Idiopathic Thrombocytopenic Purpura (ITP) - Pathology
Idiopathic Thrombocytopenic Purpura (ITP) - Pathology
Idiopathic Thrombocytopenic Purpura (ITP) - Pathology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Idiopathic</strong> <strong>Thrombocytopenic</strong> <strong>Purpura</strong> 1<br />
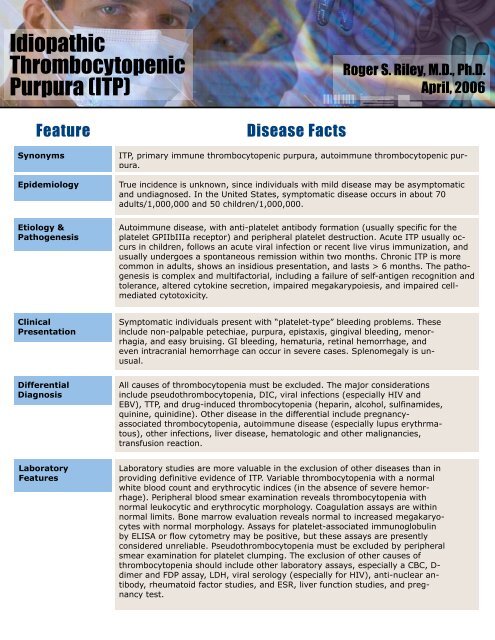
<strong>Idiopathic</strong><br />
<strong>Thrombocytopenic</strong><br />
<strong>Purpura</strong> (<strong>ITP</strong>)<br />
Roger S. Riley, M.D., Ph.D.<br />
April, 2006<br />
Feature<br />
Synonyms<br />
Epidemiology<br />
Etiology &<br />
Pathogenesis<br />
Disease Facts<br />
<strong>ITP</strong>, primary immune thrombocytopenic purpura, autoimmune thrombocytopenic purpura.<br />
True incidence is unknown, since individuals with mild disease may be asymptomatic<br />
and undiagnosed. In the United States, symptomatic disease occurs in about 70<br />
adults/1,000,000 and 50 children/1,000,000.<br />
Autoimmune disease, with anti-platelet antibody formation (usually specific for the<br />
platelet GPIIbIIIa receptor) and peripheral platelet destruction. Acute <strong>ITP</strong> usually occurs<br />
in children, follows an acute viral infection or recent live virus immunization, and<br />
usually undergoes a spontaneous remission within two months. Chronic <strong>ITP</strong> is more<br />
common in adults, shows an insidious presentation, and lasts > 6 months. The pathogenesis<br />
is complex and multifactorial, including a failure of self-antigen recognition and<br />
tolerance, altered cytokine secretion, impaired megakarypoiesis, and impaired cellmediated<br />
cytotoxicity.<br />
Clinical<br />
Presentation<br />
Symptomatic individuals present with “platelet-type” bleeding problems. These<br />
include non-palpable petechiae, purpura, epistaxis, gingival bleeding, menorrhagia,<br />
and easy bruising. GI bleeding, hematuria, retinal hemorrhage, and<br />
even intracranial hemorrhage can occur in severe cases. Splenomegaly is unusual.<br />
Differential<br />
Diagnosis<br />
All causes of thrombocytopenia must be excluded. The major considerations<br />
include pseudothrombocytopenia, DIC, viral infections (especially HIV and<br />
EBV), TTP, and drug-induced thrombocytopenia (heparin, alcohol, sulfinamides,<br />
quinine, quinidine). Other disease in the differential include pregnancyassociated<br />
thrombocytopenia, autoimmune disease (especially lupus erythrmatous),<br />
other infections, liver disease, hematologic and other malignancies,<br />
transfusion reaction.<br />
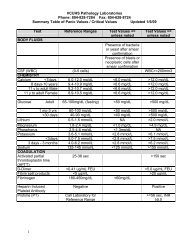
Laboratory<br />
Features<br />
Laboratory studies are more valuable in the exclusion of other diseases than in<br />
providing definitive evidence of <strong>ITP</strong>. Variable thrombocytopenia with a normal<br />
white blood count and erythrocytic indices (in the absence of severe hemorrhage).<br />
Peripheral blood smear examination reveals thrombocytopenia with<br />
normal leukocytic and erythrocytic morphology. Coagulation assays are within<br />
normal limits. Bone marrow evaluation reveals normal to increased megakaryocytes<br />
with normal morphology. Assays for platelet-associated immunoglobulin<br />
by ELISA or flow cytometry may be positive, but these assays are presently<br />
considered unreliable. Pseudothrombocytopenia must be excluded by peripheral<br />
smear examination for platelet clumping. The exclusion of other causes of<br />
thrombocytopenia should include other laboratory assays, especially a CBC, D-<br />
dimer and FDP assay, LDH, viral serology (especially for HIV), anti-nuclear antibody,<br />
rheumatoid factor studies, and ESR, liver function studies, and pregnancy<br />
test.
<strong>Idiopathic</strong> <strong>Thrombocytopenic</strong> <strong>Purpura</strong> 2<br />
Feature<br />
Treatment<br />
Disease Facts<br />
Supportive care, including platelet transfusions, must be provided until remission<br />
occurs or treatment is effective. No specific treatment is usually provided<br />
for children with platelet counts >30,000/µL or adults with >50,000 platelets/<br />
µL. Intravenous immunoglobulin (IVIG, IV Rh immune globulin, IV anti-Rh(D)<br />
and corticosteroids are the first line of therapy for patients with severe thrombocytopenia.<br />
Rituximab is often used in patients with refractory <strong>ITP</strong>.<br />
References<br />
Aledort LM et al. Prospective<br />
screening of 205 patients with<br />
<strong>ITP</strong>, including diagnosis, serological<br />
markers, and the relationship<br />
between platelet<br />
counts, endogenous thrombopoietin,<br />
and circulating antithrombopoietin<br />
antibodies.<br />
Am J Hematol 76(3):205-213,<br />
2004.<br />
Andersson PO, Wadenvik H.<br />
Chronic idiopathic thrombocytopenic<br />
purpura (<strong>ITP</strong>): molecular<br />
mechanisms and implications<br />
for therapy. Expert<br />
Rev Mol Med 6(24):1-17,<br />
2004.<br />
Blackwell J, Goolsby MJ. Diagnosis<br />
and treatment of idiopathic<br />
thrombocytopenic purpura.<br />
J Am Acad Nurse Pract<br />
15(6):244-245, 2003.<br />
Blanchette VS, Carcao M.<br />
Childhood acute immune<br />
thrombocytopenic purpura: 20<br />
years later. Semin Thromb<br />
Hemost 29(6):605-617, 2003.<br />
Cines DB, Bussel JB. How I<br />
treat idiopathic thrombocytopenic<br />
purpura (<strong>ITP</strong>). Blood<br />
106(7):2244-2251, 2005.<br />
Cines DB, McMillan R. Management<br />
of adult idiopathic<br />
thrombocytopenic purpura.<br />
Annu Rev Med 56:425-442,<br />
2005.<br />
Drachman JG. Inherited<br />
thrombocytopenia: when a<br />
low platelet count does not<br />
mean <strong>ITP</strong>. Blood 103(2):<br />
390-398, 2004.<br />
George JN, Vesely SK. Immune<br />
thrombocytopenic<br />
purpura--let the treatment fit<br />
the patient. N Engl J Med<br />
349(9):903-905, 2003.<br />
Introna M, Golay J, Barbui T.<br />
Rituximab: a new therapeutic<br />
tool for primary immune<br />
thrombocytopenic purpura?<br />
Haematologica 88(5):<br />
482-484, 2003.<br />
Kojouri K, George JN. Recent<br />
advances in the treatment of<br />
chronic refractory immune<br />
thrombocytopenic purpura.<br />
Int J Hematol 81(2):119-125,<br />
2005.<br />
Kravitz MS, Shoenfeld Y.<br />
<strong>Thrombocytopenic</strong> conditionsautoimmunity<br />
and hypercoagulability:<br />
commonalities and<br />
differences in <strong>ITP</strong>, TTP, HIT,<br />
and APS. Am J Hematol<br />
80(3):232-242, 2005.<br />
Kumar M et al. Treatment,<br />
outcome, and cost of care in<br />
children with idiopathic<br />
thrombocytopenic purpura.<br />
Am J Hematol 78(3):181-187,<br />
2005.<br />
Kuwana M et al. Initial laboratory<br />
findings useful for predicting<br />
the diagnosis of idiopathic<br />
thrombocytopenic purpura.<br />
Am J Med118(9):1026-<br />
1033, 2005.<br />
McMillan R. Antiplatelet antibodies<br />
in chronic adult immune<br />
thrombocytopenic purpura:<br />
assays and epitopes. J<br />
Pediatr Hematol Oncol 25<br />
Suppl 1:S57-61, 2003.<br />
Munson BL. Myths and facts<br />
...about idiopathic thrombocytopenic<br />
purpura. Nursing<br />
34(11):76, 2004.<br />
Provan D, Newland A. Fifty<br />
years of idiopathic thrombocytopenic<br />
purpura (<strong>ITP</strong>): management<br />
of refractory itp in<br />
adults. Br J Haematol<br />
118(4):933-944, 2002.<br />
Rodeghiero F. <strong>Idiopathic</strong><br />
thrombocytopenic purpura: an<br />
old disease revisited in the era<br />
of evidence-based medicine.<br />
Haematologica 88(10):1081-<br />
1087, 2003.<br />
Sandler SG. Review: immune<br />
thrombocytopenic purpura: an<br />
update for immunohematologists.<br />
Immunohematol<br />
20(2):112-117, 2004.<br />
Shirahata A, et al. Consensus<br />
guideline for diagnosis and<br />
treatment of childhood idiopathic<br />
thrombocytopenic purpura.<br />
Int J Hematol 83(1):29-<br />
38, 2006.<br />
Stasi R, Provan D. Management<br />
of immune thrombocytopenic<br />
purpura in adults.<br />
Mayo Clin Proc 79(4):504-<br />
522, 2004.<br />
Terrell DR et al. The incidence<br />
of thrombotic thrombocytopenic<br />
purpura-hemolytic<br />
uremic syndrome: all patients,<br />
idiopathic patients, and<br />
patients with severe ADAMTS-<br />
13 deficiency. J Thromb Haemost<br />
3(7):1432-1436.<br />
Vianelli N et al. Efficacy and<br />
safety of splenectomy in immune<br />
thrombocytopenic purpura:<br />
long-term results of 402<br />
cases. Haematologica<br />
90(1):72-77, 2005.
<strong>Idiopathic</strong> <strong>Thrombocytopenic</strong> <strong>Purpura</strong> 3<br />
References<br />
Yildirmak Y et al. Antiplatelet<br />
antibodies and their correlation<br />
with clinical findings in<br />
childhood immune thrombocytopenic<br />
purpura. Acta Haematol<br />
113(2):109-112, 2005.<br />
Zhou B, Zhao H, Yang RC,<br />
Han ZC. Multi-dysfunctional<br />
pathophysiology in <strong>ITP</strong>. Crit<br />
Rev Oncol Hematol<br />
54(2):107-116, 2005.