AHMEDABAD DISTRICT - Health and Family Welfare Department
AHMEDABAD DISTRICT - Health and Family Welfare Department
AHMEDABAD DISTRICT - Health and Family Welfare Department
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
REPRODUCTIVE AND CHILD HEALTH PROJECT<br />
<strong>DISTRICT</strong> LEVEL HOUSEHOLD SURVEY - 2002<br />
<strong>AHMEDABAD</strong> <strong>DISTRICT</strong><br />
Sponsored by<br />
Ministry of <strong>Health</strong> <strong>and</strong> <strong>Family</strong> <strong>Welfare</strong><br />
Government of India, New Delhi<br />
Centre for Operations Research <strong>and</strong> Training ( )<br />
Vadodara, Gujarat<br />
2003
W<br />
Study Team<br />
Bella Patel Uttekar<br />
N ay an K u m ar<br />
H em lata S ad h w an i<br />
aj ah at Ullah K h an<br />
V as an t Uttekar<br />
J as h o d a S h arm a<br />
J aw ah ar V i s h w akarm<br />
Prem lata K s h atri y a<br />
a<br />
2
CONTENTS<br />
List of tables ................................................................................................................................ iii<br />
List of figures................................................................................................................................ v<br />
Preface <strong>and</strong> acknowledgement ................................................................................................ vi<br />
Key indicators............................................................................................................................... viii<br />
Salient findings ............................................................................................................................. xi<br />
CHAPTER-1 INTRODUCTION<br />
Page<br />
1.1 Background <strong>and</strong> objectives of the survey................................................................................... 1<br />
1.2 About the district......................................................................................................................... 1<br />
1.3 Survey design <strong>and</strong> sample size of the DLHS-RCH survey........................................................ 2<br />
1.4 House listing ............................................................................................................................... 2<br />
1.5 Questionnaires............................................................................................................................. 3<br />
1.6 Recruitment, training <strong>and</strong> fieldwork........................................................................................... 4<br />
1.7 Data processing <strong>and</strong> tabulation................................................................................................ 4<br />
1.8 St<strong>and</strong>ard of living index (SLI)................................................................................................ 5<br />
CHAPTER-2 HOUSEHOLD CHARACTERISTICS<br />
2.1 Household population................................................................................................................. 7<br />
2.2 General characteristics................................................................................................................ 8<br />
2.3 Housing characteristics ............................................................................................................... 9<br />
2.4 Marital status of household population....................................................................................... 10<br />
2.5 Marriages <strong>and</strong> morbidity................................................................................................ 11<br />
2.6 Mortality................................................................................................................................ 12<br />
CHAPTER-3 CHARACTERISTICS OF THE WOMEN AND FERTILITY<br />
3.1 Characteristics of the currently married women ................................................................ 13<br />
3.2 Current fertility............................................................................................................... 14<br />
3.3 Children ever born <strong>and</strong> living ................................................................................................ 15<br />
3.4 Outcome of pregnancy................................................................................................................ 16<br />
3.5 Birth order ........................................................................................................................ 16<br />
CHAPTER-4 UTILIZATION OF MATERNAL HEALTH SERVICES<br />
4.1 Antenatal check-ups by service provider ................................................................ 17<br />
4.2 Antenatal check-ups at health facility................................................................................ 18<br />
4.3 Antenatal care ................................................................................................................... 19<br />
4.4 Pregnancy complications <strong>and</strong> treatment............................................................................. 22<br />
4.5 Place of delivery ............................................................................................................... 23<br />
4.6 Postnatal care .................................................................................................................... 26<br />
3
Page<br />
CHAPTER-5 CHILD CARE AND IMMUNIZATION<br />
5.1 Breastfeeding <strong>and</strong> weaning practices ................................................................ 29<br />
5.2 Immunization of children................................................................................................ 31<br />
5.3 Source of immunization................................................................................................ 33<br />
5.4 Awareness <strong>and</strong> treatment of diarrhoea................................................................ 34<br />
5.5 Awareness <strong>and</strong> treatment of pneumonia ................................................................ 35<br />
CHAPTER-6 FAMILY PLANNING<br />
6.1 Knowledge of contraceptive methods................................................................................ 37<br />
6.2 Knowledge of No-Scalpel Vasectomy (NSV)................................................................ 39<br />
6.3 Contraceptive prevalence rate ........................................................................................... 39<br />
6.4 Use of contraceptives................................................................................................41<br />
6.5 Source of modern methods of contraception................................................................ 41<br />
6.6 Side-effects of contraception <strong>and</strong> satisfaction with current use................................ 42<br />
6.7 Advice on contraception <strong>and</strong> intention to use family planning in the future....................... 43<br />
6.8 Future fertility intention................................................................................................ 45<br />
6.9 Reasons for discontinuation of use <strong>and</strong> non-use of contraceptives................................ 46<br />
6.10 Unmet need ...................................................................................................................... 48<br />
CHAPTER-7 ACCESSIBILITY AND PERCEPTION ABOUT<br />
GOVERNMENT HEALTH SERVICES<br />
7.1 Home visit by health workers............................................................................................ 49<br />
7.2 Matter discussed with health workers................................................................................ 51<br />
7.3 Visit to government health facility .................................................................................... 52<br />
7.4 Client’s perception of quality of government health services................................ 52<br />
7.5 Reasons for not visiting the government health centre....................................................... 53<br />
CHAPTER-8 REPRODUCTIVE HEALTH<br />
8.1 Awareness about reproductive tract infection (RTI)/<br />
Sexually transmitted infection (STI)................................................................................. 55<br />
8.2 Prevalence of RTI/STI among males <strong>and</strong> females ............................................................. 56<br />
8.3 Symptoms of RTI/STI................................................................................................ 57<br />
8.4 Knowledge of HIV/AIDS ................................................................................................ 59<br />
CHAPTER-9 NUTRITIONAL STATUS AND ANAEMIA<br />
9.1 Methodology .............................................................................................................................. 61<br />
9.2 Procedures ................................................................................................................................ 61<br />
9.3 Haemoglobin response rate................................................................................................ 62<br />
9.4 Weight for age of children................................................................................................63<br />
9.5 Anaemia among children, adolescent <strong>and</strong> pregnant women .................................................... 65<br />
9.6 Iodization of salt ................................................................................................ 68<br />
ANNEXURE I<br />
ANNEXURE II<br />
4
LIST OF TABLES<br />
Page<br />
Table 1.1<br />
Table 1.2<br />
Basic demographic indicators......................................................................................... 2<br />
St<strong>and</strong>ard of living index................................................................................................ 6<br />
Table 2.1 Household population by age <strong>and</strong> by residence <strong>and</strong> sex ................................ 7<br />
Table 2.2 Household characteristics ...................................................................................... 8<br />
Table 2.3 Housing characteristics.......................................................................................... 9<br />
Table 2.4 Marital status of the household population............................................................. 10<br />
Table 2.5 Marriage <strong>and</strong> morbidity rates................................................................................. 11<br />
Table 2.6 Vital rates................................................................................................ 12<br />
Table 3.1 Background characteristics of eligible women ....................................................... 14<br />
Table 3.2 Current fertility................................................................................................ 15<br />
Table 3.3 Fertility ................................................................................................................. 15<br />
Table 3.4 Outcome of pregnancy........................................................................................... 16<br />
Table 3.5 Birth order................................................................................................16<br />
Table 4.1(A) Antenatal check-up................................................................................................ 18<br />
Table 4.1(B) Antenatal check-up................................................................................................ 19<br />
Table 4.2(A) Antenatal care ................................................................................................ 20<br />
Table 4.2(B) Antenatal care ................................................................................................ 21<br />
Table 4.3 Pregnancy complications ....................................................................................... 22<br />
Table 4.4(A) Delivery characteristics ......................................................................................... 24<br />
Table 4.4(B) Delivery characteristics ......................................................................................... 25<br />
Table 4.5 Postnatal care ................................................................................................ 27<br />
Table 5.1 Breastfeeding ................................................................................................ 30<br />
Table 5.2(A) Vaccination of children......................................................................................... 31<br />
Table 5.2(B) Vaccination of children ......................................................................................... 32<br />
Table 5.2(C) Childhood vaccinations received by 12 months of age................................ 33<br />
Table 5.3 Source of vaccinations........................................................................................... 33<br />
Table 5.4 Awareness of diarrhoea ......................................................................................... 34<br />
Table 5.5 Awareness of pneumonia....................................................................................... 36<br />
5
Table 6.1 Knowledge of contraceptive methods................................................................ 38<br />
Table 6.2 No-scalpel vasectomy (NSV) ............................................................................................ 39<br />
Table 6.3 Contraceptive prevalence rate............................................................................................ 40<br />
Table 6.4 Use of contraceptives ................................................................................................ 41<br />
Table 6.5 Source of modern contraceptive methods ................................................................ 42<br />
Table 6.6 <strong>Health</strong> problems <strong>and</strong> satisfaction with current use of contraceptives................................ 42<br />
Table 6.7 Advice on contraceptive use <strong>and</strong> future intention to use..................................................... 44<br />
Table 6.8 Future fertility intention ................................................................................................ 45<br />
Table 6.9 Reasons for discontinuation of use <strong>and</strong> non-use of contraceptive methods......................... 47<br />
Table 6.10 Unmet need....................................................................................................................... 48<br />
Table 7.1 Home visits by health worker ............................................................................................ 50<br />
Table 7.2 Matters discussed during contact with a health or<br />
family planning worker ................................................................................................ 51<br />
Table 7.3 Visit to health facility................................................................................................ 52<br />
Table 7.4 Quality of government health facility ................................................................ 53<br />
Table 7.5 Reasons for not preferring government health facility........................................................ 53<br />
Table 8.1 Knowledge of reproductive tract infection (RTI)/<br />
sexually transmitted infection (STI)................................................................................... 56<br />
Table 8.2 Prevalence of symptoms of RTI/STI among women/ men ................................................. 57<br />
Table 8.3 Symptoms of RTI/STI................................................................................................ 58<br />
Table 8.4 Knowledge of HIV/AIDS................................................................................................ 60<br />
Table 9.1 Haemoglobin response rate ............................................................................................... 63<br />
Table 9.2 Weight for age of children................................................................................................ 64<br />
Table 9.3 Anaemia among children................................................................................................ 66<br />
Table 9.4 Anaemia among adolescent girls ....................................................................................... 67<br />
Table 9.5 Anaemia among pregnant women...................................................................................... 68<br />
Table 9.5 Iodization of salt ................................................................................................ 69<br />
6
LIST OF FIGURES<br />
Page<br />
Figure 4.1 Sources of antenatal care ................................................................................................<br />
17<br />
Figure 4.2 Percentage of women with pregnancy complications ........................................................<br />
23<br />
Figure 4.3 Place of delivery <strong>and</strong> assistance during delivery................................................................<br />
23<br />
Figure 4.4<br />
Institutional delivery by some selected<br />
background characteristics of women................................................................ 25<br />
Figure 5.1 Initiation of breastfeeding ................................................................................................<br />
29<br />
Figure 5.2 Vaccination of children................................................................................................ 31<br />
Figure 6.1 Knowledge of family planning..........................................................................................<br />
37<br />
Figure 6.2 Practice of family planning methods ................................................................ 39<br />
Figure 6.3 Fertility preference among men <strong>and</strong> women................................................................ 45<br />
Figure 7.1 Home visits of health workers by residence ................................................................ 49<br />
Figure 7.2 Visit to government health facility by residence................................................................<br />
52<br />
Figure 8.1 Awareness of RTI/STI by sex <strong>and</strong> residence ................................................................ 55<br />
Figure 8.2 Knowledge of HIV/AIDS by sex <strong>and</strong> residence ................................................................<br />
59<br />
Figure 9.1 Anaemia among children, adolescent girls <strong>and</strong> pregnant women................................ 68<br />
7
Preface <strong>and</strong> Acknowledgement<br />
The need for a person centered quality driven reproductive health programme is now well<br />
accepted all over the world. The Government of India (GoI) has recently launched the<br />
Reproductive <strong>and</strong> Child <strong>Health</strong> (RCH) programme to ensure that men <strong>and</strong> women have<br />
access to adequate information <strong>and</strong> services for reproductive health care. As a first step,<br />
family planning targets have been withdrawn <strong>and</strong> an effort is being made to provide a<br />
package of reproductive services at different levels of health care centers.<br />
Monitoring of the services is also being improved. New indicators are being added to<br />
assess the quality of services <strong>and</strong> provision of an integrated reproductive health care<br />
service. Thus, to assess the quality of services, district level household surveys have been<br />
initiated by the Government of India, which are financed by the World Bank, to cover all<br />
the districts in phases i.e. fifty percent of the districts each in the Phase I <strong>and</strong> Phase II<br />
respectively. Estimates of critical reproductive health indicators for each district were first<br />
obtained during 1998-99 <strong>and</strong> it is now the second time that such estimates of reproductive<br />
health indicators would be obtained during the period 2002-03. Such an exercise would<br />
help in assessing a change, if any, in the level of district wise health indicators in the area<br />
under study. These are important initiatives <strong>and</strong> are certainly quite satisfying for all those<br />
who are concerned with taking ICPD reproductive health agenda ahead. The project is<br />
being coordinated by International Institute for Population Sciences (IIPS), Mumbai <strong>and</strong><br />
implemented by a number of consulting agencies. Centre for Operations Research <strong>and</strong><br />
Training (CORT), a multi disciplinary social science research <strong>and</strong> training organisation<br />
having its headquarters at Baroda, administered this project in various districts of Gujarat.<br />
The present report provides salient findings of selected important indicators of<br />
reproductive <strong>and</strong> child health services covered in the first phase of the survey 2002<br />
collected from the district Ahmedabad in Gujarat. We hope these findings would be useful<br />
to the policy makers <strong>and</strong> researchers alike.<br />
We would like to take this opportunity to thank Shri A.R. N<strong>and</strong>a, former Secretary,<br />
<strong>Department</strong> of <strong>Family</strong> <strong>Welfare</strong>, GoI, who gave us an opportunity to participate as one of<br />
the regional agencies in the survey of national importance. We further acknowledge<br />
Shri J.V.R. Prasada Rao, former Secretary, GoI, Shri P. K. Hota, Secretary, <strong>Department</strong> of<br />
<strong>Family</strong> <strong>Welfare</strong>, GoI, for their continuous help <strong>and</strong> encouragement. We are also thankful<br />
to Dr. K.V. Rao, Chief Director, Shri S.K. Das, Chief Director, Shri S.R. Singh, Director,<br />
Shri Manoj Kumar, Assistant Director, Ministry of <strong>Health</strong> <strong>and</strong> <strong>Family</strong> <strong>Welfare</strong>, GoI. Our<br />
special thanks are due to Prof. T.K. Roy, Director <strong>and</strong> Senior Professor, IIPS, for his<br />
timely advice <strong>and</strong> valuable guidance. We also acknowledge the contributions of<br />
Prof. F. Ram, Dr. B. Paswan, Dr. L. Ladu Singh, coordinators of the project at IIPS. Our<br />
thanks are due to Prof. Sulabha Parasuraman, Ex. Coordinator of the RCH project at IIPS<br />
<strong>and</strong> Prof. K. Srinivasan, Ex. Director of IIPS <strong>and</strong> presently Consultant RCH project, for<br />
supervising the task of the survey right from the beginning of the project.<br />
8
Our special thanks are due to Shri S.K. Nath, Addl. D.G. of NSSO, Kolkata, Census<br />
<strong>and</strong> NSSO officials at the state <strong>and</strong> district level for providing all necessary supports. We<br />
wish to put on record our deep sense of appreciation <strong>and</strong> special thanks to<br />
Ms. S.K. Verma, Additional Chief Secretary <strong>and</strong> Principal Secretary (<strong>Family</strong> <strong>Welfare</strong>),<br />
Government of Gujarat, Dr. S.S. Vaishya, Director, Medical <strong>and</strong> <strong>Health</strong> Services, Union<br />
Territory of Daman <strong>and</strong> Diu, Director, State Institute of <strong>Health</strong> <strong>and</strong> <strong>Family</strong> <strong>Welfare</strong>,<br />
Gujarat, Dr. P. M. Parmar, District <strong>Health</strong> Officer (DHO) of Ahmedabad district <strong>and</strong> other<br />
District authorities without whose help <strong>and</strong> co-operation this study would have not been<br />
feasible. This facilitated us in the smooth <strong>and</strong> timely completion of the data collection.<br />
Thanks are due to UNICEF for funding the health component of survey. We are<br />
especially thankful to Dr. C. Ch<strong>and</strong>rasekar <strong>and</strong> Dr. V. Jayach<strong>and</strong>ran, for their keen interest<br />
<strong>and</strong> timely supply of necessary inputs for the successful completion of the health<br />
component of the survey. We also thank Dr. Prema Ramch<strong>and</strong>ran, Advisor, Planning<br />
Commission, for her keen interest in the subject.<br />
We thank Dr. K. Vijayaraghavan, Deputy Director, National Institute of Nutrition,<br />
Hyderabad for training the health investigators.<br />
Thanks are also due to Mr. Nizamuddin Khan, Research Officer, IIPS, for his<br />
assistance at various stages of the project.<br />
Our special thanks are due to the team of supervisors <strong>and</strong> investigators who took all<br />
the pain in collecting the data <strong>and</strong> completing the project well in time. Last but not the<br />
least, the credit goes to the respondents in the district who spared their valuable time <strong>and</strong><br />
provided key information for the RCH-DLHS project.<br />
This work would not have been completed without the full organizational support <strong>and</strong><br />
help from all our colleagues. We are thankful to all of them.<br />
Prof. M. M. G<strong>and</strong>otra November 2003<br />
Director<br />
Centre for Operations Research<br />
<strong>and</strong> Training (CORT), Vadodara<br />
9
KEY INDICATORS FOR DLHS-RCH - 2002<br />
<strong>AHMEDABAD</strong> <strong>DISTRICT</strong> OF GUJARAT STATE<br />
1. Population data, 2001 census<br />
Population 2001 Census (in thous<strong>and</strong>)<br />
Percentage of urban population<br />
Annual exponential population growth rate (1991-2001)<br />
5808<br />
80.1<br />
2.36<br />
Indicators<br />
2. Sample population<br />
Number of households interviewed<br />
Number of eligible women interviewed<br />
Number of husb<strong>and</strong>s interviewed<br />
3. Background characteristics of households interviewed<br />
Percentage Hindu<br />
Percentage Muslim<br />
Percentage Jain<br />
Percentage scheduled caste<br />
Percentage scheduled tribe<br />
Percentage other backward class<br />
Percentage with low st<strong>and</strong>ard of living index (SLI)<br />
Percentage with high st<strong>and</strong>ard of living index (SLI)<br />
4. Background characteristics of eligible women interviewed<br />
Percentage below age 30<br />
Percentage with age at first cohabitation below age 18<br />
Percentage Illiterate<br />
Percentage having 10+ years of schooling<br />
Percentage with Illiterate husb<strong>and</strong><br />
Percentage with husb<strong>and</strong> having 10+ years of schooling<br />
5. Marriages (after 1-1-1999)<br />
Mean age at marriage for boys<br />
Mean age at marriage for girls<br />
Percentage of boys married at age less than 21<br />
Percentage of girls married at age less than 18<br />
6. Fertility<br />
Mean children ever born to women age 40-44<br />
Crude birth rate (CBR)<br />
Total fertility rate (TFR)<br />
Birth order<br />
1<br />
2<br />
3<br />
4+<br />
7. Mortality <strong>and</strong> Morbidity<br />
Crude death rate (CDR)<br />
Infant mortality rate (IMR)<br />
Prevalence** of complete blindness<br />
Prevalence** of partial blindness<br />
Prevalence** of tuberculosis<br />
Prevalence** of malaria<br />
8. Knowledge of <strong>Family</strong> Planning<br />
Percentage of eligible women knowing<br />
Any modern method<br />
Any modern spacing method<br />
All modern methods<br />
Percentage of husb<strong>and</strong>s knowing No-Scalpel Vasectomy (NSV)<br />
Note: ** Prevalence rate per 100000 population<br />
1007<br />
769<br />
404<br />
90.2<br />
3.2<br />
5.6<br />
10.1<br />
2.5<br />
43.2<br />
10.2<br />
59.3<br />
48.1<br />
32.9<br />
32.9<br />
34.6<br />
10.7<br />
54.3<br />
20.9<br />
17.5<br />
28.8<br />
32.5<br />
3.3<br />
23.3<br />
2.1<br />
51.9<br />
18.4<br />
21.0<br />
8.7<br />
4.94<br />
47.63<br />
255<br />
3146<br />
85<br />
506<br />
100.0<br />
99.1<br />
81.9<br />
52.9<br />
10
Indicators<br />
9. Current users of family planning<br />
Percentage of eligible women/husb<strong>and</strong>s using<br />
Any method<br />
Any modern method<br />
Female sterilisation<br />
Male sterilisation<br />
IUD<br />
Pills<br />
Condom<br />
Any traditional method<br />
10. Unmet Need<br />
Percentage of women having unmet need for<br />
Limiting<br />
Spacing<br />
Total<br />
11. Maternal <strong>Health</strong> Care<br />
Percent of eligible women with last live/still birth after 01-01-1999<br />
A. ANC check-up<br />
(i) No ANC check-up<br />
(ii) Who had ANC check-up<br />
(iii) Who had three or more ANC check-up<br />
(iv) Who had ANC at home<br />
B. T.T. injection during pregnancy<br />
(i) Who had no TT injection<br />
(ii) Who had one TT injection<br />
(iii) Who had two or more TT injections<br />
C. IFA tablets during pregnancy<br />
(i) Who consumed two or more tablets regularly<br />
(ii) Who had received 100 or more tablets<br />
D. Received full ANC<br />
(3 ANC check-ups <strong>and</strong> at least one TT <strong>and</strong> 100+ IFA tablets)<br />
E. Institutional delivery<br />
(i) Government health facility<br />
(ii) Private health facility<br />
F. Home delivery<br />
(i) Attended by Doctor/ ANM/ Nurse/TBA<br />
G. Safe delivery :<br />
(Either Institutional delivery or home delivery attended by Doctor/ ANM/ Nurse/TBA)<br />
12. Child Care<br />
A. Percentage of women who started breastfeeding immediately/within 2<br />
hours of the birth to their children<br />
B. Percentage of women who gave exclusive breast milk for at least 4 months to their children<br />
(A <strong>and</strong> B relate to the youngest child born after 1-1-1999 )<br />
C. Percentage of children (born after 1-1-1999 <strong>and</strong> age 12 months <strong>and</strong> older at the time of survey)<br />
who received<br />
(i) BCG<br />
(ii) DPT (Three injections)<br />
(iii) Polio (Three doses)<br />
(iv) Measles<br />
(v) Complete immunizations (BCG + 3 DPT + 3 Polio + measles)<br />
D. Percentage of eligible women whose children (born after 1-1-1999) had diarrhoea <strong>and</strong> who were<br />
treated with ORS<br />
(i) Had Diarrhoea<br />
(ii) Given ORS<br />
56.3<br />
50.2<br />
26.8<br />
1.0<br />
5.6<br />
8.1<br />
8.7<br />
6.1<br />
9.9<br />
2.4<br />
12.3<br />
39.1<br />
8.2<br />
91.8<br />
77.6<br />
6.3<br />
10.6<br />
5.7<br />
83.7<br />
20.4<br />
29.1<br />
28.3<br />
12.3<br />
59.4<br />
45.5<br />
84.6<br />
22.9<br />
5.0<br />
93.3<br />
74.4<br />
72.4<br />
76.7<br />
64.2<br />
4.8<br />
7.5<br />
11
Indicators<br />
13. Awareness of RTI/STI <strong>and</strong> HIV/AIDS<br />
(i) Percentage of eligible women aware of RTI/STI<br />
(ii) Percentage of husb<strong>and</strong>s aware of RTI/STI<br />
(iii) Percentage of eligible women aware of HIV/AIDS<br />
(iv) Percentage of husb<strong>and</strong>s aware of HIV/AIDS<br />
14. Reproductive Morbidity<br />
A. Percent of eligible women had their last pregnancy since 1-1-1999, having<br />
(i) Pregnancy complication<br />
(ii) Delivery complication<br />
(iii) Post-Delivery complication<br />
B. Percent of eligible women having side effects due to use of contraceptive method<br />
(i) Female sterilization<br />
(ii) IUD<br />
(iii) Pills<br />
C. Menstruation related problem<br />
D. Any symptom of RTI/STI (abnormal vaginal discharge)<br />
E. Percent of husb<strong>and</strong> having any symptom of RTI/STI<br />
15. Home Visit by <strong>Health</strong> Worker<br />
A. Percent of women visited by ANM/ health worker during three months prior to survey date<br />
B. Percent of women who had said worker spent enough time with them<br />
16. Utilisation of Government <strong>Health</strong> Services<br />
Percentage of women who utilised government health facility for<br />
(i) Antenatal care<br />
(ii) Treatment of complications during pregnancy<br />
(iii) Treatment of post-delivery complications<br />
(iv) Treatment of complications due to contraceptive use<br />
(a) Female sterilization<br />
(b) IUD<br />
(c) Pills<br />
(v) Treatment for RTI/STI (vaginal discharge)<br />
36.6<br />
59.5<br />
59.8<br />
88.3<br />
26.6<br />
51.7<br />
14.8<br />
11.3<br />
6.9<br />
16.6<br />
12.7<br />
13.7<br />
4.7<br />
14.1<br />
77.9<br />
20.4<br />
11.4<br />
4.2<br />
5.0<br />
0.0<br />
0.0<br />
12.5<br />
12
CHAPTER – 1<br />
INTRODUCTION<br />
1.1 BACKGROUND AND OBJECTIVES OF THE SURVEY<br />
The Reproductive <strong>and</strong> Child <strong>Health</strong> (RCH) programme interventions that are being<br />
implemented by Government of India (GoI) are expected to provide quality services <strong>and</strong><br />
achieve multiple objectives. There has been a positive paradigm shift from Method-Mix-<br />
Target based activity to client-centred-dem<strong>and</strong> driven quality services. Attempts are being<br />
made by GoI to not only re-orient the programme <strong>and</strong> the attitude of service provider's<br />
attitude at grass-roots level, but also to strengthen the services at outreach levels.<br />
The new approach requires decentralisation of planning, monitoring <strong>and</strong> evaluation of<br />
the services. Under such objectives, the district being the basic nucleus of administration, GoI<br />
has been interested in generate district level data, other than service statistics, on the<br />
utilisation of services provided by government health facilities. It is also of interest to GoI<br />
assess people's perceptions of the quality of these services. Therefore, it was decided to<br />
undertake District Level Household Surveys (DLHS) under the RCH Project in the country.<br />
In the Phase I of the second round of DLHS-RCH about 50 percent of the districts were<br />
covered <strong>and</strong> the remaining districts are to be taken-up in the Phase II of the DLHS-RCH.<br />
Ahmedabad district is one of the selected districts covered in the Phase I of the project in<br />
Gujarat.<br />
The main focus of the District Level Household Survey is on the following aspects:<br />
1. Coverage of ANC & immunisation services<br />
2. Proportion of safe deliveries<br />
3. Contraceptive Prevalence Rates<br />
4. Unmet need for <strong>Family</strong> Planning<br />
5. Awareness about RTI/STI <strong>and</strong> HIV/AIDS<br />
6. Utilisation of health services <strong>and</strong> the users’ satisfaction.<br />
1.2 ABOUT THE <strong>DISTRICT</strong><br />
Ahmedabad district is situated in the central part of Gujarat. The total l<strong>and</strong> area of the district<br />
is 8086 sq.kms.<br />
As shown in Table 1.1, the population of Ahmedabad district is 58.1 lakh as per 2001<br />
census <strong>and</strong> constitutes about 11 percent of the population of the state. The district has a<br />
population density of 718 persons per sq. km., which is high compared to 258 persons per<br />
square kilometre in the state. The annual exponential growth rate of the district during 1991-<br />
2001 is 2.3 percent, which is higher than that of the state (2.03 percent). About 80 percent of<br />
the population of the district live in urban areas in contrast to 38 percent in the state. The sex<br />
ratio of the district is 892 females per 1000 males, which is lower than that of the state<br />
average of 921.<br />
13
The literacy rate (population age 7+ years) of the district is 80 percent, with 87 percent<br />
for males <strong>and</strong> 71 percent for females, which are higher than the respective rates of the state.<br />
Thus, both in terms of level of literacy rate as well as the extent of urbanisation Ahmedabad<br />
district is at an advantage position as compared to the state as a whole.<br />
Table 1.1: BASIC DEMOGRAPHIC INDICATORS<br />
Demographic indicators of Ahmedabad district of Gujarat<br />
Indicators Ahmedabad Gujarat<br />
Population (in thous<strong>and</strong>s)<br />
5808 50597<br />
Average annual exponential growth rate (in percent)<br />
Population density (per sq km)<br />
Sex ratio (females per 1000 males)<br />
Percent urban<br />
Percent of literate population age 7+ years<br />
Person<br />
Male<br />
Female<br />
Source : Census, 2001<br />
2.359<br />
718<br />
892<br />
80.09<br />
79.89<br />
86.81<br />
71.12<br />
2.028<br />
258<br />
921<br />
37.67<br />
69.97<br />
80.50<br />
58.60<br />
1.3 SURVEY DESIGN AND SAMPLE SIZE OF THE DLHS-RCH SURVEY<br />
Like the First Round, in Round II again in the Phase I of the DLHS-RCH, nearly 50 percent<br />
of the 25 districts as existed in 2001 census were selected with r<strong>and</strong>om start from either the<br />
first or the second district <strong>and</strong> then every alternative district were selected. With this<br />
procedure, 13 districts were covered in Gujarat state in the Phase I in 2002 <strong>and</strong> the remaining<br />
12 districts will be taken-up for the second phase of the DLHS-RCH. In each of the selected<br />
districts, 40 Primary Sampling Units (PSUs - Villages/Wards/UFS) were selected with<br />
probability proportional to size (PPS) after stratification of the PSU. The village/ward level<br />
population as per 1991 census was used for this purpose. The list of PSUs covered for the<br />
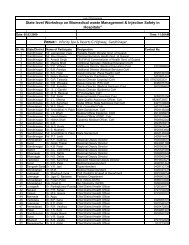
survey in Ahmedabad district is given in Annexure II.<br />
The sample size for the DLHS-RCH was fixed at 1000 households, i.e. 25 households<br />
from each of the 40 selected PSUs. In order to take care of non-response due to various<br />
reasons, over sampling of 10 percent of the households was done. In addition to this, each<br />
selected PSU was visited twice to improve the coverage. Thus, in all, 28 households from<br />
each PSU were selected following circular systematic r<strong>and</strong>om sampling procedure.<br />
1.4 HOUSE LISTING<br />
A household listing operation carried out in each of the selected PSUs prior to the data<br />
collection provided the necessary frame for selecting the households for the DLHS-RCH.<br />
The household listing involved, preparation of location map of each selected PSU, layout<br />
sketch of the structures, <strong>and</strong> recording details of the households in these structures in the<br />
selected PSU (village/urban frame size). Twelve independent teams carried out this exercise,<br />
each comprising, one lister <strong>and</strong> one mapper under the overall supervision <strong>and</strong> monitoring of<br />
the research staff of CORT.<br />
A complete listing was carried out in the villages with households up to 300. In case of<br />
large villages with more than 300 household, the villages were divided into two or more<br />
segments of equal size depending on the estimated number of households <strong>and</strong> one segment in<br />
14
each village was selected at r<strong>and</strong>om. In each of the selected segments, a complete listing was<br />
carried out for the selection of the households.<br />
In the case of small villages with less than 50 households, the village was combined with<br />
the nearest village available. After combining it with the nearest village the same sampling<br />
procedure was adopted as mentioned above.<br />
1.5 QUESTIONNAIRES<br />
The International Institute for Population Sciences (IIPS), Mumbai, the Nodal Agency for<br />
DLHS-RCH Project has made necessary modifications in Household Questionnaire <strong>and</strong><br />
Women's Questionnaire <strong>and</strong> added three more Questionnaires i.e., Husb<strong>and</strong>'s<br />
Questionnaire, Village Questionnaire <strong>and</strong> <strong>Health</strong> <strong>and</strong> Nutritional Questionnaire in<br />
consultation with MoHFW <strong>and</strong> World Bank. These questionnaires were discussed <strong>and</strong><br />
finalized in training cum workshop organized at IIPS during the first week of November<br />
2001.<br />
These questionnaires had been canvassed in the Phase I of Round II of the DLHS-<br />
RCH survey, taking into consideration the viewpoints of all the regional agencies involved<br />
in the survey. The house listing teams <strong>and</strong> the interviewers <strong>and</strong> the supervisors for the<br />
main survey were given rigorous training, based on the manuals developed for the purpose<br />
by the Nodal Agency.<br />
The Household Questionnaire was used to list all the usual members in the selected<br />
households as well any visitors who stayed in the household, the night before the<br />
interview, <strong>and</strong> to collect information on marriages, births, infant <strong>and</strong> maternal deaths since<br />
1 st January, 1999 among the usual residents of the households. In addition, the<br />
questionnaire contained question for collecting information on socio-economic<br />
characteristics of the households, <strong>and</strong> the incidence/prevalence of malaria, tuberculosis<br />
<strong>and</strong> blindness. For all the marriages reported in the survey, the age at marriage of boys <strong>and</strong><br />
girls that were performed in the household since 1 st January 1999 was recorded.<br />
The Women's Questionnaire was used to collect information from the eligible women<br />
listed in the household questionnaire, i.e., all currently married women age 15-44 years<br />
who were usual residents of the selected household or visitors who stayed in the selected<br />
household the night before the interview <strong>and</strong> whose marriage were consummated.<br />
The Women's Questionnaire consisted of the following broad sections:<br />
Woman's characteristics<br />
Antenatal, natal <strong>and</strong> postnatal care<br />
Immunization <strong>and</strong> childcare<br />
Contraception<br />
Quality of Government health services <strong>and</strong> client's satisfaction<br />
Awareness of RTI/STI <strong>and</strong> HIV/AIDS <strong>and</strong> reported symptoms of RTI/STI.<br />
The Husb<strong>and</strong> Questionnaire was used to collect information, from the husb<strong>and</strong>'s of<br />
eligible women listed in the household questionnaire, on knowledge of RTI/STI <strong>and</strong><br />
HIV/AIDS, <strong>and</strong> reported symptoms of RTI/STI <strong>and</strong> male participation in family planning.<br />
15
The Village Questionnaire collected information on availability on health <strong>and</strong><br />
education facilities in the village <strong>and</strong> whether the health facilities accessible throughout<br />
the year.<br />
In addition, the health investigator in each survey team measured the weight of<br />
children below 72 months of age at the time of survey. The health investigator also<br />
collected the blood sample from children below 72 months of the age, pregnant women<br />
<strong>and</strong> adolescent's girls from selected households to assess hemoglobin level. This<br />
information is useful for assessing prevalence rates of anemia among pregnant women,<br />
adolescents'girls <strong>and</strong> children.<br />
The questionnaires were printed in both English <strong>and</strong> Gujarati languages.<br />
1.6 RECRUITMENT, TRAINING AND FIELDWORK<br />
A total of 72 field persons were recruited for conducting the survey in Gujarat state. The field<br />
investigators were both males <strong>and</strong> females with at least a Bachelor’s degree in social science<br />
subjects. Most of the field interviewers had some work experience after obtaining their<br />
Bachelor’s degree <strong>and</strong> had previous field experience. All health investigators were DMLT<br />
<strong>and</strong> had worked in some laboratory. All the supervisors were males <strong>and</strong> had obtained a<br />
Master’s degree. Most of the field interviewers had some working experience after<br />
Bachelor’s degree. The supervisors were those who had more field experience.<br />
A total of 12 teams were formed for data collection in the state. Each team consisted of<br />
one male supervisor, three female interviewers, one male investigator <strong>and</strong> one health<br />
investigator.<br />
The training of field staff for the main survey was organised for the teams at Jeevan<br />
Darshan, Baroda during July 2002 following the guidelines given by the Nodal Agency. The<br />
professional staff members of the CORT were involved in the training. After 8 days of<br />
classroom training, the teams were taken to the field to collect data from the rural/urban areas<br />
in the presence of trainers. Their filled in questionnaires were thoroughly scrutinised to see<br />
gaps in their underst<strong>and</strong>ing. Such classroom <strong>and</strong> field training exercise were repeated till the<br />
trainers were satisfied with the total underst<strong>and</strong>ing of the questionnaires by the field teams.<br />
Monitoring <strong>and</strong> supervision was carried out by the professional staff of the CORT. During<br />
the period of survey, the IIPS team headed by a Research Officer did the 10 percent quality<br />
check. Fieldwork was carried out in the Ahmedabad district of Gujarat state in January 2003.<br />
1.7 DATA PROCESSING AND TABULATION<br />
All the completed questionnaires were brought to headquarters of CORT, Baroda for data<br />
processing. The data were processed using Micro Computers. The process consisted of<br />
office editing of questionnaires, data entry, data cleaning <strong>and</strong> tabulation. Data cleaning<br />
included validation, range <strong>and</strong> consistency checks. IIPS developed the software package<br />
for both data entry <strong>and</strong> tabulation of the data<br />
In generating state level demographic indicator sample weight for household, women,<br />
husb<strong>and</strong> <strong>and</strong> children’s, weight have been used <strong>and</strong> these for a particular district are based on<br />
three sections probabilities f i i<br />
1 , f 2<br />
i<br />
<strong>and</strong> f 3 pertaining to i th PSU of the district. These<br />
probabilities are defined as,<br />
i<br />
f 1 =Probability of selection of i th PSU of the district<br />
16
=( n<br />
r * H i )/ H, where n r is the number of rural PSU to be selected from the district, H i<br />
refers to the number of households in the i th PSU <strong>and</strong> H = Σ H i , total number of households<br />
in the district.<br />
f 2<br />
i<br />
= Probability of selecting segment (s) from segmented PSU (in case the i th selected<br />
PSU is segmented)<br />
= (number of segments selected after segmentation of PSU) / (number of segment a PSU<br />
is divided)<br />
The value of f 2<br />
i<br />
is to be equal to one for unsegmented PSU.<br />
f 3<br />
i<br />
=probability of selecting a household from the total listed households of a PSU or<br />
segment of a PSU<br />
=(28*HR i )/ HL i<br />
Where HR i is the household response rate of the i th sampled PSU <strong>and</strong> HL i is the number of<br />
households listed in i th PSU of the district.<br />
For urban PSU, f 1<br />
i<br />
is computed either as the ratio of number of urban PSUs to be included<br />
from the district to the total number of UFS blocks of the district or as the ratio of urban<br />
population of the selected PSU to the total urban population of the district.<br />
The probability of selecting a household from the district works out as<br />
f i = f 1<br />
i<br />
* f 2<br />
i<br />
* f 3<br />
i<br />
The non- normalized weight for the i th PSU of the district is, w i = 1/f i while the normalized<br />
weight used in the generation of district indicators separately for rural <strong>and</strong> urban PSUs of the<br />
i th district is<br />
∑<br />
n<br />
i<br />
= i<br />
i<br />
* w<br />
i<br />
∑ n i * w<br />
i<br />
.<br />
Where n i is the number of households interviewed in the i th PSU. The weight for women,<br />
husb<strong>and</strong>s <strong>and</strong> children respectively is computed in a similar manner considering the<br />
corresponding response rate.<br />
1.8 STANDARD OF LIVING INDEX (SLI)<br />
In Phase-I of First Round of the RHS, type of house alone was taken as the proxy for the<br />
economic status of the households. But in Phase-II, questions related to household amenities<br />
<strong>and</strong> possession of some selected household items were considered for developing economic<br />
status index. In order to develop SLI, the following scores related to response categories for<br />
each question were given:<br />
17
Table 1.2: STANDARD OF LIVING INDEX (SLI)<br />
Sr. No Variable Categories Scores<br />
1 Source of Drinking Water 1.Tap (own)<br />
2.Tap shared<br />
3.H<strong>and</strong> pump + Well<br />
4.Others<br />
3<br />
2<br />
1<br />
0<br />
2 Type of House 1. Pucca<br />
2. Semi Pucca<br />
3.Kachcha<br />
3 Source of Lighting 1.Electricity<br />
2.Kerosene<br />
3.Other<br />
4<br />
2<br />
0<br />
2<br />
1<br />
0<br />
4 Fuel for Cooking 1.LPG<br />
2.Kerosene<br />
3.Others<br />
5 Toilet Facility 1.Own Flush Toilet<br />
2.Own Pit Toilet<br />
3.Shared Toilet<br />
4.No Toilet<br />
6 Ownership of items 1.Fan<br />
2.Radio/Transistor<br />
3. Sewing machine<br />
4.Television<br />
5.Telephone<br />
6.Bicycle<br />
7.Motor cycle/Scooter<br />
8.Car<br />
9.Tractor<br />
2<br />
1<br />
0<br />
4<br />
2<br />
2<br />
0<br />
2<br />
2<br />
2<br />
3<br />
3<br />
2<br />
3<br />
4<br />
4<br />
The total of the scores may vary from the lowest of 0 to a maximum of 40. On the basis of<br />
total score, households are divided into three categories as:<br />
(a) Low if total score is less than or equal to 9.<br />
(b) Medium if total score is greater than 9 but less than or equal to 19.<br />
(c) High if total score is greater than 19.<br />
Most of the indicators under DLHS-RCH, Phase I of the Second Round are also<br />
tabulated by these three categories of SLI, in addition to variables like residence<br />
(rural/urban), caste <strong>and</strong> education.<br />
18
CHAPTER – 2<br />
HOUSEHOLD CHARACTERISTICS<br />
This chapter presents the demographic <strong>and</strong> socio-economic characteristics of the households<br />
interviewed in the DLHS-RCH Ahmedabad district of Gujarat. The DLHS-RCH household<br />
population is tabulated by de facto population only. This may differ from the de jure<br />
population because of temporary population movements <strong>and</strong> would result in non-coverage of<br />
usual residents who are temporarily elsewhere at the time of the survey.<br />
2.1 HOUSEHOLD POPULATION<br />
Table 2.1 presents the percentage of household population by age, residence <strong>and</strong> sex. The sex<br />
ratio i.e., the number of males per 100 females is 105. There was not much variation in the<br />
sex ratio in urban <strong>and</strong> the rural areas of the district. The total sample population covered in<br />
district is 4,943 with 2530 males <strong>and</strong> 2413 females. Around 29 percent of them fall in age<br />
group 0-14 <strong>and</strong> 32 percent in the age group of 15-29 years. A significant difference was<br />
observed in the age distribution of population in rural <strong>and</strong> urban areas. About one-third of the<br />
total population in the rural areas (33 percent) were in the age cohort of 0-14 years whereas in<br />
urban areas the corresponding proportion of this age group was 28 percent. On the other<br />
h<strong>and</strong>, while 25 percent of the rural population was in the age group (15-29), slightly higher<br />
percentage (34 percent) of the urban population is in this age group. Higher proportion below<br />
age 15 in rural areas is an indication of the fact that rural fertility is slightly higher than that of<br />
the urban fertility in this district. About seven percent of the total population were reported to<br />
be in the older age group of 60 years <strong>and</strong> above.<br />
Table 2.1 HOUSEHOLD POPULATION<br />
Percentage distribution of the household population by age <strong>and</strong> by residence <strong>and</strong> sex, Ahmedabad district of Gujarat, RCH,<br />
2002<br />
Age group<br />
(in years)<br />
0-4<br />
5-9<br />
10-14<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
45-49<br />
50-59<br />
60+<br />
Total<br />
10.1<br />
9.4<br />
9.7<br />
12.1<br />
11.2<br />
8.6<br />
6.0<br />
6.9<br />
6.2<br />
4.4<br />
8.4<br />
7.0<br />
Residence<br />
Sex<br />
Rural Urban Male Female<br />
Total Percentage 100.0 100.0 100.0 100.0 100.0<br />
Number of persons 4943 969 3974 2530 2413<br />
Sex Ratio (100*M/F) 105 103 105 NA NA<br />
Table is based on the 'de facto' population<br />
11.0<br />
12.2<br />
9.9<br />
8.9<br />
7.9<br />
7.8<br />
6.8<br />
7.3<br />
5.8<br />
4.1<br />
9.1<br />
9.0<br />
9.8<br />
8.8<br />
9.6<br />
12.8<br />
12.0<br />
8.7<br />
5.8<br />
6.8<br />
6.3<br />
4.5<br />
8.3<br />
6.5<br />
NA: Not applicable<br />
10.7<br />
8.7<br />
10.0<br />
10.7<br />
11.9<br />
8.9<br />
5.6<br />
7.0<br />
6.2<br />
4.2<br />
9.8<br />
6.2<br />
9.5<br />
10.2<br />
9.4<br />
13.5<br />
10.5<br />
8.2<br />
6.4<br />
6.8<br />
6.3<br />
4.6<br />
6.9<br />
7.8<br />
19
2.2 GENERAL CHARACTERISTICS<br />
Table 2.2 presents the percentage distribution of households by selected background<br />
characteristics. Male is the head in almost all of the households in Ahmedabad district.<br />
Almost 95 percent of the households are headed by male <strong>and</strong> only five percent households<br />
are headed by female. More or less same situation existed in rural <strong>and</strong> urban areas of the<br />
district.<br />
Table 2.2 HOUSEHOLD CHARACTERISTICS<br />
Percent distribution of households by selected characteristics of household head <strong>and</strong> household size, according to<br />
residence, Ahmedabad district of Gujarat, RCH, 2002<br />
Residence<br />
Characteristic<br />
Total<br />
Rural<br />
Sex of the household head<br />
Male<br />
Female<br />
Age of the household head<br />
Less than 30<br />
30-44<br />
45-59<br />
60+<br />
95.1<br />
4.9<br />
14.4<br />
35.8<br />
34.2<br />
15.6<br />
95.5<br />
4.5<br />
8.8<br />
39.6<br />
29.6<br />
22.0<br />
Urban<br />
95.0<br />
5.0<br />
15.8<br />
34.8<br />
35.3<br />
14.0<br />
Median age of the household head 44.9 45.8 44.7<br />
Religion of household head<br />
Hindu<br />
Muslim<br />
Christian<br />
Jain<br />
Zoroastrian<br />
90.2<br />
3.2<br />
0.5<br />
5.6<br />
0.5<br />
93.5<br />
6.5<br />
0.0<br />
0.0<br />
0.0<br />
89.4<br />
2.4<br />
0.6<br />
7.0<br />
0.6<br />
Caste/tribe of household head<br />
Scheduled caste<br />
Scheduled tribe<br />
Other backward class<br />
Other#<br />
Don’t know<br />
Number of usual members*<br />
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9+<br />
3.5<br />
4.7<br />
16.8<br />
20.5<br />
18.3<br />
14.3<br />
9.8<br />
2.1<br />
10.1<br />
3.3<br />
9.6<br />
11.2<br />
12.4<br />
25.4<br />
17.1<br />
8.7<br />
3.1<br />
9.3<br />
3.6<br />
3.4<br />
18.2<br />
22.4<br />
16.5<br />
13.6<br />
10.1<br />
1.8<br />
10.3<br />
Mean household size 5.2 5.2 5.2<br />
Number of households 1007 198 809<br />
* Based on the de jure population<br />
# Higher caste (not belonging to scheduled caste, scheduled tribe or other backward class)<br />
10.1<br />
2.5<br />
43.2<br />
43.2<br />
0.9<br />
20.7<br />
0.0<br />
49.0<br />
30.3<br />
0.0<br />
7.6<br />
3.1<br />
41.8<br />
46.4<br />
1.1<br />
Around 14 percent of the head of the households are below 30 years of age. The<br />
corresponding percentage is nine in the rural area <strong>and</strong> 16 in the urban area. The heads of the<br />
households belonging to age group 30-44 are 40 percent in rural <strong>and</strong> 35 percent in the urban<br />
areas. The median age of the head of the households is 45 years. Majority of the sample<br />
population are Hindus (90 percent). Very small percent belonged to other religious group, six<br />
percent Jain, three percent Muslims <strong>and</strong> negligible proportion to other groups. Overall, there<br />
are about 10 percent of SC <strong>and</strong> three percent of ST households. Nearly 70 percent of the rural<br />
households <strong>and</strong> 53 percent of the urban households belong to Scheduled castes, Scheduled<br />
tribes <strong>and</strong> other backward castes. The average household size is 5.2 in rural <strong>and</strong> urban areas<br />
of the district.<br />
20
2.3 HOUSING CHARACTERISTICS<br />
Table 2.3 presents the percentage distribution of households by selected background<br />
characteristics. The main source of lighting is electricity in nearly 97 percent of the<br />
households being 98 percent in the urban areas <strong>and</strong> 94 percent in the rural areas.<br />
Table 2.3 HOUSING CHARACTERISTICS<br />
Percentage distribution of households by housing characteristics, according to residence, Ahmedabad district of Gujarat,<br />
RCH, 2002<br />
Housing characteristics<br />
Electricity<br />
No<br />
Yes<br />
Source of drinking water<br />
Tap<br />
H<strong>and</strong> pump/bore well<br />
Well<br />
Other<br />
Sanitation facility<br />
Own flush toilet<br />
Shared toilet (any type)<br />
Public/community toilet (any type)<br />
No toilet facility<br />
Main type of fuel used for cooking<br />
Liquid petroleum gas/electricity<br />
Kerosene<br />
Wood<br />
Other<br />
Type of house<br />
Kachcha<br />
Semi-pucca<br />
Pucca<br />
Households assets<br />
Fan<br />
Radio/transistor<br />
Sewing machine<br />
Television<br />
Telephone<br />
Bicycle<br />
Motor cycle/scooter<br />
Car/ jeep<br />
Tractor<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
21<br />
Total<br />
2.6<br />
97.4<br />
93.6<br />
1.8<br />
2.4<br />
2.2<br />
65.1<br />
8.5<br />
0.8<br />
25.6<br />
63.7<br />
8.6<br />
27.4<br />
0.3<br />
6.0<br />
21.3<br />
72.7<br />
94.9<br />
39.2<br />
15.5<br />
74.1<br />
27.5<br />
55.8<br />
34.6<br />
4.0<br />
1.5<br />
Residence<br />
Rural<br />
5.6<br />
94.4<br />
82.6<br />
4.9<br />
1.2<br />
11.3<br />
17.5<br />
1.3<br />
0.0<br />
81.2<br />
11.0<br />
2.9<br />
85.2<br />
0.9<br />
27.5<br />
48.7<br />
23.8<br />
85.4<br />
18.5<br />
4.2<br />
44.1<br />
11.6<br />
41.3<br />
14.3<br />
0.6<br />
7.5<br />
Urban<br />
10.2<br />
30.5<br />
59.3<br />
42.4<br />
41.8<br />
15.8<br />
2.3<br />
27.7<br />
70.0<br />
Number of households 1007 198 809<br />
Majority (94 percent) of the households have access to tap water for drinking, only two<br />
percent each received water through h<strong>and</strong> pump or from wells. About 96 percent of the<br />
households in urban <strong>and</strong> 83 percent in rural areas get piped water for drinking. However,<br />
about 11 percent of the households in rural areas depended on other sources for drinking<br />
water.<br />
Only 65 percent of the households have a flush toilet facility <strong>and</strong> above nine percent are<br />
utilize shared (public <strong>and</strong> own) toilet while about 26 percent of the households have no toilet<br />
facility at all. Household with flush toilet facility is high (77 percent) in the urban areas <strong>and</strong><br />
18 percent of the rural areas had this facility. Majority of the households in the rural areas did<br />
not have toilet facility (81 percent).<br />
Liquid petroleum gas (LPG) is the most commonly used fuel for cooking as more than<br />
three-fifths of the households depend on it while 27 percent of the households use wood <strong>and</strong><br />
nine percent rely on kerosene, as expected use of wood is high in rural areas (85 percent).<br />
1.9<br />
98.1<br />
96.3<br />
1.0<br />
2.7<br />
0.0<br />
76.7<br />
10.2<br />
1.0<br />
12.0<br />
76.6<br />
10.1<br />
13.2<br />
0.2<br />
0.7<br />
14.6<br />
84.7<br />
97.3<br />
44.3<br />
18.2<br />
81.5<br />
31.3<br />
59.3<br />
39.5<br />
4.9<br />
0.0
About six percent of the households live in kachcha <strong>and</strong> 21 percent in semi- pucca<br />
houses <strong>and</strong> 73 percent reside in pucca houses. As expected, a majority of the urban<br />
households (85 percent) are living in pucca houses compared to the rural households (24<br />
percent).<br />
In addition to the above amenities information on possession of some durable goods is<br />
also collected from surveyed households. Analysis of the same shows that about 95 percent<br />
of the households reported owning a fan, while 74 percent reported owning of Television.<br />
Another 56 percent reported owning bicycle. And 39 percent of them reported owning<br />
Radio/transistor, 35 percent motorcycle. About 28 percent reported that they own telephone.<br />
The other durable goods found are sewing machine (16 percent). Ownership of all these<br />
items is more among the urban households than among the rural households.<br />
Taking all these indicators into consideration, SLI was computed. As per the analysis<br />
around three-fifths of the households (59 percent) have high st<strong>and</strong>ard of living, 31 percent<br />
have a medium level of st<strong>and</strong>ard of living <strong>and</strong> only 10 percent of the households have low<br />
st<strong>and</strong>ard of living. The percent of households with medium or higher-level of st<strong>and</strong>ard of<br />
living is more in urban areas (98 percent) compared to the rural areas (58 percent).<br />
2.4 MARITAL STATUS OF HOUSEHOLD POPULATION<br />
The DLHS-RCH, collected information on marital status of all household members above 10<br />
years of age. Table 2.4 shows the percent distribution of household population by marital<br />
status classified by age <strong>and</strong> sex. Among females aged 10-14; about four percent are currently<br />
married. The proportion of never married reached lowest among men by the time they reach<br />
the age 30, while in the case of women the never married reached lowest by the time they<br />
reach the age 25. The proportions divorced, separated, or deserted are small, <strong>and</strong> widowhood<br />
is quite limited until the older ages. More women were widowed by the age 45 <strong>and</strong> above<br />
compared with males.<br />
Table 2.4 MARITAL STATUS OF THE HOUSEHOLD POPULATION<br />
Percentage distribution of the household population age 10 <strong>and</strong> above by marital status, according to age group <strong>and</strong> sex in<br />
Ahmedabad district of Gujarat, RCH,2002<br />
Age Group<br />
Marital Status<br />
Male<br />
Female<br />
Never Currently Widower/ Total Number Never Currently Widow/ Total Number<br />
married married Divorced/ percent of married married Divorced/ percent of<br />
Separated<br />
males<br />
Separated females<br />
10-14 99.6 0.4 0.0 100.0 252 96.2 3.8 0.0 100.0 227<br />
15-19 90.9 9.1 0.0 100.0 272 87.8 12.2 0.0 100.0 325<br />
20-24 68.3 31.6 0.2 100.0 301 16.1 79.3 4.6 100.0 254<br />
25-29 20.7 78.8 0.4 100.0 226 2.9 94.3 2.8 100.0 197<br />
30-44<br />
3.6 92.3 4.0 100.0 476 0.8 96.4 2.8 100.0 469<br />
45-59<br />
0.2 95.1 4.6 100.0 356 0.2 88.5 11.3 100.0 278<br />
60+<br />
0.8 84.2 15.0 100.0 157 0.0 38.5 61.5 100.0 188<br />
Total 37.7 59.3 3.0 100.0 2041 28.6 62.2 9.2 100.0 1937<br />
Table is based on the 'de facto'population<br />
22
2.5 MARRIAGES AND MORBIDITY<br />
Table 2.5 presents data on marriages, <strong>and</strong> morbidity in the households surveyed. In total 149<br />
boys <strong>and</strong> 125 girls were married in the district Ahmedabad during the period 1 st January 1999<br />
till the date of the survey. The mean ages at marriage for boys in district Ahmedabad is found<br />
to be 21 years <strong>and</strong> for girls it is less than 18 years. The mean ages at marriage for boys <strong>and</strong><br />
girls married since 1 st January 1999 in rural areas were 25 <strong>and</strong> 13 years respectively <strong>and</strong> the<br />
comparative figures for urban areas are 20 <strong>and</strong> 19 years.<br />
Practice of early marriage is more prominent in rural areas as higher percent of boys (56<br />
percent) <strong>and</strong> (41 percent) girls were married below the legal age at marriage. Compared to<br />
this such practice is less prominent in the urban areas.<br />
The prevalence rate of blindness, tuberculosis <strong>and</strong> malaria, as reported in the surveyed<br />
households are 255, 85 <strong>and</strong> 506 per 100,000 population respectively in the district. The<br />
prevalence rate of complete blindness per 100,000 population is 258 among males <strong>and</strong> 251<br />
among females. The extent of partial blindness, however, is reported to be much higher (3146<br />
per 100,000 population) as compared to complete blindness (255 per 100,000 population).<br />
Similarly prevalence rate of tuberculosis among males <strong>and</strong> females is 99 <strong>and</strong> 71 per 100,000<br />
population respectively. The prevalence rate of malaria is 296 among males <strong>and</strong> 726 among<br />
females per 100,000 population. This clearly illustrates that the prevalence of the two<br />
morbidities (blindness <strong>and</strong> malaria) is higher among females than males. The prevalence rate<br />
of each of the morbidity blindness, tuberculosis <strong>and</strong> malaria was reported to be much higher<br />
in the rural as compared to urban areas of this district.<br />
Table 2.5 MARRIAGE AND MORBIDITY RATES<br />
Number of marriages, mean age at marriage <strong>and</strong> prevalence of blindness, tuberculosis <strong>and</strong> malaria, according to<br />
residence, Ahmedabad district of Gujarat, RCH, 2002<br />
Characteristic<br />
Total<br />
Residence<br />
Rural<br />
Number of marriages reported since 1 st January 1999<br />
Boys<br />
Girls<br />
Mean age at marriage<br />
Boys<br />
Girls<br />
Percentage of marriages below legal age at marriage<br />
Boys<br />
Girls<br />
Morbidity<br />
Prevalence** rate of blindness<br />
Male<br />
Complete<br />
Partial<br />
Female<br />
Complete<br />
Partial<br />
Person<br />
Complete<br />
Partial<br />
Prevalence** rate of tuberculosis (2002)<br />
Male<br />
Female<br />
Person<br />
Prevalence ** rate of malaria for last two week<br />
Male<br />
Female<br />
Person<br />
23<br />
149<br />
125<br />
20.9<br />
17.5<br />
28.8<br />
32.5<br />
258<br />
2048<br />
251<br />
4298<br />
255<br />
3146<br />
99<br />
71<br />
85<br />
22<br />
38<br />
24.7<br />
13.3<br />
55.6<br />
41.1<br />
450<br />
3791<br />
158<br />
6283<br />
306<br />
5015<br />
467<br />
229<br />
350<br />
Urban<br />
296<br />
726<br />
506<br />
1273<br />
539<br />
912<br />
57<br />
773<br />
405<br />
Total population 5068 1005 4063<br />
** Prevalence rate per 100,000 population<br />
Note: All the rates refer to 'de jure’ population<br />
2.6 MORTALITY<br />
127<br />
87<br />
20.3<br />
19.4<br />
24.1<br />
28.6<br />
211<br />
1621<br />
274<br />
3803<br />
242<br />
2684<br />
9<br />
32<br />
20
Table 2.6 presents data on various mortality measures per 1000 population of the de jure<br />
population three year prior to survey in the district of Ahmedabad in Gujarat. The crude death<br />
rate is found to be 5. The neo-natal mortality <strong>and</strong> post neo-natal mortality rates are 40 <strong>and</strong> 8<br />
per 1000 births respectively. The infant mortality rate was estimated to be 48, per 1000 live<br />
births <strong>and</strong> the under five-mortality rate is 53 in Ahmedabad district.<br />
Table 2.6 VITAL RATES<br />
Crude death rate, neonatal, postneonatal, infant, child <strong>and</strong> under-five mortality rates, Ahmedabad district of Gujarat,<br />
RCH, 2002<br />
Crude death rate<br />
Neonatal mortality rate<br />
Post neonatal mortality rate<br />
Infant mortality rate<br />
Child mortality rate<br />
Under-five mortality rate<br />
* Refers to per 1000 population Note: All the rates refer to ‘de jure’ population.<br />
4.94<br />
39.76<br />
7.87<br />
47.63<br />
5.19<br />
52.83<br />
24
CHAPTER – 3<br />
CHARACTERISTICS OF THE WOMEN AND FERTILITY<br />
In this chapter a brief background <strong>and</strong> fertility profile of the currently married women (age<br />
15-44 years) interviewed for the survey is presented. The cohort fertility of the district as<br />
measured by the number of children ever born to the women age 15-44 years <strong>and</strong> the<br />
completed fertility as measured by the number of children ever born to the women age 40-44<br />
years is presented. The children ever born <strong>and</strong> the children surviving by sex <strong>and</strong> age per<br />
woman are also presented by some selected characteristics of woman. The coverage of the<br />
chapter also includes distribution of total pregnancies of the currently married women by type<br />
of outcome, in addition to fertility indicators in terms of age specific fertility rates, crude birth<br />
rate <strong>and</strong> total fertility rate.<br />
3.1 CHARACTERISTICS OF THE CURRENTLY MARRIED WOMEN<br />
The basic characteristics of the currently married women age 15-44 years are presented in<br />
Table 3.1. The currently married women interviewed are young, as almost half (48<br />
percent) of them interviewed were in the age group 15-29 years <strong>and</strong> the remaining women<br />
were aged 30 years <strong>and</strong> above. For a majority (67 percent) of the currently married<br />
women, marriages were consummated after age 18 years i.e. above the legal age at<br />
marriage. This figure is 42 percent in rural areas <strong>and</strong> it is 73 percent in urban areas. The<br />
early consummation of marriage is high in the rural areas.<br />
About 92 percent of the currently married women are Hindus, five percent are Jain<br />
<strong>and</strong> four percent are Muslims. Three-fifths of the women belong to scheduled caste (SC),<br />
scheduled tribe (ST) or other backward classes. Educational status of the women shows<br />
that thirty-three percent are illiterate <strong>and</strong> slightly more than one-third (35 percent) have<br />
completed 10 or more years of schooling. Compared to the respondents the educational<br />
status of their spouse is better as only 11 percent of them are illiterate <strong>and</strong> 54 percent have<br />
completed 10 or more years of schooling. The educational status in urban areas is much<br />
better in terms of literacy. About 42 percent of the women respondents <strong>and</strong> 61 percent of<br />
their spouses in urban areas had completed 10 or more years of schooling; the corresponding<br />
figures in rural areas is only four <strong>and</strong> 25 percent respectively. With regard to the st<strong>and</strong>ard of<br />
living, about nine percent of the women belong to low level (42 percent in rural <strong>and</strong> one<br />
percent in urban areas), 34 percent have medium level <strong>and</strong> 57 percent have high st<strong>and</strong>ard of<br />
living. Those having medium or higher level of st<strong>and</strong>ard of living are more in urban areas<br />
compared to the rural areas.<br />
25
Table 3.1 BACKGROUND CHARACTERISTICS OF ELIGIBLE WOMEN<br />
Percentage distribution of currently married women age 15-44 by selected background characteristic, according to<br />
residence, Ahmedabad district of Gujarat, RCH, 2002<br />
Background characteristic<br />
Total<br />
Residence<br />
Rural<br />
Age Group (Years)<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
Age at consummation of marriage<br />
Below 18 years<br />
18 years & above<br />
Religion<br />
Hindu<br />
Muslim<br />
Jain<br />
Caste<br />
Scheduled caste<br />
Scheduled tribe<br />
Other backward class<br />
Other#<br />
Don’t know<br />
Education (Years of schooling)<br />
Illiterate<br />
0-9@ years<br />
10 years & above<br />
Husb<strong>and</strong>’s education (Years of schooling)<br />
Illiterate<br />
0-9 @ years<br />
10 years <strong>and</strong> above<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
Availability of health facility in the village<br />
No<br />
Yes<br />
4.8<br />
17.6<br />
25.7<br />
17.2<br />
16.5<br />
18.2<br />
32.9<br />
67.1<br />
91.5<br />
3.8<br />
4.7<br />
11.9<br />
3.0<br />
44.7<br />
40.3<br />
0.1<br />
32.9<br />
32.4<br />
34.6<br />
7.8<br />
19.1<br />
24.5<br />
19.7<br />
17.8<br />
11.1<br />
57.9<br />
42.1<br />
91.5<br />
8.5<br />
0.0<br />
20.2<br />
0.0<br />
50.0<br />
29.8<br />
0.0<br />
60.9<br />
34.9<br />
4.2<br />
Urban<br />
Number of women 769 149 620<br />
# Higher caste (not belonging to scheduled caste, scheduled tribe, or other backward class)<br />
@ Literate women with no years of schooling are also included NA: Not applicable<br />
10.7<br />
34.9<br />
54.3<br />
9.2<br />
33.7<br />
57.1<br />
NA<br />
NA<br />
25.9<br />
49.4<br />
24.7<br />
42.3<br />
41.7<br />
16.0<br />
55.0<br />
45.0<br />
4.1<br />
17.3<br />
26.0<br />
16.6<br />
16.2<br />
19.8<br />
26.9<br />
73.1<br />
91.5<br />
2.7<br />
5.7<br />
9.9<br />
3.7<br />
43.4<br />
42.8<br />
0.1<br />
26.2<br />
31.8<br />
41.9<br />
7.1<br />
31.4<br />
61.4<br />
1.2<br />
31.8<br />
67.0<br />
NA<br />
NA<br />
3.2 CURRENT FERTILITY<br />
In the present phase of the DLHS-RCH survey currently married women in the age group of<br />
15-44 years were asked about the live births they had during the three-year period preceding<br />
the survey, along with the corresponding age of women at the time of delivery. On the basis<br />
of this information, average annual births experienced by women in the conventional five<br />
year age groups during the aforesaid period, that is age specific fertility rates are computed<br />
taking into account the age distribution of all women in the reproductive age group of 15-44<br />
years <strong>and</strong> person-years lived during the period preceding the survey since 1 st January 1999.<br />
The age specific fertility rates are subsequently utilized for the estimation of total fertility rate<br />
(TFR) <strong>and</strong> crude birth rate (CBR). These indicators of current fertility rate are shown in the<br />
Table 3.2. It may be observed that average annual births per woman attain peak in the mid<br />
twenties thereafter it declines with increasing age of women. The average number of children<br />
that a woman had, on an average, in the reproductive life time as depicted by TFR st<strong>and</strong>s at<br />
2.1 The average annual births per thous<strong>and</strong> population during the three years period<br />
preceding the survey in the form of CBR is 23 in Ahmedabad district. TFR of 2.1 in<br />
Ahmedabad district illustrates that this district probably has reached the replacement level of<br />
fertility.<br />
26
Table 3.2 CURRENT FERTILITY<br />
Age-specific fertility rates <strong>and</strong> total fertility rates, <strong>and</strong> crude birth rate, during the three years period preceding the survey,<br />
Ahmedabad district of Gujarat, RCH, 1999-2002.<br />
Age Group<br />
Age specific fertility rate<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
0.038<br />
0.160<br />
0.163<br />
0.036<br />
0.014<br />
0.004<br />
TFR (15-44) 2.08<br />
CBR 23.33<br />
Rates refer to period from 1.1.1999 to the date of survey<br />
3.3 CHILDREN EVER BORN AND LIVING<br />
Table 3.3 presents data on children ever born <strong>and</strong> surviving by selected characteristics of<br />
the currently married women. The mean number of children ever born is 2.7 per currently<br />
married woman <strong>and</strong> the mean number of children surviving is 2.5. The corresponding<br />
figures for children ever born in the rural <strong>and</strong> urban areas were 3.2 <strong>and</strong> 2.6 respectively.<br />
The mean number of children surviving in the rural <strong>and</strong> urban areas of this district were<br />
2.0 <strong>and</strong> 2.4 respectively. The completed fertility i.e. the mean number of children ever<br />
born to women of age 40-44 years is 3.3 in the district.<br />
Table 3.3 FERTILITY<br />
Mean number of children ever born (CEB) <strong>and</strong> children surviving (CS) by selected background characteristics of currently<br />
married women* age 15-44, Ahmedabad district of Gujarat, RCH, 2002<br />
Background characteristic<br />
Age group<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
Duration of marriage<br />
0-4<br />
5-9<br />
10-14<br />
15+<br />
Residence<br />
Rural<br />
Urban<br />
Religion<br />
Hindu<br />
Muslim<br />
Jain<br />
Casteβ<br />
Scheduled castes<br />
Scheduled tribes<br />
Other backward communities<br />
Other<br />
Education<br />
Illiterate<br />
0-9 @ years<br />
10 years <strong>and</strong> above<br />
St<strong>and</strong>ard of living Index<br />
Low<br />
Medium<br />
High<br />
Mean children<br />
ever born<br />
Mean children surviving<br />
Male Female Total Male Female Total<br />
0.27<br />
0.85<br />
1.07<br />
1.36<br />
1.61<br />
1.79<br />
0.39<br />
1.12<br />
1.29<br />
1.85<br />
1.54<br />
1.28<br />
1.34<br />
1.46<br />
0.91<br />
1.37<br />
1.27<br />
1.49<br />
1.13<br />
1.71<br />
1.26<br />
0.98<br />
0.93<br />
1.00<br />
1.01<br />
1.48<br />
1.92<br />
1.49<br />
0.95<br />
0.83<br />
1.45<br />
1.79<br />
1.67<br />
1.29<br />
1.39<br />
1.48<br />
0.85<br />
2.08<br />
1.78<br />
1.40<br />
1.08<br />
1.89<br />
1.22<br />
0.95<br />
1.21<br />
1.85<br />
2.09<br />
2.85<br />
3.54<br />
3.29<br />
1.35<br />
1.96<br />
2.74<br />
3.65<br />
3.21<br />
2.58<br />
2.73<br />
2.94<br />
1.76<br />
3.46<br />
3.05<br />
2.90<br />
2.22<br />
3.61<br />
2.48<br />
1.94<br />
0.05<br />
0.83<br />
1.00<br />
1.17<br />
1.48<br />
1.56<br />
0.37<br />
1.10<br />
1.20<br />
1.59<br />
1.33<br />
1.16<br />
1.20<br />
1.34<br />
0.91<br />
1.30<br />
0.66<br />
1.30<br />
1.07<br />
1.49<br />
1.13<br />
0.94<br />
0.72<br />
0.88<br />
0.99<br />
1.39<br />
1.84<br />
1.34<br />
0.93<br />
0.74<br />
1.36<br />
1.66<br />
1.48<br />
1.23<br />
1.29<br />
1.39<br />
0.81<br />
2.05<br />
1.78<br />
1.28<br />
0.99<br />
1.74<br />
1.13<br />
0.91<br />
0.77<br />
1.71<br />
1.99<br />
2.56<br />
3.32<br />
2.91<br />
1.30<br />
1.84<br />
2.56<br />
3.26<br />
2.82<br />
2.39<br />
2.50<br />
2.73<br />
1.73<br />
3.35<br />
2.45<br />
2.59<br />
2.07<br />
3.23<br />
2.26<br />
1.86<br />
Number of<br />
women<br />
1.70<br />
1.48<br />
1.18<br />
1.84<br />
1.61<br />
1.15<br />
3.55<br />
3.09<br />
2.33<br />
1.44<br />
1.35<br />
1.06<br />
1.67<br />
1.49<br />
1.09<br />
3.11<br />
2.85<br />
2.16<br />
65<br />
217<br />
384<br />
All women 1.33 1.37 2.70 1.19 1.27 2.47 667<br />
β The total figure may not add to (N) <strong>and</strong> percentage may not add up to 100.0 due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included<br />
* Women who have/had given live birth<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
(11)<br />
106<br />
160<br />
129<br />
125<br />
136<br />
111<br />
143<br />
145<br />
268<br />
132<br />
535<br />
612<br />
27<br />
28<br />
82<br />
(16)<br />
305<br />
263<br />
238<br />
206<br />
223<br />
27
The mean number of children ever born is 2.7 for Hindus, 1.8 for Jain <strong>and</strong> 2.9 for<br />
Muslims. The mean number of children ever born is 3.5 for SCs <strong>and</strong> 3.1 for STs <strong>and</strong> it is 2.9<br />
for other backward classes. It may be mentioned here that the mean values are not<br />
st<strong>and</strong>ardised <strong>and</strong> therefore, the comparisons made here have this limitation. The mean<br />
number of children ever born has declined with the increase in the level of education of the<br />
currently married women. An illiterate woman in the reproductive ages, on an average, bears<br />
3.6 children compared to 1.9 children borne by those with at least 10 years of schooling. The<br />
mean number of children ever born has also declined with the increase in the st<strong>and</strong>ard of<br />
living of the household.<br />
3.4 OUTCOME OF PREGNANCY<br />
Keeping in view the implication of socio-economic, health care <strong>and</strong> nutritional status of<br />
currently married women on pregnancy outcome. Table 3.4 presents the distribution of total<br />
pregnancies of the eligible women by type of outcome. The outcome of pregnancy are live<br />
births, stillbirths, spontaneous abortion <strong>and</strong> induced abortion. There were 2010 reported<br />
pregnancies. About 90 percent of these ended as live births. The percentages of pregnancies<br />
that ended in spontaneous <strong>and</strong> induced abortions were five each, while the rest resulted in<br />
stillbirths. The incidence of pregnancy wastage in the absence of external intervention is<br />
more among women in the age group of 20-29 <strong>and</strong> 35-39. But the external intervention is<br />
concentrated among women in 25-29 <strong>and</strong> 40-44 age group.<br />
Table 3.4 OUTCOME OF PREGNANCY<br />
Percentage distribution of total pregnancies of currently married women age 15-44, Ahmedabad district of Gujarat,<br />
RCH, 2002<br />
Age group<br />
Type of outcome<br />
Number of<br />
Live birth Still birth Spontaneous<br />
abortion<br />
Induced<br />
abortion<br />
Total Pregnancies<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
98.0<br />
85.3<br />
87.2<br />
91.6<br />
90.2<br />
91.6<br />
0.0<br />
0.2<br />
1.5<br />
1.6<br />
0.5<br />
0.2<br />
28<br />
2.0<br />
9.9<br />
5.3<br />
2.2<br />
6.7<br />
1.1<br />
0.0<br />
4.6<br />
6.0<br />
4.6<br />
2.6<br />
7.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
All women 89.7 0.8 4.5 5.0 100.0 2010<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
3.5 BIRTH ORDER<br />
The study of distribution of births by birth order is necessary to underst<strong>and</strong> the<br />
fertility. Table 3.5 shows the distribution of the births during the three years period<br />
before the survey by birth order <strong>and</strong> age group of women.<br />
Table 3.5 BIRTH ORDER<br />
Percentage distribution of births during three years preceding the survey by birth order, according to women 15-44 age,<br />
Ahmedabad district of Gujarat, RCH, 2002<br />
Age group 1 2 3 4+ Total Number<br />
of births<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
76.6<br />
44.6<br />
58.4<br />
48.8<br />
30.4<br />
43.5<br />
23.4<br />
39.3<br />
10.9<br />
6.7<br />
31.9<br />
12.6<br />
0.0<br />
14.6<br />
26.8<br />
24.3<br />
0.0<br />
3.8<br />
0.0<br />
1.5<br />
3.9<br />
20.2<br />
37.7<br />
40.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
All women 51.9 18.4 21.0 8.7 100.0 624<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
Table 3.5 reveals that 52 percent of all births are first order birth, 18 percent are<br />
second order births, 21 percent are third order births <strong>and</strong> nine percent are births of order<br />
four or higher. Further, age-specific birth order shows that, first order births are higher<br />
among women in the younger age group of 15-29 years of age. Higher order birth of four<br />
or more was high among older women above 40 years of age.<br />
(13)<br />
230<br />
384<br />
402<br />
491<br />
490<br />
(16)<br />
155<br />
286<br />
130<br />
30<br />
(7)
CHAPTER - 4<br />
UTILIZATION OF MATERNAL HEALTH SERVICES<br />
An important objective of the District Level Household Survey (DLHS) is to provide<br />
information on maternal <strong>and</strong> child health care practices. This chapter presents information<br />
on antenatal, natal <strong>and</strong> postnatal care received by CMW (from 1 st January 1999 till the<br />
date of the survey). `<br />
4.1 ANTENATAL CHECK-UPS BY SERVICE PROVIDER<br />
Table 4.1(A), presents data<br />
on ANC coverage <strong>and</strong><br />
service providers by<br />
selected background<br />
characteristics of the CMW.<br />
In the district of<br />
Ahmedabad, around 92<br />
percent of pregnant women<br />
had received any ANC<br />
service. Doctors are the<br />
main ANC service<br />
providers followed by<br />
ANM. About 68 percent of<br />
the women availed the<br />
services from doctor<br />
followed by ANM,<br />
Nurse/LHV (20 percent). It<br />
Sources<br />
ANM at home<br />
ANM/Nurse/LHV<br />
DLHS-RCH, 2002<br />
Any ANC<br />
may be mentioned that only six percent of the women received ANC services at home<br />
(Figure 4.1).<br />
Almost all the women in the three-age cohorts had availed the ANC services. This<br />
indicates that the services are reaching the target population in this district. Younger<br />
women below 20 years of age received the services from ANM (71 percent) while those<br />
above 20 years received ANC services from doctor. The proportion of women who<br />
reported having availed at least one antenatal care service decreased with the increase in<br />
the number of children. The proportion of women having received any ANC services was<br />
82 percent in the rural areas <strong>and</strong> 95 percent in the urban areas. Relatively higher<br />
proportion of women belonging to other caste (96 percent), as compared to scheduled<br />
caste (SC)/scheduled tribe (ST) women (74 percent) reported to have received any ANC<br />
services.<br />
The proportion of pregnant women who had received at least one antenatal care<br />
services steadily increased with the number of years of schooling. Among the illiterate<br />
women, 80 percent had received any ANC services, whereas cent percent of the women,<br />
with 10 or more years of schooling, reported to have received such services.<br />
29<br />
Figure: 4.1<br />
Sources of antenatal care<br />
Doctor<br />
6.3<br />
19.8<br />
67.5<br />
91.8<br />
0 20 40 60 80 100<br />
Percent
Similarly, less percent of women belonging to low st<strong>and</strong>ard of living (87 percent) had<br />
received ANC services, whereas this was 100 percent for women belonging to high<br />
st<strong>and</strong>ard of living. It is observed that utilization of ANC services is comparatively less in<br />
villages having health facility (78 percent) than in the villages without health facility (84<br />
percent). More specifically, health facilities where doctors are available are better utilized<br />
than those having ANM or nurse.<br />
>>>><br />
Table 4.1 (A) ANTENATAL CHECK-UP<br />
Percentage of women* who received any antenatal check-ups (ANC) during pregnancy by health personnel, according to<br />
selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Background characteristics<br />
Any ANC <strong>Health</strong> personnel<br />
providing ANC<br />
Number of<br />
Women<br />
Age group<br />
Less than 20 years<br />
20-34 years<br />
35 years & above<br />
Children ever born<br />
1<br />
2<br />
3<br />
4+<br />
Residence<br />
Rural<br />
Urban<br />
Religion<br />
Hindu<br />
Muslim<br />
Other<br />
Caste#<br />
SC/ST<br />
Other<br />
Education<br />
Illiterate<br />
0-9@ years<br />
10 years <strong>and</strong> above<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
Availability of health facility in village<br />
No<br />
Yes<br />
30<br />
100.0<br />
91.4<br />
92.9<br />
100.0<br />
86.2<br />
90.2<br />
86.7<br />
82.1<br />
94.6<br />
91.9<br />
85.8<br />
100.0<br />
73.8<br />
95.3<br />
79.5<br />
95.7<br />
100.0<br />
86.6<br />
84.3<br />
99.9<br />
Only at<br />
home by<br />
ANM<br />
0.0<br />
6.4<br />
9.0<br />
1.2<br />
3.6<br />
14.2<br />
13.7<br />
24.5<br />
1.2<br />
6.4<br />
0.0<br />
11.8<br />
8.4<br />
5.9<br />
12.5<br />
5.2<br />
1.3<br />
30.1<br />
5.5<br />
0.0<br />
Doctor<br />
29.4<br />
68.8<br />
75.3<br />
80.5<br />
68.4<br />
46.7<br />
61.2<br />
40.1<br />
75.3<br />
66.5<br />
85.8<br />
88.2<br />
53.2<br />
70.3<br />
45.9<br />
67.1<br />
89.2<br />
25.5<br />
54.7<br />
91.1<br />
ANM<br />
Nurse/<br />
LHV<br />
84.3<br />
78.2<br />
37.6<br />
1.8<br />
31.0<br />
55.8<br />
15.7<br />
26.6<br />
37<br />
(21)<br />
All Women 91.8 6.3 67.5 19.8 261<br />
# The total figure may not add to (N) <strong>and</strong> percentage may not add upto 100.0 due to multiple responses<br />
@ Literate women with no years of schooling are also included<br />
* Women who had their last live/still birth since 1-1-1999<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
4.2 ANTENATAL CHECK-UPS AT HEALTH FACILITY<br />
Table 4.1(B) presents data on ANC coverage <strong>and</strong> ANC services by different categories of<br />
health facilities by selected background characteristics of the CMW. Concerning the<br />
source of ANC service, the data shows that women preferred private source to avail the<br />
ANC services to Government. About 66 percent of the women had approached private<br />
health facility, 30 percent went to government health facility including PHC <strong>and</strong> SC <strong>and</strong><br />
only six percent of them had received the services at their doorstep provided by ANM. A<br />
very negligible percent of women approached ISM facilities (both government as well as<br />
private).<br />
Utilization of ANC services by place of residence shows that private health facilities<br />
were more preferred by women in urban (75 percent) than rural areas (35 percent). The<br />
proportion of women who had received ANC services through private health facility<br />
increased with the increase in education, from 42 percent of illiterate women to as high as<br />
70.6<br />
18.1<br />
8.7<br />
19.6<br />
17.1<br />
30.2<br />
13.2<br />
19.7<br />
19.8<br />
20.7<br />
5.2<br />
0.0<br />
13.9<br />
20.9<br />
23.3<br />
25.6<br />
10.3<br />
34.1<br />
25.5<br />
10.6<br />
(10)<br />
238<br />
(13)<br />
99<br />
70<br />
48<br />
43<br />
58<br />
203<br />
247<br />
(9)<br />
(5)<br />
42<br />
219<br />
85<br />
89<br />
87<br />
36<br />
105<br />
120
96 percent for those women who had 10 or more years of schooling. A relatively large<br />
proportion of the other caste group (71 percent) received ANC services from private<br />
sources as compared to the SC/ST (43 percent) women. The proportion of women who<br />
received ANC from private sources was directly related to their st<strong>and</strong>ard of living. The<br />
proportion of women who had received ANC services through government facility<br />
considerably increased with the availability of government health facilities of any type in<br />
the village.<br />
Table 4.1(B) ANTENATAL CHECK-UP<br />
Percentage of women* who received any antenatal check-ups (ANC) during pregnancy by source, according to selected<br />
background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Background characteristics<br />
Age group<br />
Less than 20 years<br />
20-34 years<br />
35 years & above<br />
Children ever born<br />
1<br />
2<br />
3<br />
4+<br />
Residence<br />
Rural<br />
Urban<br />
Religion<br />
Hindu<br />
Muslim<br />
Other<br />
Caste#<br />
SC/ST<br />
Other<br />
Education<br />
Illiterate<br />
0-9@ years<br />
10 years <strong>and</strong> above<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
Availability of health facility in village<br />
No<br />
Yes<br />
Home<br />
0.0<br />
6.4<br />
9.0<br />
1.2<br />
3.6<br />
14.2<br />
13.7<br />
24.5<br />
1.2<br />
6.4<br />
0.0<br />
11.8<br />
8.4<br />
5.9<br />
12.5<br />
5.2<br />
1.3<br />
30.1<br />
5.5<br />
0.0<br />
Govt.<br />
health<br />
facility<br />
73.1<br />
19.1<br />
1.8<br />
24.4<br />
17.2<br />
30.6<br />
5.5<br />
13.4<br />
22.3<br />
21.3<br />
4.4<br />
0.0<br />
19.5<br />
20.5<br />
20.1<br />
39.2<br />
1.3<br />
19.4<br />
26.5<br />
15.3<br />
Place of ANC¢<br />
Private<br />
health<br />
facility<br />
26.9<br />
67.8<br />
73.5<br />
84.3<br />
63.4<br />
43.3<br />
57.9<br />
34.6<br />
75.4<br />
65.6<br />
76.2<br />
88.2<br />
43.1<br />
71.0<br />
41.8<br />
60.8<br />
96.2<br />
20.2<br />
53.3<br />
91.5<br />
PHC$<br />
70.6<br />
6.3<br />
0.0<br />
9.8<br />
0.8<br />
21.8<br />
4.0<br />
8.5<br />
8.6<br />
9.0<br />
0.0<br />
0.0<br />
7.0<br />
8.9<br />
14.3<br />
11.4<br />
0.0<br />
6.6<br />
16.3<br />
2.4<br />
SC^<br />
3.0<br />
0.8<br />
0.0<br />
1.1<br />
1.1<br />
0.0<br />
0.9<br />
3.9<br />
0.0<br />
0.9<br />
0.0<br />
0.0<br />
0.7<br />
0.9<br />
2.2<br />
0.4<br />
0.0<br />
4.0<br />
0.8<br />
0.0<br />
ISM facility<br />
Govt. Private<br />
0.0<br />
0.1<br />
0.0<br />
0.0<br />
0.2<br />
0.0<br />
0.0<br />
0.0<br />
0.1<br />
0.1<br />
0.0<br />
0.0<br />
0.0<br />
0.1<br />
0.0<br />
0.2<br />
0.0<br />
0.4<br />
0.0<br />
0.0<br />
0.0<br />
0.6<br />
0.0<br />
0.5<br />
1.4<br />
0.0<br />
0.0<br />
0.0<br />
0.8<br />
0.6<br />
0.0<br />
0.0<br />
0.0<br />
0.7<br />
0.0<br />
0.3<br />
1.4<br />
0.0<br />
0.0<br />
1.3<br />
Number<br />
of<br />
Women<br />
37.6<br />
1.8<br />
6.1<br />
26.1<br />
24.9<br />
51.4<br />
6.1<br />
12.7<br />
0.0<br />
10.6<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
37<br />
(21)<br />
All Women 6.3 20.4 66.4 8.6 0.9 0.1 0.6 261<br />
¢ Other health facility is not included in the analysis,<br />
# The total figure may not add to (N) <strong>and</strong> percentage may not add upto 100.0 due to multiple responses<br />
$ Primary health center ^ Sub-center<br />
@ Literate women with no years of schooling are also included<br />
* Women who had their last live/still birth since 1-1-1999<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
4.3 ANTENATAL CARE<br />
Antenatal care refers to care provided to the mother during pregnancy by a doctor or<br />
health worker at a medical facility or at home. To assess whether the women had received<br />
all the cares <strong>and</strong> services during pregnancy, information was collected regarding the<br />
number of home visits by ANM, timing of the first visit <strong>and</strong> type of services received.<br />
Information collected has been presented in the Table 4.2(A), <strong>and</strong> Table 4.2(B), by<br />
selected background characteristics of the women. The number of antenatal visits <strong>and</strong><br />
timing of first ANC is important for the health of the mother <strong>and</strong> outcome of pregnancy.<br />
For proper monitoring of the pregnancy, the first check-up is m<strong>and</strong>atory, immediately on<br />
(10)<br />
238<br />
(13)<br />
99<br />
70<br />
48<br />
43<br />
58<br />
203<br />
247<br />
(9)<br />
(5)<br />
42<br />
219<br />
85<br />
89<br />
87<br />
36<br />
105<br />
120<br />
31
confirmation or at least before twenty weeks of gestation. Minimum of three check-ups are<br />
essential.<br />
Table 4.2 (A) ANTENATAL CARE<br />
Percentage of women* by type of antenatal care <strong>and</strong> by some selected background characteristics, Ahmedabad district of<br />
Gujarat, RCH, 2002<br />
Type of antenatal care<br />
Total Residence Caste# Availability of health<br />
facility in the village<br />
Rural Urban SC/ST Other No Yes<br />
Number of ANC visits<br />
No visit<br />
1<br />
2<br />
3<br />
4+<br />
Stage of pregnancy at the time of the<br />
first antenatal check-up<br />
No antenatal check-up<br />
First trimester<br />
Second trimester<br />
Third trimester<br />
Services received<br />
Weight measured<br />
Height measured<br />
Blood pressure checked<br />
Blood tested<br />
Urine tested<br />
Abdomen examined<br />
Internal examination done<br />
Breast examined<br />
X-ray<br />
Sonography/ultrasound<br />
Amniocentesis<br />
Advice received<br />
Diet<br />
Danger signs<br />
Delivery care<br />
Breastfeeding<br />
New born care<br />
<strong>Family</strong> planning<br />
8.2<br />
3.6<br />
10.5<br />
12.7<br />
64.9<br />
8.2<br />
62.6<br />
19.4<br />
9.9<br />
69.8<br />
19.9<br />
70.4<br />
76.8<br />
66.4<br />
78.3<br />
47.9<br />
23.0<br />
9.6<br />
48.2<br />
3.3<br />
88.3<br />
58.5<br />
48.9<br />
26.7<br />
40.8<br />
23.4<br />
76.1<br />
30.2<br />
18.8<br />
15.5<br />
14.2<br />
13.4<br />
91.8<br />
66.5<br />
57.4<br />
29.9<br />
48.3<br />
26.3<br />
64.9<br />
53.9<br />
9.1<br />
6.0<br />
5.2<br />
1.0<br />
92.9<br />
59.4<br />
56.6<br />
30.7<br />
47.7<br />
27.8<br />
84.4<br />
24.8<br />
9.4<br />
12.7<br />
15.7<br />
6.2<br />
61.6<br />
39.7<br />
35.1<br />
20.2<br />
11.8<br />
25.9<br />
Women who received IFA tablets 86.7 73.9 90.3 73.0 89.3 78.2 66.3<br />
Daily dose (consumed)<br />
One IFA tablet<br />
Two or more IFA tablets<br />
Women who consumed IFA tablets<br />
Less than 100 IFA tablets<br />
100+ IFA tablets<br />
Women who received TT<br />
No TT<br />
1<br />
2+<br />
63.2<br />
20.4<br />
53.3<br />
29.1<br />
10.6<br />
5.7<br />
83.7<br />
Full ANC £ 28.3 11.8 33.0 16.6 30.6 9.3 16.1<br />
Number of women 261 58 203 42 219 37 (21)<br />
32<br />
17.9<br />
14.1<br />
27.4<br />
17.5<br />
23.2<br />
17.9<br />
37.2<br />
42.4<br />
2.5<br />
27.4<br />
3.2<br />
26.6<br />
42.4<br />
25.9<br />
51.1<br />
24.9<br />
6.3<br />
3.9<br />
17.7<br />
4.1<br />
44.0<br />
19.9<br />
46.2<br />
14.0<br />
27.8<br />
4.5<br />
67.7<br />
5.4<br />
0.9<br />
5.8<br />
11.4<br />
76.7<br />
5.4<br />
69.8<br />
12.9<br />
11.9<br />
81.8<br />
24.6<br />
82.8<br />
86.5<br />
77.9<br />
86.0<br />
54.5<br />
27.8<br />
11.2<br />
56.9<br />
3.1<br />
68.7<br />
20.5<br />
55.3<br />
33.3<br />
5.7<br />
6.1<br />
88.2<br />
26.2<br />
0.0<br />
7.7<br />
35.0<br />
31.1<br />
26.2<br />
27.2<br />
31.9<br />
14.7<br />
50.2<br />
3.4<br />
52.7<br />
58.0<br />
48.5<br />
63.3<br />
17.8<br />
8.6<br />
0.5<br />
8.2<br />
0.0<br />
56.0<br />
11.7<br />
51.1<br />
16.6<br />
29.2<br />
0.8<br />
70.1<br />
4.7<br />
4.3<br />
11.1<br />
8.4<br />
71.5<br />
4.7<br />
69.4<br />
17.0<br />
8.9<br />
73.6<br />
23.1<br />
73.8<br />
80.4<br />
69.9<br />
81.2<br />
53.8<br />
25.8<br />
11.3<br />
56.0<br />
3.9<br />
64.7<br />
22.0<br />
53.7<br />
31.5<br />
7.0<br />
6.7<br />
86.3<br />
# The total figure may not add to (N) <strong>and</strong> percentage may not add upto 100.0 due to don’t know <strong>and</strong> missing cases<br />
£<br />
At least 3 ANC visits <strong>and</strong> 100+ IFA tablets <strong>and</strong> at least one TT injection<br />
* Women who had their last live/still birth since 1.1.1999<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
About 78 percent of the women had undergone all the three check-ups in Ahmedabad<br />
district of Gujarat during their pregnancy period. This was high among urban women (88<br />
percent) than their rural counterparts (41 percent). Further, education <strong>and</strong> st<strong>and</strong>ard of<br />
living had positive impact on number of women having received or having undergone all<br />
the three check-ups. Timing of the first check-up shows that, 63 percent of the women,<br />
had their first check-up done during their first trimester. Relatively higher proportion of<br />
women in the urban areas (70 percent) as compared to the rural areas (37 percent) reported<br />
first trimester check-up. Further, relatively higher proportion of other caste (higher caste)<br />
groups compared to SC/ST groups had their first check-up done during their first trimester<br />
of pregnancy. Again higher percent of women educated with high st<strong>and</strong>ard of living<br />
respected timely check-up during the first trimester. Interestingly, this practice is more<br />
common in villages with health facility as compared to those villages, which did not have<br />
any health facility.<br />
15.7<br />
15.5<br />
38.0<br />
18.3<br />
12.5<br />
15.7<br />
25.0<br />
56.2<br />
3.1<br />
15.9<br />
3.2<br />
22.0<br />
40.8<br />
21.8<br />
43.2<br />
12.2<br />
3.2<br />
6.1<br />
9.3<br />
3.2<br />
53.2<br />
9.3<br />
50.0<br />
9.3<br />
31.1<br />
6.2<br />
62.7<br />
21.8<br />
11.6<br />
9.0<br />
16.0<br />
41.7<br />
21.8<br />
58.3<br />
18.5<br />
1.5<br />
47.4<br />
3.2<br />
34.7<br />
45.3<br />
33.0<br />
64.9<br />
47.0<br />
11.8<br />
0.0<br />
32.2<br />
5.8<br />
28.1<br />
38.3<br />
39.8<br />
22.2<br />
22.1<br />
1.5<br />
76.4
About the routine check-up during pregnancy, around 70 percent of the women had<br />
their weight monitored <strong>and</strong> about 70 percent of the women also had their blood pressure<br />
measured. About 78 percent women had abdominal check-ups <strong>and</strong> 77 percent had their<br />
blood tested. Women with better education <strong>and</strong> living st<strong>and</strong>ard were more conscious about<br />
such routine check-up.<br />
A pregnant women needs six times more iron than a non-pregnant women <strong>and</strong> about<br />
87 percent of the pregnant women were given iron <strong>and</strong> folic acid tablets <strong>and</strong> among them<br />
84 percent had consumed it daily. Tetanus toxoid injection protects the mother <strong>and</strong> her<br />
baby against tetanus. About 84 percent women had received two doses of TT in this<br />
district.<br />
Overall only 28 percent of the pregnant women had received full ANC care that is one<br />
dose of TT, 100 IFA tablet <strong>and</strong> at least 3 ANC visit during their pregnancy period. This<br />
indicates that for better coverage, health workers have to educate women on the<br />
importance of ANC <strong>and</strong> provide them with the service.<br />
Table 4.2 (B) ANTENATAL CARE<br />
Percentage of women* by type of antenatal care <strong>and</strong> by some selected background characteristics, Ahmedabad district of<br />
Gujarat, RCH, 2002<br />
Type of antenatal care<br />
Education St<strong>and</strong>ard of living index Children Ever Born<br />
Number of ANC visits<br />
No visit<br />
1<br />
2<br />
3<br />
4+<br />
Stage of pregnancy at the time of the<br />
first antenatal check-up<br />
No antenatal check-up<br />
First trimester<br />
Second trimester<br />
Third trimester<br />
Services received<br />
Weight measured<br />
Height measured<br />
Blood pressure checked<br />
Blood tested<br />
Urine tested<br />
Abdomen examined<br />
Internal examination done<br />
Breast examined<br />
X-ray<br />
Sonography/ultrasound<br />
Amniocentesis<br />
Advice received<br />
Diet<br />
Danger sign<br />
Delivery care<br />
Breastfeeding<br />
New born care<br />
<strong>Family</strong> planning<br />
Illiterate<br />
20.5<br />
8.1<br />
16.7<br />
14.9<br />
39.8<br />
20.5<br />
35.4<br />
21.8<br />
22.3<br />
43.4<br />
4.4<br />
43.3<br />
59.2<br />
39.1<br />
55.0<br />
15.5<br />
6.8<br />
7.7<br />
10.8<br />
3.6<br />
0-9@<br />
years<br />
4.3<br />
2.6<br />
8.5<br />
16.3<br />
68.2<br />
4.3<br />
65.9<br />
24.0<br />
5.8<br />
68.3<br />
21.4<br />
70.4<br />
74.9<br />
66.6<br />
80.8<br />
51.6<br />
19.4<br />
11.6<br />
54.3<br />
0.7<br />
10 &<br />
above<br />
0.0<br />
0.3<br />
6.6<br />
7.0<br />
86.1<br />
0.0<br />
85.8<br />
12.4<br />
1.8<br />
97.2<br />
33.5<br />
96.9<br />
96.0<br />
93.1<br />
98.7<br />
76.0<br />
42.7<br />
9.3<br />
78.7<br />
5.7<br />
Low Medium High 1 2 3+<br />
76.7<br />
52.1<br />
16.5<br />
12.8<br />
12.2<br />
10.1<br />
89.7<br />
57.2<br />
58.9<br />
20.3<br />
45.2<br />
32.1<br />
98.4<br />
66.1<br />
70.2<br />
46.8<br />
64.2<br />
27.6<br />
79.5<br />
35.2<br />
25.0<br />
19.2<br />
20.5<br />
11.7<br />
83.9<br />
64.0<br />
30.9<br />
10.0<br />
29.3<br />
20.1<br />
94.8<br />
60.6<br />
71.5<br />
43.4<br />
56.8<br />
29.8<br />
98.7<br />
56.5<br />
73.1<br />
39.1<br />
68.2<br />
25.6<br />
86.0<br />
61.0<br />
35.8<br />
19.1<br />
30.5<br />
23.5<br />
78.9<br />
59.6<br />
33.3<br />
19.4<br />
19.7<br />
21.3<br />
Women who received IFA tablets 76.7 85.6 97.6 82.2 75.3 97.9 91.8 81.8 86.0<br />
Daily dose (consumed)<br />
One IFA tablet<br />
Two IFA tablets or more<br />
Women who consumed IFA tablets<br />
Less than 100 IFA tablets<br />
100+ IFA tablets<br />
Women who received TT<br />
No TT<br />
58.0<br />
13.1<br />
49.8<br />
18.9<br />
23.4<br />
16.7<br />
59.9<br />
55.5<br />
27.0<br />
57.5<br />
25.0<br />
8.4<br />
0.6<br />
91.0<br />
1<br />
2+<br />
Full ANC £ 16.9 25.0 43.0 21.7 16.7 40.4 38.9 28.0 17.5<br />
Number of women 85 89 87 36 105 120 99 70 91<br />
76.3<br />
20.7<br />
52.5<br />
43.2<br />
0.3<br />
0.3<br />
99.5<br />
13.4<br />
13.0<br />
34.3<br />
11.4<br />
27.8<br />
13.4<br />
35.5<br />
46.6<br />
4.5<br />
28.5<br />
2.7<br />
26.9<br />
46.4<br />
21.4<br />
42.5<br />
14.5<br />
5.9<br />
0.0<br />
7.8<br />
0.0<br />
49.0<br />
23.3<br />
44.4<br />
25.3<br />
19.6<br />
7.9<br />
72.5<br />
15.7<br />
4.4<br />
6.6<br />
13.9<br />
59.5<br />
15.7<br />
50.8<br />
16.9<br />
16.7<br />
55.6<br />
10.5<br />
58.2<br />
74.7<br />
63.1<br />
69.4<br />
34.7<br />
7.8<br />
14.7<br />
31.3<br />
2.9<br />
59.5<br />
14.4<br />
56.1<br />
16.7<br />
16.8<br />
10.4<br />
72.8<br />
0.1<br />
0.2<br />
7.0<br />
12.1<br />
80.6<br />
0.1<br />
80.9<br />
13.6<br />
5.5<br />
94.4<br />
33.1<br />
93.9<br />
87.6<br />
82.7<br />
96.7<br />
69.4<br />
41.4<br />
8.0<br />
75.0<br />
4.7<br />
70.7<br />
24.6<br />
53.5<br />
40.9<br />
2.5<br />
1.1<br />
96.4<br />
0.0<br />
1.5<br />
1.4<br />
5.2<br />
92.0<br />
0.0<br />
88.6<br />
11.0<br />
0.4<br />
80.3<br />
28.4<br />
83.2<br />
91.2<br />
89.7<br />
98.7<br />
82.2<br />
38.2<br />
8.1<br />
79.8<br />
4.1<br />
65.5<br />
21.7<br />
46.7<br />
40.2<br />
5.0<br />
0.2<br />
94.8<br />
13.8<br />
3.2<br />
12.1<br />
9.2<br />
61.7<br />
13.8<br />
51.0<br />
22.2<br />
13.0<br />
76.9<br />
16.6<br />
78.7<br />
78.1<br />
70.4<br />
62.5<br />
33.6<br />
11.7<br />
22.3<br />
33.3<br />
3.9<br />
60.5<br />
18.9<br />
48.5<br />
28.4<br />
17.3<br />
1.5<br />
81.2<br />
11.5<br />
6.4<br />
19.4<br />
23.8<br />
38.9<br />
11.5<br />
44.1<br />
26.7<br />
17.7<br />
54.0<br />
13.4<br />
51.1<br />
61.1<br />
39.2<br />
69.5<br />
22.5<br />
15.6<br />
1.6<br />
26.3<br />
2.0<br />
63.8<br />
20.3<br />
64.9<br />
18.0<br />
10.3<br />
15.0<br />
74.6<br />
33
* Women who had their last live/still birth since 1.1.1999<br />
£<br />
At least 3 ANC visits <strong>and</strong> 100+ IFA tablets <strong>and</strong> at least one TT injection<br />
@ Literate women with no years of schooling are also included<br />
The proportion of women who received advice for diet, danger sign, delivery care,<br />
breastfeeding, new born care <strong>and</strong> family planning were found increasing with the increase<br />
in education level <strong>and</strong> st<strong>and</strong>ard of living.<br />
4.4 PREGNANCY COMPLICATIONS AND TREATMENT<br />
Complications during pregnancy may adversely affect both women’s health <strong>and</strong> the<br />
outcome of pregnancy. Early detection of pregnancy complications <strong>and</strong> their management<br />
are important components of the Safe Motherhood Programme. In the survey, the women<br />
were asked if they had faced such problems, <strong>and</strong> their treatment seeking behavior. The<br />
data analyzed is presented in Table 4.3.<br />
Table 4.3 PREGNANCY COMPLICATIONS<br />
Percentage of women* by pregnancy complication <strong>and</strong> type of treatment sought by selected background characteristics,<br />
Ahmedabad district of Gujarat, RCH, 2002<br />
Pregnancy complication <strong>and</strong> type of<br />
treatment<br />
Total<br />
Residence Availability of health<br />
facility in the village<br />
ANC<br />
Rural Urban No Yes No Yes<br />
Women who reported at least one symptom<br />
of pregnancy complication 26.6 20.8 28.3 15.6 29.8 8.1 28.3<br />
Symptoms<br />
Swelling of h<strong>and</strong>s <strong>and</strong> feet<br />
Paleness<br />
Visual disturbances<br />
Excessive bleeding<br />
Convulsion<br />
Abnormal position of foetus<br />
Other<br />
18.0<br />
6.4<br />
6.4<br />
0.3<br />
0.5<br />
1.1<br />
7.9<br />
8.4<br />
10.0<br />
14.4<br />
0.0<br />
2.1<br />
1.6<br />
10.2<br />
Women who sought treatment for pregnancy<br />
complication 57.8 40.5 61.4 0.0 77.2 70.5 57.5<br />
Source of treatment**<br />
Government health facility<br />
PHC<br />
SC<br />
Private health facility<br />
ISM facility<br />
11.4<br />
1.6<br />
0.4<br />
87.7<br />
1.3<br />
31.5<br />
6.4<br />
0.0<br />
68.5<br />
0.0<br />
Number of women 261 58 203 37 (21) (21) 240<br />
* Women who had their last live/still birth since 1-1-1999<br />
** Total percent may add to more than 100.0 due to multiple responses<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
The table reveals that, 27 percent of the women had suffered from at least one<br />
complication during pregnancy. Relatively higher percent of women in the urban area (28<br />
percent) reported at least one symptom of pregnancy complication as compared to the<br />
women in the rural area (21 percent). Further, a higher proportion of women in the rural<br />
area reported any symptom of pregnancy complication especially in those villages with<br />
health facilities (30 percent) compared to those villages, which had no health facility (16<br />
percent). It was observed that among women who availed ANC services the proportion of<br />
women having any symptoms of pregnancy complications was higher (28 percent) as<br />
compared to those who did not utilize the ANC services (8 percent). This implies that<br />
women who seek ANC are probably more aware about pregnancy complications <strong>and</strong> as a<br />
result could recognize <strong>and</strong> report the complication they had experienced.<br />
20.7<br />
5.4<br />
4.2<br />
0.4<br />
0.0<br />
1.0<br />
7.3<br />
8.6<br />
1.0<br />
0.5<br />
90.3<br />
1.5<br />
0.0<br />
3.1<br />
12.4<br />
0.0<br />
0.0<br />
0.0<br />
6.3<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
23.0<br />
22.1<br />
17.7<br />
0.0<br />
5.8<br />
4.4<br />
16.9<br />
31.5<br />
6.4<br />
0.0<br />
68.5<br />
0.0<br />
6.7<br />
8.1<br />
7.2<br />
0.0<br />
5.7<br />
0.0<br />
0.0<br />
100.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
19.0<br />
6.2<br />
6.4<br />
0.4<br />
0.0<br />
1.2<br />
8.6<br />
8.6<br />
1.7<br />
0.4<br />
90.4<br />
1.4<br />
34
The availability of health<br />
services also has a positive impact<br />
on the utilization of ANC service,<br />
which in turn may have resulted<br />
in increased level of awareness<br />
about such complications. The<br />
most frequently reported<br />
complications were swelling on<br />
h<strong>and</strong>s <strong>and</strong> feet (18 percent),<br />
followed by visual disturbances (6<br />
percent) <strong>and</strong> paleness (6 percent).<br />
Very few reported other problems<br />
like abnormal position,<br />
convulsion, bleeding etc. (Figure<br />
4.2). Among those who had any<br />
complications, 58 percent of them<br />
had sought treatment mainly from<br />
the private health facility (88 percent). Relatively higher proportion of urban women<br />
sought treatment (61 percent) for pregnancy complications than the rural counterpart (41<br />
percent).<br />
4.5 PLACE OF DELIVERY<br />
Complications<br />
Figure: 4.2<br />
Percentage of women with pregnancy<br />
complications<br />
Swelling of h<strong>and</strong>s <strong>and</strong> feet<br />
Abnormal position of foetus<br />
DLHS-RCH, 2002<br />
Paleness<br />
Visual disturbances<br />
Excessive bleeding<br />
Convulsion<br />
Tables 4.4(A) <strong>and</strong> 4.4(B) present the delivery characteristics by selected background<br />
characteristics of women. One of the thrust areas of the maternal <strong>and</strong> child health services<br />
is the encouragement for the safe delivery under proper hygienic conditions <strong>and</strong> under the<br />
supervision of trained health personnel to ensure better health of the mother <strong>and</strong> child.<br />
Other<br />
Figure: 4.3<br />
Place of delivery <strong>and</strong> assistance during delivery<br />
0.3<br />
0.5<br />
1.1<br />
6.4<br />
6.4<br />
7.9<br />
18.0<br />
0 10 20 30 40 50<br />
Percent<br />
Percent disribution of women by place of<br />
delivery<br />
Percent disribution of home deliveries<br />
by type of assistance during delivery<br />
Private<br />
health<br />
institutions<br />
59.4%<br />
Home<br />
28.3%<br />
Relative/<br />
friends<br />
6.4%<br />
None<br />
1.1% Doctor<br />
10.9%<br />
ANM/<br />
Nurse<br />
18.8%<br />
Government<br />
health<br />
institutions<br />
12.3%<br />
Untrained<br />
dai<br />
46.9%<br />
Trained dai<br />
15.8%<br />
DLHS-RCH, 2002<br />
Most of the deliveries in the district were normal deliveries (79 percent). The<br />
proportion of caesarian deliveries is substantially high in urban areas (22 percent) than<br />
rural areas (5 percent). Of the total deliveries conducted, 28 percent of deliveries were<br />
reported to be home deliveries while majority of deliveries (72 percent) took place in the<br />
institutions (Figure 4.3).<br />
35
Majority (85 percent) of the total deliveries were safe delivery. Safe deliveries were<br />
more prominent in urban areas than rural areas. Education, st<strong>and</strong>ard of living <strong>and</strong> children<br />
ever born had positive impact on the percentage of women who had safe deliveries that is<br />
higher percentage of women having 10 <strong>and</strong> above years of schooling belonging to higher<br />
st<strong>and</strong>ard of living <strong>and</strong> having one child had safe delivery. Most of the institutional<br />
deliveries (59 percent) had taken place in the private institutions. About seven percent of<br />
deliveries in the rural areas <strong>and</strong> 14 percent in the urban areas took place in government<br />
health facility. Home deliveries were reported to be high in rural areas of Ahmedabad<br />
district (62 percent) than in urban areas (19 percent). As usual home deliveries were<br />
observed more amongst women with low st<strong>and</strong>ard of living (70 percent) than those<br />
belonging to high st<strong>and</strong>ard of living (10 percent).<br />
Table 4.4 (A) DELIVERY CHARACTERISTICS<br />
Percentage of women* by place of delivery, assistance during delivery <strong>and</strong> delivery complications by selected background<br />
characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Place of delivery, assistance received <strong>and</strong><br />
complications<br />
Percentage distribution of women who had<br />
Normal delivery<br />
Caesarean delivery<br />
Assisted delivery<br />
Total<br />
78.5<br />
18.4<br />
3.1<br />
Residence Caste# Availability of<br />
health facility in<br />
the village<br />
Rural Urban SC/ST Other No Yes<br />
94.7<br />
5.3<br />
0.0<br />
73.9<br />
22.2<br />
4.0<br />
79.0<br />
21.0<br />
0.0<br />
78.4<br />
17.9<br />
3.7<br />
93.9<br />
6.1<br />
0.0<br />
96.2<br />
3.8<br />
0.0<br />
Percentage distribution of women by place of<br />
delivery<br />
<strong>Health</strong> institution<br />
Government<br />
Private<br />
Home<br />
71.7<br />
12.3<br />
59.4<br />
28.3<br />
37.8<br />
6.5<br />
31.2<br />
62.2<br />
81.4<br />
14.0<br />
67.4<br />
18.6<br />
69.5<br />
9.5<br />
60.0<br />
30.5<br />
72.2<br />
12.9<br />
59.3<br />
27.8<br />
37.5<br />
6.1<br />
31.4<br />
62.5<br />
38.2<br />
7.3<br />
30.9<br />
61.8<br />
Percentage of home deliveries by type of<br />
assistance during delivery $<br />
Doctor<br />
ANM/nurse<br />
Trained dai<br />
Untrained dai<br />
Relatives/friends<br />
None<br />
10.9<br />
18.8<br />
15.8<br />
46.9<br />
6.4<br />
1.1<br />
14.5<br />
0.0<br />
8.4<br />
66.5<br />
8.3<br />
2.3<br />
7.6<br />
36.6<br />
22.8<br />
28.5<br />
4.6<br />
0.0<br />
40.8<br />
1.4<br />
7.2<br />
50.6<br />
0.0<br />
0.0<br />
4.6<br />
22.5<br />
17.6<br />
46.2<br />
7.8<br />
1.3<br />
19.5<br />
0.0<br />
5.1<br />
65.3<br />
10.1<br />
0.0<br />
5.7<br />
0.0<br />
14.3<br />
68.6<br />
5.2<br />
6.2<br />
Percentage of women who had safe delivery £ 84.6 52.0 93.8 84.6 84.6 52.9 50.5<br />
Percentage of women who had delivery<br />
complications<br />
Premature labour<br />
Excessive bleeding<br />
Prolonged labour (12+ hours)<br />
Obstructed labour<br />
Breech presentation<br />
Other<br />
51.7<br />
17.3<br />
3.2<br />
12.9<br />
29.1<br />
10.5<br />
8.6<br />
59.8<br />
22.9<br />
9.9<br />
9.7<br />
39.5<br />
7.6<br />
4.6<br />
49.3<br />
15.7<br />
1.3<br />
13.8<br />
26.1<br />
11.3<br />
9.7<br />
46.2<br />
12.7<br />
1.6<br />
7.4<br />
18.4<br />
8.7<br />
15.0<br />
52.7<br />
18.2<br />
3.5<br />
14.0<br />
31.2<br />
10.8<br />
7.3<br />
49.7<br />
9.4<br />
6.4<br />
6.1<br />
34.3<br />
6.1<br />
3.2<br />
77.4<br />
46.4<br />
16.0<br />
15.9<br />
48.6<br />
10.1<br />
7.1<br />
Number of women 261 58 203 42 219 37 (21)<br />
# The total figure may not add to (N) due to don’t know <strong>and</strong> missing cases $ Based on home delivery<br />
£ Either institution delivery or home delivery assisted by Doctor/ Nurse/ANM/Trained dai<br />
* Women who had their last live/still birth since 1.1.1999<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
Further, 53 percent of home deliveries were attended by untrained person. This<br />
practice remained the same in all the caste groups. The trained dai <strong>and</strong> trained personnel<br />
(doctor, ANM, nurse, LHV etc.) conducted only 16 percent <strong>and</strong> 30 percent home<br />
deliveries respectively (Figure 4.3). There is a need to increase the awareness, especially<br />
among the rural women to seek assistance from trained personnel for conducting the<br />
deliveries.<br />
36
The proportion of<br />
institutional deliveries are<br />
markedly higher (81 percent) in<br />
the urban areas as compared to the<br />
rural areas (38 percent). The<br />
proportion of institutional<br />
deliveries increased with the<br />
increase in st<strong>and</strong>ard of living.<br />
About 65 percent of the illiterate<br />
women, as against 92 percent of<br />
those with at least 10 years of<br />
education had institutional<br />
deliveries (Figure 4.4).<br />
Nearly 52 percent of the<br />
women had suffered from delivery<br />
10 + years<br />
STANDARD OF LIVING INDEX<br />
92.3<br />
complications <strong>and</strong> such<br />
Low 29.7<br />
proportions of women were more<br />
Medium<br />
65.0<br />
in rural areas (60 percent)<br />
High<br />
90.1<br />
compared to the urban areas (49<br />
percent). Of those who had<br />
0 20 40 60 80 100<br />
DLHS-RCH, 2002<br />
Percent<br />
delivery complications, 29 percent<br />
had suffered from obstructed labour <strong>and</strong> around 17 percent from premature labour, 13<br />
percent from prolonged labour <strong>and</strong> 11 percent from breech presentation.<br />
Table 4.4 (B) DELIVERY CHARACTERISTICS<br />
Percentage of women* by place of delivery, assistance during delivery <strong>and</strong> delivery complications by selected background<br />
characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Place of delivery, assistance<br />
received <strong>and</strong> complications<br />
Education<br />
St<strong>and</strong>ard of living<br />
index<br />
Children ever born<br />
Percentage distribution of women<br />
who had<br />
Normal delivery<br />
Caesarean delivery<br />
Assisted delivery<br />
Percentage distribution of women by<br />
place of delivery<br />
<strong>Health</strong> institution<br />
Government<br />
Illiterate<br />
89.7<br />
10.3<br />
0.0<br />
64.7<br />
6.0<br />
58.7<br />
35.3<br />
0-9@<br />
years<br />
97.5<br />
1.8<br />
0.7<br />
58.4<br />
23.5<br />
34.9<br />
41.6<br />
Figure: 4.4<br />
Institutional deliveries by some selected<br />
background characteristics of women<br />
RESIDENCE<br />
10 &<br />
above<br />
48.0<br />
43.4<br />
8.6<br />
92.3<br />
7.1<br />
85.2<br />
7.7<br />
CASTE<br />
EDUCATION<br />
Low Medium High 1 2 3+<br />
Private<br />
Home<br />
Percentage distribution of home<br />
deliveries by type of assistance<br />
during delivery $<br />
Doctor<br />
3.9 18.7 0.0 12.2 7.6 18.7 19.2 13.2 3.1<br />
ANM/nurse<br />
0.6 26.2 59.5 0.6 20.1 52.8 27.7 24.5 8.8<br />
Trained dai<br />
9.2 22.3 9.3 6.6 25.2 6.2 35.9 13.8 0.4<br />
Untrained dai<br />
72.9 29.4 27.5 65.4 43.4 19.3 17.3 42.4 76.6<br />
Relatives/friends<br />
10.7 3.4 3.8 11.9 3.8 3.1 0.0 6.1 8.4<br />
None<br />
2.7 0.0 0.0 3.2 0.0 0.0 0.0 0.0 2.7<br />
Percentage of women who had safe<br />
delivery £ 69.5 86.4 97.6 43.4 83.5 97.8 95.5 88.3 71.1<br />
Percentage of women who had<br />
delivery complications**<br />
Premature labour<br />
Excessive bleeding<br />
Prolonged labour (12+ hours)<br />
Obstructed labour<br />
Breech presentation<br />
Other<br />
39.9<br />
16.2<br />
4.4<br />
5.1<br />
24.0<br />
5.1<br />
9.2<br />
43.9<br />
7.4<br />
3.2<br />
9.0<br />
35.2<br />
1.0<br />
1.5<br />
71.1<br />
28.6<br />
2.0<br />
24.6<br />
27.8<br />
25.4<br />
15.3<br />
54.2<br />
21.6<br />
16.0<br />
7.3<br />
45.3<br />
6.0<br />
4.3<br />
27.2<br />
7.6<br />
0.4<br />
5.5<br />
12.8<br />
2.7<br />
6.3<br />
72.2<br />
24.5<br />
1.8<br />
21.0<br />
38.5<br />
18.5<br />
11.9<br />
65.6<br />
21.7<br />
3.4<br />
22.2<br />
39.4<br />
13.5<br />
13.0<br />
39.8<br />
13.8<br />
1.3<br />
9.4<br />
20.6<br />
1.2<br />
11.1<br />
46.4<br />
15.5<br />
4.4<br />
5.8<br />
24.8<br />
14.3<br />
2.0<br />
Number of women 85 89 87 36 105 120 99 70 91<br />
100.0<br />
0.0<br />
0.0<br />
29.7<br />
6.3<br />
23.5<br />
70.3<br />
Rural<br />
Urban<br />
SC/ST<br />
Others<br />
Illiterate<br />
0-9 years<br />
91.3<br />
8.2<br />
0.6<br />
65.0<br />
10.7<br />
54.3<br />
35.0<br />
61.0<br />
32.8<br />
6.2<br />
90.1<br />
15.5<br />
74.6<br />
9.9<br />
37.8<br />
58.4<br />
66.1<br />
25.7<br />
8.2<br />
74.0<br />
16.5<br />
57.5<br />
26.0<br />
69.5<br />
64.7<br />
72.5<br />
81.4<br />
85.5<br />
14.5<br />
0.0<br />
75.9<br />
15.8<br />
60.1<br />
24.1<br />
86.1<br />
13.9<br />
0.0<br />
67.1<br />
5.3<br />
61.8<br />
32.9<br />
37
* Women who had their last live/still birth since 1.1.1999 ** Multiple responses<br />
£ Either institution delivery or home delivery assisted by Doctor/ Nurse/ANM/Trained dai<br />
$ Based on home deliveries @ Literate women with no years of schooling are also included<br />
4.6 POSTNATAL CARE<br />
Table 4.5 presents women by post-delivery complications <strong>and</strong> type of treatment of these<br />
complications by background characteristics. About 10 percent women in both the rural<br />
<strong>and</strong> the urban areas had post-delivery follow up visit within two weeks. The percentage of<br />
women who had at least one symptom of post-delivery complication was reported to be<br />
15. Women reporting post-delivery complication were high in rural areas (31 percent),<br />
belonging to low st<strong>and</strong>ard of living (27 percent) <strong>and</strong> villages where there was health<br />
facility (43 percent).<br />
Lower abdominal pain, severe headache, <strong>and</strong> high fever were the major complications<br />
reported by women who had post-delivery complications. It is observed that 56 percent of<br />
the women who had post delivery complications had sought treatment for their problems<br />
mainly from private facility (94 percent). Treatment seeking behaviour was better among<br />
women living in urban areas, belonging to other caste community with 10 year <strong>and</strong> above<br />
education, belonging to higher st<strong>and</strong>ard of living <strong>and</strong> villages with health facilities.<br />
Table 4.5 POSTNATAL CARE<br />
Percentage of women* by post-delivery complication <strong>and</strong> sought treatment by type of treatment by background<br />
characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Complication <strong>and</strong> type of<br />
treatment<br />
Women who had postdelivery<br />
follow up visit<br />
(within two weeks)<br />
Women who reported at<br />
least one symptom of postdelivery<br />
complication<br />
Women who had postdelivery<br />
complication by<br />
type of complication<br />
High fever<br />
Lower abdominal pain<br />
Foul smelling vaginal<br />
discharge<br />
Excessive bleeding<br />
Convulsion<br />
Severe headache<br />
Other<br />
Women who sought<br />
treatment for post- delivery<br />
complication<br />
Women who sought<br />
treatment by source of<br />
treatment **<br />
Government health<br />
facility<br />
PHC<br />
SC<br />
Private health facility<br />
ISM facility<br />
Total<br />
Residence Caste# Education St<strong>and</strong>ard of living<br />
index<br />
Rural Urban SC/ST Other Illiterate 0-9@<br />
years<br />
38<br />
10 Low Medium High<br />
years<br />
&<br />
above<br />
Availability<br />
of health<br />
facility in<br />
the village<br />
No Yes<br />
9.6 9.8 9.5 2.3 11.0 8.6 17.9 2.0 10.8 17.8 2.1 3.1 21.4<br />
14.8 31.4 10.1 12.8 15.2 12.3 24.3 7.5 26.7 8.3 17.0 24.8 42.9<br />
5.9<br />
5.2<br />
2.1<br />
1.4<br />
0.6<br />
6.3<br />
4.5<br />
15.8<br />
15.3<br />
6.8<br />
3.7<br />
2.1<br />
20.7<br />
1.4<br />
3.0<br />
2.3<br />
0.7<br />
0.7<br />
0.2<br />
2.2<br />
5.3<br />
6.2<br />
3.3<br />
3.5<br />
0.4<br />
0.0<br />
10.5<br />
0.0<br />
5.8<br />
5.5<br />
1.8<br />
1.5<br />
0.8<br />
5.4<br />
5.3<br />
7.2<br />
7.8<br />
1.8<br />
1.3<br />
1.4<br />
9.2<br />
0.0<br />
7.3<br />
3.9<br />
3.2<br />
1.4<br />
0.0<br />
6.4<br />
11.5<br />
3.1<br />
3.9<br />
1.1<br />
14.4<br />
0.5<br />
3.3<br />
1.6<br />
10.0<br />
11.0<br />
7.6<br />
6.0<br />
0.0<br />
16.7<br />
0.0<br />
7.3<br />
6.4<br />
1.2<br />
0.2<br />
1.2<br />
4.2<br />
0.8<br />
3.4<br />
2.3<br />
1.2<br />
1.0<br />
0.3<br />
4.9<br />
9.0<br />
9.2<br />
9.3<br />
3.2<br />
0.0<br />
0.0<br />
12.3<br />
0.0<br />
27.4<br />
25.6<br />
13.1<br />
10.1<br />
5.8<br />
35.3<br />
3.8<br />
56.3 24.5 84.2 26.0 61.2 39.2 55.6 85.7 19.3 44.3 78.6 0.0 49.1<br />
4.2<br />
1.4<br />
0.0<br />
93.7<br />
2.1<br />
7.0<br />
7.0<br />
0.0<br />
93.0<br />
0.0<br />
3.5<br />
0.0<br />
0.0<br />
93.9<br />
2.6<br />
29.8<br />
0.0<br />
0.0<br />
70.2<br />
0.0<br />
2.4<br />
1.5<br />
0.0<br />
95.4<br />
2.2<br />
11.4<br />
7.5<br />
0.0<br />
77.7<br />
10.9<br />
3.7<br />
0.0<br />
0.0<br />
96.3<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
100.0<br />
0.0<br />
Number of women 261 58 203 42 219 85 89 87 36 105 120 37 (21)<br />
@ Literate women with no year of schooling are also included<br />
* Women who had their last live/ still birth since 1-1-1999 ** Total percent may<br />
add more than 100.0 due to multiple responses<br />
# Total figure may not add to (N) due to don’t know <strong>and</strong> missing cases<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
16.8<br />
16.8<br />
0.0<br />
83.2<br />
0.0<br />
4.1<br />
0.0<br />
0.0<br />
95.9<br />
0.0<br />
2.7<br />
0.0<br />
0.0<br />
94.5<br />
2.8<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
7.0<br />
7.0<br />
0.0<br />
93.0<br />
0.0
CHAPTER - 5<br />
CHILD CARE AND IMMUNIZATION<br />
The vaccination of children against six major diseases has been an important part of the<br />
child health care programme in India. The National Immunization Porgramme has been<br />
implemented as per the National <strong>Health</strong> Policy. The Exp<strong>and</strong>ed Programme on<br />
Immunization (EPI) was started by the Government of India in 1978. The main objective<br />
of this programme was to reduce the morbidity, mortality <strong>and</strong> disabilities. The Universal<br />
Immunization Programme (UIP) was also introduced in 1985-86. The st<strong>and</strong>ard<br />
immunization schedule developed for the child immunization programme specifics the age<br />
at which vaccine is to be administered, the number of doses to be given. In this chapter the<br />
information on immunization status of the children, breastfeeding practices, the awareness<br />
<strong>and</strong> practice of women during diarrhoea <strong>and</strong> pneumonia among children have been<br />
discussed <strong>and</strong> presented below.<br />
5.1 BREASTFEEDING AND WEANING PRACTICES<br />
As recommended by WHO,<br />
breastfeeding should be initiated<br />
immediately after birth <strong>and</strong> should be<br />
continued exclusively up to four<br />
months. The WHO also suggests that<br />
the mother’s first milk (yellowish<br />
milk, known as colostrum) should be<br />
given to the baby because it provides<br />
protection against certain infections.<br />
In the later months, breast milk it has<br />
to be supplemented with other semisolid<br />
<strong>and</strong> solid foods. Table 5.1<br />
presents the breastfeeding practices<br />
among the CMW of Ahmedabad<br />
district.<br />
Same day<br />
after two<br />
hours of<br />
birth<br />
27.5%<br />
DLHS-RCH, 2002<br />
Figure: 5.1<br />
Initiation of breastfeeding<br />
1-3 days<br />
39.1%<br />
After 3 days<br />
10.3%<br />
Never<br />
0.2%<br />
Immediately<br />
/ within two<br />
hours of<br />
birth<br />
22.9%<br />
As Table 5.1 shows, about 23 percent of the mothers breastfed their children<br />
immediately/within two hours of birth. About five percent of the children were breastfed<br />
exclusively for stipulated period of 4 months. Here it needs to be mentioned that,<br />
exclusive breastfeeding includes breastfeeding the child without giving any thing<br />
including water. Practice of colostrum feeding shows that around three-fifths of the<br />
women squeezed out the first milk. This practice was found to be relatively high among<br />
the women residing in the rural area (72 percent), belonging to scheduled caste<br />
(SC)/scheduled tribe (ST) community (68 percent) <strong>and</strong> belonging to low st<strong>and</strong>ard of living<br />
2
(68 percent). This indicates urgent need to educate women about the importance of<br />
colostrums milk for the health of the child.<br />
3
Table 5.1 BREASTFEEDING<br />
Percentage of women* by timing of first breastfeeding to child by selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Breastfeeding<br />
Total Residence Caste# Education St<strong>and</strong>ard of Living Index<br />
Rural Urban SC/ST Other Illiterate 0-9@<br />
years<br />
10 years &<br />
above<br />
Low Medium High<br />
Percent distribution of women who breastfed the child by<br />
timing of first breastfeeding<br />
Immediately/Within two hours of birth<br />
Same day after two hours of birth<br />
1-3 days<br />
After 3 days<br />
Never<br />
22.9<br />
27.5<br />
39.1<br />
10.3<br />
0.2<br />
19.2<br />
12.7<br />
55.8<br />
11.6<br />
0.7<br />
23.8<br />
31.0<br />
35.0<br />
10.0<br />
0.1<br />
Percentage of women who squeezed out the first breast milk 58.9 71.5 55.8 67.7 57.2 50.3 73.3 53.5 67.5 62.8 53.4<br />
16.9<br />
35.7<br />
38.4<br />
9.0<br />
0.0<br />
24.1<br />
25.8<br />
39.3<br />
10.6<br />
0.3<br />
29.1<br />
21.4<br />
41.4<br />
7.6<br />
0.4<br />
29.9<br />
32.4<br />
36.9<br />
0.6<br />
0.3<br />
10.7<br />
28.4<br />
39.1<br />
21.8<br />
0.0<br />
12.2<br />
13.7<br />
68.8<br />
4.2<br />
1.2<br />
23.8<br />
34.4<br />
36.3<br />
5.2<br />
0.2<br />
25.0<br />
25.2<br />
33.8<br />
16.1<br />
0.0<br />
Percentage of women whose children were on exclusive breast<br />
milk<br />
For four month **<br />
For six months ***<br />
5.0<br />
0.5<br />
3.0<br />
0.7<br />
5.5<br />
0.4<br />
1.3<br />
1.3<br />
5.8<br />
0.3<br />
14.1<br />
1.2<br />
0.0<br />
0.0<br />
1.3<br />
0.3<br />
4.8<br />
1.2<br />
9.7<br />
0.2<br />
1.2<br />
0.5<br />
Number of women 257 51 206 41 216 84 83 90 32 102 123<br />
* With youngest child born after 1-1-1999<br />
** With youngest child born after 1.1.1999 <strong>and</strong> 4 months or older at the time of survey <strong>and</strong> breastfed for more than 4 months<br />
*** With youngest child born after 1.1.1999 <strong>and</strong> 6 months or older at the time of survey <strong>and</strong> breastfed for more than 6 months<br />
# The total figure may not add to (N) due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included<br />
4
5.2 IMMUNIZATION OF THE CHILDREN<br />
Immunization of the children is a very important component of the Exp<strong>and</strong>ed Programme<br />
on Immunization (EPI) started by the Govt. of India in 1978. To underst<strong>and</strong> the coverage<br />
of immunization, data of all those children who were born since 1 st January 1999 <strong>and</strong> were<br />
age 12 months at the time of survey was collected. The immunization status of the<br />
children is presented in Tables 5.2(A) <strong>and</strong> 5.2(B).<br />
Table 5.2 (A) VACCINATION OF CHILDREN<br />
Percentage of children* who received vaccination, Hepatitis B, Vitamin A, IFA tablets/liquid by some selected background<br />
characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Type of vaccination<br />
Total Residence Caste# Availability of health<br />
facility in the village<br />
Rural Urban SC/ST Other No Yes<br />
Polio zero 61.0 38.9 65.7 63.1 60.6 31.5 49.6<br />
BCG 93.3 87.2 94.6 97.0 92.6 91.8 80.7<br />
DPT injection<br />
No DPT<br />
1<br />
2<br />
3<br />
Don’t remember<br />
Polio doses<br />
No Polio<br />
1<br />
2<br />
3<br />
5.5<br />
94.3<br />
85.8<br />
74.4<br />
0.3<br />
3.5<br />
92.6<br />
87.3<br />
72.4<br />
13.0<br />
87.0<br />
80.8<br />
73.0<br />
0.0<br />
6.5<br />
92.8<br />
89.1<br />
78.3<br />
3.9<br />
95.8<br />
86.9<br />
74.7<br />
0.4<br />
2.9<br />
92.6<br />
87.0<br />
71.2<br />
5.7<br />
94.3<br />
90.8<br />
72.3<br />
0.0<br />
16.2<br />
82.4<br />
81.6<br />
76.2<br />
5.4<br />
94.2<br />
84.9<br />
74.8<br />
0.3<br />
1.1<br />
98.9<br />
82.8<br />
76.1<br />
8.2<br />
91.8<br />
87.7<br />
75.4<br />
0.0<br />
8.2<br />
91.8<br />
87.7<br />
71.5<br />
Measles 76.7 66.2 76.2 48.9 82.0 83.6 72.5<br />
Full vaccination £ 64.2 66.2 63.7 45.1 67.8 71.5 58.7<br />
No vaccination at all 1.3 6.5 0.2 2.6 1.0 8.2 4.0<br />
Hepatitis B 19.3 8.6 21.5 0.0 23.1 11.9 4.0<br />
Vitamin A<br />
None<br />
1<br />
2<br />
3<br />
Don’t remember<br />
45.2<br />
33.2<br />
8.3<br />
0.3<br />
1.3<br />
41.4<br />
45.4<br />
15.5<br />
0.0<br />
4.7<br />
Iron Folic Acid Tablets/ Liquid 20.1 17.8 20.6 1.8 23.7 11.9 26.1<br />
Number of children 281 49 232 45 234 29 (20)<br />
* Includes only last <strong>and</strong> last but one living child born since 1.1.1999 <strong>and</strong> 12 months or older at the time of survey<br />
# The total figure may not add to (N) due to don’t know <strong>and</strong> missing cases<br />
£ BCG, three doses of DPT, three doses of Polio (excluding Polio zero) <strong>and</strong> Measles<br />
46.0<br />
30.6<br />
6.8<br />
0.4<br />
0.5<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
Immediately after birth,<br />
the baby is given one drop<br />
of oral polio, which is called<br />
zero polio. Out of 281<br />
children, around 61 percent<br />
had received Polio – zero.<br />
This proportion was quite<br />
high in the urban areas (66<br />
percent) compared to rural<br />
areas (39 percent).<br />
Percentage of children<br />
protected against all the six<br />
killer diseases shows that 93<br />
percent were given BCG, 74<br />
Percent<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Boy<br />
57.0<br />
Girl<br />
64.6<br />
Full<br />
vaccination<br />
DLHS-RCH, 2002<br />
Boy<br />
81.7<br />
18.1<br />
21.8<br />
3.8<br />
0.0<br />
0.0<br />
50.6<br />
35.0<br />
8.7<br />
0.4<br />
1.5<br />
Figure: 5.2<br />
Vaccination of children<br />
Girl<br />
71.5<br />
Measles<br />
Girl<br />
Boy 79.2<br />
65.9<br />
3 Doses of<br />
Polio<br />
Girl<br />
Boy<br />
77.7<br />
71.2<br />
3 Doses of<br />
DPT<br />
28.7<br />
51.4<br />
11.8<br />
0.0<br />
8.1<br />
Boy<br />
90.2<br />
BCG<br />
Girl<br />
96.5<br />
19.9<br />
80.1<br />
71.0<br />
69.4<br />
0.0<br />
4.0<br />
94.1<br />
91.1<br />
88.0<br />
59.5<br />
36.8<br />
20.8<br />
0.0<br />
0.0<br />
5
percent were given all the three doses of DPT, 72 percent received all the three drops of<br />
polio <strong>and</strong> 77 percent were protected by measles vaccine (see Figure 5.2).<br />
Overall, 64 percent of the children were fully immunized. Full immunization status<br />
was below 50 percent among SC/ ST group (45 percent) <strong>and</strong> illiterate mothers (49 percent)<br />
but the economic status of the family did not influence much. Slightly more than threefifths<br />
(64 percent) of the children belonging to the economically poor family were fully<br />
immunized. Availability of health facilities in villages did not have any significant impact<br />
on the immunization status of the children in the district as 72 percent of the children were<br />
fully immunized in the villages without health facility compared to those belonging to<br />
health facility (59 percent). To reduce the risk of night blindness, babies are supposed to<br />
get required doses of Vitamin A supplement, more than half (55 percent) of the children,<br />
slightly higher percent of children in rural than urban areas, received at least one does of<br />
Vitamin A. Higher percentage of children with mothers having 10 <strong>and</strong> above years of<br />
schooling belonging to high st<strong>and</strong>ard of living had received at least one dose of Vitamin<br />
A. Again more male than female had received Vitamin A solution. Further, children are<br />
also given IFA tablets for iron supplements under the national programme. The table<br />
reveals that 20 percent of the children had received IFA tablets.<br />
Table 5.2 (B) VACCINATION OF CHILDREN<br />
Percentage of children* who received vaccinations, Hepatitis B, Vitamin A, IFA tablets/liquid by some selected background<br />
characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Type of vaccination<br />
Mother’s Education St<strong>and</strong>ard of living index Sex of the child<br />
Illiterate 0-9@<br />
years<br />
10 years<br />
& above<br />
Low Medium High Male Female<br />
Polio zero 38.2 64.4 81.4 21.2 56.0 76.5 45.0 77.7<br />
BCG 82.4 97.9 99.9 88.8 89.3 98.5 90.2 96.5<br />
DPT injection<br />
No DPT<br />
1<br />
2<br />
3<br />
Don’t remember<br />
Polio doses<br />
No Polio<br />
1<br />
2<br />
3<br />
7.0<br />
92.4<br />
77.8<br />
67.0<br />
0.6<br />
8.7<br />
90.0<br />
76.7<br />
70.5<br />
9.0<br />
90.7<br />
80.9<br />
70.4<br />
0.2<br />
1.6<br />
98.4<br />
96.4<br />
71.1<br />
0.1<br />
99.9<br />
99.3<br />
86.2<br />
0.0<br />
0.1<br />
89.2<br />
89.0<br />
75.9<br />
6<br />
12.5<br />
87.5<br />
84.6<br />
75.6<br />
0.0<br />
2.5<br />
94.4<br />
93.4<br />
79.9<br />
8.3<br />
91.2<br />
80.8<br />
67.4<br />
0.5<br />
7.2<br />
92.6<br />
83.3<br />
69.0<br />
0.7<br />
99.1<br />
91.2<br />
81.1<br />
0.2<br />
0.0<br />
92.2<br />
89.9<br />
74.0<br />
2.2<br />
97.6<br />
82.3<br />
71.2<br />
0.2<br />
0.8<br />
92.0<br />
82.9<br />
65.9<br />
Measles 56.4 79.2 95.3 77.0 60.4 93.2 81.7 71.5<br />
Full vaccination £ 48.9 62.2 71.5 64.3 51.4 69.3 57.0 64.6<br />
No vaccination at all 2.1 1.6 0.1 2.5 2.2 0.0 0.7 1.9<br />
Hepatitis B 0.5 6.1 52.7 3.7 3.8 39.0 24.0 14.3<br />
Vitamin A<br />
None<br />
1<br />
2<br />
3<br />
Don’t remember<br />
40.7<br />
22.5<br />
8.3<br />
0.9<br />
3.1<br />
58.7<br />
28.3<br />
6.7<br />
0.0<br />
0.6<br />
35.8<br />
49.5<br />
10.0<br />
0.0<br />
0.0<br />
Iron Folic Acid Tablets/ Liquid 5.8 25.5 29.5 14.8 11.5 30.2 10.5 30.1<br />
Number of children 95 95 91 32 126 123 143 138<br />
* Includes only last <strong>and</strong> last but one living child born since 1.1.1999 <strong>and</strong> 12 months or older at the time of survey<br />
£<br />
BCG, three doses of DPT, three doses of Polio (excluding Polio zero) <strong>and</strong> Measles<br />
@ Literate women with no years of schooling are also included<br />
Table 5.2(C) shows the percentage of children age 12-23 months <strong>and</strong> 24-35 months<br />
who received specific vaccination by age according to residence in Ahmedabad district of<br />
Gujarat state. It can be seen from the Table 5.2(C) that two percent of children in age<br />
group 24-35 months did not receive any vaccination at all, while 66 percent of the children<br />
in the age group 24-35 months were fully immunized in the district, children fully<br />
immunized in 12-23 months of age is 44 percent. In Ahmedabad district eight percent<br />
43.0<br />
47.5<br />
10.5<br />
1.9<br />
7.2<br />
54.3<br />
14.2<br />
6.5<br />
0.0<br />
1.0<br />
36.6<br />
48.7<br />
9.5<br />
0.2<br />
0.0<br />
46.9<br />
36.1<br />
11.0<br />
0.2<br />
2.5<br />
8.8<br />
90.8<br />
89.5<br />
77.7<br />
0.4<br />
6.3<br />
93.2<br />
91.9<br />
79.2<br />
43.4<br />
30.1<br />
5.5<br />
0.4<br />
0.0
children in age group 12-23 months, <strong>and</strong> four percent in age group 24-35 months did not<br />
receive DPT injection. The percentage of children (in both the age group) who received all<br />
the three DPT injection (61 <strong>and</strong> 80 percent respectively in 12-23 <strong>and</strong> 24-35 months) is less<br />
as compared to those who received the at least one DPT injection (92 <strong>and</strong> 95 percent<br />
respectively in 12-23 <strong>and</strong> 24-35 months). Similar type of situation did exist in case of<br />
children receiving the polio doses in the district. It was observed that the percentage of<br />
children specially in the age group of 12-23 months who received full vaccination was<br />
higher in rural areas (66 percent) than urban areas (41 percent) of the district. Otherwise<br />
the immunization status was found to be more or less the same among children aged 24-35<br />
years in rural <strong>and</strong> urban areas.<br />
Table 5.2 (C) CHILDHOOD VACCINATIONS RECEIVED BY 12 MONTHS OF AGE<br />
Percentage of children age 12-23 months <strong>and</strong> 24-35 months who received specific vaccinations by age according to<br />
residence, Ahmedabad district of Gujarat, RCH, 2002<br />
Type of vaccination<br />
Total Rural Urban<br />
12-23<br />
months<br />
24-35<br />
months<br />
12-23<br />
months<br />
24-35<br />
months<br />
12-23<br />
months<br />
24-35<br />
months<br />
Polio zero 60.2 63.7 56.5 31.9 60.7 68.9<br />
BCG 89.4 95.4 89.3 80.1 89.4 97.9<br />
DPT Injection<br />
No DPT<br />
1<br />
2<br />
3<br />
Don’t remember<br />
Polio doses<br />
No Polio<br />
1<br />
2<br />
3<br />
7.8<br />
92.2<br />
75.1<br />
61.0<br />
0.0<br />
5.7<br />
94.1<br />
83.6<br />
62.4<br />
4.3<br />
94.9<br />
91.9<br />
80.0<br />
0.8<br />
2.0<br />
83.8<br />
81.3<br />
69.1<br />
8.5<br />
91.5<br />
87.2<br />
79.0<br />
0.0<br />
0.0<br />
100.0<br />
95.7<br />
87.5<br />
23.4<br />
76.6<br />
65.4<br />
65.4<br />
0.0<br />
11.1<br />
85.3<br />
74.2<br />
74.2<br />
7.7<br />
92.3<br />
73.4<br />
58.4<br />
0.0<br />
6.5<br />
93.3<br />
81.8<br />
58.8<br />
Measles 58.0 92.0 72.6 76.6 55.9 94.5<br />
Full vaccination £ 44.0 65.9 66.2 65.4 40.7 66.0<br />
No vaccination at all 0.1 2.0 0.0 11.1 0.1 0.5<br />
Number of children 113 75 (14) (11) 98 64<br />
£ BCG, three doses of DPT, three doses of polio (excluding polio zero) <strong>and</strong> measles<br />
Note: Table includes only surviving children from among the two most recent births in the three years preceding the survey<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
5.3 SOURCE OF IMMUNIZATION<br />
Table 5.3 shows the sources of immunization by residence <strong>and</strong> availability of health<br />
facilities. Most of the children (43 percent) were immunized at a government health<br />
facility <strong>and</strong> 23 percent of them at a private health facility. Further, among the children<br />
immunized at a government health facility, 35 percent of them were immunized at<br />
PHC/CHC, seven percent at government hospital <strong>and</strong> two percent at sub-centre.<br />
Table 5.3 SOURCE OF VACCINATIONS<br />
Percentage distribution of children* who had received any vaccination by source of last vaccination <strong>and</strong> by residence <strong>and</strong><br />
availability of health facility in the village, Ahmedabad district of Gujarat, RCH, 2002<br />
Source of vaccination<br />
Total Residence<br />
Availability of health<br />
facility in the village<br />
Rural Urban No Yes<br />
1.2<br />
97.9<br />
96.3<br />
82.4<br />
0.9<br />
0.5<br />
83.5<br />
82.4<br />
68.3<br />
7
Government<br />
Government hospital<br />
PHC/CHC<br />
Sub-centre<br />
ANM (Village session)<br />
Other<br />
Private<br />
Private hospital<br />
Private doctor<br />
6.8<br />
34.9<br />
1.7<br />
0.1<br />
32.7<br />
19.4<br />
3.4<br />
ISM facility 1.1 0.0 1.3 0.0 0.0<br />
Total percent 100.0 100.0 100.0 100.0 100.0<br />
No. of children who received a vaccination 277 46 232 26 (19)<br />
* Includes only last <strong>and</strong> last but one living child born since 1.1.1999 <strong>and</strong> 12 months or older at the time of survey<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
As can be observed from the table that in the district Ahmedabad, government sources<br />
are more preferred to private hospital for immunization of children. This clearly indicates<br />
that government health facilities in majority of cases have been providing immunization<br />
services in this district.<br />
0.0<br />
8.0<br />
5.0<br />
0.0<br />
83.4<br />
3.6<br />
0.0<br />
8.2<br />
40.1<br />
1.0<br />
0.1<br />
22.7<br />
22.5<br />
4.0<br />
0.0<br />
4.5<br />
0.0<br />
0.0<br />
95.5<br />
0.0<br />
0.0<br />
0.0<br />
12.8<br />
11.9<br />
0.0<br />
66.9<br />
8.4<br />
0.0<br />
5.4 AWARENESS AND TREATMENT OF DIARRHOEA<br />
Diarrhoea is a major killer disease among children under five years of age. Deaths from<br />
acute diarrhoea are mostly due to dehydration resulting from loss of water <strong>and</strong> electrolyte.<br />
Here an attempt was made to collect the data on awareness among women about the<br />
causes <strong>and</strong> treatment of diarrhoea, which has been presented in Table 5.4.<br />
,<br />
Table 5.4 AWARENESS OF DIARRHOEA<br />
Percentage of women* with last child born after 1-1-1999, who are aware of diarrhoea management <strong>and</strong> practices followed<br />
during diarrhoea by selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Diarrhoea<br />
Total<br />
Residence Caste# Education St<strong>and</strong>ard of living<br />
index<br />
Rural Urban SC/ST Other Illiterate 0-9@ 10 yrs & Low Medium High<br />
years above<br />
8<br />
Availability<br />
of health<br />
facility in<br />
the village<br />
No Yes<br />
Women aware of what to do if child<br />
gets diarrhoea 98.8 99.3 98.7 98.9 98.8 98.2 98.5 99.8 98.1 98.3 99.5 100.0 98.0<br />
Type of practices to be followed if<br />
child gets diarrhoea**<br />
Give ORS<br />
Salt <strong>and</strong> sugar solution<br />
Continue normal food<br />
Continue breastfeeding<br />
Give plenty of fluids<br />
Other<br />
35.5<br />
25.8<br />
7.4<br />
3.9<br />
6.1<br />
85.5<br />
24.2<br />
24.0<br />
8.7<br />
0.0<br />
2.2<br />
87.2<br />
38.3<br />
26.2<br />
7.1<br />
4.9<br />
7.0<br />
85.1<br />
16.2<br />
11.7<br />
4.6<br />
0.6<br />
14.8<br />
73.9<br />
39.2<br />
28.5<br />
8.0<br />
4.5<br />
4.4<br />
87.7<br />
15.1<br />
21.0<br />
7.6<br />
0.7<br />
7.6<br />
75.1<br />
52.6<br />
21.1<br />
6.8<br />
6.2<br />
1.5<br />
86.9<br />
38.8 22.1<br />
34.5 24.2<br />
7.9 10.9<br />
4.8 0.7<br />
8.8 1.0<br />
93.8 84.9<br />
38.6 36.6<br />
19.5 31.3<br />
4.4 9.1<br />
2.7 5.7<br />
6.1 7.4<br />
77.4 92.3<br />
Women whose child suffered from<br />
diarrhoea during two weeks prior to<br />
survey 4.8 11.2 3.2 7.1 4.3 7.4 4.6 2.5 10.9 4.0 3.8 3.5 24.4<br />
Women who continued breastfeeding<br />
same as before diarrhoea 3.6 11.2 1.7 7.1 2.9 7.4 2.1 1.4 10.9 3.7 1.6 3.5 24.4<br />
Women $ who gave child to drink<br />
amount of fluid<br />
Less than usual quantity<br />
Same as usual quantity<br />
More than usual quantity<br />
Women $ who gave child the<br />
amount of the food<br />
Less than usual quantity<br />
Same as usual quantity<br />
More than usual quantity<br />
0.3<br />
3.8<br />
0.1<br />
0.3<br />
2.9<br />
0.2<br />
0.6<br />
9.3<br />
0.6<br />
0.6<br />
7.0<br />
0.6<br />
0.2<br />
2.5<br />
0.0<br />
0.2<br />
1.9<br />
0.1<br />
0.0<br />
6.5<br />
0.0<br />
0.0<br />
3.4<br />
0.6<br />
0.4<br />
3.3<br />
0.1<br />
0.4<br />
2.8<br />
0.1<br />
0.4<br />
6.3<br />
0.0<br />
0.4<br />
4.2<br />
0.4<br />
0.3<br />
3.0<br />
0.4<br />
0.3<br />
3.1<br />
0.3<br />
0.3<br />
2.2<br />
0.0<br />
0.3<br />
1.5<br />
0.0<br />
1.0<br />
8.3<br />
0.0<br />
1.0<br />
3.8<br />
1.0<br />
0.0<br />
2.8<br />
0.3<br />
0.0<br />
2.8<br />
0.0<br />
0.4<br />
3.5<br />
0.0<br />
0.4<br />
2.7<br />
0.2<br />
21.3<br />
28.4<br />
7.1<br />
0.0<br />
0.0<br />
85.7<br />
29.1<br />
16.5<br />
11.5<br />
0.0<br />
6.0<br />
89.8<br />
0.0 1.7<br />
3.5 19.1<br />
0.0 1.7<br />
Women who gave ORS during<br />
diarrhoea 7.5 5.5 9.3 0.0 9.8 8.7 0.0 17.2 8.9 5.7 8.0 0.0 6.8<br />
Women who consulted any body or<br />
sought treatment 50.1 58.6 42.8 21.6 59.0 58.6 30.0 61.1 28.3 94.3 28.5 0.0 73.2<br />
0.0<br />
0.0<br />
0.0<br />
1.7<br />
19.1<br />
1.7
Number of women 257 51 206 41 216 84 83 90 32 102 123 32 (19)<br />
* With youngest child born after 1.1.1999<br />
# The total figure may not add to (N) due to don’t know <strong>and</strong> missing cases<br />
** Percentage may exceed 100.0 due to multiple responses<br />
$ Percentages may not add upto 100 due to cases where child is on exclusive breast milk<br />
@ Literate women with no years of schooling are also included<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
Almost all the women (99 percent) are aware of what to do when child gets diarrhoea.<br />
Among those who are aware, 36 percent of them reported giving ORS, <strong>and</strong> 26 percent of<br />
them reported giving salt sugar solution as one of the important remedial measure against<br />
diarrhoea. This was reported more by women in the urban areas than those in the rural<br />
areas as the remedial measure against diarrhoea. Women who are literate, belonging to<br />
high st<strong>and</strong>ard of living, mentioned these remedial measures more. Some of the women<br />
also reported that the child should be kept on continued breastfeeding (4 percent) <strong>and</strong><br />
given normal food (7 percent) <strong>and</strong> plenty of fluids (6 percent) if the child gets diarrhoea.<br />
During two weeks prior to the survey, only five percent of women reported that their<br />
child had suffered from diarrhoea <strong>and</strong> four percent of mothers continued breastfeeding in<br />
the same way as before diarrhoea. Among those who suffered from diarrhoea, eight<br />
percent of the mothers mentioned that they gave ORS to their child. Practice of giving<br />
more liquids was absolutely absent as very negligible percent of the mothers mentioned<br />
about it. The practice remained more or less same irrespective of the caste or education or<br />
economic status of the family or even availability of having health facility in the village.<br />
5.5 AWARENESS AND TREATMENT OF PNEUMONIA<br />
Another major killer disease among infants <strong>and</strong> children is ARI (Acute Respiratory<br />
Infection), also called pneumonia. An attempt was made to underst<strong>and</strong> the proportion of<br />
children who suffered from it in the last two weeks before the survey <strong>and</strong> their health<br />
seeking behaviour. About 25 percent of the women are aware of danger signs of<br />
pneumonia. Slightly higher percent of women in the rural areas (29 percent) are aware of<br />
danger signs of pneumonia, whereas this figure is 24 percent in the urban areas.<br />
Furthermore, Table 5.5 shows that the level of knowledge of the danger signs of<br />
pneumonia is associated with education, st<strong>and</strong>ard of living, <strong>and</strong> availability of health<br />
facility in the village.<br />
The danger sign of pneumonia more commonly reported by women are: difficulty in<br />
breathing (18 percent), pain in chest <strong>and</strong> productive cough (14 percent), rapid breathing<br />
(12 percent), excessively drowsy <strong>and</strong> difficulty in keeping awake (8 percent), chest in<br />
drawing (6 percent), <strong>and</strong> wheezing/whistling (5 percent). Unable to drink or take a feeding<br />
were also reported as the danger signs of pneumonia.<br />
The data shows that 13 percent of the children had suffered from pneumonia. More<br />
proportion of women in the rural (16 percent) as compared to the urban (12 percent)<br />
reported about the child’s ill health due to pneumonia. About 51 percent of the children<br />
were given treatment mainly at private hospitals (69 percent).<br />
9
Table 5.5 AWARENESS OF PNEUMONIA<br />
Percentage of women* who are aware of danger signs of pneumonia <strong>and</strong> practices followed during pneumonia episodes by<br />
selected backgrounds characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Pneumonia<br />
Total<br />
Residence Caste# Education St<strong>and</strong>ard of living<br />
index<br />
Rural Urban SC/ST Other Illiterate 0-9@<br />
years<br />
10<br />
yrs. &<br />
above<br />
Availability<br />
of health<br />
facility in<br />
the village<br />
Low Medium High No Yes<br />
Women aware of danger 25.1 28.6 24.2 7.0 28.5 10.5 31.4 32.8 21.8 23.6 27.2 24.7 35.3<br />
signs of pneumonia<br />
Danger signs**<br />
Difficulty in breathing 17.7 8.0 20.1 3.6 20.4 5.7 20.0 26.9 10.8 17.2 20.0 3.5 15.6<br />
Chest in-drawing<br />
Not able to drink or take a<br />
feeding<br />
Excessively drowsy <strong>and</strong><br />
difficulty in keeping awake<br />
Pain in chest <strong>and</strong><br />
5.8<br />
1.0<br />
8.2<br />
13.9<br />
1.3<br />
4.7<br />
2.8<br />
2.4<br />
0.0<br />
13.1<br />
0.0<br />
1.6<br />
6.5<br />
0.7<br />
10.3<br />
14.2<br />
1.6<br />
5.5<br />
0.5<br />
0.5<br />
0.0<br />
5.1<br />
1.1<br />
1.1<br />
6.8<br />
1.1<br />
9.8<br />
15.6<br />
1.3<br />
5.4<br />
2.6<br />
1.7<br />
0.0<br />
4.4<br />
0.8<br />
0.0<br />
12.1<br />
0.0<br />
17.0<br />
8.6<br />
2.8<br />
0.0<br />
2.9<br />
1.4<br />
7.8<br />
27.8<br />
0.3<br />
13.6<br />
5.4<br />
0.0<br />
0.0<br />
9.3<br />
0.0<br />
0.0<br />
7.6<br />
1.4<br />
14.1<br />
4.7<br />
0.5<br />
0.9<br />
4.3<br />
1.0<br />
5.6<br />
22.8<br />
2.3<br />
9.1<br />
3.5<br />
0.0<br />
0.0<br />
10.5<br />
0.0<br />
0.0<br />
1.7<br />
6.5<br />
0.0<br />
17.5<br />
0.0<br />
4.3<br />
productive cough<br />
11.9 21.0 9.7 5.0 13.3 4.7 12.1 18.5 10.0 7.5 16.1 21.1 20.8<br />
Conditions get worse<br />
than before<br />
Wheezing/ whistling<br />
Rapid breathing<br />
Women whose child<br />
suffered from cough, cold 13.1 16.2 12.3 5.5 14.5 12.0 6.1 20.5 19.4 5.8 17.5 7.2 31.6<br />
<strong>and</strong> difficulty in breathing<br />
during two weeks prior to<br />
survey<br />
Women who sought 51.2 38.2 55.4 84.1 48.8 46.2 81.1 45.6 40.6 60.3 51.8 0.0 53.1<br />
treatment for child’s cough<br />
<strong>and</strong> cold<br />
Source of treatment**<br />
Home remedy<br />
Government health<br />
facility<br />
12.1<br />
6.4<br />
69.4<br />
9.9<br />
0.0<br />
51.1<br />
12.6<br />
7.8<br />
73.4<br />
23.7<br />
13.7<br />
30.0<br />
10.6<br />
5.5<br />
74.3<br />
6.7<br />
18.7<br />
48.4<br />
10.8<br />
5.5<br />
83.6<br />
15.7 12.3<br />
0.0 24.2<br />
74.0 63.5<br />
12.7<br />
7.4<br />
45.3<br />
11.8<br />
2.1<br />
78.3<br />
0.0<br />
0.0<br />
0.0<br />
9.9<br />
0.0<br />
51.1<br />
Private health facility<br />
ISM facility<br />
1.5<br />
10.7<br />
0.0<br />
39.0<br />
1.8<br />
4.4<br />
0.0<br />
32.6<br />
1.6<br />
8.0<br />
0.0<br />
26.2<br />
0.0<br />
0.0<br />
3.0<br />
7.4<br />
0.0<br />
0.0<br />
0.0<br />
34.6<br />
2.2<br />
5.6<br />
0.0<br />
0.0<br />
0.0<br />
39.0<br />
Other<br />
Number of women 257 51 206 41 216 84 83 90 32 102 123 32 (19)<br />
* With youngest child born after 1.1.1999 ** Percentage may exceed<br />
100.0 due to multiple responses<br />
# The total figure may not add to (N) <strong>and</strong> percentage may not add upto 100.0 due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included<br />
Note: Percentage may not be reliable as based on less than 25 cases.
CHAPTER - 6<br />
FAMILY PLANNING<br />
Information about the knowledge of family planning <strong>and</strong> the use of contraceptive methods<br />
is of practical use to policy makers <strong>and</strong> programme administrators for formulating policies<br />
<strong>and</strong> strategies. This chapter begins with an assessment of women’s knowledge of family<br />
planning methods <strong>and</strong> special attention is focussed on non-use, reasons for<br />
discontinuation, health problems <strong>and</strong> satisfaction with the current use <strong>and</strong> their sources of<br />
motivation to use family planning. It also deals with the past users, future intention to use,<br />
unmet need of family planning <strong>and</strong> future fertility intention of the respondents. In addition,<br />
the chapter presents males’ attitude towards <strong>and</strong> perception of family planning methods.<br />
6.1 KNOWLEDGE OF CONTRACEPTIVE METHODS<br />
The awareness of<br />
contraceptives by selected<br />
background characteristics<br />
of CMW is shown in<br />
Table 6.1 All women are<br />
aware of at least one<br />
modern method of<br />
contraception <strong>and</strong> 82<br />
percent of them are aware<br />
of all modern methods (73<br />
percent in rural <strong>and</strong> 84<br />
percent in urban areas).<br />
Further, 99 percent of<br />
them are aware of any<br />
modern spacing method<br />
(97 percent in rural areas,<br />
<strong>and</strong> 100 percent in urban<br />
areas) (Figure 6.1).<br />
Awareness of all modern<br />
methods <strong>and</strong> any spacing<br />
methods is relatively more<br />
among the other caste<br />
groups, literate <strong>and</strong> those<br />
who were economically<br />
well off.<br />
Methods<br />
Any modern<br />
method<br />
Any modern<br />
spacing method<br />
All modern<br />
methods<br />
Female<br />
sterilization<br />
Male sterilization<br />
Contraceptive<br />
herbs<br />
DLHS-RCH, 2002<br />
IUD/Loop<br />
Pills<br />
Condom<br />
Traditional<br />
methods<br />
Figure: 6.1<br />
Knowledge of family planning methods<br />
9<br />
58.8<br />
81.9<br />
85.9<br />
93.8<br />
100<br />
99.1<br />
100<br />
97.7<br />
97.5<br />
0 20 40 60 80 100<br />
Percent<br />
2
Method-wise awareness shows that all the women knew about female sterilization.<br />
The proportion of those women who are aware of male sterilization, IUD/loop, <strong>and</strong> pills<br />
ranged between 94-98 percent. About 86 percent of the women know about condom.<br />
About 26 percent of the women knew about injectables <strong>and</strong> 19 percent about sponge<br />
method of family planning.<br />
3
Table 6.1 KNOWLEDGE OF CONTRACEPTIVE METHODS<br />
Percentage of currently married women age 15-44 who know any contraceptive method by method <strong>and</strong> by selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Contraceptive Method<br />
Total Residence Caste# Education St<strong>and</strong>ard of living index Availability of health<br />
facility in the village<br />
Rural Urban SC/ST Other Illiterate 0-9@ 10 years & Low Medium High No Yes<br />
years above<br />
Any modern method<br />
Any modern spacing* method<br />
All modern** methods<br />
100.0<br />
99.1<br />
81.9<br />
100.0<br />
96.7<br />
72.7<br />
100.0<br />
99.7<br />
84.1<br />
100.0<br />
98.3<br />
66.2<br />
100.0<br />
99.3<br />
84.6<br />
100.0<br />
97.7<br />
69.7<br />
100.0<br />
99.7<br />
83.2<br />
100.0<br />
99.9<br />
92.2<br />
100.0<br />
94.2<br />
62.8<br />
100.0<br />
99.4<br />
79.9<br />
100.0<br />
99.7<br />
86.1<br />
100.0<br />
98.6<br />
68.0<br />
100.0<br />
94.5<br />
78.4<br />
Female sterilization<br />
Tubectomy<br />
Laparoscopic<br />
100.0<br />
96.8<br />
95.7<br />
100.0<br />
100.0<br />
99.8<br />
100.0<br />
96.1<br />
94.7<br />
100.0<br />
99.8<br />
99.8<br />
100.0<br />
96.3<br />
95.0<br />
100.0<br />
95.8<br />
95.6<br />
100.0<br />
97.6<br />
91.2<br />
100.0<br />
97.2<br />
100.0<br />
100.0<br />
100.0<br />
99.5<br />
100.0<br />
96.1<br />
92.3<br />
100.0<br />
96.8<br />
97.1<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
100.0<br />
99.4<br />
Male sterilization<br />
Vasectomy<br />
No-scalpel vasectomy<br />
93.8<br />
62.6<br />
30.1<br />
87.5<br />
45.1<br />
6.5<br />
95.3<br />
66.8<br />
35.8<br />
93.2<br />
56.4<br />
32.4<br />
94.0<br />
63.7<br />
29.8<br />
89.5<br />
50.9<br />
22.1<br />
97.2<br />
55.4<br />
20.3<br />
94.8<br />
80.5<br />
46.9<br />
83.5<br />
49.5<br />
1.1<br />
92.2<br />
49.1<br />
22.4<br />
96.5<br />
72.7<br />
39.3<br />
86.2<br />
18.0<br />
5.5<br />
89.2<br />
78.4<br />
7.9<br />
IUD/Loop 97.7 95.6 98.3 98.0 97.7 97.0 99.0 97.2 92.7 98.9 97.9 98.6 92.0<br />
Pills<br />
Daily<br />
Weekly<br />
Condom/Nirodh<br />
Sponge (today)<br />
Injectables<br />
Norplant<br />
Contraceptive herbs<br />
Any traditional method<br />
Any other Indian system of medicinal<br />
97.5<br />
84.6<br />
38.6<br />
85.9<br />
19.2<br />
26.1<br />
2.8<br />
9.0<br />
58.8<br />
3.2<br />
92.3<br />
70.5<br />
10.7<br />
81.7<br />
1.1<br />
12.2<br />
0.0<br />
2.2<br />
33.0<br />
0.2<br />
98.7<br />
88.0<br />
45.2<br />
86.9<br />
23.6<br />
29.5<br />
3.5<br />
10.6<br />
64.9<br />
3.9<br />
93.0<br />
59.5<br />
35.4<br />
76.1<br />
6.8<br />
14.4<br />
0.1<br />
7.3<br />
27.0<br />
0.6<br />
98.2<br />
89.0<br />
39.2<br />
87.6<br />
21.4<br />
28.2<br />
3.3<br />
9.3<br />
64.3<br />
3.7<br />
92.6<br />
67.4<br />
23.6<br />
77.3<br />
4.5<br />
13.8<br />
0.1<br />
4.1<br />
33.0<br />
0.3<br />
99.7<br />
87.0<br />
28.3<br />
85.0<br />
9.9<br />
20.1<br />
0.1<br />
5.2<br />
55.6<br />
4.9<br />
99.9<br />
98.7<br />
62.4<br />
94.7<br />
42.0<br />
43.5<br />
7.9<br />
17.2<br />
86.2<br />
4.4<br />
91.2<br />
76.4<br />
5.4<br />
72.7<br />
1.3<br />
13.7<br />
0.2<br />
1.1<br />
32.3<br />
0.0<br />
95.3<br />
77.1<br />
31.5<br />
86.0<br />
10.2<br />
18.3<br />
0.1<br />
4.6<br />
40.1<br />
2.9<br />
99.7<br />
90.4<br />
48.0<br />
87.9<br />
27.5<br />
32.8<br />
4.8<br />
12.9<br />
74.0<br />
3.9<br />
91.7<br />
54.0<br />
6.8<br />
79.0<br />
0.0<br />
5.6<br />
0.0<br />
0.0<br />
26.5<br />
0.0<br />
93.1<br />
90.6<br />
15.3<br />
84.9<br />
2.4<br />
20.2<br />
0.0<br />
4.8<br />
40.9<br />
0.6<br />
Number of women 769 149 620 115 654 254 249 266 71 259 439 82 67<br />
4
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases<br />
* Include IUD, pills <strong>and</strong> condom<br />
** Include Female sterilization, Male sterilization, IUD, pills <strong>and</strong> condom<br />
@ Literate women with no years of schooling are also included<br />
5
Around two-fifths (59 percent) of women were aware of any traditional methods.<br />
Only three percent of woman reported knowing of any other contraceptive of the Indian<br />
System of medicine.<br />
6.2 KNOWLEDGE OF NO-SCALPEL VASECTOMY (NSV)<br />
The Table 6.2 presents percent of husb<strong>and</strong>s of eligible women by knowledge of NSV. The<br />
table shows that slightly more than half (53 percent) of husb<strong>and</strong>s are aware about the NSV<br />
as a contraceptive method. The knowledge of NSV is higher in urban area (56 percent)<br />
than rural area (45 percent) but the percentage remained more or less the same among<br />
those belonging to villages having or not having health facilities in the village. Among<br />
those who reported that they have heard of NSV, 52 percent of them say it is simpler than<br />
conventional method. Further, analysis of this data shows that 41 percent of the husb<strong>and</strong>s<br />
feel that NSV does not lead to any complication, <strong>and</strong> 36 percent of them feel that NSV<br />
does not affect the man’s sexual performance.<br />
Table 6.2 NO-SCALPEL VASECTOMY (NSV)<br />
Percentage of husb<strong>and</strong>s of eligible women by knowledge of NSV by residence <strong>and</strong> availability of health facility in the<br />
village, Ahmedabad district of Gujarat, RCH, 2002<br />
Knowledge of NSV<br />
Total Residence Availability of<br />
health facility in<br />
the village<br />
Rural Urban No Yes<br />
Percentage of husb<strong>and</strong>s who have knowledge about NSV<br />
Who know that NSV is simpler than conventional vasectomy<br />
Who feel that NSV does not lead to any complication<br />
Who feel that NSV does not affect man’s sexual performance<br />
52.9<br />
52.4<br />
40.7<br />
35.9<br />
44.7<br />
45.6<br />
61.3<br />
42.9<br />
55.5<br />
54.1<br />
35.6<br />
34.2<br />
45.7<br />
31.7<br />
61.8<br />
37.9<br />
43.4<br />
64.6<br />
60.5<br />
49.6<br />
Number of husb<strong>and</strong>s 404 95 308 54 42<br />
6.3 CONTRACEPTIVE PREVALENCE RATE<br />
Table 6.3 shows the contraceptive prevalence rate by selected background characteristics<br />
in Ahmedabad district, 56 percent of the couples use any methods of contraception of<br />
whom 50 percent had acceptors of modern method. Among the acceptors of modern<br />
methods 28 percent had accepted permanent method of sterilization. The use of modern<br />
method is same in the urban <strong>and</strong> rural areas of the district. The use of traditional method is<br />
six percent in this district.<br />
About 27 percent of the women had<br />
undergone sterilization. Percentage of<br />
sterilization acceptors is higher in the<br />
rural areas (40 percent) than those in the<br />
urban areas (25 percent). Acceptance of<br />
male sterilization is almost negligible in<br />
the district. Further, six percent are IUD<br />
users, eight percent pills users <strong>and</strong> nine<br />
percent condom users (Figure 6.2).<br />
Usership of spacing methods is relatively<br />
high among urban, educated <strong>and</strong> couples<br />
having high st<strong>and</strong>ard of living. The use<br />
of modern methods of contraception is<br />
high among the literate couples, having<br />
high st<strong>and</strong>ard of living <strong>and</strong> with availability of government health facilities.<br />
6<br />
Figure: 6.2<br />
Practice of family planning methods<br />
Female<br />
sterilization<br />
26.8%<br />
IUD/Loop<br />
5.6%<br />
Pills<br />
8.1%<br />
DLHS-RCH, 2002<br />
Condom<br />
8.7%<br />
Any<br />
traditional<br />
method<br />
6.1%<br />
Male<br />
sterilization<br />
1.0%<br />
Not using<br />
any method<br />
43.7%
Table 6.3 CONTRACEPTIVE PREVALENCE RATE<br />
Percentage of currently married women aged 15-44 by current use of contraceptive method <strong>and</strong> by selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Method<br />
Percentage of women/husb<strong>and</strong>s using<br />
Any method<br />
Any modern method<br />
Any sterilization<br />
Any traditional method<br />
Percentage distribution of<br />
women/husb<strong>and</strong> using Modern method<br />
Male sterilization<br />
Female sterilization<br />
IUD/Loop<br />
Pills<br />
Condom/Nirodh<br />
Traditional method<br />
Rhythm/periodic abstinence<br />
Withdrawal<br />
Total<br />
56.3<br />
50.2<br />
27.8<br />
6.1<br />
1.0<br />
26.8<br />
5.6<br />
8.1<br />
8.7<br />
5.3<br />
0.8<br />
Residence Caste# Education St<strong>and</strong>ard of living index Availability of<br />
health facility in<br />
the village<br />
Rural Urban SC/ST Other Illiterate 0-9@ years 10 years Low Medium High No Yes<br />
& above<br />
52.6<br />
50.4<br />
40.1<br />
2.2<br />
0.0<br />
40.1<br />
5.1<br />
1.0<br />
4.3<br />
1.1<br />
1.1<br />
57.3<br />
50.3<br />
24.9<br />
7.0<br />
1.3<br />
23.6<br />
5.7<br />
9.8<br />
9.8<br />
6.3<br />
0.7<br />
43.4<br />
36.8<br />
25.7<br />
6.7<br />
0.6<br />
25.1<br />
1.1<br />
0.9<br />
9.1<br />
6.5<br />
0.2<br />
58.7<br />
52.7<br />
28.2<br />
6.0<br />
1.1<br />
27.1<br />
6.4<br />
9.4<br />
8.7<br />
5.1<br />
0.9<br />
Any other modern method 0.0 0.0 0.0 0.0 0.0 0.0 0.0 0.1 0.0 0.0 0.1 0.0 0.0<br />
Number of women 769 148 620 115 654 253 249 266 71 259 439 82 67<br />
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases.<br />
@<br />
Literate women with no years of schooling are also included.<br />
56.3<br />
48.7<br />
44.4<br />
7.6<br />
0.5<br />
44.0<br />
1.5<br />
0.4<br />
2.4<br />
7.2<br />
0.4<br />
48.3<br />
44.3<br />
27.0<br />
4.0<br />
2.7<br />
24.3<br />
4.3<br />
8.3<br />
4.7<br />
3.6<br />
0.4<br />
64.1<br />
57.5<br />
12.8<br />
6.6<br />
0.1<br />
12.7<br />
10.7<br />
15.4<br />
18.4<br />
5.1<br />
1.4<br />
41.4<br />
39.6<br />
36.5<br />
1.7<br />
0.3<br />
36.2<br />
0.0<br />
0.0<br />
3.2<br />
1.7<br />
0.0<br />
47.5<br />
43.2<br />
34.4<br />
4.4<br />
2.9<br />
31.5<br />
2.8<br />
2.8<br />
3.2<br />
4.0<br />
0.3<br />
64.0<br />
56.2<br />
22.6<br />
7.8<br />
0.1<br />
22.5<br />
8.2<br />
12.6<br />
12.9<br />
6.6<br />
1.1<br />
47.1<br />
47.1<br />
32.0<br />
0.0<br />
0.0<br />
32.0<br />
8.2<br />
1.4<br />
5.5<br />
0.0<br />
0.0<br />
59.4<br />
54.5<br />
50.0<br />
4.8<br />
0.0<br />
50.0<br />
1.2<br />
0.5<br />
2.8<br />
2.4<br />
2.4<br />
7
6.4 USE OF CONTRACEPTIVES<br />
Table 6.4 shows the current use of contraceptive by selected background characteristics of<br />
CMW. Contraceptive prevalence rate in this district is 56 percent. The use of<br />
contraceptives increased from four percent among the currently married adolescent aged<br />
15-19, to as high as 69 percent among women aged 30-34 <strong>and</strong> 82 percent among women<br />
aged 40-44 years. The use of contraceptives increases with the increase in number of<br />
surviving children. However, the proportion of women accepting a method with no living<br />
daughters is 44 percent against 19 percent of the women accepting a method with no living<br />
son. The data clearly indicates that preference for sons is existing in this district.<br />
Table 6.4 USE OF CONTRACEPTIVES<br />
Percentage of currently married women aged 15-44 by current use <strong>and</strong> by ever use of contraceptives, according to<br />
selected demographic characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Demographic<br />
Characteristics<br />
Age-group<br />
15-19<br />
20-24<br />
25-29<br />
30-34<br />
35-39<br />
40-44<br />
Surviving children<br />
0<br />
1<br />
2<br />
3 or more<br />
Surviving sons<br />
0<br />
1<br />
2 or more<br />
Surviving daughters<br />
0<br />
1<br />
2 or more<br />
Modern<br />
method<br />
4.2<br />
32.7<br />
39.7<br />
53.5<br />
61.6<br />
81.2<br />
2.7<br />
36.7<br />
59.4<br />
68.9<br />
17.7<br />
55.2<br />
80.7<br />
42.3<br />
53.1<br />
55.3<br />
Percentage of women/<br />
their husb<strong>and</strong>s using<br />
Traditional<br />
method<br />
0.0<br />
8.5<br />
2.4<br />
15.1<br />
7.1<br />
1.2<br />
0.0<br />
2.1<br />
9.8<br />
7.4<br />
0.9<br />
14.4<br />
1.2<br />
1.2<br />
8.3<br />
8.5<br />
Any<br />
method<br />
4.2<br />
41.2<br />
42.1<br />
68.6<br />
68.7<br />
82.3<br />
2.7<br />
38.8<br />
69.2<br />
76.3<br />
18.6<br />
69.6<br />
81.9<br />
Not using<br />
any method<br />
95.8<br />
58.8<br />
57.9<br />
31.4<br />
31.3<br />
17.7<br />
97.3<br />
61.2<br />
30.8<br />
23.7<br />
81.4<br />
30.4<br />
18.1<br />
Percentage distribution<br />
of women/their<br />
husb<strong>and</strong>s by use of<br />
contraceptives<br />
Ever Never<br />
6.4<br />
46.7<br />
64.7<br />
75.2<br />
77.1<br />
83.4<br />
4.0<br />
66.7<br />
76.0<br />
80.9<br />
36.0<br />
78.0<br />
84.1<br />
93.6<br />
53.3<br />
35.3<br />
24.8<br />
22.9<br />
16.6<br />
96.0<br />
33.3<br />
24.0<br />
19.1<br />
64.0<br />
22.0<br />
15.9<br />
Number of<br />
women<br />
All women 50.3 6.1 56.3 43.6 66.0 34.0 769<br />
The total percent may not add up to 100.0 due to missing cases.<br />
43.5<br />
61.4<br />
63.8<br />
56.5<br />
38.6<br />
36.2<br />
49.0<br />
74.6<br />
73.1<br />
51.0<br />
25.4<br />
26.9<br />
37<br />
136<br />
198<br />
132<br />
127<br />
140<br />
105<br />
157<br />
244<br />
263<br />
253<br />
290<br />
225<br />
245<br />
303<br />
221<br />
6.5 SOURCE OF MODERN METHODS OF CONTRACEPTION<br />
During the survey, information was also collected regarding the sources of supply of<br />
contraceptives. Table 6.5 shows that government health facility was the main source of<br />
supply for the permanent family planning methods. Almost all acceptors of male <strong>and</strong> 69<br />
percent of the female sterilization used the government health facility. However, about 23<br />
percent of the acceptors of female sterilization used private health facility. But in the case<br />
of IUD/Loop the method was mainly accepted from private facility (66 percent) than the<br />
government (16 percent) facility. However, 94 percent each of pill <strong>and</strong> condom users<br />
obtained these contraceptives from chemist or medical store.<br />
8
Table 6.5 SOURCE OF MODERN CONTRACEPTIVE METHODS<br />
Percentage distribution of current users of modern contraceptive methods by source, according to specific method,<br />
Ahmedabad district of Gujarat, RCH, 2002<br />
Source<br />
Percentage distribution of current<br />
users by source of supply<br />
Government/municipal hospital<br />
CHC/PHC<br />
<strong>Family</strong> planning/ RCH camp<br />
Private hospital<br />
Government doctor<br />
Private doctor<br />
Government nurse/ ANM<br />
Private nurse<br />
Medical shop/chemist<br />
Other<br />
Female<br />
sterilization<br />
23.6<br />
30.7<br />
14.6<br />
22.6<br />
0.0<br />
0.5<br />
0.0<br />
0.0<br />
0.0<br />
8.0<br />
Male<br />
sterilization<br />
92.4<br />
4.7<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
2.9<br />
IUD/<br />
Loop<br />
8.1<br />
8.1<br />
0.0<br />
65.8<br />
1.4<br />
10.5<br />
0.0<br />
5.2<br />
0.0<br />
0.8<br />
Pill<br />
0.3<br />
4.3<br />
0.0<br />
0.4<br />
0.0<br />
0.0<br />
0.7<br />
0.0<br />
93.9<br />
0.4<br />
Condom/<br />
Nirodh<br />
Number of users of modern method 205 (8) 43 62 66<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
0.0<br />
0.5<br />
0.0<br />
0.0<br />
0.3<br />
0.0<br />
0.0<br />
0.0<br />
94.9<br />
4.2<br />
6.6 SIDE-EFFECTS OF CONTRACEPTION AND SATISFACTION WITH<br />
CURRENT USE<br />
Table 6.6 summarizes the data on side-effects of the contraceptive methods being used,<br />
prior knowledge of possible side-effects <strong>and</strong> related aspects.<br />
Table 6.6 HEALTH PROBLEMS AND SATISFACTION WITH CURRENT USE OF CONTRACEPTIVES<br />
Percentage of women informed about side-effects, had side-effects, sought treatment, follow-up <strong>and</strong> satisfaction with<br />
the method by use of method, Ahmedabad district of Gujarat, RCH, 2002<br />
<strong>Health</strong> problem/type of treatment<br />
Type of method<br />
Female IUD/loop<br />
Pill<br />
Sterilization<br />
Women who were informed about all the available methods 13.5 - -<br />
Women who were informed about the side-effects before adoption of method 36.0 51.8 31.8<br />
Women who had side-effect/health problem due to use of method 11.3 6.9 16.6<br />
Type of health problems/side-effects*<br />
Weakness/ inability to work<br />
Body ache/ backache<br />
Cramps<br />
Weight gain<br />
Dizziness<br />
Nausea/vomiting<br />
Breast tenderness<br />
Irregular periods<br />
Excessive bleeding<br />
Spotting<br />
White discharge<br />
Women who sought treatment for the health problem 52.3 22.1 0.0<br />
Source of treatment<br />
Government health facility<br />
Private health facility<br />
Other<br />
9<br />
1.4<br />
8.5<br />
0.1<br />
0.5<br />
0.2<br />
0.4<br />
0.0<br />
0.3<br />
06<br />
0.6<br />
2.8<br />
5.0<br />
95.0<br />
0.1<br />
0.0<br />
5.4<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.6<br />
0.0<br />
1.0<br />
0.0<br />
1.0<br />
0.0<br />
100.0<br />
0.0<br />
Women who had follow-up visit by health worker after adoption of method 38.2 1.7 1.7<br />
Women who are satisfied with method of current use 98.9 100.0 83.8<br />
Number of current users 206 43 63<br />
The data reveal that 37 percent of current users were informed about side-effects<br />
before adopting the respective method. About half (52 percent) of the IUD users, 32<br />
percent pill user <strong>and</strong> 36 percent acceptors of female sterilization reported being informed<br />
15.4<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.7<br />
0.0<br />
0.0<br />
0.4<br />
0.0<br />
0.7<br />
0.0<br />
0.0<br />
0.0
about side-effects before adopting the method. About 11 percent of the women sterilized<br />
reported that they had suffered from some health problems after adopting the method.<br />
These percentages in the case of IUD/Loop users is seven <strong>and</strong> 17 among pill users. Those<br />
who adopted sterilization as a method of family planning mainly experienced problems<br />
like bodyache, weakness, white discharge etc. after its acceptance. Out of those who had<br />
health problems, slightly more than half (52 percent) of them sought treatment mainly<br />
from private health facility (95 percent) followed by government health facility (5<br />
percent). None of the women, using pills sought the treatment for their problem while 22<br />
percent of the IUD/loop users sought the treatments. About 38 percent of the sterilization<br />
users reported being visited by health worker after adoption of contraception while only<br />
two percent each of IUD <strong>and</strong> pill users reported follow-up visit by health worker. Further,<br />
majority of the current users were satisfied with the current use of contraceptives<br />
irrespective of method adopted.<br />
6.7 ADVICE ON CONTRACEPTION AND INTENTION TO USE FAMILY<br />
PLANNING IN THE FUTURE<br />
During the survey, all CMW who were not using contraceptives at the time of survey were<br />
asked about their future intention regarding the use of family planning method. This type<br />
of information would help family planning programme administrators in identifying<br />
potential groups of users <strong>and</strong> in providing the types of contraception that are likely to be in<br />
dem<strong>and</strong>.<br />
Table 6.7 gives the extent of coverage of family planning counselling <strong>and</strong> intention to<br />
use family planning methods in the future. Around 18 percent of the current non-users<br />
were advised by ANM/health worker to use contraceptives. This proportion was 22<br />
percent in rural areas as compared to 16 percent in urban areas. About 43 percent of the<br />
women reported that they were advised to accept IUD/loop followed by female<br />
sterilization (34 percent) <strong>and</strong> pills (21 percent). It is evident from the table that the health<br />
workers are promoting IUD/loop than other spacing methods. Nearly 36 percent of the<br />
current non-users intended to use contraceptives in future. This percentage is found more<br />
in rural areas (43 percent) than urban areas (34 percent).<br />
Almost 80 percent of the women intend to accept female sterilization in the future.<br />
Slightly more than one-tenth (13 percent) of women intend to use IUD in future. A higher<br />
percent of the women in rural areas (19 percent) than those in urban areas (11 percent)<br />
intend to accept IUD in future.<br />
10
Table 6.7 ADVISE ON CONTRACEPTIVE USE AND FUTURE INTENTION TO USE<br />
Percentage of current non-users* who were advised by the ANM/health worker to use contraceptives by suggested method, <strong>and</strong> who intend to use contraceptives in future by preferred method by selected<br />
background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Advice Future intention of method<br />
Total Residence Caste# Education St<strong>and</strong>ard of living index Availability of<br />
health facility in<br />
the village<br />
Rural Urban SC/ST Other Illiterate 0-9@<br />
years<br />
10 years &<br />
above<br />
Low Medium High No Yes<br />
Percentage of current non-users advised by ANM/health worker<br />
to use of contraceptive method 17.5 22.4 16.0 13.4 18.5 15.2 28.8 4.6 37.7 17.9 11.3 24.4 18.2<br />
Percentage distribution of women who were advised<br />
Female sterilization<br />
Male sterilization<br />
IUD/loop<br />
Pill<br />
34.4<br />
1.1<br />
43.1<br />
21.4<br />
83.1<br />
0.0<br />
16.9<br />
0.0<br />
14.5<br />
1.6<br />
53.8<br />
30.2<br />
Percentage of current non-users intended to use contraceptive in<br />
future 36.1 43.2 34.0 20.6 39.9 23.5 37.9 50.2 44.8 39.2 30.7 42.2 45.3<br />
Percentage distribution of women who Intend to use<br />
contraceptive in future by preferred method<br />
Female sterilization<br />
IUD/loop<br />
Pill<br />
Condom/Nirodh<br />
Other method<br />
80.3<br />
13.1<br />
1.6<br />
0.7<br />
4.4<br />
80.8<br />
19.2<br />
0.0<br />
0.0<br />
0.0<br />
80.1<br />
10.8<br />
2.2<br />
0.9<br />
6.0<br />
Number of non-users 244 55 189 48 196 87 91 66 32 101 111 37 (18)<br />
* Exclude women in menopause or those who have undergone hysterectomy<br />
# The total figure may not add to (N) due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
71.7<br />
7.3<br />
17.9<br />
3.1<br />
100.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
27.7<br />
0.0<br />
47.6<br />
24.7<br />
77.7<br />
14.7<br />
1.8<br />
0.8<br />
4.9<br />
90.3<br />
3.6<br />
0.0<br />
6.2<br />
91.2<br />
5.8<br />
3.0<br />
0.0<br />
0.0<br />
7.6<br />
0.0<br />
63.2<br />
29.2<br />
71.3<br />
27.3<br />
0.7<br />
0.7<br />
0.0<br />
25.4<br />
0.0<br />
54.2<br />
20.4<br />
82.9<br />
2.6<br />
1.8<br />
1.1<br />
11.7<br />
85.2<br />
0.0<br />
9.7<br />
5.1<br />
79.4<br />
16.3<br />
4.3<br />
0.0<br />
0.0<br />
17.3<br />
0.0<br />
42.3<br />
40.4<br />
79.0<br />
21.0<br />
0.0<br />
0.0<br />
0.0<br />
10.0<br />
3.8<br />
76.4<br />
9.8<br />
82.1<br />
2.5<br />
2.4<br />
1.8<br />
11.3<br />
87.2<br />
0.0<br />
12.8<br />
0.0<br />
71.2<br />
28.8<br />
0.0<br />
0.0<br />
0.0<br />
71.2<br />
0.0<br />
28.8<br />
0.0<br />
100.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
11
6.8 FUTURE FERTILITY INTENTION<br />
About 31 percent of<br />
CMW say that they do<br />
not want any more<br />
children. Similarly 24<br />
percent of the husb<strong>and</strong>s<br />
do not want additional<br />
children. In total 21<br />
percent of couples said<br />
that they do not want any<br />
more children. The<br />
couples wanting no more<br />
children is higher in rural<br />
areas than in urban areas.<br />
The percentage of<br />
women who desire the<br />
next child to be a boy is<br />
24 percent, which is high<br />
in rural areas than urban<br />
areas. Slightly higher<br />
percent of husb<strong>and</strong><br />
Percentage<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Figure 6.3:<br />
Fertility preferences among men <strong>and</strong> women<br />
Women<br />
31.2<br />
DLHS-RCH, 2002<br />
Men<br />
24.2<br />
Not desiring<br />
additional child<br />
Women<br />
23.7<br />
desire next child to be a boy. This suggests that there is a prevalence of son preference<br />
among the people.<br />
Men<br />
33.6<br />
Desiring<br />
additional child<br />
to be a Boy<br />
Women<br />
3.4<br />
Men<br />
1.0<br />
Desiring<br />
additional child<br />
to be a Girl<br />
Women<br />
5.5<br />
Men<br />
8.4<br />
Desiring next<br />
child after 2<br />
years<br />
Table 6.8 FUTURE FERTILITY INTENTION<br />
Percentage of eligible women* <strong>and</strong> men** desiring additional child by preference of sex <strong>and</strong> waiting time, according to<br />
selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Characteristics<br />
Total Residence Caste# Education of husb<strong>and</strong> St<strong>and</strong>ard of living<br />
index<br />
Rural Urban SC/ST Other Illiterate 0-9@ 10 years Low Medium High<br />
years & above<br />
Women reported<br />
Not desiring additional children<br />
Desiring the next child to be<br />
Boy<br />
Girl<br />
Desiring next child after two years<br />
Men reported<br />
Not desiring additional children<br />
Desiring the next child to be<br />
Boy<br />
Girl<br />
Desiring next child after two years<br />
31.2<br />
23.7<br />
3.4<br />
5.5<br />
24.2<br />
33.6<br />
1.0<br />
8.4<br />
41.2<br />
26.4<br />
2.1<br />
4.2<br />
45.0<br />
36.7<br />
3.0<br />
6.3<br />
28.3<br />
22.9<br />
3.8<br />
5.9<br />
15.8<br />
32.4<br />
0.2<br />
9.3<br />
45.7<br />
28.9<br />
4.4<br />
0.0<br />
24.0<br />
9.3<br />
6.4<br />
0.0<br />
27.6<br />
22.4<br />
3.2<br />
6.9<br />
23.8<br />
37.6<br />
0.2<br />
9.8<br />
44.2<br />
24.0<br />
1.5<br />
2.4<br />
NA<br />
NA<br />
NA<br />
NA<br />
23.2<br />
21.1<br />
1.6<br />
1.3<br />
NA<br />
NA<br />
NA<br />
NA<br />
25.2<br />
27.1<br />
8.4<br />
15.7<br />
NA<br />
NA<br />
NA<br />
NA<br />
47.1<br />
25.0<br />
3.5<br />
7.3<br />
48.6<br />
33.2<br />
5.2<br />
5.5<br />
32.5<br />
17.0<br />
0.8<br />
10.8<br />
15.4<br />
37.4<br />
0.2<br />
2.7<br />
25.5<br />
29.5<br />
5.8<br />
0.2<br />
22.5<br />
30.6<br />
0.1<br />
14.2<br />
Couples reported<br />
Not desiring additional children<br />
Desiring the next child to be<br />
Boy<br />
Girl<br />
Desiring next child after two years<br />
21.2<br />
20.5<br />
1.3<br />
1.4<br />
34.4<br />
16.6<br />
4.5<br />
4.6<br />
15.5<br />
22.2<br />
0.0<br />
0.0<br />
* Refers to women who are non-users <strong>and</strong> who are either menstruating or in amenorrhoea<br />
** Refers to men who are non-users<br />
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included NA: Not applicable<br />
22.4<br />
0.7<br />
7.0<br />
0.0<br />
20.9<br />
25.2<br />
0.0<br />
1.7<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
45.8<br />
24.4<br />
8.2<br />
8.4<br />
16.6<br />
23.3<br />
0.0<br />
0.0<br />
16.1<br />
16.1<br />
0.0<br />
0.0<br />
12
It is interesting to note that 22 percent of the couples reported desire for additional<br />
children, <strong>and</strong> the percentage reporting the same varies by caste <strong>and</strong> st<strong>and</strong>ard of living.<br />
About 21 percent couples who want another child say that they want the next child to be a<br />
son, only one percent say that they want a daughter, suggesting a strong son preference<br />
existing in the district, <strong>and</strong> this is not much affected by the background characteristics of<br />
the couples. A negligible percent of the couples in Ahmedabad reported their desire for<br />
spacing the next child. The desire for spacing the next child is reported by the couple in<br />
rural areas <strong>and</strong> those with low st<strong>and</strong>ard of living only.<br />
6.9 REASONS FOR DISCONTINUATION OF USE AND NON-USE OF<br />
CONTRACEPTIVES<br />
All CMW who had discontinued using contraceptive <strong>and</strong> those who had never used any<br />
method of contraceptive at the time of survey <strong>and</strong> were not pregnant were asked about the<br />
reasons for the same. Their response analyzed is summarized in Table 6.9. Seventy-four<br />
respondents discontinued the method in the surveyed households because most of them<br />
(37 percent) wanted to have a child, <strong>and</strong> the remaining were apprehensive of health<br />
problems like weakness/inability to work, body ache, etc.<br />
There were 129 current non-users in the surveyed households, of these 30 respondents<br />
were from rural areas <strong>and</strong> the remaining 99 were from urban areas. About 18 percent of<br />
them had fear of side-effects with the use of contraceptives or afraid of sterilization.<br />
Hence, they did not accept the method. These cases were more in the urban areas (22<br />
percent) than in rural (8 percent). <strong>Health</strong> does not permit, against religion were reported<br />
as other reasons for non-use of contraceptives by around two to four percent of the<br />
respondents.<br />
13
Table 6.9 REASONS FOR DISCONTINUATION OF USE AND NON-USE OF CONTRACEPTIVE METHODS<br />
Percent distribution of past users (current non-users) by reason for discontinuation of the current method <strong>and</strong> current non-users by reasons for non-use by selected background characteristics,<br />
Ahmedabad district of Gujarat, RCH, 2002<br />
Reason<br />
Total Residence Caste# Education St<strong>and</strong>ard of living index<br />
Rural Urban SC/ST Other Illiterate 0-9@ 10 years & Low Medium High<br />
years above<br />
Number of past users (current non-users) 74 (15) 59 (5) 68 (11) 41 (22) (7) (22) 45<br />
Reason for discontinuation<br />
Wanted child<br />
Method failed/became pregnant<br />
Supply not available<br />
Difficult to get method<br />
Weakness/inability to work<br />
Bodyache/backache<br />
Dizziness<br />
Irregular period<br />
Excessive bleeding<br />
Spotting<br />
White discharge<br />
Lack of pleasure<br />
Method was inconvenient<br />
Other<br />
37.0<br />
1.0<br />
0.3<br />
1.5<br />
9.9<br />
5.8<br />
1.7<br />
0.9<br />
10.2<br />
13.1<br />
5.4<br />
1.1<br />
1.3<br />
10.7<br />
49.3<br />
0.0<br />
0.0<br />
7.6<br />
0.0<br />
0.0<br />
8.2<br />
0.0<br />
0.0<br />
0.0<br />
22.7<br />
0.0<br />
0.0<br />
12.3<br />
33.8<br />
1.3<br />
0.4<br />
0.0<br />
12.5<br />
7.3<br />
0.0<br />
1.1<br />
12.8<br />
16.4<br />
1.1<br />
1.4<br />
1.6<br />
10.3<br />
50.3<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
3.0<br />
0.0<br />
0.0<br />
41.7<br />
0.0<br />
5.0<br />
0.0<br />
35.9<br />
1.1<br />
0.3<br />
1.7<br />
10.7<br />
6.3<br />
1.8<br />
0.7<br />
11.0<br />
14.1<br />
2.6<br />
1.2<br />
1.0<br />
11.5<br />
36.0<br />
0.0<br />
0.0<br />
10.0<br />
0.0<br />
0.0<br />
10.8<br />
0.0<br />
0.0<br />
0.0<br />
19.7<br />
0.0<br />
4.0<br />
19.6<br />
31.6<br />
1.9<br />
0.6<br />
0.0<br />
18.0<br />
0.0<br />
0.0<br />
1.0<br />
18.1<br />
23.8<br />
4.4<br />
0.0<br />
0.0<br />
0.7<br />
47.4<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
19.7<br />
0.0<br />
1.1<br />
1.0<br />
0.0<br />
0.0<br />
3.8<br />
2.4<br />
24.6<br />
17.7<br />
0.0<br />
0.0<br />
17.1<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
51.4<br />
0.0<br />
0.0<br />
13.9<br />
20.5<br />
0.0<br />
0.0<br />
0.0<br />
32.5<br />
0.0<br />
5.6<br />
1.8<br />
32.5<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
7.0<br />
47.7<br />
1.7<br />
0.5<br />
0.0<br />
0.5<br />
9.5<br />
0.0<br />
0.6<br />
1.0<br />
21.3<br />
1.4<br />
1.9<br />
2.1<br />
12.0<br />
Number of current Non-users 129 30 99 (24) 105 58 32 39 (22) 65 42<br />
Reason for non-use<br />
Against the religion<br />
Opposed to family planning<br />
Husb<strong>and</strong> opposed<br />
Other family members opposed<br />
Does not like existing methods<br />
Afraid of sterilization<br />
Cannot work after sterilization<br />
Worry about side-effects<br />
Cost too much<br />
<strong>Health</strong> does not permit<br />
Inconvenient to use method<br />
Difficult to become pregnant<br />
Other<br />
2.3<br />
0.9<br />
1.3<br />
0.3<br />
5.1<br />
8.4<br />
2.1<br />
10.4<br />
0.2<br />
4.4<br />
0.6<br />
3.1<br />
60.8<br />
7.6<br />
3.8<br />
0.0<br />
1.2<br />
0.0<br />
7.6<br />
3.9<br />
0.0<br />
0.0<br />
11.8<br />
0.0<br />
4.1<br />
59.9<br />
0.8<br />
0.0<br />
1.7<br />
0.0<br />
6.6<br />
8.7<br />
1.6<br />
13.5<br />
0.3<br />
2.2<br />
0.8<br />
2.8<br />
61.1<br />
0.0<br />
4.7<br />
2.4<br />
0.0<br />
0.0<br />
30.2<br />
2.6<br />
2.7<br />
0.0<br />
1.1<br />
0.0<br />
0.5<br />
55.8<br />
2.9<br />
0.0<br />
1.1<br />
0.4<br />
6.2<br />
3.5<br />
2.0<br />
12.2<br />
0.3<br />
5.1<br />
0.7<br />
3.7<br />
62.0<br />
3.9<br />
2.0<br />
1.5<br />
0.6<br />
3.6<br />
14.4<br />
2.0<br />
0.4<br />
0.3<br />
6.3<br />
0.4<br />
0.0<br />
64.5<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
8.0<br />
1.4<br />
10.6<br />
0.0<br />
0.7<br />
0.8<br />
5.4<br />
73.0<br />
1.9<br />
0.0<br />
2.2<br />
0.0<br />
11.3<br />
0.0<br />
2.9<br />
25.0<br />
0.3<br />
4.6<br />
0.6<br />
5.7<br />
45.6<br />
10.3<br />
0.0<br />
0.0<br />
1.7<br />
2.8<br />
10.3<br />
5.3<br />
0.0<br />
0.0<br />
10.5<br />
0.0<br />
0.0<br />
59.1<br />
0.0<br />
1.7<br />
0.9<br />
0.0<br />
3.2<br />
11.3<br />
0.0<br />
16.4<br />
0.5<br />
2.1<br />
0.0<br />
0.0<br />
63.9<br />
1.8<br />
0.0<br />
2.6<br />
0.0<br />
9.1<br />
3.1<br />
3.8<br />
6.6<br />
0.0<br />
4.8<br />
14.8<br />
9.4<br />
57.0<br />
@ Literate women with no years of schooling are also included<br />
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
14
6.10 UNMET NEED<br />
Table 6.10 subdivides unmet need for family planning into unmet need for spacing <strong>and</strong><br />
limiting. The total unmet need of family planning among women in this district is12<br />
percent. In other words, 12 percent of women did not want any more children or wanted<br />
more children, but after two or more years <strong>and</strong> were still not practicing any method of<br />
contraception. The proportion of unmet need was higher 19 percent in rural areas<br />
compared to urban areas (11 percent). Unmet need is high for limiting than for spacing.<br />
An almost equal percentage of husb<strong>and</strong>s (13 percent) reported unmet need for family<br />
planning, though a higher proportion of husb<strong>and</strong>s in the rural (24 percent) than those in the<br />
urban areas (9 percent) reported the same.<br />
About five percent of the couples reported unmet need for family planning. The<br />
unmet need for limiting is three percent <strong>and</strong> very negligible proportion is for spacing.<br />
Table 6.10 UNMET NEED<br />
Percentage of currently married women aged 15-44 years, their husb<strong>and</strong>s <strong>and</strong> both the partners with unmet need for family<br />
planning by selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Percentage with<br />
unmet need<br />
Total<br />
Limiting<br />
Spacing<br />
Total<br />
12.3<br />
9.9<br />
2.4<br />
Residence<br />
Rural Urban Illiterate<br />
18.6<br />
15.3<br />
3.4<br />
10.8<br />
8.6<br />
2.2<br />
17.0<br />
15.1<br />
1.9<br />
Education of<br />
husb<strong>and</strong><br />
0-9@<br />
Years<br />
9.4<br />
8.5<br />
0.9<br />
10 years<br />
& above<br />
10.5<br />
6.2<br />
4.3<br />
St<strong>and</strong>ard of living<br />
index<br />
Availability of<br />
health facility in<br />
the village<br />
Low Medium High No Yes<br />
Number of women 769 148 620 253 249 266 71 259 439 82 67<br />
Total<br />
Limiting<br />
Spacing<br />
12.6<br />
9.3<br />
3.3<br />
24.0<br />
21.0<br />
3.0<br />
9.1<br />
5.7<br />
3.4<br />
NA<br />
NA<br />
NA<br />
Number of men 404 95 308 NA NA NA 47 115 242 54 42<br />
Total<br />
Limiting<br />
Spacing<br />
5.0<br />
4.7<br />
0.3<br />
12.7<br />
11.2<br />
1.5<br />
3.1<br />
3.1<br />
0.0<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
19.2<br />
16.2<br />
3.0<br />
5.5<br />
5.5<br />
0.0<br />
2.4<br />
2.4<br />
0.0<br />
19.7<br />
16.9<br />
2.9<br />
5.0<br />
5.0<br />
0.0<br />
Number of couples 380 78 303 NA NA NA 39 108 233 41 37<br />
@ Literate women with no years of schooling are included.<br />
NA: Not applicable<br />
Note:<br />
Unmet need for limiting:<br />
The proportion of currently married women who are neither in menopause nor had hysterectomy nor are currently pregnant<br />
<strong>and</strong> do not want any more children but are currently not using any family planning method.<br />
Unmet need for spacing:<br />
The proportion of currently married women who are neither in menopause nor had hysterectomy nor are currently pregnant<br />
<strong>and</strong> who want more children but after two years or later <strong>and</strong> are currently not using any family planning method. The<br />
women who are not sure about whether <strong>and</strong> when to have next child are also included in unmet need for spacing<br />
Total unmet need: Unmet need for limiting <strong>and</strong> spacing<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
28.4<br />
21.3<br />
7.14<br />
29.9<br />
26.9<br />
3.0<br />
17.2<br />
12.7<br />
4.5<br />
9.2<br />
7.9<br />
1.4<br />
6.8<br />
6.4<br />
0.4<br />
10.9<br />
6.7<br />
4.2<br />
25.2<br />
19.4<br />
5.7<br />
36.6<br />
31.4<br />
5.2<br />
10.7<br />
10.2<br />
0.5<br />
7.7<br />
7.7<br />
0.0
CHAPTER - 7<br />
ACCESSIBILITY AND PERCEPTION ABOUT<br />
GOVERNMENT HEALTH SERVICES<br />
This chapter deals with the accessibility <strong>and</strong> the opinion of the currently married women<br />
about the services provided by government health workers. The quality of care offered by<br />
the government health programme as perceived by currently married women is also<br />
presented in this chapter.<br />
7.1 HOME VISIT BY HEALTH WORKERS<br />
In the rural areas, the health workers are deputed to visit each household in their work area<br />
to provide health care services to the community. In view of this, all the eligible women<br />
were asked whether any health worker had visited them at their home during the three<br />
months prior to the survey, the analysis of their responses is presented in Table 7.1.<br />
As can be seen from the Table<br />
7.1, 14 percent of the respondents<br />
reported that a health worker had<br />
visited them during the reference<br />
period. Same was reported by<br />
women belonging to different<br />
socioeconomic characteristics.<br />
Mainly ANM/LHV (97 percent)<br />
had visited them, followed by male<br />
health worker (10 percent) (Figure<br />
7.1). Most of them (78 percent)<br />
expressed satisfaction over the<br />
amount of time spent by the ANM.<br />
Similarly, 89 percent of them<br />
reported satisfaction with service/<br />
advice given by health workers.<br />
The level of satisfaction does not<br />
vary much by the socio-economic<br />
background of the CMW.<br />
TOTAL<br />
Figure: 7.1<br />
Home visits of health workers by<br />
residence<br />
ANM/LHV<br />
<strong>Health</strong> worker- male<br />
RURAL<br />
ANM/LHV<br />
<strong>Health</strong> worker- male<br />
URBAN<br />
ANM/LHV<br />
<strong>Health</strong> worker- male<br />
DLHS-RCH, 2002<br />
4.7<br />
10.1<br />
30.1<br />
96.5<br />
98.7<br />
95.9<br />
0 20 40 60 80 100<br />
Percent<br />
2
Table 7.1 HOME VISITS BY HEALTH WORKERS<br />
Percentage of currently married women aged 15-44 years who were visited by selected health worker <strong>and</strong> the background characteristics of the Respondents, Ahmedabad district of Gujarat,<br />
RCH, 2002<br />
Visit/satisfaction<br />
Total Residence Caste# Education St<strong>and</strong>ard of living index Availability of health<br />
facility in the village<br />
Rural Urban SC/ST Other Illiterate 0-9@ years 10 years Low Medium High No Yes<br />
& above<br />
Women who were visited by health<br />
worker at home during 3 months prior to<br />
survey 14.1 15.7 13.8 17.4 13.4 11.8 21.2 9.7 16.8 13.8 13.9 20.6 9.7<br />
Category of health worker<br />
ANM/LHV<br />
<strong>Health</strong> worker- male<br />
96.5<br />
10.1<br />
98.7<br />
30.1<br />
95.9<br />
4.7<br />
96.3<br />
27.2<br />
96.7<br />
6.1<br />
94.5<br />
13.7<br />
97.5<br />
11.4<br />
96.6<br />
3.4<br />
97.4<br />
21.4<br />
95.1<br />
5.5<br />
97.1<br />
10.6<br />
100.0<br />
39.8<br />
95.2<br />
4.8<br />
Women who said worker spent enough<br />
time with them 77.9 82.2 76.7 91.2 74.6 65.4 88.6 70.6 69.8 77.6 79.7 86.3 71.6<br />
Percentage of women who satisfied with<br />
service/advice given by health worker<br />
88.5 82.2 90.2 91.2 87.8 85.8 95.9 76.7 69.8 94.7 88.5 86.3 71.6<br />
Number of women 769 148 620 115 652 253 249 266 71 259 439 82 67<br />
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included<br />
3
7.2 MATTER DISCUSSED WITH HEALTH WORKERS<br />
The Table 7.2 shows percentage of women who were visited by health workers <strong>and</strong> those<br />
who visited government health facility <strong>and</strong> discussed the health <strong>and</strong> family planning or<br />
any matter with the health worker. About 63 pregnant women or women with children<br />
born after 1 st January 1999, 29 current users of contraceptives <strong>and</strong> 16 non-users women<br />
were visited by health workers at home. During home visits the health worker generally<br />
discussed with pregnant women or women with children born after 1st January 1999 on<br />
issues related to immunization, disease prevention, antenatal care <strong>and</strong> on other topics as<br />
can be seen from the table. On the other h<strong>and</strong> women currently using family planning<br />
reported that during the visit the health workers mainly discussed about disease prevention<br />
<strong>and</strong> immunization of children <strong>and</strong> to some extent on treatment of health problem. Nonusers<br />
of family planning methods were informed about immunization, disease prevention<br />
<strong>and</strong> antenatal care practice. More or less a similar kind of discussion took place when<br />
respondents themselves visited the government health facilities.<br />
Table 7.2: MATTERS DISCUSSED DURING CONTACT WITH HEALTH OR FAMILY PLANNING WORKER<br />
Percentage of women who were visited by health worker <strong>and</strong> those who visited government health facility in three months<br />
preceding the survey by the specific topics discussed with the health worker, Ahmedabad district of Gujarat, RCH, 2002<br />
Topic discussed<br />
During home visit<br />
<strong>Family</strong> planning<br />
Breastfeeding<br />
Supplementary feeding<br />
Immunization<br />
Nutrition<br />
Disease prevention<br />
Treatment of health problem<br />
Antenatal care<br />
Delivery care<br />
Child care<br />
Sanitation/cleanliness<br />
Oral rehydration<br />
Other<br />
Pregnant women or<br />
women with<br />
children born after<br />
1-1-1999<br />
Other women<br />
Current<br />
contraceptive<br />
users<br />
Current non<br />
users<br />
Number of women 63 29 (16) 109<br />
1.6<br />
0.6<br />
1.7<br />
57.8<br />
0.6<br />
17.1<br />
4.7<br />
16.6<br />
0.7<br />
4.4<br />
0.5<br />
0.0<br />
3.7<br />
1.8<br />
0.0<br />
0.0<br />
48.4<br />
0.0<br />
58.8<br />
10.8<br />
0.0<br />
0.0<br />
2.6<br />
1.1<br />
1.1<br />
5.5<br />
0.0<br />
0.0<br />
0.0<br />
82.6<br />
1.1<br />
5.3<br />
5.8<br />
38.7<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
5.1<br />
Total<br />
1.4<br />
0.3<br />
1.0<br />
58.9<br />
0.5<br />
26.6<br />
6.5<br />
15.3<br />
0.4<br />
3.3<br />
0.6<br />
0.3<br />
4.4<br />
During visit to health facility<br />
<strong>Family</strong> planning<br />
Supplementary feeding<br />
Immunization<br />
Disease prevention<br />
Treatment of health problem<br />
Antenatal care<br />
Postpartum care<br />
Child care<br />
Sanitation/cleanliness<br />
Other<br />
4.1<br />
2.0<br />
14.9<br />
5.2<br />
58.7<br />
17.6<br />
7.0<br />
7.5<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
1.4<br />
34.1<br />
60.0<br />
0.0<br />
1.3<br />
1.6<br />
1.6<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
1.8<br />
0.8<br />
6.4<br />
3.0<br />
43.8<br />
39.1<br />
3.0<br />
7.8<br />
0.8<br />
0.8<br />
Number of women (13) (16) 0 31<br />
Note: Percentages add to more than 100.0 due to multiple responses<br />
Note: Percentage may not be reliable as based on less than 25 cases.
7.3 VISIT TO GOVERNMENT HEALTH FACILITY<br />
The Table 7.3<br />
represents<br />
percentage of CMW<br />
who visited health<br />
facility by their<br />
residence <strong>and</strong><br />
availability of health<br />
facility in the village.<br />
It is clear from the<br />
table that majority<br />
(76 percent) of<br />
women who required<br />
treatment for their<br />
health problems had<br />
sought treatment<br />
from health facility.<br />
Only 10 percent of<br />
CMW had visited<br />
government health DLHS-RCH, 2002<br />
Percent<br />
facilities during the<br />
last three months before the survey <strong>and</strong> majority (86 percent) visited private facility.<br />
Among those who visited government health facility visited hospital <strong>and</strong> dispensary or<br />
PHC/SC (Figure 7.2).<br />
Table 7.3 VISIT TO HEALTH FACILITY<br />
Percentage of currently married women age 15-44 who visited health facility according to residence <strong>and</strong> availability of<br />
health facility in the village, Ahmedabad district of Gujarat, RCH, 2002<br />
<strong>Health</strong> facility<br />
Total<br />
2<br />
Residence<br />
Availability of health<br />
facility in the village<br />
Rural Urban No Yes<br />
Women who needed to visit health facility <strong>and</strong> visited 75.5 55.6 79.4 46.8 69.4<br />
Government health facility<br />
Government hospital/CHC/FRU/RH<br />
Government dispensary<br />
PHC<br />
Sub centre<br />
4.4<br />
3.5<br />
2.2<br />
0.3<br />
0.0<br />
0.0<br />
17.7<br />
2.1<br />
5.1<br />
4.0<br />
0.1<br />
0.1<br />
0.0<br />
0.0<br />
18.8<br />
0.0<br />
0.0<br />
0.0<br />
16.6<br />
4.3<br />
Private health facility<br />
Private hospital<br />
Private dispensary<br />
Private ISM hospital/dispensary<br />
Figure: 7.2<br />
Visits to government health facility by residence<br />
TOTAL<br />
Government hospital/ CHC/FRU/RH<br />
Government dispensary<br />
RURAL<br />
URBAN<br />
72.0<br />
13.8<br />
0.5<br />
Other 3.3 0.0 3.7 00 0.0<br />
Number of women 386 63 322 39 25<br />
7.4 CLIENT’S PERCEPTION OF QUALITY OF GOVERNMENT HEALTH<br />
SERVICES<br />
Utilization of services is an essential indicator reflecting the quality of services. Better<br />
quality of services would have a higher utilization rate <strong>and</strong> this is very important from the<br />
policy point because, unless clients are satisfied with the services provided by the<br />
government, efforts made by the government will be wasted. In order to assess the<br />
utilization of government health facilities, the CMW were asked whether they had visited<br />
any government health facility during the three months before the date of survey. It is<br />
PHC<br />
Sub centre<br />
Government hospital/ CHC/FRU/RH<br />
Government dispensary<br />
PHC<br />
Sub centre<br />
Government hospital/ CHC/FRU/RH<br />
Government dispensary<br />
PHC<br />
Sub centre<br />
0.3<br />
0.0<br />
0.0<br />
0.1<br />
0.1<br />
2.2<br />
2.1<br />
3.5<br />
4.0<br />
60.3<br />
19.8<br />
0.0<br />
4.4<br />
5.1<br />
73.6<br />
12.9<br />
0.5<br />
17.7<br />
0 10 20 30<br />
55.9<br />
25.3<br />
0.0<br />
65.0<br />
14.1<br />
0.0
interesting to note that majority of the women had positive opinion about the quality of<br />
services provided at the government health facility. However, about 32 percent<br />
of the women found the location to be inconvenient <strong>and</strong> 24 percent felt the waiting time<br />
very long <strong>and</strong> about 10 percent of them also opined that the staff is technically<br />
incompetent.<br />
Table 7.4 QUALITY OF GOVERNMENT HEALTH FACILITY<br />
Percentage of women who visited Government health facility <strong>and</strong> rated quality <strong>and</strong> availability of services, Ahmedabad<br />
district of Gujarat, RCH, 2002<br />
Quality of services<br />
1. The convenience of the health facility location<br />
2. Length of time spend towards waiting*<br />
3. Personal manner (courtesy, respect, sensitivity, friendliness) of the physician<br />
4. The technical skills <strong>and</strong> quality (thoroughness, carefulness, competence) of the<br />
physician<br />
5. Personal manner (courtesy, respect, sensitivity, friendliness) of nurse<br />
6. The technical skills <strong>and</strong> quality (thoroughness, carefulness, competence) of nurse<br />
7. Personal manner (courtesy, respect, sensitivity, friendliness) of other staff<br />
8. The technical skills <strong>and</strong> quality (thoroughness, carefulness, competence) of other staff<br />
9. The explanation of what was done to her<br />
10. Medical, surgical <strong>and</strong> diagnostic equipment<br />
11. General comfort<br />
3<br />
Poor<br />
32.0<br />
23.8<br />
4.6<br />
6.0<br />
5.9<br />
9.8<br />
5.4<br />
11.1<br />
3.8<br />
9.2<br />
3.5<br />
1 2 3<br />
Good Excellent<br />
* Poor indicate waiting long time. Good indicate average waiting time. Excellent indicate short waiting time<br />
7.5 REASONS FOR NOT VISITING THE GOVERNMENT HEALTH CENTRE<br />
Table 7.5 presents the reasons for not visiting government health center during the last<br />
three months before the survey. Eight percent women who needed to visit health facility<br />
visited government health facility. The percentage of women visiting government health<br />
facility is higher (11 percent) in rural areas as compared to eight percent in urban areas.<br />
Table 7.5 REASONS FOR NOT PREFERRING GOVERNMENT HEALTH FACILITY<br />
Percentage of currently married women age 15-44 who visited private health facility by reason for not preferring<br />
government health facility according to residence <strong>and</strong> availability of health facility in the village, Ahmedabad district of<br />
Gujarat, RCH, 2002<br />
Reasons for not visiting government<br />
<strong>Health</strong> facility<br />
Women who needed to visit health facility <strong>and</strong> visited government health<br />
facility<br />
Total<br />
Residence<br />
15.8<br />
48.4<br />
28.5<br />
34.0<br />
23.9<br />
41.4<br />
64.8<br />
64.8<br />
69.9<br />
63.5<br />
45.3<br />
Availability of<br />
34.0<br />
8.7<br />
44.2<br />
37.4<br />
33.8<br />
11.7<br />
7.7<br />
1.4<br />
6.0<br />
5.5<br />
6.0<br />
health facility in<br />
the village<br />
Rural Urban No Yes<br />
8.0 11.0 7.3 8.8 14.5<br />
Women who needed to visit health facility <strong>and</strong> visited private health facility 65.1 44.6 69.1 38.0 54.9<br />
Percentage distribution of women who visited<br />
private health facility by reason for not preferring government health<br />
facility<br />
Not conveniently located<br />
Time is not suited<br />
Poor quality of services<br />
Heavy rush<br />
Non-availability of doctors/health workers<br />
Rare availability of doctors/health workers<br />
Doctors/health workers do not examine properly<br />
Medicine are not/rarely given<br />
Medicine are of bad quality<br />
Referred by Government Doctor<br />
Other<br />
Number of women 386 63 322 39 25<br />
About 65 percent of women who needed to visit health facility had visited private<br />
health facility. Among those who visited private health facility, did so due to inconvenient<br />
timing of the government health center (24 percent), inconvenient location of the facility<br />
(23 percent) <strong>and</strong> poor quality of government services (17 percent). These reasons were<br />
23.0<br />
24.1<br />
17.4<br />
7.6<br />
0.8<br />
0.2<br />
3.3<br />
0.6<br />
5.3<br />
2.8<br />
14.8<br />
26.7<br />
13.7<br />
30.6<br />
4.0<br />
0.0<br />
0.0<br />
1.1<br />
5.7<br />
18.1<br />
0.0<br />
0.0<br />
22.5<br />
25.5<br />
15.8<br />
8.1<br />
0.9<br />
0.2<br />
3.6<br />
0.0<br />
3.7<br />
3.2<br />
16.7<br />
23.2<br />
15.4<br />
46.0<br />
7.7<br />
0.0<br />
0.0<br />
0.0<br />
0.0<br />
7.7<br />
0.0<br />
0.0<br />
30.6<br />
11.9<br />
14.0<br />
0.0<br />
0.0<br />
0.0<br />
2.3<br />
11.9<br />
29.3<br />
0.0<br />
0.0
considered to be some of the major reason for not preferring government services. Women<br />
also reported, poor quality of medicines, heavy rush etc. as some of the other reason for<br />
not visiting government health facility. In light of the expressed grievances, matter need to<br />
be seriously looked into <strong>and</strong> accordingly redressed.<br />
CHAPTER – 8<br />
REPRODUCTIVE HEALTH<br />
The RCH programme gives a lot of emphasis on promoting <strong>and</strong> encouraging healthy<br />
sexual behaviour among couples by various IEC activities. The DLHS-RCH made an<br />
attempt to collect information on awareness of reproductive tract infection (RTI)/sexually<br />
transmitted infection (STI) <strong>and</strong> prevalence of these problems along with certain specific<br />
socio-economic <strong>and</strong> demographic background that can pre-dispose individuals toward<br />
various dimensions of risk through self reported symptoms among married male <strong>and</strong><br />
female respondents in the sampled households. Information was also collected on the<br />
awareness of HIV/AIDS.<br />
8.1 AWARENESS ABOUT REPRODUCTIVE TRACT INFECTION (RTI)/<br />
SEXUALLY TRANSMITTED INFECTION (STI)<br />
In an attempt to assess whether couples had the right knowledge about RTI/STI <strong>and</strong><br />
HIV/AIDS, both males <strong>and</strong> females in each of the sampled households were asked if they<br />
were aware about it, its mode of transmission <strong>and</strong> curability. Their responses analyzed are<br />
presented in Table 8.1.<br />
Table illustrates that a<br />
higher proportion of males<br />
<strong>and</strong> females in urban areas<br />
(66 percent males <strong>and</strong> 40<br />
percent females) have heard<br />
about RTI/STI as compared<br />
to their rural counterparts<br />
(39 percent males <strong>and</strong> 23<br />
percent females) (Figure<br />
8.1). Males got to know<br />
about it through print media<br />
or through slogans or<br />
pamphlets or seen it on the<br />
wall hording (55 <strong>and</strong> 45<br />
percent respectively). In<br />
case of women,<br />
friends/relatives have been<br />
the major source of<br />
information (74 percent). A<br />
significant proportion of<br />
TOTAL<br />
RURAL<br />
URBAN<br />
Figure: 8.1<br />
Awareness of RTI/STI by sex <strong>and</strong> residence<br />
Female<br />
Male<br />
Female<br />
Male<br />
Female<br />
Male<br />
DLHS-RCH, 2002<br />
4<br />
23.1<br />
36.6<br />
38.9<br />
39.8<br />
59.5<br />
65.9<br />
0 20 40 60 80 100<br />
Percent
males came to know about it from TV (29 percent), while 13 percent of females came to<br />
know about RTI/STI through the same source. A negligible proportion of males (5<br />
percent) <strong>and</strong> females (1 percent) acquired knowledge about it from health workers.<br />
5
Regarding mode of transmission, about 70 percent of males in urban areas reported<br />
correctly that RTI/STI is transmitted through sexual intercourse while males in rural areas<br />
had less knowledge about it (56 percent). In case of females about 58 percent in urban<br />
areas reported sexual intercourse as the mode of transmission <strong>and</strong> in rural areas, this<br />
percentage is only 41. More females than males reported lack of personal hygiene as a<br />
cause of RTI/STI (39 <strong>and</strong> 28 percent respectively). A sizeable proportion of males (19<br />
percent) <strong>and</strong> females (25 percent) did not have the knowledge about mode of RTI/STI<br />
transmission. However, it is encouraging to note that majority of males (82 percent) <strong>and</strong><br />
females (78 percent) stated that RTI/STI is curable, about 18 percent females <strong>and</strong> 13<br />
percent males had no knowledge about curability of the infection. It is important to note<br />
that four percent each of male <strong>and</strong> female were of the notion that RTI/STI is not curable.<br />
Table 8.1 KNOWLEDGE OF REPRODUCTIVE TRACT INFECTION (RTI)/ SEXUALLY TRANSMITTED INFECTION (STI)<br />
Percentage of currently married women aged 15-44 years <strong>and</strong> their husb<strong>and</strong>s aware of RTI/STI by source of information,<br />
knowledge about mode of transmission <strong>and</strong> curability by sex <strong>and</strong> residence, Ahmedabad district of Gujarat, RCH, 2002<br />
Knowledge<br />
Male<br />
Female<br />
Total Rural Urban Total Rural Urban<br />
Percentage of respondents who are aware of RTI/STI £ 59.5 38.9 65.9 36.6 23.1 39.8<br />
Percentage of respondents* who are aware of RTI/STI by source<br />
Radio<br />
TV<br />
Newspaper/book/Magazine<br />
Slogan/ pamphlet/poster/ wall hoarding<br />
Doctor<br />
<strong>Health</strong> worker<br />
School teacher<br />
Community meeting<br />
Friends/relatives<br />
Other<br />
Percentage of respondents aware of mode of transmission<br />
Sexual intercourse<br />
Lack of personal hygiene<br />
Other<br />
Do not know<br />
Percent distribution of respondents who are aware of RTI/STI by<br />
knowledge about curability ¢<br />
Curable<br />
Not curable<br />
Do not know<br />
4.2<br />
28.8<br />
55.1<br />
45.1<br />
7.4<br />
5.0<br />
0.4<br />
2.0<br />
35.5<br />
2.0<br />
67.6<br />
28.4<br />
12.1<br />
18.5<br />
81.7<br />
4.3<br />
12.9<br />
3.8<br />
41.0<br />
10.8<br />
15.4<br />
2.6<br />
7.6<br />
0.0<br />
11.4<br />
29.4<br />
6.8<br />
56.1<br />
10.5<br />
3.6<br />
37.0<br />
82.7<br />
0.0<br />
17.3<br />
4.3<br />
26.6<br />
63.2<br />
50.5<br />
8.3<br />
4.5<br />
0.5<br />
0.3<br />
36.6<br />
1.2<br />
69.7<br />
31.7<br />
13.7<br />
15.1<br />
81.5<br />
5.0<br />
12.1<br />
0.1<br />
13.1<br />
13.1<br />
14.4<br />
3.9<br />
1.2<br />
0.2<br />
0.6<br />
73.7<br />
0.8<br />
55.9<br />
39.2<br />
21.2<br />
25.2<br />
77.8<br />
4.0<br />
18.1<br />
0.0<br />
3.6<br />
3.6<br />
8.8<br />
2.7<br />
7.0<br />
0.0<br />
3.4<br />
96.4<br />
0.0<br />
41.2<br />
45.9<br />
46.3<br />
3.4<br />
88.4<br />
4.2<br />
7.4<br />
0.1<br />
14.5<br />
14.5<br />
15.1<br />
4.1<br />
0.4<br />
0.2<br />
0.2<br />
70.6<br />
0.9<br />
58.0<br />
38.2<br />
17.8<br />
28.2<br />
76.4<br />
4.0<br />
19.6<br />
Number of respondents (aware of STI/RTI) 240 37 203 281 34 247<br />
* Total percent may add more than 100.0 due to multiple responses<br />
£ Based on all respondents. ¢ Total percentage may not add 100.0 due to missing cases<br />
8.2 PREVALENCE OF RTI/STI AMONG MALES AND FEMALES<br />
In order to assess the incidence of RTI/STI respondents were asked about the various<br />
symptoms of this infection, which they had experienced in the past. The male respondents<br />
were asked to report whether they ever experienced problems like discharge from penis,<br />
sore in genital area etc. The question addressed to female respondents are whether they<br />
experienced unusual vaginal discharge, pain during sexual intercourse, pain in lower<br />
abdomen etc. during the past three months preceding the survey. Attempts have also been<br />
made to unearth whether those suffering from any of the symptoms of RTI/STI sought<br />
treatment <strong>and</strong> the place from where treatment was sought. The results are presented in<br />
Table 8.2. From this it can be noticed that five percent of males had suffered from at least<br />
one symptom of RTI/STI whereas 14 percent of females suffered from abnormal vaginal<br />
discharge. The treatment seeking behaviour shows that 12 percent of females <strong>and</strong> 18<br />
percent of males sought treatment for their problem mainly from the private facility.<br />
6
Table 8.2 PREVALENCE OF SYMPTOMS OF RTI/STI AMONG WOMEN/ MEN<br />
Percentage of eligible women aged 15-44 having menstruation related problems <strong>and</strong> abnormal vaginal discharge, <strong>and</strong> their<br />
husb<strong>and</strong>s having symptoms of RTI/STI by residence, Ahmedabad district of Gujarat, RCH, 2002<br />
Prevalence of RTI/STI symptoms <strong>and</strong> treatment<br />
Total<br />
Residence<br />
Rural<br />
Urban<br />
*1. Number of women 78 (15) 63<br />
Women who reported having at least one menstruation related problem 12.7 13.3 12.6<br />
Women had at least one menstruation related problem 21.1 24.8 20.3<br />
Source of treatment<br />
<strong>Health</strong> facility<br />
Government<br />
Private<br />
ISM<br />
Other<br />
<strong>Health</strong> personnel<br />
Doctor<br />
ANM/Nurse/LHV/Trained Dai<br />
Other<br />
*2. Number of women 105 42 63<br />
27.5<br />
66.3<br />
1.2<br />
10.6<br />
95.6<br />
2.5<br />
1.9<br />
33.4<br />
50.0<br />
0.0<br />
41.6<br />
91.6<br />
0.0<br />
8.4<br />
25.8<br />
71.0<br />
1.6<br />
1.6<br />
96.7<br />
3.3<br />
0.0<br />
Women who reported having any abnormal vaginal discharge<br />
Women sought treatment for vaginal discharge<br />
13.7<br />
11.9<br />
28.1<br />
11.9<br />
10.2<br />
11.9<br />
Source of treatment<br />
<strong>Health</strong> facility<br />
Government<br />
Private<br />
ISM<br />
Other<br />
12.5<br />
62.3<br />
7.8<br />
17.5<br />
16.3<br />
44.6<br />
16.3<br />
22.8<br />
10.0<br />
73.9<br />
2.1<br />
14.0<br />
<strong>Health</strong> personnel<br />
Doctor<br />
ANM/Nurse/LHV/ Trained dai<br />
Other<br />
*3. Number of men (19) (8) (11)<br />
Men who reported having at least one symptom of RTI/STI<br />
Men had at least one symptom of RTI/STI <strong>and</strong> sought treatment<br />
Source of treatment<br />
<strong>Health</strong> facility<br />
Private<br />
Other<br />
<strong>Health</strong> personnel<br />
Doctor<br />
Other<br />
*1 Number of women who reported having at least one menstrual related problems<br />
*2 Number of women who reported having any vaginal discharge<br />
*3 Number of men who reported having at least one symptoms of RTI/STI problems<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
8.3 SYMPTOMS OF RTI/STI<br />
Table 8.3 shows that around 50 percent of the eligible women have at least one symptom<br />
of RTI/STI. The major problems reported are low backache (42 percent), followed by pain<br />
in lower abdomen (12 percent) <strong>and</strong> around eight percent reported itching over vulva. The<br />
percentage of women having most of the symptoms of the RTI/STI is higher in rural areas<br />
than in urban areas. The percentage of women having symptoms of RTI/STI is slightly<br />
higher for scheduled caste <strong>and</strong> scheduled tribes women <strong>and</strong> women belonging to medium<br />
or low st<strong>and</strong>ard of living in the district. The prevalence of symptoms of RTI/STI is more<br />
among illiterate women (53 percent) than literate women who have completed at least 10<br />
years of schooling (46 percent).<br />
7<br />
79.7<br />
9.2<br />
11.1<br />
4.7<br />
18.3<br />
54.9<br />
45.1<br />
54.9<br />
45.1<br />
60.9<br />
16.3<br />
22.8<br />
8.3<br />
36.9<br />
51.5<br />
48.5<br />
51.5<br />
48.5<br />
92.2<br />
4.5<br />
3.3<br />
3.5<br />
4.8<br />
73.6<br />
26.4<br />
73.6<br />
26.4
Table 8.3: SYMPTOMS OF RTI/STI<br />
Percentage of eligible women aged 15-44 having symptoms of RTI/STI by selected background characteristics Ahmedabad district of Gujarat, RCH, 2002.<br />
Symptoms<br />
Total Residence Caste# Education St<strong>and</strong>ard of living index<br />
Rural Urban SC/ST Other Illiterate 0-9@ 10 years Low Medium High<br />
years & above<br />
Women who reported at least one symptom of RTI/STI 50.5 61.2 47.9 73.0 46.6 53.3 52.1 46.3 56.2 55.7 46.5<br />
Symptoms<br />
Itching over vulva<br />
Boils/ulcers/warts around vulva<br />
Pain in lower abdomen<br />
Low backache<br />
Pain during sexual intercourse<br />
Bleeding after sexual intercourse<br />
Swelling in the groin<br />
Frequent/painful passage of urine<br />
Fever<br />
Some mass coming out of vagina<br />
Any involuntary escape of urine while<br />
coughing or sneezing<br />
8.0<br />
2.5<br />
12.4<br />
42.3<br />
3.5<br />
0.2<br />
0.8<br />
5.4<br />
3.9<br />
1.1<br />
1.6<br />
13.9<br />
4.8<br />
17.1<br />
51.3<br />
8.5<br />
0.5<br />
2.4<br />
10.5<br />
6.9<br />
3.3<br />
5.8<br />
6.6<br />
2.0<br />
11.3<br />
40.1<br />
2.3<br />
0.1<br />
0.5<br />
4.2<br />
3.2<br />
0.6<br />
0.6<br />
16.2<br />
3.5<br />
7.8<br />
69.6<br />
4.1<br />
0.0<br />
0.2<br />
5.9<br />
2.7<br />
2.1<br />
3.4<br />
6.6<br />
2.4<br />
13.3<br />
37.5<br />
3.4<br />
0.2<br />
0.9<br />
5.3<br />
4.1<br />
0.9<br />
1.3<br />
12.5<br />
2.0<br />
15.5<br />
45.3<br />
6.4<br />
0.0<br />
1.5<br />
7.0<br />
3.2<br />
1.4<br />
2.5<br />
7.0<br />
2.4<br />
9.7<br />
46.1<br />
2.6<br />
0.5<br />
0.2<br />
4.6<br />
3.8<br />
0.8<br />
2.0<br />
4.7<br />
3.2<br />
12.1<br />
35.8<br />
1.5<br />
0.0<br />
0.8<br />
4.6<br />
4.7<br />
1.0<br />
0.3<br />
13.8<br />
4.9<br />
17.7<br />
42.5<br />
7.8<br />
0.0<br />
1.8<br />
10.6<br />
6.4<br />
2.3<br />
6.7<br />
5.3<br />
1.9<br />
9.6<br />
51.6<br />
5.9<br />
0.3<br />
1.1<br />
3.1<br />
4.1<br />
1.4<br />
1.7<br />
8.7<br />
2.6<br />
13.3<br />
36.7<br />
1.4<br />
0.1<br />
0.5<br />
5.9<br />
3.3<br />
0.7<br />
0.7<br />
Number of women 769 148 620 115 654 253 249 266 71 259 439<br />
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases<br />
@ Literate women with no years of schooling are also included<br />
8
8.4 KNOWLEDGE OF HIV/AIDS<br />
The awareness of HIV/AIDS by<br />
certain selected background<br />
characteristics of respondents is<br />
presented in Table 8.4 More<br />
male (88 percent) than female<br />
respondents (60 percent) are<br />
aware of HIV/AIDS. Higher<br />
percent of male <strong>and</strong> female in<br />
the urban areas knew about<br />
HIV/AIDS as compared to their<br />
rural counterparts (Figure 8.2).<br />
Around 80 percent of the<br />
respondents reported TV as<br />
source of information (both<br />
males <strong>and</strong> females). The other<br />
source of information as<br />
reported by males were slogan<br />
(64 percent), print media (55<br />
TOTAL<br />
RURAL<br />
URBAN<br />
Female<br />
Male<br />
Female<br />
Male<br />
Female<br />
Male<br />
DLHS-RCH, 2002<br />
Figure: 8.2<br />
Knowledge of HIV/AIDS by sex <strong>and</strong><br />
residence<br />
percent) <strong>and</strong> friends/relatives (25 percent) whereas in case of females, friends (51 percent)<br />
had been the other major source in the campaign for communicating awareness about the<br />
dreaded disease. A small proportion (6 percent) of males reported doctors as the source of<br />
knowledge, the same was reported by only three percent of females. <strong>Health</strong> workers are<br />
yet to take initiative for spreading awareness about HIV/AIDS.<br />
With regard to the knowledge about the mode of transmission of the virus, the table<br />
reflects that most of the males (97 percent) <strong>and</strong> females (73 percent) knew that sexual<br />
intercourse with infected person is one of the major mode of transmission. The other<br />
modes reported were use of un-sterilized or infected needles (41 percent males <strong>and</strong> 29<br />
percent females). About 42 percent of males <strong>and</strong> 28 percent of females were also aware<br />
that it could be transmitted through infected blood. Few reported homosexual intercourse<br />
<strong>and</strong> mother to child as mode of transmission. This indicates that only sexual intercourse<br />
was considered as the major mode of acquiring the virus. With regard to curability, males<br />
had relatively better knowledge as compared to females. Half of the males knew correctly<br />
that the disease is not curable. The corresponding percentage for females is only 33<br />
percent. A matter of concern for everyone that emerges from the table is that nearly 37<br />
percent of females did not know anything about curability of HIV/AIDS as against the<br />
corresponding percentage of 19 for males.<br />
Though HIV/AIDS is not curable, there are preventive measures, which can avoid<br />
acquiring the virus. When the respondents were asked about their knowledge regarding<br />
preventive measures, majority of males (89 percent) <strong>and</strong> females (73 percent) reported that<br />
sex with only one partner as one of the preventive measures. Other preventive measure<br />
reported were checking blood prior to transfusion (37 percent male <strong>and</strong> 33 percent<br />
female), use of sterilized needles <strong>and</strong> syringes for injection (34 percent male <strong>and</strong> 27<br />
percent female) <strong>and</strong> using condom correctly during each sexual intercourse (32 percent<br />
male <strong>and</strong> 16 percent female). A very small percent of them had no knowledge about any<br />
such preventive measures. Further, the survey data reveals that 37 percent of males <strong>and</strong> 38<br />
percent of females had misconceptions that HIV/AIDS is transmitted by shaking h<strong>and</strong>s,<br />
hugging, kissing, sharing clothes, sharing kitchen utensils, mosquito bites, etc. This is an<br />
indication of the fact that in spite of having awareness, the respondents lack complete<br />
knowledge about the route <strong>and</strong> preventive care to avoid acquiring HIV/AIDS.<br />
Table 8.4 KNOWLEDGE OF HIV/ AIDS<br />
Percentage of currently married women age 15-44 years <strong>and</strong> their husb<strong>and</strong>s aware of HIV/ AIDS by source of knowledge,<br />
knowledge of mode of transmission <strong>and</strong> knowledge about curability by sex <strong>and</strong> residence, Ahmedabad district of Gujarat,<br />
RCH, 2002<br />
HIV/AIDS Male Female<br />
28.3<br />
59.8<br />
62.0<br />
67.3<br />
88.3<br />
96.5<br />
0 20 40 60 80 100<br />
Percent
Total Rural Urban Total Rural Urban<br />
Respondents are aware of HIV/AIDS 88.3 62.0 96.5 59.8 28.3 67.3<br />
Respondents* aware of HIV/AIDS by source<br />
Radio<br />
TV<br />
Newspaper/book/magazines<br />
Slogan/ pamphlet/posters/ wall hoarding<br />
Doctor<br />
<strong>Health</strong> worker<br />
School teacher<br />
Community meeting<br />
Relatives/friends<br />
Other<br />
14.2<br />
79.2<br />
55.1<br />
63.6<br />
6.2<br />
0.9<br />
0.6<br />
1.4<br />
24.9<br />
0.9<br />
4.1<br />
67.1<br />
37.7<br />
27.7<br />
5.7<br />
0.9<br />
2.4<br />
0.0<br />
21.9<br />
1.3<br />
16.2<br />
81.6<br />
58.5<br />
70.8<br />
6.3<br />
1.0<br />
0.3<br />
1.7<br />
25.5<br />
0.8<br />
3.0<br />
81.7<br />
33.1<br />
31.6<br />
3.2<br />
0.7<br />
2.5<br />
0.3<br />
50.5<br />
2.9<br />
5.3<br />
67.6<br />
9.7<br />
15.9<br />
5.9<br />
0.7<br />
0.0<br />
0.0<br />
52.9<br />
2.8<br />
2.8<br />
83.2<br />
35.4<br />
33.2<br />
2.9<br />
0.7<br />
2.8<br />
0.3<br />
50.2<br />
2.9<br />
Respondents* aware of HIV/AIDS by knowledge of<br />
mode of transmission<br />
Homosexual intercourse<br />
Heterosexual intercourse<br />
Needles/blades/skin puncture<br />
Mother to child<br />
Transfusion of infected blood<br />
Other<br />
Do not know<br />
7.6<br />
96.8<br />
41.2<br />
2.2<br />
41.9<br />
2.8<br />
3.1<br />
3.7<br />
92.1<br />
14.6<br />
0.4<br />
11.8<br />
2.7<br />
7.9<br />
8.4<br />
97.7<br />
46.5<br />
2.5<br />
47.9<br />
2.8<br />
2.1<br />
1.7<br />
73.3<br />
28.7<br />
8.8<br />
28.4<br />
2.4<br />
24.5<br />
0.0<br />
80.8<br />
13.8<br />
5.6<br />
27.2<br />
0.0<br />
19.2<br />
1.9<br />
72.5<br />
30.2<br />
9.1<br />
28.5<br />
2.7<br />
25.0<br />
Respondents* aware of preventive measures by type<br />
of measure<br />
Sex with only one partner<br />
Using condom correctly during each sexual<br />
intercourse<br />
Checking blood prior to transfusion<br />
Sterilize needles & syringes for injection<br />
Avoid pregnancy when having HIV/AIDS<br />
Other<br />
Do not know<br />
89.2<br />
31.6<br />
36.5<br />
34.4<br />
2.1<br />
12.9<br />
3.4<br />
81.5<br />
25.3<br />
12.8<br />
10.9<br />
0.4<br />
22.0<br />
7.0<br />
90.7<br />
32.8<br />
41.3<br />
39.1<br />
2.4<br />
11.1<br />
2.5<br />
73.0<br />
16.1<br />
33.0<br />
27.2<br />
8.4<br />
8.9<br />
23.1<br />
67.6<br />
2.2<br />
27.2<br />
13.8<br />
2.7<br />
10.1<br />
24.5<br />
73.6<br />
17.6<br />
33.6<br />
28.5<br />
8.9<br />
8.8<br />
22.9<br />
Respondents having misconception about HIV/AIDS 36.5 36.9 36.5 38.1 56.0 36.3<br />
Respondents* having misconceptions about mode of<br />
transmission by type of misconception<br />
Shaking h<strong>and</strong>s<br />
Hugging<br />
Kissing<br />
Sharing clothes<br />
Sharing kitchen utensil<br />
Stepping on urine/stool<br />
Mosquito, flea or bedbug bites<br />
8.1<br />
8.0<br />
16.5<br />
12.2<br />
18.1<br />
15.3<br />
30.9<br />
26.2<br />
26.7<br />
28.0<br />
27.4<br />
27.4<br />
32.0<br />
32.6<br />
4.5<br />
4.3<br />
14.3<br />
9.2<br />
16.3<br />
12.0<br />
30.5<br />
10.7<br />
11.8<br />
23.1<br />
11.9<br />
17.4<br />
11.5<br />
22.2<br />
12.5<br />
23.8<br />
44.1<br />
14.6<br />
32.2<br />
30.2<br />
34.8<br />
10.5<br />
10.5<br />
20.9<br />
11.7<br />
15.9<br />
9.6<br />
20.9<br />
Percentage distribution of respondents by knowledge<br />
about curability<br />
Curable<br />
Not curable<br />
Don’t know<br />
31.5<br />
49.9<br />
18.6<br />
30.5<br />
39.8<br />
29.7<br />
31.6<br />
51.9<br />
16.4<br />
29.8<br />
32.9<br />
37.4<br />
28.0<br />
23.8<br />
48.2<br />
29.9<br />
33.8<br />
36.3<br />
Number of respondents (aware of HIV/AIDS) 357 60 297 460 42 418<br />
* Total percent may add more than 100.0 due to multiple responses
CHAPTER - 9<br />
NUTRITIONAL STATUS AND ANAEMIA<br />
In the second round of DLHS-RCH information on weight of children under 6 years of<br />
age, <strong>and</strong> prevalence of iron deficiency, anaemia among children under 6 years (0-71<br />
months), adolescent girls age 10-19 years <strong>and</strong> pregnant women age 15-44 years, are<br />
collected. To facilitate assessment of prevalence of malnutrition among children, the<br />
weight of children under 6 years was measured using Uni-Scale, <strong>and</strong> haemoglobin level of<br />
children, adolescent girls <strong>and</strong> pregnant women were measured from the blood samples<br />
collected using the test-kit. This information’s were not collected during earlier (First<br />
round) RHS-RCH. The following paragraphs give details of methodology followed in<br />
blood sample collection<br />
9.1 METHODOLOGY<br />
Haemoglobin level provides an assessment of nutritional status. It is best measured by directly adding 20 µl of blood into<br />
Drabkin's solution.<br />
Equipment required<br />
1. Haemoglobin pipette<br />
2. Whatman No. 1 fitter paper 1.5 X 1.5 cm<br />
3. Disposable lancet<br />
4. Drabkin's solution<br />
5. Vortex mixer<br />
A measured amount of 20 µl of blood is accurately pipettes on to 1.5 X 1.5 cm<br />
whatman No. 1 filter paper. This is allowed to dry. The filter papers is marked with a<br />
lead pencil <strong>and</strong> kept in a polythene bag. The filter papers are dispatched or carried to the<br />
laboratory (Institute for Research in Reproduction (IRR), Mumbai) at a convenient time<br />
during the next six days. The blood is then eluted from the filter paper in 5 ml of<br />
Drabkin's solution for 2 hours. The tube is shaken well or preferably vortexed for about<br />
one minute <strong>and</strong> optical density measured by appropriate equipment.<br />
9.2 PROCEDURES<br />
A. Selection of skin puncture site: In adults skin puncture is conveniently made on the<br />
centre of the palmer surface of the terminal segment of any of the first three fingers.<br />
Puncturing the tip too close to the nail or the side of the finger is avoided. In children<br />
less than 4 months of age, heel puncture is preferred. The selected site must be warm<br />
<strong>and</strong> free of oedema <strong>and</strong> infections.
B. Preparation of site <strong>and</strong> method of puncture<br />
i. Reassure the patient. If it is extremely cold, warm the skin by vigorously rubbing<br />
site; this will increase the blood flow <strong>and</strong> facilitated sampling.<br />
ii. Clean the selected site with a sprit with a sprit swab <strong>and</strong> allow it to dry completely<br />
(alcohol causes haemolysis in the sample)<br />
iii. Hold the finger firmly in a dependent position <strong>and</strong> apply gentle pressure just<br />
proximal to the puncture site.<br />
iv. Use the lancet to puncture the skim at right angles to the direction of skin creases.<br />
This allows the blood to form a drop <strong>and</strong> prevents it from running into the skin<br />
creases.<br />
v. Wipe the first drop away.<br />
C. Collection of blood sample<br />
i. Quickly place the tip of the haemoglobin pipette over the puncture <strong>and</strong> fill upto 20<br />
µl level or slightly more.<br />
ii. Once collection is over, elevate the finger <strong>and</strong> apply sufficient pressure to stop<br />
further bleeding<br />
iii. Wipe the outside of the pipette with wet gauze. If the level of the blood is higher<br />
than the 20 µl mark, bring it to the exact 20 µl mark by absorbing the extra<br />
blood on a wet snab.<br />
iv. Deliver the blood from the haemoglobin pipette on to the whatman No. 1 filter<br />
paper.<br />
v. Allow to dry admark the filter paper with the identification number using a lead<br />
pencil. Air-dry <strong>and</strong> keep in a polythene bag which also bears the<br />
identifications number.<br />
D. Hb estimation<br />
i. Drop the filter paper into 5 ml drabkin's solution <strong>and</strong> allow it to st<strong>and</strong> for an hour.<br />
ii. Vortex it for one minute <strong>and</strong> measure the optical density at 540 nm using<br />
Drabkins solutions blank <strong>and</strong> a commercial st<strong>and</strong>ard.<br />
iii. Calculate the Hb in g/dl by using the following formula:<br />
OD of sample × Concentration of Hb st<strong>and</strong>ard<br />
Hb in g/dl =<br />
× dilution factor (251)<br />
OD of st<strong>and</strong>ard × 1000<br />
where Concentration of Hb st<strong>and</strong>ard = 60 mg/dl<br />
9.3 HAEMOGLOBIN RESPONSE RATE<br />
The superstitious belief of people towards giving blood sample <strong>and</strong> non-availability<br />
particularly, of children <strong>and</strong> adolescent girls at the time of survey have affected the<br />
response rate used in the estimation of haemoglobin level. Any interpretation <strong>and</strong><br />
conclusion drawn from the results shown in this chapter should take into consideration the<br />
response rate. To facilitate interpretation of results, haemoglobin response rate for<br />
Ahmedabad district for children (age 0-71 months), adolescent girls (age 10-19 years) <strong>and</strong><br />
pregnant women (age 15-44 years) are shown in Table 9.1
Table 9.1 HAEMOGLOBIN RESPONSE RATE<br />
Percentage of children (age 0–71 months), adolescent girls (age 10-19 years) <strong>and</strong> pregnant women (age 15-44 years),<br />
Ahmedabad district of Gujarat, RCH, 2002<br />
Respondent Response Rate Percent Invalid Number<br />
Children 52.7 2.4 624<br />
Adolescents girls 59.8 2.2 526<br />
Pregnant women* 75.9 2.3 58<br />
Total 57.0 2.3 1208<br />
*Non-pregnant women age 15–19 years considered as adolescent girls.<br />
9.4 WEIGHT FOR AGE OF CHILDREN<br />
In the RCH program, emphasis is given to the monitoring of the health <strong>and</strong> well being of<br />
children on the basis of their nutritional status. To assess the nutritional status of children,<br />
the weight of all children under 6 years of age living in the selected households was<br />
obtained. The weights of children are subsequently adopted for construction of<br />
anthropometrics index, weight-for-age, for comparison with the international reference<br />
population recommended by the World <strong>Health</strong> Organization. The weight-for-age index is<br />
expressed in st<strong>and</strong>ard deviation (SD) units (Z-scores) from the median of international<br />
reference population, as empirical evidence has shown that well-nourished children in all<br />
population groups for which data exist follow similar growth pattern. On the basis of this<br />
comparison, children who are below –2SD reference median are considered to be<br />
moderately undernourished <strong>and</strong> those below –3SD are considered severely<br />
undernourished. The analysis has to exclude children whose weight could not be<br />
measured either due to their non-availability at home or refusal by their parents/guardians.<br />
While making inference about the nutritional status of children on the basis of weight-forage<br />
index using the above said criteria, we have to keep in mind that the index value is<br />
sensitive to age misreporting of children which results in age heaping at preferred digits.<br />
Nutritional status of children under 6 years of age, classified by weight-for-age index according to the selected<br />
characteristics is depicted in Table 9.2. Out of all the children, who had been investigated in the Ahmedabad district of<br />
Gujarat, in 2002, in the second round of the DLHS-RCH survey, 33 percent of them are found to be underweight, while<br />
10 percent are severely underweight. This gives an unimpressive nutritional status of children. The condition worsens<br />
with the age of children, which is evident from the data that children in the age group of 6-71 months are largely<br />
underweight.<br />
The sex of the children <strong>and</strong> place of residence influence under-nourishment. More male (36 percent) than female (30<br />
percent) children are found under-nourished, similarly higher percent of the children in the rural areas are undernourished<br />
(41 percent) as compared to their urban counterparts (31 percent). Similarly, substantial differentiation is noticed in caste<br />
in the district. More number of SC/ST children are underweight (39 percent) as compared to other caste children (32<br />
percent). The proportion of undernourished children in terms of weight-for-age index shows inverse relationship with<br />
st<strong>and</strong>ard of living index, as it decreased from 44 to 25 percent of underweight children as the index passes from low to<br />
high category.
Table 9.2 WEIGHT FOR AGE OF CHILDREN<br />
Percentage of children (aged 0–71 months) classified as undernourished by weight for age anthropometric index of<br />
nutritional status, according to selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002<br />
Background characteristic<br />
Age of child (in months)<br />
0–5<br />
6–11<br />
12–23<br />
24–47<br />
48–71<br />
Birth order<br />
1<br />
2–3<br />
4–5<br />
6+<br />
Sex of Child<br />
Male<br />
Female<br />
Residence<br />
Rural<br />
Urban<br />
Religion<br />
Hindu<br />
Muslim<br />
Other<br />
Caste<br />
SC/ST<br />
Other<br />
Mother’s education<br />
Percentage below<br />
–3 SD<br />
Weight-for-age<br />
-<br />
5.7<br />
10.0<br />
14.4<br />
11.1<br />
11.0<br />
8.7<br />
12.5<br />
20.0<br />
11.4<br />
9.1<br />
14.9<br />
9.3<br />
10.3<br />
3.8<br />
21.1<br />
10.9<br />
10.2<br />
16.3<br />
Illiterate<br />
0–9 years 2<br />
12.7<br />
1.7<br />
10 <strong>and</strong> above<br />
Other 3 11.5<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
19.0<br />
14.4<br />
5.7<br />
Number of<br />
Percentage below<br />
children<br />
–2 SD 1<br />
2.9<br />
20.0<br />
35.7<br />
35.1<br />
41.5<br />
31.5<br />
34.4<br />
27.5<br />
60.0<br />
36.0<br />
29.7<br />
40.5<br />
31.4<br />
33.4<br />
26.9<br />
36.8<br />
39.1<br />
32.0<br />
41.1<br />
35.5<br />
23.1<br />
30.8<br />
44.4<br />
42.3<br />
25.0<br />
35<br />
35<br />
70<br />
111<br />
135<br />
127<br />
183<br />
40<br />
(10)<br />
211<br />
175<br />
74<br />
312<br />
341<br />
26<br />
(19)<br />
64<br />
322<br />
129<br />
110<br />
121<br />
26<br />
63<br />
111<br />
212<br />
Total 10.4 33.2 386<br />
Note: The index is expressed in st<strong>and</strong>ard deviation units (SD) from the median of the International Reference<br />
Population.<br />
1<br />
Includes children who are below –3 SD from the International Reference Population median<br />
2<br />
Literate women with no year of schooling are also included<br />
3<br />
Women who were not present at the time of survey<br />
SC/ST: Scheduled Caste/Scheduled Tribe<br />
Table is based on unweighted cases<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
A similar pattern of inverse relationship also emerges with educational level of mothers. The proportion of underweight<br />
children decreased from 41 percent for illiterate mothers to 23 percent for mothers with at least ten years of completed<br />
education.
9.5 ANAEMIA AMONG CHILDREN, ADOLESCENT GIRLS AND PREGNANT<br />
WOMEN<br />
A minimum level of haemoglobin in the blood is necessary for transfer of oxygen from the<br />
lungs to different tissues <strong>and</strong> other organs of the body. Low level of haemoglobin in the<br />
blood characterizes anaemia <strong>and</strong> it has detrimental effects on the health of children,<br />
adolescent girls <strong>and</strong> pregnant women, in particular. Children aged 6-24 months are most<br />
vulnerable to anaemia <strong>and</strong> it can result in impaired cognitive performance, behavioural<br />
<strong>and</strong> motor development, coordination, language development <strong>and</strong> scholastic achievement,<br />
besides increasing morbidity from infectious diseases. Associated with physiological <strong>and</strong><br />
biological changes with age, adolescent girls do need an optimum level of haemoglobin to<br />
prepare themselves for children bearing in course of time. As a matter of fact the emerging<br />
medical sciences <strong>and</strong> the Government’s RCH Programme are recommending antenatal<br />
care right from the adolescent stage itself, instead of the conventional practice of<br />
beginning from conception. Anaemia among pregnant women results in increased risk of<br />
premature delivery <strong>and</strong> low birth weight.<br />
As anaemia is a serious health problem affecting nearly half of the population, DLHS-<br />
RCH undertook direct measurement of haemoglobin levels among children under 6 years<br />
of age, adolescent girls aged 10-19 years <strong>and</strong> pregnant women aged 15-44 years by<br />
collecting blood sample in the field using filter paper technique <strong>and</strong> these samples were<br />
sent to the Institute for Research in Reproduction (IRR), Mumbai, for ascertaining the<br />
level of haemoglobin using proper pathological procedures.<br />
On the basis of the measurement of haemoglobin level, children, adolescent girls <strong>and</strong><br />
pregnant women were classified as anaemic or not anaemic. Those identified in the<br />
anaemic group were further classified as suffering from mild, moderate <strong>and</strong> severe<br />
anaemia. The recommended level of haemoglobin for classifying pregnant women <strong>and</strong><br />
children (6-71 months) into not anaemic, mild, moderate <strong>and</strong> severe anaemic categories<br />
are a minimum of 11.0 g/dl, 8.0–10.9 g/dl, 5.0–7.9 g/dl <strong>and</strong> less than 5.0 g/dl respectively.<br />
Whereas for adolescent girls the recommended haemoglobin levels for the same categories<br />
are a minimum of 12.0 g/dl, 10.0-11.9 g/dl, 8.0-9.9 g/dl <strong>and</strong> less than 8.0 g/dl. Percentage<br />
distribution of children below 6 years <strong>and</strong> adolescent girls aged 10-19 years according to<br />
anaemia levels by selected characteristics, <strong>and</strong> for pregnant women aged 15-44 years by<br />
place of residence are presented in Table 9.3 through Table 9.5.<br />
Anaemia is a common problem amongst children in this district. It can be noted from<br />
Table 9.3 that 96 percent of the children under 6 years of age suffer from some level of<br />
anaemia. Of these, 60 percent are mildly anaemic <strong>and</strong> rest 36 percent are moderately<br />
anaemic. Moderate anaemia is very high amongst children below six months of age (44<br />
percent), followed by 24-71 months (43 percent), <strong>and</strong> about 28 percent of the children in<br />
the age group of 12-23 months are suffering from moderate anaemia. There was no<br />
systematic pattern of relationship between prevalence of anaemia <strong>and</strong> other background<br />
characteristics, such as, sex, religion, <strong>and</strong> caste/tribe.
Table 9.3 ANAEMIA AMONG CHILDREN<br />
Percentage of children (aged 0-71 months) classified as having iron-deficiency anaemia by selected background<br />
characteristics, Ahmedabad district of Gujarat, RCH, 2002.<br />
Background characteristics<br />
Age of child (in months)<br />
0–5<br />
6–11<br />
12–23<br />
24–47<br />
48–71<br />
Sex of child<br />
Male<br />
Female<br />
Birth order<br />
1<br />
2–3<br />
4–5<br />
6+<br />
Weight for age of child<br />
Normal<br />
Below –2 SD 1<br />
Below –3 SD<br />
Place of residence<br />
Rural<br />
Urban<br />
Religion<br />
Hindu<br />
Muslim<br />
Other<br />
Caste/tribe<br />
SC/ST<br />
Other<br />
Percentage of<br />
children with<br />
any anaemia<br />
94.4<br />
100.0<br />
98.1<br />
96.1<br />
94.9<br />
96.6<br />
95.8<br />
95.0<br />
96.1<br />
100.0<br />
100.0<br />
95.7<br />
97.3<br />
97.1<br />
98.4<br />
95.8<br />
96.5<br />
100.0<br />
84.6<br />
100.0<br />
95.5<br />
Mother’s education<br />
Illiterate<br />
95.3<br />
0-9 2<br />
99.0<br />
10 +<br />
Other 3 94.6<br />
95.7<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
98.1<br />
96.8<br />
95.3<br />
Percentage of children with<br />
anaemia<br />
Mild<br />
anaemia<br />
50.0<br />
72.4<br />
55.6<br />
53.4<br />
66.7<br />
61.6<br />
58.3<br />
63.0<br />
54.5<br />
70.3<br />
42.9<br />
60.7<br />
59.1<br />
55.9<br />
72.1<br />
57.3<br />
60.9<br />
73.7<br />
23.1<br />
69.1<br />
58.3<br />
Moderate<br />
Anaemia<br />
44.4<br />
27.6<br />
42.6<br />
42.7<br />
28.2<br />
35.0<br />
37.5<br />
32.0<br />
41.6<br />
29.7<br />
57.1<br />
35.1<br />
38.2<br />
41.2<br />
26.2<br />
38.5<br />
35.6<br />
26.3<br />
61.5<br />
30.9<br />
37.2<br />
Number of<br />
children<br />
Total 96.3 60.1 36.1 321<br />
Note: Haemoglobin level between 8.0-10.9 g/dl is mild anaemia, 5.0-7.9 g/dl is moderate anaemia <strong>and</strong> below 5.0 g/dl is<br />
severe anaemia.<br />
1<br />
Includes children who are below –3SD from the International Reference Population median<br />
2<br />
Literate women with no years of schooling are also included.<br />
3<br />
Women who were not present at the time of survey<br />
Table is based on unweighted cases<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
Different in prevalence of anaemia among the children of rural <strong>and</strong> urban is notices.<br />
Slightly more percent of the children in the urban areas were moderately anaemic (39<br />
percent) as compared to their counterpart in rural areas (26 percent). None of the children<br />
were severely anaemic.<br />
Prevalence of anaemia among adolescent girls of age 10-19 years by selected socioeconomic<br />
<strong>and</strong> demographic characteristics are shown in Table 9.4. It is real matter of<br />
concern that in the district, 303 out of a sample of 308 adolescent girls were having<br />
anaemia of different degrees, mild (28 percent), moderate (54 percent) <strong>and</strong> 18 percent of<br />
them were severely anaemic. Almost equal percent of the adolescents belonging to<br />
different religious group are anaemic. No systematic <strong>and</strong> major differences in the<br />
59.8<br />
57.1<br />
60.2<br />
73.9<br />
64.8<br />
66.3<br />
55.2<br />
35.5<br />
41.8<br />
34.4<br />
21.7<br />
33.3<br />
30.5<br />
40.1<br />
(18)<br />
29<br />
54<br />
103<br />
117<br />
177<br />
144<br />
100<br />
154<br />
37<br />
(7)<br />
211<br />
110<br />
34<br />
61<br />
260<br />
289<br />
(19)<br />
(13)<br />
55<br />
266<br />
107<br />
98<br />
93<br />
(23)<br />
54<br />
95<br />
172
prevalence of degrees of anaemia by residence, marital status <strong>and</strong> caste/tribe of the<br />
adolescents. Moderate to acute type of anaemia were more seen amongst educated girls.<br />
Twenty percent girls belonging to households with high st<strong>and</strong>ard of living were suffering<br />
from acute anaemia as against 18 percent of girls belonging to low <strong>and</strong> 13 percent of girls<br />
from medium st<strong>and</strong>ard of living households.<br />
Table 9.4 ANAEMIA AMONG ADOLESCENT GIRLS<br />
Percentage of adolescent girls (aged 10-19 years) classified as having iron-deficiency anaemia by degree of anaemia,<br />
according to selected background characteristics, Ahmedabad district of Gujarat, RCH, 2002.<br />
Background characteristic<br />
Age (in years)<br />
10–14<br />
15–19<br />
Marital status<br />
Currently married<br />
Not currently married<br />
Place of residence<br />
Rural<br />
Urban<br />
Religion<br />
Hindu<br />
Muslim<br />
Other<br />
Caste/tribe<br />
SC/ST<br />
Other<br />
Education<br />
Illiterate 1<br />
1–9<br />
10+<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
Percentage of<br />
adolescent girls with<br />
any anaemia<br />
100.0<br />
99.4<br />
94.7<br />
100.0<br />
98.0<br />
100.0<br />
99.6<br />
100.0<br />
100.0<br />
100.0<br />
99.6<br />
96.3<br />
100.0<br />
100.0<br />
100.0<br />
98.9<br />
100.0<br />
Percentage of adolescent girls with<br />
Mild<br />
anaemia<br />
22.7<br />
31.1<br />
21.1<br />
28.0<br />
31.4<br />
26.8<br />
28.0<br />
24.0<br />
26.7<br />
20.9<br />
28.7<br />
Moderate<br />
anaemia<br />
61.7<br />
48.9<br />
52.6<br />
54.3<br />
58.8<br />
53.3<br />
52.6<br />
64.0<br />
66.7<br />
58.1<br />
53.6<br />
Severe<br />
anaemia<br />
15.6<br />
19.4<br />
21.1<br />
17.6<br />
7.8<br />
19.8<br />
19.0<br />
12.0<br />
6.7<br />
20.9<br />
17.4<br />
Number of<br />
adolescent<br />
girls<br />
Total 99.7 27.6 54.2 17.9 308<br />
Note: Haemoglobin level between 10.0-11.9 g/dl is mild anaemia, 8.0-9.9 g/dl is moderate anaemia <strong>and</strong> below 8.0 g/dl<br />
is severe anaemia.<br />
1<br />
Literate women with no years of schooling are also included.<br />
SC/ST: Scheduled Caste/Scheduled Tribe<br />
Table is based on unweighted cases<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
Prevalence of anaemia among pregnant women aged 15-44 years by background<br />
characteristics are shown in Table 9.5. As outlined earlier in this section anaemia is<br />
classified into three categories - mild, moderate <strong>and</strong> severe on the basis of haemoglobin<br />
levels 8.0-10.9 g/dl, 5.1-7.9 g/dl <strong>and</strong> less than 5.0 g/dl respectively. The recommended<br />
haemoglobin count for classifying a pregnant woman as non-anaemic is 11.0 g/dl or more.<br />
25.9<br />
24.4<br />
36.8<br />
32.1<br />
32.2<br />
24.9<br />
55.6<br />
57.1<br />
46.1<br />
50.0<br />
54.0<br />
54.9<br />
14.8<br />
18.5<br />
17.1<br />
17.9<br />
12.6<br />
20.2<br />
128<br />
180<br />
(19)<br />
289<br />
51<br />
257<br />
268<br />
25<br />
(15)<br />
43<br />
265<br />
27<br />
205<br />
76<br />
28<br />
87<br />
193
Table 9.5 ANAEMIA AMONG PREGNANT WOMEN<br />
Percentage of pregnant women (age 15-44 years) classified as having iron-deficiency anaemia by degree of anaemia<br />
according to residence Ahmedabad district of Gujarat, RCH, 2002.<br />
Background characteristic<br />
Percentage of<br />
pregnant women<br />
with any anaemia<br />
Percentage of pregnant<br />
women with<br />
Mild<br />
anaemia<br />
Moderate<br />
anaemia<br />
Number of<br />
pregnant<br />
women<br />
Place of residence<br />
Rural<br />
Urban<br />
100.0<br />
97.2<br />
71.4<br />
58.3<br />
28.6<br />
38.9<br />
(7)<br />
36<br />
Total 97.7 60.5 37.2 43<br />
Note: Haemoglobin level between 8.0-10.9 g/dl is mild anaemia, 5.0-7.9 g/dl is moderate anaemia <strong>and</strong> below 5.0 g/dl is<br />
severe anaemia.<br />
Note: Percentage may not be reliable as based on less than 25 cases.<br />
In the district, almost all<br />
pregnant women in the<br />
sampled households were<br />
found to be anaemic.<br />
Among those anaemic<br />
pregnant women, 61 percent<br />
are mildly anaemic <strong>and</strong> 37<br />
percent are moderately<br />
anaemic. There were no<br />
cases of severe anaemia<br />
amongst pregnant women in<br />
the district (Figure 9.1).<br />
Urban women are more<br />
vulnerable to anaemia with<br />
39 percent of the urban<br />
women moderately anaemic<br />
as compared to 29 percent of<br />
moderately anaemic rural women. The whole analysis indicates that there is an urgent<br />
need to make people aware about the ill effect of anaemia <strong>and</strong> the need to control it<br />
through better nourishment. Only a healthy <strong>and</strong> well-nourished woman can give birth to a<br />
healthy child <strong>and</strong> in turn will help in making a healthy nation.<br />
9.6 IODIZATION OF SALT<br />
Percent<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Figure: 9.1<br />
Anaemia among children, adolescent girls <strong>and</strong><br />
pregnant women<br />
96.3 99.7 97.7<br />
60.1<br />
DLHS-RCH, 2002<br />
Consumption of salt fortified with iodine can prevent Iodine Deficiency Disorders, which<br />
are known to cause miscarriages, brain disorders, cretinism, <strong>and</strong> retarded psychomotor<br />
development. Under the Prevention of Food Adulteration Act, 1998, the minimum iodine<br />
content of edible salt is 30 parts per million (PPM) at the manufacturing level. A test kit<br />
was provided to each interviewer to measure the level of iodine content of salt consumed<br />
by the selected households. The test kit consists of stabilized starch solution, when a drop<br />
of which is put on edible salt it changes colour from light blue through dark violet as<br />
iodine level varies from 7 to 30 PPM. A confirmatory test is further carried out by putting<br />
a drop of acid-based solution on the starch based salt, if the colour does not change in the<br />
first test, the experimental result indicating the level of iodine content is finally recorded<br />
by matching the outcome of colour of the salt with that on the cover of the test kit.<br />
36.1<br />
0.0<br />
Children age 0-71<br />
months<br />
27.6<br />
54.2<br />
17.9<br />
Adolescent girls age<br />
10-19 years<br />
60.5<br />
37.2<br />
0.0<br />
Pregnant women aged<br />
15-44<br />
Any anaemia<br />
Mild aneamia<br />
Moderate anaemia<br />
Severe anaemia
Table 9.6 IODIZATION OF SALT<br />
Percentage distribution of households by degree of iodization of salt, according to selected background characteristics,<br />
Ahmedabad district of Gujarat, RCH, 2002<br />
Background Characteristic Not iodized 7 ppm 15 <strong>and</strong><br />
higher ppm<br />
Residence<br />
Rural<br />
48.4 31.0 16.4<br />
Urban<br />
27.2 26.5 44.4<br />
Missing<br />
4.2<br />
1.9<br />
Total<br />
percent<br />
100.0<br />
100.0<br />
Number of<br />
households<br />
198<br />
809<br />
Caste#<br />
SC/ST<br />
Other<br />
43.3<br />
29.9<br />
20.8<br />
27.7<br />
33.0<br />
40.1<br />
2.9<br />
2.3<br />
100.0<br />
100.0<br />
127<br />
871<br />
Education<br />
Illiterate<br />
0-9@ years<br />
10 <strong>and</strong> above<br />
49.7<br />
34.5<br />
21.0<br />
22.6<br />
32.3<br />
24.5<br />
24.0<br />
29.9<br />
53.6<br />
3.7<br />
3.3<br />
1.0<br />
100.0<br />
100.0<br />
100.0<br />
169<br />
415<br />
423<br />
St<strong>and</strong>ard of living index<br />
Low<br />
Medium<br />
High<br />
48.1<br />
41.0<br />
23.5<br />
37.1<br />
27.7<br />
25.6<br />
13.0<br />
29.8<br />
48.0<br />
1.8<br />
1.6<br />
2.9<br />
100.0<br />
100.0<br />
100.0<br />
Total 31.4 27.4 38.9 2.4 100.0 1007<br />
Note: ppm: Parts per million<br />
# The total figure may not add to (N) 100.0 due to don’t know <strong>and</strong> missing cases<br />
@ Literate person with no years of schooling are also included<br />
The percent distribution of households by degree of iodization of salt, according to<br />
background characteristics in Ahmedabad District, Gujarat, 2002 are shown in Table 9.6.<br />
It can be noticed that two-fifths of the households of this district (39 percent) use cooking<br />
salt that contains the minimum recommended 15 PPM or higher level of iodine <strong>and</strong> about<br />
31 percent households used salt that is not iodized at all. Use of minimum recommended<br />
iodized salt for cooking is used more by those in urban areas (44 percent), belonging to<br />
other caste (40 percent), literate with 10 <strong>and</strong> above years of schooling (54 percent) <strong>and</strong><br />
belonging to high st<strong>and</strong>ard of living (48 percent) compared to this counterpart in rural<br />
areas (16 percent), illiterate (24 percent) <strong>and</strong> belonging to poor family (13 percent).<br />
102<br />
307<br />
598
ANNEXURE - II<br />
PSU<br />
NO.<br />
PSU NAME BLOCK NAME NO. OF<br />
RESIDENTIAL<br />
HOUSEHOLD<br />
POPULATION<br />
SIZE<br />
1 KAMATALAV DHANDHUKA 148 828<br />
2 INGOLI DHOLKA 289 1591<br />
3 NAVAGAM VIRAMGAM 210 1007<br />
4 TRENT VIRAMGAM 544 2739<br />
5 FEDRA DHANDHUKA 490 2615<br />
6 DADHANA VIRAMGAM 475 2404<br />
7 KASINDARA DASKROI 1186 6500<br />
8 LIHODA DEHGAM 996 5539
ANNEXURE – II<br />
USF NO. TOWN/CITY WARD BLOCK NO. POPULATION SIZE<br />
NAME<br />
1.<br />
VASTRAPUR (VP)<br />
2 10 3619<br />
2. VEJALPUR (VP) 18 10 4385<br />
3. <strong>AHMEDABAD</strong> (CANTT) 2 10 4895<br />
4. GHATLODIYA (NP) 4 10 5562<br />
5. DHANDHUKA (NP) 2 40 10777<br />
6. <strong>AHMEDABAD</strong> (MC) 3 10 20232<br />
7. <strong>AHMEDABAD</strong> (MC) 10 10 29981<br />
8. KALI (NP) 1 20 29950<br />
9. <strong>AHMEDABAD</strong> (MC) 29 10 41090<br />
10. <strong>AHMEDABAD</strong> (MC) 12 10 47075<br />
11. <strong>AHMEDABAD</strong> (MC) 8 10 46315<br />
12. <strong>AHMEDABAD</strong> (MC) 41 10 48779<br />
13. <strong>AHMEDABAD</strong> (MC) 39 10 57604<br />
14. <strong>AHMEDABAD</strong> (MC) 36 10 67639<br />
15. <strong>AHMEDABAD</strong> (MC) 27 10 78442<br />
16. <strong>AHMEDABAD</strong> (MC) 24 10 73438<br />
17. <strong>AHMEDABAD</strong> (MC) 30 10 85706<br />
18. <strong>AHMEDABAD</strong> (MC) 18 10 80957<br />
19. <strong>AHMEDABAD</strong> (MC) 33 10 80158<br />
20. <strong>AHMEDABAD</strong> (MC) 23 10 98059<br />
21. <strong>AHMEDABAD</strong> (MC) 32 10 91360<br />
22. <strong>AHMEDABAD</strong> (MC) 40 10 86695<br />
23. <strong>AHMEDABAD</strong> (MC) 15 10 99001<br />
24. <strong>AHMEDABAD</strong> (MC) 26 10 112112<br />
25. <strong>AHMEDABAD</strong> (MC) 17 10 101465<br />
26. <strong>AHMEDABAD</strong> (MC) 37 10 116379<br />
27. <strong>AHMEDABAD</strong> (MC) 14 10 113793<br />
28. <strong>AHMEDABAD</strong> (MC) 43 10 105824<br />
29. <strong>AHMEDABAD</strong> (MC) 31 10 115821<br />
30. <strong>AHMEDABAD</strong> (MC) 16 10 139584<br />
31. <strong>AHMEDABAD</strong> (MC) 38 10 161349<br />
32. <strong>AHMEDABAD</strong> (MC) 38 10 161349