Management of Boerhaave's Syndrome: Report of Three ... - rjge.ro
Management of Boerhaave's Syndrome: Report of Three ... - rjge.ro
Management of Boerhaave's Syndrome: Report of Three ... - rjge.ro
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<st<strong>ro</strong>ng>Management</st<strong>ro</strong>ng> <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> Boerhaave’s <st<strong>ro</strong>ng>Synd<strong>ro</strong>me</st<strong>ro</strong>ng>: <st<strong>ro</strong>ng>Report</st<strong>ro</strong>ng><br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> <st<strong>ro</strong>ng>Three</st<strong>ro</strong>ng> Cases<br />
Konstantinos Tsalis, Konstantinos Vasiliadis, Theodor Tsachalis, Emmanuel Christ<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng>oridis,<br />
Konstantinos Blouhos, Dimitrios Betsis<br />
4 th Surgical Department, Aristotle University <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> Thessaloniki, Exohi 570 10, Thessaloniki, Greece<br />
Abstract<br />
F<strong>ro</strong>m 2000 to 2005, three patients with Boerhaave’s<br />
synd<strong>ro</strong>me were successfully managed in our Department.<br />
Two <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> them received the app<strong>ro</strong>priate treatment belatedly,<br />
with primary closure and bolstering tissue wrap. One <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> them<br />
required further intervention with a cervical esophagostomy<br />
and exclusion <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the perforated esophagus. The third<br />
patient with an esophageal perforation related disorder,<br />
was managed with surgical exploration and drainage alone.<br />
Primary suturing <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus should be performed only<br />
in patients with an early perforation. In cases <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> p<strong>ro</strong>longed<br />
delay between rupture and diagnosis, esophageal resection<br />
with cervical esophagostomy and gast<strong>ro</strong>stomy is advocated<br />
as the safest therapy.<br />
Key words<br />
Primary esophageal perforation - Boerhaave’s synd<strong>ro</strong>me<br />
- current treatment<br />
Int<strong>ro</strong>duction<br />
Boerhaave’s synd<strong>ro</strong>me represents the most sinister cause<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> esophageal perforation [1]. It remains a potentially lethal<br />
complication, and is still associated with a high mortality rate<br />
[1-6]. Classical presentation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> this synd<strong>ro</strong>me is vomiting,<br />
chest pain, and subcutaneous emphysema. However, this<br />
triad, first described by Mackler [3] is seldom found. Delay<br />
in diagnosis is common, resulting in substantial mortality.<br />
Some authors report mortality figures more than 65% after<br />
24 hours and 75-89% after 48 hours [1,2,4].<br />
The general consensus, concerning the management <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
this synd<strong>ro</strong>me, is early diagnosis and timely inhibition <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the<br />
J Gast<strong>ro</strong>intestin Liver Dis<br />
March 2008 Vol.17 No 1, 81-85<br />
Address for correspondence:<br />
K. Vasiliadis<br />
Dorileou 3<br />
55133 Kalamaria<br />
Thessaloniki, Greece<br />
E-mail: keva@med.auth.gr<br />
fatal esophageal injury-induced inflammatory p<strong>ro</strong>cess[1,7-<br />
10]. Nevertheless, the optimal therapeutic app<strong>ro</strong>ach remains<br />
cont<strong>ro</strong>versial. Indeed, divergent therapeutic app<strong>ro</strong>aches<br />
have been reported with significant variance in outcome<br />
and complications, with mortality rates ranging f<strong>ro</strong>m<br />
3% to more than 50% [1]. The aim <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> this study is to<br />
present our experience on diagnosis and management <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
spontaneous esophageal rupture and assess the current<br />
management status according to recent literature data.<br />
Case report<br />
F<strong>ro</strong>m 2000 to 2005, three consecutive spontaneous<br />
esophageal perforations were managed in our Department.<br />
All were men, aged between 32 and 47 years. Clinical<br />
presentation, radiographic findings, localization <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> rupture,<br />
degree <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> contamination in the thorax, days f<strong>ro</strong>m admission<br />
till operation, treatment method, complications, the period<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> admission and ICU stay are listed in Table I.<br />
Patient 1<br />
A 42-year-old man, with a history <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> organic psychosynd<strong>ro</strong>me<br />
and pyloric channel stricture secondary to ch<strong>ro</strong>nic<br />
duodenal ulcer, was transferred to our Department after a<br />
spontaneous esophageal rupture that had been diagnosed<br />
elsewhere. The original diagnosis was delayed because mid<br />
epigastric and lower thoracic pain after forcible c<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng>fee-g<strong>ro</strong>und<br />
emesis was misinterpreted as an upper gast<strong>ro</strong>intestinal (GI)<br />
tract hemorrhage. On the fifth day <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> hospitalisation, after<br />
a hemorrhage relapse along with hemodynamic instability<br />
and systemic septic clinical signs, the patient underwent<br />
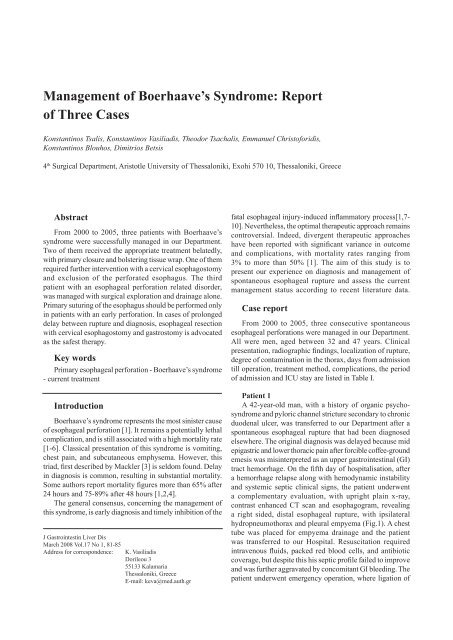
a complementary evaluation, with upright plain x-ray,<br />
contrast enhanced CT scan and esophagogram, revealing<br />
a right sided, distal esophageal rupture, with ipsilateral<br />
hyd<strong>ro</strong>pneumothorax and pleural empyema (Fig.1). A chest<br />
tube was placed for empyema drainage and the patient<br />
was transferred to our Hospital. Resuscitation required<br />
intravenous fluids, packed red blood cells, and antibiotic<br />
coverage, but despite this his septic pr<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng>ile failed to imp<strong>ro</strong>ve<br />
and was further aggravated by concomitant GI bleeding. The<br />
patient underwent emergency operation, where ligation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng>
82 Tsalis et al<br />
Table I Characteristics, treatment and outcome <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> patients who suffered spontaneous esophageal rupture<br />
Pt<br />
Sex/Age<br />
Chief<br />
complaints<br />
Time f<strong>ro</strong>m<br />
onset till<br />
surgery<br />
Imaging studies<br />
Chest X-ray CT Esophgography<br />
Location <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
rupture<br />
Surgical p<strong>ro</strong>cedure<br />
1M 42<br />
Postemetic, midepigastric,<br />
lower<br />
thoracic pain, dyspnea<br />
5 days<br />
Right hyd<strong>ro</strong>- Right Leakage into<br />
pneumo- pleural right pleural<br />
thorax empyema cavity<br />
Right side<br />
wall <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> LTE<br />
Right thoracotomydrainge,<br />
lapa<strong>ro</strong>tomybleeding<br />
duodenal ulcer<br />
oversewing-pylo<strong>ro</strong>plasty<br />
2M 32<br />
Postemetic lower<br />
thoracic pain,<br />
dyspnea, subcutaneous<br />
emphysema<br />
>25 hours<br />
Bilateral Bilateral Leakage<br />
pleural pleural into left<br />
effusion effusion pleural cavity<br />
Left side wall<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> LTE<br />
Bilateral thoracotomiesdrainage,<br />
primary<br />
closure<br />
3M 47<br />
Postemetic midepigastric<br />
and back<br />
pain, dyspnea<br />
12 hours<br />
Pneumo- Left Leakage into<br />
mediastinum pleural left pleural<br />
effusion cavity<br />
Left side wall<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> LTE<br />
Left thoracotomydrainage,lapa<strong>ro</strong>tomyprimary<br />
closure+foundoplication<br />
M=Male, LTE=Lower Thoracic Esophagus, SECMS=Self-Expandable Covered Metallic Stent, CT=Computed Tomography<br />
Subsequent p<strong>ro</strong>cedures<br />
Esophageal<br />
SECMS<br />
Cervical esophagostomy,<br />
esophageal exclusion,<br />
gast<strong>ro</strong>stomy, feeding<br />
jejunostomy, continuous<br />
pleural irrigation.<br />
Delayed esophageal<br />
reconstruction with left<br />
colic flexure<br />
None<br />
ICU<br />
stay<br />
10 days<br />
35 days<br />
2 days<br />
Time <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
discharge<br />
15 weeks<br />
9 weeks<br />
5 weeks
Boerhaave’s synd<strong>ro</strong>me 83<br />
Fig.1 Patient 1.Upright plain x-ray (a), esophagogram (b), and<br />
contrast enhanced CT scan (c) revealing a right sided, distal<br />
esophageal rupture, with ipsilateral hyd<strong>ro</strong>pneumothorax and<br />
pleural empyema.<br />
a bleeding vessel in the duodenal ulceration, pylo<strong>ro</strong>plasty,<br />
draining gast<strong>ro</strong>stomy and feeding jejunostomy were<br />
fashioned via an upper midline lapa<strong>ro</strong>tomy. Additionally, a<br />
right thoracotomy for better drainage and lavage <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the right<br />
thoracic cavity was performed and the chest was closed with<br />
two large thoracostomy tubes in situ. A hypaque swallow<br />
study, on the 4th postoperative week demonstrated closure<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophageal rent but revealed the development <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> a<br />
stricture along the lower third <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus, which p<strong>ro</strong>ved<br />
to be refractory to multiple endoscopic dilatations performed<br />
between the 9th and 11th postoperative weeks. The patient<br />
was considered to be unfit for esophageal replacement and in<br />
addition he was reluctant to undergo any major intervention.<br />
Hence, a covered self-expanding metallic stent (Ultraflex,<br />
Boston Scientific) was inserted on the 12th postoperative<br />
week, endoscopically. During the follow-up period he was<br />
able to eat normally and maintain his weight. He survived<br />
for 3 years and finally died <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> a severe depression disorder.<br />
Patient 2<br />
A 32-year-old man, with no history <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> previous illness<br />
but with an ambiguous reference to recent food and drink<br />
overindulgence, was presented to a peripheral Hospital<br />
Emergency department complaining <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the sudden onset<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> gradually increasing, lower thorax post emetic pain and<br />
subcutaneous emphysema. The suspicion <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> spontaneous<br />
esophageal rupture was confirmed on a subsequent erect<br />
x-ray film, CT scan and esophagogram by the presentation<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> bilateral pleural effusion together with left sided contrast<br />
extravasation f<strong>ro</strong>m the lower third <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus (Fig.2).<br />
Fig.2 Patient 2. Esophagogram depicting a leftsided<br />
leak.<br />
Bilateral thoracotomies, closure <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophageal<br />
perforation in two layers, buttress <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the defect with viable<br />
regional pleural flap and placement <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> chest tubes were<br />
performed. Subsequently, the patient was transferred to<br />
our department because <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> lack <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> ICU. On postoperative<br />
day 8, the patient demonstrated clinical signs <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> a recurrent<br />
leak, with recrudescing systemic sepsis, dyspnea, and<br />
hemodynamic instability. The subsequent CT scan study<br />
demonstrated contrast medium extravasation accompanied<br />
with large pleural effusion bilaterally. Re-operation was<br />
considered inevitable, during which mediastinum and pleural<br />
debridement, forcible irrigation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> pleural spaces, cervical<br />
esophagostomy in combination with closure <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the distal<br />
esophagus, feeding jejunostomy and draining gast<strong>ro</strong>stomy,<br />
were performed. Postoperatively, thoracotomies were left<br />
opened and continuous irrigation systems were applied to our<br />
patient’s thoracic wounds [6]. The patient had a p<strong>ro</strong>longed<br />
ICU stay, mainly because <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the need for ventilation, as a<br />
result <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> severe pneumonitis, along with relapsing incidences<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> systemic sepsis. Eventually, he was returned to the main<br />
ward on the 5th postoperative week. After a total period <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
14 weeks, the patient was discharged, continuing total enteral<br />
alimentation. Five months later, he underwent reconstruction<br />
by joining the cervical esophagus to the stomach using<br />
ret<strong>ro</strong>sternal left colic flexure based on the left branch <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the<br />
middle colic vessels. He can now eat normally and maintain<br />
his weight and is leading a normal existence.<br />
Patient 3<br />
A 47-year-old man, with no history <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> previous illness,<br />
and with reference to a preceding overindulgence in a<br />
large meal, presented to our Department, complaining <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng>
84 Tsalis et al<br />
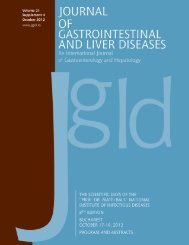
Fig.3 Patient 3. Contrast enhanced CT scan, demonstrating<br />
significant mediastinal free air, and extended left sided<br />
pleural effusion.<br />
the sudden onset <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> a sharp, post emetic, mid epigastric<br />
pain, radiating to the left shoulder. On the basis <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> classic<br />
esophageal rupture history, the diagnosis was readily made<br />
by means <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> erect chest x-ray and CT (Fig.3). A confirmative<br />
subsequent hypaque swallow study demonstrated small<br />
extravasation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> contrast medium f<strong>ro</strong>m a distal esophageal<br />
perforation. After a short resuscitation period, the patient<br />
was transferred to the Operating Theatres, where the<br />
rupture site, located on the left esophageal wall next to the<br />
gast<strong>ro</strong>esophageal junction, was app<strong>ro</strong>ached with midline<br />
lapa<strong>ro</strong>tomy. A primary esophageal closure in two layers with<br />
additional fundoplication was performed. Furthermore, a<br />
small left thoracotomy was performed and the thoracic cavity<br />
was copiously irrigated. Finally the chest was closed with<br />
a large (32-gauge) thoracostomy tube in situ. On the third<br />
postoperative day the patient was returned to the main ward<br />
where repeated esophageal contrast medium studies verified<br />
a successful outcome. On postoperative day 15 the patient<br />
began oral feeding. Five weeks after surgery, the patient was<br />
discharged in good general condition. At the time <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> writing,<br />
6 years after the initial operation, he continues to do well.<br />
Discussion<br />
The presentation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> Boerhaave’s synd<strong>ro</strong>me is usually nonspecific<br />
and may mimic many other clinical disorders [11].<br />
Our diagnostic tools were chest X-ray, CT, esophagography,<br />
and esophagoscopy, but principally a high index <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> suspicion<br />
is required for timely diagnosis. In our cases, CT scans were<br />
done immediately after oral contrast administration, to detect<br />
the level and size <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> perforation and define the sur<strong>ro</strong>unding<br />
tissue inflammation, which helped as in deciding on the most<br />
app<strong>ro</strong>priate therapy [12,13].<br />
The management <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the synd<strong>ro</strong>me remains cont<strong>ro</strong>versial<br />
since treatment can be surgical or non-surgical, and indications<br />
vary according to the functional state <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus, the<br />
presence <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> associated lesions and the habits <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the different<br />
medical teams [1,9,14]. Today, it is accepted that the method<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> treatment plays an important <strong>ro</strong>le in the mortality rate<br />
and although surgery has been the most common app<strong>ro</strong>ach,<br />
the selection criteria for conservative treatment reported by<br />
Altorjay et al [15] (intramural perforation, benign defects,<br />
and the absence <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> sepsis) in 1977, and Came<strong>ro</strong>n et al [16]<br />
in 1979 (disruption contained in the mediastinum; the cavity<br />
draining back into the esophagus; minimal symptoms; and<br />
minimal signs <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> sepsis), are still valid and should be taken<br />
into account. With reference to the above, perforations<br />
and pleural contamination, once cont<strong>ro</strong>lled by adequate<br />
drainage, simply become an esophagocutaneous fistula and<br />
will heal the same as most gast<strong>ro</strong>intestinal fistulas [17].<br />
Recently, some authors claimed that rapid closure <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the<br />
esophageal leak and drainage, could also be achieved by<br />
the minimal invasive endoscopic app<strong>ro</strong>ach by inserting an<br />
endop<strong>ro</strong>sthesis, followed by interventional drainage and/or<br />
thoracoscopic irrigation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the contaminated thoracic cavity<br />
[18-20]. Nevertheless, we believe that this app<strong>ro</strong>ach can be<br />
applied only for iat<strong>ro</strong>genic and early detected perforations.<br />
A self-expandable covered metallic esophageal stent<br />
was placed in one <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> our patients in order to treat a distal<br />
esophageal post perforation stricture. Esophageal stenting<br />
for non-malignant strictures is cont<strong>ro</strong>versial. The covered<br />
self-expanding metallic stent was originally used for the<br />
stricture or fistula caused by malignant diseases [18]. On the<br />
other hand, many authors investigated the application <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> this<br />
alternative method to the management <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> benign conditions<br />
[21]. In our case, stent placement was used mainly because<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the patient’s refusal for further invasive p<strong>ro</strong>cedure, as well<br />
as considering his moderate medical condition.<br />
There is still cont<strong>ro</strong>versy about the most app<strong>ro</strong>priate<br />
type <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> surgery for patients with esophageal perforation.<br />
Some surgeons performed primary repair, regardless <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the<br />
interval between the perforation and intervention, resulting<br />
in a diverse outcome [8,10]. Our opinion on primary<br />
repair is that it is better to be avoided in delayed patients.<br />
Conversely, if the inflammatory p<strong>ro</strong>cess is limited, primary<br />
repair is a reasonable option and may result in an excellent<br />
outcome [10]. Some others suggest that esophagectomy<br />
may be better f<strong>ro</strong>m primary repair for patients with delayed<br />
perforation, because <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the high risk <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> leakage [1,22].<br />
We believe that primary reconstruction must be the first<br />
treatment option in stable, nonseptic patients. Debridement<br />
and drainage with or without continuous lavage [23, 24] is<br />
another option, especially if the patient’s general condition<br />
is impaired or p<strong>ro</strong>gressive sepsis is apparent. We applied this<br />
method in one <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> our patients with satisfactory results. If the<br />
interval between injury and intervention exceeds 24h or CT<br />
shows signs <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> p<strong>ro</strong>gressive periesophageal inflammation,<br />
reinforcement <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophageal repair by viable regional<br />
tissue is recommended [11].<br />
If delayed reconstruction is being considered, it is<br />
possible to bring up the stomach, the small intestine or<br />
the colon to join the cervical esophagus. The timing <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
reconstruction must be based on the patient’s condition or/and<br />
recovery. Reconstruction <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus can be performed<br />
simultaneously if there is no severe systemic inflammatory<br />
response. Otherwise, delayed reconstruction (2-4 months)<br />
is possibly the best option [1]. The new esophagus can be
Boerhaave’s synd<strong>ro</strong>me 85<br />
placed in the posterior mediastinum or in the ret<strong>ro</strong>sternal<br />
or subcutaneous positions. In patient 2 delayed esophageal<br />
reconstruction was performed with colonic graft positioned<br />
ret<strong>ro</strong>sternally in order to achieve a better cosmetic result.<br />
All our patients were surgically treated after resuscitative<br />
measures such as fluids and antibiotics. Our intention<br />
was to prevent ongoing spoilage, to p<strong>ro</strong>vide debridement<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> devitalized tissue and to perform wide drainage.<br />
Postoperatively, all patients received supportive management<br />
including nasogastric tube decompression <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the stomach,<br />
b<strong>ro</strong>ad-spectrum antibiotic administration, and nutrition.<br />
In conclusion, without treatment, patients with esophageal<br />
rupture frequently die <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> mediastinitis. Because <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the very<br />
small numbers <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> cases, no standard therapy has been<br />
established. Conservative treatment remains a cont<strong>ro</strong>versial<br />
topic, although recent sporadic reports have documented<br />
the efficacy <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> nonoperative care, especially following<br />
perforations in nonseptic patients. Primary suturing <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the<br />
esophagus should be performed only in patients with an<br />
early perforation. When ongoing mediastinitis and pleural<br />
contamination has occurred, only esophageal exclusion or<br />
resection can definitely eliminate the source <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> intrathoracic<br />
sepsis.<br />
References<br />
1. Huber-Lang M, Henne–Bruns D, Schmitz B, Wuerl P. Esophageal<br />
perforation: principles <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> diagnosis and surgical management. Surg<br />
Today 2006; 36:332-340.<br />
2. Lawrence DR, Ohri SK, Moxon RE, Townsend ER, Fountain SW.<br />
Primary esophageal repair for Boerhaave’s synd<strong>ro</strong>me. Ann Thorac<br />
Surg 1999; 67:818-812.<br />
3. Mackler SA. Spontaneous rupture <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus; an experimental<br />
and clinical study. Surg Gynecol Obstet 1952; 95:345-356.<br />
4. Pate JW, Walker WA, Cole FH Jr, Owen EW, Johnson WH.<br />
Spontaneous rupture <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the esophagus: a 30-year experience. Ann<br />
Thorac Surg 1989; 47: 689-692.<br />
5. Hafer G, Haunhorst WH, Stallkamp B. Atraumatic rupture <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> the<br />
esophagus (Boerhaave synd<strong>ro</strong>me). Zentralbl Chir 1990; 115: 729-<br />
735.<br />
6. XWitte J, Pratschke E. Esophageal perforation. In: Baue A D,<br />
ed. Glenn’s Thoracic and Cardiovascular Surgery. Norwalk, CT:<br />
Appleton and Lange, 1991: 669.<br />
7. Lundell L, Liedman B, Hyltander A. Emergency oeso-phagectomy<br />
and p<strong>ro</strong>ximal deviating oesophagostomy for fulminent mediastinal<br />
sepsis. Eur J Surg 2001; 167:675-678.<br />
8. Sung SW, Park JJ, Kim YT, Kim JH. Surgery in thoracic esophageal<br />
perforation: primary repair is feasible. Dis Esophagus 2002; 15:204-<br />
209.<br />
9. Ökten I, Cangir AK, Özdemir N, Kavukcu S, Akay H, Yavuzer S.<br />
<st<strong>ro</strong>ng>Management</st<strong>ro</strong>ng> <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> esophageal perforation. Surg Today 2001; 31:36-<br />
39.<br />
10. Port JL, Kent MS, Korst RJ, Bacchetta M, Altorki NK. Thoracic<br />
esophageal perforations: a decade <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> experience. Ann Thorac Surg<br />
2003; 75:1071-1074.<br />
11. Henderson JA, Peloquin AJ. Boerhaave revisited: spontaneous<br />
esophageal perforation as a diagnostic masquerader. Am J Med 1989;<br />
86:559-567.<br />
12. Akman C, Kantarci F, Cetinkaya S. Imaging in mediastinitis: a<br />
systematic review based on aetiology. Clin Radiol 2004; 59:573-<br />
585.<br />
13. Fadoo F, Ruiz DE, Dawn SK, Webb WR, Gotway MB. Helical<br />
CT esophagography for the evaluation <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> suspected esophageal<br />
perforation. AJR Am J Roentgenol 2004; 182:1177-1179.<br />
14. Chao YK, Liu YH, Ko PJ, et al. Treatment <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> esophageal perforation<br />
in a referral center in taiwan. Surg Today 2005; 35:828-832.<br />
15. Altorjay A, Kiss J, Vörös A, Sziranyi E. The <strong>ro</strong>le <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> esophagectomy in<br />
the management <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> esophageal perforations. Ann Thorac Surg 1998;<br />
65:1433-1436.<br />
16. Came<strong>ro</strong>n JL, Kieffer RF, Hendrix TR, Mehigan DG, Baker RR.<br />
Selective nonoperative management <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> contained intrathoracic<br />
esophageal disruptions. Ann Thorac Surg 1979; 27: 404-408.<br />
17. Lawrence DR, Moxon RE, Fountain SW, Ohri SK, Townsend ER,.<br />
Iat<strong>ro</strong>genic oesophageal perforations: a clinical review. Ann R Coll<br />
Surg Engl 1998; 80:115-118.<br />
18. Fischer A, Thomusch O, Benz S, von Dobschuetz E, Baier P,<br />
Hopt UT. Nonoperative treatment <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> 15 benign esophageal<br />
perforations with self-expandable covered metal stents.<br />
Ann Thorac Surg 2006; 81:467-472.<br />
19. Radecke K, Gerken G, Treichel U. Impact <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> a self-expanding,<br />
plastic esophageal stent on various esophageal stenoses, fistulas,<br />
and leakages: a single-center experience in 39 patients. Gast<strong>ro</strong>intest<br />
Endosc 2005; 61:812-818.<br />
20. Gelbmann CM, Ratiu NL, Rath HC, et al. Use <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> self-expandable<br />
plastic stents for the treatment <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> esophageal perforations and<br />
symptomatic anastomotic leaks. Endoscopy 2004; 36:695-699.<br />
21. Sheikh RA, Trudeau WL. Expandable metallic stent placement<br />
in patients with benign esophageal strictures: results <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> long-term<br />
follow-up. Gast<strong>ro</strong>intest Endosc 1998; 48: 227-229.<br />
22. Attar S, Hankins JR, Suter CM, Coughlin TR, Sequeira A, McLaughlin<br />
JS. Esophageal perforation: a therapeutic challenge. Ann Thorac Surg<br />
1990; 50: 45-49.<br />
23. Rao KV, Mir M, Cogbill CL. <st<strong>ro</strong>ng>Management</st<strong>ro</strong>ng> <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> perforations <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
the thoracic esophagus: a new technic utilizing a pedicle flap <st<strong>ro</strong>ng>of</st<strong>ro</strong>ng><br />
diaphragm. Am J Surg 1974; 127: 609-612.<br />
24. Grillo HC, Wilkins EW Jr. Esophageal repair following late diagnosis<br />
<st<strong>ro</strong>ng>of</st<strong>ro</strong>ng> intrathoracic perforation. Ann Thorac Surg 1975; 20: 387-399.