PDF 586 KB - Department of Health and Ageing
PDF 586 KB - Department of Health and Ageing
PDF 586 KB - Department of Health and Ageing
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
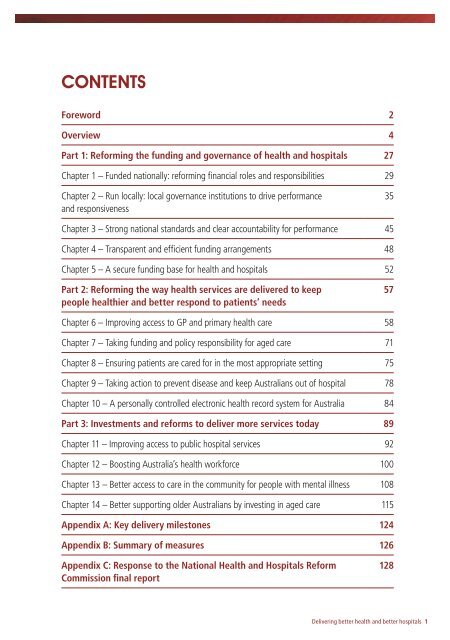
Contents<br />
Foreword 2<br />
Overview 4<br />
Part 1: Reforming the funding <strong>and</strong> governance <strong>of</strong> health <strong>and</strong> hospitals 27<br />
Chapter 1 – Funded nationally: reforming financial roles <strong>and</strong> responsibilities 29<br />
Chapter 2 – Run locally: local governance institutions to drive performance<br />
<strong>and</strong> responsiveness<br />
35<br />
Chapter 3 – Strong national st<strong>and</strong>ards <strong>and</strong> clear accountability for performance 45<br />
Chapter 4 – Transparent <strong>and</strong> efficient funding arrangements 48<br />
Chapter 5 – A secure funding base for health <strong>and</strong> hospitals 52<br />
Part 2: Reforming the way health services are delivered to keep<br />
people healthier <strong>and</strong> better respond to patients’ needs<br />
57<br />
Chapter 6 – Improving access to GP <strong>and</strong> primary health care 58<br />
Chapter 7 – Taking funding <strong>and</strong> policy responsibility for aged care 71<br />
Chapter 8 – Ensuring patients are cared for in the most appropriate setting 75<br />
Chapter 9 – Taking action to prevent disease <strong>and</strong> keep Australians out <strong>of</strong> hospital 78<br />
Chapter 10 – A personally controlled electronic health record system for Australia 84<br />
Part 3: Investments <strong>and</strong> reforms to deliver more services today 89<br />
Chapter 11 – Improving access to public hospital services 92<br />
Chapter 12 – Boosting Australia’s health workforce 100<br />
Chapter 13 – Better access to care in the community for people with mental illness 108<br />
Chapter 14 – Better supporting older Australians by investing in aged care 115<br />
Appendix A: Key delivery milestones 124<br />
Appendix B: Summary <strong>of</strong> measures 126<br />
Appendix C: Response to the National <strong>Health</strong> <strong>and</strong> Hospitals Reform<br />
Commission final report<br />
128<br />
Delivering better health <strong>and</strong> better hospitals 1
Foreword<br />
The provision <strong>of</strong> quality, accessible health care is a major challenge facing governments<br />
around the world.<br />
Dem<strong>and</strong> for health services is increasing as populations are ageing <strong>and</strong> more people are<br />
living with chronic diseases.<br />
Meanwhile, medical care is becoming more expensive as technology <strong>and</strong> medicines<br />
continue to advance. While fiscal constraints are intensifying, the community is expecting<br />
more <strong>of</strong> the health care system.<br />
The choice for governments is whether they act now so their health system can cope with<br />
these increasing challenges, or whether they sit back <strong>and</strong> let their health systems gradually<br />
become overwhelmed.<br />
The Government has made the choice to act <strong>and</strong> to implement the most far-reaching<br />
structural reforms to the health system since the introduction <strong>of</strong> Medicare.<br />
We will establish a new National <strong>Health</strong> <strong>and</strong> Hospitals Network – that is funded nationally<br />
<strong>and</strong> run locally.<br />
We are implementing major reforms to the funding <strong>and</strong> governance <strong>of</strong> our health system,<br />
to place it on sustainable long-term foundations.<br />
We are changing the way that health services are delivered, through better access to<br />
quality services designed around the needs <strong>of</strong> patients, <strong>and</strong> placing a greater focus on<br />
prevention, early intervention <strong>and</strong> the provision <strong>of</strong> care outside <strong>of</strong> hospitals.<br />
We are also increasing the national investment in our health <strong>and</strong> hospitals <strong>and</strong> our health<br />
workforce, to deliver better care <strong>and</strong> better access to services for patients right now.<br />
Some <strong>of</strong> the benefits <strong>of</strong> these reforms will be felt immediately, but many will only be seen<br />
in the medium to longer term.<br />
2 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
As we have said in health forums conducted across every state <strong>and</strong> territory <strong>of</strong> the nation,<br />
health reform is ultimately about one thing – better health <strong>and</strong> hospitals for all Australians.<br />
The goal <strong>of</strong> our reform agenda is simply that all Australians may enjoy access to high quality,<br />
better coordinated <strong>and</strong> sustainable health care in the decades ahead.<br />
The Hon. Kevin Rudd MP The Hon. Wayne Swan MP The Hon. Nicola Roxon MP<br />
Prime Minister Treasurer Minister for <strong>Health</strong> <strong>and</strong> <strong>Ageing</strong><br />
Delivering better health <strong>and</strong> better hospitals 3
Overview<br />
1. A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s future<br />
The Government has secured agreement to deliver a National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
– the most significant reforms to Australia’s health <strong>and</strong> hospital system since the introduction<br />
<strong>of</strong> Medicare, <strong>and</strong> one <strong>of</strong> the biggest reforms to the federation in its history. State <strong>and</strong><br />
territory governments (referred to throughout this document as ‘states’) will work with the<br />
Commonwealth Government to deliver the National <strong>Health</strong> <strong>and</strong> Hospitals Network. 1<br />
These reforms have three primary objectives:<br />
1. Reforming the fundamentals <strong>of</strong> our health <strong>and</strong> hospital system, including funding <strong>and</strong><br />
governance, to provide a sustainable foundation for providing better services now <strong>and</strong> in<br />
the future.<br />
2. Changing the way health services are delivered, through better access to high quality<br />
integrated care designed around the needs <strong>of</strong> patients, <strong>and</strong> a greater focus on prevention,<br />
early intervention <strong>and</strong> the provision <strong>of</strong> care outside <strong>of</strong> hospitals.<br />
3. Providing better care <strong>and</strong> better access to services for patients right now, through increased<br />
investments to provide better hospitals, better infrastructure, <strong>and</strong> more doctors <strong>and</strong> nurses.<br />
These reforms to establish the National <strong>Health</strong> <strong>and</strong> Hospitals Network will drive major<br />
improvements in service delivery <strong>and</strong> better health for patients. They will equip the health<br />
<strong>and</strong> hospital system to better serve the Australian community into the future.<br />
1.1 Funding <strong>and</strong> governance reforms to provide a sustainable foundation for<br />
health <strong>and</strong> hospitals<br />
Funded nationally – the Commonwealth taking majority funding responsibility across<br />
Australia’s health <strong>and</strong> hospital system<br />
Under the National <strong>Health</strong> <strong>and</strong> Hospitals Network, the Commonwealth Government will<br />
become the majority funder <strong>of</strong> Australian public hospitals. The Commonwealth will fund<br />
60 per cent <strong>of</strong> the efficient price for all public hospital services, <strong>and</strong> 60 per cent <strong>of</strong> capital,<br />
research <strong>and</strong> training in our public hospitals. The Commonwealth will also take full funding<br />
<strong>and</strong> policy responsibility for GP <strong>and</strong> primary health care services, <strong>and</strong> for aged care services.<br />
1 See page 24 for a description <strong>of</strong> the current status <strong>of</strong> negotiations with Western Australia.<br />
4 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
To reduce cost shifting <strong>and</strong> strengthen integration between care provided in hospitals <strong>and</strong> care<br />
provided in the community, the Commonwealth will, over time, also move to fund 100 per cent<br />
<strong>of</strong> the efficient price <strong>of</strong> primary health care equivalent outpatient services.<br />
The Government will ensure new financing arrangements effectively support small regional<br />
<strong>and</strong> rural hospitals. The Government will ensure funding reflects the higher costs associated<br />
with delivering services in regional <strong>and</strong> rural areas <strong>of</strong> Australia, including providing block<br />
funding where appropriate so that small rural <strong>and</strong> regional hospitals can continue to deliver on<br />
Community Service Obligations.<br />
Delivered locally – devolving responsibility for service delivery to the local level<br />
The governance <strong>and</strong> management <strong>of</strong> local health <strong>and</strong> hospital services will be devolved to the<br />
local level. New local institutions will work together to deliver more integrated health services<br />
in their local community, <strong>and</strong> drive improvements across the entire health system.<br />
Responsibility for hospital management will be devolved to Local Hospital Networks. This will<br />
increase local autonomy <strong>and</strong> flexibility so that services are more responsive to local needs.<br />
Local Hospital Networks will provide more flexibility for local managers <strong>and</strong> local clinicians<br />
to drive innovation, efficiency <strong>and</strong> improvements for patients. They will deliver improved<br />
clinical engagement, an important driver <strong>of</strong> innovation <strong>and</strong> productivity. Local Hospital<br />
Networks will work with clinicians to incorporate their views, especially on quality <strong>and</strong> safety,<br />
into day to day operations.<br />
Independent primary health care organisations – to be called Medicare Locals – with strong<br />
links to local communities <strong>and</strong> health pr<strong>of</strong>essionals will be established to provide better<br />
services, improve access to care <strong>and</strong> drive integration across GP <strong>and</strong> primary health care<br />
services. Medicare Locals will work closely with Local Hospital Networks to improve patient<br />
care <strong>and</strong> the quality <strong>of</strong> health <strong>and</strong> hospital services. Together they will ensure that GP <strong>and</strong><br />
primary health care <strong>and</strong> hospital care are better integrated, so patients smoothly transition in<br />
<strong>and</strong> out <strong>of</strong> hospital <strong>and</strong> continue to receive all the care they need.<br />
One stop shops located across the country will ensure Australians can more easily access<br />
information <strong>and</strong> assessment for aged care services. Aged care one stop shops will provide<br />
advice <strong>and</strong> help people access the care that meets their needs – from basic home based services<br />
to high level residential care – <strong>and</strong> will link up with Local Hospital Networks <strong>and</strong> Medicare<br />
Locals to improve integration between all the health services that older Australians require.<br />
Delivering better health <strong>and</strong> better hospitals 5
Clear <strong>and</strong> transparent performance reporting against new, higher national st<strong>and</strong>ards<br />
New, higher national st<strong>and</strong>ards <strong>and</strong> transparent reporting will provide Australians with more<br />
information than ever before about the performance <strong>of</strong> their health <strong>and</strong> hospital system. This<br />
performance information will be nationally consistent <strong>and</strong> locally relevant, better informing<br />
communities about the performance <strong>of</strong> their local health <strong>and</strong> hospital services against strong<br />
national st<strong>and</strong>ards.<br />
Regular Hospital Performance Reports will provide clear <strong>and</strong> transparent reporting on the<br />
performance <strong>of</strong> every Local Hospital Network, <strong>and</strong> the hospitals within it, <strong>and</strong> every private<br />
hospital. They will show how all Australian hospitals perform against new national st<strong>and</strong>ards<br />
<strong>and</strong> other performance indicators. The Government will also develop <strong>Health</strong>y Communities<br />
Reports on GP <strong>and</strong> primary health care performance – including on access to GP services <strong>and</strong><br />
out <strong>of</strong> hours GP care, preventive health risk factors <strong>and</strong> other measures <strong>of</strong> community health<br />
<strong>and</strong> wellbeing.<br />
Transparent reporting will help health providers promote a culture <strong>of</strong> continuous improvement.<br />
It will allow strong performance to be identified <strong>and</strong> transferred across the sector, while<br />
supporting early identification <strong>of</strong> poor performance, so that interventions can be made before<br />
problems become entrenched.<br />
Paying Local Hospital Networks for the services they provide through activity<br />
based funding<br />
To drive transparency <strong>and</strong> efficiency in funding <strong>of</strong> health services, Local Hospital Networks will<br />
be paid on the basis <strong>of</strong> each service they provide to public patients under service agreements<br />
negotiated with states. The Commonwealth’s contribution will be based on a national efficient<br />
price, to be determined by a new, independent national umpire – the Independent Hospital<br />
Pricing Authority (IHPA). This will reduce waste <strong>and</strong> increase the number <strong>of</strong> services provided<br />
for each dollar invested.<br />
For the first time, both Commonwealth <strong>and</strong> state funding for public hospital services will be<br />
clearly identified, <strong>and</strong> delivered transparently <strong>and</strong> directly to Local Hospital Networks through<br />
a National <strong>Health</strong> <strong>and</strong> Hospitals Network Funding Authority (‘Funding Authority’) in each<br />
state. Jointly governed by the Commonwealth <strong>and</strong> the relevant state, these Funding Authorities<br />
will transparently report on the number <strong>of</strong> services provided <strong>and</strong> paid for. This will introduce<br />
new levels <strong>of</strong> transparency in funding for public hospitals, <strong>and</strong> give greater confidence to the<br />
community that scarce health dollars are going directly to hospital services.<br />
6 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Commonwealth funding will flow automatically through Funding Authorities directly to Local<br />
Hospital Networks based on services actually provided – there will be no scope to divert<br />
taxpayer funds dedicated to health to other uses. Funding Authorities will have no policy or<br />
operational role, beyond receiving activity based payments from governments <strong>and</strong> making<br />
payments to Local Hospital Networks. This will give hospitals more funding certainty than ever<br />
before. Transparent funding arrangements will also support transparent performance reporting<br />
<strong>and</strong> drive continuous improvement within each public hospital.<br />
Public hospital services will be provided under service agreements between each Local Hospital<br />
Network <strong>and</strong> states. The Commonwealth will make payments to states for system‐wide<br />
matters such as research <strong>and</strong> training payments, <strong>and</strong> block grants, including for small rural <strong>and</strong><br />
regional hospitals to recognise Community Service Obligations. The Commonwealth will place<br />
strong conditions on this funding to ensure it is spent consistently with the overall objectives<br />
<strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network. States will manage system‐wide issues for<br />
public hospitals, operating within a framework <strong>of</strong> unified national funding <strong>and</strong> governance<br />
arrangements. States will be held to account for meeting strong national st<strong>and</strong>ards – including<br />
st<strong>and</strong>ards backed by funding linked to performance – <strong>and</strong> the community will have much<br />
better information about each hospital’s performance.<br />
The combination <strong>of</strong> national funding <strong>and</strong> st<strong>and</strong>ards, local management <strong>and</strong> service delivery,<br />
<strong>and</strong> transparent reporting, is at the core <strong>of</strong> the new National <strong>Health</strong> <strong>and</strong> Hospitals Network.<br />
The disparate performance <strong>and</strong> operating models <strong>of</strong> states will become a thing <strong>of</strong> the past<br />
with this shift to a single national network.<br />
Financing the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
Under these new funding arrangements, the Commonwealth Government will pay for the<br />
majority <strong>of</strong> growth in public hospital costs over time – including growth over <strong>and</strong> above the<br />
share <strong>of</strong> Goods <strong>and</strong> Services Tax (GST) dedicated to health <strong>and</strong> hospitals in each state.<br />
The Commonwealth’s share <strong>of</strong> public hospital funding has slowly declined over the past two<br />
decades. Under present arrangements, if a state decides to invest more in health <strong>and</strong> hospital<br />
services, the Commonwealth does not make any contribution.<br />
Through the establishment <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network, the Commonwealth<br />
will permanently pay 60 cents in each dollar <strong>of</strong> growth in health costs. If states need to provide<br />
more elective surgery procedures, to meet community expectations for instance, <strong>and</strong> they are<br />
willing to fund their share, Commonwealth funding will automatically flow.<br />
Delivering better health <strong>and</strong> better hospitals 7
As costs continue to grow, this reform will provide an increasing benefit to health <strong>and</strong><br />
hospital services in each state, starting with at least $15.6 billion in additional growth costs<br />
guaranteed by the Commonwealth from 2014–15 to 2019–20. This will underpin the financial<br />
sustainability <strong>of</strong> our health <strong>and</strong> hospitals system into the future. It will also improve the long<br />
run productivity <strong>of</strong> the Australian economy: the level <strong>of</strong> government with the most stable <strong>and</strong><br />
efficient means <strong>of</strong> raising revenue will now be the majority funder <strong>of</strong> the fastest growing area<br />
<strong>of</strong> public expenditure.<br />
Reducing blame shifting <strong>and</strong> cost shifting<br />
The funding <strong>and</strong> governance reforms outlined above will reduce blame shifting <strong>and</strong> cost<br />
shifting between levels <strong>of</strong> government in a number <strong>of</strong> critical ways.<br />
Over the past decade, the states have blamed the Commonwealth for the pressures facing<br />
public hospitals because its funding share has not kept up with growth in costs <strong>and</strong> increased<br />
dem<strong>and</strong> for services. For the first time, the Commonwealth’s share <strong>of</strong> public hospital funding<br />
will become a fixed, majority share <strong>of</strong> public hospital costs, with the efficient price <strong>of</strong> hospital<br />
services determined by a new, independent umpire – the IHPA. The IHPA’s ruling will be<br />
binding, <strong>and</strong> the Commonwealth will pay its fixed 60 per cent share <strong>of</strong> every public hospital<br />
service that Local Hospital Networks <strong>and</strong> states agree to provide. This will end arrangements<br />
whereby the Commonwealth’s contribution to public hospitals bears little relationship to health<br />
service dem<strong>and</strong> or increasing costs.<br />
Currently, the states <strong>and</strong> Commonwealth shift costs onto one another, as no one level <strong>of</strong><br />
Government is responsible for the majority share <strong>of</strong> funding in key parts <strong>of</strong> the health system –<br />
public hospitals <strong>and</strong> GP <strong>and</strong> primary health care. The Commonwealth will become the majority<br />
funder <strong>of</strong> public hospital services, <strong>and</strong> also take full funding <strong>and</strong> policy responsibility for GP<br />
<strong>and</strong> primary health care <strong>and</strong> aged care. This means the Commonwealth will have a strong<br />
incentive not to cost shift into the hospital system – because it will be left footing the majority<br />
share <strong>of</strong> the bill for expensive acute care services in public hospitals if it does. The IHPA will<br />
also provide binding independent arbitration on cost-shifting <strong>and</strong> boundary issues, <strong>and</strong> on<br />
cross-border charging between states, to further reduce cost shifting.<br />
Historically, the Commonwealth <strong>and</strong> the states have blamed each other for poor service<br />
delivery <strong>and</strong> performance. Under the National <strong>Health</strong> <strong>and</strong> Hospitals Network, the<br />
Commonwealth will set strong national st<strong>and</strong>ards – <strong>and</strong> it will provide the resources to deliver<br />
them. This document outlines new investments <strong>of</strong> $7.3 billion – linked to improving waiting<br />
times in our hospitals <strong>and</strong> improving access to comprehensive GP <strong>and</strong> primary health care<br />
services in the community.<br />
8 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
These reforms will deliver better health <strong>and</strong> hospitals by helping patients receive more<br />
seamless care across sectors <strong>of</strong> the health system. They will improve the quality <strong>of</strong> care<br />
patients receive through high-performance st<strong>and</strong>ards <strong>and</strong> improved engagement <strong>of</strong> local<br />
clinicians. They will provide a secure funding base for health <strong>and</strong> hospitals into the future.<br />
1.2. Reforming the way health services are delivered to keep people healthier<br />
<strong>and</strong> better respond to patients’ needs<br />
The National <strong>Health</strong> <strong>and</strong> Hospitals Network will ensure that services are designed around the<br />
needs <strong>of</strong> patients, <strong>and</strong> more strongly oriented to early intervention <strong>and</strong> high quality integrated<br />
care in the community.<br />
The Commonwealth’s role as the majority funder across the entire health system will provide a<br />
foundation for a health system that helps Australians stay healthy <strong>and</strong> out <strong>of</strong> hospital. By footing<br />
the majority <strong>of</strong> the hospital bill, for the first time, the Commonwealth will have a direct financial<br />
interest in driving better integration <strong>of</strong> care for patients <strong>and</strong> ensuring that resources are allocated<br />
more efficiently across the health system. Better treatment in the community will help keep<br />
Australians healthy <strong>and</strong> out <strong>of</strong> hospital. In many cases, it will also keep people in the workforce<br />
<strong>and</strong> therefore improve workforce participation <strong>and</strong> productivity – a crucial economic reform.<br />
To deliver better early intervention <strong>and</strong> high quality integrated care in the community, the<br />
Government will implement measures that:<br />
››<br />
focus on prevention <strong>and</strong> early intervention, rather than waiting until patients become<br />
more unwell;<br />
››<br />
organise care around the needs <strong>of</strong> patients, rather than governments or service providers;<br />
››<br />
ensure patients experience smoother transitions between different kinds <strong>of</strong> care;<br />
››<br />
exp<strong>and</strong> access to care outside the acute hospital setting, including GP <strong>and</strong> primary health<br />
care, aged care <strong>and</strong> sub-acute care, as well as ensuring better integration within <strong>and</strong><br />
between these sectors; <strong>and</strong><br />
››<br />
make much better use <strong>of</strong> patients’ health information to improve the quality <strong>of</strong> care they<br />
receive, <strong>and</strong> reduce inefficiency <strong>and</strong> avoidable errors.<br />
These reforms will improve patients’ quality <strong>of</strong> life, take pressure <strong>of</strong>f our public hospitals, <strong>and</strong><br />
improve the financial sustainability <strong>of</strong> our health <strong>and</strong> hospital system.<br />
Delivering better health <strong>and</strong> better hospitals 9
Responding to the challenge <strong>of</strong> chronic disease through prevention, early intervention<br />
<strong>and</strong> coordinated care for patients with diabetes<br />
Central to keeping Australians healthy will be countering the high <strong>and</strong> increasing rates <strong>of</strong><br />
chronic disease, much <strong>of</strong> which is avoidable. That is why the Government is tackling the<br />
lifestyle related risks that cause chronic disease – targeting smoking in particular. To achieve<br />
this, the Government will:<br />
››<br />
increase the tobacco excise by 25 per cent above normal CPI adjustments;<br />
››<br />
require plain packaging for cigarettes; <strong>and</strong><br />
››<br />
implement the largest ever national public education campaign on smoking.<br />
The Government will also ensure patients suffering from chronic disease are able to access<br />
personalised care that better responds to their needs, <strong>and</strong> helps them stay healthy over time.<br />
Coordinated care for Australians living with diabetes is an important first step in transforming<br />
the way Australians with long term illness are treated. It will benefit patients by ensuring that:<br />
››<br />
their GP is supported to manage their condition <strong>and</strong> keep them healthy over time;<br />
››<br />
they have access to the services they need to manage their condition;<br />
››<br />
they play a more significant role, guided by their GP, in determining their own care<br />
plans; <strong>and</strong><br />
››<br />
their care, which will <strong>of</strong>ten involve multiple health pr<strong>of</strong>essionals, is coordinated to meet<br />
their needs.<br />
Increasing access to high quality GP <strong>and</strong> primary health care<br />
Building on its funding <strong>and</strong> policy responsibility for GP <strong>and</strong> primary health care, the<br />
Government will strengthen these services <strong>and</strong> drive improved integration to ensure patients<br />
receive better care in the community. These reforms will help deliver more appropriate <strong>and</strong><br />
convenient care for patients, <strong>and</strong> take pressure <strong>of</strong>f public hospital services:<br />
››<br />
Medicare Locals will help improve access to services <strong>and</strong> integration <strong>of</strong> services – both<br />
with other primary health care services <strong>and</strong> with Local Hospital Networks <strong>and</strong> aged care<br />
services.<br />
› › Communities will have access to GP advice <strong>and</strong> services after hours, with more GPs<br />
available in the community, <strong>and</strong> 24 hour telephone assistance to provide advice <strong>and</strong> place<br />
Australians in contact with a GP service in their community when they need it, coordinated<br />
by Medicare Locals.<br />
10 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
››<br />
Australians will have better access to integrated care provided by teams <strong>of</strong> primary health<br />
care providers through a major investment in around 23 new GP Super Clinics <strong>and</strong> 425<br />
upgrades to GP <strong>and</strong> primary health care services to provide GP Super Clinic-style services.<br />
››<br />
Increases in GP training places to record levels will deliver more doctors providing primary<br />
health care services.<br />
››<br />
Reforms to GP <strong>and</strong> primary health care provide a platform for better integration <strong>of</strong> mental<br />
health care now, <strong>and</strong> for further reforms to mental health services into the future –<br />
including through the Commonwealth providing greater policy <strong>and</strong> funding leadership for<br />
specialist community mental health services over time.<br />
Improving aged care <strong>and</strong> sub-acute care to help patients access more appropriate,<br />
better integrated care<br />
The Government will make significant investments <strong>and</strong> reforms to sub-acute care <strong>and</strong> aged<br />
care, recognising that many patients with significant care needs could be better served by care<br />
that is more appropriate to their needs, <strong>and</strong> supported to make smoother transitions between<br />
different kinds <strong>of</strong> care. These reforms will also help take the pressure <strong>of</strong>f acute hospital<br />
services.<br />
By taking full funding <strong>and</strong> policy responsibility for aged care services, including the Home <strong>and</strong><br />
Community Care Program (HACC), the Government will deliver simplified assessments across<br />
all forms <strong>of</strong> aged care, <strong>and</strong> more integrated care so older Australians experience smoother<br />
transitions as their needs change. The Government will work with the full spectrum <strong>of</strong> aged<br />
care providers – including community <strong>and</strong> respite care – to ensure that they are better<br />
supported in:<br />
››<br />
helping older Australians <strong>and</strong> their families receive different types <strong>of</strong> care services as their<br />
needs change;<br />
››<br />
working with Local Hospital Networks to identify appropriate care options that best suit<br />
the needs <strong>of</strong> older Australians <strong>and</strong> avoid unnecessary hospital stays, including through<br />
sub‐acute <strong>and</strong> step-down care; <strong>and</strong><br />
››<br />
working with Medicare Locals to improve older Australians’ access to high quality GP <strong>and</strong><br />
primary health care services in their local community.<br />
In addition to these investments today, the Government has provided terms <strong>of</strong> reference to the<br />
Productivity Commission to undertake a major inquiry into the aged care sector, to ensure that<br />
it is equipped to meet the challenges <strong>of</strong> tomorrow.<br />
Delivering better health <strong>and</strong> better hospitals 11
A major investment in sub-acute care will ensure patients’ transitions in <strong>and</strong> out <strong>of</strong> hospital are<br />
smoother – delivering more appropriate care <strong>and</strong> reducing the risk <strong>of</strong> readmission. For many<br />
patients this will reduce the need for acute hospital care.<br />
A personally controlled electronic health record system<br />
The Government will make a l<strong>and</strong>mark $467 million investment in an electronic health record<br />
system, so that all Australians have access to a personally controlled electronic health record if<br />
they choose to. This will enable better <strong>and</strong> safer care, help patients transition more smoothly<br />
between health care providers, <strong>and</strong> reduce waste.<br />
Australians who choose to use this service – <strong>and</strong> their chosen health care providers – will<br />
have better access to their health information such as medications, test results <strong>and</strong> allergies<br />
when <strong>and</strong> where they need it. Patients will control what is stored on their health records <strong>and</strong><br />
will decide which health <strong>and</strong> medical pr<strong>of</strong>essionals can view or add to their files, meaning<br />
privacy will be strengthened, compared to the current fragmented, paper-based system. The<br />
Government will work with the health sector to ensure the new e-health infrastructure securely<br />
<strong>and</strong> efficiently connects current data systems.<br />
Under this system, critical information will follow patients as they move through different<br />
health <strong>and</strong> hospital services, rather than being physically isolated amongst a number <strong>of</strong> health<br />
services. More accurate patient information will also better equip health pr<strong>of</strong>essionals to tailor<br />
patients’ care to their needs, <strong>and</strong> will help reduce complications <strong>and</strong> duplication. This will be<br />
particularly valuable in helping the growing number <strong>of</strong> people with long term illness manage<br />
their conditions more effectively, as this <strong>of</strong>ten involves them seeing several care providers <strong>and</strong><br />
taking several types <strong>of</strong> medication.<br />
As a condition <strong>of</strong> this investment, states will be required to commit to making the investments<br />
required to link public hospital data systems into the electronic health record system – around<br />
$286 million over the next four years.<br />
1.3. Investments <strong>and</strong> reforms to deliver better access to care through more<br />
services today<br />
The establishment <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospital Network will deliver important changes<br />
to the way health services are organised <strong>and</strong> delivered, <strong>and</strong> better equip our health system<br />
to serve the Australian community well into the future. Building on these changes, the<br />
Government is also investing in key gaps <strong>and</strong> pressure points in our health system today – to<br />
deliver more easily accessible, <strong>and</strong> higher quality services to patients right now.<br />
12 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
In total, the Government will invest an additional $7.3 billion as part <strong>of</strong> establishing the<br />
National <strong>Health</strong> <strong>and</strong> Hospitals Network. This substantial investment will begin rolling out from<br />
1 July 2010, including:<br />
››<br />
Hospitals – to increase the number <strong>of</strong> beds, <strong>and</strong> over time deliver quicker access to<br />
emergency department treatment, <strong>and</strong> shorter elective surgery waiting times in public<br />
hospitals ($3.5 billion).<br />
››<br />
GP <strong>and</strong> primary health care services – to deliver high quality integrated care in the<br />
community, <strong>and</strong> take pressure <strong>of</strong>f public hospital services ($1.2 billion).<br />
››<br />
Workforce – to ensure there are more doctors, nurses <strong>and</strong> allied health pr<strong>of</strong>essionals<br />
across the country to meet the growing need for health <strong>and</strong> hospital services ($1.2 billion).<br />
››<br />
Aged care – to provide more aged care places <strong>and</strong> beds for older Australians<br />
($813 million, including $533 million <strong>of</strong> new investment).<br />
››<br />
Mental health – to provide a foundation for better mental health care, <strong>and</strong> help young<br />
people get access to mental health services ($176 million, including $123 million <strong>of</strong> new<br />
investment).<br />
››<br />
E-health – to deliver a personally controlled electronic health record system ($467 million).<br />
››<br />
Prevention – to tackling the lifestyle related risks that cause chronic disease – targeting<br />
smoking in particular.<br />
A detailed breakdown <strong>of</strong> these investments is provided in Appendix B.<br />
The Government’s substantial new investments will deliver better access to services now,<br />
improve care for patients, <strong>and</strong> build the system’s capacity to meet the needs <strong>of</strong> the future.<br />
Additional funding is provided consistent with the Commonwealth Government’s fiscal rules,<br />
including holding spending growth to two per cent in real terms.<br />
When added to the Government’s previous investments, the health <strong>and</strong> hospitals system<br />
is benefitting from a major step-up in its funding – both now <strong>and</strong> into the future. This is<br />
demonstrated in figure one below, which shows the combined impact <strong>of</strong> the Government’s<br />
investments through:<br />
››<br />
a major increase in funding provided through the National <strong>Health</strong>care Agreement;<br />
››<br />
guaranteeing the Commonwealth’s increased contribution to growth in hospital costs by<br />
becoming the majority funder <strong>of</strong> public hospital services; <strong>and</strong><br />
› › a further $7.3 billion in investments to build on the establishment <strong>of</strong> the National <strong>Health</strong><br />
<strong>and</strong> Hospitals Network, as outlined in this document.<br />
Delivering better health <strong>and</strong> better hospitals 13
Figure 1: Additional Commonwealth Government health <strong>and</strong> hospital<br />
expenditure under the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
30,000<br />
25,000<br />
Change <strong>of</strong><br />
Government<br />
End <strong>of</strong> the<br />
future forward<br />
estimates<br />
*Only base funding<br />
shown beyond<br />
forward estimates<br />
$ million<br />
20,000<br />
15,000<br />
10,000<br />
5,000<br />
2003-04 2005-06 2007-08 2009-10 2011-12 2013-14* 2015-16 2017-18 2019-20<br />
Additional funding provided since the release <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
Additional Benefits to all states from National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
Other new Australian Government hospital funding announced to date<br />
(including Emergency <strong>Department</strong>s, elective surgery <strong>and</strong> hospital capital funding)<br />
Additional funding provided through the new National <strong>Health</strong> Care Agreement<br />
Old Australian <strong>Health</strong> Care Agreements<br />
Source: Commonwealth Budget Papers, Commonwealth <strong>Department</strong> <strong>of</strong> <strong>Health</strong> <strong>and</strong> <strong>Ageing</strong> <strong>and</strong> <strong>Department</strong> <strong>of</strong> the Prime<br />
Minister <strong>and</strong> Cabinet analysis.<br />
14 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
2. Why we are acting: challenges facing our health system today<br />
There is strong evidence demonstrating that the Australian health <strong>and</strong> hospital system is at a<br />
tipping point. The time to act is now, <strong>and</strong> bold reform is necessary to ensure that Australians<br />
can access a high quality health system that is sustainable into the future. Some <strong>of</strong> the major<br />
challenges facing our health <strong>and</strong> hospital system are outlined below.<br />
2.1 A system that isn’t prepared for future challenges<br />
While Australia’s health system serves most Australians well, at a cost to the community<br />
around the average <strong>of</strong> other advanced nations, it is facing a number <strong>of</strong> serious challenges:<br />
››<br />
An ageing population will substantially increase both health care needs <strong>and</strong> expenditure,<br />
while further constraining our health workforce. The 2010 Intergenerational Report<br />
forecasts the proportion <strong>of</strong> our population aged over 65 will increase from 14 per cent in<br />
2010 to 23 per cent by 2050.<br />
››<br />
Population growth will create the need for more health services, new investment in health<br />
infrastructure <strong>and</strong> an exp<strong>and</strong>ed health workforce.<br />
››<br />
Costs have increased sharply in recent years <strong>and</strong> are expected to continue growing. The<br />
2010 Intergenerational Report projects health costs will increase from 15 per cent <strong>of</strong> all<br />
Commonwealth Government spending now (4.0 per cent <strong>of</strong> GDP) to 26 per cent by 2050<br />
(7.1 per cent <strong>of</strong> GDP).<br />
2.2 Too much blame <strong>and</strong> fragmentation between governments<br />
Australia currently has eight different state <strong>and</strong> territory health systems. The distribution<br />
<strong>of</strong> responsibilities for health between different levels <strong>of</strong> government is blurred, resulting in<br />
duplication, cost-shifting <strong>and</strong> blame-shifting. Patients find it hard to work out the level <strong>of</strong><br />
government accountable for their care, when all they want is the services they need.<br />
Delivering better health <strong>and</strong> better hospitals 15
2.3 Too much pressure on public hospitals <strong>and</strong> health pr<strong>of</strong>essionals<br />
Our public hospital system is struggling to cope with growing patient dem<strong>and</strong> <strong>and</strong> stretched<br />
budgets. For more than half a decade, almost one in six elective surgery patients <strong>and</strong> one<br />
in three people attending emergency departments have been waiting longer than the<br />
recommended time for treatment.<br />
Australia’s rates <strong>of</strong> hospital admission are above the Organisation for Economic Cooperation<br />
<strong>and</strong> Development (OECD) average <strong>and</strong> significantly higher than comparable countries such as<br />
the United States, New Zeal<strong>and</strong>, <strong>and</strong> Canada. This pressure <strong>and</strong> constant strain on resources is<br />
also felt in the everyday working lives <strong>of</strong> health pr<strong>of</strong>essionals.<br />
2.4 Shortages <strong>of</strong> doctors, nurses <strong>and</strong> health pr<strong>of</strong>essionals<br />
Large parts <strong>of</strong> Australia are experiencing health workforce shortages. Many <strong>of</strong> the problems<br />
with our health system today arise because there are not enough health pr<strong>of</strong>essionals to meet<br />
the dem<strong>and</strong> for services.<br />
Workforce shortages are most acute outside Australia’s major cities. The number <strong>of</strong> GPs per<br />
100,000 head <strong>of</strong> population varies from under 60 in very remote Australia through to almost<br />
200 GPs per 100,000 people in major cities. The majority <strong>of</strong> allied health practitioners also<br />
work in metropolitan locations. Only 64 allied health workers per 100,000 population work in<br />
very remote areas <strong>of</strong> Australia, compared to 354 per 100,000 in major cities.<br />
2.5 Gaps <strong>and</strong> poor coordination in health services that people need<br />
Too many patients are either falling through the gaps or receiving uncoordinated care. Changes<br />
that streamline the delivery <strong>of</strong> care <strong>and</strong> remove fragmentation in services are long overdue,<br />
particularly for people living with chronic disease. In addition, not all Australians get the<br />
services they need, <strong>and</strong> many people are unable to access out <strong>of</strong> hours GP services.<br />
Limited planning for GP <strong>and</strong> primary health care services, including identifying <strong>and</strong> responding<br />
to gaps in services, has contributed to this. The Medicare Benefits Schedule (MBS) – the<br />
principal means by which GP <strong>and</strong> primary health care is funded in Australia – provides limited<br />
support for health pr<strong>of</strong>essionals to work together to improve patient care.<br />
Access gaps <strong>and</strong> poor coordination between services contribute to high rates <strong>of</strong> hospitalisation<br />
in Australia, a proportion <strong>of</strong> which could be avoided. The Australian Institute <strong>of</strong> <strong>Health</strong> <strong>and</strong><br />
Welfare has estimated that potentially preventable hospitalisations represented 9.3 per cent <strong>of</strong><br />
all hospitalisations in 2007–08.<br />
16 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
2.6 The large <strong>and</strong> increasing burden <strong>of</strong> chronic disease<br />
Chronic diseases already represent a major challenge for Australia’s health <strong>and</strong> hospital system,<br />
<strong>and</strong> are estimated to be responsible for more than 80 per cent <strong>of</strong> the burden <strong>of</strong> disease <strong>and</strong><br />
injury in Australia. More than 50 per cent <strong>of</strong> GP consultations are for people with a chronic<br />
condition.<br />
The burden <strong>of</strong> chronic disease is projected to dramatically increase into the future. By<br />
2032–33 combined spending on cardiovascular <strong>and</strong> respiratory diseases is projected to be<br />
around $40 billion annually, while spending on type 2 diabetes is projected to increase by 520<br />
per cent between 2002–03 <strong>and</strong> 2032–33.<br />
2.7 Insufficient alternatives to acute care beds<br />
Many Australians are unnecessarily admitted or readmitted to hospital due to a lack <strong>of</strong><br />
palliative <strong>and</strong> sub-acute care services (such as rehabilitation, geriatric <strong>and</strong> psychogeriatric care)<br />
in the community. This is a particular challenge for older Australians.<br />
People with mental illness also experience a lack <strong>of</strong> community based sub-acute facilities,<br />
which can be particularly important as a step up or step down between hospital <strong>and</strong><br />
community based care.<br />
2.8 Inconsistent <strong>and</strong> inadequate access to mental health services<br />
Australia’s community mental health system for people with severe mental illness remains<br />
fragmented. The quality <strong>of</strong> services vary, <strong>and</strong> service coordination remains poor. This means<br />
that many people with severe mental illness find it difficult to access the care appropriate for<br />
their needs, or fall through the cracks between services. On discharge, patients may find it<br />
difficult to access appropriate step-down or sub-acute care. Many will experience a ‘revolving<br />
door’ <strong>of</strong> repeated crisis <strong>and</strong> admission to hospitals.<br />
While young people are most in need <strong>of</strong> help, they are the least likely age group to receive it.<br />
Only 25 per cent <strong>of</strong> 16–24 year olds with a mental illness have accessed treatment, compared<br />
to 35 per cent <strong>of</strong> all people with a mental illness.<br />
Delivering better health <strong>and</strong> better hospitals 17
2.9 Fragmented patient health information<br />
Patients currently have limited access to <strong>and</strong> control over their own health information. <strong>Health</strong><br />
information is largely fragmented across the record systems <strong>of</strong> each health care provider they<br />
have seen. Each health care provider usually only has an incomplete record <strong>of</strong> a patient’s<br />
medical history <strong>and</strong> care needs. This means a patient’s critical health information may not be<br />
available when <strong>and</strong> where they are being treated, especially in emergencies or when seeing<br />
multiple doctors <strong>and</strong> health pr<strong>of</strong>essionals.<br />
As well as being frustrating for patients <strong>and</strong> their health care providers, this can also have<br />
damaging effects on patients’ health <strong>and</strong> the quality <strong>of</strong> care they receive . Many adverse drug<br />
events <strong>and</strong> poor transitions from one health care setting to another could be avoided with<br />
better access to patients’ health information across care settings.<br />
2.10 Challenges in ensuring our aged care system meets the needs <strong>of</strong> growing<br />
numbers <strong>of</strong> older Australians<br />
The aged care system is currently fragmented, with responsibilities for community care divided<br />
between the Commonwealth <strong>and</strong> the states. This leads to overlap between the services<br />
provided by different governments’ programs. It leads to care being too closely tied to program<br />
<strong>and</strong> funding criteria <strong>and</strong> not responsive enough to people’s changing needs.<br />
Older Australians, their families <strong>and</strong> carers find it hard to access the services they need <strong>and</strong><br />
<strong>of</strong>ten do not know what services are available. This is because different levels <strong>of</strong> government<br />
<strong>and</strong> different programs tend to <strong>of</strong>fer information on their own services rather than on the aged<br />
care system as a whole.<br />
The supply <strong>of</strong> high level residential care is not keeping up with increased dem<strong>and</strong> from<br />
population ageing. This has been accompanied by falls in recent years in the numbers <strong>of</strong><br />
registered <strong>and</strong> enrolled nurses working in residential aged care. In addition, too many older<br />
Australians are unnecessarily admitted to hospital when better care in the community would<br />
have kept them healthy <strong>and</strong> out <strong>of</strong> hospital.<br />
2.11 An unsustainable funding model, with insufficient transparency<br />
The cost <strong>of</strong> providing health care is expected to continue to increase into the future. But state<br />
government revenue growth has not kept pace with growing health care costs in recent years.<br />
In the five years to 2007–08, public hospital expenditure has grown at an average <strong>of</strong> close<br />
to ten per cent per year. Projections show that by 2045–46, health spending alone would be<br />
more than all revenue collected by state <strong>and</strong> local governments.<br />
18 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Despite recent improvements through the National <strong>Health</strong>care Agreement, the transparency <strong>of</strong><br />
health care funding <strong>and</strong> spending at a local level is still relatively limited. This means taxpayers<br />
<strong>and</strong> governments are unable to make robust comparisons across states or health services, <strong>and</strong><br />
easily identify where there is inefficiency.<br />
2.12 Not enough local or clinical engagement<br />
Many clinicians <strong>and</strong> citizens are not adequately involved in decisions about the delivery <strong>of</strong><br />
health services in their local community. Current arrangements fail to make the most <strong>of</strong> the<br />
expertise <strong>and</strong> commitment <strong>of</strong> our clinical workforce. It also means that some services are<br />
poorly tailored to community needs.<br />
In addition, the National <strong>Health</strong> <strong>and</strong> Hospitals Reform Commission (NHHRC) indicated that<br />
adverse events result in approximately 4,550 unnecessary deaths a year <strong>and</strong> add a cost <strong>of</strong><br />
around $2 billion annually to the health budget.<br />
3. Building on strong foundations: what the Government has<br />
already done<br />
Since 2007, the Government has undertaken major reforms across health <strong>and</strong> hospitals to<br />
tackle key pressure points in the system: increasing funding for public hospitals, targeting<br />
key pressure points such as emergency departments <strong>and</strong> elective surgery <strong>and</strong> training more<br />
doctors <strong>and</strong> nurses.<br />
3.1 Increased funding for health <strong>and</strong> hospitals<br />
In November 2008, the Government signed a $64 billion agreement for health <strong>and</strong> hospitals<br />
funding, which delivered a 50 per cent increase on the previous Australian <strong>Health</strong> Care<br />
Agreement. Additional funding was linked to a range <strong>of</strong> performance indicators across<br />
prevention, primary <strong>and</strong> community care, hospital <strong>and</strong> related care, aged care, the patient<br />
experience <strong>and</strong> sustainability. States <strong>and</strong> territories agreed to national outcomes <strong>and</strong> outputs,<br />
challenging new targets, <strong>and</strong> increased service levels.<br />
Delivering better health <strong>and</strong> better hospitals 19
The agreement also included:<br />
››<br />
$1.1 billion to train more doctors, nurses <strong>and</strong> allied health workers in the largest single<br />
investment ever made by an Australian government in the health workforce;<br />
››<br />
$750 million to take pressure <strong>of</strong>f emergency departments, with 37 hospitals around the<br />
country receiving upgrades as a result <strong>of</strong> this investment; <strong>and</strong><br />
››<br />
$500 million for sub-acute care facilities including rehabilitation, palliative care, geriatric<br />
evaluation <strong>and</strong> psychogeriatric services.<br />
In addition, the Government has invested $600 million in an elective surgery waiting list<br />
reduction plan that has already delivered more than 62,000 additional procedures <strong>and</strong> new<br />
elective surgery equipment <strong>and</strong> operating theatres for 125 hospitals.<br />
3.2 More doctors, nurses <strong>and</strong> allied health pr<strong>of</strong>essionals – <strong>and</strong> making smarter<br />
use <strong>of</strong> our health workforce<br />
As part <strong>of</strong> the November 2008 COAG agreement, the Government made an unprecedented<br />
investment in training more doctors, nurses <strong>and</strong> allied health pr<strong>of</strong>essionals. This includes:<br />
››<br />
raising the number <strong>of</strong> GP training places to a total <strong>of</strong> 812 by 2011;<br />
››<br />
73 additional specialist training places in the private sector each year;<br />
››<br />
additional funding to train nursing, allied health <strong>and</strong> medical supervisors; <strong>and</strong><br />
››<br />
establishing <strong>Health</strong> Workforce Australia to plan for future workforce needs.<br />
The Government is also working to make smarter use <strong>of</strong> our workforce by providing nurses <strong>and</strong><br />
midwives with access to the MBS <strong>and</strong> Pharmaceutical Benefits Scheme.<br />
3.3 Comprehensive health care that is close to home through GP Super Clinics<br />
To provide comprehensive services close to home, 36 GP Super Clinics are being built across<br />
the country. GP Super Clinics bring together GPs, nurses, visiting medical specialists, allied<br />
health pr<strong>of</strong>essionals <strong>and</strong> other health care providers to provide integrated, multidisciplinary<br />
care in a single convenient location. This infrastructure will particularly benefit Australians with<br />
chronic <strong>and</strong> complex diseases.<br />
20 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
3.4 Focusing on prevention rather than cure<br />
The Government has made an $872 million investment in preventative health programs to<br />
be rolled out in schools, workplaces <strong>and</strong> local communities with a high incidence <strong>of</strong> chronic<br />
disease. These programs will focus on reducing lifestyle risk factors such as smoking <strong>and</strong><br />
obesity <strong>and</strong> increasing physical activity <strong>and</strong> healthy eating.<br />
To tackle binge drinking amongst young people, the Government has increased the excise on<br />
ready-to-drink beverages <strong>and</strong> implemented a National Binge Drinking Strategy.<br />
3.5 Closing the life expectancy gap between Indigenous <strong>and</strong><br />
non-Indigenous Australians<br />
To help close the gap between Indigenous <strong>and</strong> non-Indigenous health outcomes, the<br />
Commonwealth, states <strong>and</strong> territories are investing $1.6 billion in measures to reduce the<br />
burden <strong>of</strong> chronic disease in the Indigenous population — the biggest contributor to the life<br />
expectancy gap. These measures include support for tackling high rates <strong>of</strong> smoking in the<br />
Indigenous community, <strong>and</strong> improving management <strong>of</strong> chronic diseases such as diabetes<br />
through additional support for primary health care practices with Indigenous patients.<br />
3.6 Addressing workforce shortages in regional <strong>and</strong> rural Australia<br />
The Government has recognised the challenges faced by Australians living in regional <strong>and</strong> rural<br />
areas in accessing basic health care services. As part <strong>of</strong> a $134 million investment, some 500<br />
communities will benefit from a number <strong>of</strong> new initiatives, which means that around 2,400<br />
doctors in rural Australia will, for the first time, become eligible for financial support to stay in<br />
rural <strong>and</strong> remote areas.<br />
3.7 Investing in hospitals, medical research <strong>and</strong> clinical training infrastructure<br />
In the first ever major investment by a Commonwealth Government in state health<br />
infrastructure, $3.2 billion has been invested in 35 infrastructure projects across the country,<br />
including:<br />
››<br />
$1.5 billion to upgrade 18 hospitals around the country;<br />
››<br />
$1.3 billion over six years to modernise Australia’s cancer infrastructure — including two<br />
comprehensive cancer centres in Sydney <strong>and</strong> Melbourne linked into a network <strong>of</strong> regional<br />
cancer centres; <strong>and</strong><br />
››<br />
$430 million to upgrade 12 medical research <strong>and</strong> clinical training facilities.<br />
Delivering better health <strong>and</strong> better hospitals 21
3.8 Sustainable, high quality aged care<br />
The Government is committed to sustainable, high quality aged care <strong>and</strong> to providing funding<br />
for more services to older Australians. Since November 2007, more than 10,000 new aged<br />
care places have become operational <strong>and</strong> the Government is making more than 12,000 new<br />
aged care places available this year, with a strong focus on community care. Overall, the<br />
Government has increased total funding for aged <strong>and</strong> community care from $8.3 billion in<br />
2007–08 to $10.0 billion in 2009–10, an increase <strong>of</strong> around 20 per cent.<br />
3.9 Improving access to dental care<br />
The Australian Government is committed to exp<strong>and</strong>ing access to dental care in Australia.<br />
The Medicare Teen Dental Plan was implemented on 1 July 2008 <strong>and</strong> to 31 March 2010 has<br />
provided $116 million in benefits for 792,321 preventive dental check-ups.<br />
The Government remains committed to providing $290 million to states to fund around one<br />
million additional public dental services, including priority treatment for people who have<br />
chronic conditions relating to their oral health. This would be funded by closing the chronic<br />
disease dental scheme to make funding available for the introduction <strong>of</strong> a fairer <strong>and</strong> more<br />
accessible Commonwealth Dental <strong>Health</strong> Program, but the Senate has prevented closure<br />
<strong>of</strong> the scheme. This means the Government has not to date been able to implement the<br />
Commonwealth Dental <strong>Health</strong> Program.<br />
3.10 A more financially sustainable health system<br />
The Government has undertaken reforms to health care spending to ensure our system<br />
remains fair <strong>and</strong> sustainable into the future. This includes rebalancing support for private<br />
health insurance, so that those with greater capacity to pay do so. This is expected to save<br />
$100 billion over the next 40 years, with coverage expected to remain at around 99.7 per cent<br />
<strong>of</strong> existing levels. At this time this savings measure has not been passed by the Senate.<br />
22 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
4. How we got here: listening to the community <strong>and</strong> experts, <strong>and</strong><br />
working with the states<br />
At the same time as making investments to fix immediate gaps, the Government set in train<br />
long-term, system-wide health reform. It commissioned the most comprehensive structural<br />
review <strong>of</strong> Australia’s health <strong>and</strong> hospital system in 20 years, by establishing the National<br />
<strong>Health</strong> <strong>and</strong> Hospitals Reform Commission. The NHHRC’s final report, which was released at the<br />
end <strong>of</strong> July 2009, contained 123 recommendations for immediate <strong>and</strong> longer‐term reforms.<br />
Following the release <strong>of</strong> the NHHRC report, the Government undertook an extensive<br />
consultation process to test the report’s recommendations with patients, health pr<strong>of</strong>essionals<br />
<strong>and</strong> the Australian people. In 2009 <strong>and</strong> 2010, the Prime Minister, <strong>Health</strong> Minister, <strong>and</strong> other<br />
Ministers conducted more than 100 consultations with patients, health pr<strong>of</strong>essionals <strong>and</strong> the<br />
public, as displayed in figure two.<br />
Figure 2: Locations <strong>of</strong> Government’s health reform consultations<br />
WA<br />
NT<br />
QLD<br />
ACT<br />
NSW<br />
QLD<br />
VIC<br />
NT<br />
SA<br />
TAS<br />
WA<br />
National<br />
TOTAL<br />
2<br />
28<br />
15<br />
17<br />
2<br />
10<br />
6<br />
12<br />
11<br />
103<br />
SA<br />
NSW<br />
VIC<br />
ACT<br />
TAS<br />
Delivering better health <strong>and</strong> better hospitals 23
The Government has listened carefully to the expert advice <strong>and</strong> views put forward by the<br />
Australian community. Key feedback from consultations indicated a community desire for:<br />
››<br />
a stronger Commonwealth Government leadership role, coupled with higher st<strong>and</strong>ards <strong>and</strong><br />
increased funding for public hospitals;<br />
››<br />
reduced health sector bureaucracy, simplified governance <strong>and</strong> accountability, <strong>and</strong> greater<br />
autonomy <strong>and</strong> flexibility at the local level;<br />
››<br />
better access to multidisciplinary primary health care;<br />
››<br />
better public hospital services <strong>and</strong> waiting times;<br />
››<br />
better access to health care in rural Australia <strong>and</strong> disadvantaged areas; <strong>and</strong><br />
››<br />
improved integration <strong>of</strong> information technology across our health system.<br />
A full response to the NHHRC’s recommendations is provided at Appendix C.<br />
Another source <strong>of</strong> expert input has been the 2010 Intergenerational Report. This report<br />
projected that growth in all categories <strong>of</strong> Commonwealth health spending would increase,<br />
driven by population growth <strong>and</strong> ageing, increased dem<strong>and</strong> for health services, <strong>and</strong> new<br />
technology. It provides further evidence that reform is needed to ensure the ongoing<br />
sustainability <strong>of</strong> health <strong>and</strong> hospital services.<br />
The Government has also worked closely with states to develop <strong>and</strong> refine these reforms.<br />
This included extensive discussions at the COAG meeting in December 2009, <strong>and</strong> intensive<br />
negotiations in early 2010.<br />
At the COAG meeting in April 2010, all governments, with the exception <strong>of</strong> Western Australia,<br />
reached an historic agreement to establish the National <strong>Health</strong> <strong>and</strong> Hospitals Network. This<br />
included reaching a comprehensive intergovernmental agreement – the National <strong>Health</strong> <strong>and</strong><br />
Hospitals Network Agreement – which provides policy detail for these reforms, <strong>and</strong> outlines<br />
the responsibilities that governments have committed to in order to deliver the National <strong>Health</strong><br />
<strong>and</strong> Hospitals Network.<br />
The Government is continuing negotiations with Western Australia to seek their agreement<br />
to these reforms, to ensure people in Western Australia receive the full benefits the National<br />
<strong>Health</strong> <strong>and</strong> Hospitals Network will deliver. Funding in this document reflects the establishment<br />
<strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network across all states. However, throughout this<br />
document, the term ‘states’ does not refer to Western Australia unless otherwise specified.<br />
24 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
5. Building the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
The National <strong>Health</strong> <strong>and</strong> Hospitals Network will deliver an effective <strong>and</strong> efficient health system<br />
that will deliver better health <strong>and</strong> better hospitals. It will be funded nationally <strong>and</strong> run locally.<br />
Following these reforms, Governments <strong>and</strong> taxpayers can be confident that health <strong>and</strong> hospital<br />
services are placed on a more financially sustainable footing into the future.<br />
Improving care for those Australians who need it most<br />
<strong>Health</strong> is a major indicator <strong>of</strong> inequity. Poor health contributes to disadvantage, <strong>and</strong><br />
disadvantage contributes to poor health. Indicators such as rates <strong>of</strong> diabetes, rates <strong>of</strong> heart<br />
disease, early deaths <strong>and</strong> infant mortality are all clear markers <strong>of</strong> socio-economic status.<br />
The greatest beneficiaries <strong>of</strong> these reforms will be those Australians who use these core public<br />
services like public hospitals most frequently. The establishment <strong>of</strong> a National <strong>Health</strong> <strong>and</strong><br />
Hospitals Network will help reduce the impact <strong>of</strong> disadvantage on Australians’ access to health<br />
<strong>and</strong> hospital services. For instance:<br />
››<br />
Better GP <strong>and</strong> primary health care will assist disadvantaged Australians, who experience<br />
higher rates <strong>of</strong> avoidable hospitalisation than more well-<strong>of</strong>f Australians.<br />
››<br />
Patients with chronic <strong>and</strong> complex conditions, such as people with severe mental illness,<br />
will benefit from improved integration <strong>of</strong> care <strong>and</strong> smoother transitions between different<br />
health services that they use.<br />
››<br />
Measures to increase support for the rural health workforce, <strong>and</strong> to increase access to<br />
aged care services in rural <strong>and</strong> remote areas, will help address the disparity between health<br />
outcomes for people living in rural <strong>and</strong> remote Australia, <strong>and</strong> for people in metropolitan<br />
Australia.<br />
››<br />
Indigenous <strong>and</strong> disadvantaged Australians are proportionally much greater users <strong>of</strong> public<br />
hospital services than other Australians, <strong>and</strong> will benefit from the Government’s reforms<br />
to public hospital services <strong>and</strong> investments to deliver better access to public hospital care.<br />
Nearly 93 per cent <strong>of</strong> hospital attendances by Indigenous people in 2007–08 were at<br />
public hospitals, compared to 59 per cent for non-Indigenous Australians.<br />
› › Coordinated care for patients with diabetes will be particularly important for improving<br />
the health <strong>of</strong> Indigenous Australians, who suffer from diabetes at much higher rates than<br />
non‐Indigenous Australians.<br />
Delivering better health <strong>and</strong> better hospitals 25
Areas for future action<br />
The Government will continue to work with states <strong>and</strong> other stakeholders to undertake<br />
ongoing reform <strong>and</strong> investment which could be delivered in the future to support the<br />
establishment <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network. In particular, the Government:<br />
››<br />
Will pursue reform <strong>and</strong> further improvements in improving access to mental health services<br />
– particularly for young people – to build on the benefits that will be delivered through<br />
investments in this package.<br />
››<br />
Recognises there is much more to be done to improve access to dental care, <strong>and</strong> is committed<br />
to exp<strong>and</strong>ing access to dental care in Australia. Many Australians experience poor access to<br />
care, <strong>of</strong>ten because there are not enough dentists <strong>and</strong> dental pr<strong>of</strong>essionals. Current estimates<br />
project there will be a shortfall <strong>of</strong> 2.3 million dental services in 2020. People who are socially<br />
<strong>and</strong> economically disadvantaged are much more likely to have poor dental health.<br />
››<br />
Will continue to prioritise aged care reform, with further reforms to ensure the aged care<br />
sector is equipped to meet the challenges <strong>of</strong> tomorrow following the outcomes <strong>of</strong> the<br />
Productivity Commission Inquiry into Aged Care.<br />
A strong focus on delivering reform – now <strong>and</strong> into the future<br />
The Government is already working hard to deliver the National <strong>Health</strong> <strong>and</strong> Hospitals Network.<br />
The Government will work closely with states, health pr<strong>of</strong>essionals, service providers <strong>and</strong> other<br />
stakeholders to ensure that these reforms deliver better health <strong>and</strong> better hospitals for all<br />
Australians. The scale <strong>of</strong> investment, speed <strong>of</strong> rollout <strong>and</strong> interaction between a large number<br />
<strong>of</strong> major reforms mean this will be essential. The Australian community will be given clear, up<br />
to date information about progress <strong>of</strong> the reforms.<br />
Many measures, including funding for additional public hospital services, will commence<br />
on 1 July 2010. These will deliver immediate benefits while foundational reforms – such as<br />
the establishment <strong>of</strong> Local Hospital Networks <strong>and</strong> moving to activity based funding – are<br />
bedded down.<br />
The impact <strong>of</strong> many reforms will extend <strong>and</strong> be realised in the long-term. For instance, the<br />
health <strong>and</strong> quality <strong>of</strong> life benefits <strong>of</strong> prevention measures to reduce smoking will accrue over<br />
decades to come.<br />
The Government, in consultation with states <strong>and</strong> the health sector, will continue to work hard<br />
to deliver these historic reforms. The Government looks forward to ensuring Australians can<br />
access better services <strong>and</strong> more integrated care now, <strong>and</strong> a high quality health system that is<br />
sustainable into the future.<br />
26 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
PART 1 – Reforming the funding<br />
<strong>and</strong> governance <strong>of</strong> health <strong>and</strong><br />
hospitals<br />
Funded nationally<br />
The Commonwealth Government will become the majority funder <strong>of</strong> Australian public<br />
hospitals. The Commonwealth will fund 60 per cent <strong>of</strong> the efficient price <strong>of</strong> public hospital<br />
services, with this price to be determined by a new independent national umpire, IHPA. The<br />
Commonwealth will also fund 60 per cent <strong>of</strong> capital, research <strong>and</strong> training in our public<br />
hospitals; <strong>and</strong> 60 per cent <strong>of</strong> public hospital funding provided through block grants, including<br />
for small rural <strong>and</strong> regional hospitals to meet Community Service Obligations.<br />
The Commonwealth will also take full funding <strong>and</strong> policy responsibility for GP <strong>and</strong> primary<br />
health care services, <strong>and</strong> aged care services.<br />
To improve integration between the acute <strong>and</strong> primary health care sectors – <strong>and</strong> help patients<br />
access more appropriate <strong>and</strong> cost-effective care in the community – the Commonwealth<br />
will also move over time to fund 100 per cent <strong>of</strong> the efficient price <strong>of</strong> primary health care<br />
equivalent outpatient services.<br />
Having one level <strong>of</strong> Government – the Commonwealth – as majority funder across the health<br />
<strong>and</strong> hospital system will ensure there are nationally consistent funding arrangements that<br />
support the best allocation <strong>of</strong> health services throughout the system.<br />
To support these new funding arrangements, around one-third <strong>of</strong> total GST revenue will be<br />
retained by the Commonwealth <strong>and</strong> invested in health <strong>and</strong> hospitals through a National<br />
<strong>Health</strong> <strong>and</strong> Hospitals Network Fund. This will provide an increasing benefit to states over<br />
time, starting with a guaranteed minimum <strong>of</strong> at least $15.6 billion in additional growth costs<br />
absorbed by the Commonwealth from 2014–15 to 2019–20. These reforms provide a secure<br />
funding base for health <strong>and</strong> hospitals into the future. They respond to the risk that states will<br />
not have the financial capacity to meet rapidly increasing health spending obligations in the<br />
longer term.<br />
Delivering better health <strong>and</strong> better hospitals 27
Run locally<br />
To improve responsiveness to local communities’ needs <strong>and</strong> improve clinician engagement,<br />
governance <strong>and</strong> management <strong>of</strong> local health <strong>and</strong> hospital services will be devolved to the local<br />
level. New local institutions will work together to deliver better integration <strong>and</strong> improvements<br />
across the entire health system:<br />
››<br />
Local Hospital Networks will be responsible for managing <strong>and</strong> delivering hospital services.<br />
This will lead to increased autonomy <strong>and</strong> flexibility so that services are more responsive to<br />
local needs.<br />
››<br />
Medicare Locals – independent primary health care organisations with strong links to<br />
local communities <strong>and</strong> health pr<strong>of</strong>essionals – will be established to provide better services,<br />
improve access to care <strong>and</strong> drive integration across GP <strong>and</strong> primary health care services.<br />
››<br />
One stop shops located across the country will ensure Australians can more easily access<br />
information <strong>and</strong> assistance in receiving aged care services.<br />
These institutions will work together to integrate the health system to improve patient<br />
transition between the acute, primary <strong>and</strong> aged care sectors.<br />
To drive transparency <strong>and</strong> efficiency in funding <strong>of</strong> health services, Local Hospital Networks will<br />
be paid on the basis <strong>of</strong> each service they provide to public patients under service agreements<br />
with states. This will reduce waste <strong>and</strong> increase the number <strong>of</strong> services provided for each dollar<br />
invested.<br />
Reported transparently<br />
The Government will introduce clear <strong>and</strong> transparent performance reporting against new,<br />
higher national st<strong>and</strong>ards <strong>and</strong> other performance indicators. Hospital Performance Reports <strong>and</strong><br />
<strong>Health</strong>y Communities Reports (on primary health care performance) will provide performance<br />
information that is nationally consistent <strong>and</strong> locally relevant – including reporting on the<br />
performance <strong>of</strong> every hospital <strong>and</strong> Local Hospital Network in every local community across<br />
Australia. Transparent reporting will allow strong performance to be identified <strong>and</strong> transferred<br />
across the sector <strong>and</strong> allow poor performance to be quickly <strong>and</strong> easily identified, so that<br />
interventions can be made before problems become entrenched. It will also help Australians<br />
make more informed choices about their health services.<br />
The combination <strong>of</strong> national funding <strong>and</strong> st<strong>and</strong>ards, local management <strong>and</strong> service delivery,<br />
<strong>and</strong> transparent reporting, is at the core <strong>of</strong> the new National <strong>Health</strong> <strong>and</strong> Hospitals Network.<br />
The disparate performance <strong>and</strong> operating models <strong>of</strong> states will become a thing <strong>of</strong> the past<br />
with this shift to a single national network.<br />
28 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Chapter 1: FUNDED NATIONALLY:<br />
Reforming FINANCIAL ROLES AND<br />
RESPONSIBILITIES<br />
The Commonwealth <strong>and</strong> states have agreed to major reforms to roles<br />
<strong>and</strong> responsibilities, to ensure future generations <strong>of</strong> Australians continue<br />
to enjoy universally accessible health care.<br />
The Commonwealth Government will become the majority funder <strong>of</strong> the<br />
Australian public hospital system.<br />
The Government will fund:<br />
››<br />
60 per cent <strong>of</strong> the efficient price <strong>of</strong> every public hospital service<br />
provided to public patients;<br />
››<br />
60 per cent <strong>of</strong> recurrent expenditure on research <strong>and</strong> training<br />
undertaken in public hospitals currently funded by states;<br />
››<br />
60 per cent <strong>of</strong> capital expenditure, to maintain <strong>and</strong> improve public<br />
hospital infrastructure;<br />
››<br />
60 per cent <strong>of</strong> public hospital funding provided through block grants,<br />
including for small rural <strong>and</strong> regional hospitals to meet Community<br />
Service Obligations; <strong>and</strong><br />
››<br />
Over time, up to 100 per cent <strong>of</strong> the efficient price <strong>of</strong> ‘primary<br />
health care equivalent’ outpatient services provided to public<br />
hospital patients.<br />
The Commonwealth will also have full funding <strong>and</strong> policy responsibility<br />
for GP <strong>and</strong> primary health care services, <strong>and</strong> for aged care services.<br />
In return for a secure funding base for public hospitals into the future,<br />
the states have committed to becoming part <strong>of</strong> the new National <strong>Health</strong><br />
<strong>and</strong> Hospitals Network. They have committed to system wide reform to<br />
devolve governance, report on performance transparently, <strong>and</strong> meet new<br />
national st<strong>and</strong>ards.<br />
Delivering better health <strong>and</strong> better hospitals 29
A fragmented <strong>and</strong> blame ridden system<br />
The Australian health system is hard to navigate for both patients <strong>and</strong> health pr<strong>of</strong>essionals. It is<br />
characterised by different state <strong>and</strong> territory systems, with a variety <strong>of</strong> funding sources <strong>and</strong> funding<br />
boundaries. A number <strong>of</strong> the problems within the current system can be attributed to lack <strong>of</strong><br />
transparency <strong>and</strong> cohesion, <strong>of</strong>ten arising from lack <strong>of</strong> clear financial leadership. This has resulted in<br />
blame shifting — an issue that has dominated debates on health for a number <strong>of</strong> years.<br />
At its most basic level, blame shifting centres on the relative financial contribution <strong>of</strong> different<br />
levels <strong>of</strong> government. In the last two decades, the most contentious issue arising from<br />
arrangements for hospital funding has been the slow decline over time <strong>of</strong> the Commonwealth’s<br />
share <strong>of</strong> public hospital funding. In 1995–96, the Commonwealth’s share <strong>of</strong> public hospital<br />
funding was over 45 per cent. By the final year <strong>of</strong> the previous Australian <strong>Health</strong> Care<br />
Agreements, it had declined to under 40 per cent. Moreover, under present arrangements, if a<br />
state decides to invest more in health <strong>and</strong> hospital services, the Commonwealth does not make<br />
any contribution.<br />
Cost pressures <strong>and</strong> excess dem<strong>and</strong> within parts <strong>of</strong> the health system have also fed cost shifting<br />
between different levels <strong>of</strong> government. This makes it very hard for Australians to tell which<br />
level <strong>of</strong> government is responsible for their health care, <strong>and</strong> to hold it accountable.<br />
Majority funding responsibility for public hospitals<br />
To overcome fragmentation, blame shifting <strong>and</strong> cost shifting across the health system, the<br />
Commonwealth will ensure that one level <strong>of</strong> government has majority funding responsibility for<br />
the hospital system.<br />
In a fundamental change to hospital funding arrangements, the Commonwealth will increase<br />
its funding contribution to:<br />
››<br />
60 per cent <strong>of</strong> the efficient price <strong>of</strong> every public hospital service provided to public patients;<br />
››<br />
60 per cent <strong>of</strong> recurrent expenditure on research <strong>and</strong> training undertaken in public<br />
hospitals;<br />
››<br />
60 per cent <strong>of</strong> capital expenditure, to maintain <strong>and</strong> improve public hospital infrastructure;<br />
››<br />
60 per cent <strong>of</strong> public hospital funding provided through block grants, including for small rural<br />
<strong>and</strong> regional hospitals to meet Community Service Obligations; <strong>and</strong><br />
› › over time, up to 100 per cent <strong>of</strong> the efficient price <strong>of</strong> primary health care equivalent<br />
outpatient services provided to public hospital patients.<br />
30 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Under these new funding arrangements, the Commonwealth will meet its share <strong>of</strong> the efficient<br />
price <strong>of</strong> all public hospital services provided to public patients under service agreements<br />
between Local Hospital Networks (discussed further in chapter two) <strong>and</strong> states.<br />
The Commonwealth will assume greater financial responsibility by progressively moving<br />
from payment for public hospital services on the basis <strong>of</strong> recurrent expenditure to payment<br />
on the basis <strong>of</strong> a national efficient price for each hospital service. An independent umpire<br />
at arm’s length from Commonwealth <strong>and</strong> state governments, the IHPA, will set the national<br />
efficient price. In doing so it will strike an appropriate balance between reasonable access to<br />
public hospital services, clinical safety <strong>and</strong> quality, efficiency <strong>and</strong> effectiveness, <strong>and</strong> financial<br />
sustainability <strong>of</strong> the public hospital system.<br />
For the first time, this means that where the Commonwealth, on behalf <strong>of</strong> the community,<br />
wants to improve public hospital performance, the Commonwealth will have a direct funding<br />
mechanism to drive improvements, <strong>and</strong> will also be exposed to the cost <strong>of</strong> delivering on that<br />
improvement. From 1 July 2014, the Commonwealth will bear 60 per cent <strong>of</strong> any increased<br />
dem<strong>and</strong>, increased st<strong>and</strong>ards <strong>and</strong> increased community expectations.<br />
Blame shifting over declining shares, base funding <strong>and</strong> indexation rates will be replaced with a<br />
stable, secure funding base.<br />
Primary health care equivalent outpatient services<br />
The Government will also fund 60 per cent <strong>of</strong> the efficient cost <strong>of</strong> outpatient services provided<br />
to public hospital patients. The Commonwealth will work with the states to move to fund<br />
100 per cent <strong>of</strong> the efficient price <strong>of</strong> those outpatient services that are better characterised as<br />
primary health care services.<br />
This reform will help improve integration between the acute <strong>and</strong> primary health care sectors,<br />
<strong>and</strong> help patients access more appropriate <strong>and</strong> cost-effective care in the community.<br />
Some outpatient services are more closely associated with admitted services, whereas others<br />
can be more appropriately associated with primary health care. With the assistance <strong>of</strong> the<br />
states, <strong>and</strong> the increased data that will become available as a result <strong>of</strong> these reforms, the<br />
Government aims to distinguish between these different types <strong>of</strong> outpatient services, <strong>and</strong> over<br />
time, move to funding them in a manner that better reflects the character <strong>of</strong> the service. In<br />
doing this, the Government will ensure patients continue to receive public hospital services free<br />
<strong>of</strong> charge.<br />
Delivering better health <strong>and</strong> better hospitals 31
Support for small regional <strong>and</strong> rural hospitals<br />
The Commonwealth recognises that in some circumstances, particularly in rural <strong>and</strong> remote<br />
Australia, activity based funding will not be able to fully reflect the higher cost bases <strong>and</strong><br />
limited economies <strong>of</strong> scale that smaller hospitals face. This is particularly due to the need to<br />
keep facilities staffed <strong>and</strong> available for patients to access, even when not delivering services, in<br />
order to meet Community Service Obligations.<br />
The Government will ensure new financing arrangements effectively support small regional<br />
<strong>and</strong> rural hospitals. The Government will ensure funding reflects the higher costs associated<br />
with delivering services in regional <strong>and</strong> rural areas <strong>of</strong> Australia, including providing block<br />
funding where appropriate so that small rural <strong>and</strong> regional hospitals can continue to deliver on<br />
Community Service Obligations.<br />
Funding for research <strong>and</strong> training<br />
Funding pressures in public hospitals have <strong>of</strong>ten resulted in limited funding for non-patient<br />
services such as research <strong>and</strong> training, which are essential to building the specialist workforce<br />
for the future <strong>and</strong> retaining expertise within the public hospital system.<br />
The Commonwealth will pay 60 per cent <strong>of</strong> recurrent expenditure on research <strong>and</strong> training<br />
undertaken in public hospitals. The Commonwealth will place strong conditions on this<br />
funding to ensure it is spent consistently with the overall objectives <strong>of</strong> the National <strong>Health</strong> <strong>and</strong><br />
Hospitals Network. This will strengthen links with the research <strong>and</strong> training sector (including<br />
universities) <strong>and</strong> the teaching hospital sector not only through funding arrangements, but also<br />
through improved formal linkages. This is a critical component <strong>of</strong> the reform agenda, bringing<br />
together research, clinical training <strong>and</strong> teaching together to improve care for patients <strong>and</strong> build<br />
the health workforce <strong>of</strong> the future.<br />
Funding for capital expenditure<br />
State governments are currently responsible for meeting the full cost <strong>of</strong> major capital<br />
investments in public hospital infrastructure. With the Commonwealth making a greater<br />
investment in recurrent public hospital services, the Government faces strong incentives to<br />
ensure that public hospitals have appropriate facilities <strong>and</strong> equipment to ensure that they can<br />
continue to provide services efficiently.<br />
The Commonwealth will fund capital on the basis <strong>of</strong> the ‘user cost’ <strong>of</strong> capital, where possible,<br />
which consists <strong>of</strong> a stream <strong>of</strong> payments to cover both depreciation <strong>and</strong> the cost <strong>of</strong> capital.<br />
32 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Major capital planning will continue to be a responsibility <strong>of</strong> states. The capital funding stream<br />
directly paid to each state will vary over time to reflect:<br />
››<br />
the nature <strong>and</strong> location <strong>of</strong> hospital services;<br />
››<br />
service activity; <strong>and</strong><br />
››<br />
size <strong>of</strong> the state’s capital program.<br />
Local Hospital Networks will receive <strong>and</strong> manage payments for minor capital, including for<br />
maintenance <strong>and</strong> small scale operational needs.<br />
The role <strong>of</strong> states <strong>and</strong> territories<br />
In return for the Commonwealth providing a secure funding base for public hospitals into<br />
the future, states have committed to system wide reform to devolve governance, report on<br />
performance transparently, <strong>and</strong> meet new national st<strong>and</strong>ards.<br />
States will be responsible for state-wide system management, <strong>and</strong> for supporting Local<br />
Hospital Networks. States will operate within a framework <strong>of</strong> unified national funding <strong>and</strong><br />
governance arrangements, <strong>and</strong> will be held to account for meeting strong national st<strong>and</strong>ards<br />
– including st<strong>and</strong>ards backed by funding linked to performance. States will continue to be<br />
responsible for meeting the remaining costs <strong>of</strong> public hospital services, including meeting any<br />
costs over <strong>and</strong> above the efficient price, as well as the remainder <strong>of</strong> teaching, research, capital<br />
<strong>and</strong> block grants. This creates a strong incentive for states to be as efficient as possible in<br />
playing their ongoing role in our public hospital system.<br />
States will also continue to own public hospital assets. They will work with Local Hospital<br />
Networks to determine the range <strong>and</strong> number <strong>of</strong> public hospital services to be provided within<br />
their jurisdiction, <strong>and</strong> to be responsible for all aspects <strong>of</strong> industrial relations policy.<br />
Taking full funding <strong>and</strong> policy responsibility for GP <strong>and</strong> primary health care,<br />
<strong>and</strong> aged care<br />
The Commonwealth will take full funding <strong>and</strong> policy responsibility for GP <strong>and</strong> primary health<br />
care services, <strong>and</strong> for aged care services.<br />
This important structural change to roles <strong>and</strong> responsibilities within the health system means<br />
that one level <strong>of</strong> government – the Commonwealth – will be responsible <strong>and</strong> accountable for<br />
the strategic direction, planning <strong>and</strong> public funding <strong>of</strong> primary health care <strong>and</strong> aged care, as<br />
recommended by the NHHRC.<br />
Delivering better health <strong>and</strong> better hospitals 33
Currently, the Commonwealth <strong>and</strong> state governments share responsibility for primary health care<br />
services. Over time, this has resulted in duplication <strong>of</strong> effort in some areas <strong>and</strong> has created gaps<br />
in delivery in others. Consequently, the delivery <strong>of</strong> primary health care <strong>and</strong> aged care services are<br />
not as effective as they need to be.<br />
This means that many patients end up in hospital, when they could have received better care in<br />
the community.<br />
The Commonwealth will be responsible for setting national st<strong>and</strong>ards <strong>and</strong> policy. As a result<br />
<strong>of</strong> taking full funding responsibility for all primary health care <strong>and</strong> aged care services, the<br />
Commonwealth will be able to draw services together so they are better integrated, better<br />
coordinated, <strong>and</strong> more responsive to the needs <strong>of</strong> patients.<br />
New primary health care organisations – Medicare Locals – will be established to support the<br />
delivery <strong>of</strong> primary care services, better integrate services <strong>and</strong> plan for local population needs.<br />
Medicare Locals are discussed further in chapter two.<br />
For the aged care sector, this change in roles <strong>and</strong> responsibilities will deliver a nationally<br />
consistent aged care system that will enable older patients to seamlessly move from basic<br />
help at home to residential care as their needs change. This will provide a greater platform for<br />
integration <strong>and</strong> innovation.<br />
Ultimately, these changes will allow services to be provided in the most appropriate care setting for<br />
the patient, breaking down the artificial barriers that are created by having multiple funders. These<br />
changes will:<br />
››<br />
improve the efficiency <strong>of</strong> the system;<br />
››<br />
reduce cost-shifting <strong>and</strong> blame-shifting, as the Commonwealth Government will clearly be<br />
accountable for GP <strong>and</strong> primary health care, <strong>and</strong> for aged care services;<br />
››<br />
allow the Commonwealth to reduce duplication <strong>of</strong> services, improving efficiency <strong>and</strong> reducing<br />
waste, while improving overall capacity in the primary care <strong>and</strong> aged care sectors; <strong>and</strong><br />
››<br />
make it easier for patients to access care that is integrated around their needs.<br />
At this point, Victoria has not agreed to the transfer <strong>of</strong> responsibility for aged care Home <strong>and</strong><br />
Community Care (HACC) services to the Commonwealth. The Commonwealth Government remains<br />
committed to continuing discussions with Victoria <strong>and</strong> other stakeholders, so that Victorians can also<br />
benefit from a unified aged <strong>and</strong> community care system. The Commonwealth recognises the unique<br />
role played by local government in Victoria. References in this document to ‘states’ in the context <strong>of</strong><br />
reforms to roles <strong>and</strong> responsibilities to deliver a unified aged care system do not refer to Victoria.<br />
Further information on the shift to full funding <strong>and</strong> policy responsibility for GP <strong>and</strong> primary health<br />
care services, <strong>and</strong> aged care services, is provided in chapters six <strong>and</strong> seven.<br />
34 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Chapter 2: Run Locally: local<br />
governance institutions to drive<br />
performance <strong>and</strong> responsiveness<br />
Governance <strong>and</strong> management <strong>of</strong> local health <strong>and</strong> hospital services will<br />
be devolved to the local level. New local institutions will ensure health<br />
services respond better to the needs <strong>of</strong> their local communities right<br />
across the system:<br />
››<br />
Local Hospital Networks will be responsible for managing <strong>and</strong><br />
delivering hospital services. This will lead to increased autonomy <strong>and</strong><br />
flexibility so that services are more responsive to local needs.<br />
››<br />
Medicare Locals – a network <strong>of</strong> independent primary health care<br />
organisations with strong links to local communities <strong>and</strong> health<br />
pr<strong>of</strong>essionals – will be established to provide better services, improve<br />
access to care <strong>and</strong> drive integration across GP <strong>and</strong> primary health care<br />
services.<br />
››<br />
One stop shops located across the country will ensure older<br />
Australians can more easily access information <strong>and</strong> assistance in<br />
receiving aged care services.<br />
These new local institutions will work together to deliver better<br />
integration <strong>and</strong> smoother transitions for patients across the entire health<br />
<strong>and</strong> hospital system, breaking down the artificial barriers between<br />
different services.<br />
Devolution <strong>of</strong> responsibility for health <strong>and</strong> hospital services will also<br />
improve responsiveness to local communities’ needs <strong>and</strong> better support<br />
<strong>and</strong> engage clinicians.<br />
Delivering better health <strong>and</strong> better hospitals 35
A hospital system without enough clinical <strong>and</strong> local engagement<br />
Public hospital governance structures vary across Australia, from highly centralised models to<br />
those that are more devolved to the hospital level. In the Government’s consultations, many<br />
clinicians <strong>and</strong> local communities made it clear they do not feel they have the opportunity to<br />
be involved in decisions about the delivery <strong>of</strong> health services in their communities. This is a<br />
particular issue in rural <strong>and</strong> regional communities.<br />
The result is that services are not responsive to local needs <strong>and</strong> opportunities to improve<br />
clinical safety <strong>and</strong> quality are lost.<br />
Local Hospital Networks with the flexibility to improve performance<br />
Local Hospital Networks will be single or small groups <strong>of</strong> public hospitals with a geographic<br />
or functional connection, large enough to operate efficiently <strong>and</strong> to provide a reasonable<br />
range <strong>of</strong> hospital services. They will be established by states in line with nationally agreed<br />
characteristics, <strong>and</strong> in close consultation with the Commonwealth. Devolving decision making<br />
to Local Hospital Networks will give communities <strong>and</strong> clinicians a greater say in how their<br />
hospitals are run.<br />
Local Hospital Networks will be responsible for making decisions on the day to day operations<br />
<strong>of</strong> hospitals within their Network. This includes planning at the Network level to deliver on<br />
performance st<strong>and</strong>ards <strong>and</strong> manage budgets. Networks will be responsible for delivering on<br />
agreed services <strong>and</strong> performance st<strong>and</strong>ards, formalised through an annual service agreement.<br />
The state will set out a target for the amount <strong>of</strong> hospital services to be purchased, <strong>and</strong><br />
the Network will set out the performance targets <strong>and</strong> benchmarks that it agrees to reach.<br />
Service agreements will be set within a framework <strong>of</strong> unified national funding arrangements,<br />
<strong>and</strong> will be required to deliver on strong national st<strong>and</strong>ards. In general, they will leave<br />
significant flexibility for Networks to determine the most appropriate service mix to meet their<br />
performance targets <strong>and</strong> the needs <strong>of</strong> their community.<br />
Local Hospital Networks will be established as separate legal entities under state legislation,<br />
in order to devolve operational management for public hospitals, <strong>and</strong> accountability for local<br />
delivery, to the local level. Networks will avoid the fragmentation <strong>and</strong> duplication that would<br />
come from individual hospitals operating independently from each other, <strong>and</strong> also avoid the<br />
centralised controls <strong>and</strong> excess layers <strong>of</strong> bureaucracy that characterise some systems. The<br />
Commonwealth <strong>and</strong> the states will work cooperatively to ensure, wherever possible, common<br />
geographic boundaries with Medicare Locals.<br />
36 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Local Hospital Networks will be consistent with the following broad characteristics:<br />
››<br />
Local Hospital Networks in metropolitan areas will comprise at least one hospital, built<br />
around principal referral hospitals or specialist hospitals, <strong>and</strong> including smaller metropolitan<br />
hospitals. They will take into account patient catchment <strong>and</strong> referral linkages.<br />
››<br />
Many Local Hospital Networks will have a geographic focus with responsibility for<br />
particular areas, while other Local Hospital Networks will have a functional focus – for<br />
instance specialist women’s <strong>and</strong> children’s hospitals.<br />
››<br />
In regional Australia, a flexible approach will be adopted to determine the regional, rural<br />
<strong>and</strong> remote network structure that best meets the needs <strong>of</strong> these communities <strong>and</strong> best<br />
takes into account the challenges <strong>of</strong> managing multiple small hospitals.<br />
The Commonwealth <strong>and</strong> states have agreed that the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
should be delivered with no net increase in bureaucracy as a proportion <strong>of</strong> the ongoing health<br />
workforce. The Commonwealth Government expects that Local Hospital Networks should be<br />
established by states within current health department staffing levels.<br />
Pr<strong>of</strong>essional governance to drive local responsiveness <strong>and</strong> improve efficiency<br />
Local Hospital Networks will have a pr<strong>of</strong>essional Governing Council <strong>and</strong> Chief Executive Officer<br />
(CEO), who will be responsible for delivering agreed services <strong>and</strong> performance st<strong>and</strong>ards within<br />
an agreed budget. Governing Councils will include local health, management <strong>and</strong> finance<br />
pr<strong>of</strong>essionals, with an appropriate mix <strong>of</strong> skills, expertise <strong>and</strong> backgrounds. Members will<br />
need to have the pr<strong>of</strong>essional capability to run the large, complex organisations that most<br />
Local Hospital Networks will be. Each Network’s CEO will be appointed by the Council <strong>and</strong><br />
accountable to the Council.<br />
The devolution <strong>of</strong> management accountability, combined with paying hospitals for the services<br />
they provide, places incentives on local managers <strong>and</strong> clinicians to increase service levels<br />
<strong>and</strong> reduce costs. This will also mean that a local hospital should no longer have to seek the<br />
approval <strong>of</strong> a large bureaucracy for matters that relate to the day-to-day delivery <strong>of</strong> hospital<br />
services.<br />
Delivering better health <strong>and</strong> better hospitals 37
The role <strong>of</strong> state health departments<br />
State health departments will specialise in system-wide service planning <strong>and</strong> performance<br />
management issues, <strong>and</strong> work with Local Hospital Networks to negotiate service agreements,<br />
meet unanticipated challenges, transfer good practice <strong>and</strong> identify <strong>and</strong> remediate poor<br />
practice. They will work within a unified national funding <strong>and</strong> governance framework, <strong>and</strong><br />
support Local Hospital Networks in achieving national performance st<strong>and</strong>ards. Local Hospital<br />
Networks will be the employers <strong>of</strong> hospital staff, but with industrial relations negotiations<br />
conducted by states. Current employment conditions will not change as a result <strong>of</strong> these<br />
reforms.<br />
In circumstances in which independent <strong>and</strong> transparent reporting concludes that Local Hospital<br />
Network performance is good, Governing Councils <strong>and</strong> CEOs could expect relatively ‘light<br />
touch’ management from states in an earned autonomy system. Conversely, where Network<br />
performance is not meeting the performance st<strong>and</strong>ards outlined in the service agreement,<br />
state health departments will take a more visible <strong>and</strong> intrusive role. As a last resort, the<br />
Council may decide to remove the CEO, or the state minister may choose to remove the Chair<br />
<strong>of</strong> the Council, or both.<br />
Further detail on the distribution <strong>of</strong> roles <strong>and</strong> responsibilities for public hospitals services is<br />
provided in figure three below.<br />
38 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Figure 3: Roles <strong>and</strong> responsibilities for public hospital services in the National<br />
<strong>Health</strong> <strong>and</strong> Hospitals Network<br />
Decisions relating<br />
to public hospitals<br />
Determine efficient price, pay 60% for<br />
each service provided, <strong>and</strong> pay 60% <strong>of</strong><br />
other costs including capital<br />
Determine national governance<br />
arrangements<br />
Determine national performance <strong>and</strong><br />
accountability framework, including<br />
requirements for transparent, local,<br />
nationally consistent performance<br />
reporting<br />
Performance measures <strong>and</strong> target setting<br />
St<strong>and</strong>ards setting, guidelines, quality <strong>and</strong><br />
safety <strong>and</strong> national clinical leadership<br />
Hospital workforce planning<br />
Pay remaining costs, including any costs<br />
above the efficient price<br />
Capital planning <strong>and</strong> management<br />
Capital ownership<br />
Receive Commonwealth funding for<br />
research, training, capital <strong>and</strong> block<br />
funding<br />
Performance management <strong>and</strong><br />
remediation<br />
Industrial relations negotiations<br />
Agree local activity targets, service<br />
mix <strong>and</strong> provision for highly specialised<br />
services<br />
Procurement<br />
Receive Commonwealth <strong>and</strong> state funding<br />
for services under activity based funding<br />
Provisioning services between facilities<br />
Corporate services (human resources,<br />
payroll, etc.)<br />
Managing an operational budget<br />
Local implementation <strong>of</strong> clinical guidelines<br />
<strong>and</strong> pathways<br />
Location<br />
Local Hospital<br />
Networks<br />
Regions (e.g.<br />
Area <strong>Health</strong><br />
Services) States National<br />
Delivering better health <strong>and</strong> better hospitals 39
New primary health care organisations – Medicare Locals<br />
The Commonwealth will build on its responsibility for GP <strong>and</strong> primary health care with the<br />
introduction <strong>of</strong> primary health care organisations – Medicare Locals. Medicare Locals will be<br />
responsible for improving integration <strong>of</strong> services <strong>and</strong> reducing access gaps so that their local<br />
community can access care that meets local needs.<br />
Medicare Locals will be independent entities (not government bodies) with strong links to<br />
local communities, health pr<strong>of</strong>essionals <strong>and</strong> service providers, including GPs, allied health<br />
pr<strong>of</strong>essionals <strong>and</strong> Aboriginal Medical Services. It is expected that the first Medicare Locals will<br />
commence operations by mid-2011 with the rest to be rolled out by mid-2012.<br />
Medicare Locals will be responsible for a range <strong>of</strong> functions aimed at making it easier for<br />
patients to navigate the local health care system <strong>and</strong> to provide more integrated care. They<br />
will be integral to the Government’s reforms to ensure communities can access GP <strong>and</strong> primary<br />
health care after hours.<br />
Medicare Locals will be responsible for improving primary health care service delivery at the<br />
local level, to reduce service gaps <strong>and</strong> improve access to high quality integrated care centred<br />
around patients’ needs. For instance, a Medicare Local, in consultation with local GPs, might<br />
identify that there are a large number <strong>of</strong> diabetics in a particular area – <strong>and</strong> organise a roster<br />
<strong>of</strong> allied health pr<strong>of</strong>essionals such as nutritionists <strong>and</strong> diabetes educators to provide sessional<br />
services to different GP clinics in that area.<br />
Subject to final agreement with the states, Medicare Locals may play an increasing role in<br />
delivering services currently funded by states but set to transfer to the Commonwealth through<br />
the Government’s reforms. The Commonwealth <strong>and</strong> the states have already agreed to roll any<br />
primary care coordination functions into Medicare Locals to reduce duplication. States have<br />
agreed to align related programs with Medicare Locals as much as possible.<br />
Over time, in conjunction with the Australian National Preventive <strong>Health</strong> Agency, Medicare<br />
Locals will also drive an increased focus on local community based approaches to preventive<br />
health, by identifying <strong>and</strong> managing risk factors in local communities.<br />
Where possible, Medicare Locals will be drawn from those Divisions <strong>of</strong> General Practice that<br />
have the capacity to take on the roles <strong>and</strong> functions expected under the new arrangements. A<br />
key principle will be to minimise disruption to health practitioners <strong>and</strong> service providers so that<br />
clinical care to patients is not affected during the transition or establishment phase.<br />
40 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Helping older people to move seamlessly through the aged care system<br />
To ensure that older Australians are served as best they can, the Government will establish<br />
arrangements that help older Australians find <strong>and</strong> access the services that suit their needs <strong>and</strong><br />
better integrate aged care with other parts <strong>of</strong> the health system.<br />
As a step towards achieving this outcome, the Commonwealth will invest $37 million over the<br />
next four years to establish aged care one stop shops across the country. This will help older<br />
Australians <strong>and</strong> their families more easily access information <strong>and</strong> assessment for aged care<br />
services, connect with assessment services, <strong>and</strong> access services in the place that best suits<br />
them.<br />
Over time, the Government will work with aged care providers to ensure that they are:<br />
››<br />
supported in helping older Australians <strong>and</strong> their families receive the right services as their<br />
needs change; <strong>and</strong><br />
››<br />
supported in working with Local Hospital Networks <strong>and</strong> Medicare Locals to ensure that the<br />
health <strong>and</strong> aged care system works seamlessly in the interests <strong>of</strong> patients.<br />
The Commonwealth’s full funding responsibility across all aged care services will also provide a<br />
platform to promote the development <strong>of</strong> a wider variety <strong>of</strong> services <strong>and</strong> allow more innovative<br />
approaches.<br />
Clear accountability across the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
The establishment <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network will clarify roles <strong>and</strong><br />
responsibilities in the Australian health system. For too long, accountability has been<br />
fragmented, with no clear lines <strong>of</strong> accountability <strong>and</strong> blame shifting occurring between<br />
different levels <strong>of</strong> government.<br />
The Commonwealth will have responsibility for majority funding across the health system <strong>and</strong><br />
for overall governance <strong>and</strong> policy setting for the health system.<br />
Responsibility for local service delivery will rest at the local level – through Local Hospital<br />
Networks, GPs <strong>and</strong> other primary health care pr<strong>of</strong>essionals, <strong>and</strong> aged care services.<br />
System-wide issues for public hospitals will be managed by states, within a national funding<br />
<strong>and</strong> governance framework, <strong>and</strong> working to meet strong national st<strong>and</strong>ards. States will also be<br />
responsible for providing funding to Local Hospital Networks on top <strong>of</strong> the Commonwealth’s<br />
majority contribution.<br />
Delivering better health <strong>and</strong> better hospitals 41
Medicare Locals will be responsible for driving more integrated primary health care in local<br />
communities, <strong>and</strong> reducing access gaps, likewise within a national funding, governance <strong>and</strong><br />
performance framework.<br />
Clinical leadership to drive continuous improvement<br />
Clinical leadership is an integral part <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network. The<br />
Government will support clinicians to lead the drive towards continuous improvement in quality<br />
<strong>and</strong> to safeguard high st<strong>and</strong>ards <strong>of</strong> care, as they are the experts in this field.<br />
Providing a platform for clinicians to encourage the use <strong>of</strong> evidence based medicine, <strong>and</strong> help<br />
shape nationally appropriate quality <strong>and</strong> safety st<strong>and</strong>ards, is a critical component <strong>of</strong> improving<br />
health outcomes <strong>and</strong> encouraging best practice. The National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
will build on other measures to improve hospital st<strong>and</strong>ards through increased levels <strong>of</strong> clinical<br />
engagement.<br />
Clinical engagement will be improved through:<br />
1. Local Hospital Networks:<br />
Networks will work with local clinicians to incorporate their views, especially on quality <strong>and</strong><br />
safety, into the day to day operation <strong>of</strong> the hospitals. The Government will also support<br />
local clinicians to turn national clinical guidance into local practice, <strong>and</strong> guide improved<br />
safety <strong>and</strong> quality outcomes for the Local Hospital Network.<br />
2. A permanent Australian Commission on Safety <strong>and</strong> Quality in <strong>Health</strong> Care:<br />
The permanent Commission will work with clinicians to identify best practice clinical care,<br />
set national quality <strong>and</strong> safety st<strong>and</strong>ards, <strong>and</strong> take on a broader role in developing new<br />
clinical safety <strong>and</strong> quality st<strong>and</strong>ards across the health system.<br />
3. Medicare Locals:<br />
Strong clinical engagement will be a key feature <strong>of</strong> Medicare Locals. The role <strong>of</strong> Medicare<br />
Locals will be to support clinicians, not to get involved in clinical decision making about<br />
individual patients.<br />
The Government will also give clinicians more <strong>of</strong> a voice in planning <strong>and</strong> service provision,<br />
<strong>and</strong> drive improvements in quality <strong>and</strong> safety, by continuing to build on the improved clinician<br />
engagement that Local Hospital Networks will deliver. The Government will also introduce<br />
measures to improve the evidence base available to clinicians, allowing for more effective <strong>and</strong><br />
efficient clinical care. Specific reform measures building on current Commonwealth <strong>and</strong> state<br />
efforts to improve clinician engagement will be announced by the Government shortly.<br />
42 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Driving integration across the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
Local Hospital Networks will work with Medicare Locals to improve patient care <strong>and</strong> the<br />
quality <strong>of</strong> health <strong>and</strong> hospital services. Together they will ensure that GP <strong>and</strong> primary health<br />
care <strong>and</strong> public hospital care are better integrated, so patients smoothly transition in <strong>and</strong><br />
out <strong>of</strong> hospital <strong>and</strong> continue to receive all the care they need. This could include working<br />
with relevant providers to help patients manage their recovery <strong>and</strong> stay healthy as they are<br />
discharged from hospital.<br />
Local Hospital Networks <strong>and</strong> Medicare Locals will also work together to identify <strong>and</strong> address<br />
particular local needs. To formally enhance cooperation between hospitals <strong>and</strong> primary care<br />
services in a community, Medicare Locals will be expected to have some common membership<br />
<strong>of</strong> governance structures with Local Hospital Networks, <strong>and</strong> vice versa. In addition, Medicare<br />
Locals funding agreements will require them to work closely with Local Hospital Networks, <strong>and</strong><br />
vice versa. These linkages will help to drive more integrated care for patients.<br />
Local Hospital Networks will need to develop a number <strong>of</strong> critical relationships with other parts<br />
<strong>of</strong> the health <strong>and</strong> hospital system. Good communication between public <strong>and</strong> private hospitals<br />
will continue to be necessary, as will care pathways <strong>and</strong> linkages with local primary health<br />
care <strong>and</strong> aged care providers. Local Hospital Networks will be expected to strongly engage<br />
with university clinical schools <strong>and</strong> research centres, <strong>and</strong> this engagement will be critical<br />
to translating clinical research into clinical practice, ongoing pr<strong>of</strong>essional development <strong>and</strong><br />
training the next generation <strong>of</strong> clinical leaders.<br />
Medicare Locals will work with local GPs <strong>and</strong> Local Hospital Networks to improve patient<br />
care <strong>and</strong> quality <strong>and</strong> safety <strong>of</strong> health services. They will also work closely with practitioners<br />
<strong>and</strong> services in the primary health care, hospital, aged care <strong>and</strong> Indigenous health sectors to<br />
support greater collaboration between service providers.<br />
In addition, to ensure that older Australians are served as best as they can, the Government<br />
will establish arrangements that better integrate aged care with the other parts <strong>of</strong> the health<br />
system. This will help older Australians find <strong>and</strong> access the services that suit their needs.<br />
Over time, the Government will work with the full spectrum <strong>of</strong> aged care providers – including<br />
community <strong>and</strong> respite care – to ensure that they are supported to:<br />
› › Help older Australians <strong>and</strong> their families receive different types <strong>of</strong> care services as their<br />
needs change – for example, through more intensive or specialised community care<br />
packages, respite care <strong>and</strong> residential aged care.<br />
Delivering better health <strong>and</strong> better hospitals 43
››<br />
Work with Local Hospital Networks to identify appropriate care options that best suit<br />
the needs <strong>of</strong> older Australians <strong>and</strong> avoid unnecessary hospital stays, including through<br />
sub‐acute <strong>and</strong> step-down care.<br />
››<br />
Work with Medicare Locals to improve access to <strong>and</strong> quality <strong>of</strong> GP <strong>and</strong> primary health care<br />
services provided to older Australians in a local community, irrespective <strong>of</strong> where they live.<br />
These arrangements will ultimately ensure that aged care is coordinated with hospitals <strong>and</strong> GP<br />
<strong>and</strong> primary health care services, as shown in figure four. They will provide the foundation for<br />
a community <strong>of</strong> services which work with one another to provide better integrated <strong>and</strong> more<br />
efficient care across the entire health system. These arrangements will ultimately ensure that<br />
aged care services are coordinated with hospitals <strong>and</strong> primary health care services <strong>and</strong> they<br />
work with one another to provide better integrated care that is centred around patients’ needs.<br />
Figure 4: An integrated National <strong>Health</strong> <strong>and</strong> Hospitals Network across hospital,<br />
aged care <strong>and</strong> GP <strong>and</strong> primary health care services<br />
National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
Local Hospital Networks<br />
Manage day to day delivery <strong>of</strong><br />
hospital services<br />
Medicare Locals<br />
Support GP <strong>and</strong> primary<br />
health care providers, help<br />
integrate services<br />
Aged care services<br />
One stop shops<br />
Link with Local Hospital<br />
Networks <strong>and</strong> Medicare<br />
Locals<br />
44 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Chapter 3: Strong National<br />
st<strong>and</strong>ards <strong>and</strong> clear accountability<br />
for performance<br />
A core element <strong>of</strong> the National <strong>Health</strong> <strong>and</strong> Hospitals Network will be<br />
strong national st<strong>and</strong>ards <strong>and</strong> transparent reporting that is nationally<br />
consistent, <strong>and</strong> locally relevant.<br />
Strong national st<strong>and</strong>ards will drive improved performance across<br />
the health <strong>and</strong> hospital system, with funding increasingly linked to<br />
performance.<br />
For the first time, Australians will be able to access transparent <strong>and</strong><br />
nationally comparable performance data <strong>and</strong> information on their local<br />
hospitals <strong>and</strong> health services — including emergency department <strong>and</strong><br />
elective surgery waiting times, bed occupancy rates <strong>and</strong> reporting <strong>of</strong><br />
adverse events <strong>and</strong> hospital acquired infections.<br />
New Hospital Performance Reports <strong>and</strong> <strong>Health</strong>y Communities Reports<br />
(on primary health care performance) will help Australians make more<br />
informed choices about their health services, <strong>and</strong> help ensure the<br />
st<strong>and</strong>ard <strong>of</strong> care patients receive continues to improve.<br />
A lack <strong>of</strong> transparency for a significant taxpayer investment —<br />
particularly at individual hospital level<br />
Although around $70 billion in taxpayer funding was spent on health <strong>and</strong> hospitals over the<br />
last year, there is little nationally consistent <strong>and</strong> comparable information available on the<br />
performance outcomes <strong>of</strong> individual health <strong>and</strong> hospital services. Patients <strong>and</strong> the Australian<br />
community do not have sufficient information about the performance <strong>of</strong> their local hospitals,<br />
GPs <strong>and</strong> other health care providers in the system.<br />
While a substantial amount <strong>of</strong> system <strong>and</strong> government-level information is available,<br />
less information is published about local health services, how they are delivered <strong>and</strong> how<br />
they perform.<br />
Delivering better health <strong>and</strong> better hospitals 45
Setting national st<strong>and</strong>ards to deliver a nationally unified system<br />
The Commonwealth Government will use its position as the majority funder <strong>of</strong> health <strong>and</strong><br />
hospital services in Australia to drive strong national st<strong>and</strong>ards for health care <strong>and</strong> build a<br />
nationally unified health system. The Commonwealth has secured states’ agreement to a new<br />
performance <strong>and</strong> accountability framework to clearly state the high expectations all Australians<br />
can have <strong>of</strong> their health <strong>and</strong> hospital services.<br />
As part <strong>of</strong> its national leadership role, the Commonwealth will insist on higher national<br />
st<strong>and</strong>ards <strong>of</strong> performance, more consistently applied across the country, with new targets<br />
backed up by explicit financial rewards.<br />
The Commonwealth has already begun to move to increase the link between health <strong>and</strong><br />
hospital performance <strong>and</strong> funding — particularly in critical pressure points such as elective<br />
surgery <strong>and</strong> emergency departments. The Commonwealth has secured states’ agreement to a<br />
four hour National Access Target for emergency department services, <strong>and</strong> an elective surgery<br />
target <strong>and</strong> National Access Guarantee. The Commonwealth is providing $1.6 billion over the<br />
next four years for the achievement <strong>of</strong> these new, higher national st<strong>and</strong>ards.<br />
Other areas in which national st<strong>and</strong>ards will be developed include:<br />
››<br />
access to GPs <strong>and</strong> other health pr<strong>of</strong>essionals;<br />
››<br />
safety <strong>and</strong> quality <strong>of</strong> care (for instance through reporting on adverse events <strong>and</strong> hospital<br />
re-admission rates);<br />
››<br />
patient satisfaction; <strong>and</strong><br />
››<br />
financial management.<br />
A new National Performance Authority will monitor <strong>and</strong> report on the performance <strong>of</strong> Local<br />
Hospital Networks, individual hospitals <strong>and</strong> Medicare Locals. This will provide clear <strong>and</strong><br />
transparent reporting on public <strong>and</strong> private hospital performance, as well as state performance,<br />
<strong>and</strong> independent reporting on the Commonwealth’s primary health care performance.<br />
A permanent Australian Commission on Safety <strong>and</strong> Quality in <strong>Health</strong> Care will set national<br />
quality <strong>and</strong> safety st<strong>and</strong>ards <strong>and</strong> work with clinicians to identify best practice clinical care, to<br />
ensure the appropriateness <strong>of</strong> services being delivered in a particular setting.<br />
46 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Transparent reporting <strong>of</strong> performance against new, higher national st<strong>and</strong>ards<br />
The Government will introduce clear <strong>and</strong> transparent performance reporting against these<br />
strong national st<strong>and</strong>ards <strong>and</strong> other performance indicators to provide Australians with more<br />
information than ever before about the performance <strong>of</strong> their health <strong>and</strong> hospital services.<br />
For the first time, this performance information will be both nationally consistent <strong>and</strong> locally<br />
relevant.<br />
The Government will introduce clear <strong>and</strong> transparent reporting on the performance <strong>of</strong> every<br />
Local Hospital Network, <strong>and</strong> the hospitals within it, <strong>and</strong> every private hospital, through regular<br />
Hospital Performance Reports. This will show how all Australian hospitals perform against new<br />
national st<strong>and</strong>ards <strong>and</strong> other performance indicators.<br />
In addition, the Government will develop a <strong>Health</strong>y Communities Report for each Medicare<br />
Local’s geographic area. This Report will include, on a nationally consistent basis, local <strong>and</strong><br />
regional area information covering:<br />
››<br />
preventive health risk factors <strong>and</strong> other measures <strong>of</strong> community health <strong>and</strong> wellbeing;<br />
››<br />
access to GP services <strong>and</strong> out <strong>of</strong> hours GP care; <strong>and</strong><br />
››<br />
the extent to which the health system is working in a coordinated way, for example through<br />
the number <strong>of</strong> avoidable hospital admissions <strong>and</strong> trends in this information over time.<br />
The Government will work with clinicians, states <strong>and</strong> other stakeholders to develop the<br />
structure <strong>of</strong> these reports, <strong>and</strong> to identify what data is already available <strong>and</strong> what will need to<br />
be developed over time.<br />
Hospital Performance Reports <strong>and</strong> <strong>Health</strong>y Communities Reports will help Australians make<br />
more informed choices about their health services. They will clearly <strong>and</strong> quickly identify areas<br />
<strong>of</strong> high performance, <strong>and</strong> support the spread <strong>of</strong> effective <strong>and</strong> innovative practices across the<br />
country. They will help ensure the st<strong>and</strong>ard <strong>of</strong> care patients receive continues to improve.<br />
Transparent reporting will also allow poor performance to be quickly <strong>and</strong> easily identified, so<br />
that interventions can be made before problems become entrenched.<br />
Delivering better health <strong>and</strong> better hospitals 47
Chapter 4: Transparent <strong>and</strong> efficient<br />
funding arrangements<br />
The Commonwealth Government will pay 60 per cent <strong>of</strong> the efficient<br />
price <strong>of</strong> every public hospital service provided to public patients. The<br />
national efficient price will be determined by a new independent umpire,<br />
the Independent Hospital Pricing Authority.<br />
For the first time, both Commonwealth <strong>and</strong> state funding for public<br />
hospitals will be clearly identified, <strong>and</strong> will be explicitly linked to services<br />
actually delivered to patients.<br />
This will introduce new levels <strong>of</strong> transparency in funding for public<br />
hospitals, <strong>and</strong> give taxpayers confidence that scarce health dollars are<br />
going directly to hospital services. Commonwealth funding for each<br />
service will be calculated <strong>and</strong> paid automatically, through National<br />
<strong>Health</strong> <strong>and</strong> Hospitals Network Funding Authorities, to Local Hospital<br />
Networks.<br />
These Funding Authorities will be jointly governed by the Commonwealth<br />
<strong>and</strong> the relevant state. Funding Authorities will transparently report on<br />
the number <strong>of</strong> services provided <strong>and</strong> paid for.<br />
This transparent system <strong>of</strong> activity based funding will provide Local<br />
Hospital Networks with funding certainty, <strong>and</strong> give them flexibility to<br />
shape the mix <strong>of</strong> services they deliver.<br />
Some payments will be made to states for system-wide resource<br />
allocation, including payments for research <strong>and</strong> training, <strong>and</strong> block<br />
grants, including for small rural <strong>and</strong> regional hospitals to recognise<br />
Community Service Obligations.<br />
48 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
Too much inefficiency <strong>and</strong> waste<br />
Today, the Commonwealth supports the delivery <strong>of</strong> free public hospital services through block<br />
grant funding paid to the states. Each state then determines funding for individual hospitals.<br />
There is considerable variation in mechanisms for payment to individual hospitals around the<br />
country, though many states are shifting to some form <strong>of</strong> activity based funding for acute care.<br />
Improving their efficiency will allow hospitals to keep downward pressure on costs, <strong>and</strong> to free<br />
up resources to meet increasing dem<strong>and</strong>.<br />
Reforming funding arrangements for public hospitals<br />
The Commonwealth will create a National <strong>Health</strong> <strong>and</strong> Hospitals Network Fund comprising:<br />
››<br />
funding sourced from the National <strong>Health</strong>care Specific Purpose Payment;<br />
››<br />
an agreed amount <strong>of</strong> GST revenue, which would then be allocated to health <strong>and</strong> hospitals<br />
reform; <strong>and</strong><br />
››<br />
additional top-up funding to be paid by the Commonwealth, reflecting the<br />
Commonwealth’s greater responsibility for financing growth in hospital costs.<br />
Commonwealth funding for public hospitals will be made from this Fund.<br />
Commonwealth <strong>and</strong> state funding for public hospital services will be clearly identified, <strong>and</strong><br />
delivered transparently <strong>and</strong> directly to Funding Authorities in each state. Jointly governed<br />
by the Commonwealth <strong>and</strong> the relevant state, Funding Authorities will transparently report<br />
on the number <strong>of</strong> services provided <strong>and</strong> paid for, introducing new levels <strong>of</strong> transparency in<br />
how hospital funding is distributed, <strong>and</strong> giving greater confidence to governments <strong>and</strong> the<br />
community that scarce health dollars are going directly to hospital services.<br />
Commonwealth funding will flow automatically through Funding Authorities directly to<br />
Local Hospital Networks based on services actually provided. States have also agreed to<br />
be transparent about their funding contribution for each public hospital service, by making<br />
payments on an activity basis through Funding Authorities. There will be no scope to divert<br />
these funds for other uses, <strong>and</strong> no scope for health departments to use the money for<br />
bureaucracy. This will give hospitals more funding certainty than ever before. Transparent<br />
funding arrangements will also support transparent performance reporting <strong>and</strong> drive<br />
continuous improvement within each public hospital.<br />
Funding Authorities will have no policy or operational role, beyond receiving activity based<br />
payments from governments <strong>and</strong> making payments directly to Local Hospital Networks.<br />
Delivering better health <strong>and</strong> better hospitals 49
These arrangements will ensure each Local Hospital Network is funded for the services it<br />
provides. This gives Local Hospital Networks a strong financial incentive to provide more<br />
services <strong>and</strong> provide services more efficiently, subject to meeting safety <strong>and</strong> quality st<strong>and</strong>ards.<br />
Local Hospital Networks will negotiate with states to determine the range <strong>and</strong> number <strong>of</strong><br />
services each Network will provide. The Commonwealth will fund 60 per cent <strong>of</strong> the efficient<br />
price <strong>of</strong> each <strong>of</strong> these services <strong>and</strong> Commonwealth funding will be provided automatically for<br />
each service provided under a service agreement. This represents a significant departure from<br />
current arrangements, under which the Commonwealth contributes to public hospital funding<br />
through block grants, which are not explicitly tied to delivery <strong>of</strong> services.<br />
International experience suggests that activity based funding in concert with effective clinical<br />
leadership <strong>and</strong> a strong safety <strong>and</strong> quality regime can support improvements in quality <strong>and</strong><br />
patient care. It also has the capacity to slow the rate <strong>of</strong> growth in hospital costs over time,<br />
increasing the long-term sustainability <strong>of</strong> health care funding.<br />
These reforms will help to ensure that hospital financing can dynamically adjust to:<br />
››<br />
shifting populations;<br />
››<br />
local demographic characteristics;<br />
››<br />
changing costs <strong>of</strong> delivering medical services from technological <strong>and</strong> clinical innovation; <strong>and</strong><br />
››<br />
the complexity <strong>and</strong> location <strong>of</strong> delivering hospital services.<br />
In addition to funding public hospital services through activity based funding, the Government<br />
will ensure that the new financing arrangements effectively support small regional <strong>and</strong> rural<br />
hospitals, <strong>and</strong> other services that are not suitable for activity based funding. The Government<br />
will provide block funding to these services either instead <strong>of</strong> or on top <strong>of</strong> activity based<br />
funding. This will reflect the higher costs associated with delivering services in regional <strong>and</strong><br />
rural areas <strong>of</strong> Australia, <strong>and</strong> ensure small rural <strong>and</strong> regional hospitals are funded to deliver on<br />
Community Service Obligations.<br />
An independent umpire to determine the efficient price<br />
To ensure that the nationally efficient price is determined on a fair <strong>and</strong> equitable basis, a new<br />
independent umpire, the IHPA, will set the national efficient price <strong>and</strong> advise the Government<br />
on appropriate timelines <strong>and</strong> the path for transition for all hospital services. It will engage with<br />
clinicians on technical issues to ensure that the efficient price continues to reflect the actual<br />
cost <strong>of</strong> providing hospital services, <strong>and</strong> developments in best practice.<br />
50 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
The national efficient price will cover both the recurrent costs <strong>of</strong> patient services <strong>and</strong> the<br />
operating capital required to deliver those services. The umpire will also advise on the mechanism<br />
to provide the Commonwealth’s contribution to teaching <strong>and</strong> research, capital, <strong>and</strong> block grant<br />
funding (as outlined in chapter one).<br />
In setting the national efficient price, the IHPA will be required to strike an appropriate balance<br />
between reasonable access, clinical safety, efficiency <strong>and</strong> fiscal considerations. Price loadings will<br />
be established to recognise, for example, the particular circumstances <strong>and</strong> health care needs <strong>of</strong><br />
people living in rural Australia <strong>and</strong> Indigenous Australians.<br />
The IHPA will also provide binding <strong>and</strong> independent arbitration on cost‐shifting <strong>and</strong> boundary<br />
issues, both between the Commonwealth <strong>and</strong> the states, <strong>and</strong> cross-border charging between<br />
states. The IHPA will be empowered to resolve cost-shifting issues in a definitive <strong>and</strong> nationally<br />
consistent manner.<br />
Driving efficiency — within Local Hospital Networks <strong>and</strong> across the system<br />
Payments on the basis <strong>of</strong> an efficient price will help drive efficiency in all hospitals across<br />
the country. This reform will give the Commonwealth <strong>and</strong> the community confidence that in<br />
the future, additional investment <strong>of</strong> scarce new health funds is being used as efficiently <strong>and</strong><br />
effectively as possible.<br />
It is estimated that activity based funding will be applied to at least half <strong>of</strong> all public hospitals.<br />
These will mostly be larger hospitals in metropolitan areas but will also include many large<br />
hospitals in regional areas. These hospitals account for around 90 per cent <strong>of</strong> all admitted patient<br />
hospital services. The remaining hospitals – mostly small, rural hospitals – account for around 10<br />
per cent <strong>of</strong> services. The Government will provide block funding to these services, either instead<br />
<strong>of</strong> or on top <strong>of</strong> activity based funding.<br />
Those Local Hospital Networks that deliver high quality services more efficiently will be able to<br />
reinvest in further innovation or more services, <strong>and</strong> have the flexibility to shape local services<br />
according to local needs. The need for payments to be passed through state <strong>and</strong> regional health<br />
bureaucracies will be avoided.<br />
The combination <strong>of</strong> funding for services actually provided <strong>and</strong> new national transparency<br />
measures will mean communities have more information than ever before on how well hospitals<br />
are performing, how their hospitals are funded, <strong>and</strong> what services are provided.<br />
This increased transparency will also allow ready identification <strong>of</strong> high-performing hospitals, support<br />
sharing innovative practices with other hospitals, <strong>and</strong> help to create a self‐improving hospital<br />
system. Moreover, states will be able to easily identify hospitals that are struggling <strong>and</strong> make early<br />
interventions to lift hospital performance.<br />
Delivering better health <strong>and</strong> better hospitals 51
Chapter 5: A SECURE FUNDING BASE<br />
FOR HEALTH AND HOSPITALS<br />
The Commonwealth Government will take responsibility for an increased<br />
share <strong>of</strong> health care costs by increasing its contribution to public hospital<br />
services <strong>and</strong> taking full responsibility for funding GP <strong>and</strong> primary<br />
health care <strong>and</strong> aged care. These changes will be financed through a<br />
combination <strong>of</strong>:<br />
››<br />
funding currently provided by the National <strong>Health</strong>care Specific<br />
Purpose Payment;<br />
››<br />
dedication <strong>of</strong> GST revenue (expected to be about one-third <strong>of</strong> total GST);<br />
››<br />
top-up funding <strong>of</strong> at least $15.6 billion between 2014–15 <strong>and</strong> 2019–20<br />
to be paid by the Commonwealth, reflecting its greater responsibility<br />
for financing health <strong>and</strong> hospital expenditure growth.<br />
This will also improve the long run productivity <strong>of</strong> the Australian<br />
economy: the level <strong>of</strong> government with the most stable <strong>and</strong> efficient<br />
revenue base will now be the majority funder <strong>of</strong> the fastest growing area<br />
<strong>of</strong> public expenditure.<br />
A health system under financial pressure<br />
The cost <strong>of</strong> health care has risen significantly in past decades <strong>and</strong> will continue to rise into<br />
the future. <strong>Health</strong> costs are projected to increase from 15 per cent <strong>of</strong> all Commonwealth<br />
Government spending now (4.0 per cent <strong>of</strong> GDP) to 26 per cent by 2050 (7.1 per cent <strong>of</strong> GDP)<br />
— an increase in 2049–50 <strong>of</strong> around $200 billion from today’s spending.<br />
Population ageing will be a major contributor to this: from 2009–10 to 2049–50, real health<br />
spending on those aged over 65 years is expected to increase around seven-fold, <strong>and</strong> around<br />
twelve-fold for those over 85 years.<br />
The costs <strong>of</strong> providing health care have increased sharply in recent years: health spending was<br />
45 per cent more in 2005–06 than a decade before, even after adjusting for inflation.<br />
52 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
On the basis <strong>of</strong> current spending <strong>and</strong> revenue trends, there is a real risk that state governments<br />
will not have the financial capacity to meet health spending obligations in the longer term,<br />
placing our health system <strong>and</strong> services at risk.<br />
In the five years to 2007–08, public hospital expenditure has grown at an average <strong>of</strong> close to<br />
ten per cent per year. As shown in figure five below, if current spending <strong>and</strong> revenue trends<br />
continue, health spending alone is projected to absorb more than the entire revenue collected<br />
by all states by 2045–46 – <strong>and</strong> earlier in some states.<br />
Figure 5: <strong>Health</strong> funding responsibility as a proportion <strong>of</strong> own source tax<br />
revenue (illustrative)<br />
Per cent<br />
120<br />
Per cent<br />
120<br />
100<br />
100<br />
80<br />
80<br />
60<br />
60<br />
40<br />
40<br />
20<br />
20<br />
0<br />
0<br />
2008-09 2013-14 2018-19 2023-24 2028-29 2033-34 2038-39 2043-44 2048-49<br />
State <strong>and</strong> local All governments Commonwealth<br />
Source: Treasury projections based on data from the Australian Institute <strong>of</strong> <strong>Health</strong> <strong>and</strong> Welfare. Tax held constant as a share <strong>of</strong><br />
GDP. Based on current arrangements at the time <strong>of</strong> the 2010 Intergenerational Report.<br />
Part <strong>of</strong> the answer to this challenge will lie in achieving greater system wide efficiencies —<br />
these are central to the reforms to establish the National <strong>Health</strong> <strong>and</strong> Hospitals Network.<br />
These gains will be driven by better clarification <strong>of</strong> roles <strong>and</strong> responsibilities (see chapter one),<br />
the devolution <strong>of</strong> hospital management (chapter two), national st<strong>and</strong>ards with improved<br />
accountability for performance (chapter three), <strong>and</strong> the introduction <strong>of</strong> activity based funding<br />
(chapter four). However, fundamental reform <strong>of</strong> federal financial relations is also necessary if<br />
we are to address the challenge <strong>of</strong> growing health care costs.<br />
Delivering better health <strong>and</strong> better hospitals 53
Financing the National <strong>Health</strong> <strong>and</strong> Hospitals Network<br />
The Commonwealth has secured states’ agreement that these reforms will be financed through<br />
a combination <strong>of</strong>:<br />
››<br />
funding sourced from the National <strong>Health</strong>care Specific Purpose Payment;<br />
››<br />
an agreed amount <strong>of</strong> GST revenue, which would then be allocated to health <strong>and</strong> hospitals<br />
reform; 1 <strong>and</strong><br />
››<br />
additional top-up funding to be paid by the Commonwealth, reflecting the<br />
Commonwealth’s greater responsibility for financing growth in hospital costs.<br />
From 1 July 2011, an agreed amount <strong>of</strong> GST revenue will be retained <strong>and</strong> allocated by the<br />
Commonwealth to health <strong>and</strong> hospital services. Each state’s retained GST will be allocated to<br />
health <strong>and</strong> hospital services in that state. The amount <strong>of</strong> GST to be retained <strong>and</strong> allocated to<br />
health <strong>and</strong> hospitals will then be fixed from 2014–15, based on 2013–14 costs.<br />
This reform will provide an increasing benefit to states over time, as the gap widens year on<br />
year between the growth <strong>of</strong> general consumption – the GST revenue base – <strong>and</strong> increasing<br />
health costs. The Commonwealth will guarantee that the ‘top-up’ payment during the period<br />
2014–15 to 2019–20 will be at least $15.6 billion. The benefits to health <strong>and</strong> hospital services<br />
in each state will grow significantly beyond this period. As a result <strong>of</strong> the Commonwealth’s<br />
retention <strong>of</strong> GST, all states will be no worse <strong>of</strong>f in the short term, <strong>and</strong> significantly better <strong>of</strong>f<br />
over the longer term.<br />
Should the Commonwealth’s responsibility for health system growth be less than the predicted<br />
$15.6 billion, states will be required to spend the residual on any health service that will<br />
assist in ameliorating the growth in dem<strong>and</strong> for hospital services, including programs for<br />
chronic disease management, preventive health, mental health, hospital admission avoidance<br />
programs <strong>and</strong> hospital early discharge programs.<br />
This change represents a significant shift in financial responsibilities, not least because<br />
hospital costs have been growing at close to ten per cent per annum, <strong>and</strong> are expected to<br />
continue to outpace growth in GST <strong>of</strong> around six per cent per annum over the medium term.<br />
The Commonwealth’s enhanced funding responsibility will commence as the foundations<br />
<strong>of</strong> a new health <strong>and</strong> hospital system — particularly reformed roles <strong>and</strong> responsibilities,<br />
national st<strong>and</strong>ards, activity based funding, <strong>and</strong> local management <strong>of</strong> hospital services — are<br />
established.<br />
1 For a discussion <strong>of</strong> the specific circumstances <strong>of</strong> Western Australia see page 24.<br />
54 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future
A secure funding base for health <strong>and</strong> hospitals into the future<br />
The Commonwealth Government taking a greater share <strong>of</strong> funding for our nation’s health<br />
system will help to secure the funding base for health <strong>and</strong> hospital services into the future.<br />
It will reduce the reliance on less efficient state taxes to finance health services. The<br />
Commonwealth Government is better placed to take responsibility for the future growth across<br />
health <strong>and</strong> hospitals, due to its stronger budget position, characterised by revenue sources that<br />
are better able to h<strong>and</strong>le fiscal adjustment over time. This will also yield productivity dividends<br />
across the national economy, <strong>and</strong> better alignment between spending responsibilities <strong>and</strong><br />
revenue-raising capacity in both Commonwealth <strong>and</strong> state governments.<br />
These reforms will reduce future pressure on the states to raise more revenue to finance health<br />
services through their less efficient taxes. Figure six below shows an estimate <strong>of</strong> the significant<br />
financial benefits that each state will receive from these reforms. The difference in gains for<br />
each state reflects their different population sizes <strong>and</strong> growth.<br />
Figure 6: Expected improvement in budgetary position on a population share<br />
basis (by state, 2014–15 to 2019–20)<br />
5,000<br />
$million<br />
$million<br />
5,000<br />
4,000<br />
4,000<br />
3,000<br />
3,000<br />
2,000<br />
2,000<br />
1,000<br />
1,000<br />
0<br />
NSW VIC QLD WA SA TAS ACT NT<br />
0<br />
Source: Treasury projection. Based on current arrangements. Note inclusion <strong>of</strong> WA assumes agreement to these reforms. Final<br />
distribution <strong>of</strong> guaranteed top-up to states subject to further discussion between Treasurers.<br />
Delivering better health <strong>and</strong> better hospitals 55
Fiscally responsible reform<br />
This reform is consistent with the Government’s fiscal strategy to return the budget to surplus,<br />
<strong>and</strong> is fully funded over the upcoming forward estimates.<br />
The Government has already delivered $56 billion in savings in the 2008–09 <strong>and</strong> 2009–10<br />
Budgets. The Government is prepared to make further savings decisions in order to ensure the<br />
long term sustainability <strong>of</strong> the health system <strong>and</strong> the delivery <strong>of</strong> the fiscal strategy.<br />
The Government recognises that additional investments will be required over time to meet<br />
increased dem<strong>and</strong>s on the health system. The investments outlined in this document, as well as<br />
any additional investment in our health system, will be consistent with the Government’s fiscal<br />
strategy. The Government has already undertaken significant reforms in order to place health<br />
costs on a more sustainable footing.<br />
56 A National <strong>Health</strong> <strong>and</strong> Hospitals Network for Australia’s Future