Simulation Interest Group Scenario Template
Simulation Interest Group Scenario Template
Simulation Interest Group Scenario Template
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
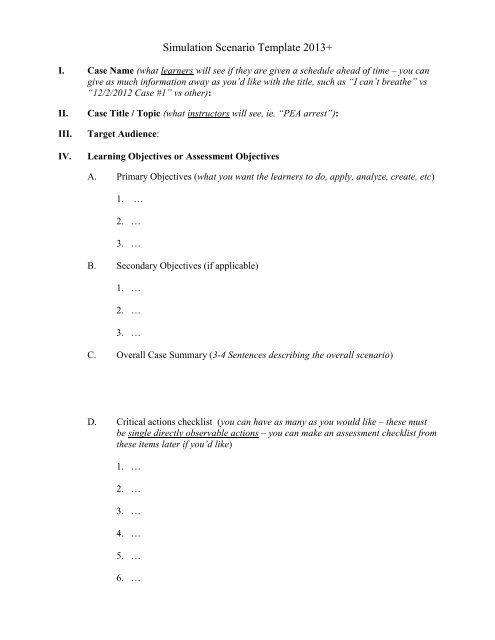
<strong>Simulation</strong> <strong>Scenario</strong> <strong>Template</strong> 2013+<br />
I. Case Name (what learners will see if they are given a schedule ahead of time – you can<br />
give as much information away as you‟d like with the title, such as “I can‟t breathe” vs<br />
“12/2/2012 Case #1” vs other):<br />
II.<br />
III.<br />
IV.<br />
Case Title / Topic (what instructors will see, ie. “PEA arrest”):<br />
Target Audience:<br />
Learning Objectives or Assessment Objectives<br />
A. Primary Objectives (what you want the learners to do, apply, analyze, create, etc)<br />
1. …<br />
2. …<br />
3. …<br />
B. Secondary Objectives (if applicable)<br />
1. …<br />
2. …<br />
3. …<br />
C. Overall Case Summary (3-4 Sentences describing the overall scenario)<br />
D. Critical actions checklist (you can have as many as you would like – these must<br />
be single directly observable actions – you can make an assessment checklist from<br />
these items later if you‟d like)<br />
1. …<br />
2. …<br />
3. …<br />
4. …<br />
5. …<br />
6. …
V. Environment<br />
A. Lab Set Up<br />
1. Type of Room / Area:<br />
2. Beds / stretchers:<br />
3. Other large equipment:<br />
B. Manikin Set Up<br />
1. High Fidelity Simulator? (If so, which one):<br />
2. Moulage (ie. abrasions, lacerations, pale skin, cyanosis, impaled object,<br />
amputated leg with persistent hemorrhage, lower extremity edema, etc):<br />
a. …<br />
b. …<br />
c. …<br />
3. Attire, etc<br />
a. Clothes:<br />
b. Shoes:<br />
c. Wig:<br />
d. Glasses:<br />
e. Other:<br />
C. Supplies<br />
1. IV Fluids Needed<br />
a. …<br />
b. …<br />
2. Drugs Needed<br />
a. …<br />
b. …<br />
c. …<br />
3. Vascular Access Equipment Needed<br />
a. …<br />
b. …<br />
c. …<br />
4. Airway Equipment Needed<br />
a. …<br />
b. …<br />
c. …<br />
5. Other Procedural Supplies Needed<br />
a. …<br />
b. …<br />
c. …<br />
6. Other Medical Equipment Needed (ie. backboard, etc)<br />
a. …<br />
b. …<br />
c. …
D. Props<br />
1. EKGs:<br />
2. XRays:<br />
3. US images:<br />
4. CT scans:<br />
5. Other imaging:<br />
6. Lab results in a printable / electronic format to show participants:<br />
7. Hospital chart information or other materials (EMS run sheet, nursing home<br />
paperwork, code status sheet, etc) to show the participants:<br />
8. Other Props (ie. spray bottle for diaphoresis, urine in urinal, blood all over<br />
sheets, etc)<br />
E. Distractors (distressed family member, additional disruptive / psychotic patient<br />
not initially in scenario, etc)<br />
VI.<br />
VII.<br />
Actors<br />
A. Roles (ie. paramedic, nurse, consultant, patient‟s family member, etc)<br />
1. …<br />
2. …<br />
3. …<br />
B. Who may play them (ie. other residents, other nurses, trained actors)<br />
1. …<br />
2. …<br />
3. …<br />
C. Action Role<br />
1. …<br />
2. …<br />
3. …<br />
Other Personnel Required<br />
i. Sim Jockey (person running simulator):<br />
ii. Debriefer (usually watching from control room and then debriefs):<br />
iii. Other:<br />
VIII. <strong>Simulation</strong> Center Personnel (do you want any of ISEC staff filling any roles above)?<br />
a. Lisa<br />
b. Gene
IX.<br />
Case Narrative (describes what the learner will experience)<br />
A. <strong>Scenario</strong> Background Given to Participants (specify if given freely or must be<br />
asked for)<br />
1. Scene introduction (ie. “you are in a small rural hospital…” etc)<br />
2. Chief complaint<br />
3. Medic report / triage note / nursing home note / EHR info<br />
4. Past medical history<br />
5. Medications<br />
6. Allergies<br />
7. Family/social history<br />
B. <strong>Scenario</strong> conditions initially<br />
1. History patient (or family, parent, etc) gives:<br />
2. Patients initial exam<br />
c. VS: BP HR RR SpO2 T<br />
d. General:<br />
e. Neuro:<br />
f. HENT:<br />
g. Eyes:<br />
h. Chest/Pulm:<br />
i. CV:<br />
j. Abd:<br />
k. Back:<br />
l. Ext:<br />
m. Skin:<br />
3. Patients physiology
C. <strong>Scenario</strong> branch points / Play of Case Guidelines (ie. Changes in patient<br />
condition, responses to treatments, etc. Can be written as many IF-THEN<br />
statements, designed as a flowsheet / branch diagram, spreadsheet, or other. Write<br />
this so someone else can look at it and understand how your scenario will flow<br />
based on the actions that the learners do / do not do.)<br />
1. …<br />
2. …<br />
3. …<br />
4. …<br />
5. …<br />
6. …<br />
7. …<br />
8. …<br />
9. …<br />
10. …<br />
11. …<br />
12. …<br />
X. Instructors Notes (what the instructor must do to create the experience)<br />
A. Tips to keep scenario flowing in lab and via computer – see above<br />
B. Tips to direct actors – see above<br />
C. <strong>Scenario</strong> programming<br />
1. Optimal management path<br />
2. Potential complications / errors paths (can write „see above‟ if this has<br />
been described in your play of case guidelines)
XI.<br />
Debriefing Plan<br />
A. Method of debriefing – group vs individual, with vs without video, etc<br />
B. Actual debriefing materials (if you have handouts on scenario content, please<br />
include that as well)<br />
C. Rules for the debriefing<br />
How to Create a Good Learning Environment<br />
• The Basic Assumption: Assuming competence and good intention of the learners<br />
• Theory: Mistakes made in the simulation lab are viewed as puzzles / mysteries, not<br />
“mistakes”<br />
• Utilizing the debriefing with good judgment approach (see below)<br />
Debriefing: Theory & How It‟s Done. The “Debriefing with Good Judgment” Approach<br />
Goal #1: Identify knowledge gaps, discover the learner‟s „frames‟, and match teaching points<br />
• Frames are what drive people‟s actions (why the learners did what they did)<br />
Driven by assumptions, knowledge, situations, context, feelings, goals, and preexisting<br />
thought processes<br />
• You must FOCUS on changing the trainee‟s frames, not just their actions<br />
Goal #2: To facilitate the discussion, helping learners develop their own self-reflection skills<br />
• The debriefer should be speaking < 50% of the time<br />
Phases of Debriefing<br />
• Reactions Phase: Clears the air and can guide discussion. (Don‟t miss listening to the<br />
participants talk amongst themselves as they are walking out of the room.)<br />
“So, how do you feel about that case?”<br />
• Understanding Phase: Understand what happened and explore deeper meaning.<br />
Discovering learner‟s frames (advocacy / inquiry, etc. – see below)<br />
• Summary Phase: Review what was learned and apply this to a larger context.<br />
“Let‟s identify a few take home points that you will take away from this case<br />
and apply to your future clinical practice.” (I have each learner identify 1 or 2,<br />
then I add in any important ones that weren‟t reiterated at the end.)<br />
The Debriefers<br />
• Share observations, opinions, & judgments<br />
• Have a stance of curiosity, mutuality and respect<br />
• Are respectful and honest; you don‟t have to be “nice”<br />
Debriefer Roles<br />
o Lead debriefer – responsible for overall flow and structure of debriefing<br />
o Assistant debriefer – provides additional thoughts and insight<br />
The DOs:<br />
• ADVOCACY / INQUIRY<br />
Advocacy: “I noticed _______”…<br />
Inquiry: “I was wondering what you thought about that?”<br />
Example: “I noticed _____, I‟m concerned that _____, and am wondering what<br />
_____. I think it may be helpful to talk about this in more detail.”<br />
Increases participation - people are more willing to share their thoughts if you<br />
share yours first<br />
• Ask questions to invite the learners to participate and share their thoughts<br />
• Use normalization “many people have trouble with this” or “this is a difficult case, we<br />
don‟t expect you to manage it perfectly”<br />
• Try to get everyone to participate – pull in the quiet ones (consider using a „softball‟)
• Use group silence to your advantage – someone will eventually talk (max 7 seconds)<br />
• Use the think aloud strategy – have the learner go through their thought processes for a<br />
certain part of the case, ie. “tell me what was going through your mind at this point in the<br />
case.” (This is often asked of the „team leader‟.)<br />
• Have 1-2 short riffs (1-3 minutes each) for clinical content you want to teach<br />
• IF using the + / Delta Debriefing technique, USE IT SPARINGLY<br />
„+‟ = what went well, „delta‟ = what could be done better<br />
Superficial debriefing style – focuses on actions (not frames)<br />
The DON‟Ts:<br />
• Don‟t use the omniscient voice. Use first person instead, since they may have done<br />
something you didn‟t notice. Instead of, “___ wasn‟t done,” state, “I didn‟t notice ___”<br />
• Don‟t use “you” or subjective measures of time (this can be interpreted as accusatory).<br />
Instead of saying “why didn‟t you start CPR for a long time?” state, “I noticed that CPR<br />
wasn‟t started for 2.5 minutes after the patient had a cardiac arrest.” Your objectivity<br />
will keep the learners from becoming defensive and promote meaningful discussion.<br />
• Don‟t try to be “nonjudgmental” (ie. “So, how do you think that case went?”). This is<br />
interpreted as “read my mind” or “guess what I‟m thinking” by the learners. They know<br />
that you know how the case went, since you just watched it. A better question is “That<br />
was a difficult case, how do you feel about it?”<br />
• Don‟t tell them “great job” - they will often disagree and then not trust you<br />
• Don‟t bring up the game, ie. “we tried to get you to do ______, but ….“<br />
• Don‟t let the participants get sidetracked with technical difficulties or limitations of the<br />
simulator. Acknowledge these and move towards your learning points, or relate such<br />
things to clinical practice (ie. Referred breath sounds with PTX)<br />
My General Debriefing Molecule<br />
1) Reactions Phase: Listen to and discuss the participants‟ feelings & thoughts<br />
2) Quick 1 sentence recap of the case / pathology so that everyone is on the same page when<br />
discussing MDM<br />
3) Discuss objectives (MDM & behavioral) and gaps in learner knowledge<br />
i. Understanding Phase: Working feedback (advocacy / inquiry, use of think aloud<br />
strategy, exploring frames, etc). The goal here is to identify why the learners<br />
did what they did, not focus on whether the action was “right” or “wrong.”<br />
ii. Give simple tips on how to improve performance next time if not covered above<br />
iii. Your 2-3 minute riff on important clinical content if not covered above<br />
4) Summary: take home points (I have the learners do this) & application to a larger context
D. Questions to facilitate the debriefing (these are examples below – feel free to use<br />
some / all / none of these or design your own)<br />
1. So, how do you feel about this case? (Reactions Phase)<br />
2. When the patient arrived and was ____________, what was going through<br />
your mind? (Understanding Phase)<br />
3. What was going through your mind when ____________ was discovered?<br />
(Understanding Phase)<br />
4. Do you have an approach that you use every time for ____________?<br />
(Understanding Phase)<br />
5. I noticed that the nurse kept asking about _____________; what was going<br />
through your mind then? (Understanding Phase)<br />
6. What main learning points will you take away from this case and apply to<br />
your clinical practice in the future? (Summary Phase) (I often go around the<br />
table and have each participant state one learning point, and then add on any<br />
important take home points that were not restated during this activity at the<br />
end.)<br />
XII.<br />
XI.<br />
Pilot Testing and Revisions<br />
A. Numbers of participants (maximum of 5 per case):<br />
B. Number of observers (observe from outside of the room):<br />
C. Performance expectations:<br />
D. Anticipated management mistakes (if not covered above):<br />
E. Evaluation form for participants to evaluate the learning experience (if<br />
applicable):<br />
Assessment Tool (if applicable)<br />
XII.<br />
Authors and their affiliations
<strong>Simulation</strong> Module Evaluation – ___________<br />
Faculty: __________________________ Date: ____________ Your Level of Training: __________<br />
1 2 3 4<br />
Strongly Disagree Disagree Agree Strongly Agree<br />
1. This teaching module met the stated clinical objectives (list objectives here).<br />
1 2 3 4<br />
2. The presented case scenario was appropriate for my level of training.<br />
1 2 3 4<br />
3. It was easy to suspend disbelief and buy into the fiction contract.<br />
1 2 3 4<br />
4. The overall utility of this simulated case was very useful.<br />
1 2 3 4<br />
5. The overall quality and utility of the debriefing was good.<br />
1 2 3 4<br />
6. Your debriefers effectively moderated the debriefing and successfully promoted a meaningful group discussion<br />
(versus the debriefing becoming a didactic style learning session).<br />
1 2 3 4<br />
7. This teaching module will better prepare me to manage this type of critically ill patient.<br />
1 2 3 4<br />
8. If you were LEADING in the scenario, this experience was more useful than reading a chapter.<br />
1 2 3 4<br />
9. If you were LEADING in the scenario, this experience was more useful than attending a didactic lecture.<br />
1 2 3 4<br />
10. If you were ASSISTING in the scenario, this experience was more useful than reading a chapter.<br />
1 2 3 4<br />
11. If you were ASSISTING in the scenario, this experience was more useful that attending a didactic lecture.<br />
1 2 3 4<br />
What would you change about this teaching module? Other comments?<br />
_____________________________________________________________________________________________<br />
_______________________________________________________________________________<br />
_____________________________________________________________________________________________<br />
_____________________________________________________________________________________________<br />
________________________________________________________________________
Critical Actions Checklist (for debriefer)<br />
Other Comments<br />
Critical Action #1<br />
Critical Action #2<br />
Critical Action #3<br />
Critical Action #4<br />
Critical Action #5<br />
Critical Action #6