />
GAMASTAN .................................................. 71<br />
GAMMAGARD .............................................. 72<br />
GAMUNEX..................................................... 73<br />
GLEEVEC....................................................... 74<br />
H<br />
HEPATITIS C ................................................. 77<br />
HEPSERA ....................................................... 79<br />
HUMIRA......................................................... 81<br />
I<br />
IMITREX ........................................................ 85<br />
INCRELEX ..................................................... 86<br />
INSPRA........................................................... 88<br />
INTRON A ...................................................... 90<br />
INVEGA.......................................................... 96<br />
ITRACONAZOLE .......................................... 98<br />
IVEEGAM....................................................... 99<br />
IXEMPRA ..................................................... 100<br />
K<br />
KEPPRA XR ................................................. 101<br />
KETEK.......................................................... 102<br />
KINERET ...................................................... 103<br />
L<br />
LAMISIL AT TOPICAL SPRAY 1%........... 104<br />
LETAIRIS ..................................................... 105<br />
LEUCOVORIN ............................................. 106<br />
LEUSTATIN ................................................. 107<br />
LIDODERM .................................................. 108<br />
207
LOVAZA .......................................................109<br />
LUPRON DEPOT ..........................................110<br />
M<br />
MARINOL .....................................................111<br />
MESNEX .......................................................114<br />
MIACALCIN .................................................115<br />
MYFORTIC ...................................................116<br />
MYOZYME ...................................................117<br />
N<br />
NAGALZYME...............................................118<br />
NEURONTIN SOLUTION............................119<br />
NEUTREXIN .................................................120<br />
NEXAVAR ....................................................121<br />
NICOTROL....................................................123<br />
NOVANTRONE ............................................124<br />
NOVAREL.....................................................125<br />
O<br />
OCTAGAM....................................................126<br />
OCTREOTIDE...............................................127<br />
ORENCIA ......................................................128<br />
ORFADIN ......................................................129<br />
ORTHOCLONE.............................................130<br />
OXANDROLONE .........................................131<br />
OXSORALEN................................................132<br />
P<br />
PAMIDRONATE...........................................133<br />
PANGLOBULIN............................................134<br />
POLYGAM ....................................................135<br />
PREGNYL......................................................136<br />
PROGRAF......................................................137<br />
PROMACTA..................................................138<br />
PROVIGIL .....................................................139<br />
PULMOZYME...............................................141<br />
R<br />
RANEXA .......................................................142<br />
RAPAMUNE..................................................144<br />
REGRANEX ..................................................145<br />
RELISTOR.....................................................146<br />
REVATIO ......................................................147<br />
REVLIMID ....................................................149<br />
RISPERDAL ..................................................151<br />
<strong>RxAmerica</strong><br />
<strong>Prior</strong> <strong>Authorization</strong> <strong>Criteria</strong>:<br />
ROTATEQ .................................................... 152<br />
S<br />
SAIZEN......................................................... 153<br />
SANCUSO .................................................... 158<br />
SIMULECT ................................................... 159<br />
SOMAVERT ................................................. 160<br />
SPORANOX.................................................. 161<br />
SUCRAID...................................................... 162<br />
SUTENT........................................................ 163<br />
SYMLIN........................................................ 165<br />
SYNAREL..................................................... 167<br />
T<br />
TAMIFLU ..................................................... 168<br />
TARCEVA .................................................... 169<br />
TARGRETIN ................................................ 171<br />
TASIGNA...................................................... 172<br />
TEV-TROPIN................................................ 173<br />
TORISEL....................................................... 178<br />
TRACLEER .................................................. 179<br />
TRETINOIN PRODUCTS ............................ 181<br />
TRICOR ........................................................ 182<br />
TYKERB ....................................................... 183<br />
TYZEKA ....................................................... 185<br />
V<br />
VESANOID................................................... 187<br />
VFEND.......................................................... 188<br />
VIDAZA........................................................ 189<br />
VIMPAT........................................................ 190<br />
VISTIDE........................................................ 191<br />
VIVAGLOBIN .............................................. 192<br />
X<br />
XENAZINE................................................... 193<br />
XOLAIR........................................................ 194<br />
XYREM......................................................... 196<br />
Z<br />
ZAVESCA..................................................... 198<br />
ZEMPLAR .................................................... 200<br />
ZENAPAX .................................................... 201<br />
ZYPREXA ZYDIS........................................ 202<br />
ZYVOX ......................................................... 203<br />
208