Activated Partial Thromboplastin Time - Pathology
Activated Partial Thromboplastin Time - Pathology
Activated Partial Thromboplastin Time - Pathology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Activated</strong> <strong>Partial</strong> <strong>Thromboplastin</strong> <strong>Time</strong> 1<br />
<strong>Activated</strong> <strong>Partial</strong><br />
<strong>Thromboplastin</strong> <strong>Time</strong><br />
Roger S. Riley, M.D., Ph.D.<br />
April, 2005<br />
Feature<br />
Synonyms<br />
aPTT, APTT.<br />
Test Description<br />
The aPTT is functional determination of the intrinsic pathway of coagulation (factors<br />
XII, XI, IX, VIII, V, II, I, prekallikrein, high molecular weight kininogen). This pathway<br />
is intitated by the interaction of Factor XII with a negatively charged surface. A cascade<br />
mechanism results in fibrin production and clot formation. The aPTT is utilized to<br />
detect congenital and qcquired abnormalities of the intrinsic coagulation pathway and<br />
to monitor patients receiving heparin.<br />
Patient<br />
Preparation<br />
No specific patient preparation is required. However, since lipemia may interfere with<br />
photo-electric measurements of clot formation, specimens should not be obtained after<br />
a meal. In patients receiving intermittent heparin injections, peripheral blood for<br />
aPTT analysis should be obtained one hour before the next dose of heparin is scheduled.<br />
The specimen should not be drawn from an arm with a heparinized catheter or<br />
heparin lock.<br />
Specimen<br />
Citrated, platelet-poor plasma is used for the aPTT.<br />
Specimen<br />
Collection<br />
and<br />
Preparation<br />
Specimen requirements for coagulation assays are described in NCCLS H21-A3 (Collection,<br />
Transport, and Processing of Blood Specimens for Coagulation Assays; Approved<br />
Guideline - Third Edition, December, 1998). These requirements are summarized<br />
below.<br />
Citrated, platelet-poor plasma is prepared from peripheral venous blood collected by<br />
clean, nontraumatic venipuncture directly into a plastic or siliconized glass tube containing<br />
109 nM (3.2%) trisodium citrate at a ratio of 9:1. With a blood collection set,<br />
the tube for coagulation analysis automatically fills to the correct volume. The tube<br />
should be immediately inverted at least four time after filling. A needle with a gauge<br />
of 22 to 19 should be utilized in adult patients, while a 21 to 23 gauge needle is suitable<br />
in pediatric patients. A traumatic venipuncture can activate coagulation factors,<br />
leading to a shortened aPTT. In patients receiving heparin, extreme care must be<br />
taken to avoid release of platelet factor 4 (PF4), which is a potent heparin inhibitor.<br />
Syringe draws - Blood obtained from a syringe draw is not preferred for aPTT analysis<br />
due to safety issues and the increased chance of specimen hemolysis or clotting. If a<br />
syringe must be used for aPTT specimen collection, a small volume syringe (< 20<br />
mL) is recommended. The double syringe technique is recommended, with the second<br />
tube used for coagulation alalysis. The blood must be transferred from the syringe<br />
to a plastic or siliconized glass tube tube containing the proper amount of anticoagulant<br />
within one minute after collection.<br />
Indwelling catheters - Blood dilution and contamination with heparin are risks when<br />
blood specimens collected from an indwelling catheter are utilized for the aPTT. If<br />
such a specimen must be used, the line should first be flushed with saline, and the<br />
first 5 mL or six dead space volumes of the catheter drawn and discarded. Care must<br />
also be taken free the catheter and blood collection system from air leaks.
<strong>Activated</strong> <strong>Partial</strong> <strong>Thromboplastin</strong> <strong>Time</strong> 2<br />
Specimen<br />
Collection and<br />
Preparation<br />
(Cont’D)<br />
Multiple specimens - If multiple blood specimens are obtained, the aPTT should<br />
be performed on the second or third tube. If the blood is being obtained only<br />
for coagulation testing, the first tube should be drawn and discarded, and the<br />
second tube submitted to the laboratory.<br />
Specimen preparation - Platelet-poor plasma (platelet count < 10 x 10 9 /L) is prepared<br />
from the whole blood specimen by centrifuging the capped specimen tube at<br />
an appropriate speed for an appropriate time. Centrifugation at 1500 g for 15 minutes<br />
at room temperature is recommended for this purpose. A centrifuge with a<br />
swing-out bucket rotor should be used to avoid remixing of platelets and plasma during<br />
plasma removal.<br />
Specimen storage -<br />
Unheparinized specimens - Specimens for aPTT analysis from unheparinized<br />
patients should be maintained centrifuged or uncentrifuged with plasma remaining<br />
on top of the cells in an unopened tube maintained at 2-4 o C or 18-<br />
24 o C and tested within four hours of specimen collection.<br />
Heparinized specimens - Specimens suspected of containing heparin should<br />
be centrifuged within one hour of collection and the plasma analyzed within<br />
four hours of collection. Plasma should be separated and removed within one<br />
hour if the specimen is being transported to a remote location for analysis or<br />
otherwise agitated.<br />
Frozen plasma - Plasma should be separated from specimens which cannot be<br />
analyzed within four hours and frozen at -20 o C for up to two weeks or at<br />
-70 o C for up to six months in a frost-free freezer. Frozen plasma specimens<br />
should be rapidly thawed at 37 o C, gently mixed, and analyzed immediately or<br />
stored at 4 o C for a maximum of two hours prior to analysis.<br />
Causes for Specimen Rejection - The aPTT cannot be performed on speciments that<br />
are clotted, visibly hemolyzed, collected into the wrong anticoagulant, collected into<br />
an improper quantity of anticoagulant, not labeled, or improperly labeled.<br />
Test<br />
Methodology<br />
The aPTT is usually performed by automated testing in the batch or stat mode. In<br />
the aPTT an aliquot of undiluted, platelet-poor plasma is incubated at 37 o C with a<br />
particulate factor XII activator (i.e., silica, celite, kaolin, micronized silica, ellagic<br />
acid, etc.). A reagent containing phospholipid (partial thromboplastin) is added, followed<br />
by CaCl2. The time required for clot formation is measured by one of a variety<br />
of techniques (photo-optical, electromechanical, etc.). The aPTT result is reported as<br />
the time required for clot formation after the addition of CaCl2.<br />
Many different phosophlipid reagents animal and plant origin, such as cephalin, have<br />
been used as partial thromboplastins, and a variety of activating substances are in<br />
use. The sensitivity of the assay to factor deficiencies, inhibitors, and heparin varies<br />
with the reagents used in the assay.<br />
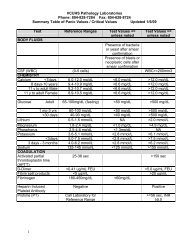
Normal Values and<br />
Critical Limits<br />
Interferences<br />
24 - 37 sec (Jordan, C.D. et al., Normal reference laboratory values. N. Engl. J. Med.<br />
327:718-724, 1992). Statistically, the aPTT is slightly lengthened in young individuals<br />
and slightly shortened in older populations. Premature infants have prolonged<br />
aPTT values which return to normal by 6 months of age. However, age-specific normal<br />
ranges are not utilized in patient care at this time.<br />
Lipemia and hyperbilirubinemia interfere with the detection of clot formation by<br />
photo-optical methods. The results of the aPTT may be affected by a wide variety of<br />
factors, including the manner of blood coagulation, the type of container, the type of<br />
anticoagulant, specimen transport and storage conditions, incubation time and temperature,<br />
assay reagents, and the method of end point detection.
<strong>Activated</strong> <strong>Partial</strong> <strong>Thromboplastin</strong> <strong>Time</strong> 3<br />
Clinical Utilization<br />
The PT and aPTT are the fundamental assays of the coagulation system. The principal<br />
clinical uses of the aPTT include: (1) the detection of hereditary or acquired deficiencies<br />
or defects of the intrinsic and common pathway coagulation factors (factors<br />
XII, XI, IX, VIII, prekallikrein, high molecular weight kininogen), (2) monitoring<br />
heparin anticoagulant therapy, (3) the detection of coagulation inhibitors (i.e., lupus<br />
anticoagulant), and (4) to monitor coagulation factor replacement therapy in patients<br />
with hemophilia.<br />
The aPTT is increased above the upper limit of normal with hereditary or acquired<br />
intrinsic factor deficiencies < 40% (factor VIII:C, Factor IX, Factor XI, Factor XII,<br />
vWf), lupus anticoagulants, or specific inhibitors of the intrinsic coagulation factors.<br />
Other causes of an elevated aPTT include liver disease, disseminated intravascular<br />
coagulation (DIC), heparin or anticoagulant therapy, or improper specimen collection<br />
(i.e., traumatic phlebetomy or hemolyzed specimen).<br />
References<br />
Asaf T, Reuveni H, Yermiahu T, et<br />
al: The need for routine preoperative<br />
coagulation screening<br />
tests (prothrombin time PT/partial<br />
thromboplastin time PTT) for<br />
healthy children undergoing elective<br />
tonsillectomy and/or adenoidectomy.<br />
Int J Pediatr Otorhinolaryngol<br />
61:217-222, 2001<br />
Bajaj SP, Joist JH: New insights<br />
into how blood clots: implications<br />
for the use of APTT and PT as<br />
coagulation screening tests and in<br />
monitoring of anticoagulant therapy.<br />
Semin Thromb Hemost<br />
25:407-418, 1999<br />
Bamberg R, Cottle JN, Williams<br />
JC: Effect of drawing a discard<br />
tube on PT and APTT results in<br />
healthy adults. Clin Lab Sci<br />
16:16-19, 2003<br />
Chen CC, You JY, Ho CH: The<br />
aPTT assay as a monitor of heparin<br />
anticoagulation efficacy in clinical<br />
settings. Adv Ther 20:231-236,<br />
2003<br />
Dahlback B: The multiple faces of<br />
the partial thromboplastin time<br />
APTT. J Thromb Haemost<br />
2:2256-2257, 2004<br />
Hirsh J, Bates S: The multiple<br />
faces of the partial thromboplastin<br />
time APTT. J Thromb Haemost<br />
2:2254-2256, 2004<br />
Liepman CI, Koerber JM, Mattson<br />
JC, et al: Comparing methods of<br />
establishing the aPTT therapeutic<br />
range of heparin. Ann Pharmacother<br />
37:794-798, 2003<br />
rationale of measuring APTT in<br />
risk assessment. Haematologica<br />
86:328, 2001<br />
Olson JD: Addressing clinical etiologies<br />
of a prolonged aPTT. CAP<br />
Today 13:28, 30, 32 passim, 1999<br />
Palkuti HS: Selecting an APTT<br />
reagent. MLO Med Lab Obs<br />
32:14-16, 2000<br />
Poller L: The multiple faces of the<br />
partial thromboplastin time APTT.<br />
J Thromb Haemost 2:2258-2259,<br />
2004<br />
Shetty S, Ghosh K, Mohanty D:<br />
Comparison of four commercially<br />
available activated partial thromboplastin<br />
time reagents using a<br />
semi-automated coagulometer.<br />
Blood Coagul Fibrinolysis<br />
14:493-497, 2003<br />
Siegel JE, Bernard DW, Swami<br />
VK, et al: Monitoring heparin therapy:<br />
APTT results from partial- vs<br />
full-draw tubes. Am J Clin Pathol<br />
110:184-187, 1998<br />
Smythe MA, Koerber JM, Westley<br />
SJ, et al: Use of the activated partial<br />
thromboplastin time for heparin<br />
monitoring. Am J Clin Pathol<br />
115:148-155, 2001<br />
ten Boekel E, de Kieviet W, Bartels<br />
PC: Subjects with a shortened<br />
activated partial thromboplastin<br />
time show increased in-hospital<br />
mortality associated with elevated<br />
D-dimer, C-reactive protein and<br />
glucose levels. Scand J Clin Lab<br />
Invest 63:441-448, 2003<br />
tee adequate coagulation factor<br />
levels. Anesthesiology 94:542;<br />
author reply 543, 2001<br />
Tetrault G: Establishing reference<br />
ranges for PT and aPTT times. Am<br />
J Clin Pathol 113:741-742, 2000<br />
van den Besselaar AM, Sturk A,<br />
Reijnierse GL: Monitoring of unfractionated<br />
heparin with the activated<br />
partial thromboplastin time:<br />
determination of therapeutic<br />
ranges. Thromb Res 107:235-240,<br />
2002<br />
White GC, 2nd: The partial thromboplastin<br />
time: defining an era in<br />
coagulation. J Thromb Haemost<br />
1:2267-2270, 2003<br />
Wojtkowski TA, Rutledge JC, Matthews<br />
DC: The clinical impact of<br />
increased sensitivity PT and APTT<br />
coagulation assays. Am J Clin<br />
Pathol 112:225-232, 1999<br />
Lippi G, Franchini M, Brazzarola P,<br />
et al: Preoperative screening: the<br />
Teruya J, Oropeza M, Ramsey G:<br />
A normal aPTT does not guaran-