BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
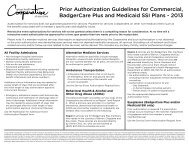
<strong>BadgerCare</strong> <strong>Plus</strong> & <strong>Medicaid</strong> <strong>SSI</strong> <strong>Provider</strong> <strong>Manual</strong> - GHC of Eau Claire May 2012<br />
Out-of-Network Referral Requests<br />
Any request for a member to obtain professional services from an out-of-network provider must be authorized by<br />
the GHC <strong>Health</strong> Management Department. Use the ‘Event Authorization for Out-of-Network Referral Form’<br />
located in Appendix A.<br />
Out-of-Practice-<strong>Group</strong> Referral Requests (as applicable)<br />
Out-of-Practice-<strong>Group</strong> referrals for <strong>BadgerCare</strong> <strong>Plus</strong> members to other GHC network providers must be<br />
authorized by the GHC <strong>Health</strong> Management Department. Use the ‘Event Authorization for Out-of-Practice <strong>Group</strong><br />
Referral Form’ located in Appendix A.<br />
Outpatient Care<br />
Prior authorization is required for:<br />
<br />
<br />
all home care services (excluding one maternity follow-up visit within 48 hours of hospital discharge for<br />
vaginal delivery or 96 hours of hospital discharge for C-section), and<br />
hospice services<br />
Use the ‘Request for Home <strong>Health</strong> Authorization Form located in Appendix A.<br />
Outpatient Laboratory<br />
Prior authorization is required for any genetic testing such as DNA testing except:<br />
when billed in conjunction with amniocentesis or;<br />
prenatal triple test or AFP: alpha-fetoprotein, hCG: human chorionic gonadotropin; and Estriol<br />
when provided in conjunction with Bone Marrow Biopsy<br />
Use the ‘Request for Service Event Authorization Form’ located in Appendix A.<br />
Outpatient Radiology<br />
Prior authorization is required for the following outpatient scans (i.e. not performed at the time of an emergency<br />
department visit, emergency department service, inpatient stay or observation stay)<br />
MRI<br />
PET Scans / SPECT Scans<br />
CT Scans / CTA Scans<br />
Cardiac CT Scans for calcium scoring<br />
Use the ‘Request for Service Event Authorization Form’ located in Appendix A.<br />
Outpatient Psychological Testing<br />
All authorization requests for outpatient psychological testing must be obtained prior to members receiving the<br />
service and can be requested from GHC’s <strong>Health</strong> Management Department. Use the appropriate authorization<br />
form(s) located in Appendix B.<br />
Outpatient Therapies<br />
Medically necessary short-term outpatient therapy (when a covered benefit) must be prescribed and monitored by<br />
a Primary or Specialty MD.<br />
Prior authorization is not required for the first six visits, including the initial evaluation, for Physical Therapy,<br />
Occupational Therapy, Pulmonary Therapy and Cardiac Therapy. If additional visits beyond the first six are<br />
needed, prior authorization is required before the seventh visit. Use the appropriate authorization forms located in<br />
Appendix A. For Cardiac Therapy use the Request for Service Event Authorization Form.<br />
[54]