Case Studies in Clinical Hemostasis Case Studies in ... - Pathology
Case Studies in Clinical Hemostasis Case Studies in ... - Pathology
Case Studies in Clinical Hemostasis Case Studies in ... - Pathology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Case</strong> <strong>Studies</strong><br />
<strong>in</strong><br />
Cl<strong>in</strong>ical<br />
<strong>Hemostasis</strong>
<strong>Case</strong> <strong>Studies</strong><br />
<strong>in</strong><br />
Cl<strong>in</strong>ical<br />
<strong>Hemostasis</strong><br />
<strong>Case</strong> #1<br />
Patient J.M.
Patient J.M.<br />
! Middle-aged man admitted for elective<br />
cholecystomy<br />
! Two previous dental extractions associated<br />
with rebleed<strong>in</strong>g requir<strong>in</strong>g repack<strong>in</strong>g<br />
! History of easy bruis<strong>in</strong>g and occasional<br />
nosebleeds<br />
! No other operative procedures<br />
! No history of trauma<br />
! Family history negative for bleed<strong>in</strong>g and<br />
thrombosis<br />
! Physical exam<strong>in</strong>ation unremarkable except for<br />
abdom<strong>in</strong>al tenderness
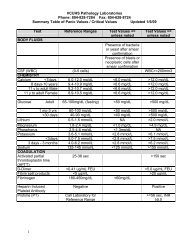
Patient J.M.<br />
600<br />
20<br />
50<br />
20<br />
THOU/uL<br />
500<br />
400<br />
300<br />
200<br />
100<br />
●<br />
Seconds<br />
15<br />
10<br />
5<br />
●<br />
Seconds<br />
45<br />
40<br />
35<br />
30<br />
25<br />
●<br />
M<strong>in</strong>utes<br />
15<br />
10<br />
5<br />
●<br />
0<br />
PLTS<br />
0<br />
PT<br />
20<br />
APTT<br />
0<br />
Bleed<strong>in</strong>g Time
Primary & Secondary <strong>Hemostasis</strong><br />
Primary <strong>Hemostasis</strong><br />
Platelet Adhesion & Aggregation<br />
Platelet Plug Formation<br />
Secondary <strong>Hemostasis</strong><br />
Coagulation<br />
Platelet Plug Stabilization
Platelet Structure<br />
Surface canalicular system<br />
Surface receptors<br />
Mitochondria<br />
Lysozymes<br />
α-granules<br />
Microtubules<br />
Dense bodies<br />
Cell membrane<br />
Glycogen granules
Damaged Damaged Vessel Vessel Wall Wall<br />
Platelet<br />
Function<br />
Platelet Platelet Adhesion Adhesion<br />
Platelet Platelet Shape Shape Change Change<br />
Primary Primary Aggregation<br />
Aggregation<br />
Metabolic Metabolic Events Events<br />
Degranulation<br />
Secondary Secondary Aggregation<br />
Aggregation
Platelet Activation<br />
ADP<br />
Rest<strong>in</strong>g<br />
platelet<br />
Activated platelet<br />
with FbR<br />
Doublet and<br />
multiplet formation
GPIb<br />
GPIIbIIIa<br />
PLT<br />
Function<br />
Platelet membrane<br />
Adhesion site<br />
Aggregation, vWF, and<br />
fibr<strong>in</strong>ogen b<strong>in</strong>d<strong>in</strong>g site<br />
vWF<br />
VIII:C<br />
Subendothelial<br />
collagen
Sources of vWF<br />
Platelets<br />
Endothelial Cell<br />
Weibel-Palade<br />
Body (HMW)<br />
α-Granule (LMW)
Platelet<br />
Agonists<br />
Membrane<br />
Glycoprote<strong>in</strong><br />
Membrane<br />
Phospholipids<br />
Phospholipase<br />
Arachidonic Acid<br />
Platelet<br />
Metabolism<br />
Dense<br />
Granules<br />
Cyclo-oxygenase<br />
Cyclic<br />
Endoperoxidases<br />
ADP<br />
Thromboxane<br />
Synthetase<br />
Platelet<br />
Aggregation<br />
TxA 2<br />
TxA 2
Platelet Aggregation <strong>Studies</strong><br />
Platelet agonist*<br />
Incubate 10 m<strong>in</strong>utes<br />
Measure light transmission<br />
Platelet rich plasma<br />
Aggregated platelets<br />
* Platelet agonists - ADP, ep<strong>in</strong>ephr<strong>in</strong>e, collagen<br />
ristocet<strong>in</strong>, arachidonic acid, thromb<strong>in</strong>
Platelet Aggregation<br />
Light<br />
Shape<br />
Change<br />
Secondary<br />
Aggregation<br />
Primary<br />
Aggregation<br />
Time
100<br />
80<br />
60<br />
ADP<br />
Normal Aggregation<br />
100<br />
80<br />
60<br />
EPI<br />
40<br />
ADP - 1 µM<br />
40<br />
20<br />
ADP - 1 µM<br />
ADP - 1 µM<br />
20<br />
EPI 5 µM<br />
0<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
0 2 4 6 8 10<br />
Time (M<strong>in</strong>utes)<br />
COLL<br />
Collagen 2 µg/mL<br />
0 2 4 6 8 10<br />
Time (M<strong>in</strong>utes)<br />
0<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
0 2 4 6 8 10<br />
Time (M<strong>in</strong>utes)<br />
RIST<br />
Ristocet<strong>in</strong> 1.2 mg/mL<br />
0 2 4 6 8 10<br />
Time (M<strong>in</strong>utes)
Coagulation<br />
Prothromb<strong>in</strong><br />
Thromb<strong>in</strong><br />
Fibr<strong>in</strong>ogen<br />
Fibr<strong>in</strong>
Coagulation<br />
Prothromb<strong>in</strong><br />
Tissue<br />
Factor<br />
Extr<strong>in</strong>sic<br />
Pathway<br />
Va<br />
VIIIa<br />
Xa<br />
Va<br />
VIIIa<br />
Xa<br />
Intr<strong>in</strong>sic<br />
Pathway<br />
Factor<br />
XII<br />
Thromb<strong>in</strong><br />
Fibr<strong>in</strong>ogen<br />
Fibr<strong>in</strong>
Contact<br />
Factors<br />
- Charged<br />
Surface<br />
Modern Concept<br />
of Coagulation<br />
XI XI<br />
XIa XIa<br />
VII<br />
IX IX<br />
IXa IXa<br />
Tissue<br />
Factor<br />
Injured<br />
Tissue<br />
VIII<br />
VII<br />
XX<br />
Xa Xa<br />
V<br />
Prothromb<strong>in</strong><br />
Thromb<strong>in</strong>
Coagulation<br />
Prothromb<strong>in</strong><br />
Tissue<br />
Factor<br />
Prothromb<strong>in</strong><br />
Time<br />
Extr<strong>in</strong>sic<br />
Pathway<br />
Va<br />
VIIIa<br />
Xa<br />
Va<br />
VIIIa<br />
Xa<br />
Intr<strong>in</strong>sic<br />
Pathway<br />
Factor<br />
XII<br />
Thromb<strong>in</strong><br />
Fibr<strong>in</strong>ogen<br />
Fibr<strong>in</strong>
Prothromb<strong>in</strong><br />
Time (PT)<br />
Thromboplast<strong>in</strong><br />
Ca ++<br />
Plateletrich<br />
plasma<br />
Incubate<br />
Fibr<strong>in</strong><br />
clot
Coagulation<br />
Prothromb<strong>in</strong><br />
Tissue<br />
Factor<br />
Extr<strong>in</strong>sic<br />
Pathway<br />
Va<br />
VIIIa<br />
Xa<br />
Va<br />
VIIIa<br />
Xa<br />
Thromb<strong>in</strong><br />
Intr<strong>in</strong>sic<br />
Pathway<br />
Factor<br />
XII<br />
Activated Partial<br />
Thromboplastic<br />
Time (aPTT)<br />
Fibr<strong>in</strong>ogen<br />
Fibr<strong>in</strong>
Activated Partial<br />
Thromboplast<strong>in</strong><br />
Time (aPTT)<br />
Partial<br />
Thromboplast<strong>in</strong><br />
Platelet Activator<br />
Ca ++<br />
Plateletrich<br />
plasma<br />
Incubate<br />
Fibr<strong>in</strong><br />
clot
Patient J.M.<br />
! Middle-aged man admitted for elective<br />
cholecystomy<br />
! Two previous dental extractions associated<br />
with rebleed<strong>in</strong>g requir<strong>in</strong>g repack<strong>in</strong>g<br />
! History of easy bruis<strong>in</strong>g and occasional<br />
nosebleeds<br />
! No other operative procedures<br />
! No history of trauma<br />
! Family history negative for bleed<strong>in</strong>g and<br />
thrombosis<br />
! Physical exam<strong>in</strong>ation unremarkable except for<br />
abdom<strong>in</strong>al tenderness
Defects of <strong>Hemostasis</strong><br />
Bleed<strong>in</strong>g<br />
Thrombosis
Vascular Defects<br />
! Hereditary vascular purpuras<br />
Hereditary connective tissue diseases<br />
Hereditary vascular malformations<br />
! Acquired vascular purpuras<br />
Age-related vascular purpura<br />
Mechanical purpuras<br />
Vitam<strong>in</strong> C deficiency (Scurvy)<br />
Vasculitis/<strong>in</strong>fection<br />
Henoch-Schonle<strong>in</strong> purpura<br />
Miscellaneous diseases
Platelet Diseases<br />
Bleed<strong>in</strong>g<br />
Thrombosis<br />
Platelet production<br />
Shortened survival<br />
Defective adhesion<br />
Defective aggregation<br />
Defective activation<br />
Antiplatelet antibodies<br />
Hyperactive<br />
platelets<br />
Excess activation
Diseases of Coagulation<br />
! Inherited diseases<br />
von Willebrand’s disease<br />
Factor deficiencies<br />
! Acquired<br />
diseases<br />
Dissem<strong>in</strong>ated <strong>in</strong>travascular coagulation<br />
Caogulation <strong>in</strong>hibitors<br />
Vitam<strong>in</strong> K deficiency<br />
Drug-<strong>in</strong>duced hemorrhage<br />
Dysprote<strong>in</strong>emias<br />
Bleed<strong>in</strong>g after cardiopulmonary bypass
Factor Activity (%)<br />
200<br />
180<br />
160<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Factor I<br />
Factor II<br />
Factor V<br />
Factor VII<br />
Factor VIII<br />
Factor IX<br />
Factor X<br />
Factor XI<br />
Factor XII<br />
vWF:RCoF<br />
vWF:Ag<br />
Patient J.M.<br />
●<br />
● ●<br />
●<br />
●<br />
●<br />
●<br />
Prekallikre<strong>in</strong><br />
●<br />
HMWK<br />
●
GPIb<br />
GPIIbIIIa<br />
PLT<br />
Function<br />
Platelet membrane<br />
Adhesion site<br />
Aggregation, vWF, and<br />
fibr<strong>in</strong>ogen b<strong>in</strong>d<strong>in</strong>g site<br />
vWF<br />
VIII:C<br />
Subendothelial collagen
GPIb<br />
GPIIbIIIa<br />
vWD<br />
Platelet membrane<br />
Adhesion site<br />
Aggregation, vWF, and<br />
fibr<strong>in</strong>ogen b<strong>in</strong>d<strong>in</strong>g site<br />
vWF<br />
VIII:C<br />
Subendothelial<br />
collagen
Worldwide<br />
Prevalence of<br />
vWD is 1-3%
History of vWD<br />
! 1926 - Erik Adolf von Willebrand<br />
described family with bleed<strong>in</strong>g disorder<br />
! Swedish island of Foglo <strong>in</strong> Aland<br />
archipelago<br />
! Termed “hereditary pseudohemophilia”<br />
! 1953 - Deficiency of plasma prote<strong>in</strong><br />
dist<strong>in</strong>ct from factor VIII<br />
! Multiple cl<strong>in</strong>ical variants discovered<br />
! Most common congenital hemostatic<br />
disorder
von Willebrand’s Disease<br />
Cl<strong>in</strong>ical Features<br />
! Common hereditary procoagulant disease<br />
! Frequently mild, most cases undiagnosed<br />
! Multiple cl<strong>in</strong>ical variants<br />
! Easy brusis<strong>in</strong>g very common<br />
! Mucosal bleed<strong>in</strong>g (epistaxis, GI bleed<strong>in</strong>g,<br />
menorrhagia) very common<br />
! Prolonged bleed<strong>in</strong>g after surgery or trauma<br />
a<br />
! Bleed<strong>in</strong>g caused by drugs affect<strong>in</strong>g platelet<br />
function<br />
! No history of hemarthroses or <strong>in</strong>tramuscular<br />
hematomas
Cl<strong>in</strong>ical<br />
Features<br />
of vWD<br />
Epistaxis<br />
Easy Bruis<strong>in</strong>g<br />
Drug-Induced<br />
Bleed<strong>in</strong>g<br />
Prolonged<br />
bleed<strong>in</strong>g after<br />
trauma<br />
Menorrhagia<br />
GI Bleed<strong>in</strong>g
Relationship Between vWF<br />
and ABO Blood Groups<br />
Individuals with<br />
Blood Group O have<br />
significantly lower<br />
levels of vWF than<br />
those with blood<br />
groups A, B, or AB
von Willebrand’s Disease<br />
Classification<br />
! Type 1 - 70-80%, mild, autosomal recessive<br />
! Type 2<br />
Type 2A - 15-20%, mild<br />
Type 2N - Rare, moderate, failure of vWF to<br />
complex with VIII:C<br />
Type 2B - Rare, thrombocytopenia,<br />
<strong>in</strong>creased vWF aff<strong>in</strong>ity for PLTS<br />
! Type 3 - Very rare, severe, decreased vWF and<br />
factor VIII, autosomal recessive<br />
! Platelet-Type Pseudo vWF - Abnormality of PLT<br />
GP1b receptor, <strong>in</strong>creased vWF aff<strong>in</strong>ity,<br />
resembles Type 2B<br />
! Acquired vWF - Usually autoimmune etiology
von Willebrand’s Disease<br />
Laboratory Features<br />
! Normal PLT (with exceptions)<br />
! Prolonged bleed<strong>in</strong>g time<br />
! Prolonged aPTT<br />
! Decreased factor VIII activity<br />
(FVIII:C)<br />
! Decreased vWF antigen<br />
(vWF:Ag)<br />
! Abnormal ristocet<strong>in</strong> cofactor<br />
activity (vWF:RCoF)<br />
! Abnormal vWF multimeric<br />
composition<br />
! Molecular<br />
abnormalities
Diagnostic Assays for vWD I<br />
! Factor VIII activity<br />
Clott<strong>in</strong>g assay<br />
Capacity of patient plasma dilutions to correct<br />
clott<strong>in</strong>g time of FVIII-deficient plasma<br />
! vWF Activity (RCoF Activity)<br />
Platelet aggregation assa y<br />
Different concentrations of ristocet<strong>in</strong> mixed with<br />
patient PPP and normal platelets<br />
! vWF Antigen<br />
Immunoassay quantitation<br />
ELISA commonly utiized
Diagnostic Assays for vWD II<br />
! Ristocet<strong>in</strong>-<strong>in</strong>duced agglut<strong>in</strong>ation assay<br />
Platelet aggregation assay<br />
Patient PRP + graded ristocet<strong>in</strong> concentrations<br />
! Cryoprecipitate-<strong>in</strong>duced agglut<strong>in</strong>ation assay<br />
Patient PRP + normal cryoprecipitate<br />
Spontaneous agglut<strong>in</strong>ation with platelet-type<br />
pseudo-vWD<br />
! vWF multimer analysis<br />
Gel<br />
electrophoresis<br />
Subtypes show different migration patterns<br />
Used to subtype vWD after Dx established<br />
Laborious and expensive
vWF Multimers<br />
Large<br />
Multimers<br />
Intermediate<br />
Multimers<br />
Small<br />
Multimers<br />
Normal<br />
Type I<br />
Type IIA<br />
Type IIB<br />
Type III
vWF Treatment<br />
! Replacement therapy<br />
Plasma derived factor VIII concentrates<br />
Type 3, type 2B, type 2N<br />
Factor VIII concentrates, cryoprecipitate<br />
Platelets<br />
Platelet-type<br />
pseudo-vWD<br />
Plasma concentrates contra<strong>in</strong>dicated<br />
! Desmopress<strong>in</strong><br />
acetate<br />
Synthetic analog of vasopress<strong>in</strong><br />
Stimulates vWF and factor VIII release<br />
Ma<strong>in</strong>stay of Rx for Type I and Type 2A<br />
Injection and nasal spray<br />
! Ancillary therapy<br />
Fibr<strong>in</strong>olytic <strong>in</strong>hibitors and “fibr<strong>in</strong> glue”
<strong>Case</strong> <strong>Studies</strong><br />
<strong>in</strong><br />
Cl<strong>in</strong>ical<br />
<strong>Hemostasis</strong><br />
<strong>Case</strong> #1<br />
The End