Guideline for The Early Detection of Breast Cancer - Toward ...
Guideline for The Early Detection of Breast Cancer - Toward ...
Guideline for The Early Detection of Breast Cancer - Toward ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
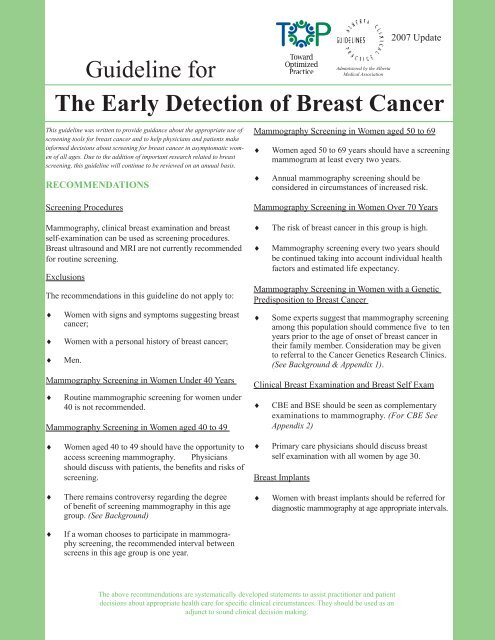
2007 Update<br />
Administered by the Alberta<br />
<strong>Guideline</strong> <strong>for</strong><br />
Medical Association<br />
<strong>The</strong> <strong>Early</strong> <strong>Detection</strong> <strong>of</strong> <strong>Breast</strong> <strong>Cancer</strong><br />
This guideline was written to provide guidance about the appropriate use <strong>of</strong><br />
screening tools <strong>for</strong> breast cancer and to help physicians and patients make<br />
in<strong>for</strong>med decisions about screening <strong>for</strong> breast cancer in asymptomatic women<br />
<strong>of</strong> all ages. Due to the addition <strong>of</strong> important research related to breast<br />
screening, this guideline will continue to be reviewed on an anuual basis.<br />
RECOMMENDATIONS<br />
Screening Procedures<br />
Mammography, clinical breast examination and breast<br />
self-examination can be used as screening procedures.<br />
<strong>Breast</strong> ultrasound and MRI are not currently recommended<br />
<strong>for</strong> routine screening.<br />
Exclusions<br />
<strong>The</strong> recommendations in this guideline do not apply to:<br />
♦<br />
♦<br />
♦<br />
Women with signs and symptoms suggesting breast<br />
cancer;<br />
Women with a personal history <strong>of</strong> breast cancer;<br />
Men.<br />
Mammography Screening in Women Under 40 Years<br />
♦<br />
Routine mammographic screening <strong>for</strong> women under<br />
40 is not recommended.<br />
Mammography Screening in Women aged 40 to 49<br />
Mammography Screening in Women aged 50 to 69<br />
♦<br />
♦<br />
Women aged 50 to 69 years should have a screening<br />
mammogram at least every two years.<br />
Annual mammography screening should be<br />
considered in circumstances <strong>of</strong> increased risk.<br />
Mammography Screening in Women Over 70 Years<br />
♦<br />
♦<br />
<strong>The</strong> risk <strong>of</strong> breast cancer in this group is high.<br />
Mammography screening every two years should<br />
be continued taking into account individual health<br />
factors and estimated life expectancy.<br />
Mammography Screening in Women with a Genetic<br />
Predisposition to <strong>Breast</strong> <strong>Cancer</strong><br />
♦<br />
Some experts suggest that mammography screening<br />
among this population should commence five to ten<br />
years prior to the age <strong>of</strong> onset <strong>of</strong> breast cancer in<br />
their family member. Consideration may be given<br />
to referral to the <strong>Cancer</strong> Genetics Research Clinics.<br />
(See Background & Appendix 1).<br />
Clinical <strong>Breast</strong> Examination and <strong>Breast</strong> Self Exam<br />
♦<br />
CBE and BSE should be seen as complementary<br />
examinations to mammography. (For CBE See<br />
Appendix 2)<br />
♦<br />
Women aged 40 to 49 should have the opportunity to<br />
access screening mammography. Physicians<br />
should discuss with patients, the benefits and risks <strong>of</strong><br />
screening.<br />
♦<br />
Primary care physicians should discuss breast<br />
self examination with all women by age 30.<br />
<strong>Breast</strong> Implants<br />
♦<br />
<strong>The</strong>re remains controversy regarding the degree<br />
<strong>of</strong> benefit <strong>of</strong> screening mammography in this age<br />
group. (See Background)<br />
♦<br />
Women with breast implants should be referred <strong>for</strong><br />
diagnostic mammography at age appropriate intervals.<br />
♦<br />
If a woman chooses to participate in mammography<br />
screening, the recommended interval between<br />
screens in this age group is one year.<br />
<strong>The</strong> above recommendations are systematically developed statements to assist practitioner and patient<br />
decisions about appropriate health care <strong>for</strong> specific clinical circumstances. <strong>The</strong>y should be used as an<br />
adjunct to sound clinical decision making.
BACKGROUND<br />
Epidemiology<br />
<strong>Breast</strong> cancer is one <strong>of</strong> the most serious health concerns <strong>of</strong><br />
Canadian women and is the most common <strong>for</strong>m <strong>of</strong> cancer<br />
in women excluding non-melanoma skin cancer. <strong>Breast</strong><br />
cancer accounts <strong>for</strong> 30% <strong>of</strong> all new cancer cases. 1,2,3,4 In<br />
2001, 1,644 Alberta women were diagnosed with invasive<br />
breast cancer and 425 women died <strong>of</strong> the disease. 5 <strong>Breast</strong><br />
cancer accounts <strong>for</strong> nearly 21% <strong>of</strong> all cancer deaths in<br />
Alberta women. 1<br />
Risk Factors<br />
<strong>The</strong> lifetime risk <strong>for</strong> breast cancer is one in nine. <strong>The</strong> risk<br />
however, varies over a woman’s lifetime. Table 1 reflects<br />
the age specific risk <strong>of</strong> breast cancer <strong>for</strong> women. 6<br />
Table One<br />
Probability <strong>of</strong> Developing <strong>Breast</strong> <strong>Cancer</strong><br />
in the Next Five Years, by Age, <strong>for</strong><br />
Women Who Reside in Alberta and<br />
Currently Do Not Have <strong>Breast</strong> <strong>Cancer</strong><br />
Age<br />
Probability<br />
35 1/384<br />
40 1/208<br />
45 1/128<br />
50 1/109<br />
55 1/94<br />
60 1/78<br />
65 1/70<br />
70 1/65<br />
Increasing age, being born in North America and<br />
northwest Europe, and having two or more first degree<br />
relatives with a history <strong>of</strong> breast cancer are identified as<br />
the strongest risk factors.<br />
<strong>The</strong>re are many other identifiable risk factors, but few<br />
are amenable to change. It is estimated that up to 80% <strong>of</strong><br />
women who develop breast cancer have no risk factors<br />
other than being female, and in a higher risk age group. 7<br />
Evidence from the WHI 8 studies indicate that in any<br />
single year, 0.08 percent more women in the HRT group<br />
developed breast cancer than women in the placebo<br />
group, suggesting that the effect <strong>of</strong> HRT on the risk <strong>of</strong><br />
breast cancer is small.<br />
Definition <strong>of</strong> Screening <strong>for</strong> <strong>Breast</strong> <strong>Cancer</strong> used in this<br />
CPG<br />
<strong>Breast</strong> cancer screening refers to the application <strong>of</strong> a<br />
procedure to asymptomatic women <strong>for</strong> the purpose <strong>of</strong><br />
detecting unsuspected breast cancer at a stage when early<br />
intervention can affect the outcome.<br />
Mammography Screening<br />
A normal screening mammography does not rule out breast<br />
cancer in the presence <strong>of</strong> persistent palpable abnormalities.<br />
Further evaluation may still be required.<br />
Screening in Women Under 40 Years<br />
Randomized controlled studies have not included women<br />
in this age group. 9 Routine screening is not recommended.<br />
Screening in Women Aged 40 to 49 Years<br />
In women aged 40 to 49, breast cancer is the single<br />
leading cause <strong>of</strong> death. 3,4 Some <strong>of</strong> the reservations about<br />
making population-based recommendations <strong>for</strong> women in<br />
this age group, are based on limitations in the scientific evidence<br />
available to date. While there is emerging evidence<br />
<strong>of</strong> benefit from some combined analyses <strong>of</strong> the randomized<br />
trials, the benefit is smaller than in older women,<br />
and is <strong>of</strong> borderline statistical significance. 10,11<br />
<strong>The</strong>re has been a lot <strong>of</strong> debate in the literature regarding<br />
the reasons <strong>for</strong> the apparent decreased benefit <strong>of</strong> screening.<br />
Evidence to date suggests that screening mammography<br />
is less sensitive <strong>for</strong> women in their <strong>for</strong>ties than<br />
<strong>for</strong> older women. 12 It has also been suggested that due to<br />
more rapid growth <strong>of</strong> tumours in this age group that the<br />
interval between screens in some studies has been too<br />
long to show a benefit. 13 Data suggests that annual mammography<br />
in this age group will be required 14 in order to<br />
detect breast cancer at its earliest stages and achieve a<br />
reduction in breast cancer mortality similar to that seen in<br />
older women. 14,15 Finally, there may be statistically insufficient<br />
numbers <strong>of</strong> women in this age group included in<br />
the controlled trials to definitively show a benefit. 16<br />
Concerns have also been raised about the decreased<br />
positive predictive value <strong>of</strong> any <strong>of</strong> the three breast screening<br />
procedures in women in their <strong>for</strong>ties when compared<br />
to older women. In other words, the probability that a<br />
younger woman would have a benign biopsy as a consequence<br />
<strong>of</strong> screening is higher than <strong>for</strong> older women.
Women Aged 50 to 69 Years<br />
Many studies have shown the efficacy <strong>of</strong> mammography<br />
screening <strong>for</strong> breast cancer <strong>for</strong> women aged 50 to<br />
69 years. Regular mammographic screening in this age<br />
group is estimated to reduce mortality from breast carcinoma<br />
by approximately one third. Because additional<br />
benefit with annual screening has not been demonstrated,<br />
screening every two years is <strong>of</strong>ten recommended. 9<br />
Women Over 70 Years<br />
<strong>The</strong> incidence <strong>of</strong> breast cancer increases with age, and<br />
there<strong>for</strong>e women over 70 years continue to be at high<br />
risk. Although no randomized clinical trials have<br />
specifically addressed the efficacy <strong>of</strong> screening in this<br />
age group, it should be continued in the context <strong>of</strong> individual<br />
health factors and life expectancy.<br />
Women a Genetic Predisposition <strong>for</strong> <strong>Breast</strong> <strong>Cancer</strong><br />
Women with a strong family history <strong>of</strong> breast cancer<br />
should be advised <strong>of</strong> the availability <strong>of</strong> counselling and<br />
in<strong>for</strong>mation provided by the <strong>Cancer</strong> Genetics Research<br />
Clinics. (See Appendix 1 <strong>for</strong> referral criteria)<br />
<strong>The</strong> recommended screening interval <strong>for</strong> women in this<br />
group is yearly beginning at age 40 or 5 - 10 years prior<br />
to the age <strong>of</strong> onset <strong>of</strong> breast cancer in a first degree family<br />
member. Additional screening tools <strong>for</strong> this group <strong>of</strong><br />
women are currently being studied including MRI, ultrasound,<br />
and Sestamibi Nuclear Medicine Scans.<br />
Radiation Risk<br />
<strong>The</strong> risk <strong>of</strong> mammographically-induced cancer is generally<br />
considered to be negligible. Some experts have expressed<br />
concern over the theoretical risk <strong>of</strong> radiation-induced<br />
breast cancers, especially among younger women. However,<br />
the studies which have raised this concern involved<br />
much higher levels <strong>of</strong> radiation than are found in present<br />
day mammography. 17,18 <strong>The</strong> radiation dose delivered by<br />
mammography is lower than that <strong>of</strong> an ordinary chest<br />
X-ray.<br />
Factors Affecting the Acceptance <strong>of</strong> Screening Recommendations<br />
<strong>The</strong> strongest stimulus <strong>for</strong> a woman to participate in<br />
mammography screening is the recommendation from<br />
her physician. Studies indicate that many factors affect a<br />
woman’s choice to participate in breast cancer screening.<br />
Adverse factors include age, i.e., younger (40-49) and<br />
older (70 plus) women; socioeconomically disadvantaged;<br />
limited contact with a physician; single martial status;<br />
unemployed and retired; country <strong>of</strong> birth and fewer years<br />
since immigration, i.e., Asia, South and Central America,<br />
Caribbean and Africa; lower educational attainment; and,<br />
rural residence. 19,20,21 Physicians should ensure that all<br />
women who would benefit from screening be in<strong>for</strong>med <strong>of</strong><br />
its potential advantages.<br />
SELECTED REFERENCES<br />
1. National <strong>Cancer</strong> Institute, Canadian <strong>Cancer</strong> Statistics,<br />
1997.<br />
2. Statistics Canada. HEALTH REPORTS. Catalogue<br />
82.003XPB.1997;9(1).<br />
3. Gaudette LA, Silberger C, Altmayer CA et al. Trends<br />
in breast cancer incidence and mortality. HEALTH<br />
REPORTS. Statistics Canada, Catalogue 82.003-<br />
XPB. 1996;8(2):29-37.<br />
4. Bondy M, Luskbader E, Halabi S, et al. Validation<br />
<strong>of</strong> a breast cancer risk assessment model in women<br />
with a positive family history. Journal <strong>of</strong> the<br />
National <strong>Cancer</strong> Institute 1994;86:620-25.<br />
5. Alberta <strong>Cancer</strong> Board. Alberta cancer registry (2003).<br />
<strong>Cancer</strong> statistics<br />
6. Bryant HE, Brasher PMA. Risks and probabilities <strong>of</strong><br />
breast cancer: short term versus lifetime probabilities.<br />
CMAJ 1994;150(2):211-216.<br />
7. Alberta <strong>Cancer</strong> Board. A Snapshot <strong>of</strong> <strong>Cancer</strong> in<br />
Alberta. 1996.<br />
8. Women’s Health Initiative. NIH Publication No.<br />
02-5200 October 2002.<br />
9. Tabar L, Faberberg G, Day N, et al. What is the<br />
optimum interval between mammographic screening<br />
examinations? An analysis based on the latest results<br />
<strong>of</strong> the Swedish two-county breast cancer screening<br />
trial. International Journal <strong>of</strong> <strong>Cancer</strong>, 1987; 55: 547-<br />
551.<br />
10. Smart C, Hendrick R, Rutledge J, Smith R. Benefit<br />
<strong>of</strong> mammography screening in women ages 40 to 49.<br />
Current evidence from randomized controlled trials.<br />
<strong>Cancer</strong>, April 1995; 75(7): 1619-1626.<br />
11. American <strong>Cancer</strong> Society. Workshop on <strong>Guideline</strong>s<br />
<strong>for</strong> <strong>Breast</strong> <strong>Cancer</strong> <strong>Detection</strong>. Chicago, March 1998.
12. Kerlikowske K, Grady D, Barclay J, et al. Effect<br />
<strong>of</strong> age, breast density, and family history on the<br />
sensitivity <strong>of</strong> first screening mammography. JAMA,<br />
July 1996; 276(1): 33-38.<br />
13. Feig S. Determination <strong>of</strong> mammographic screening<br />
intervals with surrogate measures <strong>for</strong> women aged<br />
40-49 years. Radiology, 1994; 193: 311-314.<br />
14. Duffy S, Chen H, Tabar L, et al. Sojourn time,<br />
sensitivity and positive predictive value <strong>of</strong><br />
mammography screening <strong>for</strong> breast cancer in<br />
women aged 40-49. International Journal <strong>of</strong><br />
Epidemiology, 1996; 25(8): 1139-1145.<br />
15 Tabar L, Fagerberg G, Chen H, et al. Tumour<br />
development histology and grade <strong>of</strong> breast cancers:<br />
prognosis and progression. International Journal <strong>of</strong><br />
<strong>Cancer</strong>, 1996; 66: 413-419.<br />
16. Kopans D, Halpern E, Hulka C. Statistical power<br />
in breast cancer screening trials and mortality<br />
reduction among women 40-49 years with particular<br />
emphasis on the national <strong>Breast</strong> Screening Study <strong>of</strong><br />
Canada. <strong>Cancer</strong> 1994; 74: 1196-1203.<br />
17. Mettler F, Upton A, Kelsey C, et al. Benefits versus<br />
risks from mammography: a critical reassessment.<br />
<strong>Cancer</strong>, March 1996; 77(5): 903-909.<br />
18. NIH Consensus Statement. <strong>Breast</strong> <strong>Cancer</strong> Screening<br />
<strong>of</strong> Women Ages 40-49. January 1997; 15(1).<br />
19. Dodd GD. Screening <strong>for</strong> <strong>Breast</strong> <strong>Cancer</strong>. CANCER<br />
SUPPLEMENT. August 1, 1993; 72(3):1038-1042<br />
20. Maxwell CJ, Parboosingh J, Kozak JF,<br />
Desjardins-Denault SD. Factors Important in<br />
Promoting Mammography Screening among<br />
Canadian Women. Canadian Journal <strong>of</strong> Public<br />
Health,Sept 1997; 88(5):346-350.<br />
21. Gentleman JF, Lee J. Who Doesn’t get a<br />
Mammogram? Statistics Canada, Catalogue<br />
82-003-XPB, Health Reports, Summer 1997. Vol.9,<br />
No.1<br />
22. Bates B. A Guide to Physical Examination and History<br />
Taking. (pp317-328) 4th Edition, 1987 J.B. Lippincott<br />
Company, Philadelphia.<br />
<strong>Toward</strong> Optimized Practice (TOP)<br />
Program<br />
Arising out <strong>of</strong> the 2003 Master Agreement, TOP succeeds<br />
the <strong>for</strong>mer Alberta Clinical Practice <strong>Guideline</strong>s program, and<br />
maintains and distributes Alberta CPGs. TOP is a health quality<br />
improvement initiative that fits within the broader health system<br />
focus on quality and complements other strategies such as Primary<br />
Care Initiative and the Physician Office System Program.<br />
<strong>The</strong> TOP program supports physician practices, and the teams<br />
they work with, by fostering the use <strong>of</strong> evidence-based best<br />
practices and quality initiatives in medical care in Alberta. <strong>The</strong><br />
program <strong>of</strong>fers a variety <strong>of</strong> tools and out-reach services to help<br />
physicians and their colleagues meet the challenge <strong>of</strong> keeping<br />
practices current in an environment <strong>of</strong> continually emerging<br />
evidence.<br />
TO PROVIDE FEEDBACK<br />
<strong>The</strong> <strong>Early</strong> <strong>Detection</strong> <strong>of</strong> <strong>Breast</strong> <strong>Cancer</strong> Working Group is a multidisciplinary<br />
team composed <strong>of</strong> a family physician, general practitioners,<br />
radiologists, general surgeons, a gynecologist, oncologist,<br />
pathologist, epidemiologist, Medical Officer <strong>of</strong> Health, nurse,<br />
medical student, public representatives, the Canadian <strong>Cancer</strong><br />
Society, and <strong>Breast</strong> <strong>Cancer</strong> Policy Council representatives.<br />
<strong>The</strong> Working Group encourages your feedback. If you need further<br />
in<strong>for</strong>mation or if you have difficulty applying this guideline,<br />
please contact:<br />
Clinical Practice <strong>Guideline</strong>s Manager<br />
TOP Program<br />
12230 - 106 Avenue NW<br />
Edmonton AB T5N 3Z1<br />
Phone: 780.482.0319<br />
or toll free 1.866.505.3302<br />
Fax: 780.482.5445<br />
Email: cpg@topalbertadoctors.org<br />
Website: www.topalbertadoctors.org<br />
<strong>Early</strong> <strong>Detection</strong> <strong>of</strong> <strong>Breast</strong> <strong>Cancer</strong> - April 1999<br />
Reviewed - August 2000<br />
Reviewed - March 2002<br />
Reviewed - November 2004
APPENDIX 1: CANCER GENETICS CLINICS<br />
CANCER GENETICS CLINIC<br />
Contact In<strong>for</strong>mation<br />
Cross <strong>Cancer</strong> Institute and Edmonton/Calgary Genetics Clinics.<br />
By Mail:<br />
Edmonton Genetics Clinic<br />
Clinical Sciences Building B-139<br />
University <strong>of</strong> Alberta<br />
Edmonton, Alberta T6G 2B7<br />
By Telephone:<br />
Cross <strong>Cancer</strong> Institute (780) 432-8422<br />
Edmonton Genetics Clinic (780) 407-7333<br />
<strong>Cancer</strong> Genetics Research Clinic (403) 670-2438<br />
<strong>Cancer</strong> Genetics Research Clinic<br />
Tom Baker <strong>Cancer</strong> Centre<br />
1331-29th Street NW<br />
Calgary, Alberta T2N 4N2<br />
Note: Referrals MUST be made by a physician and are preferred by mail. Appointments will be made with<br />
patient(s) after initial work up completed.<br />
Referral Criteria<br />
<strong>The</strong> following are <strong>of</strong>fered as considerations <strong>for</strong> selecting women who may benefit from genetic counselling. <strong>The</strong><br />
criteria do not necessarily define women at increased risk <strong>of</strong> developing breast carcinoma who merit earlier or<br />
more frequent mammographic screening.<br />
• Personal or close family history <strong>of</strong> breast cancer < 35 years; ovarian cancer < 50 years; bilateral breast cancer<br />
- first onset < 50 years; or breast and ovarian cancer<br />
• Two related family members with breast cancer and/or ovarian cancer with onset in both < 50 years<br />
• Three or more related family members with breast and/or ovarian cancer, one onset < 50 years<br />
• Four or more related family members with breast and/or ovarian cancer, any age<br />
• Ashkenazi descent, breast and/or ovarian cancer, any age<br />
• Any case <strong>of</strong> male breast cancer<br />
• Known mutation in a cancer susceptibility gene such as the BRCA1 or BRCA2 gene is present in a family<br />
member<br />
• Families which may not meet the above criteria, but have a strong family history suggestive <strong>of</strong> the presence <strong>of</strong><br />
a mutated cancer susceptibility gene
APPENDIX 2: CLINICAL BREAST EXAMINATION<br />
Clinical breast examination (CBE) may detect some breast cancers which are not evident on mammography. However, the<br />
effectiveness <strong>of</strong> CBE depends upon systematic examination <strong>of</strong> all quadrants <strong>of</strong> both breasts and all regional lymph nodes. One<br />
systematic approach is illustrated below. 22<br />
Region<br />
Examined<br />
BREASTS<br />
AXILLAE<br />
AXILLARY LYMPH<br />
NODES<br />
INFRACLAVICULAR<br />
LYMPH NODES<br />
Examination<br />
Skills and Focus<br />
Inspection<br />
BREAST, AREOLA, NIPPLE<br />
Inspection<br />
AXILLAE<br />
Palpation<br />
CENTRAL,<br />
PECTORAL,<br />
SUBSCAPULAR,<br />
LATERAL LYMPH NODES<br />
Palpation<br />
INFRACLAVICULAR<br />
Procedures and Techniques<br />
Client in SITTING position disrobed to waist. Inspect breast, areola and<br />
nipple bilaterally from anterior and lateral view:<br />
1. With arms at side<br />
2. With arms raised over head<br />
3. With hands pressed against hips<br />
or<br />
With hands squeezed together at shoulder level<br />
4. DO ONLY IF breasts are pendulous or very large: inspect with<br />
client leaning <strong>for</strong>ward.<br />
Inspects skin <strong>of</strong> axillae with arms raised over head<br />
Supports client’s “L” hand and wrist with “L” hand to examine “L”<br />
axilla and reverses <strong>for</strong> “R” axilla. Cup fingers together. Reaches as<br />
high as possible into axilla<br />
1. Brings fingers down over ribs and feels <strong>for</strong> CENTRAL nodes<br />
2. Feels inside anterior axillary folds (PECTORAL)<br />
3. Feels inside posterior axillary folds (SUBSCAPULAR)<br />
4. Feels against humerus (LATERAL)<br />
Palpates bilaterally <strong>for</strong> INFRACLAVICULAR nodes in 1st interspace<br />
with finger pads<br />
SUPRACLAVICULAR<br />
LYMPH NODES<br />
BREASTS<br />
Palpation<br />
SUPRACLAVICULAR<br />
Inspection<br />
BREAST, AREOLA,<br />
NIPPLE (same as above)<br />
Palpation<br />
BREAST, AREOLA,<br />
NIPPLE and<br />
TAIL OF SPENCE<br />
Palpates bilaterally <strong>for</strong> SUPRACLAVICULAR nodes above clavicle<br />
with finger pads<br />
Client SUPINE, with pillow removed from under head. Uses small<br />
pillow under client’s shoulder on side examined to shift breasts medially<br />
(NO PILLOW IF BREASTS ARE SMALL)<br />
1. Inspects breasts.<br />
Palpates each breast:<br />
1. Asks client to move arm away from chest on side being examined<br />
2. Uses flat <strong>of</strong> 4 fingers, in a rotary motion to compress breast tissue<br />
3. Flexes, from the wrist, not the fingers<br />
4. Applies moderate pressure, keeping constant contact with skin<br />
5. Moves back and <strong>for</strong>th across breast in straight lines, making<br />
constant small circles<br />
6. Slides hand down 1 finger width <strong>for</strong> each pass<br />
7. Covers full area from below clavicle to 3 cm below breast from<br />
anterior axillary line to midsternal line:<br />
a) glandular tissue c) nipple<br />
b) areolar area d) Tail <strong>of</strong> Spence<br />
Adopted and reproduced with permission from: Skillen DL & Day R. (Eds). 1998. A syllabus <strong>for</strong> adult health assessment (pp.61-62). Edmonton: University <strong>of</strong><br />
Alberta, Faculty <strong>of</strong> Nursing.