D-Dimer Assays - Pathology
D-Dimer Assays - Pathology
D-Dimer Assays - Pathology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
D-<strong>Dimer</strong> <strong>Assays</strong> 1<br />
D-<strong>Dimer</strong> <strong>Assays</strong><br />
Feature<br />
Roger S. Riley, M.D., Ph.D.<br />
Ann Tidwell, M.T. (ASCP) SH<br />
April, 2005<br />
Synonyms<br />
XDP, Fragment D-dimer, Fibrin degradation fragment.<br />
Test Description<br />
The D-dimer assay is specific for fibrin derivatives. In this assay, the presence of<br />
cross-linked D-dimer domain is diagnostic for lysis of a fibrin clot, and confirm that<br />
thrombin was formed and Factor XIII was activated with reactive fibrinolysis. Since<br />
fibrinogen derivatives do not contain the cross-linked D-dimer domain, they are not<br />
recognized by the D-dimer assay, even when present in high concentration. In other<br />
words, fibrin derivatives in plasma containing D-<strong>Dimer</strong> (XDP) are specific<br />
markers for fibrinolysis, as opposed to fibrinogenolysis. D-dimers are detected<br />
by immunoassays using monoclonal antibodies specific for the cross-linked D-dimer<br />
domain in fibrinogen. Commercially available assays include latex agglutination, immunoturbidimetry,<br />
and ELISA.<br />
Patient<br />
Preparation<br />
Specimen<br />
No specific patient preparation is required for the measurement of D-dimers.<br />
Citrated, platelet-poor plasma is used for the D-dimer assay.<br />
Specimen<br />
Collection<br />
and<br />
Preparation<br />
Citrated, platelet-poor plasma is prepared from venous blood collected by venipuncture<br />
or from an indwelling catheter. The blood is collected into 3.2%) trisodium citrate<br />
at a ratio of 9:1. The blue-top tube automatically fills to the correct volume; spurious<br />
results may occur if this ratio is not maintained. The citrate concentration must be adjusted<br />
in patients with a HCT >55%. Plasma should be separated from the cells as<br />
soon as possible after the specimen is obtained. D-dimers are stable for 8 hours in citrated<br />
plasma maintained at room temperature, for seven days if stored at 2-8 o C, and<br />
up to two months at -20 o C.<br />
Test<br />
Methodology<br />
D-dimers are detected by immunoassays using monoclonal antibodies specific for the<br />
cross-linked D-dimer domain in fibrinogen. Present commercially available assays are<br />
based on particle agglutination, immunoturbidimetry, and ELISA.<br />
ELISA assays are the reference standard for D-dimer quantitation. These assays utilize<br />
microtiter wells coated with an antibody with a high affinity for D-dimer. Incubation<br />
with plasma results in the binding of any D-dimer present. A labeled antibody is then<br />
added and the amount of bound labeled substance is determined by a colormetric reaction.<br />
In spite of their high sensitivity and specificity, conventional ELISA assays are<br />
expensive, labor intensive, and time consuming to perform. Therefore, they have not<br />
been practical in most clinical situations, where rapidly available results are needed.<br />
Latex agglutination (LA) assays use latex microparticles coated with monoclonal antibodies<br />
specific for D-dimer. Incubation with plasma results in the formation of macroscopic<br />
agglutinates. The sensitivity of the assay is usually adjusted to 1 g/ml during<br />
the manufacture of the latex particles. Although conventional latex agglutination as-
D-<strong>Dimer</strong> <strong>Assays</strong> 2<br />
Test<br />
Methodology<br />
says are inexpensive and rapid to perform, numerous studies have shown that they<br />
lack the sensitivity to detect D-dimers in critical clinical situations, particularly in the<br />
detection of pulmonary embolism and acute venous thrombosis.<br />
Immunoturbidometric assays are automated microparticle assays in which a beam of<br />
monochromatic light is passed through a suspension of latex microparticles coated by<br />
covalent bonding with monoclonal antibodies specific for D-dimer. The wavelength of<br />
the light (540 nm) is greater than the diameter of the latex microparticles and so the<br />
solution of latex microparticles only slightly absorbs the light. When the plasma is<br />
added to the suspension, any D-dimer present in the sample causes the latex microparticles<br />
to agglutinate, becoming aggregates with diameters greater than the wavelength<br />
of the light. This increases the absorbance of the light, which is measured photometrically,<br />
and proportional to the amount of D-dimer present in the test sample.<br />
These assays are cost effective, relatively rapid to perform, and have a sensitivity<br />
comparable to conventional ELISA.<br />
A commercially available whole blood assay for D-dimer uses a bispecific antibody specific<br />
for D-dimer and a red blood cell antigen. A drop of whole blood is incubated with<br />
the monoclonal antibody solution, causing visible agglutination of the red cells if D-<br />
dimers are present. Many reports have indicated a high sensitivity for the assay, and it<br />
is widely used in clinical settings.<br />
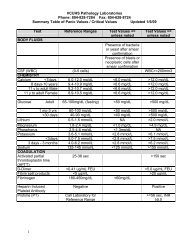
Normal Values and<br />
Critical Limits<br />
The reporting standard for D-dimers varies with the test methodology and reagent<br />
manufacturer. Latex and whole blood agglutination results are usually reported<br />
as a D-dimer range (ng/mL). ELISA and immunoturbidimetric assays are<br />
usually reported in fibrinogen equivalent units (FEU). One FEU is the quantity of<br />
fibrinogen that was initially present before it was broken down. The actual<br />
quantity of D-dimer is approximately half of an FEU (when 1.0 of fibrinogen g/<br />
mL is broken down, 0.5 g/mL of D-<strong>Dimer</strong> remain).<br />
Interferences<br />
Rheumatoid factor may cause a false positive D-dimer assay. Lipemia may interfere<br />
with immunoturbidimetric and ELISA assays.<br />
Clinical Utilization<br />
XDPs are cross-linked fibrin degradation products which arise directly from fibrin.<br />
Thus, the measurement of XDPs, unlike total FDPs, is a specific measure of fibrinolysis.<br />
Elevated D dimers are seen in DIC, pulmonary embolism, arterial and venous<br />
thrombosis, septicemia, cirrhosis, carcinoma, sickle cell crisis, and following operative<br />
procedures. Both FDPs and XDPs are present during late pregnancy and for approximately<br />
48 hours post-surgery. During fibrinolytic therapy the FDP test is positive, while<br />
the D-dimer test is negative in the absence of thrombolysis.<br />
Disseminated intravascular coagulation (DIC, consumption coagulopathy) is one of the<br />
most common and clinically important acquired disorders of hemostasis. In DIC, intravascular<br />
activation of the coagulation system results in the widespread deposition of<br />
fibrin microthrombi in the microcirculation, the consumption of platelets and clotting<br />
factors, and activation of the fibrinolytic system. At the same time that thrombin converts<br />
fibrinogen to fibrin, it also activated Factor XIII to form a plasma transglutaminase,<br />
Factor XIIIa, which stabilizes fibrin by cross-linking the gamma chains of fibrinogen<br />
in the region of the D-domain. Plasmin digests fibrin and fibrinogen to produce<br />
fibrin(ogen) degradation (FDP) (or split, FSP) products (X,Y,D, and E), which are removed<br />
from the circulation by the reticuloendothelial system.
D-<strong>Dimer</strong> <strong>Assays</strong> 3<br />
Clinical Utilization<br />
DIC is not a specific disease, but a sequalae of many pathologic conditions, including<br />
acute intravascular hemolysis, hemolytic transfusion reactions, shock, hyperthermia,<br />
extensive tissue damage, malignancies, obstetric complications, hyperthermia, snake<br />
bites, etc. Prompt diagnosis and therapy of DIC is essential, since the associated hemorrhage,<br />
small vessel thrombosis, and occasional large vessel thrombosis can lead to<br />
the impairment of blood flow, ischemia, end-organ damage, and death. The clinical<br />
signs and symptoms in DIC are variable and non-specific, and include fever, hypotension,<br />
acidosis, proteinuria, hypoxia, petechiae and purpura, subcutaneous hematomas,<br />
bleeding (surgical wound, traumatic wound, venipuncture), and arterial line oozing.<br />
There is no laboratory assay pathognomonic of DIC. However, peripheral smear examination<br />
is among the most helpful. In fulminent cases, this shows a characteristic<br />
combination of schistocytes (red blood cell fragments), mild polychromatophilia, leukocytosis<br />
with a left shift, thrombocytopenia, and large young platelets. However, the<br />
diagnosis of DIC cannot be excluded by an absence of schistocytes, since these occur<br />
in only 50% of patients. In addition to peripheral smear review, the prothrombin time<br />
(PT), activated partial thromboplastin time (aPTT), platelet count, and serum fibrin/<br />
fibrinogen degradation products are the best screening tests for DIC. The D-dimer assay<br />
is more specific, and can be used to confirm the diagnosis.<br />
The D-dimer has received much attention in recent years as a critical part of the<br />
evaluation of emergency care patients with suspected pulmonary embolism (PE) or<br />
deep venous thrombosis (DVT). Generally, numerous studies have shown that the<br />
more advanced ELISA and immunoturbidometric assays have a sensitivity of 90% or<br />
greater for PE or DVT in this setting, and a negative predictive value of 90% or greater<br />
for the exclusion of disease. However, there is presently much debate about how the<br />
results should be correlated with other findings, particularly radiographic studies.<br />
The analysis of plasma D-dimers has been reported to be of diagnostic value in patients<br />
with suspected complications of pregnancy such as pre-eclampsia and the HELLP<br />
syndrome, to monitor anticoagulant and thrombolytic therapy, and to correlate with<br />
disease severity in rheumatoid arthritis. CSF D-dimers have been reported positive in<br />
patients with subarachnoid hemorrhage, but not in normal patients or those with<br />
traumatic lumbar puncture.<br />
References<br />
Andreescu AC, Cushman M, Rosendaal<br />
FR: D-dimer as a risk<br />
factor for deep vein thrombosis:<br />
the Leiden Thrombophilia Study.<br />
Thromb Haemost 87:47-51, 2002<br />
Arkel YS, Paidas MJ, Ku DH: The<br />
use of coagulation activation<br />
markers (soluble fibrin polymer,<br />
TpP, prothrombin fragment 1.2,<br />
thrombin-antithrombin, and D-<br />
dimer) in the assessment of hypercoagulability<br />
in patients with<br />
inherited and acquired prothrombotic<br />
disorders. Blood Coagul Fibrinolysis<br />
13:199-205, 2002<br />
Bates SM, Kearon C, Crowther M,<br />
et al: A diagnostic strategy involving<br />
a quantitative latex D-dimer<br />
assay reliably excludes deep venous<br />
thrombosis. Ann Intern Med<br />
138:787-794, 2003<br />
Bosson JL, Barro C, Satger B, et<br />
al: Quantitative high D-dimer value<br />
is predictive of pulmonary embolism<br />
occurrence independently of<br />
clinical score in a well-defined low<br />
risk factor population. J Thromb<br />
Haemost 3:93-99, 2005<br />
Brown MD, Lau J, Nelson RD, et<br />
al: Turbidimetric D-dimer test in<br />
the diagnosis of pulmonary embolism:<br />
a metaanalysis. Clin Chem<br />
49:1846-1853, 2003<br />
Caine GJ, Lip GY: D-dimer tests<br />
for assessment of patients with<br />
suspected pulmonary embolism.<br />
Arch Intern Med 163:243, 2003<br />
Epiney M, Boehlen F, Boulvain M,<br />
et al: D-dimer levels during delivery<br />
and the postpartum. J Thromb<br />
Haemost 3:268-271, 2005<br />
Falanga A: The predictive value of<br />
D-dimer measurement for cancer<br />
in patients with deep vein thrombosis.<br />
Haematologica 90:149b,<br />
2005<br />
Fancher TL, White RH, Kravitz RL:<br />
Combined use of rapid D-dimer<br />
testing and estimation of clinical<br />
probability in the diagnosis of deep<br />
vein thrombosis: systematic review.<br />
Bmj 329:821, 2004<br />
Froehling DA, Elkin PL, Swensen<br />
SJ, et al: Sensitivity and specificity<br />
of the semiquantitative latex agglutination<br />
D-dimer assay for the<br />
diagnosis of acute pulmonary embolism<br />
as defined by computed<br />
tomographic angiography. Mayo<br />
Clin Proc 79:164-168, 2004<br />
Gardiner C, Pennaneac'h C, Walford<br />
C, et al: An evaluation of rapid<br />
D-dimer assays for the exclusion<br />
of deep vein thrombosis. Br J<br />
Haematol 128:842-848, 2005
D-<strong>Dimer</strong> <strong>Assays</strong> 4<br />
References<br />
(Cont’d)<br />
Gosselin RC, Owings JT, Kehoe J,<br />
et al: Comparison of six D-dimer<br />
methods in patients suspected of<br />
deep vein thrombosis. Blood Coagul<br />
Fibrinolysis 14:545-550, 2003<br />
Heim SW, Schectman JM, Siadaty<br />
MS, et al: D-dimer testing for deep<br />
venous thrombosis: a metaanalysis.<br />
Clin Chem 50:1136-1147,<br />
2004<br />
Ireland B: Negative ELISA D-dimer<br />
assay can miss pulmonary embolism.<br />
J Fam Pract 52:99, 103,<br />
2003<br />
Le Gal G, Bounameaux H: D-<br />
dimer for the diagnosis of pulmonary<br />
embolism: a call for sticking<br />
to evidence. Intensive Care Med<br />
31:1-2, 2005<br />
Lippi G, Guidi GC: Effect of<br />
specimen collection on routine<br />
coagulation assays and D-dimer<br />
measurement. Clin Chem<br />
50:2150-2152, 2004<br />
Mavromatis BH, Kessler CM: D-<br />
dimer testing: the role of the clinical<br />
laboratory in the diagnosis of<br />
pulmonary embolism. J Clin Pathol<br />
54:664-668, 2001<br />
Monaco J, Newton W: Elevated D-<br />
dimer level predicts recurrent VTE.<br />
J Fam Pract 53:20, 23, 2004<br />
Monreal L: D-dimer as a new test<br />
for the diagnosis of DIC and<br />
thromboembolic disease. J Vet<br />
Intern Med 17:757-759, 2003<br />
Oswald CT, Menon V, Stouffer GA:<br />
The use of D-dimer in emergency<br />
room patients with suspected<br />
deep vein thrombosis: a test<br />
whose time has come. J Thromb<br />
Haemost 1:635-636, 2003<br />
Perrier A: D-dimer for suspected<br />
pulmonary embolism: whom<br />
should we test? Chest<br />
125:807-809, 2004<br />
Perrier A, Palareti G: D-dimer testing<br />
and venous thromboembolism:<br />
four view points. J Thromb Haemost<br />
3:382-384, 2005<br />
Reber G, Bounameaux H, Perrier<br />
A, et al: A new rapid point-of-care<br />
D-dimer enzyme-linked immunosorbent<br />
assay (Stratus CS D-<br />
dimer) for the exclusion of venous<br />
thromboembolism. Blood Coagul<br />
Fibrinolysis 15:435-438, 2004<br />
Saigo M, Waters DD, Abe S, et al:<br />
Soluble fibrin, C-reactive protein,<br />
fibrinogen, factor VII, antithrombin,<br />
proteins C and S, tissue factor, D-<br />
dimer, and prothrombin fragment 1<br />
+ 2 in men with acute myocardial<br />
infarction