download magazine pdf - Ohio University College of Osteopathic ...
download magazine pdf - Ohio University College of Osteopathic ...
download magazine pdf - Ohio University College of Osteopathic ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
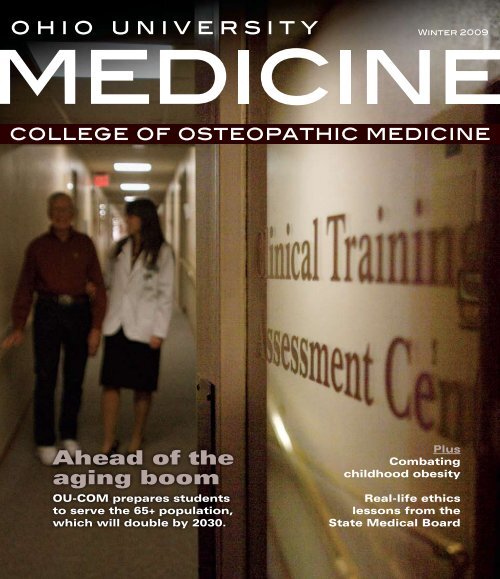
Winter 2009<br />
college <strong>of</strong> osteopathic medicine<br />
Ahead <strong>of</strong> the<br />
aging boom<br />
OU-COM prepares students<br />
to serve the 65+ population,<br />
which will double by 2030.<br />
Plus<br />
Combating<br />
childhood obesity<br />
Real-life ethics<br />
lessons from the<br />
State Medical Board
ohio university<br />
Winter 2009<br />
A publication <strong>of</strong> the <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Medicine<br />
02<br />
From the Dean<br />
Medical education for a new generation<br />
03<br />
05<br />
06<br />
<strong>College</strong> Check-up<br />
Noteworthy<br />
Research News<br />
Q&A: Rathindra Bose, Ph.D.<br />
<strong>Ohio</strong> <strong>University</strong> Vice President for<br />
Research and Creative Activity<br />
08<br />
Features<br />
Michael Kleinfeld<br />
Features<br />
17<br />
18<br />
20<br />
24<br />
Follow-up<br />
Gumption and goodwill<br />
Georgenna Riley, D.O.<br />
Class Notes<br />
Going to extremes<br />
Stephen Augustine, D.O.<br />
More than 40 students and clinical faculty from OU-COM and about 800 others from<br />
across the U.S. attended the 2008 D.O. Day on the Hill this April. This national lobbying<br />
event, coordinated by the American <strong>Osteopathic</strong> Association, brings together D.O.s and<br />
medical students to advocate for health care policy reform.<br />
OUM<br />
For more photos from D.O. Day on the Hill 2008, go to<br />
www.oucom.ohiou.edu/oum.<br />
Getting a grip on<br />
the aging boom<br />
In thirty years, the senior population<br />
will nearly double, while the number<br />
<strong>of</strong> geriatricians continues to dwindle.<br />
OU-COM trains students to help<br />
meet the demand.<br />
08 12 14<br />
First: Do no harm<br />
Soon after receiving their short white<br />
coats, the class <strong>of</strong> 2012 will do something<br />
they had hoped to avoid throughout their<br />
careers: appear before the State Medical<br />
Board <strong>of</strong> <strong>Ohio</strong>.<br />
Fit kids,<br />
fit communities<br />
Through education and perspiration,<br />
OU-COM tackles the intricacies <strong>of</strong><br />
childhood obesity.<br />
Michael Kleinfeld<br />
OUM<br />
Visit <strong>Ohio</strong> <strong>University</strong> Medicine online for additional content. www.oucom.ohiou.edu/oum
<strong>College</strong> Check-up<br />
From the Dean<br />
<strong>College</strong> News<br />
ohio university<br />
<strong>Ohio</strong> <strong>University</strong> Medicine is published twice a year by the<br />
<strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Medicine Office <strong>of</strong> Communication.<br />
Editorial Advisory Board<br />
John A. Brose, D.O.<br />
Dean, <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> Medicine<br />
Pat Burnett, Ph.D.<br />
Director, Student Affairs<br />
George Dunigan II<br />
Director, Governmental Affairs<br />
Judith Edinger, M.Ed.<br />
Director, Predoctoral Education<br />
Andrea Gibson<br />
Director, Research Communications<br />
<strong>Ohio</strong> <strong>University</strong><br />
Jill Harman, M.Ed.<br />
Director <strong>of</strong> Alumni Affairs<br />
Christine Knisely, M.A.<br />
Executive Director <strong>of</strong> Research<br />
and Grants<br />
Editor<br />
Karoline Lane, M.L.S.<br />
Managing Editor<br />
Anita Martin<br />
Copy Editor<br />
Shelby Mullins<br />
Design<br />
Jeff Brown<br />
Photography<br />
John Sattler<br />
Contributing Photographers<br />
Leonardo Carrizo<br />
Michael Kleinfeld<br />
Kevin Riddell<br />
Writers<br />
Natalie Cammarata<br />
Anita Martin<br />
Mary Reed<br />
Dwayne Stewart<br />
Richard Heck<br />
Stephen McKean<br />
Susie Shutts<br />
Administration<br />
Roderick McDavis, Ph.D.<br />
President, <strong>Ohio</strong> <strong>University</strong><br />
John A. Brose, D.O.<br />
Dean, <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Medicine<br />
Karoline Lane, M.L.S.<br />
Director, Office <strong>of</strong> Communication<br />
Marie Graham<br />
Associate Director, Communication Design Services<br />
Daniel Silbiger<br />
Student Government Past President<br />
Edwin Rowland, Ph.D.<br />
Chair, Department <strong>of</strong><br />
Biomedical Sciences<br />
John Schriner, Ph.D.<br />
Director <strong>of</strong> Admissions<br />
Kathy Trace, M.H.A.<br />
Director <strong>of</strong> the Area Health Education<br />
Center, Community Health Programs<br />
Patricia Westfall, M.S.<br />
Pr<strong>of</strong>essor <strong>of</strong> Magazine Journalism<br />
E.W. Scripps School <strong>of</strong> Journalism<br />
Sharon Zimmerman, M.P.A.<br />
Director <strong>of</strong> Medical Development,<br />
Executive Director <strong>of</strong> Alumni Affairs<br />
Opinions expressed in <strong>Ohio</strong> <strong>University</strong> Medicine are those <strong>of</strong> the authors and do<br />
not necessarily reflect viewpoints <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
Medicine. © ’08 <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Medicine.<br />
Editorial <strong>of</strong>fices: Room 330, Grosvenor Hall, <strong>Ohio</strong> <strong>University</strong>, Athens, <strong>Ohio</strong>, 45701.<br />
Address updates for <strong>Ohio</strong> <strong>University</strong> Medicine should be referred to:<br />
Sheila Byc<strong>of</strong>ski<br />
OU-COM, 332 Grosvenor Hall<br />
Athens, OH 45701<br />
phone: (740) 593-2346<br />
e-mail: byc<strong>of</strong>ski@ohio.edu<br />
Medical education for a new generation<br />
We are publishing our college <strong>magazine</strong> with a new name, a new look and a renewed commitment to<br />
storytelling. It seems fitting that as we publish this revitalized <strong>magazine</strong>, change envelops us as never before.<br />
We are surrounded by changes on Wall Street, in Washington and in the environment, many <strong>of</strong> which<br />
require us to challenge long-held beliefs and design new methods to improve quality, despite diminishing<br />
resources. For our communication efforts, this means better quality publications that place a high value<br />
on your time and interests. For the <strong>magazine</strong> specifically, it means a well-defined editorial purpose, more<br />
economical in-house development, a polished look and stories that quickly and effectively express the<br />
values and activities <strong>of</strong> OU-COM. Even though <strong>Ohio</strong> <strong>University</strong> Medicine is smaller than Today’s D.O.,<br />
our newfound vibrancy and the accompanying Web site help extend our reach.<br />
Medical education is another area fertile for innovation. A new generation <strong>of</strong> student physicians<br />
now enters medical school with knowledge and abilities far different from those who preceded them.<br />
Our incoming students grew up with portable computers, video games, cell phones and PDAs as major<br />
components <strong>of</strong> their lives. Many can’t imagine a world without them. They pride themselves on their<br />
abilities to multitask, switching from one activity to another and back at dizzying speeds. Indeed, for many<br />
students, concentrating on a single task for a prolonged period is difficult and dull. Medical educators must<br />
take advantage <strong>of</strong> these skills and adapt curricula to better engage this new generation <strong>of</strong> learners.<br />
Perhaps lectures as we once gave them are no longer the best way for most students to learn. At OU-COM,<br />
we have created curricula that emphasize active and small-group learning. While these efforts have proven<br />
very successful, it is now time to take a next step.<br />
To supplement small-group learning and traditional lectures, faculty members now have opportunities<br />
to develop computerized instruction tailored to today’s medical student. Computerized instruction allows<br />
students to move through material at their own pace. Learners can repeat sections, speed up or slow down<br />
presentations and take breaks. Instructors can embed movies (such as surgical procedures), animate<br />
diagrams and demonstrate medical technology such as echocardiograms and MRIs. These demonstrations<br />
can utilize voice-over explanations, highlighting and interactive quizzes to keep the learners engaged.<br />
In an era emphasizing energy conservation, modern classroom technology and videoconferencing <strong>of</strong>fer<br />
greener and more economical possibilities for medical training. Problem sets, grand rounds and clinical<br />
demonstrations could be conducted from hundreds <strong>of</strong> miles away. Students could participate both on the<br />
college campus and from their homes.<br />
Developing these new methodologies won’t be easy. They will require some time and faculty<br />
development. However, creating learning experiences tailored to a new generation <strong>of</strong> students has the<br />
potential to free faculty time, include new instructors from distant sites and create a richer learning<br />
environment that will make it well worth the effort.<br />
And as with our <strong>magazine</strong>, we’d better get started quickly, or the world will change again before<br />
we get there.<br />
Jack Brose, D.O.<br />
Dean, <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Medicine<br />
04<br />
05<br />
06<br />
07<br />
Surgery rotation in Honduras<br />
OU-COM’s first international<br />
surgery rotation<br />
Keith Watson, D.O.,<br />
named Educator <strong>of</strong> the Year<br />
American <strong>Osteopathic</strong> Foundation<br />
honors Dr. Watson<br />
Noteworthy<br />
Honors, accolades & retirements<br />
Research<br />
•OU-COM discovery pays <strong>of</strong>f<br />
•Artificial intelligence in insulin pumps<br />
•Dinosaur discoveries<br />
Q&A: Rathindra Bose, Ph.D.<br />
New OU-COM pr<strong>of</strong>essor and cancer<br />
researcher also oversees research, creative<br />
activity and graduate studies at<br />
<strong>Ohio</strong> <strong>University</strong><br />
Serving the State<br />
OU-COM fills primary<br />
care gap in <strong>Ohio</strong><br />
While recent studies show a steep national<br />
decline in young physicians choosing primary<br />
care, OU-COM graduates continue to do so<br />
in large numbers.<br />
Of the 106 members <strong>of</strong> the Class <strong>of</strong> 2008,<br />
52 graduates—49 percent—started primary<br />
care graduate medical programs this summer.<br />
Of those programs, 26 were family medicine<br />
residencies; six, pediatric; and 20, internal<br />
medicine (though many internal medicine<br />
residents may go on to sub-specialize).<br />
The number <strong>of</strong> U.S. medical graduates<br />
entering family practice dropped 50 percent<br />
in the past decade, as reported in the Sept. 10,<br />
Journal <strong>of</strong> the American Medical Association<br />
( JAMA), while the American Academy <strong>of</strong><br />
Family Physicians projects that the need for<br />
primary care specialists will skyrocket by<br />
2020, when the nation will need more than<br />
139,000 family physicians.<br />
The JAMA studies reveal a strong<br />
correlation between salary and popularity <strong>of</strong><br />
a specialty—and that primary care specialties<br />
rank among lowest average salaries. Despite<br />
these trends, OU-COM has long trained<br />
physicians committed to primary care, many<br />
<strong>of</strong> whom choose to practice in underserved<br />
regions <strong>of</strong> <strong>Ohio</strong>.<br />
Of total OU-COM graduates, 54 percent<br />
are primary care providers, 62 percent<br />
practice medicine in <strong>Ohio</strong>, and 46 percent<br />
serve communities with populations less than<br />
50,000, with 11 percent in Appalachia <strong>Ohio</strong>.<br />
Those figures reflect the college mission,<br />
mandated by the <strong>Ohio</strong> General Assembly,<br />
<strong>of</strong> serving <strong>Ohio</strong> populations in need and<br />
emphasizing family medicine. The OU-COM<br />
Office <strong>of</strong> Admissions highly considers these<br />
factors during interviews, recruiting mainly<br />
within the state and seeking applicants who<br />
value primary care training.<br />
“We require out-<strong>of</strong>-state students to<br />
practice at least five years in <strong>Ohio</strong> following<br />
medical school and residency, which can<br />
be waived if students choose an American<br />
<strong>Osteopathic</strong> Association accredited three-year<br />
primary care residency within the Centers for<br />
<strong>Osteopathic</strong> Research and Education,” said<br />
John Schriner, Ph.D., director <strong>of</strong> admissions.<br />
“Many <strong>of</strong> these physicians choose to stay in<br />
the state indefinitely, making OU-COM a<br />
state importer <strong>of</strong> medical talent.”<br />
From early clinical contact hours through<br />
third- and fourth-year rotations, OU-COM<br />
prioritizes primary care medicine. With<br />
few exceptions, students’ early Clinical and<br />
Community Experience requirements take<br />
place in primary care settings, and in both<br />
curricular tracks at OU-COM, the vast<br />
majority <strong>of</strong> first-year case studies involve<br />
patients who initially present to their primary<br />
care physicians, emphasizing family medicine<br />
as the first clinical contact point.<br />
OU-COM students begin their third<br />
year with a four-week primary care rotation.<br />
Before they finish their fourth year, they will<br />
have spent an additional six weeks in family<br />
medicine and other primary care rotations.<br />
“We are one <strong>of</strong> a dwindling number <strong>of</strong><br />
medical schools who maintain primary care as<br />
a high priority,” said Dean Jack Brose, D.O.<br />
“We draw a lot <strong>of</strong> outstanding students here<br />
because <strong>of</strong> our reputation for providing an<br />
excellent foundation in primary care.”<br />
Winter 2009<br />
3
<strong>College</strong> Check-up<br />
<strong>College</strong> Check-up<br />
Transitions<br />
Noteworthy<br />
Commencement 2008<br />
<strong>Ohio</strong> Secretary <strong>of</strong> State Jennifer Brunner gave the keynote<br />
address at the 29th annual Commencement ceremony<br />
on June 7. Brunner, <strong>Ohio</strong>’s first female secretary <strong>of</strong> state,<br />
received the 2008 John F. Kennedy Pr<strong>of</strong>ile in Courage Award,<br />
the nation’s most prestigious honor for elected <strong>of</strong>ficials.<br />
Convocation 2008<br />
With 117 students, the class <strong>of</strong> 2012 marks OU-COM’s largestever—and<br />
its top-performing. “I am extremely proud <strong>of</strong> this<br />
year’s class, which has both the highest grade point average<br />
and the best medical college admission test scores in our<br />
college’s history,” says Dean Jack Brose, D.O.<br />
Anne Pope, federal co-chair <strong>of</strong> the Appalachian Regional<br />
Commission, delivered the keynote address at the 33rd<br />
Convocation ceremony August 18.<br />
2012 class pr<strong>of</strong>ile<br />
56% female, 44% male<br />
85% <strong>Ohio</strong> residents<br />
10% from Southeastern <strong>Ohio</strong><br />
or Appalachian <strong>Ohio</strong> counties<br />
27% minority students<br />
Cultural Competency<br />
First international<br />
surgery rotation<br />
A group <strong>of</strong> OU-COM students headed to La<br />
Ceiba, Honduras, in November for the college’s<br />
new clinical immersion in Hospital Suizo.<br />
“The hospital-based experience gives a<br />
perspective on a foreign medical system. This is<br />
unlike our other international rotations that set<br />
up temporary clinics,” says Assistant Pr<strong>of</strong>essor<br />
<strong>of</strong> Surgery David Drozek, D.O. (’83), who led<br />
the two-week program for third- and fourthyear<br />
students.<br />
In the first week, the group performed<br />
surgeries at Hospital Suizo for patients waitlisted<br />
at the local government-sponsored<br />
hospital. Drozek says that Hondurans unable<br />
to afford private hospital fees <strong>of</strong>ten wait months<br />
for federally funded care.<br />
Next, students followed up with surgery<br />
patients and visited local health care facilities<br />
Student Life<br />
Tapped out<br />
Chad Keller, OMS II, (right) Student<br />
Government Association president,<br />
welcomed the Class <strong>of</strong> 2012 with collegebranded,<br />
reusable water bottles. Keller<br />
says the bottles will replace about 12,000<br />
disposable water bottles previously served<br />
at SGA-sponsored lunch lectures this year,<br />
reducing waste and saving the SGA $2,500.<br />
and a medical school in San Pedro Sula, where<br />
they shadowed local medical students.<br />
Hospital Suizo is part <strong>of</strong> a non-pr<strong>of</strong>it<br />
foundation that provides medical care at about<br />
half the cost <strong>of</strong> private hospitals, without the<br />
wait <strong>of</strong> government-sponsored hospitals.<br />
Drozek lived in Honduras for seven years,<br />
where he worked with Hospital Suizo’s<br />
General Director Doris Eggenberger. In March,<br />
Eggenberger visited OU-COM, where she<br />
recounted leaving her home in Switzerland to<br />
found Hospital Suizo in 2000 after witnessing<br />
Honduras’ poverty-stricken health care system.<br />
“A lot <strong>of</strong> people don’t have dreams or goals,”<br />
Eggenberger said. “You just have to have one<br />
and do it.”<br />
By Natalie Cammarata<br />
OUM<br />
For photos and reports from our students who<br />
went to Honduras, go to<br />
www.oucom.ohiou.edu/oum.<br />
Accolades<br />
Keith Watson, D.O., named<br />
AOF Educator <strong>of</strong> the Year<br />
“Few osteopathic physicians have had more<br />
influence on postdoctoral medicine than<br />
Dr. Keith Watson,” (above) says American<br />
<strong>Osteopathic</strong> Foundation President Gilbert S.<br />
Bucholz, D.O., who presented Watson’s award at<br />
the July 2008 American <strong>Osteopathic</strong> Association<br />
House <strong>of</strong> Delegates meeting in Chicago.<br />
Watson, associate dean for graduate medical<br />
education and associate pr<strong>of</strong>essor <strong>of</strong> surgery,<br />
is also chair <strong>of</strong> the Centers for <strong>Osteopathic</strong><br />
Research and Education board. Bucholz says<br />
that Watson has brought the CORE, OU-<br />
COM’s statewide consortium <strong>of</strong> teaching<br />
hospitals, to a national prominence that is the<br />
envy <strong>of</strong> medical educators, both osteopathic<br />
and allopathic.<br />
Regional Innovations<br />
Health information network<br />
connects Southeastern <strong>Ohio</strong><br />
Twenty health care organizations have<br />
formed the Appalachian Health Information<br />
Exchange (AHIE) to help coordinate use<br />
<strong>of</strong> health information technologies such as<br />
electronic record keeping and the electronic<br />
exchange <strong>of</strong> health information in <strong>Ohio</strong>’s<br />
Appalachian communities.<br />
AHIE, which elected its first board in April,<br />
was born out <strong>of</strong> a National Library <strong>of</strong> Medicine<br />
grant OU-COM won through the National<br />
Institutes <strong>of</strong> Health. The association is assessing<br />
needs and developing strategies to incorporate<br />
information technologies into the region.<br />
Before coming to <strong>Ohio</strong>, Watson taught first<br />
at the Oklahoma State <strong>University</strong> <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> Medicine, where he chaired the<br />
Department <strong>of</strong> Surgery, and then at the Des<br />
Moines <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
Medicine, where he was a pr<strong>of</strong>essor <strong>of</strong> surgery,<br />
associate dean for clinical affairs and project<br />
director <strong>of</strong> the Standardized Performance<br />
Assessment Laboratory.<br />
“Dr. Watson has gone to extraordinary<br />
lengths to improve and promote osteopathic<br />
postgraduate education by developing new<br />
programs, conducting mock accreditations<br />
and increasing the visibility <strong>of</strong> osteopathic<br />
residency programs,” Bucholz says.<br />
“I am very honored,” Watson says. “I see this<br />
award as reflecting all the individuals at the<br />
CORE and OU-COM. We do this together.<br />
It’s important for all <strong>of</strong> us to share this honor.”<br />
By Richard Heck<br />
Ross<br />
Franklin<br />
Fairfield<br />
Pickaway<br />
Pike<br />
Scioto<br />
Licking<br />
Hocking<br />
Vinton<br />
Jackson<br />
Lawrence<br />
Guernsey<br />
Muskingum<br />
Perry<br />
Gallia<br />
Visit the AHIE Web site at<br />
www.oucom.ohiou.edu/AHIE/<br />
Coshocton<br />
Morgan<br />
Athens<br />
Meigs<br />
Noble<br />
Washington<br />
Belmont<br />
Monroe<br />
HONORS & APPOINTMENTS<br />
Mario Grijalva, Ph.D.<br />
Director <strong>of</strong> the Tropical Disease Institute<br />
Coordinator <strong>of</strong> the Surveillance and Information Systems Work Group<br />
World Health Organization’s Global Network for Chagas Elimination<br />
John Kopchick, Ph.D.<br />
Goll-<strong>Ohio</strong> Pr<strong>of</strong>essor <strong>of</strong> Molecular and Cellular Biology<br />
• AMVETS Silver Helmet Award<br />
54 th Silver Helmet Awards Banquet (March 29; Alexandria, Va.)<br />
• Honorary Doctor <strong>of</strong> Science degree<br />
Indiana <strong>University</strong> <strong>of</strong> Pennsylvania Commencement (May 10)<br />
Brian Phillips<br />
Chief Information Officer<br />
<strong>Ohio</strong> Broadband Council (appointed by Gov. Ted Strickland)<br />
Barbara Ross-Lee, D.O.<br />
Former Dean<br />
Ruth Purdy, D.O., FACOI<br />
<strong>College</strong> Advocate<br />
Both named “Pioneers in <strong>Osteopathic</strong> Medicine”<br />
American <strong>Osteopathic</strong> Association House <strong>of</strong> Delegates Annual<br />
Meeting (July 18; Chicago, Ill.)<br />
Martha Simpson, D.O.<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Family Medicine<br />
<strong>Ohio</strong> Department <strong>of</strong> Insurance Advisory Committee on Eligibility<br />
and Real Time Claim Adjudication<br />
GRANTS<br />
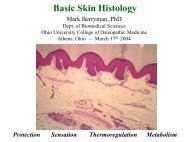
Mark Berryman, Ph.D.<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Biomedical Sciences<br />
“Role <strong>of</strong> CLIC in epithelial morphogenesis”<br />
$154,875, NIH (4/1/2008 – 3/31/2010)<br />
Karen Coschigano, Ph.D.<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Biomedical Sciences<br />
“Cross-talk between growth hormone and inflammation pathways<br />
in kidney damage”<br />
$221,250, NIH (3/10/2008 – 3/9/2010)<br />
Mario Grijalva, Ph.D.<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Biomedical Sciences<br />
“Characterization <strong>of</strong> Trypanosoma cruzi in Southern Ecuador”<br />
$201,839, NIH (5/1/2008 – 3/31/2010)<br />
Jane Hamel-Lambert, Ph.D.<br />
Director <strong>of</strong> Interdisciplinary Mental Health, and<br />
Kathy Trace, M.H.A., R.N.<br />
Director <strong>of</strong> Community Health Programs<br />
“Rural health outreach special initiative”<br />
$189,677, HRSA (8/1/2008 – 7/31/2009)<br />
Frank Horodyski, Ph.D.<br />
Pr<strong>of</strong>essor <strong>of</strong> Biomedical Sciences<br />
“Molecular and functional characterization <strong>of</strong><br />
the allatotropin receptor”<br />
$420,000, NSF (11/1/2008 – 10/31/2011)<br />
Susan Williams, Ph.D.<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Biomedical Sciences<br />
“Collaborative research: Ecological and functional morphology<br />
<strong>of</strong> feeding in free-ranging mantled howling monkeys”<br />
$6,200, NIH (5/1/2008 – 12/31/2008)<br />
RETIREMENTS<br />
Gerald Rubin, D.O.<br />
Associate Pr<strong>of</strong>essor, Family Medicine<br />
Suzanna Theodoras<br />
Diabetes Nurse Educator<br />
4<br />
Winter 2009<br />
Robert Woodworth, D.O., M.P.H.<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Social Medicine<br />
5
<strong>College</strong> Check-up<br />
Research Revenues<br />
<strong>Ohio</strong> <strong>University</strong> ranks fourth<br />
in nation for research returns<br />
on investment<br />
Forbes <strong>magazine</strong> has ranked <strong>Ohio</strong> <strong>University</strong><br />
first in the state and fourth in the nation for<br />
returns on research investment, largely due<br />
to OU-COM research. The university earned<br />
$9.3 million in licensing royalties in the past<br />
two years for the acromegaly drug Somavert ® ,<br />
which developed out <strong>of</strong> a 1988 research<br />
discovery by John Kopchick, Ph.D., Goll-<strong>Ohio</strong><br />
Eminent Scholar and pr<strong>of</strong>essor <strong>of</strong> molecular<br />
biology.<br />
The Forbes study was based on 2006 data<br />
from the Association <strong>of</strong> <strong>University</strong> Technology<br />
Managers. Income generated by Somavert ®<br />
is reinvested in research at all levels <strong>of</strong> the<br />
<strong>University</strong>.<br />
6<br />
Treatment Technologies<br />
Intelligent Therapy<br />
Efforts to bring artificial intelligence to insulin<br />
pump therapy could make life easier for patients<br />
with type 1 diabetes—and their doctors.<br />
Frank Schwartz, M.D. (above), associate<br />
pr<strong>of</strong>essor <strong>of</strong> endocrinology and director <strong>of</strong> the<br />
Appalachian Rural Health Institute (ARHI)<br />
Diabetes/Endocrine Center, is working with<br />
diabetologist Jay Shubrook, D.O. (’96),<br />
assistant pr<strong>of</strong>essor <strong>of</strong> family medicine, and<br />
Cindy Marling, Ph.D., a computer scientist<br />
at the Russ <strong>College</strong> <strong>of</strong> Engineering and<br />
Technology, to design the smarter pump<br />
therapy.<br />
Today’s insulin pumps measure glucose<br />
levels, which project a dizzying array <strong>of</strong><br />
data difficult even for an endocrinologist to<br />
interpret. They do not adjust insulin levels<br />
automatically or make treatment suggestions,<br />
but the s<strong>of</strong>tware Schwartz, Shubrook and<br />
Marling are developing will do just that.<br />
“The technology will remember patterns<br />
and interpret daily lifestyle information to<br />
make suggestions about how patients can<br />
better manage their glucose,” Schwartz says.<br />
In last year’s initial study, 20 patients<br />
documented their treatments and lifestyles—<br />
diet, stress, sleep and exercise habits—in an<br />
online database for six weeks. Schwartz and<br />
Shubrook reviewed the data to propose action<br />
plans for each patient. Based on the outcomes<br />
<strong>of</strong> these plans, the researchers began teaching<br />
the insulin pump therapy program to recognize<br />
problematic patterns and possible solutions.<br />
ohio university medicine<br />
“If someone’s glucose levels are high at night,<br />
Dr. Schwartz may tell them to increase their<br />
pump basal rates <strong>of</strong> insulin infusion,” Marling<br />
says. If the recommendation works, they plug<br />
it into the computer program as a solution to<br />
this problem.<br />
The team has identified 50 problems and<br />
solutions so far. This year, they will follow up<br />
with two studies. The first, which involves 60<br />
patients, will test and validate the s<strong>of</strong>tware.<br />
The second will expand the s<strong>of</strong>tware with the<br />
help <strong>of</strong> 28 new patients.<br />
The project receives support from OU-<br />
COM, the Russ <strong>College</strong> and the ARHI<br />
Diabetes Research Initiative, and equipment<br />
from Medtronic MiniMed, an insulin pump<br />
manufacturer.<br />
Initial findings will appear in the Journal <strong>of</strong><br />
Diabetes Science and Technology, Computational<br />
Intelligence, and the Proceedings <strong>of</strong> the European<br />
Conference on Case-based Reasoning.<br />
“We’ve registered a patent application, and<br />
we’re meeting with insulin pump companies in<br />
hopes <strong>of</strong> forming a collaborative partnership,”<br />
Schwartz says. “Putting the technology in the<br />
hands <strong>of</strong> a national manufacturer would help<br />
it reach more patients.”<br />
By Dwayne Stewart<br />
A version <strong>of</strong> this story originally appeared in the Autumn/<br />
Winter 2007 issue <strong>of</strong> Perspectives <strong>magazine</strong>.<br />
Biomedical Sciences<br />
Dinosaur discoveries<br />
When they’re not teaching human anatomy, a few<br />
<strong>of</strong> our biomedical sciences pr<strong>of</strong>essors stay busy with<br />
high-pr<strong>of</strong>ile paleontology research.<br />
Duck-billed hadrosaurs outgrew<br />
T-rex to survive<br />
With its s<strong>of</strong>t body and long limbs, the duck-billed hadrosaur<br />
had few defenses, but research by OU-COM postdoctoral<br />
fellow Drew Lee, Ph.D., suggests at least one; it grew<br />
much faster than its predators, giving it superiority in size.<br />
Lee and collaborators compared growth rate data from the<br />
bones <strong>of</strong> the hadrosaur to that <strong>of</strong> three predators: two kinds<br />
<strong>of</strong> tyrannosaurs and the small Velociraptor-like Troodon.<br />
They found that the hadrosaur reached adulthood in half<br />
the time as these predators.<br />
Q & A<br />
Rathindra Bose, Ph.D.<br />
Cancer researcher,<br />
university administrator<br />
Our new biomedical sciences pr<strong>of</strong>essor is also<br />
<strong>Ohio</strong> <strong>University</strong>’s vice president for research<br />
and creative activity, and dean <strong>of</strong> the graduate<br />
college—a new unit designed to enhance<br />
graduate education. He assumed all roles July 1.<br />
Meanwhile, he conducts preclinical trials on<br />
compounds with the potential to treat ovarian,<br />
testicular, and head and neck cancers.<br />
OUM: How will your role as VP for<br />
research complement your role as dean <strong>of</strong><br />
the new graduate college?<br />
RB: It’s all integrated. Graduate students<br />
are in the forefront <strong>of</strong> research, under the<br />
supervision <strong>of</strong> their advisors. Faculty shape<br />
graduate students: their overall perspectives,<br />
their projects—and they use graduate<br />
students to drive their own research to the<br />
next levels.<br />
Describe the biochemical research<br />
you do at OU-COM.<br />
I’ve spent 25 years working to find out why<br />
cancer in some patients develops resistance to<br />
drugs while other patients do fine. If you can<br />
figure that out, you can create better drugs.<br />
Dinosaur tracks discovered<br />
on Arabian Peninsula<br />
Nancy Stevens, Ph.D., assistant pr<strong>of</strong>essor <strong>of</strong> biomedical<br />
sciences, was part <strong>of</strong> a team that discovered the first<br />
dinosaur tracks on the Arabian Peninsula. The tracks,<br />
preserved in the Republic <strong>of</strong> Yemen, date back some 150<br />
million years to the Late Jurassic period.<br />
Paleontological findings have been rare in the Arabian<br />
Peninsula, but Stevens and her Dutch and Yemeni<br />
colleagues suspect the area to be rich in discovery. This<br />
finding provides insights into the geological and<br />
chronological overlap <strong>of</strong> dinosaur species, as well as<br />
their herding behaviors.<br />
<strong>College</strong> Check-up<br />
The compounds that we found kill cancer<br />
cells at the same rate in both sensitive and<br />
resistant models. We’re doing trials with<br />
mouse models <strong>of</strong> both (resistant and sensitive)<br />
cell lines for ovarian, testicular, and head and<br />
neck cancers.<br />
How did you get into this line <strong>of</strong> research?<br />
As a chemistry student, I understood<br />
that most diseases are caused and treated by<br />
chemical compounds. Chemists can redesign,<br />
synthesize and reshape molecules based on<br />
what properties we want. I’ve always wanted<br />
to find out how the properties <strong>of</strong> compounds<br />
can best benefit society, so I decided to focus on<br />
cancer biochemistry.<br />
If you had free time, what would you do with it?<br />
Soccer. I used to play in two teams, until<br />
about five years ago. One day, I saw the ball<br />
coming at the optimal height for a bicycle kick,<br />
(for which) you turn your body between 180<br />
and 360 degrees. I hit the ball, but I landed<br />
right on my shoulder and injured it. My wife<br />
said, “Okay, Biomedical that’s enough.” Sciences<br />
By Anita Martin<br />
Prime time dinos<br />
Lawrence Witmer, Ph.D., Chang Ying-Chien endowed<br />
pr<strong>of</strong>essor <strong>of</strong> paleontology and pr<strong>of</strong>essor <strong>of</strong> anatomy,<br />
attracted film crews from the National Geographic<br />
Channel, the History Channel, the Discovery Channel and<br />
the Japanese public broadcast network NHK this year.<br />
The National Geographic Channel interviewed Witmer<br />
for their series, “Prehistoric Predators,” and chronicled his<br />
paleontological research, which uses CT scans performed<br />
at O’Bleness Memorial Hospital, for a documentary,<br />
“Bizarre Dinosaurs.”<br />
Meanwhile, the History Channel has featured Witmer in<br />
two new programs: “Prehistoric Monsters Revealed,” a<br />
documentary, and “Jurassic Fight Club,” a new series; and<br />
the Discovery Channel interviewed Witmer for a show<br />
about terror birds and saber-toothed cats.<br />
Witmer (second from right)<br />
and National Geographic crew.
Faculty monitor from a control room as students<br />
interview community members with Parkinson’s Disease<br />
in the Clinical Skills Assessment Lab.<br />
By 2030, one in five Americans will be 65 or<br />
older. The senior population will double to 71<br />
million in that year. But there will be only<br />
about 8,000 geriatricians.<br />
Feature<br />
Getting a<br />
grip on the<br />
aging boom<br />
In thirty years, the senior population will nearly<br />
double, while the number <strong>of</strong> geriatricians<br />
continues to dwindle. OU-COM trains<br />
students to help meet the demand.<br />
By Anita Martin<br />
Photos by John Sattler<br />
“Ok, Stevens, you’re blind. Schilb, you’re deaf. Martin, you’re visually<br />
impaired. Lykens, you have arthritis.”<br />
Sarah McGrew, B.S.N., manager <strong>of</strong> clinical and community<br />
experiences, passes out assignments to OU-COM students for the<br />
Sensory Changes Lab. The lab is part <strong>of</strong> their required three-week<br />
block <strong>of</strong> coursework in geriatrics, the medical specialty focused on<br />
elderly care, before they begin third-year rotations.<br />
Depending on the students’ “conditions”—all reflecting common<br />
afflictions <strong>of</strong> aging—some wear blindfolds or earphones transmitting loud<br />
static. Others put on goggles covered with semi-opaque plastic wrap or<br />
tape Popsicle sticks to their fingers above the knuckles to hinder dexterity.<br />
For two hours, the students wear their prosthetic impairments through<br />
a series <strong>of</strong> exercises: from buttoning coats to walking with a cane, while<br />
carrying two bags <strong>of</strong> groceries and attempting to unlock a door.<br />
“By simulating experiences related to aging, we’re hoping students<br />
gain a sense <strong>of</strong> empathy for their older patients,” says Deborah Meyer,<br />
Ph.D., R.N., administer and assistant pr<strong>of</strong>essor for OU-COM’s<br />
Department <strong>of</strong> Geriatric Medicine and Gerontology.<br />
These future physicians will have more elderly patients than they may<br />
realize, according to an Institute <strong>of</strong> Medicine study released in April. By<br />
2030, the IOM reports, roughly one in five Americans will be 65 or older<br />
(now it’s about one in ten). The senior population will reach 71 million in<br />
that year, making them the fastest growing national age demographic.<br />
Despite the impending demand, there will be only about 8,000<br />
geriatricians (up slightly from the 7,100 in practice today) in 2030. The<br />
Alliance for Aging Research estimates that the nation will need 36,000.<br />
There are a number <strong>of</strong> reasons for the discrepancy. According to<br />
a 2006 study by the Association <strong>of</strong> Directors <strong>of</strong> Geriatric Academic<br />
Programs (ADGAP), geriatricians are the lowest paid physicians in<br />
the United States—and the only medical specialists who are actually<br />
paid less after completing additional training.<br />
“Geriatric medicine is largely exempt from the usual supply-demand<br />
economics, since Medicare reimbursement is set by the federal<br />
government,” says Wayne Carlsen, D.O., chair <strong>of</strong> geriatric medicine and<br />
gerontology. “When all other expenses in the practice go up and Medicare<br />
reimbursements either stay the same or get cut, physician salaries go down.”<br />
Meanwhile, medical students typically incur between $120,000<br />
and $160,000 in educational debt, as reported by the Association <strong>of</strong><br />
American <strong>College</strong>s <strong>of</strong> Medicine reported in 2007.<br />
“With the rising costs <strong>of</strong> medical school, students are worried about<br />
repaying loans, which can deter even very interested students from<br />
becoming geriatricians,” says Katie Wehri, OMS III, who served as<br />
president <strong>of</strong> the OU-COM Geriatric Medicine Club last year.<br />
Wehri adds that because elderly patients <strong>of</strong>ten have multiple chronic<br />
conditions and can present symptoms differently, medical students<br />
may find it overwhelming to care for this population.<br />
It doesn’t help that few American medical schools actually require<br />
geriatric coursework. In 2006, the New York Times reported that <strong>of</strong> the<br />
145 U.S. medical schools at the time, only nine percent had a distinct<br />
department <strong>of</strong> geriatric medicine.<br />
“We’re pretty far ahead <strong>of</strong> the game at OU-COM in terms <strong>of</strong> what<br />
we <strong>of</strong>fer,” says Meyer, pointing out that the college’s former Geriatric<br />
Medicine/Gerontology Section (then in the Department <strong>of</strong> Family<br />
Medicine) gained departmental status in 1998. The three-week<br />
intensive geriatrics block <strong>of</strong> coursework began one year later.<br />
OU-COM students received distinctive geriatric medical training<br />
long before that. The Sensory Changes Lab dates back almost as far<br />
as the college itself, as does the required two- to four-week geriatrics<br />
rotation, which can be completed through any site in the Centers for<br />
<strong>Osteopathic</strong> Research and Education (CORE) system. And for 23<br />
years, OU-COM medical students have chosen to study international<br />
policy issues related to geriatric medicine in Edinburgh, Scotland,<br />
through the Charles J. Cannon Edinburgh Geriatric Tutorial.<br />
Meyer adds that OU-COM students begin thinking about geriatric<br />
medicine from the start. In 2007, geriatric medicine faculty facilitated 350<br />
hours in small-group, case-based studies; 80 hours in classroom and lab<br />
time and another 432 hours supervising students’ early clinical contact, all<br />
<strong>of</strong> which takes place within the first two years <strong>of</strong> medical school.<br />
“This is so important, because (physicians) will encounter more and more<br />
elderly patients in every area <strong>of</strong> medicine,” Meyer says. Especially in primary<br />
care, she adds, the field <strong>of</strong> choice for 54 percent <strong>of</strong> OU-COM graduates.<br />
An unexpected calling<br />
Sarah Snyder, D.O. (’06), wasn’t exactly looking forward to her<br />
required geriatric medicine rotation three years ago. “(The rotation<br />
is) perceived as somewhat sad—not exciting like sports medicine or<br />
cardiology,” she says. “I thought I wasn’t going to like it.”<br />
Snyder originally planned to go into pediatrics. But that changed<br />
when she began her geriatrics rotation.<br />
“There was one patient I interviewed, a female in her 90s, very frail,”<br />
Snyder says, “She talked to me for about an hour about how her life is,<br />
how it used to be.”<br />
When Snyder stood to go, she says the patient began crying. “She<br />
just thanked me for listening to her. She said a lot <strong>of</strong> docs are in and<br />
out, and that I really made her feel listened to. Right there I thought,<br />
wow. This is it. This is my calling.”<br />
Snyder is currently a family medicine resident at Firelands Hospital<br />
in Sandusky, <strong>Ohio</strong>. She has completed three additional geriatric medicine<br />
out-rotations as a resident: at Akron City Hospital, the Mountain Area<br />
Health Education Center in Asheville, N.C., and Christ Hospital in<br />
Cincinnati, <strong>Ohio</strong>.<br />
Snyder also received eight weeks <strong>of</strong> hospice training this year.<br />
Next she plans to pursue a fellowship in geriatric medicine, followed<br />
by another in palliative care (non-curative medicine aimed at relieving<br />
pain and suffering) before becoming a full-time geriatrician.<br />
“That (initial required geriatrics) rotation is the whole reason I’m<br />
choosing geriatrics. It gave me a new respect for the field,” Snyder<br />
says. “I really thought the experience was much more in line with the<br />
osteopathic philosophy than a lot <strong>of</strong> my other rotations in terms <strong>of</strong><br />
treating the whole patient, physically, mentally and emotionally.”<br />
To illustrate the holistic approach to treating older adults, Snyder<br />
describes how, upon starting her residency in Akron, she was given<br />
a five-page questionnaire to go over with each new patient. It covers<br />
everything from medications, sleep patterns and diet to social habits,<br />
mood trends and living space.<br />
“I found that I really love home visits, seeing people in their own<br />
environment,” Snyder says. “Now I can’t imagine practicing medicine<br />
without understanding how patients function in their everyday lives.”<br />
8 ohio university medicine Winter 2009<br />
9
Embracing end-<strong>of</strong>-life care<br />
In addition to holistic care and human contact, Snyder’s passion for<br />
geriatric medicine is fueled by concerns about how the U.S. manages<br />
chronic illnesses and palliative care.<br />
“I think that particularly end-<strong>of</strong>-life issues are where we, as a medical<br />
pr<strong>of</strong>ession, fail,” Snyder says. “We’re taught to do everything possible at<br />
all times—that people aren’t supposed to die, which is ridiculous.”<br />
Snyder recalls a patient from her internal medicine rotation—for a<br />
month and a half he couldn’t breathe without a respirator, and he showed<br />
no signs <strong>of</strong> improvement. Snyder asked her attending physician at what<br />
point he planned to suggest hospice, an organization that helps patients<br />
with terminal conditions—and their families—to cope with the process.<br />
“He looked at me like he was insulted. He just said, ‘I’m not giving<br />
up,’” Snyder says. “No one would talk to this dying patient about<br />
hospice. I think a lot <strong>of</strong> docs feel like a failure when a patient dies—<br />
even with older patients. They’re just not willing to face it. As a result,<br />
patients suffer—and so do physicians.”<br />
Snyder believes that the inability <strong>of</strong> physicians to accept and cope<br />
with death contributes to the low popularity <strong>of</strong> geriatric medicine,<br />
where death rates are relatively high. She suggests that all medical<br />
schools provide training in death and dying.<br />
“There’s surprisingly little medical school preparation in this area,”<br />
says Tracy (Thompson) Marx, D.O. (’92), assistant pr<strong>of</strong>essor <strong>of</strong><br />
family medicine. “But (at OU-COM) we <strong>of</strong>fer a range <strong>of</strong> classroom<br />
and clinical training on death and dying, hospice and palliative care.”<br />
The curriculum integrates interactive and multimedia approaches,<br />
including a simulated patient lab on breaking bad news and the reading<br />
<strong>of</strong> Confessions <strong>of</strong> a Reluctant Caregiver, written by playwright Merri<br />
Biechler, M.F.A., evaluation assistant in the Office <strong>of</strong> Academic Affairs.<br />
Marx has noticed that patients increasingly expect better end-<strong>of</strong>life<br />
care, and she expects that trend to continue. “As baby boomers get<br />
older, they’ll demand better palliative care… We’re trying to dispel<br />
fears and myths about death and dying among our students.”<br />
Kyle Allen, D.O. (‘86), speaks with<br />
patient Gene Phillips at Cuyahoga<br />
Falls General Hospital.<br />
Advocating for change<br />
Kyle Allen, D.O. (’86), believes that the nation’s delayed reaction<br />
to the impending geriatric medicine workforce crisis reflects a “collective<br />
denial <strong>of</strong> aging and mortality.”<br />
“There’s still this fountain <strong>of</strong> youth concept, a kind <strong>of</strong> belief that<br />
death may actually be optional,” says Allen, medical director <strong>of</strong> post<br />
acute and senior services for the Summa Health System Division <strong>of</strong><br />
Geriatric Medicine.<br />
“Every airplane has its own flight plan—each one must descend<br />
at a different slope,” he says. “We all have our own way to land, so to<br />
speak, but we don’t do a good enough job <strong>of</strong> managing these natural<br />
trajectories <strong>of</strong> older patients or patients with chronic illnesses.”<br />
At any given time, one or two OU-COM students work with Allen<br />
in Cuyahoga Falls General Hospital, an affiliate hospital <strong>of</strong> Summa<br />
Health and a CORE teaching hospital, where Allen serves as clinical<br />
associate pr<strong>of</strong>essor <strong>of</strong> geriatric medicine. Summa has increased the<br />
geriatrics rotation from two to four weeks because <strong>of</strong> its robust<br />
teaching programs for aging and geriatric medicine, reflecting how<br />
much value Allen and his colleagues place on the field.<br />
“Training in the care <strong>of</strong> older adults must be more emphasized<br />
in medical and other allied health pr<strong>of</strong>essions,” Allen says, adding,<br />
“I believe OU-COM is ahead <strong>of</strong> most medical schools in that area.”<br />
Allen teaches students that the role <strong>of</strong> the geriatrician, and any<br />
doctor dealing with chronic conditions, is to optimize the “glide path.”<br />
This can be tricky business with elderly patients, as they frequently<br />
suffer from multiple, ongoing conditions.<br />
A 2000 survey found that nearly 70 percent <strong>of</strong> adults over the age<br />
<strong>of</strong> 65 report at least one chronic condition, with the highest numbers<br />
coming from Medicare beneficiaries. This creates a major problem<br />
when it comes to physician payment, Allen says, considering how<br />
Medicare reimbursements work.<br />
Medicare, like most third-party providers, pays physicians to<br />
perform procedures, such as colonoscopies, bypass operations or hip<br />
replacements. It won’t pay for preventive or ongoing managed care,<br />
that is: the time physicians spend assessing patients’ needs or talking<br />
to them about improving lifestyle trends.<br />
Summa<br />
“We need to realize that aging is a process, not an event, and we<br />
need to reform how we train—and how we compensate—physicians<br />
and other health pr<strong>of</strong>essionals so that they can manage that process<br />
proactively, not respond to events,” Allen says. “At Summa, we’re<br />
finding innovative ways to do that.”<br />
Summa Health System, a not-for-pr<strong>of</strong>it that includes six hospitals<br />
and eight medical centers in Northeastern <strong>Ohio</strong>, <strong>of</strong>fers its own<br />
insurance plan, SummaCare, to patients. This cuts out the thirdparty<br />
provider system, so instead <strong>of</strong> paying an insurance company’s<br />
administrative costs and additional fees—which factor in a 20 percent<br />
pr<strong>of</strong>it margin for stakeholders—extra money can be reinvested directly<br />
into the health system to improve medical service.<br />
As a result <strong>of</strong> this innovative provider model, Summa was one <strong>of</strong><br />
just four hospitals out <strong>of</strong> 3,700 nationwide picked by MedPAC, the<br />
Congressional advisory panel for Medicare, for further study on cost<br />
and quality.<br />
Allen, who also serves as chief medical <strong>of</strong>ficer for the Area Agency on<br />
Aging board <strong>of</strong> directors, devotes a great deal <strong>of</strong> pr<strong>of</strong>essional energy toward<br />
reforming health care policy, particularly for older adults. He directs the<br />
new geriatric medicine fellowship at Summa Health, and he recently<br />
began a fellowship <strong>of</strong> his own. He was accepted into the Practice Change<br />
Fellow Program, designed to expand and improve leadership in promoting<br />
quality care to older adults. These efforts help to inform his research; he is<br />
currently the principal investigator for two National Institutes <strong>of</strong> Health<br />
grants studying innovative care models for older adults.<br />
“I’m motivated by being an agent <strong>of</strong> change,” Allen says. “I think<br />
that my training at OU-COM reinforced that. It’s what osteopathic<br />
medicine is all about. Dr. (Andrew Taylor) Still was an advocate for<br />
change because he saw that the current system didn’t work. When<br />
geriatricians are paid less for more training; when insurance creates<br />
disincentives for higher quality care—we need to recognize what<br />
doesn’t work about the current system and work toward change.”<br />
AIDS and aging<br />
People with HIV or AIDS are living longer,<br />
and now with higher rates <strong>of</strong> diagnosis among<br />
those over 50, Timothy Heckman, Ph.D.,<br />
realized that “we need to assess the psychological<br />
needs <strong>of</strong> older adults (with HIV/AIDS).”<br />
To do so, the pr<strong>of</strong>essor <strong>of</strong> geriatric medicine/<br />
gerontology secured a four-year NIH grant in<br />
2006. Heckman recently published the results<br />
<strong>of</strong> a study on the benefits <strong>of</strong> telephone support<br />
groups for older adults with HIV or AIDS who<br />
suffer depression.<br />
About 35 percent <strong>of</strong> older adults with HIV live<br />
alone. Many “don’t feel connected to the older<br />
community because <strong>of</strong> their HIV-positive status,”<br />
Heckman says. Telephone support groups<br />
provide community with anonymity.<br />
“By 2015 half <strong>of</strong> all new (U.S.) HIV cases will<br />
be in people over 50.” Heckman says, citing<br />
higher divorce rates, erectile dysfunction<br />
drugs, increased vaginal tearing in older<br />
women, and <strong>of</strong>ten misinformed attitudes<br />
toward safe sex.<br />
Heckman’s next study will involve 200<br />
participants nationwide. His goal: “identify<br />
intervention programs that work, and help<br />
communities implement them.”<br />
OUM<br />
Read the full story at<br />
www.oucom.ohiou.edu/oum.<br />
10 ohio university medicine<br />
Students interview Parkinson’s<br />
simulation patient caretaker<br />
Rosemary Huntsman.<br />
11
Feature<br />
“Whenever possible we want<br />
to keep someone in practice or<br />
restore them to practice, while<br />
ensuring public safety first and<br />
foremost… It’s in everyone’s<br />
interest to rehabilitate and retain<br />
qualified medical pr<strong>of</strong>essionals<br />
when we can—as long as we’re<br />
sure the public will be protected.”<br />
–Rick Whitehouse, Esq., executive director<br />
<strong>of</strong> the State Medical Board <strong>of</strong> <strong>Ohio</strong><br />
First: Do no harm<br />
OU-COM teams up with State Medical Board to train ethical physicians<br />
By Anita Martin<br />
Photos by John Sattler<br />
“This is an example <strong>of</strong> how<br />
proactive OU-COM is in its<br />
instruction. They really want us<br />
to be aware <strong>of</strong> all the aspects <strong>of</strong><br />
the medical pr<strong>of</strong>ession.”<br />
Soon after receiving their short white coats, the class <strong>of</strong> 2012 will<br />
do something they had hoped to avoid throughout their careers: appear<br />
before the State Medical Board <strong>of</strong> <strong>Ohio</strong> (SMB).<br />
Each month, as part <strong>of</strong> OU-COM’s Partners in Pr<strong>of</strong>essionalism<br />
Series, a small group <strong>of</strong> first-year students attends a Columbus board<br />
meeting, where they observe errant physicians defending their licenses.<br />
The partnership—the first <strong>of</strong> its kind in <strong>Ohio</strong> and among few<br />
nationwide—was launched in fall 2007.<br />
“It’s all about pr<strong>of</strong>essionalism,” says Dean Jack Brose, D.O.<br />
“Students should know policies and requirements so they can avoid<br />
violations. But we also want them to understand that the board is there<br />
to help physicians and improve public health care.”<br />
This exercise in real-life ethics <strong>of</strong>fers moments <strong>of</strong> poignant,<br />
unscripted education. At one recent meeting, a probationer stood<br />
before the board. To fuel his workaholic lifestyle, the physician—<br />
who managed emergency medicine full time at one hospital and<br />
moonlighted at three others—began abusing the prescription drug<br />
Ritalin. During his statement, he turned to speak directly to the whiteclad<br />
OU-COM students at the back <strong>of</strong> the room.<br />
“This has been an essential education for me,” he said, referring to<br />
his probation and rehabilitation. “I still love the ER, but life is not only<br />
about being a doctor. That job is to be taken seriously, but you have to<br />
live a balanced lifestyle.”<br />
The State Medical Board hopes to expand educational partnerships<br />
in <strong>Ohio</strong>. With limited seating at meetings, the SMB is looking into<br />
electronic resources, such as videotaping sessions, for distribution<br />
among state medical schools.<br />
Medical students may be years from licensure, but board member<br />
Anita Steinbergh, D.O., insists it’s never too early to think about<br />
pr<strong>of</strong>essionalism and ethics. “We’re very focused on the needs <strong>of</strong> young<br />
people in medicine and preventing them from getting into trouble. This<br />
(partnership) is a great opportunity to make a difference in their lives.”<br />
Top right: (From left) Rick Whitehouse, executive board director;<br />
Joan Wehrle, executive board staff coordinator; Anthony Posevitz,<br />
OMS II; Diana Haninger, OMS II; and Steven Baird, OMS II.<br />
Left: Board member Anita M. Steinbergh, D.O., and<br />
Board President Nandlal Varyani, M.D.<br />
Bottom right: Joan Wehrle, SMB staff coordinator, speaks to<br />
first-year OU-COM students about the State Medical Board.<br />
–Anthony Posevitz, OMS II<br />
12 ohio university medicine
Amesville Elementary students<br />
Feature<br />
Fit kids, fit<br />
communities<br />
Through education and perspiration, OU-COM<br />
tackles the intricacies <strong>of</strong> childhood obesity<br />
By Mary Reed<br />
Photos by Kevin Riddell<br />
Several kids, aged 12 to 17, stand in the dairy aisle <strong>of</strong> the Athens<br />
Kroger grocery store. Four kids grab a different half-gallon <strong>of</strong> milk:<br />
whole, two percent, one percent and skim. They read aloud nutrition<br />
labels to compare similarities (vitamins, mostly) and contrast fat<br />
content. Skim is pronounced the winner.<br />
Andrew Wapner, D.O., assistant pr<strong>of</strong>essor <strong>of</strong> pediatrics, points out<br />
that whole milk is packaged under the name “fortified milk”. “Every time<br />
you get smarter, [food corporations] try to get smarter than you,” he<br />
says, encouraging them to keep reading labels.<br />
It’s week four <strong>of</strong> the eight-week Take Action program, OU-COM’s<br />
supervised intervention study to teach healthy diet and exercise habits<br />
to Athens County children diagnosed as overweight or obese—and<br />
their parents, who are in a separate group on the other side <strong>of</strong> the store.<br />
Participants meet twice a week for two-hour sessions, the first hour<br />
focusing on nutrition—food choices, nutrients, serving sizes—and the<br />
second on aerobic and anaerobic exercise at the Athens Community Center.<br />
“As a doctor, I <strong>of</strong>ten see people with complaints that are a result <strong>of</strong> an<br />
overall unhealthy lifestyle,” Wapner says. In his Athens and Belpre, <strong>Ohio</strong>,<br />
practices, Wapner gets frequent referrals <strong>of</strong> overweight and obese children<br />
at risk for diabetes. As someone passionate about nutrition and exercise,<br />
Wapner jumped at the opportunity to more actively engage families. “ We<br />
know that just hearing a doctor say, ‘eat right and exercise,’ doesn’t work.”<br />
According to the Centers for Disease Control and Prevention, obesity<br />
rates for children 12-19 rose from five percent between 1976 and 1980 to<br />
17.4 percent by 2003-2004. For children 6-11, that figure went from 6.5<br />
percent to 18.8 percent in the same time. Although recent figures show<br />
rates leveling <strong>of</strong>f, childhood obesity is still an epidemic. And according to<br />
Thomson Medstat research, national childhood obesity costs about $11<br />
billion for insured children and $3 billion for those with Medicaid.<br />
To assess the local situation, Karen Montgomery-Reagan, D.O.,<br />
F.A.C.O.P., visited 11 Athens County elementary schools between May<br />
2005 and May 2006 to measure the body mass index (weight divided<br />
by height) <strong>of</strong> 1,600 children 6-12. Her study, funded by the Centers for<br />
<strong>Osteopathic</strong> Research and Education (CORE), provides a baseline for<br />
local childhood weight studies.<br />
Children at or above the 95 th percentile <strong>of</strong> weight for their age and<br />
height are considered obese. Those at or above the 85 th percentile are<br />
considered overweight. Only three <strong>of</strong> the 11 schools had obesity rates<br />
lower than the national average; not one had lower overweight rates. To<br />
take an extreme example, at Federal Hocking Elementary School, 30.7<br />
percent <strong>of</strong> students are obese. The national average is 19.4 percent.<br />
With obesity comes higher risk for type 2 diabetes. According to the<br />
Appalachian Rural Health Institute, 11.3 percent <strong>of</strong> adults and children<br />
in ARHI’s Southeastern <strong>Ohio</strong> coverage area have diabetes. Compare that<br />
to the <strong>Ohio</strong> rate, 7.8 percent, and the national rate, 7.2 percent.<br />
What explains the dramatic rise in obesity, especially in Appalachian <strong>Ohio</strong>?<br />
Wapner lists a few causes: lack <strong>of</strong> ballfields, playgrounds and other safe places<br />
for kids to play, car-centered transportation, crop subsidies that encourage<br />
high-fructose corn syrup, sedentary lifestyles, fast food … the list goes on.<br />
Wapner says his research and his practice inform his pediatrics<br />
lectures to OU-COM students. “I teach a lot more about screening for<br />
weight-related issues and nutritional concerns, mostly based on what I<br />
have seen,” he says.<br />
Finding what works – and what doesn’t<br />
Results from last year’s inaugural Take Action program were<br />
promising: fitness levels (measured by exercise tests) increased in<br />
all participants, waist circumference decreased in adolescents, and<br />
triglycerides (a type <strong>of</strong> fat in the blood) decreased in adults.<br />
But challenges remain. For parent Vivian Taylor, who talks about<br />
Take Action as the group walks from Kroger to the community center,<br />
fast food is the problem. “I love eating out,” she says, counting the Wendy’s<br />
Baconator as her favorite fast food. “(The researchers) said it was probably<br />
the worst thing you can eat.” Now she buys the chicken wrap.<br />
“I wanted to lose weight, but the program is not geared toward<br />
that,” Taylor says, repeating the mantra <strong>of</strong> Take Action physicians,<br />
nutritionists and exercise physiologists. Almost everyone today says it<br />
at some point: Take Action is a healthy lifestyle program, not a weight<br />
loss program. But Taylor has enjoyed many benefits <strong>of</strong> the program,<br />
Trans-Atlantic ties<br />
According to Gabriel Martos-Moreno,<br />
M.D., Ph.D. (above), visiting pr<strong>of</strong>essor and<br />
Take Action co-investigator, childhood<br />
obesity in his native Spain has tripled over<br />
the last 20 years from five to 15 percent.<br />
After meeting John Kopchick, Ph.D., Goll-<br />
<strong>Ohio</strong> Eminent Scholar and pr<strong>of</strong>essor <strong>of</strong><br />
molecular and cellular biology, Martos-<br />
Moreno secured a grant from the Spanish<br />
government to research childhood obesity<br />
and diabetes at OU-COM for ten months.<br />
“I came here with one project proposal: to<br />
identify potential biomarkers for obesity,”<br />
he says, adding with a laugh, “But there is<br />
so much going on here; now I’m involved<br />
with four related projects.”<br />
Martos-Moreno is comparing three sets <strong>of</strong><br />
blood samples: those <strong>of</strong> obese and healthy<br />
Spanish children, those <strong>of</strong> obese children<br />
with and without insulin resistence, and<br />
those <strong>of</strong> children before and after weight<br />
loss. For the last set he uses samples from<br />
his Spanish patients and from Take Action<br />
participants. He also works with Kopchick<br />
to study differences in surface fat tissue<br />
across the human body.<br />
In November, Martos-Moreno returned<br />
to Spain, where he will continue<br />
collaborating with OU-COM.<br />
OUM<br />
Read the full story at<br />
www.oucom.ohiou.edu/oum.<br />
14 ohio university medicine Winter 2009<br />
15<br />
Teresa Stamplis, OMS II
Molly Malone-Prioleau, OMS II,<br />
and Jay Shubrook, D.O. (’96).<br />
Follow-up<br />
including weight loss. “I can fit into my wedding band (again).”<br />
Taylor’s daughter, Riley, is walking with a pedometer. She’s taken<br />
2,190 steps today—or at least since the last time it fell <strong>of</strong>f, she says.<br />
Researchers have tracked the average American at 5,000 steps a day;<br />
10,000 is recommended. Take Action participants get pedometers as<br />
homework, along with a food log and a portion plate. Most participants<br />
were surprised to learn about their own “portion distortion,” including<br />
how much sugar and sodium was in their diet.<br />
Participants take home more than just tips and tasks—they receive<br />
vouchers for gas and for the Athens Farmers Market and passes to the<br />
community center gym. But in the case <strong>of</strong> the Taylor family, a 60-mile<br />
round trip from their rural Athens County home drastically reduces<br />
the value <strong>of</strong> those vouchers.<br />
Take Action researchers attribute 2008’s faltering recruitment<br />
primarily to high gas prices. Another challenge is child care. Today,<br />
some parents have brought children who are not part <strong>of</strong> the study,<br />
which is not allowed, but it’s either that or don’t come.<br />
“There are cracks at every level,” says Wapner, whose goal is as simple<br />
as it is daunting: “Fit a healthy kid into a healthy family into a healthy<br />
community.” Wapner and his colleagues hope this year’s program—<br />
funded by OU-COM’s Research and Scholarly Affairs Committee and<br />
the Department <strong>of</strong> Family Medicine, as well as the Athens Foundation<br />
and the American Association <strong>of</strong> Family Practitioners—will draw<br />
funding for a school-based prevention program modeled on Take Action.<br />
“I think the prevention <strong>of</strong> obesity is much more effective than the<br />
treatment <strong>of</strong> obesity,” says Jay Shubrook, D.O. (’96), co-principal<br />
investigator <strong>of</strong> Take Action and assistant pr<strong>of</strong>essor <strong>of</strong> family medicine.<br />
Shubrook adds that long-term sustainability will be the ultimate test.<br />
The researchers have given this year’s participants yearlong passes to the<br />
Athens Community Center and will monitor whether they continue their<br />
workouts without supervision. “It works as long as you do it,” he notes.<br />
Involving families and schools<br />
Fredrick (Fritz) Hagerman, Ph.D., pr<strong>of</strong>essor <strong>of</strong> physiology, never<br />
sits for long. The 70-something seems to exude more energy than the<br />
seven- and eight-year-olds from his study titled “Exercise and Nutrition<br />
Intervention Study <strong>of</strong> Rural Appalachian Schoolchildren”.<br />
Hagerman and his colleagues—pr<strong>of</strong>essors and students—completed<br />
the 16-week study at two Athens County elementary schools between<br />
January and May 2006. The control school, Coolville Elementary,<br />
received no intervention. The experimental group, Amesville<br />
Elementary, engaged in supervised exercise and nutrition lessons.<br />
(Montgomery-Reagan’s study showed 22 percent <strong>of</strong> students at both<br />
schools were overweight.)<br />
The researchers brought rowing machines, donated by Concept2<br />
Rowing, to the school. Students used their physical education class period<br />
to row, and both they and their parents received nutrition lessons.<br />
The outcomes were dramatic. By the end <strong>of</strong> the study, children in the<br />
experimental group were making better food choices and exercising with<br />
more strength and efficiency, measured by power generation and oxygen<br />
consumption. Most strikingly, over the course <strong>of</strong> 16 weeks, body fat in<br />
the control group increased from 8.8 percent to 10.1 percent. In the<br />
experimental group, body fat decreased from 8.4 percent to 7.8 percent.<br />
It turns out that intervening with younger children might be a key to<br />
success. As Montgomery-Reagan’s figures show, many kids are already<br />
obese by the time they’re 11 or 12. At that point, it’s too late for prevention.<br />
The question remains whether short-term interventions can have<br />
long-term effects. Hagerman’s colleagues plan to annually retest the<br />
students’ body mass index and body fat until they graduate from high<br />
school to find out. But the obstacles are daunting. Hagerman points out<br />
that physical education is <strong>of</strong>ten inadequate; many students no longer<br />
walk to school; and, <strong>of</strong> course, school lunches and vending machines<br />
make it difficult for students to make good food choices.<br />
“Are schools trying to do something about it? Sure,” Hagerman says.<br />
He points to California’s ban on vending machines in its public schools.<br />
But where did much <strong>of</strong> the proceeds from the vending machines go? To<br />
the schools. “You’re sort <strong>of</strong> damned if you do, damned if you don’t.”<br />
But on Hagerman’s <strong>of</strong>fice door hangs a sign <strong>of</strong> hope. It’s a twopaneled<br />
poster hand-drawn by one <strong>of</strong> the children in his study. The first<br />
panel, titled “Old Travis,” shows a boy with a frown standing by a table<br />
with a box <strong>of</strong> donuts. In the second panel, “New Travis” is smiling, and<br />
the table next to him, laden with fruits and vegetables.<br />
18<br />
20<br />
21<br />
22<br />
23<br />
24<br />
Going to extremes<br />
Stephen Augustine, D.O.<br />
Dr. Augustine serves motorized extreme sports<br />
athletes through track-side medical care.<br />
Class notes<br />
Bill Burke, D.O., in China<br />
AOA Mentor Hall <strong>of</strong> Fame<br />
Calendar <strong>of</strong> events<br />
Gumption and goodwill<br />
Georgenna Riley, D.O.<br />
Dr. Riley and others support OU-COM<br />
with endowed medical scholarships.<br />
OU-COM Construction<br />
then and now<br />
Top left: 1982 construction site <strong>of</strong> Irvine<br />
lecture halls<br />
Below: Members <strong>of</strong> the OU-COM Society<br />
<strong>of</strong> Alumni and Friends Board tour the<br />
Academic & Research Center (ARC) during<br />
their October meeting. The ARC will bring<br />
together researchers from OU-COM, Russ<br />
<strong>College</strong> <strong>of</strong> Engineering and Technology, and<br />
other colleges and institutions on campus<br />
for the development <strong>of</strong> new diagnostics and<br />
treatments.<br />
Development & Alumni News and Features<br />
16 ohio university medicine Winter 2009<br />
17
Georgenna Riley, D.O., with<br />
LaQuita Jones, OMS I<br />
Follow-up<br />
Follow-up<br />
Development Highlight<br />
Gumption<br />
and goodwill<br />
Dr. Georgenna Riley blazed her own trail. Now<br />
she helps others do the same through an<br />
endowed minority scholarship.<br />
By Susie Shutts<br />
Photos by John Sattler<br />
Growing up in the Appalachian foothills <strong>of</strong> a small Kentucky town,<br />
Georgenna Riley, D.O. (’95), had an uncommon dream.<br />
“I always wanted to be a scientist,” says Riley—though most female<br />
pr<strong>of</strong>essionals she knew at the time were either secretaries or teachers.<br />
Riley, now head <strong>of</strong> the radiology department at Kaiser Permenante<br />
in Cleveland, came to OU-COM encouraged by her mother, who<br />
in her late thirties earned her high school diploma and took postsecondary<br />
classes, and her stepfather, a tailor, to whom “education was<br />
very important,” Riley says.<br />
Her path, however, took a few more turns than the typical medical<br />
student. She first earned a degree in dentistry at the <strong>University</strong> <strong>of</strong><br />
Kentucky. Then, after practicing as a dentist for ten years in the<br />
Washington, D.C., area, Riley had a change <strong>of</strong> heart.<br />
“I’d always had an interest in medicine,” Riley says. “I wanted more<br />
opportunities to help people.”<br />
Riley wasn’t initially drawn to analytical field <strong>of</strong> radiology, but after<br />
exploring the specialty in her residency at Ruby Memorial Hospital<br />
in West Virginia, she was hooked. The field’s variety and constant<br />
innovations resonated with her personality.<br />
Riley’s ability to adapt to change and overcome adversity helped her a<br />
few years ago, when her mother died <strong>of</strong> ovarian cancer. Riley channeled<br />
her grief into purpose. “It made me more proactive with encouraging<br />
preventive measures,” Riley said. Her loss prompted an interest in the<br />
relationship among diet, exercise and disease. She constantly tracks<br />
research on the subject, sharing information with patients along the way.<br />
The experience also deepened her commitment to her family. Riley<br />
grew up one <strong>of</strong> ten children, including three—yes, three—sets <strong>of</strong><br />
twins. Riley shares the values driving her twin sister, Georgetta, who<br />
retired last year after working 28 years as a warden at the Federal<br />
Medical Center, a Lexington, Ky., a federal prison specializing in<br />
psychiatric care. “We both work with people to help them better their<br />
lives,” Riley says.<br />
To this end, Riley recently endowed the Georgenna Riley, D.O.<br />
(’95), <strong>Osteopathic</strong> Minority Medical Scholarship, a new OU-COM<br />
scholarship for underrepresented minority students who reflect<br />
leadership skills and/or research activities. Riley hopes the scholarship<br />
will inspire others to pay forward to future generations. She describes<br />
recipients as students “who got into medicine because they really want<br />
to help people.”<br />
To fund her own medical education, Riley “took out loans and<br />
earned scholarships,” says Pat Burnett, Ph.D., director <strong>of</strong> student<br />
affairs. “She didn’t have rich parents or a lot <strong>of</strong> savings.”<br />
Burnett describes Riley as a caring individual, who <strong>of</strong>ten calls<br />
“to check up on us” in the Office <strong>of</strong> Student Affairs. “She’s just very<br />
generous,” Burnett says. “She lives by a notion <strong>of</strong> reciprocity. She’s told<br />
me, ‘I’m making money now, and I want to give back.’”<br />
Riley joined the OU-COM Alumni Board three years ago, where<br />
she has put these words into action through both her endowed<br />
scholarship and generous contributions to the upcoming Academic &<br />
Research Center (ARC), a joint project <strong>of</strong> OU-COM and the Russ<br />
<strong>College</strong> <strong>of</strong> Engineering and Technology.<br />
Early last month, OU-COM awarded the inaugural Riley<br />
Scholarship to LaQuita Jones, OMS I, a Warrensville Heights native<br />
who participated in OU-COM’s Post-Baccalaureate Program, a yearlong<br />
training program focused on increasing medical school access for<br />
both economically disadvantaged students from Appalachian <strong>Ohio</strong><br />
and underrepresented minority students.<br />
“Being a first-generation college student, I do not have family<br />
members who can relate to my pursuing a career in medicine,” Jones<br />
says. “It’s great to know someone like Dr. Riley, who has been through<br />
this journey and has been successful.”<br />
Sharon Zimmerman, M.P.A.<br />
Director <strong>of</strong> Medical Development<br />
Executive Director <strong>of</strong> Alumni Affairs<br />
Medical scholarships:<br />
Attracting the best and brightest<br />
An investment in scholarships is an investment in the college’s most precious<br />
resource: its students. OU-COM depends largely on private support to attract the<br />
brightest, most promising young people who will be tomorrow’s physicians—our<br />
future alumni—and also to ensure that their dream <strong>of</strong> becoming a physician is<br />
within financial reach.<br />
Each year, approximately 400 students compete for OU-COM’s 40 scholarships.<br />
Scholarships help narrow the gap between awards requested and those granted.<br />
When we cannot <strong>of</strong>fer enough financial aid, we sometimes lose talented applicants<br />
because they simply cannot afford the expenses associated with medical education<br />
and training.<br />
Our Student Affairs staff members work diligently with our students, advising them<br />
on how to incur the least-possible medical school debt. Still, tuition and fees have<br />
risen more than 100 percent in the past decade, due in large part to steady cuts<br />
in government funding, and living expenses continually increase. As a result, the<br />
average debt <strong>of</strong> our most recent graduates has increased from $89,182 in 1999 to<br />
$150,868 for the class <strong>of</strong> 2008, even though our college tuition ranks among the<br />
lowest <strong>of</strong> all seven medical schools in <strong>Ohio</strong>.<br />
Scholarships change lives by making medical school financially possible. If you<br />
would like to help, I am always happy to talk about how you can contribute to an<br />
existing scholarship or even start your own osteopathic scholarship in your name or<br />
the name <strong>of</strong> a mentor or loved one.<br />
Your generosity means a lot to our students. We are pleased to announce the<br />
establishment <strong>of</strong> these new 2007-2008 OU-COM Scholarships:<br />
Austin-Bailey Health and Wellness<br />
Foundation Gerald L. Meck <strong>Osteopathic</strong><br />
Student Scholarship<br />
*Auxiliary to the 9 th District Academy, <strong>Ohio</strong><br />
<strong>Osteopathic</strong> Association Scholarship<br />
*Barbara A. Bennett, D.O. (’84), <strong>Osteopathic</strong><br />
Medical Scholarship<br />
*Michael E. (’83) and Ruth Campolo<br />
<strong>Osteopathic</strong> Medical Scholarship<br />
*Chang Ying-Chien <strong>Osteopathic</strong> Medical<br />
Scholarship<br />
*Alison A. Clarey, D.O., FACOS <strong>Osteopathic</strong><br />
Medical Scholarship<br />
The Cleveland Foundation <strong>Osteopathic</strong><br />
Medical Scholarship<br />
*Mae F. and A.R. Harmon Memorial<br />
Scholarship in <strong>Osteopathic</strong> Medicine<br />
*Robert S. Harris, D.O. (’82), <strong>Osteopathic</strong><br />
Memorial Scholarship<br />
*The Holzer Clinic Scholarships<br />
Northeastern <strong>Ohio</strong> Healthcare Foundation,<br />
Cpl. Joshua Harmon Memorial <strong>Osteopathic</strong><br />
Scholarship<br />
*Georgenna Riley, D.O. (’95), <strong>Osteopathic</strong><br />
Minority Scholarship<br />
*Geraldine N. Urse, D.O. (‘93), FACOFP<br />
and John S. Urse, Jr., D.O. (‘92), FACOS,<br />
<strong>Osteopathic</strong> Medical Scholarship<br />
*Endowed scholarships<br />
18 ohio university medicine Winter 2009<br />
19
Follow-up<br />
We want to hear from you!<br />
Follow-up<br />
Class Notes<br />
Please send your career and<br />
personal updates for our next issue.<br />
Fax: 740.593.0761<br />
E-mail: harmanj@ohio.edu<br />
Online form: www.oucom.ohiou.edu/Alumni/<br />
StayingConnected.htm<br />
Alumni Affairs, 203 Grosvenor Hall, Athens, <strong>Ohio</strong>, 45701<br />
1980<br />
MacGregor E. Poll, D.O., medical director at<br />
Northridge Surgery Center in Madison, Tenn.,<br />
and his wife, Nancy, welcomed their first grandchild<br />
in November 2007.<br />
1982<br />
John J. Koncelik, D.O., is pursuing his<br />
master’s degree in medical management from the<br />
<strong>University</strong> <strong>of</strong> Southern California’s Marshall School<br />
<strong>of</strong> Business. In 2006, Dr. Koncelik became CEO/<br />
president <strong>of</strong> Western Pennsylvania Anesthesia<br />
Associates in Pittsburgh, Penn.; medical director <strong>of</strong><br />
Sheridan Clinical Research, Inc., in Sunrise, Fla.,<br />
and a certified physician investigator (CPI). He<br />
continues his clinical research at Sewickley Valley<br />
Hospital in Pennsylvania.<br />
1983<br />
Michael J. Dobrovich, D.O., was elected chief<br />
medical <strong>of</strong>ficer and senior vice president <strong>of</strong> clinical<br />
affairs <strong>of</strong> St. John West Shore Hospital in Westlake,<br />
<strong>Ohio</strong>, in March 2007.<br />
1984<br />
Barbara Bennett, D.O., was appointed president<br />
<strong>of</strong> the <strong>Ohio</strong> <strong>Osteopathic</strong> Association at the 110th<br />
OOA annual convention in June.<br />
1986<br />
Kyle R. Allen, D.O., became a Practice Change<br />
Fellow in 2007. The fellowship works to improve<br />
medical care for older adults.<br />
Gregory Hill, D.O., received a Meritorious Service<br />
Medal in December 2005, during Operation Iraqi<br />
Freedom. He also presented a paper, “Volar fixation<br />
<strong>of</strong> distal radius function: Comparison <strong>of</strong> systems,” in<br />
May 2007 at the American <strong>Osteopathic</strong> Academy<br />
<strong>of</strong> Orthopedics Postgraduate Seminar.<br />
1987<br />
Doris T. Tan, D.O., coauthored the Handbook<br />
<strong>of</strong> Emergency Psychiatry in 2007. She is a clinical<br />
pr<strong>of</strong>essor <strong>of</strong> psychiatry at the <strong>University</strong> <strong>of</strong><br />
California, San Francisco—Fresno.<br />
1988<br />
Katherine (Toni) Clark, D.O., clinical pr<strong>of</strong>essor<br />
at Grandview Medical Center, received the 2008<br />
<strong>Ohio</strong> State Society <strong>of</strong> American <strong>Osteopathic</strong> Family<br />
Physicians Distinguished Service Award. She also<br />
helped establish a scholarship for OU-COM family<br />
medicine primary care fellows who choose to enter a<br />
family medicine residency program.<br />
Christopher Loyke, D.O., clinical associate pr<strong>of</strong>essor<br />
at South Pointe Hospital, is now president-elect <strong>of</strong><br />
the <strong>Ohio</strong> <strong>Osteopathic</strong> Association.<br />
1989<br />
Sandy Paul Naples, D.O., was re-elected as<br />
department chair <strong>of</strong> family medicine at St. Elizabeth<br />
Health Center in Youngstown, <strong>Ohio</strong>, for the<br />
2008-2010 term.<br />
1990<br />
Nicholas Espinoza, D.O., CORE assistant dean<br />
at St. Vincent Mercy Medical Center received the<br />
2008 Outstanding Preceptor <strong>of</strong> the Year Award.<br />
1991<br />
B. J. (Morill) Sidari, D.O., has joined Euclid<br />
Pediatrics in Euclid, <strong>Ohio</strong>.<br />
1992<br />
Joette E. Greenstein, D.O., joined Geriatric<br />
Physician Associates <strong>of</strong> Mount Carmel Health<br />
Providers in Columbus, <strong>Ohio</strong>, as director <strong>of</strong> house<br />
call services in August 2007.<br />
1993<br />
Todd R. Fredricks, D.O., completed his 2nd tour<br />
<strong>of</strong> duty in Tikrit, Iraq, in May 2008, and is now an<br />
assistant pr<strong>of</strong>essor <strong>of</strong> family medicine at OU-COM.<br />
1994<br />
Michele (Brown) Keller, D.O., accepted a position<br />
in April 2007, with Visiting Physicians, Inc., in<br />
Youngstown, <strong>Ohio</strong>.<br />
1995<br />
Joseph Looby, D.O., and his wife, Megan Elizabeth,<br />
welcomed their third child, Katherine, in May 2006,<br />
and their fourth child, Joseph, in July 2007. Dr.<br />
Looby is pursuing a fellowship in crani<strong>of</strong>acial plastic<br />
surgery at Stanford <strong>University</strong>.<br />
Chau Pham, D.O., and her husband, Frank<br />
Nguyen, welcomed their daughter, Angelina Quynh<br />
Chau Nguyen, in April 2007. She also recently<br />
opened a private practice.<br />
Tuesdae (Rogers) Stainbrook, D.O., was given<br />
the 2007 Award <strong>of</strong> Excellence at the Pennsylvania<br />
Annual Viral Hepatitis Conference in Monroeville,<br />
Penn., in October 2007.<br />
1996<br />
David A. Burke, D.O., and his wife, Jennifer, welcomed<br />
baby Aidan Thomas in November 2006.<br />
Daniel Culver, D.O., and wife, JoAnna, welcomed<br />
their third child, Josie, in February 2006.<br />
Deborah (Nicklas) Snyder, D.O., published Keto<br />
Kid: Helping Your Child Succeed on the Ketogenic Diet<br />
in 2006. She and her husband, Jeff, welcomed their<br />
third child, Abbey, in 2006.<br />
1997<br />
Sanjiv Amin, D.O., and wife, Seema, welcomed<br />
Reyna Amin to the family. She was born in June 2006.<br />
Larry Witmer, D.O., and his wife, Maria,<br />
welcomed daughter Lana in January 2007.<br />
1998<br />
Anthony Degenhard, D.O., was elected treasurer<br />
<strong>of</strong> the Aultman Medical Staff in December 2007,<br />
and has been certified by the American Society <strong>of</strong><br />
Diagnostic and Interventional Nephrology. He and<br />
his wife, Elizabeth, welcomed daughter Ella in<br />
April 2007.<br />
Deborah (Daniel) Harris, D.O., has been named<br />
chief <strong>of</strong> surgery at Selby General Hospital in<br />
Marietta, <strong>Ohio</strong>.<br />
Elizabeth North, D.O., and her husband, Robert<br />
Channler, welcomed baby Graham Channler in<br />
September 2006. She also completed a stroke<br />
fellowship at Oregon Health and Science<br />
<strong>University</strong> in Portland, where she opened a private<br />
neurology practice.<br />
1999<br />
Jeanne (Friedman) Crump, D.O., and her<br />
husband, Donald, adopted an infant son from<br />
Guatemala in September 2006. The baby, Gabriel,<br />
was born in March 2006.<br />
Andrew K. Culver, D.O., accepted a position as<br />
CORE assistant dean at Affinity Hospital in Akron,<br />
<strong>Ohio</strong>, in 2006.<br />
Joseph A. Rodrigo, D.O., director <strong>of</strong> regional<br />
anesthesia at Roper Medical Office, became boardcertified<br />
in anesthesiology in 2006.<br />
Provided by Dr. William Burke<br />
Burkes lend a hand in China<br />
Last spring, William Burke, D.O. (’88), associate<br />
pr<strong>of</strong>essor <strong>of</strong> family medicine, and his wife, Debbie,<br />
were planning a humanitarian trip to China with Heart<br />
to Heart International. He would continue his recent<br />
work training primary care physicians and she would<br />
assist a school for the deaf and a senior center.<br />
Then, ten days before their departure, the May 12<br />
earthquake struck the Sichuan province, killing or<br />
injuring hundreds <strong>of</strong> thousands and leaving millions<br />
homeless. The Burkes instead set up tents for displaced<br />
families and distributed food and medical supplies. It<br />
was Dr. Burke’s third trip to China and Ms. Burke’s first.<br />
“It’s more devastated than I imagined,” Ms. Burke<br />
told NPR’s Andrea Hsu during an on-site report.<br />
“But I’ve also seen that the spirit <strong>of</strong> the people<br />
is incredible.”<br />
Dr. Burke has since returned to China, twice, to<br />
counsel physicians and health ministries on primary<br />
care practices, equipment and training standards.<br />
In July, he presented on family practice residency<br />
training at a Chinese Medical Doctor’s Association<br />
conference in Nanjing. “I’m working to assist the<br />
The Burkes with a local mother and baby,<br />
whom Bill had just treated for mosquito bites.<br />
country’s transformation from a specialty-driven<br />
medical system to one more focused on primary<br />
care,” he says.<br />
Dr. Burke’s efforts are supported by the American<br />
<strong>Osteopathic</strong> Foundation and the American<br />
<strong>Osteopathic</strong> Association. Dr. Burke plans to bring a<br />
group <strong>of</strong> Chinese physicians to <strong>Ohio</strong> to demonstrate<br />
primary care training at OU-COM and the CORE.<br />
Dr. Burke also notes that his and Ms. Burke’s<br />
experience in May sparked an interest in continuing<br />
relief work. “The people were so welcoming and<br />
grateful. Because <strong>of</strong> that, we both feel that we got<br />
more out <strong>of</strong> the experience than we gave.”<br />
Dr. Burke is a family physician with Doctors Hospital, where<br />
he directs the Family Practice Residency Program. He<br />
previously served as president <strong>of</strong> the OU-COM Society <strong>of</strong><br />
Alumni and Friends, an <strong>Ohio</strong> <strong>University</strong> Foundation trustee<br />
and an AOA delegate. Ms. Burke graduated in 1985 from the<br />
Russ <strong>College</strong> <strong>of</strong> Engineering and Technology. She serves on<br />
the <strong>Ohio</strong> <strong>University</strong> Alumni Association Executive Committee<br />
and chairs the Russ <strong>College</strong> Board <strong>of</strong> Visitors.<br />
By Anita Martin<br />
20 ohio university medicine<br />
Winter 2009<br />
21
Follow-up<br />
Follow-up<br />
2009 Alumni Calendar <strong>of</strong> Events<br />
OU-COM alumni make the<br />
AOA Mentor Hall <strong>of</strong> Fame<br />
The American <strong>Osteopathic</strong> Association<br />
Mentor Hall <strong>of</strong> Fame inducts new osteopathic<br />
physicians annually, to recognize their<br />
excellence in training and supporting<br />
osteopathic medical students, interns,<br />
residents and other young physicians.<br />
The Hall <strong>of</strong> Fame is a part <strong>of</strong> the AOA’s Mentor<br />
Program, initially conceived in 2003 by then<br />
AOA President, Darryl Beehler, D.O. Last year,<br />
six new OU-COM alumni were nominated for<br />
AOA Mentor <strong>of</strong> the Year and subsequently<br />
inducted into the Mentor Hall <strong>of</strong> Fame.<br />
2007 AOA Mentor Hall <strong>of</strong> Fame<br />
alumni inductees<br />
Shawn R. Kerger, D.O. (’96)<br />
Stephanie V. Oberhelman, D.O. (’96)<br />
Keith U. Smith, D.O. (’86)<br />
Jeffrey A. Stanley, D.O. (’82), FACOS<br />
David N. Stroh, D.O. (’83)<br />
Celeste N. Wallace, D.O. (’02), FACOP<br />
Previous AOA Mentor Hall <strong>of</strong> Fame<br />
alumni inductees<br />
Timothy J. Barreiro, D.O. (’97), FCCP, FACOI<br />
Imber (Corcoran) Coppinger, D.O. (’97)<br />
Barbara M. Doerr, D.O. (’91), Ph.D.<br />
Paul Entler, D.O. (’00)<br />
Todd M. Friend, D.O. (’91)<br />
Anita L. Showalter, D.O. (’93)<br />
Jay H. Shubrook, D.O. (’96), FACOFP<br />
Gail M. Swarm, D.O. (’89)<br />
Steven M. Takacs, D.O. (’86)<br />
Joan E. Tamburro, D.O. (’94), FAOCD<br />
2000<br />
William J. Dobak, D.O., and Melissa Johnson were<br />
married Nov. 17, 2007, in Atlanta, Ga. Dr. Dobak is<br />
an assistant pr<strong>of</strong>essor <strong>of</strong> obstetrics and gynecology<br />
at Florida State <strong>University</strong>.<br />
Trinetta D. Masternick, D.O., and husband,<br />
William Gerhing, welcomed their third son, Will,<br />
to the family in February 2007. Dr. Masternick<br />
accepted a new position as pain management<br />
specialist. Her sister, Janeen, is a second-year student<br />
at OU-COM.<br />
2001<br />
CORRECTION: Steve Chandler, D.O., completed<br />
his orthopedic trauma fellowship at Grant<br />
Medical Center in Columbus, <strong>Ohio</strong>. He moved to<br />
Chicago, Ill., and works in two hospitals: one in Oak<br />
Lawn, Ill., and the other in Evergreen, Ill.<br />
Michael Gerardo, D.O., M.P.H., was appointed to<br />
a three-year term on the Ethnogeriatrics Committee<br />
<strong>of</strong> the American Geriatric Society. Dr. Gerardo also<br />
published seven chapters in The Practical Guide to<br />
the Care <strong>of</strong> the Geriatric Patient, published by Mosby,<br />
Inc., in 2008. He presented “Quality, language,<br />
and culture: Hispanic nursing home and care,” to<br />
the medical faculty at <strong>University</strong> Health Sciences<br />
Center in San Antonio, Texas, and again at the<br />
Center for Health Care and Policy Research, Case<br />
Western Reserve <strong>University</strong> in Cleveland, <strong>Ohio</strong>,<br />
both in July.<br />
Rachel Zevallos, D.O., and husband Carlos<br />
Zevallos, D.O., have two children: Lillie, born in<br />
2005, and Charlie, born in 2006.<br />
2002<br />
Gregory K. Applegate, D.O., completed a sixmonth<br />
Army deployment in Baghdad, Iraq, in 2007,<br />
where he served as a combat anesthesiologist.<br />
Dawn Dillinger, D.O., accepted a position at Child<br />
Care Consultants in Columbus, <strong>Ohio</strong>.<br />
Brooke Lampl, D.O., is pursuing a fellowship<br />
in pediatric radiology at New York Presbyterian<br />
Hospital-Columbia.<br />
Thomas Smith, D.O., is pursuing a fellowship<br />
in adult reconstruction at the Mayo Clinic in<br />
Rochester, Minn.<br />
Kamini Trivedi, D.O., published three abstracts<br />
in 2007: two in the Journal <strong>of</strong> Cardiac Failure and<br />
one in Circulation. She presented the abstracts at<br />
the 2007 annual meetings <strong>of</strong> the American Heart<br />
Association and the Heart Failure Society <strong>of</strong><br />
America.<br />
2003<br />
Joel W. Anders, D.O., and Kathryn Anders<br />
were married in 2006. He accepted a new position<br />
at Licking Memorial Health Systems in Newark,<br />
<strong>Ohio</strong>. The couple has two children, Declan<br />
and Camille.<br />
Christopher J. Dennis, D.O., has completed a<br />
fellowship in pulmonary/critical care medicine at<br />
the Lackland U.S. Air Force Base in San Antonio,<br />
Texas, and is practicing at the Wright Patterson Air<br />
Force Base Medical Center in Dayton, <strong>Ohio</strong>.<br />
Jennifer L. Gwilym, D.O., is now medical director<br />
<strong>of</strong> the sexual health division <strong>of</strong> the Columbus Public<br />
Health Department in <strong>Ohio</strong>.<br />
Stephen Scheper, D.O., and wife, Gina H. Y.<br />
Scheper, have relocated to Hawaii, where Dr.<br />
Scheper is completing a physical medicine and<br />
rehabilitation fellowship. He plans to remain in<br />
Hawaii after completing the fellowship.<br />
2004<br />
Derrick Blackwell, D.O., joined Piedmont Family<br />
Practice at Tega Cay in Fort Mill, S.C., as an<br />
attending physician. He also received a Michigan<br />
State <strong>University</strong> Resident Teaching Award.<br />
Joshua LeClaire, D.O., married Shoshone<br />
Richardson in 2006. He is currently pursuing<br />
a fellowship in cytopathology at MetroHealth<br />
Hospital in Cleveland, <strong>Ohio</strong>.<br />
Jean (Sheppard) Rettos, D.O., received the<br />
2005 Merck Resident <strong>of</strong> the Year award from<br />
O’Bleness Memorial Hospital, where she completed<br />
a neuromusculoskeletal medicine residency. In<br />
August 2008, She opened a private practice, Athens<br />
Health Solutions, which <strong>of</strong>fers family medicine and<br />
osteopathic manipulative medicine.<br />
Chad A. Weber, D.O., gave a presentation at the<br />
American Society for Surgery <strong>of</strong> the Hand in<br />
September 2007. He will begin a fellowship in<br />
orthopedic trauma in Indianapolis in 2009.<br />
2005<br />
Kelly Becker, D.O., accepted a new position with<br />
Strongsville Family Physicians in Strongsville, <strong>Ohio</strong>.<br />
She and her husband, Brian Jungeberg, were married<br />
in July 2006.<br />
Ron Mallick, D.O., and Bridgette Sims Mallick,<br />
were married May 24, 2008, with classmate<br />
Abelash Reddy, D.O., and his wife, Roopa Patel,<br />
D.O. (’06), in attendance.<br />
2006<br />
Christina Bagby, D.O., is pursuing a pathology<br />
residency at <strong>University</strong> Hospitals Case Medical<br />
Center in Cleveland, <strong>Ohio</strong>.<br />
Shannon (Claprood) McAfee, D.O., cowrote<br />
“Occipital compression and its potential uses in<br />
obstetrics” with Anthony Chila, D.O., pr<strong>of</strong>essor <strong>of</strong><br />
family medicine. The article was published in the<br />
AAO Journal, September 2007. Dr. McAfee and her<br />
husband, C. Curtis, also welcomed baby Caleb in<br />
November 2007.<br />
Katrina (Jones) Sabur, D.O., and Ibrahim Sabur<br />
were married in September 2006.<br />
2007<br />
Rachel Liptak, D.O., and Ryan Mast, D.O. were<br />
married in October 2008. Dr. Liptak in an internal<br />
medicine residency program at Grandview Hospital,<br />
and Dr. Mast is doing a psychiatry residency program<br />
at Wright State <strong>University</strong> in Dayton, <strong>Ohio</strong>.<br />
Kedy Jao, D.O. (’83), and John Koncelik, D.O. (’82),<br />
deliver the toast at the 25 year reunion for the<br />
classes <strong>of</strong> 1982 and 1983, held in October at the<br />
Baker <strong>University</strong> Center in Athens.<br />
January 16-17<br />
Cleveland Academy <strong>of</strong><br />
<strong>Osteopathic</strong> Medicine<br />
44th Annual Postgraduate Seminar<br />
Hilton Cleveland East<br />
Beachwood, <strong>Ohio</strong><br />
Alumni Reception, January 16<br />
February 21<br />
Society <strong>of</strong> Alumni & Friends<br />
Board <strong>of</strong> Directors Winter Meeting<br />
Columbus Hilton at Easton<br />
March 4-8<br />
ACOFP 46th Annual Convention<br />
Gaylord National Resort &<br />
Convention Center<br />
Washington, D.C.<br />
March 25-29<br />
American Academy <strong>of</strong> Osteopathy<br />
Annual Convocation<br />
Peabody Hotel<br />
Little Rock, Ark.<br />
April 15-18, 2009<br />
AACOM Annual Meeting<br />
Bethesda, Md.<br />
22 ohio university medicine
Follow-up<br />
Follow-up<br />
Alumni Pr<strong>of</strong>ile<br />
Above: (Left to right) Lauren Schlacht<br />
(physical therapist), Steve Augustine, D.O. (‘94),<br />
and Eddie Casillas (athletic trainer) at the 2005<br />
American Motorcyclists Association National<br />
Motocross Series<br />
Left: Dr. Augustine taking x-ray <strong>of</strong> injured BMX<br />
racer at the 2007 Southeast BMX Championship<br />
Lower left & facing page: ASMF Mobile<br />
Sports Medical Unit at the 2007 Florida Winter<br />
AMA Motocross Series<br />
X<br />
Passion drives Dr. Stephen Augustine to<br />
the track—as a national leader in medical<br />
care for motorized extreme sports<br />
By Stephen McKean<br />
Photos provided by Dr. Stephen Augustine<br />
Stephen Augustine, D.O. (’94), like many orthopedic surgeons, is<br />
Going to<br />
eXtremes<br />
a sports enthusiast. He was a four-year football letterman at Denison<br />
<strong>University</strong> and a club lacrosse player at OU-COM. But his passion for<br />
the new wave <strong>of</strong> motorized extreme sports—motocross racing, BMX<br />
biking, and the whole range <strong>of</strong> high-speed, high flying feats epitomized<br />
by the X Games—sets him apart from his colleagues.<br />
Augustine, who grew up racing motocross dirt bikes, says he began to<br />
notice an unsettling difference between how physicians treat action sports<br />
athletes compared to those in “stick and ball sports,” as he calls them.<br />
“If a high school kid is out riding his motocross bike—training<br />
really hard and racing—and he blows out his ACL, he’s [considered]<br />
an idiot,” says Augustine. “But a high school football player who<br />
blows out his ACL—he’s considered some kind <strong>of</strong> a hero. I think that<br />
dichotomy is ridiculous.”<br />
Augustine co-founded the non-pr<strong>of</strong>it Action Sports Medicine<br />
Foundation (ASMF) in 2004 to raise awareness about the unique<br />
medical needs <strong>of</strong> these non-traditional athletes. While “stick and ball<br />
sports” usually employ both an athletic trainer and a physician at games,<br />
Augustine says that action sports events typically provide little more<br />
than paramedics, who may or may not be familiar with the participants’<br />
particular needs.<br />
“The number one goal [<strong>of</strong> the foundation] is to improve on-site<br />
medical care for action sports athletes at their events—all levels,<br />
pr<strong>of</strong>essional and amateur,” he says.<br />
Augustine has a wealth <strong>of</strong> firsthand experience in this area, having<br />
served as an event physician for American Motorcycle Association (AMA)<br />
supercross and motocross events since 2001—as well as countless other<br />
action sports events around the country. He also serves as chief <strong>of</strong> the sports<br />
medicine division for the Asterisk Mobile Medical Unit and as the medical<br />
director <strong>of</strong> the Road 2 Recovery Foundation, a non-pr<strong>of</strong>it organization that<br />
assists AMA-licensed pr<strong>of</strong>essional motocross and supercross riders who<br />
sustain career-ending injuries.<br />
So far, Augustine is pleased with the ASMF’s progress. “We have a team<br />
<strong>of</strong> volunteers—athletic trainers, physicians’ assistants, physical therapists,<br />
doctors—who cover the events on-site. We were able to raise money to<br />
buy uniforms, and we now have our own mobile medical center.”<br />
All told, Augustine devotes more than 40 weekends a year to on-site<br />
medical service for “extreme” sports athletes, including pr<strong>of</strong>essional and<br />
amateur motocross and supercross, as well as non-motorized sports<br />
such as skateboarding. Although he mostly serves east <strong>of</strong> the Mississippi,<br />
Augustine frequently travels west to help out at major pr<strong>of</strong>essional events.<br />
In the long term, Augustine would like to extend the reach <strong>of</strong> his<br />
foundation beyond the Southeastern U.S., where it has had so much<br />
early success. He would also like to see more general research on action<br />
sports athletes, in the same way that traditional athletes have been<br />
studied for decades.<br />
Perhaps most importantly, Augustine hopes to break down negative<br />
stereotypes in the medical community surrounding action sports<br />
athletes. “Doctors in general just blow them <strong>of</strong>f because they don’t<br />
understand them,” he says.<br />
But Augustine, who still occasionally races in enduro, motocross and<br />
harescramble events, most certainly does. “When you race motocross,”<br />
he says, “it’s like hitting a home run ten times in one game.”<br />
Jill L. Harman, M.Ed.<br />
Director <strong>of</strong> Alumni Affairs<br />
Helping our students find their path<br />
The number <strong>of</strong> physicians choosing to specialize in sports medicine<br />
is rising nationwide. According to Lori A. Boyajian-O’Neill, D.O., 2007<br />
president <strong>of</strong> the American <strong>Osteopathic</strong> Academy <strong>of</strong> Sports Medicine,<br />
“We are witnessing the development <strong>of</strong> a field about to explode.”<br />
The practice trends <strong>of</strong> OU-COM graduates reflect that statement. The<br />
number <strong>of</strong> our alumni practicing sports medicine has more than doubled<br />
in the last five years. Although that figure remains relatively small,<br />
graduates like Steven Augustine, D.O. (’94) are definitely making a<br />
big impact within the specialty. And given the popularity <strong>of</strong> the OU-COM<br />
Surgery and Sports Medicine club, this trend shows no sign <strong>of</strong> slowing.<br />
To expose our students to this and other specialties, the Office <strong>of</strong> Alumni<br />
Affairs works with student organizations to coordinate our annual Career<br />
Medical Specialties Series. This September, John Walter, D.O. (’00)<br />
kicked <strong>of</strong>f the year-long series by speaking to first- and second-year<br />
students on the related specialty <strong>of</strong> physical medicine and rehabilitation.<br />
Participating in our Career Medical Specialties Series is a terrific way<br />
to reengage with OU-COM and meet your future D.O. colleagues. Please<br />
contact your Office <strong>of</strong> Alumni Affairs to learn how you can return to<br />
campus and speak about your specialty or mentor students interested<br />
in your field. I look forward to hearing from you!<br />
Practicing sports medicine alumni physicians<br />
367% increase<br />
1998 2008<br />
24 ohio university medicine Winter 2009<br />
25
Across the divide<br />
Final stages <strong>of</strong> cell division, taken<br />
with a flourescence microscope<br />
Mark Berryman, Ph.D., associate pr<strong>of</strong>essor, received a twoyear<br />
$221,250 NIH award in June for his grant proposal, “Role<br />
<strong>of</strong> CLIC in epithelial morphogenesis.” To better understand<br />
how CLIC (chloride intracellular channel) proteins affect<br />
cell development, Berryman is studying how they interact<br />
with other proteins in fruit flies. In this image, cell parts are<br />
stained: DNA is blue, microtubules are red and CLIC4 proteins<br />
are green.<br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Medicine<br />
332 Grosvenor Hall<br />
Athens, OH 45701<br />
Non Pr<strong>of</strong>it Org.<br />
US Postage<br />
PAID<br />
Permit No. 100<br />
Athens, OH<br />
ADDRESS SERVICE REQUESTED