PEPA Summer 2012-13 Newsletter - Queensland Health
PEPA Summer 2012-13 Newsletter - Queensland Health
PEPA Summer 2012-13 Newsletter - Queensland Health
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Program of<br />
Experience in the<br />
Palliative Approach<br />
Funded by the Australian Government Department of <strong>Health</strong> and Ageing<br />
NEWSLETTER SUMMER <strong>2012</strong>-<strong>13</strong><br />
Inside this issue:<br />
National News:<br />
• Update<br />
• Tracking<br />
Achievements<br />
• Making a<br />
Difference<br />
• Staffing News<br />
Educational<br />
Component:<br />
• Issues in Pain<br />
Management<br />
The Program of Experience in the Palliative Approach (<strong>PEPA</strong>) provides an opportunity for<br />
health, aged and community care professionals working in primary care or non-specialist<br />
palliative care settings to improve confidence and develop skills in working with people<br />
with palliative care needs. <strong>PEPA</strong> offers funded workforce placements in palliative care<br />
specialist services (host sites). These have three components:<br />
• A supervised clinical placement in a metropolitan or larger service (inpatient,<br />
community and/or hospital based consultancy)<br />
• Integration of learning into the participant’s practice<br />
• Post-placement support<br />
<strong>PEPA</strong> also offers tailored workshops. Please access the <strong>PEPA</strong> webpage for further<br />
details: http://www.pepaeducation.com<br />
The Program of Experience in the Palliative Approach is an initiative of the Australian<br />
Government Department of <strong>Health</strong> and Ageing.<br />
Spotlight on<br />
a Host site:<br />
• J.W. Whittle<br />
Palliative Care<br />
Unit, Hobart<br />
Participant<br />
Reflection<br />
Sector Links<br />
State News<br />
• NT<br />
• ACT<br />
• QLD<br />
• TAS<br />
• VIC<br />
• NSW<br />
• WA<br />
• SA<br />
Update from the National Team:<br />
As we enter into the new year it is great to<br />
reflect on the achievements that have been<br />
made over the past 12 months. Following<br />
the appointment of our national clinical<br />
educator and senior research officers<br />
we released a number of new<br />
resources (including our nursing<br />
and allied health learning guide and<br />
online module), we started<br />
implementing a range of<br />
quality improvement initiatives<br />
(developing the capacity<br />
of mentors, amplifying<br />
our work integrated<br />
learning component<br />
and refining our<br />
Reverse <strong>PEPA</strong> model),<br />
we renewed our focus<br />
on Aged Care and have been working on<br />
publishing more of our program outcomes.<br />
Our Indigenous Reference Group has<br />
expanded to include a greater representation<br />
from across the spectrum of Indigenous health,<br />
policy and workforce sectors and we have engaged<br />
Aboriginal Project Officers and/or consultants in<br />
all states and territories. Participants who have<br />
undertaken <strong>PEPA</strong> placements continue to report<br />
improved confidence, increased knowledge<br />
and expanded skills to deliver a palliative<br />
approach to care.<br />
I would also like to take this opportunity<br />
to thank all of our wonderful supporters,<br />
participants and host site mentors for<br />
your continuing efforts, you each<br />
make a significant contribution<br />
to the success of the program.<br />
It was great catching up with<br />
some of you at the PCNA<br />
conference and at our<br />
post-conference workshop,<br />
‘Facilitating Learning and<br />
Change Management in<br />
Palliative Care Settings’ which was<br />
held on the 12 th December.<br />
Finally, we hope you all had a fabulous<br />
Christmas and wish you all the best for a happy<br />
and fulfilling New Year!!
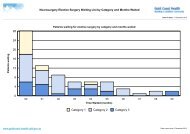
Tracking Achievements<br />
Table 1: Placements completed<br />
(1 July–30 November <strong>2012</strong>)<br />
Registered Nirse (n=71)<br />
Allied <strong>Health</strong> (n=12)<br />
Aboriginal and Torres Strait<br />
Islander <strong>Health</strong> and Community<br />
Workers (n=22)<br />
GPs and Medical<br />
Practitioners (n=20)<br />
Assistants in Nursing/<br />
Care workers (n=16)<br />
14%<br />
16%<br />
11%<br />
9%<br />
50%<br />
Table 2: Workshops completed<br />
(1 July–30 November <strong>2012</strong>)<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Palliative approach Indigenous COP Culture and diversity<br />
2<br />
Making a Difference<br />
Evaluation responses from the 1 July <strong>2012</strong> to 30 November<br />
<strong>2012</strong> indicate that <strong>PEPA</strong> keeps supporting participants to<br />
increase their knowledge and expand their skills. Participants<br />
have reported undertaking the following activities after their<br />
placements:<br />
Knowledge Sharing<br />
• Being able to share knowledge with the co-workers each<br />
day and implement the new goals of care.<br />
• Discussing in-service with staff about <strong>PEPA</strong> program.<br />
Staff Training<br />
• In-service education and assessing the palliative care<br />
material.<br />
• Providing informal symptom management education.<br />
• Organising palliative care medication education session.<br />
Changes in Facility<br />
• Providing better bowel management.<br />
• Implementing appropriate mouth care for the residents.<br />
• Early referral to the palliative care services.<br />
• Adopting a new care plan with details for all staff.<br />
Recent feedback from participants include:<br />
• [My] <strong>PEPA</strong> experience broadened my way of working with<br />
palliative patients. I have grown as a person and [as] a<br />
professional.<br />
• I had a fantastic experience at [X host site]. I learnt so much<br />
on the role of dentition in palliative care and my confidence<br />
has increased a lot.<br />
• <strong>PEPA</strong> made me look at the small things we do, the basic<br />
care provided must always be of a high standard, different<br />
ways of doing things.<br />
• I was warmly welcomed by all. All host sites conveyed<br />
a sense of professionalism that focused all efforts and<br />
resources on positive client outcomes. I left inspired and<br />
motivated.<br />
Staffing News<br />
We would like to welcome the two newest members to our<br />
<strong>PEPA</strong> team, Sally Fitzgerald & Carol Muthunesan. Sally is the<br />
new consultant for the Aboriginal and Torres Strait Islander<br />
component of <strong>PEPA</strong> in the ACT. She currently works at Calvary<br />
<strong>Health</strong> Care ACT in the role of Aboriginal and Torres Strait<br />
Islander Liaison Officer and is looking forward to working with<br />
<strong>PEPA</strong> to strengthen the delivery of palliative care to Aboriginal<br />
and Torres Strait Islander communities in ACT. Carol joined<br />
the NSW <strong>PEPA</strong> team on Monday 10th December <strong>2012</strong>.<br />
Carol is an RN (graduated 2010) and has previously worked<br />
as an Aboriginal Hep C Service Access Coordinator, an<br />
undergraduate nursing cadet (AIN) and in a number of roles<br />
with the Department of Ageing Disabilities and Homecare<br />
Service of NSW (DADHC).<br />
EDUCATIONAL COMPONENT:<br />
Living well until the end<br />
Excerpt taken from the CareSearch Residential Aged<br />
Care Hub (www.caresearch.com.au)<br />
People living in Residential Aged Care today have higher levels<br />
of disability and more complex care needs than in the past.<br />
Many residents are living with dementia, organ failure or general<br />
frailty. Their dying may be a slow process extending over<br />
months or even years.<br />
Quality care for these residents is more than good symptom<br />
control and emotional support. It is about assisting residents<br />
to live well and to maintain self-determination, relationships<br />
and social connections as their dependence on others<br />
increases. It is also about supporting the families of residents.<br />
The World <strong>Health</strong> Organization has acknowledged the needs<br />
of a rapidly ageing population. Their Active Ageing policy<br />
Framework recognises the rights of all people as they age to<br />
“independence, participation, dignity, care and self-fulfilment”.<br />
The active refers to “continuing participation in social, economic,<br />
cultural, spiritual and civic affairs”. [1]
Researchers have used the active ageing framework to describe<br />
determinants of quality of life for people living in RAC. In addition<br />
to the WHO criteria, they found that meaningful leisure, having<br />
control over their own life and care and participating in the<br />
organisation and function were important to residents’ quality of<br />
life. [2]<br />
Providing an environment where people with Huntington’s<br />
disease can maintain maximum independence and control over<br />
their lives is especially challenging. Dellafield and Ferrini report on<br />
how one nursing home supported residents with Huntington’s<br />
disease to live to their potential and to die with dignity. [3]<br />
A systematic review of qualitative research on quality of life in<br />
RAC identified factors residents say are important to their quality<br />
of life. They are:<br />
• Being able to accept and adapt to living in RAC<br />
• Having and maintaining relationships with other residents, staff<br />
and with their family and friends<br />
• A home-like environment, privacy and a sense of their own<br />
space<br />
• Competent carer’s who provided individualised care without<br />
rushing. [4]<br />
References<br />
1. World <strong>Health</strong> Organisation (WHO). Ageing and life course - Active ageing: A policy<br />
framework. WHO; 2002 April [cited <strong>2012</strong> Sep 12].<br />
2. Van Malderen L, Mets T, De Vriendt P, Gorus E. The Active Ageing-concept translated to the<br />
residential long-term care. Qual Life Res. <strong>2012</strong> Jun 8. [Epub ahead of print].<br />
3. Dellefield ME, Ferrini R. Promoting Excellence in End-of-Life Care: lessons learned from<br />
a cohort of nursing home residents with advanced Huntington disease. J Neurosci Nurs.<br />
2011 Aug;43(4):186-92.<br />
4. Bradshaw SA, Playford ED, Riazi A. Living well in care homes: a systematic review of<br />
qualitative studies. Age Ageing. <strong>2012</strong> Jul;41(4):429-40. Epub <strong>2012</strong> Jun 7.<br />
Page created 10 October <strong>2012</strong><br />
This article has been reproduced with permission from the<br />
CareSearch Palliative Care Knowledge Network. The full text is<br />
available at: http://www.caresearch.com.au/caresearch/<br />
tabid/2516/Default.aspx. Information is for education use only<br />
and is provided in good faith without any express or implied<br />
warranty. All practitioners need to use sound clinical judgement<br />
in individual situations.<br />
Spotlight on a Host site<br />
J.W. Whittle Palliative Care Unit, Hobart<br />
The J W Whittle Palliative Care Unit (Whittle Unit) is a 10-bed<br />
Hospice in Hobart, Tasmania which provides a comfortable<br />
environment for patients, family and friends who need to be<br />
cared for in a specialist Palliative Care Setting. The service is<br />
able to provide respite, symptom management and terminal<br />
care. Most people are admitted to the Unit with cancer as their<br />
principle diagnosis, but care is also provided for people with nonmalignant,<br />
terminal conditions such as end stage heart or lung<br />
failure and neurodegenerative illnesses.<br />
Whittle Unit is made up of a strong multidisciplinary team who<br />
meet weekly to review clients care and are also available at any<br />
time to provide specialist palliative care advice. The team includes<br />
nursing and medical staff, a Social Worker, a Music Therapist,<br />
a Pastoral Care Worker and a dedicated band of Hospice<br />
Volunteers. The nursing staff work closely together and are<br />
SECTOR LINKS:<br />
The National Palliative Care Program: The Australian<br />
Government provides support for people with a life-limiting<br />
illness through the National Palliative Care Program -<br />
http://www.health.gov.au/palliativecare.<br />
CareSearch: The CareSearch palliative care knowledge<br />
network is an online resource consolidating evidencebased<br />
and quality information for various groups within<br />
the palliative care community - http://www.caresearch.<br />
com.au.<br />
Palliative Care Australia: PCA works to address national<br />
palliative care issues, represent the area to the Federal<br />
Government and national media, and acts for the sector<br />
when dealing with other national peak bodies and<br />
professional organisations - http://www.palliativecare.<br />
org.au/.<br />
constantly reviewing patient needs and formalise this process<br />
with the use of a newly devised clinical assessment form. Part of<br />
the review process is discharge planning which will assist in for<br />
providing comprehensive referrals to Primary <strong>Health</strong> Providers<br />
who will be providing ongoing care to the patient when they go<br />
home. Staff resilience and satisfaction is maintained through<br />
ensuring the best possible care to those who are dying and<br />
to see that family and friends are well prepared and have felt<br />
included in their loved one’s journey.<br />
Whittle Unit takes pride in having a continuous quality review<br />
process to ensure that the unit is able to provide specialist care<br />
in comfortable surroundings. One quality improvement approach<br />
found the Unit engaging with the community and working with<br />
some local quilting groups. The response was overwhelming<br />
and we now have over 50 quilts which are used for patients’<br />
beds and to keep warm when sitting in armchairs and outside<br />
in the courtyard. This has enhanced the feeling of warmth and<br />
wellbeing for patients, family, friends and staff.<br />
Another project which has been implemented on the Unit is a<br />
bereavement support group called “Hearts and Hands”. This<br />
group was formed to provide comfort and support for bereaved<br />
family members who have been a part of the Unit and involves<br />
weekly craft sessions and companionship facilitated by the<br />
Social Worker and Hospice Volunteers. Craft items are then<br />
placed about the Unit for everyone to enjoy and in the lead up<br />
to Christmas the group are busily producing beautiful Christmas<br />
decorations.<br />
3
STATENEWS<br />
4<br />
<strong>PEPA</strong> SA: Janine Brett<br />
In the few months since the Spring <strong>Newsletter</strong>, South Australia<br />
has successfully completed placements, post placement<br />
workshops and forums. Successful placements have included<br />
General Practitioners, RNs, ENs, Aboriginal <strong>Health</strong> Workers,<br />
Aged Care Workers and Allied <strong>Health</strong> Professionals.<br />
Culturally and Linguistically Diverse (CaLD) Aged Care<br />
workshops have been held in Mt Gambier in October and the<br />
Adelaide metro in November. Attendees at the Mt Gambier<br />
workshop included a Pharmacist, GP, Social Worker, RNs, ENs<br />
and Aged Care Professionals reinforcing the need for palliative<br />
care education across this spectrum (see photo below).<br />
A <strong>PEPA</strong> multidisciplinary Aged Care workshop<br />
The following workshops have also been held:<br />
• Port Pirie at the beginning of November for Speech<br />
Pathologists with Megan Hanley from Tasmania presenting<br />
via Video Link<br />
• Nunkawarrin Yunti in Adelaide Metro area on Palliative Care<br />
– An Aboriginal perspective. Our thanks go to Auntie Irene<br />
for doing the smoking ceremony and her involvement with<br />
the workshop (see photo below).<br />
Auntie Irene conducting a smoking ceremony<br />
at a <strong>PEPA</strong> workshop<br />
We are currently working<br />
on our program for the<br />
January – June 20<strong>13</strong> period<br />
which is looking to be very<br />
busy. Planning is underway<br />
for workshops to be held<br />
in Victor Harbor, Ceduna,<br />
Whyalla and Port Augusta.<br />
<strong>PEPA</strong> South Australia would<br />
like to extend to all of our readers best wishes for 20<strong>13</strong>.<br />
For further enquiries regarding <strong>PEPA</strong> in South Australia please<br />
contact jbrett@pallcare.asn.au or 08 82914156.<br />
<strong>PEPA</strong> NT: Cindy Paardekooper<br />
Northern Territory- Cindy Paardekooper<br />
We are almost half way through this round of <strong>PEPA</strong> 2011-2014<br />
and are showing great results from clinical placements and the<br />
Community Outreach Program activities.<br />
We have embraced the new relationships gained with<br />
stakeholders of the Northern Territory and continue to meet<br />
specific educational demand of the staff of those organisations.<br />
Interactive workshops have been delivered to Alice Springs<br />
and Darwin in this period resulting in support and increased<br />
confidence to the various agencies that continue to assist in<br />
the delivery of quality end of life care to many Territorians.<br />
Recently the NT <strong>PEPA</strong> manager and Aboriginal Educator<br />
co-presented at two Indigenous-focused interstate<br />
conferences speaking about the importance of ‘Returning to<br />
Country’ for many Aboriginal patients at end of life to finish up.<br />
Firstly, we presented to delegates that attended the Rural<br />
<strong>Health</strong> West Aboriginal <strong>Health</strong> Conference in Perth. In closing<br />
of the conference a highlight was the inspirational Deborah<br />
Cheetam the first indigenous soprano opera singer, her voice<br />
was so powerful and continues to linger in our minds.<br />
Secondly was the International Network of<br />
<strong>Health</strong> and Development (INIHKD) Conference<br />
in Brisbane. Along with Darryl and Natasha<br />
presentation on <strong>PEPA</strong> We presented<br />
“Returning to Country – The direct result of<br />
Deborah Cheetam the Program of Experience in the Palliative<br />
Approach in the Northern Territory. Our<br />
presentations saw much delegate interest in the topic and<br />
the importance reflected by other Indigenous peoples such<br />
as the Maoris of New Zealand and the First Nation peoples of<br />
American Countries. It was interesting to hear of the diversities,<br />
similarities, challenges and plans for ways forward in the<br />
Indigenous Palliative Care International Arena. We found it<br />
most valuable and exhilarating in the cultural exchange and<br />
sharing of dances and songs that were held at the delegate’s<br />
conference dinner.<br />
Community Outreach Program<br />
– Beverley Derschow<br />
Thankyou for the warm welcome to my position of <strong>PEPA</strong><br />
Aboriginal Education Officer from Cindy Paardekooper NT <strong>PEPA</strong><br />
Manager and the National <strong>PEPA</strong> team. I am a descendant<br />
of the Martu Western Desert people. I come from a Western<br />
Australia Enrolled Nurse background and I have lived in Darwin
Presenters from the INIHDK<br />
conference, Brisbane<br />
Congress Group<br />
for 28 years. My experience working as an Aboriginal <strong>Health</strong><br />
Worker with the Northern Territory Palliative Care Service for <strong>13</strong><br />
years has made for a much smoother transition to the <strong>PEPA</strong><br />
Aboriginal <strong>Health</strong> Worker Education Officer’s role.<br />
In August, as part of my orientation and with support of Cindy,<br />
due to cancellation of planned Mutitjulu workshop I was able<br />
to capitalise on Central Australia visit through networking<br />
and consultations with stakeholders of government and non<br />
government Service Providers.<br />
In October I was able to facilitate two workshops for the two<br />
main Aboriginal Community Services, one for Tangentyere<br />
Aboriginal Council, which targeted their Aged Care Community<br />
service. At the request of the service and in keeping with cultural<br />
protocol, we were able to include two concurrent gender<br />
sessions which proved to be well received by participants.<br />
Second workshop held was for Central Australian Aboriginal<br />
Congress and their Aboriginal <strong>Health</strong> Professional Trainees. This<br />
workshop also was well received with good interaction between<br />
presenters and participants which is important with establishing<br />
good communication, building of relationships, understanding<br />
of services available, accessing Palliative Care Service and<br />
talking about Palliative Care which impacts on good outcomes<br />
for clients who use their service.<br />
Members of Central Palliative Care Team Jo Rhodes Clinical<br />
Nurse Manager presented on their service. A highlight was<br />
the guest speakers Fiona Haddon and Gerard Waterford from<br />
Congress Social & Emotional Wellbeing who presented on<br />
their service, what is counselling and practical exercises which<br />
could be done at home to manage own triggers. David Burgess<br />
Palliative Care Pastoral Care Worker presented on Self Care and<br />
Mindfulness.<br />
Consultations were held in September with Katherine regional<br />
government and non government services has resulted in<br />
further interest and requests for Community Outreach Program<br />
Workshops which we plan to facilitate in beginning of 20<strong>13</strong>.<br />
International Network of Indigenous <strong>Health</strong> Knowledge<br />
and Development (INIHKD) Conference held in Brisbane in<br />
September was a great opportunity for me to meet some<br />
members of the <strong>PEPA</strong> team.<br />
I have thoroughly enjoyed my time to date and look forward to<br />
the rest of the 22 months supporting the high standard of the<br />
NT <strong>PEPA</strong> Program as maintained by Cindy Paardekooper <strong>PEPA</strong><br />
Manager.<br />
Finally and most importantly on behalf of the NT <strong>PEPA</strong> Program<br />
we hope everyone had a wonderful Christmas and we wish you<br />
all a Happy and Safe New Year.<br />
<strong>PEPA</strong> ACT: Sue Turner<br />
It is with pleasure that I introduce Sally Fitzgerald. Sally has<br />
graciously accepted the position of Aboriginal and Torres Strait<br />
Islander Consultant for ACT <strong>PEPA</strong>. Together we look forward to<br />
increasing promotion of <strong>PEPA</strong> to the indigenous health workers<br />
within the region.<br />
<strong>2012</strong> has resulted in fabulous outcomes for palliative care<br />
education across the ACT with over 550 participants<br />
attending a variety of educational opportunities, in the form of<br />
placements, workshops and post placement support activities.<br />
Twenty-nine health professionals have completed placements<br />
in <strong>2012</strong>. Prospective participants interested in a placement<br />
are strongly encouraged to submit an application to avoid any<br />
disappointment. ACT is particularly looking for GPs, Aboriginal<br />
or Torres Strait Islander health workers, and Enrolled nurses for<br />
placements in 20<strong>13</strong>.<br />
In the ACT demand for palliative approach workshops outstrips<br />
availability.<br />
Upcoming workshops:<br />
Workshop Target Group Location<br />
General Palliative Approach<br />
5th February 20<strong>13</strong><br />
Culturally Diversity<br />
Workshop<br />
21st March 20<strong>13</strong><br />
General Palliative Approach<br />
Workshop<br />
16th April 20<strong>13</strong><br />
Nurses, Allied <strong>Health</strong><br />
and AINs<br />
All <strong>Health</strong> professionals<br />
Nurses, Allied <strong>Health</strong><br />
and AINs<br />
Clare Holland<br />
House<br />
Clare Holland<br />
House<br />
Clare Holland<br />
House<br />
<strong>Health</strong> professionals from the ACT region interested in<br />
attending a workshop are encouraged to apply. Please contact<br />
Sue Turner, ACT <strong>PEPA</strong> Manager, on 02 62647338 or susan.<br />
turner@calvary-act.com.au .<br />
This year’s post placement activities culminated in the event<br />
“How are you going to die?” held at the National Film and<br />
Sound Archive. The screening of the movie of the same<br />
name was the prelude to a panel discussion with Kate Maher,<br />
Palliative Care Nurse Practitioner, Dr Andrew Skeels and Dr<br />
Frank Brennan, both Palliative Medicine Physicians. The event<br />
encouraged a range of health practitioners from a diverse<br />
spectrum of health care, including industry heavy weights such<br />
as Dr Yvonne Luxford, to discuss the ways health professionals<br />
in the ACT region approach end of life issues.<br />
Kate Maher at the “How are you going to die?’ film night and forum<br />
5
6<br />
<strong>PEPA</strong> QLD: Aurora Hodges<br />
Participant Reflection:<br />
AJ, Personal Care Worker in Aged Care, QLD<br />
AJ is an Aboriginal woman who works as a Personal Care<br />
Worker in aged care in remote western <strong>Queensland</strong>.<br />
She undertook a split placement spending time with two<br />
host sites.<br />
“Palliative care is very valuable, we only get one chance to<br />
get it right. Whether people choose to die at home or in a<br />
hospital or RACF the emphasis is on providing good quality<br />
end of life care and having the knowledge and confidence<br />
to carry it out effectively. These placements provided me<br />
with a greater insight into all aspects of palliative care in<br />
different settings and social situations, the care of the client,<br />
the family and the carers. I was very much out of my zone<br />
in Brisbane however the support I received the entire time<br />
of my placement from the <strong>PEPA</strong> team and in particular the<br />
<strong>PEPA</strong> Indigenous Project Officer Darryl was invaluable. I<br />
was welcomed to Karuna with genuine warmth and was<br />
on the road with RNs doing home visits. I was encouraged<br />
to ask questions and I sat in on case conferencing learning<br />
the benefits and positive outcomes of this as a way for the<br />
multidisciplinary team to touch base and problem solve.<br />
I feel privileged to have been placed with Kris the Nurse<br />
Practitioner at Metro South. She was more than happy to<br />
share with me what she knows and ignited in me the desire<br />
to learn. With her I visited aged care facilities and [learned<br />
more] about family conferences. I strongly recommend <strong>PEPA</strong><br />
for managers, nurses AINs/PCAs as it provides professional<br />
skill development on all levels.<br />
”<strong>PEPA</strong> <strong>Queensland</strong> held a successful GP Update in Palliative<br />
Care workshop on Saturday 24 November with <strong>13</strong> local<br />
GP’s attending. Sessions presented included: ANZSPM 5<br />
domains for evidence to practice gaps for End-of-Life care,<br />
new developments and latest evidence in drug management<br />
of common symptoms and conditions at End-of-Life and<br />
Dr Greg Parker, Senior Medical Officer, QEII Palliative Care Unit, A/Prof Rohan Vora and Lorna<br />
Chess-Williams, Pharmacist, Gold Coast Palliative Care Unit.<br />
pain management in palliative care. Dr Jones Chen, recent<br />
<strong>PEPA</strong> placement participant also gave a presentation on his<br />
placement.<br />
<strong>PEPA</strong> <strong>Queensland</strong> also held a palliative approach workshop<br />
for allied health professionals on 27 November 20<strong>13</strong>. The<br />
aim of the workshop was to develop health professionals’<br />
understanding of the palliative approach and how this<br />
approach can be applied in practice. Presenters included:<br />
Allison Lovel, CNC, Palliative Care Liaison, RBWH; Leonie<br />
Naumann, Physiotherapy Team Leader, Cancer Care, RBWH;<br />
Dr James Stevenson, Director Palliative Care, The Prince<br />
Charles Hospital; Rev Linda McWilliam, Coordinating Chaplain,<br />
Anglicare, Dr Elisa Agostinelli PhD, Counsellor Coordinator, St<br />
Vincent’s Hospital; Kym Griffin, Research Officer, Centre for<br />
Palliative Care Research and Education, Christie Barrett, Social<br />
Worker, Mater <strong>Health</strong> Services Brisbane. Excellent feedback<br />
was received from the 35 allied health professionals attending.<br />
20<strong>13</strong> <strong>PEPA</strong> <strong>Queensland</strong> Workshops:<br />
• 8 February – Community Outreach workshop for Indigenous<br />
<strong>Health</strong> Workers (Mackay)<br />
• 27 February – Cultural Diversity in Palliative Care: an<br />
Indigenous Perspective (RBWH)<br />
• 30 April – Palliative Approach for Allied <strong>Health</strong> Professionals<br />
(RBWH)<br />
• May – 2 Proposed workshops in Mackay – GP and Allied<br />
<strong>Health</strong><br />
Would you like to update your skills in the palliative approach<br />
by undertaking a subsidised workforce placement with a<br />
palliative care specialist service? <strong>PEPA</strong> <strong>Queensland</strong> has<br />
placements starting in 20<strong>13</strong> for:<br />
• GPs<br />
• Allied <strong>Health</strong> Professionals<br />
• RNs<br />
• ENs<br />
• Indigenous <strong>Health</strong> Workers<br />
Please contact Aurora Hodges, <strong>PEPA</strong> Qld Manager on:<br />
Ph: 3646 6216 E: pepaqld@health.qld.gov.au<br />
<strong>PEPA</strong> VIC: Carol Pyke<br />
As the new <strong>PEPA</strong> manager in Victoria, I have found the last<br />
four months to be a challenging but very rewarding time.<br />
The challenge has been to improve my understanding of the<br />
palliative care sector but it has been rewarding to work with<br />
such wonderfully dedicated health professionals.<br />
The focus of these past months has been on increasing the<br />
uptake of <strong>PEPA</strong> placements particularly by registered nurses.<br />
<strong>PEPA</strong> has been promoted to small rural hospitals, bush nursing<br />
hospitals and bush nursing centres. We have also been<br />
promoting <strong>PEPA</strong> to the aged care sector through Leading Aged<br />
Care Services (Victoria). The result has been a steady increase<br />
in <strong>PEPA</strong> applications from nurses working in these areas.<br />
A <strong>PEPA</strong> mentoring workshop was conducted in November<br />
and we had a good attendance from both inpatient and
Clockwise from above: Bathurst <strong>PEPA</strong> workshop; JHH Newcastle; Leeton <strong>PEPA</strong> workshop; Dapto <strong>PEPA</strong> workshop.<br />
7<br />
community-based palliative care services from metropolitan<br />
and rural areas. It was clear from their feedback that<br />
participants valued <strong>PEPA</strong> and the importance of their role<br />
as <strong>PEPA</strong> mentors. They also appreciated the opportunity to<br />
network with their peers. Some work will be done to identify<br />
more networking opportunities for <strong>PEPA</strong> mentors.<br />
<strong>PEPA</strong> was promoted to general practitioners at the Palliative<br />
Care Victoria stand at the General Practitioners Conference<br />
and Exhibition held in Melbourne in mid-November. More work<br />
will be done to promote <strong>PEPA</strong> to this group in the coming year.<br />
<strong>Health</strong> professionals who have recently completed a <strong>PEPA</strong><br />
supervised clinical placement continue to report the benefits<br />
this experience gives them:<br />
• I have been able to share some of the knowledge I gained<br />
with my colleagues which has helped us to be more aware<br />
of not only the needs of our patients but also their families.<br />
• It has given me more confidence in discussing PC (palliative<br />
care) with clients and given me more knowledge of how I<br />
can help them.<br />
Placements are currently available for all health professionals<br />
including general/medical practitioners, nurses, Aboriginal<br />
health workers, and allied health staff.<br />
Carol Pyke<br />
Victorian <strong>PEPA</strong> manager<br />
http://www.health.vic.gov.au/palliativecare/programs<br />
<strong>PEPA</strong> NSW: Janeen Foffani<br />
What a year we had in <strong>2012</strong>! While rewarding and fulfilling on<br />
a number of levels, I’ll remember <strong>2012</strong> as the year that just<br />
didn’t give us a minute’s rest and on reflection I can understand<br />
why. <strong>PEPA</strong> NSW has organised over 60 supervised clinical<br />
placements since February, the majority of these placements<br />
have been for nurses and Aboriginal <strong>Health</strong> Workers. We<br />
have also completed around 20 Basic Palliative Approach<br />
workshops, 2 Palliative Approach ‘yarn ups’ and 15 Palliative<br />
Care Forums across NSW.<br />
We also recently manned <strong>PEPA</strong> NSW display tables at the<br />
NSW Palliative Care Conference (Dubbo), Agency for Clinical<br />
Innovations Network2Network Conference (Sydney) and Rural<br />
NSW GP Conference (Coogee). We met a number of new<br />
people from a diverse group and it was great to see so many<br />
familiar faces and to put a face to a number of voices/names.<br />
I’m also pleased to announce that we had a new staff member<br />
join our team in December. Carol Muthunesan has taken on<br />
the role of <strong>PEPA</strong> NSW Aboriginal Education Officer. Carol is<br />
an RN and brings with her a range of experience and will be a<br />
valued addition to our team. Carol’s focus will be primarily on<br />
the Indigenous arm of <strong>PEPA</strong> NSW however we are all looking<br />
forward to playing an active role in all <strong>PEPA</strong> NSW activities.<br />
Planning for 20<strong>13</strong> is well underway and a number of<br />
placements and workshops have already been organised.<br />
Keep an eye on our webpage for more details especially if you<br />
are in the Newcastle, Quirindi, and Lismore area. It’s starting to<br />
look like 20<strong>13</strong> will be just as busy as last year!<br />
<strong>PEPA</strong> WA: Brooke Wilkinson<br />
<strong>2012</strong> has been a very successful and busy year for <strong>PEPA</strong> in<br />
Western Australia. We had an overwhelming response for<br />
placements from regional general practitioners and nursing<br />
staff.<br />
Clinical placements are still available for Aboriginal <strong>Health</strong><br />
Workers, Enrolled Nurses, Allied <strong>Health</strong> Professionals and<br />
Rural Aged Care Facilities (Reverse <strong>PEPA</strong>). We encourage<br />
participants who are interested in undertaking a <strong>PEPA</strong><br />
placement to submit their application.<br />
<strong>PEPA</strong> WA completed our first Rural Reverse <strong>PEPA</strong> placement<br />
in August. Robyn Ellis the Midwest Palliative Care Coordinator<br />
educated staff at services within the Midwest region. With<br />
some services setting up a palliative care multidisciplinary team<br />
and others joining the regional palliative care interest group.<br />
Each service has strengthened their relationship with the<br />
Midwest palliative care service.
8<br />
Employer’s comment - “We received clear indicators of<br />
when to refer patients to palliative care, and also feel more<br />
confident to contact <strong>PEPA</strong> or our regional coordinator if<br />
we need any help with palliative care issues”.<br />
<strong>PEPA</strong> WA ran a very successful weekend workshop that<br />
focused on the difficult conversations that may arise in<br />
palliative patients. We had a variety of guest presenters<br />
over the weekend. Dr Christina Pulchalski from George<br />
Washington Institute for Spirituality and <strong>Health</strong> (GWish)<br />
DC was in Western Australia for the Palliative Care WA<br />
Conference, she has developed many resources and<br />
tools for spirituality in palliative care and was a great guest<br />
speaker. We also had a panel of palliative care experts<br />
join us; Helena Green (Clinical Nurse/Sexologist), Karen<br />
Anderson (Counsellor), Dr David Thorne (Palliative Care<br />
Consultant) and John Robinson (Clinical Nurse).The was<br />
a fantastic opportunity for participants to network and<br />
share their palliative care stories and experiences with one<br />
another.<br />
Participants’ comments - “I learnt to develop a language<br />
that is non-invasive for inviting people to talk about<br />
personal issues” “Listening is an important tool”.<br />
For further information about any of the workshops or<br />
placement opportunities please contact Brooke Wilkinson<br />
on (08)9382 9372 or go to the Cancer Council website<br />
http://www.cancerwa.asn.au/professionals/palliativecare-profs/professionaldevelopment/<br />
<strong>PEPA</strong> TAS: Susan Rasmussen<br />
Our palliative care host sites have hosted a number of<br />
health professionals over the last few months; these<br />
include Allied <strong>Health</strong>, Registered Nurses, GP’s and<br />
Indigenous <strong>Health</strong> Workers. The positive feedback<br />
from all participants has been overwhelming and the<br />
enthusiasm they all go away with is enormous.<br />
We have held three (3) general <strong>PEPA</strong> workshops with a<br />
fourth to occur just before Christmas these workshops<br />
are always well received and continue to be in high<br />
demand. Planning is in full swing for workshops in 20<strong>13</strong><br />
with one of these being an Indigenous health workers’<br />
workshop which is proposed for the NW of the state.<br />
Post placement support has taken on a new approach<br />
in Tasmania with emails being sent out to all those past<br />
participants who have provided email addresses, if you<br />
are a past participant reading this segment and you have<br />
not receive an email from Susan and you would like to be<br />
included on the email circulation list please email Susan<br />
on susan.rasmussen@dhhs.tas.gov.au.<br />
New developments:<br />
<strong>PEPA</strong> Tasmania is delighted to welcome Melwood Unit<br />
at St Lukes Calvary hospital in Launceston as a new<br />
host site offering placement opportunities in a hospice<br />
environment to northern Tasmanian future participants.<br />
We hope to commence placement in the Melwood Unit<br />
early in 20<strong>13</strong>.<br />
For further information you can<br />
contact your local <strong>PEPA</strong> manager:<br />
Australian Capital Territory<br />
Sue Turner<br />
<strong>PEPA</strong>@calvary-act.com.au<br />
Ph: 02 6264 7338 • Fax: 02 6273 0338<br />
New South Wales<br />
Janeen Foffani<br />
pepansw@sswahs.nsw.gov.au<br />
Ph: 02 9515 6424 • Fax: 02 9515 6768<br />
Northern Territory<br />
Cindy Paardekooper<br />
Cindy.Paardekooper@nt.gov.au<br />
Ph: 08 8922 7679 • Fax: 08 8922 6775<br />
<strong>Queensland</strong><br />
Aurora Hodges<br />
pepa@health.qld.gov.au<br />
Ph: 07 3646 6216 • Fax: 07 3646 7942<br />
South Australia<br />
Tracey Watters<br />
twatters@pallcare.asn.au<br />
Ph: 08 8291 4379<br />
Victoria<br />
Carol Pyke<br />
Carol.Pyke@health.vic.gov.au<br />
Ph: 03 9096 0509 • Fax: 03 9096 9206<br />
Western Australia<br />
Brooke Wilkinson<br />
<strong>PEPA</strong>@cancerwa.asn.au<br />
Ph: 08 9382 9372 • Fax: 08 9381 8103<br />
Tasmania<br />
Susan Rasmussen<br />
Susan.Rasmussen@dhhs.tas.gov.au<br />
Ph: 03 6220 2431 • Fax: 03 6222 7679<br />
National Coordinator<br />
Natasha Myers<br />
pepa@qut.edu.au<br />
Ph: 07 3<strong>13</strong>8 6121 • Fax: 07 3<strong>13</strong>8 6030<br />
National Coordinator for Indigenous <strong>PEPA</strong>:<br />
Dr Mick Adams<br />
m2.adams@qut.edu.au<br />
Ph: 07 3<strong>13</strong>8 5807<br />
A copy of this newsletter is available online at:<br />
http://www.pepaeducation.com<br />
© QUT 2011 18051