Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Occasionally, the colonic adeno<strong>carcinoma</strong><br />
is found several months to years after<br />
resection of the ovarian metastases.<br />
Rectal or sigmoid colon cancer accounts<br />
for 75% of the metastatic colon tumours<br />
to the ovary {1587,2605,3226}. The primary<br />
tumour can also be located in the<br />
pancreas, biliary tract or the appendix<br />
{590,1848,2406,3199,3200}.<br />
The Krukenberg tumour is almost always<br />
secondary to a gastric <strong>carcinoma</strong> but<br />
may occasionally originate in the intestine,<br />
appendix, <strong>breast</strong> or other sites<br />
{367,2605,3226}. Rarely, <strong>breast</strong> cancer<br />
metastatic to the ovary presents clinically<br />
as an ovarian mass. A much higher<br />
percentage of cases of lobular <strong>carcinoma</strong><br />
of the <strong>breast</strong>, including those of<br />
signet-ring cell type, metastasizes to the<br />
o v a ry than does ductal carc i n o m a<br />
{1142}. A wide variety of other tumours<br />
may metastasize to the ovary.<br />
Histopathology<br />
The identification of surface implants,<br />
multinodularity and intravascular tumour<br />
emboli are extremely helpful histological<br />
clues in the recognition of secondary<br />
ovarian tumours that spread through the<br />
abdominal cavity and tubal lumen. The<br />
histological appearance of the metastases<br />
is variable, depending on the<br />
nature of the primary tumour.<br />
Differential diagnosis<br />
Sometimes, metastases resemble primary<br />
ovarian tumours {2605,2980,3226}.<br />
Metastatic colonic adeno<strong>carcinoma</strong> to<br />
the ovary may be confused with primary<br />
endometrioid or mucinous carc i n o m a<br />
depending on whether the colonic <strong>carcinoma</strong><br />
is predominantly mucinous or nonmucinous.<br />
Features that help to distinguish<br />
colon cancer from endometrioid<br />
c a rcinoma include luminal necro t i c<br />
debris, focal segmental necrosis of the<br />
glands, occasional presence of goblet<br />
cells and the absence of müllerian features<br />
(squamous differentiation, an adenofibromatous<br />
component or association<br />
with endometriosis). Also the nuclei lining<br />
the glands of metastatic colon <strong>carcinoma</strong><br />
exhibit a higher degree of atypia than<br />
those of endometrioid <strong>carcinoma</strong>.<br />
Metastatic tumours may also closely<br />
resemble primary mucinous ovarian<br />
tumours. The former may be moderately<br />
differentiated or so well differentiated that<br />
they can be mistaken for mucinous borderline<br />
or less often benign ovarian<br />
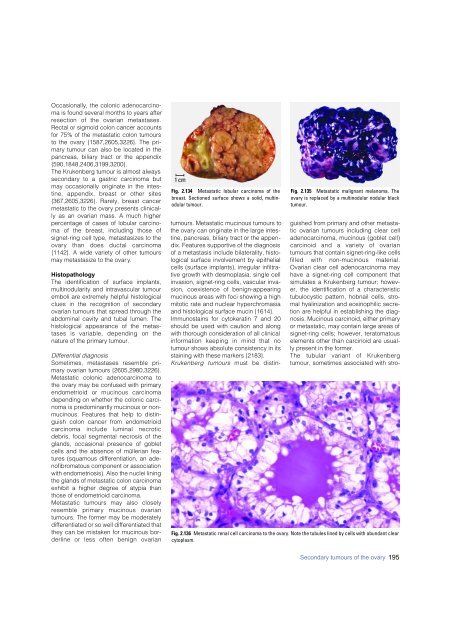
Fig. 2.134 Metastatic lobular <strong>carcinoma</strong> of the<br />
<strong>breast</strong>. Sectioned surface shows a solid, multinodular<br />
tumour.<br />
Fig. 2.135 Metastatic malignant melanoma. The<br />
ovary is replaced by a multinodular nodular black<br />
tumour.<br />
tumours. Metastatic mucinous tumours to<br />
the ovary can originate in the large intestine,<br />
pancreas, biliary tract or the appendix.<br />
Features supportive of the diagnosis<br />
of a metastasis include bilaterality, histological<br />
surface involvement by epithelial<br />
cells (surface implants), irregular infiltrative<br />
growth with desmoplasia, single cell<br />
invasion, signet-ring cells, vascular invasion,<br />
coexistence of benign-appearing<br />
mucinous areas with foci showing a high<br />
mitotic rate and nuclear hyperchromasia<br />
and histological surface mucin {1614}.<br />
Immunostains for cytokeratin 7 and 20<br />
should be used with caution and along<br />
with thorough consideration of all clinical<br />
i n f o rmation keeping in mind that no<br />
tumour shows absolute consistency in its<br />
staining with these markers {2183}.<br />
Krukenberg tumours must be distinguished<br />
from primary and other metastatic<br />
ovarian tumours including clear cell<br />
adeno<strong>carcinoma</strong>, mucinous (goblet cell)<br />
c a rcinoid and a variety of ovarian<br />
tumours that contain signet-ring-like cells<br />
filled with non-mucinous material.<br />
Ovarian clear cell adeno<strong>carcinoma</strong> may<br />
have a signet-ring cell component that<br />
simulates a Krukenberg tumour; however,<br />
the identification of a characteristic<br />
tubulocystic pattern, hobnail cells, stromal<br />
hyalinization and eosinophilic secretion<br />
are helpful in establishing the diagnosis.<br />
Mucinous carcinoid, either primary<br />
or metastatic, may contain large areas of<br />
signet-ring cells; however, teratomatous<br />
elements other than carcinoid are usually<br />
present in the former.<br />
The tubular variant of Krukenberg<br />
tumour, sometimes associated with stro-<br />
Fig. 2.136 Metastatic renal cell <strong>carcinoma</strong> to the ovary. Note the tubules lined by cells with abundant clear<br />
cytoplasm.<br />
Secondary tumours of the ovary 195