Thoracentesis and Pleural Effusions - - Clinical Departments
Thoracentesis and Pleural Effusions - - Clinical Departments
Thoracentesis and Pleural Effusions - - Clinical Departments
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Thoracentesis</strong> <strong>and</strong> <strong>Pleural</strong><br />
<strong>Effusions</strong><br />
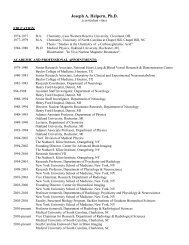
Fletcher T. Penney, MD, FHM<br />
Medical University of South Carolina<br />
Department of Medicine<br />
June 6, 2013 / Hospital Medicine Curriculum<br />
1 / 44
Outline<br />
Introduction<br />
Indications for <strong>Thoracentesis</strong><br />
Contraindications for <strong>Thoracentesis</strong><br />
How to Perform a <strong>Thoracentesis</strong><br />
How to Analyze <strong>Pleural</strong> Fluid<br />
2 / 44
Learning Objectives<br />
• To underst<strong>and</strong> which patients should undergo<br />
thoracentesis<br />
• To underst<strong>and</strong> contraindications to thoracentesis<br />
• To underst<strong>and</strong> potential complications of<br />
thoracentesis<br />
• To underst<strong>and</strong> how to interpret the results of pleural<br />
fluid studies<br />
3 / 44
Key Messages<br />
• Dullness to percussion, <strong>and</strong> the absence of of<br />
reduced tactile fremitus are the two most useful<br />
physical exam maneuvers to diagnose or exclude<br />
pleural effusions.<br />
• Patients with bilateral pleural effusions, who are<br />
afebrile <strong>and</strong> likely have CHF usually do not need a<br />
thoracentesis.<br />
• Use ultrasound.<br />
• Patients with a high probability of a transudative<br />
effusion only need protein <strong>and</strong> LDH checked.<br />
4 / 44
Outline<br />
Introduction<br />
Indications for <strong>Thoracentesis</strong><br />
Contraindications for <strong>Thoracentesis</strong><br />
How to Perform a <strong>Thoracentesis</strong><br />
How to Analyze <strong>Pleural</strong> Fluid<br />
5 / 44
Does My Patient Have a <strong>Pleural</strong> Effusion?<br />
6 / 44
Does My Patient Have a <strong>Pleural</strong> Effusion?<br />
A systematic review of the accuracy of the physical exam<br />
in the diagnosis of pleural effusion by Wong et al.<br />
evaluated<br />
• percussion<br />
• auscultatory percussion<br />
• breath sounds<br />
• chest expansion<br />
• tactile vocal fremitus<br />
• vocal resonance<br />
• crackles<br />
• pleural friction rub<br />
Wong (2009)<br />
7 / 44
Does My Patient Have a <strong>Pleural</strong> Effusion?<br />
• Dullness to percussion was the most accurate for<br />
making the diagnosis (LR+ 8.7)<br />
• Absence of reduced tactile vocal fremitus made<br />
effusion less likely (LR- 0.21)<br />
So, in patients with a low pre-test probability, the absence<br />
of reduced tactile fremitus may effectively rule out effusion<br />
without requiring a radiograph.<br />
Of note, when testing for fremitus having your patient say<br />
“boy” or “toy” is more accurate than “ninety-nine”.<br />
Wong (2009)<br />
8 / 44
Who Needs a <strong>Thoracentesis</strong>?<br />
• Patients with a pleural effusion. . .<br />
• . . . that is large enough to tap. . .<br />
• . . . without a known cause. . .<br />
• . . . <strong>and</strong> the effusion is at least 10mm thick by<br />
imaging.<br />
OR<br />
• Effusion of known etiology that has re-accumulated in<br />
order to remove fluid to improve symptoms.<br />
Light (2002)<br />
9 / 44
Who Doesn’t Need a <strong>Thoracentesis</strong>?<br />
It is likely appropriate to defer thoracentesis in a patient<br />
with:<br />
• Bilateral pleural effusions. . .<br />
• . . . with a history <strong>and</strong> exam suggesting CHF. . .<br />
• . . . without a fever. . .<br />
• . . . when the effusions resolve within three days.<br />
Light (2002)<br />
10 / 44
Outline<br />
Introduction<br />
Indications for <strong>Thoracentesis</strong><br />
Contraindications for <strong>Thoracentesis</strong><br />
How to Perform a <strong>Thoracentesis</strong><br />
How to Analyze <strong>Pleural</strong> Fluid<br />
11 / 44
Who Shouldn’t Undergo a <strong>Thoracentesis</strong>?<br />
• Elevated INR?<br />
• Thrombocytopenia?<br />
• Cellulitis overlying the target site?<br />
• Patients on mechanical ventilation?<br />
12 / 44
Elevated INR <strong>and</strong> Thrombocytopenia<br />
In a review of 1076 thoracenteses performed by trained<br />
providers, using ultrasound guidance, there was no<br />
difference in bleeding complications between patients with<br />
INR 1.5 (n = 267), INR > 2.0 (n =<br />
139), INR > 2.5 (n = 59), or INR > 3.0 (n = 32) .<br />
Similarly, no difference was noted in patients with<br />
platelets 150k).<br />
Patel <strong>and</strong> Joshi (2011)<br />
13 / 44
Elevated INR <strong>and</strong> Thrombocytopenia<br />
Consensus guidelines (2009 <strong>and</strong> 2012) from the<br />
Cardiovascular <strong>and</strong> Interventional Radiological Society of<br />
Europe classify thoracentesis as a low risk procedure for<br />
bleeding, <strong>and</strong> they recommend:<br />
• Check INR in patients on warfarin or with<br />
known/suspected liver disease<br />
• Check aPTT in patients on heparin<br />
• Do not routinely check platelets or hematocrit<br />
• Do not withhold aspirin/hold clopidogrel for five days<br />
(2012 guidelines)<br />
• Hold LMWH one dose before procedure<br />
Malloy et al. (2009)<br />
Patel et al. (2012)<br />
14 / 44
Elevated INR <strong>and</strong> Thrombocytopenia<br />
However, these guidelines did still recommend transfusing<br />
to a platelet count > 50,000 <strong>and</strong> giving FFP to INR < 2.0.<br />
Other authors have suggested this is not necessary.<br />
Malloy et al. (2009)<br />
Patel et al. (2012)<br />
15 / 44
Cellulitis<br />
If there is an infection of the skin <strong>and</strong>/or soft tissue<br />
overlying the target site, you should choose a different<br />
site.<br />
16 / 44
Mechanical Ventilation<br />
Traditional teaching was that thoracenteses should not be<br />
performed in patients who are on mechanical ventilation.<br />
However a study looking at 232 ultrasound guided<br />
thoracenteses performed on these patients with chest<br />
radiograph follow-up found that only 3 (1.3%) suffered a<br />
pneumothorax, <strong>and</strong> therefore received chest tubes.<br />
By comparison, average rates of pneumothorax have<br />
been reported from 6–18% without ultrasound <strong>and</strong> 1–5%<br />
with ultrasound, suggesting the procedure is relatively<br />
safe in this population.<br />
Daniels <strong>and</strong> Ryu (2011)<br />
Mayo et al. (2004)<br />
17 / 44
Outline<br />
Introduction<br />
Indications for <strong>Thoracentesis</strong><br />
Contraindications for <strong>Thoracentesis</strong><br />
How to Perform a <strong>Thoracentesis</strong><br />
How to Analyze <strong>Pleural</strong> Fluid<br />
18 / 44
How to Perform a <strong>Thoracentesis</strong><br />
The MUSC Library provides access to Procedures<br />
Consult, which includes information about:<br />
• Necessary equipment<br />
• Anatomical l<strong>and</strong>marks <strong>and</strong> considerations<br />
• Video demonstration of procedural technique<br />
• Procedure checklist<br />
http://www.library.musc.edu/page.php?id=1061<br />
19 / 44
How to Perform a <strong>Thoracentesis</strong><br />
Figure : Procedures Consult web site<br />
20 / 44
How to Perform a <strong>Thoracentesis</strong><br />
Key points:<br />
• Use ultrasound guidance<br />
• Do not withdraw more than 1000–1500 mL<br />
21 / 44
Post-Procedure Complications<br />
Important complications:<br />
• Pneumothorax<br />
• Bleeding<br />
• Reexpansion Pulmonary Edema (REPE)<br />
Rates of complications correlate with:<br />
• practitioner inexperience<br />
• failure to use ultrasonography<br />
• aspiration of large (> 1 L) fluid volume<br />
22 / 44
Pneumothorax<br />
Can occur from:<br />
• Puncture of the visceral pleura with air leak<br />
• Improper use of the stop-cock allowing influx of air<br />
• Drastic lowering of the intrapleural pressure<br />
• Shear trauma of the pleura<br />
Daniels <strong>and</strong> Ryu (2011)<br />
23 / 44
Pneumothorax<br />
Estimated rates range from 6–18% without ultrasound,<br />
<strong>and</strong> 1–5% with ultrasound<br />
Best practices can reduce rates of complication at an<br />
institution by:<br />
• St<strong>and</strong>ardizing the procedures performed<br />
• M<strong>and</strong>atory training<br />
• Limiting procedure to those who perform it regularly<br />
• Using real-time ultrasound<br />
Daniels <strong>and</strong> Ryu (2011)<br />
24 / 44
Pneumothorax<br />
Ultrasonography (90.9% sensitivity, 98.2% specificity) has<br />
been found to be better for the detection of<br />
pneumothoraces than chest radiography (50.2%<br />
sensitivity, 99.4% specificity) according to a<br />
meta-analysis.<br />
Additionally, the use of ultrasonography during the<br />
procedure has been shown to reduce the risk of a<br />
pneumothorax.<br />
Alrajhi et al. (2012)<br />
25 / 44
When to Check a Chest Radiograph?<br />
A chest radiograph is not m<strong>and</strong>atory after thoracentesis,<br />
however one should be obtained if air is aspirated into the<br />
syringe during the procedure, or there is loss of tactile<br />
fremitus over the upper part of the chest on the side of the<br />
procedure. Alternatively, ultrasound can be used to<br />
diagnose a pneumothorax.<br />
26 / 44
Bleeding<br />
As discussed previously, the risk of major bleeding from a<br />
thoracentesis is low, <strong>and</strong> the use of ultrasonography<br />
during the procedure can help minimize the risk of<br />
bleeding complications.<br />
27 / 44
Reexpansion Pulmonary Edema (REPE)<br />
REPE can occur when a lung is reexp<strong>and</strong>ed after multiple<br />
initial insults — pneumothorax, pleural effusion, or severe<br />
atelectasis.<br />
The mortality, pathophysiology, <strong>and</strong> risk factors of REPE<br />
are not clearly understood. In the setting of thoracentesis,<br />
it has been associated with removal of more than 1 to 1.5<br />
L of fluid.<br />
Sherman (2003)<br />
Feller-Kopman (2012)<br />
Maldonado <strong>and</strong> Mullon (2012)<br />
28 / 44
Reexpansion Pulmonary Edema (REPE)<br />
It has also been suggested that measuring pressure<br />
(manometry) during thoracentesis can allow the<br />
practitioner to stop removing fluid when the pressure is<br />
below – 20 cm H2O, though this is somewhat<br />
controversial <strong>and</strong> unproven.<br />
29 / 44
Outline<br />
Introduction<br />
Indications for <strong>Thoracentesis</strong><br />
Contraindications for <strong>Thoracentesis</strong><br />
How to Perform a <strong>Thoracentesis</strong><br />
How to Analyze <strong>Pleural</strong> Fluid<br />
30 / 44
Transudate or Exudate?<br />
The first step is to differentiate transudate from exudate. If<br />
your suspicion for a transudate is high, checking protein<br />
<strong>and</strong> LDH are all that are initially required.<br />
A transudative effusion is caused by unbalanced<br />
hydrostatic forces (high pressure), effectively “pushing”<br />
the fluid into the pleural space.<br />
An exudative effusion is caused by increased capillary<br />
permeability or lymphatic obstruction.<br />
31 / 44
Light’s Criteria<br />
Any of the following suggest that the fluid is an exudate:<br />
• Ratio of pleural-fluid protein to serum protein > 0.5<br />
• Ratio of pleural-fluid LDH to serum LDH > 0.6<br />
• <strong>Pleural</strong>-fluid LDH > 2/3 the upper limit of normal for<br />
serum<br />
Light’s Criteria (when combined) are 98% sensitive for an<br />
exudate, <strong>and</strong> 83% specific. If the clinical scenario strongly<br />
suggests transudate, but Light’s Criteria are positive, one<br />
can check the difference between the serum albumin <strong>and</strong><br />
the pleural albumin (analogous to a SAAG). A gradient of<br />
more than 1.2 g/dL suggests that the fluid is actually a<br />
transudate.<br />
Light (2002)<br />
32 / 44
Transudate<br />
If the fluid is consistent with a transudate, no further<br />
testing is generally necessary (<strong>and</strong> may in fact be<br />
misleading.) The most common etiologies for a<br />
transudate include:<br />
• Congestive heart failure<br />
• Cirrhosis<br />
• Nephrotic syndrome<br />
• Urinothorax<br />
• Myxedema<br />
• CSF leak to the pleura<br />
Light (2006)<br />
33 / 44
Exudate<br />
Exudative effusions can be caused by a variety of<br />
etiologies, <strong>and</strong> further testing is usually necessary to<br />
distinguish among them.<br />
34 / 44
Cell Count <strong>and</strong> Differential<br />
Bloody appearing fluid should prompt a hematocrit:<br />
• < 1% of peripheral hematocrit — nonsignificant<br />
• 1–20% of peripheral hematocrit — cancer, PE,<br />
trauma<br />
• > 50% of peripheral hematocrit — hemothorax<br />
Light (2002)<br />
35 / 44
pH<br />
A pH in the pleural-fluid less than 7.20 suggests the need<br />
for drainage of the fluid (empyema), usually with a chest<br />
tube. It has a been suggested that a pH in this range<br />
correlates with a life expectancy of around 30 days.<br />
Light (2002)<br />
36 / 44
Gram Stain <strong>and</strong> Culture<br />
Cultures show a higher yield if the bottles are inoculated<br />
at the bedside.<br />
Cultures for TB are rarely positive. High lymphocyte<br />
counts should prompt consideration of TB in the<br />
differential <strong>and</strong> an Adenosine deaminase or<br />
gamma-interferon may be helpful. ADA < 40 IU/L or<br />
gamma-interferon < 140 pg/mL make TB unlikely.<br />
Light (2002)<br />
Light (2006)<br />
37 / 44
Glucose<br />
Low glucose ( < 60 mg/dL) suggests a complicated<br />
parapneumonic or malignant effusion. Other potential<br />
causes include:<br />
• hemothorax<br />
• tuberculosis<br />
• rheumatoid arthritis<br />
• Churg-Strauss<br />
• paraonimiasis<br />
• lupus pleuritis<br />
Light (2002)<br />
38 / 44
LDH<br />
In addition to distinguishing between transudative <strong>and</strong><br />
exudative effusions, LDH can be useful as a marker of<br />
inflammation. Trending pleural fluid LDH levels can be<br />
useful for tracking resolution of the underlying process, as<br />
the LDH should normalize as the underlying pathology<br />
resolves.<br />
Light (2002)<br />
39 / 44
Other Tests<br />
• Cytology <strong>and</strong> flow cytometry — may be useful for<br />
diagnosing malignancy. Measuring tumor markers in<br />
the pleural fluid has not been proven reliable.<br />
• Amylase — pancreatic disease or esophageal rupture<br />
Light (2002)<br />
40 / 44
Bibliography I<br />
Alrajhi, K, Woo, MY, <strong>and</strong> Vaillancourt, C. Test<br />
characteristics of ultrasonography for the detection of<br />
pneumothorax: a systematic review <strong>and</strong> meta-analysis.<br />
Chest, 141(3):703–708, March 2012.<br />
Daniels, CE <strong>and</strong> Ryu, JH. Improving the safety of<br />
thoracentesis. Current opinion in pulmonary medicine,<br />
17(4):232–236, July 2011.<br />
Feller-Kopman, D. Point: should pleural manometry be<br />
performed routinely during thoracentesis? Yes. Chest,<br />
141(4):844–845, April 2012.<br />
Light, RW. <strong>Clinical</strong> practice. <strong>Pleural</strong> effusion. The New<br />
Engl<strong>and</strong> journal of medicine, 346(25):1971–1977, June<br />
2002.<br />
41 / 44
Bibliography II<br />
Light, RW. The undiagnosed pleural effusion. Clinics in<br />
chest medicine, 27(2):309–319, June 2006.<br />
Maldonado, F <strong>and</strong> Mullon, JJ. Counterpoint: should<br />
pleural manometry be performed routinely during<br />
thoracentesis? No. Chest, 141(4):846–8– discussion<br />
848–9, April 2012.<br />
Malloy, PC, Grassi, CJ, Kundu, S, Gervais, DA, Miller, DL,<br />
Osnis, RB, Postoak, DW, Rajan, DK, Sacks, D,<br />
Schwartzberg, MS, Zuckerman, DA, <strong>and</strong> Cardella, JF.<br />
Consensus Guidelines for Periprocedural Management<br />
of Coagulation Status <strong>and</strong> Hemostasis Risk in<br />
Percutaneous Image-guided Interventions. JVIR, 20(S):<br />
S240–S249, July 2009.<br />
42 / 44
Bibliography III<br />
Mayo, PH, Goltz, HR, Tafreshi, M, <strong>and</strong> Doelken, P. Safety<br />
of ultrasound-guided thoracentesis in patients receiving<br />
mechanical ventilation. Chest, 125(3):1059–1062,<br />
March 2004.<br />
Patel, IJ, Davidson, JC, Nikolic, B, Salazar, GM,<br />
Schwartzberg, MS, Walker, TG, <strong>and</strong> Saad, WA.<br />
Consensus Guidelines for Periprocedural Management<br />
of Coagulation Status <strong>and</strong> Hemostasis Risk in<br />
Percutaneous Image-guided Interventions. JVIR, 23(6):<br />
727–736, June 2012.<br />
Patel, MD <strong>and</strong> Joshi, SD. Abnormal preprocedural<br />
international normalized ratio <strong>and</strong> platelet counts are<br />
not associated with increased bleeding complications<br />
after ultrasound-guided thoracentesis. American<br />
Journal of Roentgenology, 197(1):W164–8, July 2011.<br />
43 / 44
Bibliography IV<br />
Sherman, SC. Reexpansion pulmonary edema: a case<br />
report <strong>and</strong> review of the current literature. J Emerg<br />
Med, 24(1):23–27, January 2003.<br />
Wong, CL. Does This Patient Have a <strong>Pleural</strong> Effusion?<br />
JAMA : the journal of the American Medical<br />
Association, 301(3):309, January 2009.<br />
44 / 44