Guidelines for Medication Error Prevention - Pharmacy Practice News
Guidelines for Medication Error Prevention - Pharmacy Practice News
Guidelines for Medication Error Prevention - Pharmacy Practice News
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Guidelines</strong> <strong>for</strong><br />
<strong>Medication</strong> <strong>Error</strong> <strong>Prevention</strong><br />
INSTITUTE FOR SAFE MEDICATION PRACTICES<br />
Huntingdon Valley, Pennsylvania<br />
<strong>Medication</strong> error prevention is an essential<br />
requirement <strong>for</strong> pharmaceutical care and<br />
must be a core mission of every pharmacy.<br />
For medication error prevention to be<br />
effective, it must become a priority. The<br />
first priority <strong>for</strong> successful error reduction is establishing<br />
a multidisciplinary medication-use improvement team<br />
and providing this team with reasonable time and<br />
resources to assess medication safety and to implement<br />
system-level changes that make it difficult or impossible<br />
<strong>for</strong> practitioners to make mistakes that reach the patient.<br />
This multidisciplinary team should accept ownership of<br />
the medication-use process and embrace the opportunity<br />
to improve medication safety.<br />
The goals of the team should include the following:<br />
• Promotion of a nonpunitive approach to reducing<br />
medication errors<br />
• Increased detection and reporting of medication<br />
errors and potentially hazardous drug-use situations<br />
• Exploration and understanding of the root causes of<br />
medication errors<br />
• Education of practitioners about the system-based<br />
causes of errors and their prevention<br />
• Responsiveness to potentially hazardous situations<br />
be<strong>for</strong>e errors occur<br />
• Recommendations to facilitate organization-wide,<br />
system-based changes to prevent medication errors<br />
• Learning from errors occurring in other organizations<br />
through the ISMP <strong>Medication</strong> Safety Alert! and other<br />
published accounts of medication errors, and taking<br />
proactive measures to prevent similar errors.<br />
PHARMACY PRACTICE NEWS SPECIAL EDITION • 2006 9
Table 1. Safety Issues Related to Labeling, Packaging, and Nomenclature<br />
<strong>Medication</strong> Problem Recommendation(s) Technology<br />
Adult and pediatric hepatitis B<br />
vaccines (Merck)<br />
The packaging of the adult and pediatric strengths of Merck’s hepatitis B<br />
vaccines look alike, and the labels do not provide sufficient visual<br />
differentiation, despite different border colors. The resemblance between<br />
the products has led to dispensing errors.<br />
Separate the adult and pediatric strengths in all areas where these<br />
products are stocked.<br />
Consider affixing auxiliary labels to better distinguish the products.<br />
2, 4<br />
ANUSOL (ointments and topical<br />
starch suppositories) product line<br />
ANUSOL (Pfizer) products, used <strong>for</strong> anorectal symptoms, are now called TUCKS.<br />
Tucks has been a registered trademark associated with topical witch hazel<br />
products (pads, topical gel) <strong>for</strong> decades. Using this trademark name is likely<br />
to cause confusion, especially in postpartum settings and outpatient settings<br />
where both product lines are commonly used.<br />
Labeling on Tucks suppository products also is inadequate, with only half of the<br />
6 suppositories in a group labeled with the product name.<br />
Apply auxiliary labels to clearly note the drug name and route of<br />
administration.<br />
Include similar warnings on medication administration records (MARs).<br />
Alert patients to the differences between various Tucks products.<br />
1, 2, 5<br />
Bag and volume do not correlate<br />
Incorrect in<strong>for</strong>mation may be communicated if the total volume of drug and<br />
diluent differs from that stated on the manufacturer’s label.<br />
An infusion of ACTIVASE (alteplase, Genentech), 30 mg/30 mL, was prepared<br />
in an empty 100-mL I.V. container <strong>for</strong> a stroke patient. The pharmacy label<br />
stated “30 mg/30 mL, to be infused over 1 hour,” but the nurse who<br />
administered the drug saw “100 mL” printed by the manufacturer of the<br />
plastic container on the top and assumed that the total volume in the bag<br />
was 100 mL. The pump there<strong>for</strong>e was set at 100 mL/h instead of 30 mL/h and<br />
the drug was infused in about 20 min. Fortunately, the patient was not harmed.<br />
Cover the portion of the manufacturer’s label that indicates the volume<br />
of the container <strong>for</strong> infusions if the preparation differs significantly from<br />
the manufacturer’s label.<br />
Revise procedures to more clearly state the total volume added to the<br />
bag to reduce the potential <strong>for</strong> confusion.<br />
Be sure that all staff involved in administering high-alert drugs (such as<br />
Activase) are familiar with applicable drug dosing and administration<br />
protocols.<br />
2, 3<br />
Confusion between DAPTOMYCIN<br />
and DACTINOMYCIN<br />
Intending to process an order <strong>for</strong> DAPTOMYCIN (Cubicin, Cubist Pharmaceuticals),<br />
a pharmacist typed “DA” into the system, made a selection from a computer<br />
system pick list, and generated an I.V. label. She prepared daptomycin, but<br />
the computer system entered into the profile and printed a label <strong>for</strong><br />
DACTINOMYCIN (Cosmegen, Ovation). The correct drug was administered, but<br />
in subsequent order processing, the wrong drug would have been dispensed<br />
because of the initial incorrect computer entry.<br />
Ensure daily pharmacist review of antibiotic usage and double checking<br />
against the original order.<br />
Include both generic and brand names in computer systems if possible.<br />
Consider use of tall man letters to enhance recognition (DAPtomycin<br />
and DACTINOmycin).<br />
Place name-alert warnings on storage bins and in any computerized<br />
order entry system.<br />
Always verify the patient diagnosis be<strong>for</strong>e dispensing these products.<br />
1, 5<br />
COUMADIN (warfarin sodium,<br />
Bristol-Myers Squibb) and<br />
CARDURA (doxazosin, Pfizer)<br />
A handwritten order <strong>for</strong> CARDURA 1 mg HS was misinterpreted and dispensed<br />
as COUMADIN <strong>for</strong> a patient in a long-term care facility. The patient received<br />
20 doses of Coumadin be<strong>for</strong>e the error was discovered during a hospitalization<br />
<strong>for</strong> uncontrolled hypertension.<br />
Both drugs are available in 1, 2, and 4 mg tablets, and are generally<br />
administered once daily.<br />
The names look similar when poorly handwritten, particularly since both<br />
Cardura and Coumadin begin with “C.”<br />
Encourage prescribers to include the medication’s purpose on all<br />
prescriptions.<br />
Verify a medication’s purpose be<strong>for</strong>e dispensing or administering<br />
medications, especially a high-alert medication such as warfarin.<br />
1, 5<br />
DEPO-SUBQ PROVERA 104<br />
(medroxyprogesterone acetate<br />
injectable suspension, Pfizer)<br />
DEPO-SUBQ PROVERA 104 is a new <strong>for</strong>mulation of the existing DEPO-PROVERA<br />
(medroxyprogesterone acetate suspension) product. It is intended to be given<br />
subcutaneously in a dose of 104 mg every 3 months. However, part of the drug<br />
name could be left off or misaligned when prescriptions are written, leading to<br />
confusion with Depo-Provera and potential administration by the wrong route.<br />
Carefully review any Depo-Provera prescription to assure the correct<br />
<strong>for</strong>mulation, route of administration, indication <strong>for</strong> use, and dosage<br />
frequency.<br />
1, 5<br />
MAALOX (aluminum hydroxidemagnesium<br />
hydroxide-simethicone,<br />
Novartis Consumer)<br />
A new <strong>for</strong>mulation of MAALOX known as Maalox Total Stomach Relief looks<br />
identical to regular Maalox but contains bismuth subsalicylate.<br />
All the products are packaged in white plastic containers that are the same size<br />
and shape; “Maalox” is highlighted on the front label panel of both products,<br />
and a banner on each proclaims, “Great new look. Same great Maalox.”<br />
Warnings are listed on the back label panel, but it is easy to overlook<br />
noteworthy side effects (eg, black stools and/or tongue) and warnings<br />
related to use by children or teens with flu symptoms, patients receiving<br />
oral anticoagulants, and patients allergic to aspirin.<br />
Alert practitioners about brand-name extensions of Maalox, especially<br />
since hospitals will need to purchase the products in look-alike, bulk<br />
bottles because Novartis has discontinued unit-dose containers.<br />
Patients also should be warned about brand-name extensions and told<br />
to check the active ingredients in these products be<strong>for</strong>e they purchase<br />
them, or to ask their community pharmacist <strong>for</strong> help.<br />
1, 5<br />
NOVOLOG MIX 70/30 (70% insulin<br />
aspart protamine suspension, 30%<br />
insulin aspart injection [rDNA origin],<br />
Novo Nordisk), NOVOLOG (insulin<br />
aspart [rDNA origin] injection,<br />
Novo Nordisk), and NOVOLIN 70/30<br />
(70% NPH, human insulin isophane<br />
suspension, 30% regular, human<br />
insulin, Novo Nordisk)<br />
Product selection errors have been reported with mix-ups between NOVOLOG<br />
MIX 70/30 and NOVOLOG.<br />
To help prevent mix-ups, Novo Nordisk implemented new packaging <strong>for</strong><br />
NOVOLOG MIX 70/30. However, the most frequently reported problem with<br />
Novo Nordisk insulin has not been addressed: name confusion between<br />
NOVOLOG MIX 70/30 and NOVOLIN 70/30.<br />
To prevent errors, consider limiting the insulin analog 70/30 mixtures<br />
on the <strong>for</strong>mulary to a single product.<br />
If both Novo Nordisk 70/30 products must be on the <strong>for</strong>mulary, place<br />
reminders about confusion on storage locations.<br />
Accentuate the differences in the products’ names by using tall man<br />
letters (eg, NovoLIN, NovoLOG MIX).<br />
1, 2, 4, 5<br />
OMACOR (omega-3-acid ethyl esters,<br />
Reliant) and AMICAR (aminocaproic<br />
acid, Xanodyne Pharmaceuticals)<br />
OMACOR is a new drug that looks and sounds nearly identical to AMICAR<br />
when handwritten or pronounced.<br />
In one report, a telephone order <strong>for</strong> Omacor was misheard as Amicar and<br />
dispensed to a patient. Fortunately, the patient read the drug in<strong>for</strong>mation sheet,<br />
and called the pharmacy to let the pharmacist know he was expecting a drug<br />
that reduced his triglycerides level.<br />
If both medications are available in your inventory, set an alert in the<br />
computerized order entry system to match the drug’s indication to the<br />
patient’s diagnosis be<strong>for</strong>e dispensing either of these drugs.<br />
1, 5<br />
10 PHARMACY PRACTICE NEWS SPECIAL EDITION • 2006
Table 1. Safety Issues Related to Labeling, Packaging, and Nomenclature (continued)<br />
<strong>Medication</strong> Problem Recommendation(s) Technology<br />
Organ storage solution resembles<br />
I.V. bag<br />
A pharmacist received what looked like a plastic liter bag of I.V. solution with<br />
other products returned <strong>for</strong> credit. On further inspection, the pharmacist realized<br />
the bag actually contained cold storage solution (VIASPAN, NPBI International<br />
BV) used <strong>for</strong> hypothermic flushing and storage of organs during procurement.<br />
The solution likely would be fatal if given intravenously.<br />
Safeguard your processes <strong>for</strong> stocking, storing, and handling organ<br />
storage solution.<br />
2<br />
PHENYTOIN (Baxter) and<br />
PHENOBARBITAL vials (Baxter)<br />
Baxter changed the color of the phenytoin label from dark orange to olive<br />
green to differentiate their heparin (5,000 units/mL, 1 mL fill in 2 mL vial) and<br />
phenytoin (100 mg/2 mL vial). However, this created a new look-alike situation<br />
between PHENYTOIN and PHENOBARBITAL (130 mg/mL, 1 mL fill in 2 mL vial).<br />
Phenytoin and phenobarbital may be used in the same patient population <strong>for</strong><br />
the same indication, status epilepticus.<br />
Until a third label change takes place, warn staff about this risk.<br />
Separate look-alike and sound-alike products.<br />
Affix warning labels to automated dispensing cabinet cells and<br />
place the vials in special plastic bags designed to alert staff to<br />
look-alike medications.<br />
2, 4<br />
SALAGEN (pilocarpine; MGI Pharma)<br />
and SELEGILINE (various)<br />
A home health nurse received a telephone order from a dentist <strong>for</strong> an elderly<br />
patient with dry mouth. He prescribed SALAGEN 5 mg, but the nurse misheard<br />
the order and called the pharmacy to request SELEGILINE 5 mg. About 2 weeks<br />
later, another pharmacist was processing a prescription <strong>for</strong> a fentanyl patch <strong>for</strong><br />
the same patient when the pharmacy computer system signaled an alert about a<br />
drug interaction between fentanyl and selegiline, and the error was recognized.<br />
Both products are available in 5 mg tablets, although selegiline is also available in<br />
5 mg capsule as ELDEPRYL (Somerset).<br />
Prescriptions <strong>for</strong> either of these medications should list both the brand<br />
and generic names and include the indication <strong>for</strong> use with the medication.<br />
Patients should be alerted to the possibility of confusion between these<br />
products.<br />
1, 5<br />
TETANUS TOXOID (Sanofi Pasteur)<br />
and TUBERCULIN PURIFIED PROTEIN<br />
DERIVATIVE (PPD, Sanofi Pasteur)<br />
A nurse came to the pharmacy to pick up a vial of PPD <strong>for</strong> the employee health<br />
clinic. The technician had accidentally retrieved a 5 mL vial of tetanus and<br />
diphtheria vaccine (Td). The nurse did not notice the mistake and administered<br />
PPD tests using the wrong drug to 8 of her co-workers. All developed skin<br />
reactions and some employees had chest X-rays, but none was started on<br />
prophylactic medications. The nurse who administered the tests discovered the<br />
error while investigating the apparent “cluster” of positive readings.<br />
Purchase these products from different manufacturers whenever possible.<br />
Remove tetanus toxoid and PPD from unit stock if feasible, and dispense<br />
from the pharmacy.<br />
Affix warning stickers on storage bins and outer cartons if both products<br />
are available.<br />
2, 4<br />
TOPROL-XL (metoprolol succinate,<br />
AstraZeneca) and TOPAMAX<br />
(topiramate, Ortho-McNeil)<br />
Several mix-ups have occurred between the anticonvulsant TOPAMAX and the<br />
β-blocker TOPROL-XL, resulting in these drugs being dispensed in error.<br />
These products also might be stored near each other if medications are stocked<br />
alphabetically by brand name.<br />
The imprint of the Topamax 25 mg tablet, which lists “TOP” on one side and<br />
“25” on the other, can facilitate a mix-up with Toprol-XL.<br />
Separate the storage of these products.<br />
Use both brand and generic names to provide redundancy.<br />
1, 2, 4, 5<br />
Key<br />
1) Computerized Prescriber Order Entry (CPOE)—A fully<br />
integrated CPOE system that includes the capability to build<br />
medication safety alerts (eg, look-alike names) and clinical decisionmaking<br />
rules. The system also should directly interface with the<br />
laboratory system and pharmacy, list drug-drug and drug-disease<br />
interactions, and offer clinical order screening capability.<br />
2) Bar code–enabled point-of-care (BPOC) systems—Systems<br />
that are designed to prevent medication errors at the point of<br />
medication administration. These systems verify and record all<br />
medications administered to the patient through the use of a bar<br />
code scanner that matches the medication to the patient, by<br />
scanning a bar code on the medication as well as a bar code<br />
on a patient’s wristband.<br />
3) “Smart” infusion pumps—Infusion systems that allow users<br />
to enter various drug infusion protocols into a drug library with<br />
predefined dose limits. If a dose is programmed outside of<br />
established limits or clinical parameters, the pumps halt or<br />
provide an alarm, in<strong>for</strong>ming the clinician that the dose is outside<br />
the recommended range. Some pumps have the capability to<br />
integrate patient monitoring and other patient parameters, such<br />
as age or clinical condition.<br />
4) Automated dispensing cabinets—A robust point-of-use<br />
dispensing system. These cabinets should be integrated with<br />
healthcare facilities’ in<strong>for</strong>mation systems and directly interface<br />
with the pharmacy system. In addition, these systems must<br />
include the ability to use bar coding technology <strong>for</strong> the<br />
restocking process to prevent medication errors.<br />
5) Robust pharmacy order entry system—A pharmacy order<br />
entry system that is fully interfaced with a CPOE system. The<br />
pharmacy system must include the capability to produce<br />
medication safety alerts as well as directly interface with a<br />
healthcare facility’s in<strong>for</strong>mation systems, such as the laboratory<br />
system. In addition, this system must be used to generate a<br />
computerized medication administration record (MAR) <strong>for</strong> use<br />
by the nursing staff when they administer medications.<br />
Effective results depend on understanding the<br />
complex medication-use process as a whole through<br />
varied perspectives and disciplines.<br />
The Institute <strong>for</strong> Safe <strong>Medication</strong> <strong>Practice</strong>s (ISMP)<br />
is a nonprofit organization that works closely with<br />
healthcare practitioners and institutions, regulatory<br />
agencies, professional organizations, and the pharmaceutical<br />
industry to provide education about<br />
medication errors and their prevention.The Institute<br />
provides an independent review of medication<br />
errors that have been voluntarily submitted by practitioners<br />
to the national <strong>Medication</strong> <strong>Error</strong>s Reporting<br />
Program (MERP) operated in the United States by the<br />
United States Pharmacopeia (USP). ISMP is an accessible<br />
resource <strong>for</strong> any pharmacist interested in implementing<br />
the actions recommended herein. Among<br />
the many ISMP products and services, the ISMP<br />
<strong>Medication</strong> Safety Alert! is a biweekly newsletter<br />
that provides timely in<strong>for</strong>mation related to error prevention.<br />
It identifies errors that have been reported<br />
by other organizations and offers recommendations<br />
to prevent those errors from occurring in the pharmacy.<br />
The in<strong>for</strong>mation in Tables 1 to 4 summarizes<br />
many of the significant error-prevention strategies<br />
that were recommended in the ISMP <strong>Medication</strong><br />
Safety Alert! during the last 12 months. The errors<br />
presented in the accompanying tables include actual<br />
or potential errors reported to ISMP. Each table consists<br />
of 4 columns: The first column presents the<br />
medications, devices, or other problematic issues<br />
involved. The second column describes the specific<br />
error or problem involved. The third column discusses<br />
ISMP’s recommendations to proactively<br />
address and prevent errors from occurring. The<br />
fourth column lists technology that may assist in the<br />
prevention of these errors. Technology certainly can<br />
be a powerful tool in the fight against medication<br />
errors but only when it is used appropriately within<br />
a well-designed medication-use system.<br />
The key summarizes the technology addressed<br />
in the tables along with specific criteria that ISMP<br />
believes should be included.<br />
Suggested Readings<br />
Cohen MR, ed. <strong>Medication</strong> <strong>Error</strong>s.Washington, DC:<br />
American Pharmaceutical Association; 1999.<br />
Institute <strong>for</strong> Safe <strong>Medication</strong> <strong>Practice</strong>s Web site:<br />
www.ismp.org.<br />
Institute <strong>for</strong> Safe <strong>Medication</strong> <strong>Practice</strong>s (2005-2006).<br />
ISMP <strong>Medication</strong> Safety Alert! newsletter. Available<br />
at www.ismp.org.<br />
PHARMACY PRACTICE NEWS SPECIAL EDITION • 2006 11
Table 2. Dangerous Abbreviations, Dose Designations, and Other Unsafe Ways of Communicating Orders<br />
Communication Problem Recommendation(s) Technology<br />
Changed directions create problem<br />
Amoxicillin was prescribed as “200 mg/5 mL. Take 5 mL TID.” The prescribed<br />
concentration was not available in the pharmacy, making the original directions<br />
inaccurate. The dispensing pharmacist changed the directions to “Take 4 cc (4/5<br />
teaspoonful).” The patient’s parent’s primary language was not English and the<br />
measuring device was marked in mL and teaspoons, so the parent mistakenly<br />
measured each dose as 4.5 teaspoons. The child was brought to the emergency<br />
department with severe diarrhea.<br />
Do not use “cc” or slash marks (/) as abbreviations.<br />
Provide counseling <strong>for</strong> all new prescriptions, especially if the directions<br />
<strong>for</strong> what is dispensed differ from what was originally prescribed.<br />
5<br />
Coumadin (warfarin sodium,<br />
Bristol-Myers Squibb) order<br />
misinterpreted due to “do not”<br />
symbol<br />
The “do not” symbol was used to indicate that a patient’s Coumadin dose<br />
should not be given, but it was misinterpreted as 4 mg instead. The error was<br />
caught be<strong>for</strong>e the patient received the unneeded 4 mg dose.<br />
Remind practitioners to use clear language rather than symbols when<br />
writing and transcribing orders.<br />
1<br />
Ideas <strong>for</strong> handling “hold” orders<br />
Warfarin was placed on hold be<strong>for</strong>e an endoscopy but was not resumed after<br />
the procedure. The patient suffered a stroke 6 days later.<br />
An order to hold a medication also can result in resuming the medication too<br />
soon.<br />
If a patient is on daily medications based on laboratory results, the<br />
pharmacy profile and the nursing MAR should reflect this as an ongoing<br />
active order with a notation that a dose must be prescribed each day.<br />
If medication doses are not guided by daily laboratory values, hold<br />
orders should not be accepted unless they include specific instructions<br />
<strong>for</strong> when to resume the medications.<br />
All orders <strong>for</strong> medications that are held <strong>for</strong> a procedure should be<br />
rewritten fully after the procedure.<br />
1, 5<br />
Is U really worth it?<br />
An order looked like 90 units of LANTUS (insulin glargine, Aventis) to a<br />
pharmacist, who then noticed that a clarification had already occurred on the<br />
order. However, he thought the nurse had clarified the unusual dose of 90 units<br />
and not the unapproved abbreviation (u), so he misinterpreted the order<br />
clarification as “…dosage 15 units” instead of “…dosage is units,” and<br />
dispensed 15 units. The correct dose was 90 units.<br />
Avoid the use of dangerous abbreviations such as “u” <strong>for</strong> units because<br />
it can lead to unnecessary confusion and the need <strong>for</strong> clarifications.<br />
Anyone who clarifies a medication order should rewrite the entire order.<br />
1, 5<br />
Oral liquid given by I.V.<br />
A long-term care nurse was unfamiliar with oral syringes and administered<br />
TUSSIONEX (hydrocodone and chlorpheniramine, Celltech) suspension, which<br />
was dispensed in an oral syringe, by the I.V. route. The manufacturer-printed<br />
words “For oral use only” had been covered by the pharmacy label.<br />
Never cover important in<strong>for</strong>mation on any drug package. If this is not<br />
possible, auxiliary labels are available with “For oral use only” printed<br />
in large red characters that can be affixed to the syringe plunger.<br />
Educate all staff about oral syringes and how their use can protect<br />
against inadvertent administration by I.V.<br />
2<br />
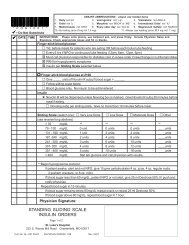
Sliding scale insulin coverage<br />
Sliding scale insulin orders may lead to misinterpretations if they are not clearly<br />
communicated.<br />
In one case, a physician prescribed insulin coverage <strong>for</strong> blood sugar between<br />
0 and 180, potentially leading to the administration of insulin to a patient with<br />
low or normal blood sugar.<br />
Standardize sliding scale insulin coverage and use standard order sets<br />
to clearly communicate orders.<br />
If possible, do not use sliding scale insulin coverage as a routine method<br />
of blood glucose control.<br />
1, 2, 5<br />
SYMLIN (pramlintide acetate,<br />
Amylin Pharmaceuticals)<br />
SYMLIN is dosed in micrograms, but the manufacturer recommends using a<br />
dosing chart and an insulin syringe to measure each dose.<br />
Using an insulin syringe, a patient or practitioner could become confused and<br />
withdraw 30 units, <strong>for</strong> example, <strong>for</strong> a prescribed 30 mcg dose.<br />
Prescribers have expressed the dose in “units” to match the syringe, also<br />
potentially causing confusion.<br />
Patient education and written dosing instructions are vital components<br />
of Symlin therapy.<br />
Patients also should be provided with comprehensive monitoring <strong>for</strong>ms<br />
on which to document all insulin and Symlin doses and corresponding<br />
glucose levels.<br />
1, 5<br />
Units, mg, or mL<br />
Growth hormone can be prescribed in milligrams or international units, causing<br />
confusion.<br />
Patients (or parents) may measure the doses using an insulin syringe, and<br />
describe their growth hormone (somatropin) “doses” in units, when in fact they<br />
are reporting a measurement of volume. When these “unit” doses are converted<br />
to milligrams, the stated doses may appear to be too high and cause confusion.<br />
Educate patients on growth hormones about the risk of confusion<br />
between international units and milligrams, especially if they use an<br />
insulin syringe to measure the dose.<br />
In<strong>for</strong>m patients that they should be familiar with their microgram dose<br />
and should understand that an insulin syringe is only being used to<br />
measure the volume needed <strong>for</strong> the prescribed dose.<br />
If the volumetric dose is large enough, patients should use a tuberculin<br />
syringe instead.<br />
None<br />
12 PHARMACY PRACTICE NEWS SPECIAL EDITION • 2006
Table 3. Problems Involving Drug In<strong>for</strong>mation, Staff Education, and Patient Education<br />
In<strong>for</strong>mation Problem Recommendation(s) Technology<br />
Inadvertent administration of<br />
nimodipine (NIMOTOP, Bayer)<br />
by I.V.<br />
For patients who are unable to swallow and have a nasogastric (NG) tube in<br />
place, doses of NIMOTOP can be prepared by extracting the contents of the<br />
soft gelatin capsule into a syringe with an 18-gauge needle, administering it<br />
via the NG tube, and flushing with 30 mL of saline. However, this procedure<br />
is potentially dangerous, and there have been several reports in which the<br />
drug was drawn into a parenteral syringe and accidentally given by I.V. The<br />
inadvertent I.V. administration of the drug has resulted in severe hypotension,<br />
cardiovascular collapse, and cardiac arrest.<br />
Whenever nimodipine is dispensed, communicate the potential danger<br />
of inadvertent I.V. injection directly to the person responsible <strong>for</strong><br />
administering the drug.<br />
Put a reminder in the computer, on the drug container, and on product<br />
labeling to help trigger this response.<br />
1, 2, 4, 5<br />
Chemical burns with PHENOL (89%)<br />
A 3-year-old child attempted to drink a cup of PHENOL left on the counter of an<br />
examination room in which the child’s mother was being treated. The cup of phenol<br />
spilled down the child’s face and chest, causing immediate pain and irritation.<br />
If possible, supply unit-dose phenol applicator kits (from Apdyne), which<br />
reduce the potential <strong>for</strong> unintended exposure to this harsh chemical.<br />
Limit access to treatment rooms <strong>for</strong> children who are not being treated.<br />
None<br />
CLIMARA (estradiol transdermal<br />
system, Berlex)<br />
The total amount of drug absorbed and the resulting plasma drug concentrations<br />
from transdermal systems can increase during heat exposure.<br />
One patient experienced hot flashes after several days of sun tanning while<br />
wearing CLIMARA (once-a-week estradiol transdermal system). She also noticed<br />
dark spots where her patch had been applied.<br />
It is unknown whether an early release of estrogen from a heated patch<br />
occurred, leading to an abrupt drop in continuous drug delivery, decreased<br />
estrogen blood levels, and the subsequent symptoms.<br />
Educate patients about problems associated with exposing transdermal<br />
systems to excessive heat and the possibility of increased drug<br />
absorption from medication patches.<br />
5<br />
PROPOFOL (various) sedation<br />
Neuromuscular blocking agents<br />
GLACIAL ACETIC ACID<br />
Intestinal per<strong>for</strong>ation after patient<br />
swallows unit-dose packaging<br />
MAGNESIUM SULFATE (various)<br />
toxicity in obstetrics<br />
Using PROPOFOL to sedate patients during endoscopic and other diagnostic<br />
procedures is gaining momentum in a growing number of hospitals, outpatient<br />
surgery centers, and physician offices.<br />
Some practitioners have been lulled into a false sense of security, allowing the<br />
drug’s good safety profile to influence their beliefs that propofol is safer than it<br />
really is.<br />
In untrained hands, propofol can be dangerous, even deadly; administration to a<br />
nonventilated patient by a practitioner who is not trained in the use of drugs<br />
that cause deep sedation and general anesthesia is not safe, even if the drug is<br />
given under the direct supervision of the physician per<strong>for</strong>ming the procedure.<br />
Neuromuscular blocking agents have been inadvertently administered to<br />
patients who were not receiving ventilatory support. Some patients have died or<br />
sustained permanent injuries.<br />
Most incidents have taken place outside operating rooms, emergency departments,<br />
and other critical care areas.<br />
Despite warning statements on GLACIAL ACETIC ACID containers, harmful<br />
mix-ups, where the concentrated <strong>for</strong>m is dispensed instead of a diluted <strong>for</strong>m,<br />
continue to occur.<br />
In one case of dispensing an undiluted <strong>for</strong>m, a nurse called the pharmacy <strong>for</strong><br />
“acetic acid <strong>for</strong> irrigation” <strong>for</strong> a 31-year-old patient with bilateral greater<br />
trochanter wounds. An experienced pharmacist, who was new to the institution,<br />
placed glacial acetic acid at the window <strong>for</strong> pickup. The undiluted solution<br />
resulted in burns to the extent that the wounds would not heal, necessitating<br />
disarticulation at the hips.<br />
Patients have been injured by swallowing plastic unit-dose packaging instead<br />
of removing tablets prior to drug administration.<br />
In one such incident, a man was injured by the sharp corner of a plastic blister<br />
package that cut through all layers of the intestinal wall.<br />
Practitioners who work in obstetrical units may feel com<strong>for</strong>table administering<br />
I.V. MAGNESIUM SULFATE, which is used to treat preterm labor and preeclampsia.<br />
Yet, many errors have been reported with this medication, resulting in overdoses<br />
of magnesium sulfate, and subsequent respiratory arrest and/or death in<br />
patients. Most of the errors were due to unfamiliarity with safe dosage ranges<br />
and signs of toxicity, inadequate patient monitoring, pump programming errors,<br />
and mix-ups between magnesium sulfate and oxytocin.<br />
Within your organization, have an interdisciplinary team, including<br />
the chair of the anesthesia department, establish policies and practice<br />
guidelines <strong>for</strong> the administration of propofol to nonventilated patients<br />
undergoing surgical or diagnostic procedures.<br />
Allow floor stock of these agents only in the operating room, emergency<br />
department, and critical care units.<br />
Sequester in both refrigerated and nonrefrigerated locations.<br />
Affix fluorescent red warning labels on products that note: “Warning:<br />
Paralyzing Agent—Causes Respiratory Arrest.”<br />
Remove glacial acetic acid from stock.<br />
Purchase diluted acetic acid from external sources. If this is not possible,<br />
dilute the product in the concentrations needed immediately upon<br />
delivery of the chemical.<br />
Place more prominent alert messages on storage shelves and bottles.<br />
Require an order <strong>for</strong> acetic acid that includes the exact strength necessary.<br />
Educate all staff about the properties of glacial acetic acid.<br />
Always provide patient education on proper drug administration if<br />
patients are administering medications to themselves.<br />
Confused, somnolent, or visually impaired patients should never be<br />
handed wrapped packages of medications.<br />
Consider the use of a standard concentration of commercially available<br />
premixed solutions <strong>for</strong> bolus doses and maintenance infusions.<br />
Label the I.V. tubing near the I.V. pump, and establish dosing and administration<br />
protocols and standard order sets <strong>for</strong> magnesium sulfate; independently<br />
double-check the drug, concentration, infusion rate, pump settings,<br />
line attachment, and patient be<strong>for</strong>e administering I.V. magnesium sulfate.<br />
Frequently monitor patients’ vital signs, oxygen saturation, deep tendon<br />
reflexes, and level of consciousness (also fetal heart rates and maternal<br />
uterine activity if the drug is used <strong>for</strong> preterm labor).<br />
1, 3, 5<br />
1, 2, 4, 5<br />
2<br />
None<br />
1, 2, 3, 4, 5<br />
New FENTANYL (various) warnings;<br />
more needed to protect patients<br />
Some patients and their healthcare providers may not be fully aware of the<br />
dangers of FENTANYL products and the important recommendations regarding<br />
the safe use of this potent narcotic agent.<br />
In one incident, a woman, who had chronic pain from Crohn’s disease, reported<br />
that her 4-year-old son either used a discarded patch retrieved from the trash or<br />
opened a wrapper of a patch from a box of stored patches, and applied one to<br />
his body. His mother found him dead on the floor of a bedroom, near an<br />
overturned trash can that held torn wrappers and discarded patches.<br />
Thoroughly review the recent alert from Janssen. (www.fda.gov/medwatch/SAFETY/2005/duragesic_ddl.pdf)<br />
as well as the July 15, 2005,<br />
FDA Public Health Advisory about changes to product labeling.<br />
Select patients appropriate <strong>for</strong> this therapy, educate patients, and take<br />
steps to ensure safe use and disposal of the products.<br />
Improve the methods of documentation to help guard against applying<br />
multiple patches to patients.<br />
1, 2, 4, 5<br />
PHYTONADIONE (Vitamin K 1 ) as<br />
pharmacy trigger<br />
PHYTONADIONE has been prescribed as an aggressive attempt to reverse the<br />
effects of warfarin in preparation <strong>for</strong> a procedure.<br />
The long-term effects of phytonadione administration may last up to a week,<br />
causing prescribers to later inappropriately increase warfarin doses over several<br />
days. The resulting warfarin dose may be dangerously high.<br />
Investigate all orders <strong>for</strong> phytonadione 10 mg or higher.<br />
Determine the circumstances of an adverse drug event from unintentional<br />
bleeding due to warfarin or of intentional pre-procedure reversal of<br />
warfarin.<br />
If intentional, recommend a lower post-procedure warfarin dose once<br />
restarted.<br />
Considering how many hospital pharmacy computer systems are today,<br />
pharmacists should not consistently depend on this technology to detect<br />
potentially harmful medication errors.<br />
Test your organization’s computer system and identify weaknesses that<br />
can be targeted to improve and safeguard against medication errors.<br />
Contact vendors <strong>for</strong> pharmacy software and drug in<strong>for</strong>mation providers<br />
to request any necessary changes.<br />
1, 5<br />
Safety still compromised by<br />
computer weaknesses<br />
An ISMP survey showed alarming findings that pharmacy computer systems in<br />
this country are vastly unreliable when used to detect and correct prescription<br />
errors or pharmacy order entry errors. These findings indicate that there has<br />
been little improvement with pharmacy computer systems over the past 6 years<br />
to safeguard against medication errors.<br />
5<br />
PHARMACY PRACTICE NEWS SPECIAL EDITION • 2006 13
Table 4. Medical Devices and Other Discussion Items<br />
Title Problem/Discussion Point Recommendation(s) Technology<br />
An exhausted work<strong>for</strong>ce increases<br />
the risk of errors<br />
Long work hours and the fatigue that results represent a serious threat to<br />
patient safety. Among its many effects, fatigue diminishes the ability to<br />
recognize important but subtle changes in a patient’s health and reduces<br />
the ability to deal with unexpected events. In fact, prolonged wakefulness<br />
leaves a person with the equivalent of a blood alcohol concentration of 0.1%<br />
(above the legal driving limit).<br />
Provide managers with in<strong>for</strong>mation about the risks of fatigue, circadian<br />
rhythm disturbances, and approaches to optimize per<strong>for</strong>mance.<br />
Set limitations on the hours worked each day and week, and <strong>for</strong> specific,<br />
potentially fatiguing physical and mental tasks.<br />
Whenever possible, recognize the circadian rhythm principles when<br />
designing work schedules.<br />
Planned breaks and naps, light therapy, and access to nutritious meals<br />
also can help to combat the effects of fatigue.<br />
None<br />
Apologies gain momentum<br />
A decade ago, physicians were told, implicitly or explicitly, during their<br />
professional training to avoid making apologies to patients <strong>for</strong> medical errors<br />
because this could lead to problems if they are sued. Today, some healthcare<br />
executives, insurers, and physicians are changing this mindset and are fully<br />
embracing disclosure and apologies, not only because they believe this will<br />
reduce malpractice claims but also because ethically this is the right thing to do.<br />
Consider developing a disclosure policy that establishes detailed<br />
procedures <strong>for</strong> physicians to acknowledge medical errors and, if<br />
possible, offers fair compensation <strong>for</strong> expenses related to the medical<br />
injuries.<br />
None<br />
False glucose results with<br />
point-of-care testing<br />
Administration of certain substances can result in erroneously high values when<br />
monitoring blood glucose with certain point-of-care glucose meters.<br />
In one case, the I.V. administration of an immunoglobulin product <strong>for</strong>mulated<br />
with maltose led to falsely elevated glucose meter results and the inappropriate<br />
escalation of a patient’s insulin dose.<br />
Similar problems have been reported with other products <strong>for</strong>mulated with<br />
maltose or icodextrin.<br />
Create special alerts in the pharmacy computer system to remind pharmacists<br />
about the potential <strong>for</strong> false glucose readings when entering<br />
orders <strong>for</strong> products that may affect the accuracy of the glucose monitors.<br />
Communicate the in<strong>for</strong>mation to the nursing staff and add a cautionary<br />
note to the MAR under the drug entry <strong>for</strong> insulin.<br />
Include the risk of false glucose determinations, and the specific<br />
circumstances surrounding this risk, in protocols <strong>for</strong> insulin administration<br />
according to glucose values.<br />
Remind staff to “treat the patient, not the glucose meter,” and always<br />
correlate the patient’s symptoms with the glucose meter reading be<strong>for</strong>e<br />
insulin administration, especially in cases in which the glucose readings<br />
are very high or very low.<br />
1, 2, 5<br />
Filtered pump sets and epoprostenol<br />
(FLOLAN, GlaxoSmithKline)<br />
interruption<br />
Administration set tubing that connects to the pump’s drug cassette at one end<br />
and the patient’s I.V. line at the other has a filter in line that allows one-way<br />
flow through the filter. Mistakenly connecting the wrong end of the tubing to<br />
the infusion pump may interrupt the flow of FLOLAN and cause severe<br />
worsening of pulmonary hypertension and even death in minutes.<br />
Properly identify the distal and proximal ends of the administration set<br />
be<strong>for</strong>e connecting.<br />
Labeling the end of the tubing with the filter with a sticker “filter end to<br />
patient” may serve as a reminder to the nursing staff.<br />
None<br />
Inhaler dust caps protect from more<br />
than dust<br />
A patient had to have a dime removed from his trachea after using his albuterol<br />
inhaler, which he had kept in his pocket without a dust cap on it.<br />
When educating patients on proper inhaler use, be sure to remind them<br />
to keep the dust cap in place when the inhaler is not in use.<br />
None<br />
Medtronic SYNCHROMED pump<br />
fatal injection<br />
An inadvertent intraspinal injection occurred due to a mix-up of access kits<br />
and inadequate labeling on the templates. The patient received nearly 1 g of<br />
morphine (18 mL of a 50 mg/mL solution) through the catheter access port of an<br />
implanted Medtronic SYNCHROMED pump instead of through the drug reservoir.<br />
Overlay templates currently supplied with each kit (refill and catheter access)<br />
do not display any text indicating which template is in use; nor do they display<br />
warnings against accidental injection into the wrong port.<br />
Until changes are made to the kits and templates, verify credentials and<br />
competencies <strong>for</strong> any staff who stock and/or dispense the kits or refill<br />
the devices.<br />
Segregate the catheter access kits in storage areas and add auxiliary<br />
warning labels to them.<br />
1, 5<br />
Monitoring alarms mistakenly<br />
interpreted as a technical problem<br />
leading to neonatal death<br />
Patient tampering with opioid<br />
infusion pumps<br />
A neonate was given arterial solution that was compounded with concentrated<br />
sodium chloride (23.4%) instead of sterile water. When the nurses began to<br />
experience what they perceived to be technical problems with the inline<br />
monitor, the monitor was replaced. When this replacement monitor seemed<br />
to be faulty, it also was replaced. Approximately 18 hours later, the monitor<br />
displayed a sodium level of more than 190 mmol/L. The patient deteriorated<br />
and required several interventions, but there was no change in serum sodium<br />
level, and the baby died.<br />
A patient with a history of chronic pain was admitted to the hospital and<br />
permitted to use the opioid-infusing pump he had brought from home. It<br />
was discovered that the patient had been able to alter pump settings with<br />
knowledge of lock level and clinician bolus codes.<br />
Never assume that equipment malfunction is the sole cause <strong>for</strong> what<br />
appears to be an abnormal clinical value; this can delay rescue from harm.<br />
Never completely cover the manufacturer’s label with the patient label<br />
because this prohibits an independent double check by nursing personnel.<br />
Use only hospital-approved pumps to administer opioids to hospitalized<br />
patients.<br />
Monitor prescribed doses against doses dispensed and administered.<br />
Educate staff to shield pump programming codes and actions from<br />
non-clinicians.<br />
Consider having biomedical engineering change codes temporarily as<br />
long as the new codes can be securely communicated to those who<br />
need the in<strong>for</strong>mation.<br />
None<br />
3<br />
V.A.C. INSTILL SYSTEM (Kinetic<br />
Concepts, Inc.) may pose a risk<br />
<strong>for</strong> I.V. misconnections<br />
The V.A.C. INSTILL SYSTEM by KCI is a wound healing system that facilitates<br />
automated delivery of topical solutions to wound sites. While very different from<br />
an infusion pump, the device is programmed to deliver a desired rate of infusion;<br />
however, it lacks protection from gravity free-flow if the tubing is removed. The<br />
device is designed to accommodate I.V. tubing to deliver the topical solution,<br />
and one could inadvertently attach the I.V. tubing intended <strong>for</strong> the V.A.C. to an<br />
I.V. port.<br />
Prepare topical solutions in a container dissimilar to typical I.V. solutions,<br />
such as a 500-mL bottle.<br />
Misconnections also are less likely if you label all lines; affix bold<br />
cautionary labels to topical solutions, and physically trace all lines from<br />
the source solution to the port of insertion.<br />
None<br />
14 PHARMACY PRACTICE NEWS SPECIAL EDITION • 2006