FT Making Waves Sept 06 - James Paget University Hospitals
FT Making Waves Sept 06 - James Paget University Hospitals
FT Making Waves Sept 06 - James Paget University Hospitals
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
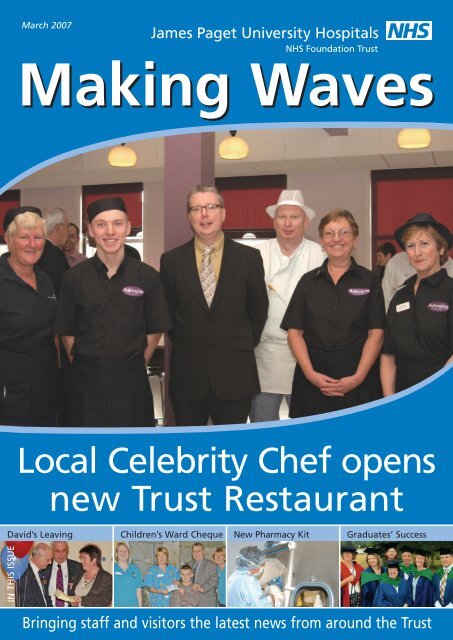
March 2007<br />
<strong>Making</strong> <strong>Waves</strong><br />
Local Celebrity Chef opens<br />
new Trust Restaurant<br />
David’s Leaving<br />
Children’s Ward Cheque New Pharmacy Kit Graduates’ Success<br />
IN THIS ISSUE<br />
Bringing staff and visitors the latest news from around the Trust
Editorial<br />
<strong>Making</strong> <strong>Waves</strong> has been swamped<br />
with material for this March<br />
edition, and we hope you like<br />
what we’ve selected for you. Not<br />
only have we said farewell to our<br />
Chief Executive David Hill, we’ll<br />
be welcoming his successor<br />
Adrian Pennington on 1st April.<br />
Find out what he’s looking<br />
forward to when he arrives at the<br />
<strong>Paget</strong> (opposite).<br />
We were also fortunate to<br />
have a local celebrity chef open<br />
our fabulous new staff restaurant<br />
in January. Richard Hughes really<br />
mucked in, rolling up his sleeves<br />
and having a laugh with our<br />
chefs. He was really impressed by<br />
the quality of food we offer<br />
patients and staff alike.<br />
We’ve completed our<br />
communications survey in the last<br />
few weeks. I was really pleased<br />
with the high response rate,<br />
showing that staff really do care<br />
about communications and want<br />
to help to make a difference. The<br />
results of this survey give us some<br />
really positive ways to improve<br />
internal communications in the<br />
Trust, and we’ll be working on<br />
these over the coming months.<br />
We want your feedback so let us<br />
know how you think we’re doing.<br />
The June <strong>Making</strong> <strong>Waves</strong> will<br />
be a special commemorative<br />
edition to celebrate our 25th<br />
anniversary. We’ll be on the look<br />
out for stories from all around<br />
our hospitals and clinics that<br />
celebrate the way healthcare has<br />
changed over the years, and<br />
personal memories from staff,<br />
patients and the local community.<br />
If you’ve got a story, please share<br />
it with us by email to<br />
rebecca.driver@jpaget.nhs.uk or<br />
on ext. 2268. The deadline is<br />
Friday 27th April.<br />
Rebecca Driver<br />
Head of Communications and<br />
Foundation Secretary ext. 2269<br />
2 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
Welcome to our<br />
new Chief Executive<br />
Adrian Pennington joins the <strong>James</strong> <strong>Paget</strong><br />
<strong>University</strong> Hospital on 1st April as our new<br />
Chief Executive.<br />
Adrian will be moving to the local area with his wife<br />
Linda, a nurse, and twin girls Harriet and Georgia, eight.<br />
Adrian went through a rigorous assessment process and<br />
joins the <strong>Paget</strong> from the national Heart Improvement<br />
Programme where he was Chief Officer. Adrian has worked<br />
in the NHS for 28 years and has a wealth of experience in<br />
acute hospitals, most recently as Deputy Chief Executive<br />
and Director of Operations at Northampton General<br />
Hospital. He has previously worked as a Divisional Manager in Plymouth <strong>Hospitals</strong>, and in<br />
a wide range of managerial roles in North Warwickshire Trust, Birmingham <strong>University</strong><br />
<strong>Hospitals</strong>, and George Eliot Hospital. He has significant Executive Board leadership<br />
experience.<br />
Asked about the challenge ahead, Adrian said: ‘I am really pleased to be joining the<br />
<strong>James</strong> <strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong> at a strong point in the hospitals’ history, having<br />
recently achieved NHS Foundation Trust status. I have visited hospitals all over the<br />
country and without doubt, the <strong>Paget</strong> is one of the friendliest I’ve been to. I hope to be<br />
able to help carry on the achievements of the hospital so far, and ensure that the <strong>James</strong><br />
<strong>Paget</strong> remains one of the best hospitals in the country.’<br />
On his plans and his management style, Adrian says staff will soon know his name<br />
and recognise who he is. ‘They will see me out and about regularly day and night,<br />
including some weekends. I am a leader who strongly believes that I need to understand<br />
the services and roles of people for whom I am responsible and can therefore make<br />
better more informed decisions. I will make every effort to schedule time on a regular<br />
basis to visit different departments, staff etc to talk about how they are doing. My<br />
management style, is and always has been open, honest, informative and I constantly<br />
look for opportunities to develop willing capable people.’<br />
Finally, on a personal note, Adrian says: ‘I am a big football fan and regularly travel to<br />
Anfield, Liverpool. My hobbies are not extensive, as I am usually shattered by the<br />
weekend! I enjoy a good film and a bottle of wine (shared of course). I love holidays to<br />
hot climates and, when I get the time, I like to keep fit in the gym or swimming.’<br />
Adrian will be arranging to meet staff as soon as he arrives so look out for more<br />
information in April and May.<br />
Farewell<br />
Russell Pearson, Deputy Director of Finance and Julie Smith, Matron, Lowestoft<br />
Hospital, have left the Trust recently to take up challenges elsewhere.<br />
We wish them every success in their new roles.<br />
Communications Survey<br />
Many thanks to everyone who took part in the communications survey and sent their<br />
completed questionnaire back. We’ve had a great response, and a report on the<br />
findings was presented to the Board of Directors at the end of February and will be<br />
shared with staff in March. This will help us to continue to improve our internal<br />
communications.<br />
The draw for the Argos vouchers was completed and the lucky winners are:-<br />
£30 – Margaret Hardesty, Finance Department<br />
£10 – Rebecca Piggott, ICU/HDU<br />
£10 – David Flatman, HSDU<br />
Once again, many thanks to all of you that took part.<br />
www.jpaget.nhs.uk
New Intranet<br />
for staff goes<br />
LIVE<br />
The new intranet went ‘live’<br />
on Monday 15th January.<br />
Hopefully it is already a<br />
useful resource for all staff –<br />
do let me know if you have<br />
any comments to make.<br />
There has been lots of<br />
interest from clinical<br />
departments wanting to<br />
manage their own page and<br />
more information will be<br />
available as these are<br />
added.<br />
I would like to say a<br />
personal thank you to<br />
everyone who enabled the<br />
launch to happen,<br />
particularly Andrew Palmer,<br />
Head of Information<br />
Services, Mike Scott and his<br />
IT team and Ann Bowles<br />
and Belinda Colman from<br />
the NPfIT training team,<br />
together with all the<br />
administrators for the<br />
current sections.<br />
Outpatient<br />
Project Update<br />
<strong>Making</strong> <strong>Waves</strong> caught up with Fran O’Driscoll for a progress<br />
report on the outpatient project.<br />
‘The outpatient project is progressing and the new management team led by<br />
Wendy Mitchell is in place. Over the next few months work will be undertaken to<br />
make sure there’s a clear understanding of the needs of each specialty now, and,<br />
most importantly in the future. The development of the Outpatient Assistant role<br />
will continue with many staff expressing an interest in moving into such a role.<br />
The plans for the new build have been finalised and the contract will be tendered<br />
soon. The new build will provide generic outpatient clinic facilities with associated<br />
diagnostic support and treatment rooms which will link into the current day care<br />
unit. On completion of the build there will be an upgrading programme for the<br />
other outpatient areas.’<br />
Fran finished by saying: ‘I would like to take this opportunity to offer thanks<br />
on behalf of the management team to all OP staff who have worked with us to<br />
make quite difficult changes during the course of this project.’<br />
Fran O'Driscoll<br />
Divisional Manager, Core Clinical Services Division<br />
Women and Child Health Division<br />
Nurses’ Graduation Success<br />
If you have any queries,<br />
or would like to manage<br />
your own section, please<br />
contact Ann Filby on<br />
ext. 2162<br />
■ Pictured are (left to right) Katharine Kite, Consultant Nurse, Kate Allen, Lecturer UEA, Helen<br />
Humber, Senior Staff Nurse, Bridget Inyang, Clinical Nurse Specialist, Sarah Robson, Senior Staff Nurse,<br />
Gavin Shiers, Charge Nurse, and in front - Michelle Butt, Clinical Nurse Specialist.<br />
We celebrated an important day last summer when, not only did we enjoy the<br />
success of some of our nurses in gaining their Honours degrees from UEA, but we<br />
also celebrated with our first graduates who had completed the PACS course<br />
(Practitioners’ Acute Care Skills Course) as the clinical module on their degree<br />
courses. This double module was developed specifically to help ward-based staff<br />
further their knowledge and skills in identifying and managing actually or<br />
potentially critically ill patients on the wards. It is now recognised as one of the<br />
most successful courses on the UEA post-registration programme. Kate Allen<br />
(pictured second from left) was instrumental in developing the course in her role as<br />
lecturer in critical care at UEA, along with Dr Katharine Kite (pictured far left),<br />
consultant nurse for critical care at the JPUH. Successful graduates were Helen<br />
Humber, Michelle Butt, Bridget Inyang, Sarah Philpot and Gavin Shears. Helen had<br />
completed the PACS modules for her degree, along with Sonia Cole who also<br />
graduated that day. Many congratulations to all.<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 3
18 weeks: The Consultant’s View<br />
From December 2008 patients across the NHS will wait no more that 18 weeks<br />
from their GP referral to the start of their treatment? David Ellis, Consultant<br />
Physician, told <strong>Making</strong> <strong>Waves</strong> how he’s getting involved to make sure the <strong>James</strong><br />
<strong>Paget</strong> meets this new Government target.<br />
I became closely involved with waiting time<br />
targets as part of the implementation of the<br />
National Cancer Plan, issued in 2000. The<br />
objectives were December 2005, to treat all<br />
new cancer patients within 31 days of diagnosis and to treat all new<br />
urgent suspected cancer referrals within 62 days. At first sight it<br />
seemed as though we had enough time to work on this but it soon<br />
became clear that we didn’t know:<br />
• what the definitions of the points on the patient pathway were,<br />
• what methods we might use to improve pathways,<br />
• what organisational changes were needed in order to monitor<br />
progress towards the targets.<br />
‘In the end we left some actions much too late in the day, leading<br />
to extra stresses for clinical and admin staff. Even now, when we have<br />
achieved the cancer waiting times, the task is not over. The need for<br />
constant monitoring of waiting times is always there. The challenge<br />
now is to make monitoring of cancer waits a part of routine clinical<br />
practice and not a separate admin task. Then there is the challenge of<br />
meeting the 2008 cancer waiting time target of 31 days from urgent<br />
referral to treatment!’<br />
‘So how is this relevant to the 18 week target for all treatments in<br />
secondary care? I think that we will need early engagement of<br />
clinicians throughout the Trust, in all disciplines. Clinicians and<br />
managers will need to look carefully at patient pathways, even those<br />
that look straightforward. We will need urgent action on the major<br />
diagnostic areas where there are long waits. It’s really important that<br />
we have good feedback on progress at all levels as this is an issue<br />
which we all share.’<br />
<strong>Making</strong> <strong>Waves</strong> caught up with 18 weeks Project Manager Helen<br />
French to find out what progress is being made. ‘Roll out of the new<br />
clinic outcome form began successfully in the clinics held within the<br />
Gynaecology department on 18th December 20<strong>06</strong>. This was followed<br />
by the clinics held within the Department of Medicine from 1st<br />
January 2007. Roll out will continue over the following weeks to<br />
incorporate Surgical Outpatients and all clinics held on the JPUH site.<br />
Attention then focussed on outreach clinics held at other localities off<br />
site. It is anticipated roll out will be completed by the end of March<br />
2007. Each specialty has a Consultant 18 week representative who has<br />
taken the lead on producing the "Crib sheets" in consultation with<br />
their colleagues. This document provides examples which facilitate the<br />
completion of the new outcomes form. All crib sheets developed so<br />
far are available on the new Trust intranet.’<br />
Patient Confidentiality it’s up to YOU!<br />
We all work for the NHS, so we think we know how to keep<br />
information on patients safe. But are we all as careful as we<br />
could be? Here, Russ Crawford, Data Quality Manager, gives<br />
us a reminder about why patient confidentiality is so<br />
important.<br />
There are two new documents on the Trust intranet that<br />
need to be read and understood; Patient Confidentiality Policy<br />
and Data Confidentiality - Keeping a Clear Desk and Screen.<br />
Remember, patient confidentiality is all about:<br />
• telling patients in advance what we will do with any<br />
information they give to us<br />
• recording and storing any information about patients in a<br />
secure way<br />
• giving patients options on how we use information about<br />
them<br />
• ensuring information is not used or disclosed without the<br />
patient’s agreement<br />
Patients entrust us with sensitive, personal information<br />
about themselves and their health as part of seeking<br />
treatment from us. They do so in confidence and they have<br />
the expectation that Trust staff will respect their personal<br />
privacy and act appropriately.<br />
All staff members with access to confidential personal<br />
information have a duty to keep that information safe and<br />
secure, and should be aware of their responsibilities.<br />
It’s essential for us to maintain the confidence of our<br />
patients by demonstrating that the Trust provides a<br />
confidential service. Any information that can identify<br />
individual patients must not be used or disclosed for purposes<br />
other than health care, without the individual’s explicit<br />
agreement (unless there is a robust public interest or legal<br />
justification to do so).<br />
Recent Department of Health guidance gives advice on<br />
seeking the patient’s permission to record data about them,<br />
under what circumstances that information will be shared<br />
(including with the Police) and how that information will be<br />
shared in a secure manner (Safe Haven Policy).<br />
This data confidentiality document provides best practice<br />
guidance on keeping information safe. The principle behind<br />
this is for all staff to adopt ‘clear desk and clear screen’<br />
practices, to reduce the risks of unauthorised access,<br />
accidental damage to or the loss of sensitive or confidential<br />
information.<br />
Please be aware of these documents and include their<br />
contents in your everyday working life.<br />
If you want to know more, call Russ on ext. 3833<br />
4 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
A Day in the Life of…<br />
Les and Keith – Domestics<br />
Affectionately known to<br />
all staff on the<br />
orthopaedic wards as<br />
‘The Twins’, Keith and<br />
Les are the Domestics<br />
based on Wards 6 & 7<br />
respectively. Both men<br />
are former school<br />
caretakers and there is<br />
only 9 months<br />
difference between<br />
them in age. They are<br />
also the first ward based male domestics. Les lives locally in<br />
Rollesby and it was family ties that brought Keith to this area.<br />
Keith’s father was a patient at JPUH and on his regular<br />
weekend trips from north London to visit, his father would<br />
often say to him that he ought to find a job at the <strong>Paget</strong>. It was<br />
on such a trip that Keith noticed an advert for the post of<br />
domestic and he applied and was successful. Alas Keith’s father<br />
died and did not get to see his son working in an environment<br />
that he knew would be ideal for him.<br />
Although their day starts officially at 7am, Keith and Les<br />
meet up in the ward kitchen at around 6.45am. Patients can<br />
always be guaranteed of a big smile as they get their first<br />
cuppa of the day. Jugs and glasses are collected, bins are<br />
emptied and the lads are back with the trolley for breakfasts at<br />
8am. After this has been done and all trays collected and put<br />
onto the trolley for the kitchen, the lads put on their aprons<br />
and rubber gloves and start cleaning the floors. They are<br />
renowned for their buffing skills!! Keith has exacting standards<br />
when it comes to beds, lockers and chairs as he likes to ensure<br />
that these are all kept straight and tidy. Woe betide any staff<br />
who undo his good work especially if they drag chairs across his<br />
beautifully buffed floors. Both Les and Keith are very aware of<br />
the importance of infection control measures on the ward and<br />
are always ready for an impromptu visit by Matron who is<br />
renowned for her high standards. There is rivalry between the<br />
lads when it comes to the high and low dusting. Cleaning is a<br />
continual process on the wards with washing of the lockers etc.<br />
and Keith and Les maintain a good rapport with patients at all<br />
times. The lads are also supported by other domestics. The day<br />
finishes for Les at 1pm after the patients have had their lunch<br />
and Keith continues until 3pm incorporating afternoon tea.<br />
Both men take extreme pride in<br />
keeping their wards clean and tidy.<br />
In fact Rosie Winterton, when she<br />
met Keith and Les on her visit, told<br />
them she had heard how clean their<br />
wards were! Praise indeed.<br />
25th<br />
Anniversary<br />
Celebrations<br />
Gather Pace<br />
To celebrate these 25 years the following activities are being planned:<br />
• Exhibition in Boardroom from Monday 16th to Saturday 21st July<br />
• Golf Tournament organised by Gorleston Golf Club on Friday 13th July<br />
• Conference in Burrage Centre on Friday 20th July. Presentations of 10 minutes each looking at<br />
how diseases and their management have changed.<br />
• Fete at the Hospital on Saturday, 21st July<br />
• Petanque Competition organised by Burrage Centre Team on 22nd July<br />
• Articles in local newspapers about the Hospital<br />
• Special issue of <strong>Making</strong> <strong>Waves</strong> giving historical details about the hospital with programme of<br />
events of the celebrations<br />
• Other activities which will bring together people in the local community, publicise the hospital<br />
and hopefully raise some money<br />
If you or your department would like to be involved with any of these activities please contact:<br />
For Exhibition: madeleine.borg@jpaget.nhs.uk<br />
Conference: tracy.moyse@jpaget.nhs.uk<br />
<strong>Making</strong> <strong>Waves</strong> and articles for local newspapers: rebecca.driver@jpaget.nhs.uk<br />
Hugh Sturzaker<br />
Chairman – 25th Anniversary Committee<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 5
Farewell to David<br />
On Wednesday 15th November, over 250<br />
people gathered in the Celebration Suite to bid<br />
farewell to the Chief Executive, David Hill.<br />
There was a real cross section of staff present<br />
from both within and outside the organisation,<br />
reflecting the high regard that David is held in<br />
by everyone who knew him.<br />
The event began with a speech from Trust Chairman, John<br />
Hemming, who highlighted David’s achievements over the<br />
years. These included meeting cancer waiting time targets,<br />
reducing waiting times for patients in A&E, the opening of the<br />
EADU and the links forged with the UEA that have resulted in<br />
the <strong>Paget</strong> training one third of their medical students in our<br />
new Education and Training Centre. The Chairman said: ‘David,<br />
you are so helpful and friendly, everyone thinks so. There will<br />
always be something of you in the <strong>Paget</strong>.’<br />
Then Dr David Ellis took the stage, with a powerpoint<br />
presentation on the reasons why David would be leaving the<br />
<strong>Paget</strong> to go to Bermuda. These included the availability of a<br />
drink on the sub tropical island called ‘dark and stormy’,<br />
reputed to make your hair grow, to becoming a member of the<br />
famous Tucker’s Point golf course, of which Catherine Zeta<br />
Jones is a member. There were a lot of laughs, particularly at<br />
the photo of David asleep on a boat in a woolly hat! David Ellis<br />
said: ’It is a true honour to speak at your leaving presentation.<br />
You are always smiling, kind and considerate, a friend to<br />
everyone. You make people feel comfortable and you are very<br />
modest about your achievements.’<br />
David Hill spoke last, and was clearly moved by the words<br />
that had already been said. He spoke whilst his wife Jan looked<br />
on. He said: ‘It is fantastic to see everyone here. It is all of you<br />
who have made things happen at the <strong>Paget</strong> and made it the<br />
success it is. But the wider health system, the wider health<br />
community is also important and our network must continue if<br />
the <strong>Paget</strong> is to continue to be successful. The people at the<br />
<strong>Paget</strong> have talent, and passion, and they care. This is what<br />
really matters.’<br />
David paid special thanks to three people. He mentioned his<br />
PA Wendy Burman, who he admitted actually ‘ran the place’,<br />
and to the two Chairmen with whom he has worked, John<br />
Wells and John Hemming.<br />
David finished with a special thank you to his wife Jan. He<br />
said: ‘You cannot believe the fond memories that Jan and I<br />
have of this place. We will remember these and all of you as we<br />
set off on our next adventure.’<br />
Jan was presented with an amber necklace and earrings set,<br />
and David was presented with a book of thoughts and<br />
memories from staff, a watch and a set of engraved glasses<br />
with the new Trust logo on them.<br />
■ Pictured: David with his wife Jan and John Hemming. David shares a joke<br />
with Dave Todd from Pharmacy and with Dr Nottcutt and Dr Forster.<br />
Fundraising Success for<br />
Catering Department<br />
The Trust’s Catering Department held a Christmas Fayre in December to raise<br />
money for the Palliative Care Appeal. They had a range of traditional stalls<br />
selling homemade cakes, a raffle and a tombola. They managed to raise a<br />
magnificent £507 which was gratefully received by Patrick Blossfeldt on<br />
behalf of the appeal.<br />
Andrew Head, Catering Manager said: ‘I want to thank everyone who<br />
got involved in this event in the catering department. They put in a lot of<br />
hard work to organise the day, particularly David Himpleman who drummed<br />
up the support from local businesses and collected all the prizes.’<br />
Thanks to all local businesses who supported the appeal by generously<br />
donating prizes.<br />
Charity walk<br />
for ICU<br />
The Great Yarmouth Rotary Club<br />
Spring Charity Fun Walk will be held<br />
at Somerleyton on Sunday 20th May.<br />
They will be raising money for our<br />
Intensive Care and High Dependency<br />
Unit. Matron Rosemary Smalley said:<br />
‘This will be a great day out for all<br />
the family, and it will raise money<br />
for a good cause at the same time.<br />
We hope that staff will be able to<br />
support this charity fun walk.’<br />
6 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Newberry Feeding Clinic –<br />
Helping young children with feeding problems<br />
The Newberry Feeding Clinic has been running<br />
since 1998. It was set up to help children under<br />
5 years with complex feeding difficulties.<br />
The team see children with cerebral palsy, developmental<br />
delay, autism, Prader-Willi, food sensitivities and bowel disease.<br />
In spite of their difficulties, the team found that the mainstay<br />
of treatment plans was balancing nutritional requirements with<br />
a behavioural approach, once the treatment plan was<br />
alleviating any symptomatic pathology. They felt the<br />
techniques could be used by other professionals who support<br />
children and families, for example, a child who will not eat<br />
after an episode of tonsillitis. So they decided to hold a Study<br />
Day in <strong>Sept</strong>ember 20<strong>06</strong>. Here, Dr Louise Eastwood, Community<br />
Paediatrician (now retired), tells <strong>Making</strong> <strong>Waves</strong> how it went.<br />
Our study day was really well attended. The team presented<br />
papers on breast feeding, the health visitor feeding advice<br />
service in Great Yarmouth, the dental management of children<br />
with feeding problems, the readiness for textures promoting<br />
early feeding, the use of thrive lines, calcium and iron nutrition,<br />
helping with fussy eaters and gave an audit of the Newberry<br />
Feeding Clinic.<br />
A few facts from the presentations worth a mention include:<br />
• In Great Yarmouth in 2005, 58% of mothers started breast<br />
feeding, but after 1 month 54% of these had given up<br />
breast feeding.<br />
• Resistant eaters have limited food selection and food<br />
groups, and show anxiety and tantrums when given new<br />
foods. The Health Visiting Feeding Advice Service can help<br />
with this. Contact needs to be intensive and frequent in<br />
order to find realistic and long term solutions for these<br />
children.<br />
• Resistant eaters may be very sensory sensitive. Readiness for<br />
textures is a developmental milestone. A stable sitting<br />
position, the ability to move food around the mouth and<br />
chewing practice are required.<br />
• Tam Fry demonstrated the use of the 5% and 95% Thrive<br />
Lines. These allow predictions of under and over feeding<br />
from weight gain for those under 2 years old, and therefore<br />
earlier intervention if there is a problem.<br />
• 17% of children under 5 years of age in industrialised<br />
countries are anaemic. The Department of Health<br />
recommends:<br />
• Not giving cows milk which is low in iron as the main<br />
drink before 12 months of age.<br />
• Introducing meat and fish from 6 to 8 months of age<br />
• Providing fruit, vegetables or vitamin C at every meal<br />
to increase the absorption of iron.<br />
• Not giving tea and coffee at meal times because they<br />
reduce absorption.<br />
In discussion the following points were raised:<br />
• The talk on breast feeding was much appreciated, although<br />
it was recognised that some mothers are unable to breast<br />
feed and care should be taken not to make them feel guilty<br />
about this.<br />
• Several people felt they would like more on behavioural<br />
management, especially for autistic children.<br />
• The staff from Lothingland felt that they needed more<br />
support for children with learning difficulties and feeding<br />
problems.<br />
• Constipation was often an associated problem for children<br />
with feeding difficulties.<br />
• All Health Visitors should be using thrive lines. At the<br />
moment on request SMA will provide these for some<br />
registered Health Visitors, but if necessary they should be<br />
provided by their employing trust.<br />
We ran this day with £500 from the legacy fund and support<br />
from three Pharmaceutical Companies. There was no charge for<br />
attendance and we appreciated the excellent support of the<br />
Feeding Clinic Secretary. I feel it was money well spent.<br />
Dr Louise Eastwood<br />
Community Paediatrician<br />
• Calcium and iron intake are really important for<br />
development. Bone length is improved by exercise.<br />
Therefore, calcium intake is particularly important for<br />
children with restricted mobility.<br />
For more information on the Newberry<br />
Feeding Clinic, please telephone:<br />
01493 442322<br />
www.jpaget.nhs.uk<br />
■ The speakers from left to right: Marie Hearney, Judith Worthy , Bernie<br />
Lipscombe, Patrick Friel, Sam Paolantonio , Eve Harrison, Louise Eastwood<br />
and Sue Foster.<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 7
Fund raising going<br />
Telephone<br />
Jenny<br />
01493 453348<br />
jenny.westgate@jpaget.nhs.uk<br />
well for Appeal<br />
The public appeal for the East Coast Palliative Care Centre which was<br />
launched last October is well underway with a running total of £76,525.17<br />
at the end of January 2007. The Centre will provide a welcoming familycentred<br />
environment for patients and their families whose lives are<br />
affected by cancer and other life-threatening illnesses.<br />
Professionals and volunteers will work<br />
hand in hand at the centre and support<br />
patients and families with the aim of<br />
improving their quality of life.<br />
The vision for the centre is to bring<br />
together the art and science of care.<br />
The science of care will be represented<br />
by first class clinical facilities for the<br />
assessment and management of pain and<br />
other physical symptoms, as well as help<br />
for emotional needs through psychological<br />
support and counselling and social needs<br />
through financial and benefits advice.<br />
The art of care is about setting these<br />
services in an attractive therapeutic<br />
environment, full of light, warmth and<br />
welcome which can inspire peace and hope<br />
and offer space for the soul as well as care<br />
for the body.<br />
The art of care is further expressed<br />
through a beautiful garden, drawing on<br />
the therapeutic power of nature, a creative<br />
interior design incorporating works of art<br />
and the exploration of artful therapies<br />
such as complementary therapies, music<br />
and art therapy.<br />
An architectural design competition is<br />
underway which draws on the creative<br />
power of local and regional architectural<br />
firms in order to find the best design. By<br />
the end of March / early April, the winner<br />
of the competition will be known so watch<br />
out to see in the media what the centre<br />
will look like.<br />
If you have ideas about fundraising, or want<br />
to make a contribution or have questions<br />
about the appeal, please don’t hesitate to<br />
phone Jenny on 453348.<br />
Dr Patrick Blossfeldt who is lead<br />
consultant for palliative care and also<br />
heads the campaign for the East Coast<br />
Palliative Care Centre said: ‘I will be<br />
running the London Marathon to raise<br />
money for the public appeal. I love running<br />
but I’ve never done a marathon before! I’d<br />
like to ask all people who know me for<br />
their sponsorship and support please.<br />
Sponsor forms are available from the Pain<br />
Clinic or Jenny Westgate, the palliative care<br />
appeal coordinator.’<br />
Planned Events (so far) 2007<br />
9th March<br />
In the Mood Dinner and<br />
Dance Ocean Rooms /£25.00<br />
23rd March<br />
Race Night, Cliff Hotel, Gorleston<br />
Hot buffet meals / £10.00<br />
8th April<br />
Sponsored Dog Walk, Gorleston<br />
21st April<br />
Artichoke Day – Ladies day, Fashion show,<br />
Jewellery, Make up artists, Manicures,<br />
Indian head massage.<br />
20th May<br />
Annual Somerleyton Walk<br />
7th July<br />
St Lawrence, South Walsham. The Big Sky<br />
Singers will be giving a concert in support<br />
of the Palliative Care Appeal.<br />
25th <strong>Sept</strong>ember<br />
Ready, Steady, Cook hosted by<br />
The Lavender House, Brundall<br />
Date TBA<br />
Fashion Show, Cliff Hotel, Gorleston<br />
with Sophisticats<br />
1st / 2nd November<br />
Art Exhibition of local artists<br />
8 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Play Specialists<br />
share their<br />
Knowledge<br />
As part of our role as advocates for children, young people and<br />
their families, we network with other professional bodies both<br />
nationally and regionally including the National Association of<br />
Hospital Play Staff (NAHPS) and the East Anglian Hospital Play<br />
Staff (EAHPS). In July of this year, we hosted a successful<br />
regional study day here at the <strong>James</strong> <strong>Paget</strong> <strong>University</strong> Hospital<br />
looking at ways of implementing the National Service<br />
Framework (NSF) for children, young people and maternity<br />
services through the eyes of a Play Specialist including the use<br />
of audit tools, evidence based research, benchmarking etc.<br />
We were then invited to share our experiences and the<br />
work we have carried out by giving a full presentation at the<br />
NAHPS Annual Hugh Jolly memorial lecture / conference<br />
afternoon at Great Ormond Street Children’s hospital in<br />
London on 1st November 20<strong>06</strong><br />
The meeting was chaired by Jackie McClelland, play coordinator<br />
at Addenbrookes and also vice chairman of NAHPS.<br />
We wanted to share the experience with you and give a<br />
snapshot of the kind of work we are continuing to do to put<br />
play on the map. We were able to show the ways in which we<br />
have gathered our documentation over the past three years<br />
since the introduction of the first NSF documents in April 2003.<br />
We talked about how the play service has developed and the<br />
ways in which we have helped to improve play facilities, child<br />
friendly environments and access to the appropriate<br />
information/therapeutic play preparation for children, young<br />
people and families throughout the Trust. This included joining<br />
the Accident and Emergency team working shifts on a weekly<br />
basis.<br />
❝ We were also privileged to be amongst the first<br />
members of NAHPS to see and obtain the new Audit<br />
Tool for Play as it was launched at the conference. It is<br />
fronted by Dr Patricia Hamilton (President, Royal College<br />
of Paediatrics and Child Health) and gives us clear<br />
guidelines to enable us to work towards reaching the<br />
standards set by the Healthcare Commission. This<br />
document replaces the 1991 Quality Management for<br />
Children (Hospital Liaison Committee). ❞<br />
The day gave way to discussion and evaluation of how play<br />
staff from other Trusts are managing in the current climate<br />
and we gained valuable experience, especially in how to keep<br />
calm in front of a room full of adults!<br />
Jane Whiteside and Jeanette Cotton, Senior Hospital Play<br />
Specialists, Ward 10<br />
Nursery is a hit with<br />
little ones<br />
Busy Bees at <strong>James</strong> <strong>Paget</strong> is situated in the hospital<br />
grounds. It’s a brand new purpose built nursery for up to<br />
71 children aged 0-5 years. The nursery consists of five<br />
separate rooms made up of five different age groups. All<br />
the staff are qualified and very experienced. We offer<br />
extra curricular activities including PRESMA music<br />
sessions. We have our own chef on site and will cater for<br />
your child’s individual needs.<br />
The nursery is Ofsted inspected and offers a very high<br />
standard of quality childcare and education. Look out<br />
for special offers, open evenings/days and fun filled<br />
events throughout the year!<br />
Spaces are available but please book quickly to avoid<br />
disappointment. If you have any enquiries or want to<br />
have a look around the nursery, please don’t hesitate to<br />
contact Jenny Norton, Manager, on 01493 661583 for an<br />
appointment.<br />
Marathon run for<br />
local charity<br />
Tracy Moyse will be running the Flora London Marathon<br />
on 22 April this year in aid of the Special Objectives for<br />
the Local Disabled (SOLD) charity.<br />
For those of you that do not know, Tracy is<br />
PA/Executive Assistant to the Chairman, Medical Director<br />
and the Head of Communications. The aim of SOLD is to<br />
promote the welfare of disabled, blind and long term<br />
sick people within the Suffolk and Norfolk area.<br />
If you would like to sponsor Tracy for this event you<br />
can do so by popping along to her office in the<br />
Executive Corridor or giving her a call on x2268 or via<br />
tracy.moyse@jpaget.nhs.uk<br />
All donations gratefully received, no matter how<br />
small, as it will all go towards a good cause in<br />
helping the lives of our local disabled people.<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 9
Local Celebrity Chef opens<br />
Staff can eat in style now, thanks to a full refurbishment of our staff restaurant. The new facility was<br />
officially opened on Monday 29th January by local celebrity Chef Richard Hughes from the Lavender<br />
House in Brundall.<br />
Richard writes regularly for EDP Norfolk magazine and is very<br />
well known in the local area. He was thrilled to be invited<br />
along and to get a taste of catering at the sharp end as he<br />
worked with our chefs cooking for patients and staff in our<br />
hospital kitchens!<br />
Nichola Hicks, Head of Support Services at the <strong>James</strong> <strong>Paget</strong><br />
<strong>University</strong> <strong>Hospitals</strong> NHS Foundation Trust said. ‘Our staff dining<br />
room had not been updated for over 20 years. It was so shabby<br />
and really needed a makeover. I’m sure everyone will remember<br />
the striking paisley wall paper and matching curtains which<br />
were removed, and the worn out carpet. The first stage of the<br />
project included the replacement of the windows followed by<br />
radiators, flooring, ceiling and lighting. The old furniture was<br />
then replaced with modern tables, chairs and leather sofas.’<br />
Nichola continued: ’The refurbishment was completed over<br />
six months, and we now have a fantastic facility for all our staff.<br />
A recent competition named the new-look restaurant<br />
‘Aubergine’ recognising the calming colours it’s been decorated<br />
in. We have leather sofas in a relaxed eating area. It’s really<br />
important that staff have a haven from the day to day business<br />
in the hospital to get a break and catch up with colleagues.’<br />
A final touch will soon be added in the form of some backlit<br />
art work from the hospital Arts Committee.<br />
❝ I was delighted to be asked to open this<br />
new facility for staff at the <strong>James</strong> <strong>Paget</strong><br />
<strong>University</strong> Hospital. Everyone knows how hard<br />
health professionals work to provide the local<br />
community with high quality services. This new<br />
restaurant gives them a place to relax for a<br />
short while before returning to their hectic<br />
schedules. I have been really impressed with<br />
the relaxed feel of the place, and the quality of<br />
the food produced for staff and visitors alike,<br />
using locally sourced produce. ❞<br />
As he left, Richard offered to bring along three of his chefs<br />
to work alongside our catering team to cook up a speciality<br />
themed lunch for staff. It’s hoped that this will be in the<br />
summer, so keep an eye out for details.<br />
Well done to Sue Allen, Dietician who came up with the<br />
winning entry ‘Aubergine’ as the name for the new restaurant.<br />
Other entries that made it to the final shortlist were ‘Hill’s<br />
Kitchen’ (in homage to our last Chief Executive of course!),<br />
‘Mango’ and ‘<strong>University</strong> Retreat’.<br />
10 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Richard with<br />
the Dietiticans<br />
department<br />
who came up<br />
with the name<br />
‘Aubergine’<br />
Thank you to everyone<br />
involved in making<br />
this project a success<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 11
Essence of Care Update<br />
The NHS Plan (2000) reinforced and stressed the<br />
importance of improving the patient<br />
experience by delivering quality patient care by<br />
focusing on “getting the basics right”.<br />
The Essence of Care document was launched by the<br />
Department of Health in February (2001) as a benchmarking<br />
tool to address the unacceptable variations in the quality of<br />
care being delivered nationally and to help practitioners take a<br />
patient-focused and structured approach to sharing and<br />
comparing practice. It has enabled practitioners to work with<br />
patients to identify best practice and to develop action plans to<br />
improve care. (NHS Modernisation Agency 2003).<br />
Collaborative working between patients, carers and<br />
professionals resulted in agreement of good quality care and<br />
best practice. This resulted in benchmarks covering nine<br />
fundamental areas of care including continence, bladder and<br />
bowel care, personal and oral hygiene, privacy and dignity and<br />
food and nutrition.<br />
Essence of Care within the Trust was launched in March<br />
2003.<br />
Food and Nutrition<br />
The first benchmark to be tackled was food and nutrition, the<br />
benchmark was completed in <strong>Sept</strong>ember 2003 and then<br />
audited in August 2004. A re-audit took place May 20<strong>06</strong>.<br />
Achievements within the Food and Nutrition benchmark<br />
include:<br />
• Introduction of protected meal times (in some clinical areas).<br />
• The increase of food availability between meal times and<br />
out of hours.<br />
• Increased availability of hand wipes of patients and use of<br />
hand gel prior to meal times.<br />
• All patients nutritional statuses are assessed by use of a<br />
malnutrition universal screening tool (MUST). All at risk<br />
patients will have a plan of care.<br />
• All food and fluid intake are documented appropriately.<br />
• All wards should have a nutritional link nurse.<br />
• Increased carbohydrate choice to the normal menu.<br />
• Annual calibration of all Trust scales.<br />
• Use of red trays to highlight patients who are nutritionally<br />
compromised.<br />
• Nutrition Study days and staff training.<br />
Privacy and Dignity<br />
The second benchmark was launched October 2004. Re-audit<br />
April/May 20<strong>06</strong>. To assist ward staff Nurse Education performed<br />
the second re-audit.<br />
Achievements with the Privacy and Dignity benchmark:<br />
• ‘Please Do Not Enter’ signs for doors and curtains.<br />
• Raising awareness of private/quiet rooms for patients.<br />
• Shredding of confidential information, e.g. Handover sheets.<br />
• Increased awareness of discussing confidential information<br />
in patient areas, e.g. change of handover procedures and<br />
white board information.<br />
12 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
• White Board Policy on Intranet describing only essential<br />
information.<br />
• Increasing staff awareness of the Code of Valued<br />
Behaviours.<br />
• Patients having access to a telephone for private<br />
conversations, cordless telephones now available in some<br />
ward areas.<br />
• Chaperone policy now available on Intranet.<br />
Continence Care<br />
This third benchmark commenced in <strong>Sept</strong>ember 2005 with a reaudit<br />
requested for February 2007.<br />
Achievements to date with the Continence benchmark:<br />
• All wards and departments now have continence education<br />
material for patients and visitors.<br />
• Posters providing information on continence advice and<br />
help lines have been designed.<br />
• Home packs for patients with catheters to be available on<br />
all wards that want them and training for use available.<br />
Use of these packs will ensure a better service for patients<br />
and will potentially save the Trust £6000 per year.<br />
• Coloplast training, promoting urinary continence education<br />
and staff awareness.<br />
• Flow charts and continence assessments have been<br />
produced.<br />
• A new continence assessment proforma is being piloted on<br />
Ward 5.<br />
• Standardisation of Multisticks used for urine analysis.<br />
Future Planning<br />
The next benchmark(s) to be undertaken and the strategy<br />
for taking Essence of Care forward, will take place at the next<br />
project board meeting in January 2007. Prior to the next<br />
benchmark work commencing, any outstanding re-audits and<br />
subsequent action planning must be completed.<br />
Essence of Care benchmarking is an ongoing process of<br />
comparing, sharing and developing practice in order to achieve<br />
and sustain best practice.<br />
Many areas within the Trust have displayed much<br />
enthusiasm and have made great changes in search of best<br />
practice, making a considerable difference in their working<br />
areas.<br />
Essence of Care as it implies describes the fundamentals and<br />
the ‘basics’ of what we do everyday within the hospital setting<br />
and despite the many pressures facing us each day, all staff<br />
need to take ownership of the Essence of Care process and<br />
keep this enthusiasm and momentum going in order to deliver<br />
care to the highest possible standard.<br />
If you need any assistance with any stages of the Essence of<br />
Care process, please do not hesitate to contact me.<br />
Cherry Townsend,<br />
Clinical Educator - Essence of Care,<br />
Nurse Education Department x3371<br />
www.jpaget.nhs.uk
Hospital at Night<br />
The Hospital at Night project is a national initiative launched to<br />
reorganise care for patients at night and reduce junior doctors’<br />
hours. The project was piloted at three sites across the country,<br />
with all sites noting that the frequency of tasks and calls<br />
reduced after midnight. They concluded that a more<br />
concentrated team, combining medical and nursing staff could<br />
deliver a quality service during the night.<br />
1600<br />
1400<br />
1200<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
17.00<br />
19.00<br />
21.00<br />
23.00<br />
01.00<br />
03.00<br />
05.00<br />
07.00<br />
Activity<br />
levels<br />
fall after<br />
midnight<br />
but are<br />
high in<br />
the<br />
evening<br />
<strong>James</strong> <strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong><br />
www.jpaget.nhs.uk<br />
NHS Foundation Trust<br />
PLEASE<br />
DO NOT ENTER<br />
THERAPY IN<br />
PROGRESS<br />
They also noted that routine day work extended into the<br />
evening and it is expected that individuals on twilight shifts will<br />
proactively address clinical needs on the wards by ensuring that<br />
routine tasks and clerking are completed earlier.<br />
The Hospital at Night Team at the <strong>James</strong> <strong>Paget</strong> <strong>University</strong><br />
Hospital will include:<br />
• Night Site Coordinator<br />
• Clinical Support Practitioner (CSP)<br />
• Clinical Support Assistant (CSA)<br />
• Specialist registrar in Medicine<br />
• Specialist registrar in Surgery<br />
• 3 Foundation Year 2 (FY2) / Senior House Officers made up<br />
from medicine, surgery and other surgical specialties rotating<br />
into the night shift.<br />
Anaesthesia and Paediatrics will continue to have their own<br />
dedicated teams and the arrest call arrangements will remain<br />
unchanged.<br />
The Trust piloted the Hospital at Night Team approach in<br />
January 2007. This included different rotas for medical staff and<br />
all bleeps being directed through the Night Site Coordinator for<br />
allocation to CSAs, CSPs and Junior Medical Staff. The aims of<br />
the pilot were to:<br />
• Test systems of communication and co-ordinate care between<br />
medical and nursing staff in the team<br />
• Test team dynamics and skill mix, to improve prioritisation of<br />
work and to match it to patient needs.<br />
• Test multi-disciplinary handovers<br />
The pilot highlighted the communication difficulties faced but<br />
demonstrated a huge willingness by staff of all professional<br />
backgrounds and levels of the organisation to work together to<br />
ensure quality patient care.<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 13
View Point<br />
Introducing the new ‘Viewpoint’ section in <strong>Making</strong> <strong>Waves</strong>.This gives anyone the chance<br />
to have their views published for everyone to read.<br />
Transport IVF - The <strong>James</strong> <strong>Paget</strong><br />
<strong>University</strong> Hospital - Bourn Hall Programme<br />
Consultant Obstetrician and Gynaecologist,<br />
Peter Greenwood, is the lead for subfertility<br />
services. <strong>Making</strong> <strong>Waves</strong> caught up with Mr<br />
Greenwood, to find how the programme is<br />
going at the <strong>Paget</strong>.<br />
‘It’s now 13 years since the first cycle of transport IVF was carried<br />
out at the <strong>James</strong> <strong>Paget</strong> Hospital in November 1993. The outcome for<br />
that couple was very disappointing as the eggs transferred to Bourn<br />
Hall Clinic failed to fertilise. Luckily the programme has gone from<br />
strength to strength since that first case.’<br />
‘The essence of Transport IVF for Suffolk couples is that the<br />
ovarian stimulation, cycle monitoring and egg retrieval are all<br />
carried out at their local hospital whilst the ‘high-tech’ embryology<br />
and embryo transfer are performed at an Assisted Conception Unit<br />
with highly skilled embryologists. The female partner undergoes<br />
hormone down-regulation for two weeks before having drug<br />
stimulation to the ovaries for 11-15 days before egg retrieval. The<br />
egg retrieval is carried out under general anaesthesia in an<br />
operating theatre if it is on a Monday - or under sedation and<br />
analgesia in the Waveney Suite if, due to delayed response, the eggs<br />
are not ready until later in the week. Over the past two years more<br />
than 50% of the procedures have been carried out under sedation<br />
rather than general anaesthesia.’<br />
‘The most successful year for the programme so far was 20<strong>06</strong>. 55<br />
cycles of treatment were started during the 12 months. More than<br />
50% of the couples are referred for treatment at the <strong>James</strong> <strong>Paget</strong><br />
Hospital by the Consultant Gynaecologists at the West Suffolk<br />
Hospital as they do not have the necessary expertise to offer the<br />
service themselves. The Suffolk PCTs currently fully fund one cycle of<br />
Transport IVF for a couple provided they fulfil various criteria. These<br />
include – no previous child in the relationship – a maximum age of<br />
39 years old for the female – a maximum and minimum Body Mass<br />
Index for the female and neither partner can have undergone<br />
sterilisation in the past. The criteria are based around making the<br />
best and fairest use of limited resources whilst aiming for a good<br />
success rate for couples going through treatment. The criteria for<br />
Norfolk based couples are the same but they have to be referred for<br />
treatment at St. Bartholomew’s Hospital in London because of a<br />
longstanding Norfolk Subfertility Contract. If funding was more<br />
limited or the criteria less demanding then the outcome would be<br />
longer and longer waiting lists with couples’ chances of successful<br />
treatment going down as the woman became older. The success rate<br />
of IVF for the ‘average’ 25 year old female is about 30% whilst the<br />
success rate for a woman over the age of 40 is 5-10%.’<br />
‘The outcome of our treatment cycles in 2005 is fully known<br />
now. 37 couples started a treatment cycle. In 34 cases the treatment<br />
cycle led to an egg retrieval and of those 32 resulted in the creation<br />
of embryos. 30 then had a fresh embryo transfer (in the other 2<br />
cases all the embryos were frozen for future use on clinical<br />
grounds). The 30 embryo replacements resulted in 13 positive<br />
pregnancy tests but 2 of these did not lead onto a pregnancy that<br />
could be seen on ultrasound scan at 6-7 weeks (defined by the<br />
presence of a fetal pulse – a clinical pregnancy). One further<br />
pregnancy sadly ended in miscarriage and the other 10 proceeded<br />
to a successful outcome. 4 couples had liveborn twins and six<br />
couples single babies. The take home baby rate per embryo transfer<br />
was therefore 33% across all ages which is significantly better than<br />
the national average.’<br />
‘The results from 20<strong>06</strong> look as though they will be even better.<br />
55 cycles have been completed. These cycles have resulted in 22<br />
pregnancies where a fetal heart has been seen on ultrasound scan<br />
and 21 of these are progressing satisfactorily – the ones from early<br />
20<strong>06</strong> have already delivered. There have been 8 twin pregnancies<br />
and 14 singleton pregnancies (sadly one singleton pregnancy has<br />
miscarried). The success rate per embryo transfer for 20<strong>06</strong> has been<br />
55% and fingers are tightly crossed in the Waveney Suite that these<br />
pregnancies will all lead to ‘take home babies’ for the lucky couples<br />
that are pregnant at the moment through the IVF programme.’<br />
‘There is always uncertainty in the NHS with regard to funding.<br />
There has been some slight improvement in funding for subfertile<br />
couples since the NICE report on Infertility came out 3 years ago.<br />
However, it was the Government’s stated hope that appropriate<br />
couples would have 3 cycles of IVF funded by the NHS and to date<br />
the vast majority of PCTs are only funding one cycle of treatment.<br />
The talk of cuts to NHS services in many parts of the country may<br />
lead to additional pressures on subfertility services. In a nation<br />
where fertility is falling and many couples find it very difficult to<br />
adopt a young child to achieve a family unit my personal opinion is<br />
that it’s very sad that in the face of steadily improving IVF success<br />
rates the funding is still not forthcoming to provide an adequate<br />
NHS based subfertility Service.’<br />
■ Katie and Lucy Shingfield, IVF twins.<br />
The viewpoint column is written from a personal perspective and may not necessarily reflect the views of the Trust.<br />
If you have a view to share, and you would like it published in <strong>Making</strong> <strong>Waves</strong>, send your letter or email to the Communications and<br />
Foundation office. We’ll give £10 in Argos vouchers (donated) for every ’View Point’ printed. So get writing and let everyone know<br />
what you think! Rebecca Driver, Head of Communications and Foundation Secretary x2269<br />
14 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Profile<br />
Introducing the Head & Neck/<br />
Tracheostomy Support Service<br />
As we are such a specialist service Denise and I thought it would be<br />
useful to explain a little of what we do and the service we provide; so<br />
in this issue of <strong>Making</strong> <strong>Waves</strong> we thought it would be a good idea to<br />
present a profile of the service and in a later issue both Denise and I<br />
will present the role and benefits of the Oncology Clinical Nurse<br />
Specialist and the Tracheostomy Clinical Nurse Practitioner.<br />
The Head & Neck/Tracheostomy Support Service was set up in 1994<br />
to provide a service for patients who had undergone tracheostomy<br />
and laryngectomy. These ‘neck-breathing’ patients’ present a huge<br />
challenge for staff, both within the Trust and the wider community.<br />
The provision of information and support for the patient, their family,<br />
and the clinical team, is vital to address preoperative and<br />
postoperative psychological and physiological issues; for instance, in<br />
the case of laryngectomy – the removal of the larynx (voice-box) - it<br />
not only leaves the individual and family coping with a cancer<br />
diagnosis but also with a major disability. In 1996 it was deemed<br />
necessary to include all patients diagnosed with a head & neck cancer;<br />
therefore the service was expanded and provision made for these<br />
patients.<br />
The service has won two Charter Mark awards - one in 1997 for<br />
the tracheostomy service and again in 2000 for the combined service.<br />
In 2001, to address a significant increase in workload of each speciality,<br />
the service was split into two - Head & Neck Oncology, to offer support<br />
and improve the pathway of communication for all patients diagnosed<br />
with a cancer of the head or neck, and Tracheostomy Support; to<br />
address the needs of neck-breathing patients. Although both services<br />
still remain under the same support service umbrella Denise Smith, the<br />
Head & Neck Oncology Clinical Nurse Specialist, predominately<br />
manages the oncology side of the service, whilst Netta Delfino, Clinical<br />
Nurse Practitioner, oversees the tracheostomy/laryngectomy side.<br />
As the demands on the service have increased so has the need for<br />
additional education and clinical support to areas within the Trust and<br />
local communities. The development of an educational and training<br />
program has ensured evidence based practice has been implemented<br />
that has enhanced clinical practice throughout the Trust and therefore<br />
a trend towards safer practice for this special group of patients.<br />
Training is a huge commitment of this specialist service and<br />
provides not only general training but also tailored training for<br />
specialised clinical areas, for example, A&E, ICU, and Theatres and<br />
Recovery. Training is also provided on a regular basis as part of the<br />
Clinical Skills Program and the commitment for regular training has<br />
expanded to the UEA Medical Students. Last year, on the back of the<br />
report by the National Patient Safety Agency (NPSA) entitled<br />
‘Improving emergency care for patients who breathe through their<br />
neck’ we achieved in getting tracheostomy care training as part of the<br />
professional staff stat-day. The NPSA report highlighted a lack of<br />
understanding of the specific needs of neck-breathing patients<br />
amongst some ambulance and hospital staff and called for improved<br />
training of all NHS staff involved in the emergency treatment of<br />
patients with special breathing needs. Although this training was<br />
recommended for emergency staff we felt by presenting this specific<br />
training on the stat day we would reach a wider audience; after all,<br />
these patients may get into difficulties whilst living their lives in the<br />
wider community and an awareness that some people breathe<br />
through their necks may be vital in giving appropriate emergency care.<br />
We believe we are one of the first Trusts to instigate this – another<br />
achievement for the JPUH.<br />
Denise Smith, Head & Neck Oncology Clinical Nurse Specialist<br />
Netta Delfino, Clinical Nurse Practitioner<br />
Jo Randell, New Trust Consultant Physician<br />
I joined the trust on 15 January 2007 as Consultant Physician in Diabetes and Endocrinology.<br />
I qualified at the London Hospital Medical College in 1996. I was a Senior House Officer in Southampton and<br />
unsure as to what branch of medicine I wished to specialise in, when I found myself acting up as a registrar in<br />
Diabetes and Endocrinology after the intended post holder pulled out with a week’s notice and I enjoyed it<br />
immensely.<br />
I spent some time in Bath as a Specialist Registrar before taking up a post in the Eastern Deanery. I am no<br />
stranger to the area having lived in Norfolk for nearly 5 years and previously worked as a Specialist Registrar at the<br />
Norfolk and Norwich <strong>University</strong> Hospital, Addenbrooke’s Hospital and Southend Hospital.<br />
As it has become more outpatient and community focussed, the specialty is less popular with junior doctors in recent years and I think<br />
that many of them perceive diabetes in particular as being rather dull when in fact I find it incredibly diverse and complex. Our patients can<br />
be challenging (in many ways) and communication and teamwork are very important (talking is something I quite enjoy).<br />
As well as sharing Ward 14 with Dr Huston and general Diabetes and Endocrinology clinics, I will be involved in the Joint Antenatal<br />
Diabetes Clinic with Dr Rashid and Mr Pozyczka and the Joint Adolescent Diabetes clinic with Dr Garg.<br />
I am married. I enjoy travelling – my most recent trip was to Madagascar taking in a variety of national parks (complete with cute<br />
lemurs) and coral reef fringed sun drenched beaches. We keep a tropical marine aquarium at home complete with several colourful fish,<br />
shrimps, crabs etc. I also play the piano (badly) and like “arty” things – both creating and buying them.<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 15
Governors Council Progress<br />
Our 33 Governors have now been in post for<br />
almost 11 months and the Governors Council<br />
and the four Committees have all met. Here’s<br />
an update on what they’re working on at the<br />
moment.<br />
Governors Council:<br />
The Council has approved the selection process and<br />
remuneration levels for Non Executive Directors and also<br />
approved the appointment of the Chief Executive at an<br />
extraordinary meeting held on 17th January.<br />
Nomination and Remuneration Committee:<br />
This Committee is leading the selection process to appoint to<br />
the vacant Non Executive Director post. There has been lots<br />
of interest and an appointment will be ratified at the next<br />
meeting of the Governors Council on 9th March 2007. The<br />
Committee have also reviewed the remuneration levels of the<br />
Chairman and Non Executive Directors.<br />
Strategic Planning Committee:<br />
Presentations were given by the Director of Finance &<br />
Performance on the history of the Trust, where it stands now<br />
and its future and the Director of Nursing & Patient Services<br />
on the ward upgrade programme. The Committee has<br />
considered the current Trust Vision Statement and this will be<br />
revised for 2007/08.<br />
Membership Committee:<br />
Two meetings of this Committee have been held to consider<br />
how to use the Foundation Trust’s membership of 12,000+ to<br />
add value to the Trust. The membership strategy for this year<br />
will be considered by the Board of Directors and the<br />
Governors Council in early March. Two governors, Dennis<br />
Cave and Rachel Hulse, have done some work with the local<br />
colleges to engage young people which is a really positive<br />
step forward. Governors also hope to be involved in the 25th<br />
anniversary celebrations to highlight the benefits of being a<br />
member, using the fete planned for 21st July as the main<br />
membership event for the year.<br />
Audit Performance Committee<br />
The Committee considered the audit process, annual audit<br />
letter and agreed the Standing Orders for the Governors<br />
Council. These will be presented to the next meeting of the<br />
Governors Council on 9th March for approval.<br />
There is a Foundation Trust area on the new intranet where<br />
you can access Governors Council meeting papers and see<br />
details of your staff governors.<br />
If you have any queries, please contact<br />
Ann Filby on ext. 2162, ann.filby@jpaget.nhs.uk<br />
To contact your staff governors,<br />
email staffgovernors@jpaget.nhs.uk<br />
Local Author Publishes Book on the<br />
History of the <strong>James</strong> <strong>Paget</strong> Hospital<br />
On Tuesday 16th January, local author and exhospital<br />
employee Brian Callan presented his new<br />
book on the history of the local hospital to the Trust.<br />
Brian has spent six long years writing the book called<br />
‘Treatment for Two Guineas’ which explains how the local<br />
hospitals came to Great Yarmouth. The academic work<br />
involved in the research of the book was fully supported by<br />
a team of Professors at Nottingham <strong>University</strong>. In<br />
recognition of his studies, Brian was made Master of<br />
Philosophy in the School of History in July last year, a<br />
moment he was particularly proud of.<br />
Brian says: ‘I am delighted to make a presentation of<br />
my book to the hospital. I have received tremendous<br />
support from staff there in helping me to write this, and<br />
it’s good news for the local people of Yarmouth and<br />
Waveney to know that there is now a clear record of how<br />
the <strong>James</strong> <strong>Paget</strong> Hospital came to be in Yarmouth.’<br />
The first Yarmouth General Hospital was open by 1840.<br />
As it expanded, it was decided to ask one of the country’s<br />
leading medical practitioners to open it. Sir <strong>James</strong> <strong>Paget</strong><br />
was born in Yarmouth and educated at Reverend Bowles<br />
private school in Queen’s Street. He was appointed<br />
Surgeon to Queen Victoria. The hospital moved to its<br />
current site in late 1981, and was officially opened seven<br />
months later on 21st July 1982 by Professor Dorothy<br />
Crowfoot Hodgkin.<br />
Pictured: Dr Grabau, Wendy Slaney with Brian Callan,<br />
Madeleine Borg and Chris Thompson.<br />
16 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Thank You!<br />
Lions support the Renal Unit<br />
The Lions supported the Renal Unit with another generous<br />
donation in November. Pictured below are: Matron Rosemary<br />
Smalley, Tony Talbot, Sister Belinda Burrows, Margaret Talbot,<br />
Lion Margaret Woodruff and patient Irene Codman from Caister.<br />
PSL Energy Services give £250 to the<br />
Children's Ward<br />
On Thursday 14th December 20<strong>06</strong>, the Children's Ward was<br />
presented with a cheque for £250 to be spent on toys for the<br />
ward which the children have asked for.<br />
The cheque was presented by Mr Frank Mortimer<br />
(pictured) on behalf of PSL Energy Services, Great Yarmouth.<br />
The decision to donate the monies was a management<br />
decision under the direction of Mr Nick Birch, Operations<br />
Manager.<br />
The money was raised by staff not sending Christmas<br />
cards.<br />
Justine Goodwin of Ward 10 said: ‘We are really grateful<br />
for this donation and it really brightened up Christmas for<br />
our patients.’<br />
Lions fund a special chair for the Stroke Unit<br />
In February, the Great Yarmouth Lions kindly donated £2,200<br />
to the Stroke Unit to purchase a special seat. Evie Cooper,<br />
Stroke Coordinator, said: ‘The Kirton Delta Chair is very<br />
supportive and includes a tilt-in-space facility so patients can<br />
lie back to rest without necessarily returning to bed. The<br />
support allows us to sit patients out of bed earlier than<br />
would otherwise be possible, providing them with all the<br />
benefits of earlier mobilisation and a sitting position. It’s<br />
much safer and easier for patients to eat, they have better<br />
respiratory function, and can control their posture. The chair<br />
has wheels so it’s mobile around the ward and even around<br />
the hospital. The adjustable nature of the leg and back rest<br />
means it can be used for all patients.’<br />
Evie finished by saying: ‘This was such a generous<br />
donation and we are very grateful to the Lions for<br />
supporting us.’<br />
Head shave for Neonatal Unit<br />
Regulars of the Mariners Tavern on Howard Street South in<br />
Yarmouth took part in a sponsored head shave evening.<br />
The event was a great success, with over £460 being raised<br />
for the Neonatal Unit.<br />
New cytotoxic isolator for the Pharmacy<br />
Support Services Unit<br />
A big thank<br />
you to the<br />
Big C local<br />
charity for<br />
the donation<br />
of a new<br />
cytotoxic<br />
isolator for<br />
the Pharmacy<br />
Support<br />
Services Unit<br />
at the <strong>James</strong><br />
<strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong> NHS Foundation Trust. We are<br />
delighted with this donation as this isolator will benefit all<br />
patients receiving intravenous chemotherapy. It will help to<br />
reduce waiting times and will enable the service to continue<br />
in the case of failure of our old isolator.<br />
Once again many thanks.<br />
The Great Antique Hunt<br />
Peter Maleczek, the Trust’s Back Care Advisor, is an avid collector of nursing badges and<br />
memorabilia. He is currently looking for a particular badge (see photo) and wondered if anyone<br />
working in the Trust would be able to help him, either because they have one or know where one<br />
can be found. Peter can be contacted via email (peter.maleczk@jpaget.nhs.uk) or on ext. 2159.<br />
And, of course, he is open to all bargaining and negotiation!<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 17
Behind the scenes<br />
The Medical Photography and<br />
Illustration Department<br />
We all know where the Medical Photography & Illustration<br />
Department is situated but how much do we actually know<br />
about the services that the Department provides? During an<br />
interview with Madeleine Borg, Medical Illustration/DRSS<br />
Manager, it became very clear that there is much more to the<br />
Medical Photography and Illustration Department than just<br />
taking photographs. Madeleine says: People always ask me what<br />
I take photographs of, and my answer is always ‘anything and<br />
everything in or outside of the human body’ ‘.<br />
The services of the Medical Photography cover five main<br />
areas:<br />
Patient photography<br />
This is the largest part of the department’s workload and<br />
includes the taking and producing of clinical photographs or<br />
videos that provide visual documentation of internal and<br />
external disease. These are often ‘before and after’ comparisons<br />
such as breast reconstruction, skin diseases and orthodontics.<br />
Photographs are not just taken in the Department;<br />
photographers often attend the wards and theatres to do their<br />
work.<br />
Support to training and teaching<br />
For many years Medical Photography produced the bulk of<br />
teaching slides using a number or chemical processes and a<br />
great deal of time was spent in the darkroom as nearly all films<br />
were processed in-house. Since the introduction of the computer<br />
and software such as Powerpoint, many more medical staff do<br />
their own presentations. However, there is still a role for the<br />
medical illustrator with experience in graphic design to produce<br />
professional posters and assisting medical staff not so<br />
comfortable with the new technology - especially when editing<br />
video and adding clips to presentations is required.<br />
Research<br />
The Department is occasionally involved in taking photographs<br />
that can become a main factor of research, the most recent<br />
being the ‘Age Related Macular Degeneration’ project organised<br />
by a Research Ophthalmologist at Cambridge.<br />
Provision of photographs for litigation<br />
The Department also receives requests from external solicitors<br />
and patients to take photographs for litigation purposes outside<br />
the Trust which acts as income generation.<br />
Morbid photography<br />
This is perhaps the most sensitive of all areas of medical<br />
photography work. It involves the photographers working<br />
closely with the mortuary staff in the taking of a range of<br />
clinical photographs at post mortem and especially in relation to<br />
families who have lost a baby who may like to have a<br />
photograph to help with the process of mourning the loss of<br />
18 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
their child. On a lighter note the Department also offers staff a<br />
passport photograph service and bus pass photographs for those<br />
that need them!<br />
So what makes a good Medical Photographer?<br />
As Madeleine explains: ‘It takes someone with a high level of<br />
sensitivity, infinite patience, compassion and a kindness without<br />
being condescending’.<br />
So when did Medical Photography start and evolve?<br />
The formal introduction of medical photography started in 1948<br />
in the larger university hospitals and was often undertaken by<br />
staff from other professions who had an interest in the ‘new’<br />
science of photography.<br />
The service for the Great Yarmouth & Waveney area started<br />
in 1975 where accommodation consisted of a prefabricated<br />
building at Northgate Hospital that Madeleine shared with a<br />
Librarian and a Post Graduate Secretary. Madeleine recalls: ‘I<br />
used the store cupboard for taking photographs and the kitchen<br />
to develop films. I also thought I was busy if I saw 7 patients a<br />
week! How times have changed!’<br />
Madeleine added: ‘The profession has seen many changes<br />
especially in technology i.e. computers and digitisation. This has<br />
in turn affected the speed at which images can be produced.<br />
Doctors can now access their patient’s images via computer<br />
moments after they have been photographed’.<br />
‘The only qualifications originally available were the City &<br />
Guilds Scientific Course, the Institute of Illustration Diploma and<br />
the British Institute of Professional Photographers (BIPP) medical<br />
exam. There are now 2 degree courses i.e. BSc in Medical<br />
Photography (Glasgow) and MSc in Medical Photography<br />
(Cardiff) but there are very few opportunities for trainee posts<br />
across the country.’<br />
Diabetic Retinal Screening Service<br />
The other major service provided by the Department is the<br />
Diabetic Retinal Screening Service which began in earnest in<br />
1987 when the first specialised camera was purchased from<br />
charitable donations. This service provided an annual retinal<br />
(eye) screen for diabetic patients in the Great Yarmouth &<br />
Waveney area.<br />
Since the publication of the National Service Framework for<br />
Diabetes (1999) the service has now necessitated working<br />
collaboratively as a network with other Trusts and PCTs. A<br />
contract was secured on behalf of the Trust by Madeleine in<br />
20<strong>06</strong> and this now provides an annual retinal screening service<br />
to those patients living in the East Suffolk as well as the Great<br />
Yarmouth & Waveney area (a total of 22,000 patients).<br />
Madeleine explains: ‘Whereas previously patients did not<br />
have a choice of where to be screened we can now offer several<br />
www.jpaget.nhs.uk
different community venues in places such as Beccles Hospital,<br />
Aldeburgh, Lowestoft, and for those patients in the East Suffolk<br />
catchment area a variety of GP Practices, Hadleigh, East Bergholt,<br />
Woodbridge, Wickham Market, Eye as well as Ipswich Hospital.’<br />
Madeleine adds: ‘To accommodate all these clinics we have a<br />
travelling band of retinal screeners!’ The service also has a call<br />
centre which provides more choice when booking appointments.<br />
So what is Retinal Screening?<br />
Retinal Screening requires the acquisition of a high quality<br />
photograph of the retina (the visual layer at the back of the eye)<br />
taken on a special fundus camera to acquire a high quality<br />
image. The patients are required to have some eye drops<br />
administered to enlarge the pupil prior to photography thus<br />
allowing a maximum amount of light to fall onto the retina and<br />
to be reflected back onto the lens of a camera. Once the<br />
photographs are taken the images are uploaded onto a central<br />
server based at JPUH and the images go through a process of<br />
grading i.e. primary, secondary and final grading. Primary and<br />
secondary grading can be carried out by a trained technician but<br />
final grading requires the expertise of the Ophthalmologist. The<br />
photographs are graded and reports are sent out to GPs with a<br />
copy to the patient. Those requiring treatment for diabetic<br />
retinopathy or maculopathy or any other identified eye disease,<br />
such as cataracts or glaucoma area, are referred to the Eye Clinic.<br />
Meet the Medical Photography team<br />
Madeleine Borg<br />
Medical<br />
Photography<br />
and DRSS<br />
Programme<br />
Manager<br />
National Inpatient<br />
Survey Results, 20<strong>06</strong><br />
We’ve just had the results of the national inpatient survey for<br />
20<strong>06</strong>. This national survey gives us some really useful findings<br />
to work with, and also compares our performance against<br />
similar hospitals across the country. 521 inpatients replied, a<br />
63% response rate.<br />
There’s too much data to note everything, but some particular<br />
highlights were:<br />
• Our food and cleaning scores are well above the national<br />
average, and have improved on our performance in 2005.<br />
• More than 3 out of 4 patients felt they were admitted to<br />
hospital as soon as they thought necessary.<br />
• Confidence and trust in doctors and nursing staff was high.<br />
• Most patients felt they were treated with dignity and<br />
respect when they were in hospital. This was up from 72%<br />
in 2005 to 80% now.<br />
• Most patients rated the care they received as excellent or<br />
very good.<br />
• We have more emergency admissions than most acute<br />
hospitals both in 2005 and 20<strong>06</strong>.<br />
There are some areas for action, including patient information,<br />
and discharge procedures. Nick Coveney, Director of Nursing<br />
and Patient Care, and Liz Cooke, Acting Director of Human<br />
Resources, will be sharing the findings with staff over the<br />
coming months.<br />
Derek Rogers<br />
DRSS Grader,<br />
Senior Medical<br />
Photographer<br />
Douglas<br />
Middleton<br />
Medical<br />
Photographer<br />
Annette Tovell<br />
Medical<br />
Photographer<br />
Rachael Bolton<br />
Medical<br />
Photographer,<br />
Diabetic Retinal<br />
Screener<br />
Lorna Aston<br />
Personal<br />
Assistant<br />
Christine<br />
Merrikin<br />
Administration<br />
Assistant /<br />
Receptionist<br />
So the next time you walk past<br />
the department or see any of the<br />
staff, remember there is more to<br />
them than meets the eye!!<br />
Diabetic Retinal<br />
Screening Service Staff<br />
Wendy Norman<br />
Darrell Atkinson<br />
Janet Ravenscroft<br />
Michelle Alberto<br />
Barry Norton<br />
Glynis Castleton<br />
Lindsay Ditcham<br />
Beryl Nettleship<br />
Linda Hirst<br />
Alison Whittle<br />
Lesley Branch<br />
Maureen Newark and<br />
Doris Middleton<br />
(Volunteers)<br />
Money raised for<br />
Breast Care Services<br />
On 1st October 20<strong>06</strong> a company of auctioneers and valuation<br />
experts held an event at the Burrage Centre to raise funds for<br />
the Breast Care Unit appeal. This followed the diagnosis and<br />
treatment of a relative of a company member who was<br />
impressed by the service she received and wanted to show her<br />
appreciation.<br />
Sue Jones, Superintendent Radiographer in Breast Imaging<br />
said: ‘Lockdales of Ipswich organised the event where they<br />
offered a valuation of collectable items for a nominal fee and<br />
also held an auction. Money raised on the day, plus a donation<br />
from the company, took the sum raised to £200.’<br />
Sue continued: ‘The breast care team would like to express<br />
their appreciation to Lockdales as there are exciting times<br />
ahead, especially in Breast Imaging with the imminent move to<br />
replace the ageing mammography machines with full field<br />
digital equipment.<br />
Donated monies are always welcomed as they allow the<br />
team to have additional training and to provide the extra<br />
touches which go a long way to improve the patient<br />
experience.’<br />
www.jpaget.nhs.uk<br />
March 2007 <strong>Making</strong> <strong>Waves</strong> 19
View from the top:<br />
Meet the SHA’s<br />
Chief Executive<br />
As a Foundation Trust, we are accountable to<br />
Monitor, but we still link closely with the East<br />
of England Strategic Health Authority, based<br />
in Cambridge. Have you ever wondered what<br />
the SHA’s Chief Executive, Neil McKay, thinks<br />
about the local NHS and his vision for the<br />
future? Here, <strong>Making</strong> <strong>Waves</strong> brings you his<br />
views, on the NHS in the east now, and what<br />
lies ahead.<br />
No-one working in the NHS across the east of England<br />
needs reminding that the health service is going through a<br />
period of enormous change, but I would like to reassure<br />
everyone that we now have a clearer vision of strong, viable<br />
health services for years ahead.<br />
We have all heard how higher levels of investment in<br />
recent years has led to improvements in a number of areas;<br />
how waiting times are down, cancer treatment times are<br />
down and so on, but there has also been significant upheaval<br />
for many staff across the region.<br />
Reorganisation of Primary Care Trusts and Strategic Health<br />
Authorities following Commissioning a patient-led NHS, a<br />
poor financial situation in many areas and a range of changes<br />
to the way we work – coupled with myriad changes to the<br />
day-to-day lives of almost everyone – have all had an impact.<br />
This period of change has not been easy, and I am not<br />
shying away from the fact that we still face considerable<br />
pressures, not least in terms of getting the health economy’s<br />
finances back on track. However, I sincerely believe that we<br />
are in the process of creating a modern, sustainable health<br />
service that we can all be proud of.<br />
The most important people in delivering change within<br />
the local NHS are those with the best knowledge of how it<br />
works and where it can be improved. One thing that has<br />
struck me since taking up the post of chief executive is the<br />
vast knowledge of staff across the eastern region. This<br />
knowledge has already formed the basis for change in a<br />
number of areas, and it will continue to inform the change<br />
agenda.<br />
The SHA is looking at new ways to involve people at all<br />
levels, in all NHS organisations across the region, in<br />
determining how we create a health service that is fit for<br />
purpose and that people can feel proud to work for.<br />
Also, where decisions have already been made about the<br />
way services should look we need the full cooperation of<br />
staff to ensure both clinical quality and to achieve truly<br />
excellent services.<br />
Uncertainty breeds concern, which is why I would like to<br />
see changes happen as speedily as possible where they are<br />
needed. In some areas, this is progressing well; we are seeing<br />
well thought-through plans being implemented and some<br />
real improvements to frontline services.<br />
I have also been impressed by the strength of the<br />
relationship between clinicians and managers; there are some<br />
really good examples of doctors working with managers to<br />
improve services, of Trusts working closely with GPs to enable<br />
even greater success and of staff at all levels making a<br />
commitment to providing better services in their area of<br />
expertise.<br />
I know this has often been difficult in a time of change,<br />
but I believe that we are now on a clear path. Development<br />
of hospital services now has a clear direction following the<br />
publication of Looking to the future – development of<br />
hospital services in the east of England. This review will<br />
provide recommendations for high-quality services, with the<br />
best possible clinical outcomes, services that will provide a<br />
good working environment for all NHS staff in the region for<br />
decades to come.<br />
Look out for more details on the<br />
progress of the acute services review<br />
in future editions of <strong>Making</strong> <strong>Waves</strong>.<br />
Missed any back issues of <strong>Making</strong> <strong>Waves</strong>?<br />
This edition and previous editions can be found on the <strong>James</strong> <strong>Paget</strong><br />
<strong>University</strong> <strong>Hospitals</strong> intranet in pdf or paper copies are available from the<br />
Communications Dept.<br />
20 March 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk