MAKETA 6/2 po - Jesseniova lekárska fakulta
MAKETA 6/2 po - Jesseniova lekárska fakulta
MAKETA 6/2 po - Jesseniova lekárska fakulta
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ISSN 1335-8421 Acta Med Mart 2006, 6(2)<br />
ACTA MEDICA<br />
MARTINIANA<br />
Journal for Biomedical Sciences,<br />
Clinical Medicine and Nursing<br />
Contents<br />
3<br />
Evaluation of diastolic dysfunction in children<br />
Review<br />
Sylvia Krupičková, Alexander Jurko jr., Alexander Jurko, Vanda Pedanová, Zuzana Lehotská<br />
10<br />
Heart rate variability during hypertensive reaction in s<strong>po</strong>ntaneously breathing<br />
and artificially ventilated rabbits<br />
Juraj Mokrý, Tatiana Remeňová, Kamil Javorka<br />
16<br />
Ischemia – reperfusion effect on cochlear function. An animal model<br />
Krzysztof Morawski, Grazyna Lisowska, Kazimierz Niemczyk<br />
21<br />
Experimental meconium aspiration: Effect of dexamethasone treatment<br />
on the lung functions – a pilot study<br />
Daniela Mokra, Andrea Calkovska, Janka Bulikova,<br />
Maria Petraskova, Kamil Javorka<br />
27<br />
Formulation and implementation of the National Immunization Programme<br />
in Slovak Republic<br />
Henrieta Hudečková, Mária Szilágyiová, Vladimír Oleár, Tibor Baška, Štefan Straka<br />
31<br />
Screening of diabetic foot in nursing practice<br />
Jana Nemcová, Tibor Baška, Milan Ochodnický, Dušan Mištuna<br />
Published by the Jessenius Faculty of Medicine in Martin,<br />
Comenius University in Bratislava, Slovakia
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
E d i t o r - i n - C h i e f :<br />
Javorka, K., Martin, Slovakia<br />
I n t e r n a t i o n a l E d i t o r i a l B o a r d :<br />
Belej, K., Martin, Slovakia<br />
Buchanec, J., Martin, Slovakia<br />
Honzíková, N., Brno, Czech Republic<br />
Kliment, J., Martin, Slovakia<br />
Lehotský, J., Martin, Slovakia<br />
Lichnovský, V., Olomouc, Czech Republic<br />
Mareš, J., Praha, Czech Republic<br />
Plank, L., Martin, Slovakia<br />
Stránsky, A., Martin, Slovakia<br />
Tatár, M., Martin, Slovakia<br />
Żwirska-Korczala, K., Zabrze-Katowice, Poland<br />
E d i t o r i a l O f f i c e :<br />
Acta Medica Martiniana<br />
Jessenius Faculty of Medicine, Comenius University<br />
(Dept. of Physiology)<br />
Malá Hora 4<br />
037 54 Martin<br />
Slovakia<br />
Instructions for authors: http:|www.jfmed.uniba.sk (Acta Medica Martiniana)<br />
T l a č :<br />
P+M Turany<br />
© Jessenius Faculty of Medicine, Comenius University, Martin, Slovakia, 2006
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 3<br />
EVALUATION OF DIASTOLIC DYSFUNCTION IN CHILDREN<br />
Review<br />
SYLVIA KRUPIČKOVÁ, ALEXANDER JURKO JR., ALEXANDER JURKO, VANDA PEDANOVÁ,<br />
ZUZANA LEHOTSKÁ<br />
Clinic of Children and Adolescents, Jessenius Faculty of Medicine, Comenius University and Martin Faculty Hospital,<br />
Martin, Slovak Republic<br />
A b s t r a c t<br />
It has been determined, that 20 to 40 % of patients with symptoms of heart failure have normal left ventricular ejection<br />
fraction and the reason of heart failure is isolated diastolic dysfunction. Normal diastolic function of the left ventricle<br />
is defined as the capacity to receive filling volume and insure adequate heart output in condition of low ventricular<br />
pressures. Diastolic function is evaluated by transmitral flow and flow in pulmonary veins by ultrasound. Following<br />
parameters are measured: isovolumic relaxation time /IVRT/; deceleration time /DT/; velocity of wave E, A, and their<br />
ratio; velocity-time integral of wave E and A; velocity and duration of wave AR.<br />
Three types of diastolic dysfunction are distinguished. Relaxation disorder is the least severe stage of diastolic dysfunction.<br />
It is characterized by reversed ratio of velocities of wave E and A /less then 1/, prolonged DT over the norm<br />
given for age and lenghtening of IVRT. The restrictive filling pattern is characterized by high velocity of wave E with short<br />
DT and short wave A. Pseudonormal transmitral filling pattern is characterized by wave AR changes in the pulmonary<br />
venous flow. Its amplitude is higher than 25 cm/s and longer than transmitral wave A.<br />
Treatment of diastolic heart failure is difficult because there are only few clinical studies available. The baseline for efective<br />
therapy is identification of the cause of the heart failure and its treatment. There are two main approaches in pharmacological<br />
treatment: repair of abnormal relaxation properties and decrease of filling pressures - elimination of venous stagnation.<br />
K e y w o r d s : diastolic dysfunction, heart diseases, therapy<br />
INTRODUCTION<br />
Pathophysiology of heart failure is different in paediatric and adult <strong>po</strong>pulation. The most frequent<br />
reason of ventricular dysfunction in children are structural heart diseases, often complicated<br />
by surgical interventions./1,2/<br />
Combined pharmacological therapy /diuretics, digoxin, amrinon, milrinon, ACE inhibitors/<br />
often improves heart failure in adults. However, this is not so successful in children because of<br />
residual structural lesions, immaturity of heart muscle and decreased ability to control of intracellular<br />
calcium homeostasis.<br />
The decrease in incidence of ventricular dysfunction allowed application of one-stage neonatal<br />
surgery and catheter intervention techniques, used e.g. for closure of ductus arteriosus, defect of<br />
interatrial septum and of muscular part of ventricular septum./3/<br />
It has been determined, that 20 to 40 % of patients with symptoms of heart failure have<br />
normal ejection fraction of left ventricule and the reason of heart failure is isolated diastolic dysfunction.<br />
/4, 5/ Systolic dysfunction is determined by disturbance of pumping function of the<br />
ventricle. Diastolic dysfunction means the failure of filling of heart ventricle.<br />
Normal diastolic function of left ventricle is present, when the ventricle can receive adequate<br />
filling volume after early relaxation and with low diastolic pressure in early diastole in condition<br />
of subtle pressure increase. /6/<br />
PATHOPHYSIOLOGY OF HEART DIASTOLIC DYSFUNCTION<br />
Diastole is integral part of heart cycle, essential for accurate function of the heart. It represents<br />
complex process, which needs energy, lasts longer then systole and has its own regulatory<br />
mechanisms. Diastole is the interval between aortic valve closure and mitral valve closure.<br />
Address for corres<strong>po</strong>ndence:<br />
MUDr. Sylvia Krupičková, Pod hájom 956/8, 018 41 Dubnica nad Váhom<br />
Phone: +421 905 321 498, e-mail: sylviakrupickova@inmail.sk
4<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
Diastole is divided to 4 phases:<br />
- isovolumic relaxation,<br />
- early diastolic filling,<br />
- diastase,<br />
- atrial contraction. /7/<br />
During early diastole in normal conditions, ventricle receives 55 % of filling volume and during<br />
passive phase 20 % of filling volume. Last phase of diastole is atrial contraction, during which<br />
the remaining 25 % of pulse volume comes into ventricle. /8/<br />
Normal diastolic function of left ventricle is defined by capacity of left ventricle to receive filling<br />
volume of left ventricle and insure adequate heart output at low pressures in left ventricle. /9/<br />
Diastole is divided into early, active phase - relaxation, which is result of changes in myocard<br />
and late, passive phase, which is ifluenced by external forces. So, active relaxation and passive<br />
compliance are distinguished. Both events overlap, because relaxation is not finished until<br />
beginning of the filling.<br />
Diastolic dysfunction of left ventricle is:<br />
1. incompetence to fill left ventricle at rest or at exertion to normal end-diastolic volume without<br />
abnormal increase of end-diastolic pressure in left ventricle or mean pressure in left atrium,<br />
or<br />
2. failure of increase of end-diastolic volume in left ventricle and cardiac output during physical<br />
activity. /7/<br />
Actually, the diastolic dysfunction of left ventricle is incapability of the ventricle to relax and<br />
to fill in.<br />
Systolic function influences relaxation of left ventricle and often also its compliance, so all<br />
patients with decreased ejection fraction of left ventricle have diastolic abnormalities /7/.<br />
The most frequent consequence of diastolic dysfunction is venous congestion of the lungs<br />
/10/. It means, that normal systolic function of left ventricle does not exclude the <strong>po</strong>ssibility of<br />
cardiac reason of dyspnoe /5, 11/.<br />
The diastolic dysfunction can cause only little delay of the relaxation of left ventricle without<br />
increase of the pressures in the earliest stages and the patient can be asymptomatic.<br />
Heart failure is clinical syndrome, which is characterised by symptoms and signs of<br />
increased amount of fluids and decreased perfusion of tissues/organs /12/. To evaluate this<br />
clinical syndrome, it is im<strong>po</strong>rtant to measure not only systolic, but also diastolic function. We<br />
speak about diastolic heart failure, if the heart failure is caused predominantly or exclusively by<br />
abnormalities in diastolic dysfunction.<br />
Diagnosis of diastolic heart failure involves fulfilment of three conditions:<br />
a) presence of clinical signs of heart failure, especially left heart failure,<br />
b) normal ejection fraction /over 50%/,<br />
c) increased diastolic filling pressure.<br />
The first 2 criterions can be easily identified. The problem is to find out an indicator of diastolic<br />
pressures.<br />
The invasive method of catheterisation, at which pressure and volume are simultaneously<br />
measured, allows measurement of velocity of diastolic filling and stiffness of myocard. But it is<br />
not <strong>po</strong>ssible to use it for routine diagnostic evaluation /13/.<br />
The noninvasive evaluation of diastolic function can be done by 2D and Doppler echocardiography,<br />
TDI, M-mode echocardiography, radionuclid ventriculography and magnetic imaging. It<br />
has been proven, that echocardiography is appropriate for routine measurement of diastolic<br />
function and is often used in clinical studies.
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 5<br />
THE ULTRASOUND EVALUATION OF DIASTOLIC DYSFUNCTION<br />
Ultrasound evaluation of transmitral flow and flow in pulmonary veins /Fig. 1, Fig. 2/ allows<br />
to assess following parameters:<br />
Isovolumic relaxation time /IVRT/ is interval between aortic valve closure and mitral valve<br />
opening. Aortic valve closure can be found out most exactly during simultaneous recording with<br />
phonocardiogram, but more practical way is <strong>po</strong>sitioning assay volume of PW Doppler between anterior<br />
cusp of mitral valve and outflow tract of left ventricle. IVRT reflects the velocity at the beginning<br />
of myocardial relaxation. Longer IVRT is a sensitive marker of abnormal relaxation of myocard.<br />
Wave E -is the intensity of pressure gradient between atrium and ventricle at the beginning<br />
of diastole. Its intensity reflects the velocity of ventricle relaxation /in relaxation disorder the<br />
pressure in left ventricle at the beginning of diastole is relatively higher and the velocity of wave<br />
E decreases/, pressure in left atrium /in high filling pressures the velocity of wave E increases/<br />
and compliance of left ventricle.<br />
Deceleration time - DT - reflects the velocity of the pressure increase in left ventricle in early<br />
diastole, which follows after its maximal initial decrease. DT is dependent on duration of relaxation<br />
of left ventricle and its compliance.<br />
Wave A - maximal velocity during atrial contraction. It depends on the compliance of left ventricle,<br />
preload and the contractility of left atrium.<br />
In normal persons the ratio E/A is more than one until the middle age and does not exceed<br />
200 ms. Persons over 50 years have the ratio E/A about 1 and over 60 years bellow 1. So relaxation<br />
disorder appears in increased age.<br />
The main problem of diagnosis of diastolic function disorder with PW Doppler is the fact, that<br />
parameters of transmitral flow are significantly dependent on preload and afterload of atria and<br />
ventricles /14/.<br />
Wave AR – this wave describes retrograde flow in pulmonary veins during atrial contraction.<br />
Its amplitude and duration have relationship to diastolic pressure in left ventricle, compliance of<br />
left atrium and heart rate. In healthy persons the amplitude of AR is less than 30 cm/s and lasts<br />
less then transmitral wave A.<br />
Fig.1. In the left screen,<br />
methodological outline for<br />
the measurement of Doppler<br />
transmitral indexes of diastolic<br />
function. In the right<br />
screen, normal diastolic pattern<br />
(upper part) and pattern<br />
of abnormal relaxation (lower<br />
part). A = atrial velocity<br />
(m/s), DT = deceleration time<br />
of E velocity (ms), E = early<br />
diastolic velocity (cm/s),<br />
IVRT = isovolumic relaxation<br />
time (ms)
6<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
Fig.2. In the left screen,<br />
methodological outline for the<br />
measurement of pulmonary<br />
veins flow. In the right screen,<br />
normal pulmonary veins flow<br />
pattern (upper part) and pattern<br />
of abnormal relaxation<br />
(lower part).<br />
Three types of diastolic dysfunction are distinguished:<br />
Relaxation disorder - is the least severe stage of diastolic dysfunction. The relaxation disorder<br />
leads to deceleration of pressure decrease in left ventricle at the beginning of diastole<br />
between atrium and ventricle. The velocity of wave E decreases. The relaxation<br />
further continues to relatively late diastole, the pressures between atrium and ventricle<br />
equalize slower and this process leads to lenghtening of DT. A big volume of blood remains in left<br />
atrium until late diastole, its preload increases and its contraction intensifies /Frank - Starling<br />
mechanism/. So the velocity of wave A increases. Thus the relaxation disorder is characterized<br />
by reversed ratio of velocities of wave E and A /less then 1/ and prolonged DT over<br />
the norm for given age. Next sign of relaxation disorder is lenghtening of IVRT. The patients<br />
with relaxation disorder are asymptomatic.<br />
Pseudonormal and restrictive pattern. The compliance of left ventricle decreases with<br />
continuing disorder of diastolic function. This leads to increase of end-diastolic pressure in<br />
left ventricle and mean pressure in left atrium. High filling pressures lead to increase of<br />
velocity of wave E with shortening of DT, and the velocity of wave A decreases. The increased<br />
afterload in left atrium causes the larger volume of blood coming during systole of the atrium<br />
into pulmonary veins, where the velocity and duration of wave AR increases. The restrictive<br />
filling pattern is characterized by high velocity of wave E with short DT and short<br />
wave A.<br />
Pseudonormal filling pattern - u<strong>po</strong>n analysis of mitral flow can not be distinguished from<br />
normal filling /E is higher then A/.<br />
The pseudonormal pattern can be distinguished by following:<br />
° left atrium is slightly enlarged - diastolic dysfunction in normal size of left atrium is very unlikely,<br />
° wave AR in the pulmonary venous flow pattern has amplitude more then 25 cm/s and is longer<br />
then transmitral wave A,<br />
° wave Em by examination with TDI is diminished and the E/Em ratio is more then 15 /look below/,<br />
° by examination with color M-mode the velocity of propagation flow is decreased /less then 40 cm/s/<br />
/look below/,
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 7<br />
Fig.3. In the left screen,<br />
methodological outline for the<br />
measurement of Tissue Doppler<br />
indexes. In the right<br />
screen, normal myocardial<br />
diastolic pattern (upper part)<br />
and pattern of abnormal<br />
myocardial relaxation (lower<br />
part). Am = myocardial atrial<br />
velocity (cm/s), CTm = myocardial<br />
contraction time (ms),<br />
DTm = myocardial deceleration<br />
time of Em(ms), Em = myocardial<br />
early-diastolic velocity<br />
(cm/s), PCTm = myocardial<br />
pre-contraction time (ms),<br />
RTm = myocardial relaxation<br />
time (ms).<br />
° by the change of loading conditions for example with nitroglycerine, nitroprusid or Valsalva maneuver,<br />
relaxation disorder pattern develops,<br />
° patients with pseudonormal pattern have dyspnoe by exertion /15/<br />
TDI /tissue Doppler imaging/ is modification of conventional doppler echocardiography and<br />
is directed for recording of velocities of systolic and diastolic motions of myocard or annulus of<br />
valves. Classic doppler technique uses setting by which higher velocities /10-100 cm/s/ with low<br />
amplitude are recorded, which are typical for motion of flowing blood. On the contrary, TDI analyzes<br />
mainly signals of low velocity and high amplitude, which are typical for motion of myocard<br />
and annulus of valves. /14/.<br />
By pulse TDI, sample volume is <strong>po</strong>sitioned to arbitrary site of myocard, which function we<br />
want to evaluate and we receive doppler trace with velocities of motion of myocard in chosen<br />
region.<br />
For evaluation of regional diastolic function are used IVRT /interval between end of wave<br />
S and beginning of wave A/, Em /early diastolic velocity of relaxation - reflects velocity of relaxation<br />
in examinate <strong>po</strong>sition, it is independent of preload/ and Am /reflects velocity of motion of<br />
myocard in late diastole//Fig. 3/. In diastolic dysfunction Em decreases, Am increases, Em/Am<br />
ratio decreases under 1. Decrease of Em is a sensitive marker of relaxation disorder of the left<br />
ventricle. We don’t face the problem of pseudonormalisation by increasing of filling pressure of<br />
left ventricle as it is in evaluation of transmitral flow /16/.<br />
It has been found out, that E/Em ratio correlates very well with mean pulmonary capillary<br />
wedge pressure and can be used for examination of wedge pressures /17/.<br />
Color Doppler M-mode mapping /color M-mode/<br />
The velocity of blood flow propagation into left ventricle /Vp/ is one of the newest parameters<br />
used for evaluation of diastolic function of left ventricle and describes mainly the quality of its<br />
relaxation. For its measurement, the largest and longest blood flow from left atrium in the direction<br />
of apex of left ventricle is used.<br />
The velocity of propagation Vp in healthy people is about 80 cm/s, in patients with relaxation<br />
disorder it decreases under 40 cm/s. It is independent on changes of preload and allows to dis-
8<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
tinguish advanced disorders of diastolic dysfunction /pseudonormalisation, restrictive filling<br />
pattern//14, 15/.<br />
TREATMENT OF DIASTOLIC HEART FAILURE<br />
The treatment of diastolic heart failure is difficult and rather empirical, because of few clinical<br />
studies conducted. The baseline for efective treatment is identification of the cause of heart<br />
failure, e.g. ischemia of myocard, arterial hypertension, hypertrophy of myocard, constriction of<br />
myocard and pericard and their treatment. An im<strong>po</strong>rtant role has surgical and interventional<br />
management of congenital heart diseases.<br />
Two main approaches in pharmacological treatment are used:<br />
- repair of abnormal diastolic properties,<br />
- decrease of filling pressures - elimination of venous congestion.<br />
Ca-antagonists improve directly diastolic function, increase homeostasis of Ca and indirectly<br />
decrease blood pressure, decrease myocardial ischemia, sup<strong>po</strong>rt regression of hypertrophy of<br />
left ventricle, reduce frequency of heart rate /verapamil, diltiazem/ and improve filling parameters<br />
of left ventricle.<br />
Sympathetic nervous system affects favourably relaxation of ventricle, it has also <strong>po</strong>sitive<br />
chronotropic and inotropic effects.<br />
Despite beta - blockers block this favorable effect of catecholamins, they improve filling of<br />
ventricle by the mechanism of decreasing heart rate and prolongation of time of diastolic filling,<br />
decrease of blood pressure, myocardial ischemia and regression of hypertrophy of left ventricle.<br />
Beta - blockers with smaller beta2-agonistic activity, as celiprolol, are even more effective.<br />
Celiprolol directly improves diastolic relaxation.<br />
ACE - inhibitors directly influence relaxation of myocard and compliance by decreasing of<br />
production of angiotensin II, which is res<strong>po</strong>nsible for de<strong>po</strong>sition of interstitial collagen and fibrosis.<br />
The indirect effect of ACE - inhibitors includes decrease of blood pressure, improvement of<br />
filling parameters of left ventricle and regression of hypertrophy of left ventricle.<br />
Positive inotropic and chronotropic medications /digoxin, dobutamin/, arterial vasodilators<br />
/hydralasine/ and blockers of alpha-adrenergic receptors /prazosin/ should be avoided. In<br />
absence of systolic dysfunction, they can worsen diastolic function through increasing of contractility<br />
or heart rate.<br />
Diuretics and nitrates are used in certain situations. In situations when very high pressure<br />
for filling of left ventricle is needed, the decrease of preload can worsen cardiac output.<br />
First of all, we need to maintain sinus rythm, avoid tachycardia /decrease heart rate to<br />
lengthen diastole/ and maintain for patients with diastolic heart failure the contribution of atrial<br />
systole.<br />
CONCLUSION<br />
The Doppler evaluation of diastolic function of heart is a new, nowadyas verified method,<br />
which can be used not only in adults, but also in children. Diastolic function is evaluated in<br />
myocardial ischemia, hypertrophy of left ventricle following arterial hypertension, hypertrophic<br />
cardiomyopathy, restrictive cardiomyopathy, diseases of pericard, hypertrophy of one or both<br />
ventricles following congenital heart diseases, coarctation of aorta, complex diseases of myocard<br />
and in evaluation of function of heart in oncologic patients after treatment.<br />
REFERENCES:<br />
1. Behrman RE, Kliegman RM, Jenson HB. Nelson textbook of pediatrics. Philadelphia: W. B. Saunders Company; 2000.<br />
2. Keck EW, Hausdorf G. Pädiatrische Kardiologie. München: Urban und Fischer; 2002.<br />
3. Hanna BD. Ventricular dysfunction in the pediatric <strong>po</strong>pulation: evaluation and intervention. J Heart Lung Transplant<br />
1997; 16 (7): 16-18.<br />
4. Jurko A ml. Vybrané echokardiografické parametrov novorodencov a dojčiat. Martin: Fli<strong>po</strong>; 2000.<br />
5. Grossman W. Defining diastolic dysfunction. Circulation 2000; 101 (4): 2020-2021.
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 9<br />
6. Kohler E, Taturu MCH. Klinische echokardiographie. Stuttgart: Georg Thieme Verlag; 2001.<br />
7. Appleton CHP, Firstenberg MS, Garcia MJ. The echo-doppler evaluation of left ventricular diastolic function. Cardiol<br />
Clin 2000; 18 (3): 513-546.<br />
8.Yoshii K, Iwao H, Fukuda S. Left ventricular diastolic pressure-volume and stress-strain relationship in children. Jap<br />
Circ J 1985; 49 (3): 385-394.<br />
9. Gajderisi M. Diastolic dysfunction and diastolic heart failure: diagnostic, prognostic and therapeutic aspects. Cardiovascular<br />
Ultrasound 2005; 3 (9): 1-20.<br />
10. Chatterjee K, Karliner J, Rapa<strong>po</strong>rt E. Cardiology. Philadelphia: J. B. Lippincott company; 1991.<br />
11. Warltier DC. Ventricular function. Baltimore: Williams and Wilkins; 1995.<br />
12. Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part I. Circulation 2002;<br />
105 (11): 1387-1402.<br />
13. Rosei EA. Clinical value of diastolic dysfunction in hypertension. J Hypert 2002; 20 (6): 1083-1084.<br />
14. Linhart A, Paleček T, Aschermann M. Echokardiografie pro praxi. Praha: Audioscan; 2002.<br />
15. Roelandt JRTC, Pozzoli M. Non-invasive assessment of left ventricular diastolic (dys)function and filling pressure.<br />
Heart views 2001; 2 (3): 1-14.<br />
16. Niederle P. Echokardiografie. Praha: Triton; 2002.<br />
17. Nagueh SF, Middleton KJ, Kopelen HA. Doppler Tissue Imaging: A noninvasive technique for evaluation of left ventricular<br />
relaxation and estimation of filling pressures. J Am Coll Cardiol 1997; 30 (6): 1527-1533.
10<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
HEART RATE VARIABILITY DURING HYPERTENSIVE REACTION IN SPON-<br />
TANEOUSLY BREATHING AND ARTIFICIALLY VENTILATED RABBITS<br />
JURAJ MOKRÝ 1 , TATIANA REMEŇOVÁ 2 , KAMIL JAVORKA 2<br />
1<br />
Department of Pharmacology, Jessenius Faculty of Medicine, Comenius University, Martin, 2 Department of Physiology,<br />
Jessenius Faculty of Medicine, Comenius University, Martin, Slovak Republic<br />
A b s t r a c t<br />
The pur<strong>po</strong>se of the study was to evaluate the changes of heart rate variability parameters (HRV) during hypertensive<br />
reaction evoked by norepinephrine (NE) infusion in anaesthetized rabbits. Furthermore, these changes were studied<br />
during artificial ventilation to study the mechanisms participating in activity of spectral frequency bands of HRV.<br />
Methods: 8 adult rabbits (Chinchilla) were anesthetized by ketamine and flunitrazepam. The R-R intervals, systemic<br />
blood pressure (BP) and respiratory rate were registered and evaluated. The R-R intervals were derived from the electrocardiogram<br />
signal from subcutaneous needle electrodes. HRV was analyzed by microcomputer system VariaPulse TF3E.<br />
The evaluation of HRV in very low (VLF; 0.01-0.05 Hz), low (LF; 0.05-0.15 Hz) and high frequency bands (HF; 0.15-2.0<br />
Hz) was made and parameters of time and frequency analysis were calculated. The measurements were made before,<br />
during and after 30 minutes lasting NE infusion (10 μg/kg/min) in s<strong>po</strong>ntaneously breathing (SB) as well as in artificially<br />
ventilated (AV) anaesthetized rabbits.<br />
Results: The NE infusion in anaesthetized rabbits caused significant increase of systolic and diastolic BP in both SB<br />
and AV animals, which was accompanied by significant prolongation of R-R intervals. The respiratory rate (in SB animals)<br />
was not changed. The HRV parameters, especially total <strong>po</strong>wer spectral density (PSD), PSD in VLF and HF bands,<br />
significantly increased during NE infusion. This elevation was not eliminated during artificial ventilation.<br />
Conclusion: Increased spectral activity in the VLF and HF bands during the hypertensive and bradycardiac reactions<br />
evoked by NE infusion reflects both the sympathetic and parasympathetic regulation of the heart rate in Chinchilla<br />
rabbits.<br />
K e y w o r d s : heart rate variability, artificial ventilation, autonomic nervous system, norepinephrine, hypertension, rabbit<br />
INTRODUCTION<br />
The evaluation of heart rate variability (HRV) by spectral analysis is a suitable, sensitive and<br />
non-invasive tool for studying the influence of autonomic nervous system (ANS) and endocrine<br />
system on the heart (1). Short-term fluctuations of the R-R intervals – instantaneous heart rate<br />
– express the beat-to-beat regulation of the heart pacemaker and the fine-tuning of heart rate<br />
around an average value especially via activity of ANS. The interactions of parasympathetic and<br />
sympathetic nervous system together with other intrinsic mechanisms are considered to be<br />
essential for rapid and short-term changes in HRV (2).<br />
In our recent study (3) we showed that the orthostasis in anaesthetized rabbits is accompanied<br />
by decrease of systemic blood pressure, unchanged heart rate and increased characteristics<br />
of heart rate variability, with predominant increase of spectral <strong>po</strong>wer in low frequency (LF)<br />
and very low frequency (VLF) bands.<br />
The aim of this study was to evaluate the changes of heart rate variability parameters during<br />
hypertensive reaction evoked by norepinephrine (NE) infusion in anaesthetized rabbits. These<br />
changes were evaluated during s<strong>po</strong>ntaneous breathing and artificial ventilation to study the<br />
mechanisms participating in activity of spectral frequency bands of HRV in rabbits.<br />
METHODS<br />
We used 8 adult rabbits (Chinchilla) with mean body weight (b.w.) of 2.6±0.5 kg. The animals<br />
were housed and bred in central menagerie with standard food and water ad libitum.<br />
Address for corres<strong>po</strong>ndence:<br />
Juraj Mokrý, MD, PhD.,Department of Pharmacology,<br />
Jessenius Faculty of Medicine, Comenius University, Sklabinská 26, 037 53 Martin, Slovak Republic<br />
Phone: +421 43 4132535, fax: +421 43 4134807, e-mail: mokry@jfmed.uniba.sk
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 11<br />
During the experiment, the animals were anesthetized by ketamine (Narkamon 5%, Léčiva,<br />
Czech Republic) at the dose of 0.7 ml/kg b.w. and flunitrazepam (Rohypnol 2%, Léčiva, Czech<br />
Republic) at the dose of 0.2 ml/kg b.w. to vena marginalis auriculae. Furthermore, every 30<br />
minutes the combination of ketamine (0.2 ml/kg b.w.) and flunitrazepam (0.07 ml/kg b.w.)<br />
was administered to maintain the sufficient depth of anesthesia. Anesthetics and other drugs<br />
were administered through catheter in the right femoral vein. The systemic BP was monitored<br />
continuously using the electromanometer (LDP 102, Tesla Valašské Meziříčí, Czech Republic)<br />
connected to catheter in arteria femoralis, tidal volume and respiratory rate through the<br />
pneumotachograph (ÚMMT, Bratislava, Slovak Republic) and endotracheal cannula. The registration<br />
was made using 6 NEK 6 recorder (RFT, Dresden, Germany).<br />
HRV was evaluated by microcomputer system VariaPulse TF3E (SIMA MEDIA, Olomouc,<br />
Czech Republic) recording the telemetrically transmitted R-R intervals through a receiver to<br />
computer. The R-R intervals were derived from the electrocardiogram (ECG) signal from subcutaneous<br />
needle electrodes. Special software using spectral analysis (Fast Fourier Transformation)<br />
enables the evaluation of HRV in time and frequency domains in very low (0.01-<br />
0.05 Hz), low (0.05-0.15 Hz) and high frequency bands (HF; 0.15-2.0 Hz) (4,5). The frequency<br />
analysis, besides total spectral <strong>po</strong>wer (TP), offers the characteristics of the individual frequency<br />
bands – spectral <strong>po</strong>wer VLF, LF and HF, <strong>po</strong>wer spectral density (PSD VLF, PSD LF,<br />
PSD HF), and peak of the frequency in the band. Furthermore, the program calculates total<br />
<strong>po</strong>wer, relative <strong>po</strong>wer VLF, LF and HF) and ratios between activities in each frequency band<br />
(VLF/LF, VLF/HF, LF/HF) useful for evaluation of relative activity of sympathetic or parasympathetic<br />
ANS regulating the heart rate. The range of the HF band in the TF3E system in comparison<br />
to the conventional clinical system (TF3) is wider to map the spectral activities up to<br />
the frequency 2.0 Hz (120/min) respecting higher respiratory rate in rabbits.<br />
The time analysis offers further parameters: R-R intervals (and instantaneous reciprocal<br />
heart rate), and MSSD (mean squared successive differences). These parameters characterize<br />
mean heart rate and the magnitude of HRV, whereas the other parameters from frequency<br />
analysis using fast Fourier analysis of non-harmonic signals informs about the rhythms<br />
(2,6).<br />
The hypertensive reaction was evoked by 30 minutes lasting norepinephrine (NE) infusion<br />
(10 μg/kg/min). After cessation of the infusion and normalization of the blood pressure to the<br />
previous initial values, pipecuronium bromide (ARDUAN, Gedeon Richter, Hungary) at a dose<br />
of 0.3 mg/kg/30 min was administered to animals and the endotracheal canulla was connected<br />
to ventilator (Beat-2, Chirana, Slovakia) to ventilate the rabbit in intermittent <strong>po</strong>sitive<br />
pressure ventilation (IPPV) regimen with room air. The respiratory rate was set on average to<br />
36/min with tidal volume from 8 to 10 ml/kg b.w. to keep blood gases (p a<br />
O 2<br />
and p a<br />
CO 2<br />
) in<br />
normal range. The NE infusion was repeated under these conditions.<br />
All the measurements were made before (BEFORE), during NE infusion at 5 th (NE05) and<br />
at 30 th minute (NE30), after connecting to artificial ventilation (AV), during consecutive NE<br />
infusion at 5 th (AVNE05) and 30 th minute (AVNE30) as well as 5 (AV05) and 10 minutes after<br />
stopping the infusion (AV10).<br />
The parameters in Figures (1,2) and in Table 1 are given as means and standard error of<br />
the mean (x±SEM). Non-parametric Wilcoxon test was used for statistical analysis. Statistical<br />
level at p0.05).
12<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
Fig. 1: Changes of systolic and diastolic<br />
blood pressure (for explanations<br />
see the text; significant change of<br />
parameter vs. BEFORE or AV: *<br />
p
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 13<br />
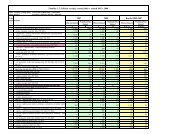
Table 1: Changes of frequency analysis parameters of HRV (for explanations see the text).<br />
Parameter<br />
S<strong>po</strong>ntaneous breathing<br />
Artificial ventilation<br />
BEFORE<br />
NE05<br />
NE30<br />
AV<br />
AVNE05<br />
AVNE30<br />
AV05<br />
AV10<br />
Total<br />
p<br />
*<br />
*<br />
PSD<br />
mean<br />
6.39<br />
31.66<br />
41.90<br />
6.12<br />
18.04<br />
67.22<br />
8.36<br />
8.48<br />
(ms 2 /Hz)<br />
SEM<br />
3.14<br />
9.39<br />
16.64<br />
2.91<br />
6.13<br />
32.27<br />
2.61<br />
3.04<br />
PSD VLF<br />
p<br />
*<br />
(ms 2 /Hz)<br />
mean<br />
5.49<br />
71.76<br />
90.59<br />
4.36<br />
21.37<br />
115.06<br />
7.39<br />
5.17<br />
SEM<br />
0.86<br />
19.13<br />
44.25<br />
2.46<br />
15.80<br />
91.76<br />
2.77<br />
1.63<br />
PSD LF<br />
p<br />
+<br />
+<br />
+<br />
(ms 2 /Hz)<br />
mean<br />
11.44<br />
13.64<br />
28.09<br />
0.85<br />
9.07<br />
62.84<br />
0.86<br />
0.80<br />
SEM<br />
8.96<br />
3.37<br />
10.3<br />
0.48<br />
5.02<br />
54.48<br />
0.39<br />
0.18<br />
PSD HF<br />
p<br />
*<br />
*<br />
+<br />
+<br />
+<br />
+<br />
+<br />
(ms 2 /Hz)<br />
mean<br />
2.13<br />
5.88<br />
7.02<br />
13.17<br />
23.68<br />
23.74<br />
16.83<br />
19.48<br />
SEM<br />
0.94<br />
1.99<br />
1.87<br />
8.05<br />
8.50<br />
7.39<br />
6.22<br />
7.62<br />
Ratio<br />
p<br />
VLF/HF<br />
mean<br />
1.41<br />
1.27<br />
2.78<br />
0.89<br />
1.24<br />
1.79<br />
0.85<br />
0.79<br />
SEM<br />
0.42<br />
0.35<br />
1.12<br />
0.09<br />
0.55<br />
0.82<br />
0.74<br />
0.10<br />
Ratio<br />
p<br />
LF/HF<br />
mean<br />
0.97<br />
0.83<br />
1.25<br />
0.89<br />
0.67<br />
1.34<br />
0.85<br />
0.79<br />
SEM<br />
0.02<br />
0.22<br />
0.28<br />
0.09<br />
0.15<br />
0.46<br />
0.07<br />
0.10<br />
Significant change of parameter vs. BEFORE or AV: * p
14<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
venous return due to <strong>po</strong>sitive pressure), reflex changes (via baroreceptors and pulmonary stretch<br />
receptors), humoral factors and others. Artificial ventilation with almost constant frequency<br />
allows the evaluation of HRV changes, which are independent from changes in respiration.<br />
Also, in AV rabbits with constant frequency of breathing and tidal volume, the NE infusion<br />
caused increase in BP and total PSD based on increase of spectral activities in all frequency<br />
bands, and a decrease in heart rate. Increased spectral activity in HF band without changes of<br />
respiratory characteristics reflects probably enhanced parasympathetic influence on the heart –<br />
bradycardiac reaction, confirming that the activity in HF band is influenced not only by respiratory<br />
sinus arrhythmia, but also via other mechanisms.<br />
Increased PSD HF immediately after initiation as well as during AV compared to SB animals<br />
confirms the decisive role of breathing influences on HRV in determination of the spectral activity<br />
in HF band. Considering the fact the frequency of breathing in SB rabbits was 80-100/min<br />
and in AV animals about 36/min, increased tidal volume to keep blood gases in physiological<br />
range leads to the increased HF band activity. This is in concordance with results of Iwao et al.<br />
(11), who demonstrated the association of HF com<strong>po</strong>nent of HRV with magnitude of fluctuations<br />
of vagal input associated with respiratory modulation.<br />
We conclude the hypertensive reaction evoked by norepinephrine was accompanied by bradycardia<br />
and increase in heart rate variability in rabbits. The rise of spectral activity in the VLF<br />
and HF bands reflects the sympathetic and parasympathetic regulation of the heart rate in the<br />
conditions. The results confirm that complex influences of both sympathetic and parasympathetic<br />
nervous systems participate in individual frequency bands in Chinchilla rabbits<br />
REFERENCES<br />
1. Kleiger RE, Stein PK, Bosner MS, Rottman JN. The domain measurements of heart rate variability. Cardiol Clin 1992;<br />
10: 487-98.<br />
2. Javorka K. Methods and benefits of examining the heart rate regulation in children (in Slovak). Ces-slov Pediat 1996;<br />
51: 462-8.<br />
3. Mokrý J, Remeňová T, Javorka K. Changes in respiratory rate, blood pressure and heart rate variability in rabbits<br />
during orthostasis. Acta Veterinaria 2006; 75: 3-12<br />
4. Salinger J, Opavský J, Búla J, Vychodil R, Novotný J, Vaverka F. Software equipment of measure instrument TF-2<br />
for spectral analysis of variation of R-R interval in cardiology (in Czech). Lékař a technika 1994; 25: 58-62.<br />
5. Salinger J, Opavský J, Novotný J, Vychodil R, Vaverka F, Hudcová Z. Software equipment of measure instrument<br />
TF-2 for diagnostics of autonomous neuropathy (in Czech). Lékař a technika 1993; 24: 133-8.<br />
6. Tonhajzerová I. Heart rate variability and the benefit of its evaluation in physiological research (in Slovak). PhD thesis.<br />
Comenius University, Bratislava, 2000.<br />
7. Javorka K, Javorková J, Petrášková M, Tonhajzerová I, Buchanec J, Chromá O. Heart rate variability and cardiovascular<br />
tests in young patients with diabetes mellitus type 1. J Pediat Endocrin Metab 1999; 12: 423-31.<br />
8. Tonhajzerová I, Javorka K, Petrášková M. Changes of heart rate variability in mental stress (in Slovak). Ces-slov Pediat<br />
2000; 55: 562-7.<br />
9. Tonhajzerová I. Autonomic nervous system (ANS) and the <strong>po</strong>ssibilities of ANS activity assessment in obesity (in Slovak).<br />
Ces-slov Pediat 2005; 60: 228-34.<br />
10. Kawamoto M, Kanek, K, Hardian Yuge O. Heart rate variability during artificial ventilation and apnea in brain-damaged<br />
rabbits. Am J Physiol 1996; 271: H410-6.<br />
11. Iwao T, Yonemochi H, Nakagawa M, Takahashi N, Saikawa T, Ito M. Effect of constant and intermittent vagal stimulation<br />
on the heart rate and heart rate variability in rabbits. Jpn J Physiol 2000; 50: 33-9.<br />
12. Nadareishvili KSh, Meskhishvili II, Kakhiani DD, Ormotsadze GL, Nazarishvili GT, Gvasalia MG, Khvedelidze MT,<br />
Sandodze VY. Heart rate variability in Chinchilla Rabbits. Bull Exp Biol Med 2002; 134: 568-70.<br />
13. Javorka K, Javorková J, Petrášková M, Parížeková I, Buchanec J, Chromá O. Heart rate variability in young patients<br />
with diabetes mellitus type I (in Slovak). Ces-slov Pediat 1997; 52: 17-22.<br />
14. Tonhajzerová I, Javorka K. Evaluation of heart rate variability and its benefit (in Slovak). Ces fysiol 2000; 49: 51-60.<br />
15. Guzzetti S, Dassi S, Pecis M, Casati R, Masu AM, Longoni P, Tinelli M, Cerutti S, Pagani M, Malliani A. Altered pattern<br />
of circadian neural control of heart period in mild hypertension. J Hypertens 1991; 9: 831-8.<br />
16. Novak V, Novak P, de Champlain J, Nadeau R. Altered cardiorespiratory transfer in hypertension. Hypertension<br />
1994; 23: 104-13.<br />
17. Takalo R, Korhonen I, Turjanmaa V, Majahalme S, Tuomisto M, Uusitalo A. Short-term variability of blood pressure<br />
and heart rate in borderline and mildly hypertensive subjects. Hypertension 1994; 23: 18-24.<br />
18. Piccirillo G, Bucca C, Durante M, Santagada E, Munizzi MR, Cacciafesta M, Marigliano V. Heart rate and blood pressure<br />
variabilities in salt-sensitive hypertension. Hypertension 1996; 28: 944-52.
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 15<br />
19. Olosová A, Javorka K, Zibolen M, Tonhajzerová I, Javorková J, Buchanec J, Petrášková M. Spektrálna analýza variability<br />
frekvencie akcie srdca u juvenilných hypertonikov. Ces-slov Pediat 1999; 54: 340-3.<br />
20. van Ravenswaaij-Arts CM, Hopman JC, Kollee LA, Stoelinga GB, van Geijn HP. The influence of artificial ventilation<br />
on heart rate variability in very preterm infants. Pediat Res 1995; 37: 124-30.<br />
21. Gecelovská V, Javorka K. Cardiovascular and haemodynamic changes during artificial ventilation of the lungs.<br />
Bratisl Lek Listy 1996; 97: 260-6.<br />
22. Javorka K, Drgová A, Petrášková M, Gecelovská V. Plasma catecholamine level during Short-term artificial ventilation<br />
(IPPV/HFJV) in rabbits. Abstract. Eur Respir J 1996; 9: 132.<br />
23. Frazier SK, Moser DK, Stone KS. Heart rate variability and hemodynamic alterations in canines with normal cardiac<br />
function during ex<strong>po</strong>sure to pressure sup<strong>po</strong>rt, continuous <strong>po</strong>sitive airway pressure, and a combination of pressure<br />
sup<strong>po</strong>rt and continuous <strong>po</strong>sitive airway pressure. Biol Res Nurs 2001; 2: 167-74.<br />
24. Shen HN, Lin LY, Chen KY, Kuo PH, Yu CJ, Wu HD, Yang PC. Changes of heart rate variability during ventilator<br />
weaning. Chest 2003; 123: 1222-8.<br />
Acknowledgements: This study was sup<strong>po</strong>rted by the Grant VEGA No. 1/2305/05.<br />
Authors thank to S. Svorková, D. Kulišková, M. Barčíková, M. Petrášková, and I. Štritz for technical assistance.
16<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
ISCHEMIA – REPERFUSION EFFECT ON COCHLEAR FUNCTION.<br />
AN ANIMAL MODEL<br />
KRZYSZTOF MORAWSKI 1 , GRAZYNA LISOWSKA 2 , KAZIMIERZ NIEMCZYK 1<br />
1<br />
Department of Otolaryngology, Medical University of Warsaw, Poland<br />
2<br />
Department of Otolaryngology, Medical University of Silesia, Zabrze, Poland<br />
A b s t r a c t<br />
Background and aim: Development of new computer technologies, better and more precise imaging and audiological<br />
diagnostics result in faster diagnosis of patients with cerebello<strong>po</strong>ntine angle tumors (CPAT) in such a stage of this<br />
pathology in which hearing is still relatively well preserved. Therefore, animal experiments enable to develop and check<br />
new conception of intraoperative monitoring of hearing organ and, then, to apply them in clinical practice in patients<br />
with CPAT. The aim of the study was to evaluate and compare the utility of distortion product otoacoustic emissions and<br />
cochlear evoked <strong>po</strong>tentials for monitoring cochlear and eighth nerve functions during reversible cochlear ischemia.<br />
Methods: The authors presented data collected in animal experiments in which the cochlear and the eight nerve<br />
function were monitored during inducing cochlear reversible ischemic episodes. In all cases laser-Doppler cochlear blood<br />
flow techniques (LD-CBF), distortion product otoacoustic emissions (DPOAEs), and evoked auditory <strong>po</strong>tentials (AEP) (i.e.,<br />
cochlear microphonics [CM] and com<strong>po</strong>und action <strong>po</strong>tentials [CAP]) were measured using the otic probe placed into the<br />
round window (RW) niche. Hearing organ activity was assessed by stimulating the basis, middle, and apex of the cochlea.<br />
Results: An animal model of prevention of intraoperative hearing damage was developed and, then, referred to clinical<br />
situations occurring during CPAT surgery. Including and excluding criteria for intraoperative monitoring were presented<br />
with some principles of intraoperative monitoring in patients basing on data collected during animal experiments.<br />
Conclusions: Intraoperative monitoring by AEP was found to be more complex and useful to differ cochlear and<br />
retrocochlear damage occurring intraoperatively. DPOAE is a better method in aspect of monitoring in real time. AEP was<br />
found to be more complex res<strong>po</strong>nse reflecting changes in cochlear and retrocochlear structures as a result of different<br />
manipulation of surgeon but consuming more time needed for averaging procedure.<br />
K e y w o r d s : cochlear blood flow, otoacoustic emissions, evoked auditory <strong>po</strong>tentials<br />
INTRODUCTION<br />
Surgery of the cerebello<strong>po</strong>ntine angle tumor (CPAT) is associated with a high risk of damaging<br />
such im<strong>po</strong>rtant structures as facial nerve, vestibulocochlear nerve, internal auditory artery, anterior<br />
inferior cerebellar artery, and inner ear function, if they escaped earlier damage by the invading<br />
tumor. Although the attempts to monitor intraoperatively function of the above structures has<br />
been still tested, an efficacious monitoring of the inner ear and the eight nerve function remains<br />
to be established (1-7). Distortion product otoacoustic emissions (DPOAEs) or electrophysiological<br />
recordings using either electrocochleography (EcoG) involving com<strong>po</strong>und action <strong>po</strong>tentials of the<br />
VIII nerve (CAP) and cochlear microphonics (CM), or auditory brainstem res<strong>po</strong>nses (ABR), as well<br />
as evoked <strong>po</strong>tentials from the cochlear nucleus provide considerable information about the status<br />
of the peripheral parts of the auditory system (8-11). On the basis of the above tests, any surgically<br />
induced trauma whether directly damaging inner ear structures or indirectly harming<br />
neurepithelial or neural parts of the inner ear through the compromise of the blood vessels supplying<br />
the cochlea, can only be detected after some delay. This delay in recognizing a surgically<br />
induced trauma during the course of an operation can lead to the irreversible damage of cochlear<br />
function and permanent deafness for the ear on the operated side. Audiological tests that permits<br />
recording cochlear activity fast and more directly involves DPOAEs and EcoG.<br />
Evoked otoacoustic emissions (OAEs), are measures of acoustic energy recorded from the ear<br />
canal and generated from the cochlea in res<strong>po</strong>nse to acoustic stimulation (12, 13). It is thought<br />
that OAEs reflect the function of the cochlea that is associated with electromotility of the outer<br />
Address for corres<strong>po</strong>ndence:<br />
Krzysztof Morawski, MD, PhD, Department of Otolaryngology, Medical University of Warsaw,<br />
Banacha 1a Street, 02-097 Warsaw, Poland<br />
E-mail: hno@<strong>po</strong>czta.onet.pl
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 17<br />
hair cells (OHCs) that are extremely sensitive to such harmful factors as excessive noise, ototoxic<br />
drugs, and hy<strong>po</strong>xic or anoxic conditions. Such insults can quickly alter OHC function, which<br />
results in either reduced or absent OAEs, depending on the severity of the damage (13-16). In<br />
particular, the evoked emissions that are used most commonly for clinical applications are the<br />
transiently-evoked (TEOAEs) and DPOAE (13).<br />
The aim of the study was to evaluate and compare the utility of DPOAEs and cochlear evoked<br />
<strong>po</strong>tentials for monitoring cochlear and eighth nerve functions during reversible cochlear<br />
ischemia.<br />
METHODS<br />
Fifteen young (2.5-6-mo old) albino rabbits weighing between 2.5 and 4.0 kg were used for<br />
this study. The animals were anesthetized routinely with an intramuscular injection of ketamine<br />
hydrochloride (50mg/kg) mixed with xylazine hydrochloride (10mg/kg). A head stabilization<br />
device was placed according to a standard procedure previously described by Telischi et al. and<br />
Morawski et al. (11, 17, 18). The first surgical step was a <strong>po</strong>st-auricular approach to ex<strong>po</strong>se the<br />
cochlea and round window (RW). Using an operating microscope, the middle ear was entered<br />
through the auditory bulla for placement of the laser-Doppler probe to measure cochlear blood<br />
flow (CBF). The cerebello<strong>po</strong>ntine angle was ex<strong>po</strong>sed via a sub-occipital <strong>po</strong>sterior craniotomy.<br />
With the use of the operating microscope, the <strong>po</strong>rus of the internal auditory canal (IAC) was distinguished.<br />
Then, CBF probe tip was <strong>po</strong>sitioned at RW niche to measure cochlear blood supply.<br />
DPOAEs res<strong>po</strong>nse functions were obtained for each ear using special probe at 4, 8 and 12 kHz<br />
GMF by measuring the DPOAEs level as a function of the primary tones at 60 dB SPL. Auditory<br />
res<strong>po</strong>nses were obtained using tone bursts at 4, 8 and 12 kHz and 70 dB SPL intensity. Needle<br />
electrodes for EcoG recordings were fixed in the neck muscles (reference), in the back muscles<br />
(ground) and as a measuring electrode the otic probe placed into the RW niche was used (10).<br />
The IAA compression inducing cochlear ischemia was maintained for 3-min. DPOAE-CBF data<br />
obtained in the first subgroup of animals and CM/CAP-CBF obtained in the second subgroup<br />
were recorded from the onset of ischemia through 20 min after reperfusion.<br />
The protocol for the care and use of rabbits was approved by the Institutional Animal Care<br />
and Use Committee.<br />
RESULTS<br />
In all ears following internal auditory artery (IAA) compression CBF was reduced to a background<br />
level. The DPOAEs phase increase for all frequencies occurred within a few seconds while<br />
the DPOAEs amplitudes decreased with slightly longer delay. CM/CAP reduction was analogous<br />
to DPOAEs pattern though in all cases 10-15 sec initial enhancement of CAP was recorded. After<br />
reperfusion, in both animal subgroups, DPOAEs and CM recovered in the same way for both<br />
compressions stabilizing near the baseline. CM measured for 3 min compression for all frequencies<br />
was reduced 1-1.5 dB, while DPOAEs were reduced only at 12 GMF kHz by 0.5-1 dB.<br />
Basically, DPOAEs and CM reduction and recovery patterns are very similar while CAP reduction<br />
and recovery patterns for test frequencies are different. CM and DPOAEs begin dropping in<br />
a couple of seconds, and then, during reperfusion begin recovering with relatively short time of<br />
delay ranging from 35-45 seconds at all test frequencies. CAP patterns occurring just after IAA<br />
compression reveal presence of initial elevation lasting 10-15 sec, and then, during next 20-30<br />
seconds CAP disappears. Following IAA release and subsequent cochlear reperfusion CAP begins<br />
returning though differently at all test frequencies. At 4 kHz CAP reaches 50% of its BL value in<br />
34-38 sec and 100% of its BL value in 42-48 sec after IAA release. At 8 kHz 50% and 100% of<br />
its BL value CAP reaches respectively in 49-54 sec and 91-100 sec, while at 12 kHz respectively<br />
in about 114-125 sec and 215-240 sec. Finally, CAP stabilizes above BL for 4 kHz, while at 8<br />
and 12 kHz around BL values. Figure 1 shows an example of DPOAE, CAP and CM changes following<br />
cochlear ischemia and reperfusion recorded at 8 kHz.
18<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
Fig. 1. Three minute cochlear<br />
ischemia effect on DPOAEs<br />
(black line), CM (lower gray line),<br />
and CAP (upper gray line) and<br />
their recovery patterns observed<br />
following cochlear reperfusion<br />
recorded at 8 kHz. DPOAEs<br />
–Distortion Product Otoacoustic<br />
Emissions; CM – Cochlear<br />
Microphonics; CAP – Com<strong>po</strong>und<br />
Action Potentials<br />
In the second part of the result section mutual relationships of DPOAEs, CM, CAP and CBF<br />
values were analyzed. As presented in table 1, during the first 60 sec of cochlear ischemia all<br />
parameters correlated each other on statistically significant levels (R ranged from +0.90 to +0.99;<br />
p
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 19<br />
ing both ischemia onset and reperfusion were non-linear revealing slightly different characteristics<br />
than DPOAEs. (10, 11, 17, 19, 20). Thus, due to CAP nonlinearity and its <strong>po</strong>orer correlation<br />
with CBF, mostly during reperfusion, its utility in term of intraoperative monitoring of cochlear<br />
ischemic processes in real time domain sees less useful than DPOAEs. Considering intraoperative<br />
monitoring of hearing in people the most complex tool seems to be ABR recording since it<br />
reflects the hearing pathway activity including spiral ganglion neurons and the cochlear nerve,<br />
cochlear nuclei and other structures. Theoretically, this technique could provide information<br />
about hearing pathway dysfunction and the anatomic level at which the hearing pathway was<br />
affected. Practically, in the operating room, electrostatic conditions are may not be optimal,<br />
resulting in a number of artifacts and, at times, only ABR wave V is detectable as an intraoperative<br />
monitoring parameter. Additionally, high level click-stimulation of about 70-100 dB nHL<br />
used and the number of averaged samples ranging between 250-1000 significantly limit both<br />
intraoperative monitoring in real time domain and sensitivity of monitoring (3, 21, 22, 23).<br />
DPOAEs effectively mirrored cochlear ischemia confirming earlier data and revealing stronger<br />
susceptibility of the basal part of the cochlea to damaging effect of reversible local ischemia. Different<br />
susceptibility of the apical and basal hair cells may be due to unequal levels of natural<br />
free-radical scavengers in basal and apical parts of the cochlea. The level of natural glutathione<br />
within the OHCs at the basal cochlea was found to be significantly lower than that at the apical<br />
turn, confirming a key role of the glutathione-dependent antioxidant system in protection<br />
against various factors damaging cochlear function (24). Radical scavengers, iron chelators and<br />
nitric oxide synthase inhibitors attenuated the damaging effects of ROS following<br />
ischemia/reperfusion episodes by enhancing efficacy of the antioxidant system within the<br />
cochlea (18, 25).<br />
Concluding, we showed that DPOAEs and CM showed very similar patterns of reduction and<br />
recovering during ischemia/reperfusion episode confirming its great usefulness to intraoperative<br />
monitoring of the cochlear function. CAP reduction and recovering during ischemia/reperfusion<br />
episode revealed slightly different characteristics than CM or DPOAEs. Neural function changes<br />
observed during both ischemia onset and reperfusion were non-linear. Due to this CAP nonlinearity,<br />
mostly during reperfusion, its utility for monitoring local ischemic processes is <strong>po</strong>orer<br />
than CM and DPOAEs, though CAP provides better information about the most peripheral neural<br />
auditory function.<br />
REFERENCES<br />
1. Kwartler JA, Luxford WM, Atknins JA, Shelton C. Facial nerve monitoring in acoustic tumor surgery. Otolaryngol Head<br />
Neck Surg 1991; 104: 814-817.<br />
2. Moller AR. Monitoring auditory function during operations to remove acoustic tumors. Am J Otol 1996; 17: 452-460.<br />
3. Colletti V, Fiorino FG. Advances in monitoring of seventh and eighth cranial nerve function during <strong>po</strong>sterior fossa surgery.<br />
Am J Otol 1998; 19: 503-512.<br />
4. Telischi FF, Stagner BB, Widick MP, Balkany TJ, Lonsbury-Martin BL. Distortion-product otoacoustic emission monitoring<br />
of cochlear blood flow. Laryngoscope 1998; 108: 837-842.<br />
5. Battista RA, Wiet RJ, Paauwe L. Evaluation of three intraoperative auditory monitoring techniques in acoustic neuroma<br />
surgery. Am J Otol 2000; 21: 244-248.<br />
6. Kwiek SJ, Bazowski P, Luszawski J, Namyslowski G, Morawski K, Lisowska G, Wolwender A. Monitoring of neurophysiological<br />
modalities during surgery for cerebello<strong>po</strong>ntine angle tumors. Personal experiences. Otolaryngol Pol<br />
2001; 55: 85-90.<br />
7. Morawski K, Telischi FF, Niemczyk K. A Model of Real Time Monitoring of the Cochlear Function During an Induced<br />
Local Ischemia. Hear Res 2006 – in press<br />
8. Morawski K, Namyslowski G, Lisowska G, Bazowski P, Kwiek S, Telischi FF. Intraoperative monitoring of the cochlear<br />
function using distortion product otoacoustic emissions (DPOAEs) in patients with cerebello-<strong>po</strong>ntine angle tumors.<br />
Otol Neurotol 2004; 25: 818-825.<br />
9. Bohórquez J, Ozdamar O, Morawski K, Telischi FF, Delgado R, Yavuz E. Neuromonitoring of Cochlea and Auditory<br />
Nerve with Multiple Extracted Parameters during Induced Hy<strong>po</strong>xia and Nerve Manipulation. Journal of Neural Engineering<br />
2005; 2(2): 1-10.<br />
10. Yavuz E, Morawski K, Telischi FF, Ozdamar O, Delagado RE, Manns F, Parel JM. Simultaneous measurement of electrocochleography<br />
and cochlear blood flow during cochlear hy<strong>po</strong>xia in rabbits. Journal of Neuroscience Methods<br />
2005; 147:55-64.
20<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
11. Telischi FF, Mom T, Agrama M, Stagner BB, Ozdamar O, Bustillo A, Martin GK. Comparison of the auditory-evoked<br />
brainstem res<strong>po</strong>nse wave I to distortion-product otoacoustic emissions resulting from changes to inner ear blood<br />
flow. Laryngoscope 1999; 109: 186-191.<br />
12. Kemp DT. Stimulated acoustic emissions from within the human auditory system. J Acoust Soc Am 1978; 64: 1386-<br />
1391.<br />
13. Probst R, Lonsbury-Martin BL, Martin GK. A review of otoacoustic emissions. J Acoust Soc Am 1991; 89: 2027-2067.<br />
14. Lonsbury-Martin BL, Probst R, Coats AC, Martin GK. Acoustic distortion products in rabbits. I. otoacoustic emissions<br />
by interference tones above f2. I. Basic features and physiological vulnerability. Hear Res 1987; 28: 173-189.<br />
15. Brownell WE. Outer hair cell electromotility and otoacoustic emissions. Ear Hear 1990; 11: 82-92.<br />
16. Whitehead ML, Lonsbury-Martin BL, Martin GK. Evidence for two discrete sources of 2f1-f2 distortion product otoacoustic<br />
emission in rabbits. II. Differential physiological vulnerability. J Acoust Soc Am 1992; 92: 2662-2682.<br />
17. Morawski K, Telischi FF, Merchant F, Namyslowski G, Lisowska G, Lonsbury-Martin BL. Preventing internal auditory<br />
canal vasospasm using topical papaverine: an animal study. Otol Neurotol 2003; 24: 918-926.<br />
18. Morawski K, Telischi FF, Merchant F, Abiy LW, Lisowska G, Namyslowski G. Role of mannitol in reducing <strong>po</strong>stischemic<br />
changes in distortion-product otoacoustic emissions (DPOAEs): a rabbit model. Laryngoscope 2003; 113:<br />
1615-1622.<br />
19. Mom T, Avan P, Romand R, Gilain L. Monitoring of functional changes after transient ischemia in gerbil cochlea.<br />
Brain Res 1997; 751: 20-30.<br />
20. Mom T, Avan P, Bonfils P, Gilain L. A model of cochlear function assessment during reversible ischemia in the Mongolian<br />
gerbil. Brain Res 1999; 4: 249-257.<br />
21. Nadol JB, Chiong CM, Ojemann RG, McKenna MJ, Martuza RL, Montgomery WW, Levine RA, Ronner SF, Glynn RJ.<br />
Preservation of hearing function in resection of acoustic neuroma. Laryngoscope 1992; 102: 1153-1158.<br />
22. Wazen JJ. Intraoperative monitoring of auditory function: experimental observations and new applications. Laryngoscope<br />
1994; 104: 446-455.<br />
23. Witzmann A, Reisecker F. Somatosensory and auditory evoked <strong>po</strong>tentials monitoring in tumor removal and brainstem<br />
surgery. In: Desmedt JE (Ed) Neuromonitoring in Surgery. Elsevier Science Publishers B.V. (Biomedical Division)<br />
1989; pp: 219-241.<br />
24. Sha SH, Taylor R, Forge A, Schacht J. Differential vulnerability of basal and apical hair cells is based on intrinsic<br />
susceptibility to free radicals. Hear Res 2001; 155: 1-8.<br />
25. Tabuchi K, Tsuji S, Asaka Y, Hara A, Kusakari J. Ischemia-reperfusion injury of the cochlea: effects of an iron chelator<br />
and nitric oxide synthase inhibitors. Hear Res 2001; 160: 31-36.
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 21<br />
EXPERIMENTAL MECONIUM ASPIRATION: EFFECT OF DEXAMETHASONE<br />
TREATMENT ON THE LUNG FUNCTIONS – A PILOT STUDY<br />
DANIELA MOKRA, ANDREA CALKOVSKA, JANKA BULIKOVA,<br />
MARIA PETRASKOVA, KAMIL JAVORKA<br />
Department of Physiology, Jessenius Faculty of Medicine, Comenius University, Martin, Slovak Republic<br />
A b s t r a c t<br />
Since corticosteroids reduce lung edema formation, inflammation, and vasoconstriction, effects of single-dose intravenous<br />
dexamethasone on the lung functions were studied in an animal model of MAS.<br />
Adult rabbits were ventilated with 100% oxygen. Three animals were sacrificed and used as controls. Other animals<br />
were administered 4 ml/kg of saline (n=4) or meconium suspension. When the respiratory failure developed, meconiuminstilled<br />
animals received 0.5 mg/kg of dexamethasone i.v. (n=6) or were left without treatment (n=5), and were ventilated<br />
for additional 5 hours. White blood cell (WBC) count was estimated and lung function parameters were measured.<br />
Then, animals were sacrificed and lungs were excised. Left lungs were lavaged to estimate WBC in the lavage fluid. Right<br />
lungs were dried to determine the wet/dry weight ratio.<br />
Meconium instillation decreased the lung compliance and gas exchange and increased right-to-left shunts, edema<br />
formation and WBC count in the lungs (all p
22<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
METHODS<br />
Design of experiments was approved by Local Ethics Committee of Jessenius Faculty of Medicine.<br />
Adult rabbits (chinchilla) of the mean body weight (b.w.) of 2.0±0.5 kg were anesthetized with intramuscular<br />
ketamine (20 mg/kg b.w.; Narkamon, S<strong>po</strong>fa, Czech Republic) and xylazine (5 mg/kg b.w.;<br />
Rometar, S<strong>po</strong>fa, Czech Republic) followed by continuous infusion of ketamine (20 mg/kg b.w./hour).<br />
Tracheotomy was performed and catheters were inserted into the femoral artery and right atrium for<br />
sampling the blood, and into the femoral vein to administer anesthetics. Animals were then paralyzed<br />
by pipecuronium bromide (0.3 mg/kg b.w./30 min; Arduan, Gedeon Richter, Hungary) and<br />
subjected to the pressure-controlled ventilator Beat-2 (Chirana, Slovakia). All animals were ventilated<br />
with a frequency of 30/min, fraction of inspired oxygen (FiO 2<br />
) of 0.21, peak inspiratory pressure<br />
(PIP) to keep a tidal volume (V T<br />
) between 7-9 ml/kg b.w. and no <strong>po</strong>sitive end-expiratory pressure<br />
(PEEP). After the stabilization, ventilatory parameters were recorded and samples of arterial and<br />
mixed venous blood were taken for blood gas analysis and estimation of hemoglobin and white blood<br />
cell (WBC) count. Then, three animals were killed by an overdose of anesthetics and were used as<br />
controls (Contr group, n=3). Other animals were instilled saline (Sal group, n=4) or suspension of<br />
human meconium (25 mg/ml), both at a dose of 4 ml/kg b.w., and from this moment were ventilated<br />
with 100 % oxygen. Then, animals received 5 ml of 4.2 % sodium bicarbonate to keep the blood<br />
pH in the normal range. Within 30 minutes after the meconium instillation respiratory failure developed,<br />
defined as >30% decrease in dynamic lung-thorax compliance (C dyn<br />
) and PaO 2<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 23<br />
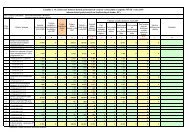
Table. 1. Lung function parameters before and after meconium (M) instillation and 30 minutes, 1, 2, 3, 4, and 5 hours of the treatment in saline-(Sal), meconium-<br />
(Meco) and meconium+dexamethasone-instilled (Meco+Dexa) groups. Data are expressed as means±SEM. Significant between-group differences: a Meco+Dexa vs. Sal<br />
(p
24<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
Fig. 1. Mean airway pressure (MAP)<br />
before and after meconium (M) instillation<br />
and after the treatment in saline-<br />
(Sal), meconium- (Meco), and meconium+dexamethasone-<br />
(Meco+Dexa)<br />
groups. Significant between-group differences:<br />
Meco vs. Sal since 30 min of<br />
the treatment; Meco+Dexa vs. Sal at 3,<br />
4, and 5 hours of the treatment;<br />
Meco+Dexa vs. Meco at 30 min of the<br />
treatment (all p
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 25<br />
Lung edema (lung wet/dry weight ratio)<br />
Meconium instillation increased fluid acummulation in the lungs compared to Sal group<br />
(p0.05). Number of blood neutrophils was lower in all Sal, Meco, and Meco+Dexa groups compared<br />
to controls (p
26<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
ethical problems, neonatal animals are rarely used as models of MAS. Nevertheless, with respect<br />
to the changes observed after meconium aspiration several-week-old rabbits and piglets were<br />
proved to be suitable animal models of MAS.<br />
Finally, we conclude that the single-dose intravenous administration of dexamethasone in<br />
rabbits with meconium aspiration diminished number of neutrophils in the lungs and ventilatory<br />
pressures and slightly reduced lung edema formation and OI. However, further testing of the<br />
corticosteroid use regarding the dosage and <strong>po</strong>ssible adverse effects, as well as the testing of<br />
other anti-inflammatory drugs in the management of MAS is warranted.<br />
REFERENCES<br />
1. Cleary GM, Wiswell TE. Meconium-stained amniotic fluid and meconium aspiration syndrome: an update. Pediatr<br />
Clin North Am 1998; 45: 955-81.<br />
2. Fernandes ABS, Zin WA, Rocco PRM. Corticosteroids in acute respiratory distress syndrome. Braz J Med Biol Res<br />
2005; 38 (2): 147-59.<br />
3. Jantz MA, Sahn SA. Corticosteroids in acute respiratory failure. Am J Respir Crit Care Med 1999; 160: 1079-100.<br />
4. Frantz ID, Wang NS, Thach BT. Experimental meconium aspiration: Effects of glucocorticoid treatment. J Pediatr<br />
1975; 86: 438-41.<br />
5. Yeh TF, Srinivasan G, Harris V, Pildes RS. Hydrocortisone therapy in meconium aspiration syndrome: a controlled<br />
study. J Pediatr 1977; 90: 140-3.<br />
6. Soukka H, Halkola L, Aho H, Rautanen M, Kero P, Kääpä P. Methylprednisolone attenuates the pulmonary hypertensive<br />
res<strong>po</strong>nse in <strong>po</strong>rcine meconium aspiration. Pediatr Res 1997; 42: 145-50.<br />
7. Holopainen R, Laine J, Halkola L, Aho H, Kääpä P. Dexamethasone treatment attenuates pulmonary injury in piglet<br />
meconium aspiration. Pediatr Res 2001; 49:162-8.<br />
8. Khan AM, Shabarek FM, Kutchback JW, Lally KP. Effects of dexamethasone on meconium aspiration syndrome in<br />
newborn piglets. Pediatr Res 1999; 46: 179-83.<br />
9. Wu JM, Yeh TF, Wang JY, Wang JN, Lin YJ, Hsieh WS, Lin CH. The role of inflammation in the development of pulmonary<br />
hypertension in newborn with meconium aspiration syndrome (MAS). Pediatr Pulmonol 1999; S18: 205-8.<br />
10. da Costa DE, Nair AK, Pai MG, Al Khusaiby SM. Steroids in full term infants with respiratory failure and pulmonary<br />
hypertension due to meconium aspiration syndrome. Eur J Pediatr 2001; 160: 150-3.<br />
11. Sevecova-Mokra D, Calkovska A, Drgova A, Javorka M, Javorka K. Treatment of experimental meconium aspiration<br />
syndrome with surfactant lung lavage and conventional vs. asymmetric high-frequency jet ventilation. Pediatr Pulmonol<br />
2004; 38: 285-91.<br />
12. Davey A, Kueser T, Turner H. Randomised controlled trial of early dexamethasone therapy in meconium aspiration<br />
syndrome. Pediatr Res 1995; 37: 329A.<br />
Acknowledgements<br />
The study was sup<strong>po</strong>rted by Grant VEGA No. 1/2306/05 and Grant of Comenius University No. 43/2004. Authors thank<br />
S. Svorkova, D. Kuliskova, and I. Stritz for technical assistance.
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 27<br />
FORMULATION AND IMPLEMENTATION OF THE NATIONAL<br />
IMMUNIZATION PROGRAMME IN SLOVAK REPUBLIC<br />
HENRIETA HUDEČKOVÁ 1 , MÁRIA SZILÁGYIOVÁ 2 , VLADIMÍR OLEÁR 3 , TIBOR BAŠKA 1 ,<br />
ŠTEFAN STRAKA 1<br />
1<br />
Department of Hygiene, Institute of Public Health, Jessenius Faculty of Medicine, Comenius University, Martin,<br />
2<br />
Clinic of Infectology, Jessenius Faculty of Medicine, Comenius University, Martin Faculty Hospital, Martin,<br />
3<br />
Aventis Pasteur, Žilina, Slovak Republic<br />
A b s t r a c t<br />
Active immunization of the <strong>po</strong>pulation against communicable diseases is the most successful and cost-effective preventive<br />
measure of modern medicine. Containment of the last outbreaks of small<strong>po</strong>x encircling the detected sources of<br />
infection by immune barriers using centrifugal vaccination was the key to substantial reduce the global incidence of <strong>po</strong>lio<br />
and other infectious diseases and thus to reduce the consequent disability and death. In 2005, the old centralized system<br />
of organization of preventive vaccination has been replaced by a decentralized one which necessitated its thorough<br />
formulation and new strategy of its implementation. The outcome of the work in this field has been the formulation of<br />
the National Immunization Programme of the Slovak Republic (NIP) for the coming years. The current system of preventive<br />
vaccination (NIP) is rational and scientifically based. Its implementation necessitates an active approach of all who<br />
participate in it: comprehensive surveillance, monitoring of epidemiological and economic situation and organization of<br />
vaccination. The indispensable requirement here is maintaining of the highest <strong>po</strong>ssible vaccination coverage of the particular<br />
sections of <strong>po</strong>pulation.<br />
K e y w o r d s : immunization, organization of immunization system, national immunization programme<br />
INTRODUCTION<br />
Active immunization of the <strong>po</strong>pulation against communicable diseases belongs to the most<br />
effective preventive measures. Its formulation and implementation deserves therefore the utmost<br />
attention and proficiency. Until the time the final document of national immunization could be<br />
issued, it usually would need the work of a well-coordinated team of experts in several scientific<br />
branches: vaccine-producers, paediatricians, infectologists, immunologists, microbiologists,<br />
toxicologists, biochemists, geneticists, economists, public health workers, and primarily epidemiologists.<br />
The team is usually coordinated and led by the Chief Epidemiologist of the respective<br />
country (1).<br />
The main objectives of our contribution are to sum up the links of the final chain of the<br />
National Immunization Programme in Slovakia, to bring up a brief review of the history of its<br />
development, and to define the main issues of the organization of immunization in Slovakia.<br />
HISTORY<br />
Before entering the recent history of immunization let us briefly review its “prehistory”. It<br />
began in ancient China with the first steps of prevention against small<strong>po</strong>x which was in that time<br />
the scourge of mankind taking high toll of lives. The method was based on the knowledge of <strong>po</strong>st<br />
infection immunity. The ancient Chinese used several ways how to introduce an artificial infection<br />
with the aim to build up the <strong>po</strong>stinfection immunity: scarification of material taken from<br />
small<strong>po</strong>x pustules to the skin, insufflation of the <strong>po</strong>wder made of the small<strong>po</strong>x crusts to nostrils,<br />
Address for corres<strong>po</strong>ndence:<br />
Henrieta Hudečková, MD, PhD, MPH, Assoc. Prof., Institute of Public Health,<br />
Comenius University in Bratislava,<br />
Jessenius Faculty of Medicine, Martin, Sklabinská 26, 037 53 Martin, Slovak Republic<br />
Phone: ++421 43 4132507, e-mail: hudeckova@jfmed.uniba.sk
28<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
etc. The consequent clinically mitigated disease made the person immune against natural infection,<br />
however it was not without risk. A small pro<strong>po</strong>rtion of such immunized persons could develop<br />
the clinically severe disease and even die. Another disadvantage of “variolation” was the<br />
spread of infection within the community. Variolation in Slovakia was first used by Jan Adam<br />
Reiman, the Chief Physician of the town of Prešov (1721). Some decades later, Edward Jenner,<br />
an English physician, motivated by the long-years’ experience of milkwomen, scarified material<br />
from vaccinia pustules (a harmless for man zoonosis) of a milkwoman infected from cow to a boy<br />
(1796). After curing from local reaction and general symptoms (fever, malaise), the boy, when<br />
ex<strong>po</strong>sed to natural infection with small<strong>po</strong>x, proved immune. Thus the era of “vaccination” started<br />
long before man discovered the infectious agents of communicable diseases. Then the way to<br />
scientific immunization had been shown by Pasteur, Koch and others, and in the last century,<br />
vaccination received its steady place as a leading preventive measure in control of communicable<br />
diseases. From that time the scope of preventive vaccines has extended tremendously, tri-,<br />
tetra- and penta-vaccines have been developed, as well as “split” and “subunit” influenza vaccines<br />
that can be used also to pregnant women and people weakened by chronic diseases. All<br />
these achievements can be ascribed to the advances of biotechnology and genetic engineering<br />
(2,3,4).<br />
RECENT ACTIVITIES OF THE GLOBAL MANAGEMENT OF IMMUNIZATION<br />
In 1974, WHO introduced the Expanded Programme on Immunization (EPI) which, along with<br />
the Small<strong>po</strong>x Eradication Programme, proved to be the greatest health protecting achievements<br />
of the 20 th century. However, the experiences have shown that the original expectations of EPI<br />
were not met, and, in the early 1990s, the Programme had to be extended by further diseases,<br />
new candidates for elimination and new operational objectives for immunization and surveillance<br />
of communicable diseases and expanded EPI – the EPI Plus. The new immunization visions and<br />
strategies for 2006-2015 have been outlined by WHO/UNICEF with the goals: extended vaccination,<br />
introduction of new vaccines and technologies, integration of immunization and surveillance<br />
of communicable diseases into health care system, and promotion of EPI to the context of<br />
mutual global relations. Highest attention is focused on the sup<strong>po</strong>rt and safety of vaccination,<br />
introduction of new antigens to practical use, elimination of measles and maintaining the <strong>po</strong>liofree<br />
status in European Region (4,5,6,7,8).<br />
ORGANIZATION OF IMMUNIZATION SYSTEM IN SLOVAKIA<br />
The outcome of the work of our team was the formulation of the National Immunization<br />
Programme of the Slovak Republic (NIP SR), a comprehensive preventive programme focused<br />
on prevention of infectious diseases preventable by vaccination (Fig.1). NIP in Slovakia is legislatively<br />
based on the acts issued in 1994 (NR SR No. 272/1994) and in 1997 (MZ SR No.<br />
79/1997).<br />
The centralized system of distribution of vaccines in Slovakia funded from state budget, has<br />
been changed from January 2005 to a decentralized system. Vaccines in decentralized system<br />
are financed by the health insurance companies and their distribution is maintained by the<br />
Guidelines of the Ministry of Health of the Slovak Republic issued in 2005. Vaccines used in NIP<br />
SR are categorized, and the preventive vaccination of children (category “V”) is completely free of<br />
charge, paid by health insurance. If parents for their children wish to use vaccines beyond the<br />
category “V”, they can be provided by vaccines of the category “S”, and the difference of price<br />
then should be paid from their personal budget.<br />
Regular compulsory vaccination of children should follow the terms and doses determined<br />
by the Vaccination Calendar (Fig. 2). New vaccine and vaccination should be considered to be<br />
integrated into NIP SR, and the Vaccination Calendar should then be adequately supplemented.
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 29<br />
Fig. 1 National Immunization Programme of Slovak Republic, 2005 (NIP); * Ministry of Health of the Slovak Republic; **<br />
Public Health Authorities of the Slovak Republic; *** Regional Public Health Authorities<br />
Fig. 2 Vaccination Calendar, Slovak Republic, 2005; * The table does not involve categorisation of vaccines
30<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
DISCUSSION<br />
The current system of preventive vaccination – NIP SR – is rational, scientifically based and<br />
economic, however, its implementation necessitates an active approach of all who participate<br />
in it: comprehensive surveillance, monitoring of epidemiological and economic situation and<br />
organization of vaccination (9,10).<br />
Favourable epidemiological situation in vaccination-preventable infectious diseases that we<br />
currently enjoy in Slovakia, is an im<strong>po</strong>rtant achievement first of all of epidemiologists and paediatricians,<br />
and maximum attention should be paid to maintain the highest vaccination coverage<br />
also in the future. The indispensable requirement here is strict sticking to vaccination programmes<br />
and maintaining the highest <strong>po</strong>ssible vaccination coverage of the respective sections of<br />
<strong>po</strong>pulation.<br />
NIP SR follows adequately the recommendations of WHO, and the application of particular<br />
vaccination doses is in full consonance with the legal regulations (NR SR No. 577/2004).<br />
CONCLUSIONS<br />
In recent time we can witnessed the spread of doubts and misinformation about the efficacy<br />
of vaccination, emphasizing the blown-up re<strong>po</strong>rts on its adverse effects and complications. These<br />
confusing pieces of information, lacking scientific arguments, may negatively influence the compliance<br />
of the public with NIP SR. All health workers and a reasonable majority of lay public<br />
should strongly reject such tendencies and sup<strong>po</strong>rt the NIP SR to maintain the favourable epidemiological<br />
situation in Slovakia.<br />
REFERENCES<br />
1. Ajjan N: Vaccination. Pasteur Mérieux Sérums et vaccins, Lyon, 1991, 188 pp. 3<br />
2. Atkinson W, Humiston S, Wolfe CH, Nelson R: Epidemiology and Prevention of Vaccine-Preventable Diseases. 5-th<br />
Edition, Department of Health & Human Services. Public Health Service, CDC, 1999, 289 pp.6<br />
3. Bagar B: 200 years from first vaccination against small<strong>po</strong>x. Med. Monit. 2, 1996, s.18-20.<br />
4. Public health surveillance. WHO, www.who.int/immunization_monitoring/burden/routine_surveillance<br />
5. Global Immunization Vision and Strategy 2006 – 2015. WHO/IVB/05.05, October 2005, 80 pp.<br />
6. Immunization against diseases of public health im<strong>po</strong>rtance. WHO, Fact sheet N.288, Marcch 2005.<br />
7. Salisbury DM, Olivé JM: Immunization in Europe. In:Plotkin SA, Orenstein WA, editors: Vaccines. 4-th ed. Philadelphia:<br />
Saunders, 2004, p.1387-1406.<br />
8. Vaccine-preventable Diseases and Immunization programme. Programme re<strong>po</strong>rt and future initiatives 2001-2005.<br />
EUR/05/505418, WHO, 2005. 25 pp.<br />
9. Making surveillance work. Modul 1: Rapid assessment of surveillance for vaccine-preventable diseases. WHO,<br />
Department of Vaccines and Biologicals, Geneva, 2001,24 pp.<br />
10. Making surveillance work. Modul 3: Logistic managemnet. WHO, Department of Vaccines and Biologicals, Geneva,<br />
2001,24 pp.<br />
Acknowledgement:<br />
This work is a part of VEGA No.1/2307/05 “Cost - effectiveness, benefit and safety of individual vaccination strategies of<br />
selected vaccination - preventable infectious diseases.”
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 31<br />
SCREENING OF DIABETIC FOOT IN NURSING PRACTICE<br />
JANA NEMCOVÁ 1 , TIBOR BAŠKA 2 , MILAN OCHODNICKÝ 3 , DUŠAN MIŠTUNA 4<br />
1<br />
Department of Nursing, Jessenius Faculty of Medicine, Comenius University, Martin, 2 Institute of Public Health,<br />
Department of Epidemiology, Jessenius Faculty of Medicine, Comenius University, Martin, 3 Internal Clinic I, Jessenius<br />
Faculty of Medicine, Comenius University, Martin Faculty Hospital 4 Clinic of Surgery I, Jessenius Faculty of Medicine,<br />
Comenius University,Martin Faculty Hospital, Martin, Slovak Republic<br />
A b s t r a c t<br />
Introduction. According to the recommendations of the International Consensus on the Syndrome of Diabetic Foot,<br />
most attention should be paid to its early detection. This can be considerably contributed also by screening assessment<br />
of the feet of diabetics accomplished by the nurse in diabetologic outpatient department. As a tool for this practice we<br />
recommend the nursing standard and the corres<strong>po</strong>nding nursing protocol.<br />
Methods. We carried out screening of 100 diabetic patients with diabetes mellitus of the 2nd type(DM-II) in the Diabetologic<br />
Outpatient Department in Martin Faculty Hospital, Slovak Republic. By means of a screening examination of<br />
neuropathy using the basic equipment – a monofilament 10-g (5.07) and a tuning fork 128Hz, we tried to identify the<br />
risk of diabetic foot. As a reference method served the diagnosed neuropathy established by a neurologist.<br />
Results. We have found 84.8% sensitivity and 79.4% specificity of our screening method. Analysing risk factors by<br />
gender we found statistically significantly higher occurrence in females: halluces, bone prominences, pains of feet. In the<br />
rest of risk factors there were no significant differences between genders.<br />
Discussion. This simple, inexpensive and timesaving method that can be accomplished also by nurses in primary<br />
care could bring, beside its contribution in preventive field, also economic effect. Even if this test cannot detect all patients<br />
in danger of diabetic foot, it could contribute to its earlier diagnosis in wider extent already on the level of outpatient<br />
diabetologic departments.<br />
K e y w o r d s : nursing standards, protocol, screening<br />
INTRODUCTION<br />
To the late complications of diabetes belongs also the syndrome of diabetic foot, affecting 15-<br />
25% of diabetics. The feet of diabetic patient are endangered by the disturbed integrity of the tissues.<br />
The most serious complications here are ulcerations and gangrenes, which can result in<br />
amputation of the affected part of the foot (in 0.5-1.0% of diabetic patients) (4). Considering the<br />
total number of diabetics it is an alarming number. In 2002 in Slovakia 3623 amputations were<br />
performed in diabetics (11).<br />
The current trend in professional training of nurses is that they should take over not only the<br />
res<strong>po</strong>nsibility when following the physician’s orders, but also contribute actively to improve the<br />
quality of health care provided to their patients.<br />
One of the <strong>po</strong>ssible ways is also using of standards in the field of assessment the risk of diabetic<br />
foot in their patients.<br />
The main objective of our work is to introduce the ways in which nurses can contribute to the<br />
detection of the risk of the development of diabetic foot. Our recommendation here is the screening<br />
evaluation of the feet of diabetics by a nurse.<br />
For the screening evaluation of diabetic feet we recommended a specific nursing standard<br />
and nursing protocol. The screened patients found in higher risk will then be referred to<br />
a neurologist for final diagnosis (reference method). Our objective was also to test the validity<br />
of our screening and nursing protocol worked out for this specific pur<strong>po</strong>se. In prevalence<br />
of risk factors found in our screening we also tried to identify the differences by genders. As<br />
a main marker for a risk we selected <strong>po</strong>sitive examination by monofilament and tuning fork<br />
Address for corres<strong>po</strong>ndence:<br />
Nemcová Jana, Department of Nursing, Comenius University.<br />
Jessenius Faculty of Medicine, Malá Hora 5, 036 01 Martin, Slovak Republic<br />
Phone: ++421 43 4133 326, e-mail: nemcova@jfmed.uniba.sk
32<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
according to guidelines of screening examinations of diabetic feet based on the respective<br />
international consensus (1). We also assume that entirely ischaemic form of diabetic foot represents<br />
only 7-13% of all forms.<br />
In our pro<strong>po</strong>sed nursing protocol for the diabetic foot screening also other risk factors are<br />
examined such as duration of the diabetic disease, compensation of the diabetes, body mass<br />
index (BMI), dryness of the skin, thylomas, mycoses, excoriations, small injuries, appropriateness<br />
of shoes, previous education of the patient regarding foot care.<br />
METHODS<br />
The main method was screening evaluation of the feet of diabetics carried out according to<br />
the recommendations of International Consensus for the Syndrome of Diabetic Foot (1) in Diabetological<br />
Outpatient Department of the Martin Faculty Hospital. The screening was carried out<br />
with patients with DM-II who came to the department for regular medical check-up from October<br />
2002 to May 2003.<br />
The screening provided information based on subjective data of the patient, from inspection<br />
of the foot and examination of the neuropathy using simple tools – monofilament 10-g (5.07) and<br />
a tuning fork 128Hz (6,8,9).<br />
When the deficiency of the pressure and/or vibration sensitivity were detected, the existing<br />
risk was recorded in the protocol for the risk for diabetic foot.<br />
The screening examination was performed according to the International Consensus for the<br />
Syndrome of Diabetic Foot (1). Table 1 shows the risk of development of diabetic foot found by<br />
the screening examination in our study. Table 2 informs about neurologically based diagnosis of<br />
<strong>po</strong>lyneuropathy among patients of the study.<br />
The protocol recorded also further risk factors: HbA 1C<br />
, body mass index, dryness of skin, thylomas,<br />
infection, inflammation, mycoses, small excoriations, ulcerations, amputations, halluces,<br />
prominences, pain, shoes, instructions to the patient.<br />
In statistical testing of the results the methods of descriptive statistics were used, and data<br />
were analysed by Student’s t-test and Χ 2 -test.<br />
For evaluation of the validity of screening examination we calculated its sensitivity and specificity<br />
(2), where the reference method was the medical diagnosis of <strong>po</strong>lyneuropathy.<br />
Table 1. Patients with DM-2 (n=100) at risk of the development of diabetic foot according to the screening examination<br />
Result of the<br />
females<br />
males<br />
total<br />
screening<br />
<strong>po</strong>sitive<br />
negative<br />
total<br />
33<br />
23<br />
56<br />
30<br />
14<br />
44<br />
63<br />
37<br />
100<br />
Table 2. Patients with DM-2 (n=100) with diagnosed <strong>po</strong>lyneuropathy<br />
Polyneuropathy<br />
diagnosed<br />
not diagnosed<br />
total<br />
females<br />
32<br />
24<br />
56<br />
males<br />
34<br />
10<br />
44<br />
total<br />
66<br />
34<br />
100
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 33<br />
RESULTS<br />
In our series of 100 patients with DM-II were 56 females and 44 males of average age of<br />
66.2±8.9 years, with the average to duration of the disease of DM-II 11.9±7.7 years.<br />
Statistically confirmed was the fact that the patients with the diagnosed <strong>po</strong>lyneuropathy had<br />
in average longer duration of diabetes (p=0.012).<br />
From the comparison of the diagnosed <strong>po</strong>lyneuropathy from the patients’ records and the<br />
examination of tactile and vibration sensitivity we have calculated 84.8% sensitivity and 79.4%<br />
specificity of the used nursing protocol (Table 3.).<br />
In analysis of the occurrence of risk factors between genders we have found statistically significant<br />
difference where females prevailed: halluces (37.5% females and 13.6% males,<br />
p=0.0076), bone prominences (25.0% females and 6.8% males, p=0.0163), pain of feet (10.7%<br />
females and 0.0% males, p=0,0251). In the rest of risk factors there were no significant differences<br />
found between genders.<br />
Table 3. Comparison of the results of screening and diagnosis of <strong>po</strong>lyneuropathy in patients with DM-II (n=100)<br />
risk diagnosed<br />
risk not diagnosed<br />
by the screening<br />
56<br />
by the screening<br />
10<br />
<strong>po</strong>lyneuropathy<br />
diagnosed<br />
<strong>po</strong>lyneuropathy not<br />
diagnosed<br />
sensitivity<br />
84.8%<br />
specificity<br />
79.4%<br />
7<br />
27<br />
DISCUSSION<br />
In practice we often meet the situation when patients have their feet examined for the first time<br />
when already serious problems exist evidencing for the advanced syndrome of diabetic foot. The late<br />
diagnosis of diabetic foot was also proved by the study of 690 patients hospitalised for diabetic foot at<br />
the Surgical Clinic of the Martin Faculty Hospital over the period of 20 years. Im<strong>po</strong>rtant is also time<br />
data evidencing for the fact that the patients experienced their first complains well before admission<br />
to the Surgical Clinic, in average 28.0 months, and they sought for the first medical check-up in average<br />
21 month before. This delay from the first symptoms to consequent surgical treatment resulted<br />
often to the development of extensive inflammatory-necrotic changes of the feet. Gangrenous changes<br />
on foot were present in 50.9% of males and 69.5% of females, while this group had not started specific<br />
treatment of the diabetic neuropathy and in their medical records there was no entry on subjective<br />
and objective changes evidencing for neuropathy despite their obvious presence (7).<br />
The pur<strong>po</strong>se of the screening examination is to detect the symptoms and signs of the risk of<br />
the further development of the diabetic foot in its earliest stage.<br />
The validity of the screening examination recommended by our group and involved in the<br />
nursing protocol has proved to be comparable with the literary data.<br />
In a prospective study of Rith Najarjane the patients were examined for the presence of vibration<br />
sensitivity (biothesiometer, tuning fork) and tactile sensitivity (monofilament 5.07), and the<br />
tests provided sensitivity of 90% and specificity of 86% for the prediction of the development of<br />
the ulcer or amputation. The patients were followed-up for 32 months from the development of<br />
first ulcer or amputation. The patients in whom sensoric sensitivity was disturbed had 5 times<br />
more frequent occurrence of ulcer or amputation than those in which no disturbance of the sensitivity<br />
was found (5).
34<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
The criterion for evaluation of the used tests, which are equal to ours, is in that study the<br />
objective findings of ulcers or amputations. In our study it is the comparison of our testing of<br />
sensitivity with the diagnosed <strong>po</strong>lyneuropathy by a neurologist.<br />
Current studies, e.g. Krahulec (3), recommend to carry out first the screening examination<br />
and not to refer patients straight to neurological examination, which is more expensive. In case<br />
of the suspect neuropathy diagnosed by a diabetologist or in patients screened as <strong>po</strong>sitive by<br />
a nurse, the reference neurological examination is indicated.<br />
The recommended nursing protocol could be involved among the documentation of diabetic<br />
patients as a regular com<strong>po</strong>nent already in diabetological outpatient department.<br />
This simple, cheap and timesaving method (performance of our screening examination lasts<br />
only about 15 minutes), which can be accomplished also by nurses of primary care, could bring<br />
also economic effect.<br />
Though our test is not able to detect all the cases, considering the delayed diagnosis of the<br />
diabetic foot as described in extensive study by Mištuna (7), it could be of assistance in earlier<br />
diagnosis already in patients referred to diabetological outpatient departments.<br />
REFERENCES<br />
1. Apelqvist J., Larson, J. What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes<br />
Metab Res Rev. 2000, no 16, (Suppl 1):S75- S83.<br />
2. Fletcher R.H., Fletcher S.W., WAGNER E.H.: Clinical Epidemiology. The Essentials. 3rd Edition, Baltimore, Philadelphia,<br />
London, Williams and Wilkins, 1996, 276 pp.<br />
3. Krahulec B. et al. Diabetic neuropathy. Current diagnostic and therapeutic <strong>po</strong>ssibilities. Bratislava: Lufema, 1999.<br />
119 s.<br />
4. Martinka E., Kurča E., Bencúr O. A complex view on the problem of diabetic foot. Lekárske listy, Odborná príloha<br />
Zdravotníckych novín, 2003, č. 14, s. 30-37.<br />
5. Mason J. et al. A systematic review of foot ulcer in patients with Type 2 diabetes mellitus I: prevention. Diabetic Med,<br />
1999, vol 16, pp. 801-812.<br />
6. Meier J.W.G. et al. Clinical diagnosis of diabetic <strong>po</strong>lyneuropathy with the diabetic neuropathy symptom and diabetic<br />
neuropathy examination scores. Diabetes Care, 2003, vol 26, no 3.<br />
7. Mištuna D. Diabetic foot. Martin: <strong>Jesseniova</strong> <strong>lekárska</strong> <strong>fakulta</strong> Univerzity Komenského, 2001. Habilitačná práca. 62<br />
s.<br />
8. Perkins B.A. et al. Simple screening Tests for peripheral neuropathy in the diabetes clinic. Diabetes Care, 2001, 24,<br />
pp 250-256.<br />
9. Vozár J., Kreze A., Klimeš I. Diabetes mellitus. Bratislava: Slovac Academic Press, 1992. 286 s.<br />
10. Zachary S., Feldman E.L. Update on diabetic neuropathy. Cur Opin Neurol, 2002, 15, pp 595-603.<br />
11. http://www.uzis.sk
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2 35<br />
Instructions to authors for manuscripts submitted to<br />
ACTA MEDICA MARTINIANA<br />
Journal Acta Medica Martiniana (AMM) publishes original papers and review articles of high<br />
quality from medical and biomedical sciences and from nursery, which have not been published<br />
yet, and will not be submitted for publication elsewhere. The papers are published in English,<br />
non-native English authors are res<strong>po</strong>nsible for the translation. The AMM is open access journal<br />
in print and online versions (http://www.jfmed.uniba.sk).<br />
The Editorial Board of AMM requires the treatments of manuscripts in accordance with uniform<br />
requirements of biomedical journal editors (Vancouver, 1978 with the revisions in 1997<br />
and 2000): Uniform Requirements for Manuscripts Submitted to Biomedical Journals:<br />
http://www.icmje.org./index.html<br />
Original papers in extenso should not exceed 15 pages (including references) and 5 figures<br />
or tables or their combination. The manuscript has to be written double-spaced (30 lines and<br />
maximum 60 keystrokes in a line per page) in the standard structure:<br />
1. The title page (separately) should have the title of the article, full names of the authors, the<br />
name of department(s) or institution(s), full address of the corres<strong>po</strong>nding author (including the<br />
phone, fax number and e-mail, if applicable).<br />
2. Abstract (separately) in the extent of 1 standard page. Three to five key words are appended<br />
at the end of the abstract page.<br />
3. Introduction should introduce into the problem and state the pur<strong>po</strong>se of the article.<br />
4. Methods should be complete to allow other workers to reproduce the results. Describe statistical<br />
methods. Indicate whether the procedure followed was in accordance with the ethical<br />
standards and with the Helsinki Declaration from 1975 as revised on 1983.<br />
5. Results: Present your results in logical sequence in the text, tables and illustrations.<br />
6. Discussion: Emphasize the new and im<strong>po</strong>rtant aspects of the study, link the conclusions<br />
with the presented goals of the study, relate the results to other relevant studies with a short<br />
summary of results at the end.<br />
7. References: All publication cited in the text should be presented in references. References<br />
have to be numbered consecutively in the order in which they are first mentioned within the<br />
text. Identify references in the text by Arabic numerals in parantheses. Use abbreviations of the<br />
journals according to Index Medicus (List of Journal Indexed in Index Medicus,<br />
http://www.nlm.nih.gov).<br />
Examples as follow (other examples are included on the web page being mentioned):<br />
Article in Journal: Vega KJ, Puna I, Krevsky B. Heart transplantation is associated with risk<br />
for pancreatobiliary disease. Ann Intern Med 1996; 124 (11): 980-3.<br />
Books and other Monographs: Bond J. Ageing of spy. New York: Churchill Livingstone; 1999.<br />
Chapter in a book: Phillips SJ, Whisnant JP. Hypertension and stroke. In: Laragh JH, Brenner<br />
BM, editors. Hypertension: pathophysiology, diagnosis, and management. 2nd ed. New York:<br />
Raven Press; 2001. p. 465-78.
36<br />
A C T A M E D I C A M A R T I N I A N A 2 0 0 6 6/2<br />
Illustrations and tables: Letters, numbers and symbols should be sufficient size that when<br />
reduced for publication each item will still be legible. Type legends for illustrations on a separate<br />
page. Each table has to be on a separate page too. Place explanatory matter in footnotes.<br />
Vertical rules should be omitted. Figures and tables should be numbered consecutively according<br />
to the order in which they have been first cited in text. Color illustrations will be accepted.<br />
However, the author well be expected to make a contribution towards the additional costs for<br />
color illustrations.<br />
Units of Measurement and Symbols: Measurements of length, height, weight, and volume<br />
should be re<strong>po</strong>rted in metric units. Temperatures should be given in degrees Celsius, blood pressure<br />
in millimeters of mercury. All other measurements should be re<strong>po</strong>rted in the terms of the<br />
International System of Units (SI).<br />
Review article should give personal view on current development in the author’s field of<br />
interest. The structure of the manuscript depends on the authors however, the manuscript must<br />
be prepared according to the instructions for full papers.<br />
One complete original manuscript with one set of high-quality prints of the figures and two<br />
complete copies, each containing tables and copies of the figures, must be submitted to the<br />
address of the Editorial Board Office.<br />
All manuscripts will be peer-reviewed anonymously by external experts pursuant to the standard<br />
evaluation criteria. Based on the review opinions, the Editorial Board will decide, whether<br />
the paper is to be included in the journal.<br />
After a manuscript is accepted for publication, one hardcopy of the final revised, accepted version<br />
of the paper must be submitted along with the same version on a 3.5-in. diskette. Text files<br />
should be saved as word processing document using Microsoft Word. The manuscipt has to<br />
include an attachment as follows: The work is an original, which has not been published in its full<br />
extent yet and will not be submitted elsewhere before a decision has been taken as to its acceptability<br />
by Acta Medica Martiniana. In consideration of the acceptance of the above work for publication,<br />
I do hereby assign and transfer to the publisher the copyright including display of the article<br />
in electronic form on web (open access).<br />
Publication of articles is free of charge excepting the color illustrations.<br />
AMM EDITORIAL BOARD<br />
Dept. of Physiology Jessenius Medical Faculty<br />
Comenius University<br />
Mala Hora Str. N. 4<br />
037 54 MARTIN<br />
SLOVAKIA