What's In a Red Blood Cell?
What's In a Red Blood Cell?
What's In a Red Blood Cell?
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The Laboratory <strong>In</strong>vestigation of<br />
Hemolytic Anemia : A Logical<br />
Approach<br />
Mr. Andrew McFarlane<br />
Supervisor Genetic Services<br />
Hamilton Regional Laboratory Medicine Program<br />
McMaster University Medical Centre
Conflicts of <strong>In</strong>terest<br />
• Financial Conflicts of <strong>In</strong>terest: NONE<br />
• Non-Financial Conflicts of <strong>In</strong>terest:<br />
NONE<br />
• Unlabelled/ unapproved Use Disclosure:<br />
NONE
Objectives<br />
• Review normal red cell physiology<br />
• Discuss the pathophysiology and<br />
clinical presentation of hemolytic<br />
anemia<br />
• Construct a practical diagnostic<br />
approach to hemolytic anemia
A <strong>Red</strong> <strong>Blood</strong> <strong>Cell</strong><br />
A very flexible and deformable cell able to negotiate the 3 u<br />
sinusoids of the spleen.
What’s <strong>In</strong> A <strong>Red</strong> <strong>Cell</strong>?<br />
<strong>In</strong>trinsic Components<br />
‣ Phospholipid Membrane<br />
connected to<br />
‣ Protein cytoskeleton<br />
contains<br />
‣ Hemoglobin
Life Cycle of an RBC<br />
~120 days<br />
GLUCOSE<br />
ANTIOXIDANT<br />
PROTECTION<br />
METHEMOGLOBIN<br />
REDUCTION<br />
4-6 days 3 days Glycolysis<br />
HEMOGLOBIN<br />
FUNCTION<br />
MEMBRANE<br />
iNTEGRITY
Normal erythrocyte destruction<br />
120 days<br />
1% of RBCs destroyed<br />
every day<br />
Reticulocytes produced to<br />
replace RBCs
Hemolysis<br />
• Heme is Greek for “blood”.<br />
• Lysis means “Break down” in Greek.<br />
• Hemolysis is the end stage of the<br />
erythrocyte 120 life span which occurs<br />
normal in the Reticulo Endothelial System<br />
(RES) of the spleen.
Why do we see overt hemolysis?<br />
Extracorpuscular defects<br />
-acquired hemolysis<br />
• ANTIBODIES against RBC<br />
membrane (e.g., AIHA, DHTR,<br />
some drug-induced anemias)<br />
• SPLENIC TRAPPING<br />
• TRAUMA (e.g. MAHA,<br />
thermal burns)<br />
• OXIDANT exposure (e.g.,<br />
aniline dyes, dapsone,<br />
pyridium)<br />
• PATHOGEN destruction by<br />
(e.g., malaria, babesiosis,<br />
clostridium perfringens)
Why do we see overt hemolysis?<br />
<strong>In</strong>tracorpuscular defectsinherited<br />
hemolysis<br />
• HEMOGLOBIN DEFECTS -<br />
unstable variants (e.g. Hb Köln),<br />
defective globin chains (HbS,<br />
thalassemia)<br />
• MEMBRANE DEFECTS –<br />
altered or missing proteins (e.g.<br />
hereditary<br />
spherocytosis,elliptocytes,<br />
abnormal hydration (e.g.<br />
xerocytosis)<br />
• ENZYME DEFECTS – defective<br />
glycolysis (e.g. PK deficiency),<br />
defective reducing power (e.g.<br />
G6PD deficiency)
<strong>In</strong>creased hemolysis happens in 2 sites<br />
1. Extravascular - localized in the spleen<br />
• <strong>In</strong>trinsic red blood cell defects<br />
– Hemoglobin, membrane or enzyme problems<br />
• Extrinsic red blood cell defects<br />
– Liver disease<br />
– Hypersplenism<br />
– <strong>In</strong>fections (eg, bartonella, babesia, malaria)<br />
– Oxidant agents (eg, dapsone, nitrites, aniline dyes)<br />
– Autoimmune hemolytic anemias<br />
2. <strong>In</strong>travascular - in the circulation<br />
• Direct trauma, shear stress, thermal burns<br />
• Complement-induced lysis (i.e., PCH)<br />
• Lysis from osmotic change, bacterial toxins
EXTRAVASCULAR<br />
• RED CELLS REMOVED VIA RE<br />
SYSTEM<br />
BONE MARROW<br />
Fe++<br />
RBC<br />
RE SYSTEM<br />
globin<br />
BILIVERDIN<br />
L<br />
I<br />
V<br />
E<br />
R<br />
Glucoronal<br />
transferase<br />
UNCONJGATED<br />
BILIRUBIN<br />
GUT<br />
UROBILINOGEN<br />
acted on by<br />
bacteria<br />
CONJUGATED<br />
BILIRUBIN<br />
STERCOBILINOGEN<br />
excreted in feces
INTRAVASCULAR<br />
• CELLS LYSED IN VESSELS<br />
FREE HB<br />
HAPTOGLOBIN<br />
b globulin<br />
HB<br />
HAPTOGLOBIN<br />
Binds at 1:1 ratio (NR 0.3-<br />
0.75 g/l )<br />
Excreted by phagocytic cells-<br />
30min half life<br />
FREE HEME<br />
HEMOPEXIN<br />
FREE HEME<br />
HEME<br />
ox<br />
albumin<br />
HEMOPEXIN<br />
a globulin Binds at 1:1 ratio(NR<br />
0.6-1.0 g/l)<br />
Excreted by hepatic cells - 3.5hr half<br />
life<br />
Excreted by<br />
phagocytic cells -half<br />
METHEMALBUMIN life 20hrs
Excess Extravascular hemolysis
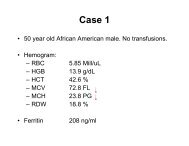
Case: A post-operative patient with a<br />
sudden hemoglobin drop<br />
• 47 yo Italian-Canadian woman, sphenoid tumour<br />
resection and post-op right MCA stroke<br />
• Past medical history:<br />
– Diabetic<br />
– Depression/anxiety<br />
• Sudden hemoglobin drop on post op day 2 and 32<br />
– Admission: Hb 158<br />
– Post op day 1 : Hb 114 dropped to 83 transfused<br />
– Post op day 29: Hb 110<br />
– POD 32: Hb 68 –Hematology consulted
Identifying hemolysis<br />
• Clinical clues<br />
– Rapid fall in hemoglobin with no evidence of blood<br />
loss<br />
– Jaundice<br />
– Dark urine, pale stools, pigmented gallstones<br />
– Splenomegaly<br />
• Laboratory clues<br />
– Reticulocytosis<br />
– <strong>In</strong>crease in serum lactate dehydrogenase (LDH) and<br />
indirect bilirubin concentrations
Does the patient have increased<br />
hemolysis?<br />
1. <strong>In</strong>creased erythrocyte destruction<br />
2. <strong>In</strong>creased erythrocyte regeneration
HEMOLYTIC SCREEN<br />
• CBC - include Retic count<br />
• RBC MORPHOLOGY- fragments,<br />
membranes<br />
• SUPRAVITAL STAINS<br />
– <strong>In</strong>cubated BCB<br />
– Methyl violet<br />
• BILIRUBIN TOTAL AND DIRECT<br />
• HAPTOGLOBIN ELECTROPHORESIS<br />
• COOMB’S TEST (DAT)
Haptoglobin Electrophoresis<br />
• Protein electrophoresis utilizing agar matrix<br />
• Barbituate buffer – alkaline pH<br />
• Electrophoresed @ 4 o C for 1hr at<br />
10 mamps / plate<br />
• Stained with a heme specific dye<br />
• Assesses presence of free hemoglobin, hemopexinheme<br />
complex, methemalbumin<br />
• Gives a semi-quantitative measurement of<br />
haptoglobin
1volume<br />
Plasma/Serum<br />
1 volume<br />
0.6g/l free<br />
Hb solution<br />
Completely binds all<br />
free Hb added<br />
Partially binds free<br />
Hb added<br />
<strong>In</strong>cubated @<br />
room temperature<br />
for 30 mins<br />
Does not bind any free<br />
Hb added
Haptoglobin Agar Gel<br />
Plasma<br />
+<br />
Controls<br />
Normal <strong>Red</strong>uced Absent<br />
1:1 mix with<br />
0.6g/l Hb<br />
Free Hb<br />
Hemopexin/Heme<br />
complex<br />
Hb/Hapt<br />
complex<br />
Methemealbumin<br />
_<br />
Lane 1 2 3 4 5 6 7 8
Haptoglobin Electrophoresis<br />
MHA<br />
Hb/HAPT<br />
Heme/Hx<br />
Free Hb
Case: A post-operative patient<br />
with a sudden hemoglobin drop<br />
• Clinical assessment<br />
– No evidence of blood loss<br />
– Jaundice, pallor, dark urine<br />
– Abdominal ultrasound<br />
• Gallbladder stones and sludge, thickening of gall bladder wall<br />
• Splenomegaly not noted<br />
• Laboratory assessment<br />
– Ferritin elevated at 2029 ug/L<br />
– Reticulocyte count elevated at 246 x 10 9 /L, RPI 2.6<br />
– LDH elevated at 1977 U/L (ref 110-220 U/L)<br />
– Bilirubin elevated at 28 umol/L (ref
Further hemolytic testing<br />
Haptoglobin<br />
Free Hb<br />
Hemopexin-Heme<br />
Methemalbumin<br />
Osmotic fragility<br />
Hb electropheresis<br />
G6PD Assay<br />
Pyruvate kinase assay<br />
• Absent<br />
• Absent<br />
• Absent<br />
• Normal<br />
• Abnormal = Hb Setif [HBA2c.283G>T]<br />
• Normal<br />
• 1.59 U/mL RBC (ref 1.87-3.90)
GLUCOSE<br />
Met Hb<br />
reduction<br />
Pyruvate kinase<br />
Glucose-6 P<br />
Fructose-6 P<br />
Fructose-1,6 BP<br />
Glyceraldehyde-3 P<br />
1,3 BP-Glycerate<br />
3 P-Glycerate<br />
2 P-Glycerate<br />
Phosphoenol –<br />
Pyruvate (PEP)<br />
Pyruvate<br />
Lactate<br />
ADP<br />
ATP<br />
Hexose<br />
monophosphate<br />
shunt<br />
Rapoport-<br />
Luebering<br />
shunt<br />
Adapted from Israels et al.<br />
Mechanisms in Hematology.
Impact of pyruvate kinase deficiency<br />
on the red cell<br />
• <strong>Red</strong> cell can’t produce enough energy to maintain<br />
integrity, causing hemolysis<br />
• Metabolites upstream to PK accumulate<br />
– PEP<br />
– 2,3 BPG (from Rapoport-Luebering shunt)
Genetics of PK Deficiency<br />
• Gene frequency is 1-2%,<br />
distributed worldwide<br />
• Autosomal recessive<br />
inheritance<br />
• Phenotype varies!<br />
• 158 mutations reported<br />
Zanella A et al. <strong>Blood</strong> Reviews 2007:21,217-231.<br />
Anastasiou D et al. Nature Chemical Biology 2012: 8, 839–847.
Genetic testing in post-operative<br />
• PKLR gene analyzed by<br />
PCR and direct<br />
nucleotide sequencing<br />
of coding exons<br />
• Patient heterozygous<br />
for pARG486Trp<br />
(c.1456C>T)<br />
• Missense mutation of<br />
pyruvate kinase gene<br />
• Mild clinical phenotype<br />
patient<br />
Beutler E, Gelbart T. <strong>Blood</strong> 2000, 95(11):3585-3588.
Clinical consequences of pyruvate<br />
kinase deficiency<br />
• Lifelong chronic hemolysis may have anemia<br />
• Splenomegaly<br />
• Gallstones<br />
• Iron overload<br />
– from chronic transfusion therapy, ineffective<br />
erythropoiesis, synergistic effect of<br />
hemochromatosis mutations<br />
• Rare outcomes<br />
– transient aplastic crises, folate deficiency,<br />
neonatal jaundice and kernicterus<br />
Zanella A et al. Br J Hem 2005.
Treatment of PK deficiency<br />
• No specific therapy available<br />
• <strong>Red</strong> cell transfusions for severe, symptomatic<br />
anemia<br />
• Splenectomy for severe, symptomatic anemia<br />
and transfusion dependence<br />
– Does not stop hemolysis, but can increase Hb<br />
– No way to predict therapeutic efficacy<br />
• Iron chelation may be needed<br />
• Gene therapies on the horizon<br />
Zanella A et al. Br J Hem 2005.<br />
Tanphaichitr VS et al. Bone Marrow Transplant. 2000;26(6):689.<br />
Tani K et al. <strong>Blood</strong>. 1994;83(8):2305.
Hb Setif: Unstable Hb Testing<br />
• Isopropanol <strong>In</strong>stability Test<br />
• Heat Denaturation Test
HEINZ BODIES<br />
• Denatured hemoglobin - intracellular body<br />
stained by supravital stains<br />
• Seen in oxidative hemolysis<br />
• Usually shows typical “bite cells”<br />
‣G6PD deficiency<br />
‣Unstable Hemoglobin<br />
‣Oxidative drugs
Methemoglobinemia<br />
• Several chemical and drugs can increase<br />
MetHb levels.<br />
• An acquired MetHb is suggested when<br />
sudden cyanosis appears with the absence<br />
of cardiopulmonary pathology.
Methemoglobin<br />
• Normal levels of less than 1%.<br />
• <strong>In</strong>crease of MetHb causes cyanosis because<br />
of the decreased O2 delivery.<br />
• Can be genetic causes- Hb M or deficiency<br />
of NADH-dependent cytochrome b5<br />
reductase (b5R)<br />
• Exogenous oxidizing agents.
Glucose-6-phosphate<br />
dehydrogenase deficiency<br />
(G6PD)<br />
• The most common enzymatic disorder of<br />
the human erythrocyte.<br />
• estimates =>200-400 million people world<br />
wide.<br />
• Most are asymptomatic some will have<br />
hemolytic episodes or chronic hemolysis.
G6PD Deficiency<br />
• Lack of G6PD means decreased NADPH<br />
and therefore an inability to regenerate GSH<br />
• Globin denaturation and precipitation -<br />
Results in Heinz bodies and bite cells<br />
• Damaged membrane, non-deformability<br />
• Extravascular hemolysis<br />
• X-linked disease
Hexose Monophosphate Shunt<br />
• Production of NADPH, which is used to produce<br />
GSH (Glutathione) the main protection vs oxidative<br />
injury
WHO Classification of G6PD<br />
• Class I- Severe deficiency with chronic anemia.<br />
• Class II- Severe deficiency with intermittent<br />
hemolysis.<br />
• Class III- moderate deficiency with intermittent<br />
hemolysis- associated infections and drugs.<br />
• Class IV- No enzyme deficiency or hemolysis<br />
• Class V- increased enzyme activity.
Fluorescent spot test for G6PD<br />
• Small amount of blood incubated with G6P<br />
and NADP .<br />
• G6PD enzyme source is patients whole<br />
blood<br />
• Spotted every 5 minutes on filter paper.<br />
• Normal will show fluoresence in 5-10<br />
minutes.<br />
Glucose-6-Phospate +NADP<br />
No Fluorescence<br />
G6PD<br />
6-Phosphogluconate +NADPH<br />
Fluorescence
0<br />
TIME<br />
5 10 15 20<br />
Mediterranean<br />
G6PD<br />
Normal<br />
<strong>In</strong>termediate<br />
G6PD<br />
Reagent
Glucose 6 Phosphate Dehydrogenase<br />
Deficiency Assay<br />
Buffer containing:<br />
Glucose 6 Phophate, NADP<br />
Patients Whole<br />
<strong>Blood</strong><br />
<strong>In</strong>c @ 30oC<br />
Using average<br />
change in OD<br />
/min,millimolar<br />
absorptivity of<br />
NADP and patients<br />
Hb level<br />
Calculate units of<br />
activity in U/g Hb<br />
OD read each minute at 340nm<br />
for 10 minutes
G6PD Assay<br />
• Same reaction and principle as screen.<br />
• Performed at specific temperature and<br />
measured on a spectrophotometer at 340<br />
nm.<br />
• Measure rate of change in Absorbance.<br />
• Reference = 146-376 U/10 12 RBC<br />
4.6-13.5 U/g Hb
Other Enzyme Deficiencies<br />
• Pyrimidine 5’ Nucleotidase Deficiency<br />
– Marked basophilic stippling due to deficiency.<br />
– Prevents RNA degradation products from leaving the maturing reticulocyte.<br />
– Results in a build up of insoluable pyrimidines.<br />
• Hexokinase deficiency<br />
– <strong>In</strong>ability to phosphorylize glucose and therefore keep it<br />
intracellular<br />
• Glucose Phosphate Isomerase Deficiency<br />
• Phosphofructokinase deficiency<br />
• Triosephosphate isomerase deficiency<br />
• Phosphoglycerate kinase deficiency<br />
• Adenylated Kinase deficiency<br />
• Aldolase Deficiency<br />
• Lactate Dehydrogenase deficiency<br />
• Biphosphoglycerate Mutase deficiency
Basophilic Stippling<br />
• Pyrimidine 5’ nucleotidase deficiency
Conclusions: Take-home<br />
message<br />
• A systematic approach to for investigation of<br />
unexplained anemia is be useful – CBC including the<br />
retic count and red cell morphology.<br />
• Think about hemolysis in all patients with anemia<br />
– Careful review of basic labs are useful for identification of<br />
hemolytic anemia<br />
– Consider causes of hemolysis congenital -inside the RBC<br />
and acquired - outside the RBC.<br />
• Patients with chronic, sometimes well compensated<br />
and stable hemolytic conditions can develop acute<br />
exacerbations with other medical conditions