BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
BadgerCare Plus & Medicaid SSI Provider Manual - Group Health ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
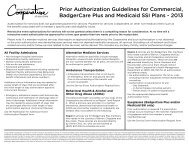
<strong>BadgerCare</strong> <strong>Plus</strong> & <strong>Medicaid</strong> <strong>SSI</strong> <strong>Provider</strong> <strong>Manual</strong> - GHC of Eau Claire May 2012<br />
Modifier Description GHC Claims Processing Policy<br />
26 Professional component Do not bill global fee in addition to a<br />
Professional Component<br />
TC Technical component Do not bill global fee in addition to a<br />
Technical Component<br />
32 Mandated services Not reimbursable<br />
47 Anesthesia by surgeon Does not impact reimbursement<br />
50 Bilateral procedure Reimbursed at Forward <strong>Health</strong> Fee<br />
51 Multiple procedures Highest dollar amount billed considered<br />
primary procedure and is reimbursed at<br />
100% of Forward <strong>Health</strong> fee. Secondary<br />
procedure reimbursed at 50% of Forward<br />
<strong>Health</strong> fee, Tertiary at 25% of Forward<br />
<strong>Health</strong> fee and all subsequent reimbursed<br />
at 13% of Forward <strong>Health</strong> fee.<br />
56 Preoperative management only Not covered (included in surgical care)<br />
57 Decision for surgery An E&M service that resulted in the initial<br />
decision to perform a major surgery (90<br />
day global) may be identified by adding<br />
modifier 57 to the appropriate E&M level.<br />
58 Staged or related procedure or service Does not impact reimbursement<br />
by the same physician during<br />
postoperative period<br />
59 Distinct procedural service Requires review. Documentation must<br />
support a different session, different<br />
procedure or surgery, different site or organ<br />
system, separate incision or excision,<br />
separate lesion or separate injury, etc.<br />
62 Two surgeons (i.e. co-surgery) Each surgeon reimbursed at Forward<br />
<strong>Health</strong> fee.<br />
63 Procedure performed on infants less Does not impact reimbursement<br />
than 4 kgs.<br />
66 Surgical team Does not impact reimbursement<br />
74 Discontinued outpatient hospital/ASC Does not impact reimbursement<br />
procedure after anesthesia<br />
administration. (For physician<br />
reporting of a discontinued procedure,<br />
see modifier 53)<br />
76 Repeat procedure by same physician Does not impact reimbursement<br />
77 Repeat procedure by another Does not impact reimbursement<br />
physician<br />
79 Unrelated procedure or service during Does not impact reimbursement<br />
the postoperative period<br />
80 Assistant surgeon MD Reimbursed at Forward <strong>Health</strong> fee.<br />
Assistants at surgery are covered when an<br />
assistant is considered medically necessary<br />
and appropriate. Documentation must<br />
support why assistant was needed.<br />
[27]