DO - Ohio University College of Osteopathic Medicine
DO - Ohio University College of Osteopathic Medicine
DO - Ohio University College of Osteopathic Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
perspectives from<br />
<strong>DO</strong><br />
the college <strong>of</strong> osteopathic medicine<br />
TODAY’S<br />
summer/fall 2 0 0 7<br />
ohio university<br />
Our Alumni
Second-year student<br />
Kristen Conrad is the<br />
“Hamburgler” during<br />
the annual OU-COM<br />
Talent Follies.
<strong>DO</strong><br />
the college <strong>of</strong> osteopathic medicine<br />
TODAY’S<br />
perspectives from<br />
<strong>DO</strong><br />
TODAY’S<br />
F e a t u r e s<br />
12<br />
14<br />
18<br />
20<br />
A Family Physician takes an<br />
Alternative Path<br />
Out in “Custer Country,” Cmdr. George<br />
Ceremuga, D.O. (’93), provides health<br />
care to Native Americans on the Northern<br />
Cheyenne Reservation.<br />
Melting Pot <strong>Medicine</strong><br />
A new intercultural communications seminar<br />
at OU-COM fosters cultural competency in<br />
future physicians.<br />
Global Health<br />
By participating in international programs,<br />
students become aware <strong>of</strong> cultural differences<br />
and learn how to interact with patients from<br />
diverse backgrounds.<br />
The Long Road Back<br />
Injured when his humvee was hit by an<br />
improvised explosive device, Capt. Larry<br />
Robinson, D.O. (’02), describes his experience<br />
in Iraq.<br />
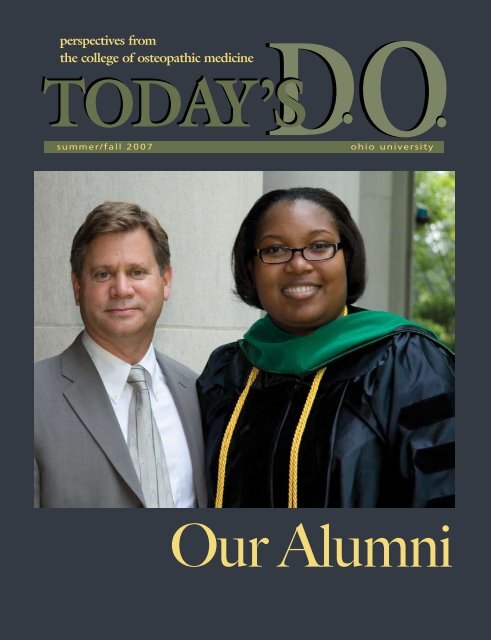
On the cover…<br />
Incoming Society <strong>of</strong> Alumni and<br />
Friends President Jeffrey A.<br />
Stanley, D.O. (’82), congratulates<br />
Kerwyn Flowers, D.O. (’07), after<br />
OU-COM’s 28th commencement<br />
exercises Saturday, June 2..pher:<br />
Christian Stork<br />
3 On Campus<br />
7 CORE News<br />
9 Commencement<br />
24 Research<br />
26 Alumni Note<br />
28 Alumni Board<br />
31 Alumni Events<br />
32 Class Notes<br />
36 Congratulations
<strong>DO</strong><br />
TODAY’S <strong>DO</strong><br />
volume 25.2<br />
Today’s D.O. is published two<br />
times a year by the Office <strong>of</strong><br />
Communication <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Editorial <strong>of</strong>fices:<br />
Room 330, Grosvenor Hall,<br />
<strong>Ohio</strong> <strong>University</strong>, Athens, <strong>Ohio</strong>, 45701.<br />
Editorial Board<br />
George Dunigan II<br />
Director <strong>of</strong> Governmental Affairs<br />
Ryan Palmer<br />
Student Government President<br />
Edwin Rowland, Ph.D.<br />
Chair, Department<br />
<strong>of</strong> Biomedical Sciences<br />
John Schriner, Ph.D.<br />
Director <strong>of</strong> Admissions<br />
Sharon Zimmerman<br />
Director <strong>of</strong> Medical Development<br />
Executive Diretor Alumni Affairs<br />
Content Editor<br />
Susan Green<br />
Copy Editor<br />
Shelby Mullins<br />
Design<br />
Marie Graham<br />
Kari Gunter-Seymour<br />
Photography<br />
Leonardo Carrizo<br />
Tim Creamer<br />
John Sattler<br />
Writers and Contributors<br />
Anita Martin<br />
Mary Reed<br />
Jared Rutecki<br />
Carla Saavedra-Santiago<br />
Tracey Thomas<br />
Andrew Tillotson<br />
Administration<br />
Roderick McDavis, Ph.D<br />
President, <strong>Ohio</strong> <strong>University</strong><br />
A New <strong>Osteopathic</strong> Oath<br />
Recently, the <strong>Ohio</strong> Board <strong>of</strong> Regents commissioned the<br />
Robert Graham Center to perform a physician workload<br />
analysis for <strong>Ohio</strong>. The report showed that approximately 62<br />
percent <strong>of</strong> OU-COM graduates practice in <strong>Ohio</strong>—by far the<br />
most successful medical school in the state. This compares to<br />
42 percent <strong>of</strong> all the <strong>Ohio</strong> medical schools combined. It also<br />
showed that D.O.s are more likely to practice in underserved<br />
areas <strong>of</strong> the state.<br />
What explains these findings? While there are a number <strong>of</strong> factors,<br />
I believe the primary reason for our success is the CORE<br />
training hospital consortium. The seventeen institutions that<br />
make up the CORE provide exceptional training to students<br />
who enjoy a different atmosphere from most medical schools.<br />
Our clinical faculty teach because they enjoy it, and CORE<br />
staff develop personal relationships with our students. Our clinical faculty live the osteopathic<br />
physician’s oath they took when they graduated:<br />
“To my college I will be loyal and strive always for its best interests and for the interests<br />
<strong>of</strong> the students who will come after me.”<br />
Now the <strong>Ohio</strong> CORE is embarking on a new and broader mission. By 2020, it is estimated<br />
that there will be more than 95,000 active osteopathic physicians. That will be 79 percent<br />
higher than today. Recognizing the deficiency in postgraduate positions required to<br />
accommodate the large increase in graduates, the AOA has appealed to the pr<strong>of</strong>ession to<br />
establish new postgraduate training programs. A large part <strong>of</strong> this responsibility will<br />
rest on the shoulders <strong>of</strong> the osteopathic colleges, particularly those in states with high<br />
concentrations <strong>of</strong> D.O.s, such as <strong>Ohio</strong>. The <strong>Ohio</strong> CORE is rising to the task.<br />
Medical centers all over <strong>Ohio</strong> are interested in establishing new osteopathic GME<br />
programs. CORE hospitals have put aside their individual interests to support the<br />
pr<strong>of</strong>ession’s rapidly developing need for additional outstanding GME programs. It is<br />
exciting to watch the CORE grow in size, stature and quality. No wonder so many<br />
OU-COM students elect to stay in <strong>Ohio</strong>. As the premiere postgraduate training<br />
institution in the United States, the CORE provides osteopathic physicians an<br />
unparalleled environment in which to train and practice. The CORE hospitals have<br />
clearly adopted a variant to the osteopathic oath:<br />
“To our pr<strong>of</strong>ession we will be loyal and strive always for its best interests.”<br />
I couldn’t be prouder <strong>of</strong> them.<br />
Dean’s Message<br />
John Brose, D.O.<br />
Dean, <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Karoline Lane<br />
Director, Office <strong>of</strong> Communication<br />
Opinions expressed in Today’s D.O. are<br />
those <strong>of</strong> the authors and<br />
do not necessarily reflect<br />
viewpoints <strong>of</strong> the editors or <strong>of</strong>ficial<br />
policy <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Jack Brose, D.O.<br />
Dean, <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> <strong>Medicine</strong><br />
© ’07 <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Address updates for Today’s D.O.<br />
should be referred to Sheila Byc<strong>of</strong>ski<br />
OU-COM, 332 Grosvenor Hall<br />
Athens, OH 45701<br />
phone: (740) 593-2346<br />
e-mail: byc<strong>of</strong>ski@ohio.edu<br />
www.oucom.ohio.edu<br />
2<br />
oucom.ohio. www.<br />
edu
On Campus<br />
“…a gem in the neediest setting”<br />
This is how Joe Hallet, a senior editor at The Columbus Dispatch,<br />
described OU-COM in an editorial he wrote after a campus visit in<br />
February. In the photo below right, John Schriner, Ph.D., director<br />
<strong>of</strong> admissions, points out OU-COM’s Parks Hall clinic to Hallet during<br />
a campus tour. Hallet lived in Parks Hall as an <strong>Ohio</strong> <strong>University</strong> student<br />
more than 35 years ago<br />
In his editorial, Hallet wrote about the tough funding situation in<br />
<strong>Ohio</strong> for higher education and the reality that every college “soon may<br />
have to prove its worth to obtain state funding. That challenge is not<br />
feared by Dr. Jack Brose … His medical school is attracting the best<br />
and the brightest – 3,200 applicants for 100 first-year slots in 2006<br />
– in the state’s poorest and medically neediest region.”<br />
Thanks to Dean Jack Brose, D.O., and college advocacy efforts,<br />
government constituents are getting the same message that 54 percent<br />
<strong>of</strong> OU-COM alumni practice in primary care fields, and more than 60<br />
percent remain in <strong>Ohio</strong>, where they are more likely to practice in rural<br />
and other physician-shortage areas.<br />
<strong>Ohio</strong> Governor Ted Strickland, Representative Jimmy Stewart, OHIO<br />
President Roderick McDavis and Eric Fingerhut, chancellor <strong>of</strong> the <strong>Ohio</strong><br />
Board <strong>of</strong> Regents, toured campus in April, where they spoke to Dean<br />
Brose aboard OU-COM’s<br />
mobile health clinic, top and<br />
above right.<br />
State Senator Steve Stivers,<br />
and his brother Alan, also<br />
visited the college this spring.<br />
Here, left, they look at<br />
plasticized models with<br />
Dean Brose in the anatomy<br />
lab. Stivers is vice chair <strong>of</strong> the<br />
Senate’s Finance and Financial<br />
Institutions committee.<br />
-Karoline Lane<br />
summer/fall 2007 3
Rodeo roundup<br />
Karen Montgomery-Reagan, D.O.,<br />
assistant pr<strong>of</strong>essor <strong>of</strong> pediatrics,<br />
above, has fun with bubblemaking<br />
during the 5 th annual<br />
Bike Rodeo held at the Athens<br />
Community Center.<br />
James Schulz, an emergency<br />
nurse at O’Bleness Hospital,<br />
right, teaches Lander Zook, age<br />
9, left, how to handle his bike<br />
on rough terrain. Each year, the<br />
Bike Rodeo, which aims to teach<br />
young children about bicycle<br />
safety and helmet use, donates<br />
up to 200 helmets to local children<br />
and raffles <strong>of</strong>f one bicycle.<br />
About 20 OU-COM students and<br />
faculty volunteered alongside<br />
community members at this<br />
year’s event.<br />
-Carla Saavedra-Santiago<br />
4 www.oucom.ohio.edu
Go!<br />
Nearly 90 people participated in the annual 5k <strong>Medicine</strong> Run despite the cold, cloudy weather. A health fair,<br />
which provided free screenings for blood pressure, glucose and cholesterol, and a children’s obstacle course<br />
were part <strong>of</strong> the event as well. Booths were also available to educate people on a variety <strong>of</strong> health conditions.<br />
Close to 50 students volunteered their time throughout the year to make it all happen, noted second-year<br />
student Nicole Veitinger, who chaired the events. “Knowing we are giving so much back to the clinic as a<br />
result <strong>of</strong> our hard work is all the reward I need,” she said. The <strong>Medicine</strong> Run raised $2,000 for the Free Clinic,<br />
an amount that exceeds last year’s record donation <strong>of</strong> $1,350.<br />
-Andrew Tillotson<br />
OU-COM “Today”<br />
Jacqueline Wolf, Ph.D., associate<br />
pr<strong>of</strong>essor <strong>of</strong> social medicine, far left,<br />
appeared on NBC’s “Today,” April 26,<br />
to discuss pr<strong>of</strong>essional and informal<br />
wet nursing. Wolf, a nationally<br />
recognized expert in the history <strong>of</strong><br />
breastfeeding, is the author <strong>of</strong> Don’t<br />
Kill Your Baby: Public Health and the<br />
Decline <strong>of</strong> Breastfeeding in the 19 th<br />
and 20 th Centuries.<br />
Sinn to serve on national board<br />
Second-year student Clarice Sinn, right, was recently selected to serve on the<br />
national board <strong>of</strong> the Student <strong>Osteopathic</strong> Medical Association (SOMA) as the<br />
organization’s “preventative medicine” director. She was “preventative medicine”<br />
and public relations chair in SOMA’s OU-COM chapter last quarter.<br />
In her new position, Sinn will develop programs at osteopathic medical schools<br />
nationwide and collaborate with local coordinators to identify problems in<br />
specific regional populations. Her duties include developing relationships with<br />
national medical organizations like the American Lung Association and working<br />
with other members <strong>of</strong> the national board to develop the SOMA Fall<br />
Convention National Philanthropic Project in San Diego.<br />
This fall, Sinn begins her third year-clerkship at St. Vincent Mercy Medical<br />
Center in Toledo.<br />
-Jared Rutecki<br />
summer/fall 2007 5
Grant to benefit<br />
area children<br />
Young children and<br />
their families living in<br />
Appalachian <strong>Ohio</strong> will<br />
have greater access to<br />
health care thanks to<br />
a federal grant that<br />
will fund an innovative<br />
community-university<br />
partnership. The federal<br />
Health Resources and<br />
Services Administration<br />
has awarded a threeyear,<br />
$540,000 grant<br />
to <strong>Ohio</strong> <strong>University</strong> to<br />
support Interpr<strong>of</strong>essional Partners for Appalachian<br />
Children.<br />
“We are a community-university partnership with<br />
participants who are lay consumers trying to improve<br />
our community’s ability to identify, to refer and to<br />
provide comprehensive, coordinated care to young<br />
children with behavioral and developmental concerns,”<br />
says Jane Hamel-Lambert, Ph.D., director <strong>of</strong><br />
interdisciplinary mental health education in the<br />
Department <strong>of</strong> Family <strong>Medicine</strong> and principal<br />
investigator <strong>of</strong> the program.<br />
-Mary Reed<br />
Rewarding community service<br />
Sarah McGrew, B.S.N., received the Outstanding<br />
Arthritis Educator Award from the <strong>Ohio</strong> Rheumatic<br />
Diseases Coalition for her participation in arthritisrelated<br />
initiatives in the Appalachian region. For<br />
several years she has helped the <strong>Ohio</strong> Department<br />
<strong>of</strong> Health with teaching the Arthritis Foundation’s<br />
six-week, self-help program in several Southeastern<br />
<strong>Ohio</strong> communities. She is also a charter member <strong>of</strong><br />
the <strong>Ohio</strong> Rheumatic Diseases Coalition. McGrew,<br />
coordinator <strong>of</strong> clinical and community experiences at<br />
OU-COM, is the first person to receive the award.<br />
-Carla Saavedra-Santiago<br />
A winning proposal<br />
Earlier this year, the <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> received a Canon REALiS Sx6<br />
projector from Campus Technology magazine. The publication asked educators interested<br />
in bringing ultra-high-level projection capability into their classrooms to submit proposals<br />
to the magazine for an opportunity to win a projector.<br />
Out <strong>of</strong> 149 entries, OU-COM was among the four schools chosen to receive a top-<strong>of</strong>the-<br />
line video projector with a price tag <strong>of</strong> $5,999. Allen Reed’s winning proposal<br />
detailed how the projector would enable the college to deliver content in a new way<br />
in the Grosvenor 128 microbiology lab. The new equipment was installed at the end<br />
<strong>of</strong> January, replacing dated monitors, and has been in use since then.<br />
As part <strong>of</strong> an ongoing project, the magazine is studying the real-life usage <strong>of</strong> the<br />
projectors and will share with their readers the innovative ways educators and students<br />
are using the latest “smart classroom” equipment.<br />
This spring, Reed reported on the projector’s usage. Please visit campustechnology.<br />
com/articles/48230/ to read how the projector is making a difference in teaching and<br />
learning at OU-COM.<br />
6 www.oucom.ohio.edu
C O R E N e w s<br />
Whether working with students<br />
or members <strong>of</strong> the community,<br />
Nicholas Espinoza, D.O., is dedicated to<br />
making a difference By Anita Martin<br />
As a new assistant dean in the CORE, Nicholas Espinoza, D.O. (’90), coordinates third- and<br />
fourth-year clinical experiences for students at St. Vincent Mercy Medical Center in<br />
Toledo, <strong>Ohio</strong>.<br />
Espinoza’s got a knack for forging connections, whether between students and doctors,<br />
community members or among cultural groups. For years, he served Adelante, Inc.,<br />
a not-for pr<strong>of</strong>it resource center providing the Hispanic community in Northwest <strong>Ohio</strong><br />
with mental health services, support for victims <strong>of</strong> domestic violence and substance<br />
abuse prevention and intervention.<br />
“I served as a board member, assisting the development for programs to help people with<br />
substance abuse problems, which ranged from tobacco to crack cocaine,” he says.<br />
When he wasn’t practicing family, occupational or urgent medicine—or facilitating<br />
migrant health care—Espinoza has also moonlighted as a ringside physician for the<br />
Toledo Golden Gloves boxing club.<br />
These days, he’s focusing more on his private practice in Perrysburg, <strong>Ohio</strong>. But he<br />
still makes time to work around the greater Toledo area—Oakmont Medical Hospital,<br />
Bay Park Community Hospital, St. Charles Mercy Medical Hospital and St. Anne’s<br />
Hospital, where he has courtesy privileges.<br />
<strong>Ohio</strong> Occupational Health also employs Espinoza to help manage the return <strong>of</strong> plant<br />
workers who have sustained work-related injuries. And some weekends he provides<br />
urgent care at the Blanchart Valley Hospital.<br />
“I think that’s about enough,” he laughs.<br />
But even with all <strong>of</strong> his commitments, he still makes time to connect daily with third- and<br />
fourth-year medical students at the hospital. Espinoza began working with students<br />
as a CORE medical equity teacher with Harold C. Thompson III, D.O., to oversee<br />
and advise them, if necessary, on multicultural issues pertaining to their internships<br />
and residencies.<br />
And now as an assistant CORE dean, Espinoza supervises about 35 students, interns<br />
and residents from OU-COM and other participating colleges in <strong>Ohio</strong> and surrounding<br />
states.<br />
“I’ve always enjoyed working directly with students,” says Espinoza, who fondly remembers<br />
his own time spent as a student at <strong>Ohio</strong> <strong>University</strong>.<br />
Espinoza’s talent for making connections extends to his private practice, too. His group<br />
practice makes use <strong>of</strong> hospitalist internal medicine specialists (Intermed) to care for<br />
acutely ill patients who need in-hospital medical care.<br />
“Our Intermed colleagues, Drs. J. Retholz, Sheldon, Cifuentes, Orlo, Hooker, Blood<br />
and M. Retholz—all D.O.s—work great with us, our patient families and continually<br />
support the CORE teaching activities <strong>of</strong> the students, interns and residents,” Espinoza<br />
says. “Many <strong>of</strong> the Intermed physicians themselves trained right here at this CORE site<br />
and have chosen to stay here and practice. We are very fortunate for that.”<br />
Occasionally Espinoza returns to Athens to talk with students, and he fondly recalls the<br />
euphoria <strong>of</strong> spring. “I remember how nice it felt when the weather warmed up and the<br />
trees started to bloom,” he says.<br />
Espinoza interned at Parkview Hospital, and received board certification in family medicine<br />
in 1999. He and his wife, Carole, have two daughters, Valerie and Jacqueline.<br />
summer/fall 2007 7
Seven alumni named<br />
Master Faculty<br />
Honorees received a plaque and a gold lapel pin<br />
–lapel pin enlarged for detail<br />
Seven alumni are among the 28 physicians named a Master<br />
Faculty by <strong>Ohio</strong> Universty Co llege <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong>: Jeffrey Garman, D.O. (’84), Firlands<br />
Regional Medical Center; Joni Koren, D.O.<br />
(’84), Grandview Medical Center; Leonard<br />
Tamburro, D.O. (’85), Affinity Medical<br />
Center; Thomas Wehmann, D.O. (‘85),<br />
Cuyahoga Falls General Hospital;<br />
Roger Wohlwend, D.O. (’87), St.<br />
Vincent Mercy Medical Center;<br />
John Wolf III, D.O. (’88), St.<br />
John West Shore Hospital and<br />
John Yuhas, D.O. (’87), Firelands<br />
Regional Medical Center.<br />
The appointment <strong>of</strong> Master<br />
Faculty is the highest honor<br />
that the college gives to clinical<br />
faculty members at its Center<br />
for <strong>Osteopathic</strong> Research and<br />
Education (CORE), a statewide<br />
consortium <strong>of</strong> 15 hospitals<br />
across <strong>Ohio</strong>.<br />
“The award is truly an honor to<br />
receive,” Koren says. “Many times<br />
those <strong>of</strong> us who take students into our<br />
<strong>of</strong>fices wonder if we are appreciated, and it’s<br />
very encouraging to see that we are.<br />
“I’m thankful to be rewarded and recognized for<br />
teaching the students,” she adds. “It’s something I’ve<br />
always been passionate about and hope to continue<br />
doing for many years.”<br />
Master Faculty are chosen from hundreds <strong>of</strong> nominations and<br />
awarded once every four years. The college recognizes the doctors as innovators and leaders in clinical education<br />
and the osteopathic pr<strong>of</strong>ession. They have excelled as teachers and mentors. Medical students, interns and residents<br />
respect and esteem Master Faculty members for their contributions to undergraduate and graduate medical<br />
education, as well as for being outstanding role models.<br />
“One <strong>of</strong> the greatest parts <strong>of</strong> my job is recognizing my colleagues who have played such an important role in<br />
preparing our students, interns and residents to become caring, compassionate and competent physicians,” says<br />
Dean Jack Brose, D.O.<br />
For a complete list <strong>of</strong> Master Faculty, visit www.oucom.ohiou.edu/MasterFaculty.<br />
8 www.oucom.ohio.edu
Congratulations, you’re a D.O.<br />
Jubilation, hugs, pride and family were in abundance<br />
during the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong>’s 28th commencement exercises Saturday<br />
morning, June 2, in Templeton-Blackburn Alumni<br />
Memorial Auditorium.<br />
President Roderick McDavis, Ph.D., hailed the college<br />
as “ … an outstanding example <strong>of</strong> our larger university<br />
mission … ” and congratulated the student doctors<br />
on the significant role they’ve played in the health <strong>of</strong><br />
<strong>Ohio</strong>’s citizens.<br />
In addressing the 102 graduates—59 women and<br />
43 men—Dean Jack Brose, D.O., said, “You have<br />
exceeded my expectations. … In a short while, you will<br />
understand why this ceremony is such an emotional<br />
event. There is no more pr<strong>of</strong>ound moment that<br />
watching you come to the stage as a lay person, and<br />
leave as a physician. As dean, congratulating each <strong>of</strong><br />
you is my favorite part <strong>of</strong> the job. I can’t imagine a<br />
greater honor.”<br />
Keynote speaker Alison Clarey, D.O. (Hon. ’98),<br />
president <strong>of</strong> the American <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
Surgeons, left the newly minted physicians with two<br />
thoughts: Know no limitations, and one person can<br />
make a difference.<br />
summer/fall 2007 9
Kerwyn Flowers<br />
the ministry <strong>of</strong> medicine<br />
By Mary Reed<br />
Ministering to people has been at the root <strong>of</strong> Kerwyn Flowers’<br />
lifework—from her stint as a 12-year-old Sunday school teacher<br />
to a medical school tutor to a doctor <strong>of</strong> osteopathic medicine.<br />
“God gives us gifts,” says Flowers, who received her medical<br />
degree from the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong> June 2. “I think being a physician is a ministry<br />
within itself. Physicians are engaged in every aspect <strong>of</strong> their<br />
patients’ lives—they encourage, they counsel, they listen and<br />
so much more. In my opinion, physicians don’t heal, but rather,<br />
God gives us the opportunity and privilege to facilitate healing.”<br />
Even at a young age Flowers was resolved that her life’s work<br />
would focus on health and healing. The support <strong>of</strong> her<br />
mother, Sharon Smiley Gainous—the pastor <strong>of</strong> New Israel<br />
Church <strong>of</strong> Jesus Christ in Quincy, Florida—was a foundation for<br />
Flowers’ success in medical school. “My mother said you<br />
could be whatever you wanted to be. From the beginning she<br />
has always believed in me and supported me.” Flowers also<br />
observed her mother’s role as a teacher to the church<br />
congregation, and Flowers even dabbled in teaching Sunday<br />
school as a girl herself. It turns out that she was a natural<br />
teacher, a gift that would serve her well years later in<br />
medical school.<br />
After graduating with a degree in chemistry from Florida<br />
A&M <strong>University</strong>, Flowers worked as a chemist for<br />
GlaxoSmithKline and Lannett Pharmaceuticals. When she<br />
decided it was time to attend<br />
medical school, she needed more<br />
background in biological sciences.<br />
That’s when Flowers enrolled in<br />
the OU-COM Summer Scholars<br />
Program, a rigorous six-week<br />
medical school preparatory<br />
program for underrepresented<br />
minority students, and then the<br />
Post-Baccalaureate Program, a<br />
similar preparatory program that<br />
lasts one academic year.<br />
Flowers says she had never heard<br />
<strong>of</strong> osteopathic medicine prior to<br />
coming to OU-COM. But when<br />
a friend introduced her to the<br />
osteopathic principles <strong>of</strong> approaching<br />
the whole person, Flowers was<br />
sold. “The philosophy was so similar<br />
to what I had always believed<br />
about health and wellness.”<br />
After excelling in the Summer Scholars and Post-Baccalaureate<br />
programs, Flowers became a tutor and mentor for both.<br />
“Name it, I tutored it,” she says. She also became a mentor<br />
to first-year medical students as part <strong>of</strong> a program called<br />
COMrade. When she won COMrade <strong>of</strong> the Year in 2005,<br />
she was surprised—but she shouldn’t have been. “I tutored a<br />
lot <strong>of</strong> them,” she says, figuring that “all <strong>of</strong> the students who<br />
I tutored voted for me!” But in fact, she received even more<br />
votes than that.<br />
During that time, Flowers also served as president <strong>of</strong> the<br />
OU-COM Chapter <strong>of</strong> the Christian Medical and Dental<br />
Association. She organized a Bible study group every Wednesday<br />
night. “I tried to make sure the topics were relevant to people<br />
<strong>of</strong> our age group and (were) topics specific to physicians.”<br />
Now about to begin a residency in family medicine at Akron<br />
City Hospital, Flowers is embarking on yet a new ministry<br />
and believes that by becoming a physician, her destiny and<br />
purpose are fulfilled. She will bring her faith with her to every<br />
patient interaction. “I think faith gives us hope beyond<br />
our circumstances.”<br />
Flower‘s mother, left, and 25 members <strong>of</strong> her childhood church<br />
congregation from Quincy, Fla., were in Athens to see Flowers,<br />
center, receive her medical degree June 2.<br />
10 www.oucom.ohio.edu
Eric Greenfield<br />
all the right reasons<br />
By Mary Reed<br />
The ink is still drying on the <strong>Ohio</strong> <strong>University</strong> diploma that<br />
names Eric Greenfield a doctor <strong>of</strong> osteopathic medicine, but<br />
he has already made more house calls than most physicians will<br />
make in their entire careers. This is because prior to medical<br />
school, Greenfield was a paramedic for nine years – an experience<br />
that shaped his pr<strong>of</strong>essional trajectory as well as his philosophy<br />
as a practitioner and teacher <strong>of</strong> emergency medicine.<br />
“You get to make a big impact on people’s lives,” Greenfield<br />
says about his paramedic career. He remembers treating five<br />
cardiac arrest cases on five consecutive Christmas days.<br />
“When you’re in somebody’s house and you see somebody<br />
who’s collapsed literally in front <strong>of</strong> the Christmas tree, it<br />
gives you a perspective you can’t see anywhere else.”<br />
This in-home, pre-hospital assessment as a paramedic was<br />
the formative beginning to Greenfield’s medical career.<br />
He eventually earned a nursing degree through Regents<br />
<strong>College</strong>, and then went on to earn a bachelor’s degree in<br />
health sciences through Excelsior <strong>College</strong>. He was making<br />
a good living as a nurse when he became a part-time<br />
paramedic instructor at the <strong>University</strong> <strong>of</strong> Alabama, but he<br />
again changed careers to help establish a paramedic degree<br />
program at nearby Calhoun <strong>College</strong>. “It was the best job I<br />
ever had,” Greenfield recalls.<br />
Medical school had always been on his mind, however,<br />
and he eventually hit an educational ceiling as a nurse and<br />
a paramedic instructor. He knew it was time to pursue a<br />
medical degree, and he knew it would be at an osteopathic<br />
medical school.<br />
One <strong>of</strong> the things that drew Greenfield to OU-COM was<br />
the patient-centered continuum program, a student-directed<br />
curriculum where small groups <strong>of</strong> medical students are presented<br />
with patient cases, and they come up with their own learning<br />
objectives. “It was good for me because <strong>of</strong> my nontraditional<br />
background,” Greenfield says. Describing a typical PCC<br />
discussion, he says, “We might have a patient with a cough<br />
or pneumonia. We’d start talking about the differential<br />
diagnosis <strong>of</strong> a cough … a microbiologist in a previous life<br />
might say, ‘These are the typical bugs we see.’ My contribution<br />
is typically, ‘This is what you see in real patients, this is what<br />
you look for.’”<br />
Now Greenfield interacts with patients from the perspective<br />
<strong>of</strong> a resident physician—he’s starting an emergency medicine<br />
Eric Greenfield, left, and his mentor, Henry Gaillard, M.D.<br />
residency at the Medical <strong>College</strong> <strong>of</strong> Georgia. “I didn’t really<br />
want to do emergency medicine when I started medical school,”<br />
he says. “I wanted to do a little bit <strong>of</strong> everything—which left<br />
me with family medicine or emergency medicine. Then I realized<br />
it was emergency medicine that made me want to go to<br />
medical school to begin with.<br />
“From seeing people die to delivering babies—that experience<br />
at a formative age really changed me. I think life is precious<br />
and I think we have a duty to give back to people.”<br />
summer/fall 2007 11
A Family Physician Takes<br />
an Alternative Path<br />
By Tracey Thomas<br />
photo provided by Cmdr. George Ceremuga<br />
Out in “Custer Country,” Cmdr. George Ceremuga, D.O. ('93), plays an active<br />
role in the Indian Health Services’ commitment to promoting healthy American<br />
Indian communities.<br />
Every week, he makes a three-hour commute from his home in South Dakota to the<br />
pine-covered landscape <strong>of</strong> the Northern Cheyenne Indian Reservation in Lame Deer,<br />
Mont., where he provides medical care to Native Americans on the reservation.<br />
“One minute I could be delivering a baby and the next I could be dealing with an<br />
alcohol-related trauma patient,” he says. “I see much more than runny noses.”<br />
As clinical director <strong>of</strong> the Northern Cheyenne Indian Reservation Health Center, the<br />
ongoing struggle to stem the rampant spread <strong>of</strong> alcoholism, teen pregnancy, obesity,<br />
diabetes and drug addiction in native populations looms large in Ceremuga’s pr<strong>of</strong>essional<br />
life. And these are only a few <strong>of</strong> the pressing social issues on the reservation.<br />
12 www.oucom.ohio.edu<br />
He also works with tribal organizations to promote preventive<br />
health activities to improve the health and well-being <strong>of</strong> the<br />
reservation community.<br />
Facing serious health problems every day can take its toll,<br />
but Ceremuga has a prescription for that.<br />
“It’s important to separate yourself from your patients, which<br />
means not taking it personally when someone’s diabetes is<br />
getting worse because they won’t take their medicine,” he<br />
explains. “I see my role as a cheerleader for change, and if<br />
only one person makes a lifestyle change for the better, no<br />
matter how small, I’ve succeeded.<br />
“What I do is not glamorous, but it’s honorable,” he adds.<br />
“Sure we have problems and we’re understaffed, but we’re<br />
helping to make needed change.”<br />
He encourages medical students to do the same, taking what<br />
they’ve learned and using it to help people with the most<br />
need. And he’s quick to point out that helping others doesn’t<br />
mean living a diminished life.<br />
In fact, it’s quite the opposite.<br />
For Ceremuga, it meant exchanging an 80 – 100 hour work<br />
week in private practice, for a 40 – 50 hour work week on<br />
the reservation. Shorter weeks have allowed him to spend<br />
more time with his five children and to live the active and<br />
healthy lifestyle he advocates for his patients.<br />
“I’m constantly challenged in my work and really feel energized<br />
when I can provide patient care to those in need,” he says. “It’s<br />
the reason why I went into medicine.”<br />
TODAY’S<br />
<strong>DO</strong><br />
Don Shoulderblade, “sacred hat keeper” or holy man for the Northern Cheyenne Indian Reservation,<br />
prays daily for the safety and security <strong>of</strong> his people. Cmdr. Ceremuga and Shoulderblade are<br />
collaborating on a plan to integrate western medicine with traditional Northern Cheyenne medicine.
photo provided by Cmdr. George Ceremuga<br />
The Northern Cheyenne Indian Reservation Health Center is a modern, ambulatory<br />
care facility staffed with five family physicians, a pediatrician and two nurse<br />
practitioners who <strong>of</strong>fer outpatient care as well as 24-hour urgent care to nearly 5,000<br />
patients. Services <strong>of</strong>fered include optometry and dental care, physical and behavioral<br />
health therapy, and a full service lab and radiology unit. The clinic also includes<br />
a Healing Room for traditional ceremonies.<br />
In partnership with the Northern Cheyenne Community, the health center staff strives<br />
to raise the physical, mental, social and spiritual health <strong>of</strong> the population to the<br />
highest level in a culturally sensitive manner.<br />
Dr. Ceremuga is a Commander in the U.S. Public<br />
Health Service Commissioned Corps and is currently<br />
detailed to the Indian Health Service. The<br />
Commissioned Corps provides highly trained<br />
and mobile health pr<strong>of</strong>essionals who carry out<br />
programs to promote the health <strong>of</strong> the nation,<br />
understand and prevent disease and injury, assure<br />
safe and effective drugs and medical devices,<br />
deliver health services to federal beneficiaries,<br />
and furnish health expertise in time <strong>of</strong> war or<br />
other national or international emergencies.<br />
Cmdr. Ceremuga also participated in the<br />
Commissioned Corps relief effort immediately<br />
following Hurricane Katrina.<br />
For more information about the Commissioned<br />
Corps please visit www.usphs.gov.<br />
summer/fall 2007 13
Melting Pot<br />
By Anita Martin<br />
14 www.oucom.ohio.edu
<strong>Medicine</strong><br />
N e w i n t e r c u l t u r a l c o m m u n i c a t i o n<br />
t r a i n i n g s e r i e s f o s t e r s c u l t u r a l<br />
c o m p e t e n c y i n f u t u r e p h y s i c i a n s<br />
michaeldibari.com<br />
Medical school sharpens the senses. Eyes detect<br />
subtle imbalances, hands track changes, and ears<br />
listen with heightened diagnostic awareness. But<br />
anatomical savvy and keen diagnoses alone won’t<br />
cut it in today’s medical world. The various views<br />
and priorities <strong>of</strong> humanity’s diverse cultures<br />
rival—and perhaps surpass—the complexity <strong>of</strong> the<br />
human body itself. Culture informs a patient’s<br />
perception <strong>of</strong>, and decisions about, health care.<br />
From 1990 to 2000, the United States Census saw<br />
an increase in every minority population, including<br />
a 23 percent jump in the Hispanic population.<br />
Columbus, <strong>Ohio</strong>, is home to growing enclaves<br />
<strong>of</strong> East Asian Indian, African and other minority<br />
populations. “You don’t have to go very far to<br />
encounter enormous diversity,” says Pat Burnett,<br />
Ph.D., director <strong>of</strong> student affairs at the <strong>Ohio</strong><br />
<strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
That’s why the staff <strong>of</strong> OU-COM’s Center <strong>of</strong><br />
Excellence (COE) is committed to sharpening<br />
the cultural acuity <strong>of</strong> the college’s diverse student<br />
body. Their latest project: a pr<strong>of</strong>essional development<br />
seminar conducted by Mark Orbe, Ph.D., an expert<br />
in cross-cultural medical communication.<br />
Cultural demand<br />
Orbe starts each session <strong>of</strong> his “Pr<strong>of</strong>essional<br />
Development in Cultural Competency” series for<br />
OU-COM by counting “1 – 2 – 3 … ”<br />
“Dumela!” his students shout on cue. The word<br />
dumela is a South African greeting that also<br />
means “I affirm you, I believe in you, and I see the<br />
great potential within you.” Orbe weaves this<br />
Mark Orbe, Ph.D., reviews material covered during the seminar—<br />
basic communication concepts, communication styles and<br />
explanatory models.<br />
michaeldibari.com<br />
summer/fall 2007 15
theme through the COE’s newly developed certificate<br />
program in intercultural communication at OU-COM.<br />
As warm and welcoming as this sounds, Orbe’s program is<br />
no feel-good affirmation fest. In fact, it can be downright<br />
uncomfortable. Participants must critically examine their<br />
own cultural identities, assumptions and biases; learn to<br />
implement communication principles and practice negotiating<br />
patients’ culturally based beliefs about medical care through<br />
simulated interviews.<br />
“This is not cultural sensitivity training. This is about developing<br />
strong communication skills so you get the most meaningful,<br />
productive exchange out <strong>of</strong> a 15-20 minute meeting with a<br />
patient,” Orbe says.<br />
Developing this dynamic series was a team effort. Burnett,<br />
Ann Brieck, associate director <strong>of</strong> student affairs, and Harold<br />
C. Thompson III, D.O., director <strong>of</strong> multicultural affairs, worked<br />
with Orbe to develop the OU-COM certificate program in<br />
intercultural communications, funded by a federal Health and<br />
Human Services Center <strong>of</strong> Excellence grant.<br />
“Cultural training is growing because <strong>of</strong> the demand <strong>of</strong> students,”<br />
Thompson says. “Our world is changing, and students<br />
understand the need to grasp it. We want to provide them<br />
with more practice inside and outside <strong>of</strong> the classroom.”<br />
Mindful approach<br />
As a biracial, first-generation college student, Orbe was drawn<br />
to the cultural aspects <strong>of</strong> communication. After earning his<br />
bachelor’s degree at <strong>Ohio</strong> <strong>University</strong>, he returned for a doctorate,<br />
also in communication studies, during which time his wife gave<br />
birth to their first child at O’Bleness Hospital. He now teaches<br />
intercultural communication at Western Michigan <strong>University</strong>.<br />
“There’s an inextricable relationship between culture and<br />
communication,” he says. “I explore ways in which that<br />
relationship manifests.”<br />
Orbe led his first OU-COM seminar, called “Physician-Patient<br />
Communication in a Multicultural Society,” during winter<br />
quarter 2006. Participants met twice, for a total <strong>of</strong> nine<br />
hours. They earned two academic credits and were given an<br />
overview <strong>of</strong> basic communication concepts and theories<br />
and how they relate to practical medical settings.<br />
“In terms <strong>of</strong> health-care communication, what you say and<br />
how you say it leads to different interpretations among<br />
different people,” says Becky Teagarden, a second-year<br />
medical student who attended this first seminar.<br />
In addition to differing disease propensities across cultural<br />
groups, there are differences in healing methods. Many<br />
groups trust traditional remedies—such as indigenous herbs<br />
and healing rituals—to Western medicine. Cultures can also<br />
express differences in their radius <strong>of</strong> personal space or level<br />
<strong>of</strong> family involvement in decision-making.<br />
Such cultural tips can be helpful, but it’s impossible to<br />
memorize the genetic predispositions, medical practices and<br />
social etiquette <strong>of</strong> every culture. The trick, according to<br />
Orbe, is to ask probing questions and cultivate mindfulness.<br />
michaeldibari.com<br />
From left, first-year students Nicholas Niemiec, Michael Finamore, Aaron Wolk<strong>of</strong>f, Ismail Oshogwemoh, Brett Buller, Jason<br />
Lane, and Baldassare Pipitone toss a ball <strong>of</strong> yarn to create a network <strong>of</strong> gratitude, admiration, appreciation and humanity as<br />
the seminar draws to a close.<br />
16 www.oucom.ohio.edu
Second-year students Rachel Polinski, left, and Antwon Morton, right, listen to second- year student Victoria Tong, center, as she<br />
relates one <strong>of</strong> her father’s experiences from World War II.<br />
“Most <strong>of</strong> us don’t communicate mindfully; we just say what<br />
we’re thinking and assume that there’s a shared meaning,”<br />
Orbe says. “I teach receiver orientation, a concept that says<br />
what’s more important is not what I’m saying, but how you<br />
receive it.”<br />
Investing in connecting<br />
Burnett, Brieck and Thompson knew, from the overwhelmingly<br />
positive response to the first seminar, that they needed to<br />
do more. Orbe returned to speak to OU-COM’s incoming<br />
first-year students in August 2006. They all participated in<br />
Orbe’s four-hour presentation on intercultural communication<br />
as it relates to medical practice.<br />
Meanwhile, second-year students who had attended Orbe’s<br />
winter quarter two-credit class and wanted more could<br />
attend a refresher course. Both groups had the option to<br />
attend three subsequent five-hour classes, but they earned<br />
the certificate in intercultural communication only if they<br />
attended all three.<br />
About 50 percent <strong>of</strong> this year’s first-year class completed this<br />
elective course. It’s no small feat considering the seminar’s<br />
extensive reading list and the fact that sessions are <strong>of</strong>ten on<br />
Friday evening or Saturday morning. This is in addition to<br />
the students’ already rigorous medical training schedule.<br />
“It’s a significant time commitment, but what you get out<br />
<strong>of</strong> it is well worth the hours you give up,” Teagarden says.<br />
“At medical school you’re so bombarded with the science<br />
that you don’t take the time to appreciate how intricately<br />
individual each situation is.”<br />
Through Orbe’s seminar, students gain new levels <strong>of</strong> cultural<br />
competency and mindful physician-patient communication,<br />
but they also deepen their bond with one another.<br />
Before bringing the final seminar class to a close, Orbe gathers<br />
his students into a circle and tosses a colorful ball <strong>of</strong> yarn to<br />
a young woman across the room. Still holding onto his end<br />
<strong>of</strong> the yarn, he affirms the humanity <strong>of</strong> that student, who<br />
tosses the yarn to another, and he to another. Soon multi-hued<br />
strands, each representing gratitude, admiration or appreciation,<br />
crisscross into an elaborate network <strong>of</strong> yarn.<br />
“It is through communication that we establish this web<br />
<strong>of</strong> dumela—<strong>of</strong> affirmation,” Orbe says. “Even though you<br />
didn’t speak to everyone in this room, and despite our<br />
many differences—look: we’re all connected.”<br />
TODAY’S<br />
<strong>DO</strong><br />
summer/fall 2007 17
Gl bal Hea<br />
International programs <strong>of</strong>fer research and clinical exp<br />
improve cultural sensitivity By Anita Martin<br />
A<br />
lthough Shawn Horwitz was born in South Africa, he<br />
grew up in the United States. Last year, as a second-year<br />
student at <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>,<br />
he made his first trip to Africa as an adult to conduct health<br />
care research through the Kenyan Grandparents Study.<br />
“I wanted to see the culture and the medical system <strong>of</strong> an<br />
African country,” says Horwitz, who also plans to explore the<br />
medical practices <strong>of</strong> South America and Asia. “I’m interested<br />
in going back to the third-world area. I’d like to have some<br />
kind <strong>of</strong> impact where it’s most needed.”<br />
Every year, Gillian Ice, Ph.D., founder <strong>of</strong> the Kenyan<br />
Grandparents Study and director <strong>of</strong> international programs<br />
at the college, facilitates training trips for students from<br />
the college and other participating medical schools across<br />
the country. Programming expanded last year to include El<br />
Salvador and the Dominican Republic, and participation in<br />
all programs—averaging about 30 students a year over the<br />
past few years—is growing.<br />
“Having experiences in international medicine helps students<br />
to think about the system in the U.S. with a different<br />
perspective—to not just assume that we provide the best<br />
system, but to really think about the decisions we make and<br />
why,” says Ice, also an associate pr<strong>of</strong>essor <strong>of</strong> social medicine.<br />
The college’s international programs feature tropical disease<br />
research in Ecuador, clinical and research rotations in Kenya,<br />
geriatric training in Scotland, new clinical rounds in El<br />
Salvador and the Dominican Republic, and, until recently,<br />
traditional medicine training in China.<br />
“If a third or fourth-year student wants to travel to a destination<br />
or participate in a program not <strong>of</strong>fered by OU-COM, they<br />
can set one up themselves with our approval,” Ice says. “But<br />
we still have a structure in place to ensure the student’s safety<br />
and a solid educational experience.”<br />
This past year students Andrea Molcutt and Zarinah Hudd,<br />
set up their own projects in Ghana and Ethiopia, respectively.<br />
Two more third-year students, Joseph Davis and Petter<br />
Vaagenes, traveled to Norway in 2005 to learn more about<br />
the practice <strong>of</strong> socialized medicine. All returning students<br />
Second-year student Shawn Horwitz, right, and Gillian Ice,<br />
Ph.D., distribute school uniforms to the local orphans.<br />
write and present papers comparing international medical systems<br />
based on their experiences.<br />
“Whether you practice right here, in Appalachia, or in some<br />
urban setting, it helps to be open to all cultures and be aware
lth<br />
eriences that<br />
<strong>of</strong> potential differences,” Horwitz says. “This is a good way<br />
to learn to interact with patients from different backgrounds<br />
within different health-care systems.”<br />
For example, students participating in the geriatric tutorial in<br />
Edinburgh <strong>of</strong>ten note how differently the United Kingdom<br />
rations care for its elderly. According to Ice, American doctors<br />
more <strong>of</strong>ten take extreme and intensive measures with elderly<br />
patients than do English doctors.<br />
Ice, herself, studied in the U.K. at the London <strong>University</strong><br />
while still a junior at Washington <strong>University</strong>. At the time, she<br />
majored in anthropology and worked in nursing homes on<br />
the side. Later, for her doctoral dissertation in gerontology at<br />
the <strong>University</strong> <strong>of</strong> Minnesota, Ice conducted research on the<br />
stress levels <strong>of</strong> U.S. nursing home populations.<br />
A few years after coming to OU-COM, Ice decided to diversify<br />
her research. “I was aware <strong>of</strong> the HIV epidemic in Africa<br />
and that many grandparents <strong>of</strong> orphans have unexpectedly<br />
become caregivers again,” she says. “I started thinking about<br />
the potential for stress there.”<br />
She headed to Kenya for the first time in 2002, to establish<br />
the Kenyan Grandparents Study, which examines how<br />
unanticipated childcare responsibilities affect the stress levels,<br />
nutrition and health <strong>of</strong> the elderly. What’s more, she fell in<br />
love with the place, and she’s returned every summer since<br />
with students in tow.<br />
“There are many situations in Kenya that will frustrate you or<br />
break your heart, but it’s amazing how much people appreciate<br />
the little things you do for them,” Ice says. “I always learn<br />
something new about myself and about Kenya. ... It’s neat<br />
to watch students go through the same process.”<br />
Even if students never return to the country where they studied<br />
or treat a tropical disease as physicians in the U.S., Ice believes<br />
international experience inspires better physicians.<br />
“Culture permeates everything,” she says. “We are an immigrant<br />
country, and immigrants arrive with their own attitudes, diseases<br />
and customs. It helps to be aware <strong>of</strong> all <strong>of</strong> those factors.”<br />
TODAY’S<br />
<strong>DO</strong><br />
Charles J. Cannon Edinburgh Geriatric Tutorial<br />
This clinical and educational program gives third-year medical<br />
students an opportunity to experience health care for the<br />
elderly in Scotland’s National Health Service.<br />
Deborah Meyer, Ph.D., director, 740.593.2266<br />
meyerd1@ohio.edu<br />
Community-Based Tropical Disease Research-Ecuador<br />
With a focus on Triatominae insects and mosquitoes in domestic,<br />
peridomestic and sylvatic habitats, this program seeks to<br />
reduce the spread <strong>of</strong> Chagas disease in Ecuador. Community<br />
education activities, including the production <strong>of</strong> educational<br />
tools to be used in the region, are also an important part <strong>of</strong><br />
this project.<br />
Mario Grijalva, Ph.D., director, 740.593.2192<br />
grijalva@ohio.edu<br />
Introduction to the Galapagos Islands Natural History<br />
This program provides an introduction to one <strong>of</strong> the most sensitive<br />
ecological habitats in the world. By visiting uninhabited<br />
and inhabited islands, students have a chance to compare and<br />
evaluate the impact <strong>of</strong> human activities on the island ecosystems<br />
and to discuss the struggle between economic development<br />
and conservation.<br />
Mario Grijalva, Ph.D., director, 740.593.2192<br />
grijalva@ohio.edu<br />
Tropical Disease Biology Workshop in Ecuador<br />
The objective <strong>of</strong> this multidisciplinary adventure is to gain a<br />
deeper understanding <strong>of</strong> the complex factors that play a role<br />
in the biology <strong>of</strong> tropical diseases.<br />
Mario Grijalva, Ph.D., director, 740.593.2192<br />
grijalva@ohio.edu<br />
Kenyan Grandparents Study<br />
This research project seeks to examine the effect that caregiving<br />
for orphaned children has on the health and wellbeing<br />
<strong>of</strong> Luo elders.<br />
Gillian Ice, Ph.D., M.P.H., director, 740.593.2128<br />
iceg@ohio.edu<br />
SHARE Kenya-<strong>Ohio</strong><br />
In this clinical program, students, faculty and clinicians deliver<br />
health care to residents in rural western Kenya.<br />
Christopher Simpson, D.O., M.A., director, 740.593.2257<br />
simpson@ohio.edu<br />
Village Mountain Mission<br />
This clinical program provides health care to the people <strong>of</strong><br />
Pueblo Nuevo, Dominican Republic. Identification <strong>of</strong> specific<br />
health conditions, for which there may be some immediate<br />
strategies, as well as those that require long-term strategies<br />
are an important part <strong>of</strong> this program.<br />
Roy Bontrager, M.D., director, 740.593.2207<br />
rbon@hocking.net<br />
<strong>Ohio</strong> <strong>University</strong> and CEDEINFA Partnership:<br />
Medical care for the “poorest <strong>of</strong> the poor” in San Salvador<br />
provides care for children and their families in collaboration<br />
with the Center for the Complete Development <strong>of</strong> Children and<br />
their Families.<br />
Eddith Dashiell, Ph.D., director, 740.593.2581<br />
dashiell@ohio.edu<br />
Clinical rotation in Ecuador<br />
This program provides students with an opportunity to rotate<br />
for four weeks in a variety <strong>of</strong> disciplines in select hospitals<br />
in Quito, Ecuador. Students will take orientation and training<br />
at Catholic <strong>University</strong> <strong>of</strong> Ecuador, receive classes in medical<br />
Spanish and conduct clinical rotations in the different services<br />
<strong>of</strong>fered by the participating hospitals.<br />
David Drozek, D.O., Ph.D., director, 740.593.2489<br />
drozek@oucom.ohiou.edu<br />
summer/fall 2007 19
Capt. Larry Robinson, D.O. (’02), was injured March 1, 2007, when an<br />
IED (improvised explosive device) hit his armored humvee. He required<br />
a craniotomy, cranioplasty and facial reconstruction surgery before<br />
returning to <strong>Ohio</strong>, where he’s recovering with the help <strong>of</strong> his wife,<br />
Emily, and his family.<br />
This is his story.<br />
This was my first deployment.<br />
I arrived in Iraq in August 2006 as part <strong>of</strong> the 5-73 Cavalry<br />
Squadron, which is part <strong>of</strong> the 3rd Brigade Combat Team,<br />
82nd Airborne Division out <strong>of</strong> Fort Bragg, N.C.<br />
As a family physician in the Army, it was my job to keep the<br />
nearly 600 people on my contingency operating base (COB)<br />
healthy with the help <strong>of</strong> one physician assistant and 24 medics<br />
in the squadron. We were based out <strong>of</strong> COB Caldwell in eastern<br />
Iraq, a short distance from the Iranian border. Medically, we<br />
were what the Army calls a level one aid station, which means<br />
personnel available to treat wounded soldiers. On these<br />
missions I felt well protected by the disciplined and<br />
pr<strong>of</strong>essional soldiers in the squadron.<br />
At the end <strong>of</strong> February, we left COB Caldwell to set up<br />
patrol bases in the Diyala River Valley, an area that had been<br />
infiltrated with terrorist and Al-Qaeda affiliated groups. It’s<br />
a dangerous place where many people, including U.S. soldiers,<br />
were killed. We used these bases to launch attacks and raids<br />
against terrorists.<br />
The long<br />
we had no radiology, laboratory, surgery, physical therapy or<br />
dentistry. But there was a small pharmacy along with supplies<br />
to stabilize trauma and to take care <strong>of</strong> sick call. The base<br />
was also home to around 3,000 Iraqi soldiers and to the 5th<br />
Division <strong>of</strong> the Iraqi Army.<br />
While accompanying the Iraqi Army and their medical<br />
team, we went out on several combined medical engagements<br />
where we provided free medical care to people in the<br />
village. These missions were generally well accepted by the<br />
Iraqi people and were an important way for them to see that<br />
their Army cared about them. The missions were fun for me<br />
because it gave me a chance to see Iraqi families with their<br />
children. It was also nice to help relieve a little <strong>of</strong> their suffering<br />
by treating some <strong>of</strong> their illnesses—even if it was just<br />
a temporary fix.<br />
I also went on many combat missions with my squadron.<br />
Treating trauma in the field is very different than treating<br />
trauma in an aid station or a hospital. Bombs and gunfire<br />
may be going <strong>of</strong>f, and there’s less equipment and fewer<br />
On what was to be my last mission, I went out with a<br />
platoon-sized element on a 24-hour mission to watch a<br />
dangerous stretch <strong>of</strong> road. The plan was to catch insurgents<br />
placing improvised explosive devices (IEDs) in the road.<br />
We were out all night watching and caught several insurgents.<br />
On the way back to the patrol base, we took a detour to observe<br />
a nearby town that was supposedly controlled by “The<br />
Islamic State <strong>of</strong> Iraq,” an Al-Qaeda-linked group.<br />
On the outskirts <strong>of</strong> town, our vehicle got stuck in a mud hole<br />
and began to sink. I was sitting in the back <strong>of</strong> the vehicle and<br />
could see angry villagers approaching us with Russian-made<br />
AK47 rifles and a few rocket-propelled grenades. Needless to<br />
say, I was concerned because our 50 caliber machine gun turret<br />
had malfunctioned and wouldn’t swivel. A vehicle behind us<br />
finally managed to pull us out <strong>of</strong> the mud hole. As we headed<br />
toward our patrol base, I praised God for getting me out <strong>of</strong><br />
that situation.<br />
Then my vehicle hit was hit by a large IED.<br />
20 18 www.oucom.ohio.edu
photo courtesy <strong>of</strong> Abigail Bobrow/Sandusky Register<br />
Road back<br />
A family physician recounts<br />
his experience in IraqBy Capt. Larry Robinson, D.O<br />
summer/fall 2007 21
When I woke up at Warhorse, I kept repeating “My head<br />
hurts!” I don’t remember any <strong>of</strong> this, but the doctors at<br />
Warhorse, good friends <strong>of</strong> mine, suspected I had an intracranial<br />
bleed and had me flown to LSA (logistical support area)<br />
Anaconda for treatment.<br />
Thankfully, my Kevlar helmet stopped the IED shrapnel<br />
from penetrating my skull. But the shrapnel did cause<br />
several comminuted fractures <strong>of</strong> my skull, along with facial<br />
bone fractures and epidural, subarachnoid and subdural<br />
hemorrahages. The increasing intracranial pressure from<br />
the bleeding inside my skull caused extreme nausea and<br />
unrelenting vomiting.<br />
My head hurt and I was confused.<br />
When my squadron commander, Lt. Col. Poppas, my<br />
physician’s assistant, Maj. Rather, and a few other friends<br />
from the squadron explained what happened to me and the<br />
extent <strong>of</strong> my injuries, I couldn’t believe it. I asked to see my<br />
CT scan right then and there.<br />
Lt. Col. Poppas pinned a Purple Heart on my shirt, and I<br />
remember thanking him and then jokingly told him it wasn’t<br />
the medal I wanted to receive in Iraq. Maj. Rather and<br />
I always referred to the Purple Heart as the “Iraqi Marksmanship<br />
Badge.”<br />
Capt. Larry Robinson on the Iranian border.<br />
Shrapnel struck me in the helmet and knocked me unconscious.<br />
Paratroopers in my squadron quickly pulled me from the<br />
burning wreckage before the ammunition exploded. I was<br />
taken to FOB (forward operating base) Warhorse and treated<br />
in the same trauma room that I’d worked in as a physician.<br />
Amazingly, I was the only one injured in the explosion!<br />
After that, I was evacuated to Landstuhl, Germany, and had<br />
surgery soon after landing. They performed a craniotomy<br />
with evacuation <strong>of</strong> the epidural hematoma and cranioplasty<br />
to stabilize my fractures. Four days later, I was able to fly<br />
back to the United States to the National Naval Medical<br />
Center (NNMC) in Bethesda, Md. I was very anxious to get<br />
back to the U.S. and to see my wife. I was told she had been<br />
flown to NNMC and was waiting for me.<br />
Capt. Larry Robinson,<br />
center, with Maj. Brad<br />
Rather, a physician<br />
assistant, left, and 1Lt.<br />
Braden Hestermann, a<br />
medical platoon leader,<br />
right, at LSA Anaconda<br />
before his evacuation<br />
to Germany.<br />
22 www.oucom.ohio.edu
Emily’s story<br />
I remember that morning very clearly.<br />
While chastising myself for sleeping in and leaving<br />
only 30 minutes to get ready for work, my cell phone<br />
rang. It was 7 a.m. A few days earlier, Larry told me<br />
that he was leaving for a month-long mission and<br />
would not be able to call me until the end <strong>of</strong> March.<br />
I answered. A male voice identified himself as the<br />
rear detachment <strong>of</strong>ficer for 5-73 CAV and he had news<br />
about Larry. I thought the call might be about some<br />
paperwork that Larry and I needed to fill out. It<br />
never occurred to me that he might have been hurt.<br />
Capt. Larry Robinson with an Iraqi child during a<br />
combined medical engagement mission.<br />
At NNMC I received first-rate medical care, for which I’m<br />
grateful. I wasn’t the most pleasant patient to care for—I<br />
would <strong>of</strong>ten awake from horrible nightmares where I thought<br />
the nurses were all trying to kill me. I was discharged from<br />
NNMC on March 13 to begin my three-month rehabilitation<br />
at Firelands Regional Medical Center.<br />
I did my internship and residency in family practice at Firelands.<br />
My father-in-law, Dr. James Preston, is the director <strong>of</strong> medical<br />
education there and was my first boss during my training.<br />
He’s become a great friend and an inspiration to me.<br />
The medical education I received at Firelands was great. It<br />
gave me everything I needed to be confident <strong>of</strong> my skills<br />
while in Iraq. My focus on hospital and in-patient training at<br />
Firelands—central lines, intubation, chest tubes, etc.—made<br />
procedures and trauma much easier for me in the field.<br />
Almost all soldiers in Iraq suffer from chronic thoracic and<br />
lumbar back pain. It’s one <strong>of</strong> the consequences <strong>of</strong> wearing 50<br />
pounds <strong>of</strong> body armor, spending hours sitting and sleeping in<br />
cramped humvees and sleeping outdoors on the ground while<br />
on missions. Because <strong>of</strong> my excellent OMM training, I was<br />
able to use manipulation to relieve their back pain.<br />
I still have some lingering problems, but I’m rapidly<br />
improving and expected to make a full recovery. After a few<br />
more months <strong>of</strong> rehabilitation, I’ll receive an extensive<br />
cognitive evaluation in the Traumatic Brain Injury Clinic at<br />
Walter Reed Army Hospital to see if I’m ready to return to<br />
active Army duty as a physician.<br />
My squadron has been hit really hard since my injury—I was<br />
the first—18 have been killed and over 40 have been injured<br />
during their long mission in the Diyala River Valley.<br />
I’m not sure if I’ll ever be asked to deploy to Iraq again.<br />
But this brush with death has made me realize that every<br />
day is a gift from God, and it’s important to make the<br />
most <strong>of</strong> every moment.<br />
TODAY’S<br />
<strong>DO</strong><br />
When he told me that Larry had a skull fracture, my<br />
mind went blank. He continued talking, but I couldn’t<br />
comprehend what this guy was saying. I gave the<br />
phone to my dad, hoping he could understand what<br />
was happening.<br />
The look on my father’s face told me the news wasn’t<br />
good—Larry had sustained a skull fracture and they’d<br />
call us when they had more information.<br />
I couldn’t stop crying. After praying and more crying,<br />
I called Larry’s brother, Mark, who is an OU-COM<br />
medical student at Firelands. He and his wife, Valerie,<br />
joined me and my parents for a prayerful wait at the<br />
kitchen table.<br />
We waited for what seemed like an intolerably long<br />
time, then, at 2 p.m., Larry called! His speech was<br />
slurred, but he assured me that his injuries weren’t<br />
“life-threatening,” he was going to be okay and that<br />
he loved me.<br />
I arrived in Bethesda, Md., at the National Naval Medical<br />
Center just a few hours after Larry checked into the<br />
ICU. When I saw him, he had 67 staples holding his<br />
scalp together, two black eyes from the broken bones<br />
in his face and the head trauma, and one blood-red<br />
eyeball. But I couldn’t take my eyes <strong>of</strong>f him—it was so<br />
good to see him.<br />
He’s had an amazing recovery. The doctors at Walter<br />
Reed Army Hospital are impressed with the care he’s<br />
receiving at Firelands and pleased with how well he’s<br />
healing. They expect a full recovery.<br />
We’re so blessed that we can resume our life together.<br />
What a gift.<br />
-Emily Robinson
quality<br />
Research<br />
<strong>of</strong> care<br />
Improving the<br />
By Susan Green<br />
It’s no secret that type 2 diabetes is on the rise.<br />
According to the Centers for Disease Control, 1 in 3<br />
people born in the United States in 2000 will develop<br />
diabetes in their lifetime. And over the next 50 years<br />
as those who develop diabetes continue to do so<br />
at a younger age, the number <strong>of</strong> people in nursing<br />
homes with diabetes will also increase due to the<br />
complexity <strong>of</strong> the disease in an aging population.<br />
“The fastest growing population <strong>of</strong> young people<br />
with diabetes is in this region,” says Rachel Holt, a<br />
second-year medical student at OU-COM. “Imagine<br />
the implications <strong>of</strong> this.”<br />
To examine the implications, Jay Shubrook, D.O.<br />
(’96), and Frank Schwartz, M.D., both affiliated<br />
with the Appalachian Rural Health Institute Diabetes<br />
Center at <strong>Ohio</strong> <strong>University</strong>, designed a research study<br />
to look at the quality <strong>of</strong> care diabetes patients receive<br />
in nursing homes. Holt joined the project in its early<br />
phase and was instrumental in its completion.<br />
The goal <strong>of</strong> the study was to examine physician<br />
management <strong>of</strong> patients with type 1 and type 2<br />
diabetes residing in extended care facilities and to<br />
compare this management to the American Diabetes<br />
Association Standards <strong>of</strong> Care for outpatients.<br />
After reviewing patient charts <strong>of</strong> more than 100<br />
elderly residents with diabetes in 11 nursing homes<br />
in <strong>Ohio</strong> and West Virginia, the researchers discovered<br />
that patients who had their diabetes under control<br />
either as outpatients or while hospitalized, had less<br />
success after entering a nursing home.<br />
Holt says an analysis <strong>of</strong> the data revealed the lack<br />
<strong>of</strong> a systematic approach to diabetes treatment in the<br />
facilities studied. The findings demonstrate that practice<br />
guidelines for this population are needed.<br />
Working closely with medical directors and directors<br />
<strong>of</strong> nursing, Schwartz and Shubrook are developing<br />
specific guidelines regarding the care <strong>of</strong> diabetes in<br />
the nursing home population. “The guidelines give<br />
physicians and nursing home staff a solid framework<br />
for developing treatment plans for this challenging<br />
population,” Shubrook says. “Phase 2 <strong>of</strong> the study,<br />
a second chart review <strong>of</strong> patients, will determine if<br />
following the treatment protocols results in quality<br />
<strong>of</strong> life changes for the residents.”<br />
This project is an excellent example <strong>of</strong> how the<br />
RSAF program gives medical students like Holt an<br />
opportunity to conduct valuable research. “I really<br />
enjoy research and had done basic science bench work,<br />
but I wanted to try clinical research,” she says. “And<br />
Dr. Shubrook’s project was a good fit. Next year I’ll<br />
be doing a family practice fellowship and will continue<br />
to work on phase 2 <strong>of</strong> the nursing home study.”<br />
As Holt’s research advisor, Shubrook gives her<br />
credit for the success <strong>of</strong> the project. He says she<br />
kept the project on track, analyzed the data and was<br />
the lead author on their research paper published in<br />
Diabetes Care.<br />
“The college is very supportive <strong>of</strong> research<br />
opportunities for students by helping us navigate<br />
our way through the process,” Holt adds. “Being<br />
here at OU-COM is advantageous. Through this<br />
experience and others, I’ll be better prepared to<br />
do my residency.”<br />
Holt RM, Schwartz FL, Shubrook JH. Diabetes Care<br />
in Extended Care Facilities: Appropriate Intensity <strong>of</strong><br />
Care? Diabetes Care. 2007 Jun;30(6):1454-1458;<br />
<strong>DO</strong>I: 10.2337/dc06-2311.<br />
From left, Jay Shubrook, D.O., Rachel Holt and Frank<br />
Schwartz, M.D.<br />
24 www.oucom.ohio.edu
“I really enjoy<br />
research and<br />
had done basic<br />
science bench<br />
work, but I<br />
wanted to try<br />
clinical research.”<br />
Curious Clinicians<br />
In an editorial in the New York Times, Susan Love, M.D., writes about the decline <strong>of</strong> “curious clinicians” in an age <strong>of</strong> increasingly<br />
complex medical and scientific research. What was common in the past—physicians who observed their patients and then went<br />
into the lab to test their hypothesis—is seldom practiced. Love advocates a return to medical research that begins with the<br />
patient and then leads to the lab.<br />
For nearly 30 years, the Research and Scholarly Advancement Fellowship (RSAF) has given selected OU-COM students an<br />
opportunity to conduct research. This ten-week summer program gives osteopathic medical students an introduction to<br />
scholarly work under the guidance <strong>of</strong> COM faculty members.<br />
And while not all research projects begin with the patient in mind, many do. Projects range from contributing to an ongoing<br />
faculty research project in the laboratory or clinic, to developing a review <strong>of</strong> a specific body <strong>of</strong> literature, or to an original<br />
research project designed by the student. In addition to conducting research, students are required to attend seminars on<br />
research-related topics, write a research paper and present a poster <strong>of</strong> their project during OU-COM’s annual Research Day<br />
held each fall quarter.<br />
This experience helps to set a strong foundation for future research they may pursue as clinicians.<br />
summer/fall 2007 25
A l u m n i a n d D e v e l o p m e n t<br />
Building our future together<br />
By Sharon Zimmerman<br />
This year has proven to be one <strong>of</strong> exciting changes.<br />
In January 2007, the <strong>of</strong>fices <strong>of</strong> alumni affairs and development merged in order to create a more<br />
unified outreach effort to our graduates and friends <strong>of</strong> the college. As a result <strong>of</strong> the reorganization,<br />
I’ve been named director <strong>of</strong> medical development and executive director <strong>of</strong> alumni affairs. While<br />
I’ll continue to oversee alumni programs at the college, most <strong>of</strong> my time will be dedicated to furthering<br />
the college’s fundraising efforts and working with you to enhance the alumni donor base.<br />
Our new director <strong>of</strong> alumni affairs, Jill Harman, who joined the <strong>of</strong>fice in May, is now responsible<br />
for planning alumni programs and events. Jill had been the associate director <strong>of</strong> admissions for the past<br />
five years, and she brings a wealth <strong>of</strong> knowledge about the college to her new position. Her energy and<br />
enthusiasm are unlike any I’ve seen, and if you haven’t already heard from Jill, you will. One <strong>of</strong> her first<br />
projects is to develop an easy way for you to stay in touch with us and for us to communicate with you.<br />
She has a lot <strong>of</strong> ideas and is interested in your input. Her e-mail address is: harmanj@ohio.edu.<br />
It is also my pleasure to welcome Jeffrey Stanley, D.O. (’82), as president <strong>of</strong> the Society <strong>of</strong> Alumni<br />
and Friends. Dr. Stanley joins the board after 20 years <strong>of</strong> practice as a vascular surgeon in Cleveland,<br />
<strong>Ohio</strong>. He was president <strong>of</strong> the <strong>Ohio</strong> <strong>Osteopathic</strong> Association in 2004, and in 2005 was recognized<br />
by OU-COM as Alumnus <strong>of</strong> the Year for his pr<strong>of</strong>essional achievements and for service to his alma<br />
mater. Also new to the board are Daryl Sybert, D.O. (’86), vice president, and Timothy Barreiro,<br />
D.O. (’97), secretary.<br />
Under Dr. Stanley’s leadership, the board has created several committees that will <strong>of</strong>fer suggestions<br />
concerning improved communication among alumni, and concerning alumni involvement in student<br />
recruiting, curricula and teaching, continuing medical education and development. It’s an exciting<br />
time to be an OU-COM graduate.<br />
I would like to thank Thomas Anderson, D.O. (’83), former president <strong>of</strong> the OU-COM Society<br />
<strong>of</strong> Alumni and Friends, for his three years <strong>of</strong> dedicated service to the board and to the Society.<br />
Dr. Anderson has just completed his first year <strong>of</strong> a three-year term on the <strong>Ohio</strong> <strong>University</strong> Alumni<br />
Association Board <strong>of</strong> Directors, where he’s representing 188,000 graduates. Congratulations Dr.<br />
Anderson!<br />
Congratulations also are in order for board member William ‘‘Rusty’’ Emlich, D.O. (’86), who<br />
was installed as president <strong>of</strong> the <strong>Ohio</strong> <strong>Osteopathic</strong> Association June 22, 2007.<br />
It remains our goal to engage each <strong>of</strong> you into the life <strong>of</strong> the college, whether through your time, talents<br />
or resources. Alumni are vital to the future <strong>of</strong> OU-COM’s continued success, and we look forward to a<br />
lasting relationship with you.<br />
To learn about supporting the<br />
integrated learning and research<br />
facility with a gift, contact Sharon<br />
Zimmerman, 740.593.2176.<br />
26 www.oucom.ohio.edu
C<br />
onstruction <strong>of</strong> the integrated learning and research<br />
facility—a special collaboration between the <strong>College</strong><br />
<strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> and the Russ <strong>College</strong> <strong>of</strong><br />
Engineering—will mark the second time in <strong>Ohio</strong> <strong>University</strong><br />
history that a building has been constructed using funds<br />
primarily from private gifts.<br />
Members <strong>of</strong> the osteopathic medical community have<br />
demonstrated an unprecedented show <strong>of</strong> support for<br />
this project.<br />
For instance, Thomas Anderson, D.O. (’83), and<br />
his wife, Barbara, were the first to fund a named medical<br />
laboratory. Of his reason for giving, Dr. Anderson says,<br />
“ … Because it is our school, our osteopathic family and<br />
our future.”<br />
Richard A. Vincent, president <strong>of</strong> the <strong>Osteopathic</strong> Heritage<br />
Foundations, which made a considerable gift, says, “This<br />
facility provides a significant opportunity to advance the<br />
<strong>Osteopathic</strong> Heritage Foundations’ mission <strong>of</strong> improving<br />
health and quality <strong>of</strong> life while supporting the vision <strong>of</strong><br />
<strong>Ohio</strong> <strong>University</strong>.”<br />
Our own Society <strong>of</strong> Alumni and Friends made history at<br />
<strong>Ohio</strong> <strong>University</strong> with their gift <strong>of</strong> $50,000—the single<br />
largest gift ever made on behalf <strong>of</strong> an OHIO alumni society.<br />
These contributions are part <strong>of</strong> the remarkable $16.3<br />
million in private gifts garnered for the $30 million facility.<br />
Even with additional support from the State <strong>of</strong> <strong>Ohio</strong> and<br />
the <strong>University</strong>, we still need to raise $2.3 million to reach<br />
our goal.<br />
We will be asking for your support. So watch your mail for<br />
an important letter from Dean Jack Brose, D.O., and<br />
Jeffrey Stanley, D.O. (’82).<br />
As we continue fundraising efforts, I invite each <strong>of</strong> you to join<br />
fellow alumni and friends who have shown their support <strong>of</strong><br />
our commitment to excellence in learning and research.<br />
Just like Cutler Hall—built in 1819—this new facility<br />
symbolizes our pioneering spirit and sense <strong>of</strong> community.<br />
Sharon Zimmerman is the director <strong>of</strong> medical development<br />
and executive director <strong>of</strong> alumni affairs.<br />
www.oucom.ohio.edu/researchbuilding/<br />
An artist's rendering <strong>of</strong> the new the integrated learning and research facility.<br />
Research that will be<br />
enhanced by the new facility<br />
Diabetes<br />
Molecular biologist John Kopchick, Ph.D., is<br />
creating new therapies and diagnostics.<br />
Chemist Tadeusz Malinski, Ph.D., is developing<br />
therapies to accelerate wound healing.<br />
Scientist Leonard Kohn, M.D., and engineer<br />
Douglas Goetz, Ph.D., are developing new<br />
compounds to selectively target disease<br />
sites, and Kohn is studying how to detect<br />
early-stage diabetes.<br />
Heart Disease<br />
Goetz is combining engineering and biology<br />
to develop novel ways to treat heart disease.<br />
Technology<br />
The Center for Intelligent, Distributed and<br />
Dependable Systems is helping doctors diagnose<br />
patients, treat illnesses and plan for surgery.<br />
Engineer Robert Williams, Ph.D., in collaboration<br />
with John Howell, Ph.D., associate pr<strong>of</strong>essor <strong>of</strong><br />
biomedical sciences, is developing The Virtual<br />
Haptic Back to teach palpatory diagnosis.<br />
summer/fall 2007 27
Meet the<br />
Society <strong>of</strong> Alumni<br />
Jeffrey Stanley, D.O. (’82)<br />
president<br />
Vascular Surgery, Meridia South Pointe Hospital<br />
Words or phrases that<br />
describe you:<br />
Honest, fair, workaholic,<br />
generous, impatient<br />
Passion:<br />
My work as a vascular<br />
surgeon; this is what I was<br />
born to do<br />
Favorite movie:<br />
The Doctor<br />
Nicole Wadsworth, D.O. (’97)<br />
Emergency <strong>Medicine</strong>, OU-COM<br />
O’Bleness Memorial Hospital<br />
Words or phrases that<br />
describe you:<br />
Quiet, thoughtful, fair,<br />
driven, organized<br />
Wildest dream<br />
concerning health policy:<br />
Universal health care<br />
Peak patient<br />
experience:<br />
When patients ask me if<br />
I have an <strong>of</strong>fice practice<br />
because they would like<br />
me to be their physician.<br />
I’m deeply honored when<br />
this occurs<br />
Words or phrases that<br />
describe you:<br />
Out-<strong>of</strong>-the-box, inventive,<br />
integrative, humanistic,<br />
socially concerned<br />
Passion:<br />
Building systems that<br />
make life better for people<br />
Peak patient experience:<br />
Recognition for writing<br />
policy and developing<br />
a system that improved<br />
health care for the State<br />
<strong>of</strong> <strong>Ohio</strong><br />
Ronald Moomaw, D.O. (’80)<br />
Psychiatry,<br />
<strong>Ohio</strong> Department <strong>of</strong> Rehabilitation and<br />
Correction, Bureau <strong>of</strong> Mental Health Services<br />
28 www.oucom.ohio.edu
and Friends Board<br />
Daryl Sybert, D.O. (’86)<br />
vice president<br />
Orthopedics, New Albany Surgical Hospital<br />
Words or phrases<br />
that describe you:<br />
Optimistic, humorous,<br />
pr<strong>of</strong>essional, impatient,<br />
adventuresome<br />
Inspiration:<br />
My father, who was<br />
an osteopathic family<br />
physician<br />
Timothy Barreiro, D.O. (’97)<br />
secretary<br />
Internal <strong>Medicine</strong> – pulmonary, Pulmonary <strong>Medicine</strong> Consultants<br />
Words or phrases that<br />
describe you:<br />
Researcher, teacher,<br />
learner, overweight<br />
Perfect day:<br />
Save a life, cure a<br />
disease, learn something<br />
new, and go home to<br />
family<br />
Daily edification:<br />
Knowing I can make a<br />
difference in someone’s<br />
life by caring and listening<br />
Words or phrases<br />
that describe you:<br />
Patient, balanced, happy,<br />
motivated<br />
Biggest pr<strong>of</strong>essional<br />
challenge:<br />
Balancing practice and<br />
research<br />
Perfect day:<br />
All days are good<br />
Daily edification:<br />
I truly believe in the<br />
power <strong>of</strong> an optimistic<br />
attitude in life<br />
Mitchell Silver, D.O. (’89)<br />
Cardiology,<br />
Mid<strong>Ohio</strong> Cardiology Consultants<br />
summer/fall 2007 29
Sharon Van Nostran, D.O. (’98)<br />
Family <strong>Medicine</strong>,<br />
Primary Care Physicians<br />
Words or phrases that<br />
describe you:<br />
Dedicated educator,<br />
physician, bird watcher,<br />
ice cream eater<br />
Pr<strong>of</strong>essional bane:<br />
“What are you, some kind<br />
<strong>of</strong> chiropractor?”<br />
Peak patient experience:<br />
Hand-drawn cards from<br />
pediatric patients<br />
William Emlich, D.O. (’86)<br />
Internal <strong>Medicine</strong> - gastroentology, Consolidated<br />
Medical Specialists<br />
Tinisha Jordan, D.O. (’00)<br />
Family <strong>Medicine</strong>, Kaiser Permanente Marlow Heights<br />
Medical Center<br />
Paige Gutheil, D.O. (’02)<br />
Family <strong>Medicine</strong>,<br />
Family Practice West, Inc.<br />
Words or phrases that<br />
describe you:<br />
Honest, determined,<br />
reliable, open-minded,<br />
intelligent—with a touch<br />
<strong>of</strong> “blonde”<br />
First job:<br />
Filling out billing forms for<br />
my dad’s family practice<br />
<strong>of</strong>fice<br />
Pr<strong>of</strong>essional bane:<br />
Patients that come to the<br />
doctor expecting service<br />
equivalent to a fast-food<br />
drive-through: “I’m here<br />
for Nexium, Allegra, Viagra,<br />
and that medicine for<br />
your legs that I saw on TV.”<br />
Georgenna Riley, D.O. (’95)<br />
Radiology, Parma Medical Center<br />
Charles Mehlman, D.O. (’89)<br />
Orthopedics – pediatric, Cincinnati Children’s Hospital<br />
Medical Center<br />
Jay Shubrook, D.O. (’96)<br />
Family <strong>Medicine</strong>, OU-COM<br />
Cornwell Center for Cardiovascular Care<br />
Eric Beck, EMT-P, OMS IV<br />
30 www.oucom.ohio.edu
“Listening to doctors talk about the path they took in their career is a very educational experience<br />
because it helps students find their own paths,” says Tim Neely, a second-year medical student.<br />
Alumni on Campus<br />
This spring alumni talked about their work to OU-COM students during<br />
Career Medical Specialties Week and Minority Health Month.<br />
“There are many barriers to treating the under- and uninsured.<br />
Some <strong>of</strong> the barriers are cultural, but whatever they are, it<br />
prevents patients from seeing you, which means that they<br />
are less likely to receive appropriate care. To reach these<br />
people, you have to be a physician and a social worker.”<br />
–Tinisha Jordan, D.O. (’00), is a physician at Kaiser<br />
Permanente Marlow Heights Medical Center<br />
“I went to Honduras as an expert, and I returned to Athens a<br />
student looking to increase my knowledge.” Other advice:<br />
“Provide spiritual, medical and social help to people in need.”<br />
–David Drozek, D.O. (’83), is an assistant pr<strong>of</strong>essor<br />
<strong>of</strong> surgery at OU-COM<br />
“If you don’t respect their traditions or cultural differences,<br />
then you can’t expect elderly minorities to respect your<br />
advice.”<br />
–Michael Gerardo, D.O. (’01), was a fellow at<br />
Rhode Island Hospital, Brown <strong>University</strong>; beginning<br />
July 1, 2007, he will be an assistant pr<strong>of</strong>essor <strong>of</strong><br />
geriatric medicine at OU-COM<br />
“I want students to know that being an<br />
osteopathic doctor does not limit you to<br />
just primary care.”<br />
–Karen Thomas, D.O. (’96), treats<br />
patients with motor complications at<br />
the Movement District Center, <strong>Ohio</strong><br />
State <strong>University</strong><br />
“If you’re looking for a career with lots <strong>of</strong> hands-on<br />
with patients, radiology should probably not be your first<br />
choice. Patient interaction is very limited.” Other advice:<br />
“If you’re interested in becoming a radiologist, get as<br />
much exposure—no pun intended—as you can.”<br />
<br />
–Bradley Cole, D.O. (’99), ), is a cross imaging<br />
radiologist at the Cleveland Clinic<br />
summer/fall 2007 31
1980<br />
MacGregor E. Poll, D.O., is medical director <strong>of</strong> Northridge<br />
Surgery Center in Madison, Tenn.<br />
Gary W. Welch, D.O., was recently reappointed chairman<br />
<strong>of</strong> the board <strong>of</strong> directors at the Pennsylvania Trauma Systems<br />
Foundation, the agency which accredits all trauma centers in<br />
the state.<br />
1982<br />
Barbara A. Girz, D.O., was elected president <strong>of</strong> the New<br />
Jersey Maternal-Fetal <strong>Medicine</strong> Society for the 2006-2007<br />
term.<br />
David Lance, D.O., is senior medical director at Hospice<br />
and Palliative Care <strong>of</strong> Greater Wayne County in Wooster,<br />
<strong>Ohio</strong>.<br />
William Polinski, D.O.,<br />
gave an informative and entertaining<br />
presentation about<br />
cardiovascular medicine to<br />
OU-COM students in January<br />
2007. A practicing cardiologist<br />
for 18 years, Polinski talked about future testing<br />
and drug programs that could revolutionize cardiac<br />
care. He also <strong>of</strong>fered tips on vascular health, post-heart<br />
attack care utilizing aspirin and statin drugs, exercise,<br />
and metabolic syndrome to an audience that included<br />
his daughter, second-year student Rachel Polinski.<br />
His talk was sponsored by the OU-COM chapter <strong>of</strong><br />
the Student <strong>Osteopathic</strong> Medical Association, <strong>of</strong> which<br />
Rachel is vice president.<br />
OhiO <strong>University</strong> AlUmni AssOciAtiOn<br />
The Offical Ring <strong>of</strong><br />
<strong>Ohio</strong> <strong>University</strong><br />
Find information on<br />
the ring and how to order<br />
in our Bobcat Store.<br />
OHIO Alumna <strong>of</strong> the Year<br />
1984<br />
Roberta L. Kalafut, D.O., was appointed by Governor<br />
Rick Perry to the Texas Medical Board, as chairman <strong>of</strong><br />
licensure in 2002. She is currently serving as the board’s first<br />
female president.<br />
Louis B. Kasunic, D.O., is practicing at Castle Rock<br />
Family Physicians and is the director <strong>of</strong> the Colorado<br />
Cardiovascular Risk Reduction Center in Castle Rock,<br />
Colo.<br />
Anthony Montanaro, D.O., was named the Cleveland<br />
Clinic Foundation’s annual Educator <strong>of</strong> the Year for 2006.<br />
1986<br />
Kyle Allen, D.O., received a federal grant from the Agency<br />
for Healthcare Research and Quality to study a care management<br />
model for low-income elderly.<br />
E. Joseph Carter, D.O., was named a fellow <strong>of</strong> the<br />
American <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Internists.<br />
Amelia Tunanidas, D.O. (’82), was<br />
named <strong>Ohio</strong> <strong>University</strong> Alumni Association<br />
2007 Alumna <strong>of</strong> the Year. She was recognized<br />
for her service to the osteopathic pr<strong>of</strong>ession<br />
and for her support <strong>of</strong> <strong>Ohio</strong> <strong>University</strong>.<br />
“I am most humbled and thrilled to have<br />
been selected for this recognition from<br />
my alma mater,” she says. “There are so<br />
many wonderful graduates <strong>of</strong> <strong>Ohio</strong><br />
<strong>University</strong> who are truly deserving <strong>of</strong><br />
this award, and I am spellbound to have been selected among such<br />
worthy honorees. It is quite an honor to join the ranks <strong>of</strong> OU’s<br />
finest, and I am grateful to the Lord to be blessed with this honor.”<br />
Tunanidas will be honored, along with other <strong>Ohio</strong> <strong>University</strong><br />
alumni at an awards ceremony during Homecoming Weekend,<br />
October 12-14, 2007.<br />
Gregory Hill, D.O., joined Spectrum Orthopedics in<br />
Canton, <strong>Ohio</strong>, after completing his second tour <strong>of</strong> duty in<br />
Iraq in December 2005.<br />
www.OhiOAlUmni.Org/stOre<br />
Robert Vaschak, D.O., recently gave a cardiovascular physical<br />
exam presentation to 3rd and 4th-year medical students<br />
in the OU-COM Internal <strong>Medicine</strong> Club.<br />
32 www.oucom.ohio.edu
1988<br />
Robert A. Cain, D.O., was named director <strong>of</strong> medical education<br />
at Grandview Hospital in Dayton, <strong>Ohio</strong>.<br />
Vicky Leo, D.O., is chair <strong>of</strong> the American <strong>Osteopathic</strong><br />
Board <strong>of</strong> Internal <strong>Medicine</strong> for the 2006-2007 term.<br />
Gwendolyn E. Niebler, D.O., accepted the position <strong>of</strong><br />
vice president <strong>of</strong> medical affairs at Shire Pharmaceuticals in<br />
Wayne, Pa.<br />
Michael Reeder, D.O., received the 2006 Teacher <strong>of</strong> the<br />
Year Award from St. Mary’s Family Practice Program in<br />
Grand Junction, Colo.<br />
Jill Vosler, D.O., published her first novel,<br />
Legal Larceny, a fictional depiction <strong>of</strong> the<br />
malpractice travails that shape the practice <strong>of</strong><br />
modern medicine. Inspired by a lawsuit leveled<br />
at a fellow physician, Vosler decided to take a<br />
closer look at “…our overly litigious climate”<br />
and the way it changes the practice <strong>of</strong> medicine.<br />
A family practitioner for over 17 years, Vosler practices<br />
in the same building where two <strong>of</strong> her three brothers also<br />
practice. Along with maintaining a busy practice, she serves as<br />
the Eaton High School team physician and also sits on the<br />
Preble county Mental Health and Recovery Board. And she<br />
recently became president <strong>of</strong> the Eaton Little League. How<br />
does she have time to write? “It’s tricky,” Vosler says. “But<br />
I’m quite good a making a few hours count.” Her next book<br />
will target the medical insurance industry.<br />
1990<br />
Franklin Demint, D.O., was certified by the AOA/<br />
AOBNMM in Neuromusculoskeletal <strong>Medicine</strong> and <strong>Osteopathic</strong><br />
Manipulative <strong>Medicine</strong>. He is also board certified in Family<br />
<strong>Medicine</strong> by the AOBFP and credentialed in pain management<br />
by the AAPM.<br />
1992<br />
Macy (Artis) Fox, D.O., started a solo ob/gyn practice<br />
in Snoqualmie, Wash., after relocating to the area with her<br />
husband and children.<br />
Roy Harris, D.O., received the Community Preceptor<br />
All-Star Award, selected by <strong>Ohio</strong> State <strong>University</strong> medical<br />
students. He is married to Mary “Beth” Harman, and they<br />
reside in Bucyrus, <strong>Ohio</strong>, with their two children.<br />
Tracy Marx, D.O., completed a Primary Care Faculty<br />
Development Fellowship with an emphasis on research<br />
methodology at Michigan State <strong>University</strong>.<br />
1994<br />
David D. Powell, D.O., has established a solo oncology<br />
practice, Cancer Care <strong>of</strong> West Central <strong>Ohio</strong>, in Lima, <strong>Ohio</strong>.<br />
John C. Sarantopoulos, D.O., and his wife Christina G.<br />
Sarantopoulos, D.P.M, announce the birth <strong>of</strong> a daughter, Kyra,<br />
born May 9, 2006.<br />
Charles E. Steiner, D.O., gave a lecture on somatic<br />
dysfunction and osteopathy at the Tennessee Academy <strong>of</strong><br />
Physicians Assistants CME conference Oct. 10, 2006.<br />
Timothy Wagner, D.O., and Joanne Nohra were married<br />
in July 2006. He was given command <strong>of</strong> Cc. 235 BSB (Med)<br />
in August, and was deployed to Iraq for the second time in<br />
December 2006.<br />
John J. Wilson, D.O., completed an Interventional<br />
Physiatry/Spine Fellowship at Orthopedic Specialists <strong>of</strong> the<br />
Carolinas in Winston-Salem, N.C. He opened a new practice,<br />
Piedmont Spine Specialists, PA, in Raleigh, N.C., with John G.<br />
Bentley, M.D. (B.S., ’93), and also serves as an instructor for<br />
the North American Spine Society spinal injection course.<br />
1996<br />
Susan Schrimpf Davis, D.O., completed a fellowship in<br />
geriatric medicine at the <strong>University</strong> <strong>of</strong> Cincinnati <strong>College</strong> <strong>of</strong><br />
<strong>Medicine</strong>. She is also an assistant pr<strong>of</strong>essor <strong>of</strong> family medicine<br />
at the college. She and husband, Craig M. Davis, Ph.D., have<br />
a 2-year-old son, Vincent.<br />
Deborah Gallo, D.O., and John Burlock Jr. were marred<br />
Aug. 5, 2006.<br />
Joseph M. Fabry, D.O., is practicing general and vascular<br />
surgery at the Santa Cruz Medical Clinic, a 150-physican,<br />
multi-specialty group in Santa Cruz, Calif.<br />
Michelle Kantor Herring, D.O., and husband, Jefferson<br />
Herring, M.D., have a son, Jacob, born Jan. 14, 2005.<br />
Miguel Krishnan, D.O., is an assistant pr<strong>of</strong>essor <strong>of</strong> pediatric<br />
otolaryngology at the <strong>University</strong> <strong>of</strong> Southern California, Keck<br />
School <strong>of</strong> <strong>Medicine</strong>. He and wife, Norma Marie Salmh<strong>of</strong>er,<br />
welcome their third daughter, Sara, to the family.<br />
Wayne J. Myles, D.O., is an assistant pr<strong>of</strong>essor <strong>of</strong> family<br />
medicine at OU-COM. He started a “practice within a<br />
practice” for people between 13 and 25 called TeenMed. He<br />
recently gave a presentation for the <strong>Ohio</strong> <strong>University</strong> Center for<br />
International Business Education and Development to business<br />
leaders and physicians from Brazil on how to start and run<br />
a successful family medicine practice in the U.S.<br />
Vernon Reynolds, D.O., and wife, Julie, announce the<br />
birth <strong>of</strong> a daughter, Lainey, Oct. 10, 2005.<br />
summer/fall 2007 33
William E. Saar, D.O., is the director <strong>of</strong> foot and ankle services<br />
at <strong>University</strong> Hospitals Health System-Primary and Specialty Care<br />
Practices.<br />
Mark J. Veronneau, D.O., opened an ear, nose and throat practice<br />
in Prestonsburg, Ky. He and wife, Lisa, announce the birth <strong>of</strong> a<br />
daughter, Adelle Grace, Feb. 4, 2006.<br />
1998<br />
Christopher Cirino, D.O., spent six weeks in the summer <strong>of</strong> 2006<br />
working as an HIV clinical mentor in Lesotho, Africa. He recently<br />
completed a Master <strong>of</strong> Public Health in Global Health at George<br />
Washington <strong>University</strong> School <strong>of</strong> Public Health and is currently<br />
working for St. Vincent’s Health System in Erie, Pa.<br />
Jessie Clairvil, D.O., announces the birth <strong>of</strong> a daughter, Justine,<br />
Sept. 14, 2005.<br />
Jason A. Fried, D.O., is in a vascular surgery fellowship at South Pointe<br />
Hospital in Cleveland, <strong>Ohio</strong>.<br />
Robert W. Garner, D.O., is the community physician liaison to the<br />
executive committee <strong>of</strong> Scott Air Force Base in Illinois, precepting for the<br />
St. Louis <strong>University</strong> Community and Family <strong>Medicine</strong> residency program<br />
as an individual mobilization augmentee.<br />
Vipin Koshal, D.O., is completing a Cardiology Fellowship at the<br />
<strong>University</strong> Hospital/<strong>University</strong> <strong>of</strong> Cincinnati <strong>College</strong> <strong>of</strong> <strong>Medicine</strong>.<br />
Cheryl Leuthaeuser, D.O., presented a lecture on integrated medicine<br />
and osteopathy for autism at the Autism and Asperger Association’s first<br />
international meeting last summer in Park City, Utah, August 2006. In July<br />
2006, the <strong>of</strong>fices <strong>of</strong> OsteoMed II in Middleburg Heights, <strong>Ohio</strong>, where Dr.<br />
Leuthaeuser’s practice resides, were destroyed by fire.<br />
Douglas Maurer, D.O., is completing a Madigan Faculty Development<br />
Fellowship at Madigan Army Medical Center, Fort Lewis, Wash., through<br />
which he’ll receive a Masters in Public Health from the <strong>University</strong> <strong>of</strong><br />
Washington this summer. He also is a recruiter for the Army Health<br />
Pr<strong>of</strong>essions Program.<br />
Leslie (Apacki) Nowell, D.O., and husband, Rob, announce the birth<br />
their second child, Ryan, Dec. 11, 2005.<br />
Ronald J. Russ, D.O., was named residency director <strong>of</strong> family medicine<br />
at Cuyahoga Falls General Hospital in January 2006.<br />
Jean (Weis) Schall, D.O., and husband, Steven, welcomed son, Jack,<br />
Nov. 30, 2005.<br />
Beth Schulz-Butulis, D.O., completed her Army duty last summer and<br />
entered private practice with Family Dermatology in Raleigh, N.C.<br />
Thomas Wagner, D.O., and wife, Lisa, announce the birth <strong>of</strong> a son,<br />
Jacob Thomas, born in April 2006.<br />
2000<br />
Lisa (Knight) Flarey, D.O., and her husband Anthony Flarey,<br />
D.O., (’97), finalized the adoption <strong>of</strong> a daughter, Noelle Christine,<br />
from China. Noelle was born April 3, 2005.<br />
James D. Heddleson, D.O., will complete a pulmonary/critical<br />
care fellowship at Doctors Hospital <strong>of</strong> Columbus in July 2007.<br />
Alexander Hewlett, D.O., received a Masters <strong>of</strong> Science in<br />
Clinical Investigation from the <strong>University</strong> <strong>of</strong> Texas Medical Branch in<br />
Galveston, Texas.<br />
Wendy (Morehead) Kissinger, D.O., and husband, Dan, welcomed<br />
their second son, Nicholas, to the family Dec. 16, 2005.<br />
Rebecca (Hauser) Tat, D.O., and David Tat, D.O. (’99)<br />
are the happy parents <strong>of</strong> twin girls, Madison and Kaitlyn, born June<br />
21, 2005.<br />
Marc Tressler, D.O., received the 2006-2007<br />
Orthopedic Trauma Association Kenneth Johnson<br />
Traveling Fellowship, which he is completing at the<br />
Harborview Medical Center in Seattle, Wash. He’s<br />
focusing on foot and ankle trauma and post-traumatic<br />
reconstruction. He also completed an orthopedic<br />
trauma fellowship at Vanderbilt <strong>University</strong> Medical<br />
Center, where he is now an assistant pr<strong>of</strong>essor.<br />
Kristin (Stenzel) Woodard, D.O., and husband, Todd, announce<br />
the birth <strong>of</strong> a daughter, Morgan Elizabeth, on Aug. 1, 2006.<br />
2002<br />
Gregory Applegate, D.O., completed an Anesthesiology Residency<br />
at Case Western Reserve <strong>University</strong>/<strong>University</strong> Hospital <strong>of</strong> Cleveland<br />
in June 2006 and accepted a position as an anesthesiologist at Walter<br />
Reed Army Medical Center.<br />
Dustin (Humienny) Blakeslee, D.O., is medical director <strong>of</strong><br />
consultation psychiatry at Akron General Medical Center and also<br />
maintains an outpatient private practice with the Center for Akron<br />
Psychiatry. She is involved in training NEOUCOM medical students<br />
and psychiatry residents.<br />
Patrick Blakeslee, D.O., is employed by Premier Medical Partners<br />
and is a hospitalist at Cuyahoga Falls General Hospital, Summa Health<br />
System, and Akron General Medical Center. He is a CORE assistant<br />
pr<strong>of</strong>essor <strong>of</strong> internal medicine.<br />
Catherine Kunzler Champagne, D.O., is an attending emergency<br />
medicine physician with Timberline Emergency Physicians in Saginaw,<br />
Mich.<br />
Marie Demosthenous, D.O., is in a child and adolescent psychiatry<br />
fellowship program. She and her husband, Greg Behbehani, M.D., Ph.D.,<br />
reside in Chicago.<br />
34 www.oucom.ohio.edu
James D. Heddleson, D.O., is currently the chief pulmonary/<br />
critical care fellow at Doctors Hospital in Columbus, <strong>Ohio</strong>.<br />
Brock Herring, D.O., will start an orthopedic foot and ankle fellowship<br />
at St. Joseph Mercy Hospital in Pontiac, Mich., in August.<br />
Anthony Karam, D.O., is a volunteer clinical faculty member<br />
for the <strong>University</strong> <strong>of</strong> California, Davis, and teaches family practice<br />
residents who rotate through emergency medicine at Mercy Medical<br />
Center in Redding, Calif.<br />
Sanjiv Lakhia, D.O., is working for Cincinnati Group Health<br />
Associates practicing PMR, OMT and acupuncture. He and wife,<br />
Teresa, announce the birth <strong>of</strong> a son, Kyran Sanjiv.<br />
Kari (Mann) Lucas, D.O., and husband, Jason, announce the birth<br />
<strong>of</strong> a son, Ethan, Nov. 23, 2006.<br />
Daniel Maurer, D.O., has accepted a shoulder and elbow surgery<br />
fellowship with Dr. Tom Norris in San Francisco, Calif. He announces<br />
the birth <strong>of</strong> a daughter, Mia, Aug. 9, 2006.<br />
Craig Peters, D.O., is completing a cardiology fellowship at the<br />
<strong>University</strong> <strong>of</strong> Arizona Medical Center in Tucson, Ariz.<br />
Larry Robinson, D.O., was deployed as a surgeon with the 5-73<br />
CAU (Recon), 82nd Airborne at FOB Caldwell in Iraq in August<br />
2006. He was wounded in February 2007 and flown to Germany,<br />
then on to Bethesda, where he underwent surgery at the National<br />
Naval Medical Center. The surgery went well.<br />
Tiffani Singleton, D.O., joined the family medicine faculty at the<br />
<strong>University</strong> <strong>of</strong> Alabama in Birmingham after completing an ob/gyn<br />
fellowship there.<br />
2004<br />
Andrew Guglielmi, D.O., and wife, Julie, announce the birth <strong>of</strong> a<br />
daughter, Alyssa. Andrew is a second-year radiology resident in the<br />
Aultman-NEOUCOM program in Canton, <strong>Ohio</strong>.<br />
Sarah Haley-Wien, D.O., received a Masters in Public Health from<br />
the <strong>University</strong> <strong>of</strong> Alabama at Birmingham.<br />
Alexis Johnston, D.O., received the Gold Foundation Humanism<br />
and Excellence in Teaching Award from the Northeastern <strong>Ohio</strong><br />
Universities <strong>College</strong> <strong>of</strong> <strong>Medicine</strong>.<br />
Deanna Ohms, D.O., and Joseph Anderson were<br />
married in November 2006 in Clearwater Beach, Fla.<br />
2006<br />
Jennifer (Paglia) Breedlove, D.O., and husband, Aaron, announce<br />
the birth <strong>of</strong> a son, Benjamin Aaron, Aug. 22, 2006.<br />
Jennifer A. Painter, D.O., will start aviation medicine training this<br />
summer with the U.S. Navy in Pensacola, Fla., for six months. She will<br />
then be stationed as a flight surgeon with a Navy Aviation Squadron.<br />
Keep us posted<br />
Please send us your news for the next issue.<br />
Fax: 740.593.0761<br />
E-mail: harmanj@ohio.edu<br />
Alumni Affairs, 203 Grosvenor Hall, Athens, <strong>Ohio</strong>, 45701<br />
Career_______________________________________<br />
____________________________________________<br />
__________________________________________________________________________________________<br />
_________________________________________________________________________________________<br />
_________________________________________________________________________________________<br />
Personal _____________________________________<br />
____________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
Send us a photo!<br />
Name _____________________________________<br />
Home Address _______________________________<br />
____________________________________________<br />
___________________________________________<br />
Office Address _______________________________<br />
____________________________________________<br />
___________________________________________<br />
Address change ____yes_____no____<br />
Telephone - Home __________________________<br />
Office _____________________________________<br />
E-mail address _____________________________<br />
John J. Parente, D.O., will become an attending physician this summer<br />
at the Fisher-Titus Medical Center in Norwalk, <strong>Ohio</strong>. In addition,<br />
he will be teaching at the <strong>University</strong> <strong>of</strong> Toledo Medical School.<br />
Year <strong>of</strong> graduation __________________________<br />
I would like to read more about ________________<br />
____________________________________________<br />
___________________________________________<br />
____________________________________________<br />
____________________________________________<br />
____________________________________________<br />
summer/fall 2007 35
Peter Johnson, Ph.D.<br />
Three OU-COM<br />
pr<strong>of</strong>essors retire<br />
after 81 years <strong>of</strong> collective service<br />
David Stroh, D.O.<br />
William Duerfeldt, D.O.<br />
David Stroh, D.O.<br />
associate pr<strong>of</strong>essor <strong>of</strong> family medicine<br />
“The college has been a wonderful<br />
place to work, full <strong>of</strong> new adventures,<br />
great people and challenges. I’ve met<br />
lifelong friends here and had the<br />
opportunity to influence more than a<br />
few students.”<br />
Life after OU-COM “I’ll continue<br />
to teach one quarter each year and<br />
will continue my clinical practice in<br />
Coolville. I also plan to spend time<br />
reading, golfing, socializing and taking<br />
up new endeavors.”<br />
Peter Johnson, Ph.D.<br />
pr<strong>of</strong>essor <strong>of</strong> biomedical sciences<br />
“As a founding faculty member at<br />
OU-COM, I have been very pleased<br />
about the way our college has matured<br />
and strengthened over the years. Not<br />
only in terms <strong>of</strong> teaching, but also in<br />
that the college has developed a strong<br />
research focus. I have so much enjoyed<br />
working with the different units in the<br />
college, and I’m sure that I’ll undergo<br />
withdrawal symptoms in the early years<br />
<strong>of</strong> my retirement.”<br />
Life after OU-COM “I’ll be moving<br />
to the mountains <strong>of</strong> western North<br />
Carolina, but will be back in Athens<br />
for the next few summers to continue<br />
teaching in the Prematriculation and<br />
Summer Scholars programs. In North<br />
Carolina, I plan to continue some<br />
<strong>of</strong> my research, writing and editing.<br />
And, I also want to do some volunteer<br />
tutoring in middle and high schools.”<br />
William Duerfeldt, D.O.<br />
associate pr<strong>of</strong>essor <strong>of</strong> family medicine<br />
“I’ve been truly blessed to have had<br />
the opportunity to teach and practice<br />
medicine at OU-COM. It has been a<br />
privilege to share my experiences, and<br />
my patients, with the scores <strong>of</strong> medical<br />
students who rotated through my<br />
Nelsonville <strong>of</strong>fice these past 27 years.<br />
I think that is what I’m going to miss<br />
the most.”<br />
Life after OU-COM “My wife and<br />
I are moving to Asheville, N.C., and<br />
visiting family in Oregon this summer.<br />
We plan to spend 3-6 months each<br />
year—beginning in September—working<br />
in Jerusalem for the humanitarian aid<br />
organization “Vision for Israel.”<br />
36 www.oucom.ohio.edu
June 21 – 24, 2007<br />
<strong>Ohio</strong> <strong>Osteopathic</strong> Association Annual Convention<br />
The Lodge at Sawmill Creek Resort, Sandusky, <strong>Ohio</strong><br />
Alumni Reception: June 21, 2007<br />
5:00 – 7:30 pm, Wolf Room<br />
Recognizing William Emlich, D.O. (’86)President,<br />
<strong>Ohio</strong> <strong>Osteopathic</strong> Association<br />
OU-COM Alumni Board Breakfast Meeting: June 23, 2007<br />
8:00 – 9:30 am, Moose Room<br />
Save the Date<br />
alumni calendar<br />
June 27 – 30, 2007<br />
American Association <strong>of</strong> <strong>College</strong>s <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong> Annual Meeting<br />
Renaissance Harborplace Hotel, Baltimore, Md.<br />
August 1, 2007<br />
OU-COM 1st Year Classes Begin<br />
August 18, 2007<br />
OU-COM Convocation and White Coat Ceremony<br />
10:00 a.m., Templeton Blackburn Alumni Memorial Auditorium<br />
September 5, 2007<br />
OU-COM 2nd Year Classes Begin<br />
September 30 - October 4, 2007<br />
American <strong>Osteopathic</strong> Association Annual Convention<br />
San Diego Convention Center, San Diego, Calif.<br />
Alumni Lunch & Reception: October 1, 2007<br />
Marriott/Omni<br />
October 12 - 14, 2007<br />
<strong>Ohio</strong> <strong>University</strong> Homecoming & Alumni Awards Ceremony<br />
Recognizing Amelia G. Tunanidas Pantelis, D.O. (’82)<br />
Alumna <strong>of</strong> the Year<br />
October 18 - 21, 2007<br />
Annual OU-COM Reunion/CME and Alumni Awards Program<br />
Hilton Hotel at Easton, Columbus, <strong>Ohio</strong><br />
OU-COM Alumni Board Meeting: October 18, 2007<br />
Center <strong>of</strong> Excellence Reunion: October 19, 2007<br />
Class <strong>of</strong> 1982 25 Year Reunion: October 20, 2007<br />
Hotel Reservations 614.414.5000<br />
October 18 - 21, 2007<br />
2007 Annual Clinical Assembly <strong>of</strong> <strong>Osteopathic</strong> Specialists<br />
San Francisco Marriott, San Francisco, CA<br />
January 18 – 19, 2008<br />
Cleveland Academy <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Winter CME<br />
Embassy Suites, Independence, <strong>Ohio</strong><br />
Alumni Reception, January 18, 2008<br />
Co-sponsored by OU-COM Society <strong>of</strong> Alumni & Friends<br />
February 2008<br />
Cincinnati District Academy <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Cincinnati, <strong>Ohio</strong><br />
Alumni Reception, Co-sponsored by<br />
OU-COM Society <strong>of</strong> Alumni & Friends<br />
February 2008<br />
Winter OU-COM Alumni Board Meeting<br />
Hilton Hotel, Easton, Columbus, <strong>Ohio</strong><br />
March 12 – 16, 2008<br />
ACOFP 45th Annual Convention<br />
Hyatt Regency, Denver, Colo.<br />
Alumni Recepton, Co-sponsored by<br />
OU-COM Society <strong>of</strong> Alumni & Friends<br />
cme<br />
All Class Reunion<br />
<strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
& Society <strong>of</strong> Alumni and Friends<br />
&<br />
October 19–21, 2007<br />
Hilton at Easton<br />
Columbus, <strong>Ohio</strong><br />
Mark your calendar now for this this weekend <strong>of</strong> exciting medical education programs! You<br />
can earn up to 20 hours <strong>of</strong> CME credit and have the opportunity to meet with many <strong>of</strong> your<br />
colleagues and former classmates as well as members <strong>of</strong> the OU-COM faculty and staff.<br />
Special social events are planned, so call your classmates now and ask them to join<br />
you in Columbus.<br />
Make your reservation now for a special room rate. Call 614.414.5000 or go online at<br />
Hiltoncolumbus.com and enter Code OHU.<br />
Watch your mail for more information.<br />
For additional information, please call:<br />
740.593.4232<br />
Or e-mail:<br />
harmanj@ohio.edu<br />
To register online:<br />
http://www.oucom.ohiou.edu/Alumni/<br />
Sponsored by:<br />
OU-COM Society <strong>of</strong> Alumni & Friends<br />
OU-COM Area Health Education Center
what’s inside?<br />
a p r e v i e w o f t h e s u m m e r / f a l l i s s u e . . .<br />
Capt. Larry Robinson, D.O. (’02),<br />
recounts his experience in Iraq<br />
20<br />
Second-year<br />
24<br />
student Rachel Holt leads<br />
the way in a research paper published<br />
in Diabetes Care.<br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
332 Grosvenor Hall<br />
Athens, OH 45701<br />
Non Pr<strong>of</strong>it Org.<br />
U.S. Postage<br />
PAID<br />
Permit No. 100<br />
Athens, OH<br />
ADDRESS SERVICE REQUESTED