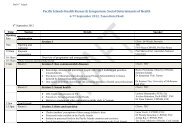
Human Resources for Health in Maternal, Neonatal and - HRH ...
Human Resources for Health in Maternal, Neonatal and - HRH ...
Human Resources for Health in Maternal, Neonatal and - HRH ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
flexibility <strong>in</strong> order to overcome gender equity, establish <strong>and</strong> ma<strong>in</strong>ta<strong>in</strong> st<strong>and</strong>ards of good<br />
practice. (UNFPA 2006)<br />
An exam<strong>in</strong>ation of country experiences of scal<strong>in</strong>g up SBAs can provide <strong>in</strong>sight <strong>in</strong>to the<br />
rational <strong>for</strong> scal<strong>in</strong>g up at community level <strong>and</strong> the approach. These experiences <strong>in</strong>clude the<br />
expansion of the Community Midwifery programme <strong>in</strong> Kenya <strong>in</strong>volv<strong>in</strong>g the scal<strong>in</strong>g-up of<br />
home-based maternal <strong>and</strong> postnatal Care, <strong>in</strong>clud<strong>in</strong>g family plann<strong>in</strong>g, (Mwangi 2008) <strong>and</strong> the<br />
Indonesian experience of scal<strong>in</strong>g up the village midwifery programme.<br />
Scal<strong>in</strong>g up the village midwifery program <strong>in</strong> Indonesia<br />
Follow<strong>in</strong>g the International Nairobi conference <strong>in</strong> 1987, at which governments pledged to<br />
reduce maternal mortality by half by 2000, the Indonesian government launched the Village<br />
Midwifery Program. This was <strong>in</strong> response to maternal mortality of over 400 per 100 000 live<br />
births <strong>and</strong> neonatal mortality of 32 per 1000 live births. The aim was to place a SBA <strong>in</strong> every<br />
village to provide MNRH care <strong>and</strong> services. Three years later <strong>in</strong> 1993, 60,000 community<br />
midwives had been deployed <strong>and</strong> about 20,000 maternity huts had been established with<br />
community participation (Utomo 2008). Midwife density <strong>in</strong>creased from 0.2 to 2.6 per 10<br />
000 people between 1986 <strong>and</strong> 1996 (Shankar, Sebayang et al. 2008).<br />
Twenty years after its <strong>in</strong>ception, progress towards reduc<strong>in</strong>g MMR <strong>and</strong> NMR has been made<br />
but it was not as large as expected. MMR <strong>in</strong> 2003 was 307 per 100 000 live births <strong>and</strong> the<br />
neonatal mortality ratio was 20 per 1000 live births. Despite its success <strong>in</strong> <strong>in</strong>creas<strong>in</strong>g density<br />
of SBA <strong>and</strong> reduc<strong>in</strong>g socioeconomic <strong>in</strong>equalities <strong>in</strong> professional attendance at birth, the focus<br />
on outreach services has meant that the poor particularly those <strong>in</strong> rural <strong>and</strong> remote areas<br />
experienced <strong>in</strong>creas<strong>in</strong>g difficulties <strong>in</strong> access<strong>in</strong>g emergency obstetric care <strong>in</strong> hospitals (Hatt,<br />
Stanton et al. 2007). This is probably the result of lack of responsive referral systems (e.g.,<br />
transport), low cultural acceptability <strong>and</strong> the high out-of-pocket cost of emergency obstetric<br />
care (EmOC) services (Ronsmans, Endang et al. 2001). Despite the calculation that the ratio<br />
of village midwife per 2389 population would translate to roughly one midwife per 54 births<br />
per year (Hatt, Stanton et al. 2007) evaluations showed that midwives‘ obstetric workload<br />
was generally low as a result of the home based delivery system. This was affected by<br />
competition with TBAs <strong>and</strong> the wide geographic spread of households. As a result, midwives<br />
were not constantly us<strong>in</strong>g <strong>and</strong> improv<strong>in</strong>g their cl<strong>in</strong>ical skills. Midwives‘ case management<br />
skills were also generally sub-st<strong>and</strong>ard due to the rapid nature of the program <strong>and</strong> low quality<br />
pre-service tra<strong>in</strong><strong>in</strong>g (Utomo 2008). Supervision <strong>and</strong> mentor<strong>in</strong>g of midwives was not adequate<br />
<strong>and</strong> their varied duties <strong>and</strong> often vague job descriptions also meant that many midwives<br />
worked <strong>in</strong> isolation with few opportunities <strong>for</strong> job support or learn<strong>in</strong>g. This had a strong<br />
impact on retention (Shankar, Sebayang et al. 2008).<br />
P a g e | 152