Postoperative pain after abdominal hysterectomy: a ... - BJA
Postoperative pain after abdominal hysterectomy: a ... - BJA
Postoperative pain after abdominal hysterectomy: a ... - BJA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
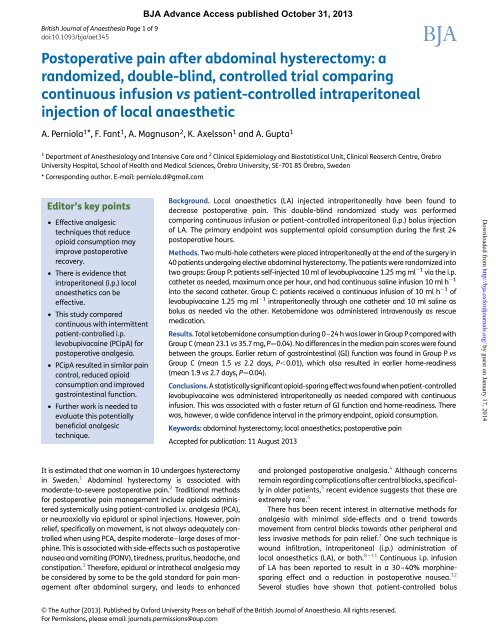
British Journal of Anaesthesia Page 1 of 9<br />
doi:10.1093/bja/aet345<br />
<strong>BJA</strong> Advance Access published October 31, 2013<br />
<strong>Postoperative</strong> <strong>pain</strong> <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong>: a<br />
randomized, double-blind, controlled trial comparing<br />
continuous infusion vs patient-controlled intraperitoneal<br />
injection of local anaesthetic<br />
A. Perniola 1 *,F.Fant 1 , A. Magnuson 2 , K. Axelsson 1 and A. Gupta 1<br />
1 Department of Anesthesiology and Intensive Care and 2 Clinical Epidemiology and Biostatistical Unit, Clinical Reaserch Centre, Örebro<br />
University Hospital, School of Health and Medical Sciences, Örebro University, SE-701 85 Örebro, Sweden<br />
* Corresponding author. E-mail: perniola.d@gmail.com<br />
Editor’s key points<br />
† Effective analgesic<br />
techniques that reduce<br />
opioid consumption may<br />
improve postoperative<br />
recovery.<br />
† There is evidence that<br />
intraperitoneal (i.p.) local<br />
anaesthetics can be<br />
effective.<br />
† This study compared<br />
continuous with intermittent<br />
patient-controlled i.p.<br />
levobupivacaine (PCipA) for<br />
postoperative analgesia.<br />
† PCipA resulted in similar <strong>pain</strong><br />
control, reduced opioid<br />
consumption and improved<br />
gastrointestinal function.<br />
† Further work is needed to<br />
evaluate this potentially<br />
beneficial analgesic<br />
technique.<br />
Background. Local anaesthetics (LA) injected intraperitoneally have been found to<br />
decrease postoperative <strong>pain</strong>. This double-blind randomized study was performed<br />
comparing continuous infusion or patient-controlled intraperitoneal (i.p.) bolus injection<br />
of LA. The primary endpoint was supplemental opioid consumption during the first 24<br />
postoperative hours.<br />
Methods. Two multi-hole catheters were placed intraperitoneally at the end of the surgery in<br />
40 patients undergoing elective <strong>abdominal</strong> <strong>hysterectomy</strong>. The patients were randomized into<br />
two groups: Group P: patients self-injected 10 ml of levobupivacaine 1.25 mg ml 21 via the i.p.<br />
catheter as needed, maximum once per hour, and had continuous saline infusion 10 ml h 21<br />
into the second catheter. Group C: patients received a continuous infusion of 10 ml h 21 of<br />
levobupivacaine 1.25 mg ml 21 intraperitoneally through one catheter and 10 ml saline as<br />
bolus as needed via the other. Ketobemidone was administered intravenously as rescue<br />
medication.<br />
Results. Total ketobemidone consumption during 0–24 h was lower in Group P compared with<br />
Group C (mean 23.1 vs 35.7 mg, P¼0.04). No differences in the median <strong>pain</strong> scores were found<br />
between the groups. Earlier return of gastrointestinal (GI) function was found in Group P vs<br />
Group C (mean 1.5 vs 2.2 days, P,0.01), which also resulted in earlier home-readiness<br />
(mean 1.9 vs 2.7 days, P¼0.04).<br />
Conclusions. A statisticallysignificantopioid-sparingeffectwasfoundwhen patient-controlled<br />
levobupivacaine was administered intraperitoneally as needed compared with continuous<br />
infusion. This was associated with a faster return of GI function and home-readiness. There<br />
was, however, a wide confidence interval in the primary endpoint, opioid consumption.<br />
Keywords: <strong>abdominal</strong> <strong>hysterectomy</strong>; local anaesthetics; postoperative <strong>pain</strong><br />
Accepted for publication: 11 August 2013<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
It is estimated that one woman in 10 undergoes <strong>hysterectomy</strong><br />
in Sweden. 1 Abdominal <strong>hysterectomy</strong> is associated with<br />
moderate-to-severe postoperative <strong>pain</strong>. 2 Traditional methods<br />
for postoperative <strong>pain</strong> management include opioids administered<br />
systemically using patient-controlled i.v. analgesia (PCA),<br />
or neuroaxially via epidural or spinal injections. However, <strong>pain</strong><br />
relief, specifically on movement, is not always adequately controlled<br />
when using PCA, despite moderate–large doses of morphine.<br />
This is associated with side-effects such as postoperative<br />
nausea and vomiting (PONV), tiredness, pruritus, headache, and<br />
constipation. 3 Therefore, epidural or intrathecal analgesia may<br />
be considered by some to be the gold standard for <strong>pain</strong> management<br />
<strong>after</strong> <strong>abdominal</strong> surgery, and leads to enhanced<br />
and prolonged postoperative analgesia. 4 Although concerns<br />
remain regarding complications <strong>after</strong>central blocks, specifically<br />
in older patients, 5 recent evidence suggests that these are<br />
extremely rare. 6<br />
There has been recent interest in alternative methods for<br />
analgesia with minimal side-effects and a trend towards<br />
movement from central blocks towards other peripheral and<br />
less invasive methods for <strong>pain</strong> relief. 7 One such technique is<br />
wound infiltration, intraperitoneal (i.p.) administration of<br />
local anaesthetics (LA), or both. 8 – 11 Continuous i.p. infusion<br />
of LA has been reported to result in a 30–40% morphinesparing<br />
effect and a reduction in postoperative nausea. 12<br />
Several studies have shown that patient-controlled bolus<br />
& The Author [2013]. Published by Oxford University Press on behalf of the British Journal of Anaesthesia. All rights reserved.<br />
For Permissions, please email: journals.permissions@oup.com
<strong>BJA</strong><br />
Perniola et al.<br />
administration of LA during neuraxial or peripheral nerve block<br />
gives better postoperative analgesia compared with continuous<br />
infusions. 13 – 17 Therefore, we decided to test the hypothesis<br />
that patient-controlled i.p. analgesia (PCipA) with LA<br />
would reduce <strong>pain</strong> intensity and thereby supplemental opioid<br />
consumption compared with continuous infusion of LA.<br />
The primary aim was therefore to analyse rescue analgesic<br />
consumption during 0–24 h <strong>after</strong> operation <strong>after</strong> <strong>abdominal</strong><br />
<strong>hysterectomy</strong> in patients receiving continuous LA infusion<br />
compared with intermittent patient-controlled i.p. injections.<br />
The secondary outcomes were analgesic consumption during<br />
0–4 h, <strong>pain</strong> intensity, incidence of nausea and vomiting,<br />
maximum expiratory pressure, time to mobilization, and<br />
length of hospital stay, and also health-related quality of life<br />
at 1 and 3 months.<br />
Methods<br />
This study was registered in an international registry, clinicaltrials.gov<br />
(identification number NCT01492075) before<br />
patient recruitment. The study was performed at the Department<br />
of Anaesthesiology and Intensive Care and the Department<br />
of Gynaecological Surgery, University Hospital, Örebro,<br />
Sweden, and monitored by an external organization not<br />
involved in any way with the study. This unit is a quality-based<br />
organization located within the hospital and initiates and<br />
monitors clinical trials. After approval from the Regional<br />
Ethics Committee, Uppsala, oral and written informed<br />
consent was obtained from 40 patients (ASA status I–II),<br />
aged 40–65 yr undergoing elective <strong>abdominal</strong> <strong>hysterectomy</strong><br />
with or without salpingo-oophorectomy in this randomized,<br />
double-blind study. The exclusion criteriawere: patients undergoing<br />
surgery for suspected gynaecological cancer, patients on<br />
chronic analgesic medication, those with known allergy to LA,<br />
patients participating in another clinical study, and those who<br />
had difficulty in understanding Swedish.<br />
Randomization and blinding<br />
On the day of surgery, the Hospital Pharmacy randomized<br />
patients into two groups (20 in each group) using computergenerated<br />
randomized numbers inserted into sealed opaque<br />
envelopes and marked 1–40. All personnel involved in<br />
patient management were fully blinded to the method of analgesia<br />
until the study was completed.<br />
Anaesthesia and surgery<br />
All patients were premedicated with midazolam 0.1 mg kg 21<br />
orally and paracetamol 1 g was given orally every 6 h with<br />
the first dose at the time of premedication. Anaesthesia was<br />
induced with fentanyl 1–2 mg kg 21 and propofol 1–2 mg<br />
kg 21 intravenously. Tracheal intubation was performed <strong>after</strong><br />
muscle relaxation with rocuronium 0.5 mg kg 21 and anaesthesia<br />
was subsequently maintained with sevoflurane 1–3% and<br />
oxygen 33% in air. End-tidal CO 2 was maintained between 4.5<br />
and 5.5 kPa using mechanical ventilation in a low-flow breathing<br />
system with CO 2 absorber. Monitoring included non-invasive<br />
arterial pressure, heart rate, peripheral oxygen saturation,<br />
Page 2 of 9<br />
end-tidal gas monitoring, ECG, and muscle relaxation using<br />
the train-of-four stimulation. Sevoflurane concentration was<br />
adjusted in order to maintain adequate anaesthetic depth,<br />
assessed clinically, and fentanyl was given intermittently intravenously<br />
when required for analgesia during the operation.<br />
Muscle relaxation was reversed at the end of surgery using glycopyrrolate<br />
(0.5 mg) and neostigmine (2.5 mg). Hysterectomy<br />
was performed using either a lower-<strong>abdominal</strong> midline incision<br />
or a Pfannenstiel incision, depending on the choice of<br />
the operator taking into consideration the size of the uterus<br />
and expected surgical difficulty.<br />
Catheter insertion and postoperative <strong>pain</strong><br />
management<br />
Before closing the peritoneum, two multi-hole catheters were<br />
inserted percutaneously by the surgeon; one catheter was tunnelled<br />
from the left side and the other from the right side, about<br />
1–2 cm lateral to the <strong>abdominal</strong> incision and the tip of the<br />
catheters was placed supravaginally as described previously. 2<br />
The catheters were not fixed intraperitoneally. In all patients,<br />
levobupivacaine 1.25 mg ml 21 (20 ml) was injected subcutaneously<br />
along both sides of the incision before skin closure by the<br />
surgeon; an additional 20 ml was injected via one of the cathetersintothe<br />
peritoneal cavity. The pharmacysent (i) oneblinded<br />
bag, containing 500 ml of levobupivacaine 1.25 mg ml 21 or<br />
placebo (normal saline) and (ii) one elastomeric pump (On-Q<br />
Pain BusterR, ref PS125071; I-Flow Corp., Lake Forest, CA, USA)<br />
containing 500 ml of levobupivacaine 1.25 mg ml 21 or placebo<br />
(normalsaline).Whenthepatientarrivedinthepost-anaesthesia<br />
care unit (PACU), the infusions were set up, connected, and<br />
started by one of the co-authors immediately as described<br />
below. The time of start of infusion was considered t¼0.<br />
Group P: PCipAwith LA. The patients self-administered 10 ml<br />
of levobupivacaine via the first i.p catheter as required<br />
(maximum once per hour) during the first 48 h <strong>after</strong> the<br />
operation via an electronic pump (Abbot GemStar, Abbot<br />
Laboratories, North Chicago, IL, USA) over 10 min. Normal<br />
saline was infused at 10 ml h 21 via the second i.p catheter<br />
using the elastomeric pump.<br />
Group C: continuous i.p. infusion of LA. Patients received a<br />
continuous infusion of levobupivacaine 10 ml h 21 intraperitoneally<br />
through the first catheter via the elastomeric pump<br />
and saline as bolus injection via the second i.p. catheter<br />
using the electronic pump. After 48 h, the i.p. bolus/infusion<br />
was stopped and both catheters were removed.<br />
Rescue medication and postoperative ward<br />
All patients received 2–4 mg ketobemidone intravenously, an<br />
opioid analgesic equipotent with morphine, 18 intermittently<br />
by the staff nurse if <strong>pain</strong> was .3 on the numerical rating<br />
scale (NRS) (0, no <strong>pain</strong>; 10, worst imaginable <strong>pain</strong>). Analgesics<br />
were administered on patient request, irrespective of whether<br />
the <strong>pain</strong> was .3 at rest, on sitting, or during coughing. The<br />
patients were observed in the PACU until the day <strong>after</strong> the<br />
surgery. In the case of severe postoperative nausea or vomiting<br />
(PONV) not relieved by anti-emetics, the nursing staff were<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014
Intraperitoneal local anaesthetics for <strong>pain</strong> relief <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong><br />
<strong>BJA</strong><br />
allowed to administer non-steroidal anti-inflammatory drugs<br />
(NSAIDs) for <strong>pain</strong> management in order to reduce opioid-induced<br />
PONV.<br />
Recording and measurements<br />
In addition to the routine postoperative protocols, the following<br />
parameters were recorded:<br />
Pain and analgesia: <strong>pain</strong> at the site of the incision, ‘deep’<br />
(visceral) <strong>pain</strong>, and <strong>pain</strong> on coughing at 1, 4, 12, 24, and<br />
48 h were measured using NRS. Rescue analgesic (ketobemidone)<br />
consumption was measured during 0–4, 0–24, and<br />
24–48 h.<br />
Side-effects: nausea, vomiting, or both (0–4, 4–24, and<br />
24–48 h) were recorded on a yes/no score; anti-emetic<br />
consumption during 0–24 and 24–48 h was also recorded.<br />
Sedation (before operation, at 4, 24, and 48 h) was recorded<br />
by nurses using a 0–10 scale (0, awake; 10, verbally arousable).<br />
Expiratory muscle function: this was measured before and<br />
24 and 48 h <strong>after</strong> the operation using maximum expiratory<br />
pressure (P Emax ) (MicroMedical, Moreton-in-Marsh, UK), in a<br />
similar way as described in previous studies. 2 10 12 P Emax<br />
was measured twice by asking the patient to blow rapidly<br />
using the full <strong>abdominal</strong> force <strong>after</strong> a maximal inspiration<br />
while in the semi-reclining position. The best of two measurements<br />
was recorded.<br />
Recovery parameters: the ability to walk with and without<br />
support, time to start drinking, eating, and time to return<br />
of gastrointestinal (GI) function (bowel movement or<br />
passing flatus), postoperative home-readiness, and length<br />
of hospital stay were recorded once a day by nurses in the gynaecological<br />
ward. Standardized home-readiness criteria<br />
were used that have been described previously. 212<br />
LA toxicity: the nurses were informed about the common<br />
signs and symptoms of LA toxicity and the patients told to<br />
inform the nurses of any side-effects and symptoms.<br />
Health-related quality of life: this was measured using the<br />
written form of SF-36 questionnaire before and 1 and 3<br />
months <strong>after</strong> the operation in both groups and the patients<br />
were asked to return it by post. The SF-36 is a validated<br />
health survey consisting of 36 questions that measure<br />
eight health concepts and has been translated and validated<br />
into the Swedish language. 212 A higher score indicates<br />
an improved level of function.<br />
Statistics<br />
In a previous study, 2 the mean [standard deviation (SD)] total<br />
morphine consumption during 0–24 h was found to be<br />
30 mg (SD 17) in patients receiving continuous i.p. LA. Our<br />
hypothesis was that this could be reduced by 50% to a mean<br />
value of 15 mg (SD 8) in patients receiving PCipA with LA.<br />
The sample size was calculated using the unpaired twosided<br />
t-test. Assuming b¼0.2 (power 80%) and a¼0.05, we<br />
determined that we would require 28 patients (14 per group)<br />
in order to achieve statistical significance for the primary endpoint.<br />
We recruited 40 patients in order to achieve adequate<br />
power in the case of missing data or patient drop out.<br />
The mean and SD are used to summarize continuous variables,<br />
while categorical variables are presented as numbers<br />
(%). Unpaired t-test with 95% confidence intervals (CIs) and<br />
P-values was used to analyse differences between study<br />
groups for morphine consumption and other continuous variables<br />
distributed approximately normally with or without log<br />
transformation. The Shapiro–Wilk test was used to evaluate<br />
normal distribution and if non-normality was found, logtransformation<br />
was performed before statistical evaluation.<br />
The results were then transformed back to original scale and<br />
the effect parameter is therefore the ratio of geometric<br />
means. The results are presented as the mean ratios together<br />
with 95% CI. Owing to multiple comparisons when evaluating<br />
the primary endpoint, 0–24 h ketobemidone consumption, the<br />
Bonferroni–Holm 19 correction was applied. The x 2 test or<br />
Fisher’s exact test when appropriate was used for categorical<br />
variables and odds ratio (OR) with normal approximated 95%<br />
CI was calculated. Owing to some missing values, a mixed<br />
model with autoregressive covariance structure was used to<br />
analyse <strong>pain</strong> on incision, deep <strong>pain</strong>, and <strong>pain</strong> on coughing,<br />
and also for assessment of sedation, P Emax , and when analysing<br />
dimensions of SF-36. Study groups and time points were<br />
fixed effects and patients were random effect in this mixed<br />
model. None of the mixed models used found an overall<br />
statistically significant difference between study groups. The<br />
estimated marginal mean differences between groups at different<br />
time-points with 95% CI and P-values are presented.<br />
When normality assumption was not valid, and log transformation<br />
did not help, sensitivity analysis was performed using the<br />
Mann–Whitney U-test, but because no different conclusions<br />
could be made from the analyses, these results are not presented.<br />
Two-tailed P-value of ,0.05 was considered to be statistically<br />
significant. All statistical analyses were performed<br />
using the SPSS version 17 (Chicago, IL, USA).<br />
Results<br />
Of the 40 patients initially randomized into the study, no<br />
patient was excluded and all patients completed the study<br />
(Fig. 1). The patient characteristic data in the two groups, the<br />
operation performed, and intraoperative fentanyl consumption<br />
are shown in Table 1.<br />
The rescue analgesic ketobemidone consumption was<br />
statistically significantly greater in Group C compared with<br />
Group P during 0–24 h and during 0–4 h <strong>after</strong> operation<br />
(Table 2). No significant difference in ketobemidone consumption<br />
was seen between the groups during the time period<br />
24–48 h. The number of patients given NSAID as rescue medication<br />
during 0–24 h did not differ significantly between the<br />
groups (Table 2).<br />
The intensity of postoperative <strong>pain</strong> on the NRS is shown in<br />
Figure 2A–C. In general, the median <strong>pain</strong> scores were ,5 in<br />
all groups, except during coughing when the median scores<br />
reached ≏7 in the early postoperative period. No significant<br />
differences were seen between the groups in NRS <strong>pain</strong> score<br />
at any time point during the 48 h study period.<br />
Page 3 of 9<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014
<strong>BJA</strong><br />
Perniola et al.<br />
Total number of patients operated during the study time period:<br />
150 patients<br />
Did not fulfil inclusion<br />
criteria or had one of the<br />
exclusion criteria: 75 patients<br />
Number of patients interviewed<br />
for possible inclusion in the<br />
study: 75 patients<br />
Group P<br />
(Patient-controlled i.p. analgesia):<br />
20 patients<br />
Number randomized into the study:<br />
40 patients<br />
Patients included for primary endpoint:<br />
20 patients<br />
Patients excluded due to missing data for<br />
secondary endpoints in 1–3 patients*<br />
Fig 1 Flow diagram of screened, excluded, and recruited patients. *See Tables for details.<br />
• Refused to participate<br />
• Not able to understand study<br />
protocol because of language limitation:<br />
35 patients<br />
Group C<br />
(Continuous i.p. infusion):<br />
20 patients<br />
Patients included for primary endpoint:<br />
20 patients<br />
Patients excluded due to missing data for<br />
secondary endpoints in 1–3 patients*<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
The total volume of levobupivacaine administered <strong>after</strong> the<br />
first 24 postoperative hours was statistically significantly lower<br />
in Group P (180 ml) than in Group C (240 ml) (P,0.01).<br />
The recovery times and time to home-readiness are shown<br />
in Table 3. A statistically significant difference between the<br />
groups was found in the return of GI function, which was<br />
shorter in Group P compared with Group C. The mean time to<br />
home-readiness was statistically significantly shorter in<br />
Group P compared with Group C, while the length of hospital<br />
stay did not differ significantly between the groups. Expiratory<br />
muscle function, measured as maximum expiratory pressure<br />
(P Emax ), decreased at 4 h compared with preoperative values<br />
in both groups, and gradually recovered over time during<br />
48 h. However, no statistically significant differences were<br />
found between the groups at any time point (Table 3). The incidence<br />
of PONV and the number of patients who received<br />
anti-emetics did not differ between the groups. The sedation<br />
scores between the groups were similar (Table 4) and no differences<br />
were seen between the groups in any of the parameters<br />
of the health-related quality of life (SF-36), or the average score<br />
in SF-36 at 1 or 3 months <strong>after</strong> surgery (Fig. 3).<br />
Discussion<br />
In this study, we found a statistically significant opioid-sparing<br />
effect when patients self-administered bolus doses of levobupivacaine<br />
compared with those having acontinuous infusion of<br />
LA. Furthermore, there was a faster return of GI function and a<br />
Page 4 of 9
Intraperitoneal local anaesthetics for <strong>pain</strong> relief <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong><br />
<strong>BJA</strong><br />
shorter time to home-readiness when intermittent injection of<br />
LA was used.<br />
Pain <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong> arises from several<br />
structures that are traumatized during surgery 8 and includes<br />
somatic <strong>pain</strong> from the incision site, and <strong>pain</strong> from deeper structures<br />
including muscle <strong>pain</strong> and peritoneal and visceral <strong>pain</strong>.<br />
Although the magnitude of <strong>pain</strong> from each component is difficult<br />
to define, <strong>pain</strong> from the incision site is often relatively mild<br />
in comparison with deeper <strong>pain</strong> from the muscles and peritoneum.<br />
212 Specifically, <strong>pain</strong> on mobilization and during coughing<br />
is multifactorial and can be very severe in the early postoperative<br />
period. 20<br />
We studied patients undergoing <strong>abdominal</strong> <strong>hysterectomy</strong><br />
since this is a procedure associated with moderate-to-severe<br />
postoperative <strong>pain</strong>, specifically in the early postoperative<br />
period. 221 We found a low supplementary analgesic consumption<br />
during the first 24 h <strong>after</strong> i.p. administration of levobupivacaine<br />
in both groups, confirming our previous studies. 2 12<br />
Table 1 Patient characteristic data, duration of anaesthesia and<br />
operation, and fentanyl consumption are shown as mean (SD)<br />
except age (range). All other data are shown as numbers (ASA<br />
physical status) or n (%) as appropriate. Group P, patient-controlled<br />
i.p. analgesia; Group C, continuous i.p. analgesia<br />
Group P (n520)<br />
Group C (n520)<br />
Age (yr) 48 (38–65) 51 (40–63)<br />
Weight (kg) 73 (12) 68 (9)<br />
Height (cm) 168 (5) 165 (6)<br />
ASA physical status (I/II) 15/5 17/3<br />
Duration of operation (min) 119 (26) 121 (29)<br />
Duration of anaesthesia (min) 156 (27) 156 (29)<br />
Type of operation<br />
Total <strong>hysterectomy</strong> 12 (60%) 15 (75%)<br />
Salpingo-oophorectomy 8 (40%) 5 (25%)<br />
Type of incision<br />
Pfannenstiel 3 (15%) 4 (20%)<br />
Lower midline 17 (85%) 16 (80%)<br />
Intraoperative fentanyl (mg) 318 (74) 277 (75)<br />
However, we also found that PCipA has an advantage over<br />
continuous infusion in that supplementary analgesic consumption<br />
was further reduced by as much as 35% (from 36 to 23 mg)<br />
during 0–24 h. This was much lower than in one study where the<br />
24 h mean morphine consumption, even with ibuprofen, was<br />
47.3 mg. 21 Although we achieved good analgesia at the incision<br />
site by LA infiltration, several other components of <strong>pain</strong> may<br />
persist including muscle, peritoneal, and visceral <strong>pain</strong>. Recent<br />
studies, including two meta-analyses of the literature, have<br />
shown that i.p. administration of LA reduces postoperative<br />
<strong>pain</strong> <strong>after</strong> <strong>abdominal</strong> surgery. 822 Although the mechanism for<br />
improved analgesia with patient-controlled bolus doses could<br />
be speculative, we believe that the analgesic efficacyof continuous<br />
infusions may be partly due to their systemic absorption,<br />
and thereby a central rather than a local effect. Significant<br />
plasma concentration of LA is reached when they are infused<br />
intraperitoneally 2 and this may produce some analgesia by<br />
central mechanisms similar to i.v. infusion. 23 24 In contrast to<br />
continuous infusion, the analgesic efficacy of PCipA may be via<br />
localanti-inflammatoryeffects, 825 and alsobyblockingafferent<br />
sensory nerves transmitting visceral <strong>pain</strong> through the vagus<br />
nerves. 26 Thus, blocking of visceral <strong>pain</strong> by the intermittent injection<br />
of i.p. LA may not only result in decreased analgesic consumption,<br />
as in our present study, but even faster recovery of<br />
visceral functions such as the earlier return of bowel function,<br />
possibly due to lower rescue opioid consumption. This is an<br />
interesting hypothesis, supported by some evidence from the<br />
literature. In a recent study, infusion of i.p. ropivacaine <strong>after</strong><br />
colectomy improved early surgical recovery. 27 The authors<br />
hypothesized that LA cause a transient chemical afferentectomy<br />
when injected intraperitoneally thereby producing analgesia<br />
and early functional recovery. However, the question<br />
that still remains unanswered from our present study is<br />
whether the analgesic effect of LA <strong>after</strong> PCipA is a systemic<br />
effect or a local analgesic and anti-inflammatory effect.<br />
In our present study, patients having PCipA with LA selfadministered<br />
180 ml of levobupivacaine while those in the<br />
continuous group received 240 ml during the first 24 h <strong>after</strong><br />
operation and yet had lower rescue analgesic consumption,<br />
which may also support a local effect. It is also possible, although<br />
speculative, that 10 ml of LA injection during 10 min<br />
in the PCipA group resulted in a wider spread of i.p. LA resulting<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
Table 2 Analgesic consumption. All data are shown as mean (SD) except number of patients n (%) for NSAIDs. Data are analysed by the<br />
unpaired t-test or Fisher exact test as appropriate. Group P, patient-controlled i.p. analgesia; Group C, continuous i.p. analgesia. *A mean ratio is the<br />
difference between two means on a relative scale, that is, mean ratio of 1.56 interprets as 56% higher geometric mean in Group C compared with<br />
Group P. † Following the Bonferroni–Holm correction for multiple comparisons, for details, see text. ‡ Group Cvs P; results are presented as odds ratio<br />
(95% CI)<br />
Group P (n520) Group C (n520) Group C–P, mean<br />
difference (95% CI)<br />
Group C/P, mean<br />
ratio* (95% CI)<br />
P-values<br />
Ketobemidone in mg 0–4 h (range) 13.4 (7.1) (4–28) 21.0 (12.6) (8–59) 7.6 (1.0–14.1) 1.56 (1.09–2.22) 0.015 0.045<br />
Ketobemidone in mg 0–24 h (range) 23.1 (13.8) (8–48) 35.7 (20.2) (10–81) 12.6 (1.5–23.6) 1.58 (1.07–2.32) 0.021 0.042<br />
Ketobemidone in mg 24–48 h 3.1 (4.2) (0–12) 6.3 (8.6) (0–31) 3.2 (21.1–7.5) 1.84 (0.97–3.48) 0.060 0.060<br />
(range)<br />
NSAID (0–24 h) [n (%)] 3 (15%) 4 (22%) 1.4 (0.2–11.1) ‡ 1.00<br />
Corrected<br />
P-values †<br />
Page 5 of 9
<strong>BJA</strong><br />
Perniola et al.<br />
A<br />
10<br />
8<br />
Group P<br />
Group C<br />
B<br />
10<br />
8<br />
Group P<br />
Group C<br />
NRS (0 – 10)<br />
6<br />
4<br />
NRS (0 – 10)<br />
6<br />
4<br />
2<br />
2<br />
0<br />
0<br />
1 4 12<br />
Hours<br />
C<br />
NRS (0 – 10)<br />
24<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
48<br />
1 4 12<br />
Hours<br />
1 4 12<br />
Hours<br />
24 48<br />
Group P<br />
Group C<br />
24 48<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
Fig 2 (A–C) Pain at the incision site, deep <strong>pain</strong>, and <strong>pain</strong> on coughing. Distributions are shown as box plots and inter-quartile range (IQR). Group P,<br />
patient-controlled i.p. analgesia; Group C, continuous i.p. infusion; NRS, numeric rating scale; circle, outliers. The whiskers represent minimum and<br />
maximum values if outliers are not present.<br />
in a block of more free afferent nerve endings within the peritoneum<br />
compared with a continuous infusion of 10 ml over<br />
60 min. The reason why patients in both groups reported moderate<br />
to severe <strong>pain</strong> on coughing when they could request<br />
further analgesia (LA or opioids) is unclear. It is possible that<br />
analgesic supplementation was requested only during <strong>pain</strong><br />
at rest and not during mobilization/coughing. Additionally, in<br />
our experience, some patients may have severe nausea or<br />
vomiting from opioid supplementation and accept <strong>pain</strong> on<br />
coughing rather than constant nausea. 28<br />
The health-related quality-of-life questionnaire (SF-36) did<br />
not show any differences between the groups <strong>after</strong> operation,<br />
which may be not surprising since we did not find any difference<br />
in postoperative <strong>pain</strong> intensity between the groups. The<br />
faster recovery of GI function in patients receiving LA via<br />
PCipA may have resulted in a shorter time to home-readiness.<br />
The shortened time to recovery of bowel function <strong>after</strong> patientcontrolled<br />
i.p. administration of LA may be due to the opioid<br />
sparing which was evident in the present study. We found no<br />
major complications when using i.p. LA, including infection,<br />
Page 6 of 9
Intraperitoneal local anaesthetics for <strong>pain</strong> relief <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong><br />
<strong>BJA</strong><br />
Table 3 <strong>Postoperative</strong> functional recovery and respiratory function. All data are shown as mean (SD) unless otherwise shown and analysed by the<br />
unpaired t-test except P Emax which was analysed by using mixed model. P Emax , maximum expiratory pressure; Group P, patient-controlled i.p.<br />
analgesia; Group C, continuous i.p. analgesia; GI, gastrointestinal<br />
Group P (n520) Group C (n520) Group C vs P, mean<br />
difference (95% CI)<br />
P-values<br />
Time to walk with help (h) 21 (4), n¼19 22 (3), n¼19 0.4 (21.8 to 2.8) 0.68<br />
Time to walk without help (h) 23 (6), n¼19 25 (6), n¼18 2.2 (22.1 to 6.6) 0.30<br />
Time to start drinking (h) 16 (7), n¼17 15 (8), n¼17 21.4 (26.8 to 3.9) 0.58<br />
Time to start eating (h) 24 (9), n¼19 26 (8), n¼18 1.7 (24.2 to 7.6) 0.56<br />
Home-readiness (days) 1.9 (0.7), n¼17 2.7 (1), n¼13 0.7 (0.03–1.5) 0.04<br />
Length of hospital stay (days) 3.9 (0.8), n¼20 4.5 (1.3), n¼20 0.6 (20.6 to 1.3) 0.07<br />
Return to GI function (days) 1.5 (0.6), n¼12 2.2 (0.6), n¼18 0.7 (0.2–1.2) ,0.01<br />
P E max (litre min 21 )<br />
Before operation 59 (16), n¼17 60 (14), n¼18<br />
4 h 35 (13), n¼18 34 (16), n¼19 21(210 to 7) 0.72<br />
24 h 42 (16), n¼19 34 (11), n¼20 27(216 to 1) 0.09<br />
48 h 45 (15), n¼19 41 (10), n¼19 24(213 to 5) 0.37<br />
Table 4 Side-effect and complications. All results are shown as number of patients n (%) except sedation which is presented as mean (SD). PON,<br />
postoperative nausea; POV, postoperative vomiting. The x 2 test or Fisher exact test was used as appropriate except sedation which was analysed<br />
using mixed model. NE, not estimated; Group P, patient-controlled i.p. analgesia; Group C, continuous i.p. analgesia. *Group C vs P is presented as<br />
mean difference (95% CI)<br />
Group P (n520) Group C (n520) Group C vs P, odds ratio (95% CI) P-value<br />
<strong>Postoperative</strong> nausea (PON)<br />
0–4 h 10 (50%) 5 (25%) 0.3 (0.1–1.3) 0.10<br />
4–24 h 2 (10%) 2 (10%) 1.0 (0.1–7.9) 1.00<br />
24–48 h 1 (5%) 0 NE 1.00<br />
<strong>Postoperative</strong> vomiting (POV)<br />
0–4 h 3 (15%) 1 (5%) 0.3 (0.03–3.1) 0.60<br />
4–24 h 2 (10%) 1 (5%) 0.5 (0.04–5.6) 1.00<br />
24–48 h 0 0 NE<br />
Total PON or POV<br />
0–48 h 11 (55%) 6 (30%) 0.3 (0.1–1.3) 0.11<br />
Anti-emetics given (0–24 h) 16 (80%) 17 (85%) 1.4 (0.3–7.3) 1.00<br />
Anti-emetics given (24–48 h) 4 (20%) 3 (15%) 0.7 (0.1–3.6) 1.00<br />
Sedation (NRS)*<br />
4 h 4.8 (2.5), n¼18 4.4 (2.7), n¼19 20.4 (22.2 to 1.4) 0.65<br />
24 h 4.0 (2.4), n¼19 4.3 (3.2), n¼20 0.4 (21.3 to 2.2) 0.61<br />
48 h 3.5 (3.0), n¼17 3.1 (2.4), n¼17 20.3 (22.1 to 1.6) 0.77<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
and no patient had any signs or symptoms of LA toxicity, which<br />
is in accordance with our earlier studies. 212<br />
Study limitations<br />
The patient-controlled i.p. analgesia group received more<br />
intraoperative fentanyl, and therefore, the reduction in the<br />
0–4 ketobemidone consumption in this group may reflect on<br />
the higher intraoperative fentanyl given. Furthermore, the<br />
wide CI of ketobemidone consumption during the first 24 h<br />
suggests caution in concluding that the primary endpoint of<br />
this study was clinically significant. However, the finding that<br />
some secondary endpoints such as return of GI function and<br />
home-readiness favour the patient-controlled i.p. method<br />
would suggest thatthere is some impact of reduced opioid consumption<br />
on recovery parameters. We did not measure plasma<br />
concentration of levobupivacaine in this study, which would be<br />
of interest in understanding the mechanism of action of LA.<br />
The PCipA with LA made it almost impossible to correctly<br />
schedule blood sampling. However, in our earlier study using<br />
higher doses of levobupivacaine via continuous i.p. infusion,<br />
we found a dose-dependent increase in plasma concentration<br />
Page 7 of 9
<strong>BJA</strong><br />
Perniola et al.<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
100<br />
Group P<br />
Group C<br />
Preop<br />
Score<br />
80<br />
60<br />
40<br />
20<br />
1 month <strong>after</strong><br />
surgery<br />
but no systemic toxicity due to the low level of free LA in the<br />
plasma. Another limitation of this study was that we did not<br />
verify catheter position by contrast injection. Therefore, we<br />
do not know the exact position of the catheter tip or if there<br />
was catheter migration during mobilization. Finally, we did<br />
not use a patient-controlled analgesia pump intravenously,<br />
which allows the correct assessment of analgesic requirement<br />
<strong>after</strong> operation since it would have been difficult for patients to<br />
handle two PCA devices, one for i.p. LA and the other for i.v. injection<br />
of opioids as rescue medication.<br />
Conclusions<br />
We found that the patient-controlled i.p. analgesia with LA<br />
resulted in statistically significant lower ketobemidone consumption<br />
compared with continuous infusion both during<br />
the initial postoperative phase and during 0–24 h <strong>after</strong><br />
operation. Because of the large confidence intervals in<br />
0<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
PF RP BP GH VT SF RE MH PCS MCS<br />
Fig 3 Health-related quality of life (SF-36). Data are presented as mean of: physical functioning (PF), role-physical (RP), bodily <strong>pain</strong> (BP), general<br />
health (GH), vitality (VT), social functioning (SF), role-emotional (RE), mental health (MH); physical component score (PCS), and mental component<br />
score (MCS). Group P, patient-controlled i.p. analgesia; Group C, continuous i.p. infusion. There were missing data for one patient in Group P before<br />
operation. After operation, at 1 month, there were missing data for five and six patients and at 3 months, for three and five patients in Groups P and<br />
C, respectively. See text for details.<br />
ketobemidone consumption, the clinical relevance for this is<br />
uncertain. However, the lower ketobemidone consumption<br />
did translate into quicker return of GI function and earlier<br />
home-readiness. Future studies should focus on identifying<br />
the mechanism of analgesic effect of LA administered intermittently<br />
intraperitoneally.<br />
Authors’ contributions<br />
3 months <strong>after</strong><br />
surgery<br />
A.P.: contributed towards designing the study, data collection,<br />
statistical analysis, and writing the manuscript. F.F.: contributed<br />
towards data collection and critical comments in the<br />
writing of the manuscript. A.M.: contributed towards all statistical<br />
analysis and discussion on presentation of results. K.A.:<br />
contributed towards designing the study, data confirmation,<br />
and critical comments in the writing of the manuscript. A.G.:<br />
contributed towards designing, data interpretation, and<br />
writing of the manuscript.<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
Page 8 of 9
Intraperitoneal local anaesthetics for <strong>pain</strong> relief <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong><br />
<strong>BJA</strong><br />
Acknowledgements<br />
We would like to thank the personnel in the operating theatres<br />
and those in the postoperative and gynaecological wards for<br />
their help and attention during the various phases of this<br />
study. Special thanks to Ingegärd Wilhelmsson for her help<br />
with the data collection and with patient recruitment.<br />
Declaration of interest<br />
None declared.<br />
Funding<br />
This study was supported partly by funds obtained from the Research<br />
Committee, Örebro County Council, Örebro, Sweden.<br />
References<br />
1 Jacobson GF, Shaber RE, Armstrong MA, Hung YY. Hysterectomy<br />
rates for benign indications. Obstet Gynecol 2006; 107: 1278–83<br />
2 Perniola A, Gupta A, Crafoord K, Darvish B, Magnuson A, Axelsson K.<br />
Intra<strong>abdominal</strong> local anaesthetics for postoperative <strong>pain</strong> relief<br />
following <strong>abdominal</strong> <strong>hysterectomy</strong>: a randomized, double-blind,<br />
dose-finding study. Eur J Anaesthesiol 2009; 26: 421–9<br />
3 White PF. The changing role of non-opioid analgesic techniques in<br />
the management of postoperative <strong>pain</strong>. Anesth Analg 2005; 101:<br />
S5–22<br />
4 Hein A, Rosblad P, Gillis-Haegerstrand C, Schedvins K, Jakobsson J,<br />
Dahlgren G. Low dose intrathecal morphine effects on post<strong>hysterectomy</strong><br />
<strong>pain</strong>: a randomized placebo-controlled study. Acta<br />
Anaesthesiol Scand 2012; 56: 102–9<br />
5 Moen V, Dahlgren N, Irestedt L. Severe neurological complications<br />
<strong>after</strong> central neuraxial blockades in sweden 1990–1999. Anesthesiology<br />
2004; 101: 950–9<br />
6 Cook TM, Counsell D, Wildsmith JA. Major complications of central<br />
neuraxial block: report on the Third National Audit Project of the<br />
Royal College of Anaesthetists. Br J Anaesth 2009; 102: 179–90<br />
7 Kehlet H, Liu SS. Continuous local anesthetic wound infusion to<br />
improve postoperative outcome: back to the periphery? Anesthesiology<br />
2007; 107: 369–71<br />
8 Kahokehr A, Sammour T, Soop M, Hill AG. Intraperitoneal local anaesthetic<br />
in <strong>abdominal</strong> surgery—a systematic review. ANZ J Surg<br />
2011; 81: 237–45<br />
9 Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound<br />
catheters delivering local anesthetic for postoperative analgesia: a<br />
quantitative and qualitative systematic review of randomized controlled<br />
trials. J Am Coll Surg 2006; 203: 914–32<br />
10 Fant F, Axelsson K, Sandblom D, Magnuson A, Andersson SO,<br />
Gupta A. Thoracic epidural analgesia or patient-controlled local analgesia<br />
for radical retropubic prostatectomy: a randomized,<br />
double-blind study. Br J Anaesth 2011; 107: 782–9<br />
11 Thornton PC, Buggy DJ. Local anaesthetic wound infusion for acute<br />
postoperative <strong>pain</strong>: a viable option? Br J Anaesth 2011; 107: 656–8<br />
12 Gupta A, Perniola A, Axelsson K, Thorn SE, Crafoord K, Rawal N. <strong>Postoperative</strong><br />
<strong>pain</strong> <strong>after</strong> <strong>abdominal</strong> <strong>hysterectomy</strong>: a double-blind<br />
comparison between placebo and local anesthetic infused intraperitoneally.<br />
Anesth Analg 2004; 99: 1173–9<br />
13 Rawal N, Allvin R, Axelsson K, et al. Patient-controlled regional analgesia<br />
(PCRA) at home: controlled comparison between bupivacaine<br />
and ropivacaine brachial plexus analgesia. Anesthesiology<br />
2002; 96: 1290–6<br />
14 Singelyn FJ, Vanderelst PE, Gouverneur JM. Extended femoral nerve<br />
sheath block <strong>after</strong> total hip arthroplasty: continuous versus<br />
patient-controlled techniques. Anesth Analg 2001; 92: 455–9<br />
15 Eledjam JJ, Cuvillon P, Capdevila X, et al. <strong>Postoperative</strong> analgesia by<br />
femoral nerve block with ropivacaine 0.2% <strong>after</strong> major knee<br />
surgery: continuous versus patient-controlled techniques. Reg<br />
Anesth Pain Med 2002; 27: 604–11<br />
16 van der Vyver M, Halpern S, Joseph G. Patient-controlled epidural<br />
analgesia versus continuous infusion for labour analgesia: a<br />
meta-analysis. Br J Anaesth 2002; 89: 459–65<br />
17 Duncan LA, Fried MJ, Lee A, Wildsmith JA. Comparison of continuous<br />
and intermittent administration of extradural bupivacaine for<br />
analgesia <strong>after</strong> lower <strong>abdominal</strong> surgery. Br J Anaesth 1998; 80:<br />
7–10<br />
18 Ohqvist G, Hallin R, Gelinder S, Lang H, Samuelson S. A comparison<br />
between morphine, meperidine and ketobemidone in continuous<br />
intravenous infusion for postoperative relief. Acta Anaesthesiol<br />
Scand 1991; 35:44–8<br />
19 Holm S. A simple sequentially rejective multiple test procedure.<br />
Scand J Stat 1979; 6:65–70<br />
20 Leung CC, Chan YM, Ngai SW, Ng KF, Tsui SL. Effect of pre-incision<br />
skin infiltration on post-<strong>hysterectomy</strong> <strong>pain</strong>—a double-blind<br />
randomized controlled trial. Anaesth Intensive Care 2000; 28:<br />
510–6<br />
21 Kroll PB, Meadows L, Rock A, Pavliv L. A multicenter, randomized,<br />
double-blind, placebo-controlled trial of intravenous ibuprofen<br />
(i.v.-ibuprofen) in the management of postoperative <strong>pain</strong> following<br />
<strong>abdominal</strong> <strong>hysterectomy</strong>. Pain Pract 2011; 11:23–32<br />
22 Kahokehr A, Sammour T, Srinivasa S, Hill AG. Systematic review and<br />
meta-analysis of intraperitoneal local anaesthetic for <strong>pain</strong> reduction<strong>after</strong>laparoscopic<br />
gastric procedures. Br J Surg 2011; 98:29–36<br />
23 Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous<br />
lidocaine and postoperative recovery <strong>after</strong> <strong>abdominal</strong> surgery.<br />
Br J Surg 2008; 95: 1331–8<br />
24 Omote K. Intravenous lidocaine to treat postoperative <strong>pain</strong>: management.<br />
Novel strategy with a long-established drug. Anesthesiology<br />
2007; 107:5–6<br />
25 Harvey KP, Adair JD, Isho M, Robinson R. Can intravenous lidocaine<br />
decrease postsurgical ileus and shorten hospital stay in elective<br />
bowel surgery? A pilot study and literature review. Am J Surg<br />
2009; 198: 231–6<br />
26 Konsman JP, Luheshi GN, Bluthe RM, Dantzer R. The vagus nerve<br />
mediates behavioural depression, but not fever, in response to peripheral<br />
immune signals; a functional anatomical analysis. Eur J<br />
Neurosci 2000; 12: 4434–46<br />
27 Kahokehr A, Sammour T, Shoshtari KZ, Taylor M, Hill AG. Intraperitoneal<br />
local anesthetic improves recovery <strong>after</strong> colon resection: a<br />
double-blinded randomized controlled trial. Ann Surg 2011; 254:<br />
28–38<br />
28 Goldstein A, Grimault P, Henique A, Keller M, Fortin A, Darai E. Preventing<br />
postoperative <strong>pain</strong> by local anesthetic instillation <strong>after</strong><br />
laparoscopic gynecologic surgery: a placebo-controlled comparison<br />
of bupivacaine and ropivacaine. Anesth Analg 2000; 91:<br />
403–7<br />
Downloaded from http://bja.oxfordjournals.org/ by guest on January 17, 2014<br />
Handling editor: L. Colvin<br />
Page 9 of 9