HIV/AIDS Pediatric Case Report Form - Pinellas County Health ...
HIV/AIDS Pediatric Case Report Form - Pinellas County Health ...
HIV/AIDS Pediatric Case Report Form - Pinellas County Health ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
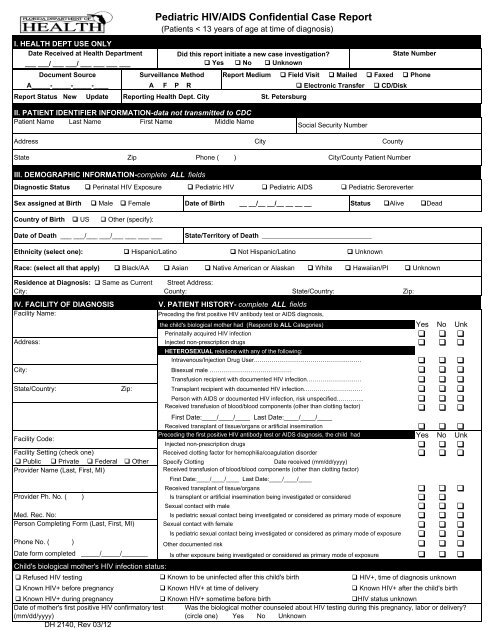
I. HEALTH DEPT USE ONLY<br />
Date Received at <strong>Health</strong> Department<br />
___ ___/ ___ ___/ ___ ___ ___ ___<br />
Document Source<br />
<strong>Pediatric</strong> <strong>HIV</strong>/<strong>AIDS</strong> Confidential <strong>Case</strong> <strong>Report</strong><br />
(Patients < 13 years of age at time of diagnosis)<br />
Surveillance Method<br />
Did this report initiate a new case investigation?<br />
Yes No Unknown<br />
A_____-_____-_____-____ A F P R<br />
Electronic Transfer CD/Disk<br />
<strong>Report</strong> Status New Update <strong>Report</strong>ing <strong>Health</strong> Dept. City St. Petersburg<br />
State Number<br />
<strong>Report</strong> Medium Field Visit Mailed Faxed Phone<br />
II. PATIENT IDENTIFIER INFORMATION-data not transmitted to CDC<br />
Patient Name Last Name First Name Middle Name<br />
Social Security Number<br />
Address City <strong>County</strong><br />
State Zip Phone ( ) City/<strong>County</strong> Patient Number<br />
III. DEMOGRAPHIC INFORMATION-complete ALL fields<br />
Diagnostic Status Perinatal <strong>HIV</strong> Exposure <strong>Pediatric</strong> <strong>HIV</strong> <strong>Pediatric</strong> <strong>AIDS</strong> <strong>Pediatric</strong> Seroreverter<br />
Sex assigned at Birth Male Female Date of Birth __ __/__ __/__ __ __ __ Status Alive Dead<br />
Country of Birth US Other (specify):<br />
Date of Death ___ ___/___ ___/___ ___ ___ ___<br />
State/Territory of Death _________________________________<br />
Ethnicity (select one): Hispanic/Latino Not Hispanic/Latino Unknown<br />
Race: (select all that apply) Black/AA Asian Native American or Alaskan White Hawaiian/PI Unknown<br />
Residence at Diagnosis: Same as Current Street Address:<br />
City: <strong>County</strong>: State/Country: Zip:<br />
IV. FACILITY OF DIAGNOSIS<br />
V. PATIENT HISTORY- complete ALL fields<br />
Facility Name:<br />
Preceding the first positive <strong>HIV</strong> antibody test or <strong>AIDS</strong> diagnosis,<br />
the child's biological mother had (Respond to ALL Categories)<br />
Perinatally acquired <strong>HIV</strong> infection<br />
Address: Injected non-prescription drugs<br />
City:<br />
HETEROSEXUAL relations with any of the following:<br />
Yes No Unk<br />
<br />
<br />
Intravenous/Injection Drug User……………………………………………….<br />
<br />
Bisexual male ……………………………………<br />
<br />
Transfusion recipient with documented <strong>HIV</strong> infection……………………….<br />
<br />
<br />
Person with <strong>AIDS</strong> or documented <strong>HIV</strong> infection, risk unspecified…………..<br />
<br />
Received transfusion of blood/blood components (other than clotting factor)<br />
<br />
State/Country: Zip: Transplant recipient with documented <strong>HIV</strong> infection…………………………<br />
First Date:____/____/____ Last Date:____/____/____<br />
Received transplant of tissue/organs or artificial insemination<br />
Facility Code:<br />
Preceding the first positive <strong>HIV</strong> antibody test or <strong>AIDS</strong> diagnosis, the child had<br />
Injected non-prescription drugs<br />
Facility Setting (check one) Received clotting factor for hemophilia/coagulation disorder<br />
Public Private Federal Other Specify Clotting<br />
Date received (mm/dd/yyyy)<br />
Provider Name (Last, First, MI)<br />
Received transfusion of blood/blood components (other than clotting factor)<br />
First Date:____/____/____ Last Date:____/____/____<br />
Received transplant of tissue/organs<br />
Provider Ph. No. ( )<br />
Sexual contact with male<br />
Med. Rec. No:<br />
Sexual contact with female<br />
Is pediatric sexual contact being investigated or considered as primary mode of exposure<br />
Phone No. ( )<br />
Other documented risk<br />
Date form completed _____/_____/_______<br />
<br />
Yes No Unk<br />
<br />
<br />
<br />
Is transplant or artificial insemination being investigated or considered <br />
<br />
Is pediatric sexual contact being investigated or considered as primary mode of exposure <br />
Person Completing <strong>Form</strong> (Last, First, MI) <br />
<br />
<br />
Is other exposure being investigated or considered as primary mode of exposure <br />
Child's biological mother's <strong>HIV</strong> infection status:<br />
Refused <strong>HIV</strong> testing<br />
Known to be uninfected after this child's birth<br />
<strong>HIV</strong>+, time of diagnosis unknown<br />
Known <strong>HIV</strong>+ before pregnancy Known <strong>HIV</strong>+ at time of delivery Known <strong>HIV</strong>+ after the child's birth<br />
Known <strong>HIV</strong>+ during pregnancy<br />
Known <strong>HIV</strong>+ sometime before birth<br />
<strong>HIV</strong> status unknown<br />
Date of mother's first positive <strong>HIV</strong> confirmatory test Was the biological mother counseled about <strong>HIV</strong> testing during this pregnancy, labor or delivery?<br />
(mm/dd/yyyy)<br />
(circle one) Yes No Unknown<br />
DH 2140, Rev 03/12
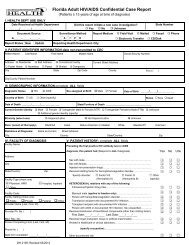
IX. TREATMENT/SERVICES REFERRALS<br />
This child received or is receiving:<br />
Neonatal zidovudine (ZDV, AZT) for <strong>HIV</strong> prevention<br />
Other neonatal anti-retroviral medication for <strong>HIV</strong> prevention<br />
If Yes, specify the medications:<br />
Anti-retroviral therapy for <strong>HIV</strong> treatment<br />
PCP prophylaxis<br />
Was the child breastfed?<br />
□ Yes □ No □ Unknown<br />
□ Yes □ No □ Unknown<br />
□ Yes □ No □ Unknown<br />
This child's primary □ Biological parents □ Foster/adoptive parent, relative □ Social service agency □ Unknown<br />
caretaker is: □ Other relative □ Foster/adoptive parent, unrelated □ Other (if Other, please specify):<br />
VI. LABORATORY DATA<br />
<strong>HIV</strong> Antibody Tests at Diagnosis (Indicate first test - mm/dd/yyyy)<br />
<strong>HIV</strong>-1 EIA<br />
<strong>HIV</strong>-1/2 EIA<br />
<strong>HIV</strong> -1/2 Ag/Ab<br />
<strong>HIV</strong>-1/2 Differentiating<br />
(e.g., Multispot)<br />
<strong>HIV</strong>-1 RNA NASBA<br />
<strong>HIV</strong>-1 RNA RT-PCR<br />
Was patient confirmed by a physician as:<br />
Positive<br />
<strong>HIV</strong>- infected □ Yes □ No □ Unknown<br />
Not <strong>HIV</strong>- infected □ Yes □ No □ Unknown<br />
Negative<br />
<strong>HIV</strong>-1 Western Blot/IFA<br />
Other<br />
Viral Load Test: ( most recent test- mm/dd/yyyy)<br />
Type Name Copies / ML Collection Date<br />
<strong>HIV</strong>-1 RNA bDNA<br />
<strong>HIV</strong>-1 RNA Other<br />
VII. CLINICAL STATUS<br />
Clinical Record Reviewed? □ Yes □ No<br />
Bacterial infection, multiple or recurrent (including<br />
Salmonella septicemia)<br />
Candidiasis, bronchi, trachea, or lungs<br />
Candidiasis, esophageal<br />
Coccidioidomycosis, disseminated or extrapulmonary<br />
Cryptococcosis, extrapulmonary<br />
Cryptosporidiosis, chronic intestinal (>1 mo. duration)<br />
Cytomegalovirus disease (other than in liver, spleen, or<br />
nodes) onset at > 1 mo of age<br />
Cytomegalovirus retinitis (with loss of vision)<br />
<strong>HIV</strong> encephalopathy<br />
Herpes simplex: chronic ulcer(s) (>1 mo. duration); or<br />
bronchitis, pneumonitis or esophagitis onset>1 mo of age<br />
Initial Dx Date<br />
mm/dd/yy<br />
Def.<br />
Pres.<br />
□ Yes □ No □ Unknown<br />
□ Yes □ No □ Unknown<br />
<strong>HIV</strong> Detection Tests: (Record earliest test-mm/dd/yyyy)<br />
Positive<br />
<strong>HIV</strong>-1 P24 Antigen<br />
<strong>HIV</strong>-1RNA PCR (Qual)<br />
<strong>HIV</strong>-1 Culture<br />
<strong>HIV</strong>-1 Proviral DNA (Qual)<br />
<strong>HIV</strong>-2 Culture<br />
Other<br />
Other<br />
Immunologic Lab Test: (test date-mm/dd/yyyy)<br />
At or closest to current diagnostic status<br />
CD4 Count:____________ cells/ul (________%)<br />
First1 mo. duration) ___/___/____ □ Wasting syndrome due to <strong>HIV</strong><br />
___/___/____ □<br />
Has the child been diagnosed with pulmonary tuberculosis? □ Yes □ No □ Unknown<br />
Def.<br />
Pres.<br />
If Yes, initial diagnosis and date<br />
□ TB pre- 1993 □ Definitive □ Presumptive □ Unknown (mm/dd/yyyy)<br />
RVCT <strong>Case</strong> Number<br />
DH 2140, Rev 03/12
VIII. BIRTH HISTORY (for PERINATAL cases only)<br />
Birth history available for this child:<br />
□ Yes □ No □ Unknown<br />
Residence at Birth: □ Same Address as patient address Address:<br />
If No or Unknown, do not complete this section.<br />
City: <strong>County</strong>: State/Country: Zip:<br />
Hospital at Birth: Facility Name: Phone No: ( ) -<br />
Address: City: <strong>County</strong>: State/Country: Zip:<br />
Birth weight<br />
Birth Type □ Single □ Twin □ > 2 □ Unknown<br />
enter lbs/oz OR grams Birth Delivery □ Vaginal □ Elective Caesarean □ Non-elective Caesarean □ Caesarean, Unk type □ Unk<br />
________ (lbs) Birth Defects □ Yes □ No □ Unknown<br />
________ (oz) Specify:<br />
________ (g) Code:<br />
Neonatal Status: □ Full term □ Premature<br />
Prenatal Care- Month of pregnancy when prenatal care began:<br />
Prenatal Care- Total number of prenatal care visits<br />
If Yes, specify types and enter codes, if known:<br />
Specify:<br />
Code:<br />
Did mother receive zidovudine (ZDV, AZT) during pregnancy? □ Yes □ No □ Refused □ Unknown<br />
If Yes, week of pregnancy when zidovudine (ZDV, AZT) began: Week ____________<br />
(99=Unknown)<br />
Did mother receive zidovudine (ZDV, AZT) during labor/delivery? □ Yes □ No □ Refused □ Unknown<br />
Did mother receive zidovudine (ZDV, AZT) prior to this pregnancy? □ Yes □ No □Unknown<br />
Did mother receive any other antiretroviral medication during pregnancy? □ Yes □ No □ Unknown<br />
If Yes, specify:<br />
Did mother receive any other antiretroviral medication during labor/delivery? □ Yes □ No □ Unknown<br />
If Yes, specify:<br />
Maternal Date of Birth<br />
Maternal State Patient Number<br />
Birthplace of Biological Mother<br />
□ U.S. □ U.S. Minor Outlying Area: (specify)<br />
□ Unknown □ Other: (specify)<br />
X. LOCAL FIELDS (health department use only)<br />
PRISM #<br />
Link with eHARS stateno(s):<br />
EPF____ EPF DATE_____________<br />
SOURCE CODE A__________<br />
No. of weeks (gestational age)<br />
Maternal Soundex<br />
(99-Unknown)<br />
(99-Unknown) (00=None)<br />
(99-Unknown) (00=None)<br />
HEPATITIS: A____ B____ C____ Other____ Unknown_____<br />
NIR STATUS: NIR_OP______ NIR OP DATE______________<br />
NIR_ CL______ NIR CL DATE________________<br />
OTHER RISKS: A____ B/C____ D____ F____ M____ V____ J____ NIR_RE_______ NIR RE DATE____________ Initials (3)________<br />
XI. COMMENTS (e.g. birth mother history on drug use, STDs, mental illness, jail history, father, siblings, etc.)<br />
DH 2140, REV. 03/12