Root Canal Obturation: An Update - IneedCE.com
Root Canal Obturation: An Update - IneedCE.com
Root Canal Obturation: An Update - IneedCE.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
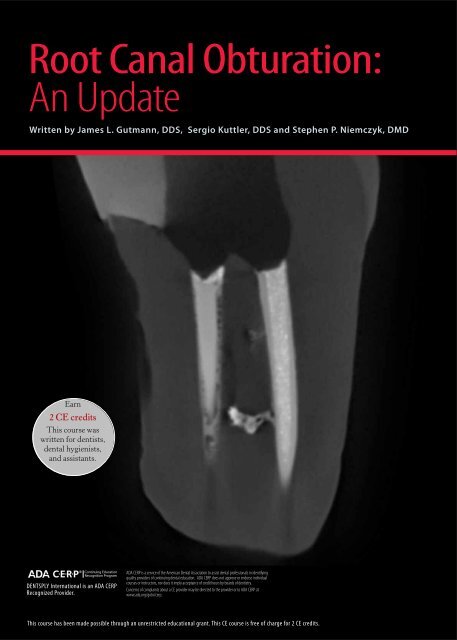
<strong>Root</strong> <strong>Canal</strong> <strong>Obturation</strong>:<br />
<strong>An</strong> <strong>Update</strong><br />
Written by James L. Gutmann, DDS, Sergio Kuttler, DDS and Stephen P. Niemczyk, DMD<br />
Earn<br />
2 CE credits<br />
This course was<br />
written for dentists,<br />
dental hygienists,<br />
and assistants.<br />
DENTSPLY International is an ADA CERP<br />
Recognized Provider.<br />
ADA CERP is a service of the American Dental Association to assist dental professionals in identifying<br />
quality providers of continuing dental education. ADA CERP does not approve or endorse individual<br />
courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry.<br />
Concerns of <strong>com</strong>plaints about a CE provider may be directed to the provider or to ADA CERP at<br />
www.ada.org/goto/cerp.<br />
This course has been made possible through an unrestricted educational grant. This CE course is free of charge for 2 CE credits.
Educational Objectives<br />
The overall goal of this article is to provide the reader with<br />
information on available materials and techniques for the<br />
obturation of root canal systems.<br />
Upon <strong>com</strong>pletion of this course, the dental professional<br />
will be able to:<br />
1. List the purposes of root canal obturation<br />
2. List the characteristics of gutta-percha used for obturation<br />
3. List and describe the contemporary materials and<br />
techniques for obturating root canals<br />
4. List the most widely-used techniques for gutta-percha<br />
carrier-based obturation and describe its strengths and<br />
short<strong>com</strong>ings.<br />
Abstract<br />
<strong>Obturation</strong> is a critical <strong>com</strong>ponent of root canal therapy, and<br />
must both provide a <strong>com</strong>plete seal for the root canal system<br />
and eliminate all avenues of leakage from the oral cavity.<br />
Historically, gutta-percha cones have been the standard<br />
material of choice for root canal obturation, used together<br />
with a sealer/cement. The first gutta-percha carrier-based<br />
obturating techniques were developed more than two decades<br />
ago. More recently, obturating techniques have been<br />
introduced that include resin-based sealers and obturators,<br />
syringe-applied heated gutta-percha, and the use of guttapercha<br />
as an outer coating on obturator carriers <strong>com</strong>posed<br />
of plastic or metal. It is important to select an obturation<br />
technique that offers consistency and is easy to use.<br />
Introduction<br />
<strong>Root</strong> canal obturation involves the three-dimensional filling<br />
of the entire root canal system and is a critical step in<br />
endodontic therapy. There are two purposes to obturation:<br />
the elimination of all avenues of leakage from the oral cavity<br />
or the periradicular tissues into the root canal system;<br />
and the sealing within the root canal system of any irritants<br />
that remain after appropriate shaping and cleaning of the<br />
canals, thereby isolating these irritants. Pulpal demise and<br />
subsequent periradicular infection result from the presence<br />
of microorganisms, microbial toxins and metabolites, and<br />
the products of pulp tissue degradation. Failure to eliminate<br />
these etiologic factors and to prevent further irritation as a<br />
result of continued contamination of the root canal system<br />
are the prime reasons for failure of nonsurgical and surgical<br />
root canal therapy. 1,2,3,4,5<br />
The importance of three-dimensional obturation of the<br />
root canal system cannot be overstated, with the ability<br />
to achieve this goal primarily dependent on the quality of<br />
canal cleaning and shaping as well as clinical skill. Other<br />
factors that influence the ultimate success or failure of each<br />
case include the materials used and how they are used. The<br />
ultimate coronal restoration of the tooth following canal<br />
obturation may loom as the most important goal, for there<br />
is reasonable evidence that coronal leakage through improperly<br />
placed restorations after root canal treatment and<br />
failure of the restorative treatment or lack of health of the<br />
supporting periodontium are the final determinants of success<br />
or failure in treatment. 6,7,8<br />
Figure 1. Factors influencing <strong>com</strong>plete obturation<br />
Quality of the cleaning and shaping of the canal system<br />
Skill and experience of the clinician<br />
Materials and their usage<br />
Restoration of the tooth<br />
Health of the supporting periodontium<br />
Characteristics of an Ideal <strong>Root</strong> <strong>Canal</strong> Filling<br />
<strong>An</strong> ideal root canal filling three-dimensionally fills the entire<br />
root canal system as close to the cemento-dentinal junction<br />
as possible. Minimal amounts of root canal sealers, most of<br />
which have been shown to be bio<strong>com</strong>patible or tolerated by<br />
the tissues in their set state, are used in conjunction with the<br />
core filling material to establish an adequate seal. Radiographically,<br />
the root canal filling should have the appearance<br />
of a dense, three-dimensional filling that extends as close as<br />
possible to the cemento-dentinal junction. These standards<br />
should serve as the benchmark for all clinicians performing<br />
root canal therapy, and it is only through a knowledgeable<br />
approach to root canal treatment that quality assurance can<br />
be continually demonstrated in the obturation of root canal<br />
systems. 9,10<br />
The ideal root canal filling<br />
Figure 2a. 3-D filling of the entire root canal space as close as<br />
possible to the cemento-dentinal junction<br />
Figure 2b. Radiographically dense fill with absence of voids<br />
2 www.ineedce.<strong>com</strong>
Figure 2c. Shape reflecting a continuously tapered funnel that is<br />
approximately the same as the external root morphology<br />
While a plethora of materials has been advocated over the last<br />
150 years for root canal obturation, historically, gutta-percha<br />
has proven to be the material of choice for successful filling<br />
of root canals from their coronal to apical extent. Although<br />
it is not the ideal filling material, gutta-percha has satisfied<br />
the majority of criteria for an ideal root filling material. The<br />
disadvantages of gutta-percha – specifically, its adhesiveness,<br />
lack of rigidity, and ease of displacement under pressure – do<br />
not overshadow its advantages. In light of its short<strong>com</strong>ings,<br />
a sealer/cement is always used with gutta-percha. However,<br />
regardless of the delivery system or technique used, neither<br />
gutta-percha nor sealer/cement alone enables standard-ofcare<br />
canal obturation. In addition, the available materials and<br />
techniques do not routinely provide for an impervious seal of<br />
the canal system; all canals leak to a greater or lesser extent.<br />
It is re<strong>com</strong>mended that clinicians master multiple obturation<br />
techniques and be<strong>com</strong>e <strong>com</strong>petent with various root canal<br />
sealers/cements, to be able to manage the diversity of anatomical<br />
scenarios that may be encountered. 11,12<br />
Contemporary Sealers/Cements<br />
The use of a sealer during root canal obturation is essential<br />
for success. Not only does it enhance the possible attainment<br />
of an impervious seal, it also serves as a filler for canal<br />
irregularities and minor discrepancies between the root canal<br />
wall and core filling material. Sealers are often expressed<br />
through lateral or accessory canals and can assist in microbial<br />
control should there be microorganisms left on the root canal<br />
walls or in the tubules. 13,14,15,16,17,18 Sealers can also serve<br />
as lubricants, enabling thorough seating of the core filling<br />
material during <strong>com</strong>paction. In canals in which the smear<br />
layer has been removed, many sealers demonstrate increased<br />
adhesive properties to dentin in addition to flowing into the<br />
patent tubules. 19,20,21,22,23,24,25,26,27,28,29 A good sealer should be<br />
bio<strong>com</strong>patible and well tolerated by the periradicular tissues,<br />
and although all sealers exhibit toxicity when freshly mixed,<br />
their toxicity is greatly reduced on setting and all are absorbable<br />
when exposed to tissues and tissue fluids. Subsequent<br />
tissue healing or repair generally appears unaffected by most<br />
sealers, provided there are no adverse breakdown products of<br />
the sealer over time. In particular, the breakdown products<br />
may have an adverse action on the proliferative capability of<br />
periradicular cell populations. Some clinicians consider that<br />
a small puff of root canal filler extending beyond the working<br />
length is indicative of a fully obturated canal space with<br />
a well-sealed apical constriction. Excessive sealer should not<br />
be routinely placed in the periradicular tissues as part of an<br />
obturation technique. 30,31,32,33,34,35,36,37,38,39,40,41,42<br />
Sealers/cements can be grouped based on their prime constituent<br />
or structure, such as zinc oxide-eugenol, polyketone,<br />
epoxy, calcium hydroxide, silicone, resin, glass ionomer, or<br />
resin-modified glass ionomer. However, many of the sealers/<br />
cements are <strong>com</strong>binations of <strong>com</strong>ponents, such as zinc oxideeugenol<br />
and calcium hydroxide, 43 with the addition of calcium<br />
hydroxide claimed to create a therapeutic material that can<br />
be inductive of hard tissue formation. 44,45 Epoxy-based and<br />
methacrylate-based resin sealers that can be bonded to the root<br />
canal dentin (but not to gutta-percha) are also now available. 46<br />
Sealers should be mixed to a creamy consistency, allowing<br />
them to adhere to the master cone and not ball up at the shaft of<br />
the cone, leaving the gutta-percha exposed. The sealer should<br />
adhere to the cone evenly along its length and at the end of the<br />
cone. Clinicians should read the product insert and material<br />
safety data sheet for each product chosen before using it.<br />
Contemporary Core Filling Materials<br />
Gutta-percha is the standard material of choice as a solid<br />
core filling material for canal obturation. It demonstrates<br />
minimal toxicity and minimal tissue irritability, is the least<br />
allergenic material available when retained within the canal<br />
system, 47 and in cases of inadvertent gutta-percha cone<br />
overextension into the periradicular tissues, is well tolerated<br />
provided the canal is clean and sealed.<br />
Chemical solvents have been used for almost 100 years to<br />
soften gutta-percha, with methods ranging from merely dipping<br />
the gutta-percha cones into the solvent for one second for<br />
better canal adaptation, to creating a <strong>com</strong>pletely softened paste<br />
of gutta-percha with the solvent. Solvents used have included<br />
chloroform, halothane, rectified white turpentine, and eucalyptol.<br />
Periradicular tissues may be irritated if the solvent is<br />
expressed beyond the canal or significant amounts of softened<br />
gutta-percha are inadvertently placed into the periradicular<br />
tissues. Failure to allow for dissipation of chemical solvents, if<br />
volatile, or the removal of excess solvent with alcohol can result<br />
in significant shrinkage and possible loss of the apical seal. The<br />
use of chemical solvents has been both praised and questioned,<br />
but with the advent of thermoplasticized gutta-percha, the<br />
need to consider the use of solvents at any time must be questioned.<br />
The use of solvents, however, may still be considered<br />
for a number of challenges the clinician may face in daily practice,<br />
such as the custom fitting of master cones in irregular apical<br />
preparations or following apexification. 48,49,50,51,52,53,54,55,56,57<br />
Gutta-percha Cones<br />
The <strong>com</strong>position of gutta-percha cones is approximately<br />
19% to 22% Balata and 59% to 75% zinc oxide, with the re-<br />
www.ineedce.<strong>com</strong> 3
mainder a <strong>com</strong>bination of various waxes, coloring agents,<br />
antioxidants, and metallic salts. 58 The specific percentages for<br />
<strong>com</strong>ponents varies by manufacturer, with resulting variations<br />
in the brittleness, stiffness, tensile strength, and radiopacity<br />
of the individual cones attributable primarily to the percentages<br />
of gutta-percha and zinc oxide. The antimicrobial activity<br />
of gutta-percha is also primarily due to the zinc oxide. 59,60<br />
The cones are manufactured in both standardized and nonstandardized<br />
sizes. The standardized sizes coordinate with<br />
the ISO root canal files sizes 15 through 140 and are used<br />
primarily as the main core material for obturation. They generally<br />
have a 2% taper, but can have a 4 or 6% taper or more<br />
(Figure 3). The non-standardized sizes are more tapered from<br />
the tip or point to the top. With some obturation techniques<br />
these cones have been used primarily as accessory or auxiliary<br />
cones during <strong>com</strong>paction, being matched with the shape of<br />
the prepared canal space or the <strong>com</strong>paction instrument.<br />
Non-standardized cones began to assume a greater role as the<br />
primary core material in the more contemporary obturation<br />
techniques, and with the development of more predictable<br />
shapes with current nickel titanium (NiTi) rotary and hand<br />
instruments, cones tapered from 4% to 10% have gained use.<br />
Figure 3. Tapered gutta-percha cones<br />
In particular, for techniques that use vertical <strong>com</strong>paction of<br />
heat-softened gutta-percha, both the non-standardized and<br />
more tapered cones have be<strong>com</strong>e quite acceptable. Custom<br />
cones can also be developed for canals with irregular or large<br />
apical anatomy, Over time, numerous methods have been<br />
advocated for obturating the prepared root canal system, each<br />
with their own claims of ease, efficiency, or superiority. Most<br />
contemporary techniques still rely on gutta-percha and sealer<br />
to achieve their goal. Four basic techniques exist for the obturation<br />
of the root canal system with gutta-percha and sealer<br />
(Figure 4): (1) the cold <strong>com</strong>paction of gutta-percha; (2) the<br />
<strong>com</strong>paction of heat-softened gutta-percha with cold instruments<br />
until it has cooled; (3) the <strong>com</strong>paction of gutta-percha<br />
that has been thermoplasticized, injected into the system, and<br />
<strong>com</strong>pacted with cold instruments; and (4) the <strong>com</strong>paction of<br />
gutta-percha that has been placed in the canal and softened<br />
through the continuous wave technique (Calamus). A multitude<br />
of variations on these four basic themes exists. For<br />
injectable thermoplastic obturation techniques, gutta-percha<br />
may <strong>com</strong>e in either pellet forms or in cannulae.<br />
Figure 4a. Figure 4b. Figure 4c.<br />
Cold <strong>com</strong>paction carrier Heated <strong>com</strong>paction Presoftened core<br />
No single technique has proven to have statistically<br />
significant superiority when considering both in vitro and<br />
in vivo studies, as the success of all techniques is highly<br />
dependent on the cleaning and shaping of the canals and the<br />
clinician’s expertise in the use of a particular technique. 61,62<br />
While many have advocated the use of the lateral <strong>com</strong>paction<br />
technique or a single cone fill (monocone) to achieve a<br />
quality apical seal, the technique in itself does not necessarily<br />
favor the filling of canal irregularities. 63 Recognizing this,<br />
use of a softened gutta-percha technique with heat or chemical<br />
softening is required to achieve a thorough obturation.<br />
In addition, while filling the entire root canal system is the<br />
major goal of canal obturation, a major controversy exists as<br />
to what constitutes the apical termination of the root canal<br />
filling material. Working length determination guidelines<br />
often cite the cemento-dentinal junction or apical constriction<br />
as the ideal position for terminating canal cleaning and<br />
shaping procedures and placing the filling material. However,<br />
the cemento-dentinal junction is a histologic and not<br />
a clinical position in the root canal system 64 (Figure 5) and,<br />
in addition, the cemento-dentinal junction is not always the<br />
most constricted portion of the canal (yellow arrows) in the<br />
apical portion of the root (Figure 6). 65,66,67,68,69,70,71,72,73,74,75<br />
Figure 5. Histologic position of cemento-dentinal junction<br />
4 www.ineedce.<strong>com</strong>
Contemporary practices of obturation favor material softening;<br />
even this does not guarantee that an impervious seal of<br />
the root canal system will be established. Also, with softened<br />
gutta-percha obturation techniques there has been a greater<br />
incidence of material extrusion beyond the confines of the<br />
canal. While softening of gutta-percha may be viewed as<br />
routinely desirable, the selective use of this technique solely<br />
or in <strong>com</strong>bination with a solid core of gutta-percha must be<br />
at the discretion of the <strong>com</strong>petent clinician when anatomy<br />
dictates this approach. 76,77<br />
However, closer examination subsequent to filling showed<br />
voids using the single cone technique throughout the length<br />
of the root filled using this technique (Figure 8). The single<br />
cone technique did not produce a monoblock obturation<br />
(Figure 9). The gutta-percha from the GT obturator flowed<br />
into the canal isthmus and filled it (Figure 10).<br />
Figure 8. Voids using single cone technique<br />
Figure 6. Apical constriction of root canal<br />
Figure 9. Cross-section with ActiV GP and GT Series X obturation<br />
Recent research conducted at Nova Southeast University<br />
using micro CT scanning technology has shown the effectiveness<br />
of scanning for imagery and the greater precision<br />
observed <strong>com</strong>pared to standard radiographs. In one example,<br />
a mesiobuccal canal was filled using GT ® Series X<br />
obturator and the mesiolingual canal was filled using a single<br />
cone technique (ActiV GP). It appeared from one angle that<br />
all canals were equally filled (Figure 7).<br />
Figure 7. Radiograph of filled canals<br />
ActiV GP<br />
GT Series X obturator<br />
Figure 10. <strong>Canal</strong> isthmus filled with GT obturator gutta-percha<br />
<strong>Canal</strong> isthmus filled<br />
with GT obturator<br />
gutta-percha<br />
Differences in obturation techniques and results are also<br />
more observable using CT scanning than using traditional<br />
radiographs. 78 Contemporary techniques include the use of<br />
bonded root canal filling materials. Recent developments in<br />
resin-bonding have led to the availability of resin cones and<br />
www.ineedce.<strong>com</strong> 5
pellets similar in shape and size to gutta-percha materials.<br />
Resin-based cones containing methacrylate resin, fillers,<br />
bioactive glass, and polymers are available that can be handled<br />
similarly to gutta-percha and can be used with a lateral<br />
or vertical <strong>com</strong>paction technique. Resin-based materials can<br />
also be delivered via a heated syringe (Obtura gun, Spartan<br />
Obtura). Since resin-based materials require a slightly moist<br />
environment, it is important to avoid using any dessicating<br />
solutions, such as alcohol, during root canal preparation.<br />
Further, if sodium hypochlorite or peroxide was used during<br />
root canal preparation, this must be thoroughly removed<br />
prior to using a resin-based material as it would reduce the<br />
ability of the resin material to bond. Similarly, the smear<br />
layer must also be thoroughly removed.<br />
Prefabricated Obturators<br />
Gutta-percha can also be formed on a plastic carrier or corecarrier.<br />
Prefabricated obturators were first described in 1978<br />
by William Ben Johnson. 79 The prototype for the obturator<br />
had been prenotched K-files wrapped in gutta-percha (hand<br />
formed) that were then heated over a flame until the surface<br />
glistened and expanded. These prenotched “obturators”<br />
were inserted into the canal and apical pressure applied<br />
while the handle was twisted off (Figure 11).<br />
Figure 11. Prototype obturator<br />
Plus, ProTaper ® Universal and ProSystem GT ® Obturators<br />
(Dentsply, Tulsa Dental), and Soft-Core ® (Soft-Core ®<br />
Texas, Inc.).<br />
Figure 12. Calamus®<br />
Current plastic obturators are available in a nonvented shape<br />
with a taper of around 0.04 (Densfil) and a vented shape<br />
with the same taper (Thermafil Plus). Both are biologically<br />
inert. 80 The carrier is thick with a thinner outer coating of<br />
gutta-percha, which helps to reduce material shrinkage as<br />
the gutta-percha cools in the canal (Figure 13). A vented<br />
prefabricated obturator helps the flow of gutta-percha during<br />
placement and also aids in retrieval of the obturator<br />
should retreatment be necessary.<br />
For sizes 40 and below in the Thermafil series, an insoluble<br />
liquid crystal plastic is used. For size 45 and above soluble<br />
polysulfone polymer is used. All of these use a size verifier to<br />
help select the correct size obturator, as do ProTaper Universal<br />
carriers, which start at a .04 taper. Systems that do not use a<br />
size verifier include the ProSystem GT carriers and GT Series<br />
X carriers, which are made in a variety of tapers between 0.04<br />
and 0.12.<br />
Figure 13. Carrier and gutta-percha coating<br />
Prefabricated obturators were introduced in 1988 (Thermafil)<br />
using first a stainless steel and subsequently a titanium<br />
core, coated with gutta-percha. Plastic obturators were first<br />
offered in 1992. Since then, a number of prefabricated obturator<br />
systems have been introduced, including one that does<br />
not involve thermosoftening of the gutta-percha (SimpliFil,<br />
Discus Dental) but instead is used cold with only the apical<br />
area coated in gutta-percha, and after placement the carrier<br />
itself is removed.<br />
A recently developed prefabricated obturator utilizes a<br />
resin-based system (RealSeal One, Sybron Endo) and is<br />
used with, and bonded to, methacrylate resin-based sealer<br />
material and is first held in its custom oven and thermosoftened.<br />
Other systems use thermosoftened gutta-percha,<br />
including Calamus® (Tulsa Dental, Dentsply) (Figure 12),<br />
Successfil® (Hygienic-Coltene-Whaledent, Inc.), Gutta-<br />
Flow ® , System B <strong>Obturation</strong> System, Thermafil, Thermafil<br />
Carrier<br />
gutta-percha<br />
venting<br />
The first case below shows a step-by-step procedure using<br />
GT ® Series X obturation, and the second shows use of the<br />
ProTaper ® Universal obturator.<br />
Case 1. GT® Series X obturation<br />
Following <strong>com</strong>plete shaping and cleaning, the canals should<br />
be thoroughly dried. For the obturator, the size matching the<br />
6 www.ineedce.<strong>com</strong>
last instrument taken to working length should be selected<br />
(Figure 14). It is vital that the calibration rings (measuring<br />
marks) on the carrier are used as opposed to actually measuring<br />
the obturator from the tip. There is more gutta-percha<br />
than plastic carrier at the apical end of the obturator and it<br />
is this gutta-percha that is intended to flow and fill the space<br />
ahead of the plastic.<br />
The plastic core delivers the gutta-percha to the full working<br />
length. If necessary, for shorter canals, excess gutta-percha<br />
should be peeled from the coronal end to facilitate setting of the<br />
working length indicator. Additionally, if BioPure ® MTAD ® is<br />
to be used in the canal space, it must be the last liquid irrigant<br />
in the canal space and should therefore be incorporated after<br />
checking the fit of the size verifiers.<br />
A ProPost ® drill with an eccentric tip can be used to cut the<br />
post channel through the obturator (note that most post drills<br />
cannot efficiently cut a solid core obturator).<br />
Figure 16. Placing sealant with a paper point<br />
Figure 14. Working<br />
length calibration<br />
Figure 15. GT® Series X<br />
obturator oven<br />
Figure 17. Obturator at working length<br />
The obturator is then heated in the GT (or GT® Series<br />
X) obturator oven to ensure even heating of the gutta-percha<br />
and consistent flow of the gutta-percha in the canal (Figure<br />
15). During the heating process, sealer is placed in the canal<br />
space. A non-eugenol sealer is re<strong>com</strong>mended for use with<br />
GT ® Series X obturators, with a thin coat applied using a<br />
paper point (Figure 16). After placing the sealer, excess should<br />
be blotted out with a paper point. It is critical that only a tiny<br />
amount of sealer be used since increasing the amount of sealer<br />
will predispose to material overextension beyond the confines<br />
of the canal. The obturator is then placed in the canal with a<br />
smooth motion until the rubber stopper touches the reference<br />
point on the crown of the tooth, indicating it has reached working<br />
length (Figure 17). It is important not to rotate the obturator<br />
or to push it with excessive force into the canal. Prior to<br />
cutting off the handle, the length and quality of the fill can be<br />
confirmed with a radiograph. The handle of the obturator can<br />
be cut off after several seconds of cooling of the gutta-percha<br />
with a Prepi ® bur, a round bur, an ultrasonic tip, or a Touch<br />
’n Heat instrument. If using a Prepi ® bur, water spray should<br />
not be used as this would needlessly soak the pulp chamber<br />
and any other open canals, thereby creating more work in<br />
cleanup. Allow for the gutta-percha to cool back to a hard<br />
consistency prior to making post space so that the obturator is<br />
not dislodged by the post drill; therefore it is re<strong>com</strong>mended to<br />
wait five minutes after placement before cutting the obturator.<br />
Figure 18. Finished case<br />
Case 2. ProTaper® Universal/Thermafil® obturator<br />
technique<br />
The ProTaper ® and Thermafil ® Plus obturators are a solid<br />
core of plastic covered in a layer of gutta-percha. As in the case<br />
above, thorough drying and cleaning of the canals is required.<br />
In this case, the obturator is selected using the size verifier to<br />
ascertain the size required for a passive fit at working length in<br />
the canal (Figures 19,20). For canals shorter than 18 mm, the<br />
www.ineedce.<strong>com</strong> 7
carrier can be stripped back from 18 and the rubber stopper<br />
repositioned, while for canals longer than 24 mm, the length<br />
can be measured on the handle and part of the handle cut back<br />
(taking care to preserve half of the handle length so that the<br />
obturator can rest on the oven hanger arm). The obturator is<br />
heated using the ProTaper ® Universal obturator oven, which<br />
is designed specifically to guarantee full and uniform guttapercha<br />
heating. A light coating of sealer should be placed to<br />
the full working length of the root canal space, then the heated<br />
obturator is placed in the canal with a smooth motion until the<br />
rubber stopper touches the reference point on the crown of the<br />
tooth, indicating it has reached working length. The obturator<br />
should not be rotated or pushed into the canal with excessive<br />
force. There is adequate time after taking the obturator out of<br />
the oven to methodically place the gutta-percha without rushing.<br />
The length and quality of the fill can be confirmed with<br />
a radiograph prior to cutting off the handle using one of the<br />
techniques described above in Case 1. Post space preparation<br />
can occur after five minutes.<br />
Figure 19. Working length indicators<br />
Figure 20. Size verifier<br />
Figure 21. Finished case<br />
Summary<br />
Appropriate cleaning and shaping of canals and obturation<br />
with an apical and coronal seal are essential for successful<br />
clinical out<strong>com</strong>es in root canal therapy. While gutta-percha<br />
cones, used together with a sealer/cement, may not meet all<br />
criteria for the ideal root filling material, it has withstood the<br />
test of time and is the standard material used for root canal<br />
obturation. Contemporary techniques include the use of<br />
gutta-percha carrier-based obturators as well as thermosoftened<br />
syringed gutta-percha and mechanically softened guttapercha.<br />
Other materials used include resin-based carriers<br />
and sealers. For successful out<strong>com</strong>es, the appropriate use of<br />
the selected materials and techniques, radiographic control<br />
during the different phases of endodontic therapy, and a high<br />
degree of clinical expertise are required.<br />
References<br />
1 Naidorf IJ. Clinical microbiology in endodontics. Dent Clin<br />
North Am. 1974;18:329.<br />
2 Buckley M, Spångberg L. The prevalence and technical quality of<br />
endodontic treatment in an American subpopulation. Oral Surg<br />
Oral Med Oral Pathol Oral Radiol Endod. 1995;79:92.<br />
3 Gutmann JL. Clinical, radiographic, and histologic perspectives<br />
on success and failure in endodontics. Dent Clin North Am.<br />
1992;36:379.<br />
4 Rud J, <strong>An</strong>dreasen JO. A study of failures after endodontic surgery<br />
by radiographic, histologic and stereomicroscopic methods. Int J<br />
Oral Surg. 1972;1:311.<br />
5 Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting<br />
the long-term results of endodontic treatment. J Endod.<br />
1990;16:498.<br />
6 Saunders WP, Saunders EM. Coronal leakage as a cause of<br />
failure in root canal therapy: a review. Endod Dent Traumatol.<br />
1994;10:105.<br />
7 Vire DE. Failure of endodontically treated teeth. J Endod.<br />
1991;17:338.<br />
8 Ray HA, Trope M. Periapical status of endodontically treated<br />
teeth in relation to the technical quality of the root filling and the<br />
coronal restoration. Int Endod J. 1995;28:12-8.<br />
9 Gutmann JL, Dumsha TC, Lovdahl PE. Problem solving in<br />
endodontics. 4th edition, St Louis, 2006, Mosby-Elsevier, Chapter 1.<br />
10 American Association of Endodontists Guide to Clinical<br />
Endodontics, Chicago, 2004.<br />
11 Gutmann JL, Dumsha TC, Lovdahl PE: Problem solving in<br />
endodontics. 4th edition, St Louis, 2006, Mosby-Elsevier, Chapter<br />
8.<br />
12 American Association of Endodontists Guide to Clinical<br />
Endodontics, Chicago, 2004.<br />
13 Khatib ZZ et al. The antimicrobial affect of various endodontic<br />
sealers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.<br />
1990;70:784.<br />
14 Peters LB, Wesselink PR, Moorer WR. The fate and role of<br />
bacteria left in root dentinal tubules. Int Endod J. 1995;28:95.<br />
15 Heling I, Chandler NP. The antimicrobial effect within dentinal<br />
tubules of four root canal sealers. J Endod. 1996;22:257.<br />
16 Baumgartner G et al. Enterococcus faecalis type strain leakage<br />
through root canals filled with gutta-percha/AH Plus or Resilon/<br />
Epiphany. J Endod. 2006;33:45.<br />
17 Lai CC et al. <strong>An</strong>timicrobial activity of four root canal sealers<br />
against endodontic pathogens. Clin Oral Investig. 2001;5:236.<br />
18 Gomes BP et al. In vitro evaluation of the antimicrobial activity of<br />
five root canal sealers. Braz Dent J. 2004;15:30.<br />
19 Al-Gutmann JL. Adaptation of injected thermoplasticized guttapercha<br />
in the absence of the dentinal smear layer. Int Endod J.<br />
1993;26:87.<br />
20 Sen BH, Piskin B, Baran N. The effect of tubular penetration of<br />
root canal sealers on dye microleakage. Int Endod J. 1996;29:23.<br />
21 Oksan T, Aktener BO, Sen BH, Tezel H. The penetration of<br />
8 www.ineedce.<strong>com</strong>
oot canal sealers into dentinal tubules: a scanning electron<br />
microscopic study. Int Endod J. 1993;26:301.<br />
22 Wennberg A, Ørstavik D. Adhesion of root canal sealers to<br />
bovine dentine and gutta-percha. Int Endod J. 1990;23:13.<br />
23 Lee K-W et al. Adhesion of endodontic sealers to dentin and<br />
gutta-percha. J Endod. 2002;28:684.<br />
24 Eldeniz AU, Erdemir A, Belli S. Shear bond strength of three resin<br />
based sealers to dentin with and without smear layer. J Endod.<br />
2005;31:293.<br />
25 Kokkas AB et al. The influence of the smear layer on dentinal<br />
tubule penetration depth by three different root canal sealers: an<br />
in vitro study. J Endod. 2004;30:100.<br />
26 ANSI/ADA specification no. 57 for endodontic filling materials.<br />
J Am Dent Assoc. 1984;108:88.<br />
27 Cobankara FK et al. The quantitative evaluation of apical sealing<br />
of four endodontic sealers. J Endod. 2006;32:66.<br />
28 Facer SR, Walton RE. Intracanal distribution patterns of sealers<br />
after lateral condensation. J Endod. 2003;29:832.<br />
29 Tagger M et al. Interaction between sealers and gutta-percha<br />
cones. J Endod. 2003;29:835.<br />
30 Granche D et al. Endodontic cements induce alterations in the<br />
cell cycle of in vitro cultured osteoblasts. Oral Surg Oral Med<br />
Oral Pathol Oral Radiol Endod. 1995;79:359.<br />
31 Briseno BM, Willerhausen B. <strong>Root</strong> canal sealer cytotoxicity on<br />
human gingival fibroblasts. I. Zinc oxide-eugenol based sealers, J<br />
Endod. 1990;16:383.<br />
32 Brodin P, Røed A, Aars H, Ørstavik D. Neurotoxic effects of<br />
root filling materials on rat phrenic nerve in vitro. J Dent Res.<br />
1982;61:1020.<br />
33 Sonat B, Dalat D, Günhan O. Periapical tissue reaction to root<br />
fillings with Sealapex. Int Endod J. 1990;23:46.<br />
34 Briseno BM, Willerhausen B. <strong>Root</strong> canal sealer cytotoxicity on<br />
human gingival fibroblasts. III. Calcium hydroxide-based sealers.<br />
J Endod. 1992;18:110.<br />
35 Briseno BM, Willerhausen B: <strong>Root</strong> canal sealer cytotoxicity on<br />
human gingival fibroblasts. II. Silicone- and resin-based sealers, J<br />
Endod. 1991;17:537.<br />
36 Schwarze T et al. The cellular <strong>com</strong>patibility of five endodontic<br />
sealers during the setting period. J Endod. 2002;28:784.<br />
37 Layhausen G et al. Genotoxicity and cytotoxicity of the epoxy<br />
resin-based root canal sealer AH plus. J Endod. 1999;25:109.<br />
38 Hensten A, Jacobsen N. Allergic reactions in endodontic practice.<br />
Endod Topics. 2005;12:44.<br />
39 Dahl JE. Toxicity of endodontic filling materials. Endod Topics.<br />
2005;12:39.<br />
40 Huang TH et al. <strong>Root</strong> canal sealers induce cytotoxicity and<br />
necrosis. J Mater Sci Mater Med. 2004;15:767.<br />
41 Gluskin A. Mishaps and serious <strong>com</strong>plications in endodontic<br />
obturation. Endod Topics. 2005;12:52.<br />
42 Ørstavik D. Materials used for root canal obturation: technical,<br />
biological and clinical testing. Endod Topics. 2005;12:25.<br />
43 Langeland K. <strong>Root</strong> canal sealants and pastes. Dent Clin North<br />
Am. 1974;18:309.<br />
44 Holland R, de Souza V. Ability of a new calcium hydroxide root<br />
canal filling material to induce hard tissue formation. J Endod.<br />
1985;11:535.<br />
45 Kontakiotis E, Panopoulos P. pH of root canal sealers containing<br />
calcium hydroxide. Int Endod J. 1996;29:202.<br />
46 Zmener O, Pameijer CH. Clinical and radiographical evaluation<br />
of a resin-based root canal sealer: a 5-year follow-up. J Endod.<br />
2007;33:676-9.<br />
47 Ørstavik D. Materials used for root canal obturation: technical,<br />
biological and clinical testing. Endod Topics. 2005;12:25.<br />
48 Barbosa SV, Burkard DH, Spångberg LSW. Cytotoxic effects of<br />
gutta-percha solvents. J Endod. 1994;20:6.<br />
49 Metzger Z et al. Residual chloroform and plasticity in customized<br />
gutta-percha master cones. J Endod. 1988;14:546.<br />
50 Wong M, Peters DB, Lorton L. Comparison of gutta-percha filling<br />
techniques: three chloroform gutta-percha filling techniques: part<br />
2. J Endod. 1982;8:4.<br />
51 Gutmann JL, Heaton JF. Management of the open (immature)<br />
apex. II. Non-vital teeth. Int Endod J. 1981;14:173.<br />
52 Gutmann JL, Dumsha TC, Lovdahl PE. Problems in root canal<br />
obturation. Problem solving in endodontics. 4th edition, St Louis,<br />
Elsevier-Mosby, 2006.<br />
53 Kaplowitz GJ. Evaluation of gutta-percha solvents. J Endod.<br />
1990;16:539.<br />
54 Haas SB et al. A <strong>com</strong>parison of four root canal filling techniques.<br />
J Endod. 1989;15:596.<br />
55 Keane K, Harrington GW. The use of a chloroform-softened<br />
gutta-percha master cone and its effect on the apical seal. J<br />
Endod. 1984;10:57.<br />
56 McDonald NM, Vire DE. Chloroform in the endodontic<br />
operatory. J Endod. 1992;18:301.<br />
57 Metzger Z et al. Apical seal by customized versus standardized<br />
master cones: a <strong>com</strong>parative study in flat and round canals. J<br />
Endod. 1988;14:381.<br />
58 Friedman CE, Sandrik JL, Heuer MA, Rapp GW. Composition<br />
and mechanical properties of gutta-percha endodontic points. J<br />
Dent Res. 1975;54:921.<br />
59 Moorer WR, Genet JM. <strong>An</strong>tibacterial activity of gutta-percha<br />
cones attributed to the zinc oxide <strong>com</strong>ponent. Oral Surg Oral<br />
Med Oral Pathol Oral Radiol Endod. 1982;53:508.<br />
60 Moorer WR, Genet JM. Evidence for antibacterial activity of<br />
endodontic gutta-percha cones, Oral Surg Oral Med Oral Pathol<br />
Oral Radiol Endod. 1982;53:503.<br />
61 Whitworth J. Methods of filling root canals: principles and<br />
practices. Endod Topics. 2005;12:2.<br />
62 Gutmann JL, Dumsha TC, Lovdahl PE. Problem solving in<br />
endodontics. 4th edition, St Louis, Elsevier-Mosby, 2006.<br />
63 Ibid.<br />
64 Kuttler Y. Microscopic investigation of root apexes. J Am Dent<br />
Assoc. 1955;50(5):544–52.<br />
65 Grove CJ. Why root canals should be filled to the dentinocemental<br />
junction. J Am Dent Assoc. 1930;17:293.<br />
66 Wu M-K, Wesselink PR, Walton RE. Apical terminus location of<br />
root canal treatment procedures. Oral Surg Oral Med Oral Pathol<br />
Oral Radiol Endod. 2000;89:99.<br />
67 Orban B. Why root canals should be filled to the dentinocemental<br />
junction. J Am Dent Assoc. 1930;7:1086.<br />
68 Seltzer S, Bender IB, Turkenkopf S. Factors affecting successful<br />
repair after root canal therapy. J Am Dent Assoc. 1963;67:651.<br />
69 Hasselgren G. Where shall the root filling end? NY State Dent J.<br />
1994;60(6):34.<br />
70 Grahnén H, Hansson L. The prognosis of pulp and root canal<br />
therapy: a clinical and radiographic follow-up examination,<br />
Odontol Revy. 1961;12:146.<br />
71 Seltzer S, Naidorf I. Flare-ups in endodontics. II. Therapeutic<br />
measures. J Endod. 1985;11:559.<br />
72 Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting<br />
the long-term results of endodontic treatment. J Endod.<br />
1990;16:498.<br />
73 Swartz DB, Skidmore AE, Griffin JA. Twenty years of endodontic<br />
success and failure. J Endod. 1983;9:198.<br />
74 Gutmann JL, Leonard JE. Problem solving in endodontic working<br />
length determination. Comp Contin Educ Dent. 1995;16:288.<br />
75 Seltzer S. Endodontology: biologic considerations in endodontic<br />
procedures. 2nd edition, Philadelphia, Lea & Febiger. 1998.<br />
76 Budd CS, Weller RN, Kulild JC. A <strong>com</strong>parison of<br />
thermoplasticized injectable gutta-percha obturation techniques.<br />
J Endod. 1991;17:260.<br />
77 Gutmann JL. Adaptation of injected thermoplasticized guttapercha<br />
in the absence of the dentinal smear layer. Int Endod J.<br />
1993;26:87.<br />
78 Wu MK, Shemesh H, Wesselink PR. Limitations of previously<br />
published systematic reviews evaluating the out<strong>com</strong>e of<br />
endodontic treatment. Int Endod J. 2009;42(8):656-66. Epub<br />
2009 Jun 22.<br />
79 Johnson, WB. A new gutta-percha technique. J Endod.<br />
1978;4(60):184-8.<br />
80 Foong W, Sutow E, Zakariasen K, Hidi P, Jones D. Cytotoxicity<br />
testing of an endodontic obturating device. J Endod. 1993;19<br />
(Abstract 74):202.<br />
Author Profile<br />
The authors of this course, James L. Gutmann, DDS,<br />
Sergio Kuttler, DDS and Stephen P. Niemczyk, DMD,<br />
are all board-certified endodontists.<br />
www.ineedce.<strong>com</strong> 9
Online Completion<br />
Use this page to review the questions and answers. Return to www.ineedce.<strong>com</strong> and sign in. If you have not previously purchased the program select it from the “Online Courses” listing and <strong>com</strong>plete the<br />
online purchase. Once purchased the exam will be added to your Archives page where a Take Exam link will be provided. Click on the “Take Exam” link, <strong>com</strong>plete all the program questions and submit your<br />
answers. <strong>An</strong> immediate grade report will be provided and upon receiving a passing grade your “Verification Form” will be provided immediately for viewing and/or printing. Verification Forms can be viewed<br />
and/or printed anytime in the future by returning to the site, sign in and return to your Archives Page.<br />
Questions<br />
1. The purpose of root canal obturation is<br />
_________.<br />
a. the elimination of all avenues of leakage<br />
b. the introduction of a medicament<br />
c. sealing within the root canal system of any irritants<br />
that remain after appropriate shaping and cleaning<br />
of the canals, thereby isolating these irritants<br />
d. a and c<br />
2. Pulpal demise and subsequent periradicular<br />
infection result from _________.<br />
a. the presence of microorganisms<br />
b. the products of pulp tissue degradation<br />
c. the presence of microbial toxins and metabolites<br />
d. all of the above<br />
3. The ability to achieve three-dimensional<br />
root canal obturation is primarily<br />
dependent on _________.<br />
a. clinical skill<br />
b. the quality of canal cleaning and shaping<br />
c. the material<br />
d. a and b<br />
4. There is reasonable evidence that<br />
_________is a final determinant of success<br />
or failure in treatment.<br />
a. coronal leakage through improperly placed restorations<br />
after root canal treatment<br />
b. failure of the restorative treatment<br />
c. lack of health of the supporting periodontium<br />
d. all of the above<br />
5. _________ should be used in conjunction<br />
with the core filling material to establish<br />
an adequate seal.<br />
a. Maximum amounts of root canal sealers<br />
b. Minimum amounts of root canal sealers<br />
c. Maximum amounts of periodontal sealers<br />
d. none of the above<br />
6. ________ enables standard-of-care canal<br />
obturation.<br />
a. Gutta percha alone<br />
b. Sealer alone<br />
c. Cement alone<br />
d. none of the above<br />
7. A disadvantage of gutta-percha is<br />
_________.<br />
a. its ease of displacement under pressure<br />
b. its lack of rigidity<br />
c. its adhesiveness<br />
d. all of the above<br />
8. To be able to manage the diversity<br />
of anatomical scenarios that may be<br />
encountered, _________.<br />
a. the clinician should <strong>com</strong>pletely master one obturation<br />
technique<br />
b. it is re<strong>com</strong>mended that the clinician master several<br />
obturation techniques<br />
c. scans are required<br />
d. all of the above<br />
9. Use of a sealant is _________.<br />
a. rarely required<br />
b. only required if the obturator is not thermoplastic<br />
c. always required<br />
d. none of the above<br />
10. <strong>Root</strong> canal sealers can _________.<br />
a. enhance the possible attainment of an impervious seal<br />
b. serve as a filler for root canal irregularities<br />
c. assist in microbial control should there be<br />
microorganisms left on the root canal walls or in the<br />
tubules<br />
d. all of the above<br />
11. In canals in which the smear layer has<br />
been removed, _________ to dentin.<br />
a. many sealers demonstrate reduced adhesive<br />
properties<br />
b. many sealers demonstrate increased adhesive<br />
properties<br />
c. no sealers demonstrate adhesive properties<br />
d. none of the above<br />
12. The toxicity of sealers _________.<br />
a. is reduced on setting<br />
b. is increased on setting<br />
c. remains the same on setting<br />
d. none of the above<br />
13. One sealer/cement <strong>com</strong>bination<br />
discussed in the article is _________.<br />
a. zinc oxide eugenol<br />
b. polyketone<br />
c. calcium hydroxide<br />
d. all of the above<br />
14. Epoxy-based and methacrylate-based<br />
resin sealers _________.<br />
a. can be bonded to the root canal dentin<br />
b. can never be bonded to the root canal dentin<br />
c. weaken the root canal dentin<br />
d. none of the above<br />
15. Bonding to gutta-percha can be achieved<br />
using _________.<br />
a. epoxy-based resins<br />
b. methacrylate-based resin sealers<br />
c. glass ionomer-based resin sealers<br />
d. none of the above<br />
16. Gutta-percha as a solid core filling material<br />
for canal obturation _________.<br />
a. demonstrates minimal toxicity<br />
b. demonstrates minimal tissue irritability<br />
c. is the least allergenic material available when<br />
retained within the canal system<br />
d. all of the above<br />
17. _________ is a chemical solvent that has<br />
been used with gutta-percha.<br />
a. Rectified black turpentine<br />
b. Chloroform<br />
c. Water<br />
d. all of the above<br />
18. The use of solvents _________ in daily<br />
practice.<br />
a. may still be considered for a number of challenges<br />
the clinician may face<br />
b. must always be considered<br />
c. should never be considered<br />
d. is no longer a viable treatment<br />
19. The <strong>com</strong>position of gutta-percha cones is<br />
approximately _________ and _________.<br />
a. 19% to 32% Balata; 59% to 85% zinc oxide<br />
b. 19% to 32% zinc oxide; 59% to 85% Balata<br />
c. 19% to 22% Balata; 59% to 75% zinc oxide<br />
d. none of the above<br />
20. With the development of more predictable<br />
root canal shapes prepared with<br />
current nickel titanium (NiTi) rotary and<br />
hand instruments, cones tapered from<br />
_________ have gained use.<br />
a. 1% – 3%<br />
b. 2% – 4%<br />
c. 4% – 8%<br />
d. 4% – 10%<br />
21. Basic techniques for the obturation of<br />
the root canal system with gutta-percha<br />
and sealer include _________.<br />
a. cold <strong>com</strong>paction or heat-softened <strong>com</strong>paction using<br />
cold instruments<br />
b. <strong>com</strong>paction of gutta-percha that has been<br />
thermoplasticized, injected into the system, and<br />
<strong>com</strong>pacted with cold instruments<br />
c. <strong>com</strong>paction of gutta-percha that has first been<br />
placed in the canal and then softened<br />
d. all of the above<br />
22. While softening of gutta-percha may be<br />
viewed as _________, the selective use of<br />
this technique solely or in <strong>com</strong>bination<br />
with a solid core of gutta-percha must<br />
be at the discretion of the <strong>com</strong>petent<br />
clinician.<br />
a. rarely desirable<br />
b. routinely desirable<br />
c. never desirable<br />
d. none of the above<br />
23. Resin-based cones are available that can<br />
be used with a _________.<br />
a. lateral <strong>com</strong>paction technique only<br />
b. vertical <strong>com</strong>paction technique only<br />
c. diagonally-positioned <strong>com</strong>paction technique only<br />
d. vertical or lateral <strong>com</strong>paction technique<br />
24. It is important to avoid using any<br />
dessicating solutions, such as _________,<br />
during root canal preparation if using<br />
resin-based obturating materials.<br />
a. water<br />
b. eugenol<br />
c. alcohol<br />
d. b and c<br />
25. Prefabricated obturators were first<br />
described in 1978 by _________.<br />
a. William Ben Thompson<br />
b. Ben William Thompson<br />
c. William Ben Johnson<br />
d. Ben William Johnson<br />
26. _________ are currently available.<br />
a. Gutta-percha-based and resin-based prefabricated<br />
obturators<br />
b. Gutta-percha-based and cement-based prefabricated<br />
obturators<br />
c. Gutta-percha-based and sealer-based prefabricated<br />
obturators<br />
d. all of the above<br />
27. Current tapered plastic obturators are<br />
available in _________ shapes.<br />
a. nonvented<br />
b. vented<br />
c. helical<br />
d. a and b<br />
28. A vented prefabricated obturator<br />
_________.<br />
a. helps the flow of gutta-percha during placement<br />
b. helps the flow of gutta-percha after placement<br />
c. aids in retrieval of the obturator should retreatment<br />
be necessary<br />
d. a and c<br />
29. With a gutta-percha-based prefabricated<br />
carrier, if BioPure ® MTAD ® is to be<br />
used in the canal space, it should be the<br />
_________ liquid irrigant used in the canal<br />
space prior to checking the fit of the size<br />
verifiers.<br />
a. first<br />
b. intermediate<br />
c. last<br />
d. none of the above<br />
30. _________ control during the different<br />
phases of endodontic therapy is required.<br />
a. Digital<br />
b. Radiographic<br />
c. Ergometric<br />
d. all of the above<br />
10 www.ineedce.<strong>com</strong>
ANSWER SHEET<br />
<strong>Root</strong> <strong>Canal</strong> <strong>Obturation</strong>: <strong>An</strong> <strong>Update</strong><br />
Name: Title: Specialty:<br />
Address:<br />
E-mail:<br />
City: State: ZIP: Country:<br />
Telephone: Home ( ) ( ) Lic. Renewal Date:<br />
Requirements for successful <strong>com</strong>pletion of the course and to obtain dental continuing education credits: 1) Read the entire course. 2) Complete all<br />
information above. 3) Complete answer sheets in either pen or pencil. 4) Mark only one answer for each question. 5) A score of 70% on this test will earn<br />
you 2 CE credits. 6) Complete the Course Evaluation below. For Questions call 216.398.7822<br />
Educational Objectives<br />
1. List the purposes of root canal obturation<br />
2. List the characteristics of gutta-percha used for obturation<br />
3. List and describe the contemporary materials and techniques for obturating root canals<br />
4. List the most widely-used techniques for gutta-percha carrier-based obturation and describe its strengths and<br />
short<strong>com</strong>ings.<br />
Course Evaluation<br />
Please evaluate this course by responding to the following statements, using a scale of Excellent = 5 to Poor = 0.<br />
If not taking online, mail <strong>com</strong>pleted answer sheet to<br />
Academy of Dental Therapeutics and Stomatology,<br />
A Division of PennWell Corp.<br />
P.O. Box 116, Chesterland, OH 44026<br />
or fax to: (440) 845-3447<br />
For IMMEDIATE results,<br />
go to www.ineedce.<strong>com</strong> to take tests online.<br />
<strong>An</strong>swer sheets can be faxed to<br />
(440) 845-3447, (216) 398-7922, or (216) 255-6619.<br />
1. Were the individual course objectives met? Objective #1: Yes No Objective #3: Yes No<br />
Objective #2: Yes No Objective #4: Yes No<br />
2. To what extent were the course objectives ac<strong>com</strong>plished overall? 5 4 3 2 1 0<br />
3. Please rate your personal mastery of the course objectives. 5 4 3 2 1 0<br />
4. How would you rate the objectives and educational methods? 5 4 3 2 1 0<br />
5. How do you rate the author’s grasp of the topic? 5 4 3 2 1 0<br />
5 4 3 2 1 0<br />
5 4 3 2 1 0<br />
8. Do you feel that the references were adequate? Yes No<br />
Yes<br />
No<br />
10. If any of the continuing education questions were unclear or ambiguous, please list them.<br />
___________________________________________________________________<br />
11. Was there any subject matter you found confusing? Please describe.<br />
___________________________________________________________________<br />
___________________________________________________________________<br />
12. What additional continuing dental education topics would you like to see?<br />
___________________________________________________________________<br />
___________________________________________________________________<br />
AGD Code 074<br />
PLEASE PHOTOCOPY ANSWER SHEET FOR ADDITIONAL PARTICIPANTS.<br />
COURSE EVALUATION and PARTICIPANT FEEDBACK<br />
We encourage participant feedback pertaining to all courses. Please be sure to <strong>com</strong>plete the survey included with<br />
the course. Please e-mail all questions to: Jim.Gray@dentsply.<strong>com</strong>. Please direct all questions pertaining to the<br />
administration of this course to Jim.Gray@dentsply.<strong>com</strong>.<br />
INSTRUCTIONS<br />
All questions should have only one answer. Grading of this examination is done manually. Participants will receive<br />
taking an examination.<br />
EDUCATIONAL DISCLAIMER<br />
herein are those of the author(s) of the course.<br />
Completing a single continuing education course does not provide enough information to give the participant the<br />
and clinical experience that allows the participant to develop skills and expertise.<br />
COURSE CREDITS/COST<br />
All participants scoring at least 70% (answering 21 or more questions correctly) on the examination will receive<br />
2<br />
the AGD for Fellowship/Mastership credit. Participants are urged to contact their state dental boards for continuing<br />
education requirements.<br />
RECORD KEEPING<br />
PennWell will maintain records of your successful <strong>com</strong>pletion of this exam.<br />
© 2010 by the Academy of Dental Therapeutics and Stomatology, a division of PennWell<br />
www.ineedce.<strong>com</strong> Customer Service 216.398.7822 11