An Audit of Consent for Minor Surgery in a General Practice in ...
An Audit of Consent for Minor Surgery in a General Practice in ...
An Audit of Consent for Minor Surgery in a General Practice in ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>An</strong> <strong>Audit</strong> <strong>of</strong> <strong>Consent</strong> <strong>for</strong> <strong>M<strong>in</strong>or</strong> <strong>Surgery</strong> <strong>in</strong> a<br />
<strong>General</strong> <strong>Practice</strong> <strong>in</strong> Northern Ireland<br />
Paula Burns, 5 th Year Medical Student, Queen’s University Belfast<br />
Address <strong>for</strong> Correspondence: M127 Monea Road, Brughas, Spr<strong>in</strong>gfield, Enniskillen,<br />
County Fermanagh, BT74 5DQ. Email: b1213803@qub.ac.uk<br />
<strong>Audit</strong> Aims: To achieve and ma<strong>in</strong>ta<strong>in</strong> a high standard <strong>of</strong> care <strong>for</strong> patients<br />
by <strong>in</strong>vestigat<strong>in</strong>g whether <strong>in</strong><strong>for</strong>med consent was obta<strong>in</strong>ed <strong>for</strong> m<strong>in</strong>or<br />
surgical procedures and to try to cont<strong>in</strong>ue or to improve standards <strong>of</strong><br />
care <strong>for</strong> patients. The audit identifies from patients medical records,<br />
with<strong>in</strong> Health Centre X, who had <strong>in</strong>jection, <strong>in</strong>cision or excision per<strong>for</strong>med<br />
and whether consent was recorded. <strong>Audit</strong> Design: <strong>An</strong> audit <strong>of</strong> all<br />
patients who have had m<strong>in</strong>or surgery (<strong>in</strong>cision, <strong>in</strong>jection and excision)<br />
between the dates, April 2005 until April 2006. The study consisted <strong>of</strong> a<br />
computer search <strong>of</strong> three general practitioners (Drs A, B and C) with<strong>in</strong><br />
Health Centre X to identify m<strong>in</strong>or surgery procedures (excision, <strong>in</strong>cision<br />
and <strong>in</strong>jection) which were carried out and if <strong>in</strong><strong>for</strong>med consent was<br />
recorded on the computer. All procedures carried out were <strong>in</strong>cluded <strong>in</strong><br />
the audit which resulted <strong>in</strong> a sample size <strong>of</strong> 122 procedures. Re-audit<br />
aims: To evaluate the changes from the previous audit. Re-audit design:<br />
The re-audit consisted <strong>of</strong> the same design, except between the dates,<br />
22 nd Jan until 2 nd April 2007. It also <strong>in</strong>cluded all procedures <strong>of</strong> excision,<br />
<strong>in</strong>cision and <strong>in</strong>jection carried out with<strong>in</strong> the time period which resulted <strong>in</strong><br />
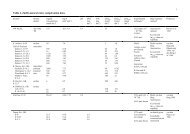
a sample size <strong>of</strong> 16. Results <strong>of</strong> <strong>Audit</strong> 2005-2006: The study found 45<br />
(36.9%) procedures had no record <strong>of</strong> consent documented by the doctor,<br />
77 (63.1%) had consent documented. 85.7% <strong>of</strong> <strong>in</strong>cision, 29.1%<br />
excisional and 38.3% <strong>for</strong> <strong>in</strong>jections had no consent recorded.<br />
Recommendations were implemented by the practice and a re-audit was<br />
carried out. Results <strong>of</strong> re-audit Jan 2007-April 2007: The re-audit found<br />
that 100% <strong>of</strong> the excisions and <strong>in</strong>jections had recorded consent obta<strong>in</strong>ed<br />
with 0% <strong>of</strong> <strong>in</strong>cisions with recorded consent obta<strong>in</strong>ed. Conclusion:<br />
<strong>Consent</strong> documented <strong>for</strong> m<strong>in</strong>or surgery was not sufficient to meet the<br />
108
standards set <strong>of</strong> 100%. After the audit from April 2005-2006 consent <strong>for</strong><br />
<strong>in</strong>jection and excision required a vast improvement. However, after<br />
changes were implemented and a re-audit was undertaken the record <strong>of</strong><br />
documented consent drastically improved to 100%. The considerable<br />
improvement may have been as a consequence <strong>of</strong> the recommendations<br />
<strong>of</strong> the first audit, due to more consent practiced with excision and<br />
<strong>in</strong>jection procedures or a heightened regard by the doctors <strong>for</strong> acquir<strong>in</strong>g<br />
consent <strong>for</strong> these procedures. With <strong>in</strong>cisions, results from the 2005-2006<br />
audit found a stagger<strong>in</strong>g 85.7% had no recorded written consent and<br />
after changes were implemented the re-audit found 0% had recorded<br />
written consent. These results may have been due to the small sample<br />
size <strong>in</strong> both audits; the <strong>in</strong>frequency <strong>of</strong> <strong>in</strong>cisions, or the possibility that<br />
<strong>in</strong>cisions were deemed less dangerous, than <strong>in</strong>jection and excision, by<br />
the general practitioner; and possibly verbal consent was be<strong>in</strong>g obta<strong>in</strong>ed<br />
but not recorded. Discussion: As a general standard, consent <strong>of</strong> a<br />
patient prior to a procedure or treatment is respectful and should be<br />
undertaken by all healthcare pr<strong>of</strong>essionals. It is a legal requirement that<br />
healthcare pr<strong>of</strong>essionals obta<strong>in</strong> consent from a patient be<strong>for</strong>e any <strong>for</strong>m <strong>of</strong><br />
contact occurs. <strong>Consent</strong> be<strong>for</strong>e a procedure on a patient converts what<br />
would otherwise be seen as a <strong>for</strong>m <strong>of</strong> assault or battery <strong>in</strong>to a lawful act.<br />
Good communication is vital <strong>for</strong> ga<strong>in</strong><strong>in</strong>g consent. Each patient should be<br />
fully <strong>in</strong><strong>for</strong>med about treatment options, the treatment proposed, what is<br />
<strong>in</strong>volved <strong>in</strong> the procedure, whether you th<strong>in</strong>k it is appropriate, likely risks<br />
<strong>of</strong> hav<strong>in</strong>g treatment and not hav<strong>in</strong>g treatment. If consent is to be valid it<br />
must be given freely, be specific, applicable to the procedure and<br />
treatment to be carried out, based on a proper understand<strong>in</strong>g <strong>of</strong> the<br />
major implications, complications and proposed treatment and/or<br />
procedure and given by a person who is legally able to consent. The<br />
doctor has an ethical obligation to help the patient make choices about<br />
the therapeutic <strong>in</strong>tervention as well as alternatives consistent with good<br />
medical practice. The paternalistic approach is no longer socially<br />
acceptable. Doctors must respect the autonomous choices <strong>of</strong> the patient<br />
as this runs deep <strong>in</strong> moral pr<strong>in</strong>ciples. J NI Ethics Forum 2008, 5: 108-129<br />
109
<strong>Audit</strong> on <strong>Consent</strong> <strong>for</strong> <strong>M<strong>in</strong>or</strong> <strong>Surgery</strong> Procedures<br />
April 2005 to April 2006<br />
Introduction<br />
<strong>Consent</strong> is a legal procedure <strong>in</strong> which a patient knows all <strong>of</strong> the risks and<br />
benefits <strong>of</strong> a particular treatment and makes an <strong>in</strong><strong>for</strong>med decision about<br />
their care. Valid <strong>in</strong><strong>for</strong>med consent is fundamental to the duty <strong>of</strong> any<br />
doctor and there are crim<strong>in</strong>al and/or civil legal implications if consent is<br />
<strong>for</strong>gotten or acquired <strong>in</strong>correctly. With<strong>in</strong> the sett<strong>in</strong>g <strong>of</strong> a general practice,<br />
<strong>in</strong><strong>for</strong>med consent should always be sought be<strong>for</strong>e per<strong>for</strong>m<strong>in</strong>g any<br />
procedure. This audit records whether <strong>in</strong><strong>for</strong>med consent was obta<strong>in</strong>ed <strong>for</strong><br />
particular m<strong>in</strong>or surgical procedures and the legal and ethical issues if<br />
consent is missed or <strong>in</strong>correctly recorded.<br />
Background<br />
This audit exam<strong>in</strong>es whether written consent was recorded <strong>for</strong> every<br />
m<strong>in</strong>or surgery procedure, <strong>of</strong> excision, <strong>in</strong>cision and <strong>in</strong>jection, with an aim<br />
<strong>of</strong> ensur<strong>in</strong>g a high standard <strong>of</strong> care <strong>for</strong> patients attend<strong>in</strong>g Health Centre<br />
X. Every patient deserves to make a well <strong>in</strong><strong>for</strong>med decision about their<br />
own care, and it is the legal duty <strong>of</strong> their doctor to accommodate this by<br />
communicat<strong>in</strong>g <strong>in</strong><strong>for</strong>mation effectively <strong>for</strong> every m<strong>in</strong>or surgical procedure<br />
they are undertak<strong>in</strong>g, provided the patient wishes to be <strong>in</strong><strong>for</strong>med and has<br />
the capacity to understand the <strong>in</strong><strong>for</strong>mation. In<strong>for</strong>med consent enhances<br />
patient care, protects the autonomy <strong>of</strong> the patient, and protects the<br />
doctor from the legal consequences <strong>of</strong> unduly harm<strong>in</strong>g patients [1] [2] [3] .<br />
<strong>M<strong>in</strong>or</strong> surgery usually refers to any surgical procedure that <strong>in</strong>volves local<br />
anaesthesia only without respiratory assistance. This audit specifically<br />
concentrates on excision, <strong>in</strong>cision, and <strong>in</strong>jection. <strong>An</strong> excision is<br />
someth<strong>in</strong>g removed by cutt<strong>in</strong>g, an <strong>in</strong>cision is a cut <strong>in</strong>to a body tissue or<br />
organ and an <strong>in</strong>jection is the <strong>for</strong>ceful <strong>in</strong>sertion <strong>of</strong> a substance under<br />
pressure. The British Medical Association (BMA) states that <strong>in</strong> each case<br />
110
<strong>of</strong> m<strong>in</strong>or surgery the patient should be fully <strong>in</strong><strong>for</strong>med <strong>of</strong> the treatment<br />
options and the treatment proposed and that the patient should give<br />
written consent <strong>for</strong> the procedure to be carried out and the completed<br />
NHS consent <strong>for</strong>m should be filed <strong>in</strong> the patient’s lifelong medical record.<br />
[4] In accordance with this, the <strong>Practice</strong> <strong>Consent</strong> Policy <strong>for</strong> Health Centre<br />
X, is to use written consent <strong>for</strong>ms <strong>for</strong> every m<strong>in</strong>or surgical procedure<br />
provided the patient is competent to make an <strong>in</strong><strong>for</strong>med decision, has<br />
received adequate <strong>in</strong><strong>for</strong>mation and has not been coerced. This aims to<br />
develop and implement a person-centred consent policy [5] .Each doctor,<br />
when registered, is expected to follow a set <strong>of</strong> pr<strong>in</strong>ciples <strong>of</strong> good practice<br />
when seek<strong>in</strong>g patients’ consent. The right <strong>of</strong> the patient to make a well<br />
<strong>in</strong><strong>for</strong>med decision is protected by law, if the patient has not received<br />
enough <strong>in</strong><strong>for</strong>mation on which to base their decision the consent may not<br />
be valid, even though it has been signed. In addition the patient is also<br />
allowed to change their m<strong>in</strong>d after sign<strong>in</strong>g the <strong>for</strong>m provided they have<br />
adequate capacity to do so. The <strong>for</strong>m is only an aide-memoir and should<br />
not be substituted <strong>for</strong> face-to-face discussion. If a patient is 16 or over<br />
they can provide consent if presumed to be competent. The GMC<br />
requires doctors to tell patients about ‘serious or frequent’ risks and to<br />
answer honestly any questions asked [6, 7] .The Medical Defence Union<br />
(MDU) pre<strong>for</strong>med a risk management analysis <strong>of</strong> m<strong>in</strong>or surgery claims<br />
and it demonstrated that lack <strong>of</strong> consent and <strong>in</strong>adequate medical records<br />
featured heavily <strong>in</strong> 26 claims settled over a five year period. This was<br />
most noticeable is the largest group <strong>of</strong> claims, <strong>for</strong> excisions or excision<br />
biopsy, <strong>in</strong> which scarr<strong>in</strong>g was the ma<strong>in</strong> <strong>in</strong>jury [8] The old traditional<br />
paternalistic role <strong>of</strong> the doctor has now shifted to one based on the<br />
patient’s autonomy and <strong>in</strong>tegrity. In<strong>for</strong>med consent reflects this, <strong>for</strong><br />
example, a 1957 case (Salgo versus Leland Stan<strong>for</strong>d Jr University Board<br />
<strong>of</strong> Trustee) <strong>in</strong> which the pla<strong>in</strong>tiff was paralysed after myelography. His<br />
doctor had not <strong>in</strong><strong>for</strong>med him that paralysis was a risk. The pla<strong>in</strong>tiff won<br />
his case even though, back then, the doctor had made no mistake. This<br />
was the first occasion the terms ‘<strong>in</strong><strong>for</strong>med’ and ‘patient’s consent’ were<br />
coupled together. The court found that had the patient been properly<br />
111
<strong>in</strong><strong>for</strong>med he would have refused myelography. [9] Inadequate <strong>in</strong><strong>for</strong>mation<br />
about risks can lead to treatment options appear<strong>in</strong>g <strong>in</strong> an undeservedly<br />
positive light and patients may agree to treatments that they would<br />
otherwise reject if given more accurate outcome probabilities [2] .Each<br />
patient requires a duty <strong>of</strong> care from their doctor. With<strong>in</strong> this, nonmaleficence,<br />
autonomy, beneficence and justice are <strong>in</strong>cluded which all<br />
underp<strong>in</strong> well <strong>in</strong><strong>for</strong>med consent. In addition, there is an <strong>in</strong>creased<br />
awareness amongst patients that they can now take action aga<strong>in</strong>st<br />
mistreatment <strong>in</strong> the <strong>for</strong>m <strong>of</strong> compla<strong>in</strong>ts or even claims. There<strong>for</strong>e ga<strong>in</strong><strong>in</strong>g<br />
and document<strong>in</strong>g <strong>in</strong><strong>for</strong>med consent <strong>for</strong> m<strong>in</strong>or surgery is <strong>in</strong> the best<br />
<strong>in</strong>terests <strong>of</strong> the patient and their doctor [3] .<br />
Aim<br />
The aim <strong>of</strong> this audit is to improve the practice <strong>of</strong> record<strong>in</strong>g consent <strong>for</strong><br />
patients attend<strong>in</strong>g the <strong>General</strong> Practitioner <strong>for</strong> m<strong>in</strong>or surgery.<br />
Additionally, it aims to ensure that <strong>in</strong><strong>for</strong>med consent is obta<strong>in</strong>ed <strong>for</strong> each<br />
m<strong>in</strong>or surgery procedure and that it is recorded <strong>in</strong> the patient’s medical<br />
notes <strong>in</strong> the same manner as other patients receiv<strong>in</strong>g the same<br />
treatment. The overall aim <strong>of</strong> this audit is to achieve and ma<strong>in</strong>ta<strong>in</strong> a high<br />
standard <strong>of</strong> care <strong>for</strong> patients by <strong>in</strong>vestigat<strong>in</strong>g whether <strong>in</strong><strong>for</strong>med consent<br />
was obta<strong>in</strong>ed <strong>for</strong> m<strong>in</strong>or surgical procedures and to try to cont<strong>in</strong>ue or to<br />
improve standards.<br />
Criteria<br />
Identify from patient’s medical records who had:<br />
a. <strong>M<strong>in</strong>or</strong> surgery done- <strong>in</strong>jection Read code: 9877<br />
b. <strong>M<strong>in</strong>or</strong> surgery done- <strong>in</strong>cision Read code: 9879<br />
c. <strong>M<strong>in</strong>or</strong> surgery done- excision Read code: 987A<br />
<strong>An</strong>d whether consent was recorded <strong>for</strong> each procedure.<br />
112
Standards set<br />
Record <strong>of</strong> record<strong>in</strong>g INFORMED CONSENT- 100%<br />
Record <strong>of</strong> record<strong>in</strong>g TYPE OF PROCEDURE-100%<br />
100% <strong>for</strong> all criteria<br />
Preparation and Plann<strong>in</strong>g<br />
Meet<strong>in</strong>g was held with GP/mentor and nurse practitioner regard<strong>in</strong>g the<br />
issue <strong>of</strong> record<strong>in</strong>g consent be<strong>for</strong>e m<strong>in</strong>or surgery procedures and the<br />
possibility <strong>of</strong> improvements with<strong>in</strong> the practice. Throughout the audit<br />
multiple meet<strong>in</strong>gs were held with my GP/mentor to discuss the audit,<br />
possible improvements and changes to the practice.<br />
Methodology<br />
1 A computer search identified all patients who had m<strong>in</strong>or surgery<br />
between the dates, 1 st April 2005 until 1 st April 2006.<br />
2 A computer search identified the m<strong>in</strong>or surgery procedures<br />
which were carried out <strong>in</strong> respect <strong>of</strong> the patient group. (Some<br />
patients may have had more than one procedure carried out<br />
with<strong>in</strong> the time period these where all analysed.)<br />
3 A computer search identified if consent was recorded as,<br />
'In<strong>for</strong>med consent obta<strong>in</strong>ed' on <strong>in</strong>dividual patients files <strong>for</strong> each<br />
procedure.<br />
4 All m<strong>in</strong>or surgery procedures <strong>of</strong>, <strong>in</strong>cision, excision or <strong>in</strong>jection,<br />
were checked dur<strong>in</strong>g the time period.<br />
5 Sample size was 122 procedures<br />
6 Over a time period from 01/04/2005 until 01/04/2006<br />
113
Results <strong>of</strong> <strong>M<strong>in</strong>or</strong> <strong>Surgery</strong> <strong>Audit</strong><br />
Total number <strong>of</strong> m<strong>in</strong>or surgery procedures = 122<br />
All patients notes were collected and analysed who were recorded on<br />
computer to have had one, <strong>of</strong> the three, procedures.<br />
Number <strong>of</strong> procedures which <strong>in</strong>volved:<br />
Excision= 55<br />
Incision= 7<br />
Injection= 60<br />
In<strong>for</strong>med consent <strong>for</strong> a procedure recorded <strong>in</strong> notes<br />
With Recorded<br />
<strong>Consent</strong><br />
Without Recorded<br />
<strong>Consent</strong><br />
Number <strong>of</strong> procedures 77 45<br />
Percentage 63.1% 36.9%<br />
Whilst 45 (36.9%) procedures had no record <strong>of</strong> consent documented by<br />
the doctor it was possible that a consent <strong>for</strong>m was completed and held<br />
separately and not recorded correctly on the computer. A rem<strong>in</strong>der <strong>of</strong> the<br />
correct and prompt method <strong>of</strong> documentation onto the computer could<br />
help avoid mis<strong>in</strong>terpretation aris<strong>in</strong>g. Additionally, the pressure <strong>of</strong> time<br />
dur<strong>in</strong>g a busy practice on a general practitioner to obta<strong>in</strong> fully <strong>in</strong><strong>for</strong>med<br />
consent and to document this dur<strong>in</strong>g each consult must also be<br />
considered throughout.<br />
In<strong>for</strong>med consent <strong>for</strong> each procedure recorded <strong>in</strong> notes<br />
<strong>Consent</strong> No consent Total<br />
recorded recorded<br />
Excision 39 16 55<br />
Incision 1 6 7<br />
Injection 37 23 60<br />
122<br />
114
% <strong>of</strong> <strong>in</strong><strong>for</strong>med consent <strong>for</strong> each procedure recorded <strong>in</strong> notes<br />
% with consent % without consent<br />
Excision 70.9 29.1<br />
Incision 14.3 85.7<br />
Injection 61.7 38.3<br />
With regard to recorded consent <strong>for</strong> <strong>in</strong>cision m<strong>in</strong>or surgery there were<br />
85.7% <strong>of</strong> procedures without recorded consent this may be because<br />
there were only 7 <strong>in</strong>cisional m<strong>in</strong>or surgical procedures with<strong>in</strong> that time<br />
period and this may not have been a true reflection on the practice.<br />
However, it must be borne <strong>in</strong> m<strong>in</strong>d that possibly because it is a relatively<br />
<strong>in</strong>frequent procedure that the method <strong>of</strong> record<strong>in</strong>g consent is less<br />
practised and there<strong>for</strong>e consent is not recorded as thoroughly.<br />
Conclusions<br />
The standards set were not achieved <strong>in</strong> any <strong>of</strong> the <strong>in</strong>vestigated areas.<br />
Overall 36.9% <strong>of</strong> the procedures either had <strong>in</strong>correctly or no consent<br />
recorded on the computer. With regards to consent <strong>for</strong> excisions, 29.1%<br />
and <strong>for</strong> <strong>in</strong>jections 38.3% had not been recorded correctly. Of the small<br />
sample <strong>of</strong> <strong>in</strong>cisions 85.7% had not recorded written consent on the<br />
computer. This could be due to the small sample size, because <strong>of</strong> the<br />
<strong>in</strong>consistency <strong>of</strong> the doctors to practice this procedure may have led to<br />
mistakes occurr<strong>in</strong>g more frequently.<br />
Recommendations<br />
1. Development <strong>of</strong> an ISIS <strong>for</strong> m<strong>in</strong>or surgery which <strong>in</strong>cludes correctly<br />
document<strong>in</strong>g written <strong>in</strong><strong>for</strong>med consent <strong>for</strong> excision, <strong>in</strong>cision and <strong>in</strong>jection<br />
procedures on computer.<br />
2. <strong>An</strong> alert <strong>for</strong> every m<strong>in</strong>or surgery procedure to check <strong>for</strong> written<br />
115
<strong>in</strong><strong>for</strong>med consent.<br />
3. Patient <strong>in</strong><strong>for</strong>mation leaflets to be given to the patient whilst wait<strong>in</strong>g <strong>for</strong><br />
the m<strong>in</strong>or surgery procedure so that <strong>in</strong><strong>for</strong>med consent can be given<br />
promptly. Plus this may act as a method <strong>of</strong> rem<strong>in</strong>d<strong>in</strong>g the doctor as the<br />
patient may object or <strong>in</strong>itiate conversation regard<strong>in</strong>g consent.<br />
4. Easy access to the documents <strong>for</strong> written consent <strong>in</strong> the doctor’s<br />
surgery.<br />
5. Visual aids <strong>in</strong> the doctor’s surgery to rem<strong>in</strong>d the doctor to record<br />
consent.<br />
6. Re-tra<strong>in</strong><strong>in</strong>g on the <strong>Practice</strong> consent policy, pay<strong>in</strong>g particular attention<br />
to record<strong>in</strong>g written <strong>in</strong><strong>for</strong>med consent <strong>for</strong> <strong>in</strong>cisions. This could take place<br />
at an audit meet<strong>in</strong>g, lunch-time meet<strong>in</strong>g or out-<strong>of</strong>-hours.<br />
7. Re-audit<br />
Re-<strong>Audit</strong><br />
Aim: Changes to be evaluated from previous audit.<br />
Criteria<br />
Identify from patient’s medical records who had:<br />
a. <strong>M<strong>in</strong>or</strong> surgery done- <strong>in</strong>jection Read code: 9877<br />
b. <strong>M<strong>in</strong>or</strong> surgery done- <strong>in</strong>cision Read code: 9879<br />
c. <strong>M<strong>in</strong>or</strong> surgery done- excision Read code: 987A<br />
<strong>An</strong>d whether consent was recorded <strong>for</strong> each procedure.<br />
Standards set<br />
Record <strong>of</strong> record<strong>in</strong>g INFORMED CONSENT- 100%<br />
Record <strong>of</strong> record<strong>in</strong>g TYPE OF PROCEDURE-100%<br />
100% <strong>for</strong> all criteria<br />
116
Methodology<br />
1 A computer search identified all patients who had m<strong>in</strong>or surgery<br />
between the dates, 22 nd January 2007 until 2 nd April 2007.<br />
2 A computer search identified the m<strong>in</strong>or surgery procedures<br />
which were carried out <strong>in</strong> respect <strong>of</strong> the patient group. (Some<br />
patients may have had more than one procedure carried out<br />
with<strong>in</strong> the time period and these were all analysed.)<br />
3 A computer search identified if consent was recorded as,<br />
'In<strong>for</strong>med consent obta<strong>in</strong>ed' on <strong>in</strong>dividual patients files <strong>for</strong> each<br />
procedure.<br />
4 All m<strong>in</strong>or surgery procedures <strong>of</strong>, <strong>in</strong>cision, excision or <strong>in</strong>jection,<br />
were checked dur<strong>in</strong>g the time period.<br />
5 Sample size was 16 procedures<br />
6 Over a time period from 22/01/2007 until 02/04/2007<br />
Data Collection 2: Results<br />
With Recorded Without Recorded <strong>Consent</strong><br />
<strong>Consent</strong><br />
Number <strong>of</strong> 15 1<br />
procedures<br />
Percentage 93.75% 6.25%<br />
In<strong>for</strong>med consent <strong>for</strong> each procedure recorded <strong>in</strong> notes<br />
<strong>Consent</strong> No consent Total<br />
recorded recorded<br />
Excision 5 0 5<br />
Incision 0 1 1<br />
Injection 10 0 10<br />
16<br />
117
Percentage <strong>of</strong> <strong>in</strong><strong>for</strong>med consent <strong>for</strong> each procedure recorded <strong>in</strong><br />
notes<br />
% with <strong>Consent</strong> % without consent<br />
Excision 100% 0%<br />
Incision 0% 100%<br />
Injection 100% 0%<br />
Conclusion<br />
Out <strong>of</strong> a possible sixteen, on only one occasion was consent missed <strong>for</strong><br />
an <strong>in</strong>cision. However, due to the small sample size, dur<strong>in</strong>g this time only<br />
one <strong>in</strong>cision was per<strong>for</strong>med leav<strong>in</strong>g 100% <strong>of</strong> the <strong>in</strong>cisions with no<br />
recorded consent. The time period <strong>for</strong> this re-audit was only 3 months<br />
and so a re-audit from 2007-08 year would be more beneficial as there<br />
would be a larger number to analyse. Although, the method <strong>of</strong> <strong>in</strong><strong>for</strong>med<br />
consent <strong>for</strong> the <strong>in</strong>jections and excisions where both 100%, this suggests<br />
improvements have been made <strong>in</strong> these areas, but aga<strong>in</strong> due to the<br />
small sample size and short time period, a re-audit over a year would be<br />
<strong>of</strong> more benefit.<br />
Recommendations<br />
Re-iterate the importance <strong>of</strong> obta<strong>in</strong><strong>in</strong>g and record<strong>in</strong>g written consent <strong>for</strong><br />
all patients com<strong>in</strong>g <strong>for</strong> m<strong>in</strong>or surgery, with emphasis on <strong>in</strong>cisional cases.<br />
Re-audit from April 2007–April 2008<br />
Discussion<br />
Our results from the audit, April 2005- April 2006, suggest that the<br />
consent documented <strong>for</strong> m<strong>in</strong>or surgery procedures <strong>of</strong> excision, <strong>in</strong>cision<br />
and <strong>in</strong>jection was not sufficient to meet the standards set <strong>of</strong> 100%.<br />
Although the standards set are high it is <strong>of</strong> medico-legal importance that<br />
118
consent is acquired <strong>for</strong> every m<strong>in</strong>or surgical procedure per<strong>for</strong>med. For<br />
<strong>in</strong>jection and excision the number <strong>of</strong> procedures <strong>for</strong> which there was fully<br />
<strong>in</strong><strong>for</strong>med written consent, which was documented, was below 75%<br />
demonstrat<strong>in</strong>g much needed improvement. The procedures which<br />
<strong>in</strong>volved excis<strong>in</strong>g the wound had recorded consent on 70.9% <strong>of</strong> cases,<br />
highest compared to the other procedures. The reason <strong>for</strong> this may be<br />
due to chance, due to the general practitioner’s views on the importance<br />
<strong>of</strong> m<strong>in</strong>or surgery and the associated risk or the pressure <strong>of</strong> time dur<strong>in</strong>g a<br />
busy practice on a general practitioner to obta<strong>in</strong> fully <strong>in</strong><strong>for</strong>med consent<br />
and to document this dur<strong>in</strong>g each consult must also be considered. For<br />
<strong>in</strong>stance, the risk management analysis <strong>of</strong> m<strong>in</strong>or surgery claims made by<br />
the Medical Defence Union showed that the lack <strong>of</strong> consent and<br />
<strong>in</strong>adequacy <strong>of</strong> medical records featured heavily <strong>in</strong> claims settled over a<br />
five year period, most noticeably the largest group <strong>of</strong> claims was <strong>for</strong><br />
excisions, <strong>in</strong> which scarr<strong>in</strong>g was the major <strong>in</strong>jury. These results may<br />
demonstrate this knowledge with<strong>in</strong> general practitioners and hence<br />
expla<strong>in</strong> the possible <strong>in</strong>creased attention to ask<strong>in</strong>g <strong>for</strong> consent <strong>for</strong><br />
excisions. [8]<br />
With <strong>in</strong>jections, 61.9% <strong>of</strong> procedures had documented written consent.<br />
Injections were the most commonly carried out procedure with<strong>in</strong> this<br />
m<strong>in</strong>or surgery audit, hav<strong>in</strong>g had 60 procedures recorded throughout the<br />
audit year, compared to 7 <strong>in</strong>cisions and 55 excisions. The result <strong>for</strong><br />
documentation <strong>of</strong> consent <strong>for</strong> <strong>in</strong>jection was much better than the 14.3%<br />
<strong>for</strong> <strong>in</strong>cisions and this may be due to the larger frequency <strong>of</strong> the <strong>in</strong>jection<br />
procedure with<strong>in</strong> the practice. The <strong>in</strong>creased frequency <strong>of</strong> <strong>in</strong>jections<br />
when compared to <strong>in</strong>cisions suggests that as a result <strong>of</strong> the doctors<br />
<strong>in</strong>creased practice <strong>of</strong> <strong>in</strong>jections that they are more <strong>in</strong>cl<strong>in</strong>ed to ask <strong>for</strong><br />
written consent and documentation <strong>of</strong> it, than <strong>for</strong> <strong>in</strong>cisions. In addition,<br />
due to the larger sample size a more realistic <strong>in</strong>terpretation <strong>of</strong> <strong>in</strong>jections<br />
can be made. However, neither 61.9% nor 70.9% were the desired result<br />
<strong>for</strong> documentation <strong>of</strong> consent after <strong>in</strong>jection and excision respectively,<br />
and action will be required to enhance the outcome. In the re-audit, the<br />
119
documentation <strong>of</strong> consent <strong>for</strong> <strong>in</strong>jection and excision reached 100%,<br />
highlight<strong>in</strong>g the importance <strong>of</strong> re-iteration and re-tra<strong>in</strong><strong>in</strong>g on consent.<br />
Furthermore, the m<strong>in</strong>or surgery specification <strong>for</strong> the directed enhanced<br />
service by the BMA, clearly states that regular audits should be<br />
conducted to susta<strong>in</strong> a cont<strong>in</strong>ued high level <strong>of</strong> activity, and to ensure<br />
records <strong>of</strong> all procedures are ma<strong>in</strong>ta<strong>in</strong>ed and up-to-date and readily<br />
accessible which is clearly demonstrated with this audit. 1 However,<br />
because <strong>of</strong> the small sample size <strong>of</strong> 16, and short time period <strong>of</strong> the reaudit,<br />
an audit after a year would be more beneficial and accurate at<br />
estimat<strong>in</strong>g whether the first audit will have a significant impact on future<br />
practice.<br />
Un<strong>for</strong>tunately, with <strong>in</strong>cisions, only 14.3% had documented written<br />
consent and with the re-audit 0% had documented written consent. With<br />
regard to the first audit, from April 2005- April 2006, there were only<br />
seven <strong>in</strong>cisions with<strong>in</strong> the whole year, un<strong>for</strong>tunately six <strong>of</strong> which had no<br />
documented consent. Were these results due to the small sample size;<br />
due to the <strong>for</strong>getfulness <strong>of</strong> the general practitioners and the general<br />
<strong>in</strong>frequency <strong>of</strong> the procedure or is there a general acceptance that<br />
<strong>in</strong>cisions are not perceived as important enough <strong>for</strong> written consent?<br />
Aga<strong>in</strong> <strong>in</strong> the re-audit our questions were not answered, only one patient<br />
had an <strong>in</strong>cision to which consent was not documented. Future plans to<br />
re-educate the doctors with<strong>in</strong> the practice on the practice’s consent<br />
policy on m<strong>in</strong>or surgery and specifically <strong>in</strong>cision will need to be<br />
undertaken, as there appears to be a lack <strong>of</strong> consent documented with<br />
regards to <strong>in</strong>cisions. Obta<strong>in</strong><strong>in</strong>g and document<strong>in</strong>g <strong>in</strong><strong>for</strong>med consent with<strong>in</strong><br />
a busy practice must also be addressed as although time consum<strong>in</strong>g it is<br />
very important and must not be <strong>for</strong>gotten.<br />
Incidence<br />
<strong>An</strong>other audit was carried out from 2004 to 2005 <strong>in</strong> the same practice,<br />
analys<strong>in</strong>g m<strong>in</strong>or surgery. With<strong>in</strong> this audit, a total <strong>of</strong> 5 procedures had<br />
120
ecorded consent, and 45 had no recorded consent. This 2005-2006<br />
audit on ‘<strong>Consent</strong> <strong>for</strong> m<strong>in</strong>or surgery” exam<strong>in</strong>ed this aspect <strong>of</strong> m<strong>in</strong>or<br />
surgery more <strong>in</strong>tensively and found that there have been improvements,<br />
as a total <strong>of</strong> 77 procedures had recorded consent, with 45 procedures<br />
without.<br />
Limitations<br />
This study has several limitations. It <strong>in</strong>vestigates <strong>in</strong>cision, <strong>in</strong>jection and<br />
excision <strong>in</strong> depth, although it does not <strong>in</strong>clude all m<strong>in</strong>or surgery practices<br />
such as cautery and cryotherapy, which would be beneficial <strong>for</strong> <strong>in</strong>clusion<br />
<strong>in</strong> future audits. In addition, there were only three doctors analysed with<strong>in</strong><br />
this audit and the lack <strong>of</strong> published literature surround<strong>in</strong>g audits <strong>in</strong> m<strong>in</strong>or<br />
surgery and specifically consent, left difficulties compar<strong>in</strong>g one practice<br />
with another and the estimation <strong>of</strong> local and national trends. This may not<br />
be very symbolic <strong>of</strong> Northern Ireland’s trends or even Belfast’s. This audit<br />
does not <strong>in</strong>vestigate each doctor separately although if it did it may allow<br />
<strong>for</strong> specific weaknesses to be p<strong>in</strong>po<strong>in</strong>ted and <strong>for</strong> unnecessary re-tra<strong>in</strong><strong>in</strong>g<br />
<strong>of</strong> some doctors, and may p<strong>in</strong>-po<strong>in</strong>t strengths <strong>in</strong> certa<strong>in</strong> practice teach<strong>in</strong>g<br />
methods. It may also act as a means to deter doctors from <strong>for</strong>gett<strong>in</strong>g to<br />
record consent <strong>in</strong> the future as they would be aware <strong>of</strong> the audit and their<br />
result with<strong>in</strong> it. Of the procedures <strong>in</strong>vestigated every procedure with<strong>in</strong> the<br />
time period was analysed and recorded allow<strong>in</strong>g <strong>for</strong> an accurate data<br />
analysis. A potential limitation was the computer abilities <strong>of</strong> each doctor<br />
and the possibility that written consent was taken but not recorded<br />
correctly due to lack <strong>of</strong> time dur<strong>in</strong>g each consult. Fortunately, the audit<br />
specifies how consent should be documented if it is to be counted. This<br />
should there<strong>for</strong>e be the only method <strong>for</strong> documentation <strong>of</strong> consent, and if<br />
there are any differences between the practices <strong>of</strong> the doctors then these<br />
could easily be rectified by a computer lesson. However, as this would<br />
occur after the audit it leaves the possibility <strong>for</strong> consent to have been<br />
taken but not recorded correctly and there<strong>for</strong>e not <strong>in</strong>cluded <strong>in</strong> the results.<br />
In addition the computer cannot record whether verbal <strong>in</strong><strong>for</strong>med consent<br />
121
was obta<strong>in</strong>ed but not documented. Furthermore, the circumstances <strong>of</strong><br />
the general practice surgery are ever chang<strong>in</strong>g and this must be<br />
remembered, <strong>for</strong> <strong>in</strong>stance the number <strong>of</strong> m<strong>in</strong>or surgery procedures<br />
carried out between the audit and re-audit had dim<strong>in</strong>ished greatly. The<br />
decrease <strong>in</strong> frequency <strong>of</strong> the number <strong>of</strong> m<strong>in</strong>or surgery procedures was<br />
due to many contribut<strong>in</strong>g factors some <strong>of</strong> which <strong>in</strong>cluded pressure on<br />
appo<strong>in</strong>tments, the retirement <strong>of</strong> one <strong>of</strong> the doctors, and the replacement<br />
doctor lack<strong>in</strong>g the qualifications to per<strong>for</strong>m m<strong>in</strong>or surgery. However,<br />
evidence suggests that it is cost-effective <strong>for</strong> m<strong>in</strong>or surgery to be<br />
per<strong>for</strong>med <strong>in</strong> the general practice sett<strong>in</strong>g. [10]<br />
Risks <strong>of</strong> <strong>M<strong>in</strong>or</strong> surgery<br />
<strong>M<strong>in</strong>or</strong> surgery <strong>in</strong> the categories <strong>of</strong> exicison, <strong>in</strong>cision and <strong>in</strong>jection, all<br />
have their complications. Each m<strong>in</strong>or surgical procedure could result <strong>in</strong><br />
failure, a referral, further treatment, pa<strong>in</strong> from the procedure to which<br />
analgesia may be necessary, adverse effects, such as bleed<strong>in</strong>g, <strong>in</strong>fection<br />
and depend<strong>in</strong>g on the site, difficulty with movement, work<strong>in</strong>g and<br />
everyday activities. [11] Research on <strong>in</strong>fection rates follow<strong>in</strong>g m<strong>in</strong>or<br />
surgery <strong>in</strong> general practice appears to be very poor with most <strong>in</strong><strong>for</strong>mation<br />
centred on hospital <strong>in</strong>fection rates. However, research by Heal et al was<br />
undertaken to <strong>in</strong>vestigate the <strong>in</strong>cidence <strong>of</strong> and risk factors <strong>for</strong> surgical<br />
site <strong>in</strong>fections <strong>in</strong> a general practice <strong>in</strong> Australia. The randomised control<br />
trial assessed 857 patients <strong>in</strong> which 74 acquired an <strong>in</strong>fection. The<br />
presence <strong>of</strong> diabetes or those undergo<strong>in</strong>g excision <strong>of</strong> a non-melanocytic<br />
sk<strong>in</strong> cancer or excision from a lower limb correlated with a higher<br />
<strong>in</strong>cidence <strong>of</strong> <strong>in</strong>fection post-m<strong>in</strong>or surgery. This <strong>in</strong><strong>for</strong>mation should<br />
encourage use <strong>of</strong> antibiotics prophylactically <strong>for</strong> high-risk patients. [10]<br />
<strong>An</strong>other complication <strong>of</strong> m<strong>in</strong>or surgery can be bleed<strong>in</strong>g. However, a<br />
number <strong>of</strong> studies have been carried out on the topic <strong>of</strong> whether<br />
antiplatelet medication should be stopped prior to m<strong>in</strong>or surgical<br />
procedures. The French Society <strong>of</strong> <strong>An</strong>aesthesiology and Intensive Care<br />
published a statement say<strong>in</strong>g that the consequences <strong>of</strong> withdraw<strong>in</strong>g<br />
122
these medic<strong>in</strong>es (which may <strong>in</strong>clude a myocardial <strong>in</strong>farction) can<br />
outweigh the risks <strong>of</strong> any <strong>in</strong>creased peri-operative bleed<strong>in</strong>g, rout<strong>in</strong>e<br />
antiplatelet withdrawal is not recommended and may even be harmful,<br />
and should only be withdrawn if risks <strong>of</strong> bleed<strong>in</strong>g are greater than the<br />
cardiovascular risks <strong>of</strong> stopp<strong>in</strong>g. A number <strong>of</strong> studies show no pro<strong>of</strong> <strong>of</strong><br />
an <strong>in</strong>crease <strong>in</strong> bleed<strong>in</strong>g complications dur<strong>in</strong>g dermatological surgery and<br />
agree that the risks <strong>of</strong> stopp<strong>in</strong>g antiplatelet medic<strong>in</strong>es far outweigh the<br />
risk <strong>of</strong> complications from withdrawal. [12] <strong>An</strong>other audit on 61 procedures<br />
was carried out <strong>in</strong> a different practice <strong>in</strong> Australia, between April 2004<br />
and November 2004. It looked at the success rate <strong>of</strong> steroid <strong>in</strong>jection,<br />
and complication rates <strong>of</strong> all procedures. In the results there were no<br />
complications recorded <strong>for</strong> any procedure. [13] It is important to recognise<br />
the potential risk factors <strong>for</strong> m<strong>in</strong>or surgery and to realise the relative<br />
frequency <strong>of</strong> each and this is equally as important when expla<strong>in</strong><strong>in</strong>g to<br />
patients. A recent MDU study <strong>of</strong> GP m<strong>in</strong>or surgery settled claims<br />
revealed that nearly two-thirds <strong>of</strong> cases arose from one <strong>of</strong> the follow<strong>in</strong>g:<br />
scarr<strong>in</strong>g, per<strong>for</strong>ated ear drum, haemorrhage or haematoma, <strong>in</strong>fection,<br />
nerve damage and pa<strong>in</strong>. This signifies the importance <strong>of</strong> ga<strong>in</strong><strong>in</strong>g<br />
consent, document<strong>in</strong>g <strong>in</strong> the notes that consent was obta<strong>in</strong>ed, that the<br />
risks and effects have been expla<strong>in</strong>ed and that the patient has consented<br />
to it understand<strong>in</strong>g this <strong>in</strong><strong>for</strong>mation. [10] With regards to m<strong>in</strong>or surgery the<br />
consent must be <strong>in</strong> written <strong>for</strong>m and discussed <strong>in</strong> detail to ensure the<br />
patients understand<strong>in</strong>g and compliance with such procedures. [14]<br />
Although, the existence <strong>of</strong> a written document does not ascerta<strong>in</strong><br />
conclusive evidence that the patient has given adequately <strong>in</strong><strong>for</strong>med<br />
consent but merely stipulates that a discussion took place and a<br />
rem<strong>in</strong>der to the doctor to give sufficient <strong>in</strong><strong>for</strong>mation. [15] Ga<strong>in</strong><strong>in</strong>g <strong>in</strong><strong>for</strong>med<br />
consent from mentally ill or <strong>in</strong>tellectually disabled is a confus<strong>in</strong>g situation.<br />
In general, where <strong>in</strong>tellectually disabled patients have atta<strong>in</strong>ed the age <strong>of</strong><br />
18 and are not <strong>in</strong>stitutionalised, doctors should not proceed with any<br />
treatment, unless consent from the patient themselves has been<br />
obta<strong>in</strong>ed, apply<strong>in</strong>g generally, also to <strong>in</strong>stitutionalised patients. Under<br />
most legislation <strong>for</strong> the treatment <strong>of</strong> mentally disabled, consent <strong>of</strong> a<br />
123
parent or a legal guardian must be obta<strong>in</strong>ed be<strong>for</strong>e a procedure can be<br />
pre<strong>for</strong>med. [14]<br />
Ethical Issues<br />
Medical ethics is a generic term <strong>for</strong> the various ways <strong>of</strong> understand<strong>in</strong>g<br />
and exam<strong>in</strong><strong>in</strong>g moral life. Some approaches are normative, others are<br />
non-normative. Normative ethics is a <strong>for</strong>m <strong>of</strong> <strong>in</strong>quiry that attempts to<br />
answer a question. Non-normative ethics has two types, firstly<br />
descriptive which is the factual <strong>in</strong>vestigation <strong>of</strong> moral conduct and beliefs.<br />
The second is meta-ethics <strong>in</strong>volv<strong>in</strong>g analysis <strong>of</strong> language, concepts and<br />
methods <strong>of</strong> reason<strong>in</strong>g <strong>in</strong> ethics. These are grouped together as nonnormative<br />
because they determ<strong>in</strong>e what is factually and conceptually the<br />
case, not ethically what should be the case. [16] The belief that some<br />
knowledge should be shared with the patient is well established and<br />
safeguarded by legal codes. However, it is reasonable to suggest that<br />
doctors still significantly control what <strong>in</strong><strong>for</strong>mation is made available to<br />
patients and others <strong>in</strong>volved. This creates two problems, firstly, the<br />
knowledge which the doctor has and what they chose to do with it is<br />
crucial <strong>in</strong> the decision mak<strong>in</strong>g by the patient, and secondly, mak<strong>in</strong>g moral<br />
decisions is a process which demands factual knowledge <strong>of</strong> the patient’s<br />
condition by the patient. [17] With regards to obta<strong>in</strong><strong>in</strong>g consent <strong>for</strong> m<strong>in</strong>or<br />
surgery the doctor should present the medical facts accurately to the<br />
patient and strive to protect the patient’s autonomy where possible. [16, 18]<br />
Legally a doctor is free to choose who they will care <strong>for</strong>, but once they<br />
have undertaken a case the doctor becomes legally liable <strong>for</strong> the<br />
consequences <strong>of</strong> their own negligence. [14, 18] A duty <strong>of</strong> care arises once a<br />
doctor undertakes the care <strong>of</strong> a patient. All doctors have an obligation to<br />
keep abreast and be <strong>in</strong><strong>for</strong>med <strong>of</strong> technical advances, new techniques<br />
and therapy appropriate to the field <strong>of</strong> medic<strong>in</strong>e <strong>in</strong> which they practise or<br />
pr<strong>of</strong>ess special skills. A doctor can be negligent <strong>in</strong> many ways <strong>in</strong>clud<strong>in</strong>g<br />
negligent advice or failure to warn about the risks <strong>of</strong> a surgical<br />
procedure, such as m<strong>in</strong>or surgery. [14] In many situations, it is uncerta<strong>in</strong>,<br />
124
as to whether a customary standard exists <strong>for</strong> the communication <strong>of</strong><br />
medical <strong>in</strong><strong>for</strong>mation. The majority <strong>of</strong> pr<strong>of</strong>essionals could <strong>of</strong>fer the same<br />
<strong>in</strong>adequate level <strong>of</strong> <strong>in</strong><strong>for</strong>mation or have total discretion to determ<strong>in</strong>e the<br />
scope <strong>of</strong> disclosure, or possibly not know what <strong>in</strong><strong>for</strong>mation is <strong>in</strong> the best<br />
<strong>in</strong>terests <strong>of</strong> their patients. [16] With<strong>in</strong> Health Centre X however, there is a<br />
standard protocol <strong>for</strong> written consent <strong>for</strong> m<strong>in</strong>or surgery, the problem lies,<br />
with whether the doctor remembers the protocol, whether they then<br />
disclose the adequate <strong>in</strong><strong>for</strong>mation that is <strong>in</strong> their patients best <strong>in</strong>terests.<br />
In 2001, a BMA work<strong>in</strong>g party report concluded that the whole process <strong>of</strong><br />
obta<strong>in</strong><strong>in</strong>g patient consent would need to be thoroughly re-assessed.<br />
Greater emphasis was needed to be placed on the <strong>in</strong>itial explanation<br />
given to the patient, with provision <strong>for</strong> cont<strong>in</strong>u<strong>in</strong>g opportunity <strong>for</strong><br />
discussion <strong>in</strong> order that the patient could raise any concerns and/or<br />
questions. The Department <strong>of</strong> Health tried to deal with this situation by<br />
publish<strong>in</strong>g booklets deal<strong>in</strong>g with consent <strong>in</strong> specific situations, leaflets <strong>for</strong><br />
patients, and an implementation guide which <strong>in</strong>cluded model consent<br />
policy and <strong>for</strong>ms. [19] This audit highlights the importance <strong>of</strong> up-to-date<br />
medical records. For <strong>in</strong>stance, on some occasions consent may have<br />
been obta<strong>in</strong>ed but not documented correctly onto the computer. The<br />
medical records orig<strong>in</strong>ally began as ‘aide memoires’ <strong>for</strong> treat<strong>in</strong>g doctors,<br />
however nowadays, under the <strong>in</strong>fluence <strong>of</strong> factors such as Freedom <strong>of</strong><br />
In<strong>for</strong>mation legislation, concepts <strong>of</strong> openness and accountability, quality<br />
assurance, <strong>in</strong>volvement <strong>of</strong> patients more closely <strong>in</strong> understand<strong>in</strong>g their<br />
illnesses and be<strong>in</strong>g falsely <strong>in</strong><strong>for</strong>med be<strong>for</strong>e decisions are taken about<br />
treatment has lead to greater importance <strong>of</strong> the accuracy and objectivity<br />
<strong>of</strong> the medical record. The importance <strong>of</strong> keep<strong>in</strong>g the medical records at<br />
a high standard help ma<strong>in</strong>ta<strong>in</strong> the standard <strong>of</strong> patient care, <strong>for</strong> <strong>in</strong>stance,<br />
like <strong>in</strong> Health Centre X, where patients see different doctors; <strong>in</strong> after<br />
hours services and where the only communication between the locum<br />
and the treat<strong>in</strong>g doctor is <strong>in</strong> writ<strong>in</strong>g. [14] The pr<strong>in</strong>ciple <strong>of</strong> non-maleficence<br />
asserts an obligation, on the doctor, not to <strong>in</strong>flict harm onto others. Harm<br />
is difficult to classify but can be viewed as setbacks to physical or<br />
psychological <strong>in</strong>terests, such as health and survival. [16] Acquir<strong>in</strong>g valid<br />
125
consent from each patient allows the patient to prepare mentally, know<br />
what to expect and why they require the said treatment, allow<strong>in</strong>g <strong>for</strong> an<br />
<strong>in</strong><strong>for</strong>med decision to accept or refuse treatment, <strong>in</strong> view <strong>of</strong> their own<br />
subjective idea <strong>of</strong> what harm or <strong>in</strong>jury entails. When a patient is under<br />
the care <strong>of</strong> a doctor they should be treated autonomously, without harm<br />
and the treatment <strong>of</strong>fered should contribute to their welfare. This is<br />
known as ‘beneficence’. This <strong>in</strong>volves the doctor tak<strong>in</strong>g positive steps to<br />
help their patients. [16] In relation to the audit, if a doctor is seek<strong>in</strong>g<br />
<strong>in</strong><strong>for</strong>med consent from a patient it should clearly state the aims and<br />
benefits <strong>of</strong> the treatment as well as the risks, there<strong>for</strong>e re<strong>in</strong><strong>for</strong>c<strong>in</strong>g the<br />
positive steps which the doctor is mak<strong>in</strong>g. The concept <strong>of</strong> justice usually<br />
<strong>in</strong>cludes the terms fairness, entitlement and what is deserved.<br />
Distributive justice refers to the distribution <strong>of</strong> all rights and<br />
responsibilities <strong>in</strong> society. Several pr<strong>in</strong>ciples <strong>of</strong> justice appear with<strong>in</strong><br />
morality and merit acceptance. One is <strong>for</strong>mal, the rest material. Virtually<br />
all accounts <strong>of</strong> justice <strong>in</strong> health care hold that delivery programs and<br />
services designed to assist persons <strong>of</strong> a certa<strong>in</strong> class, such as poor or<br />
elderly, should be available to all that social class. Is it unjust to deny<br />
access to equally needy persons outside that social class? Material<br />
pr<strong>in</strong>ciples specify the relevant characteristics <strong>for</strong> equal treatment<br />
because they identify the substantive properties <strong>for</strong> distribution, such as<br />
need. Most societies <strong>in</strong>voke several <strong>of</strong> the material pr<strong>in</strong>ciples <strong>in</strong> fram<strong>in</strong>g<br />
public policy, appeal<strong>in</strong>g to different pr<strong>in</strong>ciples <strong>in</strong> different spheres and<br />
contexts. This allows <strong>for</strong> the fair distribution <strong>of</strong> treatment across social<br />
classes accord<strong>in</strong>g to need, ef<strong>for</strong>t, contribution, merit, free-market<br />
exchanges and allows each person an equal share. This is relevant to<br />
the audit <strong>in</strong> that <strong>in</strong><strong>for</strong>med consent should be obta<strong>in</strong>ed from everyone or<br />
their guardian where possible, and treatment should be equally<br />
distributed accord<strong>in</strong>g to these pr<strong>in</strong>ciples. [16] Ethically, the importance <strong>of</strong><br />
ga<strong>in</strong><strong>in</strong>g <strong>in</strong><strong>for</strong>med valid consent from each patient or someone<br />
responsible <strong>for</strong> the patient encompasses many issues. These issues<br />
<strong>in</strong>volve many fundamental ethical pr<strong>in</strong>ciples <strong>of</strong> a doctor, demonstrat<strong>in</strong>g<br />
the importance <strong>of</strong> ga<strong>in</strong><strong>in</strong>g and record<strong>in</strong>g <strong>in</strong><strong>for</strong>med consent accurately.<br />
126
Conclusion<br />
With the ever chang<strong>in</strong>g world <strong>of</strong> medic<strong>in</strong>e fundamental rules exist to<br />
protect the patient and the doctor, such as consent. <strong>Consent</strong> is not<br />
merely sign<strong>in</strong>g a sheet; it <strong>in</strong>volves tak<strong>in</strong>g the time to communicate to your<br />
patient the importance <strong>of</strong> the treatment, the options available, the<br />
prognosis, the reasons to and not to have the treatment and the risks<br />
and adverse effects <strong>of</strong> the treatment. The patient should only consent to<br />
a treatment when all areas have been covered. <strong>Consent</strong> is not only there<br />
to protect the patient but also to protect the doctor and to rem<strong>in</strong>d them <strong>of</strong><br />
the risks, treatment options and importance <strong>of</strong> the patients op<strong>in</strong>ion.<br />
<strong>Consent</strong> if correctly obta<strong>in</strong>ed can act as a legal document to demonstrate<br />
prior consultations and prove false allegations. It also re<strong>in</strong><strong>for</strong>ces some<br />
important ethical pr<strong>in</strong>ciples such as patients’ autonomy, non-maleficence,<br />
beneficence and justice. In brief, after the audit from April 2005 to April<br />
2006 Health Centre X’s record <strong>of</strong> document<strong>in</strong>g consent <strong>for</strong> m<strong>in</strong>or<br />
surgery, <strong>in</strong>cision, excision and <strong>in</strong>jection, was <strong>in</strong> need <strong>of</strong> much<br />
improvement. Recommendations where then implemented and<br />
underwent a re-audit from January to April 2007 which demonstrated a<br />
vast improvement, especially with regards to excision and <strong>in</strong>jection<br />
ga<strong>in</strong><strong>in</strong>g 100% <strong>of</strong> patients consent. Incisions <strong>in</strong> particular will need further<br />
developments and with cont<strong>in</strong>uous monitor<strong>in</strong>g and education standards<br />
should improve across each type <strong>of</strong> m<strong>in</strong>or surgery skill.<br />
References<br />
[1] Mazur DJ. Influence <strong>of</strong> the law on risk and <strong>in</strong><strong>for</strong>med consent. BMJ<br />
2003; 327: 731-734.<br />
[2] Shanner L. In<strong>for</strong>med consent and <strong>in</strong>adequate medical <strong>in</strong><strong>for</strong>mation.<br />
The Lancet 1995; 346: 251.<br />
[3] Clegg-Lamptey JNA, Hodasi WM. <strong>An</strong> audit <strong>of</strong> aspects <strong>of</strong> <strong>in</strong><strong>for</strong>med<br />
consent and pa<strong>in</strong> relief <strong>in</strong> surgical units <strong>of</strong> Korle Bu Teach<strong>in</strong>g Hospital.<br />
Ghana Medical Journal 2005; 39(2): 63-67<br />
127
http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubm<br />
edid=17299545 (Accessed 14 May 2007)<br />
[4] British Medical Association. <strong>M<strong>in</strong>or</strong> surgery- Specification <strong>for</strong> a directed<br />
enhanced service. http://www.bma.org.uk/ap.nsf/content/dessurgery<br />
(Accessed 11 Dec 2006)<br />
[5] <strong>Practice</strong> <strong>Consent</strong> Policy.<br />
[6] Primary Care Trusts NHS. Primary Care <strong>M<strong>in</strong>or</strong> <strong>Surgery</strong> <strong>Consent</strong><br />
Form.<br />
http://www.natpact.nhs.uk/uploads/DEFINING%ZODES%20m<strong>in</strong>or%20su<br />
rgery%20-%20consent.doc (Accessed 15 May 2007)<br />
[7] <strong>General</strong> Medical Council. Seek<strong>in</strong>g Patients’ consent: the ethical<br />
considerations 1998 http://www.gmcuk.org/guidance/current/library/consent.asp<br />
(Accessed on 11 Dec 2006)<br />
[8] BMJ news. <strong>Consent</strong> and records rema<strong>in</strong> major factors <strong>in</strong> m<strong>in</strong>or<br />
surgery claims. BMJ 1997; 314: 1849<br />
http://www.bmj.com/cgi/content/full/314/7098/1849/b (Accessed 15 May<br />
2007)<br />
[9] Syse A. Norway: valid (as opposed to <strong>in</strong><strong>for</strong>med) consent. The Lancet<br />
2000; 356 (9238): 1347-1348.<br />
[10] Heal C, Buettner P, Brown<strong>in</strong>g S. Risk factors <strong>for</strong> wound <strong>in</strong>fection<br />
after m<strong>in</strong>or surgery <strong>in</strong> general practice. The Medical Journal <strong>of</strong> Australia<br />
2006; 185(5): 255-258<br />
http://www.mja.com.au/public/issues/185_05_040906/hea10211_fm.html<br />
(Accessed 01 Aug 2007)<br />
[11] Lee R. <strong>Consent</strong> <strong>for</strong> m<strong>in</strong>or surgery. MDU 2007 http://www.themdu.com/search/hidden_article.asp?articleid=1104&articletitle=cons<br />
(Accessed 01 May 2007)<br />
[12] Pevreal W. Is it necessary to stop clopidogrel, dipyridamole or low<br />
dose aspir<strong>in</strong> prior to m<strong>in</strong>or surgery? UKMI<br />
www.nelm.nhs.uk/Documents/N27.1%20<strong>An</strong>tiplatelets%20and%20<strong>M<strong>in</strong>or</strong><br />
%20<strong>Surgery</strong>.doc?id=563677 (Accessed 01 Aug 2007)<br />
[13] Preest GA. <strong>M<strong>in</strong>or</strong> <strong>Surgery</strong> <strong>Audit</strong> November 2004.<br />
http://pencoedmedical.co.uk/pencoedmedical/<strong>M<strong>in</strong>or</strong>%20<strong>Surgery</strong>%20Audi<br />
128
t%20November%202004.doc (Accessed 01 Aug 2007)<br />
[14] Plueckhahn VD, Breen KJ, Cordner SM. Law and ethics <strong>in</strong> medic<strong>in</strong>e<br />
<strong>for</strong> doctors <strong>in</strong> Victoria. 1994:105-112.<br />
[15] Gattellari M, Butow PN, Tattersail MHN. In<strong>for</strong>med consent: what did<br />
the doctor say? The Lancet 1999; 353: 1713.<br />
[16] Beauchamp TL, Childress JF. Pr<strong>in</strong>ciples <strong>of</strong> biomedical ethics, 5 th<br />
edition. 2001.<br />
[17] Mitchell KR, Lovat TJ. Bioethics <strong>for</strong> medical and health pr<strong>of</strong>essionals<br />
1991.<br />
[18] Council on Ethical and Judicial Affairs. Code <strong>of</strong> Medical Ethics.<br />
2000-2001.<br />
[19] English V, Romano-Critchley G, Sheather J, Sommerville A. Medical<br />
Ethics today the BMA’s handbook <strong>of</strong> ethics and law. 2004.<br />
129