Laboratory testing for bleeding disorders: Strategic uses of high and ...
Laboratory testing for bleeding disorders: Strategic uses of high and ...
Laboratory testing for bleeding disorders: Strategic uses of high and ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Laboratory</strong> <strong>testing</strong> <strong>for</strong> <strong>bleeding</strong> <strong>disorders</strong>:<br />
<strong>Strategic</strong> <strong>uses</strong> <strong>of</strong> <strong>high</strong> <strong>and</strong> low yield tests<br />
Catherine P. M. Hayward, MD PhD, FRCP(C)<br />
Head, Coagulation, Hamilton Regional <strong>Laboratory</strong> Medicine Program<br />
Pr<strong>of</strong>essor, Pathology <strong>and</strong> Molecular Medicine<br />
McMaster University, Hamilton, Ontario, Canada
Disclosures <strong>and</strong> Acknowledgments<br />
<strong>for</strong> Catherine P. M. Hayward<br />
• Nothing to disclose<br />
• Acknowledgment <strong>of</strong> materials from:<br />
1) Hayward, M<strong>of</strong>fat. Int J Lab Hematol. 2013 epub Mar 11<br />
2) Hayward, M<strong>of</strong>fat, Liu. STH 2012;38(7):742-52.<br />
3) Hayward, M<strong>of</strong>fat, Plumh<strong>of</strong>f, Timleck, H<strong>of</strong>fman,<br />
Spitzer, Van Cott, Meijer. STH 2012;38(6):622-31<br />
4) Other sources cited in slides
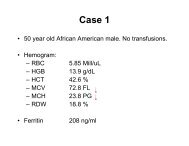
Illustrative Case<br />
• 51 year old male<br />
• Recent severe, unexplained retroperitoneal<br />
bleed (ICU stay) + many serious <strong>bleeding</strong><br />
episodes (all delayed in onset) when challenged<br />
previously.<br />
• Prior referrals to 5 hematologists, who excluded:<br />
▫ Hemophilia, other factor deficiencies (including<br />
factor XIII <strong>and</strong> fibrinogen <strong>disorders</strong>) <strong>and</strong> von<br />
Willebr<strong>and</strong> disease<br />
• What tests should be ordered now?
Perspectives on Bleeding Disorder Diagnosis<br />
• <strong>Laboratory</strong> tests are essential <strong>for</strong> diagnosis<br />
• Tests <strong>and</strong> panels <strong>of</strong>fered by labs are not<br />
st<strong>and</strong>ardized<br />
▫ Most <strong>of</strong>fer coagulation screening tests in <strong>bleeding</strong><br />
disorder panels, without complete <strong>testing</strong> <strong>for</strong> more<br />
common defects in primary hemostasis<br />
▫ Few <strong>of</strong>fer tests <strong>for</strong> rare <strong>bleeding</strong> <strong>disorders</strong><br />
• Strategies to guide investigations (including<br />
when to order tests <strong>for</strong> rare <strong>bleeding</strong> <strong>disorders</strong>)<br />
are rarely provided by laboratories
Coagulation Screening Tests in<br />
Bleeding Disorder Investigations<br />
• Detect some important <strong>disorders</strong><br />
• Problems:<br />
▫ False positives <strong>and</strong> false negatives do occur<br />
▫ More specific tests (e.g., factor assays) are required to:<br />
• Detect mild factor deficiencies<br />
including hemophilias from unstable factor VIII<br />
• Further assess abnormalities
Tests <strong>for</strong> Defects in Primary Hemostasis<br />
• Much greater sensitivity <strong>for</strong> common <strong>bleeding</strong><br />
<strong>disorders</strong> than coagulation screening tests<br />
• Pitfalls:<br />
▫ “Undefined <strong>bleeding</strong> <strong>disorders</strong>”<br />
• Similar <strong>bleeding</strong> history to von Willebr<strong>and</strong> disease<br />
<strong>and</strong> platelet function <strong>disorders</strong> but normal test<br />
findings<br />
▫ Criteria used to define “abnormal”<br />
• e.g., Cut<strong>of</strong>fs <strong>for</strong> von Willebr<strong>and</strong> disease screens
Tests <strong>for</strong> Other Bleeding Disorders<br />
• Essential to diagnose some conditions,<br />
particularly those with delayed-onset <strong>bleeding</strong>,<br />
such as:<br />
▫ Factor XIII deficiency<br />
▫ α2 antiplasmin deficiency<br />
▫ Plasminogen activator inhibitor-1 deficiency<br />
▫ Quebec platelet disorder
Other Considerations: Pretest Probabilities<br />
• Patients in preoperative clinics<br />
▫ Low pretest probability <strong>for</strong> a <strong>bleeding</strong> disorder<br />
• Patients seen <strong>for</strong> <strong>bleeding</strong> disorder evaluation<br />
▫ Much more likely to have a <strong>bleeding</strong> disorder<br />
• Family history <strong>of</strong> <strong>bleeding</strong> disorder<br />
▫ Relatives are at <strong>high</strong>er risk<br />
• Population/social factors<br />
▫ Affect <strong>bleeding</strong> disorder prevalence<br />
▫ Consanguinity: culturally accepted in some populations<br />
‣Higher prevalence <strong>of</strong> rare <strong>bleeding</strong> <strong>disorders</strong>
Other Considerations: Abnormalities Can Reflect<br />
• Age related changes in hemostasis<br />
• False positives or true positives that are not<br />
clinically important (e.g., contact pathway factor<br />
deficiency)<br />
• True positives from drugs (e.g., anticoagulants,<br />
drugs that inhibit platelet function)<br />
• True positives from clinically important,<br />
congenital or acquired <strong>bleeding</strong> problems<br />
• ADDITIONAL CHALLENGE: interpretation
CAUSE AND PATTERN OF ABNORMALITIES PT/INR APTT TT FIBRINOGEN<br />
Fibrinogen deficiency (hyp<strong>of</strong>ibrinogenemia) or dysfunction<br />
(dysfibrinogenemia)<br />
N – ↑ N – ↑ ↑ ↓<br />
Afibrinogenemia NC NC NC ND<br />
FVII deficiency ↑ N N N<br />
FVIII, FIX , <strong>and</strong>/or FXI deficiency N ↑ N N<br />
Acquired or congenital hemophilia, with an inhibitor N ↑ † N N<br />
FII, FV, <strong>and</strong>/or FX deficiency ↑ ↑ N N<br />
Factor deficiencies not associated with <strong>bleeding</strong> (FXII, <strong>high</strong> molecular<br />
weight kininogen or prekallikrein deficiency)<br />
N ↑ N N<br />
Lupus anticoagulant N – ↑ N – ↑ ‡ N N<br />
Lupus anticoagulant with FII deficiency ↑ ↑ N – ↑ N<br />
Unfractionated heparin - therapy or sample contamination N – ↑ ↑ ↑↑ * N<br />
Low molecular weight heparin therapy N N – ↑ N – ↑ N<br />
Direct thrombin inhibitors N – ↑ N – ↑ ↑↑ N<br />
Direct inhibitors <strong>of</strong> FXa N – ↑ N – ↑ N N<br />
Liver disease † (if early, <strong>of</strong>ten affects FVII, FXI <strong>and</strong>/or FXII; if late or end<br />
stage, fibrinogen is usually low; spares FVIII but can affect all other<br />
factors)<br />
N – ↑ N – ↑ N – ↑ ↓ - N – ↑<br />
Vitamin K deficiency (or treatment with a vitamin K antagonist) which<br />
reduce levels <strong>of</strong> FVII <strong>and</strong> also FII, FIX <strong>and</strong> FX †<br />
↑ N – ↑ N N<br />
Fibrinolytic therapy ↑ ↑ ↑ ↓<br />
Consumptive coagulopathy † N – ↑ ↑ N – ↑ N – ↓<br />
Dilutional coagulopathy † N – ↑ N – ↑ N – ↑ ↓ - N<br />
VWD N N – ↑ N N<br />
Preanalytical error – collected in potassium EDTA § ↑ ↑ N – ↑ N<br />
Preanalytical error – serum instead <strong>of</strong> plasma NC NC NC ND<br />
N, normal; NC, no clot; ND, not detected
Evidence on Test Sensitivity <strong>and</strong> Specificity <strong>for</strong><br />
Bleeding Disorder Investigation?<br />
• Recent research<br />
▫ Hamilton Regional <strong>Laboratory</strong> Medicine Program<br />
(HRLMP)<br />
• Center that tests local <strong>and</strong> referred samples <strong>for</strong> common <strong>and</strong><br />
rare <strong>bleeding</strong> <strong>disorders</strong><br />
• Approach<br />
▫ 1) Estimated sensitivities <strong>and</strong> specificities <strong>of</strong> lab tests<br />
<strong>for</strong> <strong>bleeding</strong> disorder diagnosis from a prospective<br />
cohort study (Hayward, M<strong>of</strong>fat, Liu. STH 2012;38(7):742-52)<br />
▫ 2) Assessed findings <strong>for</strong> rare <strong>bleeding</strong> disorder tests by<br />
a retrospective review <strong>of</strong> records (Jan 2003- Dec 2012;<br />
Hayward, M<strong>of</strong>fat. IJLH current issue)
Sensitivity <strong>and</strong> Specificity <strong>for</strong> Bleeding Disorders<br />
st<strong>and</strong>ard investigations done so this comparative analysis was possible<br />
Hayward, M<strong>of</strong>fat, Liu. Semin Thromb Hemost. 2012;38(7):742-52<br />
Test Sensitivity Specificity<br />
APTT 3.1% 98%<br />
PT/INR 0.5% 100%<br />
Fibrinogen 1.0% 100%<br />
Thrombin Time 1.0% 98%<br />
VWD Screen 6.0% 98%<br />
LTA* 25.7% 98%<br />
*LTA per<strong>for</strong>med <strong>and</strong> interpreted in accordance with North American Guidelines<br />
Hayward et al, Am J Clin Pathol 2010;134:955-963
Test<br />
APTT<br />
PT/INR<br />
Factor<br />
assays &<br />
factor<br />
inhibitors<br />
Abnormalities associated<br />
with <strong>bleeding</strong><br />
Congenital or acquired<br />
deficiencies <strong>of</strong> intrinsic<br />
(FVIII, FIX <strong>and</strong> FXI) <strong>and</strong><br />
common pathway factors<br />
(FII, FV <strong>and</strong> FX) that cause<br />
<strong>bleeding</strong><br />
Congenital or acquired<br />
deficiencies <strong>of</strong> factor VII<br />
<strong>and</strong> common pathway<br />
factors (FII, FV, <strong>and</strong> FX)<br />
Congenital <strong>and</strong> acquired<br />
deficiencies <strong>of</strong> coagulation<br />
factors II, V, VII, VIII, IX, X<br />
<strong>and</strong> XI.<br />
Practice Points<br />
Abnormalities<br />
unrelated to <strong>bleeding</strong><br />
(excl. preanalytical)<br />
Contact factor<br />
deficiencies (FXII,<br />
prekallikrein, <strong>high</strong><br />
molecular weight<br />
kininogen) <strong>and</strong> most<br />
lupus anticoagulants<br />
Considerations<br />
• Most abnormalities are not<br />
clinically significant<br />
• Does not detect some mild factor<br />
deficiencies <strong>and</strong> most fibrinogen<br />
<strong>disorders</strong><br />
• Requires follow up factor assays<br />
• Does not detect some mild factor<br />
deficiencies <strong>and</strong> most fibrinogen<br />
<strong>disorders</strong><br />
• Requires follow up factor assays<br />
• Anticoagulants <strong>and</strong> lupus<br />
anticoagulants can interfere<br />
• Two stage (or chromogenic)<br />
assays may be required to detect<br />
hemophilia due to unstable FVIII<br />
• Unknown sensitivity/specificity
Practice Points<br />
Test<br />
Thrombin<br />
time (TT)<br />
Abnormalities<br />
associated with <strong>bleeding</strong><br />
Congenital <strong>and</strong> acquired<br />
defects in fibrinogen<br />
(quantitative <strong>and</strong><br />
qualitative) <strong>and</strong> fibrin<br />
polymerization, including<br />
elevated fibrin(ogen)<br />
degradation products<br />
Abnormalities<br />
unrelated to<br />
<strong>bleeding</strong><br />
Valproic acid therapy<br />
<strong>and</strong> some<br />
paraproteins can<br />
prolong the test, as<br />
does heparin <strong>and</strong><br />
direct thrombin<br />
inhibitors<br />
Considerations<br />
• Correlate with fibrinogen level<br />
• Measure fibrinogen antigen <strong>and</strong><br />
reptilase times if a congenital<br />
defect is suspected<br />
• Acquired abnormalities are more<br />
common<br />
Clauss<br />
fibrinogen<br />
Quantitative<br />
(afibrinogenemia,<br />
hyp<strong>of</strong>ibrinogenemia) <strong>and</strong><br />
qualitative<br />
(dysfibrinogenemia)<br />
defects in fibrinogen<br />
_<br />
• Correlate with thrombin time<br />
• To distinguish quantitative from<br />
qualitative defects, consider <strong>testing</strong><br />
TT <strong>of</strong> control diluted to the same<br />
fibrinogen level<br />
• If abnormal, <strong>and</strong> congenital<br />
deficiency is suspected, test<br />
fibrinogen antigen, TT <strong>and</strong> reptilase<br />
times
Illustrative Findings: Fibrinogen Disorders<br />
From Verhovsek, M<strong>of</strong>fat, Hayward. Am J Hematol 2008;83(12):928-31<br />
Test RI Hyp<strong>of</strong>ibrinogenemia Dysfibrinogenemia Afibrinogenemia<br />
Clinical problem<br />
Recurrent pregnancy<br />
loss from abruptions<br />
without any other<br />
<strong>bleeding</strong> symtoms<br />
Menorrhagia, PPH<br />
requiring transfusion.<br />
Intracranial<br />
hemorrhage,<br />
traumatic & surgical<br />
<strong>bleeding</strong><br />
PT 11-14 s 14.2 13.0 No Clot<br />
INR 0.8-1.2 1.2 1.1 No Clot<br />
APTT 22-35 s 32 33 No Clot<br />
TT 20-30 s 46 122 No Clot<br />
Reptilase time<br />
15-27 s<br />
Clauss Fbgn<br />
1.6-4.2 g/L<br />
Fbgn antigen<br />
1.6-4.2 g/L<br />
33 40 >60<br />
0.6 1.2
Test<br />
VWD Screen<br />
(FVIII,<br />
VWF:Ag,<br />
VWF:RCo;<br />
multimers if<br />
abn. found)<br />
LTA<br />
Abnormalities<br />
associated<br />
with <strong>bleeding</strong><br />
Congenital <strong>and</strong><br />
acquired VWD<br />
Congenital <strong>and</strong><br />
acquired<br />
platelet<br />
function<br />
defects<br />
Practice Points<br />
Abnormalities<br />
unrelated to<br />
<strong>bleeding</strong><br />
Low VWF:RCo in<br />
some African<br />
Americans with<br />
polymorphisms that<br />
don’t impair VWFplatelet<br />
receptor<br />
interactions<br />
Single agonist<br />
abnormalities are<br />
<strong>of</strong>ten false positives<br />
(exceptions:<br />
collagen, ristocetin)<br />
Considerations<br />
• Cut<strong>of</strong>fs used in practice vary,<br />
which influences the<br />
sensitivity <strong>and</strong> specificity<br />
• Levels influenced by age,<br />
blood group, menstrual<br />
cycle, oral contraceptives,<br />
exercise, illness <strong>and</strong> stress<br />
• Normal in some platelet<br />
<strong>disorders</strong> (including some<br />
dense granule deficiencies<br />
<strong>and</strong> release defects)<br />
• May be falsely normalized<br />
by lumiaggregometry<br />
reagent
Practice Points<br />
Test<br />
Lumiaggregometry<br />
assay <strong>of</strong><br />
platelet dense<br />
granule ATP<br />
release<br />
Electron<br />
microscopy <strong>for</strong><br />
platelet dense<br />
granule<br />
deficiency<br />
Abnormalities<br />
associated with<br />
<strong>bleeding</strong><br />
Congenital <strong>and</strong><br />
acquired defects<br />
in dense granule<br />
release, a<br />
common type <strong>of</strong><br />
platelet function<br />
disorder<br />
Congenital <strong>and</strong><br />
acquired platelet<br />
dense granule<br />
deficiency<br />
Abnormalities<br />
unrelated to<br />
<strong>bleeding</strong><br />
False positives<br />
can reflect<br />
preanalytical<br />
errors<br />
False positives<br />
are rare <strong>and</strong><br />
can reflect<br />
preanalytical<br />
errors<br />
(platelet<br />
activation)<br />
Considerations<br />
• Usually a secondary<br />
investigation<br />
• Release with weak agonists is<br />
variable<br />
• Reagent can falsely normalize<br />
some aggregation findings<br />
• Sensitivity <strong>and</strong> specificity <strong>for</strong><br />
<strong>bleeding</strong> <strong>disorders</strong> not reported<br />
• Usually a secondary<br />
investigation<br />
• Detects only one kind <strong>of</strong><br />
platelet disorder<br />
• We test if dense granule release<br />
is reduced with strong agonists<br />
• Specificity >99%, sensitivity <strong>for</strong><br />
<strong>bleeding</strong> <strong>disorders</strong> not reported
Realities <strong>of</strong> Practice<br />
• Laboratories have greater difficult with aggregometry<br />
interpretation than with assessing findings <strong>of</strong> electron<br />
microscopy tests <strong>for</strong> platelet dense granule deficiency<br />
• Per<strong>for</strong>mance is particularly problematic <strong>for</strong> interpreting<br />
common aggregation abnormalities<br />
Hayward, M<strong>of</strong>fat, Plumh<strong>of</strong>f, Timleck, H<strong>of</strong>fman, Spitzer, Van Cott,<br />
Meijer. STH 2012;38(6):622-31
Test<br />
Sensitivities <strong>and</strong> Specificities<br />
Comparisons <strong>of</strong> Bleeding Disorder Panels<br />
Hayward, M<strong>of</strong>fat, Liu. STH 2012;38(7):742-52<br />
Sensitivity Specificity<br />
APTT, PT/INR, Fibrinogen, Thrombin Time 3.0% 98%<br />
APTT, PT/INR, Fibrinogen, Thrombin Time<br />
& VWD Screen<br />
APTT, PT/INR, Fibrinogen, Thrombin Time,<br />
VWD Screen & LTA<br />
7.8% 95%<br />
29% 93%<br />
Practice points:<br />
1. Tests <strong>for</strong> primary hemostatic defects are needed <strong>for</strong> the panel to have<br />
reasonable detection <strong>of</strong> common <strong>bleeding</strong> problems (factor deficiencies are<br />
important but less common)<br />
2. Some <strong>disorders</strong> are diagnosed without these tests (e.g. aspirin-induced<br />
<strong>bleeding</strong>, ITP, etc.) or by other tests (e.g., <strong>disorders</strong> <strong>of</strong> fibrinolysis)<br />
3. Doing VWD screens <strong>and</strong> LTA at the same time reduced false negatives
55 year old lady, very positive <strong>bleeding</strong> history & two<br />
children with VWD confirmed by genetic <strong>testing</strong><br />
Patient<br />
RI<br />
PT/INR 1.1 INR 0.8 – 1.2 INR<br />
APTT 33 sec 22 – 35 s<br />
Factor VIII 0.80 U/mL 0.50 – 1.50 U/mL<br />
VWF:RCo 0.59 U/mL 0.50 – 1.50 U/mL<br />
VWF:Ag 0.61 U/mL 0.50 – 1.50 U/mL<br />
VWF multimers<br />
Normal<br />
distribution
LTA findings<br />
%MA %MA<br />
Patient RI<br />
ADP 2.5 µM 31 >24<br />
ADP 5.0 µM 87 >43<br />
Collagen 1.25 µg/mL 87 >51<br />
Collagen 5.0 µg/mL 89 >85<br />
Epinephrine 6 µM 91 >9<br />
Arachidonic Acid 1.6 mM 88 >77<br />
Thromboxane analogue U46619 1 µM 89 >70<br />
Ristocetin 0.5 mg/mL 82/84/80 75<br />
Type 2B VWD confirmed by genetic <strong>testing</strong>
Test<br />
Tests <strong>for</strong> Rare Bleeding Disorders<br />
% abnormal among<br />
evaluated patients<br />
Practice Points<br />
Quantitative<br />
factor XIII<br />
activity assays<br />
Factor XIII<br />
antigen assays<br />
comments<br />
• Low in 12.7%<br />
patients evaluated<br />
by HRLMP<br />
• Lowest in severe<br />
FXIII deficiency<br />
(congenital <strong>and</strong><br />
acquired cases)<br />
• Common: mild<br />
deficiencies in sick,<br />
hospitalized<br />
patients<br />
• A subunit antigen<br />
results show strong<br />
correlation with<br />
activity<br />
• No sample blank in kit; most samples with<br />
0.07-0.13 U/ml (lower RI limit: 0.60 U/ml)<br />
had undetectable FXIII by urea clot solubility<br />
• Useful to follow therapy (e.g., with<br />
pregnancy, surgical interventions).<br />
• Detects some mild deficiencies (e.g., carriers<br />
among relatives <strong>of</strong> severe deficient patients)<br />
missed by clot solubility assays<br />
• CAUTION: mild deficiencies in sick<br />
hospitalized patients do not appear to be<br />
predictive <strong>of</strong> <strong>bleeding</strong><br />
• Most assays measure A subunit (B subunit<br />
assays are presently not available)<br />
• Subunit A (enzymatic) >>>> subunit B<br />
deficiency (no known B subunit deficient<br />
patients in Canada)<br />
• Per<strong>for</strong>m if there is low activity
Factor XIII Antigen Levels<br />
see Poster 349 (board 79) by M<strong>of</strong>fat et al<br />
FXIII subunit B (U/ml)<br />
2.0<br />
1.8<br />
1.6<br />
1.4<br />
1.2<br />
1.0<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
0.0<br />
0.0 0.2 0.4 0.6 0.8 1.0 1.2 1.4 1.6 1.8 2.0<br />
FXIII subunit A (U/ml)<br />
Practice points:<br />
1. Severe deficiency commonly affects subunit A<br />
2. Subunit B can be reduced or normal when subunit A is deficient
FXIII activity (U/ml)<br />
1.8<br />
1.6<br />
1.4<br />
1.2<br />
1.0<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
Factor XIII Activity Compared to Antigen Levels <strong>for</strong> Subunits<br />
see Poster 349 (board 79) by M<strong>of</strong>fat et al<br />
FXIII activity (U/mL)<br />
1.8<br />
1.6<br />
1.4<br />
1.2<br />
1<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
0.0<br />
0.0 0.2 0.4 0.6 0.8 1.0 1.2 1.4 1.6 1.8<br />
FXIII subunit A (U/ml)<br />
0<br />
0 0.2 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8<br />
FXIII subunit B (U/mL)<br />
Practice point:<br />
1. While Factor XIII circulates as a complex <strong>of</strong> A <strong>and</strong> B subunits, subunit A (which is<br />
the enzymatic component) shows stronger correlation with activity than subunit B
Tests <strong>for</strong> Rare Bleeding Disorders<br />
Test<br />
Lower<br />
reference<br />
interval limit<br />
α 2 antiplasmin<br />
(α 2 AP)<br />
0.80 U/mL<br />
% abnormal among evaluated<br />
patients<br />
comments<br />
• Low in 6.4% <strong>of</strong> tested patients<br />
• Lowest: congenital deficiency<br />
(0.18-0.23 U/mL)<br />
• Several suspected heterozygous<br />
deficiencies (milder but<br />
persisting deficiency + delayed<br />
<strong>bleeding</strong> symptoms without<br />
other ca<strong>uses</strong>)<br />
• Many abnormalities reflect<br />
acquired deficiency from<br />
consumption: 0.30-0.79 U/mL<br />
Practice Points<br />
• Homozygous<br />
deficiency: rare<br />
• Heterozygotes: milder,<br />
not all are symptomatic<br />
• Consumed in DIC <strong>and</strong><br />
other conditions with<br />
elevated D-dimer<br />
• No evidence that<br />
measuring α 2 AP is<br />
helpful in consumptive<br />
states
Tests <strong>for</strong> Rare Bleeding Disorders<br />
Disorder or Test<br />
ELT<br />
Euglobulin clot lysis<br />
time<br />
(clot made by adding<br />
thrombin to a<br />
redissolved<br />
precipitate <strong>of</strong> plasma<br />
acid-insoluble<br />
globulin)<br />
% abnormal among<br />
evaluated patients<br />
comments<br />
• Short ELT are not that<br />
common ~1.8% <strong>of</strong> patients<br />
tested; many had a<br />
documented acquired<br />
coagulopathy<br />
Practice Points<br />
• NOT a global test <strong>for</strong> fibrinolytic<br />
<strong>disorders</strong> (e.g., normal in QPD,<br />
α 2 AP deficiency)<br />
• Elevated PAI-1 prolongs ELT<br />
• Should do if: 1) fibrinogen is<br />
normal <strong>and</strong> 2) severe, congenital<br />
PAI-1 deficiency is suspected<br />
• ELT: notably short in severe PAI-1<br />
deficiency (very rare)<br />
Plasmin activator<br />
inhibitor-1 (PAI-1)<br />
assays<br />
• No deficiencies<br />
• Activity: no lower RI limit (assay<br />
designed <strong>for</strong> measuring <strong>high</strong><br />
levels; declining interest in<br />
measuring increased levels)<br />
• Antigen: can help diagnose<br />
deficiencies
Back to Initial Case with an Undiagnosed Bleeding Problem<br />
Result<br />
Reference Interval<br />
Euglobulin clot lysis<br />
time<br />
(assess <strong>for</strong> PAI-1<br />
deficiency)<br />
>6.0 (prolonged) 1.5 – 5.5 hrs<br />
α 2 antiplasmin (α 2 AP) 0.18-0.23<br />
(multiple determinations)*<br />
0.80 – 1.20 U/mL<br />
*His children had asymptomatic, milder α 2 AP deficiency (carriers)<br />
Practice points:<br />
1. Differential diagnosis <strong>of</strong> life long, <strong>bleeding</strong> problems includes<br />
congenital <strong>disorders</strong> <strong>of</strong> fibrinolysis, which should be suspected when<br />
the history indicates delayed-onset <strong>bleeding</strong> after trauma/surgery <strong>and</strong><br />
factor deficiencies have been excluded<br />
2. When making decisions on <strong>testing</strong>, one needs to consider what was<br />
not excluded by prior investigations
Concluding Practice Points<br />
laboratory diagnosis <strong>of</strong> <strong>bleeding</strong> <strong>disorders</strong><br />
• Current tests <strong>for</strong> <strong>bleeding</strong> <strong>disorders</strong> have <strong>high</strong><br />
specificity<br />
• The different sensitivities <strong>of</strong> tests <strong>for</strong> <strong>bleeding</strong><br />
<strong>disorders</strong> reflect differences in disorder<br />
prevalence amongst patients referred <strong>for</strong> <strong>bleeding</strong><br />
assessment<br />
• Some tests are <strong>of</strong> questionable value <strong>for</strong> an<br />
evaluation <strong>of</strong> an acquired coagulopathy<br />
• Consider <strong>testing</strong> strategies, <strong>and</strong> when to order<br />
tests <strong>for</strong> rare <strong>bleeding</strong> <strong>disorders</strong> (e.g., next slide)
Initial Panel <strong>for</strong> Bleeding Disorder Investigations<br />
PT/INR, APTT, TT, fibrinogen, VWD screen, LTA, complete blood count<br />
Coagulation tests abnormal<br />
If fibrinogen <strong>and</strong> TT abnormal,<br />
consider hypo- <strong>and</strong> dysfibrinogenemia,<br />
valproic acid effect, direct thrombin<br />
inhibitor treatment, DIC.<br />
Isolated, abnormal APTT: exclude<br />
clinically significant factor (factors VIII,<br />
IX, <strong>and</strong> XI deficiencies). Consider<br />
other ca<strong>uses</strong>: factor XII deficiency<br />
(other contact factor deficiencies) ,<br />
lupus anticoagulant <strong>and</strong> heparin<br />
If low factor VIII, review VWD screen,<br />
consider inhibitor <strong>testing</strong><br />
PT/INR <strong>and</strong> APTT abnormal: test to<br />
determine if there is single or multiple<br />
factor deficiency (e.g. from vitamin K<br />
deficiency, vitamin K antagonists, liver<br />
disease, combined factor V <strong>and</strong> VIII<br />
deficiency)<br />
Isolated, abnormal PT/INR : test <strong>for</strong><br />
factor VII deficiency (consider<br />
congenital <strong>and</strong> acquired ca<strong>uses</strong> such<br />
as liver disease, early vitamin K<br />
deficiency, early vitamin K<br />
antagonists)<br />
VWD Screen<br />
abnormal, with or<br />
without abnormal<br />
RIPA<br />
Quantitative or<br />
qualitative<br />
abnormality?<br />
Congenital or<br />
acquired?<br />
Review RIPA,<br />
assess multimers<br />
If quantitative,<br />
consider “low VWF”<br />
versus type 1 VWD<br />
If acquired, consider<br />
<strong>testing</strong> <strong>for</strong><br />
hypothyroidism <strong>and</strong> a<br />
monoclonal<br />
gammopathy<br />
LTA abnormal<br />
Review pattern, potential<br />
ca<strong>uses</strong>, including VWD,<br />
common platelet<br />
<strong>disorders</strong> (e.g. secretion<br />
defects, dense granule<br />
deficiency, druginduced)<br />
Consider <strong>testing</strong> <strong>for</strong> a<br />
dense granule release<br />
defect <strong>and</strong> <strong>for</strong> dense<br />
granule deficiency if<br />
release is abnormal<br />
If Glanzmann<br />
thrombasthenia or<br />
Bernard Soulier<br />
syndrome is suspected,<br />
consider glycoprotein<br />
analysis, genetic <strong>testing</strong><br />
If pattern or history<br />
suggests Quebec<br />
platelet disorder,<br />
proceed to genetic<br />
<strong>testing</strong><br />
Hayward, M<strong>of</strong>fat, Liu. Semin Thromb Hemost. 2012;38(7):742-52<br />
Immediate<br />
<strong>bleeding</strong>?<br />
Check <strong>for</strong> dense<br />
granule release<br />
defects/dense<br />
granule deficiency if<br />
release is abnormal<br />
with all agonists<br />
If these tests are<br />
normal, consider<br />
conditions that may<br />
have been missed,<br />
such as Scott<br />
syndrome, MYH9-<br />
related disorder,<br />
etc.<br />
Undefined<br />
disorder?<br />
All test results normal<br />
Delayed <strong>bleeding</strong>?<br />
Mild factor<br />
deficiency or a<br />
fibrinolytic defect?<br />
Factor VIII <strong>and</strong> IX<br />
levels, others if no<br />
cause found<br />
Factor XIII levels<br />
α2-plasmin inhibitor<br />
Euglobulin clot lysis<br />
time (short if severe<br />
PAI-1 deficiency)<br />
Genetic test <strong>for</strong><br />
Quebec platelet<br />
disorder<br />
Factor VIII (two<br />
stage if available)<br />
<strong>and</strong> other factor<br />
assays to exclude a<br />
mild factor<br />
deficiency that<br />
might have been<br />
missed by<br />
coagulation<br />
screening tests