Stroke Order Set 2 - Pharmacy Practice News
Stroke Order Set 2 - Pharmacy Practice News Stroke Order Set 2 - Pharmacy Practice News
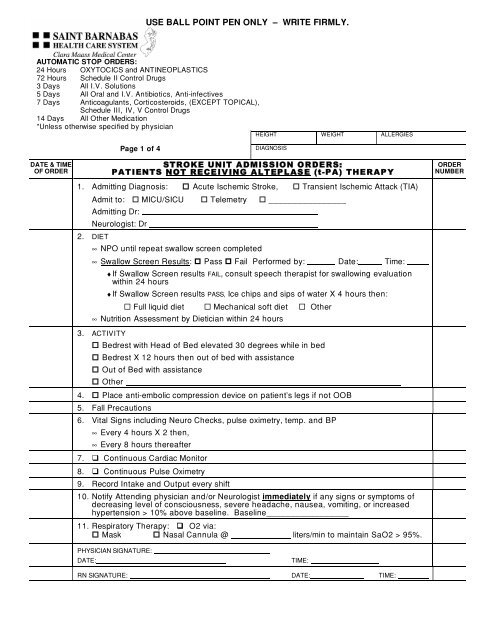
USE BALL POINT PEN ONLY – WRITE FIRMLY. AUTOMATIC STOP ORDERS: 24 Hours OXYTOCICS and ANTINEOPLASTICS 72 Hours Schedule II Control Drugs 3 Days All I.V. Solutions 5 Days All Oral and I.V. Antibiotics, Anti-infectives 7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL), Schedule III, IV, V Control Drugs 14 Days All Other Medication *Unless otherwise specified by physician HEIGHT WEIGHT ALLERGIES Page 1 of 4 DIAGNOSIS DATE & TIME OF ORDER STROKE UNIT ADMISSION ORDE RS: PATIENTS NOT RECE IVING ALTEP L AS E (t-PA) THERAP Y 1. Admitting Diagnosis: Acute Ischemic Stroke, Transient Ischemic Attack (TIA) Admit to: MICU/SICU Telemetry ________________ Admitting Dr: Neurologist: Dr 2. DIET ∞ NPO until repeat swallow screen completed ∞ Swallow Screen Results: Pass Fail Performed by: Date: Time: ♦ If Swallow Screen results FAIL, consult speech therapist for swallowing evaluation within 24 hours ♦ If Swallow Screen results PASS, Ice chips and sips of water X 4 hours then: Full liquid diet Mechanical soft diet Other ∞ Nutrition Assessment by Dietician within 24 hours 3. ACTIVITY Bedrest with Head of Bed elevated 30 degrees while in bed Bedrest X 12 hours then out of bed with assistance Out of Bed with assistance Other 4. Place anti-embolic compression device on patient’s legs if not OOB 5. Fall Precautions 6. Vital Signs including Neuro Checks, pulse oximetry, temp. and BP ∞ Every 4 hours X 2 then, ∞ Every 8 hours thereafter 7. Continuous Cardiac Monitor 8. Continuous Pulse Oximetry 9. Record Intake and Output every shift 10. Notify Attending physician and/or Neurologist immediately if any signs or symptoms of decreasing level of consciousness, severe headache, nausea, vomiting, or increased hypertension > 10% above baseline. Baseline_________________ 11. Respiratory Therapy: O2 via: Mask Nasal Cannula @ liters/min to maintain SaO2 > 95%. ORDER NUMBER PHYSICIAN SIGNATURE: DATE: TIME: RN SIGNATURE: DATE: TIME:
- Page 2 and 3: USE BALL POINT PEN ONLY - WRITE FIR
- Page 4: USE BALL POINT PEN ONLY - WRITE FIR
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 1 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
STROKE UNIT ADMISSION ORDE RS:<br />
PATIENTS NOT RECE IVING ALTEP L AS E (t-PA) THERAP Y<br />
1. Admitting Diagnosis: Acute Ischemic <strong>Stroke</strong>, Transient Ischemic Attack (TIA)<br />
Admit to: MICU/SICU Telemetry ________________<br />
Admitting Dr:<br />
Neurologist: Dr<br />
2. DIET<br />
∞ NPO until repeat swallow screen completed<br />
∞ Swallow Screen Results: Pass Fail Performed by: Date: Time:<br />
♦ If Swallow Screen results FAIL, consult speech therapist for swallowing evaluation<br />
within 24 hours<br />
♦ If Swallow Screen results PASS, Ice chips and sips of water X 4 hours then:<br />
Full liquid diet Mechanical soft diet Other<br />
∞ Nutrition Assessment by Dietician within 24 hours<br />
3. ACTIVITY<br />
Bedrest with Head of Bed elevated 30 degrees while in bed<br />
Bedrest X 12 hours then out of bed with assistance<br />
Out of Bed with assistance<br />
Other<br />
4. Place anti-embolic compression device on patient’s legs if not OOB<br />
5. Fall Precautions<br />
6. Vital Signs including Neuro Checks, pulse oximetry, temp. and BP<br />
∞ Every 4 hours X 2 then,<br />
∞ Every 8 hours thereafter<br />
7. Continuous Cardiac Monitor<br />
8. Continuous Pulse Oximetry<br />
9. Record Intake and Output every shift<br />
10. Notify Attending physician and/or Neurologist immediately if any signs or symptoms of<br />
decreasing level of consciousness, severe headache, nausea, vomiting, or increased<br />
hypertension > 10% above baseline. Baseline_________________<br />
11. Respiratory Therapy: O2 via:<br />
Mask Nasal Cannula @ liters/min to maintain SaO2 > 95%.<br />
ORDER<br />
NUMBER<br />
PHYSICIAN SIGNATURE:<br />
DATE:<br />
TIME:<br />
RN SIGNATURE: DATE: TIME:
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 2 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
STROKE UNIT ADMISSION ORDE RS:<br />
PATIENTS NOT RECE IVING ALTEP L AS E (t-PA) THERAP Y<br />
12. Medications: REMINDER: If swallow screen failed - no PO medications until evaluation by<br />
speech pathologist is completed.<br />
IV line # 1 - IV: Solution Volume Rate<br />
IV line # 2 - Saline lock; flush with 2 ml of Normal Saline every shift.<br />
Hypertension Management – Please see Page 4<br />
GI PROPHYLAXIS/BOWEL REGIMEN<br />
Pantoprazole (Protonix) 40mg by mouth once daily OR<br />
Pantoprazole (Protonix) 40mg IV once daily if patient is NPO OR<br />
Prevacid 30 mg NGT once daily<br />
Docusate (Colace) 100mg by mouth twice daily.<br />
Bisacodyl (Dulcolax) 10mg suppository per rectum once daily as needed for bowel movement.<br />
ANTITHROMBOTIC/DVT PROPHYLAXIS/ATRIAL FIBRILLATION MANAGEMENT (please specify).<br />
Aspirin 81 mg by mouth now and daily Indication: Antithrombotic DVT Proph<br />
Aspirin 325mg by mouth now and daily. Indication: Antithrombotic DVT Proph<br />
Aspirin 25mg/Dipyridamole 200mg (Aggrenox) by mouth BID Indication: Antithrombotic DVT<br />
Proph<br />
Enoxaparin (Lovenox) 40mg subcutaneously daily. Indication: Antithrombotic DVT Proph A-fib<br />
Warfarin (Coumadin) mg PO Indication: Antithrombotic DVT Proph A-fib<br />
Heparin<br />
PT/INR daily<br />
Indication: Antithrombotic DVT Proph A-fib<br />
PAIN MANAGEMENT / ANTIPYRETIC<br />
Acetaminophen (Tylenol) 650mg by mouth every 4 hours as needed for mild pain or temperature ><br />
99.6°<br />
Other:<br />
Notify physician if temperature > 101°<br />
Glucose Monitoring (fingerstick) every<br />
Glucose Management (please specify)<br />
hours.<br />
ORDER<br />
NUMBER<br />
Hyperlipidemia Management (please specify)<br />
PHYSICIAN SIGNATURE:<br />
DATE:<br />
TIME:<br />
RN SIGNATURE: DATE: TIME:
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 3 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
Other Medications:<br />
<br />
<br />
<br />
<br />
<br />
STROKE UNIT ADMISSION ORDERS -<br />
PATIENTS NOT RECEIVING ALTEPLASE (t-PA) THERAPY<br />
13. Rehabilitation Medicine Consults: (to be completed within 24 hours of admission)<br />
Physiatrist Evaluation and Treatment<br />
P.T. Evaluation and Treatment. Extension 42050<br />
Occupational Therapy Evaluation. Extension 42382<br />
14. Case Management referral and discharge planning evaluation. Extension 42280<br />
15. Clinical Laboratory Testing: Indication: Acute Ischemic <strong>Stroke</strong><br />
CBC with automated differential (if not done in ED)<br />
Lipid profile (if not done in ED)<br />
BMP (if not done in Emergency Department)<br />
B12, Folate, RPR<br />
Homocysteine level<br />
16. Additional Diagnostic Tests<br />
Carotid Ultrasound<br />
2-D Cardiac Echo<br />
<br />
<br />
<br />
<br />
Other Labs:<br />
Indication: Acute Ischemic <strong>Stroke</strong><br />
Indication: Acute Ischemic <strong>Stroke</strong><br />
Chest X ray, PA/Lateral; if not done in ED Indication: Acute Ischemic <strong>Stroke</strong><br />
MRI Brain with diffusion weighted imaging/<br />
without contrast<br />
Indication:<br />
MRA<br />
Other diagnostic tests:<br />
17. OTHER ORDERS:<br />
Indication:<br />
ORDER<br />
NUMBER<br />
PHYSICIAN SIGNATURE: ______________________________________<br />
DATE: ____________________________________ TIME: _____________________________<br />
RN SIGNATURE: __________________________ DATE: TIME: ________
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 4 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
STROKE UNIT ADMISSION ORDERS -<br />
PATIENTS NOT RECEIVING ALTEPLASE (t-PA) THERAPY<br />
Blood Pressure Management: Non-rtPA Patients<br />
Goal BP Management = 15% Reduction In BP from baseline<br />
If Systolic BP is 180 mm Hg or Diastolic BP 100 mm Hg, do not treat BP unless other<br />
end organ failure e.g., aortic dissection, acute MI, pulmonary edema, hypertensive<br />
encephalopathy is present.<br />
Systolic BP >180 mm Hg OR diastolic BP 100 mm Hg<br />
Labetalol 10 mg IV over 1-2 minutes. (Note: Labetalol may be repeated every 10-20 minutes to<br />
maximum dose of 300 mg)<br />
If BP systolic >180 mg Hg or diastolic >100 mm Hg within 10 minutes of initial dose, notify physician<br />
and<br />
Repeat Labetalol 10 mg IV over 1-2 minutes.<br />
Labetalol Infusion<br />
start.<br />
OR<br />
Labetolol 10 mg IV over 1-2 minutes bolus then start Labetalol infusion at 2-8 mg/minute<br />
Infusion: Labetalol 200 mg in 160 ml normal saline (concentration =1 mg/1ml)<br />
Notify physician if BP systolic >180 mg Hg or diastolic >100 mm Hg 15 minutes after infusion<br />
Nitropaste 1 inch to chest wall. Notify physician If BP systolic >180 mg Hg or<br />
diastolic >100 mm Hg within 10 minutes, OR<br />
Nitropaste 2 inches to chest wall. Notify physician If BP systolic >180 mg Hg or<br />
diastolic >100 mm Hg within 10 minutes, OR<br />
Nicardipine infusion 25 mg in 250 ml at 5 mg/hour, titrate up by 2.5 mg/hour<br />
at 5-15 minute intervals to maximum dose of 15 mg/hour. Reduce to 3 mg/hour when<br />
BP