PDF Format - American Nurse Today
PDF Format - American Nurse Today
PDF Format - American Nurse Today
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The Five P’s spell<br />
positive outcomes for<br />
ARDS patients<br />
Use these evidence-based interventions to avoid the<br />
dangers of ARDS, its complications, and its therapy.<br />
By Janice Powers, MSN, RN, CCRN, CCNS, CNRN, CWCN<br />
CE<br />
1.8 contact<br />
hours<br />
L E A R N I N G O B J E C T I V E S<br />
1. Identify the incidence of ARDS<br />
in the patient population.<br />
2. Discuss the causes and pathophysiology<br />
of ARDS.<br />
3. Describe strategies and nursing<br />
interventions for improving the<br />
outcomes of ARDS patients.<br />
IN THE UNITED STATES, patients<br />
with acute respiratory distress syndrome<br />
(ARDS) occupy 1 in 10 critical<br />
care beds. Each year, ARDS kills<br />
150,000 <strong>American</strong>s. Most of the<br />
deaths are triggered by an event,<br />
such as sepsis or pneumonia.<br />
What is ARDS?<br />
Usually, ARDS starts with acute<br />
lung injury (ALI), which kills about<br />
75,000 <strong>American</strong>s<br />
a year and whose<br />
risk increases with age.<br />
ARDS itself develops from an injury<br />
to the alveoli, the site of gas exchange.<br />
ALI and ARDS have these<br />
characteristics in common:<br />
• Acute onset<br />
• Bilateral infiltrates on chest X-ray<br />
• Pulmonary artery wedge pressure<br />
(PAWP) of less than 18 mm Hg.<br />
What distinguishes<br />
ALI from ARDS is the<br />
P/F ratio, the comparison<br />
of arterial partial pressure of<br />
oxygen (PaO 2 ) with inspired fractional<br />
concentration of oxygen<br />
(FiO 2 ). Simply put, the P/F ratio is<br />
a comparison of the amount of<br />
oxygen given to a patient with the<br />
amount of oxygen actually entering<br />
the patient’s bloodstream.<br />
34 <strong>American</strong> <strong>Nurse</strong> <strong>Today</strong> March 2007
The higher the P/F ratio, the better<br />
the gas exchange. The normal<br />
measurement is around 500 mm Hg.<br />
A P/F ratio below 300 mm Hg regardless<br />
of the positive end-expiratory<br />
pressure (PEEP) measurement<br />
indicates ALI. A P/F ratio below 200<br />
mm Hg regardless of the PEEP<br />
measurement indicates ARDS.<br />
If a patient’s oxygen requirements<br />
continue increasing while oxygen<br />
saturation levels (based on fingerprobe<br />
readings and arterial blood<br />
gas [ABG] measurements) remain<br />
low, ALI is progressing to ARDS.<br />
This condition is called refractory<br />
hypoxemia.<br />
A patient with ARDS has decreased<br />
functional residual lung capacity,<br />
which may lead to organ failure<br />
and death. Typically, ARDS<br />
requires admission to an intensive<br />
care unit (ICU) and mechanical ventilation.<br />
(See What causes ARDS?)<br />
What’s the damage?<br />
ARDS is marked by inflammation,<br />
increased permeability of alveoli<br />
membranes, and cytokine activation.<br />
Damage to the endothelium, or lining<br />
of the capillary, interferes with<br />
alveolar gas exchange. The damage<br />
causes macrophages to release cytokines,<br />
inflicting more damage on<br />
the alveolar endothelium. Protein<br />
levels build, pulling fluid into the<br />
alveolar spaces and causing noncardiac<br />
pulmonary edema and a reduced<br />
surfactant level.<br />
Normally, surfactant decreases<br />
surface tension and allows the alveoli<br />
to open easily. In ARDS, the edema<br />
and reduced surfactant level<br />
compromise gas exchange, causing<br />
decreased oxygen and increased carbon<br />
dioxide in the blood. The result<br />
is hypoxemia, pulmonary hypertension,<br />
and decreased pulmonary<br />
compliance. In later stages of ARDS,<br />
progressive alveolitis and fibrosis—<br />
stiff lungs—further decrease pulmonary<br />
function.<br />
Signs and symptoms<br />
In the first 24 to 48 hours, signs and<br />
What causes ARDS?<br />
Acute respiratory distress syndrome (ARDS) starts with a lung injury, either direct<br />
or indirect.<br />
Direct injuries<br />
With direct injuries, damage results from such events as:<br />
• near-drowning<br />
• aspiration<br />
• chemical inhalation<br />
• aspiration pneumonia.<br />
Indirect injuries<br />
With indirect injuries, damage results from an inflammatory response to an acute<br />
condition, such as:<br />
• sepsis<br />
• disseminated intravascular coagulation<br />
• shock<br />
• pancreatitis<br />
• multiple trauma.<br />
Cigarette smoking and alcohol abuse can also cause indirect injuries.<br />
symptoms include dyspnea, tachypnea,<br />
dry cough, fatigue, and tachycardia.<br />
Even with supplemental oxygen,<br />
a patient’s skin may look<br />
cyanotic and mottled. Auscultation<br />
reveals adventitious breath sounds<br />
(crackles, rhonchi, and wheezes) or<br />
increasingly diminished breath<br />
sounds. As oxygenation and perfusion<br />
diminish, the patient may become<br />
agitated, anxious, confused,<br />
and restless.<br />
A chest X-ray shows diffuse infiltrates,<br />
and ABG results indicate respiratory<br />
alkalosis with very low<br />
PaO 2 levels. In the later stages, hypercapnia<br />
may develop. Further<br />
metabolic imbalances can lead to<br />
mixed acidosis, signaling a low ventilation-to-perfusion<br />
(V . /Q . ) ratio and<br />
a deteriorating P/F ratio. To rule out<br />
a cardiogenic cause of pulmonary<br />
edema, a physician may order PAWP<br />
measurements.<br />
5 P’s of ARDS therapy<br />
Managing patients with ARDS requires<br />
maintaining the airway, providing<br />
adequate oxygenation, and<br />
supporting hemodynamic function.<br />
The five P’s of supportive therapy<br />
include perfusion, positioning, protective<br />
lung ventilation, protocol weaning,<br />
and preventing complications.<br />
Perfusion<br />
The goal of care for ARDS patients<br />
is to maximize perfusion in the pulmonary<br />
capillary system by increasing<br />
oxygen transport between the<br />
alveoli and pulmonary capillaries.<br />
To achieve the goal, you need to<br />
increase fluid volume without overloading<br />
the patient. Give either<br />
crystalloids or colloids to replace<br />
the fluids that have leaked from the<br />
capillaries into the alveolar spaces.<br />
Blood transfusions can improve<br />
oxygen delivery, but remember<br />
they can also cause an increased<br />
inflammatory response and increase<br />
the risk of infection and death.<br />
Evaluate the patient’s volume<br />
status by measuring blood pressure,<br />
respiratory variations of pulmonary<br />
and systemic arterial pulse pressure,<br />
central venous pressure, and urine<br />
output. Confirm intravascular status<br />
with pulmonary artery catheter data,<br />
cardiac output, cardiac index,<br />
pulmonary vascular resistance, and<br />
venous oxygen saturation (SvO 2 ).<br />
Certain drugs can also help increase<br />
perfusion. Inotropics such as<br />
dobutamine (Dobutrex) can increase<br />
cardiac output to boost oxygenation.<br />
Milrinone lactate (Primacor), another<br />
inotropic, improves perfusion by causing<br />
vasodilation in the pulmonary bed.<br />
March 2007 <strong>American</strong> <strong>Nurse</strong> <strong>Today</strong> 35
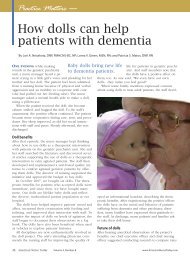
Turning your ARDS patient to the prone position<br />
Vasopressors, such as norepinephrine<br />
and dopamine, promote<br />
systemic vasoconstriction, thus increasing<br />
blood pressure and perfusion.<br />
When administering these<br />
drugs, monitor vital signs, skin color<br />
and temperature, and the patient’s<br />
tolerance to therapy.<br />
Positioning<br />
Patient positioning also affects perfusion.<br />
If a patient is standing, blood<br />
flow moves to the base of the lung<br />
and away from the apex. If a patient<br />
is supine, the posterior area of the<br />
lung will be more perfused than the<br />
anterior area. Because the better aerated<br />
surfaces of the lungs are the<br />
nondependent areas, the result is a<br />
ventilation/perfusion mismatch.<br />
The same thing happens with<br />
PEEP, which primarily aerates the<br />
anterior, nondependent areas of the<br />
lungs instead of the dependent areas<br />
that would benefit most.<br />
Immobility, a major cause of pulmonary<br />
complications, greatly influences<br />
perfusion distribution. Three<br />
positioning therapies can decrease<br />
these complications and improve<br />
perfusion in ARDS patients:<br />
• Kinetic Therapy (bilateral turning<br />
of a patient 40 degrees or more<br />
per side)<br />
• continuous lateral rotational therapy<br />
(bilateral turning of a patient<br />
no more than 40 degrees per side)<br />
• prone positioning.<br />
These therapies improve oxygenation<br />
by mobilizing secretions,<br />
resolving atelectasis, improving V . /Q .<br />
ratio, recruiting functional but collapsed<br />
or consolidated alveolar<br />
units, and decreasing interstitial fluid<br />
accumulation. Rotational therapy reduces<br />
nosocomial pneumonia, skin<br />
breakdown, ICU length of stay, and<br />
the number of ventilator days.<br />
There’s a correlation between the<br />
degree of rotation and the therapeutic<br />
benefit. With rotational therapy,<br />
the patient must be turned consistently<br />
to 40 degrees; otherwise, the<br />
therapy doesn’t significantly affect<br />
the clearance of secretions, risk of<br />
A<br />
pneumonia, or the length of ICU<br />
stay. Kinetic Therapy is effective in<br />
immobilized patients at angles up to<br />
62 degrees.<br />
Kinetic Therapy effectively prevents<br />
and treats severe respiratory<br />
complications of prolonged immobilization.<br />
When started early, it<br />
prevents and treats pneumonia and<br />
ARDS, saving hospital resources<br />
and lives.<br />
Using the prone position<br />
Prone positioning improves the V . /Q .<br />
ratio. Aeration improves because the<br />
heart no longer compresses the posterior<br />
areas of the left lung as it does<br />
in the supine position. With the patient<br />
in the prone position, most<br />
lung tissue, which is in the posterior<br />
areas, moves toward the anterior,<br />
clearing the airways of debris, decreasing<br />
atelectasis, reducing lung<br />
inflammation, and producing more<br />
efficient oxygenation and perfusion.<br />
Prone positioning can be<br />
achieved with or without a device,<br />
such as the Stryker frame,<br />
Triadyne Proning Accessory Kit,<br />
Vollman Proner, and RotoProne.<br />
If you’re not using a device, turn<br />
the patient from the supine position<br />
toward the ventilator, using the chest<br />
and pelvic area to allow for better<br />
diaphragm motion and lung mechanics.<br />
Depending on the size of<br />
B<br />
Turn the patient from the supine (A) to the prone (B) position with pillows or cushions<br />
supporting the chest and pelvis. When the patient is in the prone position, arrange the<br />
arms in the swimmer’s pose (C) and place the headrest appropriately (D). Be sure to align<br />
all tubes and drains at the head or foot of the bed to prevent dislodgement.<br />
C<br />
D<br />
the patient, the turn may take four<br />
to eight nurses. Place the patient in<br />
the prone position with pillows or<br />
cushions supporting the chest and<br />
pelvis to allow the abdomen to hang<br />
free. When the patient is in the<br />
prone position, arrange the arms in<br />
the swimmer’s pose—one at the side<br />
of the body and the other extended<br />
above the head. (See Turning your<br />
ARDS patient to the prone position.)<br />
Align all tubes and drains at the<br />
head or foot of the bed to prevent<br />
dislodgement. Rotate the patient’s<br />
head from side to side to relieve<br />
pressure and prevent skin breakdown.<br />
And reposition the patient<br />
every couple of hours and assess<br />
the pressure points.<br />
Using positioning devices<br />
The Stryker frame uses two boards<br />
that sandwich the patient to maintain<br />
the prone position. However,<br />
this device doesn’t offer any pressure<br />
relief or safety features.<br />
Both the Triadyne Proning Accessory<br />
Kit and the Vollman Proner<br />
make positioning the patient easier<br />
and more effective. The Triadyne<br />
Proning Accessory Kit consists of a<br />
sheet to aid in positioning the patient<br />
and position packs to support<br />
the patient in the prone position.<br />
The Vollman Proner positioning<br />
device is a frame with padding over<br />
36 <strong>American</strong> <strong>Nurse</strong> <strong>Today</strong> March 2007
the forehead, chin, chest, and pelvic<br />
areas and straps to aid in positioning<br />
the patient. The device goes on top<br />
of the patient, and you can use the<br />
straps to pull and roll the patient into<br />
the prone position. The patient<br />
then rests on the padded areas.<br />
The RotoProne bed is an automated<br />
system that combines Kinetic<br />
Therapy with prone positioning for<br />
up to 62 degrees. This device allows<br />
one nurse to make position changes<br />
and to provide several intervals of<br />
prone positioning throughout the<br />
day. In a 24-hour period, an ARDS<br />
patient should be in the prone position<br />
for at least 18 hours.<br />
Disadvantages of prone<br />
positioning<br />
Prone positioning does have its<br />
share of disadvantages, including<br />
possible tube dislodgement, patient<br />
desaturation, skin breakdown, and<br />
facial edema. With diligent nursing<br />
care and awareness, however, you<br />
can prevent or treat most of these<br />
complications.<br />
Typically, patients with refractory<br />
hypoxemia are placed in the prone<br />
position when ventilator settings are<br />
already maximized, with FiO 2 at<br />
100% and high levels of PEEP. We<br />
are learning that outcomes are better<br />
when positioning starts early in the<br />
course of ARDS.<br />
Protective Lung Ventilation<br />
During the early stages of ARDS, use<br />
mechanical ventilation to open collapsed<br />
alveoli.<br />
The primary goal of ventilation is<br />
to support organ function by providing<br />
adequate ventilation and oxygenation<br />
while decreasing the patient’s<br />
work of breathing. But<br />
mechanical ventilation itself can<br />
damage the alveoli, making protective<br />
lung ventilation necessary.<br />
In the past, ventilatory management<br />
of ARDS meant using high tidal<br />
volumes (VT) of 10 to 15 ml/kg to<br />
prevent atelectasis and normalize partial<br />
pressure of carbon dioxide with<br />
increased levels of PEEP to reduce<br />
Mechanical ventilation itself can<br />
damage the alveoli, making protective<br />
lung ventilation necessary.<br />
FiO 2 . But high VTs overstretch the<br />
alveoli, causing shearing forces on<br />
them and thus increasing the inflammatory<br />
response. The less affected<br />
lung regions must then accommodate<br />
most of the VT, which can lead to<br />
ventilator-induced lung injury (VILI)—<br />
a condition that exacerbates the physiologic<br />
responses to ARDS. VILI is a<br />
complex process caused by repetitive<br />
application of excessive stress or<br />
strain to the lung’s fibroskeleton, microvasculature,<br />
terminal airways, and<br />
delicate alveolar tissue.<br />
PEEP opens collapsed alveoli and<br />
prevents end-tidal alveolar collapse.<br />
This pressure also keeps the alveoli<br />
clear of fluid. For ARDS patients,<br />
ARDSNet guidelines recommend<br />
titration of PEEP up to a high level<br />
of 22 to 24 cm. Because PEEP can<br />
increase intrathoracic pressure that<br />
lowers cardiac output, you should<br />
use hemodynamic monitoring to determine<br />
the best PEEP setting for<br />
each ARDS patient.<br />
Research also shows that using<br />
continuous positive airway pressure<br />
at 35 to 40 cm H 2 O for 30 to 40 seconds<br />
can also open collapsed alveoli<br />
without severe hemodynamic compromise<br />
or barotrauma.<br />
Current recommendations for<br />
protective lung ventilation include:<br />
• limiting plateau pressures to less<br />
than 30 cm H 2 O<br />
• maintaining PEEP<br />
• reducing FiO 2 to 50% to 60%, if doing<br />
so doesn’t compromise PaO 2<br />
• providing low VTs (6 ml/kg of<br />
ideal body weight).<br />
Be sure to monitor the patient for<br />
changes in respiratory status—such<br />
as increased respiratory rate, adventitious<br />
breath sounds, decreased<br />
oxygenation saturation, and dyspnea—at<br />
least every 4 hours and after<br />
every change in PEEP or VT.<br />
Protocol weaning<br />
Weaning protocols can reduce the<br />
time and cost of care while improving<br />
outcomes for ARDS patients. The<br />
rule of thumb is: The patient either<br />
needs full ventilatory support or<br />
should be weaning. Evidence-based<br />
guidelines suggest the following:<br />
• using spontaneous breathing trials<br />
instead of synchronous intermittent<br />
mechanical ventilation<br />
• designing and implementing protocols<br />
for all appropriate healthcare<br />
professionals, not just physicians<br />
• tailoring protocols not as rigid<br />
rules but as guidelines to patient<br />
care<br />
• using protocols to enhance clinical<br />
judgment, not replace it<br />
• using sedation goals to reduce<br />
the duration of mechanical ventilation<br />
and ICU length of stay.<br />
Preventing complications<br />
The most common complications<br />
are VILI, deep vein thrombosis<br />
(DVT), pressure ulcers, decreased<br />
nutritional status, and ventilatorassociated<br />
pneumonia (VAP).<br />
Deep vein thrombosis<br />
DVT is an acute condition characterized<br />
by inflammation and thrombus<br />
formation in the deep veins<br />
that may lead to pulmonary embolism.<br />
About 16% of patients receiving<br />
mechanical ventilation develop<br />
DVT, typically during the first<br />
5 days in the ICU. To prevent DVT,<br />
therapy—including range-of-motion<br />
exercises, frequent position<br />
changes, anticoagulant prophylaxis,<br />
and use of sequential compression<br />
devices and thromboembolic stockings—should<br />
start on admission.<br />
Treatment for DVT includes these<br />
interventions:<br />
• applying warm, moist compresses<br />
• elevating the affected leg<br />
• administering anticoagulants,<br />
thrombolytics, and analgesics.<br />
Pressure ulcers<br />
Because of poor tissue perfusion<br />
March 2007 <strong>American</strong> <strong>Nurse</strong> <strong>Today</strong> 37
Using evidence-based interventions for VAP<br />
To decrease ventilator-associated pneumonia (VAP) in patients with acute respiratory<br />
distress syndrome, use these interventions:<br />
• Wear gloves and wash your hands frequently and effectively, particularly before<br />
touching the ventilator circuit.<br />
• Provide oral care every 2 hours.<br />
• Elevate the head of the bed 30 to 45 degrees.<br />
• Avoid instilling normal saline solution when suctioning the endotracheal tube.<br />
• Provide deep vein thrombosis prophylatic therapy.<br />
• Administer famotidine (Pepcid) to prevent ulcers.<br />
• Provide a daily sedation vacation, if appropriate.<br />
• Evaluate whether the patient is ready for weaning.<br />
and limited movement, pressure ulcers<br />
may develop. Nursing measures<br />
that may prevent this complication<br />
include relieving pressure with frequent<br />
position changes, restoring<br />
circulation with mobility, and promoting<br />
adequate nutrition. By assessing<br />
your patient’s skin frequently,<br />
providing meticulous skin care,<br />
monitoring nutrition status, and implementing<br />
pressure-relieving devices<br />
such as air mattresses, you can<br />
reduce the risk of pressure ulcers.<br />
Poor nutrition<br />
ARDS patients have a severely compromised<br />
nutritional status, so start<br />
nutritional support as soon as possible—within<br />
24 hours of admission,<br />
if possible. The preferred support<br />
method is enteral nutrition because<br />
it causes fewer complications than<br />
parenteral nutrition. When caring for<br />
an ARDS patient, be sure to consult<br />
with a nutrition expert.<br />
VAP<br />
As many as 40% of ARDS patients<br />
develop VAP, which is nosocomial<br />
pneumonia that develops after 48<br />
hours or more of mechanical ventilation.<br />
Most cases result from aspiration<br />
of bacteria from the mouth and<br />
GI tract. This condition complicates<br />
the ARDS patient’s recovery and requires<br />
a longer duration of mechanical<br />
ventilation and longer length of<br />
stay. (See Using evidence-based interventions<br />
for VAP.)<br />
Putting the 5 P’s into practice<br />
ARDS, its complications, and its<br />
therapy pose many dangers. By putting<br />
the five evidence-based P’s into<br />
practice, you can safely steer clear<br />
of all the dangers, while improving<br />
your patient’s outcome and decreasing<br />
his length of stay in the ICU. ✯<br />
Selected references<br />
Bernard GR. Acute respiratory distress syndrome:<br />
a historical perspective. Am J Respir<br />
Crit Care Med. 2005;172(7):798-806.<br />
Bernard GR, Artigas A, Brigham KL, Carlet J,<br />
Falke K, Hudson L, et al. The <strong>American</strong>-European<br />
Consensus Conference on ARDS.<br />
Definitions, mechanisms, relevant outcomes,<br />
and clinical trial coordination. Am J Respir<br />
Crit Care Med. 1994;149(3):818-824. Available<br />
at: http://ajrccm.atsjournals.org/cgi/content/<br />
abstract/149/3/818. Accessed January 17, 2007.<br />
Ely EW. Mechanical ventilator weaning protocols<br />
driven by nonphysician health-care<br />
professionals. Chest. 2001;120:454S-463S.<br />
Grap MJ, Munro CL. Preventing ventilatorassociated<br />
pneumonia: evidence-based care. Crit<br />
Care Nurs Clin North Am. 2006;16(3):349-358.<br />
Kollef M. Ventilator-associated pneumonia and<br />
ventilator-induced lung injury: two peas in a<br />
pod. Crit Care Med. 2002;30(10):2391-2392.<br />
Markowicz P, Wolff M, Djedaini K, Cohen Y,<br />
Chastre J, Delclaux C, et al. Multicenter<br />
prospective study of ventilator-associated<br />
pneumonia during acute respiratory distress<br />
syndrome: incidence, prognosis, and risk<br />
factors. ARDS Study Group. Am J Respir Crit<br />
Care Med. 2000;161(6):1942-1948.<br />
Marini JJ, Gattinoni L. Ventilatory management<br />
of acute respiratory distress syndrome:<br />
a consensus of two. Crit Care Med. 2004;<br />
32(1):250-255.<br />
Ware LB, Matthay MA. The acute respiratory<br />
distress syndrome. N Engl J Med. 2000;342<br />
(18):1334-1349.<br />
www.ihi.org/IHI/Programs/Campaign/<br />
Campaign.htm?TabId=2#PreventVentilator-<br />
AssociatedPneumonia<br />
For a complete list of selected references, visit<br />
www.<strong>American</strong><strong>Nurse</strong><strong>Today</strong>.com.<br />
Janice Powers, MSN, RN, CCRN, CCNS, CNRN, CWCN, is a<br />
Clinical <strong>Nurse</strong> Specialist at Critical Care and Neuroscience<br />
Methodist Hospital, Clarian Health Partners, in<br />
Indianapolis, Indiana. Ms. Powers has disclosed that<br />
she has received a speaker honorarium from KCI and<br />
Eli Lilly and Company within the previous 12 months.<br />
CE POST-TEST<br />
The Five P’s spell positive outcomes for ARDS<br />
Instructions<br />
To take the post-test for this article and earn contact hour credit,<br />
please go to www.<strong>American</strong><strong>Nurse</strong><strong>Today</strong>.com. Once you’ve successfully<br />
passed the post-test and completed the evaluation<br />
form, simply use your Visa or MasterCard to pay the processing<br />
fee. (Online: ANA members $15; nonmembers $20.) You’ll then be<br />
able to print out your certificate immediately.<br />
If you are unable to take the post-test online, complete the print<br />
form and mail it to the address at the bottom of the next page.<br />
(Mail-in test fee: ANA members $20; nonmembers $25.)<br />
Provider accreditation<br />
The <strong>American</strong> <strong>Nurse</strong>s Association (ANA) is accredited as a<br />
provider of continuing nursing education by the <strong>American</strong> <strong>Nurse</strong>s<br />
Credentialing Center’s Commission on Accreditation.<br />
ANA is approved by the California Board of Registered Nursing,<br />
Provider # CEP6178.<br />
Contact hours: 1.8. Expiration: 12/31/08.<br />
Purpose/goal: To provide registered nurses with an overview of<br />
ARDS, so they can deliver evidence-based care to ARDS patients.<br />
38 <strong>American</strong> <strong>Nurse</strong> <strong>Today</strong> March 2007
POST-TEST • The Five P’s spell positive outcomes for ARDS<br />
Earn contact hour credit online at www.<strong>American</strong><strong>Nurse</strong><strong>Today</strong>.com!<br />
(ANT070301)<br />
CE<br />
1.8 contact<br />
hours<br />
1. How many <strong>American</strong>s die from acute respiratory<br />
distress syndrome (ARDS)?<br />
a. 10% of the population a year<br />
b. 20% of the population a year<br />
c. 190,000 deaths a year<br />
d. 150,000 deaths a year<br />
2. Which of the following is a direct injury that<br />
causes ARDS?<br />
a. Disseminated intravascular coagulation<br />
b. Alcohol abuse<br />
c. Aspiration pneumonia<br />
d. Cigarette smoking<br />
3. Which of the following is an indirect injury<br />
that causes ARDS?<br />
a. Sepsis<br />
b. Asthma<br />
c. History of upper respiratory tract infection<br />
d. Sinusitis<br />
4. Which may contribute to the development of<br />
acute lung injury (ALI), a precursor of ARDS?<br />
a. Female sex<br />
b. Advancing age<br />
c. Asian heritage<br />
d. Illicit drug use<br />
5. Which drugs can improve perfusion by increasing<br />
cardiac output in ARDS patients?<br />
a. Inotropics<br />
b. Diuretics<br />
c. Anticoagulants<br />
d. Calcium channel blockers<br />
6. Which may be a side effect of giving blood<br />
transfusions to an ARDS patient?<br />
a. Increased inflammatory response<br />
b. Decreased oxygenation<br />
c. Increased skin infection<br />
d. Decreased peripheral vision<br />
7. Which positioning therapy reduces nosocomial<br />
infection and the number of ventilator days<br />
in ARDS patients?<br />
a. Kinetic Therapy<br />
b. Prone positioning<br />
c. Continuous lateral rotational therapy<br />
d. Lung percussion therapy<br />
8. Which of the following positioning therapies<br />
does not improve perfusion in ARDS patients?<br />
a. Lung percussion therapy<br />
b. Continuous lateral rotational therapy<br />
c. Supine position therapy<br />
d. Continuous positive airway pressure therapy<br />
9. Which is not a strategy for treating ARDS?<br />
a. High tidal-volume ventilation<br />
b. Positive end-expiratory pressure (PEEP)<br />
c. Prone positioning therapy<br />
d. Continuous positive airway pressure therapy<br />
10. Which is used to open collapsed alveoli?<br />
a. Increased tidal volume<br />
b. Supine positioning<br />
c. Increased carbon dioxide saturation<br />
d. PEEP<br />
11. Which is an effect of PEEP?<br />
a. Reduction in V . /Q . ratio<br />
b. Primary aeration of the anterior, nondependent<br />
lung areas<br />
c. Decreased number of functional alveoli<br />
d. Increased cardiac output<br />
12. Which of the following is an evidence-based<br />
guideline for weaning?<br />
a. Keep sedation at one level.<br />
b. Adhere strictly to protocols.<br />
c. Use spontaneous breathing trials.<br />
d. Use synchronous intermittent mechanical<br />
ventilation.<br />
13. Deep vein thrombosis (DVT) occurs most<br />
commonly:<br />
a. in the first day in the ICU.<br />
b. in the second week of hospitalization.<br />
c. in the first 5 days in the ICU.<br />
d. after discharge.<br />
14. What percentage of ARDS patients develop<br />
VAP?<br />
a. 40%<br />
b. 50%<br />
c. 60%<br />
d. 70%<br />
15. Which is an evidence-based intervention<br />
used to decrease VAP in ARDS patients?<br />
a. Administering analgesics<br />
b. Providing stringent wound care<br />
c. Using effective hand washing<br />
d. Using an air mattress overlay<br />
CE post-test registration form<br />
Are you a member of ANA/CMA? (circle) Yes No<br />
■ If “No,” please send me membership information.<br />
Test answers<br />
Test code: ANT070301<br />
a b c d a b c d a b c d<br />
1. ● ● ● ● 6. ● ● ● ● 11. ● ● ● ●<br />
2. ● ● ● ● 7. ● ● ● ● 12. ● ● ● ●<br />
3. ● ● ● ● 8. ● ● ● ● 13. ● ● ● ●<br />
4. ● ● ● ● 9. ● ● ● ● 14. ● ● ● ●<br />
5. ● ● ● ● 10. ● ● ● ● 15. ● ● ● ●<br />
Evaluation form<br />
1. In each blank, rate the extent to which you achieved each objective of this<br />
study module, from 1 (low/poor) to 5 (high/excellent).<br />
(1.) Identify the incidence of ARDS in the patient population. ____<br />
(2.) Discuss the causes and pathophysiology of ARDS. ____<br />
(3.) Describe strategies and nursing interventions for improving the outcomes<br />
of ARDS patients. ____<br />
Also rate the following from 1 to 5.<br />
2. To what extent were the purpose/goal, objectives, content, method, medium,<br />
and resources congruent and effective? ____<br />
3. To what extent was the article effective in achieving the overall purpose/goal? ____<br />
4. To what extent did the article meet your personal expectations? ____<br />
5. To what extent is the content applicable and usable in your nursing<br />
practice, specialty, setting, and role? ____<br />
6.. To what extent was the article free of evidence of bias from conflict of commercial<br />
interest, commercial support, product endorsement, and unannounced<br />
off-label product use? ____<br />
7. State the total number of minutes it took you to read the article and complete<br />
the post-test and evaluation. ____________________<br />
Please add your comments here: ______________________________________<br />
________________________________________________________________<br />
________________________________________________________________<br />
________________________________________________________________<br />
________________________________________________________________<br />
PLEASE PRINT CLEARLY<br />
E-mail address ———————————————————————<br />
Business phone ——————————————————————— State — — Zip ————— - ————<br />
Name ——————————————————————————<br />
Home phone ————————————————————————<br />
Mailing address ———————————————————————<br />
City ———————————————————————————<br />
Method of payment<br />
■ Check payable to <strong>American</strong> <strong>Nurse</strong>s Association.<br />
■ Visa ■ MasterCard<br />
Amount authorized $____________________________________<br />
PLEASE DO NOT SEND CASH<br />
Mail completed evaluation, post-test, registration form, and payment<br />
to: ANA, St. Louis, PO Box 504410, St. Louis, MO 63150-4410<br />
For credit cards:<br />
Account #<br />
■■■■■■■■■■■■■■■■■<br />
Security code (3 digit)<br />
■■■<br />
Expiration date________________________<br />
Authorized signature ________________________________________<br />
March 2007 <strong>American</strong> <strong>Nurse</strong> <strong>Today</strong> 39