Prior L - Queen's University Belfast
Prior L - Queen's University Belfast
Prior L - Queen's University Belfast
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Qualitative Research Design and Ethical<br />
Governance: some problems of ‘fit’<br />
Lindsay <strong>Prior</strong>, Professor of Sociology, Queen’s <strong>University</strong> <strong>Belfast</strong><br />
Address for Correspondence: School of Sociology, Social Policy and Social Work,<br />
Queen’s <strong>University</strong> <strong>Belfast</strong>, Room 2.01, 1 College Park East, <strong>Belfast</strong> BT7 1NN.<br />
Email: l.prior@qub.ac.uk<br />
In this paper I seek to do three things. First to consider the extent to<br />
which some of the common procedures used by qualitative researchers<br />
‘fit’ the demands of medical research ethics committees. Second, to<br />
highlight some ways in which some key principles of qualitative research<br />
have to be altered so as to facilitate any such fit. Third, to highlight the<br />
range of issues that can (and do) arise out of an actual qualitative<br />
research project. J NI Ethics Forum 2007, 4: 53-64<br />
Just by way of preface to the ensuing discussion it would be as well for<br />
me to draw attention to a number of issues. The first of these is that<br />
qualitative researchers have been sensitive to, and have discussed<br />
problems of research ethics for many decades, and many such<br />
researchers believe themselves to be well attuned to both the<br />
philosophical basis of ethical codes and the practical implications of such<br />
codes for research design and procedure. Thus Miles and Huberman<br />
(1994), for example, outline seven styles of ethical framework that can<br />
inform qualitative research practice and indicate the implications of such<br />
styles for research activity. It is also fair to say that the British<br />
Sociological Association’s statement of Ethical Practice (2002) has not<br />
only provided guidance on ethical problems connected to qualitative<br />
research work for many decades, but also touches upon issues that are<br />
rarely considered by members of contemporary research ethics<br />
committees (such as power and gender imbalances in research<br />
relationships). Similar concerns are covered in the codes of ethical<br />
53
practice of other national bodies – such as that of the American<br />
Sociological Association. Finally, there is empirical evidence (Richardson<br />
and McMullan, 2007) that many qualitative researchers hold somewhat<br />
negative opinions of the ways in which REC’s assess their research<br />
design and believe that REC’s actually inhibit, rather than facilitate good<br />
research. In what follows I hope to throw some light on why such<br />
assessments might arise. My strategy is to elaborate on the kinds of<br />
ethical issues that arose out of a specific ESRC research project for<br />
which I was a principal investigator. For a formal report on the project –<br />
outlining the aims, design and some of the findings – see <strong>Prior</strong>, 2005.<br />
Somewhat inevitably, the discussion of that project herein is selective.<br />
An ESRC Case Study:<br />
The project to which I refer formed one component of the ESRC funded<br />
Innovative Health Technologies Research Programme (Project<br />
L218252046). The research work was undertaken between 2001—04.<br />
The key aims can be summed up in three questions. Exactly how do<br />
clinical professionals in a regional cancer genetics service assemble<br />
cancer genetic risk assessments? What are the consequences of the<br />
risk assessment for patients/clients? How do patients/clients understand<br />
the risk assessment and its implications? The research work was further<br />
linked into a parallel Wellcome funded study on the ways in which<br />
genetic risks might be calculated and used for insurance purposes.<br />
Research ethics approval was sought from, and granted by an MREC<br />
and 4 LREC’s (whose approval was necessary at that stage). Each<br />
required separate applications, and attendance at a committee meeting.<br />
The Wellcome funded project was dealt with under an additional MREC<br />
application.<br />
It is worth emphasising that the research ethics approval process was<br />
time consuming (and therefore expensive) in itself. We began the<br />
process of seeking approval 3 months before the project start date (when<br />
54
we were not yet funded), and the process cut into first 3 months of the<br />
funded project. There was also intermittent approval required following<br />
research design modifications.<br />
The kinds of issues that were attended to in the MREC application<br />
involved the processes surrounding informed consent, confidentiality,<br />
anonymity, and the possibility of causing anxiety and distress to lay<br />
respondents (Richards & Shwartz, 2002). Some issues we did not raise<br />
because REC’s are so rarely concerned with them. The latter include<br />
issues relating to the exploitation of the research participants, dangers<br />
and risks that may be faced by the researchers, and the fact that in<br />
health research ‘patients’ often disclose details about their health that<br />
they have deliberately concealed from their doctors. As researchers we<br />
need strategies for handling such circumstances, but for my own part I<br />
prefer not to draw attention to such matters for fear of complications<br />
arising out of the approval process.<br />
The research design contained many features, but at base it was<br />
intended to be an ‘ethnography’ of a clinical service. The key site for<br />
research was an institute of medical genetics, and the service covered<br />
an entire UK region. I have no wish to elaborate on the theory and<br />
practice of ethnography here, so suffice it to say that ethnography truly<br />
involves immersion into the culture of the selected study group. An<br />
important feature of ethnographic practice is its capacity to capture<br />
aspects of behaviour, human interaction, events, happenings and so<br />
forth ‘on the wing’; as they emerge and unfold in the hurly burly of daily<br />
life - that’s what it’s all about. And once a study begins then everything<br />
and everyone is ‘in’ the research frame. To quote from one of the<br />
greatest exponents of the method (the anthropologist Bronislaw<br />
Malinowski);<br />
“There is a series of phenomena of great importance which cannot<br />
possibly be recorded by questioning or computing documents, but have<br />
55
to be observed in their full actuality. Let us call them the imponderabilia<br />
of actual life …” (Malinowski, 1922:18)<br />
One implication of this for the ethnographer is that the process of<br />
informed consent as conceptualized by REC’s can be somewhat<br />
stultifying and inimical to good research. That, not least because consent<br />
(in an ethnographic setting) has to be viewed as an ongoing, negotiable,<br />
and continuous process, rather than something that can be wrapped up<br />
in a single (signed) document - but more of consent in a moment.<br />
Essentially, all that I wish to emphasize at this stage is that it is the<br />
emergent, unfolding nature of the research trajectory that tends to affect<br />
the balance between the demands of the RECs and the practices of<br />
qualitative researchers.<br />
Types of data collected:<br />
In the case study to which I refer, various kinds of data were collected.<br />
These included: observations of professionals at work in the clinic and<br />
the associated laboratory; discussions between nurse-counsellors and<br />
clinical geneticists about risk assessment of patients (which I call<br />
‘naturally-occurring’ data, rather than interview data); consultations<br />
between clinical professionals and patient/clients about risk assessment<br />
and its implications; interviews between social scientists and patients<br />
about their understandings of their risk assessment; interviews with lab<br />
scientists and some clinical staff; medical records (such as pedigrees)<br />
and documents of various kinds including GP referral letters. An example<br />
of the kind of data collected is provided in Box1. The discussion begins<br />
with a nurse reading out a GP referral letter and flows into a discussion<br />
between a consultant geneticist and two nurses about the case under<br />
referral.<br />
Now, gaining informed consent from the nurse-counsellors and the<br />
consultant is not a problem – we know in advance who they are, and<br />
56
what they will be doing. However, we do not know on any one (Monday)<br />
morning who is to be referred to the clinic – this is the task at hand for<br />
the clinic professionals. To capture discussion about a referral therefore<br />
requires ‘being there’ on the day, and it would simply not be possible to<br />
get consent from either the GP or the patient under discussion about the<br />
presence of a researcher for we have no idea who is being referred in<br />
advance of the referral. This kind of problem arises in quite a few medical<br />
settings - such as studies of emergency psychiatric admissions, for<br />
example, where seeking consent from an angry and confused person<br />
who is about to be ‘sectioned’ is simply not feasible. Clearly, if ‘informed<br />
consent’ were to be held to as a sine qua non of all research activity,<br />
then large numbers of very important procedures would lay beyond the<br />
boundaries of investigation (Sin, 2005).<br />
A related problem arises in consideration of medical pedigrees – an<br />
example of which is provided in figure 1. This figure is of a family tree or<br />
pedigree of a client of a genetics service. Females are represented by<br />
means of circles and males by squares. People affected by cancers are<br />
indicated by solid black symbols and deaths by diagonal lines; the arrow<br />
(lower left) points to the proband or client of the service. The pedigree<br />
was drawn by a computerised decision-aid named ‘Cyrillic’, which also<br />
calculates a life-time risk of inheriting a known mutation. In this case (for<br />
breast cancer) the capacity to calculate the risk of inheriting a cancer<br />
related mutation for family members is not particularly easy. For some<br />
conditions, however, (such as, say, Polycystic Kidney Disease (PKD) or<br />
Huntingdon’s disease), knowledge about one member of family can<br />
provide easy-to-calculate, important and critical information about many<br />
other members of the same family. So it is more than possible to obtain<br />
key medical data on relatives of an individual without the relatives either<br />
knowing or consenting. Unfortunately, there is no easy way of getting<br />
such consent – often relatives are out of touch with the proband, or the<br />
proband does not want relatives contacted, perhaps addresses are<br />
unknown, and whether relatives are living or dead can only be guessed<br />
57
at. There are of course strategies for dealing with such problems, but<br />
none of them involve getting informed consent from each an every<br />
individual in the frame.<br />
Sampling: Another problem area<br />
Selecting samples in qualitative research designs also tends to cause<br />
problems for RECs. This is because qualitative researchers are rarely<br />
interested in getting hold of random samples from large populations. Talk<br />
of power calculations and confidence intervals is simply not appropriate.<br />
Indeed, it is usually the case that the qualitative researcher is seeking<br />
specific cases of events, happenings and people rather than general<br />
samples. Often they seek out what might be termed outliers rather than<br />
cases that might be categorised as average. On occasion the sampling<br />
strategy makes sense to all – thus a study of adverse events necessarily<br />
focuses on instances when things have ‘gone wrong’ and where a study<br />
of representative cases would be inappropriate. In other instances the<br />
qualitative researcher might invoke the techniques of grounded theory to<br />
justify their research sampling strategy.<br />
Grounded theory (Glaser & Strauss, 1967) is undoubtedly one of the<br />
most widely cited and successful qualitative research strategies yet<br />
invented. It comes in a variety of forms. In virtually all of its forms<br />
however it advocates the use of conceptual or theoretical sampling rather<br />
than random sampling. The key idea related to theoretical sampling<br />
involves comparison of cases. Crudely put, the research begins with<br />
case 1 and then seeks out an alternative and contrasting case for study,<br />
which leads to the identification of another (third) contrasting case and so<br />
on until the field of possibilities has been ‘saturated’. In the words of<br />
Glaser and Strauss (1967:45);<br />
“Theoretical sampling is the process of sampling … whereby the analyst<br />
jointly collects codes and analyzes his data and [then] decides what data<br />
58
to collect next and where to find them in order to develop his theory as it<br />
emerges.”<br />
Needless to say, this strategy is not conducive to the requirements for a<br />
carefully specified research protocol. As a result, strategies and<br />
justifications have to be devised by qualitative researchers somewhat<br />
artificially so as to fit REC queries about ‘numbers’. In my own case I<br />
always structure the sample to throw up contrasts in advance – but this is<br />
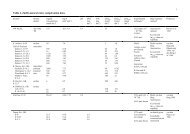
in no way a standard procedure. An example of a sample of cases<br />
structured for contrast is illustrated in Table 1 – the contrasts being site<br />
of cancer and level of risk. The cell numbers are determined on the basis<br />
of possibilities (how many ‘other’ genetically determined cancers might<br />
we get?), and experience (one rarely needs more than 10 cases to get a<br />
full sense of what is going on in any specific social environment).<br />
Table 1 .Numbers of patients interviewed by site of cancer and<br />
level of risk in the ESRC study<br />
Cancer site by risk Low Risk Moderate High Risk Total<br />
Risk<br />
Breast 8 11 6 25<br />
Ovarian 8 3 6 11<br />
Colorectal 6 10 4 20<br />
Other cancers 1 0 1 2<br />
Total 17 24 17 58<br />
The interview schedule:<br />
It would be amiss of me to ignore concerns about interview schedules.<br />
Once again, however, there are often antithetical understandings about<br />
the role of the interviewer and the interview in qualitative research. Thus,<br />
for many REC members the ‘instrument’ is the interview schedule – and<br />
therefore ought to be precisely specified. For qualitative researchers, on<br />
59
the other hand, the key instrument is the interviewer him or herself. It is<br />
they that constitute the key resource.<br />
For my own part I always try to get a ‘story’ out my respondents. In fact, I<br />
just ask respondents to ‘tell me your story’ – about how they got into a<br />
clinic, what happened next, and after that, the future. From this style of<br />
questioning one gets the data for a series of narratives, and it is in terms<br />
of narratives that such data can be (very profitably) analysed (see, for<br />
example, Frank, 1995). In the ESRC study we presented a somewhat<br />
more complicated interview schedule than was suggested above - but<br />
the ‘tell me your story’ approach would have served just as well. (For<br />
some results of the approach see Scott, <strong>Prior</strong>, Wood and Gray, 2005).<br />
Miscellaneous considerations:<br />
As I suggested in my opening statement, qualitative researchers are fully<br />
aware of a complex inter-relationship of ethical concerns that arise in the<br />
doing of research, and often pay respect to principles that RECs can be<br />
unduly quiet about. In terms of the case-study referred to here, however,<br />
it might be worth mentioning a few other considerations that arose during<br />
the course of the work. The first of these is quite common. It relates to<br />
the fact that in virtually all instances of research involving patients, some<br />
respondents will invariably seek medical advice from the (social<br />
scientific) interviewer – clear direction to interviewers on how to handle<br />
such eventualities is essential. Secondly, clinicians and others can<br />
sometimes be unhappy about the specific features of a research<br />
procedure and seek to alter the protocol or the findings – for example,<br />
nephrologists might object to PKD being described or characterised to<br />
their patients as a ‘genetic’ condition in the information leaflet. An<br />
advisory committee to which such problems can be referred can be<br />
useful in such instances. Thirdly, there can be ethical problems involved<br />
in archiving data – for whilst the identity of respondents and places can<br />
60
e rendered anonymous in written transcripts the same cannot be said<br />
about voice recordings.<br />
Conclusion:<br />
The ‘fit’ between qualitative research and research ethics committees is<br />
not an easy one. The research style and ‘ethos’ implied by the REC<br />
forms (at the outset) is geared to a specific (and very different) style of<br />
research practice and scientific rhetoric. More directly, qualitative<br />
researchers often face difficulties in justifying sample numbers, and<br />
accounting for the emergent shifts in direction that inevitably occur in<br />
qualitative work. In addition, there can be problems justifying open-ended<br />
interviews.<br />
As a result of the different interpretations of what good research design<br />
looks like, tensions can arise. Indeed, some social science researchers<br />
often feel that the procedures of ethical governance are used as forms of<br />
censorship and control – rather than a means of facilitating good<br />
research (Dingwall, 2006). For my own part I can say that only once<br />
have I ever had a real problem with a REC. In any event I shall conclude<br />
with a reference to one of the greatest ethicists of all time, namely<br />
Aristotle (384-321 BCE). In the Nicomachean Ethics, Aristotle argued<br />
that ethics aims at ‘the Good’ and that the good is a form of politics<br />
(I,1,4-ii). In that context he offers an interesting juxtaposition of a<br />
principle (the search for the good) and practice (organizing social affairs<br />
so that different interpretations of ‘the good’ can be facilitated).<br />
Unfortunately, qualitative researchers sometimes feel that interpretations<br />
of good ‘science’ as interpreted by REC members can be strangely onedimensional,<br />
and that their own (qualitative) style of understanding the<br />
world is being forced into a format that suits legalistic principles more<br />
than the requirements of sound research procedures.<br />
61
Professor <strong>Prior</strong> was one of the speakers at the NI Ethics Forum Evening Meeting in<br />
November 2007 focusing on the theme of research governance and qualitative<br />
research.<br />
References<br />
[1] Aristotle Nicomachean Ethics. Trans. H. Rackham. Cambridge: MA.<br />
Loeb Classical Library. Harvard <strong>University</strong> Press 1926.<br />
[2] BSA (2002) Statement of Ethical Practice for the British Sociological<br />
Association. http://www.sociology.org.uk/as4bsoce.pdf<br />
[3] Dingwall R. Confronting the anti-democrats. The unethical nature of<br />
ethical regulation in social science. Medical Sociology Online. 1. 2006:<br />
51-8.<br />
[4] Frank A.W. The wounded storyteller. Body, Illness and Ethics.<br />
Chicago: <strong>University</strong> of Chicago Press 1985.<br />
[5] Glaser B.G., Strauss A.L. The discovery of grounded theory.<br />
Strategies for qualitative research. Chicago: Aldine 1967.<br />
[6] Malinowski B. Argonauts of the Western Pacific. London: Routledge &<br />
Kegan Paul 1922.<br />
[7] Miles M.B., Huberman A.M. Qualitative Data Analysis. An expanded<br />
Sourcebook. 2 nd Ed. Thousand Oaks: CA. Sage 1994<br />
[8] <strong>Prior</strong> L. The construction of risk estimates in a cancer genetics clinic.<br />
Swindon: ESRC 2005.<br />
[9] Richards H.M., Schwartz L. J. Ethics of qualitative research. Are there<br />
special issues for health service research? Family Practice, 2002;<br />
19:135-9.<br />
[10] Richardson S., McMullan M. Research Ethics in the UK. Sociology<br />
2007; 41:1115-32.<br />
[11] Scott S., <strong>Prior</strong> L., Wood F., Gray J. Repositioning the patient. The<br />
implications of being at-risk. Social Science & Medicine 2005; 60: 1869-<br />
79.<br />
[12] Sin C.H. Seeking informed consent. Reflections on research<br />
practice. Sociology 2005; 39: 277-94.<br />
62
BOX1<br />
Nurse-Counsellor1 (NC1): This is JH who is 32. [Reading the referral<br />
letter from the patient’s GP] ‘This lady’s 35 year old sister has just been<br />
diagnosed with breast cancer. She herself is 33 and is naturally<br />
concerned. There are other sufferers of the disease in the family. An<br />
aunt was also diagnosed in her early 30s. She realises that the risks are<br />
going to be higher than average. She has been thinking of the<br />
contraceptive pill although I have asked her to put this on hold until she<br />
has been seen and then presumably I will be able to give her a<br />
progesterone only pill if you feel this is indicated.’ It’s from her GP.<br />
NC2: It’s a really good GP.<br />
Clinical Geneticist (CG): Yes, [examining the pedigree] the thing is if you<br />
really start to tease it apart there are lots of black lines all over the place,<br />
they are all on different parts of the family. Her grandmother’s niece. 40s.<br />
NC1: That’s 3 rd degree.<br />
CG: Well that is 3 rd degree yeah. And her mother’s grandfather’s<br />
sister at 67 so I think we can discount that one. This is the one that is of<br />
more concern. She has a sister at 35 and then somebody else at 38<br />
over here. So there are two young people and I suspect that puts her<br />
into a high – oh! – 24.6% (Looks at risk estimate from Cyrillic). Mm.<br />
NC1: What did you think, because you had some good thoughts about<br />
this one?<br />
CG: This is one that I would put into a high risk group. Can you think<br />
why I have decided to put her into a high risk group?<br />
63
Figure 1. Pedigree drawn and risk calculated via CYRILLIC<br />
64