ABO Discrepancies Disclosure Objectives Importance Recognition ...
ABO Discrepancies Disclosure Objectives Importance Recognition ...
ABO Discrepancies Disclosure Objectives Importance Recognition ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
4/12/2011<br />
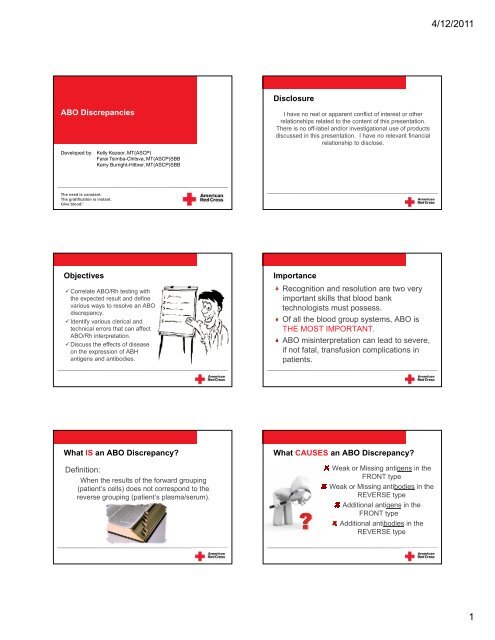
<strong>ABO</strong> <strong>Discrepancies</strong><br />
Developed by: Kelly Kezeor, MT(ASCP)<br />
Farai Tsimba-Chitsva, MT(ASCP)SBB<br />
Kerry Burright-Hittner, MT(ASCP)SBB<br />
<strong>Disclosure</strong><br />
I have no real or apparent conflict of interest or other<br />
relationships related to the content of this presentation.<br />
There is no off-label and/or investigational use of products<br />
discussed in this presentation. I have no relevant financial<br />
relationship to disclose.<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood ṬM<br />
<strong>Objectives</strong><br />
Correlate <strong>ABO</strong>/Rh testing with<br />
the expected result and define<br />
various ways to resolve an <strong>ABO</strong><br />
discrepancy.<br />
Identify various clerical l and<br />
technical errors that can affect<br />
<strong>ABO</strong>/Rh interpretation.<br />
Discuss the effects of disease<br />
on the expression of ABH<br />
antigens and antibodies.<br />
<strong>Importance</strong><br />
<strong>Recognition</strong> and resolution are two very<br />
important skills that blood bank<br />
technologists must possess.<br />
Of all the blood group systems, <strong>ABO</strong> is<br />
THE MOST IMPORTANT.<br />
<strong>ABO</strong> misinterpretation can lead to severe,<br />
if not fatal, transfusion complications in<br />
patients.<br />
What IS an <strong>ABO</strong> Discrepancy?<br />
Definition:<br />
When the results of the forward grouping<br />
(patient’s cells) does not correspond to the<br />
reverse grouping (patient’s plasma/serum).<br />
What CAUSES an <strong>ABO</strong> Discrepancy?<br />
Weak or Missing antigens in the<br />
FRONT type<br />
Weak or Missing antibodies in the<br />
REVERSE type<br />
Additional antigens in the<br />
FRONT type<br />
Additional antibodies in the<br />
REVERSE type<br />
1
4/12/2011<br />
<strong>ABO</strong> <strong>Discrepancies</strong> MUST be Resolved<br />
In PATIENTS, an <strong>ABO</strong> discrepancy must be<br />
resolved before ANY blood component is<br />
transfused.<br />
– If an <strong>ABO</strong> discrepancy cannot be resolved before<br />
blood product is needed, transfuse with Group O red<br />
blood cell units<br />
In DONORS, the discrepancy must be resolved<br />
before any blood is labeled with a blood type.<br />
Identify the Discrepancy<br />
Front Type<br />
Reverse Type<br />
Patient Anti-A Anti-B Anti-A,B A 1 cells B cells<br />
JK 0 3+ 3+ 0 0<br />
Front type: B<br />
Reverse Type: AB<br />
Theory: Weak reverse type<br />
Identify the Discrepancy<br />
Identify the Discrepancy<br />
Front Type<br />
Reverse Type<br />
Patient Anti-A Anti-B Anti-A,B A 1 cells B cells<br />
KK 4+ 4+ 4+ 3+ 3+<br />
Front Type<br />
Reverse Type<br />
Patient Anti-A Anti-B Anti-A,B A 1 cells B cells<br />
CK 4+ 0 4+ 0 4+<br />
Front Type: AB<br />
Reverse Type: O<br />
Front Type: A<br />
Back Type: A<br />
Theory: Additional antibodies in the reverse type<br />
Theory: NO DISCREPANCY NOTED<br />
Identify the Discrepancy<br />
Front Type<br />
Reverse Type<br />
Patient Anti-A Anti-B Anti-A,B A 1 cells B cells<br />
AK 0 w+ 1+ 4+ 0<br />
Front Type: B??<br />
Reverse Type: B<br />
Steps for Resolution<br />
Recheck specimen for identification<br />
Rewash EDTA cell suspension<br />
Repeat testing<br />
Confirm patient’s t’ diagnosis, i age, medication,<br />
and pregnancy history<br />
Theory: Weak reacting antigen in the front type.<br />
2
4/12/2011<br />
Types of ERRORS<br />
Clerical Errors<br />
Mislabeled tubes<br />
Patient misidentification<br />
Inaccurate interpretations recorded<br />
Transcription error<br />
Computer entry error<br />
Types of ERRORS<br />
Reagent or equipment problems<br />
Using expired reagents<br />
Using an un-calibrated centrifuge<br />
Contaminated or hemolyzed reagents<br />
Incorrect storage temperatures<br />
Types of ERRORS<br />
<strong>ABO</strong> Discrepancy Categories<br />
Procedural errors<br />
Reagents not added<br />
Manufacturer’s directions not followed<br />
RBC suspensions incorrect concentration<br />
Cell buttons not re-suspended before grading<br />
agglutination<br />
Problems with<br />
Red Blood Cells<br />
Weak-reacting/Missing<br />
antigens<br />
Extra antigens<br />
Mixed field reactions<br />
Problems with<br />
Plasma/Serum<br />
Weak-reacting/Missing<br />
antibodies<br />
Extra antibodies<br />
Grouping<br />
Forward<br />
Reverse<br />
Missing/Weak Extra Mixed Field Missing/Weak Extra<br />
Subgroup A/B Acquired B O Transfusion<br />
Young<br />
Elderly<br />
Immunocompromised<br />
Cold<br />
Autoantibody<br />
tib Forward Grouping Problems<br />
Disease<br />
(cancer)<br />
B(A) Phenotype<br />
Bone Marrow<br />
Transplant<br />
Cold<br />
Alloantibody<br />
Rouleaux<br />
True Chimera<br />
Rouleaux<br />
Anti-A 1<br />
3
4/12/2011<br />
Forward Grouping Problems<br />
Mixed field (mf) agglutination<br />
Weak or missing antigens<br />
Additional or unexpected antigens<br />
Polyagglutinable cells<br />
Forward Grouping Problems<br />
Mixed Field (mf) Reactions<br />
Small agglutinates with many un-agglutinated cells<br />
Result of:<br />
Mixed cell population from a massive transfusion of another blood<br />
group. (non-O individual receiving O red blood cells)<br />
Bone marrow transplants having both the original type and donor<br />
marrow cells.<br />
The inheritance of weak <strong>ABO</strong> subgroups such as A 3 , A x and B 3 and<br />
B can traditionally present a mixed field reaction.<br />
Chimerism due to the intrauterine exchange of red cells, fraternal<br />
twins, and mosaicism arising from dispermy presents mixed field even<br />
though it rarely occurs.<br />
Forward Grouping Problems<br />
Resolving Mixed Field (mf) Reactions<br />
Determine the CAUSE of the mixed field reaction<br />
Checking the patient’s transfusion history and clinical history<br />
e.g. HPC transplant<br />
If it is determined that it is a weak subgroup, perform<br />
specialized tests<br />
e.g. adsorption and elution, saliva, and transferase studies<br />
Molecular testing<br />
Forward Grouping Problems<br />
Weak or Missing Antigen<br />
Result of:<br />
Inheritance of a weak <strong>ABO</strong> subgroup<br />
Malignancies may result in the loss of ABH transferases<br />
Hodgkins disease<br />
Lymphomas<br />
Leukemias<br />
Massive transfusion with group O blood to a non-group O<br />
person<br />
e.g. a group A person receiving lots of group O blood.<br />
Bone marrow transplant and chemotherapy.<br />
Forward Grouping Problems<br />
Resolving Weak or Missing Antigens<br />
Check the patient’s transfusion and clinical history<br />
Read the forward group microscopically<br />
Use anti-A,B and monoclonal antisera that is known to react with<br />
A x and dA 3 weak <strong>ABO</strong> subgroups<br />
Perform adsorption and elution studies<br />
Forward Grouping Problems<br />
Additional Antigens<br />
Result of:<br />
Bacterial enzymes deacetylate the A antigen to a “B”<br />
antigen and the patient front types as an AB and reverses<br />
as an A.<br />
Acquired B antigens are observed in patients with<br />
recurring GI or colon infections with Gram negative<br />
bacteria<br />
4
4/12/2011<br />
Forward Grouping Problems<br />
Resolving Additional Antigens<br />
Check clinical history for evidence of colon infections with<br />
Gram negative sepsis<br />
Test an auto control<br />
The patient’s own anti-B will not react with their own AB cells<br />
Acidify the anti-B to a p.H. of 6 and retest<br />
Acquired B antigens will not react in acidified antiserum,<br />
whereas as normal B antigens will react.<br />
Forward Grouping Problems<br />
Spontaneous Agglutination<br />
Result of:<br />
Strong potent cold auto antibodies<br />
Would appear as AB in the front type and O in the reverse type<br />
Strong positive DAT with IgG, C3d and saline control<br />
Wharton’s jelly in cord blood<br />
Forward Grouping Problems<br />
Resolving Spontaneous Agglutination<br />
Incubate plasma and cells (separately) at 37°C for 5 to<br />
15 minutes<br />
▪ Wash cells 5 to 6 times with warm saline<br />
▪ Retest warm washed cells with warm plasma<br />
▪ Retest the DAT and saline control<br />
Treat cells with 0.01M DTT<br />
Wash cord blood a minimum of 6 times with saline<br />
Forward Grouping Problems<br />
Polyagglutination<br />
Result of:<br />
Inheriting acquired abnormalities of the red cell membranes with<br />
exposure to crypt antigens<br />
e.g. T activation.<br />
Bacterially contaminated sample<br />
Resolve by:<br />
Avoid testing with human antisera; use monoclonal antisera.<br />
Collection of a new sample<br />
Reverse Grouping Problems<br />
▪Plasma or serum <strong>ABO</strong> discrepancies are<br />
more common than red cell discrepancies.<br />
Reverse Grouping Problems<br />
Weak/Missing<br />
Additional Antibodies<br />
Rouleaux<br />
5
4/12/2011<br />
Reverse Grouping Problems<br />
Weak/Missing Antibodies<br />
Newborns<br />
Antibodies are not present at birth and only develop after 3<br />
to 6 months of age.<br />
Elderly<br />
Weakened antibody activity<br />
Hypogammaglobulinemia<br />
Little or no antibody production<br />
(immuno-compromised patient)<br />
NO agglutination on reverse grouping<br />
Reverse Grouping Problems<br />
Resolving Weak/Missing Antibodies<br />
Determine patient’s age and diagnosis<br />
Incubate serum testing for 15 minutes at room<br />
temperature or 18°C to enhance antibody reactions<br />
If negative, incubate serum testing at 4°C for 15<br />
minutes<br />
Reverse Grouping Problems<br />
Extra Antibodies<br />
Result of:<br />
Cold antibodies (allo- or auto-)<br />
Cold antibodies may include anti-I, H, M, N, P, Lewis<br />
Rouleaux<br />
Anti-A 1 in an A 2 or A 2 B individual<br />
Reverse Grouping Problems<br />
Resolving Extra Antibodies: Cold Alloantibodies<br />
Perform antibody identification at IS and or RT<br />
Use the pre-warm technique<br />
Incubate the serum and red cells separately at 37°C before<br />
testing<br />
Perform a cold adsorption<br />
Incubating equal amounts of red cells and serum at 4C for 30 to<br />
60 minutes and test adsorbed serum against reverse type cells<br />
Antigen type reverse cells for the offending antigen<br />
If reverse type cells are antigen positive find reverse type cells<br />
that are antigen negative and incubate with serum to resolve<br />
discrepancy.<br />
Reverse Grouping Problems<br />
Extra Antibodies: Rouleaux<br />
Result of:<br />
Abnormal concentrations of serum proteins<br />
Altered serum/protein ratios<br />
High-molecular-weight volume expanders<br />
Associated with:<br />
‣ Multiple myeloma<br />
‣ Waldenstrom’s macroglobulinemia (WM)<br />
‣ Hydroxyethyl starch (HES), dextran, etc<br />
Reverse Grouping Problems<br />
Resolution of Extra Antibodies: Rouleaux<br />
REMOVE PROTEINS!!<br />
If the forward grouping is affected, wash cells to<br />
remove protein and repeat test<br />
If the reverse grouping is affected, perform saline<br />
replacement technique (more common)<br />
Reagent cells and patient serum are centrifuged to allow<br />
antibody attachment (if present)<br />
Serum is removed and replaced by an equal volume of salinewhich<br />
disperses cells<br />
Tube is mixed, centrifuged, and re-examined for agglutination<br />
6
4/12/2011<br />
Reverse Grouping Problems<br />
Result of:<br />
Extra Antibodies: Anti-A 1<br />
A 2 (or A 2 B) individuals development of anti-A 1 antibody<br />
A 2 (or A 2 B) individuals have less antigen sites than A 1<br />
individuals<br />
anti-A 1 is a naturally occurring IgM antibody<br />
Antibody reacts with A 1 cells, but not A 2 cells<br />
Reverse Grouping Problems<br />
Resolution Extra Antibodies: Anti-A 1<br />
Type patient red blood cells with Anti-A 1 lectin<br />
Test patient serum with A 1 , A 2 and O cells<br />
Case Study #1<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood. TM<br />
Case Study #1: Patient History<br />
•88 year old male<br />
•Diagnosis: Immunocompromised<br />
•Medications: Corticosteroids<br />
•Transfusion T f i History: Massive plasma infusion<br />
i<br />
•Lab: Hemoglobin: 6.5 g/dL<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient 0 0 0 3+ 0 w+ w+ 0<br />
What is the problem?<br />
Both a front AND reverse typing issue<br />
Both a front AND reverse typing issue<br />
Investigation<br />
Patient age: 88 years old<br />
Diagnosis: Hypogammaglobulinemia<br />
Medications: Immunosuppressive drugs<br />
Resolution:<br />
weak front type, weak reverse type<br />
7
4/12/2011<br />
Weak front type and weak reverse type resolution:<br />
Enhance forward type<br />
Incubate patient cells with antisera (per manufacturers directions)<br />
Enhance reverse type<br />
Incubate reverse type cells with patient serum for 15 to 30 minutes<br />
Room temperature or 18°C (per manufacturers directions)<br />
4°C for 15 minutes<br />
test concurrently with autologous cells and group O screening cells<br />
Enzyme treat reverse type cells with FICIN<br />
Case Study #2<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient 0 0 0 3+ 0 w+ w+ 0<br />
30’ RT 0 1+ 2+ 1+ 1+ 0<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood. TM<br />
Case Study #2: Patient History<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
• 33 year old female<br />
• Diagnosis: Anemia<br />
• Medications: None<br />
• Transfusion History: 2 units of packed red blood<br />
cells 5 years ago<br />
• Lab: Hemoglobin: 9.1 g/dL<br />
Patient 0 4+ 4+ 3+ 0 3+ 3+ 1+<br />
Screening<br />
Cells<br />
DAT<br />
IS<br />
PEG/IAT<br />
I 1+ 0<br />
II 1+ 0<br />
III 1+ 0<br />
Anti-IgG<br />
Anti-<br />
C3dC3b<br />
Saline<br />
Control<br />
Patient 0 2+ 0<br />
What is the problem?<br />
Reverse typing issue<br />
Additional antibodies: cold??<br />
Investigation<br />
Patient age: 33 years old<br />
Diagnosis: Anemia<br />
Medications: None<br />
Resolution:<br />
Additional antibody in reverse<br />
type<br />
Additional antibody in reverse type resolution:<br />
Prewarm Technique<br />
Incubate the serum and red cells separately at 37°C before testing<br />
Cold Adsorption<br />
Incubate equal amounts of red cells (adsorbing cells) and patient<br />
serum at 4°C for 30 to 60 minutes<br />
Test adsorbed serum against reverse typing cells<br />
Case Study #3<br />
Screening<br />
Cells<br />
IS<br />
4°C Adsorbed<br />
Serum<br />
I 0<br />
II 0<br />
III 0<br />
A 1 cells A 2 cells B cells<br />
Patient 3+ 3+ 1+<br />
4°C<br />
Adsorbed<br />
Serum<br />
3+ 3+ 0<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood. TM<br />
8
4/12/2011<br />
Case Study #3: Patient History<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
• 45 year old man<br />
• Diagnosis: Recurrent GI bleed<br />
• Medications: None<br />
• Transfusion History: 10 in past year; none in last<br />
3 months<br />
• Lab: Hemoglobin: 9.2 g/dL<br />
Patient 4+ w+ 4+ 4+ 0 w+ 2+ 3+<br />
Screening<br />
Cells<br />
DAT<br />
IS<br />
PEG/IAT<br />
I 1+ 0<br />
II 1+ 0<br />
III 1+ 0<br />
Anti-IgG<br />
Anti-<br />
C3dC3b<br />
Saline<br />
Control<br />
Patient 0 0 0<br />
What is the problem?<br />
Forward and Reverse typing<br />
issue<br />
Investigation<br />
Patient age: 45 years old<br />
Diagnosis: Recurrent GI bleed<br />
Medications: None<br />
Resolution:<br />
Additional antibody in front<br />
type and reverse type<br />
Additional antibody in the front and reverse type resolution<br />
Forward type:<br />
Wash red cells extensively and repeat testing<br />
Removes proteins<br />
Reverse type<br />
Saline replacement technique;<br />
Patient cells and serum combined and centrifuged<br />
Allows for antigen/antibody reaction (if present)<br />
Remove serum and replace with equal volume of saline<br />
Mix, centrifuge, and reexamine for agglutination<br />
Both macroscopically and microscopically<br />
Front Type:<br />
Anti-A Anti-B Anti-A,B<br />
Patient 4+ w+ 4+<br />
Patient Cells<br />
washed X6<br />
with Saline<br />
4+ 0 4+<br />
Reverse Type:<br />
A 1 cells A 2 cells B cells<br />
Patient w+ 2+ 3+<br />
Saline<br />
Replacement 0 1+ 3+<br />
Screening IS<br />
PEG/IAT<br />
Cells<br />
(saline<br />
replacement)<br />
I w+ 0<br />
II 0 0<br />
III w+ 0<br />
Forward type resolved:<br />
Patient forward type: A<br />
Reverse type NOT resolved:<br />
cold alloantibody??<br />
Anti-M identified at IS<br />
53<br />
54<br />
Reverse grouping cells need to be antigen typed for the M antigen.<br />
A 1 cells<br />
(original source)<br />
A 2 cells<br />
(original source)<br />
B cells<br />
(original source)<br />
A 2 cells<br />
(second source)<br />
B cells<br />
(second source)<br />
Anti-M<br />
0<br />
2+<br />
1+<br />
0<br />
0<br />
•The original source of A 2 and B<br />
cells are M antigen positive. Since<br />
the patient has anti-M identified at<br />
IS, this antigen is interfering with<br />
the reverse grouping (causing a<br />
discrepancy).<br />
•A second source of A 2 and B cells<br />
were located that are M antigen<br />
negative. These cells will be used<br />
to perform reverse grouping on this<br />
patient.<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient 4+ w+ 4+ 4+ 0 w+ 2+ 3+<br />
Washed X6 with normal saline<br />
(second source,<br />
M antigen negative)<br />
Saline<br />
replacement<br />
4+ 0 4+ 0 0 3+<br />
9
4/12/2011<br />
Case Study #4: Patient History<br />
Case Study #4<br />
• 36 year old female<br />
• Diagnosis: Pregnancy #3<br />
• Medications: Pre-natal vitamins<br />
• Transfusion History: No transfusions<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood. TM<br />
57<br />
58<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient 4+ 0 4+ 4+ 0 2+ 0 3+<br />
Screening<br />
Cells<br />
IS<br />
PEG/IAT<br />
I 0 0<br />
II 0 0<br />
III 0 0<br />
What is the problem?<br />
Reverse typing issue<br />
Investigation<br />
Patient age: 36 years old<br />
Diagnosis: Pregnant<br />
Medications: vitamins<br />
Resolution:<br />
Additional antibody in reverse type<br />
•Test the patient’s serum<br />
against different A 1 and A 2<br />
cells<br />
Patient Serum<br />
A 1 cells 3+<br />
A 1 cells 3+<br />
A 1 cells 3+<br />
A 2 cells 0<br />
A 2 cells 0<br />
A 2 cells 0<br />
•Test the patient’s red blood<br />
cells against anti-A 1 lectin<br />
(Dolichos biflorus)<br />
Anti-A 1 Lectin<br />
(Dolichous biflorus)<br />
Patient 0<br />
Resolution: Patient is (probable)<br />
type A 2 with anti-A 1 in her serum<br />
Case Study #5: Patient History<br />
Case Study #5<br />
• 50 year old female<br />
• Diagnosis: COPD<br />
• Medications: Morphine<br />
• Transfusion History: No known transfusion per<br />
blood bank records<br />
• Lab: Hemoglobin: 7.5 g/dL<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood. TM<br />
10
4/12/2011<br />
61<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient 4+ mf 0 4+ mf 4+ 0 1+ w+ 4+<br />
Screening<br />
Cells<br />
IS<br />
PEG/IAT<br />
Investigation<br />
I 1+ 2+<br />
II 0 0<br />
III 1+ 2+<br />
What is the problem?<br />
Forward and Reverse typing issue<br />
Patient age: 50 years old<br />
Diagnosis: COPD<br />
Medications: Morphine<br />
Resolution:<br />
Mixed field in front type and extra<br />
antibody(ies) in reverse type<br />
Additional antibody in the front and reverse type resolution<br />
Forward type:<br />
Mixed field<br />
What is causing mixed field—has this patient been transfused?<br />
Harvest reticulocytes (that aren’t coated with antibody) and re-test front type<br />
Upon further investigation, patient was transfused with 4 group O<br />
Positive units last week at a different facility (explaining the mixed field<br />
reactivity identified in the front type). The antibody screen was negative<br />
at that time.<br />
Anti-A Anti-B Anti-A,B<br />
Reticulocyte Separation Cells<br />
Patient 4+ 0 4+<br />
A 2 cells<br />
2+<br />
64<br />
63<br />
Reverse type<br />
Antibody identification<br />
What antibody is in the screen?<br />
Could it be interfering with the reverse type?<br />
An elution of the patient’s red blood cells should be performed to<br />
Reverse type resolution:<br />
Antigen type the reverse group RBCs for Jk a to determine if the<br />
antibody is interfering with <strong>ABO</strong> resolution<br />
Absorb the anti-Jk a out of the patient sample and re-test the<br />
serum with the reverse type cells to resolve the <strong>ABO</strong>.<br />
identify the antibody that is coating the red blood cells (positive auto-<br />
control)<br />
Anti-Jk a<br />
Elution of the patient’s red blood cells identifies anti-Jk a is coating<br />
the cells.<br />
Antibody identification in the serum identifies anti-Jk a A 1 cells<br />
(original source)<br />
2+<br />
(original source)<br />
B cells<br />
2+<br />
(original source)<br />
65<br />
Since the patient has been recently transfused, differential adsorptions<br />
are performed at a cold temperature to fully remove the anti-Jk a from<br />
the patient serum.<br />
A 1<br />
cells<br />
A 2<br />
cells<br />
B<br />
cells<br />
Patient 1+ w+ 4+<br />
Adsorbed serum<br />
0 0 4+<br />
Case Study #6<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient 4+ mf 0 4+ mf 4+ 0 1+ w+ 4+<br />
Reticulocyte Separation Cells<br />
Adsorbed serum<br />
4+ 0 4+ 0 0 4+<br />
The need is constant.<br />
The gratification is instant.<br />
Give blood. TM<br />
11
4/12/2011<br />
68<br />
Case Study #6: Patient History<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
• 73 year old male<br />
• Diagnosis: Lymphoma and severe anemia<br />
• Medications: Aspirin<br />
• Transfusion History: 3 units 6 months ago<br />
• Laboratory: Hemoglobin: 4.5 g/dL<br />
• 4 units requested STAT!!<br />
Patient w+ 4+ 4+ 4+ w+ 4+ 2+ 0<br />
Screening<br />
Cells<br />
IS<br />
PEG/IAT<br />
I 0 0<br />
II 0 0<br />
III 0 0<br />
Auto 1+ 3+<br />
DAT<br />
Anti-IgG<br />
Anti-<br />
C3dC3b<br />
Saline<br />
Control<br />
Patient 3+ 2+ w+<br />
What is the problem?<br />
Forward typing issue<br />
Investigation<br />
Patient age: 73 years old<br />
Diagnosis: Lymphoma<br />
Medications: Aspirin<br />
Resolution:<br />
Weak reactive front type,<br />
positive D control, positive<br />
saline control<br />
69<br />
70<br />
Forward type:<br />
Weak Reactivity<br />
Weak <strong>ABO</strong> subgroup? Malignancy? Spontaneous agglutination?<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
Patient w+ 4+ 4+ 4+ w+<br />
Warm washed cells<br />
w+ 4+ 4+ 4+ w+<br />
DAT<br />
Anti-IgG<br />
Anti-<br />
C3dC3b<br />
Saline<br />
Control<br />
Patient 3+ 2+ w+<br />
Warm washed cells<br />
1+ w+ w+<br />
Spontaneous agglutination was not resolved with warm washed cells.<br />
DTT (0.01M) treatment of the red blood cells should be performed to<br />
resolve the <strong>ABO</strong>/Rh discrepancy and disperse the spontaneous<br />
agglutination.<br />
Anti-A Anti-B Anti-A,B Anti-D<br />
D<br />
Control<br />
A 1 cells A 2 cells B cells<br />
Patient w+ 4+ 4+ 4+ w+ 4+ 2+ 0<br />
Warm washed cells<br />
w+ 4+ 4+ 4+ w+<br />
0.01 M DTT Treated Cells<br />
0 4+ 4+ 4+ 0<br />
71<br />
72<br />
DAT<br />
Anti-IgG<br />
Anti-<br />
C3dC3b<br />
Saline<br />
Control<br />
Patient 3+ 2+ w+<br />
Warm washed cells<br />
1+ w+ w+<br />
0.01 M DTT treated Cells<br />
1+ w+ 0<br />
Resolution:<br />
•Patient is B Positive<br />
•Positive DAT and autocontrol was further investigated by a reference<br />
laboratory, and it was discovered the patient had a warm autoantibody<br />
in his plasma.<br />
<strong>ABO</strong> discrepancy recognition AND resolution is<br />
imperative in the blood bank.<br />
<strong>ABO</strong> discrepancies can present themselves as a<br />
front type problem, reverse type problem, or<br />
combination of both.<br />
If <strong>ABO</strong> discrepancy resolution cannot be performed,<br />
and blood is needed immediately, transfusion of<br />
type O blood may be necessary.<br />
12
4/12/2011<br />
73<br />
References<br />
• Harmening, D.M. (2005). Modern Blood Banking and Transfusion<br />
Practices (5 th Ed.)<br />
• Roback, John et.al. Technical Manual, 16th Edition. City: American<br />
Association of Blood Banks (AABB), 2008.<br />
• American Red Cross: <strong>ABO</strong> Discrepancy Standard Operating<br />
Procedure<br />
• Community Blood Bank: University of Texas at Galveston Specialist<br />
in Blood Bank: <strong>ABO</strong> <strong>Discrepancies</strong>.<br />
13