MAKETA 5/3
MAKETA 5/3
MAKETA 5/3
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A C T A M E D I C A M A R T I N I A N A 2 0 0 5 5/3 11<br />
IAP and its duration, blood cell count at birth and after the third dose of postnatal penicillin, clinical<br />
signs, amniotic water culture and newborn’s outer ear canal culture results.<br />
The study is prospective. The pilot study was started in September 2004, and in July 2005<br />
the study sample consisted of 100 newborns. The study group accounts for 11.3 % of all fullterm<br />
infants born within that time period. The mean birth weight of the study group was 3. 394<br />
grams (± SD = 490 grams). The mean gestational age was 40.2 gestational weeks (± SD = 1.1<br />
weeks). Postnatal adaptation of the newborns was adequate, only in one infant with Apgar score<br />
5/7/8 it was more difficult.<br />
RESULTS<br />
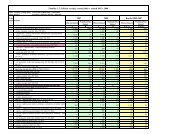
There were 11.3 % of all full-term newborns born to GBS colonized mothers. Firstly, we<br />
assess the risk for GBS sepsis according to the Swiss Society of Neonatology. Full-term infants<br />
of GBS colonized mothers, without any additional risk factors and without IAP, are considered<br />
at risk for GBS sepsis 6 / 1, 000. If there are any additional risk factors, the risk grows 12.5<br />
times. If duration of IAP is longer than 4 hours, it reduces the risk 33 times (the risk is<br />
0.18 / 1 000) (14). It is not known how much postnatal antimicrobial prophylaxis reduces the risk<br />
for the disease. In our study group there were 73 newborns at risk for sepsis 6 / 1 000. Twenty<br />
two neonates were at risk 0.18 / 1 000, because of administration of IAP. There were 4 neonates<br />
at risk 2.25 / 1 000, because of additional risk factors and IAP at the same time. Only one newborn<br />
was at risk 75 / 1 000, because of prolonged rupture of membranes and unsatisfactory<br />
duration of IAP. In this infant, to whom PAP was not administered because of adequate blood<br />
count, there were no signs of infection found and there were negative culture results. (Fig.1)<br />
Fig. 1 Distribution of risk for GBS sepsis in the study group<br />
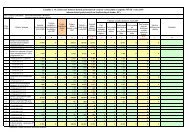
Out of 100 infants, PAP was administered in 9 cases. In 8 cases the indication criteria included<br />
leucocytosis, in 1 case it included additional risk factors such as prolonged rupture of membranes<br />
and intrapartum fever in mother (Fig.2). In 8 newborns, the total number of leucocytes<br />
went back to normal after three doses of penicillin. In 1 newborn the PNP had to be prolonged.<br />
Out of the 9 newborns with PNP, in 5 of their mothers was not administered any IAP. According<br />
to our criteria, PAP was administered to 4 infants, although their mothers received ampicillin<br />
prophylaxis and the infants were at risk 0.18 / 1000 (Fig.3). We keep in mind that IAP does not<br />
prevent all EOGBSD cases.