Spring/Summer 2002 - University of Rochester Medical Center
Spring/Summer 2002 - University of Rochester Medical Center
Spring/Summer 2002 - University of Rochester Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
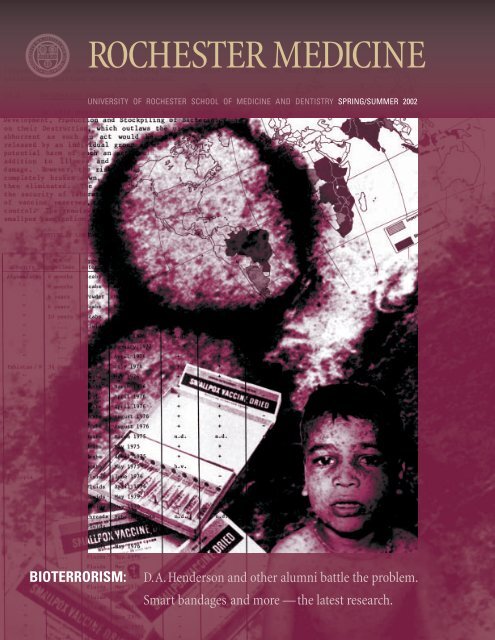
ROCHESTER MEDICINE<br />
UNIVERSITY OF ROCHESTER SCHOOL OF MEDICINE AND DENTISTRY SPRING/SUMMER <strong>2002</strong><br />
BIOTERRORISM:<br />
D.A. Henderson and other alumni battle the problem.<br />
Smart bandages and more —the latest research.
I’d<br />
like to congratulate Dean Ed Hundert on<br />
his upcoming appointment as president <strong>of</strong> Case<br />
Western Reserve <strong>University</strong>. From the work he<br />
has done here at <strong>Rochester</strong>, I can safely say<br />
that Case Western will gain immeasurably from<br />
his energy and vision.<br />
Dr. Hundert’s five years at <strong>Rochester</strong><br />
have been extremely fertile ones. As the architect<br />
<strong>of</strong> the Double Helix curriculum, which<br />
intertwines basic science and clinical work<br />
from year one, Dean Hundert led the School<br />
<strong>of</strong> Medicine and Dentistry through historic<br />
change. That change culminated in February<br />
2001, when the leading educators <strong>of</strong> the Liaison<br />
Committee on <strong>Medical</strong> Education announced<br />
the results <strong>of</strong> its inspection <strong>of</strong> our school. They<br />
had “no areas <strong>of</strong> concern — an unprecedented<br />
finding in American medical education.”<br />
And so, Dr. Hundert’s legacy will<br />
continue on as the mantle is passed to David<br />
Guzick, M.D., Ph.D., who has been named the<br />
ninth dean <strong>of</strong> the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong><br />
School <strong>of</strong> Medicine and Dentistry. Dr. Guzick<br />
has been with the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> since<br />
1995, when he joined us to serve as chair <strong>of</strong> the<br />
Department <strong>of</strong> Obstetrics and Gynecology.<br />
I hope you’ll join me in congratulating<br />
Dr. Hundert on both his contributions here and<br />
his new undertaking, and in congratulating<br />
Dr. Guzick as he carries us through the next<br />
chapter <strong>of</strong> innovative education here at <strong>Rochester</strong>.<br />
We’ve dedicated this issue <strong>of</strong> <strong>Rochester</strong><br />
Medicine to <strong>Rochester</strong> faculty and alumni<br />
working on the bioterrorism problem.<br />
The initial shock and horror <strong>of</strong><br />
September 11 may have subsided somewhat,<br />
but still we feel uneasy. The first steps have<br />
been taken to protect ourselves, but still we<br />
wonder what we need to do now. We’ve dealt<br />
with the crisis with great resolve, but still<br />
we must ask, “What about the future?”<br />
<strong>Rochester</strong> graduates and faculty are<br />
now at the forefront <strong>of</strong> preparations against a<br />
bioterrorist attack. They’re working throughout<br />
the federal government on plans and technologies<br />
that will protect whole communities.<br />
One alumnus, D. A. Henderson, was<br />
having a remarkable career even before he<br />
became director <strong>of</strong> the new federal Office <strong>of</strong><br />
Public Health Preparedness in November.<br />
Henderson led the World Health Organization’s<br />
effort in the ’60s and ’70s to eradicate smallpox.<br />
That project is still considered one <strong>of</strong> the<br />
greatest successes in the history <strong>of</strong> public<br />
health. In this issue, we take a look at how<br />
he did it, and how he’s being asked to make<br />
the world safe once again from smallpox.<br />
We also take a look at cutting-edge<br />
research being done here at the <strong>Medical</strong> <strong>Center</strong><br />
and by alumni. From better vaccines to “smart<br />
bandages” that one day could detect the presence<br />
<strong>of</strong> dangerous bacteria, scientists are<br />
moving quickly to find technological solutions<br />
to the bioterrorism problem.<br />
The government has been just as quick<br />
to act. When the NIH decided it needed to test<br />
a diluted form <strong>of</strong> smallpox vaccine, <strong>Rochester</strong><br />
was one <strong>of</strong> only four institutions chosen to<br />
conduct the study.<br />
In this issue we wanted to show how<br />
work is continuing on the bioterrorism front.<br />
That work, which actually began long before<br />
September 11, will help make us all safer.<br />
Jay H. Stein, M.D.<br />
Senior Vice President & Vice Provost for Health<br />
Affairs, <strong>Medical</strong> <strong>Center</strong> & Strong Health CEO<br />
SPRING / SUMMER <strong>2002</strong> 1
It<br />
is with very deep emotions that I write<br />
to inform you that on July 31st I will be stepping<br />
down as dean <strong>of</strong> the School <strong>of</strong> Medicine<br />
and Dentistry and pr<strong>of</strong>essor <strong>of</strong> psychiatry and<br />
medical humanities at the <strong>University</strong> <strong>of</strong><br />
<strong>Rochester</strong>, to become president <strong>of</strong> Case Western<br />
Reserve <strong>University</strong> on August 1, <strong>2002</strong>. These<br />
five years at the School <strong>of</strong> Medicine and<br />
Dentistry have been the most energizing <strong>of</strong><br />
my pr<strong>of</strong>essional life, and I cannot tell you<br />
what a privilege it has been to work with<br />
such remarkable people as yourselves. I am<br />
confident that <strong>Rochester</strong>’s educational paradigm<br />
will continue to set the national standard in<br />
medical education into the future, thanks<br />
to the remarkable students, faculty, administrators,<br />
staff, and alumni with whom it has been my<br />
great pleasure to work so hard. You are amazing.<br />
The opportunity to serve as president <strong>of</strong><br />
Case Western Reserve <strong>University</strong> is unique in a<br />
lifetime. CWRU is poised to rethink the meaning<br />
<strong>of</strong> an undergraduate education at a research<br />
university, with a plan to integrate “theory and<br />
experience” throughout the entire curriculum<br />
(a university-wide Double Helix!). They also<br />
face exciting challenges and unique opportunities<br />
in a number <strong>of</strong> their graduate and<br />
pr<strong>of</strong>essional schools, and have a Master Plan<br />
to rebuild the entire campus over the coming<br />
decade. I would add that CWRU is also poised<br />
to become a partner with the city <strong>of</strong> Cleveland,<br />
so that just as our medical school has a mission<br />
to make <strong>Rochester</strong> the healthiest city, Case<br />
Western Reserve as a whole will be engaging<br />
all <strong>of</strong> its schools and programs with a goal<br />
<strong>of</strong> making Cleveland the best possible city.<br />
Leading this effort represents a truly unique<br />
opportunity for leadership and service both<br />
to higher education and the civic role <strong>of</strong><br />
universities.<br />
I will work hard with Dr. Stein, Dean<br />
Cory-Slechta, and the rest <strong>of</strong> the senior leadership<br />
team over the coming months to ensure<br />
a smooth transition and to make sure the positive<br />
momentum we have at URMC continues<br />
unabated. This is a remarkable institution<br />
with some <strong>of</strong> the finest people it has ever been<br />
my pleasure to know. I will definitely stay in<br />
touch over the years ahead and look forward<br />
to hearing news <strong>of</strong> how our new educational<br />
paradigm has spread beyond medical student<br />
education through graduate and continuing<br />
medical education, so that the lifelong<br />
learning <strong>of</strong> both cutting-edge science and<br />
humanistic clinical practice continues to be the<br />
trademark <strong>of</strong> a <strong>Rochester</strong>-educated physician.<br />
I will miss you.<br />
Edward M. Hundert, MD<br />
Dean <strong>of</strong> the School <strong>of</strong> Medicine and Dentistry<br />
2<br />
ROCHESTER MEDICINE
CONTENTS<br />
ROCHESTER MEDICINE<br />
FEATURES<br />
10 Best prepare for the worst: How D. A . Henderson saved the planet<br />
from smallpox and how he plans to do it again<br />
17 War rooms, new vaccines and meetings with the President<br />
20 Technology vs. terrorism<br />
24 <strong>Rochester</strong> provides a national model<br />
28 A lasting memorial<br />
4 <strong>Medical</strong> <strong>Center</strong> rounds<br />
29 School news<br />
37 Alumni news<br />
40 Class notes<br />
47 In memoriam<br />
DEPARTMENTS<br />
<strong>Rochester</strong> Medicine is published by: The <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong>,<br />
Department <strong>of</strong> Public Relations and Communications, in conjunction with the<br />
Department <strong>of</strong> <strong>Medical</strong> Alumni Relations and Development<br />
Teri D’Agostino, Director <strong>of</strong> Public Relations and Communications<br />
Mark Liu, Editor<br />
Leslie Orr and Tom Rickey, Contributing Writers<br />
Mitchell Christensen, Art Director<br />
Randy Tagg and Vince Sullivan, Photographers<br />
Rita J. Ciarico, Editorial Assistant<br />
Christopher Raimy, Director <strong>of</strong> Development for <strong>Medical</strong> Alumni Programs<br />
Christina Mancini, Associate Director <strong>of</strong> <strong>Medical</strong> Alumni Relations<br />
For questions or comments, contact:<br />
Department <strong>of</strong> Alumni Relations and Development<br />
300 East River Road, <strong>Rochester</strong>, NY 14627<br />
1–800–333–4428 585–273–5954 Fax 585–461–2081<br />
E-mail address: <strong>Rochester</strong>MedicineMagazine@urmc.rochester.edu<br />
Cover montage images<br />
and selected D. A.<br />
Henderson story photos<br />
and graphics from: The<br />
Global Eradication <strong>of</strong><br />
Smallpox: Final report <strong>of</strong><br />
the Global Commission for<br />
the Certification <strong>of</strong> Smallpox<br />
Eradication. World Health<br />
Organization: Geneva,<br />
1980. Basu, R.N., Z. Jezek<br />
and N.A. Ward. Eradication<br />
<strong>of</strong> Smallpox from India.<br />
World Health Organization:<br />
Faridabad, India, 1979.<br />
SPRING / SUMMER <strong>2002</strong> 3
medical center rounds<br />
Strong deploys decade’s “single biggest<br />
advancement” for Parkinson’s patients<br />
The FDA recently put its stamp <strong>of</strong> approval on<br />
a revolutionary treatment that can enhance<br />
the quality <strong>of</strong> life for patients in the advanced<br />
stages <strong>of</strong> Parkinson’s disease.<br />
In Deep Brain Stimulation therapy,<br />
an electrode device is implanted in precisely<br />
targeted areas <strong>of</strong> the brain to deliver carefully<br />
controlled pulses <strong>of</strong> electrical stimulation,<br />
which relieves the debilitating slowness, stiffness<br />
and shaking that characterize Parkinson’s.<br />
This creates a whole new treatment option for<br />
advanced Parkinson’s disease patients, and also<br />
is the first time that motor function is actually<br />
further improved. Physicians at the <strong>University</strong><br />
<strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong> (URMC) are using<br />
the new technique, with encouraging results.<br />
“From my perspective, this is the single<br />
biggest advancement in treatment for<br />
Parkinson’s in the last decade,” says Timothy<br />
Counihan, M.D., assistant pr<strong>of</strong>essor <strong>of</strong><br />
neurology at the <strong>Medical</strong> <strong>Center</strong> and codirector<br />
<strong>of</strong> the Strong Surgical Treatment<br />
Program for Movement Disorders. “For most<br />
patients, medication eventually becomes ineffective<br />
as the disease progresses, leaving the<br />
person with no real treatment alternatives<br />
but a slow, inexorable deterioration. Deep Brain<br />
Stimulation provides a marked improvement<br />
in motor function, allowing many patients to<br />
achieve a better quality <strong>of</strong> life.”<br />
According to Counihan, clinical trials<br />
using the electronic implants have shown that<br />
patients have up to a 60 percent improvement<br />
in motor function (as measured by the standard<br />
Unified Parkinson’s Disease Rating scale)<br />
three years following the surgery, despite a<br />
substantial reduction in their medication<br />
usage, and despite the fact that the disease<br />
progressed during the same three-year period.<br />
Robert Bakos, M.D., associate pr<strong>of</strong>essor<br />
<strong>of</strong> neurosurgery at URMC, says that the surgery<br />
is unique because the patient is awake to help<br />
guide the placement <strong>of</strong> the electrodes.<br />
We use computers to pinpoint the<br />
specific “ area on the brain for placement <strong>of</strong><br />
the electrodes, but then we work with the<br />
patient during the surgery to find the precise<br />
area that is the major source <strong>of</strong> Parkinson’s<br />
disease symptoms,” says Bakos. “We then ask<br />
the patient to hold a c<strong>of</strong>fee cup or write on<br />
a pad as we fine-tune the electric impulse.”<br />
This surgery is followed by another<br />
minor procedure, in which the electrodes are<br />
connected by lead wires under the skin to a<br />
pulse generator — similar to a pacemaker —<br />
implanted under the collarbone. Medtronics<br />
Inc., <strong>of</strong> Minneapolis, makes the device, called<br />
Activa Parkinson’s Control Therapy.<br />
“Because the amount <strong>of</strong> electricity is<br />
adjustable, we can provide significant symptom<br />
4<br />
ROCHESTER MEDICINE
medical center rounds<br />
Largest ever study <strong>of</strong> Parkinson’s disease<br />
Active Parkinson’s Control Therapy.<br />
relief while minimizing side effects,” Bakos<br />
notes. “And the therapy is reversible, which<br />
means patients will be able to pursue new treatments<br />
that may be developed in the years ahead.”<br />
A debilitating disease<br />
One million Americans are estimated<br />
to have Parkinson’s disease, a progressive and<br />
degenerative movement disorder that gradually<br />
robs patients <strong>of</strong> their independence. The cause<br />
<strong>of</strong> Parkinson’s is unknown, but the symptoms<br />
stem from the degeneration <strong>of</strong> neurons (brain<br />
cells) that produce dopamine. Dopamine is<br />
a neurotransmitter that enables communication<br />
among the brain cells involved in motor<br />
control. The electrical stimulation acts on<br />
the malfunctioning circuits in the brain.<br />
Patients are typically put on medication<br />
to control the symptoms. However, after a long<br />
A neurologist at the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong><br />
<strong>Medical</strong> <strong>Center</strong> has been chosen to lead a study<br />
<strong>of</strong> 3,000 patients around the country who have<br />
Parkinson’s disease. Karl Kieburtz, M.D.,<br />
pr<strong>of</strong>essor <strong>of</strong> neurology, will lead the largest<br />
effort yet to find a way to slow the progression<br />
<strong>of</strong> the disease.<br />
The five-year study, to be launched<br />
in late <strong>2002</strong> or in 2003, will be funded with<br />
approximately $6.5 million from the National<br />
Institutes <strong>of</strong> Health.<br />
Roughly one million adults in North<br />
America have Parkinson’s disease, in which<br />
several hundred thousand cells in the substantia<br />
nigra region <strong>of</strong> the brain degenerate and die.<br />
Currently, doctors use a range <strong>of</strong><br />
medications to treat the classic symptoms —<br />
slowness <strong>of</strong> movement, difficulty walking and<br />
swallowing, muscle stiffness, tremors, and<br />
rigidity — but there is no way to slow or<br />
prevent the death <strong>of</strong> brain cells.<br />
“There is not a lot out there at this point<br />
period <strong>of</strong> time (10 to 20 years) drugs become<br />
ineffective. In these late stages <strong>of</strong> the disease,<br />
patients <strong>of</strong>ten experience uncontrollable<br />
shaking and flailing as a side effect <strong>of</strong> medication<br />
to treat Parkinson’s. The combination <strong>of</strong><br />
symptoms and side effects leads to self-isolation<br />
and avoidance <strong>of</strong> public situations, and eventually<br />
can cause patients to become totally<br />
dependent on others for their care.<br />
Since 1995, about 15,000 people in<br />
Europe, Canada and Australia have been<br />
implanted with “brain pacemakers” to treat<br />
their disease. Doctors at Strong Memorial<br />
Hospital have a waiting list <strong>of</strong> 20 people<br />
eligible for the surgery, and are working<br />
with insurance companies to provide coverage<br />
before scheduling the surgery. Medicare is<br />
currently working on its payment policy as well.<br />
to protect patients from further damage,” says<br />
Kieburtz. “We have several candidates, but thus<br />
far none has been shown to slow the disease.”<br />
Kieburtz will coordinate doctors from<br />
42 sites around North America who will track<br />
the health <strong>of</strong> the patients over a five-year<br />
period. The team will test the effectiveness<br />
<strong>of</strong> various substances at slowing the disease’s<br />
progression. Possibilities include obscure<br />
compounds in development in laboratories,<br />
as well as everyday substances like caffeine<br />
and nicotine.<br />
In similar studies bringing together<br />
doctors and patients around the country,<br />
<strong>Medical</strong> <strong>Center</strong> physicians recently led a team<br />
that found that a skin patch under development<br />
to treat Parkinson’s disease appears<br />
as effective as traditional oral medications.<br />
The research is being done through the<br />
Department <strong>of</strong> Neurology’s Clinical Trials<br />
Coordination <strong>Center</strong>, where Kieburtz serves<br />
as director.<br />
” Cache” in on<br />
research news<br />
The latest news on the <strong>University</strong>’s research<br />
in science, medicine and engineering is<br />
available via e-mail through the ScienceCache<br />
newsletter. Once or twice each month,<br />
subscribers receive a concise synopsis <strong>of</strong> the<br />
latest news in these areas, with links to the<br />
Web for more information. It’s a handy way to<br />
keep track <strong>of</strong> the <strong>University</strong>’s top research news.<br />
For more information or to subscribe, send<br />
a note to trickey@admin.rochester.edu,<br />
or send a message with the words “subscribe<br />
sciencecache” in the body <strong>of</strong> the note to<br />
majordomo@listener.uis.rochester.edu.<br />
SPRING / SUMMER <strong>2002</strong> 5
medical center rounds<br />
help prevent<br />
suicide is the 3rd leading cause <strong>of</strong> death among young adults<br />
suicide suicide is is the the 3rd 3rd leading leading cause cause <strong>of</strong> <strong>of</strong> death death among among young young adults adults<br />
$3.2 million grant will help prevent suicide here and in China<br />
Researchers at the nation’s leading center<br />
for the study and prevention <strong>of</strong> suicide have<br />
received $3.2 million from the National<br />
Institutes <strong>of</strong> Health to conduct research and<br />
training, expand their team, and establish<br />
a new venture with counterparts in China,<br />
where more than half the suicides among<br />
women worldwide occur each year.<br />
The psychiatrists and psychologists<br />
doing the research are part <strong>of</strong> the <strong>Center</strong> for<br />
the Study and Prevention <strong>of</strong> Suicide at the<br />
<strong>University</strong> <strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong>. The<br />
center was established three years ago and<br />
has quickly emerged as an international leader<br />
on suicide study and prevention. In the last<br />
two years, its scientists have attracted $6 million<br />
in funding for the study <strong>of</strong> suicide, which —<br />
in addition to its tragic human consequences—<br />
costs the U.S. economy more than $100 billion<br />
annually.<br />
A team led by Yeates Conwell, M.D.,<br />
pr<strong>of</strong>essor <strong>of</strong> psychiatry, will receive $2 million<br />
from the National Institute <strong>of</strong> Mental Health<br />
over the next five years to train researchers<br />
who focus on suicide. The training program<br />
is the largest in the country devoted to suicide,<br />
with the <strong>University</strong> <strong>of</strong> Pittsburgh, <strong>University</strong><br />
<strong>of</strong> Pennsylvania, <strong>University</strong> <strong>of</strong> Washington,<br />
and Weill <strong>Medical</strong> College <strong>of</strong> Cornell <strong>University</strong><br />
also taking part.<br />
Suicide is actually the third leading<br />
cause <strong>of</strong> death among young adults, and the<br />
eighth leading cause <strong>of</strong> death among all people<br />
in the United States. But a reluctance to talk<br />
about it complicates its study.<br />
“More people die from suicide than by<br />
homicide, yet we all understand that homicide<br />
is a major assault on our communities,”<br />
Conwell says.<br />
A second grant, for $1.2 million, focuses<br />
on suicide in China through the China-<br />
<strong>Rochester</strong> Suicide Research <strong>Center</strong>, headed by<br />
Eric Caine, M.D., the John Romano Pr<strong>of</strong>essor<br />
and chair <strong>of</strong> the Department <strong>of</strong> Psychiatry.<br />
Chinese scholars who study suicide will visit<br />
<strong>Rochester</strong>, and <strong>Rochester</strong> researchers will travel<br />
to China. Collaborations have been established<br />
with several Asian universities.<br />
The China connection opens up a new<br />
vista for researchers, says Caine. It is one <strong>of</strong><br />
few places in the world where the suicide rate<br />
among women is as high as among men;<br />
it’s also a culture with a much lower rate <strong>of</strong><br />
homicide than in the United States.<br />
“We know that cultural and social<br />
factors play a huge role in suicide,” says Caine,<br />
“ and it’s helpful to compare trends in the United<br />
States to those in another setting, like China.”<br />
The <strong>Rochester</strong> group is also leading a<br />
nationwide effort to identify and publicize the<br />
best ways to prevent suicide. Caine and Conwell<br />
last year received a grant from the NIH to<br />
support these efforts in a five-year project.<br />
“Medicine has really failed to look<br />
at suicide as a public health problem,”<br />
says Caine.<br />
The <strong>University</strong> is home to an array <strong>of</strong><br />
other studies on suicide. Kathryn Castle, Ph.D.,<br />
is looking at suicide factors among minority<br />
groups. Caine and Conwell focus on suicide<br />
among the elderly. Paul Duberstein, Ph.D.,<br />
studies how personality and social factors play<br />
a role. Other researchers include Ken Conner,<br />
Psy.D., who studies the role <strong>of</strong> alcohol; Kerry<br />
Knox, Ph.D., who is evaluating a suicideprevention<br />
model used in the armed forces;<br />
Scott Kim, M.D., Ph.D., who is looking at the<br />
ethical issues surrounding the study <strong>of</strong> suicide;<br />
and Valerie Borum, Ph.D., who is studying suicide<br />
among African Americans and deaf people.<br />
6<br />
ROCHESTER MEDICINE
medical center rounds<br />
From invention to implementation:<br />
<strong>Rochester</strong> builds a better prostate cancer treatment<br />
The <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong><br />
has begun using a new computerized medical<br />
device developed by its researchers to improve<br />
the treatment for prostate cancer.<br />
The s<strong>of</strong>tware-based device is called<br />
PIPER (Prostate Implant Planning Engine for<br />
Radiotherapy) and was developed and patented<br />
by the <strong>University</strong> and licensed to RTek <strong>Medical</strong><br />
Systems LLC, a collaboration between the<br />
<strong>University</strong> and Real Time Enterprises, Inc.<br />
<strong>of</strong> Pittsford. The <strong>University</strong>’s James P. Wilmot<br />
Cancer <strong>Center</strong> acquired the system last fall.<br />
The PIPER system assists surgeons,<br />
radiation oncologists, and medical physicists<br />
in planning and performing brachytherapy,<br />
which is an increasingly popular treatment<br />
for prostate cancer. Brachytherapy involves<br />
surgically implanting tiny radioactive seeds—<br />
roughly the size <strong>of</strong> a grain <strong>of</strong> rice — into the<br />
prostate to destroy cancer cells over a period<br />
<strong>of</strong> several weeks.<br />
The success<br />
<strong>of</strong> brachytherapy<br />
hinges on the placement<br />
<strong>of</strong> the<br />
radioactive seeds<br />
at precise locations<br />
within the prostate<br />
to destroy all nearby<br />
cancer cells without<br />
harming the healthy tissue surrounding the<br />
prostate. The PIPER system uses sophisticated<br />
optimization algorithms to help clinicians<br />
determine how many seeds are necessary and<br />
exactly where to place them within the prostate.<br />
Physicians <strong>of</strong>ten use computer programs<br />
to help them decide how and where to place<br />
the seeds, but this system is revolutionary<br />
because <strong>of</strong> its speed and optimization capabilities.<br />
Based on an ultrasound scan <strong>of</strong> a patient’s<br />
prostate and other organs, the PIPER system<br />
automatically<br />
compiles a<br />
computer-optimized<br />
radiation treatment<br />
plan in less than<br />
two minutes.<br />
This means that<br />
radiation-treatment<br />
planning can be<br />
done in the operating<br />
room<br />
immediately before<br />
surgery, instead <strong>of</strong><br />
several weeks<br />
beforehand, as<br />
is now standard.<br />
A plan created in the operating room just<br />
minutes before the procedure can better match<br />
the anatomy that surgeons actually confront.<br />
“It is a tremendous advantage to be able<br />
to plot seed placements<br />
using<br />
up-to-the-minute<br />
images <strong>of</strong> the<br />
prostate,” says<br />
surgeon Edward<br />
Messing, M.D.,<br />
chair <strong>of</strong> the<br />
Department <strong>of</strong><br />
Urology. Messing<br />
has performed scores <strong>of</strong> brachytherapy procedures<br />
at Strong Memorial Hospital.<br />
“When you enter the operating room,<br />
the prostate you see then is never the same<br />
as the one you saw a few weeks previously,”<br />
says Messing, referring to changes in the size<br />
and shape <strong>of</strong> the organ that can result from<br />
patient positioning, hormone therapy, and<br />
anesthesia. “Using PIPER helps take the guesswork<br />
and heavy, time-consuming calculations<br />
out <strong>of</strong> the process. You know exactly where<br />
The PIPER system displays the seeds implanted in the prostate.<br />
your seeds went and where you want to put<br />
the next ones.”<br />
Placement <strong>of</strong> the seeds with pinpoint<br />
precision is difficult because the tiny seeds<br />
are difficult to visualize with ultrasound.<br />
The PIPER system also helps during the procedure<br />
by providing an interactive, ultrasound<br />
interface that allows surgeons to track needle<br />
locations and determine seed positions in real<br />
time. And actual seed placements can be<br />
adjusted to match the optimized plan.<br />
“This approach improves the therapeutic<br />
outcome by optimizing the treatment<br />
<strong>of</strong> the cancer cells while lessening the effects<br />
on adjacent organs and minimizing side effects<br />
and complications,” says Ralph Brasacchio, M.D.,<br />
assistant pr<strong>of</strong>essor <strong>of</strong> radiation oncology and<br />
co-director <strong>of</strong> the Prostate Brachytherapy<br />
Program.<br />
PIPER was developed by medical physicist<br />
Yan Yu, Ph.D., associate pr<strong>of</strong>essor <strong>of</strong> radiation<br />
oncology at the Wilmot Cancer <strong>Center</strong>, based<br />
on more than six years <strong>of</strong> research funded by<br />
a variety <strong>of</strong> sources, including the National<br />
Cancer Institute and the Whitaker Foundation.<br />
SPRING / SUMMER <strong>2002</strong> 7
medical center rounds<br />
Strong Memorial unveils high-tech ORs<br />
Surgeons and faculty at Strong Memorial<br />
Hospital have more room to operate, thanks to<br />
an $8.5 million project, completed in February,<br />
that has added 12 new operating rooms to the<br />
hospital’s existing surgical center.<br />
The new surgical suite, located below<br />
the Frank and Caroline Gannett Emergency<br />
<strong>Center</strong> and adjacent to the existing ORs, uses<br />
the latest technologies and design ideas. The<br />
rooms are larger than traditionally designed<br />
rooms: 800 square feet, which is 75 percent<br />
larger than the existing rooms and 25 percent<br />
larger than the norm. They’re equipped with<br />
flat-panel video displays, which allow surgical<br />
teams to view x-ray images delivered electronically<br />
from a different part <strong>of</strong> the hospital rather<br />
than rely on the manual delivery <strong>of</strong> actual<br />
x-rays viewed on a light board.<br />
The computers and video displays also<br />
enable surgeons to communicate in real time<br />
via the Internet with other doctors within the<br />
hospital and beyond, to discuss procedures<br />
being performed or to teach other medical<br />
personnel and students. As learning labs,<br />
the rooms can be used for tele-medicine and<br />
some day could incorporate surgical robotics.<br />
The new ORs were essential because<br />
<strong>of</strong> increasing numbers <strong>of</strong> patients and a need<br />
to accommodate larger, leading-edge equipment,<br />
says Arthur S. Hengerer, M.D., F.A.C.S.,<br />
acting chief <strong>of</strong> the Department <strong>of</strong> Surgery and<br />
chair <strong>of</strong> the Division <strong>of</strong> Otolaryngology.<br />
“These operating rooms truly cater to<br />
our specialty surgical services, including<br />
general surgery, transplantation, orthopaedics,<br />
trauma, vascular, cardiac and neurosurgery,”<br />
says Hengerer.<br />
Two rooms are devoted to heart bypass<br />
and heart transplantation procedures, and two<br />
are designated for live-donor liver and kidney<br />
transplantation. Each contains a hepa-filtration<br />
system that cleans the air in the ORs to<br />
reduce the risk <strong>of</strong> infection.<br />
A vascular surgical room is enclosed<br />
by several-inch-thick lead walls that house<br />
the latest in digital x-ray equipment, some <strong>of</strong><br />
which is located below the patient and can be<br />
used to image from a very different angle than<br />
was possible in the past.<br />
Orthopaedic rooms are fitted with<br />
a laminar flow air-handling system that<br />
controls the movement <strong>of</strong> air and reduces the<br />
risk <strong>of</strong> infection. A state-<strong>of</strong>-the-art trauma bay<br />
is located directly across from private emergency<br />
elevators that lead up to the emergency<br />
department, as well as to the ro<strong>of</strong>top helipad.<br />
The 12 operating rooms are being used<br />
in conjunction with 15 existing rooms, for a total<br />
<strong>of</strong> 27. The project cost $5 million for construction<br />
and $3.5 million for medical equipment.<br />
8<br />
ROCHESTER MEDICINE
medical center rounds<br />
Weak sperm count doesn’t always mean infertility<br />
Research <strong>of</strong>fers new classifications for normal, abnormal semen levels.<br />
The nation’s most in-depth study <strong>of</strong> the quality<br />
<strong>of</strong> sperm in nearly 1,500 men shows that sperm<br />
counts previously thought to be abnormal do<br />
not always mean infertility. The <strong>University</strong> <strong>of</strong><br />
<strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong> research was published<br />
in the New England Journal <strong>of</strong> Medicine.<br />
The study proposes new recommendations<br />
for classifying semen samples as “normal”<br />
or “abnormal.” If accepted by clinicians worldwide,<br />
the research could rewrite laboratory<br />
standards used for 50 years.<br />
The findings demonstrate in scientific<br />
terms what many clinicians already suspect:<br />
that male infertility is not as clear-cut as<br />
the current laboratory guidelines suggest,<br />
says lead author David Guzick, M.D., then<br />
chair <strong>of</strong> obstetrics and gynecology at the<br />
<strong>Medical</strong> <strong>Center</strong> and newly appointed dean<br />
<strong>of</strong> the School <strong>of</strong> Medicine and Dentistry<br />
(see page 29 for more on the dean). For<br />
example, a sperm count may fall just below<br />
the laboratory criteria for infertility published<br />
by the World Health Organization (WHO). But<br />
in reality, that man may be able to establish a<br />
pregnancy. The study’s new guidelines create a<br />
“ gray zone” for such borderline semen samples.<br />
“Every treatment for infertility depends<br />
upon first establishing what’s normal and<br />
abnormal,” Guzick says. “Up until now, we’ve<br />
just been using guidelines without rigorously<br />
testing them. We hope specialists will use these<br />
revisions in their counseling <strong>of</strong> infertile couples<br />
and in tailoring treatments to individual<br />
patient circumstances.”<br />
The <strong>Medical</strong> <strong>Center</strong> is the first to<br />
compare fertile and infertile men using<br />
contemporary methods for semen analysis;<br />
other research has only gone so far as to study<br />
sperm from infertile men before and after<br />
infertility treatment. The research is also the<br />
first to analyze semen samples from a very<br />
large cross-section <strong>of</strong> men: it evaluated samples<br />
from 765 men from infertile couples and 696 men<br />
from fertile couples, at nine locations across<br />
the country. All <strong>of</strong> the men were between 20<br />
and 55 years old.<br />
The results show there is no single<br />
criteria that always leads to infertility. In fact,<br />
the shape and appearance <strong>of</strong> sperm (known<br />
as morphology) seemed to be a very important<br />
measurement for discriminating between fertile<br />
and infertile men, the study found. However,<br />
the guidelines currently used by clinicians and<br />
published in WHO laboratory manuals do not<br />
even provide a reference value for morphology.<br />
About 1 in 6 couples are unable to<br />
conceive children. Of those couples, 30 to<br />
40 percent suffer from male infertility. The<br />
routine test for diagnosing male infertility is<br />
a semen analysis. It consists <strong>of</strong> obtaining a<br />
sample and then microscopically analyzing<br />
the number <strong>of</strong> sperm per milliliter, the<br />
percentage <strong>of</strong> sperm that are moving, and<br />
the shape <strong>of</strong> the sperm. Normal sperm are<br />
uniformly oval.<br />
The WHO says that a “normal” sample<br />
contains 20 million sperm per milliliter, with at<br />
least 50 percent <strong>of</strong> the sperm moving. Anything<br />
else is considered “abnormal.” But Guzick’s study<br />
provides three new categories as reference points:<br />
• Infertility is defined as having a concentration<br />
<strong>of</strong> less than 13.5 million sperm per milliliter,<br />
less than 32 percent motility (movement)<br />
and less than 9 percent with a uniform shape.<br />
• A gray zone is defined as having a concentration<br />
<strong>of</strong> between 13.5 million and 48 million<br />
sperm, between 32 and 63 percent motility,<br />
and 9 to 12 percent <strong>of</strong> the sperm having a<br />
uniform appearance.<br />
• Fertility is established with a concentration<br />
<strong>of</strong> greater than 48 million sperm per milliliter,<br />
greater than 63 percent motility, and greater<br />
than 12 percent with a uniform appearance.<br />
The exact cause <strong>of</strong> male infertility is<br />
unknown, although hormonal and anatomic<br />
factors are sometimes responsible. Certain<br />
behaviors, such as smoking cigarettes or marijuana,<br />
are associated with lower sperm counts.<br />
SPRING / SUMMER <strong>2002</strong> 9
Best prepare for the worst<br />
How D.A. Henderson, M.D., M.P.H.,saved the planet<br />
©1980 World Health Organization<br />
from smallpox, and how he plans to do it again.<br />
Electron micrograph<br />
<strong>of</strong> variola virus<br />
isolated from<br />
a specimen from<br />
the last case <strong>of</strong><br />
smallpox in the<br />
world.<br />
by Mark Liu<br />
Really, he just wanted to be a cardiologist. Instead, in a<br />
globe-spanning career packed with high adventure and<br />
serious risk-taking, D. A. Henderson, M.D., M.P.H.(M ’54),<br />
became known as the first person in history to wipe<br />
a disease from the face <strong>of</strong> the earth.<br />
Henderson is quick to credit the many people who<br />
contributed to the World Health Organization’s smallpox<br />
eradication program in the ’60s and ’70s. But he was<br />
the one in charge. He was the one who transformed<br />
previous eradication attempts into a successful global<br />
campaign. He was the one who innovated at every step,<br />
learning on the run and applying experimental<br />
techniques against a disease that killed one <strong>of</strong> every<br />
three people who contracted it.
D.A. Henderson<br />
how he gained the insight to predict a problem that plagues us now —<br />
is the stuff <strong>of</strong> a good page-turner. And, in fact, he was working on the<br />
book. But duty called. The book will have to wait.<br />
Photo by John Dean<br />
Now, after evading gunfire and dodging land mines, after decades <strong>of</strong><br />
outfoxing epidemics and human suffering, Henderson is maneuvering<br />
through what may be the trickiest landscape <strong>of</strong> them all: government.<br />
When he was named director <strong>of</strong> the newly formed federal Office <strong>of</strong> Public<br />
Health Preparedness in November, a daunting task lay before him.<br />
He became responsible for the medical and public health response to<br />
terrorism, with a special emphasis on bioterrorism. The man who waged<br />
war against natural epidemics was now faced with the sad and ugly reality<br />
<strong>of</strong> defending against manmade ones.<br />
At least one key person thinks he’s up to the task.<br />
“ Dr. Henderson brings a lifetime <strong>of</strong> preparation for the demands<br />
<strong>of</strong> this job,” says Tommy Thompson, Secretary <strong>of</strong> the Department <strong>of</strong><br />
Health and Human Services. “His distinguished record speaks for itself,<br />
and we are fortunate to have him join the<br />
department on a full-time basis.”<br />
In many ways, the position is the logical “<br />
culmination to the work Henderson did<br />
throughout the ’90s, in his other career as<br />
a bioterrorism expert and White House advisor.<br />
Back then, he and a handful <strong>of</strong> others<br />
implored the government to take the bioterrorism<br />
threat seriously. It was a tough sell—<br />
until anthrax hit the headlines last fall.<br />
“ It felt like we were praying for rain in<br />
the desert,” says Henderson from his Baltimore<br />
home. “And then when it came, it was a flood.”<br />
How he became the man at the floodgates —<br />
Into Africa<br />
It was an incredible achievement<br />
to get people from all over<br />
the world to cooperate.”<br />
Bob Berg, M.D., pr<strong>of</strong>essor emeritus,<br />
Community and Preventive Medicine,<br />
<strong>University</strong> <strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong><br />
Donald A. Henderson earned his medical degree from <strong>Rochester</strong> in 1954,<br />
then completed his internship at Bassett Hospital in Cooperstown, N.Y.<br />
With the “doctor draft” still in effect, Henderson applied to the <strong>Center</strong>s<br />
for Disease Control and Prevention (CDC), even though the CDC was little<br />
known and very small at the time. Henderson had only one qualification<br />
for public health work: He had written a paper on the history <strong>of</strong> cholera<br />
in <strong>Rochester</strong> for a contest, which he had entered only because he wanted<br />
the prize money to buy a hi-fi.<br />
“I applied to the CDC not because I was interested in public health<br />
or anything like that. But we all had to do military service,” he says.<br />
“ I thought, ‘Well, I’ll spend two years in public health.’ ”<br />
Henderson ended up in the Epidemic Intelligence Services (EIS)<br />
in Atlanta, among a group <strong>of</strong> epidemiologists who, with the Korean War<br />
fresh in their minds, were looking into the problem <strong>of</strong> biological warfare.<br />
They were ahead <strong>of</strong> their time in other respects, as well. When they got<br />
word <strong>of</strong> an epidemic, they responded like an emergency department that<br />
made house calls. They packed their bags and went, bringing with them<br />
the latest ideas in vaccinating and isolating patients to contain outbreaks.<br />
On one assignment, to fight an outbreak <strong>of</strong> botulism toxin in<br />
Argentina, local <strong>of</strong>ficials asked Henderson if he wanted to see any sights.<br />
He said he wanted to see a case <strong>of</strong> smallpox.<br />
Henderson and a World Health Organization (WHO) doctor were<br />
flown far up the Amazon to a tiny town, where he got his first glimpse<br />
at how complicated smallpox work could be out in the trenches. The clinicians<br />
in the treatment tent were baffled by smallpox patients who seemed<br />
to be experiencing relapses several weeks later. As it turned out, some<br />
patients with chickenpox were acquiring smallpox, and others with<br />
smallpox were getting chickenpox. It was a good, first-hand lesson in<br />
differentiating one disease from the other.<br />
Henderson had come face to face with the<br />
disease that would make him famous.<br />
He tried to stick to his original plan,<br />
returning to Cooperstown to study internal<br />
medicine, but he decided that public health<br />
was far more exciting. He enrolled at Johns<br />
Hopkins <strong>University</strong> to earn his M.P.H., then<br />
found himself back in Atlanta, running<br />
the surveillance section <strong>of</strong> the EIS.<br />
Henderson was already thinking big<br />
about what the EIS could do. Lawrence Altman,<br />
M.D., now a medical correspondent for<br />
The New York Times, remembers his very first<br />
SPRING / SUMMER <strong>2002</strong> 11
©1980 World Health Organization<br />
D. A. Henderson (circled) with members <strong>of</strong> the Global Commission for the Certification <strong>of</strong> Smallpox Eradication in the late 1970s.<br />
conversation with Henderson when Altman came to the EIS for a job interview.<br />
“ He was talking about eradicating smallpox,” says Altman. “I had<br />
never heard the concept <strong>of</strong> eradicating a disease before. It was never talked<br />
about in med school, or any other training. It was just an eye-opener.”<br />
The idea was to break the human chain, which would stop the<br />
disease because it was communicable only through human contact.<br />
When an outbreak occurred, epidemiologists could vaccinate a ring <strong>of</strong><br />
people around the outbreak, effectively cutting <strong>of</strong>f all paths for it to spread.<br />
The premise was simple enough, but everything else would be dizzyingly<br />
complex. Eradication would require teams <strong>of</strong> experts to cross world<br />
cultures and negotiate through civil wars, in places that had the least<br />
developed health services in the world. They would have to secure and<br />
transport hundreds <strong>of</strong> millions <strong>of</strong> doses <strong>of</strong> vaccine in places that barely<br />
had roads, let alone communication systems — all with the Cold War<br />
heating up around them. Understandably, talk <strong>of</strong> smallpox eradication<br />
was just that: talk, with no practical plan in sight.<br />
Even when Henderson saw a chance to fight the disease in a major<br />
hot spot, he wasn’t thinking about eradication. In 1965, the U.S. Agency<br />
for International Development (AID) was fighting a losing battle against<br />
measles in West Africa. AID turned to Henderson for more manpower,<br />
which the EIS really couldn’t spare. But rather than say it that way,<br />
Henderson cleverly said the opposite. He proposed a massive, combined<br />
effort to fight measles and smallpox in 18 countries, at a staggering cost<br />
<strong>of</strong> $35 million.<br />
Essentially, it was a bluff. Henderson knew that neither group<br />
was equipped to handle such an undertaking. As he tells it, he was<br />
thinking, “We know they’ll turn it down, and then we’re <strong>of</strong>f the hook.<br />
But we needed to <strong>of</strong>fer something.”<br />
Henderson, an avid bridge player at the time, had played his<br />
cards right. AID did turn down his proposal, and he was <strong>of</strong>f the hook —<br />
for a moment. Then something completely unexpected happened.<br />
For its 20th anniversary, the United Nations had declared 1965<br />
“ International Cooperation Year,” and President Johnson was looking for<br />
a cause to showcase American cooperation. Someone in the Public Health<br />
Service brought the big, unwieldy smallpox-measles proposal to a presidential<br />
advisory committee, explains Henderson. They liked the idea,<br />
Incidence <strong>of</strong> smallpox in 1967.<br />
©1980 World Health Organization<br />
12<br />
ROCHESTER MEDICINE
and so did the president.<br />
“ He ordered AID to fund the program,” says Henderson. “So all <strong>of</strong> a<br />
sudden, there we were with an enormous program.”<br />
History would see Henderson’s bluff differently. Don Millar, M.D.,<br />
a 32-year CDC veteran who led the CDC portion <strong>of</strong> the eradication effort,<br />
says, “If a single idea can be said to have launched the global smallpox<br />
eradication program, it was D. A.’s proposal for a joint smallpox-measles<br />
program in Africa. It stands as a bold stroke <strong>of</strong> managerial genius.”<br />
The idea snowballed, and suddenly the United Nations was voting<br />
on launching a 10-year effort for global smallpox eradication. It passed<br />
by only two votes, says Henderson, and the director <strong>of</strong> WHO, a Brazilian,<br />
was livid.<br />
“ He blamed the Americans for getting us into this terrible mess,<br />
because he felt it could not succeed,” says Henderson.<br />
The WHO director wanted an American to head the program, notes<br />
Henderson, so when it failed, the United States would receive the blame<br />
it deserved. Henderson was his guy — his fall guy, actually.<br />
“ At that point I was thoroughly overwhelmed trying to get this<br />
West African program under way,” recalls Henderson.<br />
That overwhelming program was now just one piece <strong>of</strong> something<br />
much, much larger. Programs would need to be conducted in 50 countries,<br />
with a total population <strong>of</strong> more than a billion people. The WHO budget<br />
provided for only $2.6 million; the rest would have to come from contributions,<br />
volunteer work — wherever it could be found.<br />
And roughly 15 million new cases were appearing each year.<br />
Henderson was now in charge <strong>of</strong> stopping every last one <strong>of</strong> them.<br />
Bullets or missiles?<br />
Those who worked with him say that Henderson’s unique abilities made<br />
him ideal for the task. People cite his commanding presence and sonorous<br />
voice, but also his ability to foresee outcomes much larger than mere<br />
mortals can see. And when he saw opportunity, he seized it.<br />
The kingdom <strong>of</strong> Tonga in the South Pacific is a prime example.<br />
While Henderson was still with the CDC, he learned that the king <strong>of</strong><br />
Tonga had a business meeting with the Coca-Cola Company in Atlanta.<br />
Henderson saw it as an opportunity to test an experimental jet-gun vaccination<br />
technology, so he arranged his own meeting with the king.<br />
Somehow, he sold the king on his plan. Henderson got his test study,<br />
and the entire kingdom <strong>of</strong> Tonga — roughly 80,000 people — got vaccinated<br />
against smallpox.<br />
As head <strong>of</strong> the global eradication effort, Henderson would have to<br />
be just as resourceful. With Geneva as home base, he and teams <strong>of</strong> workers<br />
and volunteers began to solve problems, one at a time. Many <strong>of</strong> the problems<br />
weren’t medical at all.<br />
“It’s war,” says Millar about fighting epidemics, speaking quite<br />
literally. “I was involved in seven coups d’etat. I was under house arrest<br />
during several.”<br />
Photo by John Dean
Henderson’s scenario if an attack comes<br />
Suppose, says Henderson, that <strong>Rochester</strong> is hit<br />
with an anthrax attack. The Office <strong>of</strong> Public<br />
Health Preparedness has worked to devise a<br />
practical plan to contain the problem — for<br />
<strong>Rochester</strong> and any other location in the country.<br />
“Patients are going to hit the ERs first,”<br />
says Henderson. That’s why ER doctors and<br />
nurses need to know what a biological attack<br />
looks like and be able to recognize the symptoms.<br />
These doctors and nurses need to be able<br />
to call their health department if they suspect<br />
there may be a problem. If there is an outbreak,<br />
local health departments need to be available 24<br />
hours a day. Only a few were before the anthrax<br />
attacks, says Henderson, but that is changing<br />
under the new plans.<br />
The health departments, in turn, need to<br />
be able to call on designated infectious disease<br />
specialists quickly, to determine whether there<br />
are similar cases in other hospitals; to obtain<br />
specimens and to get them to qualified laboratories<br />
in our national laboratory network; and to<br />
call for help from state or national <strong>of</strong>ficials.<br />
“We have a new federal command center<br />
open 24 hours a day,” says Henderson. The CDC<br />
also opened a 24-hour command center.<br />
For treatment <strong>of</strong> patients, Henderson has<br />
contracted for hundreds <strong>of</strong> millions <strong>of</strong> doses <strong>of</strong><br />
vaccine. The National Pharmaceutical Stockpile<br />
Program has been expanded, so vaccine will be<br />
on hand no matter where an attack occurs. The<br />
program includes antibiotics to treat 20 million<br />
people. It has respirators, smallpox vaccine and<br />
some anthrax vaccine. Stockpiles are located at<br />
12 strategic locations around the country, guaranteeing<br />
that supplies can be delivered wherever<br />
they’re needed within 12 hours.<br />
But patients will have to go somewhere<br />
for treatment. So hospitals are embarking on<br />
regional planning to answer basic questions<br />
such as how they would deal with thousands <strong>of</strong><br />
affected patients, where they would put them,<br />
and who would treat them. Federal disaster<br />
medical teams are being formed that could fly<br />
in and augment local staffs, if needed.<br />
“The key is to find it as quickly as possible,<br />
diagnose it and take action,” says Henderson.<br />
Special treaties had to be arranged so<br />
that vaccination could proceed amid revolutions<br />
and civil wars. Sometimes, as in Nigeria,<br />
treaties were made on both sides. And where<br />
agreements couldn’t be reached, Henderson<br />
found other ways.<br />
When Ethiopia’s minister <strong>of</strong> health<br />
refused to have his country participate in the<br />
program and refused even Henderson’s request<br />
to visit, Henderson waited until the minister<br />
was out <strong>of</strong> the country, then managed to get<br />
permission through other channels. He then<br />
befriended the emperor’s personal physician<br />
who, in turn, persuaded the emperor. The<br />
minister was ordered to execute the program.<br />
Later in the campaign, Henderson found<br />
himself back in Ethiopia, flying extremely low<br />
in a helicopter while rebel soldiers fired at<br />
them from the ground. Henderson turned to<br />
the pilot and asked, “Why don’t we fly a little<br />
higher?” The pilot answered, “We heard they<br />
got surface-to-air missiles last month. We<br />
thought it was better to brave rifles than SAM<br />
missiles.”<br />
There were other difficult choices to<br />
make. In Bangladesh, Henderson was trying<br />
to get a UN team out to a health center in the<br />
middle <strong>of</strong> a revolution. As Henderson tells it,<br />
the authorities asked, “Doc, do you want a military<br />
escort? There are lots <strong>of</strong> landmines out there.<br />
Better that the car in front <strong>of</strong> you hits them.<br />
So an escort is good. But the army draws lots <strong>of</strong><br />
gunfire from militants. So an escort is bad.”<br />
Henderson thought hard, eventually<br />
choosing to go without the escort.<br />
“ I felt that trip was 200 miles, but it was<br />
more like 15,” he says.<br />
Yet he insists that the “incredible bunch<br />
<strong>of</strong> people” on the eradication staff and in local<br />
teams actually faced worse dangers. “What I<br />
experienced was really minor compared to<br />
what they did,” he says.<br />
Every few months, recalls Henderson,<br />
someone on the staff was kidnapped. They’d<br />
disappear from Ethiopia and sometimes end up<br />
in Somalia, where their release would have to<br />
be negotiated.<br />
Somehow, Henderson kept his teams<br />
“ I think it’s a travesty that<br />
he hasn’t won the Nobel Prize<br />
for the eradication<br />
<strong>of</strong> smallpox.”<br />
Don Millar, M.D.,<br />
32-year veteran <strong>of</strong> the <strong>Center</strong>s<br />
for Disease Control<br />
committed to the cause. A clue to how he<br />
pulled it <strong>of</strong>f comes from the likes <strong>of</strong> Don Millar.<br />
Millar says it “wasn’t always pleasant working<br />
for him. He was hard-driving. He expected<br />
more <strong>of</strong> me than I thought I had to give. I<br />
never had as l<strong>of</strong>ty an opinion <strong>of</strong> me as he did.”<br />
Yet, Millar also says, “Because <strong>of</strong> people like<br />
D. A., it was a wonderful career.” Henderson<br />
expected the best from people, so he <strong>of</strong>ten got<br />
it. He could drive people beyond what they felt<br />
was comfortable, yet still have them feel it was<br />
“ wonderful” in the end.<br />
The WHO teams also knew they were on<br />
a medical mission <strong>of</strong> the highest order. They<br />
made major strides in West Africa using the<br />
faster, cheaper (and Tonga-tested) jet gun,<br />
though they had to modify it to pedal power<br />
because they didn’t have electricity. Henderson<br />
convinced countries to donate vaccine or<br />
develop their own. Despite the Cold War, the<br />
USSR became the largest donor, contributing<br />
25 million doses. Still, vaccine was in short<br />
supply, so the teams experimented with a bifurcated<br />
needle just invented but not yet in use.<br />
It quadrupled the number <strong>of</strong> successful “takes”<br />
per dose, and made it easier for volunteers to<br />
administer the vaccine.<br />
Several years into the program, the<br />
teams reached a major milestone. They had<br />
eradicated smallpox in Africa and South<br />
America, but, more important, they now felt for<br />
the first time that global eradication was truly<br />
possible. Now, a major battle loomed: India.<br />
Indian <strong>of</strong>ficials had been fighting smallpox for
From left — Lowell A. Goldsmith, M.D., Robert Joynt, M.D., Ph.D., D.A. Henderson, and Jules Cohen, M.D., at Henderson’s 1999 URMC bioterrorism talk.<br />
years, but still the WHO teams faced an extremely high incidence <strong>of</strong> the<br />
disease there. As weapons, the team brought with them many solid years<br />
<strong>of</strong> resourcefulness and on-the-job learning. As Henderson puts it, “At that<br />
point, we knew better what we were doing.”<br />
The field staff had an idea for a search operation that eventually<br />
would reach every village in India. Later, it was extended to reach every<br />
house in India — a remarkable undertaking, considering India’s diverse<br />
population <strong>of</strong> half a billion people spread over more than a million square<br />
miles. More than 120,000 health workers were engaged in the search.<br />
The team came up with a final innovation: a reward to anyone who<br />
reported a case <strong>of</strong> smallpox. The operation worked. In 1975, smallpox was<br />
dead in India. Five years later, WHO declared smallpox eradicated, and the<br />
world celebrated an unimaginable accomplishment.<br />
Overlooked in the celebration was the ominous ending to this<br />
chapter <strong>of</strong> the story. The world’s last smallpox fatality didn’t occur in<br />
the midst <strong>of</strong> an epidemic in squalid surroundings. It occurred in England,<br />
in 1978, when a sample <strong>of</strong> virus accidentally escaped from a laboratory.<br />
This would foreshadow the problem that would come to haunt the world<br />
two decades later — the problem that has Henderson as busy as ever,<br />
fighting the same fight in very different circumstances.<br />
The man-made epidemic<br />
Henderson returned to Johns Hopkins in 1977, where he served as dean<br />
<strong>of</strong> the School <strong>of</strong> Public Health for 14 years. He calls that time “very gratifying,”<br />
as he cemented a relationship with the school <strong>of</strong> medicine and<br />
built up the international program. He was in the midst <strong>of</strong> overseeing<br />
major growth at the school when the White House came calling.<br />
Henderson became a science advisor for George Bush Sr. in 1990.<br />
When President Clinton took <strong>of</strong>fice, Henderson moved to the Department<br />
<strong>of</strong> Health and Human Services as senior science adviser and deputy<br />
assistant secretary.<br />
It was through briefings and work on Department <strong>of</strong> Defense<br />
committees during the Clinton administration that Henderson became<br />
especially aware <strong>of</strong> the problem <strong>of</strong> biological weapons. After the Gulf War,<br />
he says, evidence <strong>of</strong> anthrax activity in Iraq was mounting. In 1995,<br />
a Japanese cult released toxic sarin gas in the Tokyo subway system,<br />
raising the specter <strong>of</strong> domestic terrorism. But the big blow came with<br />
the revelation <strong>of</strong> a major biological-weapons program in Russia.<br />
Smallpox virus was alive and well as a potential weapon.<br />
“ There was a feeling by the President and the administration that<br />
we really had to gear up,” says Henderson.<br />
But many other people would have to be convinced. In some ways,<br />
preventing a manmade epidemic was as daunting as stopping a natural<br />
one. The whole topic <strong>of</strong> biological weapons and the diseases they could<br />
unleash was foreign to most people in public health and medicine,<br />
says Henderson: “The subject was all but taboo.” The prevalent view<br />
was that the healing arts shouldn’t be mixed with research or teaching<br />
that involved such repugnant weapons. That view was reflected in the health<br />
care system, as well.<br />
“We were doing nothing in the hospitals, nothing in the ERs,”<br />
says Henderson.<br />
SPRING / SUMMER <strong>2002</strong> 15
A handful <strong>of</strong> experts did understand the problem. In fact, Frank<br />
Young, M.D., Ph.D., former dean <strong>of</strong> the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> School <strong>of</strong><br />
Medicine and Dentistry, was talking about bioterrorism as early as 1979.<br />
“ I spoke to the State Department and said the potential to cause<br />
havoc is very high,” says Young, who served as the commissioner <strong>of</strong> the<br />
FDA from 1984 to 1989 (see “War Rooms” story, next page).<br />
Yet there was widespread complacency, in part because <strong>of</strong> a feeling<br />
that no one would cross the moral barrier <strong>of</strong> inflicting these weapons on<br />
civilians.<br />
By the late ’90s, Henderson had become a founding director <strong>of</strong><br />
the Johns Hopkins <strong>University</strong> <strong>Center</strong> for Civilian Biodefense Studies.<br />
In essence, he was trying to sound the alarm. NATO had established a list <strong>of</strong><br />
30 potential biological agents, with smallpox at the top and anthrax not<br />
far behind. Henderson started the biodefense center to talk about the<br />
dangers.<br />
He spent years trying to convert skeptics. Then, practically<br />
overnight — after the September 11 attacks and subsequent anthrax<br />
mailing — Henderson went from alarmist to visionary. The Department<br />
<strong>of</strong> Health and Human Services quickly tapped him to lead the newly<br />
formed Office <strong>of</strong> Public Health Preparedness — a position with great<br />
responsibility, but requiring cooperation among a staggering number <strong>of</strong><br />
government departments. In the words <strong>of</strong> Jerome Donlon, M.D. (M ’72, Ph.D.<br />
’ 68, R ’73), who is on detail assignment to the Office <strong>of</strong> Public Health<br />
Preparedness, “A lot <strong>of</strong> what D. A. does is referee and negotiate.”<br />
Those negotiations are crucial to the overall homeland-security<br />
efforts. So Henderson assembled a small, dedicated staff <strong>of</strong> people mostly<br />
on assignment from other government departments. Within two months,<br />
D. A. Henderson will be the keynote speaker for two big events<br />
at the <strong>University</strong>:<br />
The Gala opening<br />
<strong>of</strong> the second state-<strong>of</strong>-the-art medical research<br />
facility, adjacent to the Arthur Kornberg <strong>Medical</strong><br />
Research Building.<br />
Thursday, May 9<br />
Convergence <strong>2002</strong> conference<br />
Friday, May 10<br />
Regional events will occur simultaneously on May 9<br />
in New York, Boston and Los Angeles.<br />
his <strong>of</strong>fice was disseminating roughly $1 billion to hospitals and state<br />
and local health departments to help get them prepared. He arranged for<br />
the purchase and development <strong>of</strong> vaccines and drugs while beefing up<br />
the capabilities <strong>of</strong> diagnostic labs to enable quick identification <strong>of</strong> biological<br />
agents.<br />
Just as important, his team began detailing a response plan against<br />
a potential attack. A network <strong>of</strong> 81 laboratories has been established and<br />
hundreds <strong>of</strong> lab workers trained. And his team is assessing how prepared<br />
each state is to handle a bioterrorism attack, asking the states to submit<br />
details <strong>of</strong> the plans they have in place.<br />
Some observers have wondered how Henderson — a man who<br />
likes to get the job done — will fare amid the thick layers <strong>of</strong> Washington<br />
bureaucracy. But Henderson himself doesn’t seem too concerned.<br />
Whether he’s maneuvering around the globe to fight smallpox or around<br />
Washington to fight bioterrorism, Henderson says there’s an old lesson<br />
from his <strong>Rochester</strong> days that serves him well.<br />
“One <strong>of</strong> the most important pieces <strong>of</strong> what I learned was the Engel<br />
and Romano model in ‘Introduction to Diagnosis,’ ”says Henderson <strong>of</strong><br />
<strong>Rochester</strong>’s biopsychosocial philosophy. “Take time, question the patient<br />
thoroughly, listen carefully. More <strong>of</strong>ten than you can imagine, the patient<br />
has a remarkably keen insight and understanding <strong>of</strong> his problem and will<br />
effectively provide you the diagnosis before you do the physical examination<br />
or obtain a laboratory study.”<br />
He says it worked in far-flung countries when he tried to find out<br />
where an outbreak originated. Against popular wisdom, he would ask<br />
patients, “Where do you think you got the disease?” Surprisingly <strong>of</strong>ten,<br />
this led straight to the source.<br />
A similar approach worked just as well at the White House. When<br />
he arrived, Henderson was faced with a long agenda <strong>of</strong> problems that,<br />
for him, were new and complicated.<br />
“It was all too apparent that there were many talented and knowledgeable<br />
people who had given many <strong>of</strong> the problems a great deal <strong>of</strong><br />
thought, who understood the problems well and who had imaginative<br />
ideas as to what might be done,” he says. “One simply had to take the<br />
time to question them thoroughly and to listen carefully. It sounds simple<br />
and obvious, but all too few people seem to understand this very simple<br />
precept that came straight from that introductory course in diagnosis at<br />
<strong>Rochester</strong>.”<br />
Luckily, Henderson knows when to talk, too. Henderson appeared<br />
before the U.S. Senate Foreign Relations Committee and cautioned that<br />
terrorists would not be above attacking innocent civilians, with anthrax<br />
or other biological weapons.<br />
The date <strong>of</strong> his warning? September 5, 2001.<br />
For more information on any <strong>of</strong> these events, please call<br />
800–333–4428<br />
16<br />
ROCHESTER MEDICINE
War rooms, new vaccines and<br />
meetings with the President<br />
Experts take their places in Washington to protect the country from bioterrorism.<br />
by Mark Liu<br />
Not many associate pastors can say they spent 20 years in the dark<br />
world. Then again, Frank Young, M.D., Ph.D., isn’t your typical<br />
associate pastor. Young, former chair <strong>of</strong> the Department <strong>of</strong><br />
Microbiology at <strong>Rochester</strong> and former dean <strong>of</strong> the School <strong>of</strong><br />
Medicine and Dentistry and now an associate pastor in Maryland,<br />
worked for nearly two decades within the federal government in classified<br />
areas — known as the “dark world” to people inside the Beltway.<br />
Young’s efforts in the ’80s and ’90s helped lay the groundwork<br />
for the explosion <strong>of</strong> activity now under way as a result <strong>of</strong> September 11<br />
and the anthrax attacks. His was one <strong>of</strong> the few voices in the Washington<br />
wilderness, warning <strong>of</strong> the need to prepare for bioterrorism.<br />
Today, that preparation is a national priority, reflected both in<br />
the billions <strong>of</strong> new dollars being budgeted for bioterrorism defense and<br />
the sheer numbers <strong>of</strong> people now devoted to Eric Noji, M.D., M.P.H.,<br />
the problem. Several <strong>Rochester</strong> alumni have shakes hands with<br />
recently stepped into key leadership positions President Bush in<br />
on this new front, in the recently created Office the White House.<br />
<strong>of</strong> Homeland Security and the Office <strong>of</strong> Public<br />
Health Preparedness. They’re part <strong>of</strong> the new<br />
guard in this post-September 11 world.<br />
Young, for his part, foresaw this changed world and helped<br />
persuade President Clinton to begin preparing for it. Young was in the<br />
position to advise the president after a far-reaching Washington career<br />
that included stints as commissioner <strong>of</strong> the Food and Drug Administration,<br />
deputy assistant secretary for Health Science and Environment in the<br />
Department <strong>of</strong> Health and Human Services (HHS), U.S. representative<br />
17
to the Executive Board <strong>of</strong> the World Health Organization (a Senateconfirmed<br />
position), and director <strong>of</strong> the Office <strong>of</strong> Emergency<br />
Preparedness / National Disaster <strong>Medical</strong> System. Before that, Young’s<br />
research in <strong>Rochester</strong> involved the nontoxic form <strong>of</strong> anthrax. In effect,<br />
he has been working on bioterrorism issues for a quarter <strong>of</strong> a century.<br />
In 1993, Young took part in a simulation that helped change the<br />
face <strong>of</strong> bioterrorism response in this country. The event was the government’s<br />
first full-scale biological attack simulation “in the white world,”<br />
as Young describes it, as opposed to previous simulations held in secrecy.<br />
The tabletop exercise simulated the response to an anthrax release in the<br />
subway system <strong>of</strong> a major metropolitan area. More than 100 people took<br />
part, representing the EPA, FEMA, HHS, Department <strong>of</strong> Agriculture, and<br />
various other local, state, and federal <strong>of</strong>fices. The simulation even brought<br />
in CNN reporters to show how difficult it is to address the public in the<br />
midst <strong>of</strong> an unfolding crisis.<br />
Young, as the <strong>of</strong>ficer in charge <strong>of</strong> the public-health response to<br />
the attack, says the key players in the simulation continued to meet over<br />
the years because <strong>of</strong> what they discovered from that exercise.<br />
“The dominant thing we learned was a need for command and<br />
control,” says Young. “A clear line <strong>of</strong> authority was needed.”<br />
It takes coordination<br />
It’s no coincidence that, today, Washington is emphasizing command<br />
and control centers for better communication and coordination <strong>of</strong> information.<br />
Eric Noji, M.D., M.P.H. (M ’81), sits in one <strong>of</strong> these new centers at<br />
the White House, in the Office <strong>of</strong> Homeland Security. Noji is on assignment<br />
from his job at the <strong>Center</strong>s for Disease Control and Prevention (CDC) in<br />
Atlanta, where he serves as associate director <strong>of</strong> the Bioterrorism<br />
Preparedness and Response Program. In fact, he went immediately to<br />
Washington after September 11, then onto assignments at the World Trade<br />
<strong>Center</strong> site in Manhattan because <strong>of</strong> his disaster-medicine research<br />
expertise in the toxic effects <strong>of</strong> pulverized concrete. Typically, Noji is called<br />
to earthquake sites, which he compares the World Trade <strong>Center</strong> site to<br />
(except that Ground Zero is in a much more concentrated area).<br />
The day the first anthrax case in Florida came to light, Noji was<br />
scheduled to return home to Atlanta. Instead, he found himself called to<br />
work at the White House.<br />
“ I’ve been living in a hotel since September 13,” he muses.<br />
He’s also been working in a kind <strong>of</strong> war room, <strong>of</strong>ficially dubbed<br />
the Coalition Information <strong>Center</strong>, in a former ballroom in the old<br />
Executive Office building. Back in Teddy Roosevelt’s day it was the Indian<br />
Treaty room, but today it’s filled with several dozen desks representing<br />
various agencies. The Department <strong>of</strong> Defense is there, as is the Department<br />
<strong>of</strong> the Treasury, Department <strong>of</strong> Transportation, even a London desk.<br />
The idea is to provide some centralized coordination for what Noji —<br />
a man who knows his way around the chaos <strong>of</strong> an earthquake — deems<br />
“ an almost unbelievably complex situation.” When Noji’s boss,<br />
Governor Tom Ridge, the head <strong>of</strong> the Office <strong>of</strong> Homeland Security,<br />
displayed a diagram <strong>of</strong> who reports where within the various entities<br />
involved in terrorist and bioterrorist defense, Noji says it “looked like<br />
a quilt” because <strong>of</strong> all the lines connecting so many groups.<br />
And that’s the real challenge facing us. Noji says that, while his<br />
physician colleagues might be surprised to hear it, “the medical and health<br />
aspect is the smallest part <strong>of</strong> disaster response.” For example, after the<br />
September 11 attack, the United States discovered that incompatible telecommunications<br />
systems among first responders — police, fire, ambulance<br />
services, the Red Cross — made it extremely difficult to coordinate efforts.<br />
When other unexpected problems arose, there was no clear system<br />
in place to deal with them. Citizens, says Noji, were donating things “out<br />
<strong>of</strong> the goodness <strong>of</strong> their hearts,” but they didn’t know what was needed.<br />
So they were emptying out their medicine cabinets and sending it all.<br />
Diet pills, birth-control pills — everything imaginable was showing up in<br />
huge piles, some <strong>of</strong> it simply addressed to “U.S. Government.” Volunteers<br />
also were showing up, but some weren’t qualified and others didn’t even<br />
speak English. Yet all needed a place to stay and meals to eat. And somebody<br />
in the government had to figure out how to deal with such issues.<br />
Noji helped coordinate information during the height <strong>of</strong> the<br />
fighting in Afghanistan, when rumors were flying about hemorrhagic fever<br />
and the poisoning <strong>of</strong> wells. Now, he has settled back into his primary<br />
assignment: preparing for a smallpox attack. There’s so much emphasis<br />
on a smallpox attack because, as Frank Young explains it, it’s a low-probability<br />
event with high-risk consequences. The low probability means that<br />
some people didn’t take the threat seriously. But the high-risk consequences<br />
— spread <strong>of</strong> a horrific disease that kills a third <strong>of</strong> its victims and<br />
renders survivors severely scarred or blind — means that a response plan<br />
is now considered vital.<br />
Betting on better vaccine<br />
Just down the street from Noji, between the Washington Monument and<br />
Capitol Hill, Major General Philip K. Russell, M.D. (M ’58), and Jerome<br />
Donlon, M.D. (Ph.D. ’68, M ’72, R ’73) are working on the smallpox problem,<br />
as well. (And down the street from them, Donlon’s wife, Mildred Donlon<br />
(Mas ’64, Ph.D. ’72) works for a government <strong>of</strong>fice dedicated to futuristic<br />
defense breakthroughs; see technology story on page 20.)<br />
Russell and Donlon are part <strong>of</strong> the new federal Office <strong>of</strong> Public<br />
Health Preparedness, led by D. A. Henderson, M.D., M.P.H. (M ’54).<br />
Primarily, their task is to oversee the development and storage <strong>of</strong> vaccines,<br />
especially for anthrax and smallpox. A major project is under way to<br />
develop a second-generation anthrax vaccine that would improve on the<br />
current one, which is based on older production techniques. In March,<br />
the National Academy <strong>of</strong> Sciences came out in support <strong>of</strong> such research,<br />
saying that the current vaccine should be improved.<br />
“Genetic engineering and recombinant technology allows for<br />
isolating specific proteins, which would create a better specified vaccine,”<br />
18<br />
ROCHESTER MEDICINE
says Donlon, whose regular assignment is at the <strong>Center</strong> for Biologics<br />
Evaluation and Research at the FDA.<br />
The better vaccine might be used to protect public health workers<br />
and other first responders who would be in danger <strong>of</strong> infection during<br />
an attack. The vaccine might also be useful after exposure, says Donlon,<br />
to help the immune system produce a response to infection. The NIH has<br />
lead responsibility for the effort, with assistance from the CDC and FDA,<br />
and oversight by the Office <strong>of</strong> Public Health Preparedness.<br />
Donlon and Russell spend much <strong>of</strong> their time overseeing the<br />
government contract to produce smallpox vaccine. The job is more<br />
complicated than it might sound, requiring coordination among the CDC,<br />
the FDA, the private company producing the vaccine and the Office <strong>of</strong><br />
Public Health Preparedness. The vaccine must meet FDA standards,<br />
which means strict protocols for clinical trials and inspections, and it has<br />
to be effective. Because the vaccine is being prepared for the expanding<br />
National Pharmaceutical Stockpile Program, coordinated by the CDC,<br />
Russell and Donlon must consider practical matters such as what kind <strong>of</strong><br />
needles are needed and how many, and how best to package the vaccine<br />
for rapid deployment.<br />
Russell seems the ideal person to draw up battle plans against<br />
a smallpox attack. After graduating from <strong>Rochester</strong>, he served in the army,<br />
becoming director <strong>of</strong> the Walter Reed Army Institute <strong>of</strong> Research,<br />
commander <strong>of</strong> the Fitzsimons Army <strong>Medical</strong> <strong>Center</strong> and commander <strong>of</strong><br />
the U.S. Army <strong>Medical</strong> Research and Development Command. His military<br />
awards include the Legion <strong>of</strong> Merit and the Distinguished Service Medal,<br />
and he retired a major general. Henderson considers him “one <strong>of</strong> the<br />
nation’s most knowledgeable and respected persons in vaccine research,<br />
development and production.”<br />
Some critics have questioned the wisdom <strong>of</strong> devoting so many<br />
people and so much money to prepare for bioterrorism attacks. To Donlon,<br />
such criticism overlooks the overarching benefits <strong>of</strong> these efforts.<br />
“The training, response plans, surveillance, lab services — it all<br />
strengthens the public-health infrastructure,” says Donlon. “It’s not just<br />
for bioterrorism. It’s the same public-health response, so other outbreaks<br />
can be responded to quickly.” The same need exists for teamwork and<br />
communication during such problems as floods, flu outbreaks, or the<br />
discovery <strong>of</strong> West Nile virus.<br />
Besides, the people on the front line <strong>of</strong> a potential attack are<br />
looking for guidance.<br />
“ I get literally 300 e-mails a day from concerned doctors and<br />
nurses,” says Noji. They want to know how they should prepare, and what<br />
they can do.<br />
Meanwhile, Frank Young has retired from the dark world and now<br />
deals in the light <strong>of</strong> the world. As an associate pastor, he’s working to<br />
establish an accredited theological school. Even as he was giving his<br />
recommendations before Congressional committees in October, and even<br />
as his former <strong>Rochester</strong> colleagues were gathering in Washington to<br />
hammer out plans to protect the country from biological attacks, Young<br />
was making sure to keep working on what he has learned to be a cornerstone<br />
<strong>of</strong> the plan: faith.<br />
From left — Major General Philip K. Russell, M.D., Jerome Donlon, M.D., Ph.D., Mildred Donlon, Mas, Ph.D., and D. A. Henderson, M.D., M.P.H.<br />
SPRING / SUMMER <strong>2002</strong> 19
Technology vs.Terrorism<br />
From bomb detection to shirts that talk to satellites,<br />
researchers are working on high-tech solutions.<br />
by Mark Liu<br />
Frank Young, M.D., Ph.D., envisions a future where our<br />
shirts are smarter than we are — smart enough to monitor<br />
our health and save our lives. Where soldiers or citizens<br />
exposed to a biological attack can get a quick injection<br />
and never suffer any symptoms. Where advances in bioinformatics<br />
will be a key element <strong>of</strong> a strong civil defense.
Frank Young, M.D., Ph.D.<br />
Benjamin Miller, Ph.D., holds the sensor chip that is at the heart <strong>of</strong> the smart bandage.<br />
Young, former chair <strong>of</strong> the Department <strong>of</strong> Microbiology at <strong>Rochester</strong><br />
and former dean <strong>of</strong> the School <strong>of</strong> Medicine and Dentistry, is retired from<br />
a 20-year career as a Washington insider on bioterrorism issues. But he<br />
hasn’t stopped working on the problem. He serves on the board <strong>of</strong> two<br />
companies working to develop futuristic solutions.<br />
Scientists <strong>of</strong> all sorts are applying their knowledge to the bioterrorism<br />
problem. At <strong>Rochester</strong>, researchers at the <strong>Center</strong> for Future Health<br />
recently unveiled the first major step toward a “smart bandage” that will<br />
change color depending on what kind <strong>of</strong> bacteria is present in a wound.<br />
Benjamin Miller, Ph.D., assistant pr<strong>of</strong>essor <strong>of</strong> chemistry at <strong>Rochester</strong>,<br />
and Philippe Fauchet, Ph.D., pr<strong>of</strong>essor and chair <strong>of</strong> the Department <strong>of</strong><br />
Electrical and Computer Engineering, have devised a tiny, bacteria-identifying<br />
sensor that eventually could be reduced down to the size <strong>of</strong> a grain<br />
<strong>of</strong> sand. Their aim is to develop a bandage that will immediately alert<br />
people to the presence <strong>of</strong> dangerous bacteria. While their work began long<br />
before the September 11 attacks, they’re well aware that their technology,<br />
in theory, can be expanded to detect bioterrorist agents such as anthrax.<br />
The <strong>Center</strong> is in the initial phase <strong>of</strong> testing a handheld sensor based on<br />
their work, which was featured in the Journal <strong>of</strong> the American Chemical<br />
Society. With the right funding, says Miller, they could begin large-scale<br />
testing by the end <strong>of</strong> the year.<br />
The bandage is part <strong>of</strong> the <strong>Center</strong> for Future Health’s “smart<br />
medical home,” equipped with several prototype devices that can work<br />
together to monitor your health.<br />
In this home <strong>of</strong> the future, the smart bandage can confer with other<br />
sensors that have been monitoring your gait for signs <strong>of</strong> stroke, your skin<br />
for signs <strong>of</strong> melanoma, and your medicine cabinet for signs your current<br />
medication might conflict with any new medication. A computer, compiling<br />
the information, can suggest in spoken English what steps to take.<br />
Such futuristic ideas are a hallmark <strong>of</strong> academic researchers,<br />
but the federal government also is involved in research that sounds<br />
more like science fiction than science. In a little-known section <strong>of</strong> the<br />
Department <strong>of</strong> Defense, the Defense Advanced Research Projects Agency<br />
(DARPA) is charged with supporting research that’s considered the most<br />
innovative around.<br />
DARPA deals in high-risk, high-reward projects — the kind that,<br />
when successful, can lead to major advances both in military realms and<br />
civilian life. DARPA was founded in 1958 as a direct result <strong>of</strong> the Russian<br />
launch <strong>of</strong> Sputnik. The technology behind the launch was a surprise to<br />
the United States, and Eisenhower “didn’t like it that we were surprised,”<br />
says Mildred Donlon (Mas ’64, Ph.D. ’72). Donlon is the program manager<br />
for DARPA’s Biological Warfare Defense program. She is overseeing the<br />
research and development <strong>of</strong> about a dozen farsighted technologies,<br />
including something considered vital in this new age <strong>of</strong> bioterrorism:<br />
a sensor that could be used in the field to detect biological agents.<br />
Philippe Fauchet, Ph.D.<br />
Right — A conceptual<br />
view <strong>of</strong> the<br />
smart bandage<br />
sending data to<br />
a computer<br />
display device.<br />
SPRING / SUMMER <strong>2002</strong> 21
Ruola Ning, Ph.D., works on imaging technology at <strong>Rochester</strong>.<br />
Such a device would need to be rugged and light enough for the<br />
battlefield, extremely accurate, but not extremely expensive. It would need<br />
to do in minutes what today takes hours in a laboratory.<br />
“ It’s not going to be a single technology that will solve this<br />
problem,” says Donlon, who did radiation biology work with the<br />
Department <strong>of</strong> Defense after graduating from <strong>Rochester</strong>. “It will be<br />
a system <strong>of</strong> technologies.”<br />
Early work in this realm was truly<br />
innovative, focusing on fusing rat-brain<br />
neurons onto semiconductor chips. Today,<br />
Donlon cites three promising technologies<br />
that might some day work together to solve<br />
the problem.<br />
One, a mass spectrometer, is meant<br />
to quickly identify broad classes <strong>of</strong> biological<br />
and chemical agents. From there, an<br />
immunosensor that uses antibodies and a<br />
miniature laser could detect biological agents<br />
on a more fundamental level, by identifying<br />
specific proteins. And a chip device that examines<br />
What these technologies<br />
make clear is that some<br />
scientists were working on<br />
the terrorism problem long<br />
before it became a widespread<br />
concern in this country.<br />
ribosomal RNA messages could differentiate between biological agents that<br />
differ by only a single base pair within the RNA.<br />
It’s a daunting task not only to make the technology work, but also<br />
to make it practical for use. As Donlon puts it, “There’s no due date. These<br />
are new babies, and they need time before they’re ready to come out.”<br />
Such is the nature <strong>of</strong> technology that incorporates the very latest<br />
science. DARPA at least has the luxury <strong>of</strong> functioning as a sort <strong>of</strong> venturecapital<br />
group. Donlon’s program supports research done at private<br />
companies, so she can pick and choose from any project that looks<br />
promising for what she needs.<br />
DARPA helped fund the research behind another potential blockbuster<br />
technology: The Smart Shirt, which incorporates innovations<br />
in textile engineering, wearable computing, and wireless data. The Smart<br />
Shirt has built-in sensors that can monitor the wearer’s heart and respiration<br />
rates and detect hazardous particles in the immediate environment.<br />
The shirt, which doesn’t feel any different from a “not-so-smart” shirt,<br />
can send a person’s biometric information through wireless transmission<br />
to a computer for analysis. The computer, in turn, can alert the wearer<br />
on a wristwatch or personal display apparatus if, for example, the person’s<br />
heart is beating abnormally.<br />
While it has a pedigree that sounds straight out <strong>of</strong> a video game —<br />
coming out <strong>of</strong> the U.S. military’s 21st Century Land Warrior Program —<br />
the Smart Shirt has already proven itself in testing. And it happens to be<br />
a technology that Young believes can fill one <strong>of</strong> the holes we have in our<br />
civil defense.<br />
Young serves on the board <strong>of</strong> the company, Sensatex, that’s working<br />
to market the Smart Shirt. If a biological attack should occur, Smart Shirts<br />
could be the first means <strong>of</strong> detecting that something is wrong. The shirt<br />
can also transmit a person’s location, which Young says is crucial for first<br />
responders at a site such as the World Trade <strong>Center</strong>. “With these shirts,<br />
you can know where someone is buried in rubble,” he says.<br />
With the right funding, Young says, the shirt could be available<br />
within a year.<br />
On the treatment side, Young is devoting his energy to a New Jerseybased<br />
company called EluSys, which is<br />
developing a “heteropolymer system” that uses<br />
two antibodies joined together “like a piece<br />
<strong>of</strong> biological double-sided tape.” One antibody<br />
sticks to the target to be removed —anthrax,<br />
for example — while the other binds to a<br />
receptor found on the red blood cells <strong>of</strong> all<br />
primates. Once the target is bound, the red<br />
blood cells carry the pathogen to the liver for<br />
destruction. In principle, any blood-borne<br />
pathogen or toxin could be removed by the<br />
system, including anthrax, smallpox, plague<br />
and Ebola. In practice, EluSys needs more<br />
funding to test and develop the system.<br />
22<br />
ROCHESTER MEDICINE
What these technologies make clear is that some scientists were<br />
working on the terrorism problem long before it became a widespread<br />
concern in this country. Ruola Ning, Ph.D., an associate pr<strong>of</strong>essor <strong>of</strong> radiology<br />
at <strong>Rochester</strong>, has spent 15 years perfecting a cone-beam technology<br />
for 3-D scanner imaging. Ning says his imaging would retain all <strong>of</strong> the<br />
essential information <strong>of</strong> an object in three dimensions, as opposed to<br />
current scanners, which take a two-dimensional snapshot. Ning sees<br />
numerous applications. A year ago, at a White House conference on the<br />
black-market diamond trade believed to be a way terrorists fund their<br />
operations, Ning proposed his imaging technology for capturing the structural<br />
“fingerprint” <strong>of</strong> raw diamonds, so smuggled diamonds could be<br />
tracked. He also envisioned better airport scanners that could more effectively<br />
detect explosives.<br />
In fact, several years ago, Ning and his colleagues from the optics<br />
and computer science departments demonstrated a prototype to the<br />
Federal Aviation Authority and to the business community.<br />
“We talked to some manufacturers, but they thought this technology<br />
was not needed,” says Ning, who has secondary appointments<br />
in electrical and computer engineering, biomedical engineering, and radiation<br />
oncology. “They thought the airlines wouldn’t want it.”<br />
Much has changed in a few months, and Ning now plans to<br />
reintroduce the idea, which until recently has been more focused on<br />
health care applications.<br />
There’s reason to believe that these kinds <strong>of</strong> research projects will be<br />
taken even more seriously now, given what’s at stake. That’s the impression<br />
that Stanley M. Lemon, M.D. (M ’72), came away with after serving<br />
on a special blue-ribbon panel on bioterrorism held by the NIH National<br />
Institute <strong>of</strong> Allergy and Infectious Diseases, and after attending a workshop<br />
on bioterrorism organized by the Institute <strong>of</strong> Medicine. Participants,<br />
which included the FBI, senators, representatives from the CDC and experts<br />
in virology, bacteriology and other fields, noted the massive increase in<br />
proposed government funding for bioterrorism research.<br />
“There was a clear consensus that the increase in funding was<br />
unprecedented,” says Lemon, who serves as vice chair for the Forum<br />
on Emerging Infections within the Institute <strong>of</strong> Medicine. “The feeling<br />
was that it wasn’t going to be business as usual. There needed to be<br />
products that emerged from this to protect the American public.”<br />
Lemon has made a commitment to that effort as dean <strong>of</strong> the School<br />
<strong>of</strong> Medicine at the <strong>University</strong> <strong>of</strong> Texas <strong>Medical</strong> Branch. His school just<br />
broke ground on a Level 4 laboratory, which is a “full spacesuit containment<br />
lab” that allows researchers to handle the most dangerous materials.<br />
That includes Category A agents such as anthrax.<br />
“ It’s the first one <strong>of</strong> its kind on an academic campus,” says Lemon,<br />
who also helped found his school’s <strong>Center</strong> for Biodefense.<br />
Lemon agrees with the adage that the scourge <strong>of</strong> the 20th century<br />
was the nuclear threat, while the scourge <strong>of</strong> the 21st century will be the<br />
biological and chemical threat. But he, like other researchers dedicating<br />
themselves to finding solutions, sees hope in the quick response from<br />
scientists. And nobody can predict what the breadth <strong>of</strong> benefits might be<br />
from this research.<br />
“ We need to rebuild our scientific capabilities,” he says, “and then<br />
I think there will be lots <strong>of</strong> spin<strong>of</strong>fs for things other than bioterrorism.”<br />
Some day, all our shirts might be smart.<br />
Love Grows in the Lab<br />
It sounds like the concept for a new TV show: A husband and wife, biologist<br />
and engineer by training, spend their days fighting bioterrorism, with the<br />
latest advances in science as their weapons.<br />
But it’s just normal life for the Donlons. Jerome (Ph.D. ’68, M ’72, R ’73)<br />
and Mildred (Mas ’64, Ph.D. ’72) are both hard at work in their respective<br />
government <strong>of</strong>fices in Washington — he on assignment with the new<br />
federal Office <strong>of</strong> Public Health Preparedness, she at the Defense Advanced<br />
Research Projects Agency within the Department <strong>of</strong> Defense. One is working<br />
on the public health response to a bioterrorism attack, the other is trying to<br />
find ways to detect such an attack on the battlefield.<br />
It’s not the first time the Donlons have worked on two sides <strong>of</strong><br />
the same problem. Once upon a time, at <strong>Rochester</strong>, the two were lab partners<br />
in radiation biology class. As Mildred tells it, he was an engineer who<br />
knew math but not biology and she was a biologist who knew biology but<br />
not math. It was the ideal combination, and lab partners quickly became<br />
life partners. It made sense: “Our kids would be perfect,” Mildred jokes.<br />
So how did their experiment go? Their son is studying business at the<br />
<strong>University</strong> <strong>of</strong> Notre Dame, and their daughter is getting her degree in public<br />
health at Yale and is applying to the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> School <strong>of</strong><br />
Medicine and Dentistry.<br />
“Both <strong>of</strong> the children are bright in math, physics and biology,”<br />
says Mildred. “Genetics works!”<br />
SPRING / SUMMER <strong>2002</strong> 23
<strong>Rochester</strong> provides a national model<br />
Drills, training and planning<br />
get the region ready for a potential attack<br />
by Leslie Orr
The scenario: During a wintry day in mid-February at<br />
the height <strong>of</strong> flu season, a handful <strong>of</strong> new patients flowed<br />
into Strong Memorial Hospital’s Emergency Department<br />
with coughs, colds, headaches and fevers. One person<br />
died shortly after being admitted, and an unusually high<br />
number <strong>of</strong> people continued to seek help. Alert, worried<br />
physicians began analyzing illness patterns, and looking<br />
to blood samples and tissue specimens for evidence <strong>of</strong><br />
something other than the flu.<br />
Their answer came from the <strong>Center</strong>s for Disease Control and Prevention<br />
(CDC), which confirmed that a rare disease called tularemia, or “rabbit<br />
fever,” was sweeping through the community. A bacterial infection,<br />
tularemia is usually transmitted to people from deer flies, rodents or an<br />
infected animal’s carcass, most <strong>of</strong>ten afflicting animal handlers and<br />
furriers. But in this case, bioterrorists had released a form <strong>of</strong> tularemia into<br />
a crowded public arena (and <strong>Rochester</strong>’s disaster preparedness was put to the<br />
test.) Within a month, 5,500 local patients had sought treatment at emergency<br />
rooms, clinics and doctors’ <strong>of</strong>fices. An alarming 65 were dead.<br />
The above scenario is pure fiction, but it was devised for a very<br />
important reason. The invented “attack” was used as the basis for a<br />
disaster drill, practiced a couple <strong>of</strong> months ago with more focus than ever<br />
before by dozens <strong>of</strong> <strong>Rochester</strong> public health and safety <strong>of</strong>ficials.<br />
Indeed, when it comes to planning for the unthinkable, “suddenly<br />
everyone is paying attention, and we are truly learning a lot about our<br />
strengths and weaknesses,” says John Benitez, M.D., M.P.H., managing<br />
director <strong>of</strong> the Finger Lakes Regional Poison and Drug Information <strong>Center</strong><br />
at Strong Memorial Hospital and associate pr<strong>of</strong>essor <strong>of</strong> emergency medicine<br />
and environmental medicine. Benitez is also one <strong>of</strong> the <strong>University</strong> <strong>of</strong><br />
<strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong>’s designated representatives on a communitywide<br />
Metropolitan <strong>Medical</strong> Response System (MMRS) team. The MMRS<br />
program addresses issues such as drug distribution in the event <strong>of</strong> mass<br />
casualties, community safety and use <strong>of</strong> secure communications networks.<br />
Such community-wide coordination is one reason <strong>Rochester</strong> is<br />
considered to be at the forefront <strong>of</strong> readiness for a bioterrorism attack.<br />
According to D. A. Henderson, M.D., M.P.H. (M ’54), director <strong>of</strong> the federal<br />
Office <strong>of</strong> Public Health Preparedness, “<strong>Rochester</strong>’s plans are among the<br />
most advanced in the country and it is, in fact, a model.”<br />
<strong>Rochester</strong> stands out, in part, because <strong>of</strong> key federal funding.<br />
It’s one <strong>of</strong> 73 cities to receive a CDC grant in 2001 supporting the<br />
John Benitez, M.D., M.P.H., models the personal protective equipment kit<br />
in Strong Memorial Hospital’s Decontamination Room.<br />
Metropolitan <strong>Medical</strong> Response System, for cities identified as potential<br />
bioterrorism targets. <strong>Rochester</strong>’s proximity to the Canadian border is one<br />
qualifying characteristic. Several physicians, including Benitez, and other<br />
UR <strong>Medical</strong> <strong>Center</strong> <strong>of</strong>ficials, such as Fire Marshal Mark Cavanaugh,<br />
participate in the countywide MMRS drills and planning. And another<br />
CDC grant—one <strong>of</strong> only three in the nation—went to the County Health<br />
Department to develop innovative secure communication tools, under the<br />
Monroe County Health Alert Network. The Strong Memorial Hospital<br />
emergency department and the Finger Lakes Regional Poison <strong>Center</strong> have<br />
links to this system.<br />
Since the Gulf War in the early 1990s, the CDC has provided special<br />
training for the nation’s poison centers on responding to biological or<br />
chemical warfare.<br />
The anthrax deaths that followed the World Trade <strong>Center</strong> terrorism<br />
provided crude lessons in planning, equipment needs, and communications.<br />
Round-table discussions and drills — like the tularemia exercise<br />
that Benitez helped plan for local physicians, hospital administrators, fire,<br />
police and ambulance crews — forced the group to confront key issues<br />
without overlooking minor details.<br />
For example, if such a disaster truly taxed <strong>Rochester</strong>’s hospitals,<br />
what is the best way to provide routine medical care for the rest <strong>of</strong> the<br />
community? What would it take to set up a temporary kidney dialysis<br />
center in a high school gymnasium? How will hospitals communicate<br />
with emergency medical personnel to prevent the spread <strong>of</strong> lethal<br />
contaminates? Where’s the best place to store special equipment so that<br />
it’s easily deployable?<br />
The good news, says Eric Davis, M.D., associate pr<strong>of</strong>essor <strong>of</strong> emergency<br />
medicine at Strong Memorial and regional medical director for<br />
emergency medical services, is that <strong>Rochester</strong> has been preparing for years.<br />
SPRING / SUMMER <strong>2002</strong> 25
Helping Kids Cope, Too<br />
With adults having so much trouble comprehending the events <strong>of</strong><br />
September 11 and subsequent anthrax attacks, it’s natural to wonder how<br />
to help children understand and be safe.<br />
Pediatricians at <strong>Rochester</strong> are doing more than wondering.<br />
The Department <strong>of</strong> Pediatrics has formed the Committee on Bioterrorism/<br />
Disaster Preparedness, headed by Ge<strong>of</strong>frey A. Weinberg, M.D., associate<br />
pr<strong>of</strong>essor <strong>of</strong> pediatrics. The committee developed several ideas, and in January,<br />
Weinberg held a grand rounds entitled “Bioterrorism and You —<br />
A Pediatrician’s Primer.” He reviewed how bioterrorism might affect children<br />
differently from adults and gave background on biological preparedness.<br />
The committee also suggested working with other departments<br />
to present a pediatric grand rounds on disaster-related biopsychosocial issues.<br />
Part <strong>of</strong> being prepared means staying involved with community<br />
resources. Weinberg and Paul Graman, M.D., associate pr<strong>of</strong>essor <strong>of</strong> medicine,<br />
serve on the Monroe County Bioterrorism and Communicable Disease<br />
Task Force and are liaisons to the <strong>Rochester</strong> MMRS. Caroline Breese Hall,<br />
M.D., pr<strong>of</strong>essor <strong>of</strong> pediatrics, serves on several FDA and CDC committees<br />
concerned with bioterrorism.<br />
The work will be ongoing. As the committee put it in their recommendations,<br />
“The effect <strong>of</strong> weapons <strong>of</strong> mass destruction on the psyche <strong>of</strong><br />
the community at large and its children in particular will need to be<br />
addressed at some point.”<br />
“ We’ve always taken this very seriously here, and we are even better<br />
prepared today,” Davis says. “People are recognizing that a disaster plan needs<br />
to be a real disaster plan, and not something you just control on the fly.”<br />
Ironically, local hoaxes and other false alarms in the aftermath<br />
<strong>of</strong> September 11 actually provided opportunities for the testing <strong>of</strong> new<br />
ideas. For example, Davis is on a New York State task force that is pulling<br />
together response teams <strong>of</strong> physicians, nurses and paramedics specially<br />
trained to treat trauma victims at a moment’s notice. This would avoid<br />
having to send untrained personnel into the dangers <strong>of</strong> a ground-zero<br />
situation, Davis says.<br />
Benitez, who joined the <strong>Medical</strong> <strong>Center</strong> in September 2000 after<br />
serving as the medical director <strong>of</strong> the Children’s Hospital <strong>of</strong> Pittsburgh’s<br />
poison center, has been able to identify problem areas and improve on<br />
an already well-honed disaster plan. His team has purchased new personal<br />
protective equipment kits with respirators, special suits, gloves and booties;<br />
maintained funding for staff training on chemical toxicity issues;<br />
and worked with emergency department staffers on recognition <strong>of</strong><br />
symptoms <strong>of</strong> rare diseases and use <strong>of</strong> the facility’s new, state-<strong>of</strong>-the-art<br />
decontamination room.<br />
“ In my 20 years as a physician, I never thought I would be faced<br />
with bioterrorism,” Benitez says. “But we have learned so much about<br />
our response and our ability to integrate with the community. In general,<br />
the system has worked the way it is supposed to each time we test it.”<br />
<strong>Rochester</strong> is called on to study a new<br />
form <strong>of</strong> the old smallpox vaccine<br />
by Tom Rickey<br />
As talk <strong>of</strong> anthrax and smallpox had the nation in<br />
a frenzy last fall, word <strong>of</strong> a possible solution was causing<br />
a stir in <strong>Rochester</strong>. The <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> was one<br />
<strong>of</strong> four sites chosen by the federal government to test if<br />
a diluted form <strong>of</strong> the old smallpox vaccine would be<br />
effective in case <strong>of</strong> an outbreak due to a terrorist attack.<br />
When federal <strong>of</strong>ficials announced the smallpox study a month after<br />
September 11, the nation had only about 15 million smallpox vaccine<br />
doses on hand. Officials wanted to learn how to stretch those doses to<br />
cover a population <strong>of</strong> nearly 300 million. <strong>Rochester</strong> was chosen along<br />
with Saint Louis <strong>University</strong>, Baylor College <strong>of</strong> Medicine and the <strong>University</strong><br />
<strong>of</strong> Maryland because they're part <strong>of</strong> an NIH-funded network to develop and<br />
test vaccines for illnesses such as flu, pneumonia and whooping cough.<br />
When news <strong>of</strong> the study broke, dozens <strong>of</strong> people around the country<br />
immediately called the <strong>University</strong>, <strong>of</strong>fering to drive or fly hundreds <strong>of</strong><br />
miles, calling friends who worked at the institution, even suggesting<br />
special status as investors in vaccine companies — all in their efforts to<br />
be protected should a smallpox attack occur.<br />
“What makes smallpox so scary is that one in three people who<br />
contract it die from it,” says vaccine expert John Treanor, M.D., associate<br />
pr<strong>of</strong>essor <strong>of</strong> medicine and leader <strong>of</strong> the <strong>Rochester</strong> portion <strong>of</strong> the study.<br />
“ And it's extremely contagious. Someone would have to be out <strong>of</strong> his mind<br />
to release it, because chances are good that it would come back to kill that<br />
person's mother, father, children, and himself.”<br />
26<br />
ROCHESTER MEDICINE
Hundreds <strong>of</strong><br />
volunteers flocked<br />
to the smallpox<br />
vaccine study at<br />
the <strong>Medical</strong> <strong>Center</strong>.<br />
Before 1972, getting the vaccine was regarded as a harmless rite <strong>of</strong><br />
passage: Schoolchildren received the vaccine, then went back to the classroom<br />
the same day and compared scabs later in the week. The dime-sized<br />
scar that nearly all U.S. citizens older than 32 carry on their upper arms or<br />
elsewhere on the body is pro<strong>of</strong> that they received the vaccine as a child.<br />
The vaccine is the same one that was used in the worldwide immunization<br />
program that eradicated smallpox.<br />
The closely studied and monitored vaccinations <strong>of</strong> today are a far<br />
cry from how people in Europe used to protect themselves from smallpox,<br />
says Treanor. It was not uncommon for people in the 1700s and 1800s<br />
to pull <strong>of</strong>f a scab from an infected friend or family member, then rub<br />
the scab over their own skin in an effort to protect themselves.<br />
“ While the thought is disgusting to us, they were really undertaking<br />
a crude form <strong>of</strong> vaccination,” says Treanor. “While about one <strong>of</strong> every<br />
three people who contract the disease naturally die, the death rate drops<br />
to only about one in 100 for people who infected themselves this way.”<br />
Throughout November and December, the Vaccine Testing and<br />
Evaluation Unit fielded hundreds <strong>of</strong> calls from potential volunteers.<br />
Treanor and a team <strong>of</strong> nurses and doctors worked long hours evaluating<br />
volunteers, eventually enrolling 170 adults between the ages <strong>of</strong> 18 and<br />
30 who had never been vaccinated against smallpox. In all, 650 individuals<br />
around the country lined up in a repeat <strong>of</strong> a once-routine occurrence:<br />
Vaccination against one <strong>of</strong> the deadliest diseases ever to face humankind.<br />
Treanor and his team completed the study despite a steady stream <strong>of</strong> TV and<br />
newspaper reporters that trouped through Strong to document the study.<br />
Student Tia Neely appeared on NBC Nightly News and MSNBC as one<br />
<strong>of</strong> the first people in the world in 25 years to be vaccinated, and other<br />
participants were featured on the front page <strong>of</strong> the Boston Globe,<br />
the Baltimore Sun, and other publications around the country. Most<br />
volunteers spoke <strong>of</strong> their participation as their patriotic duty, while several<br />
simply took advantage <strong>of</strong> the opportunity to be vaccinated in case <strong>of</strong><br />
an attack. Some participated for the money <strong>of</strong>fered: $25 per visit.<br />
In March, Treanor and his colleagues announced their findings:<br />
Diluted forms <strong>of</strong> the vaccine are as effective in protecting against the<br />
disease. Treanor’s team plans to conduct further studies <strong>of</strong> people who<br />
have been vaccinated to learn more about their immunity.<br />
“ I am proud that we were able to organize and conduct the study<br />
so quickly, and to contribute something to the country’s preparations for<br />
the unthinkable,” says Treanor.<br />
John Treanor, M.D., prepares a volunteer for vaccination.<br />
SPRING / SUMMER <strong>2002</strong> 27
A lasting<br />
memorial<br />
On October 21, 2001,<br />
Howard Beaton, M.D.<br />
(M ’76), spoke at the<br />
traditional Reunion<br />
Memorial Service during Reunion Weekend.<br />
Here are his words, on the immediate tragedy<br />
<strong>of</strong> September 11 — which he witnessed —<br />
and an impassioned idea for how we can<br />
best honor those who were lost.<br />
For the last eight years, it has been my privilege<br />
to be the chief <strong>of</strong> surgery and emergency<br />
services at NYU Downtown Hospital. For those <strong>of</strong><br />
you not familiar with New York City, this is a 200-<br />
bed community hospital in lower Manhattan.<br />
Late on a summer afternoon, the western facade<br />
<strong>of</strong> the hospital and my <strong>of</strong>fice windows were<br />
formerly in the shadow <strong>of</strong> the North Tower <strong>of</strong> the<br />
World Trade <strong>Center</strong>. Today we describe the location<br />
<strong>of</strong> the hospital as “four blocks from Ground Zero.”<br />
It has been said that on September 11, every<br />
American became a New Yorker. Whether you<br />
were an eyewitness to the Towers’ collapse,<br />
as I was, or watched it on TV, you shared in the<br />
unimaginable enormity <strong>of</strong> this disaster. Whether<br />
you actually smelled the acrid odor and became<br />
covered in the gray ash that burned your eyes<br />
and skin and irritated your lungs, as I was, or<br />
just saw the images <strong>of</strong> the advancing dust cloud,<br />
you were there. Whether you actually helped to<br />
care for hundreds <strong>of</strong> injured patients in the first<br />
few hours after the planes struck and then<br />
waited in sad frustration, hour after hour and<br />
day after day, for the second wave <strong>of</strong> survivors<br />
which never materialized, as I did, or just read<br />
about it in your newspaper, you were there, too.<br />
Whether you saw the faces on the posters that<br />
were plastered on the walls <strong>of</strong> every medical<br />
facility by the families <strong>of</strong> the thousands <strong>of</strong><br />
missing victims, as I did, or just heard the grim<br />
statistics, you also grieved for their loss and pain.<br />
On September 11, we lost hundreds <strong>of</strong> incredibly<br />
brave firemen, policemen and paramedics.<br />
These individuals were extraordinary heroes. On<br />
September 11, we also lost thousands <strong>of</strong> ordinary<br />
people: men and women <strong>of</strong> every race and religion;<br />
cooks and stockbrokers, janitors and<br />
executives; people who had just gone to their<br />
daily work — people just like you and me. Every<br />
generation, it seems, goes through a tragedy<br />
that tears away its innocence. In recent memory,<br />
there have been Pearl Harbor, the assassinations<br />
<strong>of</strong> President Kennedy, Martin Luther King and<br />
Robert Kennedy, and now the terrorist attack on<br />
the World Trade <strong>Center</strong>.<br />
I have been asked how we can create a memorial<br />
to so many innocent victims. How can we<br />
explain to generations yet to come the feelings<br />
that we share today? Mayor Giuliani has<br />
suggested that we should return to our normal<br />
daily activities, and indeed we must do so. I have<br />
heard promises that the World Trade <strong>Center</strong> will<br />
be rebuilt in some yet undetermined form that<br />
will include a permanent memorial to those lost in<br />
this cowardly attack. Personally, I would like to see<br />
the Twin Towers rebuilt to be the tallest buildings<br />
in the world, as a symbol <strong>of</strong> our defiance.<br />
However, regardless <strong>of</strong> its size, I think that no<br />
structure <strong>of</strong> steel and concrete can be enough <strong>of</strong><br />
a memorial to the memory <strong>of</strong> so many people.<br />
I believe that the clues to a fitting memorial are<br />
all around us. They are in the hundreds <strong>of</strong><br />
volunteers who walked, rode bicycles or hitchhiked<br />
to our hospital and other medical<br />
facilities on the morning <strong>of</strong> September 11. There<br />
are clues in the handwritten notes and cards<br />
that we received from elementary-school<br />
children from small towns in Kentucky, Kansas<br />
and North Carolina, to name a few; in the words<br />
<strong>of</strong> encouragement we received from ER nurses<br />
from North Dakota and in a letter that I received<br />
from the medical staff at the hospital <strong>of</strong> the<br />
<strong>University</strong> <strong>of</strong> Wisconsin. Clues are present in the<br />
truckload <strong>of</strong> teddy bears we received from<br />
children in Oklahoma City.<br />
It is this pr<strong>of</strong>ound sense <strong>of</strong> unity among all<br />
Americans that we must now preserve as our<br />
memorial to these victims. September 11<br />
changed everything. We cannot simply let<br />
ourselves slip back into the way we behaved<br />
towards each other in the past. Similarly, no<br />
single act <strong>of</strong> kindness or generosity, no matter<br />
how great, is sufficient to be a permanent<br />
memorial to these victims.<br />
If you are a doctor or a nurse, you must volunteer<br />
in a clinic or take extra emergency call at<br />
your local hospital. If you are a lawyer, you must<br />
devote some <strong>of</strong> your time to pro bono cases.<br />
If you are an architect or engineer, you must<br />
volunteer your services for some needed<br />
community project. Become involved at a<br />
homeless shelter, soup kitchen or some worthy<br />
advocacy group. Help an old woman cross the<br />
street or a young mother with a stroller down the<br />
stairs. Give directions to the stranger who<br />
appears lost. Pick up a piece <strong>of</strong> someone else’s<br />
litter. And, <strong>of</strong> course, we must give to charity on<br />
a regular basis, not just now. And every time we<br />
do something for someone else just because it is<br />
the right thing to do, we should say, “September<br />
11th.” When our children ask us what this<br />
means, we should explain that this is our<br />
enduring memorial to these thousands <strong>of</strong> innocent<br />
victims <strong>of</strong> terrorism.<br />
The attack on the World Trade <strong>Center</strong> ripped<br />
apart not just the skyline <strong>of</strong> downtown<br />
Manhattan but the very fabric <strong>of</strong> our human<br />
interaction. I know it changed me. How we<br />
rebuild is up to each and every one <strong>of</strong> us.
school news<br />
Guzick was named by Good<br />
Housekeeping as one <strong>of</strong> “America’s 400<br />
Best Doctors for Women” and has published<br />
more than 100 articles. He is a member <strong>of</strong><br />
numerous societies, including the American<br />
Gynecologic and Obstetric Society, the Society<br />
for Gynecologic Investigation, and the<br />
American Board <strong>of</strong> Obstetrics and Gynecology.<br />
Guzick named Dean <strong>of</strong> School <strong>of</strong><br />
Medicine and Dentistry<br />
David S. Guzick, M.D., Ph.D., has been appointed the<br />
ninth dean <strong>of</strong> the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> School<br />
<strong>of</strong> Medicine and Dentistry. Guzick succeeds Dean<br />
Edward M. Hundert, who will become president<br />
<strong>of</strong> Case Western Reserve <strong>University</strong> in Cleveland<br />
in August. Guzick has served as the Henry A.<br />
Thiede pr<strong>of</strong>essor and chair <strong>of</strong> the Department<br />
<strong>of</strong> Obstetrics and Gynecology at the <strong>University</strong><br />
<strong>of</strong> <strong>Rochester</strong> School <strong>of</strong> Medicine and Dentistry<br />
since 1995, in addition to chief <strong>of</strong> service <strong>of</strong><br />
Obstetrics and Gynecology at Strong Memorial<br />
Hospital and Highland Hospital.<br />
Guzick came to <strong>Rochester</strong> from the<br />
<strong>University</strong> <strong>of</strong> Pittsburgh School <strong>of</strong> Medicine<br />
and Magee-Women’s Hospital, where he served<br />
as pr<strong>of</strong>essor <strong>of</strong> obstetrics, gynecology and reproductive<br />
science and director <strong>of</strong> the Division <strong>of</strong><br />
Reproductive Endocrinology. He earned his<br />
medical degree and Ph.D. from New York <strong>University</strong>.<br />
Following a residency at The Johns Hopkins<br />
Hospital, he completed a fellowship in reproductive<br />
endocrinology at the <strong>University</strong> <strong>of</strong> Texas,<br />
Southwestern <strong>Medical</strong> School. Guzick is board<br />
certified in obstetrics and gynecology and in<br />
reproductive endocrinology.<br />
Former Surgeon General Satcher<br />
accepts faculty appointment<br />
David Satcher, M.D. (R ’72), the 16th surgeon<br />
general <strong>of</strong> the United States, has joined the<br />
<strong>University</strong> <strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong> faculty<br />
in a two-year consultative role as senior advisor<br />
for community health. Satcher also will have<br />
adjunct faculty appointments with the pediatrics<br />
and community health and preventive<br />
medicine departments.<br />
Satcher will visit the <strong>University</strong> several<br />
times annually to deliver guest lectures, participate<br />
in grand rounds and visit with community<br />
organizations and government <strong>of</strong>ficials in an<br />
effort to improve access to health care.<br />
In addition, Satcher will provide<br />
strategic guidance on the planning and direction<br />
<strong>of</strong> Project Believe, a <strong>Medical</strong> <strong>Center</strong><br />
initiative to make <strong>Rochester</strong> the healthiest<br />
community in America by the year 2020.<br />
Through the project, the <strong>Medical</strong> <strong>Center</strong> has<br />
been directing the resources <strong>of</strong> its research,<br />
education and patient care teams to developing<br />
creative health interventions throughout the<br />
community.<br />
“We are thrilled and honored that Dr.<br />
Satcher has accepted this position,” says Jay<br />
Stein, M.D., senior vice president and vice<br />
provost for health affairs and CEO <strong>of</strong> the<br />
<strong>Medical</strong> <strong>Center</strong> and Strong Health. “As you can<br />
imagine, Dr. Satcher had numerous opportunities<br />
awaiting him at the end <strong>of</strong> his surgeon<br />
general’s term, and the fact that he chose to<br />
devote some <strong>of</strong> his time to Project Believe is an<br />
endorsement <strong>of</strong> the community health mission<br />
<strong>of</strong> this <strong>University</strong>.”<br />
In February, Satcher completed his term<br />
as surgeon general. In September he will<br />
become director <strong>of</strong> the National <strong>Center</strong> for<br />
Primary Care at Morehouse School <strong>of</strong><br />
Medicine. He also serves as the senior visiting<br />
fellow <strong>of</strong> the Henry J. Kaiser Family<br />
Foundation, advising on its programs and<br />
working on a book about his experiences as<br />
surgeon general.<br />
International expert named<br />
Cancer <strong>Center</strong> director<br />
The <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong><br />
appointed Richard I. Fisher, M.D., director <strong>of</strong><br />
its James P. Wilmot Cancer <strong>Center</strong> and director<br />
<strong>of</strong> Cancer Services for Strong Health. Fisher<br />
is an internationally known expert in biological<br />
research and treatment <strong>of</strong> lymphoma.<br />
He served as director <strong>of</strong> the Cardinal Bernardin<br />
Cancer <strong>Center</strong> at Loyola <strong>University</strong> Stritch<br />
School <strong>of</strong> Medicine, in Chicago, since 1984.<br />
At Loyola, Fisher was instrumental in<br />
the creation <strong>of</strong> the Cardinal Bernardin Cancer<br />
<strong>Center</strong>. He helped secure new lab space and<br />
championed building a $35 million facility for<br />
cancer prevention, treatment and research.<br />
He has big plans at <strong>Rochester</strong>, too.<br />
SPRING / SUMMER <strong>2002</strong> 29
school news<br />
Richard Fisher, M.D.<br />
“I want to build a world-class cancer<br />
research and treatment facility to provide<br />
state-<strong>of</strong>-the-art care with the newest and best<br />
treatments for patients with cancer,” says<br />
Fisher, who was also appointed chief <strong>of</strong> the<br />
Hematology / Oncology Unit in the Department<br />
<strong>of</strong> Medicine and the Samuel E. Durand<br />
Pr<strong>of</strong>essor <strong>of</strong> Medicine.<br />
Fisher will oversee clinical cancer<br />
services at Strong Memorial Hospital and<br />
Highland Hospital, which together provide<br />
comprehensive care for cancer patients<br />
throughout western and upstate New York.<br />
“Dr. Fisher is a nationally renowned<br />
cancer clinician, scientist, and educator,”<br />
says Edward M. Hundert, M.D., dean <strong>of</strong> the<br />
School <strong>of</strong> Medicine and Dentistry. “All <strong>of</strong> his<br />
science and clinical work starts with the patient<br />
at the center. We are thrilled he has taken on<br />
the leadership <strong>of</strong> the Cancer <strong>Center</strong>.”<br />
A graduate <strong>of</strong> Harvard College and<br />
Harvard <strong>Medical</strong> School, Fisher completed<br />
an internship and residency at Massachusetts<br />
General Hospital. He held an oncology fellowship<br />
and worked as a senior investigator at<br />
the National Cancer Institute from 1972 to 1984.<br />
Fisher’s research centers on the biology<br />
and treatment <strong>of</strong> lymphoma, cancers derived<br />
from white blood cells, and he has led national<br />
and international studies in Hodgkin’s disease<br />
and non-Hodgkin’s lymphoma. He is chairman<br />
<strong>of</strong> the Lymphoma Committee <strong>of</strong> the Southwest<br />
Oncology Group, a cooperative clinical research<br />
organization that includes 283 institutions and<br />
more than 4,000 physicians.<br />
Fisher is a member <strong>of</strong> numerous organizations,<br />
including the American Joint<br />
Committee on Cancer’s Lymphoma Task Force,<br />
American Society <strong>of</strong> Clinical Oncology and the<br />
American Association for Cancer Research. He<br />
has authored more than 250 articles and chapters<br />
in national and international publications.<br />
JAMA article rewrites the definition<br />
<strong>of</strong> a “good doctor”<br />
Ronald Epstein, M.D.<br />
Something important has been missing from<br />
medical-school assessments <strong>of</strong> physicians and<br />
students. Edward M. Hundert, M.D., dean <strong>of</strong> the<br />
School <strong>of</strong> Medicine and Dentistry, and Ronald<br />
M. Epstein, M.D., a practicing physician in the<br />
Department <strong>of</strong> Family Medicine, are doing<br />
something about it.<br />
The two co-authored “Defining and<br />
Assessing Pr<strong>of</strong>essional Competence,” which<br />
appeared in the Jan. 9 issue <strong>of</strong> the Journal <strong>of</strong><br />
the American <strong>Medical</strong> Association along with<br />
an endorsing editorial by the executive director<br />
<strong>of</strong> the Accreditation Council for Graduate<br />
<strong>Medical</strong> Education (ACGME).<br />
Epstein and Hundert expand on what<br />
it means to be a good doctor to include <strong>of</strong>ten<br />
overlooked areas such as interpersonal skills,<br />
teamwork, learning strategies, clinical<br />
reasoning, and managing ambiguous clinical<br />
situations. They also propose changes in assessment<br />
techniques to account for these qualities.<br />
“For patients, it’s not enough to know<br />
that their doctor scored well on a multiplechoice<br />
test,” says Epstein, who developed his<br />
ideas as part <strong>of</strong> the new competency-assessment<br />
approach within the Double Helix curriculum.<br />
As a family physician, Epstein took a<br />
broad view <strong>of</strong> what constitutes competent<br />
medical practice. After examining the ways<br />
that medical students are being taught and<br />
assessed, he found that not all the right questions<br />
were being asked.<br />
“There were lots <strong>of</strong> studies <strong>of</strong> the reliability<br />
<strong>of</strong> assessment instruments, but very little on<br />
whether what we assess is really what matters in<br />
medical care,” says Epstein. “More troubling was<br />
that few people had even identified a problem.”<br />
Epstein studied the philosophy <strong>of</strong> medicine,<br />
from the earliest writings in Greece and<br />
India to modern discussions <strong>of</strong> ethics and<br />
pr<strong>of</strong>essionalism. He also drew on his original<br />
training in music, which emphasizes the use<br />
<strong>of</strong> all mental faculties — including thinking,<br />
reasoning, judgment and emotions — along<br />
with a technical skill.<br />
Many <strong>of</strong> the ideas in the JAMA article<br />
are already embodied in <strong>Rochester</strong>’s new<br />
curriculum, which intertwines basic science<br />
and clinical work throughout training like<br />
the strands <strong>of</strong> a double helix. At the end <strong>of</strong><br />
the second and third years, students take part<br />
in a pr<strong>of</strong>essional-competency assessment that<br />
lasts two full weeks and embodies all <strong>of</strong> the<br />
elements <strong>of</strong> competence laid out in Epstein<br />
and Hundert’s article.<br />
The Department <strong>of</strong> Education’s<br />
Foundation for the Improvement <strong>of</strong> Post-<br />
Secondary Education decided to support<br />
development <strong>of</strong> the new comprehensive-assessment<br />
methodology with a half-million-dollar<br />
grant. It reasoned that the <strong>Rochester</strong> approach<br />
could become a national model.<br />
The ACGME director’s endorsement makes<br />
it likely that <strong>Rochester</strong>’s new definition <strong>of</strong><br />
competence will be widely discussed at federal<br />
agencies, medical schools, and licensing boards<br />
interested in improving the quality <strong>of</strong> care.<br />
30<br />
ROCHESTER MEDICINE
school news<br />
Above — David Sada (M '05), Mrs. Nancy Evarts (B ’54), C. McCollister<br />
Evarts (M ’57, R ’64), Elethea Caldwell (R ’69), Robert Caldwell (M ’61,<br />
R ’69), and Sean Hislop (M ’05) tour the M.E.T.A.L. Arts Gallery at the Deans’<br />
<strong>Spring</strong> Event for first-year students and local 10-Year-Club alumni.<br />
Above right — First-year medical students and Lindsey<br />
Henson, M.D., senior associate dean for medical education, gather at<br />
the event. Left to right — Chinlin Ching, Owen Halloran, Shay Martinez,<br />
Michael Kim, Dean Lindsey Henson, Denise Aronzon, Michael Hehir,<br />
Brian Recht, Arvind Bakhru, and Michael Pirri.<br />
Right — Participants grab a bite to eat. From left — Sanjeewa<br />
Goonasekera, Lakmal Kotelawala, Maureen Goodman, Adrienne<br />
Carruth, and Fernando Ontiveros-Llamas.<br />
New ophthalmology chair is<br />
an inventor and leader<br />
Steven E. Feldon, M.D., M.B.A., is an acclaimed<br />
clinical and basic scientist with a specialty in<br />
orbital disease and neuro-ophthalmology, an<br />
inventor <strong>of</strong> ophthalmic instruments, and an<br />
entrepreneur and business executive who<br />
started his own company to market his inventions.<br />
He’s also the new chair <strong>of</strong> the <strong>University</strong><br />
<strong>of</strong> <strong>Rochester</strong> Department <strong>of</strong> Ophthalmology,<br />
with a definite goal in mind.<br />
“ Ten years from today, the eye institute<br />
will be perceived as one <strong>of</strong> the top 10 centers<br />
for the study and care <strong>of</strong> the eye,” says Feldon.<br />
“ We have an unparalleled opportunity here in<br />
<strong>Rochester</strong> to advance eye care regionally,<br />
nationally and worldwide.”<br />
Existing strengths at <strong>Rochester</strong> will lay<br />
the foundation, he says.<br />
“ The <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> already has<br />
experts in various centers <strong>of</strong> excellence that<br />
focus on visual science, including the <strong>Center</strong><br />
for Visual Science, brain and cognitive sciences,<br />
computer science, optics, ophthalmology,<br />
neurobiology, anatomy and neurology,”<br />
explains Feldon. “Our opportunity is to bring<br />
them all together to advance the science <strong>of</strong><br />
ophthalmology in a very significant way, and<br />
further complement that knowledge base by<br />
recruiting additional specialists and scientists.”<br />
Feldon has a special interest in the management<br />
<strong>of</strong> patients with thyroid-associated eye<br />
disease, and his clinical expertise has been<br />
recognized in the publication Best Doctors<br />
in America.<br />
Among his career accomplishments,<br />
he has invented ophthalmic instruments and<br />
created a company to manufacture and market<br />
them. He also created a company to market<br />
an electronic medical record-keeping system,<br />
which he invented. His current research investigates<br />
the biological origin <strong>of</strong> Graves’ disease.<br />
Feldon was recruited from the No. 7-<br />
ranked Doheny Eye Institute in Los Angeles,<br />
where he served as associate chair <strong>of</strong> the<br />
Department <strong>of</strong> Ophthalmology at the <strong>University</strong><br />
<strong>of</strong> Southern California and vice president <strong>of</strong><br />
business development, marketing and finance<br />
<strong>of</strong> the Doheny Eye <strong>Medical</strong> Group Inc.<br />
Feldon earned his medical degree<br />
from Albert Einstein College <strong>of</strong> Medicine. He<br />
completed his residency at the Massachusetts<br />
Eye & Ear Infirmary, Harvard <strong>University</strong>, along<br />
with three fellowships: a research fellowship in<br />
neurosurgery at Massachusetts General Hospital,<br />
a clinical fellowship in ophthalmology at<br />
Harvard <strong>Medical</strong> School and a clinical fellowship<br />
in neuro-ophthalmology at the <strong>University</strong> <strong>of</strong><br />
California <strong>Medical</strong> <strong>Center</strong>, San Francisco.<br />
SPRING / SUMMER <strong>2002</strong> 31
school news<br />
Match Day <strong>2002</strong><br />
Getting the call, making the call and<br />
starting the celebration.<br />
32<br />
ROCHESTER MEDICINE
school news<br />
Alabama<br />
Sarah Bean<br />
Pathology<br />
U Alabama Hosp-Birmingham<br />
Birmingham<br />
California<br />
Christine Bower<br />
Neurology<br />
UC Los Angeles<br />
Los Angeles<br />
Christine Bower<br />
Medicine-Preliminary<br />
UC San Diego Med Ctr<br />
San Diego<br />
Nicholas Byrne<br />
Pathology<br />
UC San Francisco<br />
San Francisco<br />
Victor Chiu<br />
Medicine-Preliminary<br />
UC Irvine Med Ctr<br />
Orange<br />
Ilia Christy<br />
Medicine-Pediatrics<br />
UC San Diego Med Ctr<br />
San Diego<br />
Jeremy Hirst<br />
Psychiatry<br />
UC San Diego Med Ctr<br />
San Diego<br />
Sara Tamarin<br />
Pediatrics<br />
UC Davis Med Ctr-Sac<br />
Sacramento<br />
Colorado<br />
Jeffrey Faragher<br />
Emergency Medicine<br />
Denver Health Med Ctr<br />
Denver<br />
Florida<br />
Gurjeet Birdee<br />
Medicine-Pediatrics<br />
Jackson Memorial Hosp<br />
Miami<br />
Jennifer Citron<br />
Pediatrics<br />
U Florida Prog-Shands Hosp<br />
Gainesville<br />
Hawaii<br />
Christy Taoka<br />
Internal Medicine<br />
Tripler Army Med Ctr<br />
Honolulu<br />
Illinois<br />
James Goldman<br />
Ophthalmology<br />
Northwestern Med<br />
Chicago<br />
Minh-Doan Nguyen<br />
Plastic Surgery<br />
SIU SOM & Affl Hosps<br />
<strong>Spring</strong>field<br />
Maine<br />
Joseph Donohue<br />
General Surgery<br />
Maine <strong>Medical</strong> <strong>Center</strong><br />
Portland<br />
Donald Medd<br />
Internal Medicine<br />
Maine <strong>Medical</strong> <strong>Center</strong><br />
Portland<br />
Maryland<br />
Hubert Fenton<br />
Pathology<br />
Johns Hopkins Hosp<br />
Baltimore<br />
David Maine<br />
Anesthesiology<br />
Johns Hopkins Hosp<br />
Baltimore<br />
Lena Mayes<br />
Medicine-Preliminary<br />
Johns Hopkins/Sinai<br />
Baltimore<br />
Tsuyoshi Mitarai<br />
Medicine-Emergency Med<br />
Univ Maryland Med Ctr<br />
Baltimore<br />
Massachusetts<br />
Jennifer Dorantes<br />
Internal Medicine<br />
Baystate Med Ctr<br />
<strong>Spring</strong>field<br />
Keith Downing<br />
Obstetrics-Gynecology<br />
Brigham & Womens Hosp<br />
Boston<br />
Trustin Ennacheril<br />
Internal Medicine<br />
B I Deaconess Med Ctr<br />
Boston<br />
Michael Kaufman<br />
Anesthesiology<br />
Massachusetts Gen Hosp<br />
Boston<br />
Michael Kaufman<br />
Medicine-Preliminary<br />
Baystate Med Ctr<br />
<strong>Spring</strong>field<br />
Vincent Ko<br />
Pathology<br />
Massachusetts Gen Hosp<br />
Boston<br />
Brenda Lawrence<br />
Medicine-Pediatrics<br />
Baystate Med Ctr<br />
<strong>Spring</strong>field<br />
Lori Schleicher<br />
Internal Medicine<br />
Boston U Med Ctr<br />
Boston<br />
Ross Zeltser<br />
Dermatology<br />
Boston U Med Ctr<br />
Boston<br />
Michigan<br />
Joon Choi<br />
Plastic Surgery<br />
U Michigan Hosps-Ann Arbor<br />
Ann Arbor<br />
SPRING / SUMMER <strong>2002</strong> 33
school news<br />
Edward Hall<br />
Ophthalmology<br />
U. Michigan Hosps<br />
Ann Arbor<br />
Minnesota<br />
Christian Capitini<br />
Pediatrics<br />
U Minnesota Med School<br />
Minneapolis<br />
Victor Chiu<br />
Ophthalmology<br />
U Minnesota Med School<br />
Minneapolis<br />
Christina Eadie<br />
Transitional<br />
Hennepin Co Med Ctr<br />
Minneapolis<br />
North Carolina<br />
Gregory Lam<br />
Internal Medicine<br />
Duke Univ Med Ctr<br />
Durham<br />
Shane Reeves<br />
Obstetrics-Gynecology<br />
Univ North Carolina Hosp<br />
Chapel Hill<br />
New York<br />
Trinh Bang<br />
Internal Medicine<br />
Beth Israel Med Ctr<br />
New York<br />
Roman Bloch<br />
Medicine-Preliminary<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Ian Bristol<br />
Medicine-Preliminary<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Andrew Brown<br />
Medicine-Preliminary<br />
Mt Sinai Hospital<br />
New York<br />
Andrew Brown<br />
Neurology<br />
Albert Einstein<br />
New York<br />
Mark Burkard<br />
Internal Med/Research<br />
NYP Hosp Cornell<br />
New York<br />
Christina Cashimere<br />
Internal Medicine<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Eric Chang<br />
Medicine-Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Caesar Djavaherian<br />
Emergency Medicine<br />
Mt Sinai Hospital<br />
New York<br />
Caesar Djavaherian<br />
Medicine-Preliminary<br />
St Lukes-Roosevelt<br />
New York<br />
Mathew Empie<br />
Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Felix Fianko<br />
Anesthesiology<br />
NYP Hosp Cornell<br />
New York<br />
James Goldman<br />
Medicine-Preliminary<br />
Unity Health System<br />
<strong>Rochester</strong><br />
Christopher Good<br />
Orthopaedic Surgery<br />
Hosp For Special Surg<br />
New York<br />
Edward Hall<br />
Medicine-Preliminary<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Marc Halterman<br />
Internal Med/Neurology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Marc Halterman<br />
Neurology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Kelli Harding<br />
Medicine-Preliminary<br />
Mt Sinai Hospital<br />
New York<br />
Kelli Harding<br />
Psychiatry<br />
NYP Hosp-Colum Presby<br />
New York<br />
Jennifer Hayes<br />
Anesthesiology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Hoon Jung<br />
Ophthalmology<br />
SUNY-Buffalo/Ed Cons<br />
Buffalo<br />
Hoon Jung<br />
Transitional<br />
Wilson Mem Reg/UHS<br />
Johnson City<br />
Tashveen Kaur<br />
Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Adam Kelly<br />
Internal Med/Neurology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Adam Kelly<br />
Neurology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Alan Kenny<br />
Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
34<br />
ROCHESTER MEDICINE
school news<br />
Amanda Knapp<br />
Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Melissa Langdon<br />
Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Karen Leitner<br />
Medicine-Pediatrics<br />
Mt Sinai Hospital<br />
New York<br />
Quoc Lu<br />
Medicine-Preliminary<br />
St Lukes-Roosevelt<br />
New York<br />
Timothy Lum<br />
Emergency Medicine<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Lena Mayes<br />
Anesthesiology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Thalia Mayes<br />
Internal Medicine<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Laticia Mendler<br />
Internal Medicine<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Igor Mikityansky<br />
Medicine-Preliminary<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Igor Mikityansky<br />
Radiology-Diagnostic/MPH<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Gregory Nielsen<br />
Pediatrics<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Bridget O’Mara<br />
Transitional<br />
Mary Imogene Bassett<br />
Cooperstown<br />
Bridget O’Mara<br />
Radiology-Diagnostic<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Nicolas Oreskovic<br />
Medicine-Pediatrics<br />
Mt Sinai Hospital<br />
New York<br />
Pamela Polashenski<br />
Internal Medicine<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Catherine Rahilly<br />
Internal Medicine<br />
Mt Sinai Hospital<br />
New York<br />
Elizabeth Reddy<br />
Medicine-Pediatrics<br />
Mt Sinai Hospital<br />
New York<br />
James Richardson<br />
Internal Medicine<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Andrew Robinson<br />
Ophthalmology<br />
SUNY Upstate Med Ctr<br />
Syracuse<br />
Andrew Robinson<br />
Transitional<br />
St Josephs-Syracuse<br />
Syracuse<br />
Paul Rowe<br />
Surgery-Preliminary<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
George Semien<br />
Anesthesiology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
George Semien<br />
Medicine-Preliminary<br />
Unity Health System<br />
<strong>Rochester</strong><br />
Jennifer Shaulinski<br />
Anesthesiology<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Jennifer Shaulinski<br />
Medicine-Preliminary<br />
<strong>Rochester</strong> Gen Hosp<br />
<strong>Rochester</strong><br />
Chandler Shyu<br />
Radiology-Diagnostic/MPH<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Rose St. Fleur<br />
Pediatrics<br />
Winthrop-Univ Hosp<br />
Mineola<br />
Hiroshi Takeyama<br />
Transitional<br />
Sound Shore Med Ctr<br />
New Rochelle<br />
Hiroshi Takeyama<br />
Radiology-Diagnostic<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Brian Wong<br />
Medicine-Pediatrics<br />
St Vincents Hosp<br />
New York<br />
Hsiang Yin<br />
Pediatrics<br />
NYU School Of Medicine<br />
New York<br />
Alison Walker<br />
Internal Medicine<br />
U <strong>Rochester</strong>/Strong Mem<br />
<strong>Rochester</strong><br />
Ross Zeltser<br />
Medicine-Preliminary<br />
Lenox Hill Hospital<br />
New York<br />
SPRING / SUMMER <strong>2002</strong> 35
school news<br />
Ohio<br />
Christina Eadie<br />
Phys Medicine & Rehab<br />
Ohio State Univ Med Ctr<br />
Columbus<br />
Peter Letourneau<br />
Plastic Surgery<br />
Univ Hosps Cleveland<br />
Cleveland<br />
William Plerhoples<br />
Emergency Medicine<br />
Metrohealth Med Ctr<br />
Cleveland<br />
Er-Wey Teng<br />
Internal Medicine<br />
Univ Hosps Cleveland<br />
Cleveland<br />
Oregon<br />
Elizabeth Kehr<br />
Medicine-Primary<br />
Oregon Health & Science Univ<br />
Portland<br />
Alivia Thompson<br />
General Surgery<br />
Oregon Health & Science Univ<br />
Portland<br />
Pennsylvania<br />
Roman Bloch<br />
Radiology-Diagnostic<br />
Univ Health Ctr Of Pittsburgh<br />
Pittsburgh<br />
Jennifer Blum<br />
Peds/Psych/Child Psych<br />
Univ Health Ctr Of Pittsburgh<br />
Pittsburgh<br />
Leah Greenhill<br />
Ophthalmology<br />
Univ Health Ctr Of Pittsburgh<br />
Pittsburgh<br />
Leah Greenhill<br />
Transitional<br />
Mercy Hosp-Pittsburgh<br />
Pittsburgh<br />
Amy Park<br />
Obstetrics-Gynecology<br />
Univ Health Ctr Of Pittsburgh<br />
Pittsburgh<br />
Andrew Reznick<br />
Internal Medicine<br />
Univ Health Ctr Of Pittsburgh<br />
Pittsburgh<br />
Jesse Selber<br />
Plastic Surgery<br />
Hosp Of The Univ Of PA<br />
Philadelphia<br />
Chandler Shyu<br />
Medicine-Preliminary<br />
Univ Health Ctr Of Pittsburgh<br />
Pittsburgh<br />
Rhode Island<br />
Christina Baik<br />
Internal Medicine<br />
Brown U Int Med Res<br />
Providence<br />
Daisy Bassen<br />
Psychiatry<br />
Brown Univ Psych Res<br />
Providence<br />
Catherine Malone<br />
Medicine-Primary<br />
Rhode Island Hosp/Brown U<br />
Providence<br />
Cathryn Mcnamara<br />
Internal Medicine<br />
Brown U Int Med Res<br />
Providence<br />
Texas<br />
Ian Bristol<br />
Radiation-Oncology<br />
U Texas M D Anderson<br />
Houston<br />
Utah<br />
Jasmine Low<br />
Pediatrics<br />
U Utah Affil Hospitals<br />
Salt Lake City<br />
Anne Thomas<br />
Internal Medicine<br />
U Utah Affil Hospitals<br />
Salt Lake City<br />
Vermont<br />
Todd Whitman<br />
Medicine-Primary<br />
UVM/Fletcher Allen<br />
Burlington<br />
Virginia<br />
Jennifer Fulton<br />
Internal Medicine<br />
<strong>University</strong> Of Virginia<br />
Charlottesvile<br />
Nikolaus Mcfarland<br />
Medicine-Preliminary<br />
<strong>University</strong> Of Virginia<br />
Charlottesvile<br />
Nikolaus Mcfarland<br />
Neurology<br />
<strong>University</strong> Of Virginia<br />
Charlottesvile<br />
Michelle Rindos<br />
Obstetrics-Gynecology<br />
<strong>University</strong> Of Virginia<br />
Charlottesvile<br />
Jonathan Swanson<br />
Pediatrics<br />
<strong>University</strong> Of Virginia<br />
Charlottesvile<br />
Rebecca Webster<br />
Psychiatry<br />
Naval Med Ctr<br />
Portsmouth<br />
Washington, D.C.<br />
Suyoung Chang<br />
Internal Medicine<br />
Walter Reed Army Med Ctr<br />
Washington, D.C.<br />
Nia Robinson<br />
Obstetrics-Gynecology<br />
Walter Reed Army Med Ctr<br />
Washington, D.C.<br />
Ways to Give<br />
10% annuity<br />
• an annuity gift returns income<br />
to the donor for life<br />
• the <strong>University</strong> has one gift<br />
arrangement that currently<br />
guarantees, dependent on age,<br />
as high as a 10% rate!<br />
To learn more about gifts that<br />
provide the donor with income,<br />
please contact:<br />
Jack Kreckel<br />
Sr. Associate Vice President<br />
Office <strong>of</strong> Trusts and Estates<br />
590 Mt. Hope Avenue<br />
<strong>Rochester</strong>, NY 14620<br />
800–635–4672 or 585–273–5904<br />
email:<br />
kreckel@alumni.rochester.edu<br />
Join other alumni in supporting<br />
the School <strong>of</strong> Medicine & Dentistry!<br />
Washington<br />
Megan Stormo<br />
Family Practice<br />
Central WA Family Med<br />
Yakima<br />
Wisconsin<br />
Joseph Frieben<br />
Psychiatry<br />
U Wisconsin Hosp/Clinics<br />
Madison<br />
Michelle Frieben<br />
Psychiatry<br />
U Wisconsin Hosp/Clinics<br />
Madison<br />
Jennifer Weiss<br />
Internal Medicine<br />
U Wisconsin Hosp/Clinics<br />
Madison<br />
36<br />
ROCHESTER MEDICINE
alumni news<br />
The man who kept the Olympics fair<br />
Before the first Triple Lutz, before any bobsleds<br />
shot down the mountain, Don Catlin, M.D. (M ’65),<br />
was putting Olympic athletes to the test.<br />
Catlin is director <strong>of</strong> the UCLA Olympic<br />
Analytical<br />
Laboratory, the only<br />
anti-doping testing<br />
site in the United<br />
States accredited<br />
by the International<br />
Olympic Committee<br />
Don Catlin, M.D. (IOC). What that<br />
means is simple:<br />
Catlin was a busy man during the Salt Lake<br />
City Olympic Games in February.<br />
“It’s a lot <strong>of</strong> work,” says Catlin, who put<br />
in a few 20-hour days in the beginning <strong>of</strong> his<br />
Olympic quest. The tests are much more<br />
complicated than the ones done for workplace<br />
drug testing, with some samples requiring as<br />
many as 30 different tests. A single assay may<br />
require screening for 50 different steroids. The<br />
IOC bans more than 300 substances.<br />
Catlin and his colleagues began<br />
preparing for their Olympics by stocking up on<br />
testing supplies at their lab, located — appropriately<br />
enough — <strong>of</strong>f Olympic Boulevard in<br />
West Los Angeles. Then they traveled to Salt<br />
Lake City in September and essentially built a<br />
temporary, multimillion-dollar lab next to the<br />
Olympic Village. Forty lab members had to test<br />
about 1,500 samples around the clock for<br />
evidence <strong>of</strong> doping.<br />
The result was “the largest number <strong>of</strong><br />
positives ever for a Winter Games, by far,” says<br />
Catlin, who is also an associate pr<strong>of</strong>essor <strong>of</strong><br />
molecular and medical pharmacology at UCLA.<br />
In fact, the lab’s advanced testing was<br />
able to detect a new drug called darbepoetin,<br />
which led to two athletes being stripped <strong>of</strong> their<br />
gold medals.<br />
The Olympic Analytical Laboratory<br />
opened in 1984 for the <strong>Summer</strong> Olympic Games<br />
in Los Angeles. It has been open ever since,<br />
attracting clients such as the NFL, the NCAA, the<br />
United States Olympic Committee and the<br />
The October 2001 Neurosurgery Department Dinner, with the Frank P. Smith Lecture.<br />
Department <strong>of</strong> Defense.<br />
Catlin has now worked at three Olympic<br />
Games — the key word being “worked.” At the<br />
Salt Lake City Games, he says he didn’t have<br />
time to attend any events beyond the opening<br />
and closing ceremonies. His priority is getting<br />
the job done right, even as he works on a larger<br />
mission: to get drugs out <strong>of</strong> sport.<br />
He says he takes no joy in grinding out<br />
positives. “I view every positive as a failure <strong>of</strong><br />
the system,” he says.<br />
Catlin finally made it home weeks after<br />
the Olympic flame was extinguished,<br />
long after the athletes had packed up and left.<br />
Winning races takes a lot <strong>of</strong> hard work, and<br />
so does making sure the winners won fairly.<br />
He’s got the future <strong>of</strong> pediatric<br />
education in his hands<br />
After a nationwide search, Richard Behrman, M.D.<br />
(M ’60), has been chosen to become the executive<br />
chair <strong>of</strong> the Pediatric Education Steering<br />
Committee <strong>of</strong> the Federation <strong>of</strong> Pediatric<br />
Organizations (FOPO).<br />
Many exceptional candidates threw<br />
their hat into the ring, but the search<br />
committee recommended Behrman, and the<br />
seven member organizations <strong>of</strong> FOPO voted<br />
unanimously to accept the recommendation.<br />
Behrman will help carry out the recommendations<br />
<strong>of</strong> the Future <strong>of</strong> Pediatric<br />
Education II (FOPE II) Task Force, which spent<br />
three years studying medical education in the<br />
21st century and<br />
devising ideas for<br />
its future.<br />
Behrman is<br />
senior vice president<br />
<strong>of</strong> the Lucile<br />
Richard<br />
Behrman, M.D.<br />
Packard Foundation<br />
for Children’s<br />
Health and clinical<br />
pr<strong>of</strong>essor <strong>of</strong> pediatrics<br />
at Stanford <strong>University</strong> and the <strong>University</strong><br />
<strong>of</strong> California, San Francisco.<br />
Previously, he was chair <strong>of</strong> the<br />
Departments <strong>of</strong> Pediatrics at Columbia<br />
<strong>University</strong> and Case Western Reserve <strong>University</strong>,<br />
where he also served as dean and vice president<br />
for medical affairs. Behrman is editor-in-chief<br />
<strong>of</strong> Nelson Textbook <strong>of</strong> Pediatrics and the<br />
journal The Future <strong>of</strong> Children. He has<br />
published extensively in critically reviewed<br />
scientific journals and is a member <strong>of</strong> the<br />
Institute <strong>of</strong> Medicine and numerous pr<strong>of</strong>essional<br />
pediatric organizations.<br />
Behrman describes himself as a<br />
“ builder,” which will serve him well as he<br />
works to fashion a foundation for the future<br />
<strong>of</strong> pediatric education in this country.<br />
SPRING / SUMMER <strong>2002</strong> 37
alumni news<br />
Campbell heads the department,<br />
wins the award<br />
Kevin P. Campbell (Ph.D. ’79) was named<br />
interim head <strong>of</strong> the <strong>University</strong> <strong>of</strong> Iowa<br />
Department <strong>of</strong> Physiology and Biophysics in<br />
February. Campbell,<br />
the Roy J. Carver<br />
Chair <strong>of</strong> Physiology<br />
and Biophysics and<br />
Howard Hughes<br />
<strong>Medical</strong> Institute<br />
Kevin P.<br />
Campbell, Ph.D.<br />
Investigator, is<br />
internationally<br />
renowned for his<br />
neuromuscular<br />
disease research. His work has led to the<br />
identification <strong>of</strong> the molecular and genetic<br />
basis <strong>of</strong> several forms <strong>of</strong> muscular dystrophy<br />
and has provided a clearer understanding <strong>of</strong><br />
the muscular dystrophy disease processes.<br />
“I am extremely pleased that one <strong>of</strong> our<br />
brightest stars has agreed to accept an appointment<br />
as interim head <strong>of</strong> the Department <strong>of</strong><br />
Physiology and Biophysics,” said Robert P. Kelch,<br />
M.D., dean <strong>of</strong> the <strong>University</strong> <strong>of</strong> Iowa College <strong>of</strong><br />
Medicine and vice president for statewide health<br />
Timothy Aiken, M.D. (’98), and<br />
his guest Julie Jacobson enjoy<br />
the D.C. alumni event at B. Smith’s<br />
Restaurant in November.<br />
The URMC Golf Classic brought Fuzzy Zoeller to <strong>Rochester</strong> in September, but the<br />
weather had other plans. Moments after this picture was taken, rain poured down.<br />
The tournament did go on— three weeks later, under friendlier skies.<br />
services. “Dr. Campbell’s work has played a major<br />
part in bringing the department to national and<br />
international prominence.”<br />
Last September, Campbell received the<br />
Muscular Dystrophy Association’s S. Mouchly<br />
Small Scientific Achievement Award. The award,<br />
in honor <strong>of</strong> the late S. Mouchly Small, M.D.,<br />
is presented annually to an MDA-funded<br />
researcher who has made significant contributions<br />
in the field <strong>of</strong> muscular dystrophy research.<br />
Campbell received his doctoral degree in<br />
biophysics from <strong>Rochester</strong> and in 1999 was<br />
elected to the prestigious Institute <strong>of</strong> Medicine <strong>of</strong><br />
the National Academy <strong>of</strong> Sciences.<br />
From surgeon to CEO: Coughlin, Jr.,<br />
directs microbial-detection company<br />
Thomas R. Coughlin, Jr., M.D. (’ 75), has been<br />
named CEO and director <strong>of</strong> Centrex, Inc.,<br />
a development-stage company based in<br />
Oklahoma. Coughlin was formerly the medical<br />
advisor for the company, which<br />
owns the exclusive U.S. license to develop,<br />
manufacture and market a system for detecting<br />
microbial contamination from E. coli bacteria<br />
in food, air and water.<br />
The detection system, currently in<br />
development, is designed to be tailored to detect<br />
a variety <strong>of</strong> bacterial or viral organisms in real<br />
time. Centrex is considering all the agents<br />
on the Defense Intelligence Agency’s biological<br />
warfare threat list as potential organisms for<br />
the device to be able to detect.<br />
Before joining the company in 1999,<br />
Coughlin was working as a cardiovascular and<br />
transplant surgeon. At the <strong>University</strong> <strong>of</strong><br />
Maryland from 1986 to 1990, he started the<br />
heart transplant program and performed the<br />
first successful heart transplant there. He also<br />
served as medical director <strong>of</strong> the Maryland<br />
Organ Procurement <strong>Center</strong>. From 1992 to 1995,<br />
he was medical director <strong>of</strong> Cardiovascular<br />
Surgical Services at Alexandria Hospital in<br />
Alexandria, Va. From<br />
1991 to 1995, he was<br />
assistant clinical<br />
pr<strong>of</strong>essor <strong>of</strong> thoracic<br />
and cardiovascular<br />
surgery at George<br />
Washington<br />
<strong>University</strong> <strong>Medical</strong><br />
<strong>Center</strong> in<br />
Washington, D.C.<br />
Thomas R.<br />
Coughlin, Jr., M.D.<br />
From 1995 to 1999, Coughlin practiced<br />
cardiovascular surgery in Tulsa, Okla., and was<br />
assistant clinical pr<strong>of</strong>essor at the <strong>University</strong> <strong>of</strong><br />
Oklahoma <strong>Medical</strong> School.<br />
38<br />
ROCHESTER MEDICINE
alumni news<br />
U. <strong>of</strong> Deans, continued<br />
Our last issue <strong>of</strong> <strong>Rochester</strong> Medicine focused on some <strong>of</strong> the alumni<br />
who are or were deans <strong>of</strong> medical schools across the country. Of course,<br />
we didn’t have room to include everyone (which speaks volumes about<br />
the accomplishments <strong>of</strong> <strong>Rochester</strong> alumni). So from time to time,<br />
we thought we’d update you on alumni deans, past and present.<br />
Solomon Sidney Solomon, M.D. (M ’62), was the associate dean<br />
for research at the College <strong>of</strong> Medicine, <strong>University</strong> <strong>of</strong> Tennessee from 1983<br />
to 1998. Currently he’s pr<strong>of</strong>essor <strong>of</strong> medicine and pharmacology at the<br />
<strong>University</strong> <strong>of</strong> Tennessee; chair <strong>of</strong> endocrinology and metabolism section,<br />
<strong>Medical</strong> Service, Veterans Affairs <strong>Medical</strong> <strong>Center</strong> in Memphis; and<br />
attending physician (medicine), City <strong>of</strong> Memphis Hospitals and <strong>University</strong><br />
<strong>of</strong> Tennessee Hospital.<br />
Solomon says he opted to stay in academics, where he could<br />
pursue research (particularly on diabetes). The decision left him a<br />
full plate: Rounding seven months <strong>of</strong> the year, performing his duties<br />
as associate dean, and maintaining two research grants from the NIH<br />
and Veterans Affairs <strong>Medical</strong> <strong>Center</strong>.<br />
But he’s not one to slow down. Solomon has been a reviewer<br />
for dozens <strong>of</strong> publications and committees, including Science, American<br />
Journal <strong>of</strong> <strong>Medical</strong> Sciences, Cancer Research, and the American<br />
Journal <strong>of</strong> Physiology. While associate dean, he received top honors in<br />
clinical research at the Awards for Excellence in Research, sponsored by<br />
the Health Industry Council and Memphis Health Care News. And he is<br />
a member <strong>of</strong> a dozen associations, including the American Diabetes<br />
Association and the American <strong>Medical</strong> Association (special).<br />
After all, in his listing in Who’s Who in America, Solomon<br />
says his philosophy in life “has always been to get involved … my motto<br />
is, ‘I came to play, not to watch.’ ” It’s no wonder he succeeded as an<br />
associate dean all those years.<br />
As former associate dean for research at the College <strong>of</strong> Medicine,<br />
<strong>University</strong> <strong>of</strong> Tennessee, Solomon Sidney Solomon, M.D., maintained<br />
his research schedule in addition to his administrative duties.<br />
Author Author!<br />
Roger A. Brumback, M.D. (R ’80), recently published Attention, Behavior,<br />
and Learning Problems in Children: Protocols for Diagnosis and<br />
Treatment. This book was written for physicians,<br />
educators, and parents to use in<br />
evaluating children with school problems.<br />
Dr. Brumbeck was a member <strong>of</strong> the<br />
house staff in the Department <strong>of</strong> Pathology at<br />
the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong>. He was a resident<br />
in anatomic pathology and neuropathology<br />
from July 1, 1982 to May 30, 1986. Since<br />
January 1, 2001, he has held the position <strong>of</strong><br />
pr<strong>of</strong>essor and chairman <strong>of</strong> the Department<br />
<strong>of</strong> Pathology at the Creighton <strong>University</strong> School <strong>of</strong> Medicine, St. Joseph<br />
Hospital, Omaha, Neb.<br />
Robert C. Smith, M.D. (Fellow ’80, Faculty ’84), has written Patient-<br />
<strong>Center</strong>ed Interviewing: An Evidence-Based Method (Lippincott Williams<br />
and Wilkins, 2001). The book describes, orders, and prioritizes the specific<br />
behaviors needed to conduct the entire medical interview — and to<br />
establish the provider-patient relationship. This step-by-step method has<br />
been directly studied in a randomized controlled trial and shown effective.<br />
A specific, evidence-based method allows interviewers to formulate a relevant<br />
biopsychosocial description <strong>of</strong> individual patients in a scientific way.<br />
The book is used as a course text for students, residents, nurses, CME, and<br />
faculty development. The efficiency <strong>of</strong> the interviewing method and its<br />
user-friendliness have been valued.<br />
Smith also produced a teaching videotape by the same title<br />
to accompany the text. It demonstrates the method the book describes<br />
for both patient-centered and doctor-centered interviewing. The tape<br />
is distributed by the<br />
book publisher and<br />
also is available<br />
from Michigan<br />
State <strong>University</strong>,<br />
who produced it.<br />
It has proved<br />
an invaluable<br />
teaching adjunct<br />
for new learners.<br />
SPRING / SUMMER <strong>2002</strong> 39
class notes<br />
Class <strong>of</strong> 1941<br />
Allen Walker, M.D., sends his greetings to<br />
classmates and regrets that he and his wife,<br />
Mary Lee, were unable to attend Reunion<br />
2001. He and Mary Lee celebrated their 60th<br />
wedding anniversary this year.<br />
Class <strong>of</strong> 1946<br />
Walter H. Abelman, M.D., is the current<br />
director <strong>of</strong> alumni affairs at Harvard MIT<br />
Division <strong>of</strong> Health Science and Technology.<br />
John H. Kennell, M D. (B ‘44), is a pr<strong>of</strong>essor<br />
<strong>of</strong> pediatrics at Case Western Reserve<br />
<strong>University</strong>’s School <strong>of</strong> Medicine in Cleveland,<br />
OH. He is currently teaching first- and<br />
second-year medical students and is doing<br />
research under an NIH grant.<br />
Class <strong>of</strong> 1951<br />
Norman B. Abell, M.D., volunteers as a<br />
medical counselor and pharmacy assistant<br />
in the health service <strong>of</strong> Penney Retirement<br />
Community in Florida. He facilitates recycling<br />
efforts in the community and continues<br />
research on post-polio syndrome.<br />
Bernard B. Brody, M.D., is presently a trustee<br />
<strong>of</strong> The Freedom Forum and travels around the<br />
world in that capacity.<br />
George J. D’Angelo, M.D., received the John<br />
L. Robison Humanitarian Award in 2001 from<br />
the Boys and Girls Club in Erie, PA. Presently,<br />
D’Angelo is serving as trustee for the<br />
Mercyhurst College and the Boys and Girls<br />
Club in Erie, PA.<br />
Richard Koch, M.D., assumed the position <strong>of</strong><br />
principal investigator <strong>of</strong> the Material PKU<br />
Collaborative International Study for the<br />
National Institute <strong>of</strong> Child Health at the<br />
<strong>University</strong> <strong>of</strong> Southern California.<br />
Class <strong>of</strong> 1953<br />
Edward J. Zebrowski, M.D., was elected<br />
national commander <strong>of</strong> the Combat<br />
Infantrymen’s Association in June 2001.<br />
Zebrowski also founded the New England<br />
Regiment <strong>of</strong> the Combat Infantrymen’s<br />
Association, which meets monthly at Fort<br />
Devens, MA. He has written three books since<br />
his retirement: My Brother, Hail & Farewell,<br />
which is about his exploits during WWII in<br />
General Patton’s Third Army in Europe;<br />
Patient Beware — Doctor Take Care, about<br />
medical mistakes, and Health, Healing, and<br />
Healers in Conventional and Alternative<br />
Medicine, which has a list <strong>of</strong> 115 <strong>of</strong> the most<br />
commonly used medicinal plants with all their<br />
beneficial and adverse effects.<br />
Class <strong>of</strong> 1954<br />
A word from the Class <strong>of</strong> ‘54: We’re rescheduling<br />
our planned Seattle/Alaska trip for<br />
mid-August and hope to have at least the<br />
65 who had originally intended to come last<br />
September. There will be an alumni reception<br />
for all U <strong>of</strong> R med school graduates in the<br />
Seattle-West Coast area, as well as some<br />
sightseeing, possibly a Seattle Mariners ball<br />
game, and a class dinner before we board<br />
the newest <strong>of</strong> the Princess Line ships for a<br />
seven-day cruise from Vancouver to Seward.<br />
This is a follow-up <strong>of</strong> our week in San Antonio<br />
a few years ago.<br />
The <strong>Rochester</strong>-area Class <strong>of</strong> ‘54 has<br />
taken on the somewhat daunting task <strong>of</strong><br />
saving large amounts <strong>of</strong> money for the Alumni<br />
Office. We have made ourselves responsible<br />
for stuffing all the envelopes that are sent<br />
with mailings throughout the year. It’s been<br />
fun. We talk about anything and everything,<br />
drink more juice than c<strong>of</strong>fee and nibble<br />
delicately on a cookie or two. We’ve had<br />
some wonderful help from members <strong>of</strong> other<br />
classes as well, and we can always use more<br />
volunteers from any class (call Karen Gaffney<br />
at 585–273–5947).<br />
Dave Kluge, as conference faculty<br />
coordinator, put together the 8th Annual EMS<br />
Conference in April, an outstanding two-day<br />
event. These are attended each year by 450 to<br />
550 ambulance personnel, EMTs, police,<br />
firemen, and others with public safety interests.<br />
They feature a nationally known keynote<br />
speaker, individual workshops on topics such<br />
as rescue (including a live demonstration with<br />
heavy equipment); chemical and biologic<br />
hazards; EMS cases and the law; fast-food<br />
restaurant fires; incident planning and control;<br />
domestic violence; and many others.<br />
The faculty included Chloe Alexson.<br />
Class <strong>of</strong> 1956<br />
Joseph Amdur, M.D., is looking forward to<br />
hearing from any classmates passing through<br />
north Florida.<br />
Vacationing and native Floridians <strong>of</strong> the Class <strong>of</strong> '54 held a two-day mini-reunion to eat and<br />
reminisce. Seated, from left — Joae (Graham) Brooks, M.D.(’54), and Bernie Brooks (who hosted<br />
in Naples); Irwin Frank, M.D. (’54) and Marilyn Frank. Standing, from left — Mary Flatley,<br />
Joseph Flatley, M.D. (’54), Beverly Kluge, Dave Kluge, M.D. (’54), and Jean Brodell and Harold<br />
Brodell, M.D. (’54), (who hosted in Boca Raton).<br />
Lee R. Chutkow, M.D. (R ‘56), moved from<br />
Louisville, KY, to Tucson, AZ. Chutkow intends<br />
to work part time and meet new friends.<br />
Charles G. Cochrane, M.D. (BA ‘51), is a<br />
pr<strong>of</strong>essor in the Department <strong>of</strong> Immunology for<br />
the Scripps Research Institute in La Jolla, CA.<br />
40<br />
ROCHESTER MEDICINE
class notes<br />
HIGHLIGHTS OF THE WEEKEND<br />
THIS YEAR, REUNION CELEBRATES<br />
“Trailblazing:Frontiers in Medicine”<br />
William A. Kern, Jr., M.D., was a Class Agent<br />
for Reunion <strong>2002</strong> along with his wife, Kathryn<br />
Kern, M.D. (M ‘56).<br />
William C. Luft, M.D. (BA ‘52), spends time<br />
volunteering with the Red Cross<br />
(Bloodmobiles) and Habitat for Humanity. He<br />
enjoys traveling to New York City for Broadway<br />
musicals and takes a cruise each year.<br />
Sanford C. Spraragen, M.D. (MAS ‘52),<br />
is retired and spends his time serving as<br />
a docent at the Roger William Park Zoo in<br />
Providence, RI. Spraragen enjoys playing<br />
the trumpet, surfing the Net, reading good<br />
books and playing golf.<br />
Class <strong>of</strong> 1958<br />
Samuel P. Got<strong>of</strong>f, M.D., recently retired, after<br />
36 years in academic medicine. In his career<br />
as a pediatrician, he was chair <strong>of</strong> the<br />
Department <strong>of</strong> Pediatrics at Michael Reese<br />
Hospital & <strong>Medical</strong> <strong>Center</strong>, and a pr<strong>of</strong>essor<br />
at the <strong>University</strong> <strong>of</strong> Chicago, Rush <strong>Medical</strong><br />
College and Rush Children’s Hospital. He<br />
received several awards for his work and<br />
teaching. Got<strong>of</strong>f’s research focused primarily<br />
on the epidemiology, immunity and prevention<br />
<strong>of</strong> Group B streptococcal infections in<br />
newborns.<br />
eunions.html<br />
The dates have been set, and the schedule is falling<br />
into place for Fall & Reunion Weekend <strong>2002</strong>.<br />
Mark your calendars to join your classmates for<br />
a fun-filled weekend.<br />
For more information, contact the<br />
Office <strong>of</strong> <strong>Medical</strong> Alumni Relations at 800-333-4428,<br />
or visit the reunion website<br />
http://www.urmc.rochester.edu/smd/alumni/reunions.html<br />
●<br />
THURSDAY | OCTOBER 3 | <strong>2002</strong><br />
The 31st Annual George Hoyt<br />
Whipple Society Dinner at the Oak Hill<br />
Country Club.<br />
FRIDAY | OCTOBER 4 | <strong>2002</strong><br />
● A number <strong>of</strong> exciting lectures<br />
● Tours <strong>of</strong> the School <strong>of</strong> Medicine<br />
and Dentistry, Strong Memorial<br />
Hospital, and the new emergency center<br />
● A night at the <strong>Rochester</strong> Museum and<br />
Science <strong>Center</strong> featuring a family<br />
barbecue, fun events for the kids, and<br />
dancing for everyone!<br />
SATURDAY | OCTOBER 5 | <strong>2002</strong><br />
● An Erie Canal Boat tour on the<br />
Colonial Belle<br />
● Reunion Class Dinners<br />
Class <strong>of</strong> 1960<br />
William A. Peck, M.D., recently announced<br />
plans to conclude his deanship at the<br />
Washington <strong>University</strong> School <strong>of</strong> Medicine in<br />
June 2003. He will continue on as a pr<strong>of</strong>essor<br />
<strong>of</strong> medicine at the school after that time.<br />
Class <strong>of</strong> 1961<br />
Robert E. Burke, M.D., assumed a position as<br />
lab chief for the National Institutes <strong>of</strong> Health in<br />
Bethesda, MD. NIH sponsored a symposium in<br />
Burke’s honor for his research career.<br />
Robert P. Gibbons, M.D., received the<br />
Certificate <strong>of</strong> Achievement Award in 2001 for<br />
lifetime career achievements in urology from<br />
the American Urological Association.<br />
Henry T. Smith, M.D., F.A.C.P., was recently<br />
awarded the Laureate Award from the<br />
Minnesota Chapter <strong>of</strong> the ACP-American<br />
Society <strong>of</strong> Internal Medicine. The award honors<br />
a “commitment to excellence in medical care,<br />
education, research and service.”<br />
Class <strong>of</strong> 1964<br />
Charles A. Lankau, M.D., is the chief <strong>of</strong> the<br />
Department <strong>of</strong> Pediatric Surgery at Miami<br />
Children’s Hospital. He and his wife celebrated<br />
42 years <strong>of</strong> marriage in December<br />
and have five grandchildren (so far!).<br />
Class <strong>of</strong> 1966<br />
Julian M. Earls, Ph.D.<br />
(MAS ‘66), was<br />
selected to carry the<br />
Olympic Torch in the<br />
Cleveland section <strong>of</strong><br />
the Olympic Relay.<br />
An avid runner,<br />
Earls has completed<br />
over 25 marathons. He<br />
is the deputy director<br />
<strong>of</strong> operations at<br />
NASA’s Glenn<br />
Research <strong>Center</strong>,<br />
Cleveland, OH.<br />
Wayne Myers, M.D.,<br />
is semi-retired after<br />
directing the federal<br />
Office <strong>of</strong> Rural Health<br />
Policy. He is now<br />
raising heritage<br />
livestock and doing<br />
occasional consulting.<br />
Class <strong>of</strong> 1968<br />
Joseph S. Bujak, M.D., recently co-authored<br />
the book Leading Transformational Change:<br />
The Physician-Executive Partnership.<br />
Class <strong>of</strong> 1969<br />
Russell V. Luepker, M.S., M.D., was appointed<br />
the Mayo Pr<strong>of</strong>essor <strong>of</strong> Public Health in July<br />
2001. He remains pr<strong>of</strong>essor and head <strong>of</strong> the<br />
Division <strong>of</strong> Epidemiology for the School <strong>of</strong><br />
Public Health at the <strong>University</strong> <strong>of</strong> Minnesota.<br />
Class <strong>of</strong> 1971<br />
Richard Billingham, M.D., has been appointed<br />
president-elect <strong>of</strong> the American Society <strong>of</strong><br />
Colon and Rectal Surgeons and was a<br />
member <strong>of</strong> the American Board <strong>of</strong> Colon and<br />
Rectal Surgery. He lives in Seattle, WA, where<br />
he enjoys running, biking, rollerblading, skiing<br />
and hiking.<br />
Richard O. Buck, M.D., and Virginia Buck,<br />
M.D., both currently work for the Buck Allergy<br />
and Asthma Clinic in Eugene, OR. Richard<br />
is on the State <strong>of</strong> Oregon Commission on<br />
Asthma and served as assistant clinical<br />
pr<strong>of</strong>essor at Oregon Health Science<br />
<strong>University</strong>. He is an active member <strong>of</strong> the<br />
Eugene Concert Choir. Virginia has been<br />
SPRING / SUMMER <strong>2002</strong> 41
class notes<br />
Warren Zapol, M.D.<br />
(’66), and Dean<br />
Hundert talk at<br />
the D.C. reception<br />
at B. Smith’s<br />
Restaurant.<br />
<strong>of</strong> multi-organ transplantation at Cedars-Sinai<br />
<strong>Medical</strong> <strong>Center</strong> and pr<strong>of</strong>essor <strong>of</strong> medicine,<br />
UCLA School <strong>of</strong> Medicine. Last year he<br />
stepped down as chair <strong>of</strong> the Board <strong>of</strong><br />
Directors <strong>of</strong> the American Liver Foundation<br />
after six years <strong>of</strong> service. He was elected to<br />
the Council <strong>of</strong> the American Association for<br />
the Study <strong>of</strong> Liver Diseases this year and will<br />
begin serving as president in 2006.<br />
president <strong>of</strong> the Oregon Society <strong>of</strong> Allergy,<br />
Asthma & Immunology and spends time with<br />
the Eugene Recorder Ensemble.<br />
John Fitchen, M.D., has been chair <strong>of</strong> several<br />
committees, including the American Cancer<br />
Society, Oregon Chapter and Oregon Health<br />
Science Foundation. He has received a Top<br />
Ten Teacher’s Award five years in a row from<br />
OHSU. He is currently the president and CEO<br />
for Catalyst Biomedical.<br />
John Grossman III, M.D. (B ‘67, R ‘72),<br />
is currently working as senior associate vice<br />
president at George Washington <strong>University</strong>,<br />
where he has received the School <strong>of</strong><br />
Medicine and Health Sciences Golden Apple<br />
Award and the School <strong>of</strong> Public Health and<br />
Health Services Excellence in Teaching<br />
Award. He also received the Council on<br />
Resident Education in Obstetrics and<br />
Gynecology National Faculty Award in<br />
Resident Education. He recently concluded<br />
his tenure as dean <strong>of</strong> medicine at George<br />
Washington <strong>University</strong>.<br />
Jerrold Hokanson, M.D., currently lives in<br />
Martinez, CA, with his wife, Carolyn. He is<br />
staff pediatrician and associate chief <strong>of</strong><br />
pediatrics at Kaiser Permanente.<br />
Robert Lewis, M.D., is the head <strong>of</strong><br />
immunology and vice president for Aventis<br />
Pharmaceuticals, Inc. in Bridewater, NJ. He<br />
is a member <strong>of</strong> the American Association <strong>of</strong><br />
Immunologists and the American Society <strong>of</strong><br />
Molecular Biology and Biochemistry.<br />
Joseph B. Martin, M.D., Ph.D. (Ph.D. ‘71),<br />
dean <strong>of</strong> the Harvard <strong>University</strong> Faculty <strong>of</strong><br />
Medicine, has been appointed to the board <strong>of</strong><br />
directors at Baxter International, Inc., a global<br />
medical products and services company.<br />
Thomas McMeekin, M.D. (R ‘76), is currently<br />
the president <strong>of</strong> Genesee Valley Laser Centre.<br />
Ira Shoulson, M.D. (M ‘71, R ‘73, R ‘77),<br />
is president <strong>of</strong> the American Society <strong>of</strong><br />
Experimental Neurotherapeutics and is on<br />
the Editorial Board <strong>of</strong> Neurology Today. He<br />
is currently on the faculty at the <strong>University</strong> <strong>of</strong><br />
<strong>Rochester</strong> School <strong>of</strong> Medicine and Dentistry.<br />
William Taylor, M.D., is a pediatrician for<br />
Sandhills Pediatrics in Columbia, SC. He<br />
received the “Doctor <strong>of</strong> the Year” award for<br />
Columbia in 2000. He serves as chairman <strong>of</strong><br />
the Easter Seals Committee and State School<br />
Health Committee.<br />
Class <strong>of</strong> 1973<br />
Sarah C. Oxnard, M.D., and Thomas Oxnard,<br />
M.D. (M ‘71), are pleased that their son,<br />
Jeff, is a first-year medical student at the<br />
<strong>University</strong> <strong>of</strong> Chicago. As Sarah puts it, it’s<br />
“nice to have one follow in our footsteps.”<br />
Class <strong>of</strong> 1974<br />
Karl J. Marchenese, M.D. (R ‘79), sponsors<br />
a medical clinic with three full-time staff to<br />
provide services to disadvantaged children<br />
on the island <strong>of</strong> Negros in the southern<br />
Philippines. He spent several weeks there<br />
in September and October bringing medical<br />
care to rural villages.<br />
John M. Vierling, M.D. (R ‘74), is currently<br />
director <strong>of</strong> hepatology and medical director<br />
Class <strong>of</strong> 1975<br />
Dean X. Parmelee, M.D., was named associate<br />
dean for academic affairs at Wright<br />
State <strong>University</strong> School <strong>of</strong> Medicine in<br />
Dayton, OH, in October 2001. He served for<br />
15 years at Virginia Commonwealth <strong>University</strong><br />
School <strong>of</strong> Medicine as head <strong>of</strong> child and<br />
adolescent psychiatry and for many <strong>of</strong> those<br />
years directed the second-year medical<br />
school curriculum.<br />
Class <strong>of</strong> 1976<br />
Sharon Allen, M.D., is currently an associate<br />
pr<strong>of</strong>essor at the <strong>University</strong> <strong>of</strong> Minnesota<br />
<strong>Medical</strong> School. She has published many<br />
peer-reviewed journal articles. She and her<br />
husband, James, have three children (William,<br />
Julie and Katie).<br />
John Dier, M.D., is a member <strong>of</strong> the Board<br />
<strong>of</strong> Directors for the Glens Falls (NY) Hospital<br />
Board <strong>of</strong> Directors. He is a volunteer physician<br />
for the Rocky Mountain Biological<br />
Laboratory.<br />
William Feaster, M.D., is senior vice president,<br />
chief medical <strong>of</strong>ficer and chief<br />
information <strong>of</strong>ficer for Community <strong>Medical</strong><br />
<strong>Center</strong>s in Fresno, CA. He is a Certified<br />
Physician Executive — American College <strong>of</strong><br />
Physician Executives.<br />
Robert R. Johnson, M.D., is on the Board<br />
<strong>of</strong> Directors <strong>of</strong> the Tucson <strong>Medical</strong> <strong>Center</strong><br />
Foundation. He is currently an internist for<br />
Arizona Community Physicians.<br />
Beverly Love, M.D., is a member <strong>of</strong> the U.S.<br />
Chamber <strong>of</strong> Commerce, the AMA and the<br />
Fathers Active In Children’s Education, and<br />
is president <strong>of</strong> Capital City <strong>Medical</strong> Society.<br />
42<br />
ROCHESTER MEDICINE
class notes<br />
Melvin S. Rapelyea, M.D., works in the<br />
Department <strong>of</strong> Diagnostic Imaging for Howard<br />
County General Hospital in Columbia, MD.<br />
He spends time working on boards for<br />
non-pr<strong>of</strong>its and coordinates the Chestertown<br />
Jazz Festival.<br />
Neil Swanson, M.D., assumed the vice president-elect<br />
post at the American Academy<br />
<strong>of</strong> Dermatology in March 2001. He is on the<br />
medical staff at a number <strong>of</strong> Portland, OR,<br />
area hospitals and is pr<strong>of</strong>essor and chair <strong>of</strong><br />
dermatology and pr<strong>of</strong>essor <strong>of</strong> otolaryngologyhead<br />
and neck surgery at Oregon Health<br />
Sciences <strong>University</strong>. In addition, he is a<br />
member <strong>of</strong> the American Academy’s Board<br />
<strong>of</strong> Directors and is the chair <strong>of</strong> the Health<br />
Policy Council.<br />
Herman Szymanski, M.D., received the<br />
Exemplary Psychiatrist Award from the<br />
National Alliance for the Mentally Ill, which<br />
represents the families <strong>of</strong> the mentally ill.<br />
He is past president <strong>of</strong> the Western New York<br />
Psychiatric Society. Szymanski was made an<br />
honorary member <strong>of</strong> the 11th Armored Cavalry<br />
Regiment, a unit that served in Vietnam,<br />
to recognize his work treating many Vietnam<br />
veterans with post-traumatic stress.<br />
Donato Viggiano, M.D., has served on the<br />
Board <strong>of</strong> Directors <strong>of</strong> the <strong>Medical</strong> <strong>Center</strong> <strong>of</strong><br />
Port St. Lucie and has worked to regulate<br />
<strong>of</strong>fice-based surgery in Florida.<br />
Edward B. Yellig, M.D. (R ‘76), became<br />
medical director <strong>of</strong> Hospice <strong>of</strong> Wake County<br />
in North Carolina in August 2001.<br />
Class <strong>of</strong> 1979<br />
Kenneth A. Bock, M.D., has been involved<br />
in the field <strong>of</strong> integrative medicine for the<br />
greater part <strong>of</strong> 20 years.<br />
Robert J. Brommage, Ph.D. (MAS ‘76), has<br />
joined the Department <strong>of</strong> Endocrinology at<br />
Lexicon Genetics in The Woodlands, TX. He is<br />
a senior scientist specializing in osteoporosis<br />
research.<br />
Arthur Eisenberg, M.D. (FLW ‘79), is currently<br />
with St. Luke’s Roosevelt Hospital <strong>Center</strong> in<br />
New York City as the administrator for the<br />
Institute for Health Sciences and head <strong>of</strong> the<br />
Office <strong>of</strong> Grants and Research Administration.<br />
His wife, Deborah, obtained her master’s in<br />
social work from Columbia <strong>University</strong> and<br />
now works in a school system in Westchester<br />
County. His son, Michael, is a sophomore at<br />
New Rochelle High School. Eisenberg would<br />
love to hear from fellow alumni. His e-mail<br />
address is arthure @ ix.netcom.com<br />
Deborah C. German, M.D. (R ‘79), was recently<br />
named an honoree for the Academy for<br />
Women <strong>of</strong> Achievement. The Academy was<br />
founded in 1992 by the YWCA <strong>of</strong> Nashville<br />
and Middle Tennessee to honor women who,<br />
through excellence and leadership in their<br />
chosen fields, serve as role models for young<br />
women and girls. German is the senior associate<br />
dean <strong>of</strong> medical education at the<br />
Vanderbilt <strong>University</strong> School <strong>of</strong> Medicine.<br />
Carl A. Patow, M.D., M.P.H., has been<br />
appointed associate dean <strong>of</strong> faculty at<br />
HealthPartners for the <strong>University</strong> <strong>of</strong><br />
Minnesota <strong>Medical</strong> School. The appointment<br />
is recognition <strong>of</strong> the important role<br />
HealthPartners Institute for <strong>Medical</strong><br />
Education plays in the education <strong>of</strong> physicians<br />
in Minnesota. It is also a reflection <strong>of</strong><br />
Patow’s leadership role in building the relationship<br />
between the university and the<br />
medical school, strengthening their undergraduate<br />
and graduate education programs,<br />
and creating an effective infrastructure for<br />
education within HealthPartners.<br />
Class <strong>of</strong> 1980<br />
Marco Alberts, D.M.D., M.P.H. (EDC ‘80, R ‘82),<br />
received his master’s degree in public health<br />
from the <strong>University</strong> <strong>of</strong> South Florida in Tampa<br />
last year, and has assumed a position as<br />
director <strong>of</strong> the Dental/ Oral Surgery Clinic at<br />
Harborview <strong>Medical</strong> <strong>Center</strong> in Seattle, WA.<br />
He was also appointed to the faculty <strong>of</strong><br />
Restorative Dentistry at the <strong>University</strong> <strong>of</strong><br />
Washington, and will be involved with undergraduate<br />
teaching.<br />
Class <strong>of</strong> 1981<br />
Bradford C. Berk, M.D., Ph.D. (M ‘81, PhD ‘81),<br />
is the chair for the Department <strong>of</strong> Medicine,<br />
chief <strong>of</strong> the Cardiology Unit and director for<br />
the <strong>Center</strong> for Cardiovascular Research at<br />
the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong>.<br />
The Retired Surgeons Luncheon in June. From left — John Frazer, M.D. (’39), James DeWeese, M.D.<br />
(M ’49, R ’56), Seymour I. Schwartz, M.D. (R ’57), John Morton, M.D. (R ’54), James T. Adams, M.D.,<br />
Morris J. Shapiro, M.D. (B ’34, MAS ’34).<br />
Martha P. Bond, M.P.H., has been hired as<br />
director <strong>of</strong> grants at Hobart and William Smith<br />
Colleges.<br />
SPRING / SUMMER <strong>2002</strong> 43
class notes<br />
The First Annual Mary Ellen Riegel Lecture<br />
in Primary Care in October. From left —<br />
Leslie Algase, M.D. (’83), Faith Fitzgerald, M.D.,<br />
Stephen Riegel, Paul Fine, M.D. (’61).<br />
Robert H. Fisher, M.D., lives in Wisconsin,<br />
where he is the vice president <strong>of</strong> medical<br />
affairs for Community Memorial Hospital.<br />
He and his wife, Bonnie, have 3 children<br />
(Laura, Jessica and Deborah).<br />
Deborah Geer, M.D., is a certified music practitioner.<br />
She works for Surgical Associates in<br />
Waynesboro, PA, as a general surgeon. After<br />
retiring from the Army after nine years, she<br />
and her husband, Malcolm, did six years <strong>of</strong><br />
solo practice in Ohio and now are part <strong>of</strong> a<br />
small practice. They have been doing shortterm<br />
overseas medical missions and love<br />
every minute <strong>of</strong> it.<br />
Alan Kaell, M.D. (R ‘81), is currently a senior<br />
partner in an eight-person private practice<br />
rheumatology group on Long Island. He is a<br />
clinical pr<strong>of</strong>essor <strong>of</strong> medicine at SUNY Stony<br />
Brook, chief <strong>of</strong> rheumatology at St. Charles<br />
Hospital, and on the Advisory Council for<br />
Osteoporosis, NYS, DOH. He and his wife,<br />
Diana (U <strong>of</strong> R ‘75), celebrated their 27th<br />
anniversary this year. Diana is a clinical<br />
research coordinator. Their children, Laura<br />
(22, graduated from U. <strong>of</strong> Michigan in organizational<br />
management and works in Chicago),<br />
Steven (20, is in applied mathematics and<br />
neurosciences at Brown <strong>University</strong>) and<br />
Matt (16, a high school lacrosse star) are<br />
doing well. Kaell hopes the winter is mild<br />
in <strong>Rochester</strong>!<br />
Stanley D. Musgrave, M.D., lived in several<br />
developing countries since residency (Haiti,<br />
Ethiopia, Uganda, Nepal and India), and<br />
moved back to the UK in 2000, where he<br />
works as a freelance consultant.<br />
David B. Nash, M.D., is the associate dean<br />
at Jefferson <strong>Medical</strong> College <strong>of</strong> Thomas<br />
Jefferson <strong>University</strong> in Philadelphia. He is<br />
internationally recognized for his work in<br />
outcomes management, medical staff development<br />
and quality-<strong>of</strong>-care improvement. His<br />
national activities include appointment to the<br />
JCAHO Advisory Committee on Performance<br />
Measurement and the Foundation <strong>of</strong><br />
Accountability (FACCT) Board. He is a<br />
consultant to organizations in both public and<br />
private sectors. He lives in Lafayette Hill, PA,<br />
with his wife, Esther, twin daughters and son.<br />
Henry Rose, M.D. (R ‘84), is currently a<br />
medical director <strong>of</strong> renal dialysis for Berkshire<br />
Health Systems and received the Berkshire<br />
<strong>Medical</strong> Society Community Clinician <strong>of</strong> the<br />
Year Award in 2000.<br />
Peter G. Szilagyi, M.D. (R ‘84, MS ‘89), is the<br />
director <strong>of</strong> a large outreach program to help<br />
inner-city preschool children receive preventive<br />
and primary care and has received<br />
awards for teaching residents. He is on the<br />
Board <strong>of</strong> Directors for the major Medicaid<br />
managed care physician organization in<br />
<strong>Rochester</strong>. Szilagyi is at the <strong>University</strong> <strong>of</strong><br />
<strong>Rochester</strong> as chief <strong>of</strong> the Division <strong>of</strong> General<br />
Pediatrics, and is an associate pr<strong>of</strong>essor and<br />
the director <strong>of</strong> Pediatric Ambulatory Services.<br />
Leslie Tar, M.D., J.D., M.P.H., is working as<br />
a physician and attorney in Pittsburgh. As a<br />
physician, he works as a medical specialist<br />
in allergy / rheumatology / occupational medicine.<br />
As an attorney, he represents physicians<br />
in health law matters, workers’ compensation<br />
and Social Security disability law issues. He<br />
<strong>of</strong>ten thinks about the time<br />
he spent studying for exams at the U <strong>of</strong> R with<br />
classmates Mark Milner, Stuart Silverman,<br />
and John Wilinsky.<br />
Lois H. Windes, M.D., currently works part<br />
time for Holston <strong>Medical</strong> Group in Tennessee.<br />
Married with four children, Windes is<br />
chairman <strong>of</strong> Holston <strong>Medical</strong> Group’s<br />
Wellness Committee and Program and<br />
teaches parenting classes and health and<br />
wellness.<br />
Class <strong>of</strong> 1982<br />
Ronald P. Cantanese, M.D. (R ‘82), started<br />
a service to help fellow M.D.s eliminate costly<br />
answering-service bills. He practices in<br />
Greenfield, MA.<br />
Class <strong>of</strong> 1984<br />
Stephen McLeod-Bryant, M.D. (B ‘80), became<br />
the medical director <strong>of</strong> the South Carolina<br />
Department <strong>of</strong> Mental Health in August 2001.<br />
He works in Columbia, SC, but continues to<br />
live with his wife, Aleta, and their three<br />
children in Mt. Pleasant, SC, just outside <strong>of</strong><br />
Charleston. He hopes to see his classmates<br />
at their 15th medical reunion in 2004.<br />
Class <strong>of</strong> 1985<br />
Jude Sauer, M.D. (B ‘81), president and<br />
CEO <strong>of</strong> LSI Solutions, was named the Ernst &<br />
Young Upstate New York 2001 Entrepreneur<br />
<strong>of</strong> the Year. The award is based on leadership,<br />
tenacity, innovation and the creation and<br />
maintenance <strong>of</strong> a successful business<br />
environment.<br />
44<br />
ROCHESTER MEDICINE
class notes<br />
Class <strong>of</strong> 1986<br />
Christopher J. Arpey, M.D., is an associate<br />
pr<strong>of</strong>essor <strong>of</strong> dermatology at the <strong>University</strong><br />
<strong>of</strong> Iowa and has received several academic<br />
honors from local, regional and national<br />
dermatology groups. He has been happily<br />
married for 11 years to Diana Cook.<br />
Martin Cutrone, M.D., works for Albany<br />
Associates in Cardiology, P.C. He and his wife,<br />
Margaret, have four children.<br />
Thomas H. Davis, M.D., is an associate<br />
pr<strong>of</strong>essor at Dartmouth-Hitchcock <strong>Medical</strong><br />
<strong>Center</strong>. He and his wife, Robin, have three<br />
children (Bruce, Alison and Wil).<br />
David M. Lintner, M.D. (R ‘91), is the head<br />
team physician for the Houston Astros,<br />
as well as an associate pr<strong>of</strong>essor at Baylor<br />
College <strong>of</strong> Medicine and an AOSS Traveling<br />
Fellow.<br />
Class <strong>of</strong> 1987<br />
Karen Dec Rochelle, M.D., is in private practice<br />
and specializing in women’s imaging in<br />
Mount Vernon, WA. She and her husband, Rory,<br />
adopted two children from Korea — Hannah,<br />
3 years old, and Chatham, 1 1 /2 years old.<br />
Steven L. Small, M.D., is the co-director <strong>of</strong><br />
the Brain Research Imaging <strong>Center</strong> at the<br />
<strong>University</strong> <strong>of</strong> Chicago.<br />
Philip Wagner, M.D., is an anesthesiologist<br />
with a practice in pain medicine at the<br />
Hospital for Special Surgery in Manhattan.<br />
Class <strong>of</strong> 1988<br />
Randall Zielinski, M.D. (R ‘88), is in private<br />
practice in Dover, NH. He was certified<br />
by the American Society <strong>of</strong> Hypertension<br />
as a Clinical Specialist in Hypertension in<br />
August 2001.<br />
Class <strong>of</strong> 1990<br />
Peter Fung, M.D., his wife Suan, and his three<br />
children (Melanie, Christopher, and Jonathan)<br />
live in Orange County, CA. Recently, Fung<br />
became a partner physician with the Southern<br />
California Permanente <strong>Medical</strong> Group, where<br />
he practices as a staff anesthesiologist and<br />
director <strong>of</strong> the Pain Clinic at the Kaiser<br />
Permanente <strong>Medical</strong> <strong>Center</strong> in Bellflower, CA.<br />
Alex Macario, M.D., is in Madrid on a oneyear<br />
sabbatical from Stanford, working on<br />
health economics related to new drugs and<br />
technologies. Macario, his wife, Susan, 8-yearold<br />
daughter, Samantha and 7-year-old son,<br />
Kevin, report that they have settled in nicely.<br />
Ellen Louise Singer, M.D., is the lead physician<br />
for urgent care at Kaiser Interstate<br />
Emergicenter in Portland, OR. She has three<br />
boys: Ben (9), Daniel (6 1 /2 ) and Eli (18 months).<br />
Class <strong>of</strong> 1991<br />
Izchak Barzilay, D.D.S., M.S. (MS ‘91), was<br />
awarded the Bruce A. Hord Master Teaching<br />
Award by the <strong>University</strong> <strong>of</strong> Toronto Faculty <strong>of</strong><br />
Dentistry for excellence in teaching. Barzilay<br />
is the past recipient <strong>of</strong> many awards,<br />
including the Tylman Award from the<br />
American Academy <strong>of</strong> Crown and Bridge<br />
Prosthodontics; the Prosthodontics Research<br />
Award from the International Association for<br />
Dental Research, the Buonocore Award from<br />
the American Association for Dental Research<br />
<strong>Rochester</strong> Chapter, the Essay Award from the<br />
American College <strong>of</strong> Prosthodontics, and the<br />
International Journal <strong>of</strong> Oral and Maxill<strong>of</strong>acial<br />
Implants Best Paper Award. Barzilay is head<br />
<strong>of</strong> the Division <strong>of</strong> Prosthodontics and<br />
Restorative Dentistry at Mount Sinai Hospital<br />
and is assistant pr<strong>of</strong>essor at the <strong>University</strong> <strong>of</strong><br />
Toronto Faculty <strong>of</strong> Dentistry.<br />
Mignon Benjamin, M.D., and Brian Benjamin,<br />
M.D., live in Durham, NC. They both work for<br />
the <strong>University</strong> <strong>of</strong> North Carolina as family<br />
practitioners. Mignon also works for <strong>Medical</strong><br />
Reviews <strong>of</strong> North Carolina doing chart review<br />
and is medical director <strong>of</strong> 3CI.<br />
Joseph Buell, M.D., is working for the<br />
<strong>University</strong> <strong>of</strong> Cincinnati as a transplant<br />
surgeon, surgical oncologist and assistant<br />
pr<strong>of</strong>essor. He received the International Young<br />
Investigator Award from the Liver Transplant<br />
Society and served as the head <strong>of</strong> the Israel<br />
Penn International Transplant Tumor Registry.<br />
He has two boys, with a new baby on the way.<br />
Karen Johnston, M.D. (R ‘92), her husband,<br />
Jeffrey, and two children (Jeremy and Tyler)<br />
live in Charlottesville, VA. Karen works for the<br />
<strong>University</strong> <strong>of</strong> Virginia as an assistant pr<strong>of</strong>essor<br />
<strong>of</strong> neurology and health evaluation sciences.<br />
Ann O’Malley, M.D., works for Georgetown<br />
<strong>University</strong> <strong>Medical</strong> <strong>Center</strong> as an assistant<br />
pr<strong>of</strong>essor in health services research. She<br />
received various research grants from NIH<br />
and served on the Society <strong>of</strong> General Internal<br />
Medicine and the Association for Health<br />
Service Research.<br />
Patrick O’Malley, M.D., currently works<br />
for the Walter Reed Army <strong>Medical</strong> <strong>Center</strong><br />
as chief <strong>of</strong> the Division <strong>of</strong> General Internal<br />
Medicine. He served as an associate<br />
pr<strong>of</strong>essor <strong>of</strong> medicine in 2000 for the Uniformed<br />
Services <strong>University</strong> in Bethesda, MD.<br />
Bradley Schwartz, M.D., is a self-employed<br />
ophthalmologist at the Arizona Specialty Eye<br />
Care <strong>Center</strong> in Tucson, AZ. He is married to<br />
Joan Schwartz and they have three children<br />
(Ariel, Rayna and Danielle).<br />
Jeffrey Stone, M.D. (BS ‘87), lives in Martinez,<br />
GA, with his wife, Carolyn. He works for the<br />
<strong>Medical</strong> College <strong>of</strong> Georgia as an interventional<br />
neuroradiologist and an assistant<br />
pr<strong>of</strong>essor.<br />
Daniel Turner, M.D. (BA ‘87), currently works<br />
in pediatric interventional catheterization for<br />
the Children’s Hospital <strong>of</strong> Michigan. He is<br />
married to Lisa Turner, M.D., and they live in<br />
West Bloomfield, MI.<br />
Charles Whalen, M.D., works for Fort Wayne<br />
<strong>Medical</strong> Oncology/Hematology in Indiana.<br />
He and his wife, Gita, have three children<br />
(Olivia, Judson and Celeste).<br />
Class <strong>of</strong> 1992<br />
Gina A. Martin, M.D. (R ‘95) married Lloyd B.<br />
Cuyler on September 22, 2001. Martin is an<br />
internist at Wilson Health <strong>Center</strong> in <strong>Rochester</strong><br />
and Lloyd is a patrol lieutenant in the<br />
<strong>Rochester</strong> Police Department.<br />
Class <strong>of</strong> 1994<br />
Antonio J. Eppolito, M.D., a family physician<br />
serving as a U.S. Air Force flight surgeon<br />
in support <strong>of</strong> Operation Northern Watch in<br />
Turkey, was reassigned in October 2001 to<br />
Peterson AF Base in Colorado <strong>Spring</strong>s in<br />
support <strong>of</strong> Space Command.<br />
SPRING / SUMMER <strong>2002</strong> 45
class notes<br />
Paul Tulikangas, M.D., is working on the<br />
faculty at the <strong>University</strong> <strong>of</strong> Connecticut in<br />
the Department <strong>of</strong> Ob/Gyn. He and his wife,<br />
Michele, are enjoying work and their two<br />
daughters, Christine and Anne.<br />
Class <strong>of</strong> 1995<br />
Diane D. Montgomery, M.D. (R ‘98), and her<br />
husband, Craig, are proud to announce the<br />
birth <strong>of</strong> their son, Nathan, born on August 3,<br />
2001. The family lives in Syracuse, NY.<br />
Class <strong>of</strong> 1996<br />
Hugh Babineau, M.D., completed his general<br />
surgery residency at The Mary Imogene<br />
Bassett Hospital in Cooperstown, NY, and<br />
is now in solo practice in Tyler, TX.<br />
Paula Busse, M.D., is working for Mount Sinai<br />
Hospital in New York City as a clinical<br />
instructor in allergy and immunology. She has<br />
received the American Academy <strong>of</strong> Allergy<br />
and Immunology Future Leaders Award and<br />
a two-year term appointment on the American<br />
College <strong>of</strong> Graduate <strong>Medical</strong> Education Board<br />
for Review <strong>of</strong> Allergy/Immunology Fellowship<br />
Training Programs. She has been a Fellow-in-<br />
Training member <strong>of</strong> the American Academy<br />
<strong>of</strong> Allergy and Immunology and the American<br />
College <strong>of</strong> Allergy and Immunology.<br />
Mark A. Deuber, M.D., and Christina Gray<br />
Deuber, M.D. (M ‘92, R ‘95), are currently living<br />
in Dallas, where Mark is in plastic surgery<br />
private practice and Tina is a pediatrician.<br />
Louis Eichel, M.D., is the 2001 Pfizer Scholars<br />
in Urology grant recipient at the <strong>University</strong><br />
<strong>of</strong> <strong>Rochester</strong>. The award honors Eichel as<br />
an outstanding physician who has made<br />
important contributions to research and<br />
patient care in urology.<br />
Peter Fischer, M.D., is currently working as<br />
an anesthesiologist at Brigham & Women’s<br />
Hospital in Boston, MA, where he was a chief<br />
resident.<br />
Garrett Lam, M.D., is enjoying life in the South<br />
at the <strong>University</strong> <strong>of</strong> North Carolina, where he<br />
is a fellow in maternal-fetal medicine and clinical<br />
instructor in ob/gyn. He has received a<br />
Preeclampsia Foundation grant and served as<br />
speaker for the North American Society<br />
for the Study <strong>of</strong> Hypertension in Pregnancy.<br />
Yvonne Murphy, M.D., lives in Oak Park, IL,<br />
and works for MacNeal Hospital as a faculty<br />
physician. She has served on the American<br />
Academy <strong>of</strong> Family Physicians and the<br />
Society <strong>of</strong> Teachers <strong>of</strong> Family Medicine.<br />
Carla Peracchia, M.D., and Eugene<br />
Storozynsky, M.D., Ph.D. (B.S. ‘90, M.S. ‘96,<br />
Ph.D. ‘98, M ‘00), are proud to announce<br />
the birth <strong>of</strong> their third baby, Roman Mycola,<br />
on December 22, 2001. Carla is an internist<br />
at Strong Memorial Hospital and is a member<br />
<strong>of</strong> the American College <strong>of</strong> Physicians.<br />
Eugene is doing his residency in internal<br />
medicine at Strong Memorial Hospital.<br />
Dina Plekavich, M.D., received the Young<br />
Award and Morgan Award and is currently<br />
a general internist at the Fallon Clinic in<br />
Massachusetts.<br />
Kirsten Staples, M.D., and her husband,<br />
Harold, are thrilled with the birth <strong>of</strong> their son,<br />
Nathaniel. She is currently working for<br />
Penobscot Bay Physicians and Associates.<br />
David W. Toth, M.D., and his wife, Renee,<br />
are proud to announce the birth <strong>of</strong> their son,<br />
Brayden Alexander, born November 10, 2001.<br />
Brayden is growing quickly, and his parents<br />
are enjoying discovering new things with him<br />
every day. Toth is finishing his endocrine<br />
fellowship at the <strong>University</strong> <strong>of</strong> Virginia, and<br />
occasionally runs into classmates Joshua<br />
Greenhoe, Christina Bove, Jay Gangemi,<br />
Jeff Claridge, and Richard Knee. (He notes<br />
that UVA is crawling with <strong>Rochester</strong> alumni<br />
from other years as well!) The Toths just<br />
traveled down to Durham, NC, and spent<br />
a weekend catching up with Garrett Lam,<br />
his wife, Jenni, and their dog, Max. In July,<br />
Toth begins his first “real” job as an attending<br />
endocrinologist at St. Luke’s <strong>Medical</strong> <strong>Center</strong><br />
in Milwaukee, WI. He received the Endocrine<br />
Society Research Travel Grant Award in 2001.<br />
Class <strong>of</strong> 1997<br />
Kelly Goonan, M.P.H. ‘97, C.P.H.Q., moved from<br />
Raleigh, NC, to Greensboro, NC, in April 2001<br />
to begin working as evaluation coordinator<br />
for the <strong>Center</strong> for Healthcare Research and<br />
Quality at Wake Forest <strong>University</strong> School <strong>of</strong><br />
Medicine. As a former dance and biology<br />
major at SUNY-Brockport, Goonan is also<br />
excited to report making the <strong>2002</strong> dance team<br />
for Prowlers Arena Football in Greensboro.<br />
Eliana Miller Perrin, M.D., is in the last year<br />
<strong>of</strong> a Robert Wood Johnson clinical research<br />
fellowship. She is hoping to go into academic<br />
medicine. She gave birth to a son on Sept. 23,<br />
2000.<br />
Class <strong>of</strong> 1998<br />
Colleen Barber, M.D. (B.S. ‘94, M ‘98), and her<br />
husband, Keith, welcomed their first child,<br />
Lily Catherine Bromley, into the world on June<br />
22, 2001. Barber will be finishing an ob/gyn<br />
residency in June and has accepted a position<br />
with the Dartmouth-Hitchcock Clinic in<br />
Manchester, NH.<br />
Amy E. Sass, M.D., started a fellowship in<br />
adolescent medicine at Children’s Hospital<br />
in Boston, MA.<br />
Robert Whorf, M.D., and his wife, Patricia,<br />
are proud to announce the birth <strong>of</strong> their son,<br />
Jacob. He was born on November 23, 2001.<br />
Whorf recently finished his internal medicine<br />
residency at Strong and is currently doing<br />
an oncology fellowship at Yale.<br />
Class <strong>of</strong> 1999<br />
Heather Evans, M.D., is a PGY-3 in the<br />
Department <strong>of</strong> Surgery at the <strong>University</strong> <strong>of</strong><br />
Virginia Health System and just started a<br />
two-year research fellowship in the Surgical<br />
Infectious Disease Research Laboratory. She<br />
also enrolled in the Graduate School <strong>of</strong> Arts<br />
and Sciences at the <strong>University</strong> <strong>of</strong> Virginia and<br />
will be working toward a master’s in health<br />
evaluation sciences with a focus in health<br />
services research and outcomes evaluation.<br />
Andrew C. Swiderski, M.D., married Amy<br />
Yoxthimer on August 11, 2000. He is a pediatric<br />
resident at Strong Memorial Hospital, and<br />
Amy is a clinical technician in Chili, NY.<br />
Class <strong>of</strong> 2001<br />
David Sullo, M.D. (B.A. ‘94, M ‘98, R ‘01),<br />
married Sari Aintablian on July 1, 2001.<br />
46<br />
ROCHESTER MEDICINE
in memoriam<br />
James W. Bartlett, M.D. (R ’57)<br />
James W. Bartlett, M.D. (R ’57), a towering figure<br />
who drove important change at the <strong>University</strong><br />
<strong>of</strong> <strong>Rochester</strong> <strong>Medical</strong> <strong>Center</strong> in a career that<br />
spanned more than three decades, died March<br />
24, 2001, in Maryland <strong>of</strong> multiple myeloma,<br />
a bone marrow cancer. He was 75.<br />
In 1958, shortly after completing his residency<br />
at <strong>Rochester</strong>, the then 31-year-old<br />
psychiatrist was named assistant dean in the<br />
School <strong>of</strong> Medicine and Dentistry. By the time<br />
he left <strong>Rochester</strong> in 1990 to become dean <strong>of</strong><br />
health sciences at The Aga Khan <strong>University</strong> in<br />
Pakistan, he had held many key posts,<br />
including medical director <strong>of</strong> Strong Memorial<br />
Hospital, associate dean <strong>of</strong> the medical school,<br />
and chairman <strong>of</strong> health services. He is particularly<br />
remembered for the leading role he played<br />
as Strong’s medical director (1967 – 1983)<br />
during a period that included planning and<br />
construction <strong>of</strong> the “new” Strong, which<br />
opened in 1975.<br />
Pr<strong>of</strong>essor <strong>of</strong> Medicine Emeritus Paul<br />
Griner, M.D. (M ’59), whose career at the <strong>Medical</strong><br />
<strong>Center</strong> overlapped Dr. Bartlett’s, remembers his<br />
6’ 4” colleague as a “gentle giant” with<br />
tremendous presence: “Jim was one <strong>of</strong> those<br />
people, when he felt strongly, he just wouldn’t<br />
ever let things drop. He wasn’t a bulldog but<br />
he had a diplomatic way <strong>of</strong> working. His was<br />
a subtle but persistent approach.”<br />
Griner attributed three important<br />
changes to Bartlett’s interests and principles.<br />
Beginning before the new hospital was<br />
built and fully implemented after, all patients<br />
were assigned to hospital beds regardless <strong>of</strong><br />
their socioeconomic status or race.<br />
“That’s an important point because,<br />
early in the history <strong>of</strong> Strong, there was a clear<br />
separation, if not according to race, certainly<br />
according to economic status,” says Griner.<br />
“ Jim felt that was a discriminatory approach<br />
and it wasn’t healthy for either patient care or<br />
medical education to perpetuate that separation.”<br />
Prior to the new hospital, Bartlett also<br />
established an experimental unit to examine<br />
the roles and responsibilities <strong>of</strong> the many types<br />
<strong>of</strong> staff delivering health services. This led to a<br />
consolidation <strong>of</strong> functions, explains Griner, so<br />
that the new hospital required a smaller staff to<br />
care for patients.<br />
Finally, adds Griner, “Jim — more than<br />
any physician in the history <strong>of</strong> Strong —<br />
recognized the need for the integration <strong>of</strong><br />
nursing education and practice. Historically<br />
at the <strong>University</strong> and <strong>Medical</strong> <strong>Center</strong>, the<br />
education <strong>of</strong> nurses was almost totally independent<br />
<strong>of</strong> nursing practice. Nurse educators<br />
and nursing students would be on the floors<br />
but there was really very little, if any, interaction<br />
with the staff nurses on the floors or direct<br />
care <strong>of</strong> patients.”<br />
Bartlett pushed to integrate these activities<br />
under a separate School <strong>of</strong> Nursing and a<br />
revised <strong>Medical</strong> <strong>Center</strong> administrative structure,<br />
and worked closely with the first dean <strong>of</strong> the<br />
school, Loretta Ford, R.N., Ed.D., to achieve their<br />
shared vision. For a 75th anniversary <strong>Medical</strong><br />
<strong>Center</strong> book printed in 2000, Bartlett recalled<br />
the plan as ambitious and not easy to implement,<br />
but one with impressive results. He<br />
wrote: “Nursing became a major integrating<br />
force in managing the institution.”<br />
Bartlett’s widow, Nancy, and his son, Thomas,<br />
remember him as a man who was always<br />
keenly interested in the teaching <strong>of</strong> medical<br />
students as well as his own ongoing learning<br />
experiences. While in his 60s, Bartlett moved<br />
to Pakistan for three years to serve as dean<br />
and director at Aga Kahn <strong>University</strong>, a developing<br />
institution where the needs were great.<br />
Such a move, says his widow, was not out <strong>of</strong><br />
character for him.<br />
“He was intellectually curious all his<br />
life,” she explains. “It was an opportunity to<br />
do something different, a learning experience,<br />
and a chance to give back.”<br />
Bartlett attended Massachusetts Institute<br />
<strong>of</strong> Technology before entering the<br />
U.S. Navy during World War II. He subsequently<br />
earned his undergraduate degree at Harvard<br />
College and his M.D. from Johns Hopkins<br />
<strong>University</strong> before moving to <strong>Rochester</strong> to<br />
complete his internship and residency. He<br />
married Nancy, a psychiatric nurse at Strong<br />
when they met, in 1954. In addition to his<br />
widow and son, another son, John, and<br />
a daughter, Anne, survive him.<br />
Edward Bird, M.D. (‘48)<br />
A remembrance by<br />
Gordon Davenport, M.D. (‘48)<br />
Note: Edward Bird, M.D., was killed in December<br />
2000. Here, his friend and classmate <strong>of</strong>fers a<br />
fond remembrance.<br />
It was not the pursuit <strong>of</strong> medicine that brought<br />
Ed Bird to <strong>Rochester</strong>, but rather an interest<br />
in optics and a job with Bausch & Lomb.<br />
At Bausch, Ed was frequently assigned production<br />
problems that had baffled the company.<br />
And he solved them with his analytical and<br />
innovative mind. But eventually, Ed’s interest<br />
turned to medicine and before long he was<br />
admitted to the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> School<br />
<strong>of</strong> Medicine and Dentistry, class <strong>of</strong> 1948.<br />
SPRING / SUMMER <strong>2002</strong> 47
in memoriam<br />
Ed Bird, M.D. (center), adopted a Philippine<br />
village after retiring, raising funds for<br />
a new school and other buildings.<br />
Four years later, medical degree in hand,<br />
Ed took a navy internship at Long Beach Naval<br />
Hospital and completed a required six months<br />
<strong>of</strong> sea duty. Then Ed returned to <strong>Rochester</strong><br />
to begin a residency in hospital administration.<br />
But within a month, after being assigned to<br />
an entire day <strong>of</strong> helping the ladies <strong>of</strong> the<br />
hospital auxiliary make bandages, he decided<br />
to return to the navy and make it a career.<br />
Ed’s initial service was on the navy’s first<br />
guided-missile research vessel. The first rocket<br />
delivered to the ship was a concern because,<br />
for want <strong>of</strong> a better place to put it, they stood<br />
it up on the aft end. In Ed’s words, “No one<br />
knew, when it was fired, whether it would do<br />
what it had been told to do or if it would blow<br />
the end <strong>of</strong> the ship <strong>of</strong>f!” Fortunately, it followed<br />
instructions.<br />
The words that best describe Ed Bird are<br />
“ energy” and “fiery spirit.” Wonderful traits,<br />
though they sometimes got him into trouble.<br />
Energy, for example. While his ship was in<br />
harbor in Long Beach, he volunteered to make<br />
house calls on crew members’ families ashore,<br />
and the service became very popular. But then<br />
the doctors on nearby ships, who apparently<br />
did not have the benevolent nature <strong>of</strong> our<br />
classmate, protested because their crews were<br />
asking for the same service. Firm words passed.<br />
House calls continued, but more quietly, and<br />
word went out that the choice <strong>of</strong> provider was<br />
limited to our Ed. (Question: Was this the west<br />
coast’s first HMO?)<br />
And that fiery spirit. When one<br />
commanding <strong>of</strong>ficer ordered what Ed felt was<br />
unfair punishment for one <strong>of</strong> his corpsmen,<br />
Ed went toe to toe with him. A couple <strong>of</strong><br />
centuries ago that would have meant certain<br />
keel hauling. (Look it up!) Even today, Ed was<br />
flirting with charges and unpleasant action.<br />
But he stood his ground and eventually the<br />
captain capitulated, which made Ed — in the<br />
eyes <strong>of</strong> his already admiring corpsmen —<br />
another couple <strong>of</strong> feet taller.<br />
When at sea, duty consisted <strong>of</strong> the usual<br />
general practice problems and an occasional<br />
bit <strong>of</strong> surgery. Once, in the middle <strong>of</strong> the<br />
Pacific, a sailor on another ship needed an<br />
appendectomy. The sea was so rough that<br />
a helicopter had to pick Ed up and lower him<br />
to the deck <strong>of</strong> the other ship. On the way down<br />
the strong winds swung him about rather<br />
mercilessly, even bouncing him <strong>of</strong>f a stack once<br />
or twice. Eventually he touched down, intact<br />
enough to do the appendectomy.<br />
Throughout his career, Ed was dogged<br />
by the fact that he was red-green colorblind.<br />
Once retired, he admitted his defect and told<br />
how he had circumvented this little deficiency.<br />
A simple mechanism, really, known as<br />
cheating. During one examination, as he<br />
approached the eye exam section, he climbed<br />
out the window <strong>of</strong> a men’s room, papers in<br />
hand. He then filled in the blanks appropriately,<br />
re-entered beyond the eye exam section,<br />
and he was in the navy! Once in uniform, he<br />
continued to pass routine physicals by memorizing<br />
the pattern <strong>of</strong> dots on the pages <strong>of</strong> the<br />
eye color test books.<br />
Eventually, Ed became head <strong>of</strong> the<br />
Audiovisual Training Section <strong>of</strong> the Bureau<br />
<strong>of</strong> Medicine and Surgery, working at Bethesda<br />
Naval Hospital. He developed the <strong>Medical</strong><br />
Television Department <strong>of</strong> the National Naval<br />
<strong>Medical</strong> <strong>Center</strong>, and directed the production <strong>of</strong><br />
teaching films.<br />
Retired from the navy, Ed Bird remained<br />
as busy as ever. He recalled a village he had<br />
visited in the Philippines with crude conditions<br />
and hardly a decent building. He decided to<br />
adopt it. He secured funding and organized<br />
building projects, starting with a school. This<br />
was no simple task. Among other problems,<br />
construction material had to be brought over<br />
a gorge on a swinging suspension bridge. But<br />
the village was transformed. A bust <strong>of</strong> Ed now<br />
occupies a prominent site outside that school.<br />
In his later life, Ed experienced a major<br />
injustice. An acute illness left him severely<br />
neurologically impaired. He was almost quadriplegic.<br />
A lengthy period <strong>of</strong> rehabilitation<br />
followed, and eventually he was provided with<br />
a motorized chair. On his first attempt to<br />
manipulate the chair he confused the controls,<br />
and both he and the chair ended up in a swimming<br />
pool. But once mastered, the chair<br />
provided him mobility and he became reasonably<br />
active again.<br />
Ed eventually settled in his beloved<br />
Hawaii, where his candy handouts made him<br />
very popular with the younger generations.<br />
Unfortunately, one night, an adult couple<br />
decided to rob our 80-year-old friend, and in<br />
the process bludgeoned him to death. The<br />
culprits were identified and as <strong>of</strong> this writing<br />
are awaiting trial.<br />
Before his death, Ed Bird wrote an entertaining<br />
autobiography. I am fortunate to have<br />
a copy, from which comes much <strong>of</strong> the information<br />
herein.<br />
During his lifetime, Ed financed the<br />
schooling <strong>of</strong> several people. As a final salute to<br />
the value he placed on education, his will dedicated<br />
the proceeds <strong>of</strong> his insurance to the<br />
education <strong>of</strong> the children <strong>of</strong> ten families in the<br />
Philippines, as well as for an addition to the<br />
school — the school that exists because <strong>of</strong> the<br />
drive and generosity <strong>of</strong> Ed Bird.<br />
48<br />
ROCHESTER MEDICINE
in in memoriam<br />
Frank W. Masters, M.D. (‘45)<br />
By Paul R. Schloerb, M.D. (’44),<br />
and David W. Robinson, M.D.<br />
Note: Schloerb and his colleague at the<br />
<strong>University</strong> <strong>of</strong> Kansas <strong>Medical</strong> <strong>Center</strong> <strong>of</strong>fer<br />
a remembrance <strong>of</strong> their good friend.<br />
Frank W. Masters, M.D. (’45), an outstanding<br />
leader in plastic surgery, a devoted teacher and<br />
friend, died on October 14, 2001, at the age <strong>of</strong> 80<br />
at his home in Mission Hills, Kans., after a long<br />
battle with prostate cancer.<br />
Frank was born in Pittsburgh, Pa., and<br />
attended public and private schools in Kansas<br />
City, Cleveland, and New Jersey. After graduating<br />
from Hamilton College and from medical<br />
school at the <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> in 1945,<br />
he served in the Philippines as a captain in<br />
the <strong>Medical</strong> Corps. He then returned to<br />
<strong>Rochester</strong> to train as a surgical resident at<br />
Strong Memorial Hospital — he start <strong>of</strong> a long<br />
association with Robert McCormick, M.D.,<br />
later the head <strong>of</strong> plastic surgery at <strong>Rochester</strong>.<br />
In 1949, another long association began.<br />
Frank married a <strong>Rochester</strong> graduate, Jean<br />
Cooper, a nurse. It was a legend that Jean and<br />
her identical twin sister, Joan (a student nurse),<br />
could switch dates and no one would know!<br />
He completed a residency in plastic<br />
surgery at Duke <strong>University</strong> Hospital, then<br />
accepted an appointment as chief <strong>of</strong> plastic<br />
surgery at Charleston Memorial Hospital<br />
in Charleston, W. Va. In 1958, he became an<br />
associate pr<strong>of</strong>essor at the <strong>University</strong> <strong>of</strong> Kansas<br />
<strong>Medical</strong> <strong>Center</strong> and a partner <strong>of</strong> David W.<br />
Robinson, M.D., and stayed on until he retired in<br />
1989. According to Robinson, this association<br />
was characterized by not one unresolved argument<br />
over a span <strong>of</strong> 33 years!<br />
After just nine years, Frank became a<br />
pr<strong>of</strong>essor <strong>of</strong> surgery in 1967 and was appointed<br />
head <strong>of</strong> the section <strong>of</strong> plastic surgery when<br />
Dr. Robinson retired as chief. Frank’s abilities<br />
as surgeon, teacher, researcher, administrator<br />
and leader in the medical school were fully<br />
evident. He was appointed chair <strong>of</strong> the<br />
Executive Committee <strong>of</strong> the medical staff from<br />
1972 to 1976 and chair <strong>of</strong> the Department <strong>of</strong><br />
Surgery from 1976 to 1986.<br />
Frank was also a leader in many plastic<br />
surgery societies, including the American Board<br />
<strong>of</strong> Plastic Surgery (which he chaired in 1974).<br />
His memberships were numerous, including<br />
the American <strong>Medical</strong> Association and the<br />
American College <strong>of</strong> Surgeons. Testimony to his<br />
outstanding teaching ability was his election by<br />
medical students to membership in the prestigious<br />
Alpha Omega Alpha, Kansas Chapter.<br />
His influence was international, as<br />
visiting pr<strong>of</strong>essorships and lectureships took<br />
him to many academic centers around the<br />
country and overseas (including a stint in 1963<br />
at the Christian <strong>Medical</strong> College and Karagirie<br />
Leprosarium in South India).<br />
In his career, Frank authored more than<br />
75 papers — some research but mostly based<br />
on his clinical experiences.<br />
As hobbies, Frank collected Western art,<br />
played golf, did needlepoint and enjoyed traveling<br />
with Jean. He and Dr. Robinson were<br />
the surgeons for the Kansas City hockey team,<br />
and he was a loyal fan <strong>of</strong> Kansas <strong>University</strong><br />
teams as well as the Kansas City Royals and<br />
Chiefs. He and Jean were devoted members <strong>of</strong><br />
the St. Andrews Episcopal Church in Kansas<br />
City, where Frank was elected to the vestry and<br />
was a junior warden. After Jean passed away,<br />
Frank devoted much more time to this activity,<br />
which provided emotional support to him in<br />
his terminal illness.<br />
Frank will be missed by all who knew<br />
and loved him. He is survived by his three children,<br />
Frank W. Masters III, Pittsburgh, Kans.;<br />
Pam Appenfeller, Leawood, Kans.; and Randy<br />
Masters, Paola, Kans.; and five granddaughters.<br />
In Memoriam<br />
1935<br />
William E. Merrill, M.D., Sheridan, WY<br />
1936<br />
Robert A. Burns, M.D., Little River, CA<br />
1940<br />
Clara Hinton Williams, Ph.D., Towson, MD<br />
1941<br />
Carl S. Hellijas, M.D., Pinellas Park, FL<br />
George A. Moll, M.D., Hanover, PA<br />
1942<br />
David S. Parker, M.D. (R ’42), <strong>Rochester</strong>, NY<br />
1943<br />
Richard H. Koenemann, M.D., <strong>Rochester</strong>, NY<br />
Arnold A. Nutting, M.D., Redding, CA<br />
1945<br />
Francis W. Masters, M.D., Shawnee Mission, KS<br />
Gerald Miller, M.D., Somers, NY<br />
1947<br />
Edith Searles Porter, M.D., Gorham, NY<br />
1951<br />
Bernard F. Donovan, M.D. (R ’52), Henrietta, NY<br />
William E. Smedley Jr., M.D., Grand Junction, CO<br />
1952<br />
Merle L. Gibson Jr., M.D., Owings, MD<br />
1958<br />
Alden H. Hayden, M.D. (R ’58), Pittsford, NY<br />
1961<br />
Ronald W. Tatum, M.D., (R ’64, FLW ’66),<br />
Albuquerque, NM<br />
1964<br />
David P. Campbell, M.D., Placitas, NM<br />
Robert H. McLean, M.D., Towson, MD<br />
1970<br />
Jack I. Stein, M.D. (R ’70)<br />
SPRING / SUMMER <strong>2002</strong> 49
in memoriam<br />
In Memoriam<br />
1935<br />
William E. Merrill, M.D.<br />
Sheridan, WY<br />
1936<br />
Robert A. Burns, M.D .<br />
Little River, CA<br />
1940<br />
Clara Hinton Williams, Ph.D.<br />
Towson, MD<br />
1941<br />
Carl S. Hellijas, M.D .<br />
Pinellas Park, FL<br />
George A. Moll, M.D .<br />
Hanover, PA<br />
1942<br />
David S. Parker, M.D.<br />
(R ’‘42)<br />
<strong>Rochester</strong>, NY<br />
1943<br />
Richard H. Koenemann, M.D.<br />
<strong>Rochester</strong>, NY<br />
Arnold A. Nutting, M.D.<br />
Redding, CA<br />
1945<br />
Francis W. Masters, M.D.<br />
Shawnee Mission, KS<br />
Gerald Miller, M.D.<br />
Somers, NY<br />
50<br />
ROCHESTER MEDICINE
<strong>Rochester</strong> Rises in the Rankings<br />
The <strong>University</strong> <strong>of</strong> <strong>Rochester</strong> School <strong>of</strong> Medicine and<br />
Dentistry has risen from 31st last year to 28th in research,<br />
and from 14th to 7th in primary care, in U.S. News and<br />
World Report's annual ranking <strong>of</strong> the country's top<br />
medical schools.<br />
U.S. News looks at several criteria, including<br />
NIH research grants, MCAT scores, faculty-student ratio,<br />
acceptance rate and peer and residency directors'<br />
assessments.<br />
The rankings were reported in April in the magazine's<br />
annual guide to the best graduate schools.<br />
Univeristy <strong>of</strong> <strong>Rochester</strong><br />
School <strong>of</strong> Medicine and Dentistry<br />
601 Elmwood Avenue, box 643<br />
<strong>Rochester</strong>, NY 14642<br />
Non-Pr<strong>of</strong>it Org.<br />
US Postage<br />
PAID<br />
Permit No. 780<br />
<strong>Rochester</strong>, NY<br />
Change Service Requested