Adverse Drug Reactions in Clinical Practice - Journal of ...
Adverse Drug Reactions in Clinical Practice - Journal of ...
Adverse Drug Reactions in Clinical Practice - Journal of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
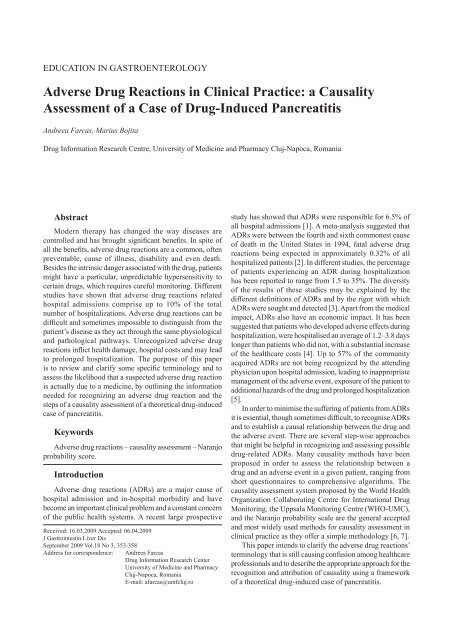
education <strong>in</strong> gastroenterology<br />
<strong>Adverse</strong> <strong>Drug</strong> <strong>Reactions</strong> <strong>in</strong> Cl<strong>in</strong>ical <strong>Practice</strong>: a Causality<br />
Assessment <strong>of</strong> a Case <strong>of</strong> <strong>Drug</strong>-Induced Pancreatitis<br />
Andreea Farcas, Marius Bojita<br />
<strong>Drug</strong> Information Research Centre, University <strong>of</strong> Medic<strong>in</strong>e and Pharmacy Cluj-Napoca, Romania<br />
Abstract<br />
Modern therapy has changed the way diseases are<br />
controlled and has brought significant benefits. In spite <strong>of</strong><br />
all the benefits, adverse drug reactions are a common, <strong>of</strong>ten<br />
preventable, cause <strong>of</strong> illness, disability and even death.<br />
Besides the <strong>in</strong>tr<strong>in</strong>sic danger associated with the drug, patients<br />
might have a particular, unpredictable hypersensitivity to<br />
certa<strong>in</strong> drugs, which requires careful monitor<strong>in</strong>g. Different<br />
studies have shown that adverse drug reactions related<br />
hospital admissions comprise up to 10% <strong>of</strong> the total<br />
number <strong>of</strong> hospitalizations. <strong>Adverse</strong> drug reactions can be<br />
difficult and sometimes impossible to dist<strong>in</strong>guish from the<br />
patient’s disease as they act through the same physiological<br />
and pathological pathways. Unrecognized adverse drug<br />
reactions <strong>in</strong>flict health damage, hospital costs and may lead<br />
to prolonged hospitalization. The purpose <strong>of</strong> this paper<br />
is to review and clarify some specific term<strong>in</strong>ology and to<br />
assess the likelihood that a suspected adverse drug reaction<br />
is actually due to a medic<strong>in</strong>e, by outl<strong>in</strong><strong>in</strong>g the <strong>in</strong>formation<br />
needed for recogniz<strong>in</strong>g an adverse drug reaction and the<br />
steps <strong>of</strong> a causality assessment <strong>of</strong> a theoretical drug-<strong>in</strong>duced<br />
case <strong>of</strong> pancreatitis.<br />
Keywords<br />
<strong>Adverse</strong> drug reactions – causality assessment – Naranjo<br />
probability score.<br />
Introduction<br />
<strong>Adverse</strong> drug reactions (ADRs) are a major cause <strong>of</strong><br />
hospital admission and <strong>in</strong>-hospital morbidity and have<br />
become an important cl<strong>in</strong>ical problem and a constant concern<br />
<strong>of</strong> the public health systems. A recent large prospective<br />
Received: 16.03.2009 Accepted: 06.04.2009<br />
J Gastro<strong>in</strong>test<strong>in</strong> Liver Dis<br />
September 2009 Vol.18 No 3, 353-358<br />
Address for correspondence: Andreea Farcas<br />
<strong>Drug</strong> Information Research Center<br />
University <strong>of</strong> Medic<strong>in</strong>e and Pharmacy<br />
Cluj-Napoca, Romania<br />
E-mail: afarcas@umfcluj.ro<br />
study has showed that ADRs were responsible for 6.5% <strong>of</strong><br />
all hospital admissions [1]. A meta-analysis suggested that<br />
ADRs were between the fourth and sixth commonest cause<br />
<strong>of</strong> death <strong>in</strong> the United States <strong>in</strong> 1994, fatal adverse drug<br />
reactions be<strong>in</strong>g expected <strong>in</strong> approximately 0.32% <strong>of</strong> all<br />
hospitalized patients [2]. In different studies, the percentage<br />
<strong>of</strong> patients experienc<strong>in</strong>g an ADR dur<strong>in</strong>g hospitalization<br />
has been reported to range from 1.5 to 35%. The diversity<br />
<strong>of</strong> the results <strong>of</strong> these studies may be expla<strong>in</strong>ed by the<br />
different def<strong>in</strong>itions <strong>of</strong> ADRs and by the rigor with which<br />
ADRs were sought and detected [3]. Apart from the medical<br />
impact, ADRs also have an economic impact. It has been<br />
suggested that patients who developed adverse effects dur<strong>in</strong>g<br />
hospitalization, were hospitalised an average <strong>of</strong> 1.2–3.8 days<br />
longer than patients who did not, with a substantial <strong>in</strong>crease<br />
<strong>of</strong> the healthcare costs [4]. Up to 57% <strong>of</strong> the community<br />
acquired ADRs are not be<strong>in</strong>g recognized by the attend<strong>in</strong>g<br />
physician upon hospital admission, lead<strong>in</strong>g to <strong>in</strong>appropriate<br />
management <strong>of</strong> the adverse event, exposure <strong>of</strong> the patient to<br />
additional hazards <strong>of</strong> the drug and prolonged hospitalization<br />
[5].<br />
In order to m<strong>in</strong>imise the suffer<strong>in</strong>g <strong>of</strong> patients from ADRs<br />
it is essential, though sometimes difficult, to recognise ADRs<br />
and to establish a causal relationship between the drug and<br />
the adverse event. There are several step-wise approaches<br />
that might be helpful <strong>in</strong> recogniz<strong>in</strong>g and assess<strong>in</strong>g possible<br />
drug-related ADRs. Many causality methods have been<br />
proposed <strong>in</strong> order to assess the relationship between a<br />
drug and an adverse event <strong>in</strong> a given patient, rang<strong>in</strong>g from<br />
short questionnaires to comprehensive algorithms. The<br />
causality assessment system proposed by the World Health<br />
Organization Collaborat<strong>in</strong>g Centre for International <strong>Drug</strong><br />
Monitor<strong>in</strong>g, the Uppsala Monitor<strong>in</strong>g Centre (WHO-UMC),<br />
and the Naranjo probability scale are the general accepted<br />
and most widely used methods for causality assessment <strong>in</strong><br />
cl<strong>in</strong>ical practice as they <strong>of</strong>fer a simple methodology [6, 7].<br />
This paper <strong>in</strong>tends to clarify the adverse drug reactions’<br />
term<strong>in</strong>ology that is still caus<strong>in</strong>g confusion among healthcare<br />
pr<strong>of</strong>essionals and to describe the appropriate approach for the<br />
recognition and attribution <strong>of</strong> causality us<strong>in</strong>g a framework<br />
<strong>of</strong> a theoretical drug-<strong>in</strong>duced case <strong>of</strong> pancreatitis.
354<br />
Def<strong>in</strong>itions and classification <strong>of</strong> ADRs<br />
An adverse drug event or experience is def<strong>in</strong>ed as<br />
‘any untoward medical occurrence that may present<br />
dur<strong>in</strong>g treatment with a medic<strong>in</strong>e but which does not<br />
necessarily have a causal relationship with this treatment’.<br />
An adverse event is an adverse outcome that occurs while<br />
a patient is tak<strong>in</strong>g a drug, but is not or not necessarily<br />
attributable to it. This dist<strong>in</strong>ction is important, for<br />
example, <strong>in</strong> cl<strong>in</strong>ical trials <strong>in</strong> which not all events are<br />
drug-related. When this term is used to describe adverse<br />
outcomes, physicians should be aware that it is not always<br />
possible to impute causality [8, 9].<br />
An adverse drug reaction (ADR) is ‘a response to a<br />
medic<strong>in</strong>e which is noxious and un<strong>in</strong>tended, and which<br />
occurs at doses normally used <strong>in</strong> man for the prophylaxis,<br />
diagnosis, or therapy <strong>of</strong> disease or for the modification<br />
<strong>of</strong> a physiological function’. An ADR, contrary to an<br />
adverse event is characterised by the suspicion <strong>of</strong> a causal<br />
relationship between the drug and the occurrence. This<br />
def<strong>in</strong>ition underl<strong>in</strong>es the fact that the phenomenon is noxious<br />
(differentiat<strong>in</strong>g adverse drug reaction from side-effects<br />
which can also be beneficial) and that it <strong>in</strong>cludes doses<br />
prescribed cl<strong>in</strong>ically, exclud<strong>in</strong>g accidental or deliberate<br />
overdose [8, 10].<br />
An unexpected adverse reaction is ‘an adverse reaction,<br />
the nature or severity <strong>of</strong> which is not consistent with<br />
domestic labell<strong>in</strong>g or market authorisation or expected from<br />
characteristics <strong>of</strong> the drug’ [11].<br />
A side effect is ‘any un<strong>in</strong>tended effect <strong>of</strong> a pharmaceutical<br />
product occurr<strong>in</strong>g at doses normally used by a patient,<br />
which is related to the pharmacological properties <strong>of</strong> the<br />
drug’. This def<strong>in</strong>ition was formulated to <strong>in</strong>clude side effects<br />
that, although are not the ma<strong>in</strong> aim <strong>of</strong> the therapy, may be<br />
beneficial rather than harmful. For example a β-blocker agent<br />
used to treat hypertension may, by β-blockade, also relieve<br />
the patient’s ang<strong>in</strong>a [9, 11].<br />
A serious adverse event (experience) or reaction is any<br />
untoward medical occurrence that at any dose results <strong>in</strong><br />
death; is life-threaten<strong>in</strong>g; requires <strong>in</strong>patient hospitalization or<br />
prolongation <strong>of</strong> exist<strong>in</strong>g hospitalization; results <strong>in</strong> persistent<br />
or significant disability/<strong>in</strong>capacity, or is a congenital<br />
anomaly/birth defect.<br />
There is a difference between the terms “serious” and<br />
“severe”, which are not synonymous. The term “severe” is<br />
used to describe <strong>in</strong>tensity (severity) <strong>of</strong> an event (as <strong>in</strong> mild,<br />
moderate or severe). The event itself can be <strong>of</strong> relatively<br />
m<strong>in</strong>or medical significance, such as a severe headache. This<br />
is not the same as the “serious” which is based on the patient<br />
and event outcome [8].<br />
The most common classification <strong>of</strong> ADRs is the one<br />
that dist<strong>in</strong>guishes dose-related (type A – augmented effects<br />
<strong>of</strong> the drug action) and non-dose-related (type B – bizarre<br />
reactions) adverse drug reactions. There are other groups <strong>in</strong><br />
this system <strong>of</strong> classification but these may also be considered<br />
as subclasses or hybrids <strong>of</strong> type A and B ADRs. These are<br />
type C ADRs (chronic reactions, dose- and time-related),<br />
Farcas et al<br />
type D (delayed reactions, time-related), type E (end <strong>of</strong><br />
use reactions) and type F (failure <strong>of</strong> therapy) [9, 12]. The<br />
characteristics, some examples and the management <strong>of</strong><br />
these ADRs are listed <strong>in</strong> Table I [9, 13-18]. An alternative<br />
classification system proposes only 3 major groups <strong>of</strong><br />
adverse reactions, referred as type A (drug actions), type B<br />
(patient reactions) and type C (statistical effects) adverse<br />
drug reactions [13[.<br />
ADRs’ diagnosis and causality assessment<br />
It might be difficult to establish a cl<strong>in</strong>ical diagnosis <strong>of</strong><br />
drug-<strong>in</strong>duced disease as ADRs tend to mimic any natural<br />
occurr<strong>in</strong>g disease process. Few drugs produce dist<strong>in</strong>ctive<br />
and specific physical signs that can be considered without<br />
any doubt ADRs (e.g. extrapyramidal disorders). In any<br />
case, if the patient is tak<strong>in</strong>g drugs, a differential diagnosis<br />
should consider the probability <strong>of</strong> an ADR. Several years<br />
ago Irey described, <strong>in</strong> a very comprehensive manner, the<br />
diagnostic problems that might <strong>in</strong>terfere <strong>in</strong> the evaluation <strong>of</strong><br />
an ADR and proposed a methodology that is still valid and<br />
applicable. When assess<strong>in</strong>g the probability <strong>of</strong> a suspected<br />
ADR, the cl<strong>in</strong>ician should always evaluate the follow<strong>in</strong>g<br />
aspects: temporal relationship between the use <strong>of</strong> the drug<br />
and the occurrence <strong>of</strong> the reaction (time to onset), the<br />
differential diagnosis (<strong>of</strong> causes other than the suspected<br />
drug), the selection <strong>of</strong> the responsible drug on the basis<br />
<strong>of</strong> pattern <strong>of</strong> the event or by exclusion, dechallenge and<br />
rechallenge. The pattern <strong>of</strong> the adverse event must fit<br />
the known pharmacology or allergy pattern <strong>of</strong> one <strong>of</strong> the<br />
suspected drugs or <strong>of</strong> chemically or pharmacological related<br />
compounds. Detailed <strong>in</strong>formation on all these aspects that<br />
must be considered when evaluat<strong>in</strong>g an ADR is presented<br />
<strong>in</strong> Panel 1 [9, 15, 19].<br />
When evaluat<strong>in</strong>g an ADR, one must take <strong>in</strong>to consideration<br />
the factors that can predispose patients to adverse reactions.<br />
Some ADRs are associated with specific patient and/or drugrelated<br />
factors. These factors are presented <strong>in</strong> Table II. Among<br />
these factors, the pharmacok<strong>in</strong>etic and pharmacodynamic<br />
pr<strong>of</strong>ile <strong>of</strong> a drug might be <strong>in</strong>fluenced by disease pathology,<br />
physiologic status, concomitant therapy and lifestyle.<br />
For example, excessively high or low concentrations <strong>of</strong> a<br />
drug at the site <strong>of</strong> action may occur as a result <strong>of</strong> altered<br />
pharmacok<strong>in</strong>etic <strong>of</strong> the drug (e.g. metabolism, excretion).<br />
Concurrent diseases such as renal impairment will lead to<br />
drug toxicity for drugs or drug metabolites that are highly<br />
dependent on the kidney for removal, if the dose <strong>of</strong> the drug<br />
is not properly adjusted. Likewise, doses <strong>of</strong> the drugs that<br />
undergo hepatic metabolism may also produce toxicity <strong>in</strong><br />
patients with severe hepatic disease, particularly cirrhosis.<br />
Cardiovascular disease such as congestive heart failure may<br />
also reduce hepatic blood flow and decrease the clearance<br />
<strong>of</strong> certa<strong>in</strong> drugs [20].<br />
<strong>Drug</strong>-drug <strong>in</strong>teractions contribute to a significant number<br />
<strong>of</strong> ADRs, especially <strong>in</strong> elderly patients and <strong>in</strong> patients that are<br />
under polymedication. There is an exponential relationship<br />
between the number <strong>of</strong> drugs taken and the probability <strong>of</strong> an
<strong>Adverse</strong> drug reactions <strong>in</strong> cl<strong>in</strong>ical practice 355<br />
Table I. The classification <strong>of</strong> adverse drug reaction<br />
Type <strong>of</strong> ADR Characteristics Examples Management<br />
Type A (augmented)<br />
Type B (bizarre)<br />
Type C (chronic)<br />
Type D (delayed)<br />
Type E (end <strong>of</strong> use)<br />
Type F (failure <strong>of</strong><br />
therapy)<br />
Dose-related<br />
Common (overall proportion <strong>of</strong> ADRs<br />
- 80%)<br />
Suggestive time relationship<br />
Related to a pharmacological action <strong>of</strong><br />
the drug<br />
Predictable from known pharmacology<br />
Variable severity, but usually mild<br />
High morbidity<br />
Low mortality<br />
Reproducible<br />
Not dose–related<br />
Uncommon<br />
Not related to a pharmacological action<br />
<strong>of</strong> the drug<br />
Not predictable from known<br />
pharmacology<br />
Variable severity, proportionately more<br />
severe than type A<br />
High morbidity<br />
High mortality<br />
Not reproducible<br />
Uncommon<br />
Related to cumulative dose<br />
Long term exposure required<br />
Uncommon<br />
Usually dose-related<br />
Seen on prolonged exposure to a drug<br />
or exposure at a critical time<br />
Uncommon<br />
Occurs soon after withdrawal <strong>of</strong> a drug<br />
Common<br />
May be dose-related<br />
Often caused by drug <strong>in</strong>teractions<br />
<strong>Drug</strong> toxicity<br />
Nephrotoxicity caused by am<strong>in</strong>oglicosides<br />
Dysrhythmia caused by digox<strong>in</strong><br />
Side effects<br />
Constipation caused by chronic opioid use<br />
Antichol<strong>in</strong>ergic effects <strong>of</strong> tricyclic<br />
antidepressants<br />
They derive from:<br />
Primary pharmacology (augmentation <strong>of</strong> known<br />
actions): β-blocker <strong>in</strong>duced bradycardia<br />
Secondary pharmacology (<strong>in</strong>volves different<br />
organ or system, but expla<strong>in</strong>able from known<br />
pharmacology): β-blocker <strong>in</strong>duced bronchospasm<br />
Intolerance<br />
T<strong>in</strong>nitus caused by small doses <strong>of</strong> aspir<strong>in</strong><br />
Allergy (hypersensitivity or immunological)<br />
Result <strong>of</strong> an immune response to a drug:<br />
Penicill<strong>in</strong>- <strong>in</strong>duced urticaria<br />
Pseudoallergic (non-immunological)<br />
Immediate, generalised reaction <strong>in</strong>volv<strong>in</strong>g<br />
mast-cell mediator release: respiratory<br />
syndromes caused by NSAIDs<br />
Idiosyncratic (unexpected response to a drug, not<br />
related to an allergic mechanism)<br />
Anticonvulsant hypersensitivity syndrome<br />
reaction<br />
Hypothalamic-pituitary-adrenal axis suppression<br />
by corticosteroids<br />
Teratogenesis<br />
Carc<strong>in</strong>ogenesis<br />
Tardive dysk<strong>in</strong>esia caused by antipsychotic<br />
medication<br />
Opiate withdrawal syndrome<br />
Rebound hypotension on clonid<strong>in</strong>e withdrawal<br />
Ineffectiveness<br />
Resistance <strong>of</strong> a micro-organism or tumour to the<br />
drug action<br />
Tolerance<br />
Tachyphylaxia<br />
Reduce dose or withhold<br />
Consider effects <strong>of</strong><br />
concomitant therapy<br />
Withhold and avoid <strong>in</strong> the<br />
future<br />
Reduce dose or withhold;<br />
withdrawal may have to be<br />
prolonged<br />
Often <strong>in</strong>tractable<br />
Re<strong>in</strong>troduce and withdraw<br />
slowly<br />
Increase dosage or change<br />
the therapeutic agent;<br />
Consider effects <strong>of</strong><br />
concomitant therapy<br />
ADR, <strong>in</strong>dependent <strong>of</strong> the therapeutic class and the patient’s<br />
underly<strong>in</strong>g disease [21]. <strong>Drug</strong> <strong>in</strong>teractions may cause altered<br />
drug bioavailability, distribution, clearance and additive or<br />
antagonistic pharmacodynamic effects. A recently published<br />
study <strong>in</strong>dicated that the percentage <strong>of</strong> drug-drug <strong>in</strong>teractions<br />
identified as cause <strong>of</strong> ADRs was 15% [22]. Another study<br />
that <strong>in</strong>vestigated potential drug <strong>in</strong>teractions concluded that<br />
68-70% <strong>of</strong> the potential <strong>in</strong>teractions detected might demand<br />
cl<strong>in</strong>ical attention, while 1-2% are life-threaten<strong>in</strong>g [23]. These<br />
<strong>in</strong>teractions have been extensively reviewed <strong>in</strong> different<br />
studies and are <strong>of</strong>ten predictable and preventable.<br />
In appropriate prescription <strong>of</strong> drugs <strong>in</strong> the elderly<br />
population is also a major risk factor for present<strong>in</strong>g ADRs<br />
although <strong>in</strong>correctly used drugs constitute a cause <strong>of</strong> ADRs<br />
<strong>in</strong> the general population too [22, 24]. A recent prospective<br />
study demonstrated that from the total number <strong>of</strong> drugs used<br />
by the study population, 26% were <strong>in</strong>correctly used and that<br />
44.5% <strong>of</strong> the ADRs detected <strong>in</strong>volved at least one <strong>in</strong>correctly<br />
used drug [25]. Unknown co-medication to the treat<strong>in</strong>g<br />
physician, <strong>in</strong>clud<strong>in</strong>g self-medication, may compromise<br />
drug safety, by <strong>in</strong>creas<strong>in</strong>g the risk <strong>of</strong> duplicate therapy, drug<br />
<strong>in</strong>teractions, and ADRs that are not recognised as such [26].<br />
Thus, it is essential to <strong>in</strong>terview the patient <strong>in</strong> order to take a<br />
proper full drug history and to consider a drug-related cause<br />
for the patient’s condition especially when other causes do<br />
not expla<strong>in</strong> it. All these factors that might predispose patients<br />
to ADR must be taken <strong>in</strong>to consideration when evaluat<strong>in</strong>g<br />
an adverse event.<br />
The development <strong>of</strong> a symptom or detrimental outcome<br />
while under therapy with several drugs, does not establish<br />
the fact that one <strong>of</strong> the drugs might be the cause <strong>of</strong> the <strong>in</strong>jury.<br />
Likewise, the development <strong>of</strong> an adverse event or disease,<br />
with no relevant time relationship with the use <strong>of</strong> a drug does<br />
not exonerate the drug from be<strong>in</strong>g the causative agent. In<br />
any case, the failure to recognise an adverse drug reaction,<br />
may lead to <strong>in</strong>appropriate measures. The universal decision<br />
to treat an unrecognised drug-related symptom with another<br />
medication exposes the patient to additional drug hazards. In
356<br />
Farcas et al<br />
Panel 1. Po<strong>in</strong>ts to consider for the evaluation <strong>of</strong> a suspected adverse drug reaction<br />
a. The temporal relationship (time to onset)<br />
There should be a plausible temporal relationship between exposure and the onset <strong>of</strong> the suspected ADR, tak<strong>in</strong>g <strong>in</strong>to consideration the<br />
pharmacological characteristics <strong>of</strong> the suspected drug. For short-term reactions, e.g. flush<strong>in</strong>g with nifedip<strong>in</strong>e, the relevant time to onset<br />
is the time between the last dose and the onset <strong>of</strong> the reaction. For long-term reactions, e.g. hepatitis with methotrexate, the relevant<br />
period is the time from the beg<strong>in</strong>n<strong>in</strong>g <strong>of</strong> the therapy and ADR onset.<br />
b. Exist<strong>in</strong>g <strong>in</strong>formation about the ADR<br />
The event described had been previously reported as an ADR <strong>in</strong> cl<strong>in</strong>ical trials, post-market<strong>in</strong>g studies, case reports. If the event is not<br />
documented anywhere else, it does not necessarily mean that it cannot occur with the suspected drug.<br />
c. Pharmacological plausibility<br />
Most type A reactions are pharmacodynamic and pharmacok<strong>in</strong>etic plausible, though easy to diagnose. However, the recognition <strong>of</strong><br />
type B reaction might be difficult if previous reports on that particular ADR are not available.<br />
d. Exclusion <strong>of</strong> other causes<br />
Alternative causes (other than the suspected drug) such as patient’s underly<strong>in</strong>g disease or other drugs cannot expla<strong>in</strong> the reaction.<br />
e. Dechallenge or dose reduction<br />
Recovery or condition improvement after stopp<strong>in</strong>g the drug or after the dose reduction is supportive for a causal relationship,<br />
particularly when the tim<strong>in</strong>g <strong>of</strong> the recovery/condition improvement is consistent with the pharmacological characteristics <strong>of</strong> the drug;<br />
some ADRs might be irreversible.<br />
f. Rechallenge or dose <strong>in</strong>crease<br />
The recurrence <strong>of</strong> the ADR after dose <strong>in</strong>crease or rechallenge is a strong <strong>in</strong>dicator <strong>of</strong> causality. Rechallenge is justifiable only if the<br />
benefit to the patient outweighs the risks <strong>of</strong> the reaction’s recurrence, as <strong>in</strong> some cases the reaction (especially type B reactions) may<br />
be more severe or even fatal on repeated exposure.<br />
g. <strong>Drug</strong> <strong>in</strong>teractions<br />
If a drug <strong>in</strong>teraction is suspected <strong>in</strong> caus<strong>in</strong>g the ADR, plausible temporal relationship with the <strong>in</strong>troduction or withdrawal <strong>of</strong> the<br />
<strong>in</strong>teract<strong>in</strong>g drug is an important consideration <strong>in</strong> causality assessment.<br />
order to avoid multiple drug events, adverse drug reactions<br />
recognition is mandatory, as <strong>in</strong> this case, the appropriate<br />
action is the dose reduction or even the discont<strong>in</strong>uation <strong>of</strong><br />
the causative drug. Determ<strong>in</strong><strong>in</strong>g if an adverse event is caused<br />
by a certa<strong>in</strong> drug with reasonable certa<strong>in</strong>ty is a difficult part<br />
<strong>of</strong> ADRs’ evaluation, but it is essential for proper cl<strong>in</strong>ical<br />
decisions [27, 28].<br />
The aim <strong>of</strong> the causality assessment is to establish a<br />
level <strong>of</strong> probability regard<strong>in</strong>g the suspicion that a certa<strong>in</strong><br />
drug is responsible for an adverse event. Accord<strong>in</strong>g to the<br />
most widely used with or without score algorithms, ADRs<br />
can be “certa<strong>in</strong>”, “probable/likely”, “possible” and “unlikely/<br />
doubtful”. The WHO-UMC developed a causality system<br />
which takes <strong>in</strong>to account the cl<strong>in</strong>ical-pharmacological<br />
aspects, whereas previous knowledge <strong>of</strong> the ADR plays a<br />
less prom<strong>in</strong>ent role [6]. Perhaps the most commonly used<br />
causality assessment method, which has ga<strong>in</strong>ed popularity<br />
among cl<strong>in</strong>icians because <strong>of</strong> its simplicity, is the Naranjo<br />
probability scale presented <strong>in</strong> Panel 2. It is a structured,<br />
transparent, consistent and easy to apply assessment method<br />
[15].<br />
Causality assessment <strong>of</strong> a theoretical drug<strong>in</strong>duced<br />
case <strong>of</strong> pancreatitis<br />
A 56-year old female with a history <strong>of</strong> hypertension,<br />
heart failure and type 2 diabetes mellitus was admitted<br />
to an <strong>in</strong>ternal medic<strong>in</strong>e department present<strong>in</strong>g abdom<strong>in</strong>al<br />
pa<strong>in</strong> radiat<strong>in</strong>g to the back, nausea and vomit<strong>in</strong>g, jaundice,<br />
anorexia, sweat<strong>in</strong>g, weakness, headache and low-grade fever<br />
(38.7°C) for the previous 3 days. The patient’s therapy <strong>in</strong><br />
the last six months <strong>in</strong>cluded digox<strong>in</strong> 0.25 mg daily except<br />
on Thursdays and Sundays, hydrochlorothiazide 25 mg once<br />
daily and a comb<strong>in</strong>ation <strong>of</strong> rosiglitazone/metform<strong>in</strong> 1mg/<br />
500 mg. Two months prior to admission alfacalcidol 2μg<br />
and calcium 1000 mg daily were <strong>in</strong>itiated for osteoporosis<br />
prophylaxis. There was no history <strong>of</strong> alcohol <strong>in</strong>gestion or<br />
previous abdom<strong>in</strong>al surgery.<br />
On physical exam<strong>in</strong>ation, the abdomen was distended<br />
and with dim<strong>in</strong>ished bowel sounds. On admission the<br />
laboratory data revealed <strong>in</strong>creased serum levels <strong>of</strong> amylase<br />
549 U/L, glucose 166 mg/dL, WBC 14,400, bilirub<strong>in</strong> 4.2 mg/<br />
dL. Except a calcium value <strong>of</strong> 12 mg/dL, all other laboratory<br />
exam<strong>in</strong>ations were normal. Abdom<strong>in</strong>al ultrasonography<br />
showed pancreatic oedema and ruled out gallstones,<br />
cysts and <strong>in</strong>test<strong>in</strong>al obstruction. No biliary dilatation was<br />
observed. <strong>Drug</strong>-<strong>in</strong>duced pancreatitis was considered after<br />
exclusion <strong>of</strong> other causes (alcohol <strong>in</strong>take, cholelithiasis,<br />
hyperlipidemia, abdom<strong>in</strong>al trauma). Hydrochlorothiazide<br />
was the suspected drug and it was discont<strong>in</strong>ued. A mild drug<br />
<strong>in</strong>duced hypercalcemia was also considered, alfacalcidol<br />
and calcium be<strong>in</strong>g stopped until the serum levels became<br />
normocalcemic. The patient received symptomatic medical<br />
treatment. The cl<strong>in</strong>ical status <strong>of</strong> the patient improved with<strong>in</strong><br />
48 hours after the discont<strong>in</strong>uation <strong>of</strong> hydrochlorothiazide.<br />
On hospital day 3 serum amylase levels returned to normal<br />
and on day 5 the patient was discharged.<br />
Case discussion<br />
Thiazide diuretics <strong>in</strong> normal doses have been reported<br />
to be associated with pancreatitis which develops with<strong>in</strong>
<strong>Adverse</strong> drug reactions <strong>in</strong> cl<strong>in</strong>ical practice 357<br />
Table II. Factors predispos<strong>in</strong>g patients to ADRs<br />
Pharmacodynamic factors<br />
Variation <strong>in</strong> receptor sensitivity<br />
Pharmacok<strong>in</strong>etic factors<br />
Absorption<br />
Distribution<br />
Metabolism<br />
Excretion<br />
Concurrent disease<br />
Renal impairment<br />
Hepatic impairment<br />
Congestive heart failure<br />
<strong>Drug</strong> <strong>in</strong>teractions<br />
Physiologic conditions<br />
Age<br />
Pregnancy<br />
Obesity<br />
Lifestyle factors<br />
Alcohol <strong>in</strong>take<br />
Smok<strong>in</strong>g<br />
Genetic variability (genetic polymorphism)<br />
Adherence to prescribed therapy<br />
Medication errors<br />
Panel 2. Naranjo probability scale<br />
1. Are there previous conclusive reports on<br />
this reaction?<br />
2. Did the adverse reaction appear after the<br />
suspected drug was adm<strong>in</strong>istered?<br />
3. Did the adverse reaction improve when<br />
the drug was discont<strong>in</strong>ued or a specific<br />
antagonist was adm<strong>in</strong>istered?<br />
4. Did the adverse reaction reappear when<br />
the drug was readm<strong>in</strong>istered?<br />
5. Are there alternative causes that could on<br />
their own have caused the reaction?<br />
6. Did the reaction reappear when a placebo<br />
was given?<br />
7. Was the drug detected <strong>in</strong> the blood (or<br />
other fluids) <strong>in</strong> concentrations known to be<br />
toxic?<br />
8. Was the reaction more severe when the<br />
dose was <strong>in</strong>creased or less severe when the<br />
dose was decreased?<br />
9. Did the patient have a similar reaction<br />
to the same or similar drug <strong>in</strong> any previous<br />
exposure?<br />
10. Was the adverse event confirmed by<br />
any objective evidence?<br />
Yes No Don’t<br />
know<br />
+1 0 0<br />
+2 -1 0<br />
+1 0 0<br />
+2 -1 0<br />
-1 +2 0<br />
-1 +1 0<br />
+1 0 0<br />
+1 0 0<br />
+1 0 0<br />
+1 0 0<br />
SCORE 9 = def<strong>in</strong>ite; 5-8 = probable; 1-4 = possible; 0 = doubtful<br />
two weeks to as long as 1 year after <strong>in</strong>itiation <strong>of</strong> the<br />
therapy. Several potential mechanisms <strong>of</strong> thiazide-<strong>in</strong>duced<br />
pancreatitis have been suggested <strong>in</strong> the literature. Thiazides<br />
Panel 3. Causality assessment <strong>of</strong> the pancreatitis case<br />
us<strong>in</strong>g the Naranjo probability scale<br />
1. There are conclusive reports on this adverse reaction<br />
as thiazide diuretics agents are known to produce<br />
pancreatitis; we found several case <strong>of</strong> pancreatitis<br />
associated with hydrochlorothiazide<br />
2. Hydrochlorothiazide, the suspected drug, was<br />
adm<strong>in</strong>istered dur<strong>in</strong>g the previous six months before the<br />
sudden onset <strong>of</strong> the adverse reaction<br />
3. The adverse reaction improved with<strong>in</strong> the 48 hours<br />
after the discont<strong>in</strong>uation <strong>of</strong> the drug<br />
4. There is no <strong>in</strong>formation about the reappearance <strong>of</strong> the<br />
drug-<strong>in</strong>duced pancreatitis <strong>in</strong> this patient as rechallenge<br />
was not performed<br />
Score<br />
5. The alternative causes for pancreatitis were ruled out +2<br />
6. A placebo was not given to the patient, the answer is<br />
“don’t know” <strong>in</strong> this case<br />
7. This analysis (drug’s plasmatic concentration) was<br />
not performed <strong>in</strong> this case, the answer is “don’t know”<br />
8. The dose was neither decreased nor <strong>in</strong>creased so we<br />
don’t know the evolution <strong>of</strong> the reaction <strong>in</strong> this case<br />
9. There is no past history <strong>of</strong> any similar reaction to the<br />
same or similar drugs<br />
10. The adverse reaction was documented by relevant<br />
laboratory tests<br />
Total score +7<br />
Category<br />
+1<br />
+2<br />
+1<br />
0<br />
0<br />
0<br />
0<br />
0<br />
+1<br />
Probable<br />
can cause hypercalcemia by decreas<strong>in</strong>g renal calcium<br />
excretion. Hypercalcemia is a condition known to <strong>in</strong>crease<br />
the risk <strong>of</strong> pancreatitis which may lead to calculi with<strong>in</strong> the<br />
pancreatic duct and/or may accelerate the conversion <strong>of</strong><br />
tryps<strong>in</strong>ogen to tryps<strong>in</strong> [20]. At the same time, hypercalcemia<br />
is a predom<strong>in</strong>ant adverse effect associated with alfacalcidol,<br />
which <strong>in</strong> this patient has been adm<strong>in</strong>istered <strong>in</strong> a high<br />
dose; the effect usually reverses rapidly on withdrawal <strong>of</strong><br />
the drug. A probable drug-drug <strong>in</strong>teraction may also be<br />
suspected to have <strong>in</strong>creased the calcium serum levels, as<br />
the concurrent use <strong>of</strong> calcium-conta<strong>in</strong><strong>in</strong>g preparations and<br />
thiazide diuretics enhance the risk <strong>of</strong> hypercalcemia. Another<br />
drug <strong>in</strong>teraction, with no relation to pancreatitis, but which<br />
should be underl<strong>in</strong>ed and considered <strong>in</strong> this case, is digox<strong>in</strong><br />
– hydrochlorothiazide <strong>in</strong>teraction which may lead to digitalis<br />
toxicity with nausea, vomit<strong>in</strong>g and arrhythmias. If a digitalis<br />
glycoside and a thiazide diuretic are used concurrently, the<br />
patient should be monitored for ECG signs <strong>of</strong> potassium<br />
depletion, and potassium supplementation should be<br />
considered. The causality assessment <strong>of</strong> this adverse event,<br />
presented <strong>in</strong> Panel 3, revealed a probable association between<br />
hydrochlorothiazide and pancreatitis as rechallenge was<br />
not performed. In a drug-<strong>in</strong>duced pancreatitis case, patients<br />
should never be rechallenged with any drug that has caused<br />
even one episode <strong>of</strong> pancreatitis [20].<br />
Conclusions<br />
Prompt recognition <strong>of</strong> adverse drug reactions, adequate<br />
and effective cl<strong>in</strong>ical management <strong>of</strong> their outcome
358<br />
is mandatory <strong>in</strong> promot<strong>in</strong>g patients’ safety. Health<br />
pr<strong>of</strong>essionals who care for patients’ drug therapy are taught<br />
to consider as well the benefit as the risk when mak<strong>in</strong>g<br />
therapeutic choices. The tra<strong>in</strong><strong>in</strong>g regard<strong>in</strong>g adverse events<br />
is <strong>of</strong>ten limited, consider<strong>in</strong>g the reality that expected (due to<br />
pharmacologic action) or unexpected (due to idiosyncratic<br />
reactions) adverse drug reactions, if not recognised, can<br />
<strong>in</strong>crease the risk <strong>of</strong> harm. Several aspects should be taken<br />
<strong>in</strong>to consideration <strong>in</strong> order to recognize and properly manage<br />
adverse drug reactions. The first is that careful observation<br />
and high cl<strong>in</strong>ical suspicion are <strong>of</strong> crucial importance <strong>in</strong><br />
order to identify a drug related problem, <strong>in</strong>clud<strong>in</strong>g adverse<br />
drug reactions. The second is that, even though a drug has<br />
been on the market for several years, is widely used and<br />
with known side effects pr<strong>of</strong>ile, unusual adverse reactions<br />
may still be identified. Tak<strong>in</strong>g <strong>in</strong>to account all these aspects<br />
will lead to better adverse drug reaction management and<br />
<strong>in</strong>creased patients’ safety.<br />
Conflicts <strong>of</strong> <strong>in</strong>terest<br />
None to declare.<br />
Acknowledgements<br />
The documentation for this study was supported by<br />
a research grant f<strong>in</strong>anced by the Romanian M<strong>in</strong>istry <strong>of</strong><br />
Education and Research – PNII Partnership <strong>in</strong> Prioritary<br />
Issues 12-102 / 2008<br />
References<br />
1. Pirmohamed M, James S, Meak<strong>in</strong> S, et al. <strong>Adverse</strong> drug reaction<br />
as cause <strong>of</strong> admission to hospital: prospective analysis <strong>of</strong> 18 820<br />
patients. BMJ 2004; 329: 15-19.<br />
2. Lazarou J, Pomeranz B, Corey PN. Incidence <strong>of</strong> adverse drug<br />
reactions <strong>in</strong> hospitalized patients. A meta-analysis <strong>of</strong> prospective<br />
studies. JAMA 1998; 279: 1200-1205.<br />
3. Dormann H, Muth-Selbach U, Krebs S, et al. Incidence and costs<br />
<strong>of</strong> adverse drug reactions dur<strong>in</strong>g hospitalization: computerized<br />
monitor<strong>in</strong>g versus stimulated spontaneous report<strong>in</strong>g. <strong>Drug</strong> Saf 2000;<br />
22: 161-168.<br />
4. Rodriguez-Monguio R, Otero MJ, Rovira J. Assess<strong>in</strong>g the economic<br />
impact <strong>of</strong> adverse drug effects. Pharmacoeconomics 2003; 21: 623-<br />
650.<br />
5. Dormann H, Criegee-Rieck M, Neubert A, et al. Lack <strong>of</strong> awareness <strong>of</strong><br />
community-acquired adverse drug reactions upon hospital admission.<br />
<strong>Drug</strong> Saf 2003; 26: 353-362.<br />
6. The use <strong>of</strong> the WHO–UMC system for standardised case causality<br />
assessment. Accessed at http://www.who-umc.org/graphics/4409.<br />
pdf on February, 28th, 2009.<br />
7. Naranjo CA, Busto U, Sellers EM, et al. A method for estimat<strong>in</strong>g the<br />
probability <strong>of</strong> adverse drug reactions. Cl<strong>in</strong> Pharmacol Ther 1981;<br />
30: 239–245.<br />
8. L<strong>in</strong>dquist M. The need for def<strong>in</strong>itions <strong>in</strong> pharmacovigilance. <strong>Drug</strong><br />
Saf 2007; 30: 825-830.<br />
Farcas et al<br />
9. Edwards IR, Aronson JK. <strong>Adverse</strong> drug reactions: def<strong>in</strong>itions,<br />
diagnosis, and management. Lancet 2000; 356:1255–1259.<br />
10. Cl<strong>in</strong>ical safety data management: def<strong>in</strong>itions and standards for<br />
expedited report<strong>in</strong>g. London: European Agency for the Evaluation<br />
<strong>of</strong> Medic<strong>in</strong>al Products, Human Medic<strong>in</strong>es Evaluation Unit; 1995.<br />
Accessed at www.emea.eu.<strong>in</strong>t/pdfs/human/ich/037795en.pdf.<br />
11. WHO safety <strong>of</strong> medic<strong>in</strong>es. A guide to detect<strong>in</strong>g and report<strong>in</strong>g adverse<br />
drug reactions. Why health pr<strong>of</strong>essionals need to take action. Geneva:<br />
World Health Organization; 2002. WHO/EDM/QSM/2002.2.<br />
12. Atuah KN, Hughes D, Pirmohamed M. Cl<strong>in</strong>ical pharmacology: special<br />
safety considerations <strong>in</strong> drug development and pharmacovigilance.<br />
<strong>Drug</strong> Saf 2004; 27: 535-554.<br />
13. Meyboom RH, L<strong>in</strong>dquist M, Egberts AC. An ABC <strong>of</strong> drug-related<br />
problems. <strong>Drug</strong> Saf 2000; 22: 415-423.<br />
14. Mann RD, Andrews EB. Pharmacovigilance. 2nd Edn, Chichester,<br />
UK: John Wiley & Sons, Ltd, 2007.<br />
15. Talbot J, Waller P. Stephens: Detection <strong>of</strong> New <strong>Adverse</strong> <strong>Drug</strong><br />
<strong>Reactions</strong>. 5th Edn, Chichester, UK: John Wiley & Sons, 2004.<br />
16. Rehan HS, Chopra D, Kakkar AK. Physician’s guide to<br />
pharmacovigilance: term<strong>in</strong>ology and causality assessment. Eur J<br />
Intern Med 2009; 20: 3-8.<br />
17. Jaquenoud Sirot E, Van der Velden JW, Rentsch K, Eap CB, Baumann<br />
P. Therapeutic drug monitor<strong>in</strong>g and pharmacogenetic tests as tools<br />
<strong>in</strong> pharmacovigilance. <strong>Drug</strong> Saf 2006; 29: 735-768.<br />
18. Meyboom RH, L<strong>in</strong>dquist M, Flygare AK, Biriell C, Edwards IR.<br />
The value <strong>of</strong> report<strong>in</strong>g therapeutic <strong>in</strong>effectiveness as an adverse drug<br />
reaction. <strong>Drug</strong> Saf 2000; 23: 95-99.<br />
19. Irey NS. Diagnostic problems <strong>in</strong> drug-<strong>in</strong>duced diseases. Ann Cl<strong>in</strong><br />
Lab Sci. 1976; 6: 272-277.<br />
20. Tisdale JE, Miller DA. <strong>Drug</strong>-Induced Diseases. Prevention,<br />
Detection and Management. Bethesda, Maryland: American Society<br />
<strong>of</strong> Health-System Pharmacists Press, 2005.<br />
21. Atk<strong>in</strong> PA, Veitch PC, Veitch EM, Ogle SJ. The epidemiology <strong>of</strong><br />
serious adverse drug reactions among the elderly. <strong>Drug</strong>s Ag<strong>in</strong>g 1999;<br />
14: 141-152.<br />
22. Passarelli MC, Jacob-Filho W, Figueras A. <strong>Adverse</strong> drug reactions<br />
<strong>in</strong> an elderly hospitalised population: <strong>in</strong>appropriate prescription is<br />
a lead<strong>in</strong>g cause. <strong>Drug</strong>s Ag<strong>in</strong>g 2005; 22: 767-777.<br />
23. Köhler GI, Bode-Böger SM, Busse R, Hoopmann M, Welte T, Böger<br />
RH. <strong>Drug</strong>-drug <strong>in</strong>teractions <strong>in</strong> medical patients: effects <strong>of</strong> <strong>in</strong>-hospital<br />
treatment and relation to multiple drug use. Int J Cl<strong>in</strong> Pharmacol Ther<br />
2000; 38: 504-513.<br />
24. Laroche ML, Charmes JP, Nouaille Y, Fourrier A, Merle L. Impact<br />
<strong>of</strong> hospitalisation <strong>in</strong> an acute medical geriatric unit on potentially<br />
<strong>in</strong>appropriate medication use. <strong>Drug</strong>s Ag<strong>in</strong>g 2006; 23: 49-59.<br />
25. Jonville-Bera AP, Bera F, Autret-Leca E. Are <strong>in</strong>correctly used drugs<br />
more frequently <strong>in</strong>volved <strong>in</strong> adverse drug reactions? A prospective<br />
study. Eur J Cl<strong>in</strong> Pharmacol 2005; 61: 231–236.<br />
26. Rieger K, Scholer A, Arnet I, et al. High prevalence <strong>of</strong> unknown<br />
co-medication <strong>in</strong> hospitalised patients. Eur J Cl<strong>in</strong> Pharmacol 2004;<br />
60: 363–368.<br />
27. Brewer T, Colditz GA. Postmarket<strong>in</strong>g surveillance and adverse drug<br />
reactions. current perspectives and future needs. JAMA 1999; 281:<br />
824-829.<br />
28. Nebeker JR, Barach P, Samore MH. Clarify<strong>in</strong>g adverse drug events:<br />
a cl<strong>in</strong>ician’s guide to term<strong>in</strong>ology, documentation, and report<strong>in</strong>g. Ann<br />
Intern Med 2004; 140: 795-801.