BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>BadgerCare</strong> <strong>Plus</strong> & <strong>Medicaid</strong> <strong>SSI</strong> <strong>Provider</strong> <strong>Manual</strong> - GHC of Eau Claire May 2012<br />
Out-of-Network: The group of non-contracted physicians, providers, clinics, and facilities outside the GHC<br />
service area.<br />
Practice <strong>Group</strong>: An organized group of physicians that have joined together in a defined structure to facilitate the<br />
care of members between primary care and specialty care.<br />
Primary Care Clinic: A clinic contracted to provide primary care services to <strong>BadgerCare</strong> <strong>Plus</strong> and <strong>Medicaid</strong> <strong>SSI</strong><br />
members. The member must choose a primary care clinic for their care. A member may change their primary<br />
care clinic up to two (2) times per year. Each family member may have a different primary care clinic. A member<br />
may see any primary care provider in their primary care clinic.<br />
Primary Care <strong>Provider</strong>: A Wisconsin <strong>Medicaid</strong> Certified network provider who is contracted to provide primary<br />
care services to members. The contracted physician evaluates the member’s total health needs and provides<br />
personal medical care in one or more medical fields. When medically needed, he/she preserves continuity of care.<br />
He/she is also in charge of coordinating other provider health services and refers the member to other contracted<br />
<strong>BadgerCare</strong> <strong>Plus</strong> and <strong>Medicaid</strong> <strong>SSI</strong> providers as appropriate to the member. Primary care providers include the<br />
following: Family Practice, Internal Medicine, Pediatric, and OB/GYN physicians in addition to Nurse Practitioners<br />
and Nurse Midwives.<br />
Receipt Date: Determined by the date marked as received by the <strong>Health</strong> Management Department when<br />
received by mail or by the date received and date stamped by fax in the <strong>Health</strong> Management Department.<br />
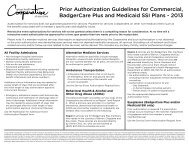
INPATIENT MANAGEMENT FACILITIES<br />
All hospital admissions, inpatient rehabilitation facility admissions (including inpatient pulmonary rehabilitation<br />
admissions), non-emergent intra-facility admissions (transfers), and long term care and skilled nursing facility care<br />
(including out-of-network 1 admissions) are reviewed for medical appropriateness of admission and continued<br />
stay. 2 Notification of an inpatient admission by the hospital can serve as a trigger for the <strong>Health</strong> Management<br />
nurse consultant to assess, in partnership with the contracted facility, the need for discharge planning or case<br />
management.<br />
Concurrent Review of inpatient management is a collaborative process with hospital staff and/or attending<br />
physicians to provide concurrent review by telephone or fax. On-site review may be necessary in some situations<br />
where the anticipated length of stay for the patient’s diagnosis is lengthened. The concurrent review process<br />
includes, but is not limited to, the following components:<br />
GHC nurse consultants provide concurrent review of medical records and are available to assist<br />
with members’ care management or discharge planning needs;<br />
When appropriate, the nurse consultant will work with members and families to explain health<br />
management decisions and facilitate discharge planning.<br />
Nurse Consultants use clinical decision support criteria to evaluate medical necessity and<br />
appropriateness of care;<br />
Potential quality issues identified during concurrent review are reported to the <strong>Group</strong> <strong>Health</strong><br />
Medical Director and if found to be significant, to the <strong>Group</strong> <strong>Health</strong> Quality Improvement<br />
Committee.<br />
1<br />
Out-of-network is defined as the group of non-contracted physicians, providers, clinics, and facilities outside the GHC<br />
service area.<br />
2<br />
Authorization for services does not guarantee payment for services. Payment for services is dependent on other nonmedical<br />
criteria such as the benefits associated with a member’s specific plan and eligibility issues.<br />
[47]