Contrast-Enhanced MR Perfusion Imaging - University of Wisconsin ...
Contrast-Enhanced MR Perfusion Imaging - University of Wisconsin ...
Contrast-Enhanced MR Perfusion Imaging - University of Wisconsin ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
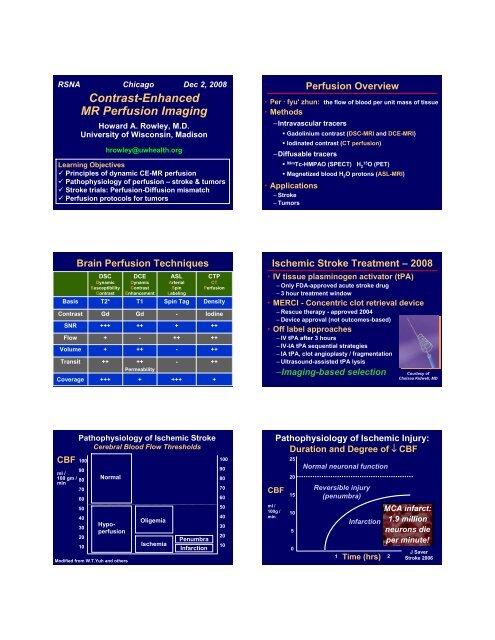
RSNA Chicago Dec 2, 2008<br />
<strong>Contrast</strong>-<strong>Enhanced</strong><br />
<strong>MR</strong> <strong>Perfusion</strong> <strong>Imaging</strong><br />
Howard A. Rowley, M.D.<br />
<strong>University</strong> <strong>of</strong> <strong>Wisconsin</strong>, Madison<br />
hrowley@uwhealth.org<br />
Learning Objectives<br />
Principles <strong>of</strong> dynamic CE-<strong>MR</strong> perfusion<br />
Pathophysiology <strong>of</strong> perfusion – stroke & tumors<br />
Stroke trials: <strong>Perfusion</strong>-Diffusion mismatch<br />
<strong>Perfusion</strong> protocols for tumors<br />
<strong>Perfusion</strong> Overview<br />
• Per · fyu' zhun: the flow <strong>of</strong> blood per unit mass <strong>of</strong> tissue<br />
• Methods<br />
–Intravascular tracers<br />
• Gadolinium contrast (DSC-<strong>MR</strong>I and DCE-<strong>MR</strong>I)<br />
• Iodinated contrast (CT perfusion)<br />
–Diffusable tracers<br />
• 99m Tc-HMPAO (SPECT) H<br />
15<br />
2 O (PET)<br />
• Magnetized blood H 2 O protons (ASL-<strong>MR</strong>I)<br />
• Applications<br />
– Stroke<br />
– Tumors<br />
Basis<br />
<strong>Contrast</strong><br />
SNR<br />
Flow<br />
Volume<br />
Transit<br />
Coverage<br />
Brain <strong>Perfusion</strong> Techniques<br />
DSC<br />
Dynamic<br />
Susceptibility<br />
<strong>Contrast</strong><br />
T2*<br />
Gd<br />
+++<br />
+<br />
+<br />
++<br />
+++<br />
DCE<br />
Dynamic<br />
<strong>Contrast</strong><br />
Enhancement<br />
T1<br />
Gd<br />
++<br />
-<br />
++<br />
++<br />
Permeability<br />
+<br />
ASL<br />
Arterial<br />
Spin<br />
Labeling<br />
Spin Tag<br />
-<br />
+<br />
++<br />
-<br />
-<br />
+++<br />
CTP<br />
CT<br />
<strong>Perfusion</strong><br />
Density<br />
Iodine<br />
++<br />
++<br />
++<br />
++<br />
+<br />
Ischemic Stroke Treatment – 2008<br />
• IV tissue plasminogen activator (tPA)<br />
– Only FDA-approved acute stroke drug<br />
– 3 hour treatment window<br />
• MERCI - Concentric clot retrieval device<br />
– Rescue therapy - approved 2004<br />
– Device approval (not outcomes-based)<br />
• Off label approaches<br />
– IV tPA after 3 hours<br />
– IV-IA tPA sequential strategies<br />
– IA tPA, clot angioplasty / fragmentation<br />
– Ultrasound-assisted tPA lysis<br />
–<strong>Imaging</strong>-based selection<br />
Courtesy <strong>of</strong><br />
Chelsea Kidwell, MD<br />
Pathophysiology <strong>of</strong> Ischemic Stroke<br />
Cerebral Blood Flow Thresholds<br />
CBF 100<br />
90<br />
ml /<br />
100 gm / 80<br />
min<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
Normal<br />
Hypoperfusion<br />
Modified from W.T.Yuh and others<br />
Oligemia<br />
Ischemia<br />
Penumbra<br />
Infarction<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
Pathophysiology <strong>of</strong> Ischemic Injury:<br />
Duration and Degree <strong>of</strong> ↓ CBF<br />
CBF<br />
ml /<br />
100g /<br />
min<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Normal neuronal function<br />
Reversible injury<br />
(penumbra)<br />
Infarction<br />
1 Time (hrs) 2<br />
MCA infarct:<br />
1.9 million<br />
neurons die<br />
per minute!<br />
J Saver<br />
Stroke 2006
Overview: CT and <strong>MR</strong> <strong>Perfusion</strong> Methods<br />
Inject Scan Model Parameter Maps<br />
Overview: CT and <strong>MR</strong> <strong>Perfusion</strong> Methods<br />
Inject Scan Model Parameter Maps<br />
CT<br />
I<br />
CT<br />
I<br />
MTT CBV<br />
CBF<br />
<strong>MR</strong><br />
Gd<br />
<strong>MR</strong><br />
Gd<br />
Key <strong>Perfusion</strong> Parameters<br />
• Cerebral Blood Flow (CBF)<br />
– Delivery <strong>of</strong> blood to tissue / unit time<br />
– Units: ml / 100g brain / min<br />
• Cerebral Blood Volume (CBV)<br />
– Measure <strong>of</strong> autoregulation<br />
– Units: ml / 100 g brain<br />
• Mean Transit Time (MTT)<br />
– Average time to flow thru<br />
capillaries (artery → vein)<br />
– Units: seconds<br />
CBF = CBV<br />
MTT<br />
Central Volume<br />
Principle<br />
Ischemia: Hemodynamics & <strong>Perfusion</strong><br />
• ↑ Collateral flow → ↑ MTT<br />
• Vasodilatation → ↑ CBV (until CPP ↓)<br />
• End result: ↓ CBF<br />
Central<br />
volume<br />
theory<br />
MTT<br />
CBF =<br />
CBV<br />
MTT<br />
CBV<br />
CBF<br />
Ischemia: Hemodynamics & <strong>Perfusion</strong><br />
<strong>Perfusion</strong> Modeling<br />
• ↑ Collateral flow → ↑ MTT<br />
• Vasodilatation → ↑ CBV (until CPP ↓)<br />
• End result: ↓ CBF<br />
MTT<br />
CBV<br />
CBF<br />
Central<br />
volume<br />
theory<br />
CBF =<br />
CBV<br />
MTT<br />
Zaharchuk, G. AJNR 2007; 28: 1850-1858
<strong>Perfusion</strong> and Traffic Jams…<br />
• Long transit times MTT<br />
• Collateral routes CBV<br />
• Variable net effect CBF<br />
Penumbral <strong>Imaging</strong><br />
<strong>Perfusion</strong>-Diffusion Mismatch<br />
DWI<br />
MTT<br />
Penumbra = Target for Intervention<br />
Clinical Trials - PWI/DWI Mismatch<br />
• DIAS, DEDAS, DIAS-2 (Hacke)<br />
– 3-9 hours, Desmoteplase vs placebo<br />
• DEFUSE (Wechsler)<br />
– 3-6 hours, open label IV tPA<br />
• EPITHET (Davis)<br />
– 3-6 hours, IV tPA vs placebo<br />
– Selected by CT, but all get PWI/DWI<br />
– <strong>MR</strong> at 3-5 days and 90 days<br />
– Unique design: is the PWI/DWI concept valid?<br />
• <strong>MR</strong> RESCUE (Kidwell)<br />
– 0-8 hours<br />
– MERCI retrieval vs medical therapy<br />
Desmoteplase Trials: DEDAS / DIAS<br />
Dose Escalation study <strong>of</strong> Desmoteplase in Acute ischemic Stroke<br />
Desmoteplase In Acute ischemic Stroke<br />
Trial Overview:<br />
Double blind, randomized, placebo controlled trials<br />
IV delivery, 3-9 hour time window<br />
Plasminogen activator – from vampire bat saliva<br />
Selection based on PWI-DWI Mismatch<br />
<strong>MR</strong>I Inclusion:<br />
PWI defect at least 2 cm AND ~20% larger than DWI<br />
PWI should be obvious, even visible on raw images<br />
<strong>MR</strong>I Exclusion:<br />
DWI > 1/3 MCA<br />
<strong>MR</strong>A: ICA occlusion<br />
DIAS Results: Hacke et al<br />
Stroke 2005; 36:66-73<br />
DEDAS Results: Furlan et al<br />
Stroke 2006; 37:1227-1231<br />
BATS<br />
Diffusion-<strong>Perfusion</strong> Mismatch<br />
Treatment Triage<br />
%<br />
80<br />
70<br />
60<br />
50<br />
40<br />
Desmoteplase – DIAS Results<br />
Hacke et al, Stroke 2005; 36:66-73<br />
46.7 46.7<br />
71.4<br />
60<br />
49.3<br />
38.7<br />
102 patients<br />
3-9 hours<br />
IV DSPA<br />
PWI > DWI<br />
30<br />
20<br />
10<br />
0<br />
23.1<br />
13<br />
19.2 22.2<br />
62.5 90 125 Total Placebo<br />
Desmoteplase dose (μg/kg) vs placebo<br />
Reperfusion<br />
Favorable<br />
Outcome
DEFUSE Trial<br />
Mismatch associated<br />
with good outcomes following reperfusion<br />
Before tPA<br />
NIHSS 16<br />
Albers et al Ann Neurol 60: 508-517, 517, 2006<br />
Key Results <strong>of</strong> the DEFUSE Study<br />
• Target Mismatch pattern (42%)<br />
identifies patients who appear to benefit<br />
substantially from early reperfusion<br />
3 cc<br />
65 cc ↓ M2 Flow<br />
• Malignant <strong>MR</strong>I pattern (8%) predicts<br />
severe ICH following reperfusion<br />
4.5 hrs<br />
After tPA<br />
NIHSS 5<br />
• Small DWI and PWI lesions (26%)<br />
are associated with favorable outcomes<br />
6 cc 0 cc Improved<br />
Albers et al Ann Neurol 60: 508-517, 517, 2006<br />
<strong>MR</strong> Rescue - Penumbral Pattern:<br />
Recanalization, Good Outcome<br />
Pre<br />
Post<br />
Baseline NIHSS 11 Left MCA Occlusion, TIMI 2<br />
Recanalization at 5 hrs 50 mins, Day 90 mRS 1<br />
<strong>MR</strong> RESCUE data courtesy <strong>of</strong> Chelsea Kidwell<br />
EPITHET Results<br />
• EPI Thrombolysis Evaluation Trial<br />
• 101 patients, 3-6 hrs IV tPA vs placebo<br />
• Selected by CT, but all got PWI/DWI<br />
• <strong>MR</strong> at 3-5 days and 90 days<br />
• Results (ISC 2008)<br />
• 83% had penumbral pattern (Tmax >2 sec)<br />
• Mean infarct growth: 1.24 tPA vs 1.78 placebo<br />
• If mismatch present, tPA ↑ reperfusion<br />
• All trends favor PWI-DWI selection<br />
• EXTEND mismatch trial being planned: 3-9 hrs<br />
Davis et al Lancet Neurology 2008; 7:299-309<br />
PWI-DWI selection better than basic CT<br />
Schellinger et al Stroke 2007; 38:2640-2645<br />
1210 patients 5 centers IV tPA<br />
CT
Stroke <strong>MR</strong> Alters Therapy Plan in 26%<br />
CT <strong>Perfusion</strong> Mismatch = DWI/PWI Mismatch<br />
Wintermark et al Neurology 2007; 68:694-697 and Stroke 2006; 37:979-985<br />
Mismatch Criteria<br />
<strong>MR</strong> CT<br />
PWI ↑ MTT<br />
DWI ↓ CBV<br />
PCT<br />
CTA<br />
<strong>Perfusion</strong> CT ‘Mismatch’: ↑ MTT >145% = penumbra ↓ CBV < 2 ml/100gm = core<br />
DWI PWI <strong>MR</strong>A<br />
Heidenreich et al Acta Radiologica 2008; 49:550-557<br />
10 Minute Acute Stroke Protocol<br />
Physiologic stroke triage: occlusion site, PWI-DWI mismatch<br />
Ischemic Penumbra<br />
Value <strong>of</strong> Dynamic <strong>Perfusion</strong> Metrics<br />
FrFSE 1:03<br />
DWI 0:40<br />
FSPGR 0:36<br />
CBV<br />
CBF - bc<br />
CBF - ASL<br />
TRICKS 0:54<br />
PWI 1:12<br />
Automated processing<br />
FMT CBV CBF<br />
FMT Tmax MTT<br />
Glioma: <strong>Perfusion</strong> Shows ↑CBV<br />
CBV & Permeability Predict Tumor Grade<br />
T2*<br />
T2*<br />
based<br />
CBV<br />
Grade 2<br />
Fibrillary<br />
astrocytoma<br />
K fp<br />
T1<br />
based<br />
ROI<br />
T2* vs time<br />
Grade 3<br />
Anaplastic<br />
astrocytoma<br />
T2*<br />
Effect<br />
T1<br />
Effect<br />
Grade 4<br />
Glioblastoma<br />
multiforme<br />
CBV<br />
T1+<br />
MTT<br />
Patankar et al AJNR 2005; 26:2455-2465
↑ CBV Predicts Glioma Transformation<br />
Post Radiation Necrosis : Low CBV<br />
Baseline 6 months 18 months<br />
Danchaivijitr et al Radiology 2008; 247: 170-178<br />
CBV Estimation in Tumors<br />
Gadolinium Preload Reduces Model Dependence<br />
UTI CTI GV PBSI MSD NEI<br />
Metastatic Breast Carcinoma (HER-2 +)<br />
Without preload<br />
CT-<br />
MTT<br />
CBF<br />
With preload<br />
Paulson and Schmainda Radiology 2008; 249:601<br />
CT+ CBV Permeability<br />
Elevated Permeability in Acute Ischemic Stroke<br />
<strong>Perfusion</strong> Summary<br />
CT<br />
CTA<br />
MTT<br />
CBF<br />
1<br />
2<br />
3<br />
1<br />
2<br />
3<br />
CBV<br />
KPS<br />
1<br />
2<br />
3<br />
1<br />
2<br />
3<br />
• <strong>Perfusion</strong> Methods<br />
–Dynamic Susceptibility <strong>Contrast</strong> – T2*<br />
–Dynamic <strong>Contrast</strong> Enhancement – T1<br />
–Arterial Spin Labeling - Tag<br />
• Key Parameters<br />
–Cerebral Blood Flow<br />
–Cerebral Blood Volume<br />
–Mean Transit Time<br />
• Applications<br />
–Stroke and Tumors